PLEURAL DISEASE Pleural Diseases Pleural effusions Pleural malignancy



- Slides: 50
PLEURAL DISEASE
Pleural Diseases Ø Pleural effusions Ø Pleural malignancy Ø Hemothorax Ø Pneumothorax
The Mechanisms of Pleural Effusion Increased hydrostatic pressure (Cardiac failure) Ø Decreased oncotic pressure (Protein deficiency) Ø Decreased pleural cavity negative pressure (Atelectasis) Ø Increased permeability in microvascular circulation (İnfections, inflammation) Ø Impaired lymphatic drainage of pleural space (Tumor, fibrosis) Ø Transperitoneal route (Congenital defects, ascite) Ø
Symptoms Ø Chest pain (inspiratory) l Decreases when the fluid increases Dyspnea Ø Cough Ø Symptoms of the underlying disease Ø l l Fever Hemoptysis Weight loss. . . Physical signs Ø Ø Ø Ø No physical signs can be detected when the fluid is less than 300 ml İncreased size of the affected hemithorax İpsilateral restriction of chest wall motion VT absent Dullness (>300 -400 ml) Diminished breath sounds or inaudible Pleural friction rub
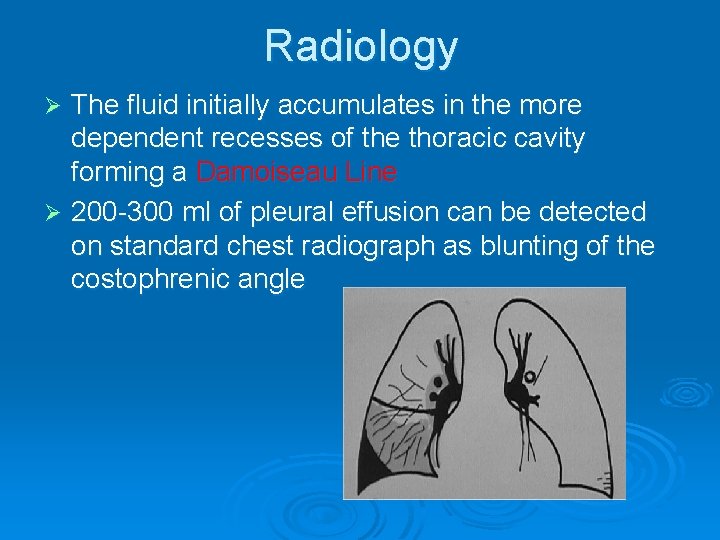
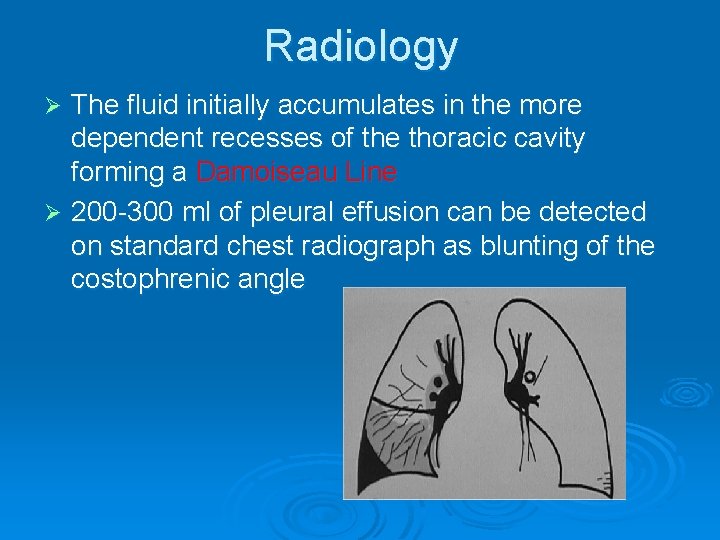
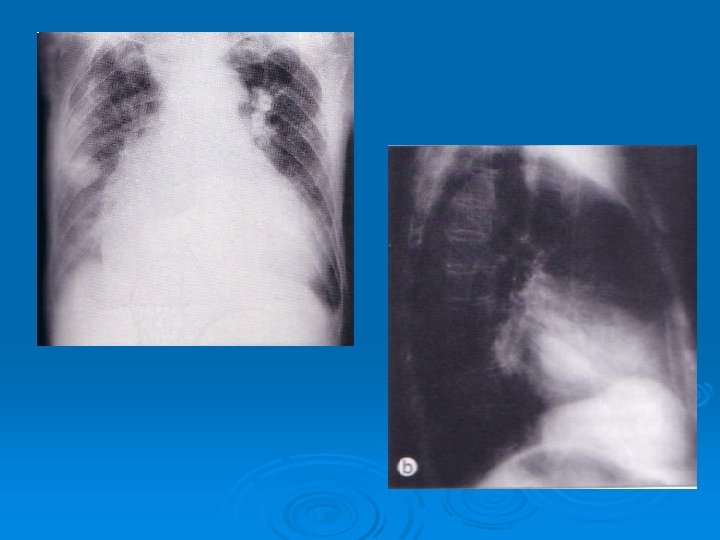
Radiology The fluid initially accumulates in the more dependent recesses of the thoracic cavity forming a Damoiseau Line Ø 200 -300 ml of pleural effusion can be detected on standard chest radiograph as blunting of the costophrenic angle Ø

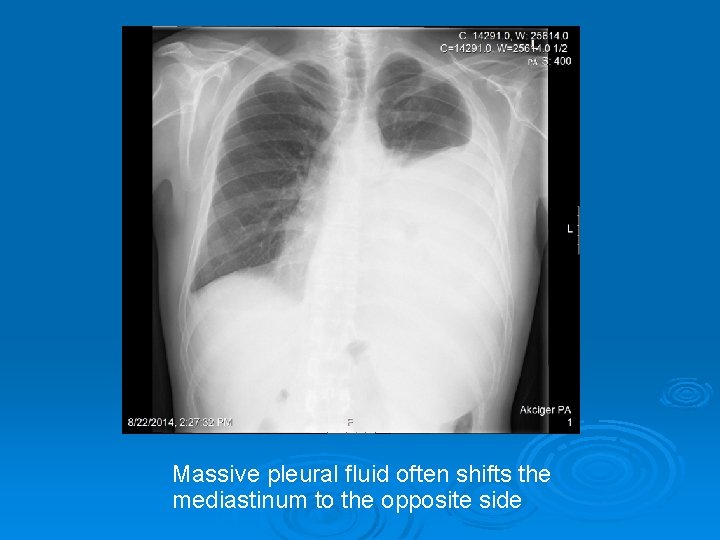
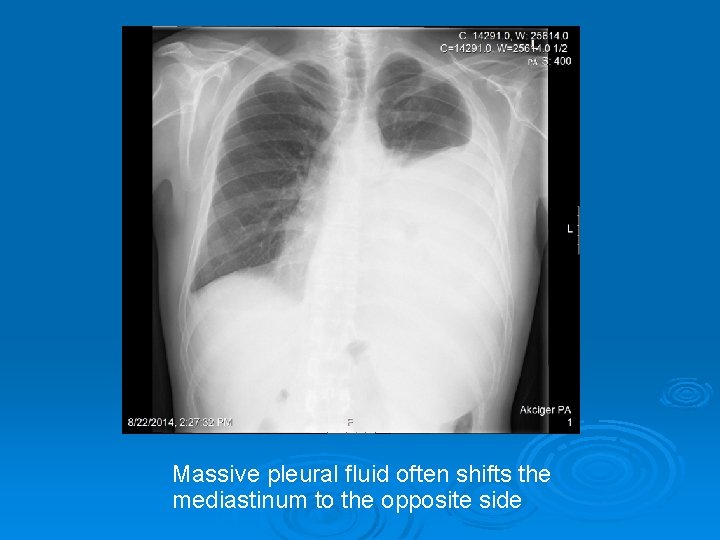
Massive pleural fluid often shifts the mediastinum to the opposite side
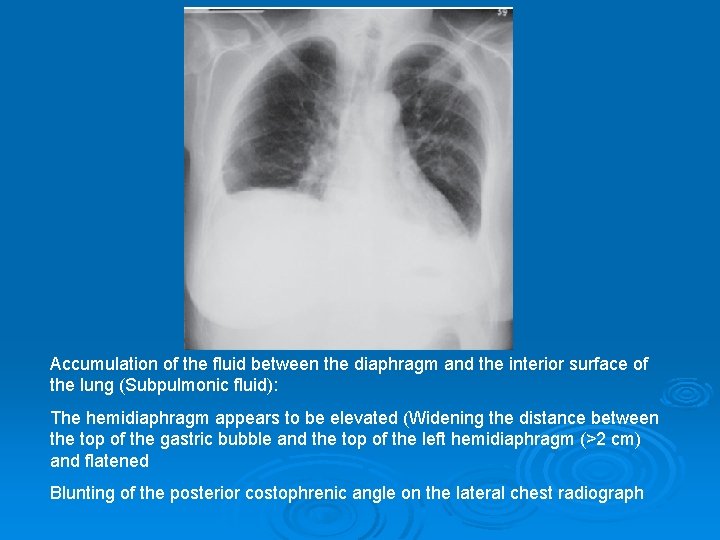
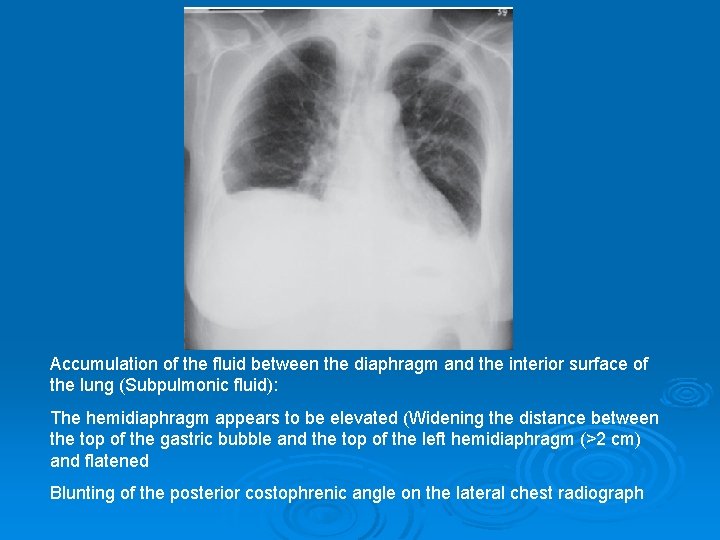
Accumulation of the fluid between the diaphragm and the interior surface of the lung (Subpulmonic fluid): The hemidiaphragm appears to be elevated (Widening the distance between the top of the gastric bubble and the top of the left hemidiaphragm (>2 cm) and flatened Blunting of the posterior costophrenic angle on the lateral chest radiograph
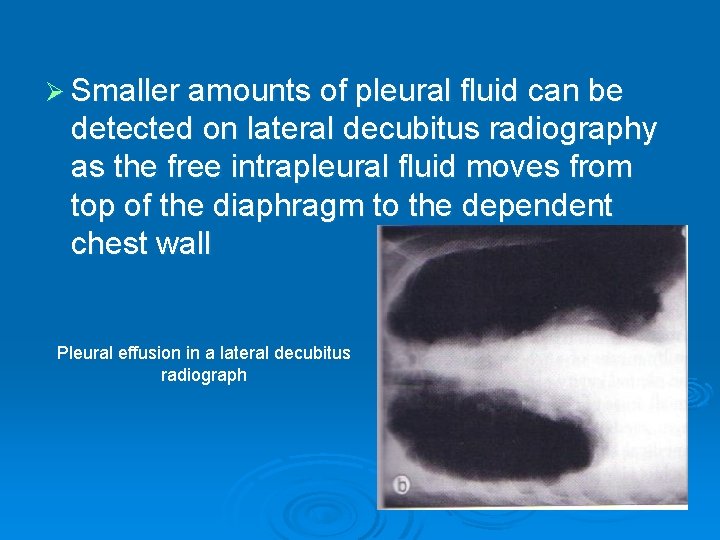
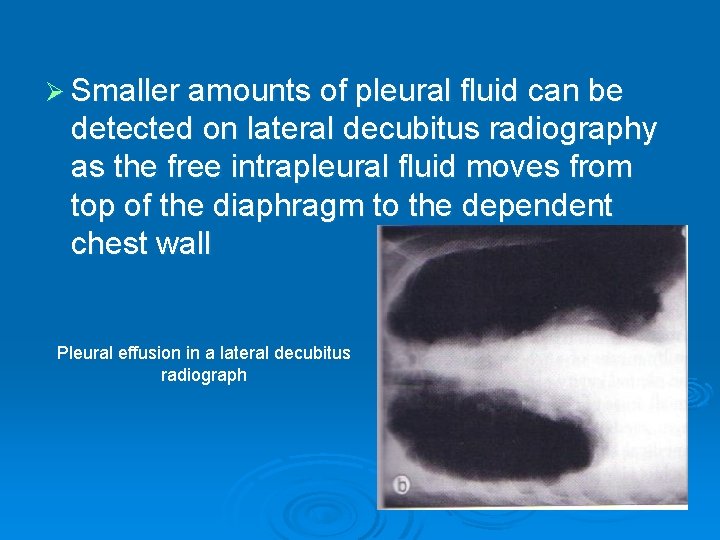
Ø Smaller amounts of pleural fluid can be detected on lateral decubitus radiography as the free intrapleural fluid moves from top of the diaphragm to the dependent chest wall Pleural effusion in a lateral decubitus radiograph
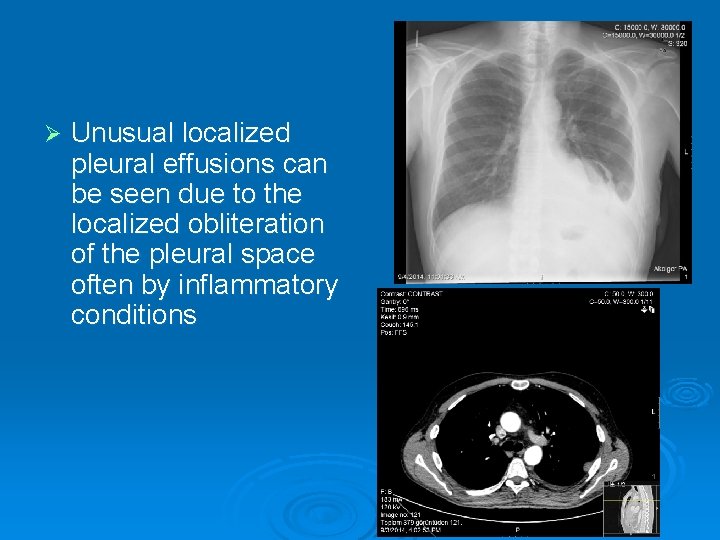
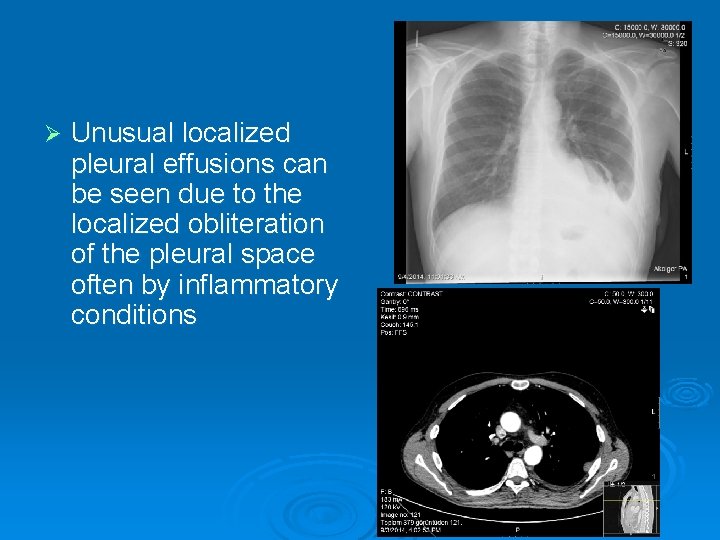
Ø Unusual localized pleural effusions can be seen due to the localized obliteration of the pleural space often by inflammatory conditions
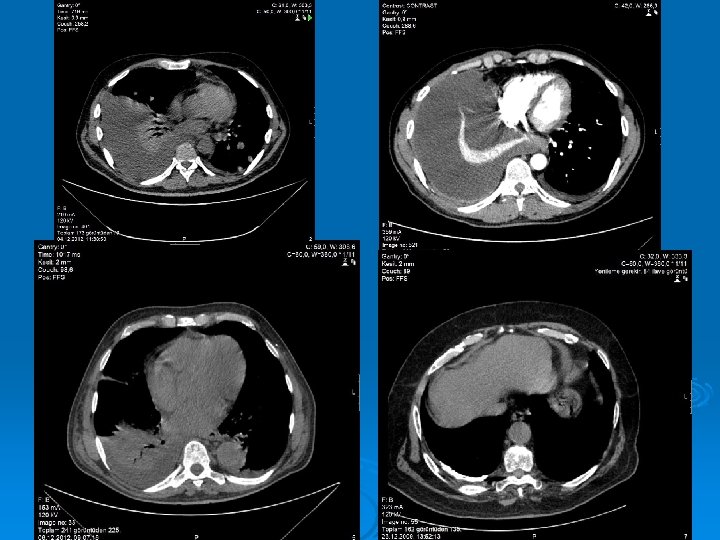
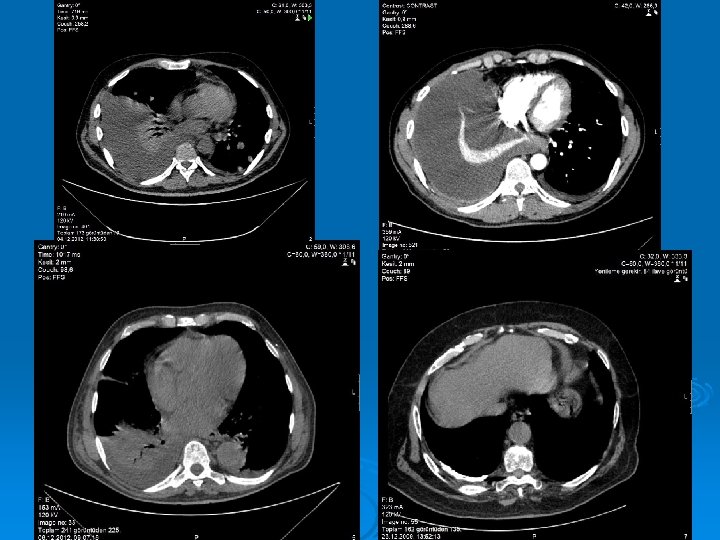
Ø Ultrasound is able to demonstrate smaller amounts of fluid as 100 ml Ø CT has similar sensitivity to ultrasound, not routine but can be performed to evaluate concomitant paranchymal lesions Ø CT is sensitive in identifying pleural thickening and calcification
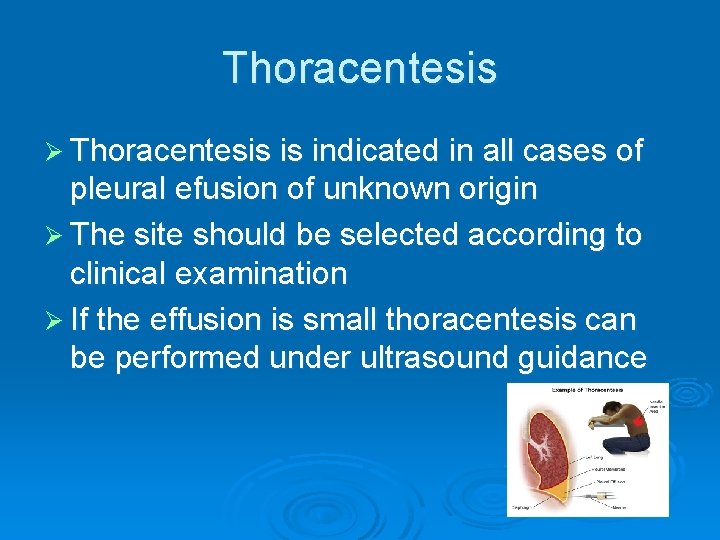
Thoracentesis Ø Thoracentesis is indicated in all cases of pleural efusion of unknown origin Ø The site should be selected according to clinical examination Ø If the effusion is small thoracentesis can be performed under ultrasound guidance
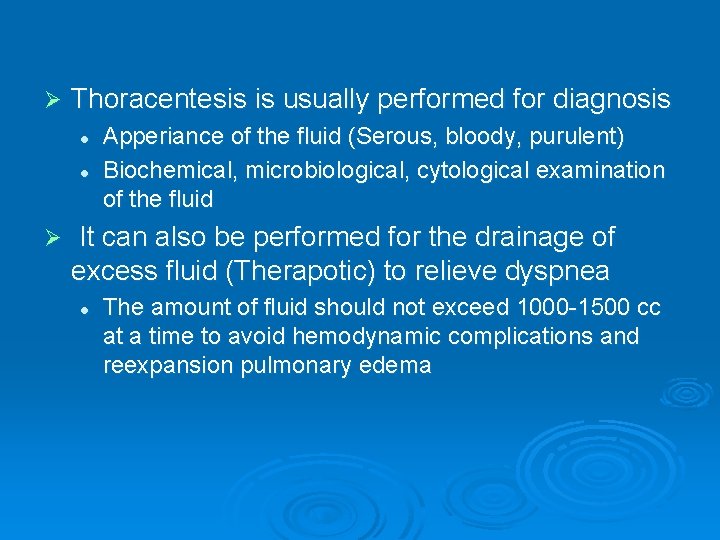
Ø Thoracentesis is usually performed for diagnosis l l Ø Apperiance of the fluid (Serous, bloody, purulent) Biochemical, microbiological, cytological examination of the fluid It can also be performed for the drainage of excess fluid (Therapotic) to relieve dyspnea l The amount of fluid should not exceed 1000 -1500 cc at a time to avoid hemodynamic complications and reexpansion pulmonary edema
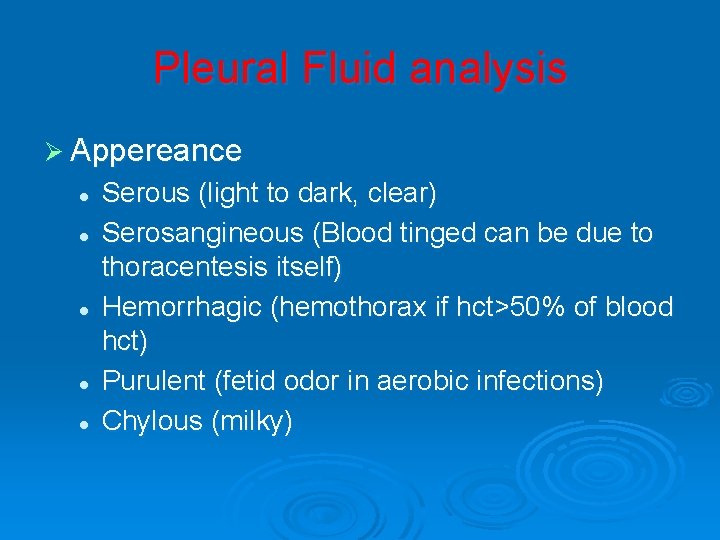
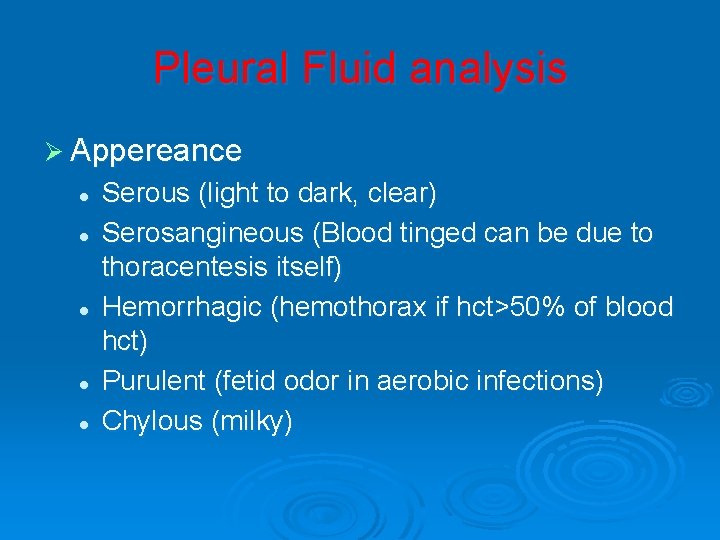
Pleural Fluid analysis Ø Appereance l l l Serous (light to dark, clear) Serosangineous (Blood tinged can be due to thoracentesis itself) Hemorrhagic (hemothorax if hct>50% of blood hct) Purulent (fetid odor in aerobic infections) Chylous (milky)
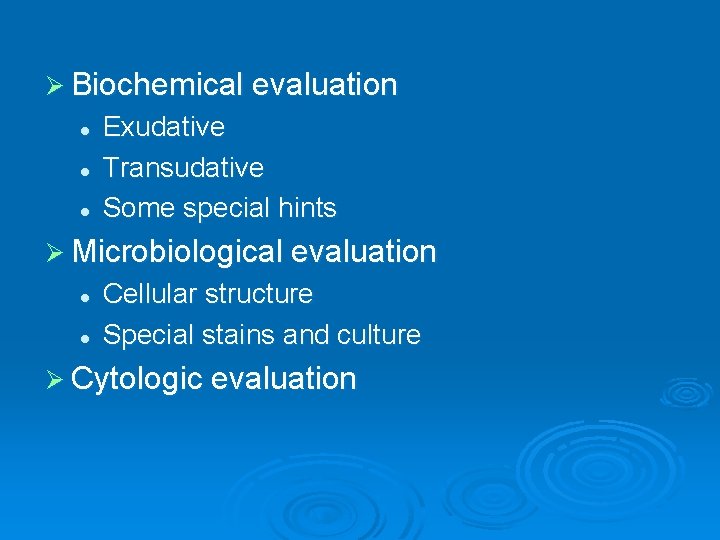
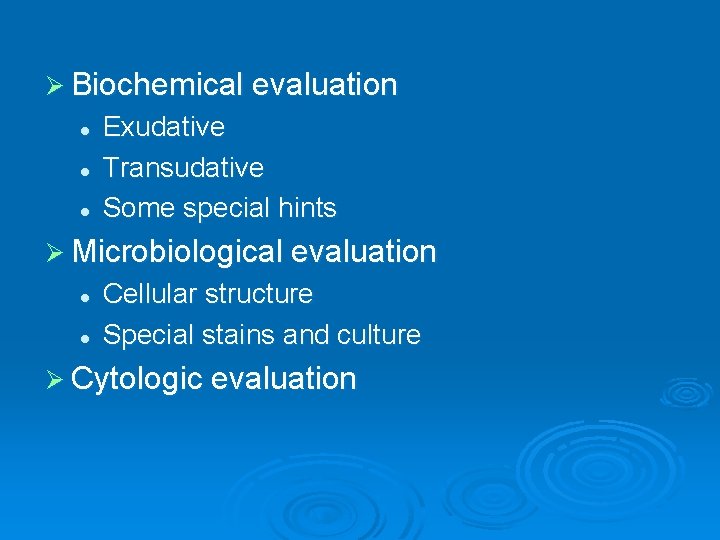
Ø Biochemical evaluation l l l Exudative Transudative Some special hints Ø Microbiological evaluation l l Cellular structure Special stains and culture Ø Cytologic evaluation
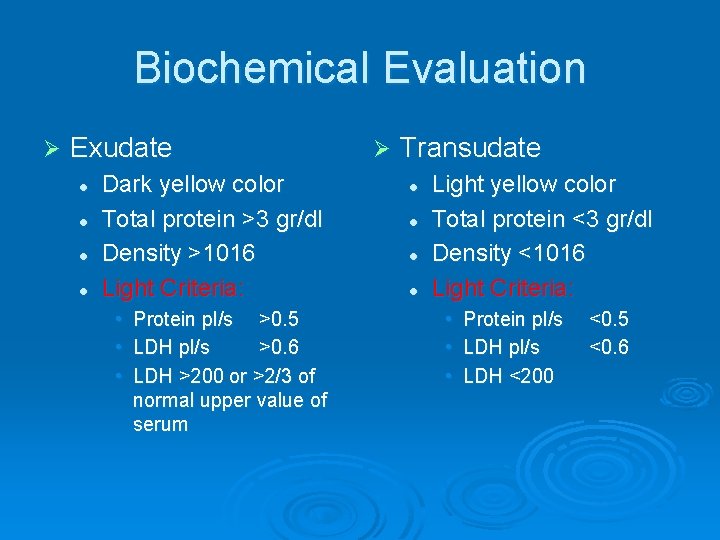
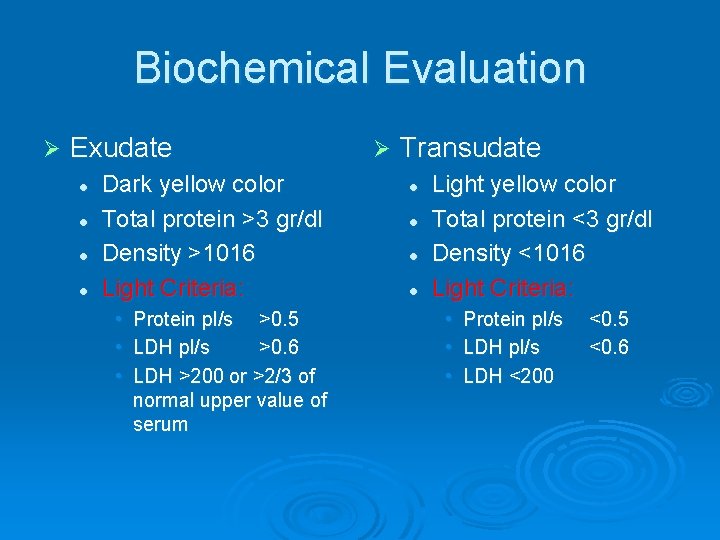
Biochemical Evaluation Ø Exudate l l Dark yellow color Total protein >3 gr/dl Density >1016 Light Criteria: • • • Protein pl/s >0. 5 LDH pl/s >0. 6 LDH >200 or >2/3 of normal upper value of serum Ø Transudate l l Light yellow color Total protein <3 gr/dl Density <1016 Light Criteria: • • • Protein pl/s LDH <200 <0. 5 <0. 6
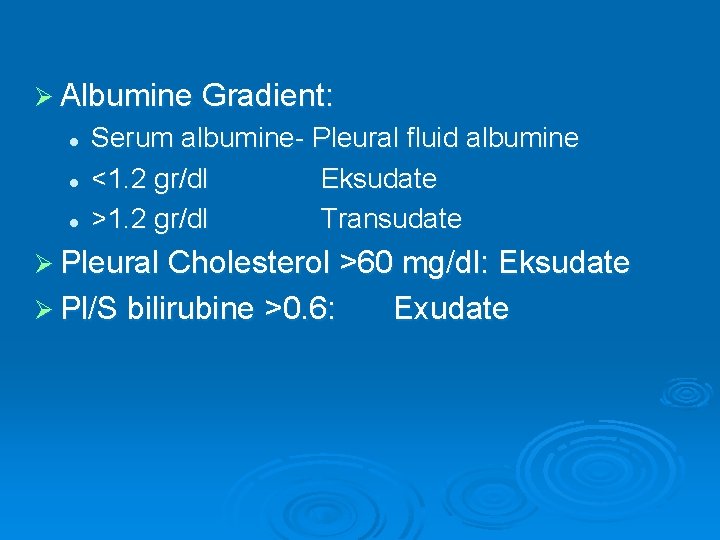
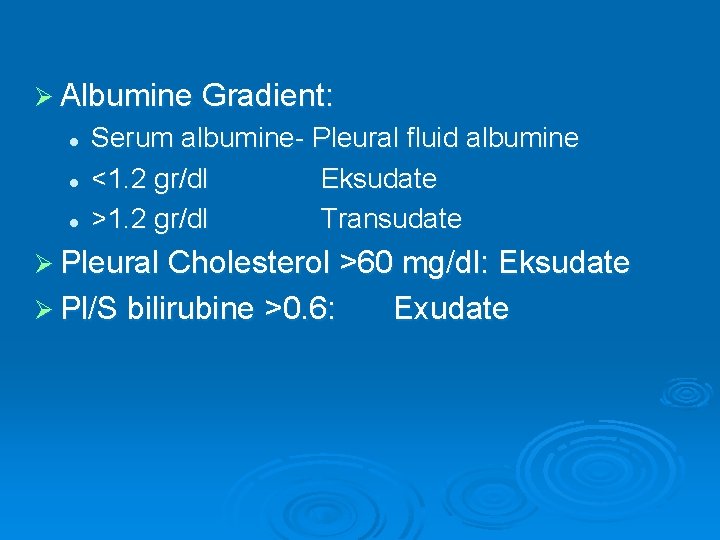
Ø Albumine Gradient: l l l Serum albumine- Pleural fluid albumine <1. 2 gr/dl Eksudate >1. 2 gr/dl Transudate Ø Pleural Cholesterol >60 mg/dl: Eksudate Ø Pl/S bilirubine >0. 6: Exudate
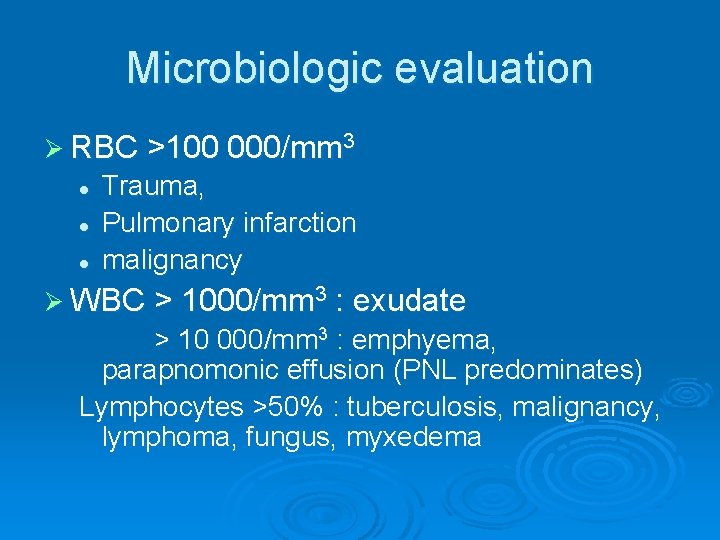
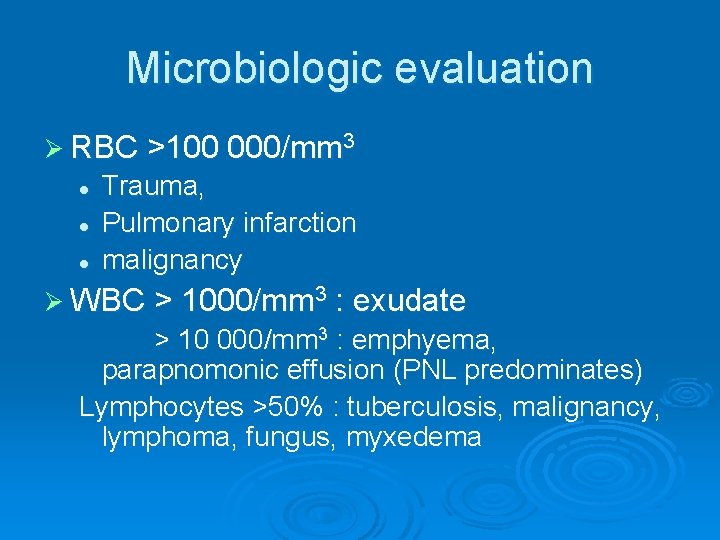
Microbiologic evaluation Ø RBC >100 000/mm 3 l l l Trauma, Pulmonary infarction malignancy Ø WBC > 1000/mm 3 : exudate > 10 000/mm 3 : emphyema, parapnomonic effusion (PNL predominates) Lymphocytes >50% : tuberculosis, malignancy, lymphoma, fungus, myxedema
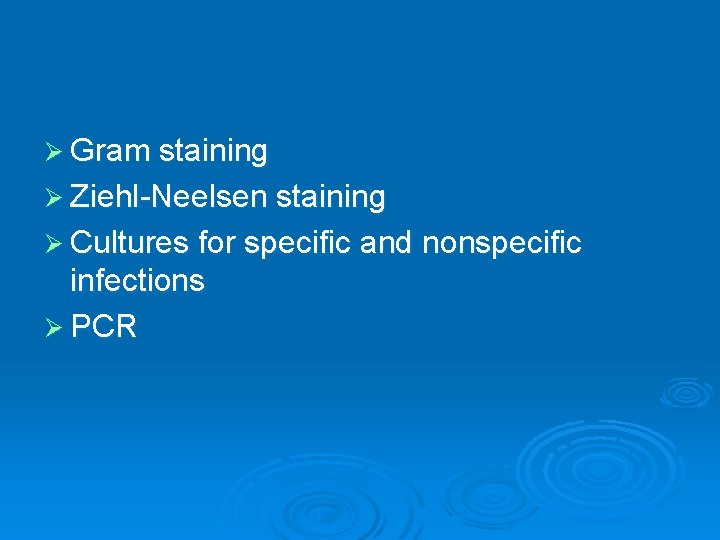
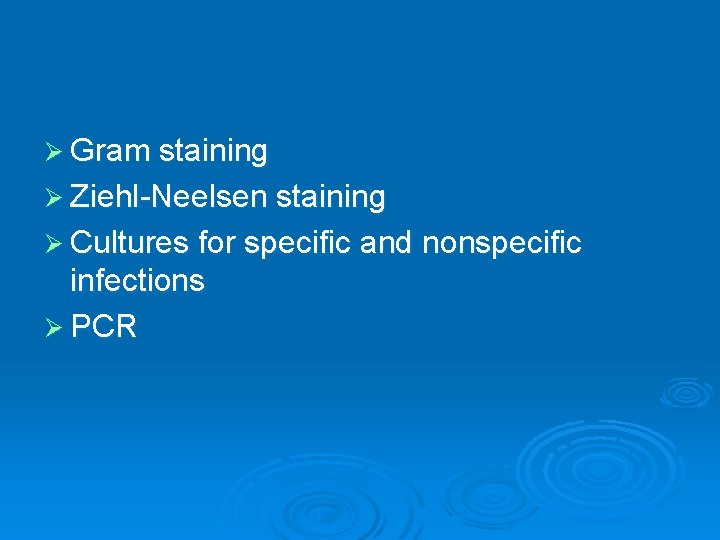
Ø Gram staining Ø Ziehl-Neelsen staining Ø Cultures for specific and nonspecific infections Ø PCR
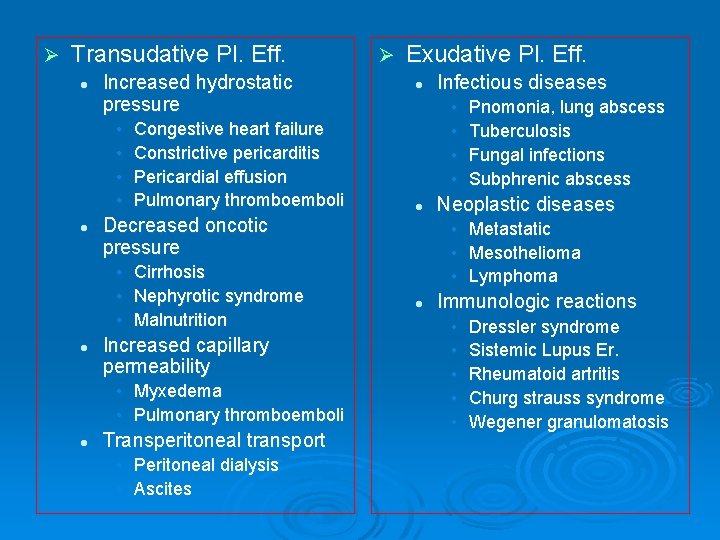
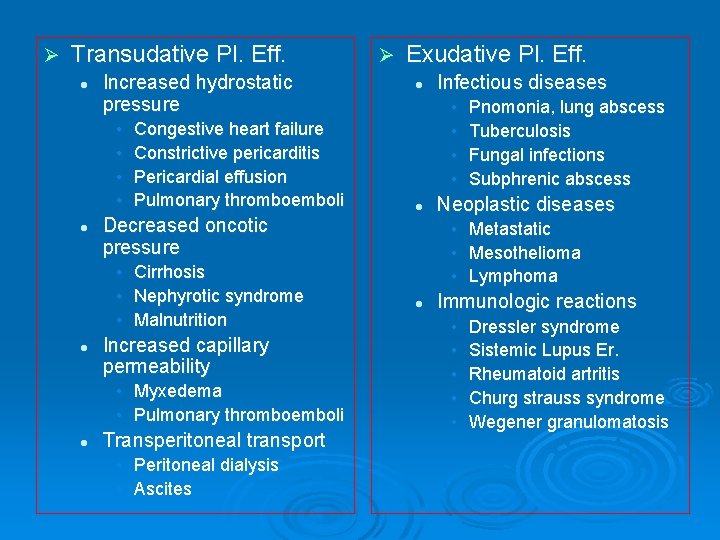
Ø Transudative Pl. Eff. l Increased hydrostatic pressure • • l Congestive heart failure Constrictive pericarditis Pericardial effusion Pulmonary thromboemboli Increased capillary permeability • Myxedema • Pulmonary thromboemboli l Exudative Pl. Eff. l Transperitoneal transport • Peritoneal dialysis • Ascites Infectious diseases • • l Decreased oncotic pressure • Cirrhosis • Nephyrotic syndrome • Malnutrition l Ø Pnomonia, lung abscess Tuberculosis Fungal infections Subphrenic abscess Neoplastic diseases • Metastatic • Mesothelioma • Lymphoma l Immunologic reactions • • • Dressler syndrome Sistemic Lupus Er. Rheumatoid artritis Churg strauss syndrome Wegener granulomatosis
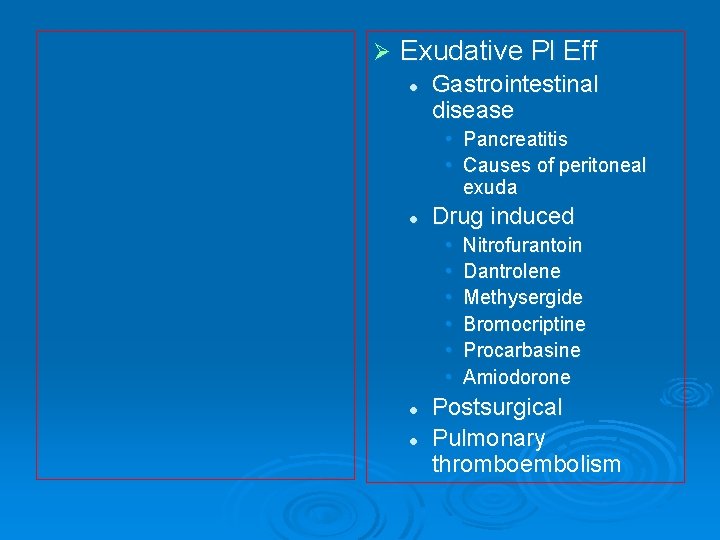
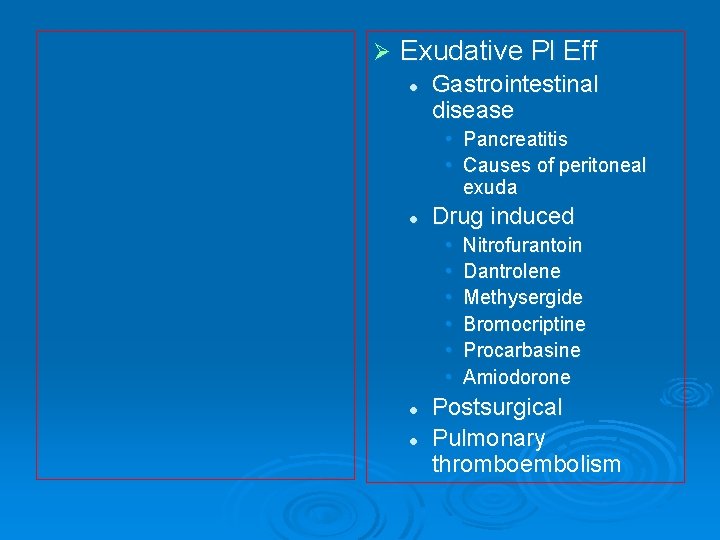
Ø Exudative Pl Eff l Gastrointestinal disease • Pancreatitis • Causes of peritoneal exuda l Drug induced • • • l l Nitrofurantoin Dantrolene Methysergide Bromocriptine Procarbasine Amiodorone Postsurgical Pulmonary thromboembolism
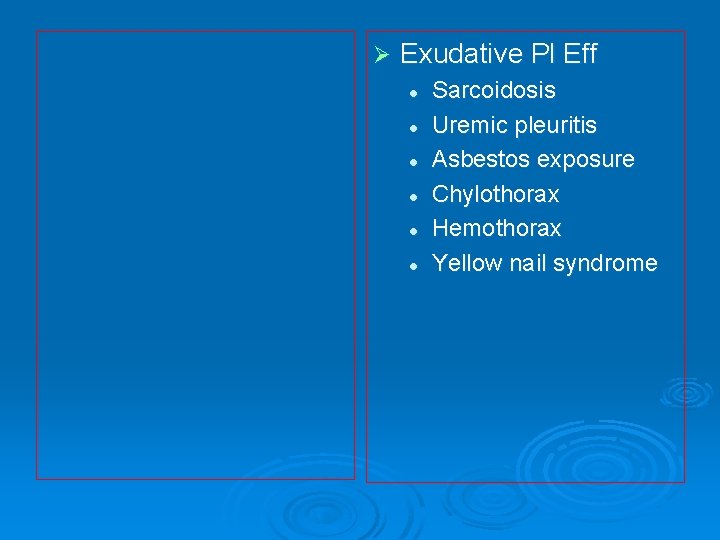
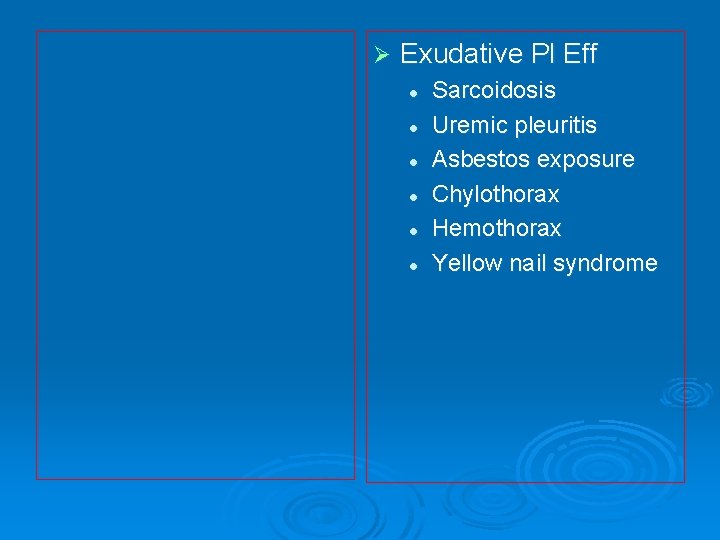
Ø Exudative Pl Eff l l l Sarcoidosis Uremic pleuritis Asbestos exposure Chylothorax Hemothorax Yellow nail syndrome
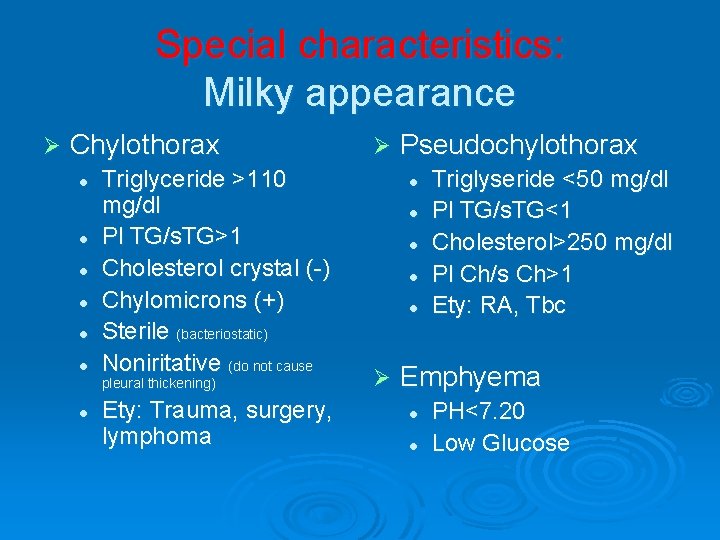
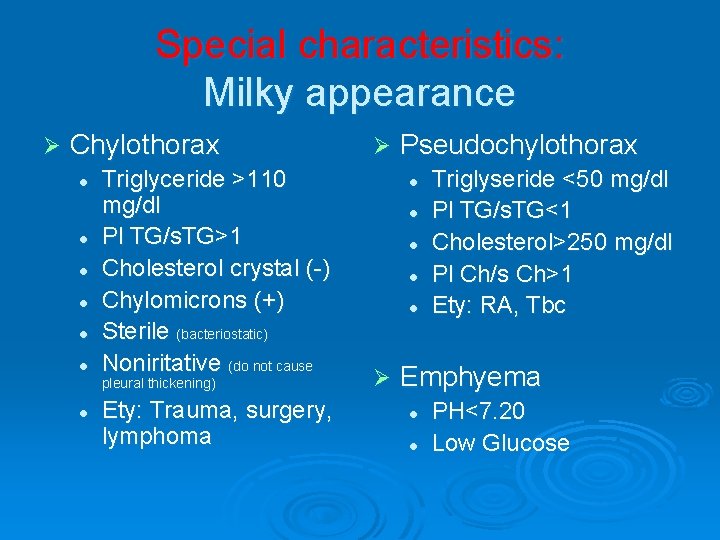
Special characteristics: Milky appearance Ø Chylothorax l l l Triglyceride >110 mg/dl Pl TG/s. TG>1 Cholesterol crystal (-) Chylomicrons (+) Sterile (bacteriostatic) Noniritative (do not cause pleural thickening) l Ety: Trauma, surgery, lymphoma Ø Pseudochylothorax l l l Ø Triglyseride <50 mg/dl Pl TG/s. TG<1 Cholesterol>250 mg/dl Pl Ch/s Ch>1 Ety: RA, Tbc Emphyema l l PH<7. 20 Low Glucose
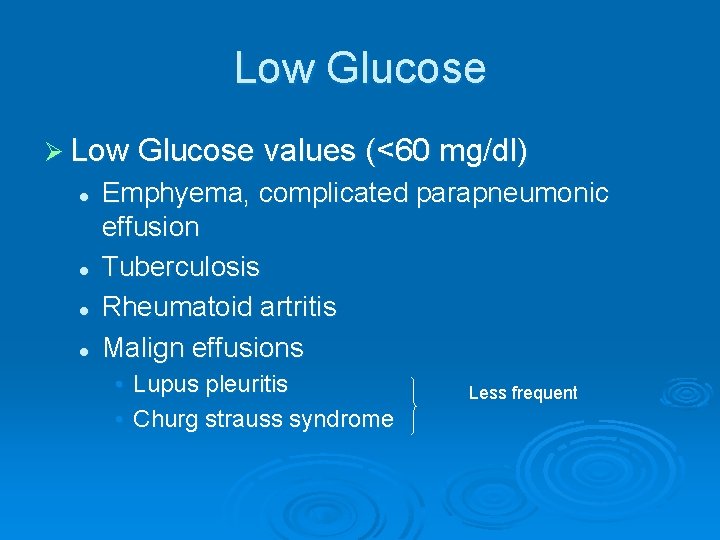
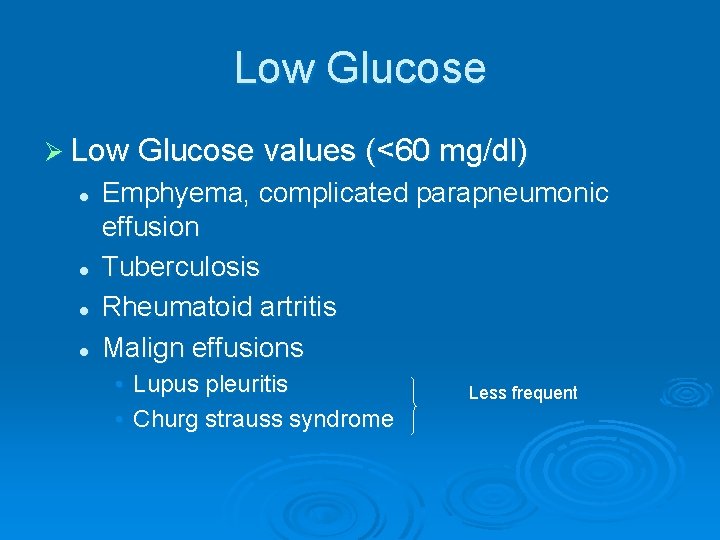
Low Glucose Ø Low Glucose values (<60 mg/dl) l l Emphyema, complicated parapneumonic effusion Tuberculosis Rheumatoid artritis Malign effusions • Lupus pleuritis • Churg strauss syndrome Less frequent
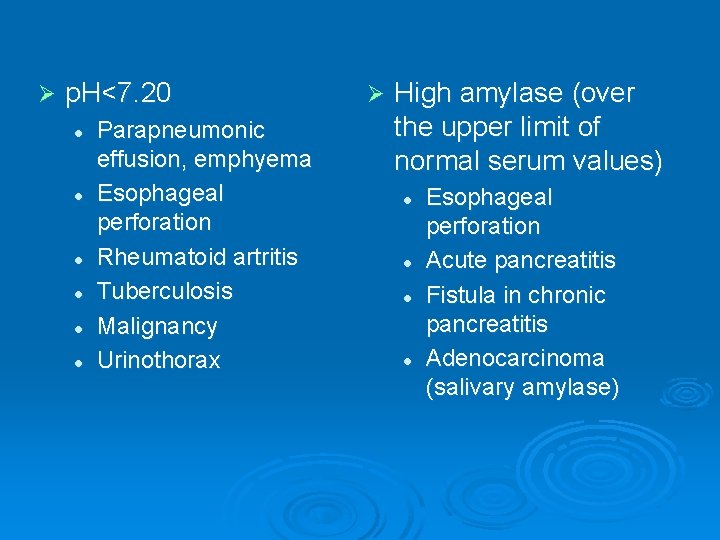
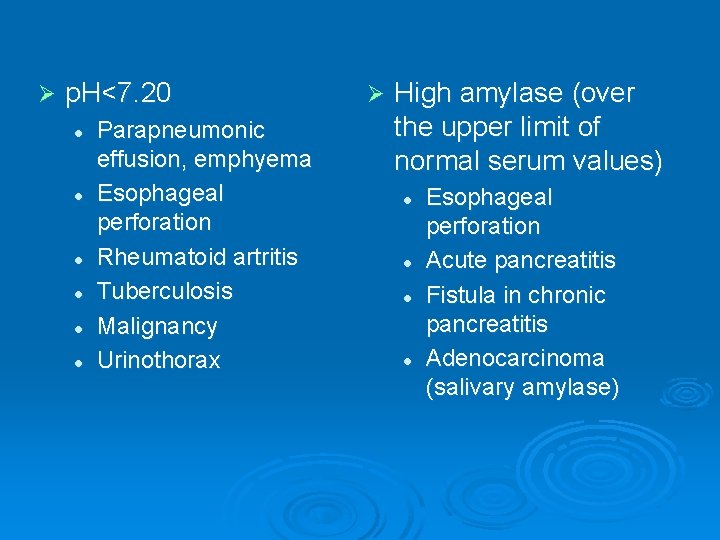
Ø p. H<7. 20 l l l Parapneumonic effusion, emphyema Esophageal perforation Rheumatoid artritis Tuberculosis Malignancy Urinothorax Ø High amylase (over the upper limit of normal serum values) l l Esophageal perforation Acute pancreatitis Fistula in chronic pancreatitis Adenocarcinoma (salivary amylase)
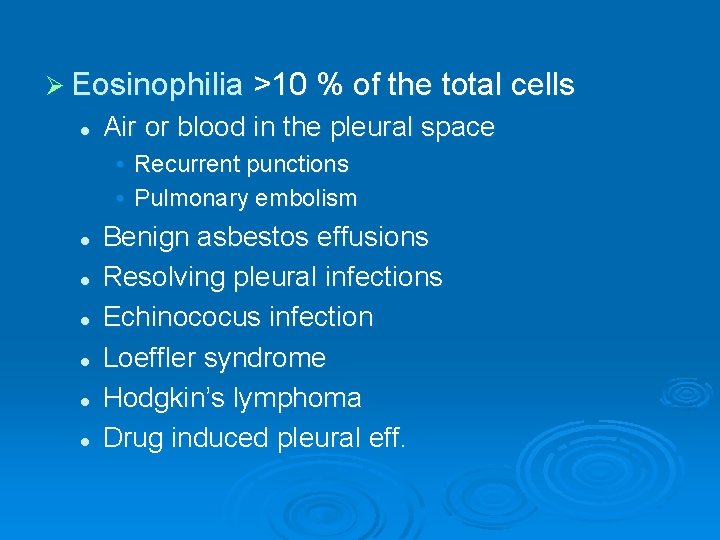
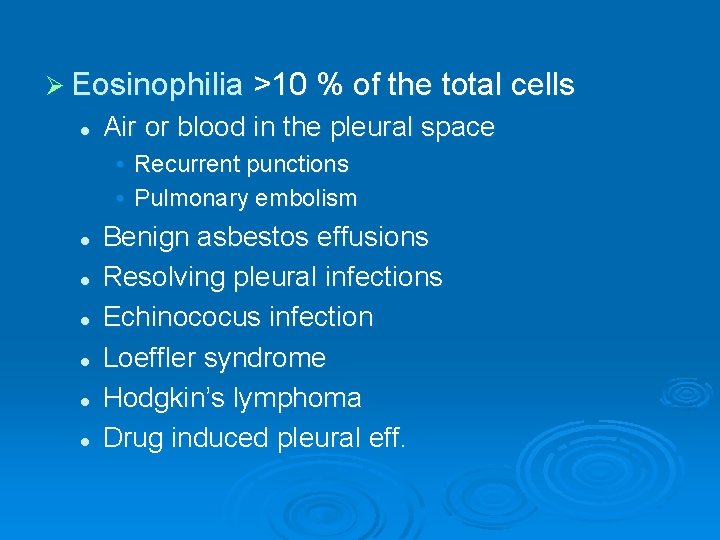
Ø Eosinophilia >10 % of the total cells l Air or blood in the pleural space • Recurrent punctions • Pulmonary embolism l l l Benign asbestos effusions Resolving pleural infections Echinococus infection Loeffler syndrome Hodgkin’s lymphoma Drug induced pleural eff.
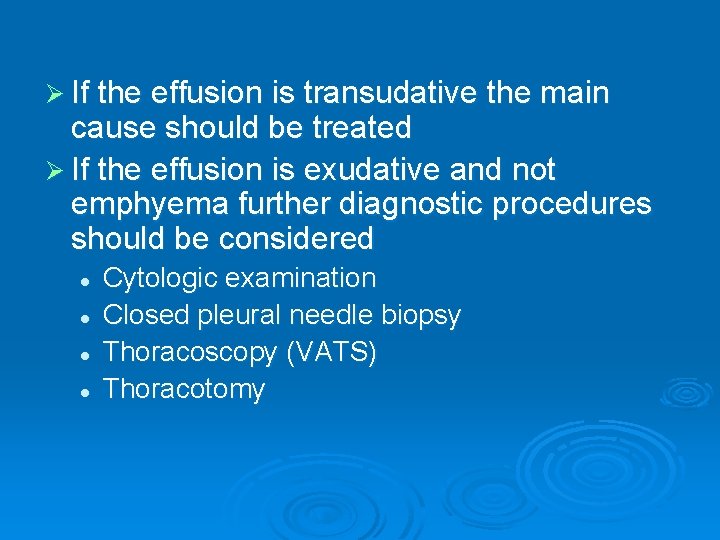
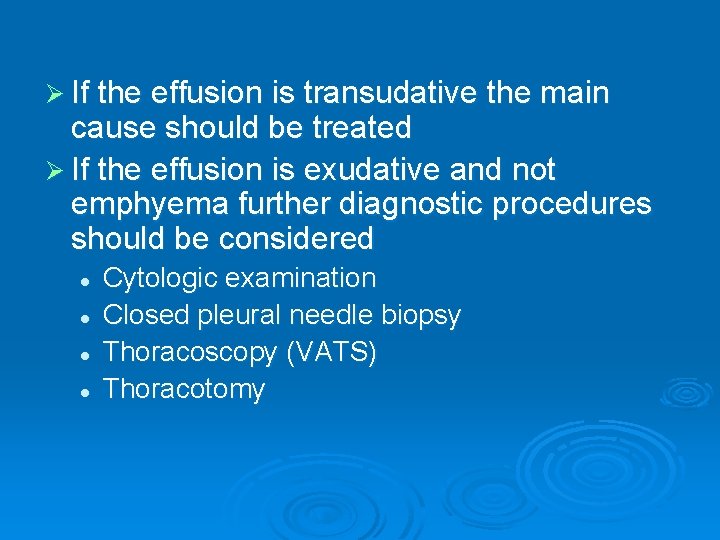
Ø If the effusion is transudative the main cause should be treated Ø If the effusion is exudative and not emphyema further diagnostic procedures should be considered l l Cytologic examination Closed pleural needle biopsy Thoracoscopy (VATS) Thoracotomy
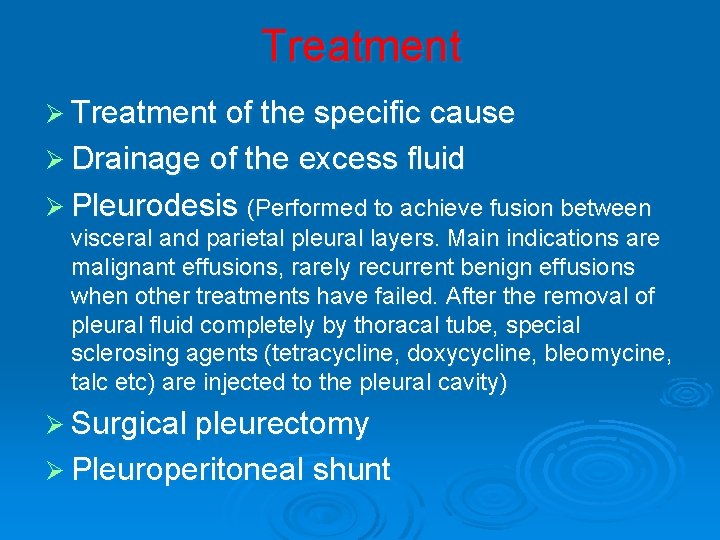
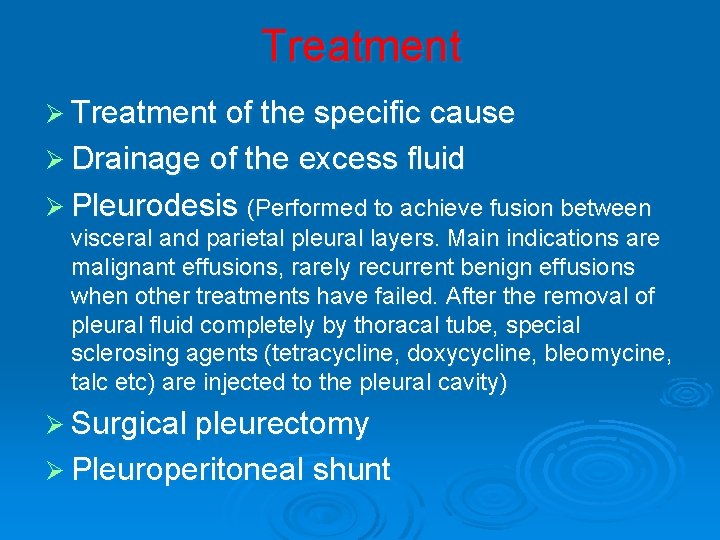
Treatment Ø Treatment of the specific cause Ø Drainage of the excess fluid Ø Pleurodesis (Performed to achieve fusion between visceral and parietal pleural layers. Main indications are malignant effusions, rarely recurrent benign effusions when other treatments have failed. After the removal of pleural fluid completely by thoracal tube, special sclerosing agents (tetracycline, doxycycline, bleomycine, talc etc) are injected to the pleural cavity) Ø Surgical pleurectomy Ø Pleuroperitoneal shunt
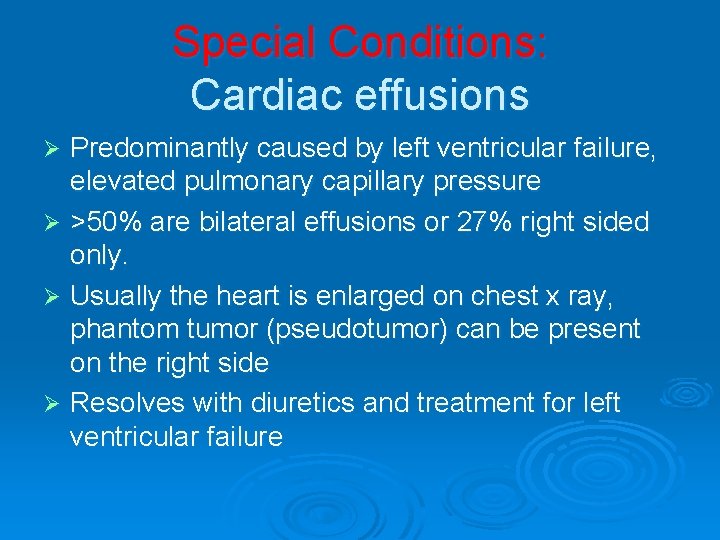
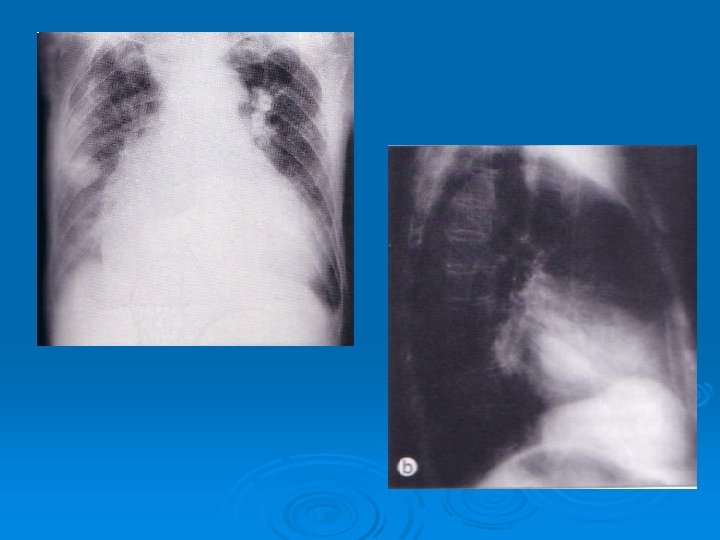
Special Conditions: Cardiac effusions Predominantly caused by left ventricular failure, elevated pulmonary capillary pressure Ø >50% are bilateral effusions or 27% right sided only. Ø Usually the heart is enlarged on chest x ray, phantom tumor (pseudotumor) can be present on the right side Ø Resolves with diuretics and treatment for left ventricular failure Ø
Infectious pleuresy, emphyema Ø Bacterial pneumonia is associated with an effusion in 40% of cases Ø The effusion may be parapneumonic without infection (uncomplicated) or culture positive (complicated, emphyema) Ø Parapneumonic effusions are treated with appropiate antibiotics Ø Antibiotic treatment + Tube drainage is indicated if emphyema occurs
Tube drainage indications in complicated parapneumonic effusion Ø Purulent appearance Ø Gram staining (+) for bacteria Ø Plevral fluid glucose<40 mg/dl Ø Pleural fluid p. H<7. 10 -7. 20 Ø Pleural fluid LDH>1000 IU/L
Tuberculosis pleurisy Usually occurs soon after the primary infection and mainly affects children or teenager group Ø Pathogenetic mechanisms include direct invasion of AFB to pleura or delayed type hypersensitivity reaction Ø The onset of symptoms may be acute or subacute Ø Typical symptoms of pleural effusion and general symptoms of tb may be present Ø
Ø Exudative effusion, lymphocyte predominance, low glucose, low mesothelial cells (<5%), high ADA Tuberculin skin test can be (-) in 30% Ø Treatment: Pulmonary tb treatment steroid +
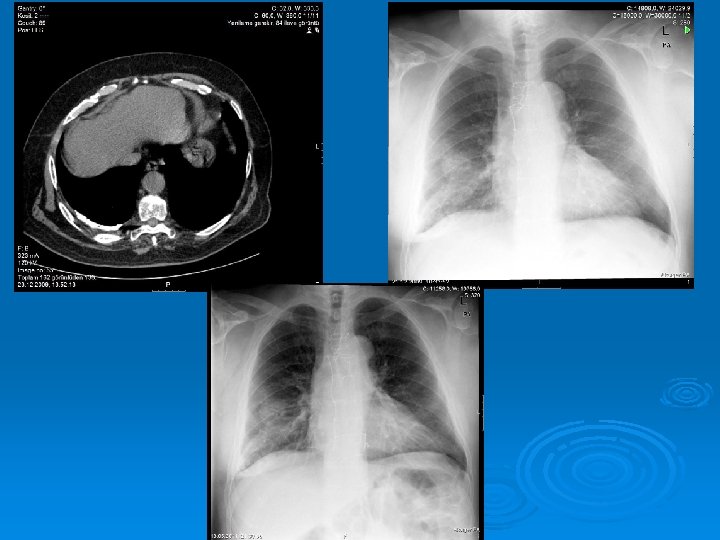
Other Pleural Diseases Ø Hemothorax l l Plevral fluid htc>50% of serum Can be traumatic or nontraumatic: • • • l İatrogenic Pulmonary infarction Tumors Rupture of aneurism Anticoagulan treatment Thoracic endometriosis Treatment: • • intrapleural drainage thoracotomy
Ø Chylothorax l l l Direct passage of chyle from the thoracic duct into the pleural cavity TG>110 mg/dl Cause: • • • Tumors (Lymphoma) Trauma (surgery) Congenital defects Lymhangioleiomyomatosis Tuberosclerosis l Treatment. • Pleural drainage • Parenteral nutrition • Bed rest (to decrease lymphatic drainage) • Surgical ligation of thoracic duct • Chemotherapy or RT
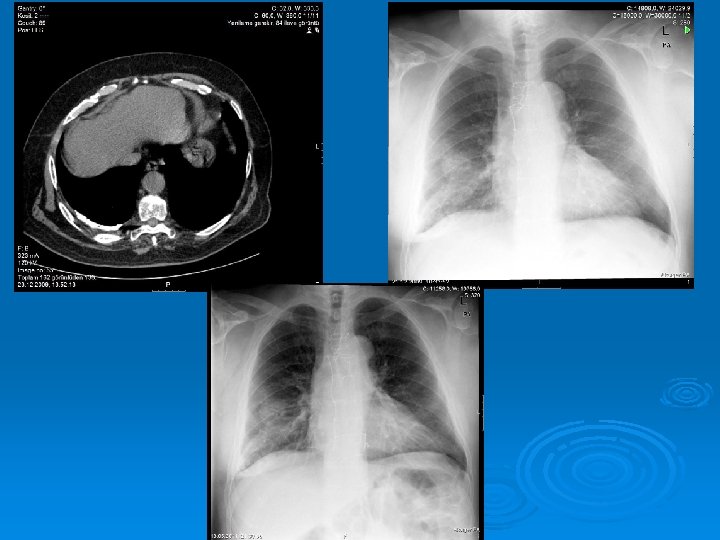
Ø Fibrothorax l l A thick fibrous tissue formed on visceral pleura Cause: • • • l Empyema Tuberculosis Hemothorax Treatment: Decortication

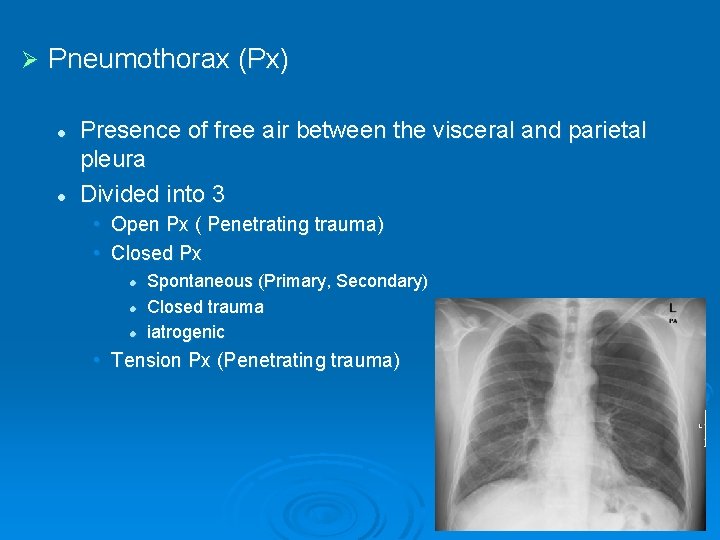
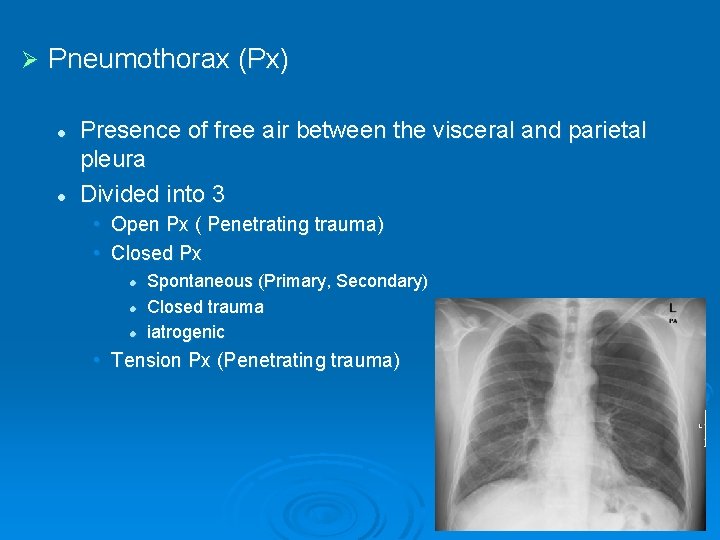
Ø Pneumothorax (Px) l l Presence of free air between the visceral and parietal pleura Divided into 3 • Open Px ( Penetrating trauma) • Closed Px l l l Spontaneous (Primary, Secondary) Closed trauma iatrogenic • Tension Px (Penetrating trauma)
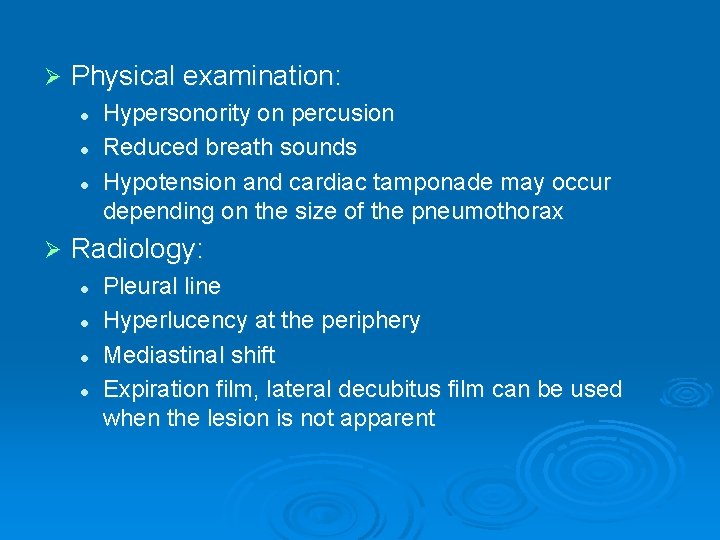
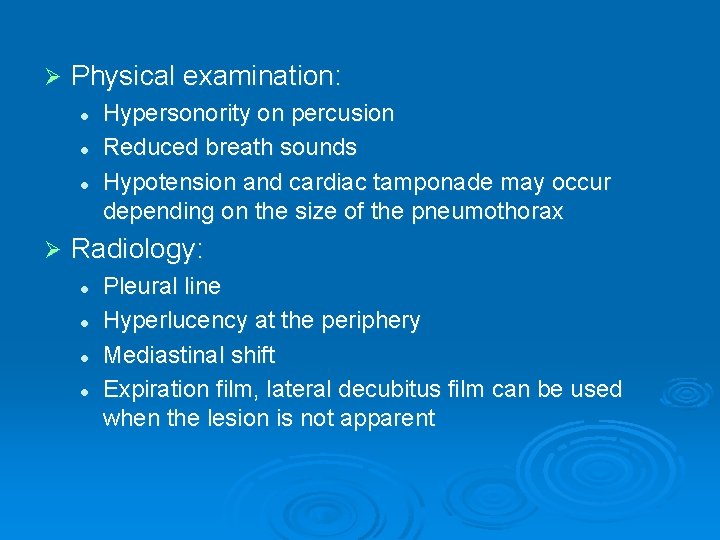
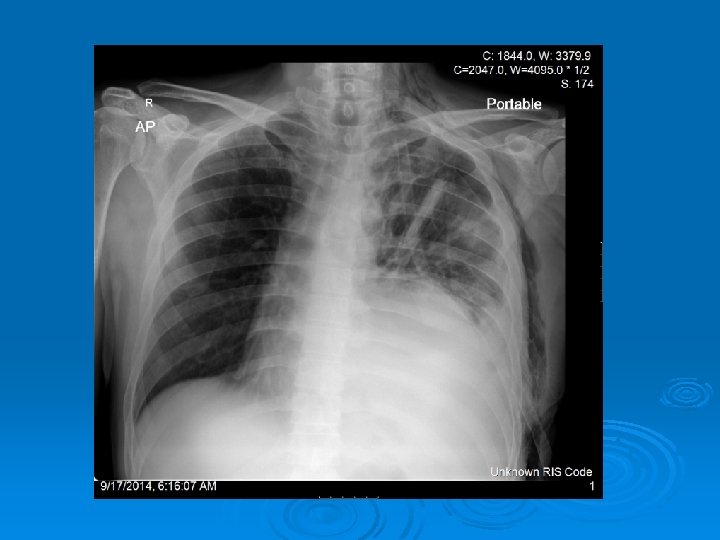
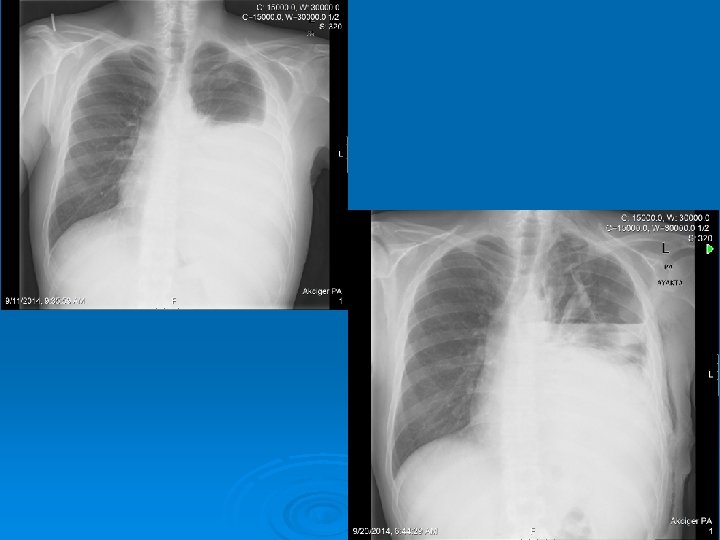
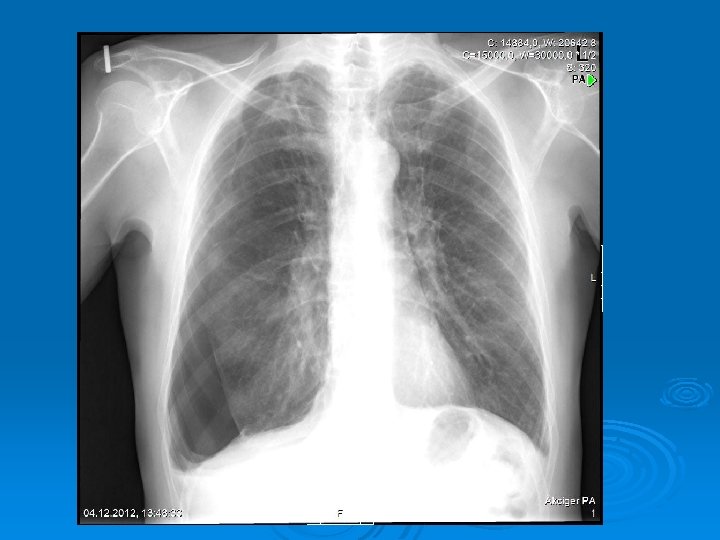
Ø Physical examination: l l l Ø Hypersonority on percusion Reduced breath sounds Hypotension and cardiac tamponade may occur depending on the size of the pneumothorax Radiology: l l Pleural line Hyperlucency at the periphery Mediastinal shift Expiration film, lateral decubitus film can be used when the lesion is not apparent

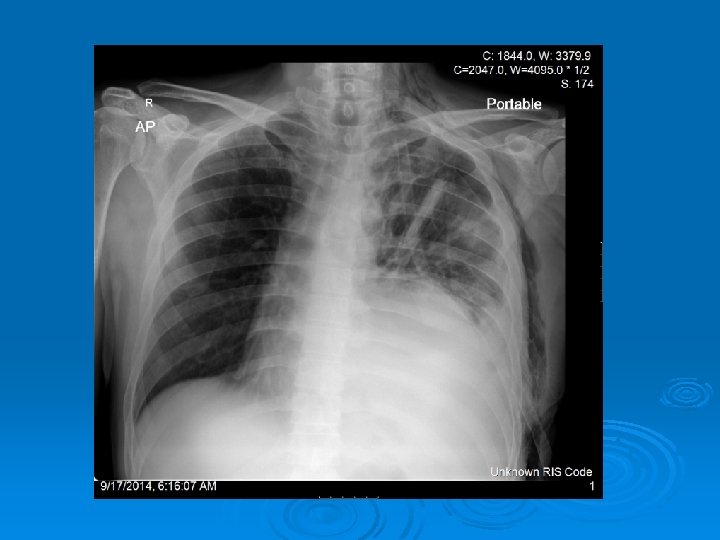
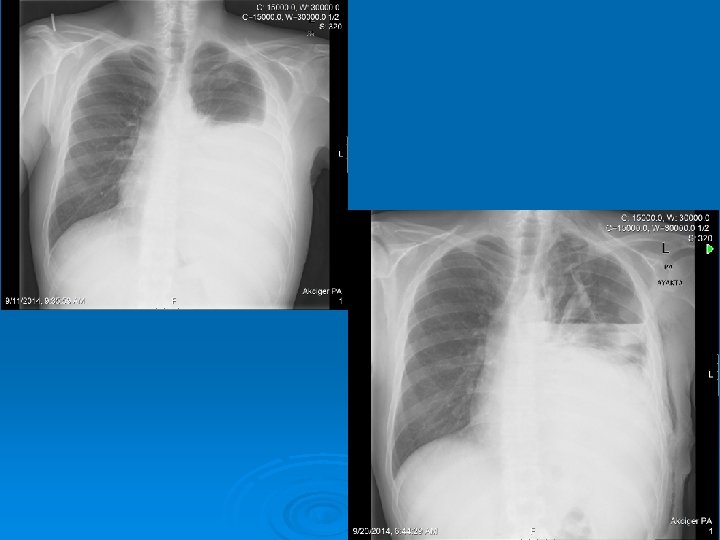
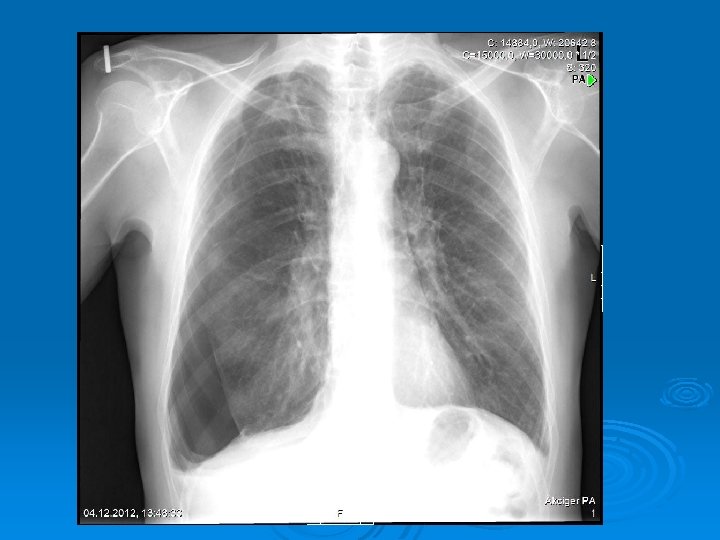
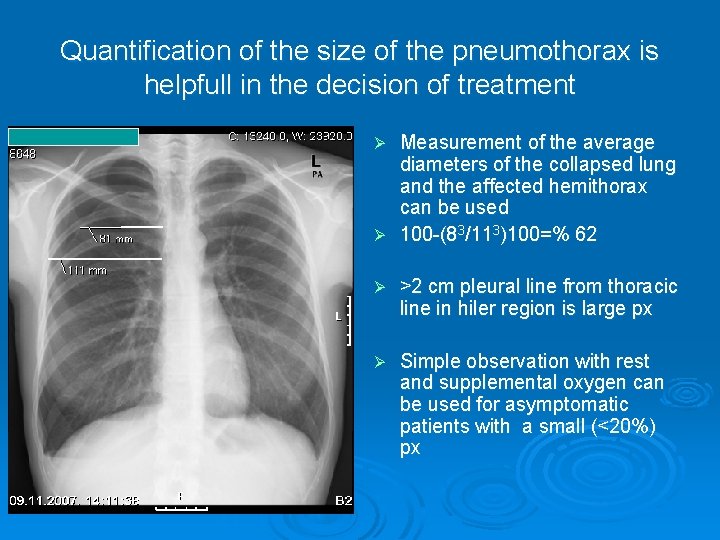
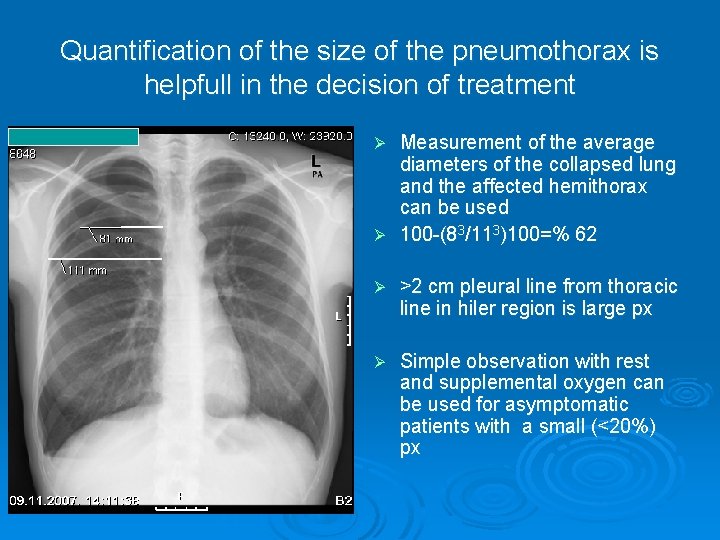
Quantification of the size of the pneumothorax is helpfull in the decision of treatment Measurement of the average diameters of the collapsed lung and the affected hemithorax can be used Ø 100 -(83/113)100=% 62 Ø Ø >2 cm pleural line from thoracic line in hiler region is large px Ø Simple observation with rest and supplemental oxygen can be used for asymptomatic patients with a small (<20%) px
Ø Intercostal drainage is indicated in large or bilateral or tension px Ø A recurrent spontaneous pneumothorax (30 -50% risk) is an indication for surgery Ø Smoking should be quited after first attack Ø A patient with px cannot travel by air until totaly expanded in chest x ray
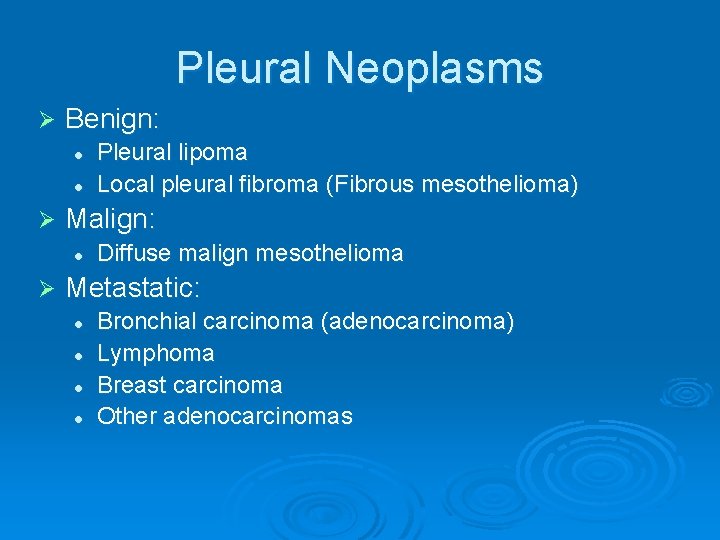
Pleural Neoplasms Ø Benign: l l Ø Malign: l Ø Pleural lipoma Local pleural fibroma (Fibrous mesothelioma) Diffuse malign mesothelioma Metastatic: l l Bronchial carcinoma (adenocarcinoma) Lymphoma Breast carcinoma Other adenocarcinomas
-END-