PHARMACOTHERAPEUTICS OF HEART FAILURE Anton Koht Cardiac failure















- Slides: 52
PHARMACOTHERAPEUTICS OF HEART FAILURE Anton Kohút

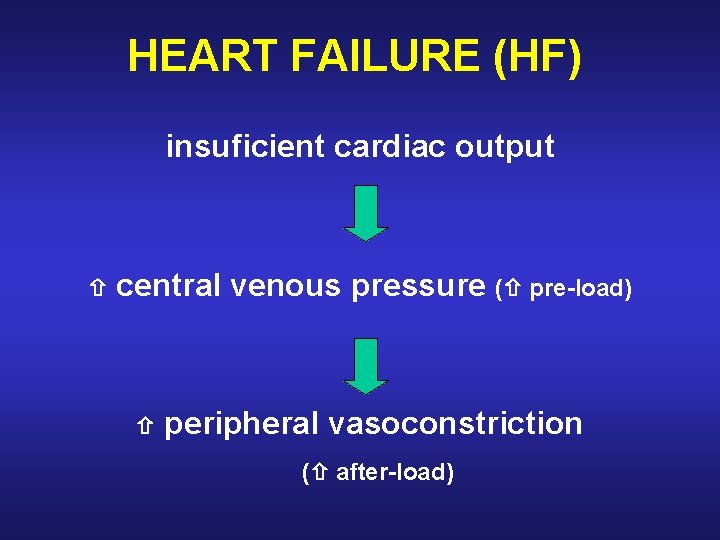
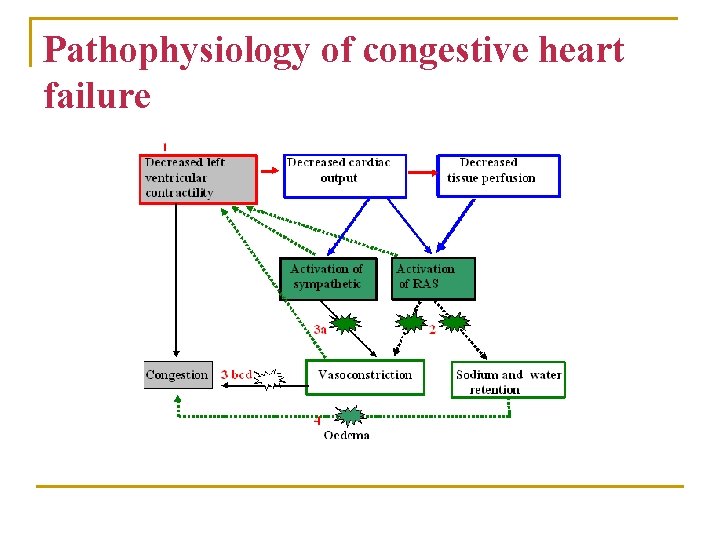
Cardiac failure is characterized by inadequate cardiac output, which leads secondarily to an increased central venous pressure (increased pre-load) and to peripheral vasoconstriction (increased after-load)
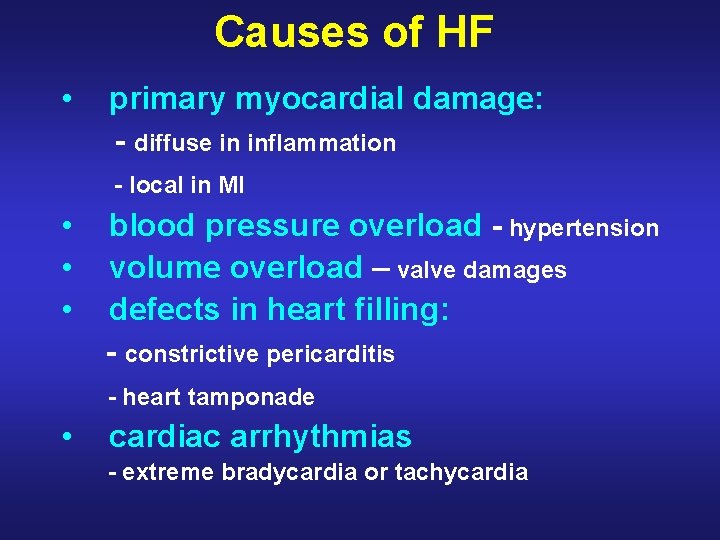
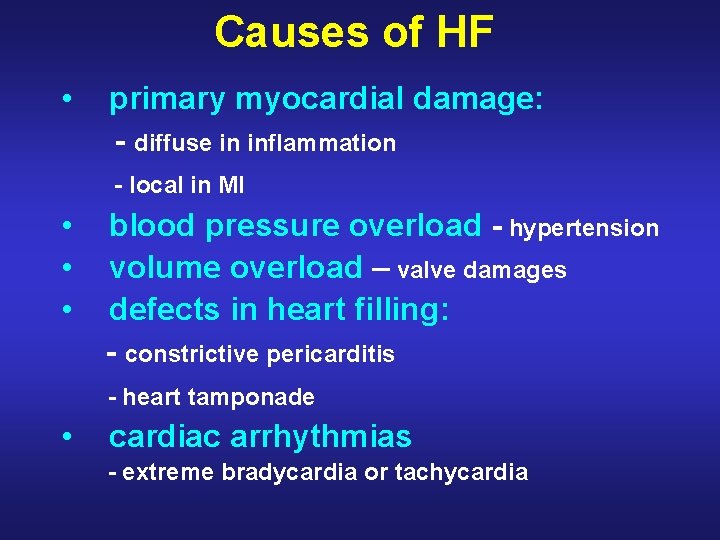
Causes of HF • primary myocardial damage: - diffuse in inflammation - local in MI • • • blood pressure overload - hypertension volume overload – valve damages defects in heart filling: - constrictive pericarditis - heart tamponade • cardiac arrhythmias - extreme bradycardia or tachycardia
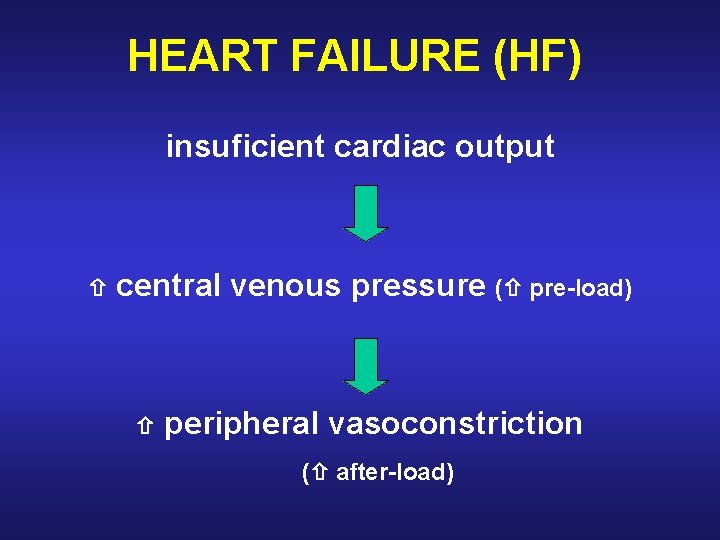
HEART FAILURE (HF) insuficient cardiac output central venous pressure ( pre-load) peripheral vasoconstriction ( after-load)
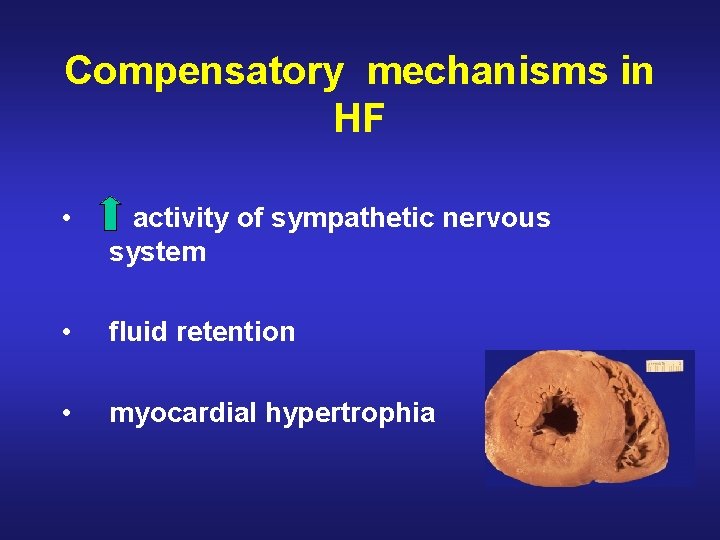
Compensatory mechanisms in HF • activity of sympathetic nervous system • fluid retention • myocardial hypertrophia
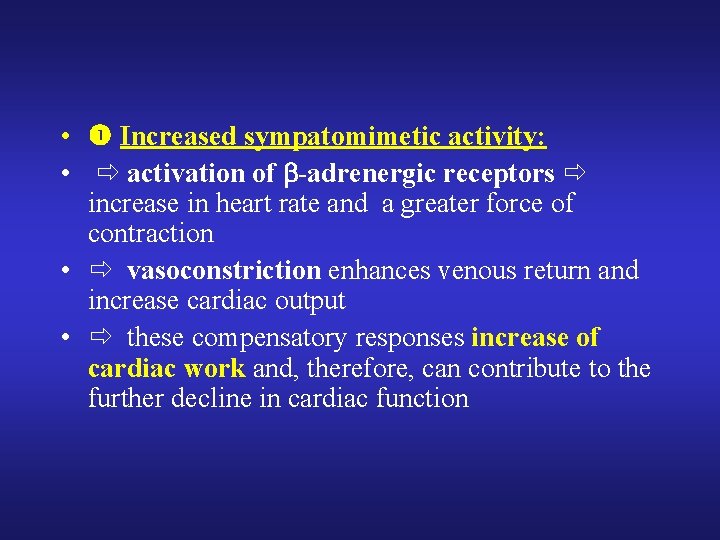
• Increased sympatomimetic activity: • activation of -adrenergic receptors increase in heart rate and a greater force of contraction • vasoconstriction enhances venous return and increase cardiac output • these compensatory responses increase of cardiac work and, therefore, can contribute to the further decline in cardiac function

• Fluid retention: • fall in cardiac output decrease blood flow to the kidney release of renin and synthesis of angiotensin II and aldosterone increase of peripheral resistance and retention of sodium and water • blood volume increase, more blood is returned to the heart • if heart is unable to pump this extra volume venous pressure increases and edema of the peripheral tissues and lung occurs • these compensatory responses increase of cardiac work and, therefore, can contribute to the further decline in cardiac function
• Myocardial hypertrophy: • the heart increases in size and the chambers dilate • stretching of the heart muscle lead to a stronger contraction of the heart • however, excessive elongation of the fibers results in weaker contractions
Acute left HF • Paroxysmal night dyspnea • Asthma cardiale • Lung edema
Chronic left HF • Cardial dyspnea • Fatigue, muscle weakness, sweting, oliguria • Tachycardia

Chronic right HF • • jugular vein filling Hepatomegalia Cardial edema Latent edema – fluid retention 2 -5 l Chronic edema Hydrothorax, hydropericard, ascites Cyanosis
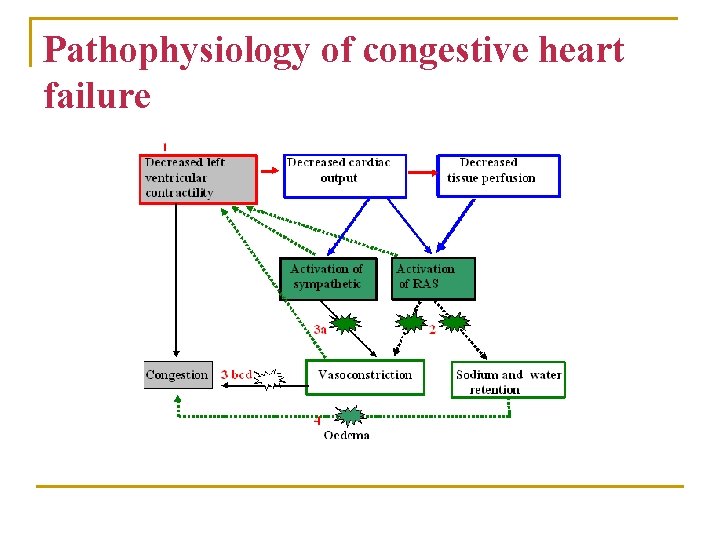
Pathophysiology of congestive heart failure
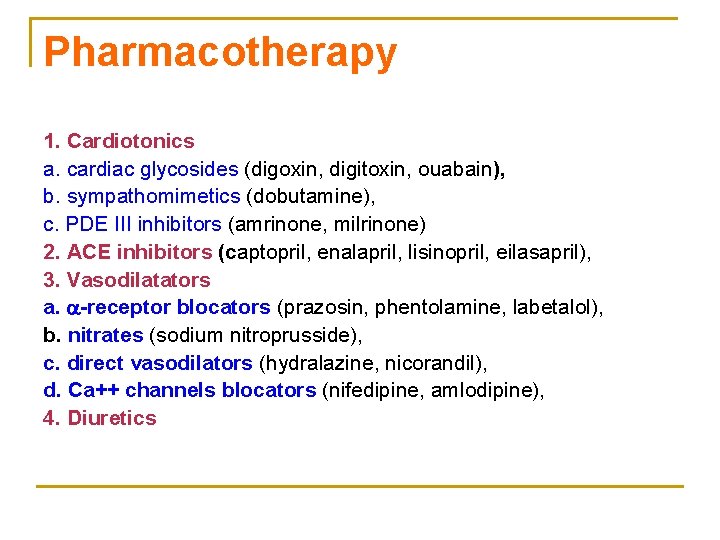
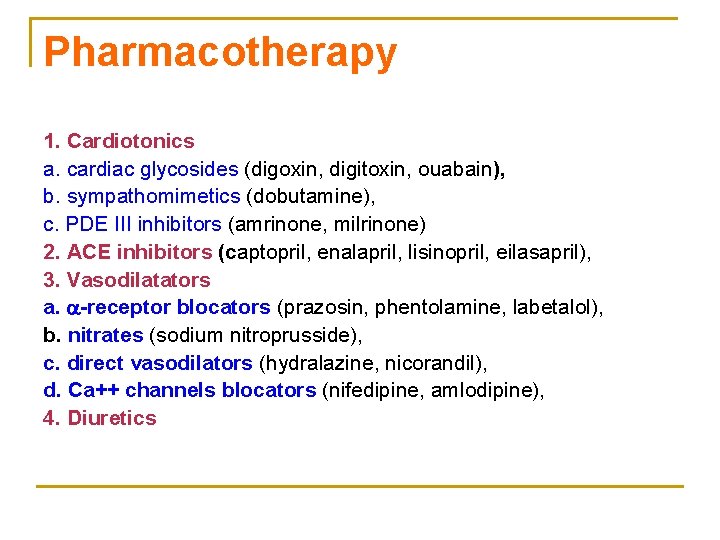
Pharmacotherapy 1. Cardiotonics a. cardiac glycosides (digoxin, digitoxin, ouabain), b. sympathomimetics (dobutamine), c. PDE III inhibitors (amrinone, milrinone) 2. ACE inhibitors (captopril, enalapril, lisinopril, eilasapril), 3. Vasodilatators a. -receptor blocators (prazosin, phentolamine, labetalol), b. nitrates (sodium nitroprusside), c. direct vasodilators (hydralazine, nicorandil), d. Ca++ channels blocators (nifedipine, amlodipine), 4. Diuretics
Basic therapy of HF • cause elimination • diet • pharmacotherapy

Pharmacotherapy • ACE-I • Diuretics • Cardioglycosides • -blockers
Cardiotonics a. cardiac glycosides (digoxin, digitoxin, ouabain), b. sympathomimetics (dobutamine), c. PDE III inhibitors (amrinone, milrinone)

Cardioglycosides

Cardioglycosides • digitoxin – Digitalis purpurea • digoxin – Digitalis lanata • strophantin (ouabain) – Strophantus gratus
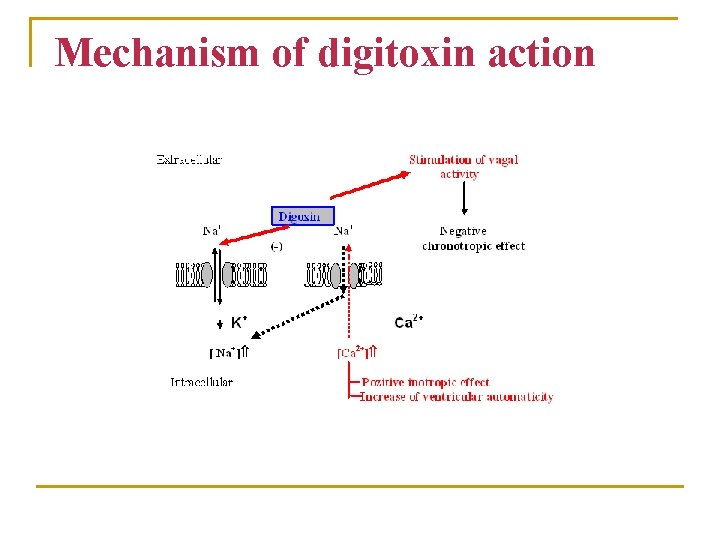
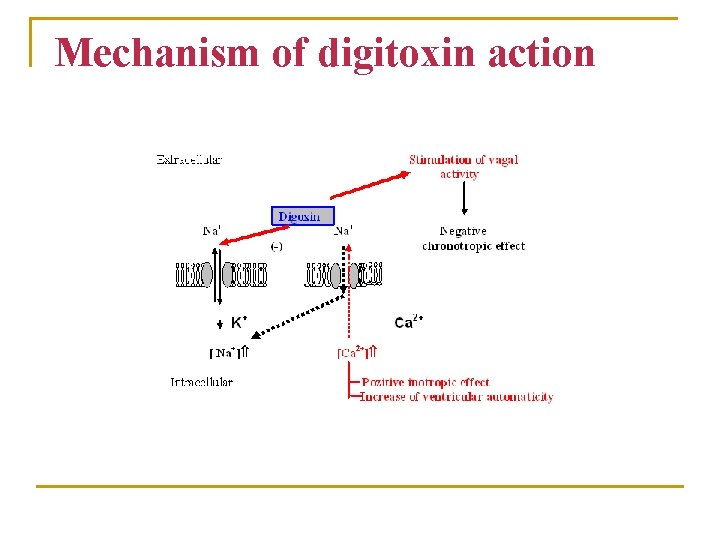
Mechanism of digitoxin action

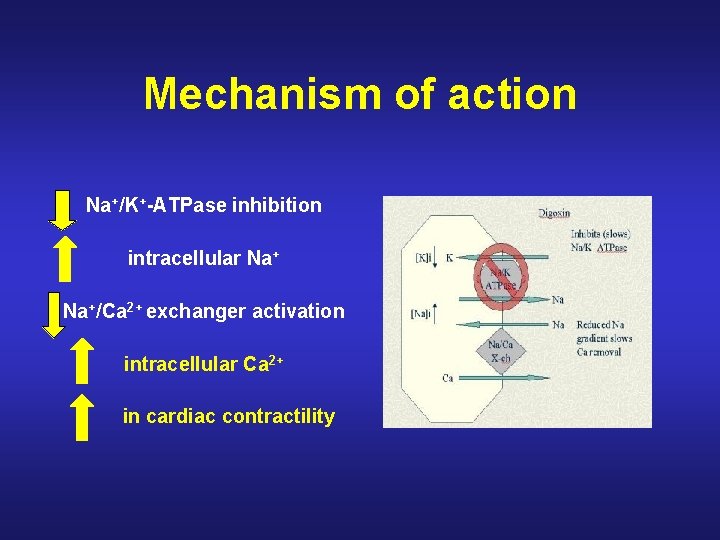
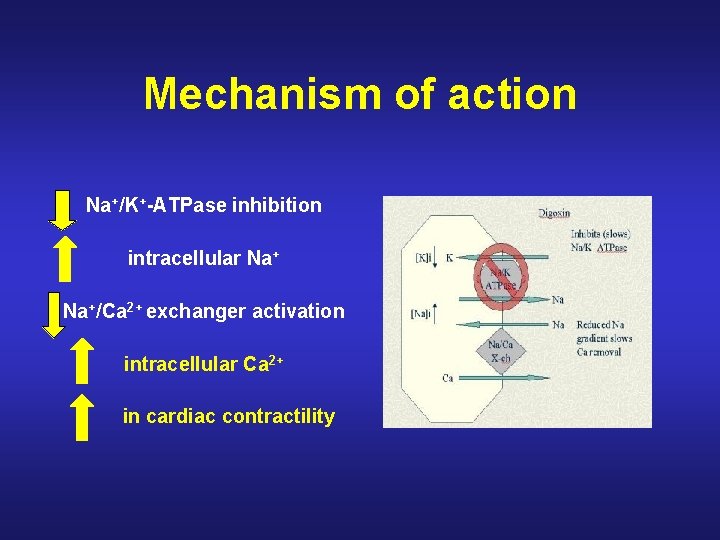
Mechanism of action Na+/K+-ATPase inhibition intracellular Na+/Ca 2+ exchanger activation intracellular Ca 2+ in cardiac contractility
1. I n heart failure the cardiac glycosides increase cardiac output (better perfusion of peripheral tissue) and reduce central venous pressure (decrease of tissue fluid volume). 2. After glycoside in patients with cardiac failure, marked diuresis occurs: - increased renal blood flow - inhibtion of Na+/K+-ATPase of the tubules (inhibition of renal-sodium transport) 3. Glycosides cause cardiac slowing - increase of vagal activity. n At higher dosage - an increase in AV conduction time is detectable (increase of P-R interval on ECG)
4. Larger doses of glycosides-AV conduction can progress to an AV block. n ectopic beats which can progress to a continous ventricular tachykardia and eventually to ventricular fibrilation 5. Have a beneficial effect in certain type of dysrhytmia - atrial tachycardia or fibrilat
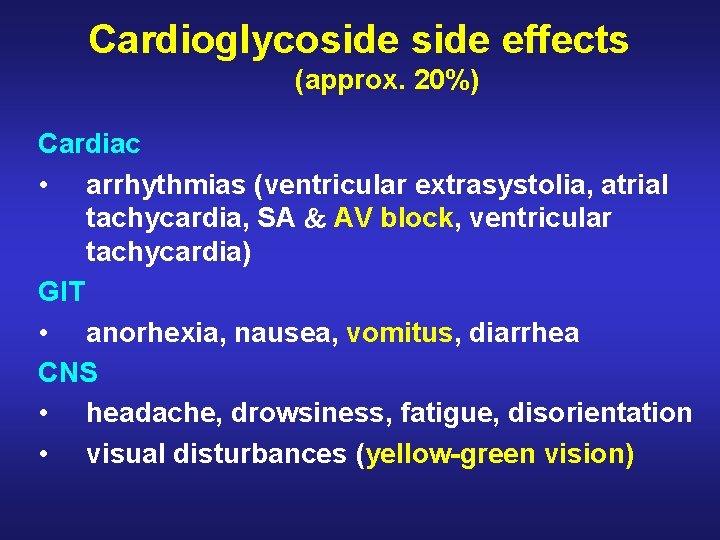
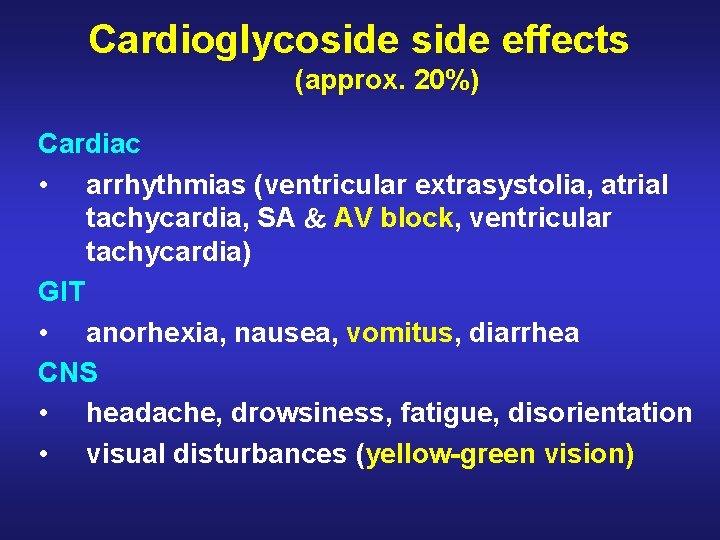
Cardioglycoside effects (approx. 20%) Cardiac • arrhythmias (ventricular extrasystolia, atrial tachycardia, SA AV block, ventricular tachycardia) GIT • anorhexia, nausea, vomitus, diarrhea CNS • headache, drowsiness, fatigue, disorientation • visual disturbances (yellow-green vision)
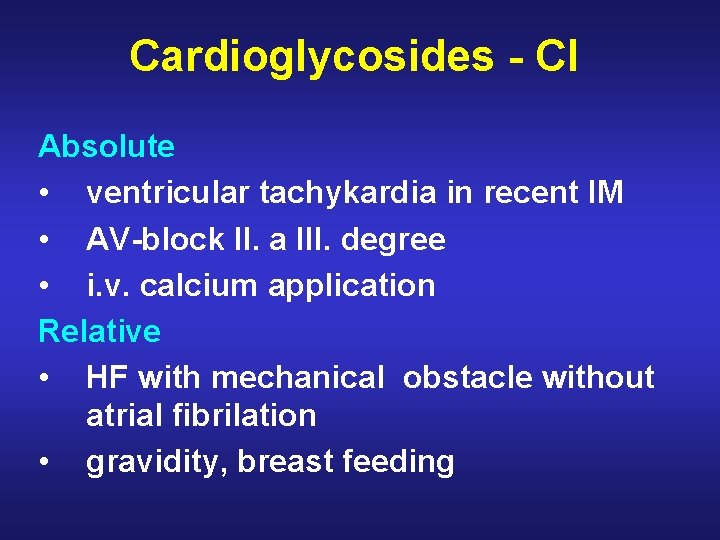
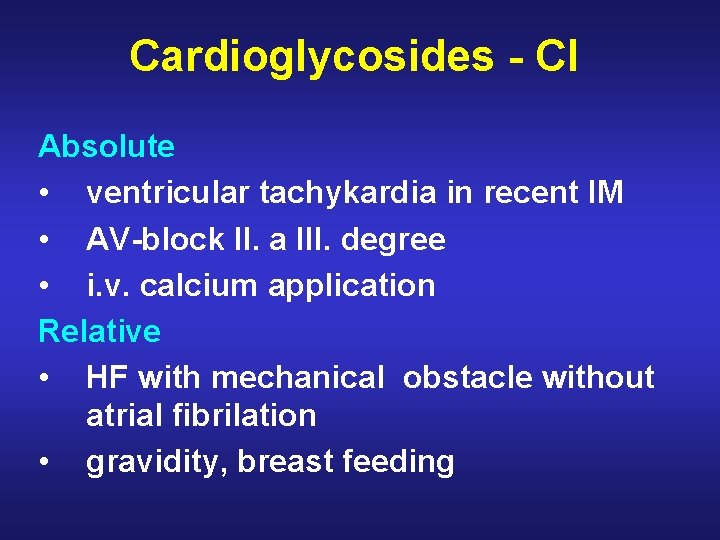
Cardioglycosides - CI Absolute • ventricular tachykardia in recent IM • AV-block II. a III. degree • i. v. calcium application Relative • HF with mechanical obstacle without atrial fibrilation • gravidity, breast feeding
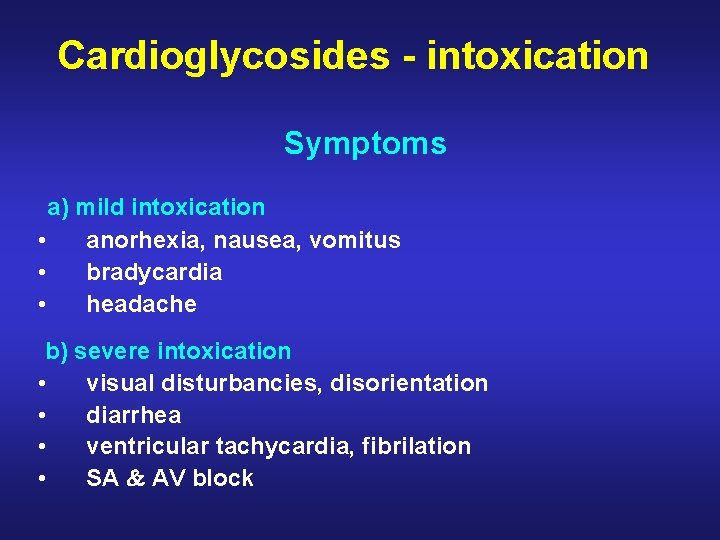
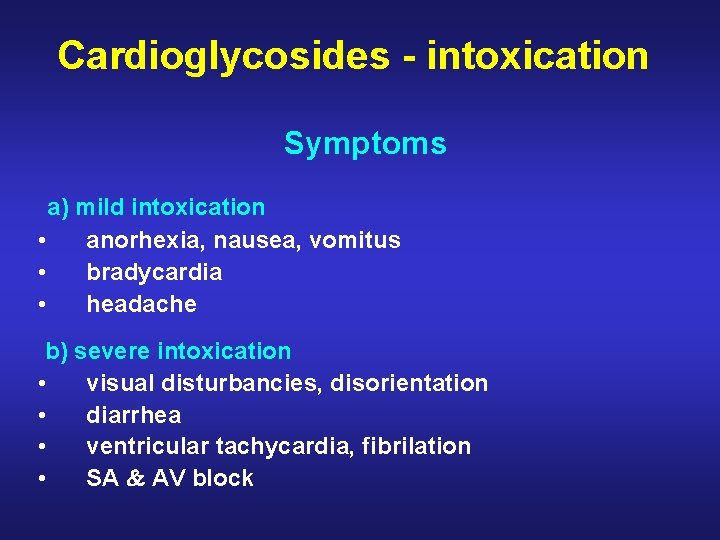
Cardioglycosides - intoxication Symptoms a) mild intoxication • anorhexia, nausea, vomitus • bradycardia • headache b) severe intoxication • visual disturbancies, disorientation • diarrhea • ventricular tachycardia, fibrilation • SA AV block
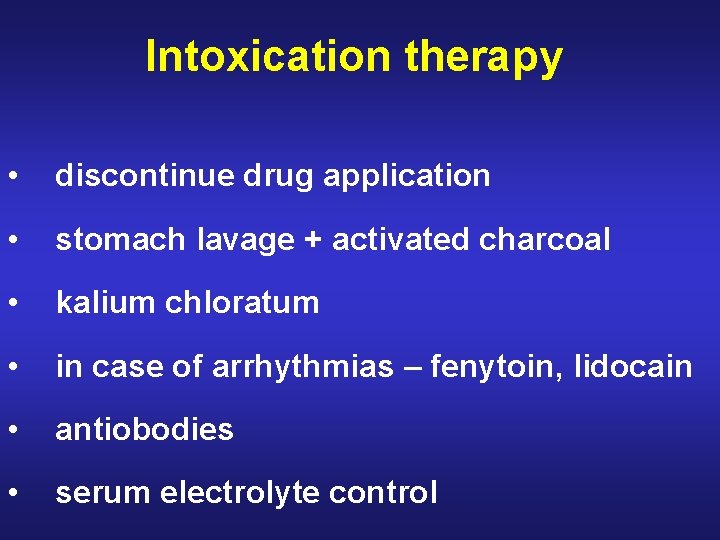
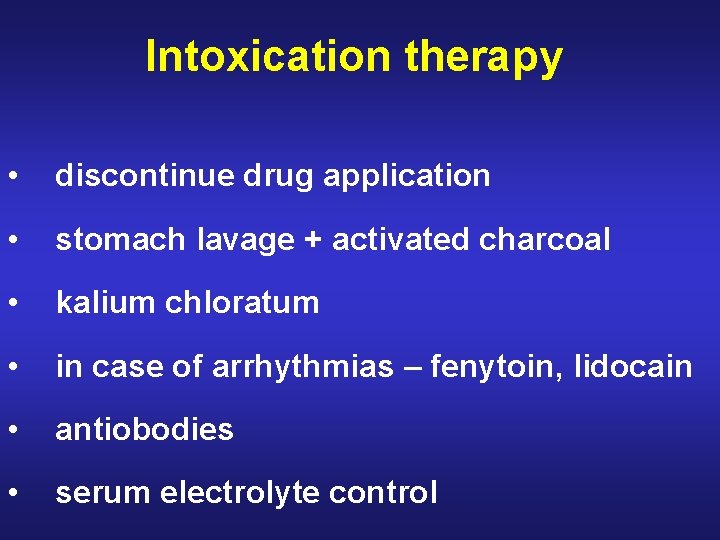
Intoxication therapy • discontinue drug application • stomach lavage + activated charcoal • kalium chloratum • in case of arrhythmias – fenytoin, lidocain • antiobodies • serum electrolyte control
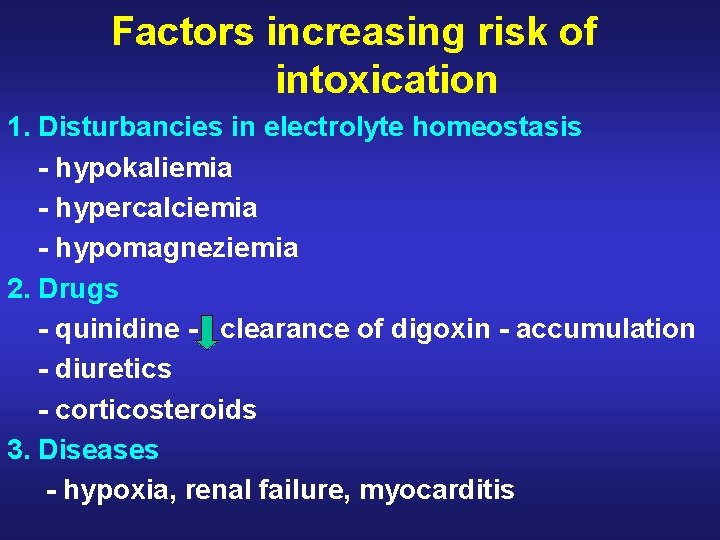
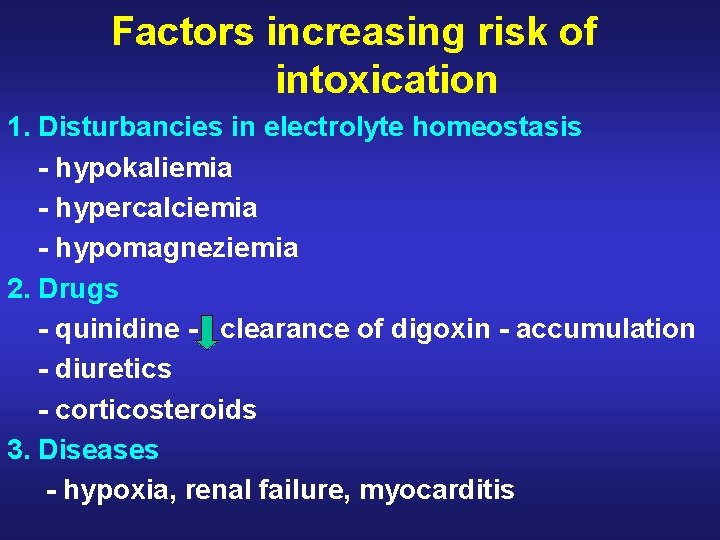
Factors increasing risk of intoxication 1. Disturbancies in electrolyte homeostasis - hypokaliemia - hypercalciemia - hypomagneziemia 2. Drugs - quinidine - clearance of digoxin - accumulation - diuretics - corticosteroids 3. Diseases - hypoxia, renal failure, myocarditis

-blockers
-blockers – immediate effects heart rate BP heart ejection fraction vasoconstriction
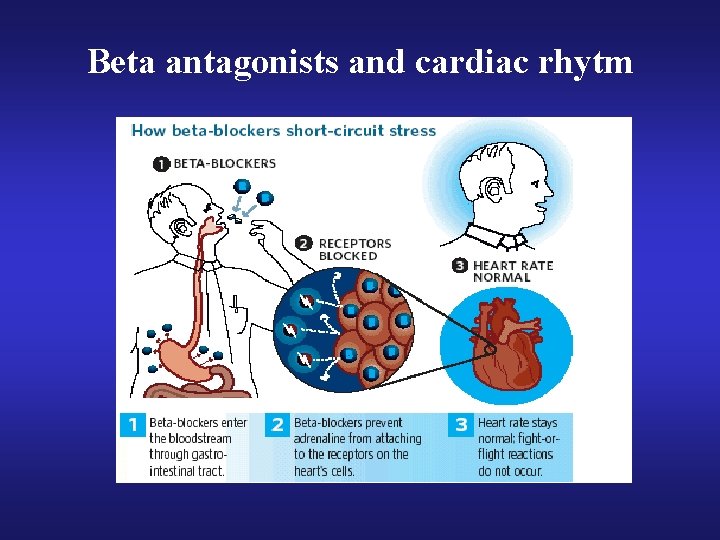
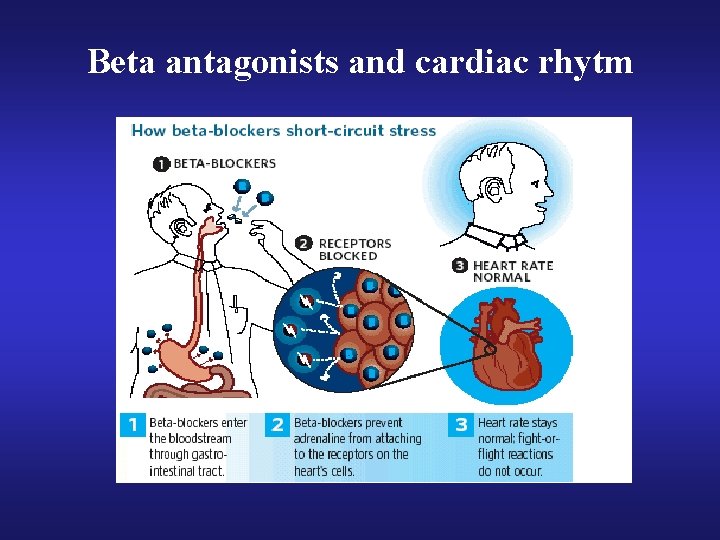
Beta antagonists and cardiac rhytm
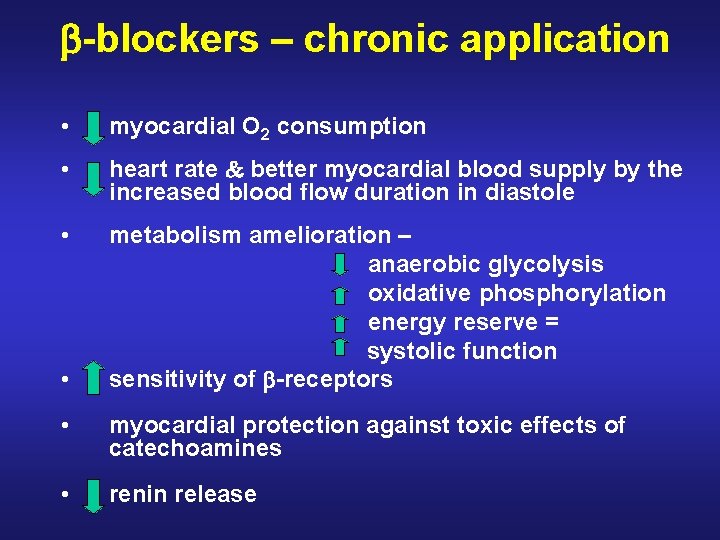
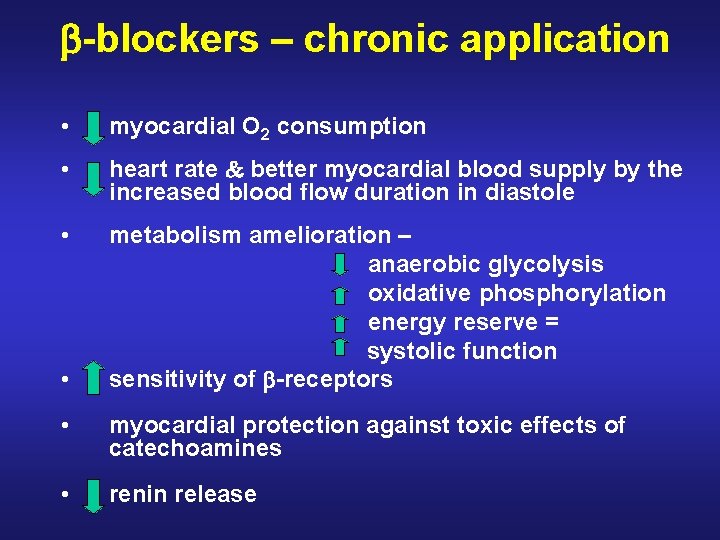
-blockers – chronic application • myocardial O 2 consumption • heart rate better myocardial blood supply by the increased blood flow duration in diastole • metabolism amelioration – anaerobic glycolysis oxidative phosphorylation energy reserve = systolic function sensitivity of -receptors • • myocardial protection against toxic effects of catechoamines • renin release

Angiotensin converting enzyme inhibitors (ACE-I)
Angiotensin converting enzyme inhibitors (ACE-I) • RAS – BP, water and mineral ion regulation • angiotensin II – main role in patophysiology of CVS diseases: - hypertension - chronic HF

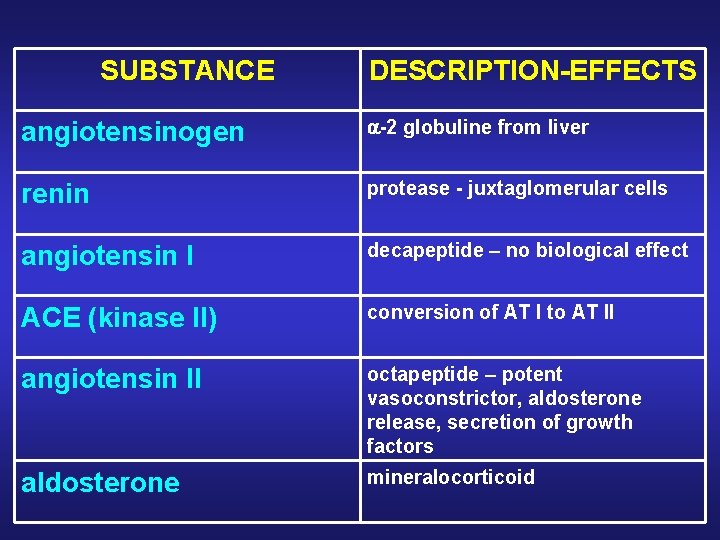
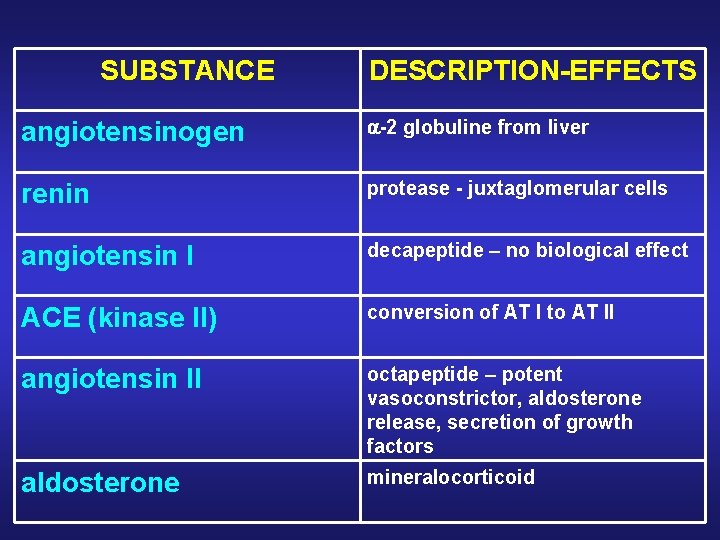
SUBSTANCE DESCRIPTION-EFFECTS angiotensinogen -2 globuline from liver renin protease - juxtaglomerular cells angiotensin I decapeptide – no biological effect ACE (kinase II) conversion of AT I to AT II angiotensin II octapeptide – potent vasoconstrictor, aldosterone release, secretion of growth factors aldosterone mineralocorticoid
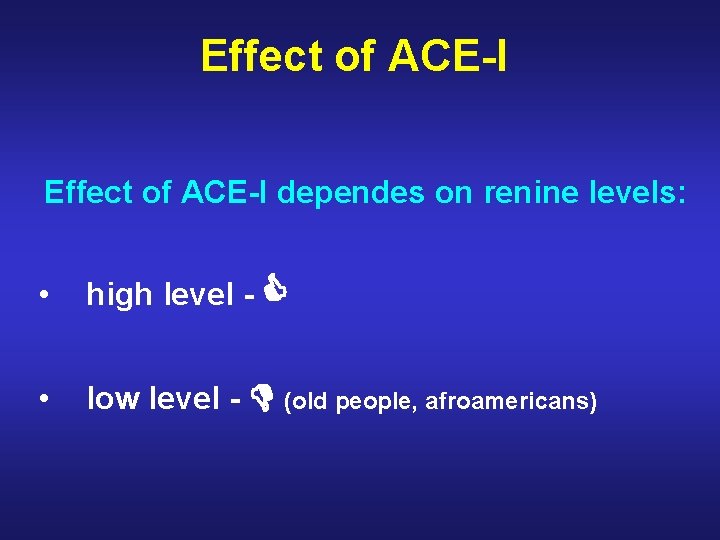
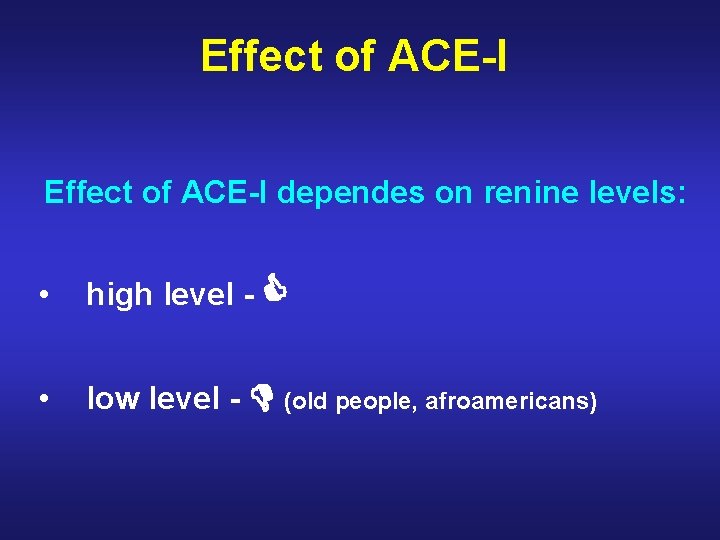
Effect of ACE-I dependes on renine levels: • high level - • low level - (old people, afroamericans)
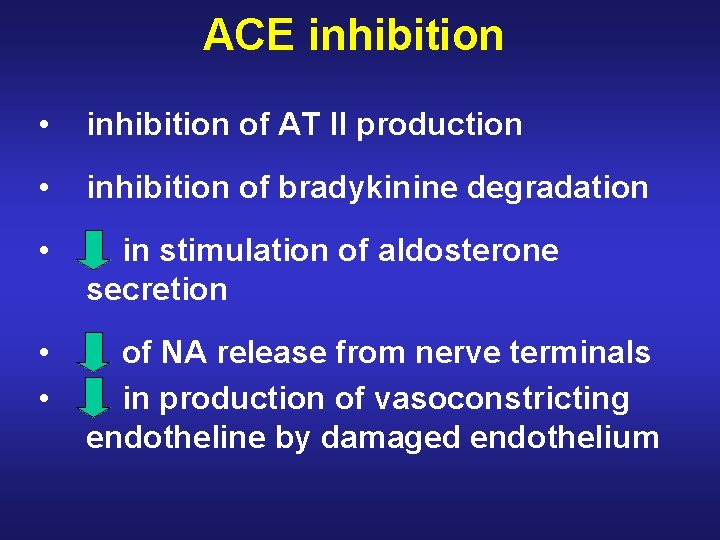
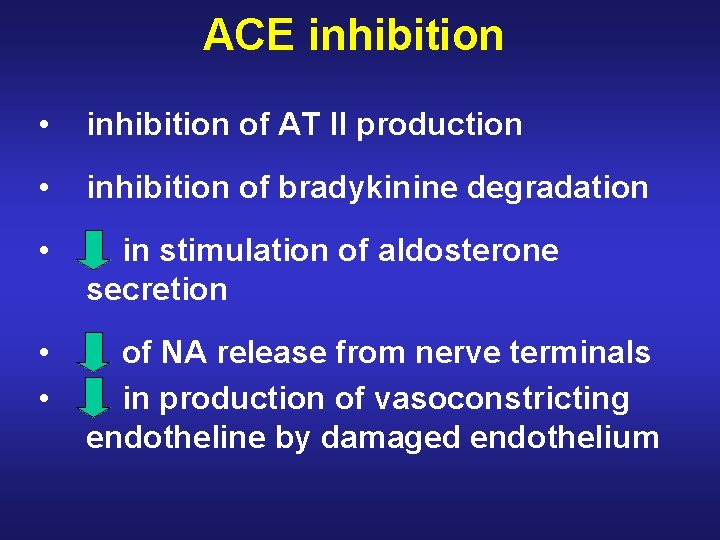
ACE inhibition • inhibition of AT II production • inhibition of bradykinine degradation • in stimulation of aldosterone secretion • • of NA release from nerve terminals in production of vasoconstricting endotheline by damaged endothelium
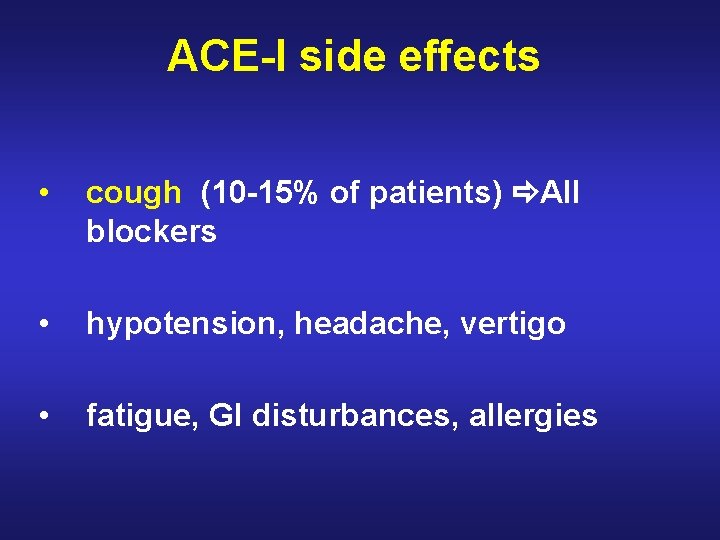
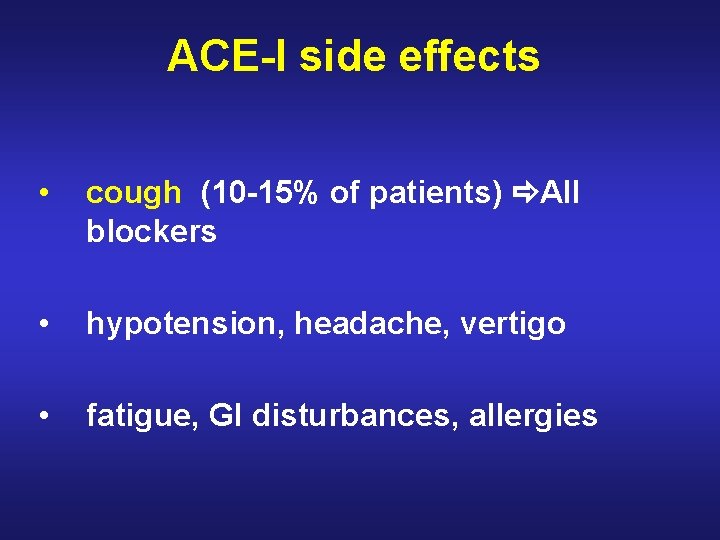
ACE-I side effects • cough (10 -15% of patients) AII blockers • hypotension, headache, vertigo • fatigue, GI disturbances, allergies
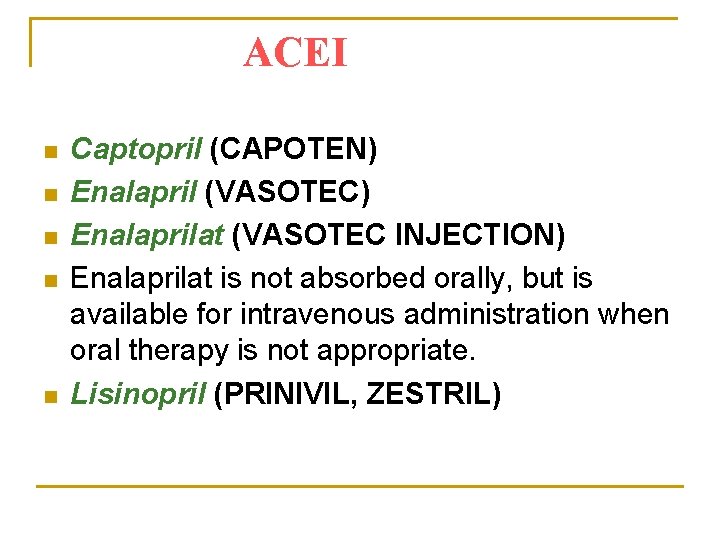
ACEI n n n Captopril (CAPOTEN) Enalapril (VASOTEC) Enalaprilat (VASOTEC INJECTION) Enalaprilat is not absorbed orally, but is available for intravenous administration when oral therapy is not appropriate. Lisinopril (PRINIVIL, ZESTRIL)
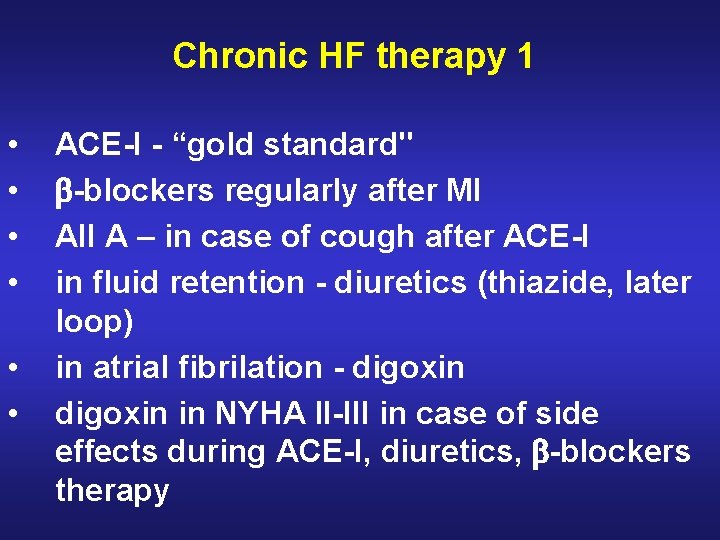
Chronic HF therapy 1 • • • ACE-I - “gold standard" -blockers regularly after MI AII A – in case of cough after ACE-I in fluid retention - diuretics (thiazide, later loop) in atrial fibrilation - digoxin in NYHA II-III in case of side effects during ACE-I, diuretics, -blockers therapy
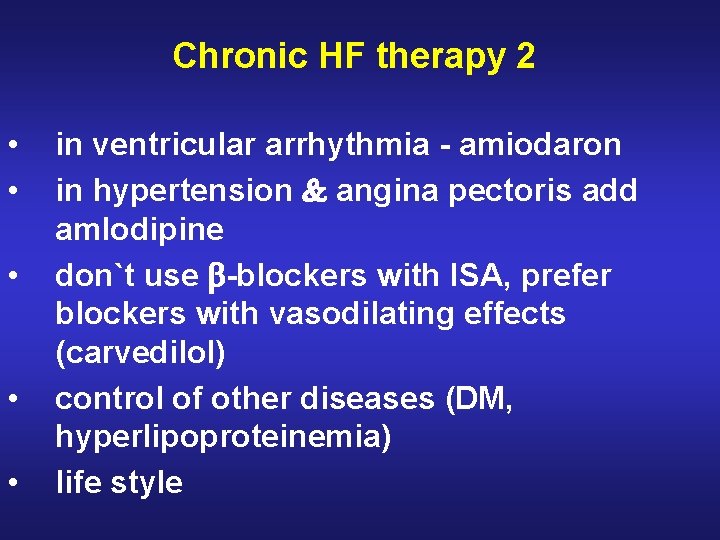
Chronic HF therapy 2 • • • in ventricular arrhythmia - amiodaron in hypertension angina pectoris add amlodipine don`t use -blockers with ISA, prefer blockers with vasodilating effects (carvedilol) control of other diseases (DM, hyperlipoproteinemia) life style
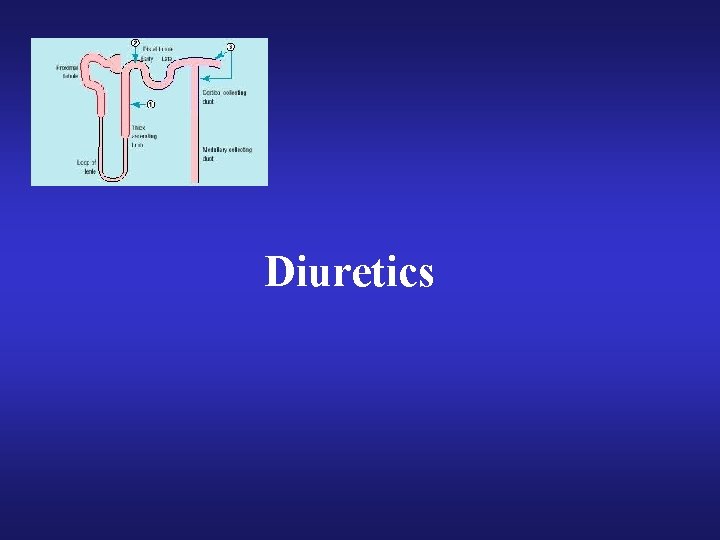
Diuretics

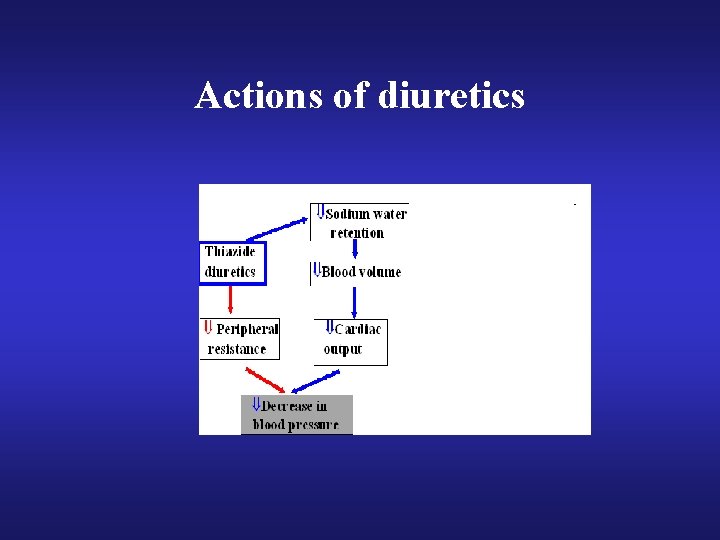
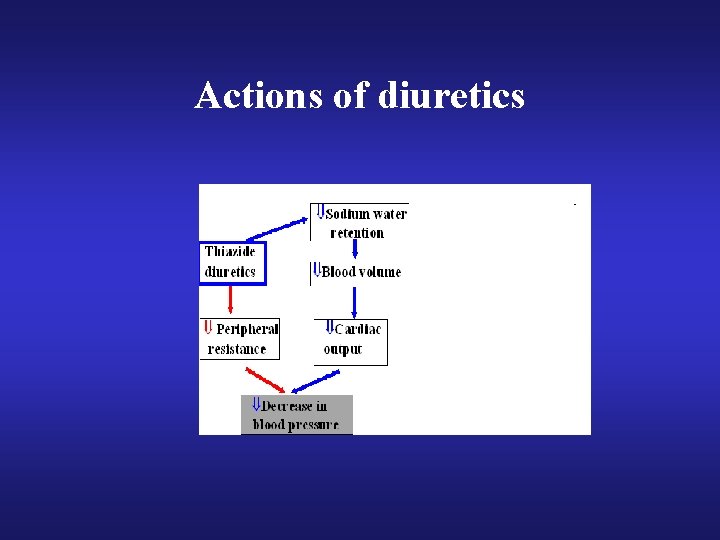
Actions of diuretics



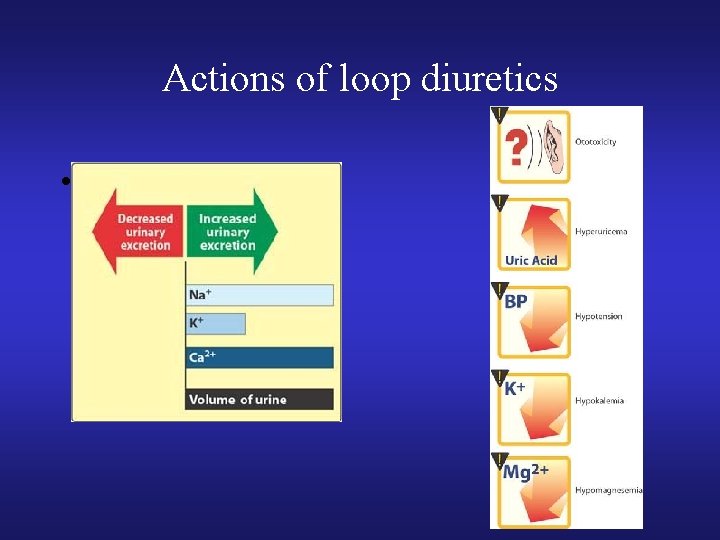
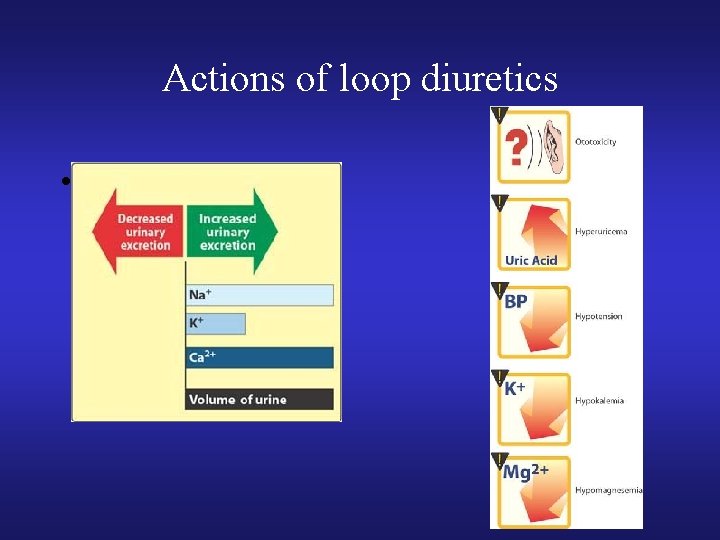
Actions of loop diuretics •
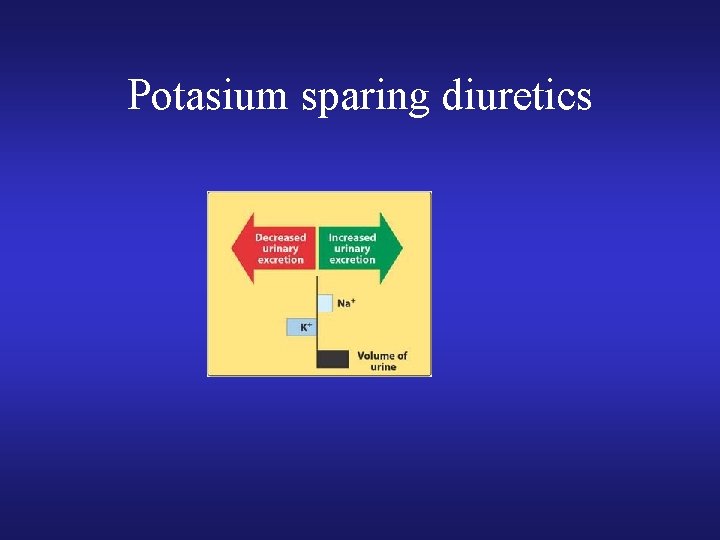
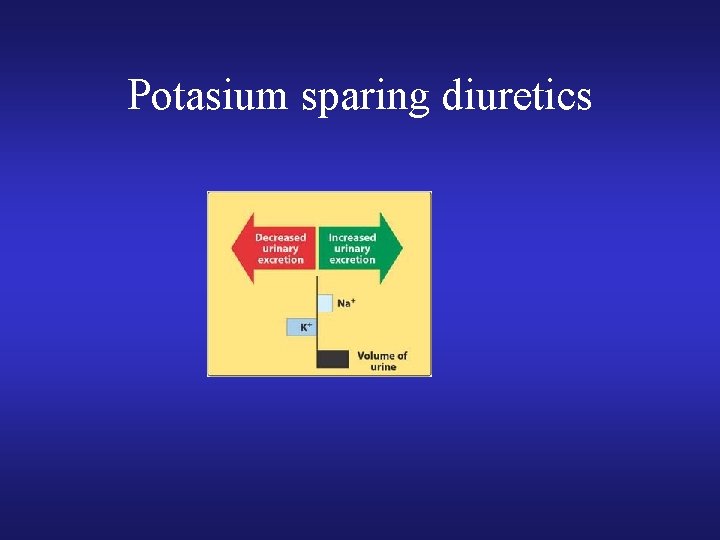
Potasium sparing diuretics

 Praktika koht
Praktika koht Relative refractory period
Relative refractory period Heart sounds and murmurs
Heart sounds and murmurs Ventricular escape rhythm
Ventricular escape rhythm Failure to pace
Failure to pace Ductile break
Ductile break Keith rischer
Keith rischer Forrester classification
Forrester classification Ecg findings of heart failure
Ecg findings of heart failure Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Chlorpromide
Chlorpromide Congestive heart failure zones for management
Congestive heart failure zones for management Heart failure
Heart failure Acute vs chronic heart failure
Acute vs chronic heart failure Classification of ejection fraction
Classification of ejection fraction Cor pulmonale
Cor pulmonale Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Diabetes and heart failure
Diabetes and heart failure Lmnop heart failure
Lmnop heart failure Heart failure definition
Heart failure definition Dr nienkemper
Dr nienkemper Acute pulmonary congestion histology
Acute pulmonary congestion histology Heart failure complications
Heart failure complications Compensatory mechanisms of heart failure
Compensatory mechanisms of heart failure Keith rn heart failure case study
Keith rn heart failure case study New york scale heart failure
New york scale heart failure Heart failure forward vs backward
Heart failure forward vs backward Chapter 24 heart failure drugs
Chapter 24 heart failure drugs Goat heart dissection
Goat heart dissection Hrt 2 hrt
Hrt 2 hrt Dullness of heart
Dullness of heart Anton-hansen-schule ottweiler
Anton-hansen-schule ottweiler Anton chilton
Anton chilton Sokol vako
Sokol vako Dr anton lishmanov
Dr anton lishmanov Anton chekhov a problem
Anton chekhov a problem Anton bernolák dejepis
Anton bernolák dejepis Jeremy pfeiffer
Jeremy pfeiffer Anton rinaldi
Anton rinaldi Anton anderson tunnel
Anton anderson tunnel Anton koekemoer
Anton koekemoer Calculus 10e
Calculus 10e Anton groenewald
Anton groenewald Anton van leeuwenhoek cell theory
Anton van leeuwenhoek cell theory Antonie van leeuwenhoek cell theory
Antonie van leeuwenhoek cell theory Karl metzler
Karl metzler 1673 anton van leeuwenhoek
1673 anton van leeuwenhoek Anton van leeuwenhoek accomplishments
Anton van leeuwenhoek accomplishments Anton supercomputer
Anton supercomputer Mvp azure
Mvp azure Anton myburgh sc
Anton myburgh sc Anton vako
Anton vako Hemerijck
Hemerijck