New Hampshire EMTIntermediate Cardiology New Hampshire Division of
























- Slides: 99
New Hampshire EMT-Intermediate Cardiology New Hampshire Division of Fire Standards & Training and Emergency Medical Services
Objectives p Describe the incidence, morbidity, and mortality of cardiovascular disease. p Discuss prevention strategies that may reduce morbidity and mortality of cardiovascular disease. p Identify the risk factors most predisposing to coronary artery disease.

Objectives p Describe the anatomy of the heart, including the position in the thoracic cavity, layers of the hear chambers, and location and function of cardiac valves. p Identify the major structures of the vascular system. p Describe the distribution of the coronary arteries and the parts of the heart supplied by each artery. p Differentiate the structural and functional aspects of arterial and venous blood vessels.

Objectives continued Define the following terms that refer to cardiac physiology: p n n n Stroke volume Starling’s Law Preload Afterload Cardiac output Blood pressure p Describe the electrical properties of the heart. p Describe the normal sequence of electrical conduction through the heart and state the purpose of this conduction system.

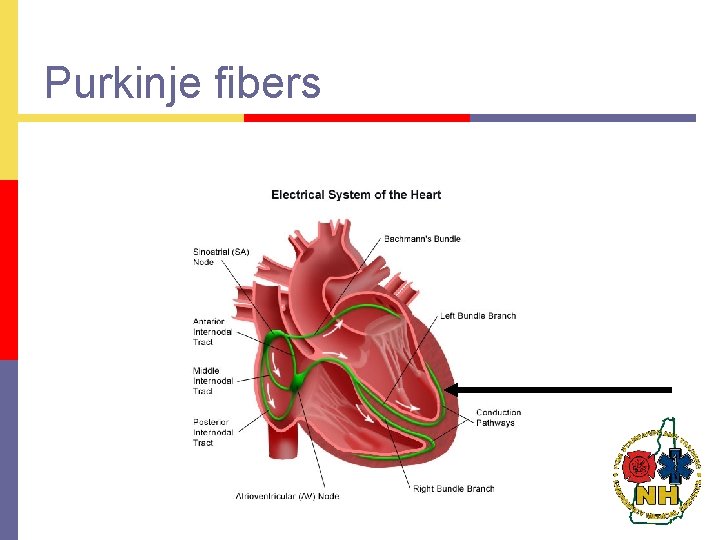
Objectives continued Describe the location and function of the following structures of the electrical conduction system: (C-1) p n n n SA node Internodal and interatrial tracts AV node Bundle of His Bundle branches Purkinje fibers p Define cardiac depolarization and repolarization and describe the major electrolyte changes that occur in each process. (C-1) p Describe an ECG. (C-1) Explain the purpose of ECG monitoring and its limitations. (C-1) p
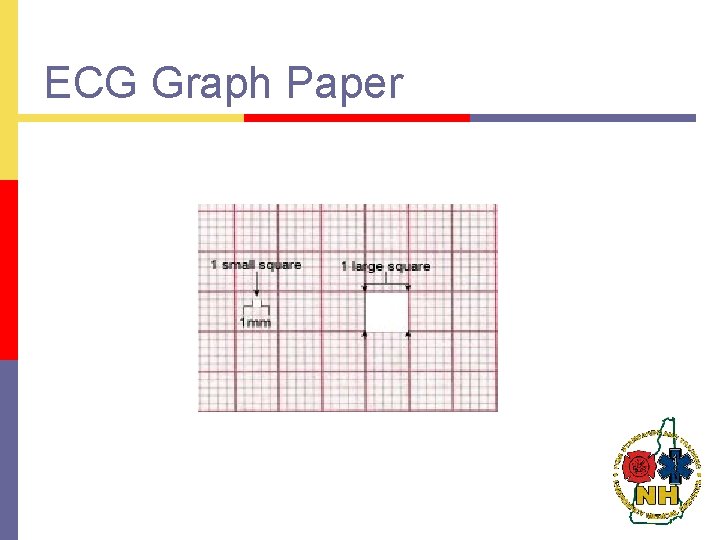
Objectives continued p p p Define the following terms as they relate to the electrical activity of the heart: n Isoelectric line n QRS complex n P wave State the numerical values assigned to each small and each large box on the ECG graph paper for each axis. Define ECG artifact and name the causes. p Correlate the electrophysiological and hemodynamic events occurring throughout the entire cardiac cycle with the various ECG wave forms, segments and intervals. p Relate the cardiac surfaces or areas represented by the ECG leads. p Given an ECG, identify the arrhythmia. p Describe a systematic approach to analysis and interpretation of cardiac dysrhythmias.
Objectives continued p p p Describe the dysrhythmias originating in the sinus node and the ventricles. Describe the process and pitfalls of differentiating wide QRS complex tachycardias. Describe the term “cardiac arrest”. Describe the arrhythmias seen in cardiac arrest. Identify the critical actions necessary in caring for the patient with cardiac arrest. Explain how to confirm asystole using the 3 -lead ECG. List the clinical indications for defibrillation. Describe the most commonly used pharmacological agents in the management of cardiac arrest for EMT-Intermediates. Identify resuscitation. Identify circumstances and situations where resuscitation efforts would not be initiated. Identify local protocol dictating circumstances and situations where resuscitation efforts would be discontinued.
Objectives continued Integrate the pathophysiology principles to the assessment of the patient with cardiac arrest. Synthesize assessment findings to formulate a rapid intervention for a patient in cardiac arrest. Describe the conditions of pulseless electrical activity. Value and defend the urgency in rapid determination of and rapid intervention of patients in cardiac arrest. Identify the location of the structures listed in cognitive objective #2. Demonstrate how to set and adjust the ECG monitor settings to varying patient situations. Demonstrate a working knowledge of various ECG lead systems Demonstrate satisfactory performance of psychomotor skills of basic and advanced life support techniques according to the current American Heart Association standards and guidelines, including: p p p p n n p Cardiopulmonary resuscitation Defibrillation Demonstrate how to record an ECG
Incidence p Prevalence of cardiac death outside of a hospital n p Prevalence of warning signs and symptoms for cardiac emergencies n p Supportive statistics Increased recognition of need for early reperfusion
Morbidity/ mortality Reduced with early recognition p Reduced with early access to EMS system p

Risk factors Age p Family history p Hypertension p Lipids p Male sex p Smoking p Carbohydrate intolerance p
Possible contributing risks Diet p Female sex p Obesity p Oral contraceptives p Sedentary living p Personality type p Psychosocial tensions p
Prevention Strategies Early recognition p Education p Alteration of life style p

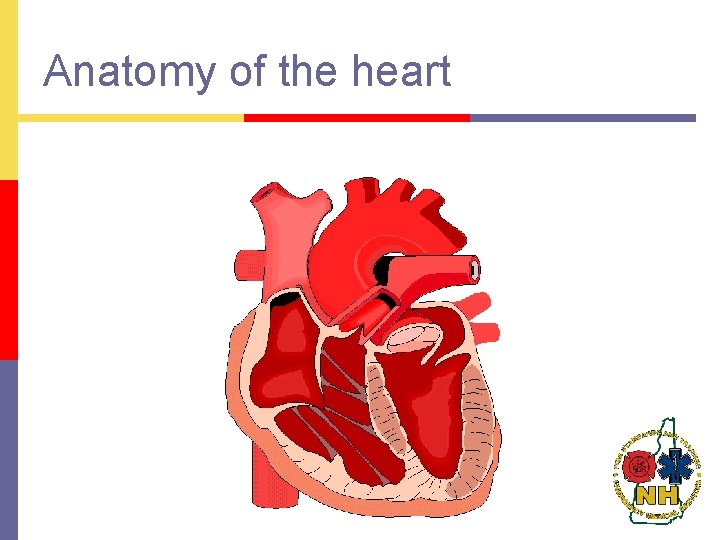
Anatomy of the Heart
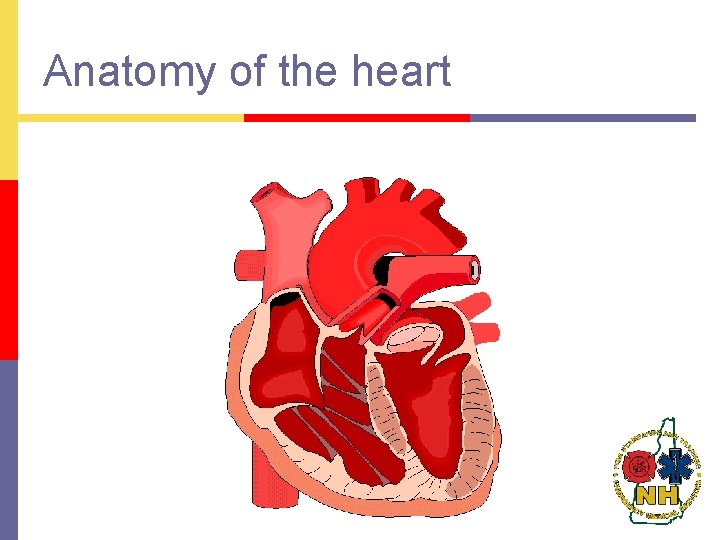
Anatomy of the heart
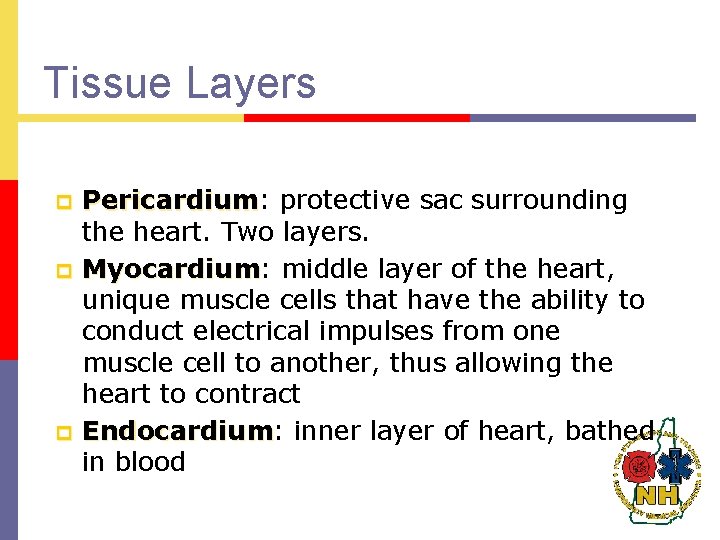
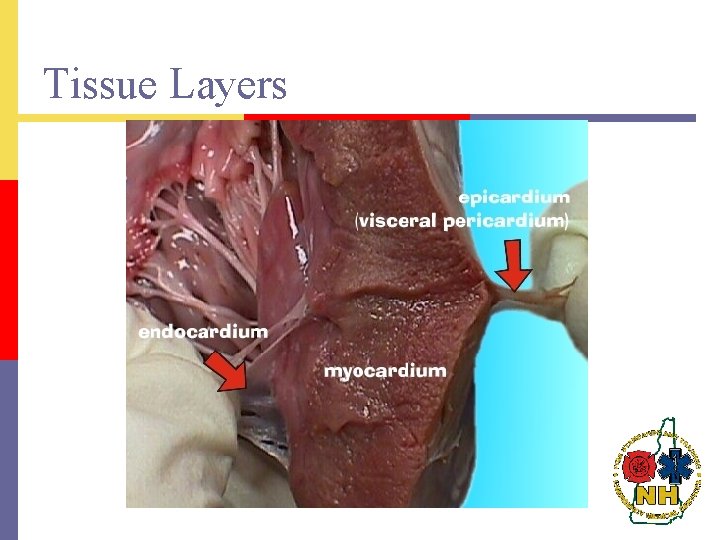
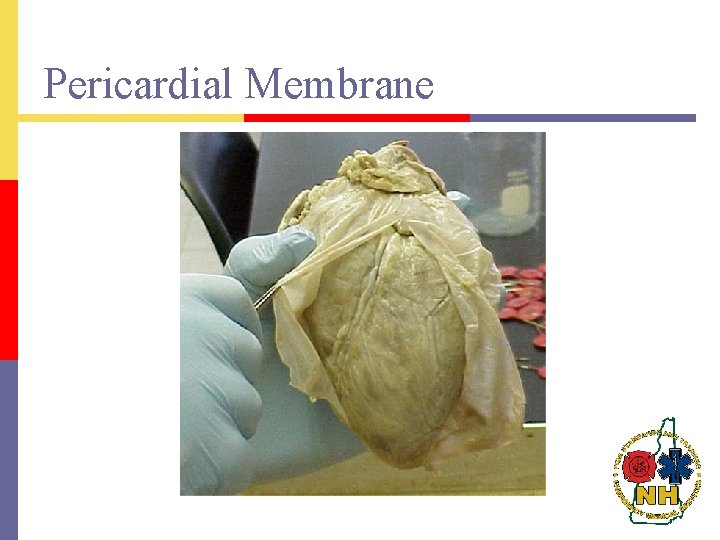
Tissue Layers p p p Pericardium: Pericardium protective sac surrounding the heart. Two layers. Myocardium: Myocardium middle layer of the heart, unique muscle cells that have the ability to conduct electrical impulses from one muscle cell to another, thus allowing the heart to contract Endocardium: Endocardium inner layer of heart, bathed in blood
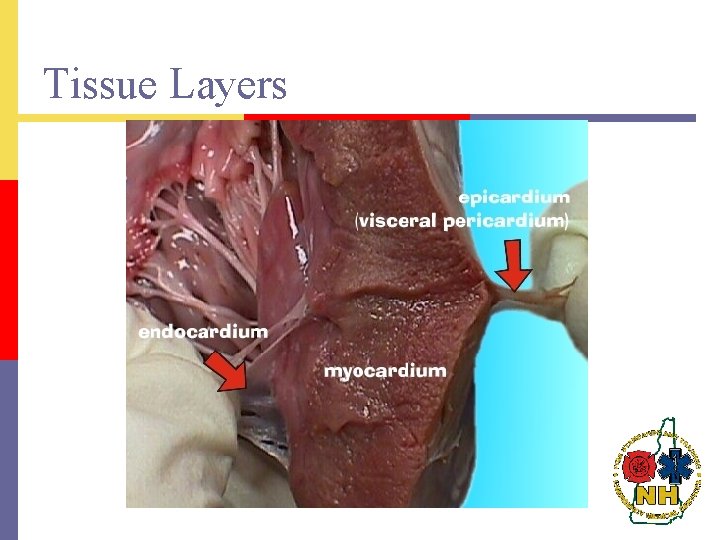
Tissue Layers
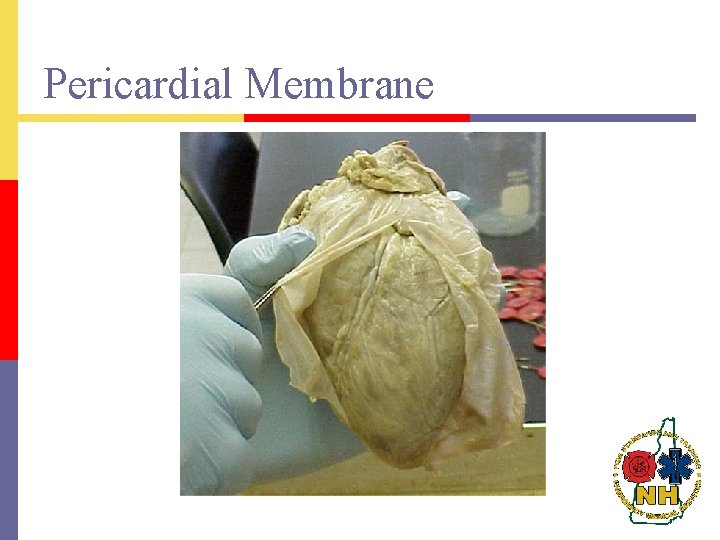
Pericardial Membrane
Chambers p Atria: Atria superior chambers that receive incoming blood n p Right & Left Ventricles: Ventricles inferior chambers that pump blood out of the heart n Right & Left
Heart Valves Tricupid Valve: Valve right aterioventricular valve; 3 cusps or leaflets p Bicupid (Mitral) Valve: Valve left aterioventricular valve; 2 cusps or leaflets p Pulmonic Valve: Valve right semilunar valve p Aortic Valve: Valve left semilunar valve p

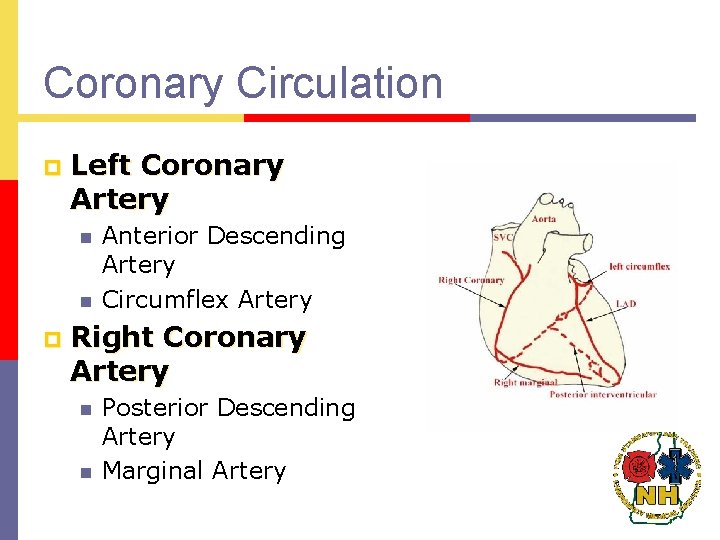
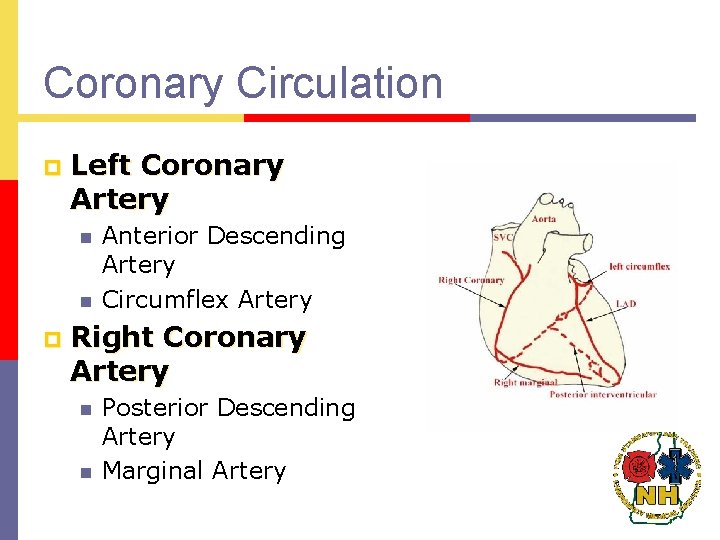
Coronary Circulation p Left Coronary Artery n n p Anterior Descending Artery Circumflex Artery Right Coronary Artery n n Posterior Descending Artery Marginal Artery
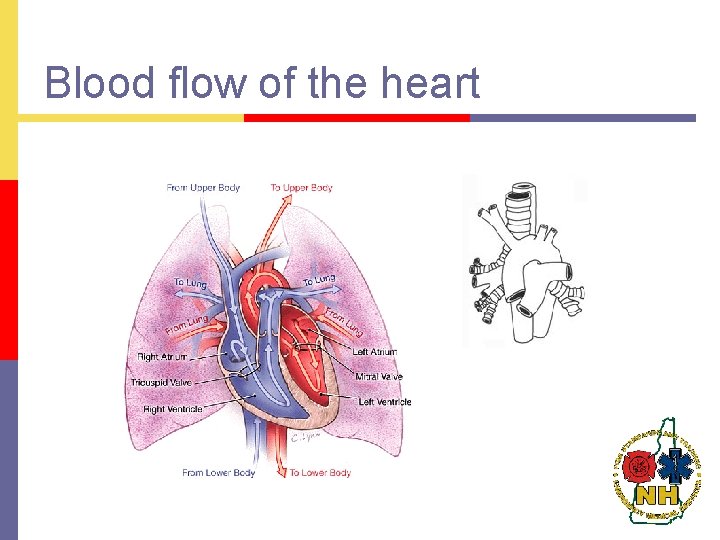
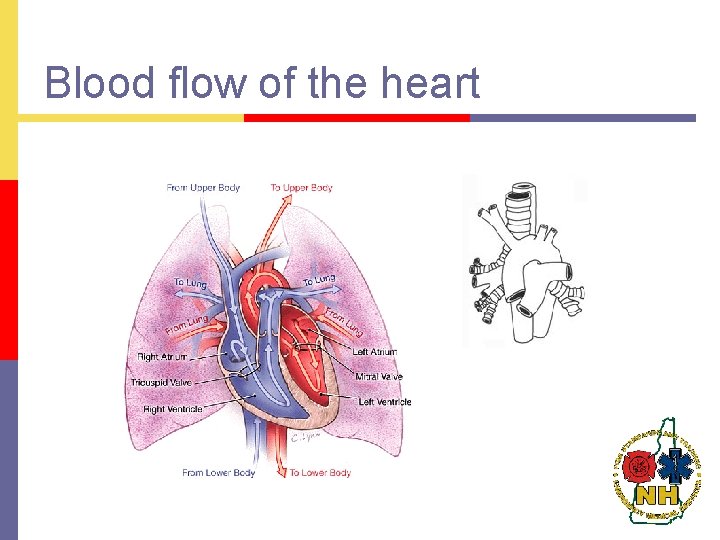
Blood flow of the heart
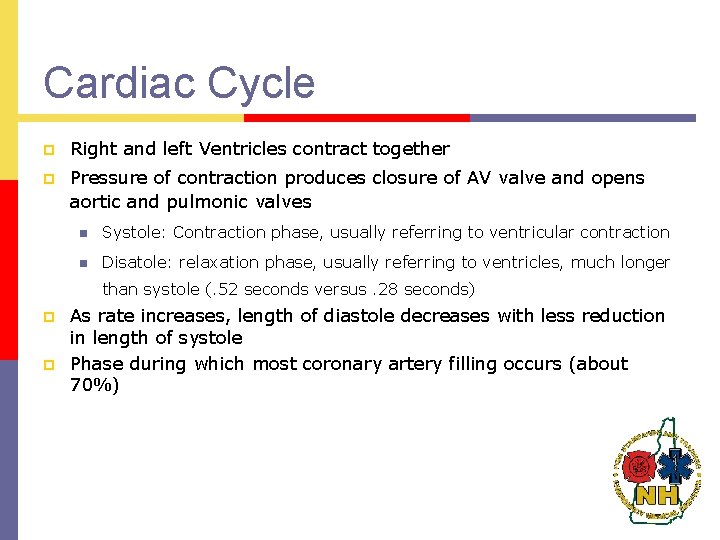
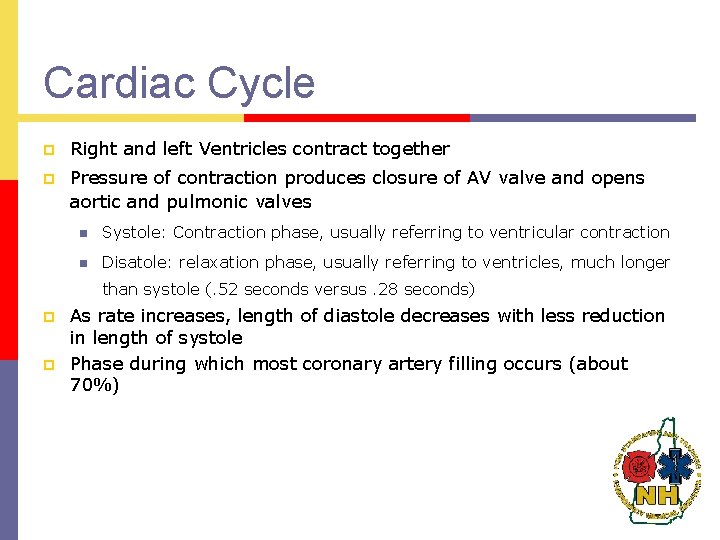
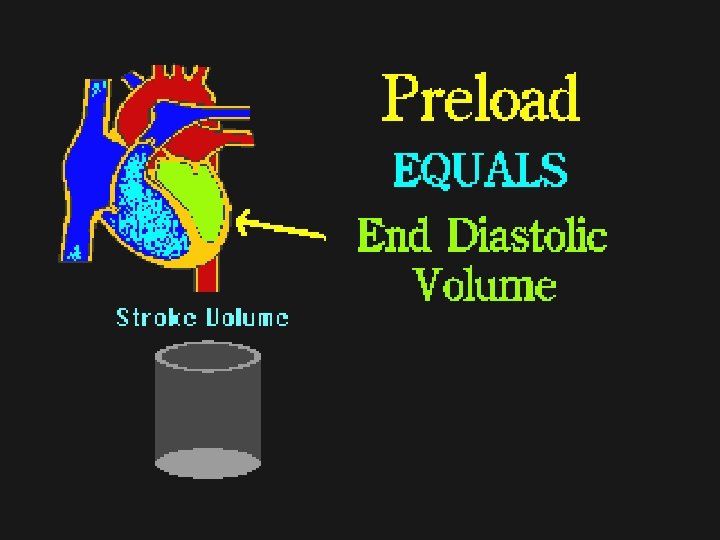
Cardiac Cycle p Right and left Ventricles contract together p Pressure of contraction produces closure of AV valve and opens aortic and pulmonic valves n Systole: Contraction phase, usually referring to ventricular contraction n Disatole: relaxation phase, usually referring to ventricles, much longer than systole (. 52 seconds versus. 28 seconds) p p As rate increases, length of diastole decreases with less reduction in length of systole Phase during which most coronary artery filling occurs (about 70%)
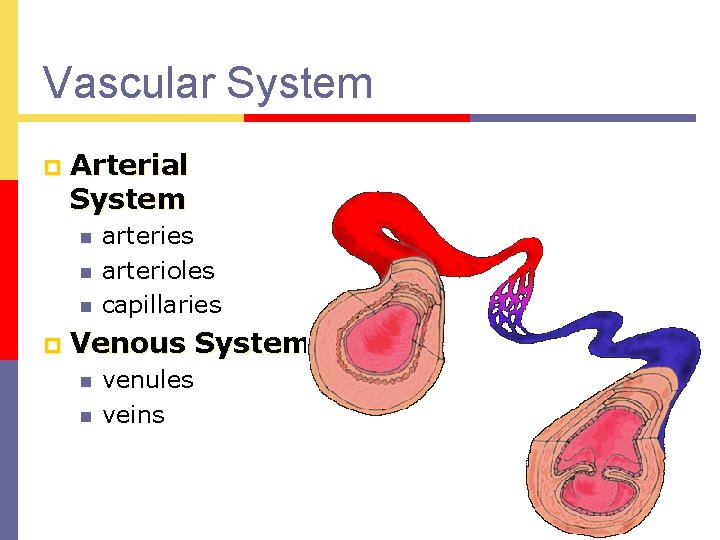
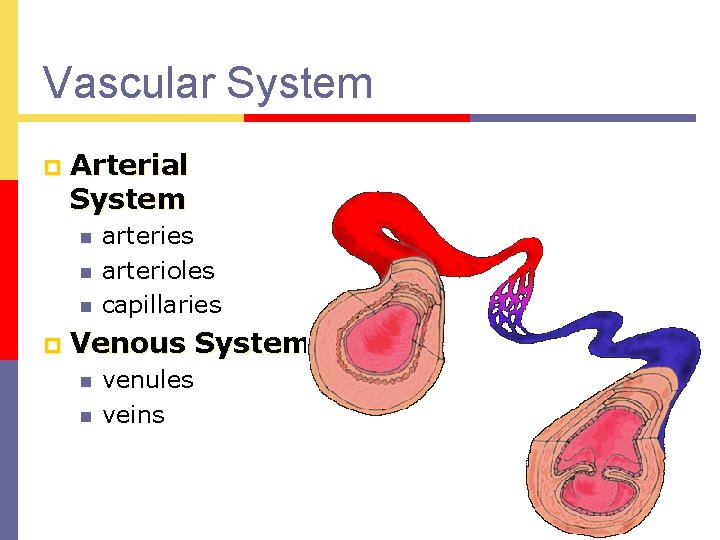
Vascular System p Arterial System n n n p arteries arterioles capillaries Venous System n n venules veins
Cardiac Physiology p To understand EKGs you must thoroughly understand the pumping actions of the cardiac cycle p Diastole: Diastole relaxation phase p Systole: Systole contraction phase
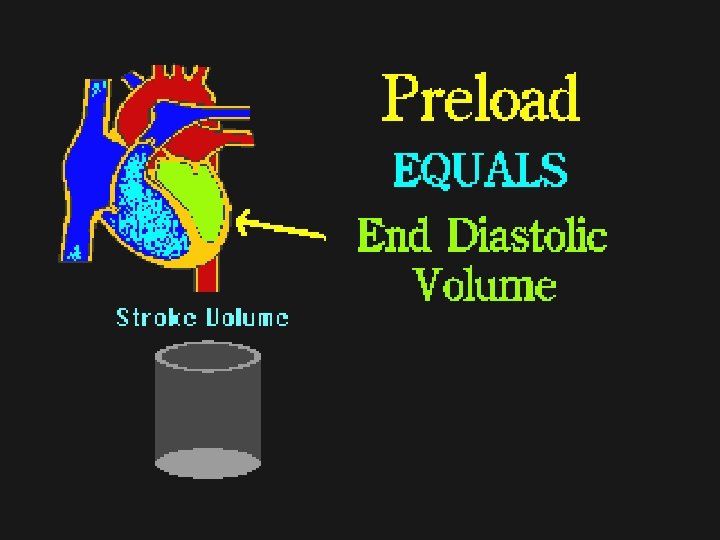
Cardiac Physiology p Stroke volume p Starling’s Law p Preload p Afterload p Cardiac Output p Blood Pressure

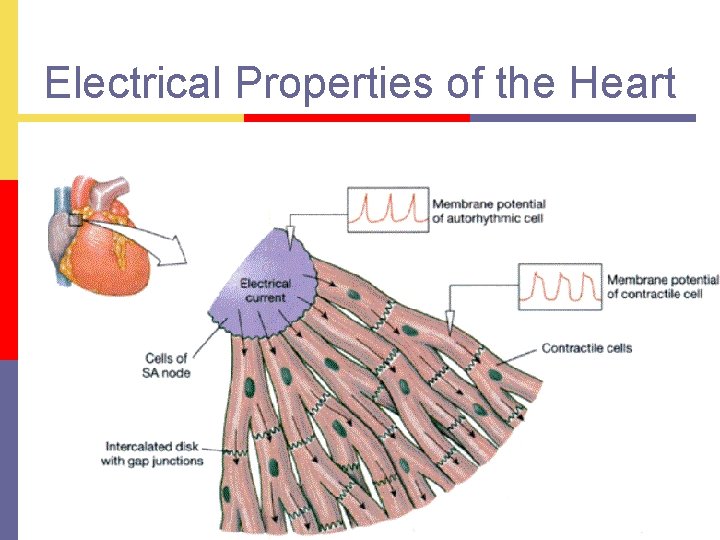
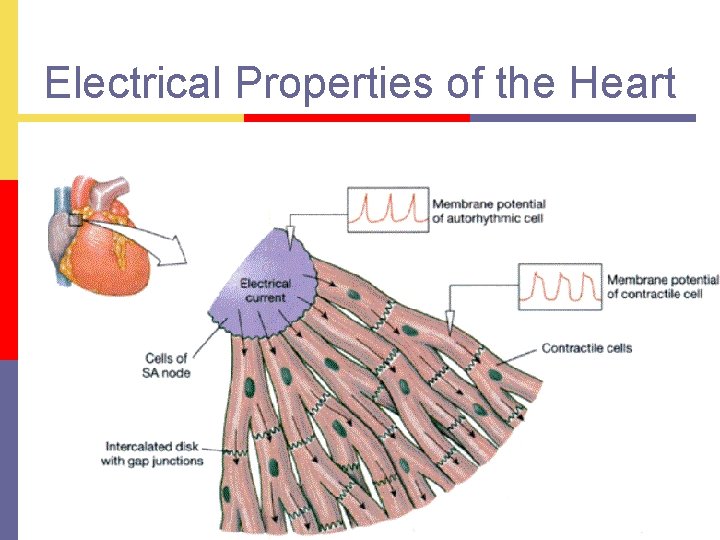
Electrical Properties of the Heart

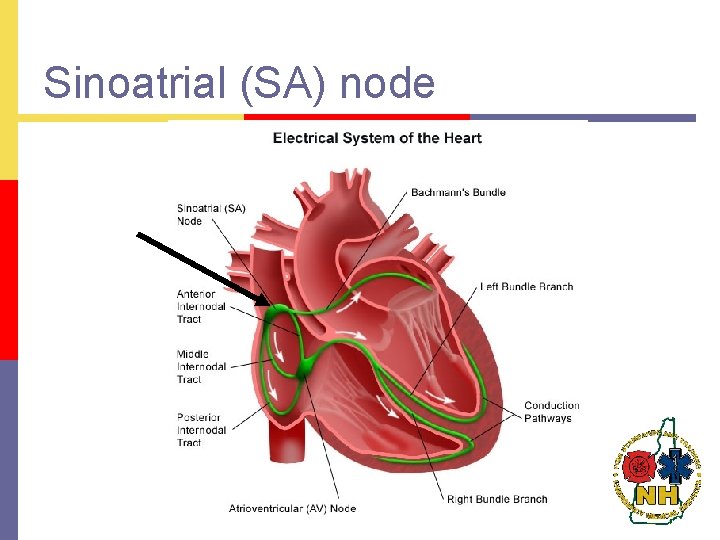
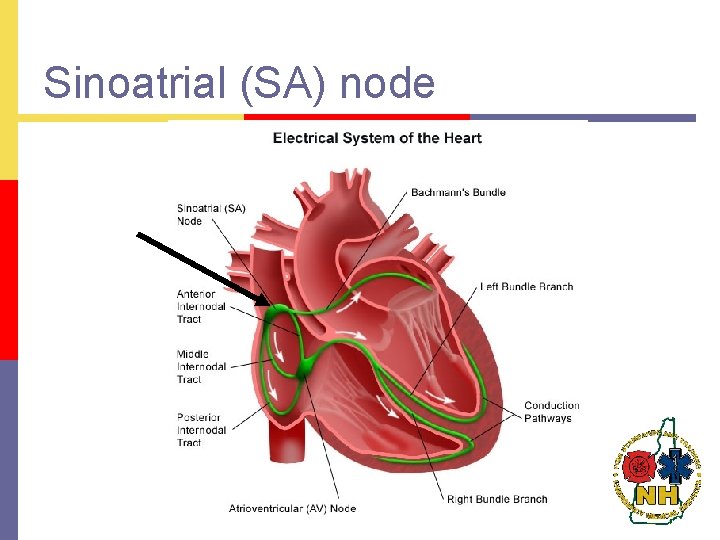
Sinoatrial (SA) node
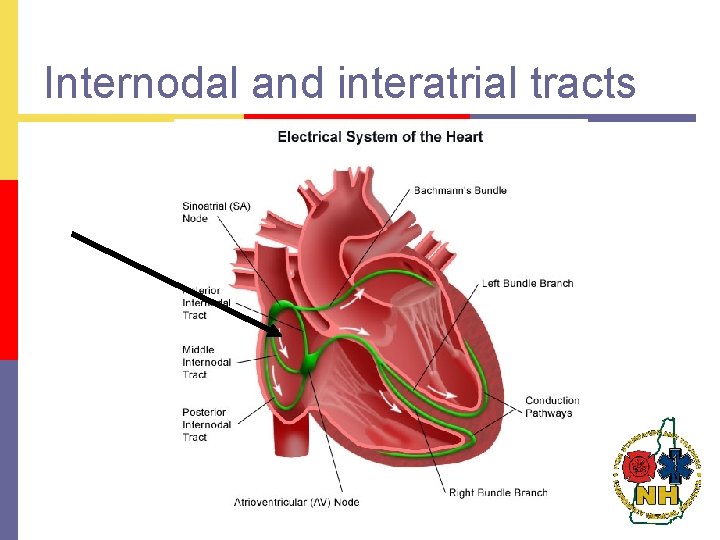
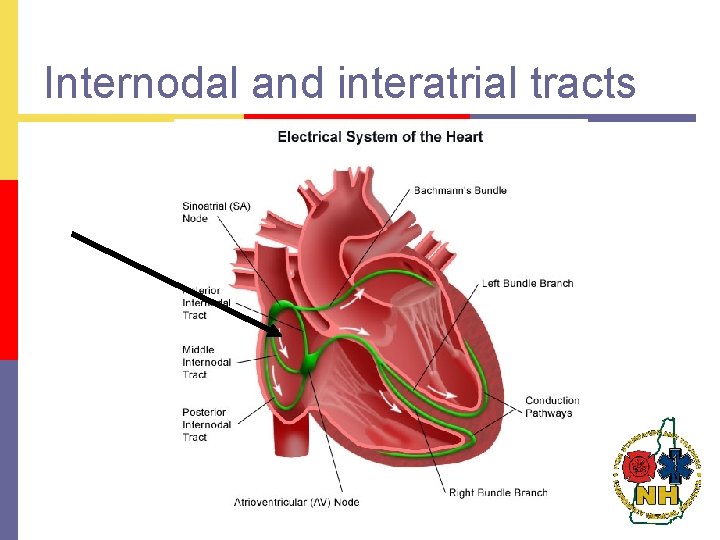
Internodal and interatrial tracts

Atrioventricular (AV) node
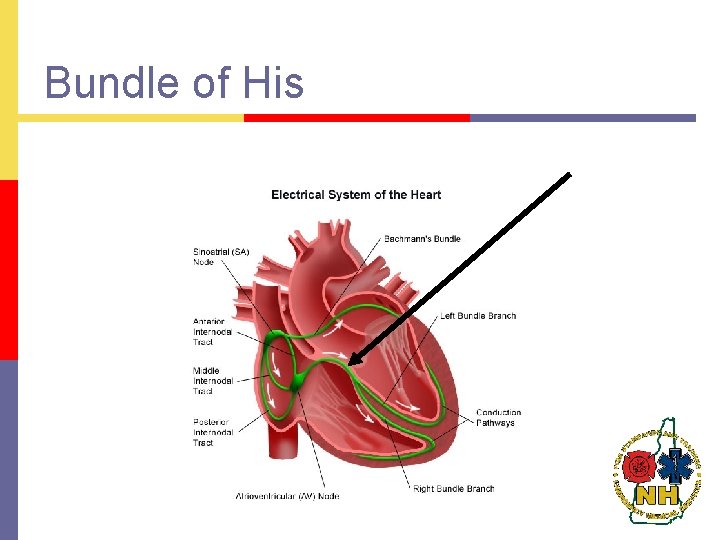
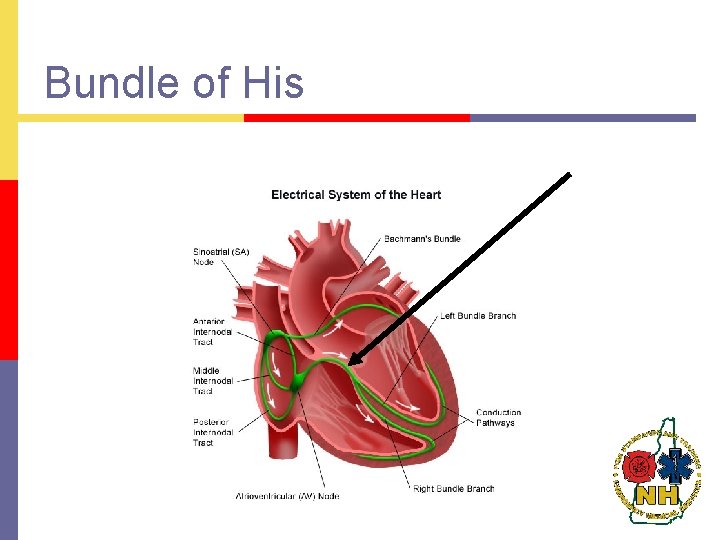
Bundle of His
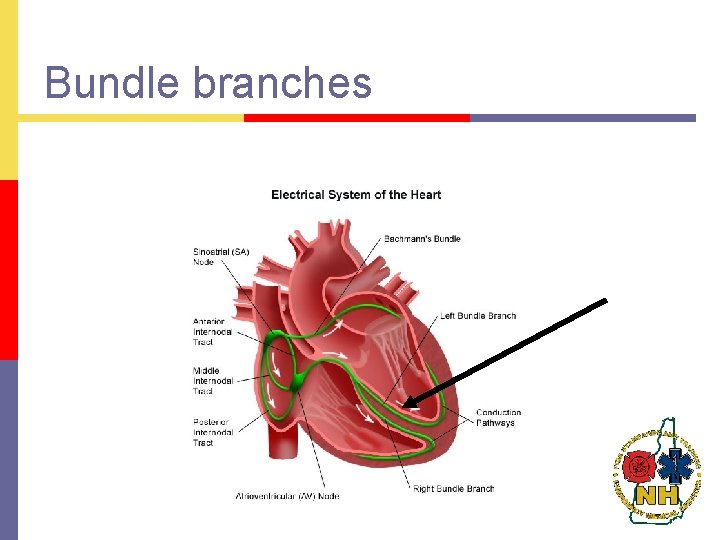
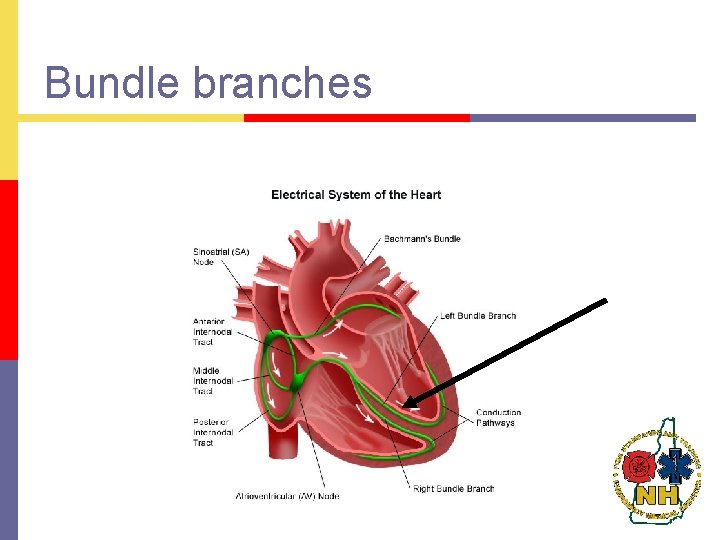
Bundle branches
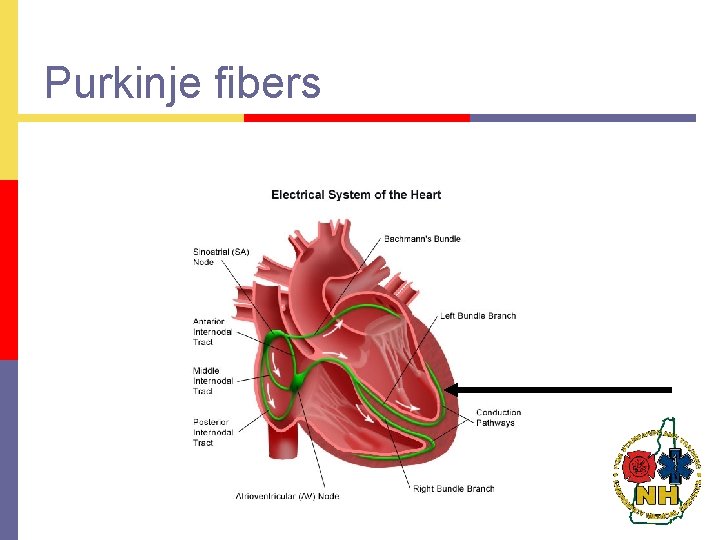
Purkinje fibers

Depolarization p Process by which muscle fibers are stimulated to contract by the alteration of the electrical charge of a cell. Accomplished by changes in electrolyte concentrations across the cell membrane.
Intrinsic Rates p Pacemaker cells capable of self initiated depolarization p Found throughout conduction system except AV node n n n SA node: 60 -100/minute intrinsic rate AV Junction tissue: 40 -60/minute intrinsic rate Ventricles (bundle branches & Purkinje fibers): 20 -40/minute intrinsic rate

Repolarization p Once cells have depolarized, the electrolytes are pumped back to their resting or polarized state. This process is called repolarization.
Autonomic nervous system relationship to Cardiovascular system Medulla Carotid sinus and baroreceptor p p n n Location Significance p Parasympathetic system p Sympathetic n n Alpha-vasoconstriction Beta p p p Inotropic Dromotropic Chronotropic

ECG Monitoring
EGC Monitoring p Electrical activity of the heart p Does NOT indicate mechanical activity of the heart. p Must take a pulse.
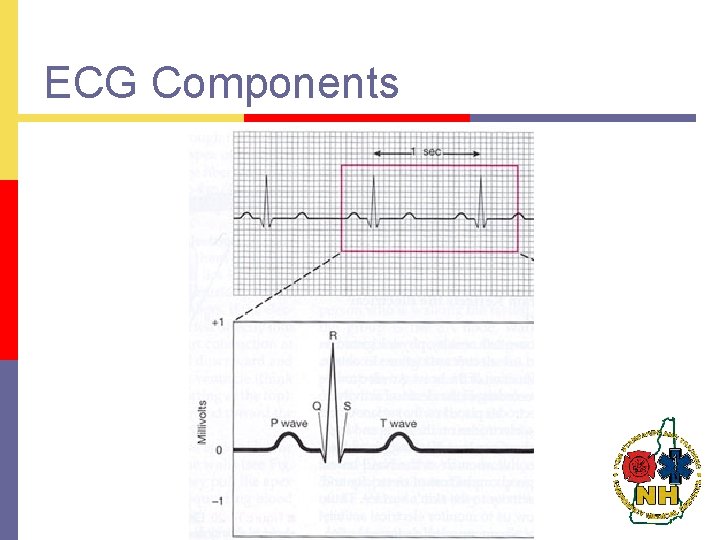
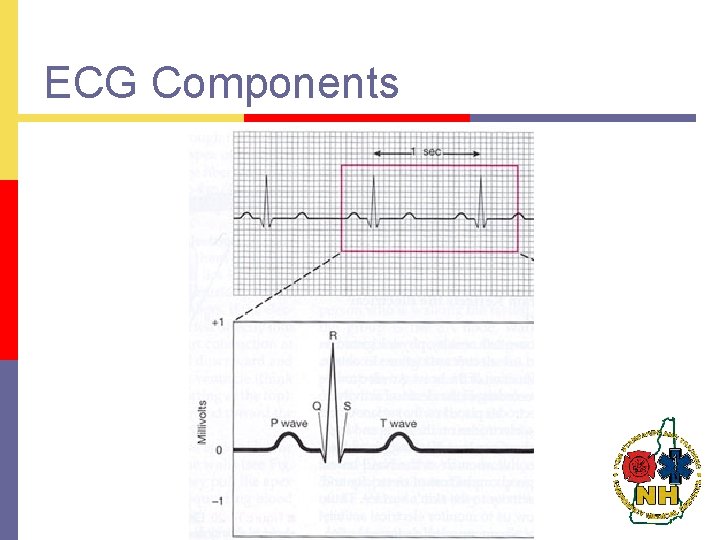
ECG Components
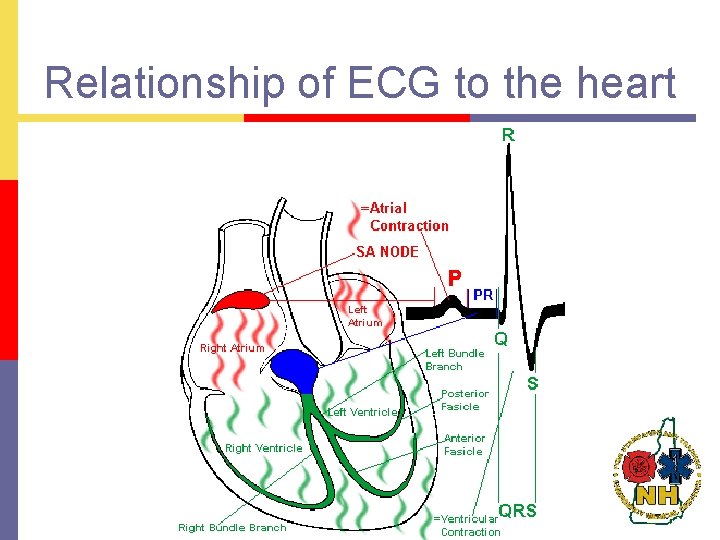
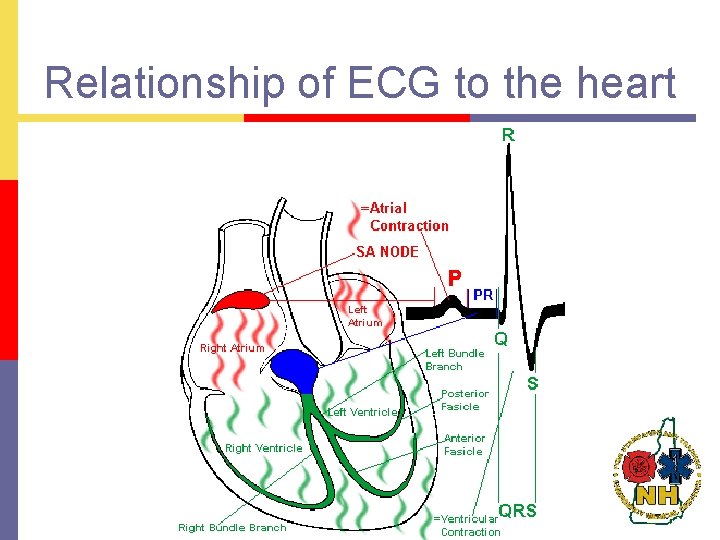
Relationship of ECG to the heart
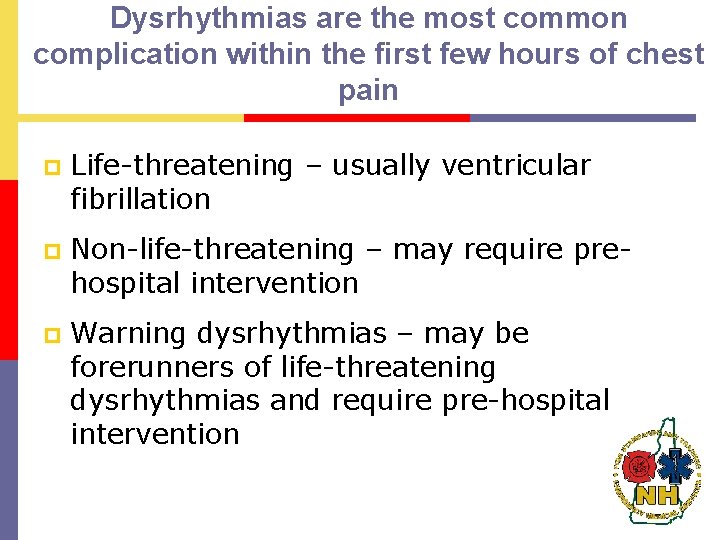
Dysrhythmias are the most common complication within the first few hours of chest pain p Life-threatening – usually ventricular fibrillation p Non-life-threatening – may require prehospital intervention p Warning dysrhythmias – may be forerunners of life-threatening dysrhythmias and require pre-hospital intervention

Basic concepts of ECG monitoring p ECG is graphic display of heart’s electrical activity p Body acts as a giant conductor of electrical current p ECG obtained by applying electrodes on body surface which detect changes in voltage of cells between sites of the electrodes
Basic concepts of ECG monitoring p Voltage may be positive (upward deflection) or negative (downward deflection) p These changes are input to ECG machine, amplified and displayed visually on a scope and/or graphically on ECG paper p Recorded as a continuous curve of waves and deflections called the electrocardiogram (ECG) Monitoring lead: any lead that shows very clear wave forms, very often, lead II p p Information that can be gained from a monitoring lead or rhythm strip: n n How fast the heart is beating How regular the heartbeat is
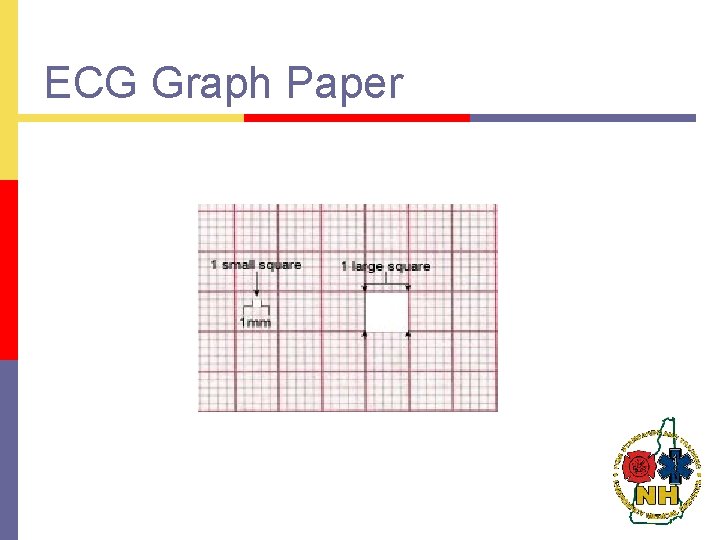
ECG Graph Paper
Artifact p Deflections on the ECG display produced by factors other than the heart’s electrical activity such as: p Standardization (calibration) marks p Muscle tremors/shivering p Patient or vehicle movement p Loose electrodes p 60 -cycle interference p Machine malfunction
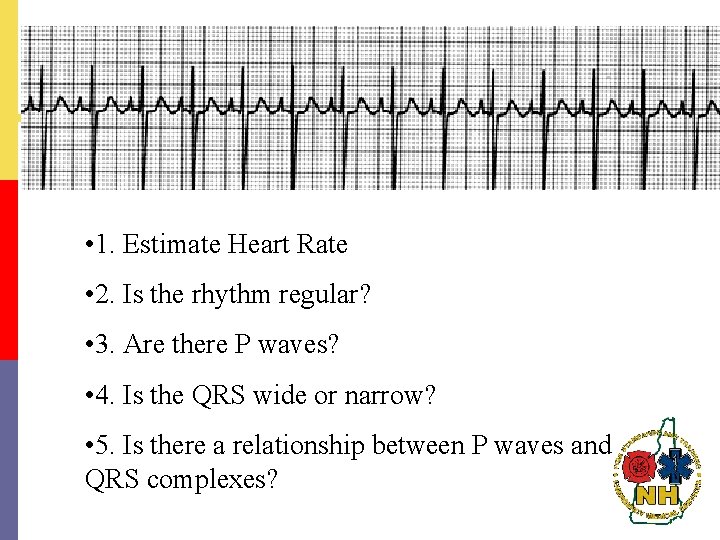
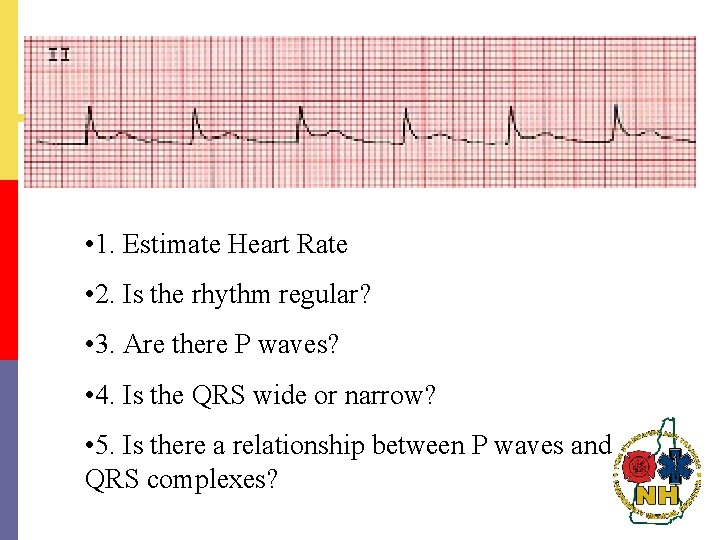
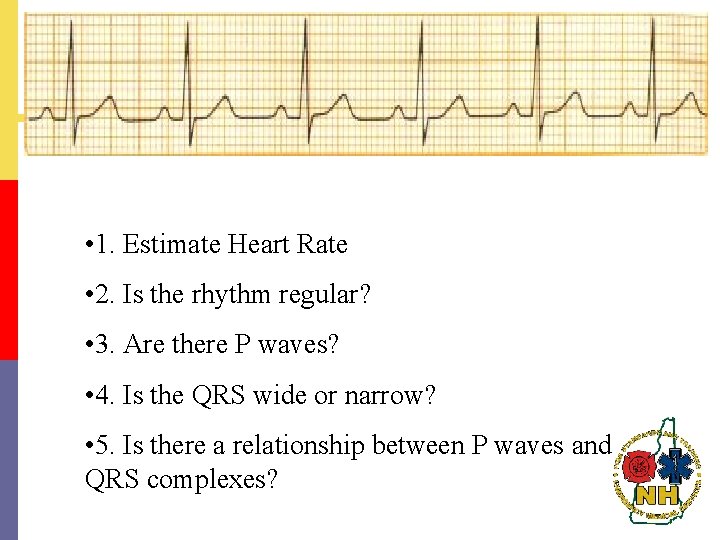
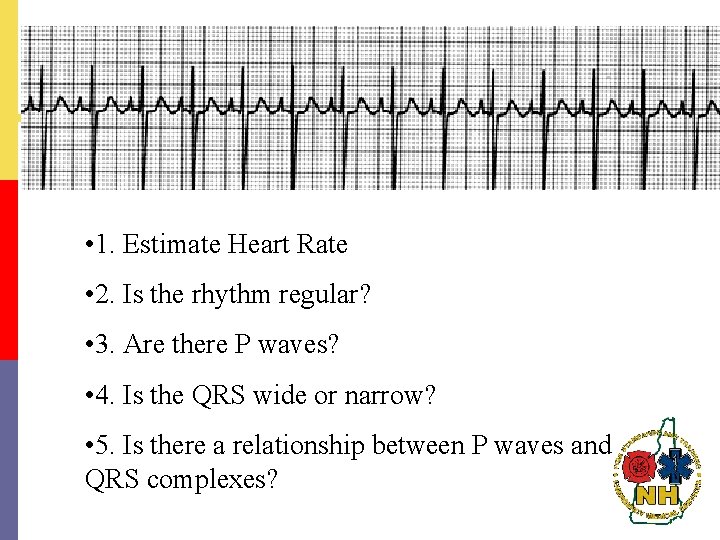
Steps to rhythm interpretation 1. Estimate Heart Rate p 2. Is the rhythm regular? p 3. Are there P waves? p 4. Is the QRS wide or narrow? p 5. Is there a relationship between P waves and QRS complexes? p
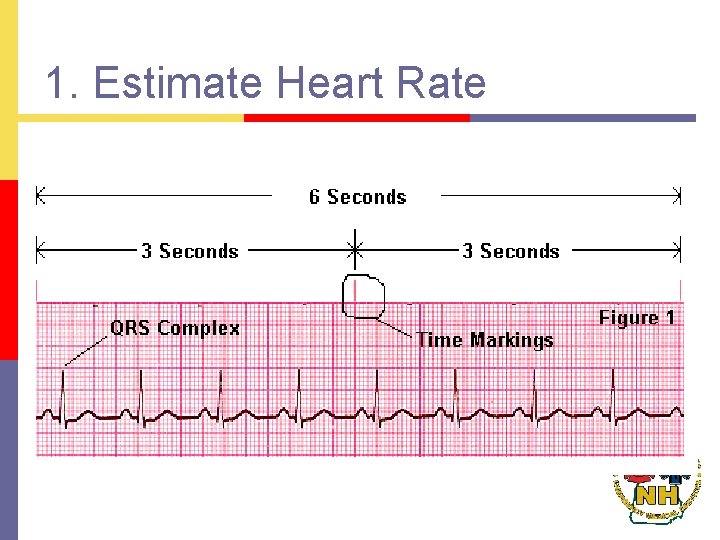
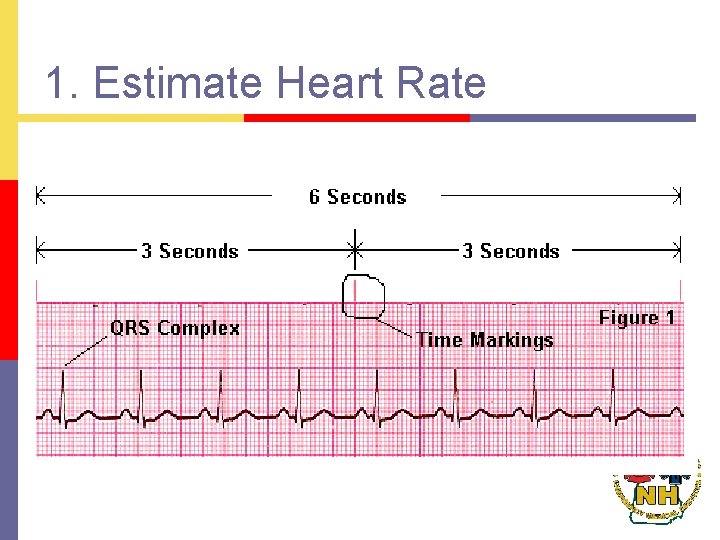
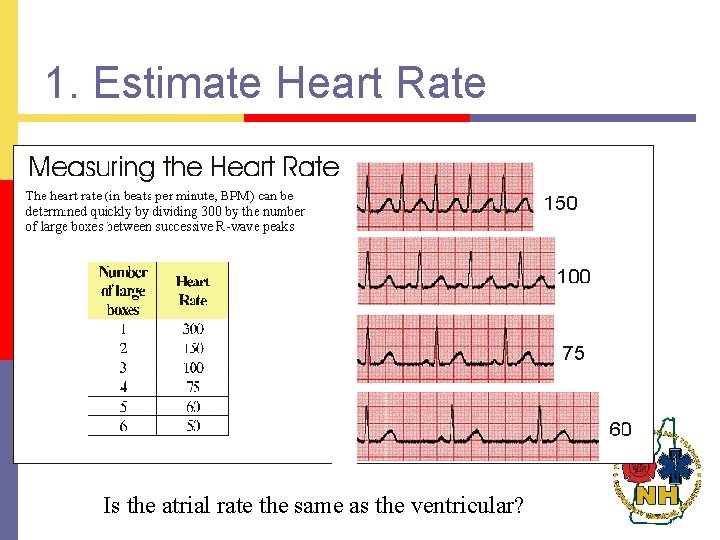
1. Estimate Heart Rate
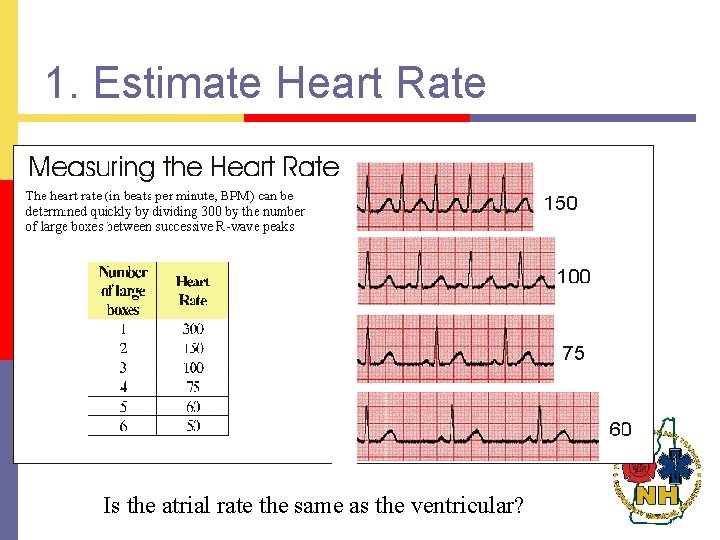
1. Estimate Heart Rate Is the atrial rate the same as the ventricular?
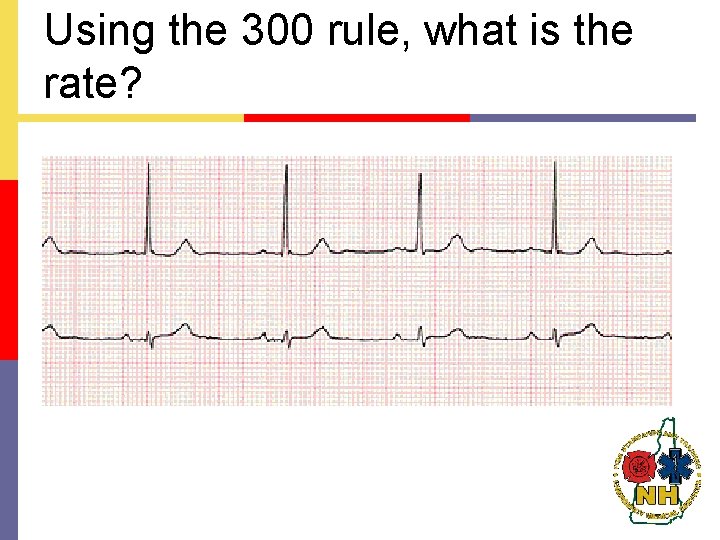
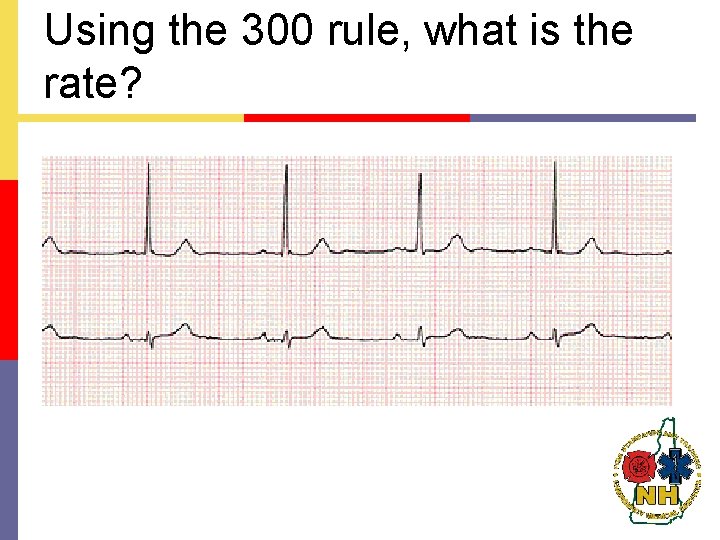
Using the 300 rule, what is the rate?
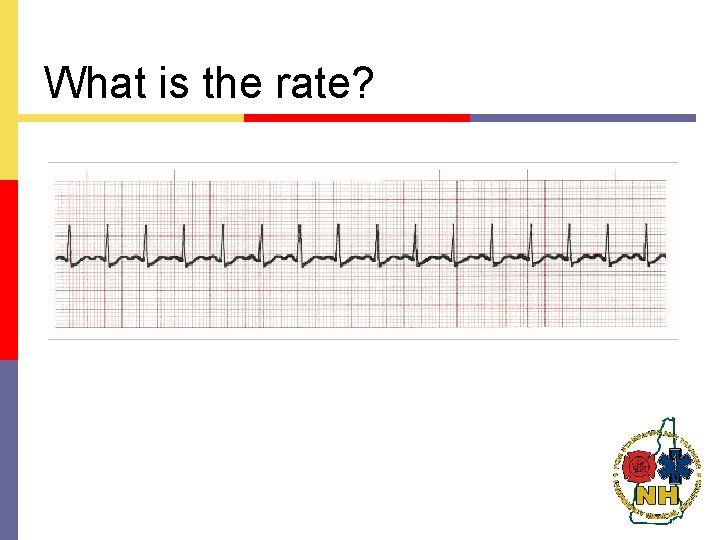
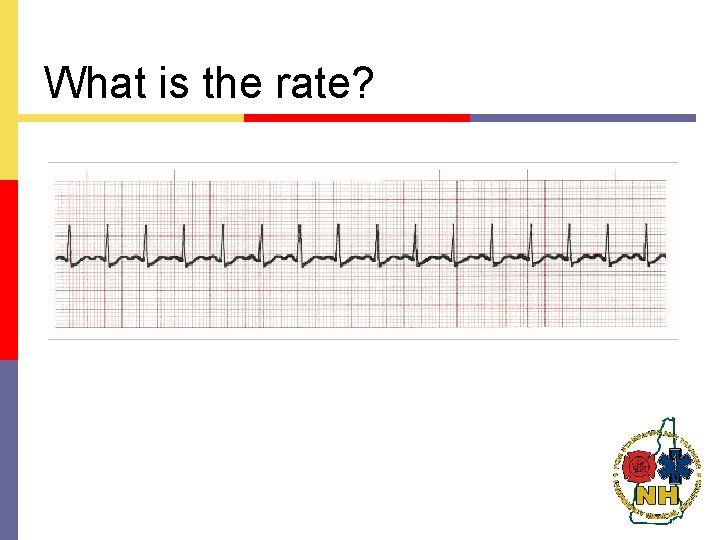
What is the rate?
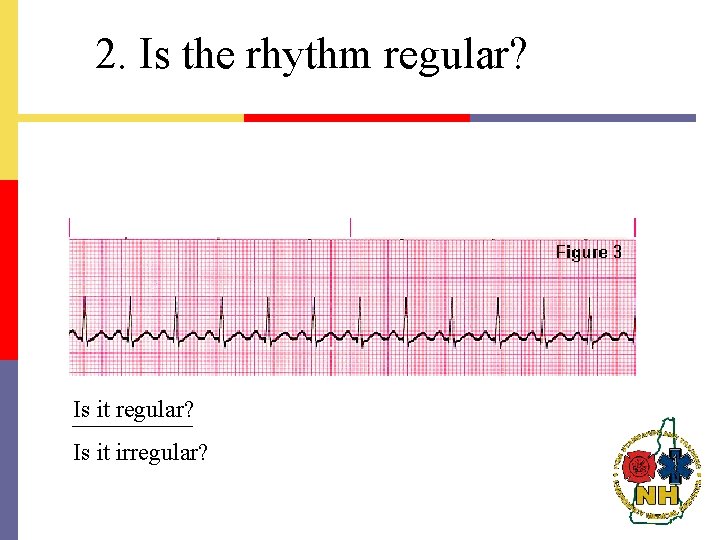
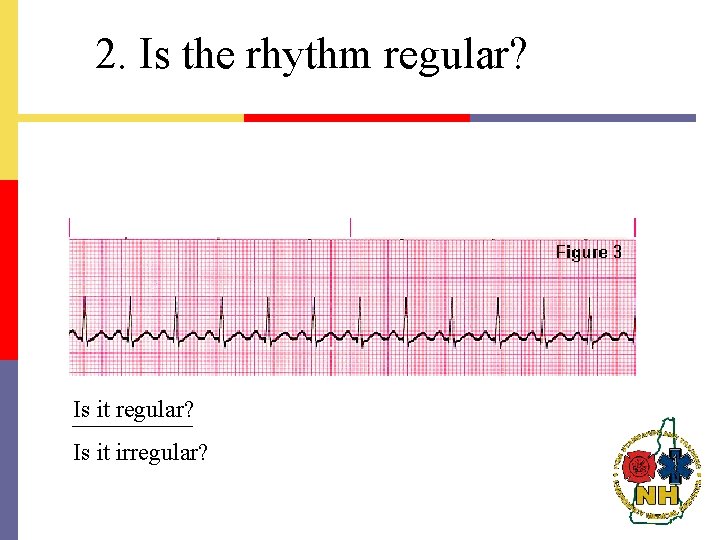
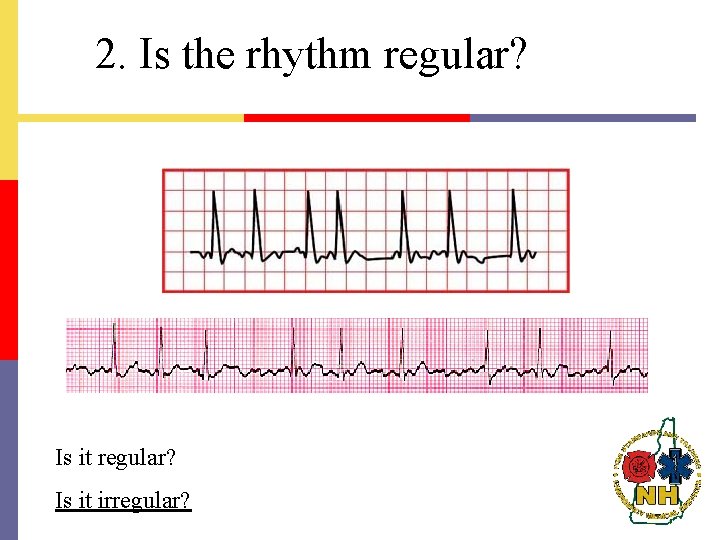
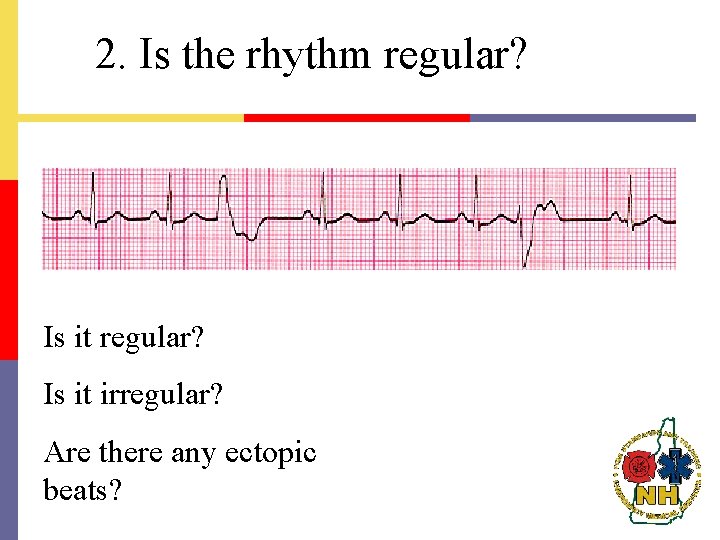
2. Is the rhythm regular? Is it regular? Is it irregular?
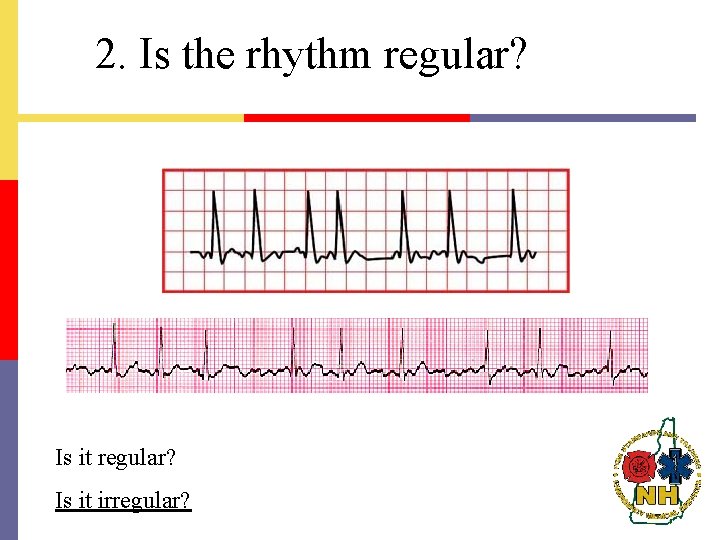
2. Is the rhythm regular? Is it regular? Is it irregular?
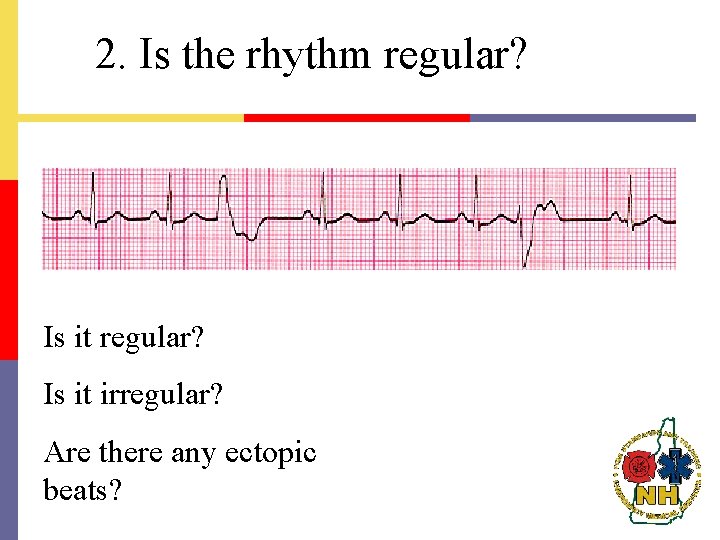
2. Is the rhythm regular? Is it regular? Is it irregular? Are there any ectopic beats?
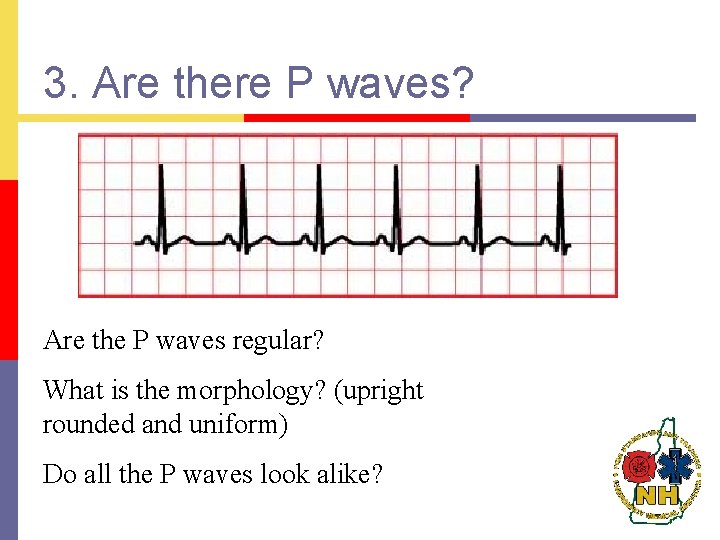
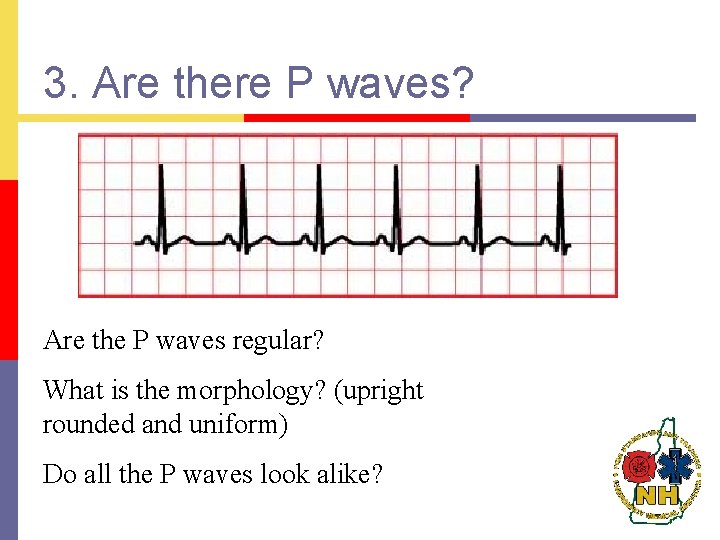
3. Are there P waves? Are the P waves regular? What is the morphology? (upright rounded and uniform) Do all the P waves look alike?
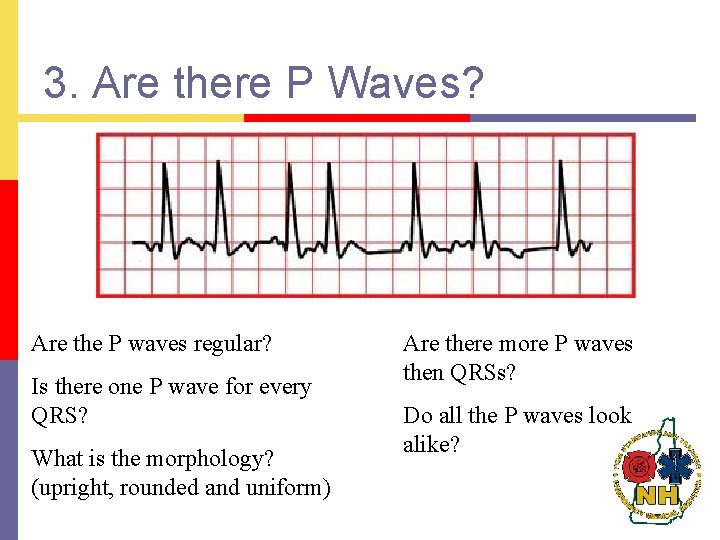
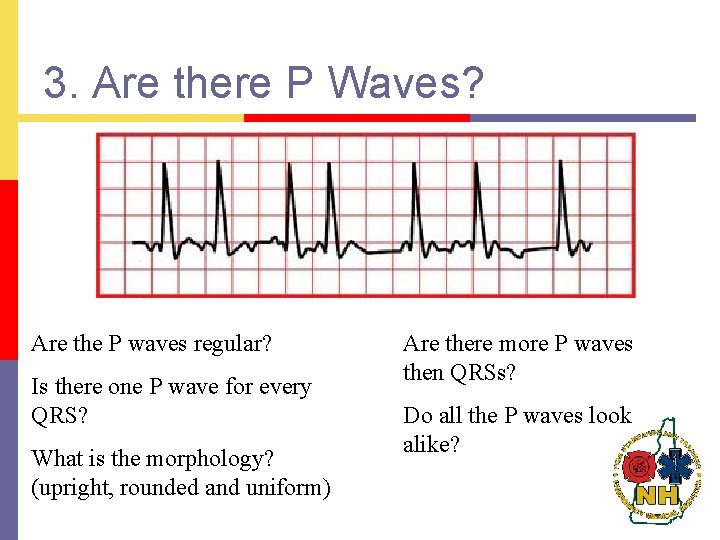
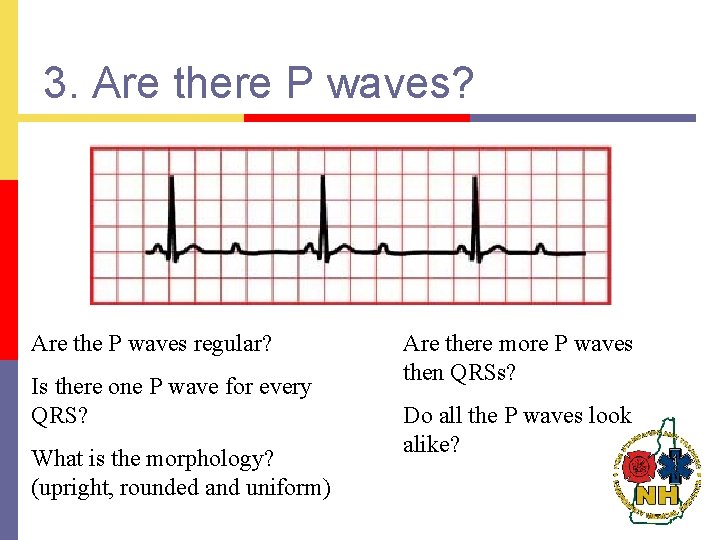
3. Are there P Waves? Are the P waves regular? Is there one P wave for every QRS? What is the morphology? (upright, rounded and uniform) Are there more P waves then QRSs? Do all the P waves look alike?

3. Are there P Waves? Are the P waves regular? Is there one P wave for every QRS? What is the morphology? (upright, rounded and uniform) Are there more P waves then QRSs? Do all the P waves look alike?
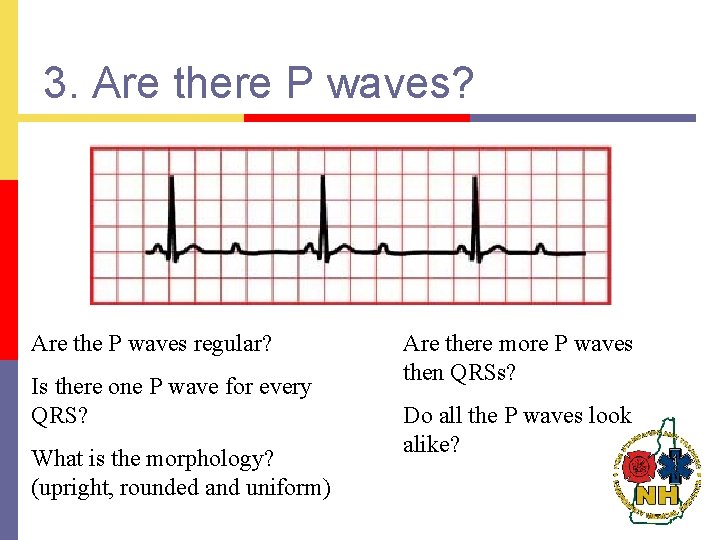
3. Are there P waves? Are the P waves regular? Is there one P wave for every QRS? What is the morphology? (upright, rounded and uniform) Are there more P waves then QRSs? Do all the P waves look alike?
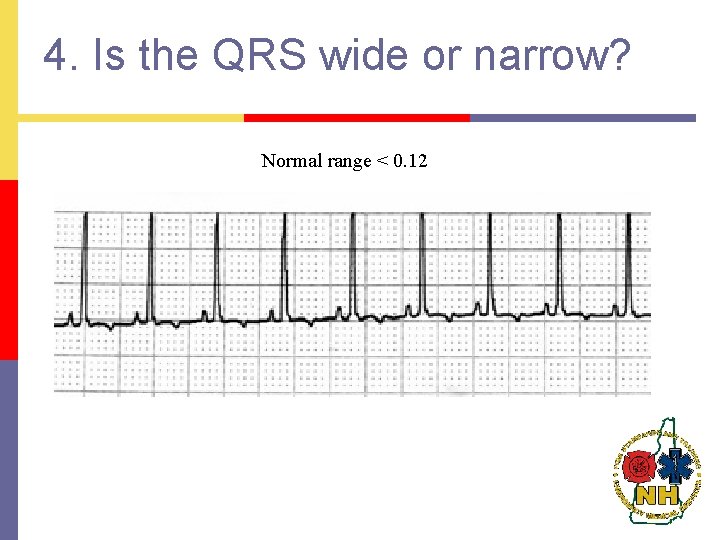
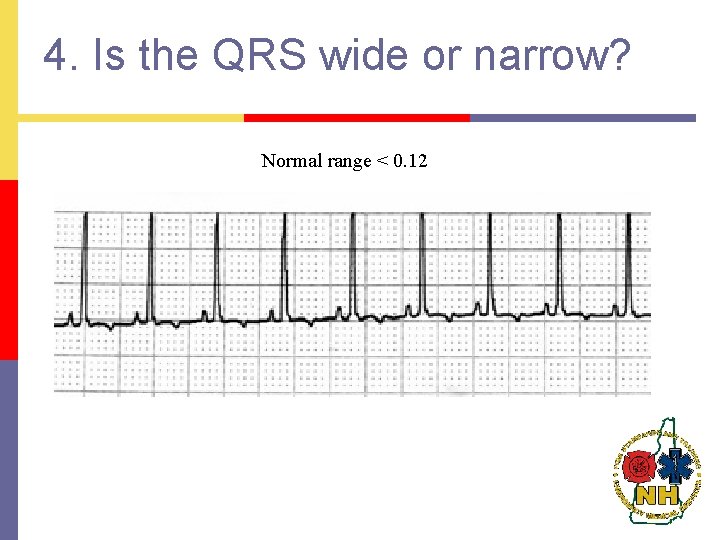
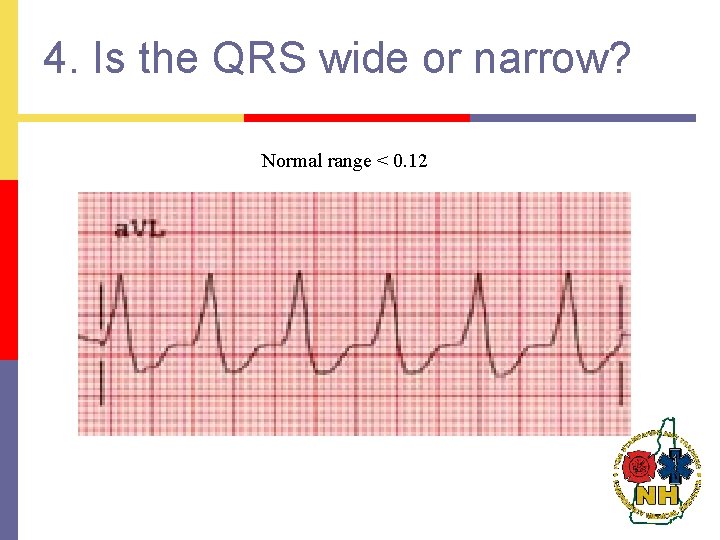
4. Is the QRS wide or narrow? Normal range < 0. 12
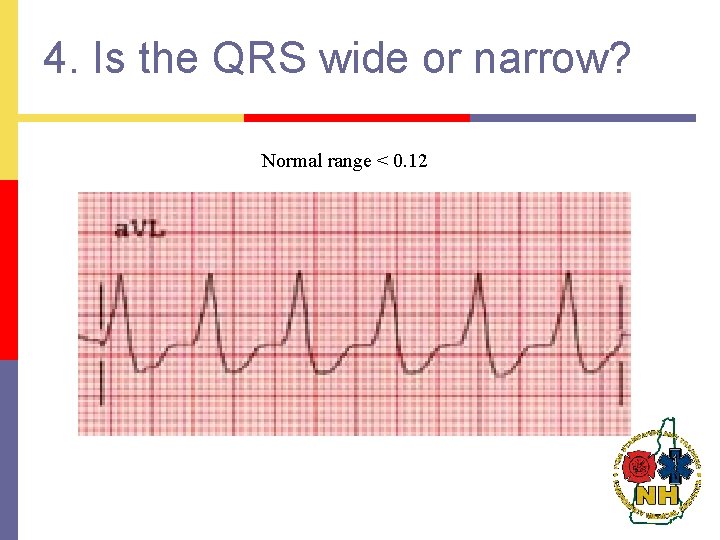
4. Is the QRS wide or narrow? Normal range < 0. 12
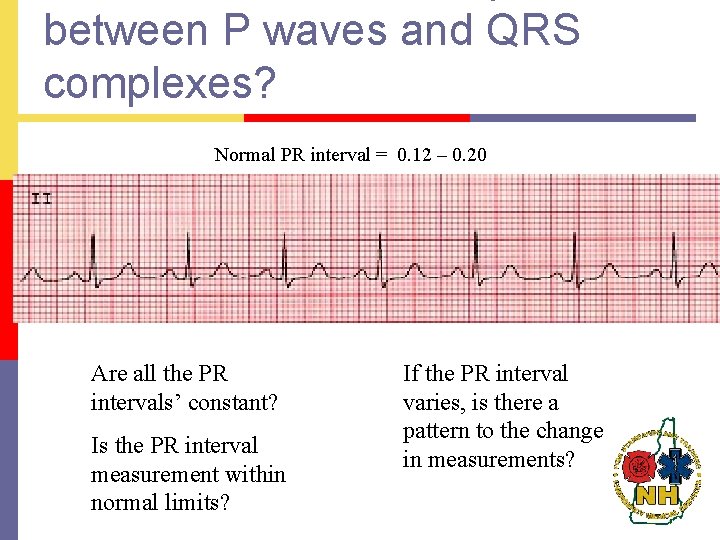
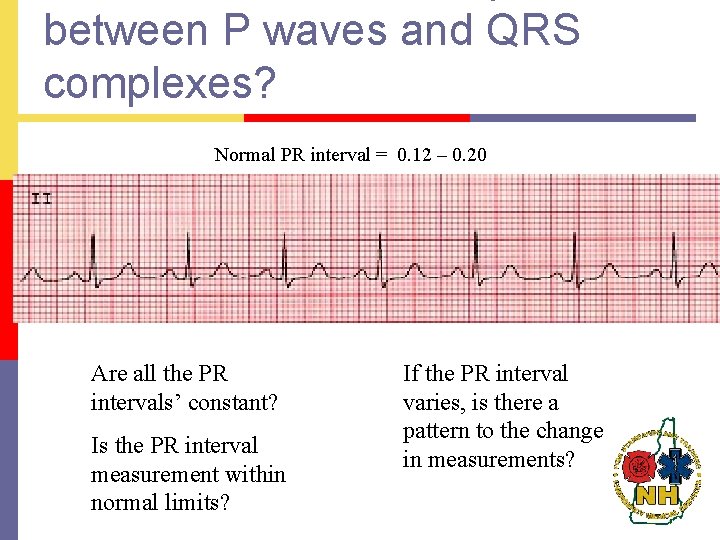
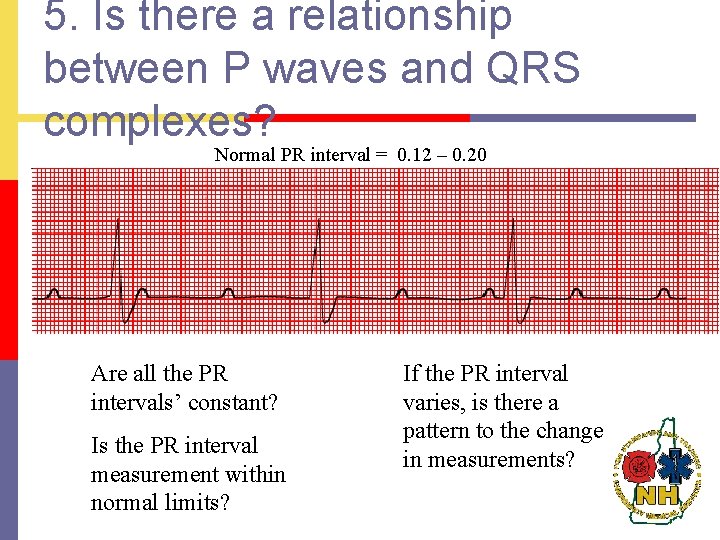
between P waves and QRS complexes? Normal PR interval = 0. 12 – 0. 20 Are all the PR intervals’ constant? Is the PR interval measurement within normal limits? If the PR interval varies, is there a pattern to the change in measurements?
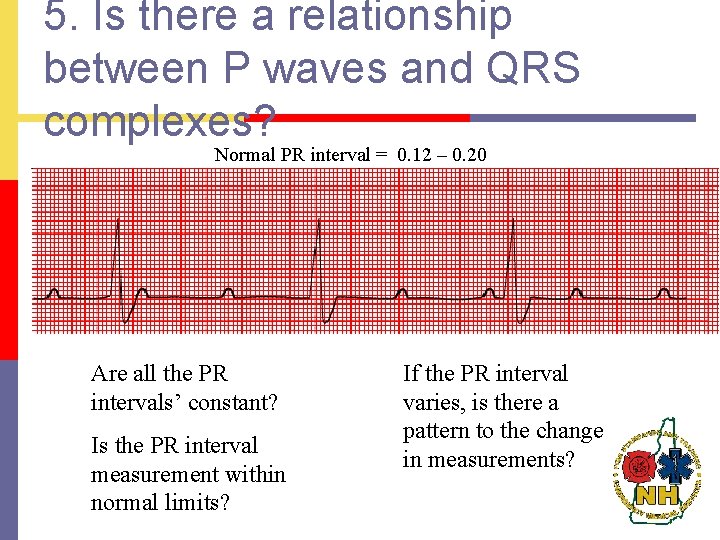
5. Is there a relationship between P waves and QRS complexes? Normal PR interval = 0. 12 – 0. 20 Are all the PR intervals’ constant? Is the PR interval measurement within normal limits? If the PR interval varies, is there a pattern to the change in measurements?
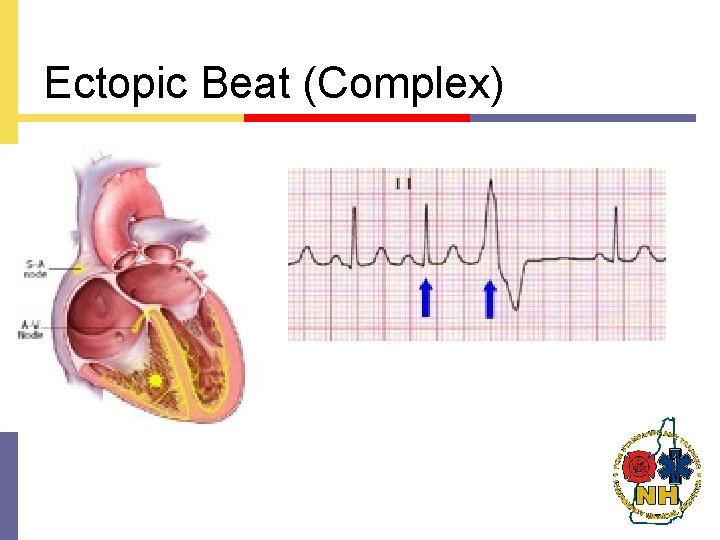
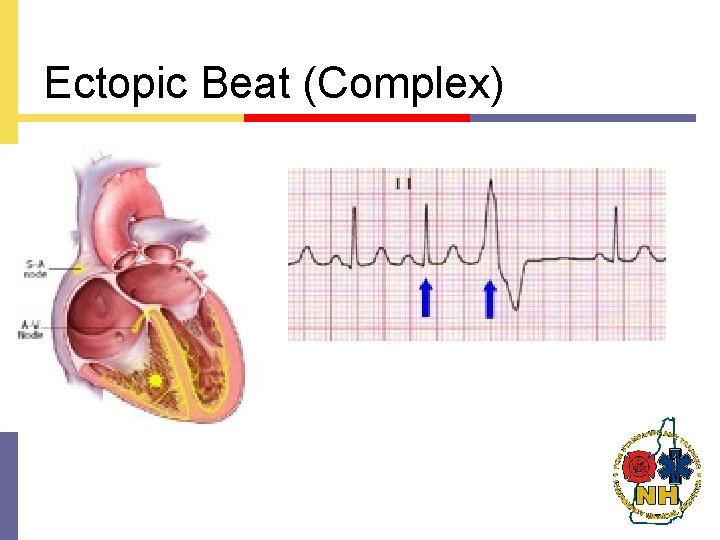
Ectopic Beat (Complex)

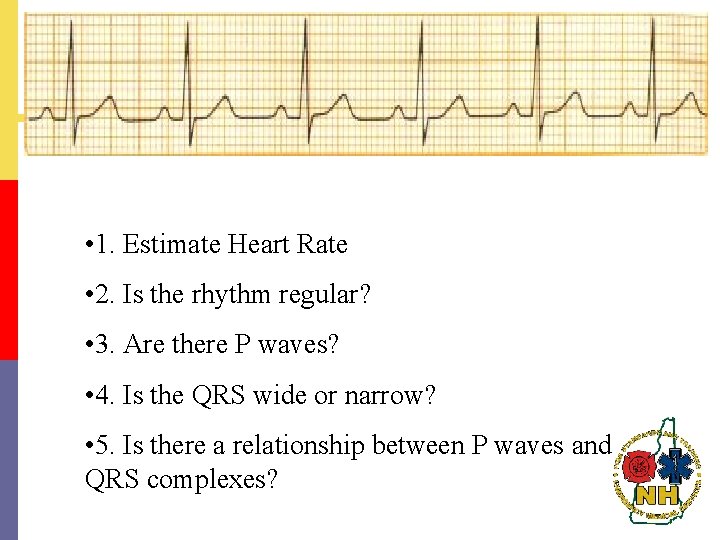
• 1. Estimate Heart Rate • 2. Is the rhythm regular? • 3. Are there P waves? • 4. Is the QRS wide or narrow? • 5. Is there a relationship between P waves and QRS complexes?
• 1. Estimate Heart Rate • 2. Is the rhythm regular? • 3. Are there P waves? • 4. Is the QRS wide or narrow? • 5. Is there a relationship between P waves and QRS complexes?
• 1. Estimate Heart Rate • 2. Is the rhythm regular? • 3. Are there P waves? • 4. Is the QRS wide or narrow? • 5. Is there a relationship between P waves and QRS complexes?
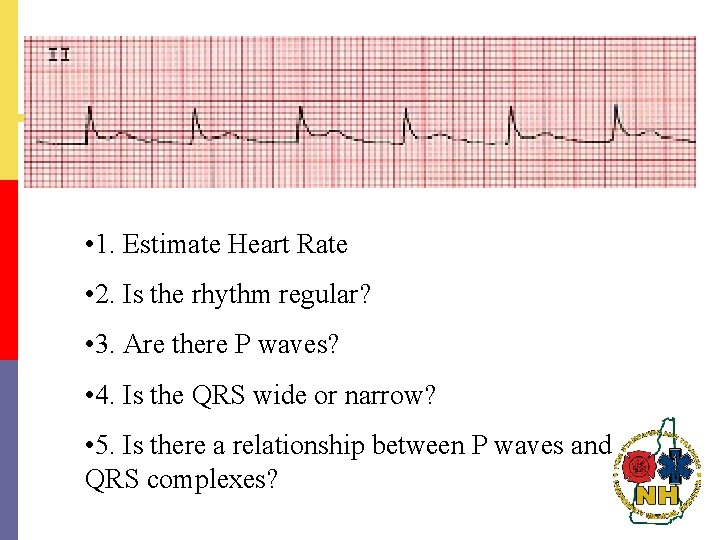
• 1. Estimate Heart Rate • 2. Is the rhythm regular? • 3. Are there P waves? • 4. Is the QRS wide or narrow? • 5. Is there a relationship between P waves and QRS complexes?
Rhythms of the SA Node p Sinus Rhythm p Sinus Bradycardia p Sinus Tachycardia p Sinus Arrhythmia
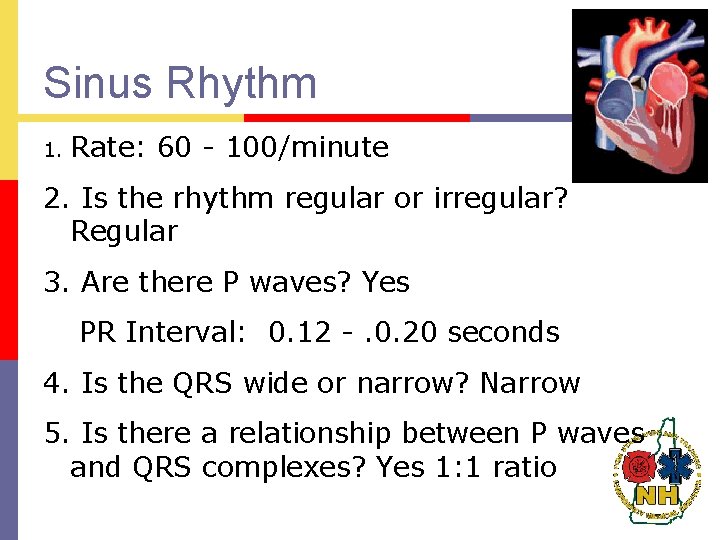
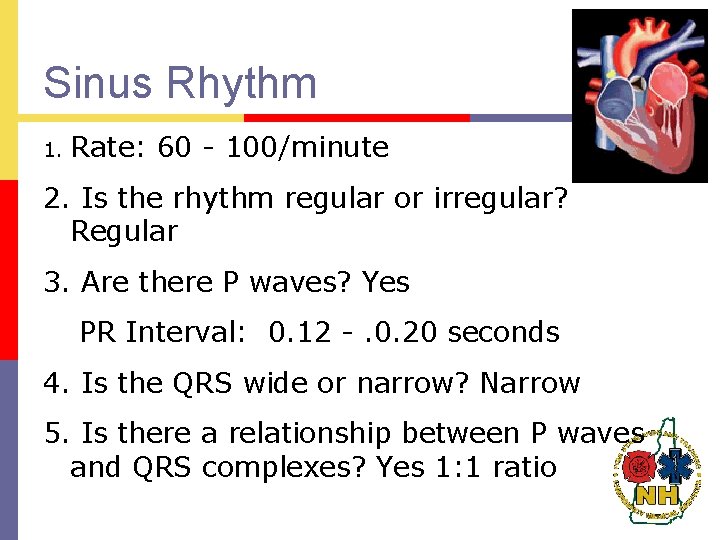
Sinus Rhythm 1. Rate: 60 - 100/minute 2. Is the rhythm regular or irregular? Regular 3. Are there P waves? Yes PR Interval: 0. 12 -. 0. 20 seconds 4. Is the QRS wide or narrow? Narrow 5. Is there a relationship between P waves and QRS complexes? Yes 1: 1 ratio

Normal Sinus Rhythm

Sinus Bradycardia 1. Rate: < 60/minute 2. Is the rhythm regular or irregular? Regular 3. Are there P waves? Yes PR Interval: normal to slightly prolonged 4. Is the QRS wide or narrow? Narrow 5. Is there a relationship between P waves and QRS complexes? Yes 1: 1 ratio
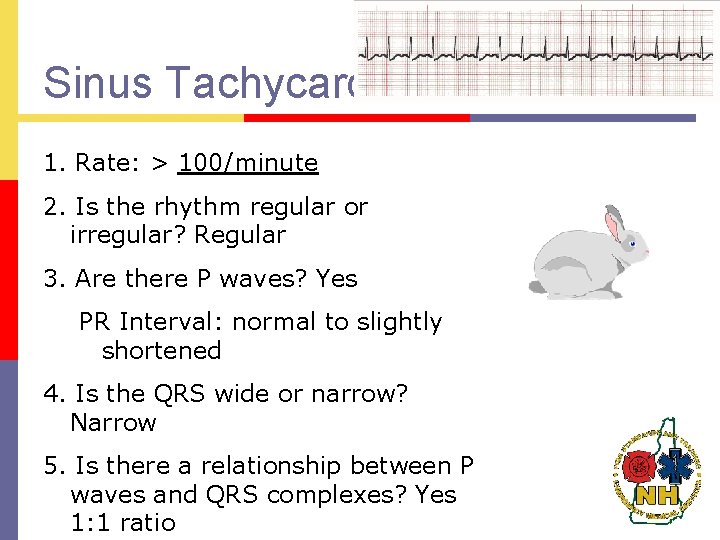
Sinus Tachycardia 1. Rate: > 100/minute 2. Is the rhythm regular or irregular? Regular 3. Are there P waves? Yes PR Interval: normal to slightly shortened 4. Is the QRS wide or narrow? Narrow 5. Is there a relationship between P waves and QRS complexes? Yes 1: 1 ratio

Sinus Arrhythmia 1. Rate: 60 - 100/minute 2. Is the rhythm regular or irregular? Irregular 3. Are there P waves? Yes PR Interval: Normal 4. Is the QRS wide or narrow? Narrow 5. Is there a relationship between P waves and QRS complexes? Yes 1: 1

Ventricular Rhythms p Idioventricular rhythm p Accelerated idioventricular rhythm p Premature ventricular complex (ventricular ectopic) p Ventricular tachycardia p Ventricular Fibrillation

Idioventricular Rhythm 1. Rate: 20 - 40/minute 2. Is the rhythm regular or irregular? regular 3. Are there P waves? No PR Interval: None 4. Is the QRS wide or narrow? Wide 5. Is there a relationship between P waves and QRS complexes? No P Waves
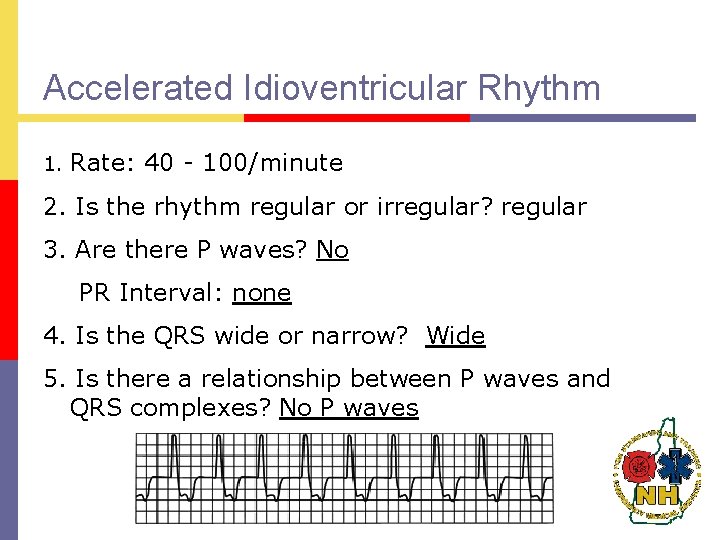
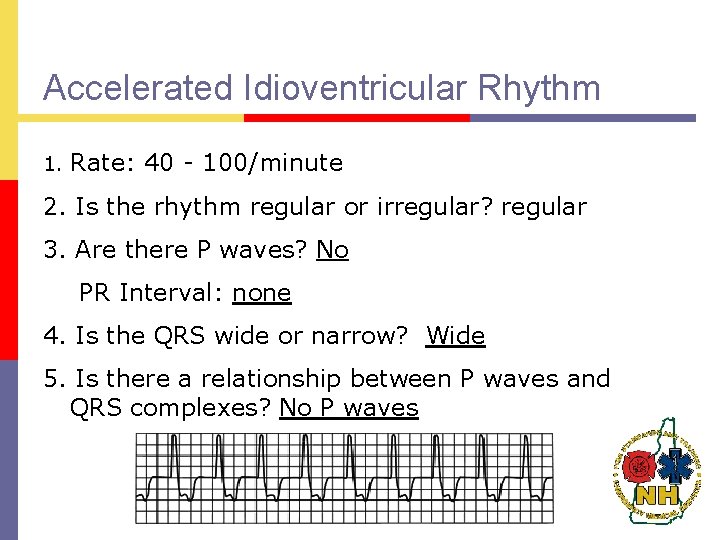
Accelerated Idioventricular Rhythm 1. Rate: 40 - 100/minute 2. Is the rhythm regular or irregular? regular 3. Are there P waves? No PR Interval: none 4. Is the QRS wide or narrow? Wide 5. Is there a relationship between P waves and QRS complexes? No P waves
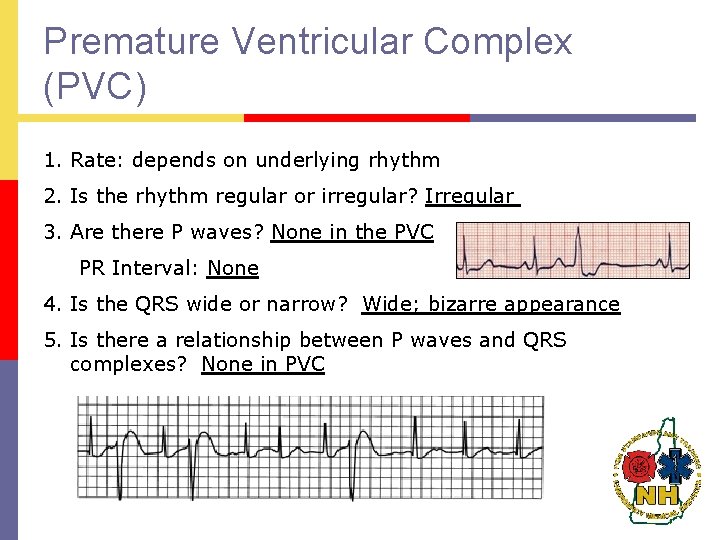
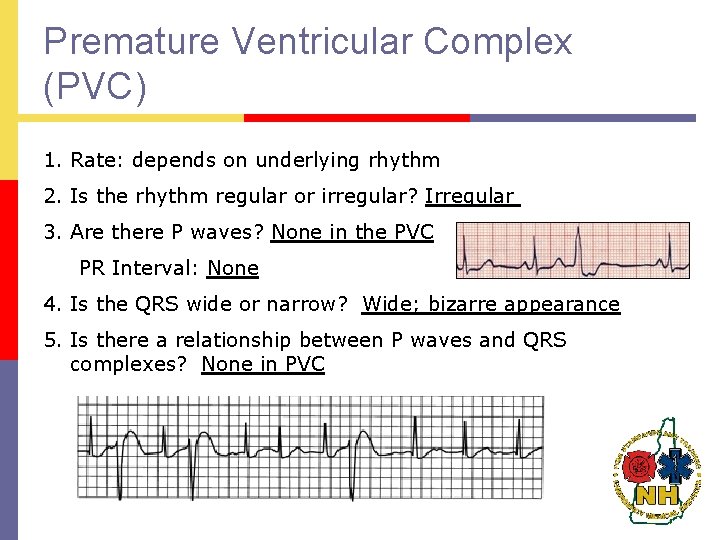
Premature Ventricular Complex (PVC) 1. Rate: depends on underlying rhythm 2. Is the rhythm regular or irregular? Irregular 3. Are there P waves? None in the PVC PR Interval: None 4. Is the QRS wide or narrow? Wide; bizarre appearance 5. Is there a relationship between P waves and QRS complexes? None in PVC
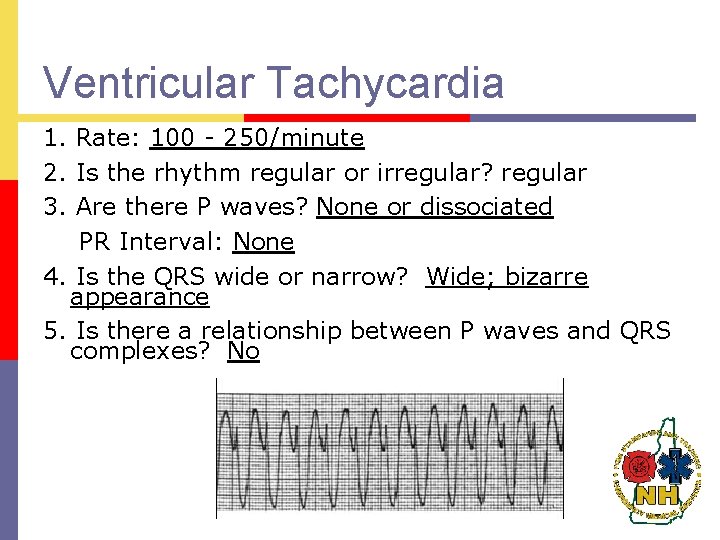
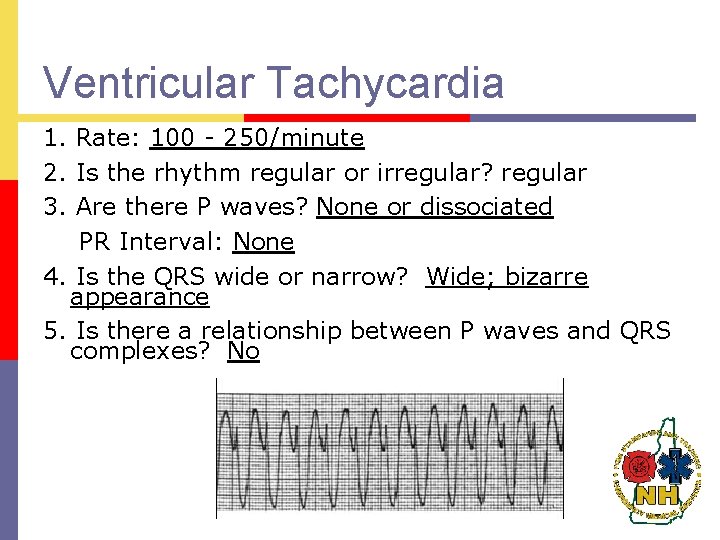
Ventricular Tachycardia 1. Rate: 100 - 250/minute 2. Is the rhythm regular or irregular? regular 3. Are there P waves? None or dissociated PR Interval: None 4. Is the QRS wide or narrow? Wide; bizarre appearance 5. Is there a relationship between P waves and QRS complexes? No

Ventricular Tachycardia

Ventricular Tachycardia
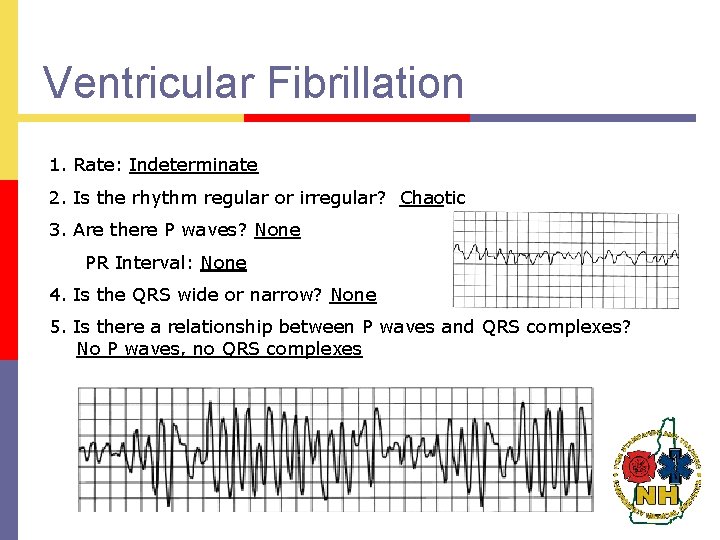
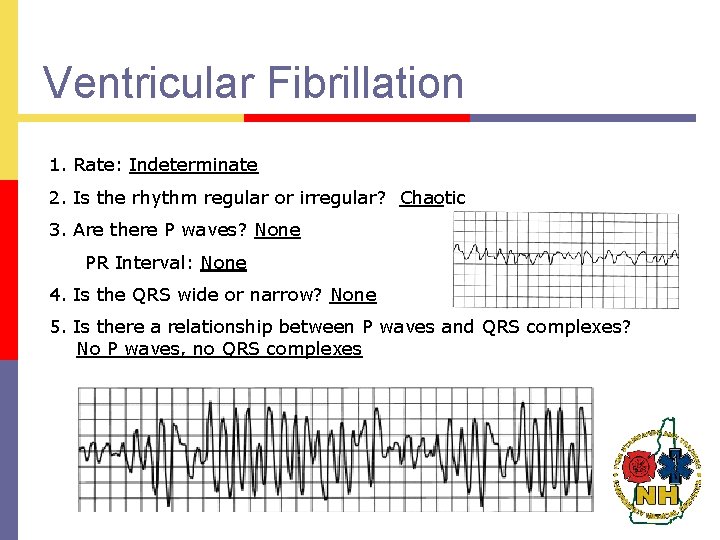
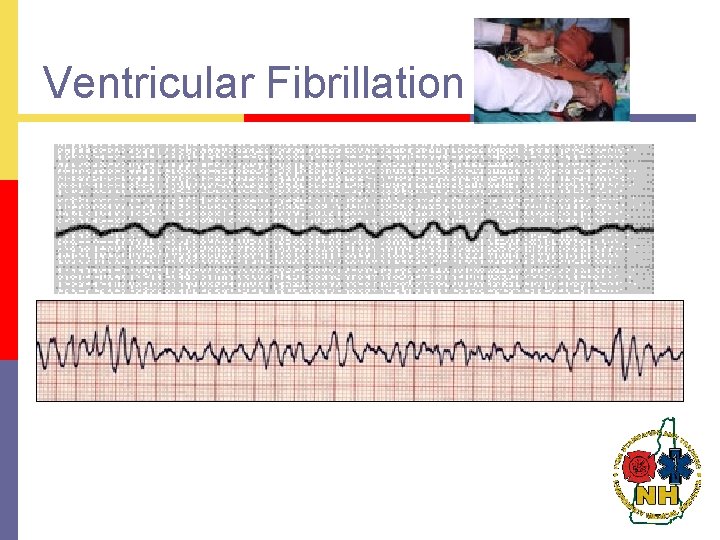
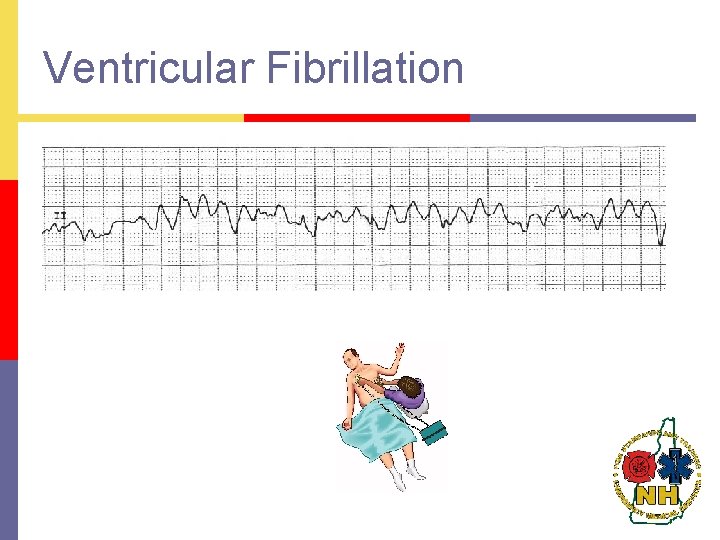
Ventricular Fibrillation 1. Rate: Indeterminate 2. Is the rhythm regular or irregular? Chaotic 3. Are there P waves? None PR Interval: None 4. Is the QRS wide or narrow? None 5. Is there a relationship between P waves and QRS complexes? No P waves, no QRS complexes
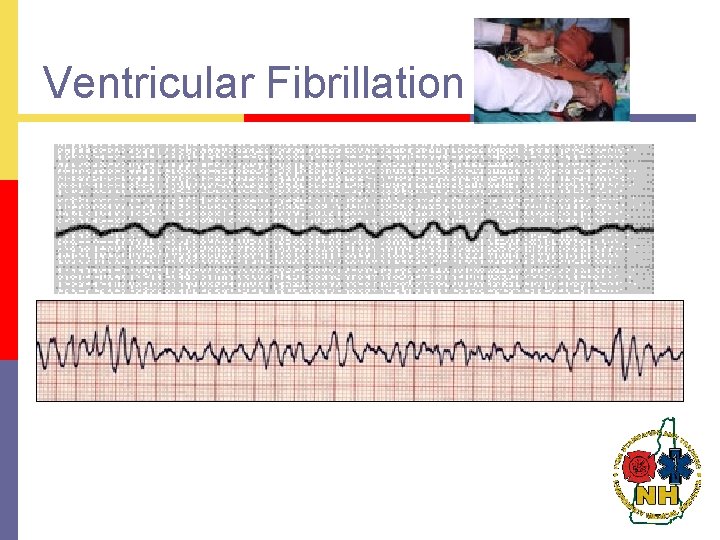
Ventricular Fibrillation
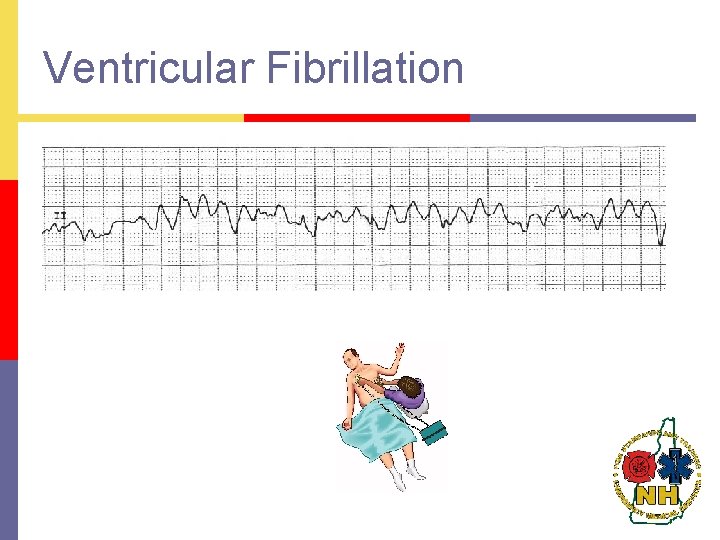
Ventricular Fibrillation

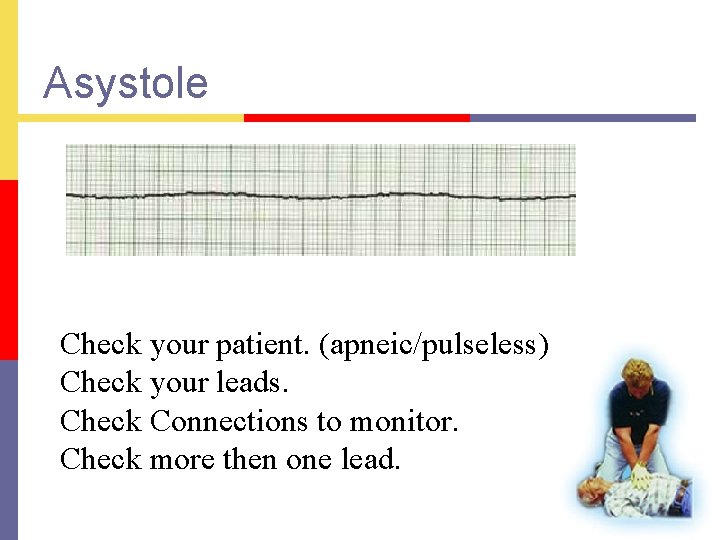
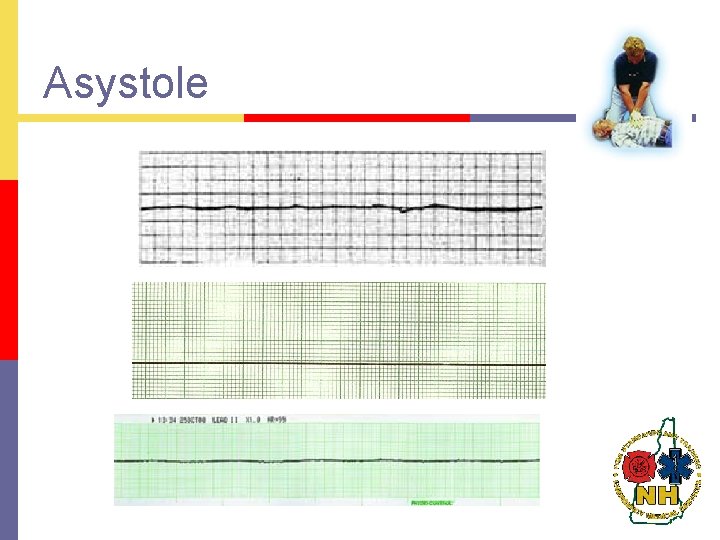
Asystole 1 . Rate: Indeterminate 2. Is the rhythm regular or irregular? No rhythm 3. Are there P waves? None PR Interval: None 4. Is the QRS wide or narrow? None 5. Is there a relationship between P waves and QRS complexes? No P waves, no QRS complexes
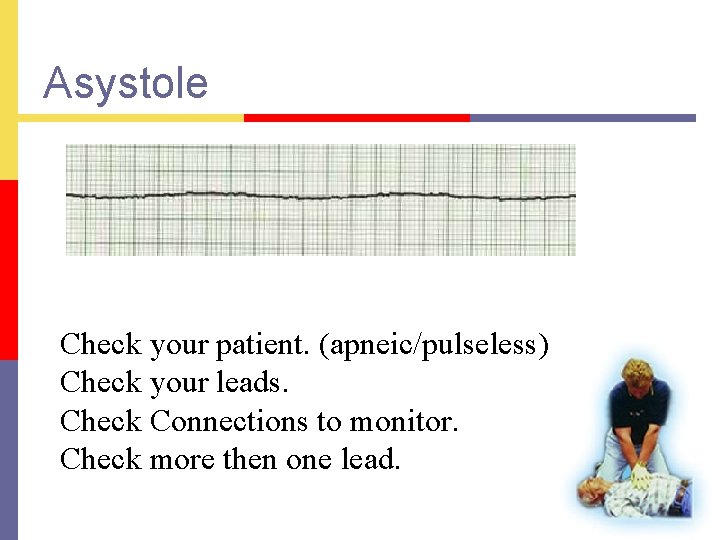
Asystole Check your patient. (apneic/pulseless) Check your leads. Check Connections to monitor. Check more then one lead.
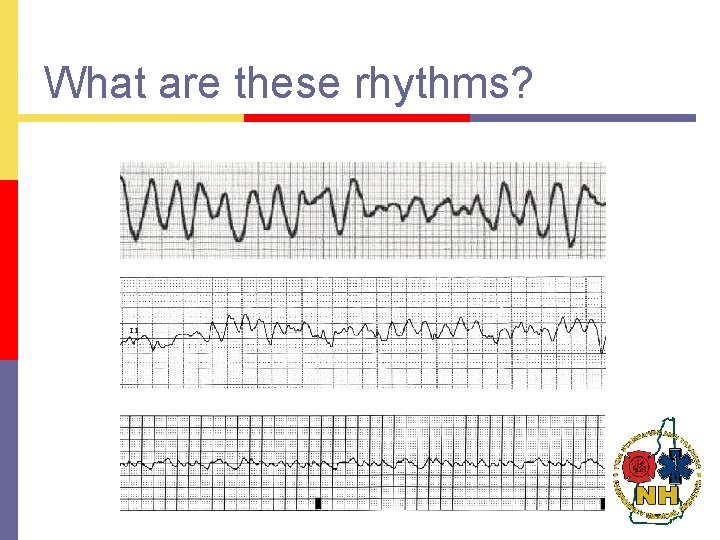
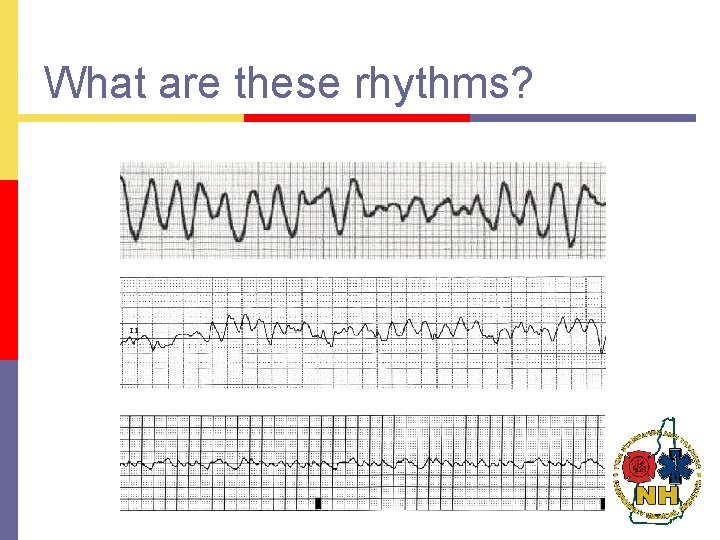
What are these rhythms?
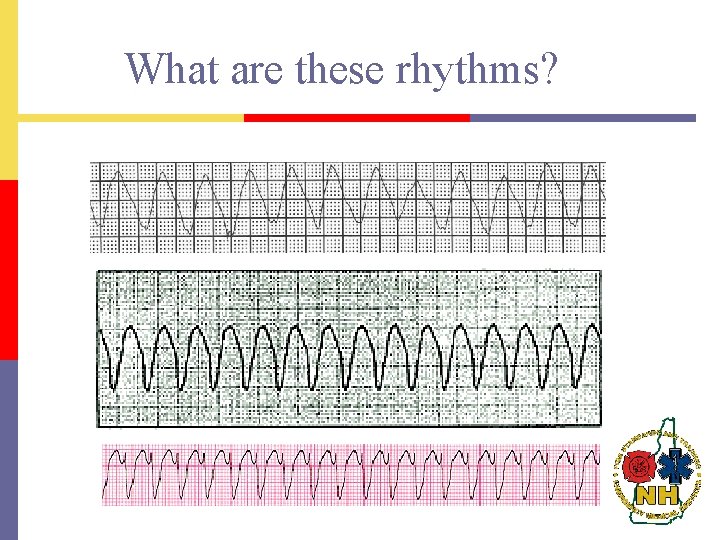
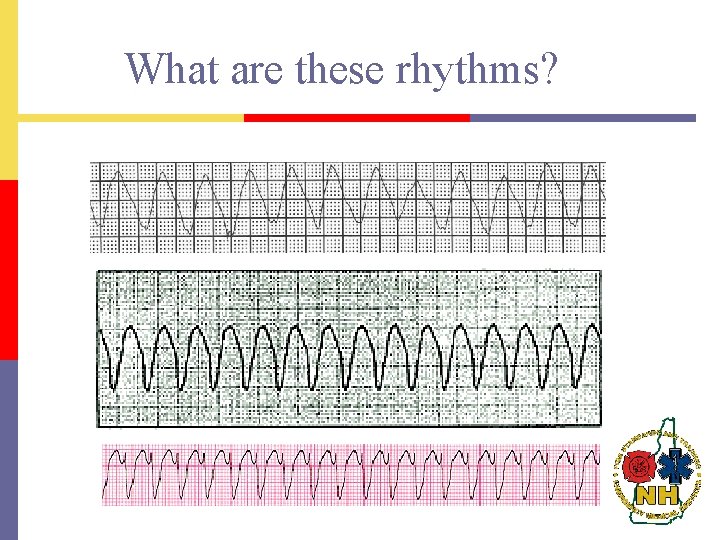
What are these rhythms?
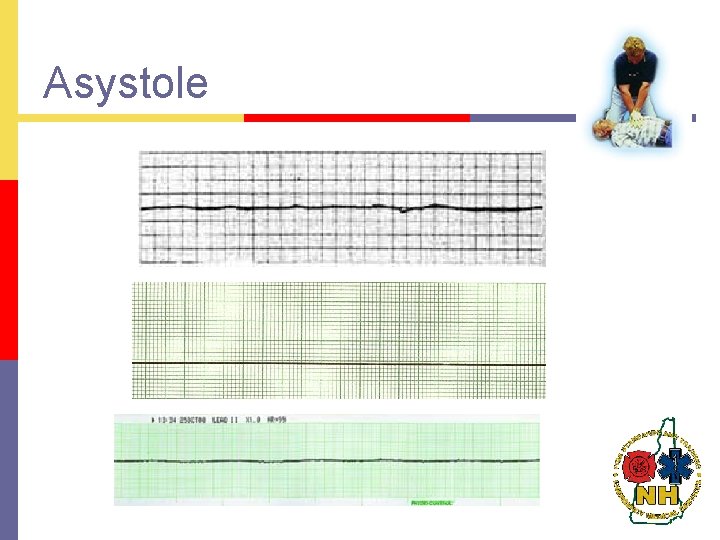
Asystole

P. E. A. Pulseless Electrical Activity p There is electrical activity on the monitor, but there is no pulse p
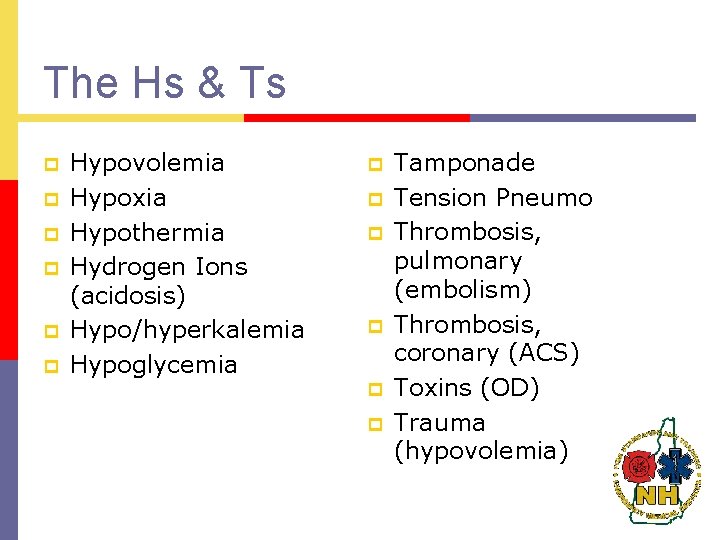
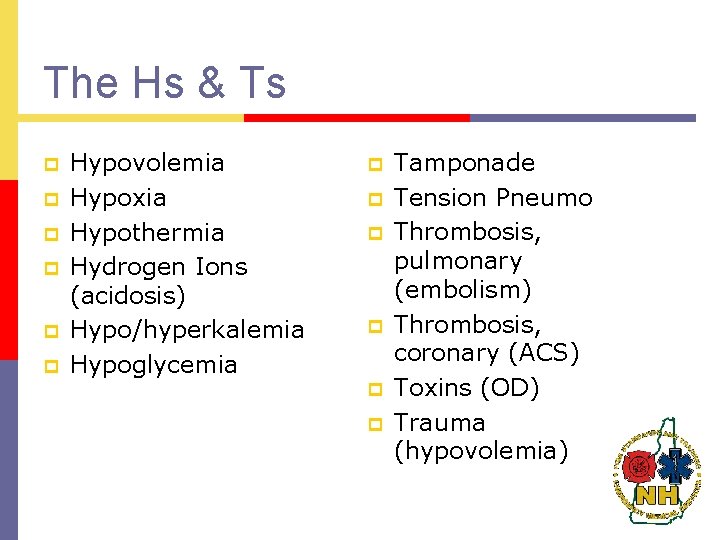
The Hs & Ts p p p Hypovolemia Hypoxia Hypothermia Hydrogen Ions (acidosis) Hypo/hyperkalemia Hypoglycemia p p p Tamponade Tension Pneumo Thrombosis, pulmonary (embolism) Thrombosis, coronary (ACS) Toxins (OD) Trauma (hypovolemia)
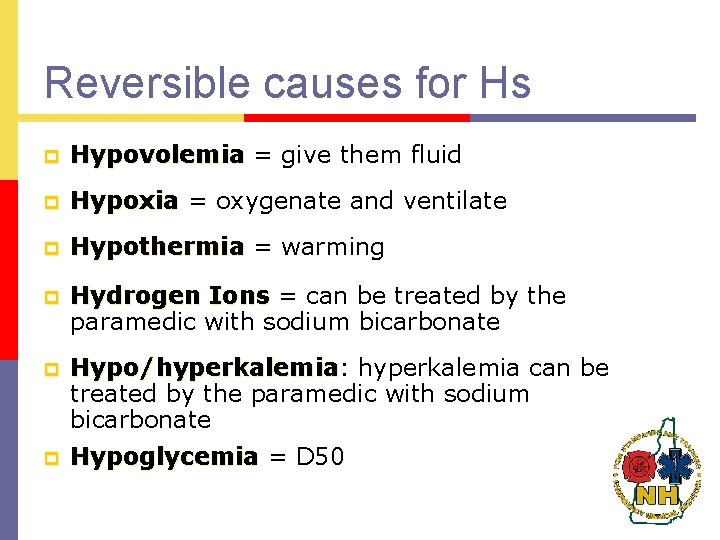
Reversible causes for Hs p Hypovolemia = give them fluid p Hypoxia = oxygenate and ventilate p Hypothermia = warming p Hydrogen Ions = can be treated by the paramedic with sodium bicarbonate p Hypo/hyperkalemia: Hypo/hyperkalemia can be treated by the paramedic with sodium bicarbonate p Hypoglycemia = D 50
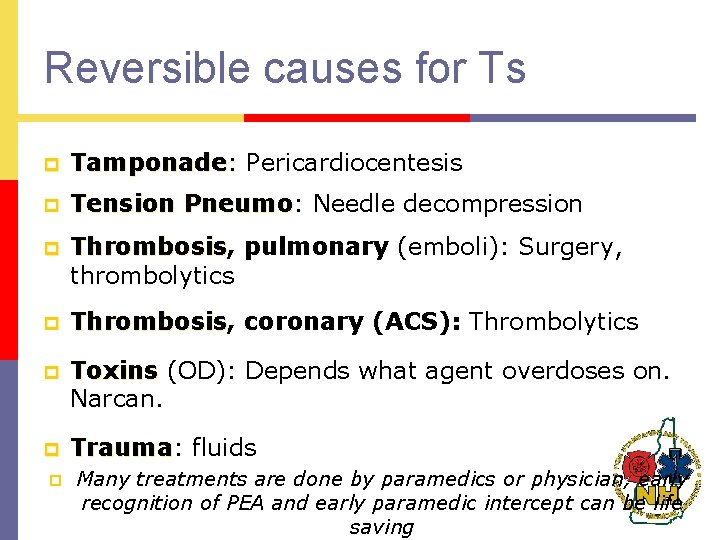
Reversible causes for Ts p Tamponade: Pericardiocentesis p Tension Pneumo: Pneumo Needle decompression p Thrombosis, Thrombosis pulmonary (emboli): Surgery, thrombolytics p Thrombosis, Thrombosis coronary (ACS): Thrombolytics p Toxins (OD): Depends what agent overdoses on. Narcan. p Trauma: Trauma fluids p Many treatments are done by paramedics or physician, early recognition of PEA and early paramedic intercept can be life saving
QUESTIONS?
Special Thank You to: p Christopher Rousseau, NREMT-I
 Strengths of the articles of confederation
Strengths of the articles of confederation Neil thisse is a loyalist answers
Neil thisse is a loyalist answers Westcliffe cardiology shipley
Westcliffe cardiology shipley Clinical documentation improvement for cardiology
Clinical documentation improvement for cardiology Cardiology procedures chapter 47
Cardiology procedures chapter 47 Accp cardiology prn
Accp cardiology prn Acc sports cardiology
Acc sports cardiology Service line management
Service line management Egsys
Egsys Muse cardiology
Muse cardiology Elias hanna cardiology
Elias hanna cardiology Craig ainsworth cardiology
Craig ainsworth cardiology Hall-garcia cardiology associates
Hall-garcia cardiology associates Enloe cardiology
Enloe cardiology Inculprate
Inculprate Cardiology structured reporting
Cardiology structured reporting Accp cardiology prn journal club
Accp cardiology prn journal club New hampshire scholars
New hampshire scholars Facsimiles ltd nashua new hampshire
Facsimiles ltd nashua new hampshire New hampshire lobbying
New hampshire lobbying New hampshire coast
New hampshire coast New hampshire department of administrative services
New hampshire department of administrative services Pratt and whitney new hampshire
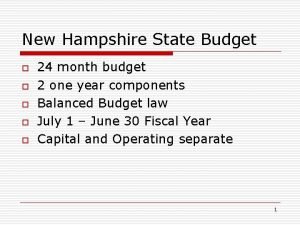
Pratt and whitney new hampshire New hampshire state budget
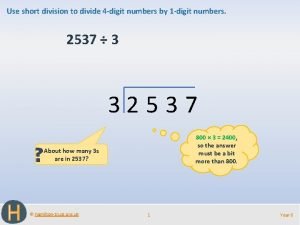
New hampshire state budget Short division vs long division
Short division vs long division Synthetic dividend
Synthetic dividend Division key vocabulary
Division key vocabulary Dividing polynomials synthetic division
Dividing polynomials synthetic division Kameroen schaap karakter
Kameroen schaap karakter Learning zone hampshire
Learning zone hampshire Services for young children hampshire
Services for young children hampshire Hampshire astronomical group
Hampshire astronomical group Hampshire safeguarding adults board
Hampshire safeguarding adults board Hampshire duroc yorkshire
Hampshire duroc yorkshire Hampshire rugby union
Hampshire rugby union Hampshire college
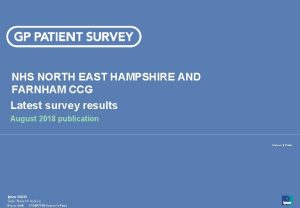
Hampshire college Nhs north east hampshire and farnham ccg
Nhs north east hampshire and farnham ccg 1817 hampshire drive
1817 hampshire drive Hampshire community bank
Hampshire community bank Emotionally based school avoidance hampshire
Emotionally based school avoidance hampshire Rick riordan hampshire book award
Rick riordan hampshire book award Ruth milton public health england
Ruth milton public health england Hampshire pension services member portal
Hampshire pension services member portal Hampshire health record
Hampshire health record Hampshire characteristics
Hampshire characteristics Department of criminal justice services ny
Department of criminal justice services ny Dvrs nj
Dvrs nj Split direct speech worksheet
Split direct speech worksheet New york pennsylvania new jersey delaware
New york pennsylvania new jersey delaware New oil and new wineskin
New oil and new wineskin Marquee theater new hartford ny
Marquee theater new hartford ny New-old approach to creating new ventures
New-old approach to creating new ventures New market realities
New market realities Njbta
Njbta New classical and new keynesian macroeconomics
New classical and new keynesian macroeconomics Chapter 16 toward a new heaven and a new earth
Chapter 16 toward a new heaven and a new earth New classical and new keynesian macroeconomics
New classical and new keynesian macroeconomics Roosevelt taft and wilson venn diagram
Roosevelt taft and wilson venn diagram Zimmer aesthetic division
Zimmer aesthetic division Wv division of personnel
Wv division of personnel Indiana gaming commission charity gaming division
Indiana gaming commission charity gaming division Four digit division
Four digit division Understanding ratios
Understanding ratios Tung shin hospital
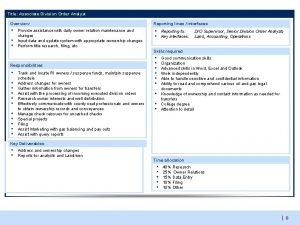
Tung shin hospital Division order analyst jobs
Division order analyst jobs Tipos de problemas de multiplicación
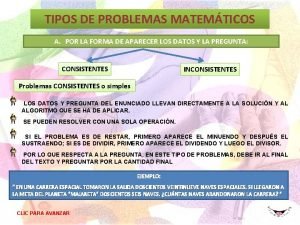
Tipos de problemas de multiplicación Sutorbilt compressors houston
Sutorbilt compressors houston Figurative language in what a wonderful world
Figurative language in what a wonderful world Hypopolarization
Hypopolarization State remainder theorem
State remainder theorem Proof remainder theorem
Proof remainder theorem Little man computer code
Little man computer code Components of trachea
Components of trachea Social structure of india
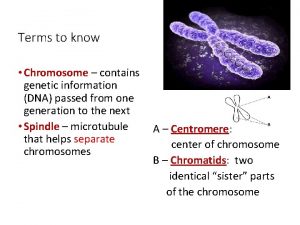
Social structure of india Mitosis pmat diagram
Mitosis pmat diagram Division del trabajo
Division del trabajo Ejercicios potencias 3 eso doc
Ejercicios potencias 3 eso doc Local 237 union
Local 237 union Dividing matrices
Dividing matrices Fp adder
Fp adder How many syllables in trampoline
How many syllables in trampoline Multiplication doc.com
Multiplication doc.com Ecc division of larsen & toubro
Ecc division of larsen & toubro Connecticut division of criminal justice
Connecticut division of criminal justice Square root of 23 by long division method
Square root of 23 by long division method 5476 square root
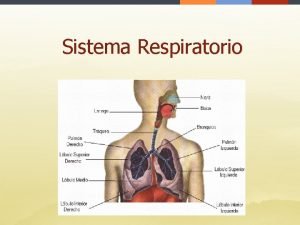
5476 square root Aparato respiratorio boca
Aparato respiratorio boca Bus stop method with remainders
Bus stop method with remainders Segment reporting and decentralization
Segment reporting and decentralization Division statement
Division statement Division statement
Division statement How to write remainder in synthetic division
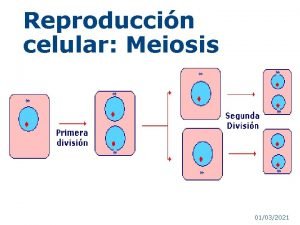
How to write remainder in synthetic division Meiosis steps
Meiosis steps What is commutative property
What is commutative property Division property of equality
Division property of equality What is the rule for adding and subtracting decimals
What is the rule for adding and subtracting decimals Paquinema
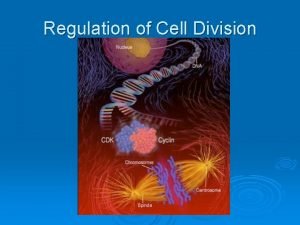
Paquinema Frequency of cell division
Frequency of cell division Caracol aguda
Caracol aguda Tcoommi
Tcoommi