Environmental Lung Diseases Dr E Sevda zdoan Environmental
- Slides: 55
Environmental Lung Diseases Dr. E. Sevda Özdoğan
• Environmental lung diseases are caused by harmful particles, mists, vapors, or gases that are inhaled (usually while people work ) • Where? within the airways or lungs an inhaled substance ends up and what type of lung disease develops depend on the size and kind of particles inhaled.
Size of the particle • Aerodynamic diameter: The diameter of a dust particle floating in the air • Inhalable particles are < 10 micron (they can pass through the nose and reach the peripheral airways • Respirabl particles: 0, 5 -5 micron ((they can reach the lung paranchym
Other factors – Chemical and physical properties of the dust (Inert dust like ferrum do not cause a reaction in the tissue, simply accumulate but silica dust cause a progressive tissue reaction) – The amount of dust in the air – The period of exposure – The effectivity of respiratory defence mechanisms of the person (Normaly clears 98 -99% of the dust)
• Many different kinds of particles can harm the lungs. Some are organic, meaning that they are made of materials that contain carbon and are part of living organisms (such as grain dusts, cotton dust, or animal dander). • Some are inorganic, meaning that they usually come from nonliving sources, such as metals or minerals.
Pneumoconiosis • Pneumoconiosis is the disease caused by the accumulation of inorganic dust and tissue reaction in the lungs that ends up with fibrosis • Pneumoconiosis is mostly an occupational disease
• Repeated and long term exposure to certain irritants on the job can lead to lung diseases called occupational lung diseases • Occupational lung diseases are the number one cause of work-related illness. • Most occupational lung diseases are caused by repeated, long-term exposure, but even a severe, single exposure to a hazardous agent can damage the lungs. • Occupational lung diseases are preventable. • Smoking can increase both the severity of an occupational lung disease and the risk of lung cancer.
Common Types of Pneumoconiosis • Silicosis • Coal Workers Pneumoconiosis • Asbestosis
Clinical Evaluation and Diagnosis in pneumoconiosis • The patient with risk factor (job) can be asympthomatic (regular check up) • Symptoms from chronic cough, mild to severe dyspnea and respiratory failure can be seen • Occupational history (detailed) including the period of exposure to toxic material is important • Diagnosis: – History of exposure – Convenient radiology – Differential diagnosis
• Workers in high risk areas should be examined regularly but the most important point is prevention • Prevention: – – – Ventilation Vacuum techniques Wet cleaning Personal precautions (mask, respirator) Alternative material use
• Differential diagnosis of pneumoconiosis includes diseases that cause milier interstitial radiologic changes – Tuberculosis – Sarcoidosis – Fungal infections – Interstitial lung diseases
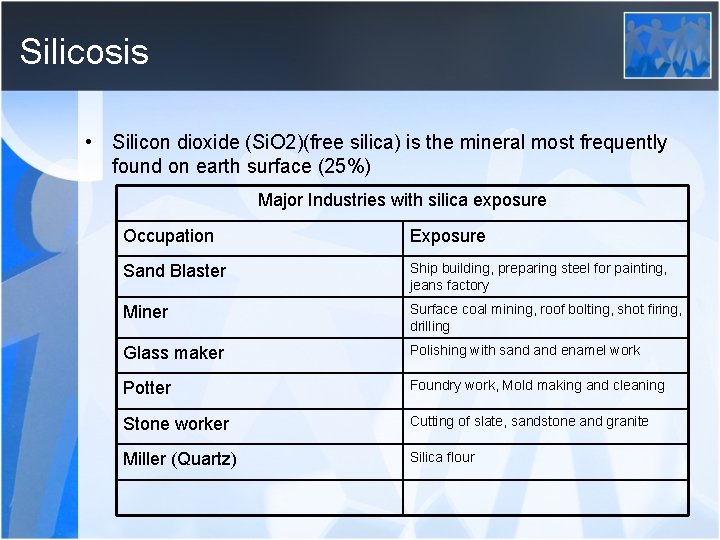
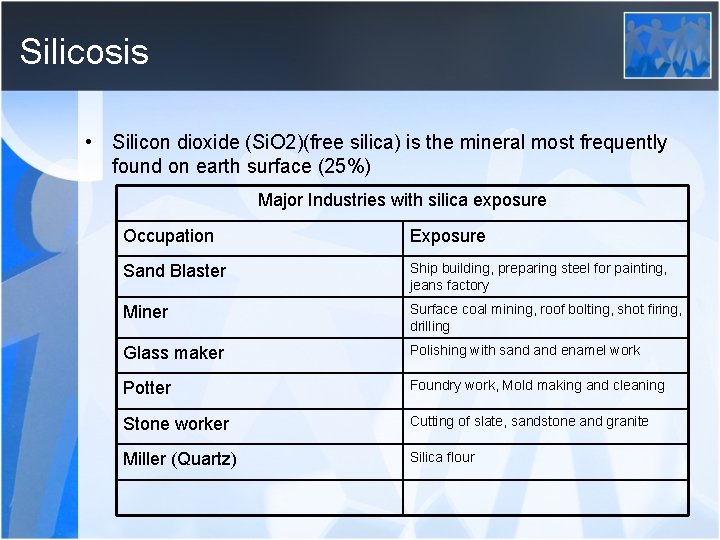
Silicosis • Silicon dioxide (Si. O 2)(free silica) is the mineral most frequently found on earth surface (25%) Major Industries with silica exposure Occupation Exposure Sand Blaster Ship building, preparing steel for painting, jeans factory Miner Surface coal mining, roof bolting, shot firing, drilling Glass maker Polishing with sand enamel work Potter Foundry work, Mold making and cleaning Stone worker Cutting of slate, sandstone and granite Miller (Quartz) Silica flour
• Early diagnosis of Silicosis is important because the disease is progressive even after the cessation of exposure • Clinical Forms – Acute Silicosis – Subacute Accelerated Silicosis – Chronic Silicosis
• Acute Silicosis (Silicoproteinosis, alveoloproteinosis) – Exposure to high concentrations of cristaloid silica, symptoms occur in a few months time – Cough, weight loss, fatique – Diffuse crackles – Lower zone asiner infiltrations on chest x ray – Progression to fulminan respiratory failure over several months – Survival after the onset of symptoms<2 years
• Subacute Accelerated Silicosis – Initial exposure to the onset of the disease is 7 -10 years – Clinicaly identical to classical forms – High levels of silica exposure – Shortened life span
• Chronic Silicosis – Initial exposure to the onset of the disease is >15 years – No symptoms in the beginning – Dispnea and nonproductive cough is the main symptoms and when it is syptomatic it is usually in the form of PMF(PMF: Progressive massive fibrosis)
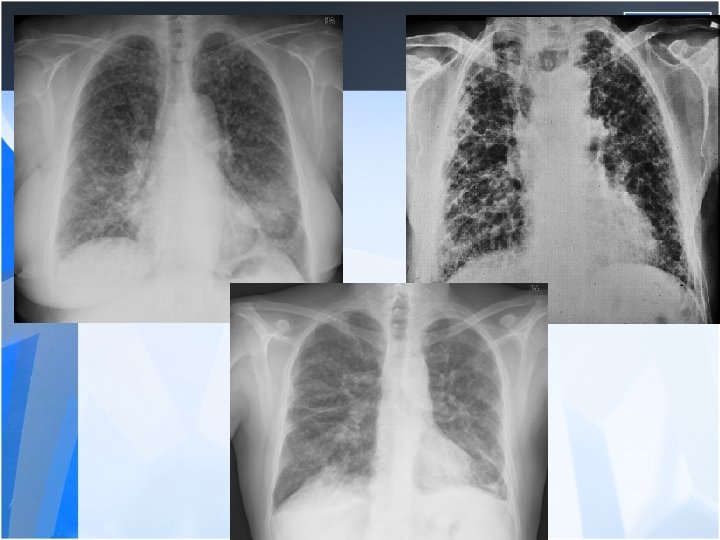
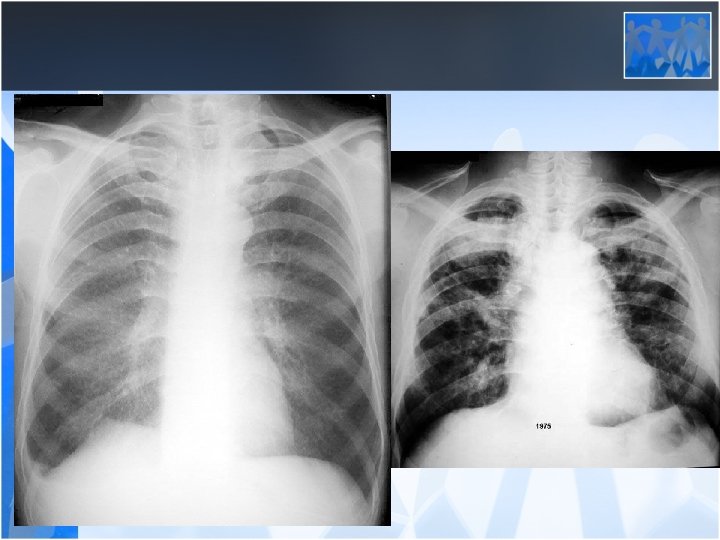
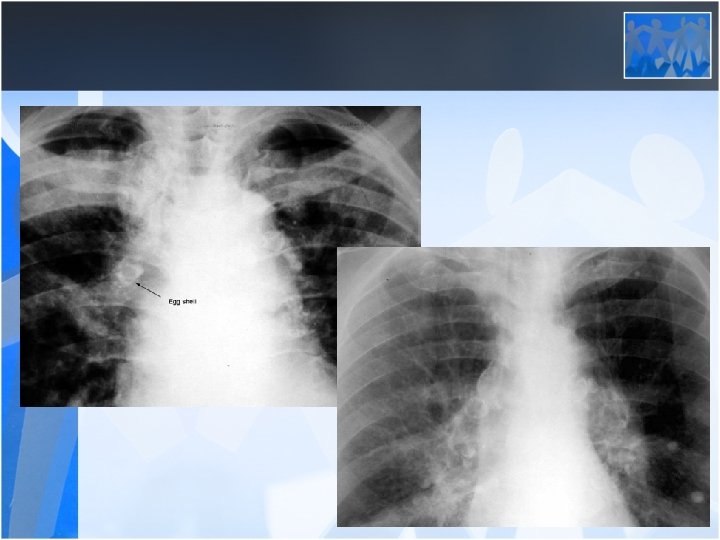
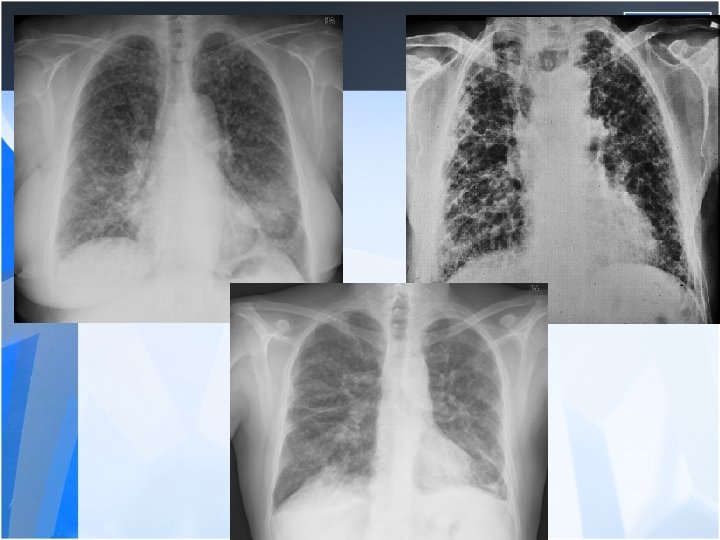
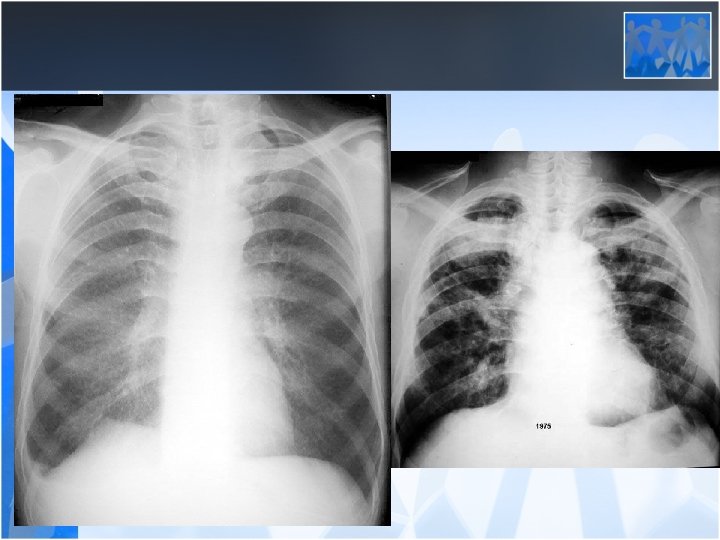
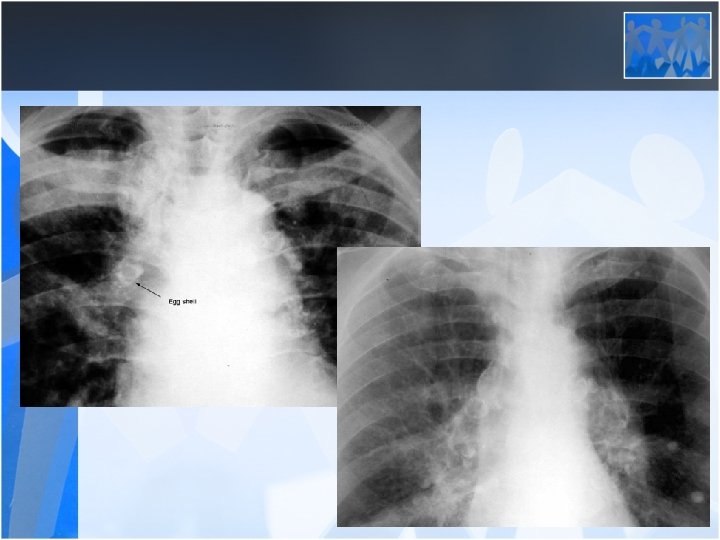
• Radiology is the most important diagnostic method for silicosis • Mainly upper and middle zone 3 -10 mm noduler opacities (silicotic nodules) • ILO clasification p, q, r • Hiler calcification (Egg shell calcification) PMF: • Coalescence of radiologic opacities (conglomeration • Nodules>10 mm • ILO clasification A, B, C • Honey combing can be seen in end stage disease
• Silicosis is a risk factor for tuberculosis • Fever, hemopthysis, weight loss should be alarming for tuberculosis • Silico-tuberculosis is frequent and difficult to diagnose Pulmonary Function Tests: • Usually normal or mild decrease in lung volumes in simple silicosis • Progressive decrease in lung volumes and diffusion in PMF (Ends up with fulminan respiratory failure)
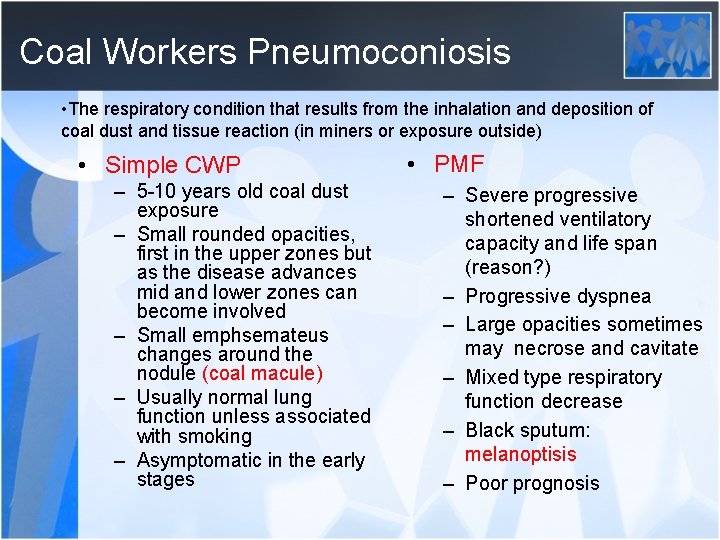
Coal Workers Pneumoconiosis • The respiratory condition that results from the inhalation and deposition of coal dust and tissue reaction (in miners or exposure outside) • Simple CWP – 5 -10 years old coal dust exposure – Small rounded opacities, first in the upper zones but as the disease advances mid and lower zones can become involved – Small emphsemateus changes around the nodule (coal macule) – Usually normal lung function unless associated with smoking – Asymptomatic in the early stages • PMF – Severe progressive shortened ventilatory capacity and life span (reason? ) – Progressive dyspnea – Large opacities sometimes may necrose and cavitate – Mixed type respiratory function decrease – Black sputum: melanoptisis – Poor prognosis
• CWP does not progress after the worker has ceased mining (cessation of exposure) • Mixed dust pneumoconiosis can be seen in miners (together with silicosis) • Caplans Syndrome: Multipl pulmonary nodules+ Rheumatoid artritis in a coal miner • There is no specific treatment for pneumoconiosis – Early diagnosis – Cessation of exposure – Supportive treatment
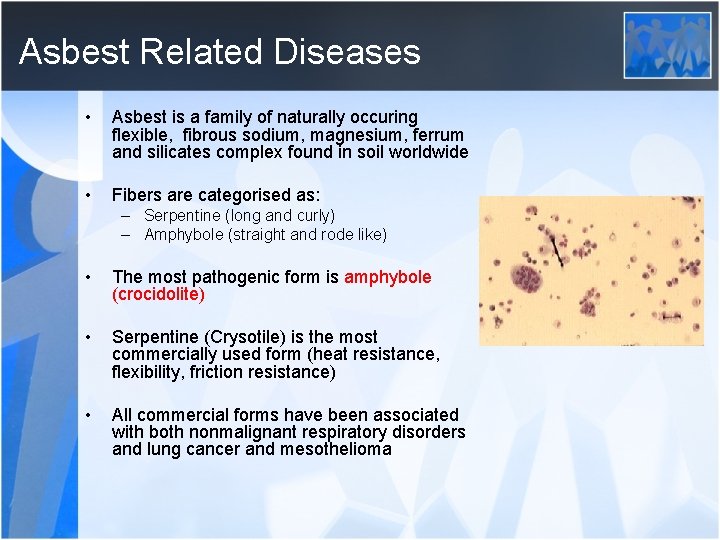
Asbest Related Diseases • Asbest is a family of naturally occuring flexible, fibrous sodium, magnesium, ferrum and silicates complex found in soil worldwide • Fibers are categorised as: – Serpentine (long and curly) – Amphybole (straight and rode like) • The most pathogenic form is amphybole (crocidolite) • Serpentine (Crysotile) is the most commercially used form (heat resistance, flexibility, friction resistance) • All commercial forms have been associated with both nonmalignant respiratory disorders and lung cancer and mesothelioma
Occupation with the risk of asbestos exposure • Construction industry – Roofing, pipes, cement, adhesive, wall covering • • • Ship building and repairing Carpenters Fireproof textile Asphalt flooring, railway insulation Friction materials, brake linings Plastic and rubber manifacture
General exposure of asbest • Occupational exposure • Carry home asbest in hair and clothes of exposed workers • Found in normal levels in buildings under use (elevated exposures from remodelling) • Geographic areas (found in soil, air) – İç anadolu, Göller bölgesi (Nevşehir, Tuzköy, Karain), Diyarbakır (beyaz toprak), Eskişehir çevresi
Asbest Related diseases • Benign – Asbestosis (DIF) – Pleural plaques – Benign pleural effusion – Diffuse pleural fibrosis • Malign – Mesothelioma – Lung Cancer – Gastric, Over, breast cancer
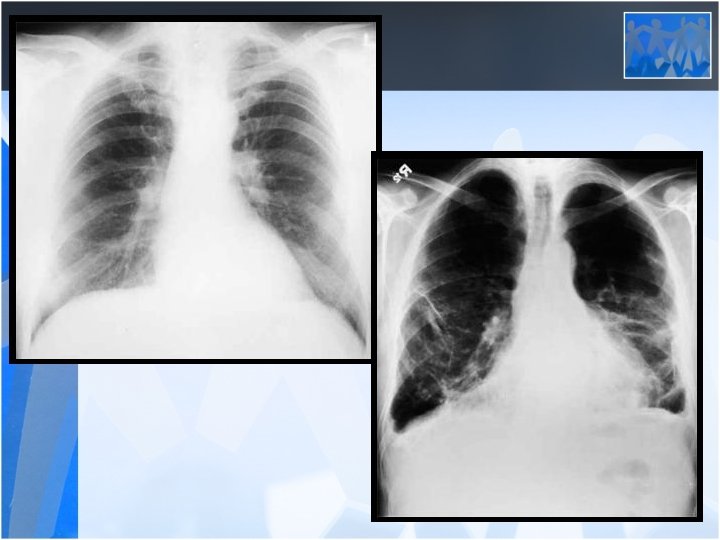
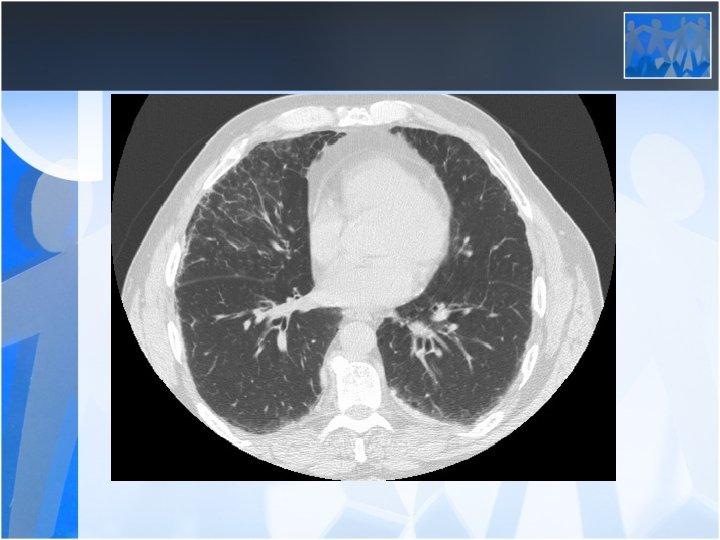
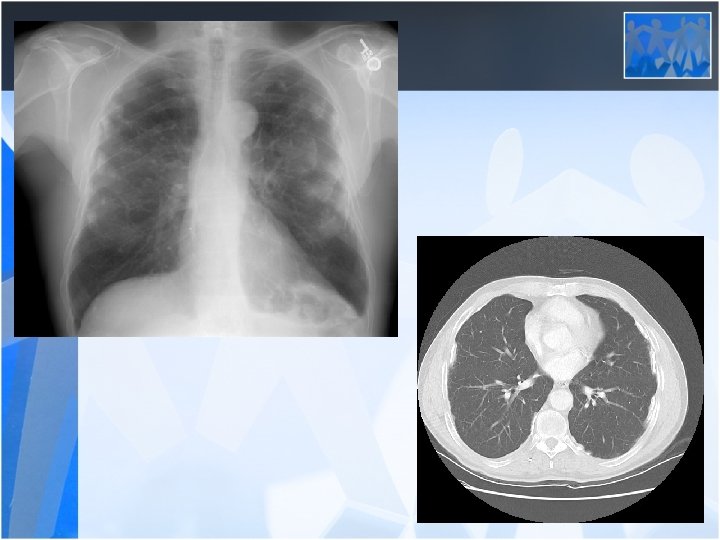
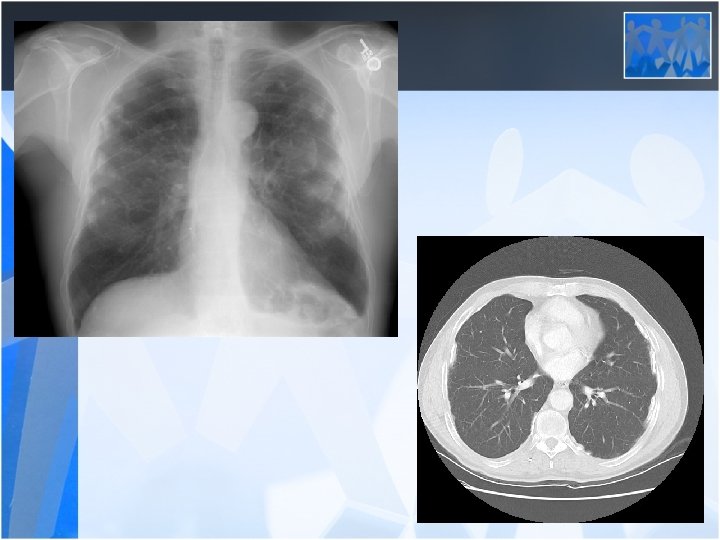
Asbestosis (Diffuse Interstitial Fibrosis) • Most patients asymptomatic 20 -30 years after first exposure • Dyspnea with exertion-progression even in the absence of further asbestos exposure. • Bibasilar, fine end-inspiratory crackles • Corpulmonale may ensue in advanced cases • PFT: Reduced lung volumes, particularly the vital capacity and total lung capacity; diminished DLCO • Cigarette smoke may accelerate the progression of pulmonary fibrosis after asbestos exposure
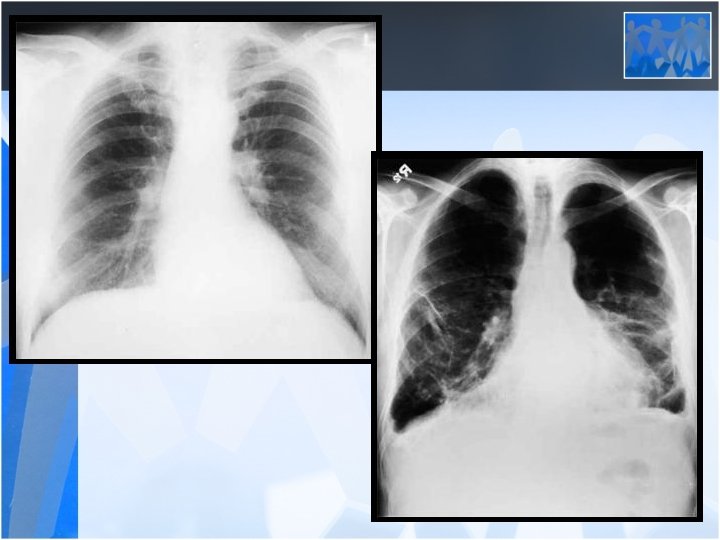
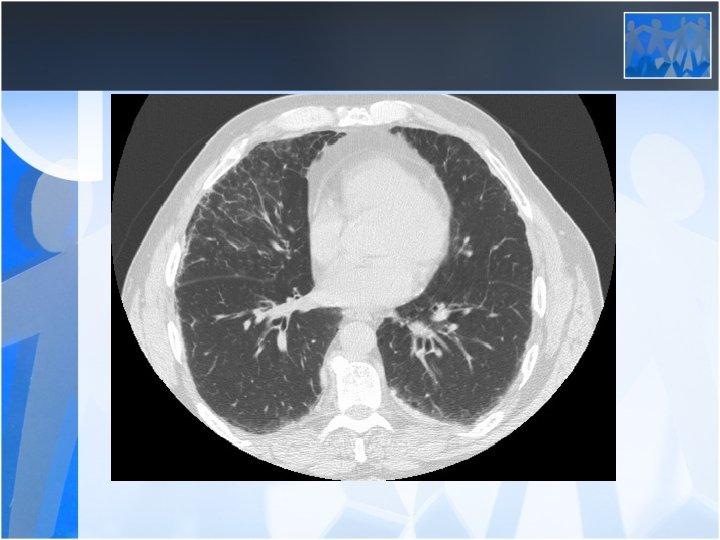
Pleural Plaques • Hyalinised pleural plaques with sharp endings and calcification localised in parietal pleura • Usually first localized on diaphragmatic pleura and lower zone • Asymptomatic • 10 -20 years after exposure
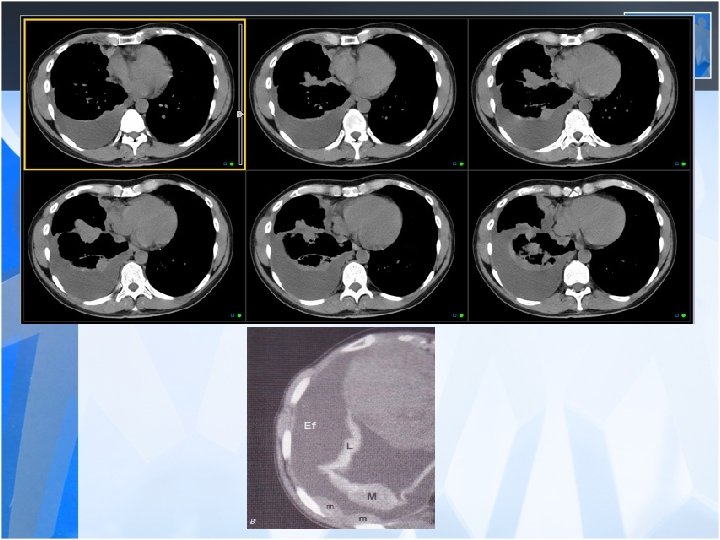
Pleural effusion • Benign pleural effusion – – Latent period 10 -20 years Exudative Asymtomatic Diagnosis by excluding other causes and history of exposure • Malign mesothelioma – The lifetime risk of developing mesothelioma among asbestos workers is thought to be as high as 10 percent. – There is a long latency of approximately 30 to 40 years from the time of asbestos exposure to the development of mesothelioma.
Lung Cancer • Asbestos exposure in the absence of a smoking history is associated with a 6 fold relative risk of lung cancer • Combined exposure to asbestos and cigarette smoke appears to be multiplicative.
Malign Mesothelioma Environmental, nonoccupational exposure to asbestos and erionite (another fibrous zeolite) also can contribute to an increased risk of mesothelioma. In certain rural areas in Greece, Turkey (Erionite in Ürgüp, Göreme region), and Bulgaria, soil contains remarkably high levels of tremolite asbestos fibers, and many cases of mesothelioma in these regions
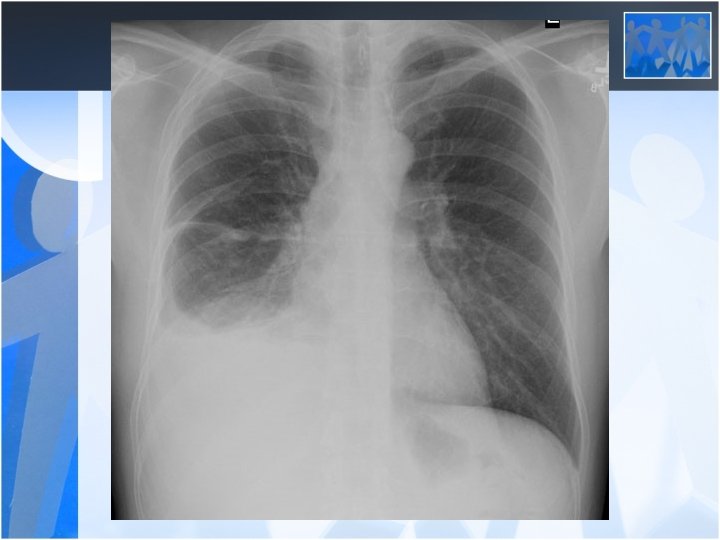
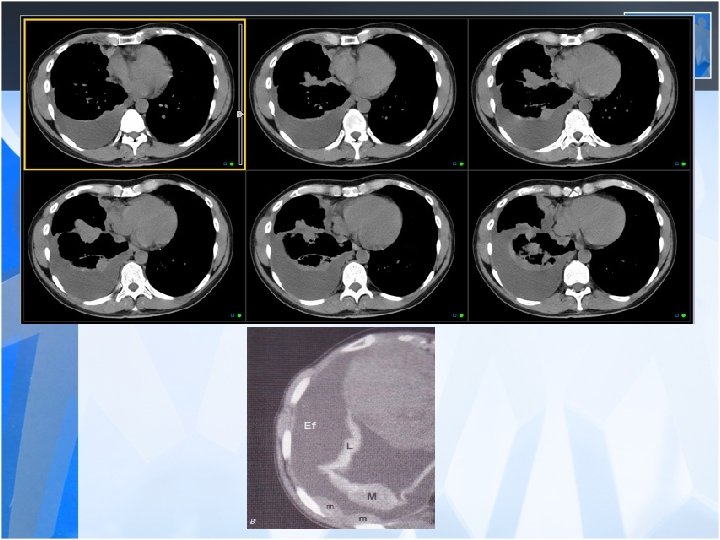
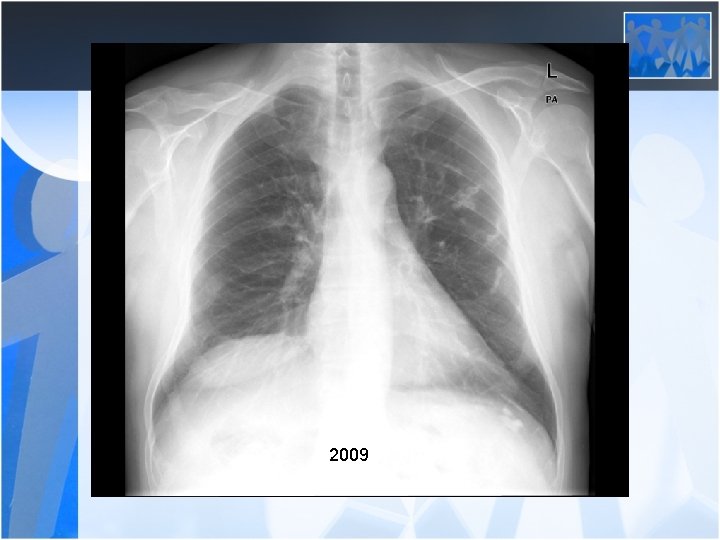
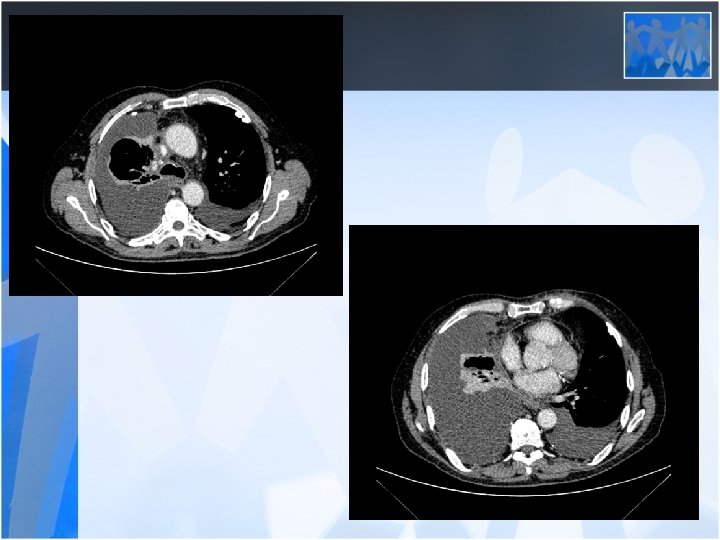
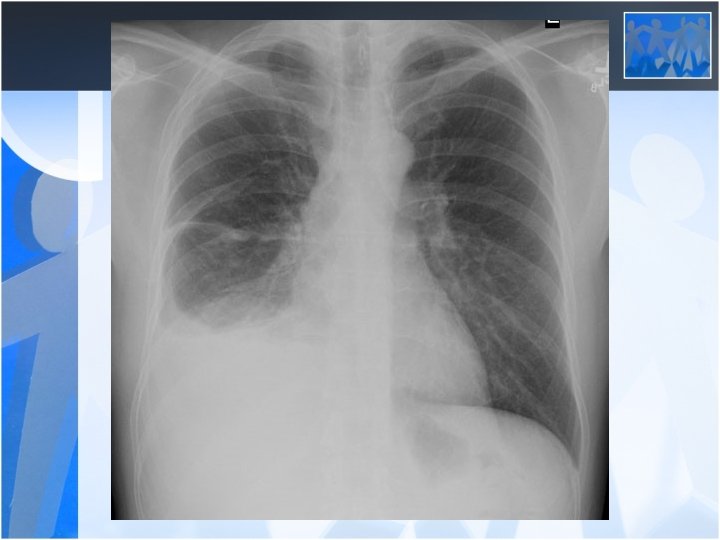
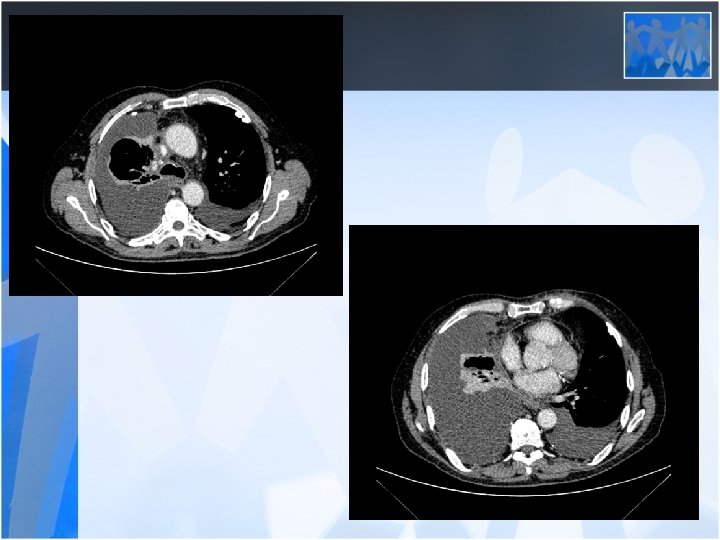
• The most common clinical presentations are dyspnea, chest pain, unilateral decreased volume of the affected hemithorax (frozen chest) • Nodular thickening of the pleura, irregular thickening of the interlobar fissure, absence of mediastinal shift with massive pleural effusion (frozen chest) • Diagnosis by histologic examination • Treatment oncologic and surgical if possible, prognosis is poor
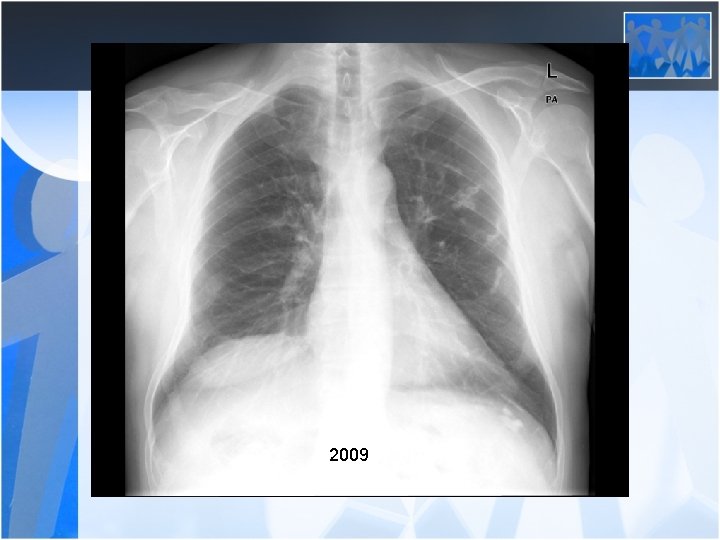
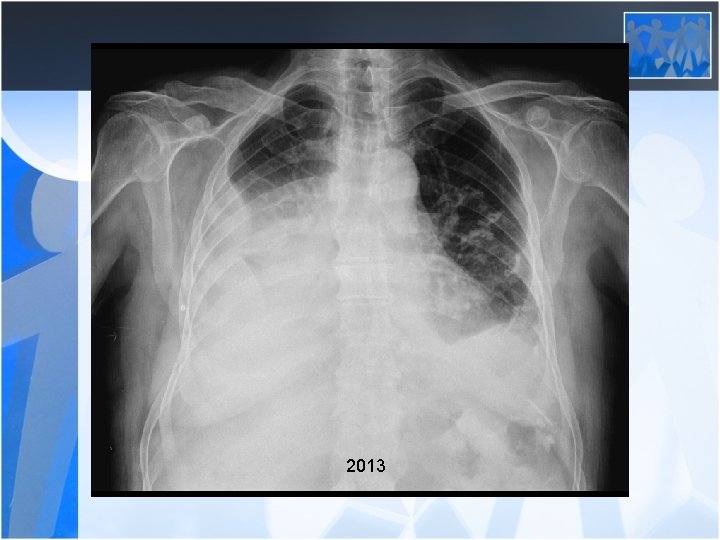
2009
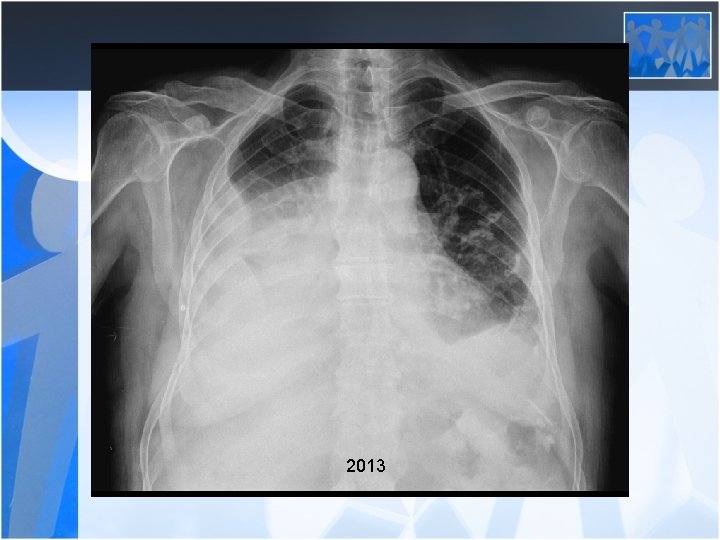
2013
Organic Dust Exposure • Byssinosis – Seen in cotton workers due to cotton and flax dust (endotoxins, immunologic mechanisms? ) – Divided into Acute and Chronic form – Acute Byssinosis: several degree of acute airway response (hyperreactivity) to cotton dust on first exposure (may cause an accelerated decline in lung function-COPD)
• Chronic Byssinosis (Classical form) – Chest tightness and difficulty in breathing on the first day of work (Monday fever) – Latent period is around 5 -6 years – Symptoms progress and becomes all week long by time ends with a COPD like disease – There is no specific chemical or radiologic sign – PFT (a decrease of 150 -200 ml in FEV 1 or FVC on the evening of mondays
Hypersensitivity Pneumonia (Extrinsic Allergic Alveolitis) • A disease that arises from hypersensitivity to inhaled organic dust and inflamatory response confined to lungs • Also known as farmers lung • Spectrum of the clinical illness varies which probably reflects factors specific to the individual, frequency and degree of exposure
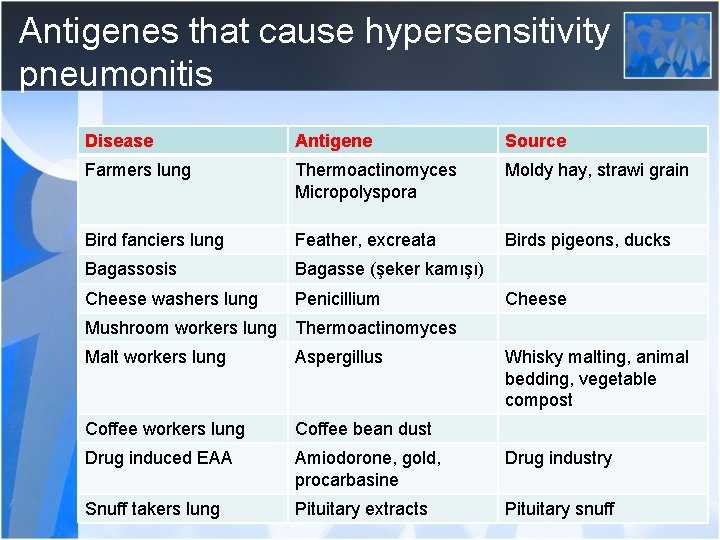
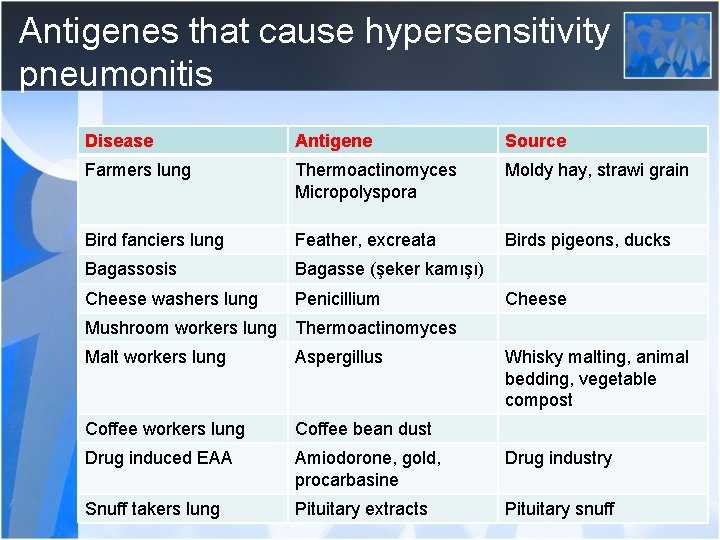
Antigenes that cause hypersensitivity pneumonitis Disease Antigene Source Farmers lung Thermoactinomyces Micropolyspora Moldy hay, strawi grain Bird fanciers lung Feather, excreata Birds pigeons, ducks Bagassosis Bagasse (şeker kamışı) Cheese washers lung Penicillium Cheese Mushroom workers lung Thermoactinomyces Malt workers lung Aspergillus Whisky malting, animal bedding, vegetable compost Coffee workers lung Coffee bean dust Drug induced EAA Amiodorone, gold, procarbasine Drug industry Snuff takers lung Pituitary extracts Pituitary snuff
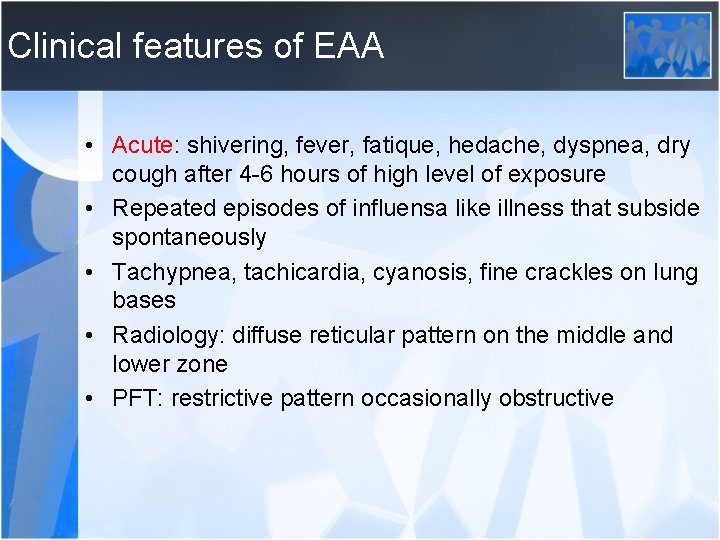
Clinical features of EAA • Acute: shivering, fever, fatique, hedache, dyspnea, dry cough after 4 -6 hours of high level of exposure • Repeated episodes of influensa like illness that subside spontaneously • Tachypnea, tachicardia, cyanosis, fine crackles on lung bases • Radiology: diffuse reticular pattern on the middle and lower zone • PFT: restrictive pattern occasionally obstructive
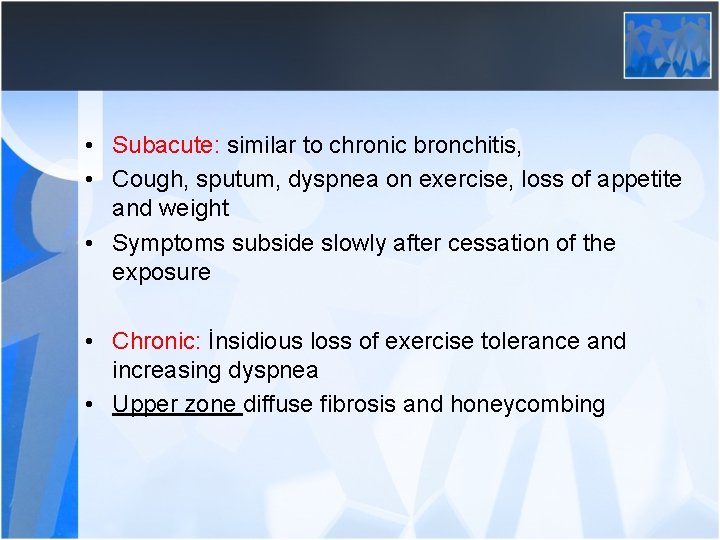
• Subacute: similar to chronic bronchitis, • Cough, sputum, dyspnea on exercise, loss of appetite and weight • Symptoms subside slowly after cessation of the exposure • Chronic: İnsidious loss of exercise tolerance and increasing dyspnea • Upper zone diffuse fibrosis and honeycombing
Treatment • Avoid exposure • Prednisolone • Supportive care
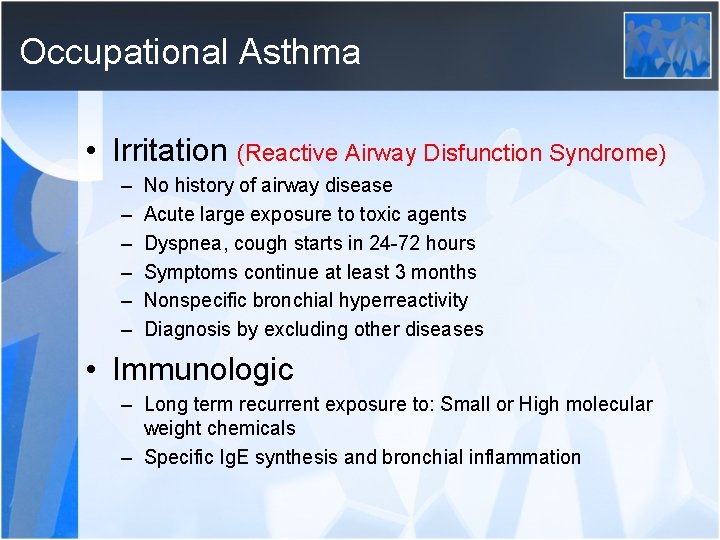
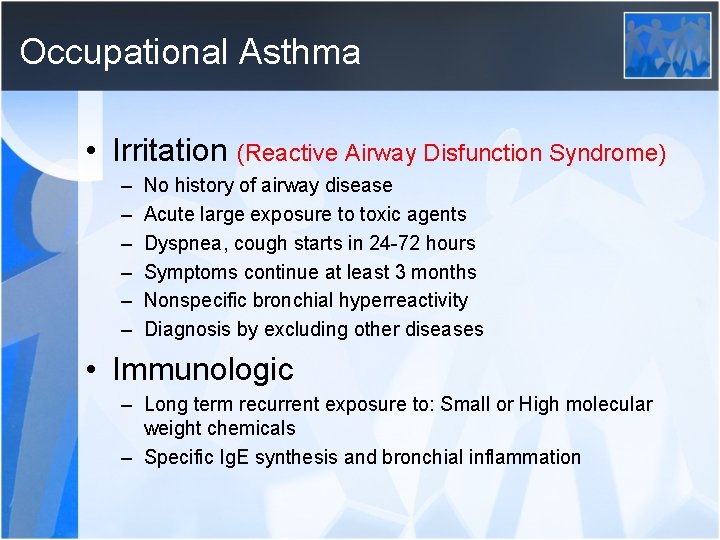
Occupational Asthma • Irritation (Reactive Airway Disfunction Syndrome) – – – No history of airway disease Acute large exposure to toxic agents Dyspnea, cough starts in 24 -72 hours Symptoms continue at least 3 months Nonspecific bronchial hyperreactivity Diagnosis by excluding other diseases • Immunologic – Long term recurrent exposure to: Small or High molecular weight chemicals – Specific Ig. E synthesis and bronchial inflammation
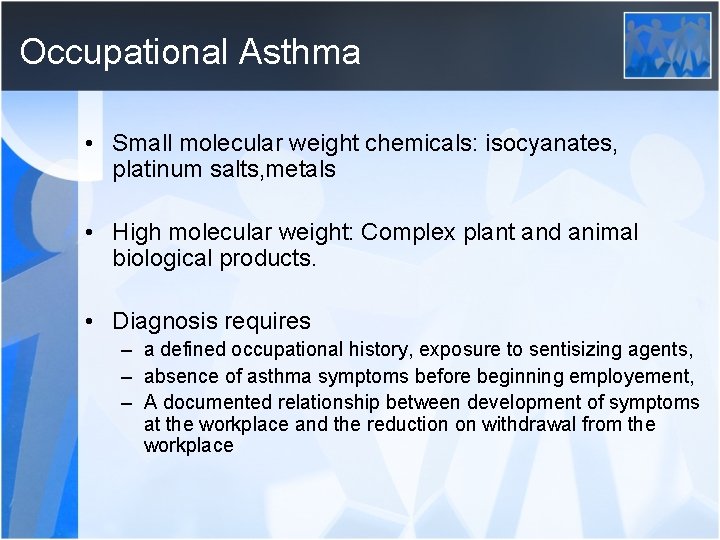
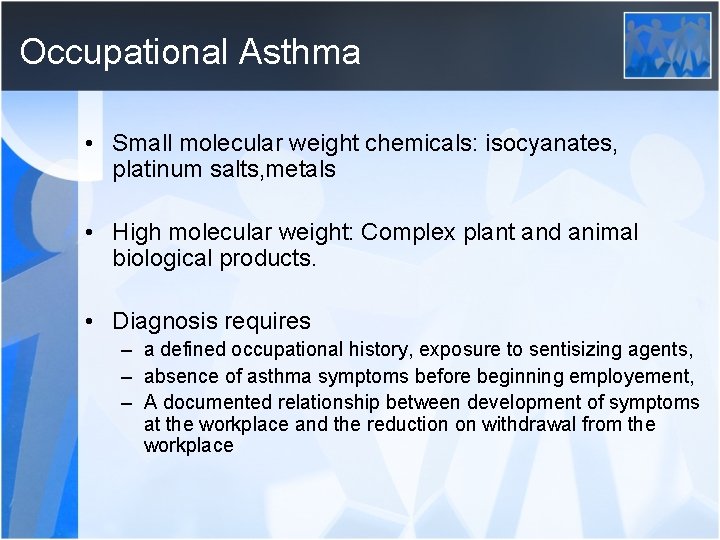
Occupational Asthma • Small molecular weight chemicals: isocyanates, platinum salts, metals • High molecular weight: Complex plant and animal biological products. • Diagnosis requires – a defined occupational history, exposure to sentisizing agents, – absence of asthma symptoms before beginning employement, – A documented relationship between development of symptoms at the workplace and the reduction on withdrawal from the workplace
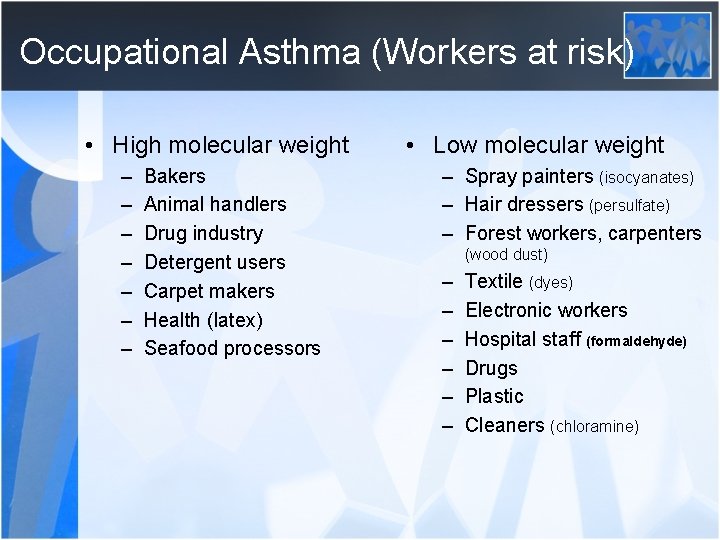
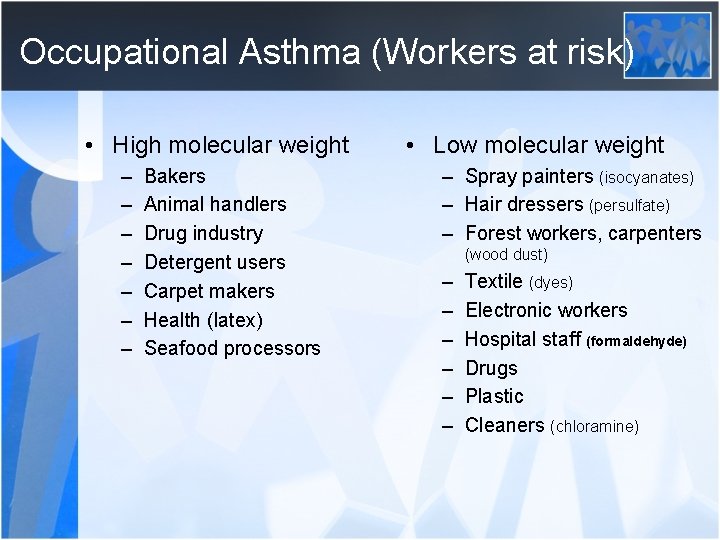
Occupational Asthma (Workers at risk) • High molecular weight – – – – Bakers Animal handlers Drug industry Detergent users Carpet makers Health (latex) Seafood processors • Low molecular weight – Spray painters (isocyanates) – Hair dressers (persulfate) – Forest workers, carpenters (wood dust) – – – Textile (dyes) Electronic workers Hospital staff (formaldehyde) Drugs Plastic Cleaners (chloramine)
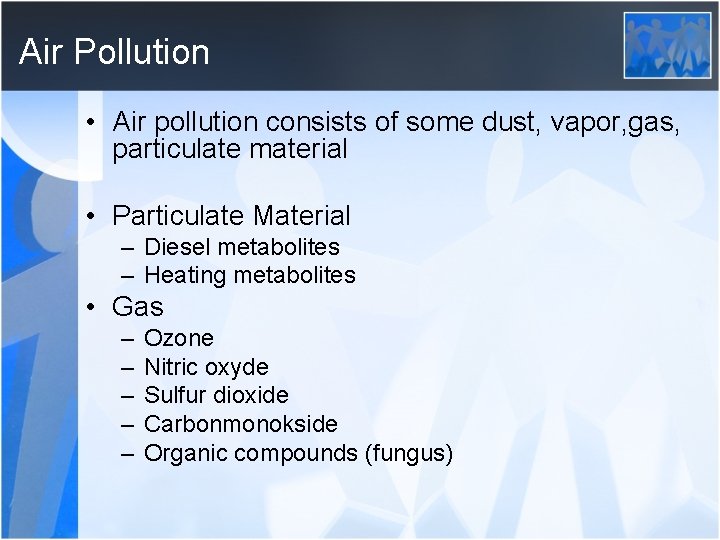
Air Pollution • Air pollution consists of some dust, vapor, gas, particulate material • Particulate Material – Diesel metabolites – Heating metabolites • Gas – – – Ozone Nitric oxyde Sulfur dioxide Carbonmonokside Organic compounds (fungus)
Effects of air polution • Increase the incidence of bronchiolitis, pneumonia, tuberculosis in children and adults as the functions of alveoler macropages are inhibited • Global warming, climatic and echologic changes influence the emergence of infectious diseases both in children and in adults • Low birth weight, impaired intrauterine growth. Adverse effects on lung development in children cause decreased lung function
• Irritating effects can cause airway muscle spasm and attacks in patients with obstructive lung diseases (Asthma, COPD) • Increased mortality of asthma • Increased incidence of COPD • Increased incidence of lung cancer (oxidative stress, impaired cellular repair mechanisms) • Increased incidence of cardiovascular diseases (increased blood viscosity, vasoconstructor activity) • Cellular damage may lead to fibrosis (ILD)