Diseases of the Musculoskeletal System Chapter 37 Skeletal









- Slides: 34
Diseases of the Musculoskeletal System Chapter 37
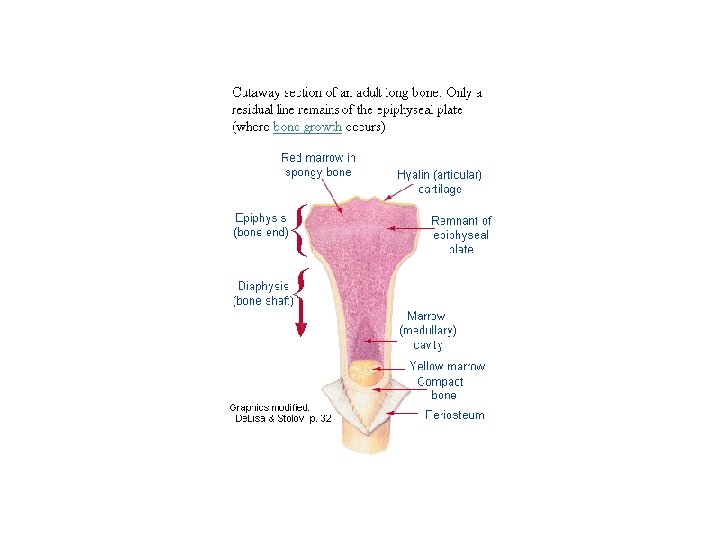
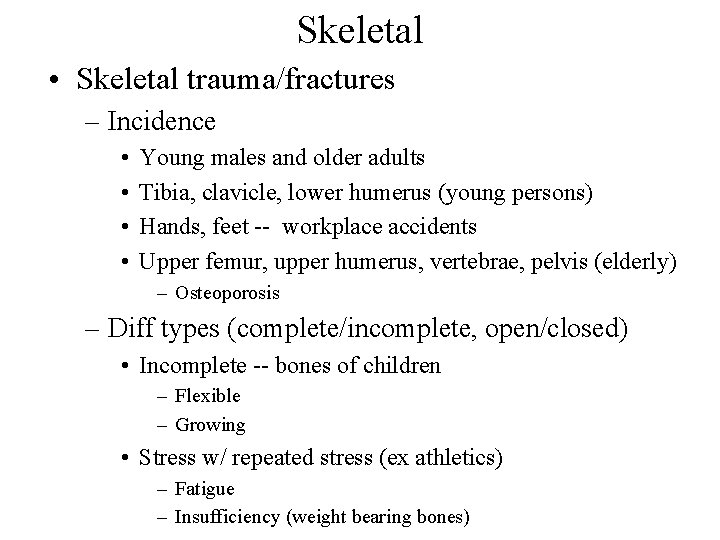
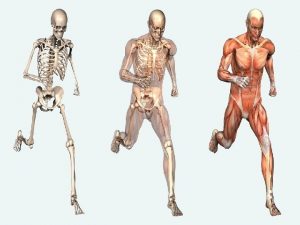
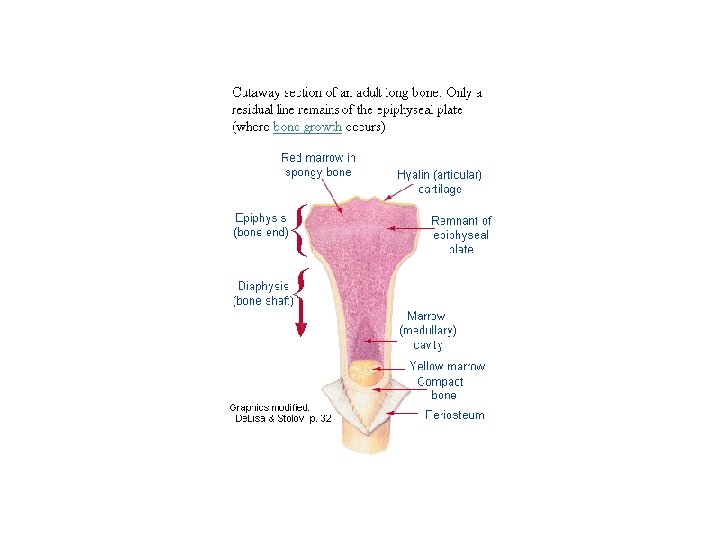
Skeletal • Skeletal trauma/fractures – Incidence • • Young males and older adults Tibia, clavicle, lower humerus (young persons) Hands, feet -- workplace accidents Upper femur, upper humerus, vertebrae, pelvis (elderly) – Osteoporosis – Diff types (complete/incomplete, open/closed) • Incomplete -- bones of children – Flexible – Growing • Stress w/ repeated stress (ex athletics) – Fatigue – Insufficiency (weight bearing bones)

- Pathophysiology • Healing similar to soft-tissue injuries stages – No scar tissue • Periosteum, blood vessels disrupted • Bleeding clot form=n (hematoma) • Stages – Hematoma – Procallus form=n » Intense inflammatory response » Fibroblasts, collagen, growth factors, osteoblasts impt – Callus » Hardened membr (woven bone) – Remodeling » Osteoclasts; original shape » Resorption unneeded callus


– Clinical • Signs/symptoms – – – Impaired function Unnatural alignment; possible rotation, angulation Swelling Tenderness Severe pain (trauma, muscle spasm) • Stress fractures -- pain with accelerated remodeling – Relieved by rest – Treatment • Realign to normal position (manipulation, traction) • Surgery – Prosthesis, screw, plate, etc. , possible • Splints, casts
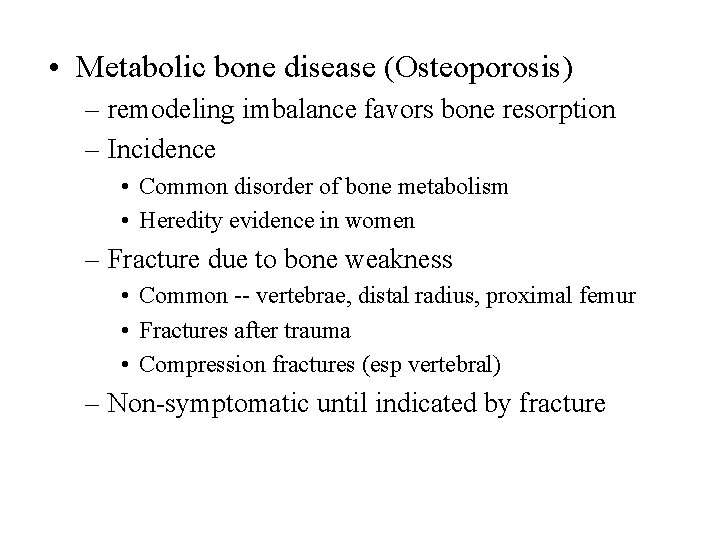
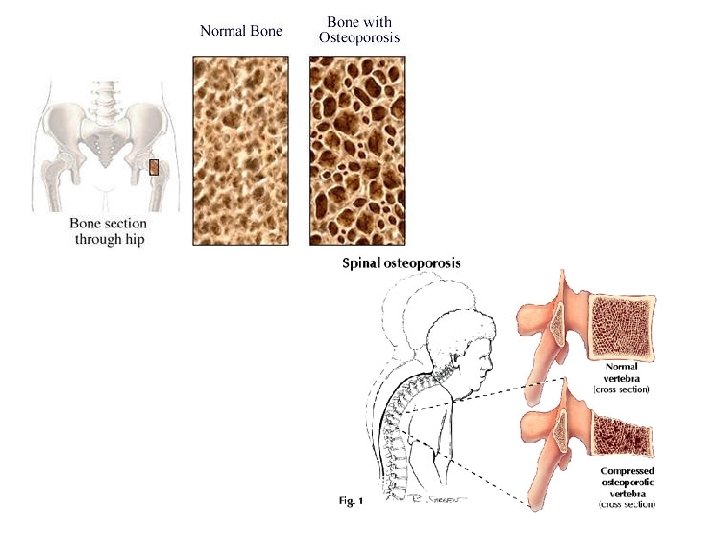
• Metabolic bone disease (Osteoporosis) – remodeling imbalance favors bone resorption – Incidence • Common disorder of bone metabolism • Heredity evidence in women – Fracture due to bone weakness • Common -- vertebrae, distal radius, proximal femur • Fractures after trauma • Compression fractures (esp vertebral) – Non-symptomatic until indicated by fracture
– Pathophysiology • Age – Bone resorption exceeding bone growth – Net bone mass loss – More rapid in women » Exaggerated at menopause » Type I (Postmenopausal) – Type II C both sexes over age 70 » Neck, hip, humerus, tibia • May involve postaglandins, interleukins, various growth factors that affect osteoclasts • Estrogen decr w/ menopause incr=d risk – Estrogen inhibits bone resorption – Also in young, female athletes » Training decr=d estrogen » Found decr=d bone mass, incr’d fractures
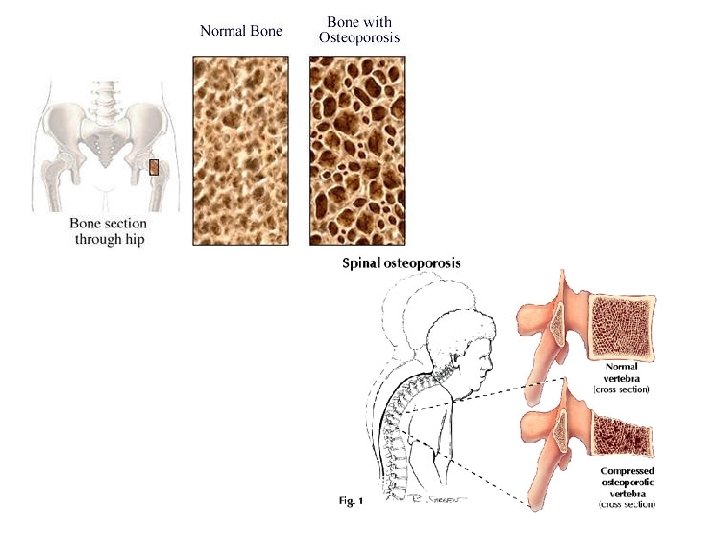
– Clinical • • Pain Bone deformity Fractures Vertebral collapse hunchback, decr=d height – Treatment C slow rate of Ca, bone loss • Incr dietary Ca • Vit D incr intestinal abs=n Ca • Regular, moderate exercise • Hormone treatment (estrogen, progesterone) • Reduce risk of falls
• Bone tumors – Common secondary tumor site • Primary often prostate, breast, thyroid, lung, kidney • Access through blood • Often axial skeleton (not skull), proximal femur, humerus • May induce bone breakdown or bone growth
– Primary tumors less common • • Actively growing bone Pain early indication May bone weakening Pressure adjacent bone deformed by abnormal remodeling • Metastasis often to lung • Most more in males than females – About 1/3 primary tumors benign • Ex: osteoma of skull and osteoid osteoma of long bone • Ex: chondroblastoma – Arises in cartilage of epiphyses of arm, leg bones – Rare
– Malignant bone tumors • Osteogenic sarcoma (=osteosarcoma) most common – – – Usually age 10 -20 years Knee often Common metastasis lung Previous metastasis by time of diagnosis poor prognosis Now better chemotherapy (80% 5 yr recovery rate) Surgery often • Chondrosarcoma – – – Usually age 30 -50 yrs Slow-growing May break through bone surface Interior of pelvis, ribs, prox femur, humerus Surgical excision

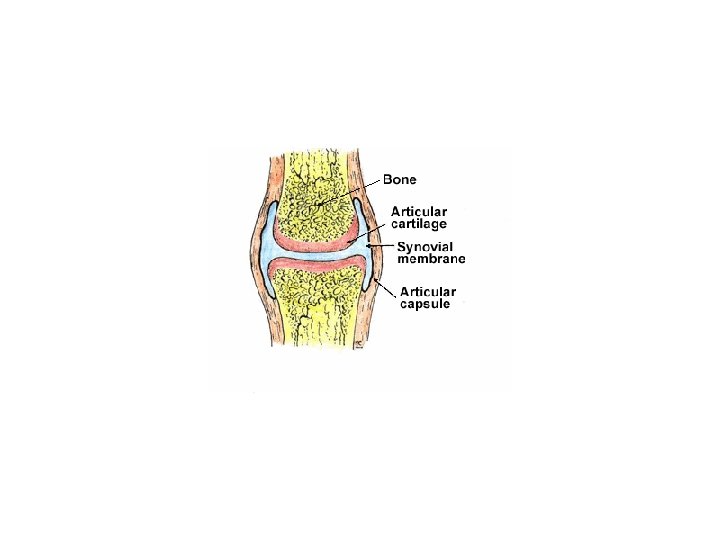
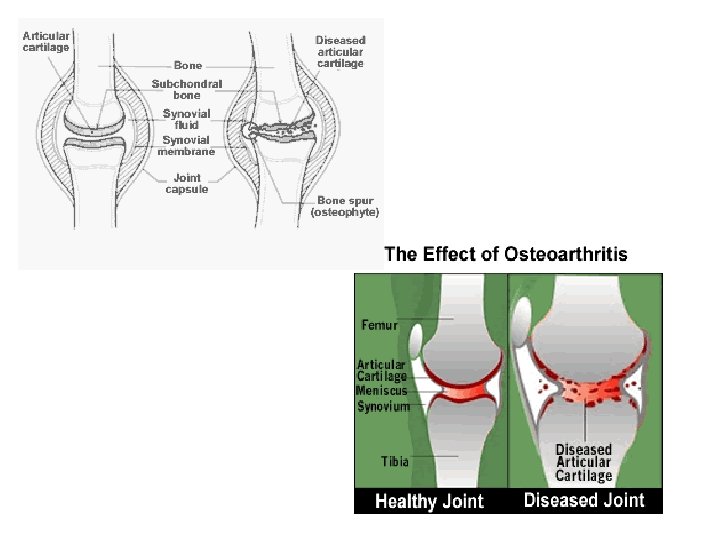
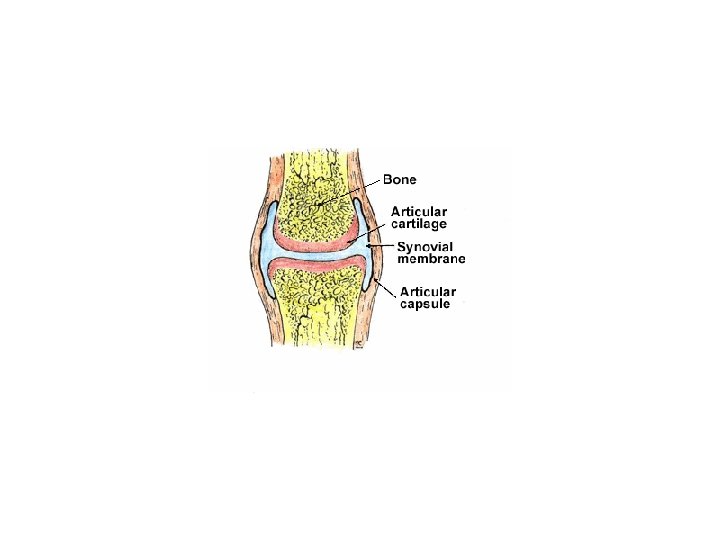
Diseases of the Joints • Osteoarthritis = Degenerative Joint Disease – Incidence • Most common joint disease in US • Incr=s w/ age – Age 60 -- most affected – > 75 yrs -- 85% affected – Pathophysiology • Articular cartilage becomes thin, irregular, frayed – Probably enz breakdown of cartilage • Cracks, fissures in articular cartilage – Fill w/ synovial fluid
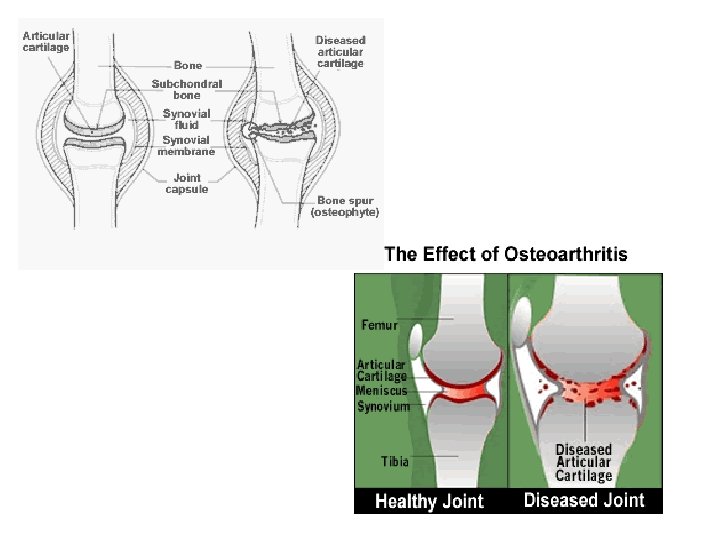
– Pathophys (cont’d) • Penetrates to underlying bone w/ progression – May fluid-filled cysts – Bone forms around cysts – May microfractures • Fibrocartilage plugs form for repair – Activyt plugs stripped away, then reformed, then restripped – Smooth bone surface • Fibrocartilage fragments may react at synovial membr surface – inflamm response C> repair – decr=d movement • Cells in synovial membr may dev into osteoblasts – form=n bone spurs at joint – pain, decr=d movement
– Degeneration • Mostly at larger weight-bearing joints (also fingers) • Related to – – Wear-and-tear OR Biochem defect in joint cartilage OR Excessive loading (malformed joint, postural defect, obesity) OR Genetic – Clinical • Joint aches, stiffness – Incr w/ activity; diminish w/ rest • Progression w/ age • Loss of mobility if hip, knee affected – Therapy limited • Analgesics for pain • Reduce obvious stresses • Surgical removal of bone spurs or artificial joint replacement

• Rheumatoid arthritis C systemic disease involving joints – Incidence • About 1% adult pop=n affected • 3 female: 1 male • Age of onset usually 20 -30 (but also infancy 90's) • May be due to – Infection – Autoimmune disorder – Genetic predisposition

– Get immune-mediated destruction of joints • Environmental stimulus immune response to Ag • If predisposed, Ab=s transform to Arheumatoid factors@ (Rfs) • Rfs complex in blood, synovial fluid inflamm response at joint • Inflamm mediators breakdown joint tissue destroyed
– Get pattern of chronic inflamm=n • Incr=d number of cells in synovium • Thickening of synovium (maybe after cartilage destroyed by inflamm=n process) • Thickened synovium covers adjacent joint surfaces – Over time may enlarge, fill joint space – In late stage = ankylosis = fused joint • Causes swelling; stiffness; pain • Swelling also due to incr=d exudate in synovial membr – Joint deformities • Loss of joint motion • Muscular atrophy

– Sytemic effects variable • Generalized weakness, malaise • Rheumatoid nodules form – – Focal subcu swelling Elbow, heel, dorsal surface of head; also internal Made of macrophages, lymphocytes, collagen, cell debris Typically painless • Rheumatoid vasculitis common – Systemic inflamm=n of blood vessels – May involve pericardium, pleural effusion – Therapy C no cure; can’t reverse destruction of structures • Relieve pain, reduce swelling (antiinflammatories) • Reduce stress • Strengthen assoc=d muscles • Replace severely effected joints
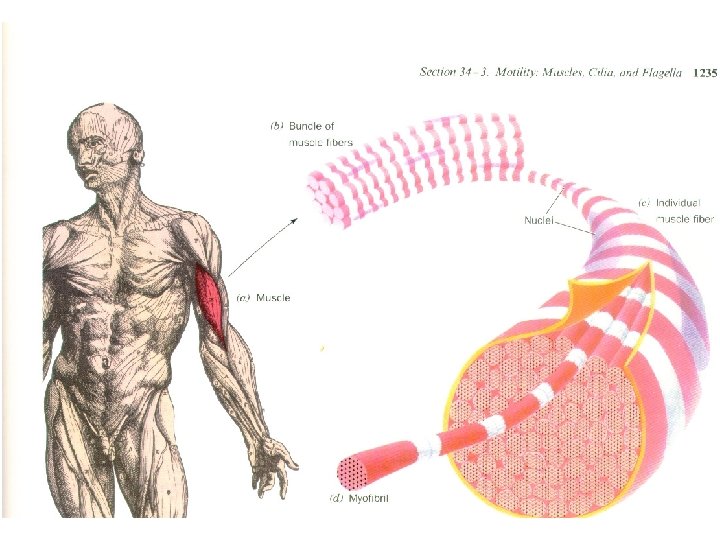
Diseases of Skeletal Muscle • Disuse atrophy – Pathologic reduction in size of muscle fibers • Follows prolonged bed rest, trauma, nerve damage – Muscle strength decr=s from baseline • About 3% per day – To prevent • Frequent isometric muscle contractions • Passive lengthening exercise – If no reuse in 1 year, regen=n muscle fibers impaired
• Fibromyalgia – Chronic musculoskel syndrome – Get diffuse chronic pain, tenderness w/ no inflamm=n, fatigue • Tenderness @ 9 common points in body (neck, shoulders, hips, knees) • Profound fatigue • May depression • Also migraine, irritable bowel disease common – Incidence • Mostly women • Peak age = 30 -50 yrs • Increases w/ age
– Probably several causes • virus, • Phys/emotional trauma, • medication – Found metab alterations in muscle • May pain, fatigue – Also found diff blood flow to thalamus • May C> chronic stress response – Treatment • Antiinflammatories (not very effective) • CNS active agents somewhat helpful

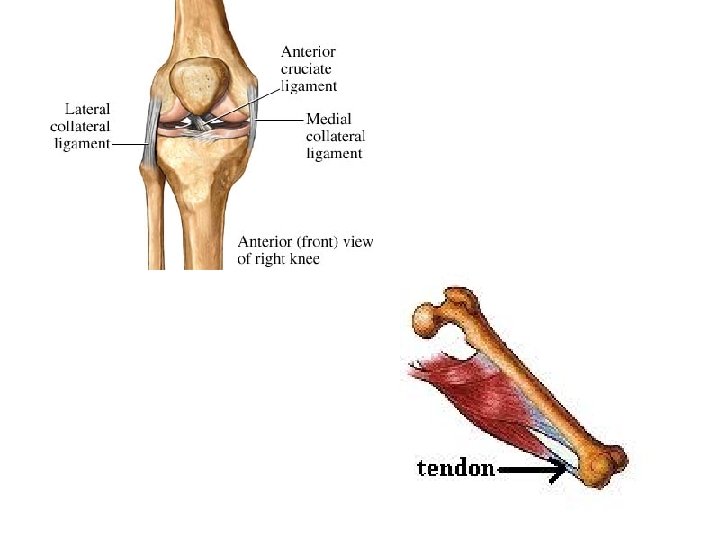
• Muscle Strains – Gen’l term for muscle damage – Seen after traumatic, sports injuries • Sudden, forced motion • Muscle becomes stretched beyond normal length • May include wounds – Often involves tendon also – May include hemorrhage, inflamm=n – Muscle cells usually regenerate in up to 6 weeks – Treatment • • Ice relieves swelling Analgesics Alternating heat/cold if more severe form Surgery, immobilization if tearing, bleeding
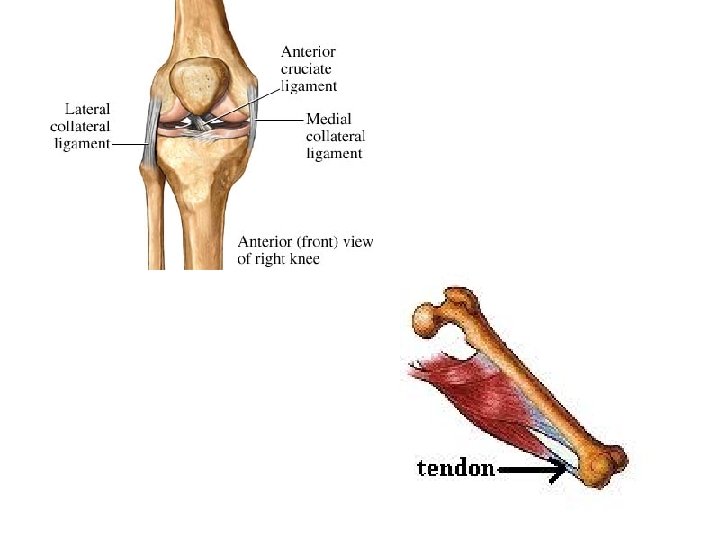
Musculoskeletal Disorders • May accompany fractures, dislocations • Ligament = fibrous connective tissue band joining bones @ joint – Needed to support bones, joints • Strain = tear in tendon – May be due to major trauma – Also spontaneous w/ corticosteroid admin, rheumatoid arthritis, lupus
– Common sites • • • Tendons of hands, feet Knee Upper arm - w/ lifting excess wt Thigh Ankle Heel - w/ forced flexion • Sprain = tear in ligament – Common sites • • Wrist Ankle Elbow Knee
– Avulsion = total sep=n tendon/ligament from bone • Due to abnormal stress • Young athletes (sprinters, hurdlers, runners) – Pathophysiology • • Tearing inflamm response Exudate forms @ torn ends Macrophages, fibroblasts Repair – Collagen form=n random, then organized – Vascular fibrous tissue fuses new, old tissues – Healing tendon separates from surrounding soft tissue – Can=t support strong pull for 4 -5 weeks

• Clinical – Pain C sharp, localized – Soft-tissue swelling – Joint swelling – Flexion deformities – If in extremities, motion affected • Treatment – Suture tendon/ligament – Tendon/ligament grafting
 Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Diseases of the musculoskeletal system
Diseases of the musculoskeletal system The musculoskeletal system chapter 21
The musculoskeletal system chapter 21 Chapter 15 musculoskeletal system
Chapter 15 musculoskeletal system Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 10 diseases of lymphatic system
10 diseases of lymphatic system Types of joint movement
Types of joint movement Unit 41 musculoskeletal system
Unit 41 musculoskeletal system Musculoskeletal system
Musculoskeletal system Language
Language Assessment of the musculoskeletal system
Assessment of the musculoskeletal system Muscle strength scale
Muscle strength scale Musculoskeletal system
Musculoskeletal system Objective data for musculoskeletal system
Objective data for musculoskeletal system Chapter 40 musculoskeletal care modalities
Chapter 40 musculoskeletal care modalities Buck's extension traction
Buck's extension traction Skeletal system
Skeletal system Chapter three skeletal system answer key
Chapter three skeletal system answer key 7:4 skeletal system
7:4 skeletal system Chapter 5 the skeletal system
Chapter 5 the skeletal system 2009 delmar cengage learning
2009 delmar cengage learning Lamina bone
Lamina bone Chapter 32 section 2 the skeletal system answer key
Chapter 32 section 2 the skeletal system answer key Chapter 8 skeletal system
Chapter 8 skeletal system Chapter 7 4 skeletal system
Chapter 7 4 skeletal system Chapter 5 the skeletal system figure 5-10
Chapter 5 the skeletal system figure 5-10 Chapter 5 the skeletal system figure 5-13
Chapter 5 the skeletal system figure 5-13 Chapter 5 the skeletal system figure 5-13
Chapter 5 the skeletal system figure 5-13 Hyoid bone lecture
Hyoid bone lecture Chapter 5 the skeletal system
Chapter 5 the skeletal system Receive
Receive Chapter 3 the skeletal system labeling exercises
Chapter 3 the skeletal system labeling exercises Chapter 5 the skeletal system figure 5-10
Chapter 5 the skeletal system figure 5-10