PLEURAL DISEASES Pleural Effusion Incidence 300 cases 100
- Slides: 41
PLEURAL DISEASES
Pleural Effusion • Incidence: ≈ 300 cases / 100, 000 population annually • Approximately 25% of all consultations in Pulmonary Medicine service concern pleural diseases • Cardiac failure, parapneumonic and malignant effusions are the most common causes
Pleural effusion is • an abnormal collection of fluid in the pleural space.
Mechanisms of such accumulation may be traced as follows: (1) An increase in the capillary hydrostatic pressure. (2) A decrease in the plasma oncotic pressure. (3) An increase in the rate of filtration across the parietal pleura. (4) A decrease in the rate of resorption of the pleural effusion. (5) A decrease in the negative pressure within the pleural space. (6) An increase in the permeability of the pleural capillaries. (7) Impairment of lymphatic drainage of the pleura. (8) Abnormal sites of entry e. g. passage of fluid from the peritoneal space through macro-diaphragmatic pores (as in hepatic hydrothorax) or misplaced central venous line.
ETIOLOGY: 1 - Transudates: • Congestive Heart Failure , Liver cirrhosis, Malnutrition, Hypoprotienemia, Myxoedema, Nephrotic Syndrome, Meig’s syndrome, Superior vena cava syndrome, Consrtictive pericarditis, and Fluid from peritoneal cavity
2 - Exudates: • Malignant Pleural Effusion, Infectious Diseases (TB, PN), Pulmonary Embolism (Infraction), Collagen Vascular Diseases (RA), Sarcoidosis, Uraemia, Drug-Induced Pleural Diseases, Radiation Therapy, Pancrititis, and Meig’s syndrome
Light's criteria • To determine the origin of effusion, a classic and useful distinction is that between transudate and exudate. Pleural fluid is likely exudates if one or more of the following Light's criteria are met: • (1) Pleural fluid protein / serum protein ratio > 0. 5 • (2) Pleural fluid LDH / serum LDH ratio > 0. 6 • (3) Pleural fluid LDH is more than two thirds the upper limit of the normal serum range.
Serum-pleural fluid albumin gradient • Serum-pleural fluid albumin gradient may be the most useful way to distinguish transudates from exudates in patients with congestive heart failure who have undergone diuresis. A gradient > 1. 2 g/ dl is indicative of a transudate.
DIAGNOSTIC APPROACHES • CLINICAL PRESENTATIONS • IMAGING STUDIES
Clinical picture • Symptoms • Stage of pleurisy: • Pleuretic chest pain : Stitching in character , Increase severity with inspiration , cough , Decreased on lying on the diseased side and Diaphragmatic pleurisy radiates to the shoulder • Fever : inflammatory causes
• Stage of pleural fluid accumulation : • Pleural pain disappear • Dull aching pain • Fever: inflammatory causes • Dyspnea : mild to severe with massive effusion Increased on lying on normal side (trepopnea) • Cough (dry)
Signs Inspection: limited movement • Decreased or absent litten `s sign wider half of the subcostal angle Palpation decreased TVF and limited movement Percussion Stony dullness Hyperresonance above effusion : Skodiac resonance Grocco`s triangle: dullness over paravertebral triangle on the opposite side • Dullness of the Traube`s area : left pleural effusion • • •
• • • • Mediastinal shift (tracheal shift) Shift to the opposite side → large effusion Central mediastinum with massive effusion: underlying atelectasis fixation of the mediastinum → LN , malignant infiltrations Auscultation Decreased intensity of breath sound, VR Pleural rub : pleurisy Bronchial breathing– Garlen`s triangle Underlying consolidation Over effusion in children Aegophony In Hydropneumothorax----- shifting dullness , succussion splash Neglected Cases ------Fibrothorax
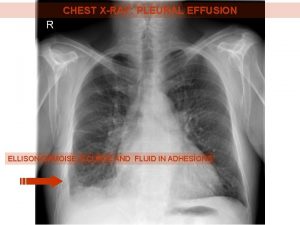
• • • IMAGING STUDIES : Chest X-ray small effusion: 300 -500 ----obliteration of costophrenic angle lateral decubitus : for little amount of effusion layered along dependent chest wall Large effusion → homogenous opacity rising to the axilla Massive effusion → ( occupies 2/3 of hemithorax( up to the 2 nd rib) Subpulmonic Effusion → elevated copula of diaphragm loculated effusion → D shape interlobar effusion → elliptical opacity along the course of fissure (CHF) Hydropneumothorax → (Airfluid level)
• CT scan • Visualize Underlying pathology , Identify loculated effusion, Measurment of pleural thickness, Identify bronchopleural fistula and Visualize small pneumothorax • Ultrasonography • diagnosis of subpulmonic effusion, helpful to locate small amounts , Detect loculated effusion
• • • • Diagnostic Thoracentesis -Tests ( pleural fluid analysis) physical examination Shape &colour straw : transudate- some exudates Turbid : empyema Haemorrhagic effusion Milky Studies to differentiate transudate from exudate : pleural fluid LDH, total protein & possibly albumin Studies to help sort out an exudate: cell count & differential, Neutrophils empyema, early TB, pulmonary infarct Lymphocyte TB, malignancy basophils –leukemic infiltration
• Lab Tests: • CEA, PRO-BNP, Mesothelin, RA, ANA • PLEURAL BIOPSY: • • • ABRAM’S OR COPE’S NEEDLE US or CT GUIDED TRANSTHORACIC BIOPSY MEDICAL THORACOSCOPY Video Assisted Thoracoscopy (VATS) OPEN PLEURAL BIOPSY • BRONCHOSCOPY (endobronchial mass, TB)
Chylous pleural effusion: • Excess fat ( triglyceride), Stain red with sudan III, Dissolve in ether • Causes: • Injury to thoracic duct (surgery, trauma) • Obstruction of TD ( lymphoma, filariasis) • Congenital abnormality • Treatment: Ligation of TD.
Chyliform pleural effusion: • Excess cholesterol, Not stained red with sudan III, Not dissolved in ether • Causes: • Chronic pleural effusion Hypercholestermia
Haemothorax • Haemorraghic pleural effusion: Blunt or penetrating trauma, Hct fluid/blood ≥ 0. 5, Will coagulate lead to fibrothorax or empyema, If small will defibiranate and remain free flowing. • Treatment: ICT Drainage.
Indications for aspiration: • • Massive effusion → severe dyspnea 2 nd infection → resisting treatment Haemothorax Empyema, complicated parapeumonic effusion (Ph <7. 1, LDH >1000 IU/ L)
• • Treatment of the cause TB effusion full anti-TB treatment corticosteroids for 3 -4 weeks → help → reabsorption of fluid & decrease deposition of fibrous tissues
Malignant effusion Cytotoxic drugs Aspiration & pleurodesis Pleurodesis : injection of sclerosing agent into the pleural space to promote adhesions between parietal and visceral pl---prevent re-accumulation of fluid • Chest tube • Tetracyclin, bleomycin talc, doxycyclin • •
• Parapneumonic effusion • Uncomplicated eff → proper antibiotics • Complicated eff → antibiotics + closed chest tube drainage under water seal • if still drain → open drainage with rib resection • Decortication : if unable to achieve drainage & lung is trapped in fibrinous peel • Bronchopleural fistula → surgical closure
• • Haemothorax Small: removed by lymphatics Large: tube drainage Persistent bleeding → surgical closure of the vessel
• Chylothorax--- surgical ligation of thoracic duct , or radiation if due to tumor • Meig `s syndrome Removal of the pelvic T • Neglected case (fibrothorax) Pleurectomy
Pneumothorax • A pneumothorax is defined as the accumulation of air in the pleural space with secondary collapse of the surrounding lung. • Pneumothoraces can be divided into spontaneous pneumothorax and traumatic pneumothorax.
• Spontaneous pneumothorax is subclassified as either: • Primary spontaneous pneumothorax or • Secondary spontaneous pneumothorax
• Primary spontaneous pneumothorax occurs without a precipitating event in a person with no clinical evidence of lung disease. Many of these individuals have occult lung disease with subpleural blebs on computed tomography (CT) scans.
• In contrast, secondary spontaneous pneumothorax occurs as a complication of underlying lung disease, most often chronic obstructive lung disease (COPD). • Traumatic (or nonspontaneous) pneumothorax occurs as accidental and as a result of blunt (non-penetrating) or penetrating trauma disrupting the lung, bronchus, or esophagus.
• Asubcategory of traumatic pneumothorax is iatrogenic pneumothorax, which occurs as a consequence of diagnostic or therapeutic maneuvers (i. e. , thoracentesis, insertion of a central venous catheter, surgery, or mechanical ventilation).
• Primary Spontaneous Pneumothorax: • Primary spontaneous pneumothorax (PSP) is an entity that occurs most commonly in young men between the ages of 20 and 40 years of age. Although women have a much lower incidence of PSP, they tend to develop PSP 2 to 5 years earlier than men. A patient rarely presents with a primary episode after the age of 40 years.
• Etiology of Secondary Spontaneous Pneumothorax: • Obstructive lung disease • Interstitial lung disease • Infection • Malignancy • Connective tissue disease
• Calssification of pneumothorax according to the type of the tear: • Closed Type. • Open Type. • Tension Pneumothorax
• Clinical picture • Sudden stabbing chest pain Exertional dyspnea dry cough Tachypnea • Signs • Inspection • bulge in the affected hemithorax limited movement • Absent litten `s sign Wider half of subcostal angle
• Palpation • Limited movement - Decreased TVF Tracheal shift to the opposite side • Percussion • Hyper-resonance
• • • Auscultation Decreased------- VR , intensity of breath Sound Bronchial breathing—over collapsed lung Amphoric breathing bronchopleural fistula Tension pneumothorax : Hypotension , shock , weak pulse, cyanosis
• Investigations • Chest X-ray • Area of jet black appearance devoid of lung reticulation found peripheral to collapsed lung • Mediastinum shifted to the opposite side , hydropneumothorax and Underlying lung disease
Treatment of Pneumothorax • Observation: • Simple observation of the patient with a pneumothorax requires evidence that the air leak is sealed (i. e. , that there is no further progression of the pneumothorax). • This form of management is generally reserved for asymptomatic patients with a small (not greater than 20 percent) unilateral pneumothorax
• Aspiration: • Aspiration of a pneumothorax has been advocated by some; with varied levels of success. These reports have prompted the British Thoracic Society to recommend simple aspiration as first line therapy for all patients with first time spontaneous pneumothorax.
• Tension Pneumothorax: • Urgent insertion of wide pore needle, then ICT under water seal. • Oxygen Inhalation. • Recurrent Pneumothorax. • Bronchopleural Fistula. • Thoracoscopy.
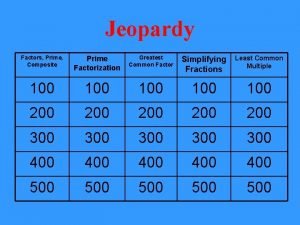
 100 100 100 100 100
100 100 100 100 100 Formula for attack rate
Formula for attack rate Incidence vs incidence rate
Incidence vs incidence rate Serosangineous
Serosangineous Anterior thorax
Anterior thorax Pleural effusion abg results
Pleural effusion abg results Succussion splash
Succussion splash Kerley b lines
Kerley b lines Ellis curve on chest x ray
Ellis curve on chest x ray Concept map for mi
Concept map for mi Pleural fluid color chart
Pleural fluid color chart Apex of the lungs
Apex of the lungs Pleural effusion types
Pleural effusion types Chest expansion test
Chest expansion test Difosfonate
Difosfonate Pleural biopsy
Pleural biopsy Visceral and parietal pleura
Visceral and parietal pleura Ellis curve
Ellis curve Increase tactile fremitus
Increase tactile fremitus Transudative
Transudative Paramalignant pleural effusion
Paramalignant pleural effusion Criminal cases vs civil cases
Criminal cases vs civil cases 200 300 300
200 300 300 300 300 400
300 300 400 300 + 300 + 400
300 + 300 + 400 100 + 100 = 200
100 + 100 = 200 100 200 300
100 200 300 What the font
What the font Prime factorization of 300,300
Prime factorization of 300,300 300+300+400
300+300+400 300+300+400
300+300+400 100 + 100 + 200
100 + 100 + 200 200+200+300+300
200+200+300+300 300+300+400
300+300+400 400 + 300 + 300
400 + 300 + 300 100+200+300+400
100+200+300+400 The conduction system
The conduction system Testojack reviews
Testojack reviews 100 + 200 + 300 + 400 + 500
100 + 200 + 300 + 400 + 500 Wandering atrial pacemaker rhythm
Wandering atrial pacemaker rhythm 100 200 300 400
100 200 300 400 100 200 300 400
100 200 300 400