Drugs used to treat GIT disordes Anton Koht













- Slides: 48
Drugs used to treat GIT disordes Anton Kohút
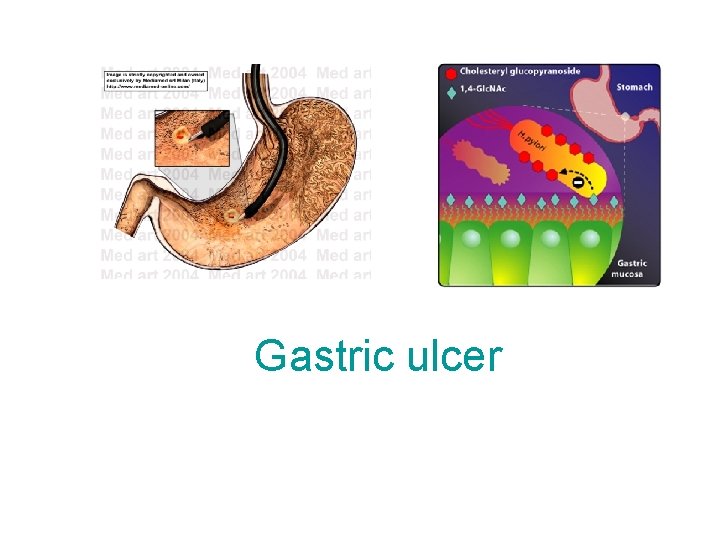
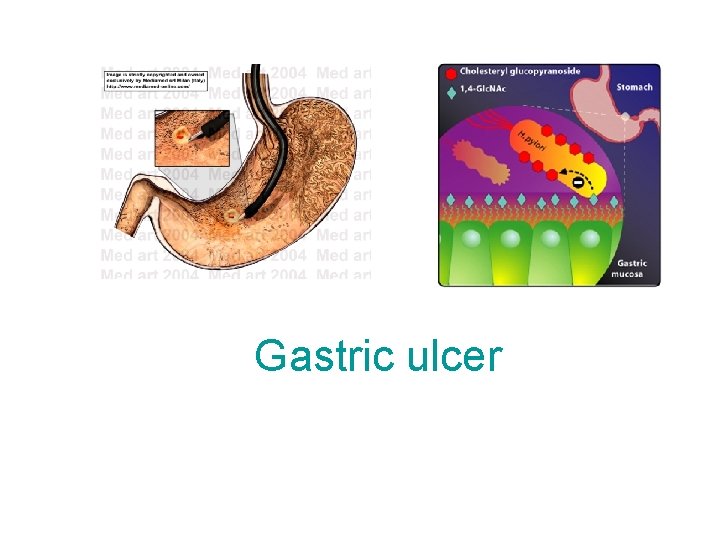
Gastric ulcer


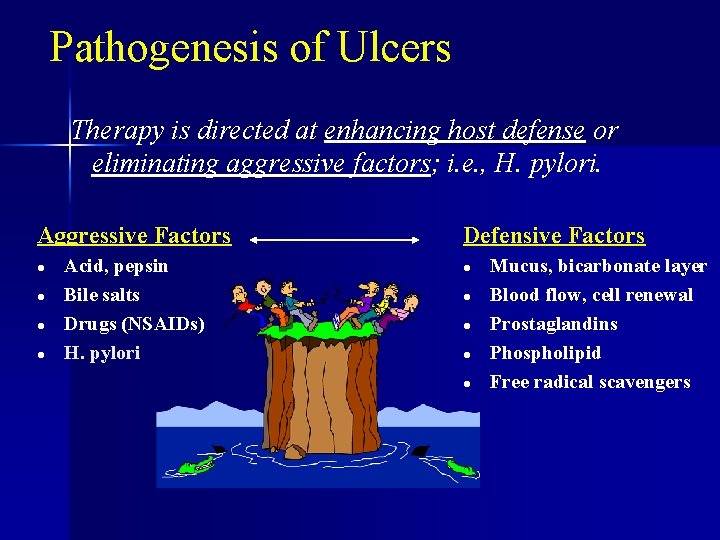
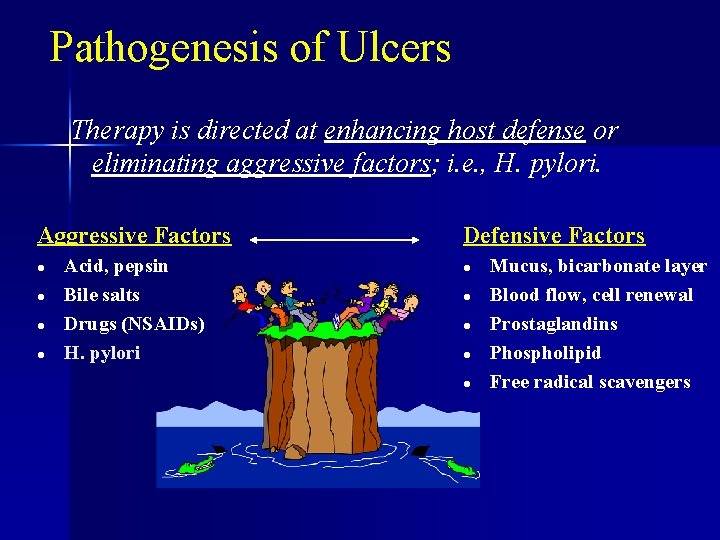
Pathogenesis of Ulcers Therapy is directed at enhancing host defense or eliminating aggressive factors; i. e. , H. pylori. Aggressive Factors l l Acid, pepsin Bile salts Drugs (NSAIDs) H. pylori Defensive Factors l l l Mucus, bicarbonate layer Blood flow, cell renewal Prostaglandins Phospholipid Free radical scavengers
Gastric ulcer and NSAIDs n infection H. pylori

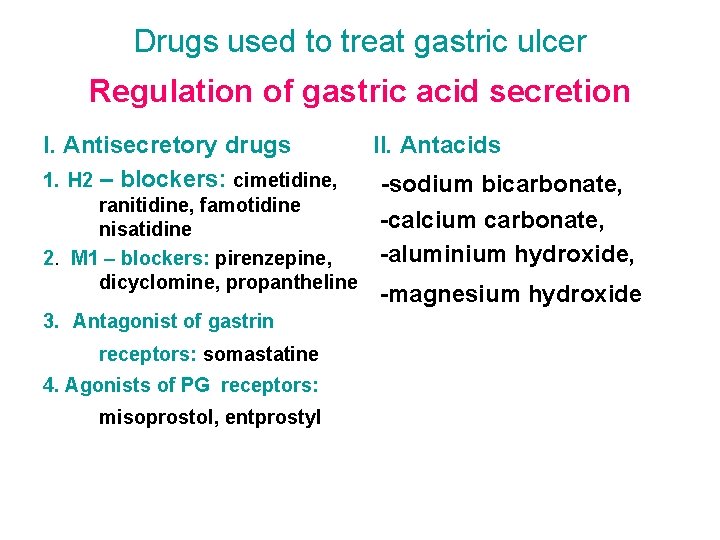
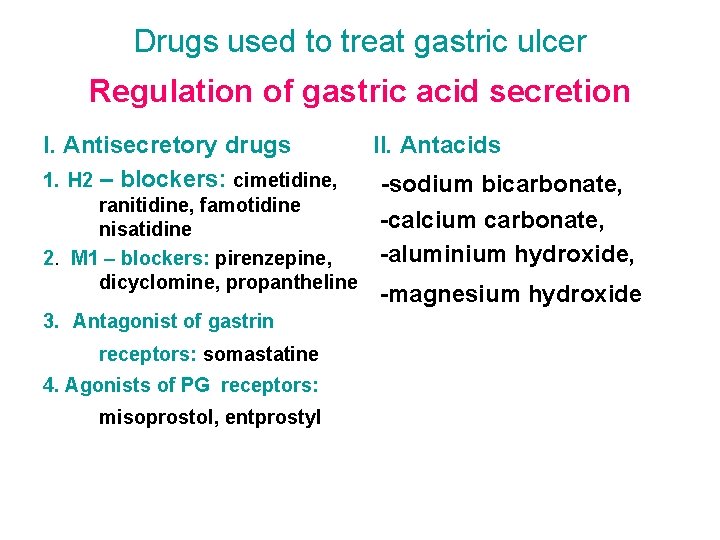
Drugs used to treat gastric ulcer Regulation of gastric acid secretion I. Antisecretory drugs 1. H 2 – blockers: cimetidine, ranitidine, famotidine nisatidine 2. M 1 – blockers: pirenzepine, dicyclomine, propantheline 3. Antagonist of gastrin receptors: somastatine 4. Agonists of PG receptors: misoprostol, entprostyl II. Antacids -sodium bicarbonate, -calcium carbonate, -aluminium hydroxide, -magnesium hydroxide
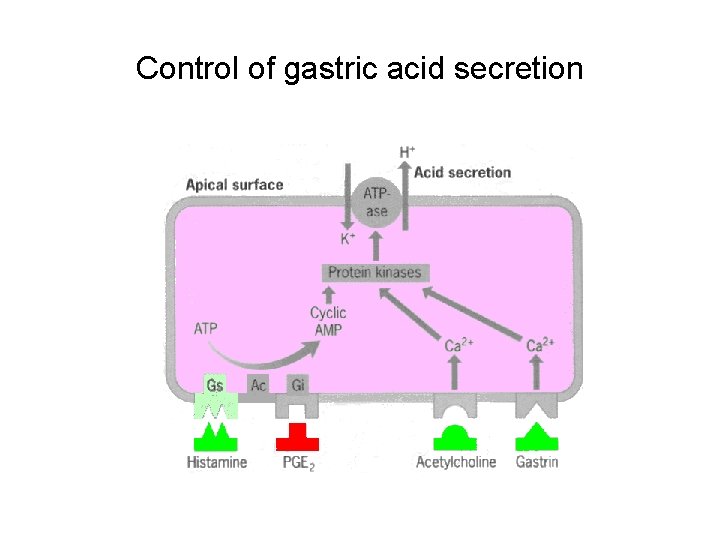
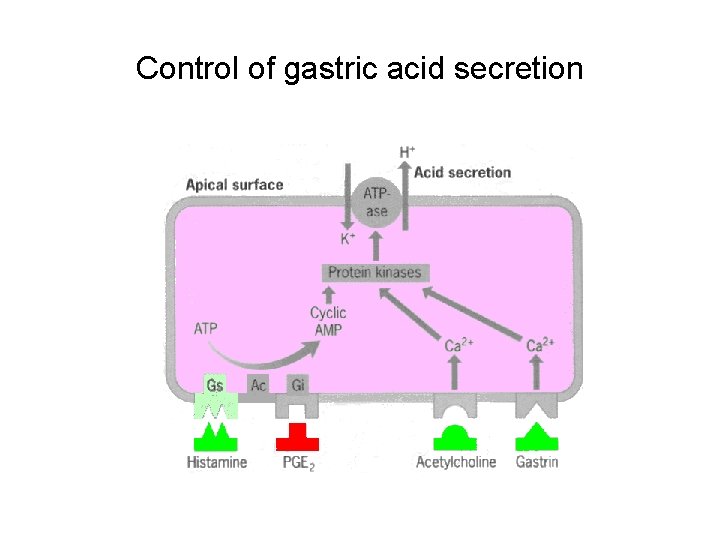
Control of gastric acid secretion

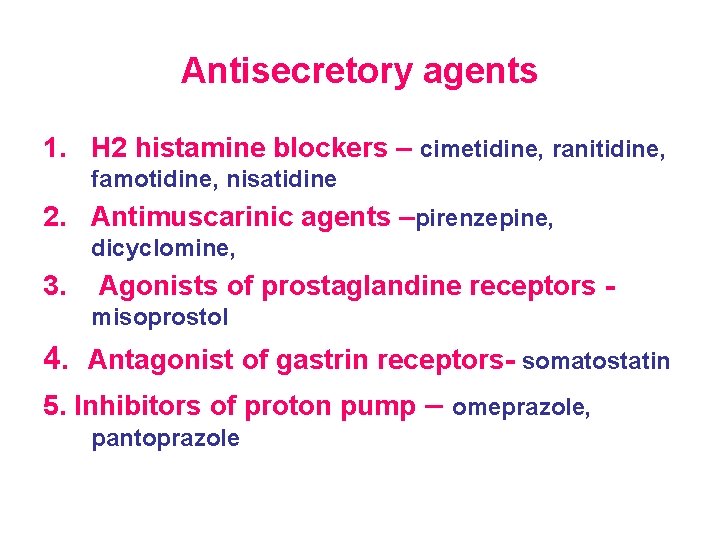
Antisecretory agents 1. H 2 histamine blockers – cimetidine, ranitidine, famotidine, nisatidine 2. Antimuscarinic agents –pirenzepine, dicyclomine, 3. Agonists of prostaglandine receptors misoprostol 4. Antagonist of gastrin receptors- somatostatin 5. Inhibitors of proton pump – omeprazole, pantoprazole
H 2 receptor antagonists
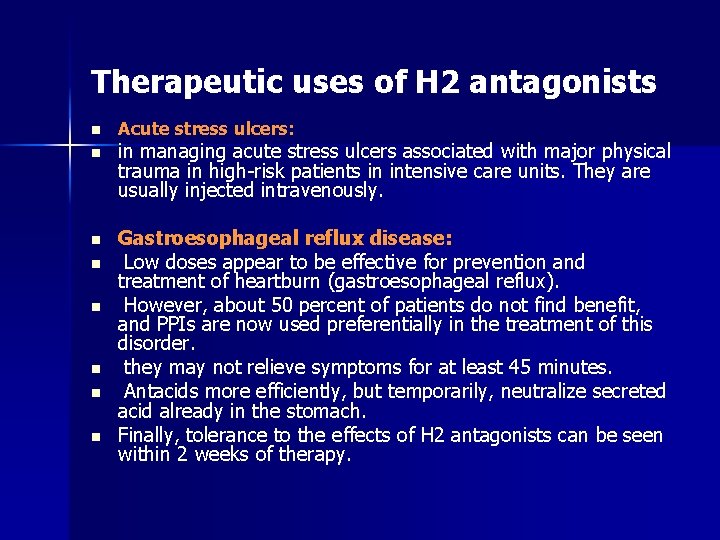
Therapeutic uses of H 2 antagonists n Acute stress ulcers: n in managing acute stress ulcers associated with major physical trauma in high-risk patients in intensive care units. They are usually injected intravenously. n Gastroesophageal reflux disease: Low doses appear to be effective for prevention and treatment of heartburn (gastroesophageal reflux). However, about 50 percent of patients do not find benefit, and PPIs are now used preferentially in the treatment of this disorder. they may not relieve symptoms for at least 45 minutes. Antacids more efficiently, but temporarily, neutralize secreted acid already in the stomach. Finally, tolerance to the effects of H 2 antagonists can be seen within 2 weeks of therapy. n n n

n n n All H 2 antagonists are equally effective in promoting healing of duodenal and gastric ulcers. However, recurrence is common after treatment with H 2 antagonists is stopped (60– 100 percent per year). The use of these agents has decreased with the advent of the PPIs. Patients with NSAID-induced ulcers should be treated with PPIs, because these agents heal and prevent future ulcers better than H 2 antagonists.
Antacids • Calcium containing Calcium carbonate • Magnesium containing Magnesium hydroxide • Aluminium containing Aluminium hydroxide Antacids may decrease absorption of other drugs

• Cytoprotective agents - misoprostol (PGE 1), sucralfate, bismuth subsalicylate • Antibacterial agents colloidal bismuth ATB: ampicilline tetracyclines, metronidazole, clarithromycin
n Sucralfate: - This complex of aluminum hydroxide and sulfated sucrose binds to positively charged groups in proteins of both normal and necrotic mucosa. - By forming complex gels with epithelial cells, sucralfate creates a physical barrier. - Effectively heals duodenal ulcers and is used in long-term maintenance therapy. - Because it requires an acidic p. H for activation, sucralfate should not be administered with H 2 antagonists or antacids.
Bismuth subsalicylate: Effectively heal peptic ulcers. In addition to their antimicrobial actions, They inhibit the activity of pepsin, increase secretion of mucus, and interact with glycoproteins in necrotic mucosal tissue to coat and protect the ulcer crater.
Antibacterial agents Currently, either n triple therapy consisting of a PPI with either metronidazole or amoxicillin plus clarithromycin, n or quadruple therapy of bismuth subsalicylate and metronidazole plus tetracycline plus a PPI, are administered for a 2 -week course. n

GIT motility disorders
GIT motility disorders • Constipation means hard stools, difficulty passing stools, or the sense of incomplete emptying after a bowel movement. • Diarrhoea is a watery stool occurring more than three times in one day. Prolonged diarrhea can be a sign of other problems and it can cause dehydration.
Constipation
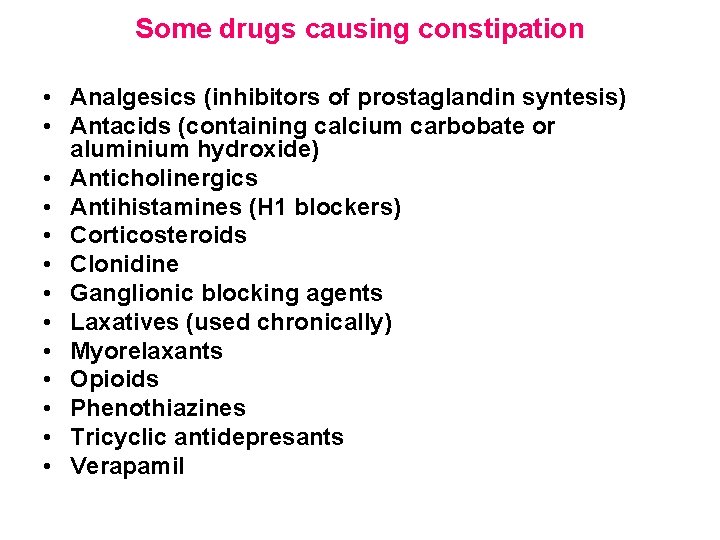
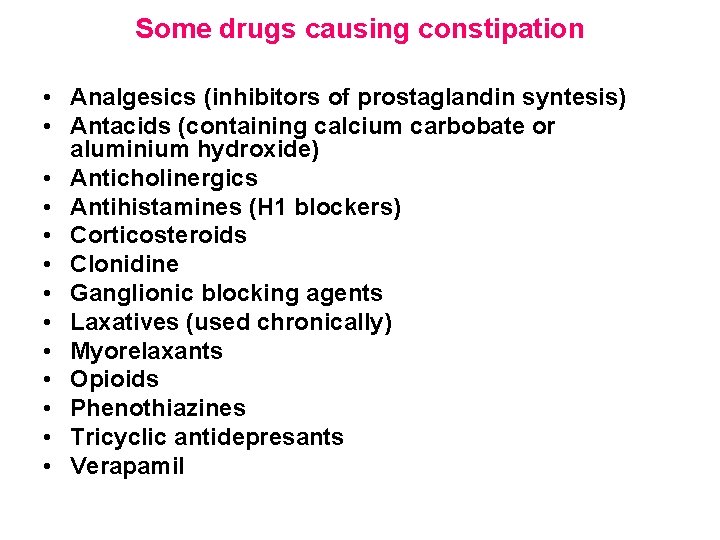
Some drugs causing constipation • Analgesics (inhibitors of prostaglandin syntesis) • Antacids (containing calcium carbobate or aluminium hydroxide) • Anticholinergics • Antihistamines (H 1 blockers) • Corticosteroids • Clonidine • Ganglionic blocking agents • Laxatives (used chronically) • Myorelaxants • Opioids • Phenothiazines • Tricyclic antidepresants • Verapamil
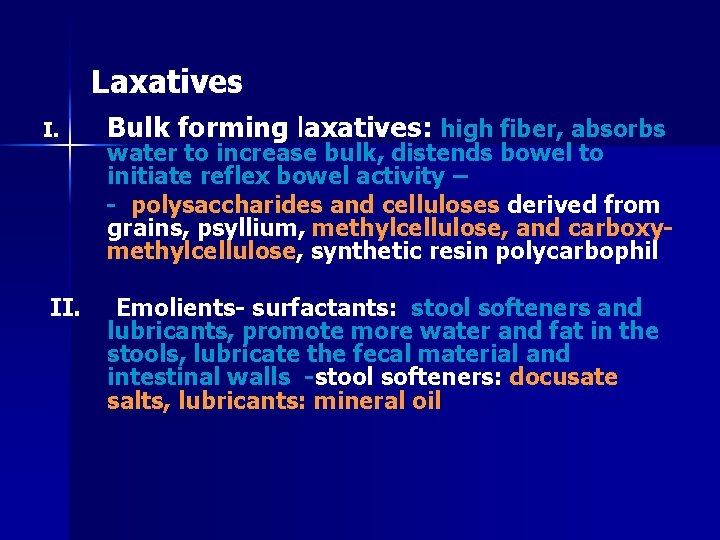
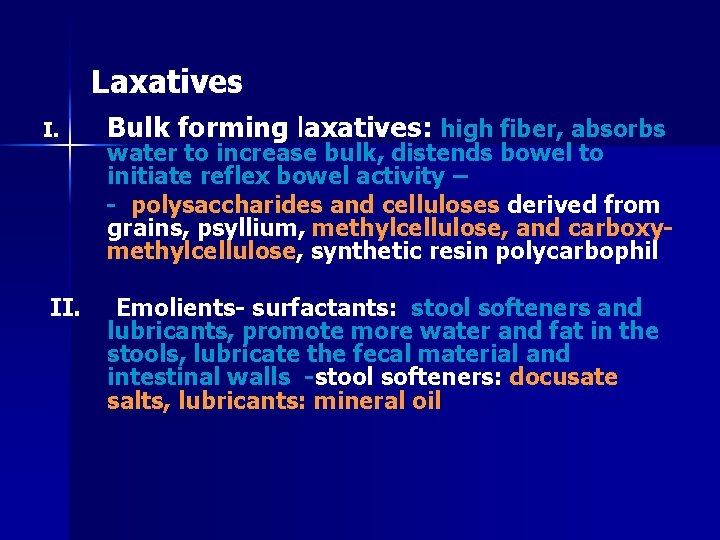
Laxatives I. II. Bulk forming laxatives: high fiber, absorbs water to increase bulk, distends bowel to initiate reflex bowel activity – - polysaccharides and celluloses derived from grains, psyllium, methylcellulose, and carboxymethylcellulose, synthetic resin polycarbophil Emolients- surfactants: stool softeners and lubricants, promote more water and fat in the stools, lubricate the fecal material and intestinal walls -stool softeners: docusate salts, lubricants: mineral oil
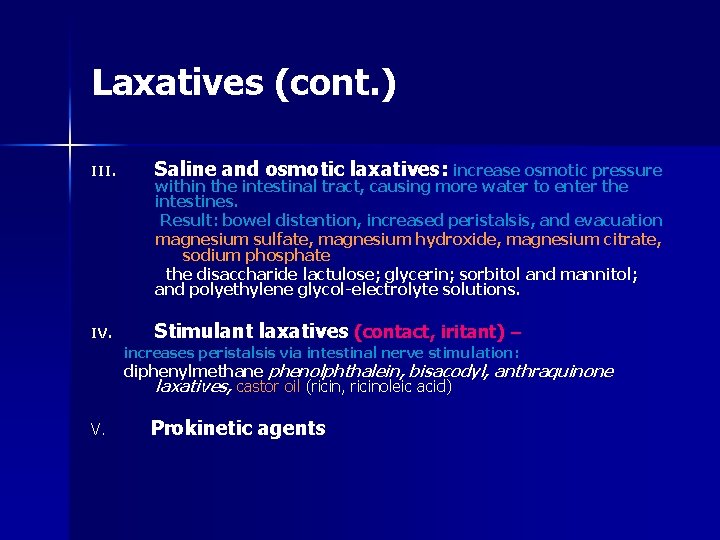
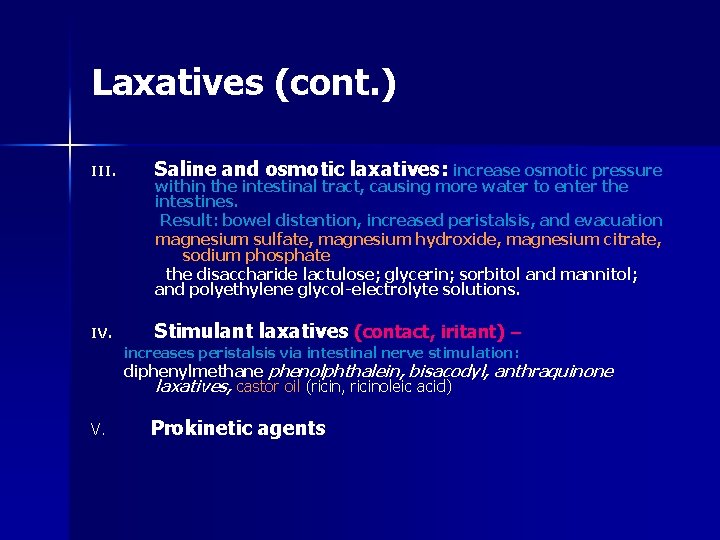
Laxatives (cont. ) III. Saline and osmotic laxatives: increase osmotic pressure IV. Stimulant laxatives (contact, iritant) – within the intestinal tract, causing more water to enter the intestines. Result: bowel distention, increased peristalsis, and evacuation magnesium sulfate, magnesium hydroxide, magnesium citrate, sodium phosphate the disaccharide lactulose; glycerin; sorbitol and mannitol; and polyethylene glycol-electrolyte solutions. increases peristalsis via intestinal nerve stimulation : diphenylmethane phenolphthalein, bisacodyl, anthraquinone laxatives, castor oil (ricin, ricinoleic acid) V. Prokinetic agents
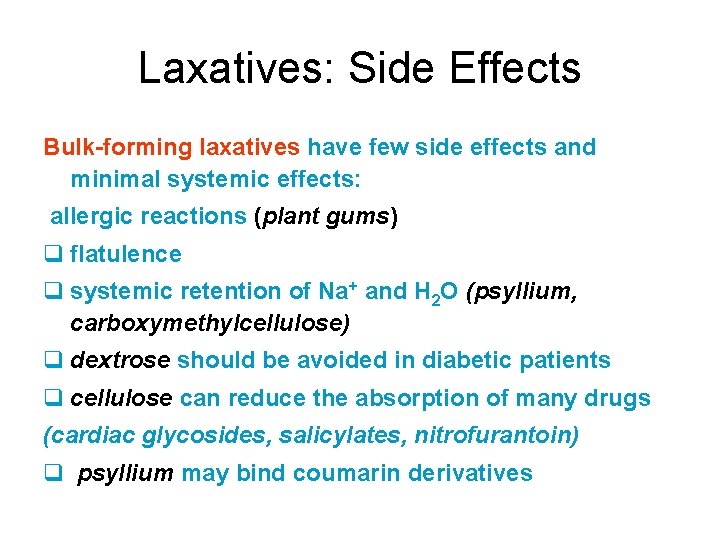
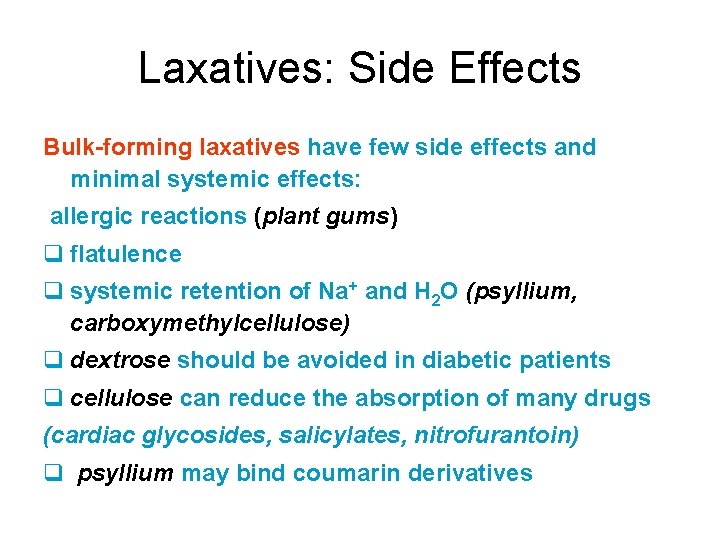
Laxatives: Side Effects Bulk-forming laxatives have few side effects and minimal systemic effects: allergic reactions (plant gums) q flatulence q systemic retention of Na+ and H 2 O (psyllium, carboxymethylcellulose) q dextrose should be avoided in diabetic patients q cellulose can reduce the absorption of many drugs (cardiac glycosides, salicylates, nitrofurantoin) q psyllium may bind coumarin derivatives
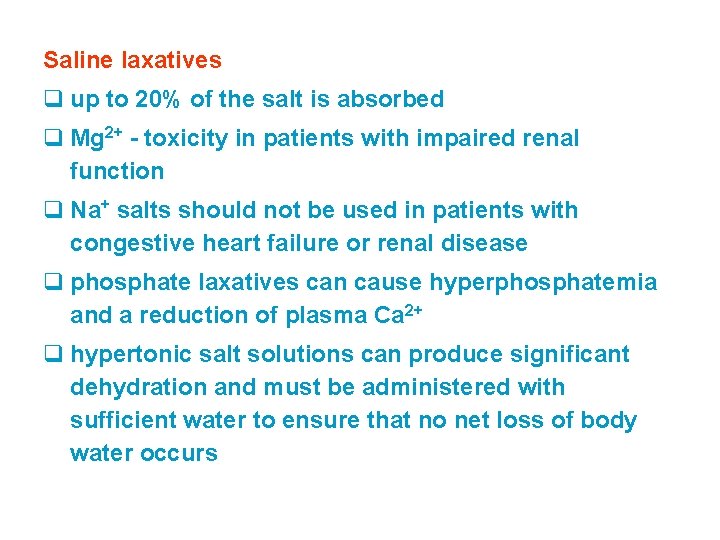
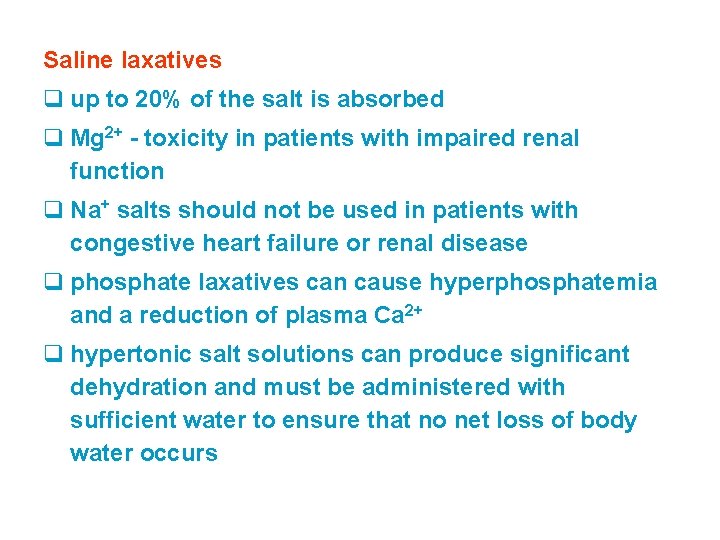
Saline laxatives q up to 20% of the salt is absorbed q Mg 2+ - toxicity in patients with impaired renal function q Na+ salts should not be used in patients with congestive heart failure or renal disease q phosphate laxatives can cause hyperphosphatemia and a reduction of plasma Ca 2+ q hypertonic salt solutions can produce significant dehydration and must be administered with sufficient water to ensure that no net loss of body water occurs
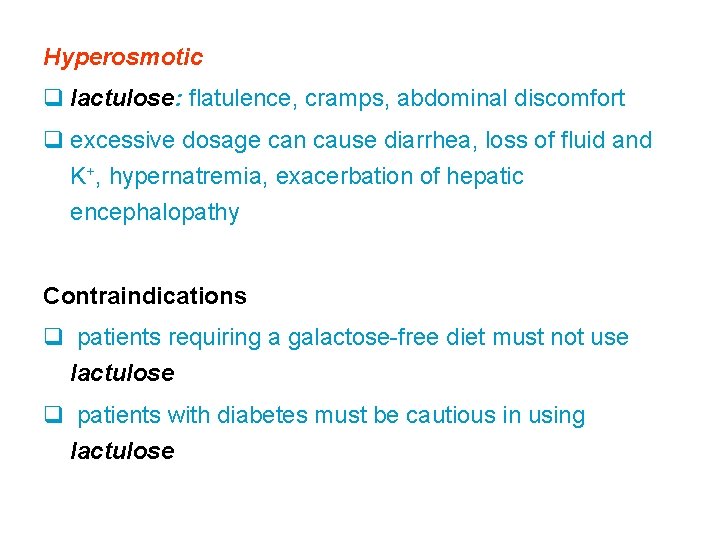
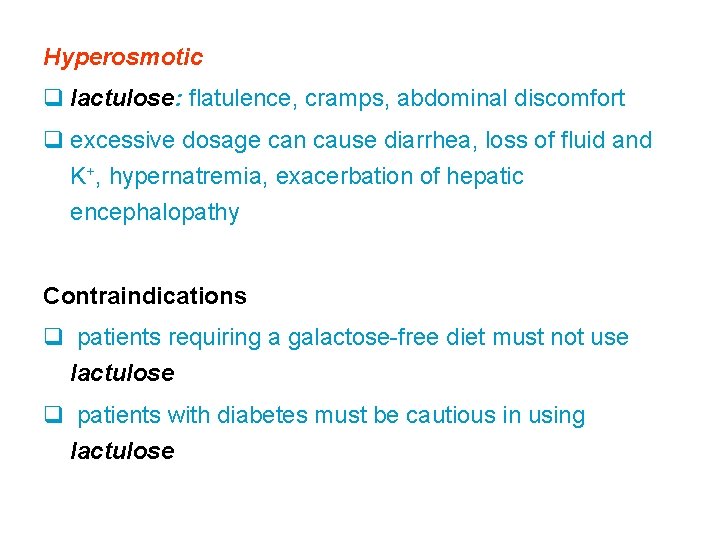
Hyperosmotic q lactulose: flatulence, cramps, abdominal discomfort q excessive dosage can cause diarrhea, loss of fluid and K+, hypernatremia, exacerbation of hepatic encephalopathy Contraindications q patients requiring a galactose-free diet must not use lactulose q patients with diabetes must be cautious in using lactulose
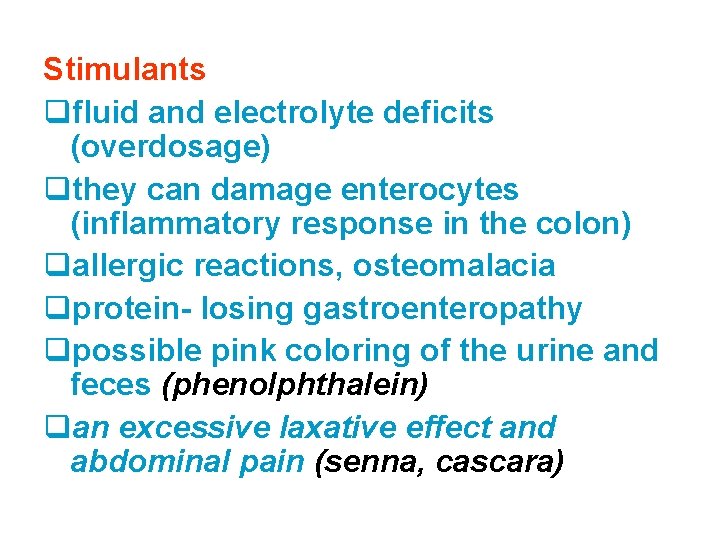
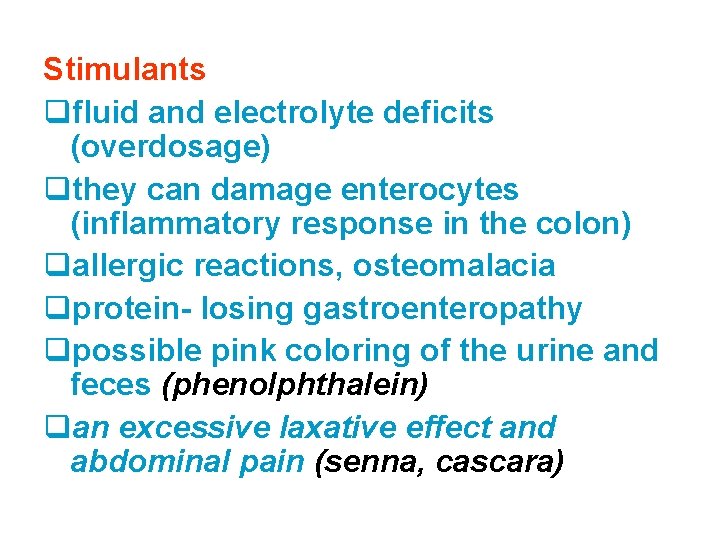
Stimulants qfluid and electrolyte deficits (overdosage) qthey can damage enterocytes (inflammatory response in the colon) qallergic reactions, osteomalacia qprotein- losing gastroenteropathy qpossible pink coloring of the urine and feces (phenolphthalein) qan excessive laxative effect and abdominal pain (senna, cascara)

Prokinetic agents
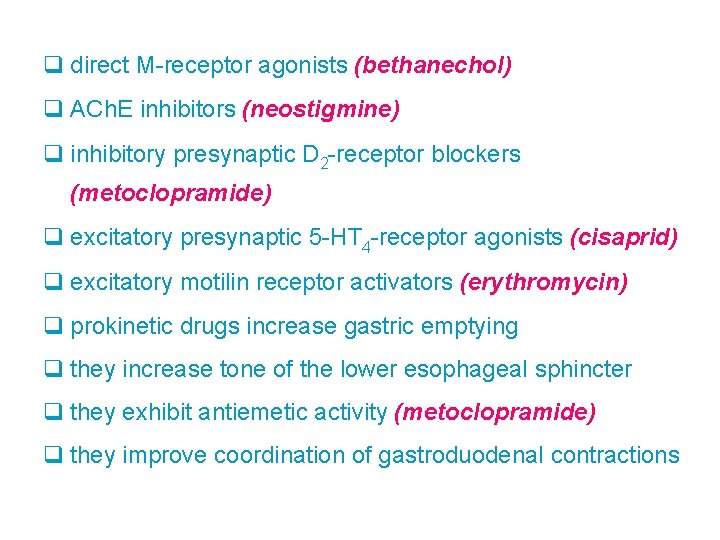
q direct M-receptor agonists (bethanechol) q ACh. E inhibitors (neostigmine) q inhibitory presynaptic D 2 -receptor blockers (metoclopramide) q excitatory presynaptic 5 -HT 4 -receptor agonists (cisaprid) q excitatory motilin receptor activators (erythromycin) q prokinetic drugs increase gastric emptying q they increase tone of the lower esophageal sphincter q they exhibit antiemetic activity (metoclopramide) q they improve coordination of gastroduodenal contractions
Side effects q cholinergic agonists have variety of muscarinic side effects (excess GI secretions, cramps, salivation, sweating, urination, lacrimation, defecation) q dopamine-receptor dystonia, antagonists Parkinson´s can induce disease-like effects hyperprolactinemia (gynecomastia, galactorhea

Diarrhoea
Diarrhoea • Traveller’s diarrhoea is one of the most common illnesses for tourists going to tropical climates. As many as 60% of all travellers suffer some form of diarrhoea


Some drugs causing diarrhoea • Adrenergic neuron blocking agents (reserpine, quanethidine) • Antimicrobials (e. g. sulfonamides, tetracyclines, most broad spectrum ATB • Cholinergic agonists and cholinesterase inhibitors • Procinetic agents (metoclopramide, domperidone, cisapride) • Prostaglandins • Quinidine
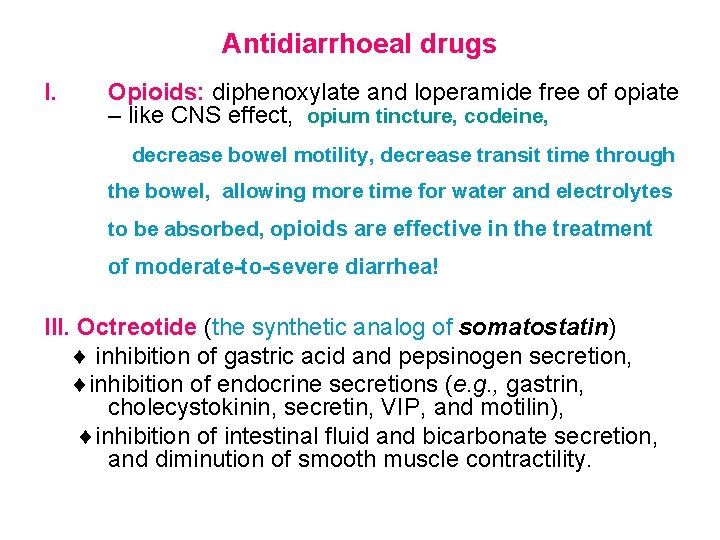
Antidiarrhoeal drugs I. Opioids: diphenoxylate and loperamide free of opiate – like CNS effect, opium tincture, codeine, decrease bowel motility, decrease transit time through the bowel, allowing more time for water and electrolytes to be absorbed, opioids are effective in the treatment of moderate-to-severe diarrhea! III. Octreotide (the synthetic analog of somatostatin) inhibition of gastric acid and pepsinogen secretion, inhibition of endocrine secretions (e. g. , gastrin, cholecystokinin, secretin, VIP, and motilin), inhibition of intestinal fluid and bicarbonate secretion, and diminution of smooth muscle contractility.
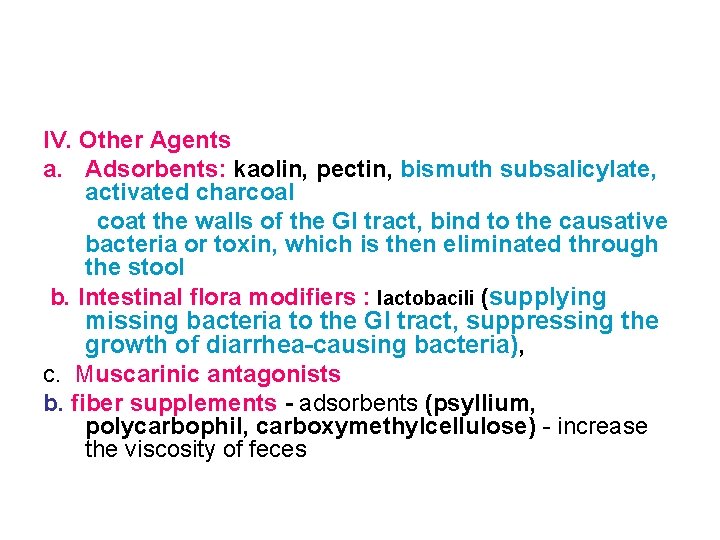
IV. Other Agents a. Adsorbents: kaolin, pectin, bismuth subsalicylate, activated charcoal coat the walls of the GI tract, bind to the causative bacteria or toxin, which is then eliminated through the stool b. Intestinal flora modifiers : lactobacili (supplying missing bacteria to the GI tract, suppressing the growth of diarrhea-causing bacteria), c. Muscarinic antagonists b. fiber supplements - adsorbents (psyllium, polycarbophil, carboxymethylcellulose) - increase the viscosity of feces

Antiemetics
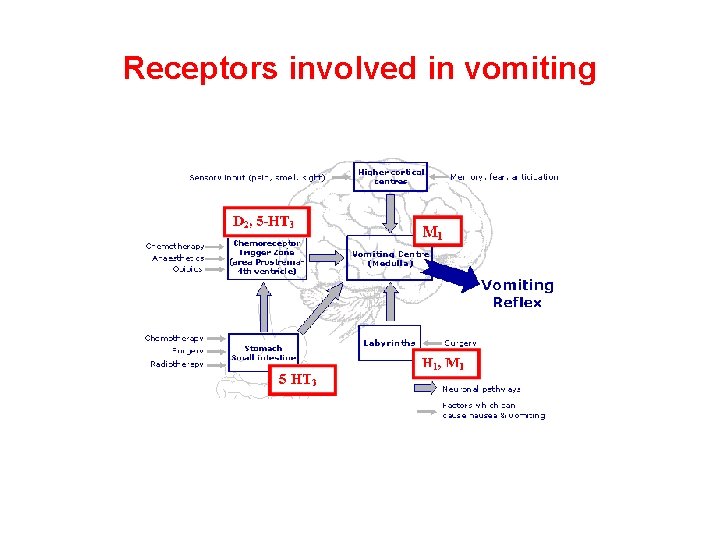
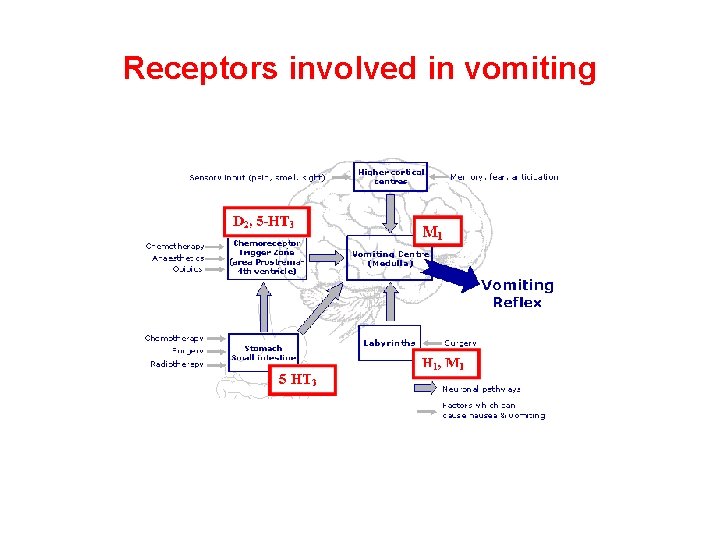
Receptors involved in vomiting

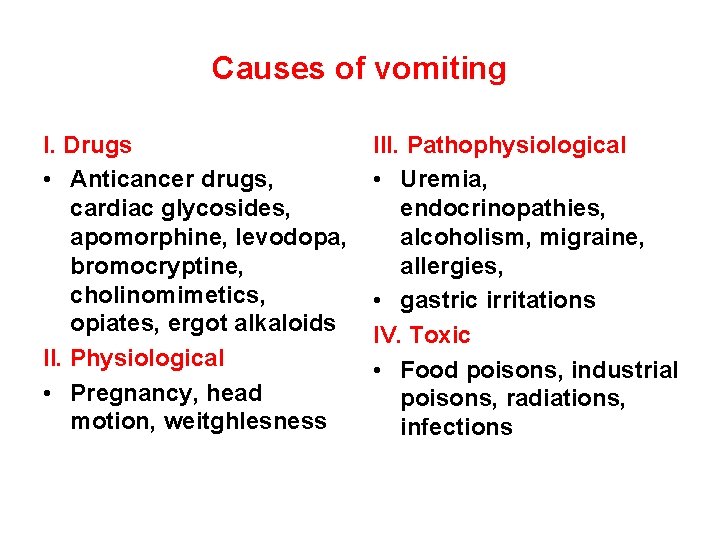
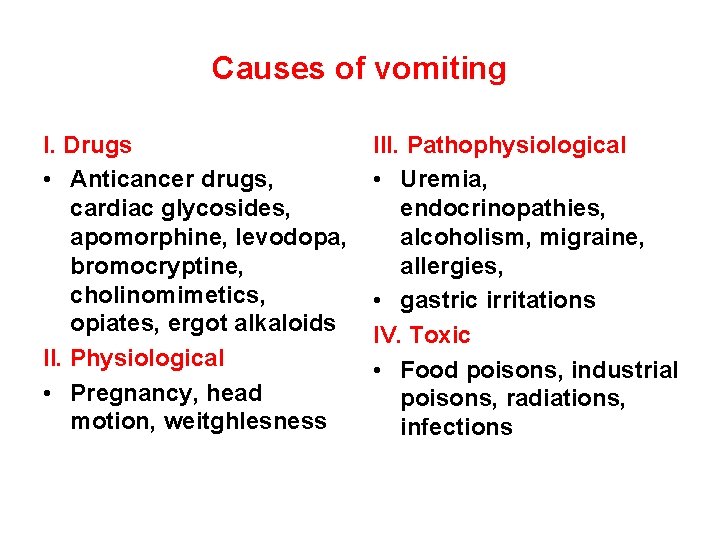
Causes of vomiting I. Drugs • Anticancer drugs, cardiac glycosides, apomorphine, levodopa, bromocryptine, cholinomimetics, opiates, ergot alkaloids II. Physiological • Pregnancy, head motion, weitghlesness III. Pathophysiological • Uremia, endocrinopathies, alcoholism, migraine, allergies, • gastric irritations IV. Toxic • Food poisons, industrial poisons, radiations, infections
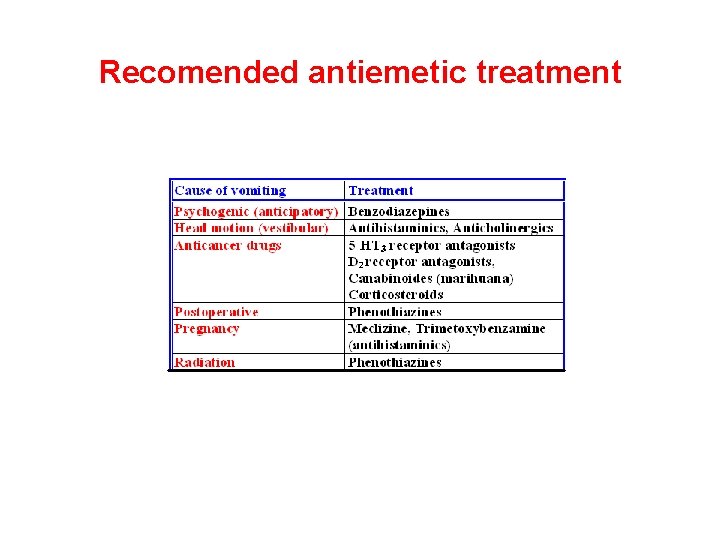
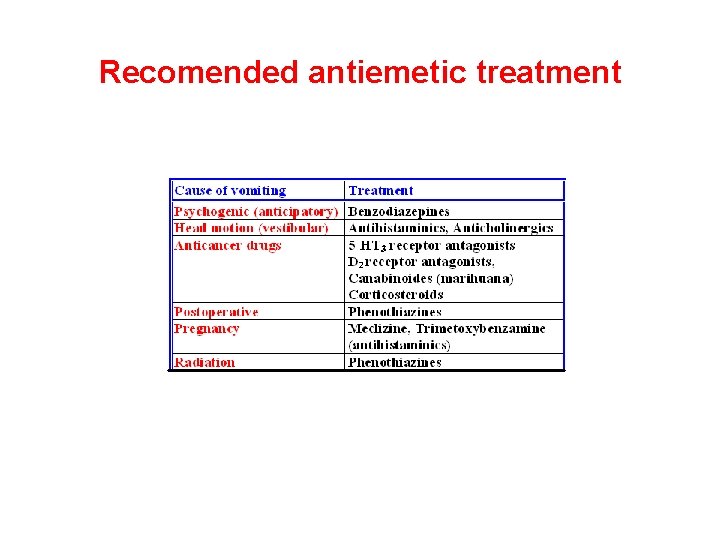
Recomended antiemetic treatment
 라즈베리 gpio
라즈베리 gpio Praktika koht
Praktika koht Boundaries meme
Boundaries meme Which seedless plants have been used to treat bee stings
Which seedless plants have been used to treat bee stings Is byetta used to treat pcos
Is byetta used to treat pcos Why are seedless vascular plants important
Why are seedless vascular plants important Eva tray in labour room
Eva tray in labour room Contraindicated drugs in pregnancy
Contraindicated drugs in pregnancy Diener 1976 trick or treat
Diener 1976 trick or treat Number needed to treat
Number needed to treat The eraser challenge
The eraser challenge Treat with confidence
Treat with confidence Invitation to treat
Invitation to treat Treat someone with contempt
Treat someone with contempt Mffmm
Mffmm How to calculate number needed to treat
How to calculate number needed to treat What is wrong with tom robinson's arm
What is wrong with tom robinson's arm How did jay gould spend his money
How did jay gould spend his money Laryngopharyngeal reflux (
Laryngopharyngeal reflux ( Colours of halloween song
Colours of halloween song Mole day treat ideas
Mole day treat ideas Guthing vs lynn case
Guthing vs lynn case Treat the earth well
Treat the earth well What would juliet rather do than marry paris?
What would juliet rather do than marry paris? Epidydmis
Epidydmis Romeo and juliet act 2 scene 4
Romeo and juliet act 2 scene 4 How to calculate number needed to treat
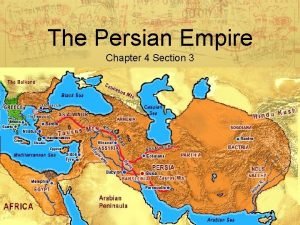
How to calculate number needed to treat Chapter 4 section 3 the persian empire
Chapter 4 section 3 the persian empire How did the scotch half breed treat the dogs
How did the scotch half breed treat the dogs Who is mr. kirwin and how does he treat victor?
Who is mr. kirwin and how does he treat victor? The persian empire chapter 4 section 3
The persian empire chapter 4 section 3 How does mirabella interact with the rest of the pack
How does mirabella interact with the rest of the pack How to treat bursitis in the hip
How to treat bursitis in the hip Number needed to harm
Number needed to harm Treat the earth well quote
Treat the earth well quote Number needed to treat calculation
Number needed to treat calculation To kill a mockingbird racism chapter 1
To kill a mockingbird racism chapter 1 Treat everyone with sincerity
Treat everyone with sincerity Numbers needed to treat
Numbers needed to treat How did henry ford treat his workers
How did henry ford treat his workers Factors that helped the spread of christianity
Factors that helped the spread of christianity Treat others the way you would like to be
Treat others the way you would like to be Equation for number needed to treat
Equation for number needed to treat Earl treat aa
Earl treat aa Fisher v bell literal rule
Fisher v bell literal rule What is the main idea of the ant and the grasshopper
What is the main idea of the ant and the grasshopper Suspension trauma treatment
Suspension trauma treatment Study population
Study population Offer
Offer