Malignant hematopoiesis 1 Myeloproliferative disorders Emanuel Neas necascesnet


- Slides: 79
Malignant hematopoiesis (1) Myeloproliferative disorders Emanuel Nečas necas@cesnet. cz
Introduction
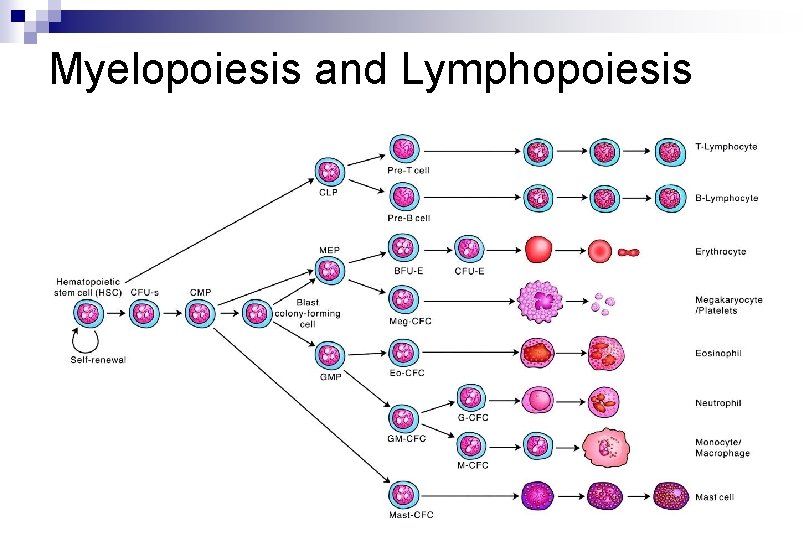
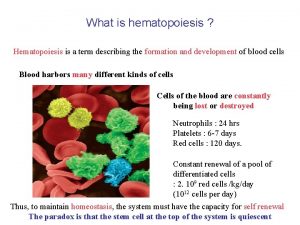
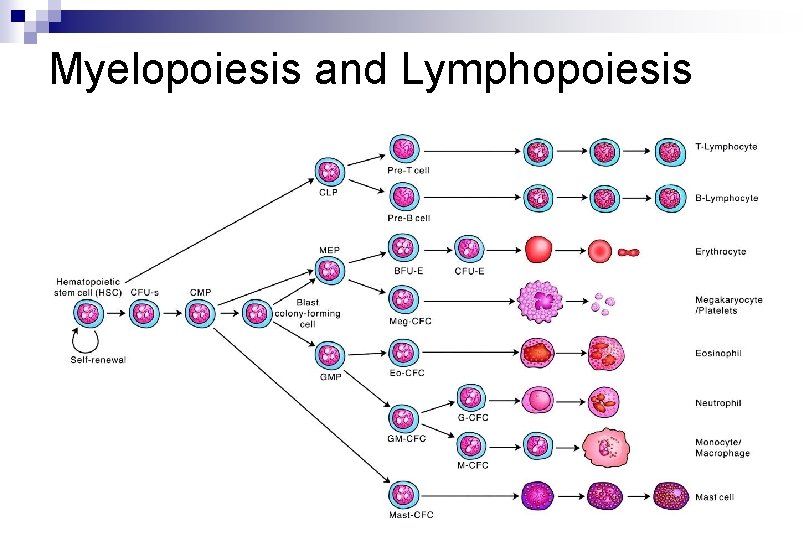
Myelopoiesis and Lymphopoiesis
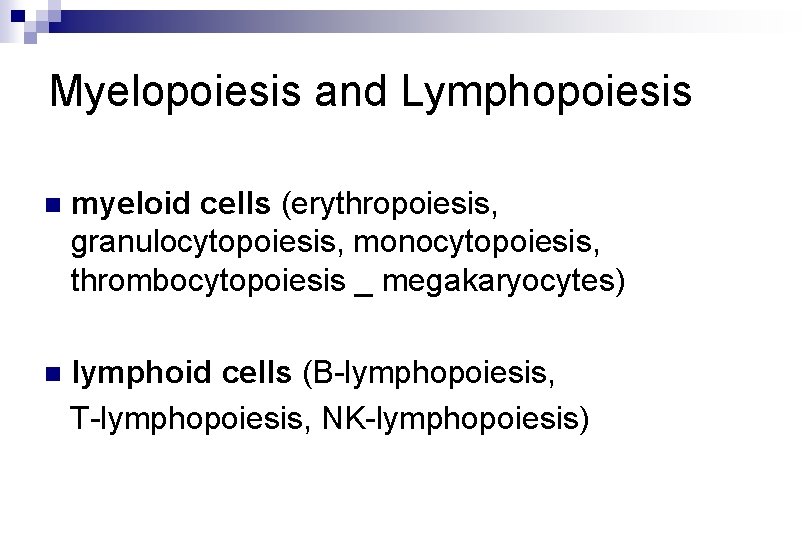
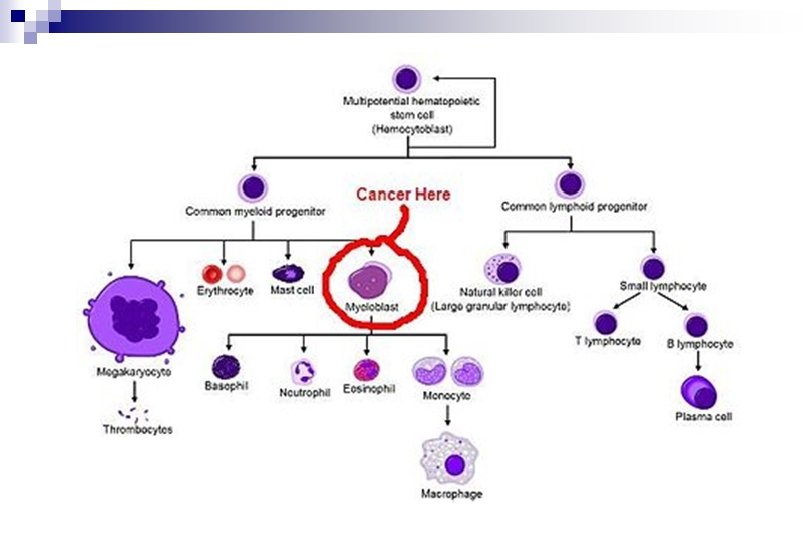
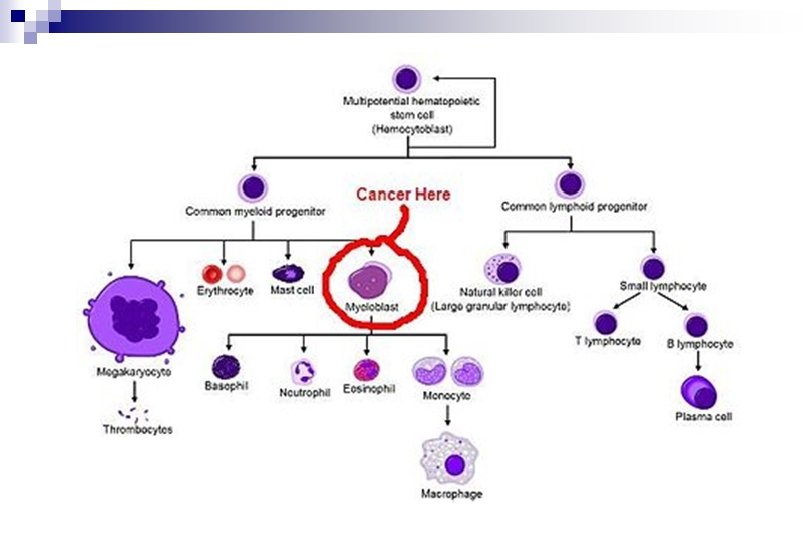
Myelopoiesis and Lymphopoiesis n myeloid cells (erythropoiesis, granulocytopoiesis, monocytopoiesis, thrombocytopoiesis _ megakaryocytes) n lymphoid cells (B-lymphopoiesis, T-lymphopoiesis, NK-lymphopoiesis)
n Myeloproliferative disorders n Lymfoproliferative disorders
n Myeloproliferative disorders - chronic - acute n Lymfoproliferative disorders - chronic - acute
Lymphoproliferative diseases can also have a form of a solid tumor, a lymphoma. Though seemingly localized to a lymphoid tissue outside the bone marrow, it is considered to be a systemic disease involving (infiltrating) the bone marrow regularly.
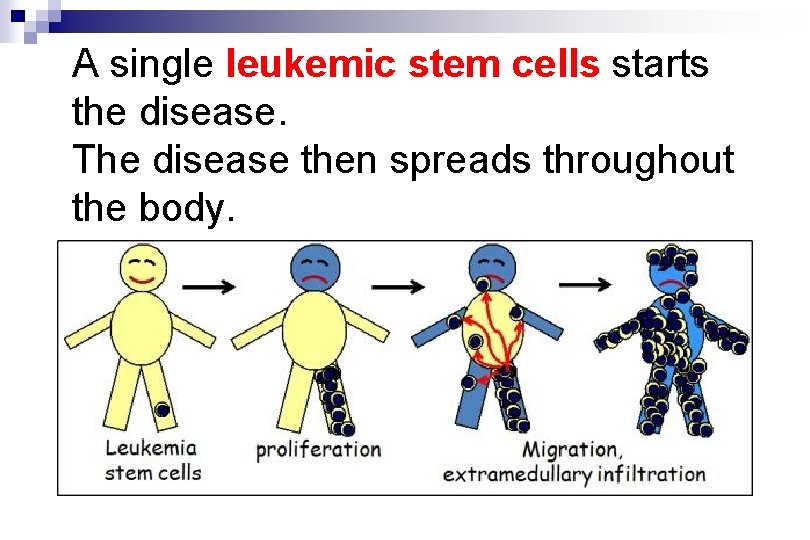
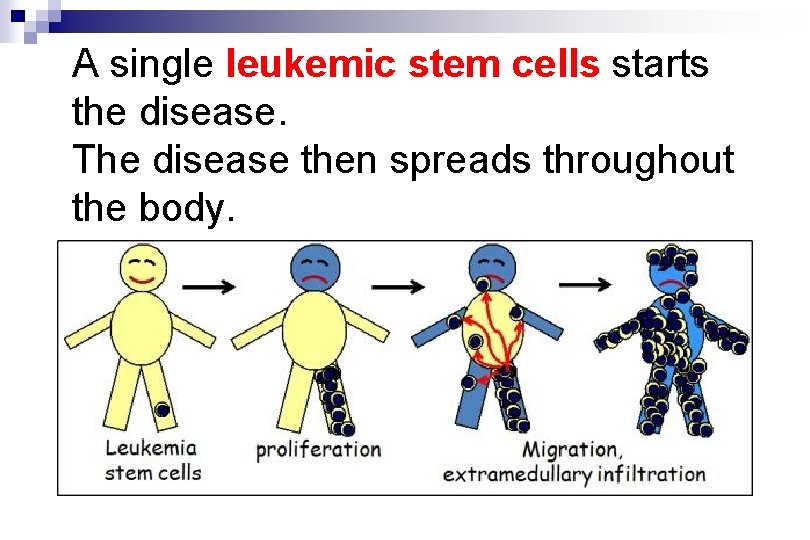
A single leukemic stem cells starts the disease. The disease then spreads throughout the body.
Malignant hematopoiesis n n is usually monoclonal is usually systemic
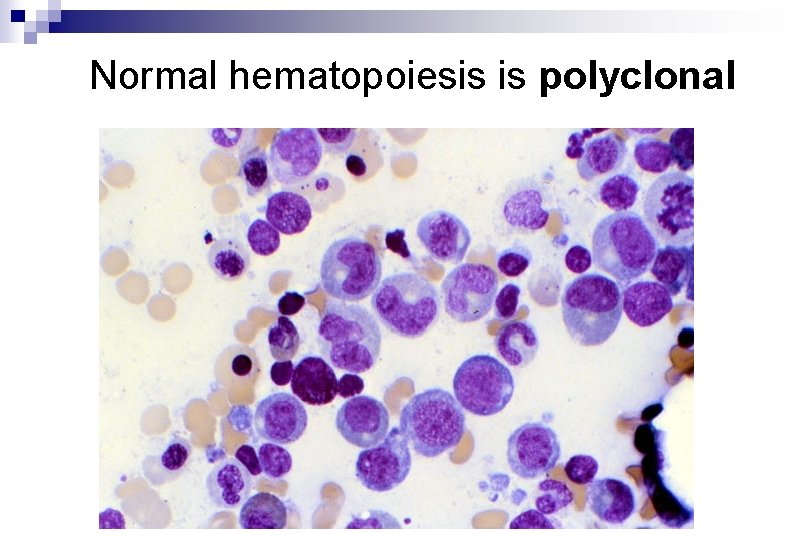
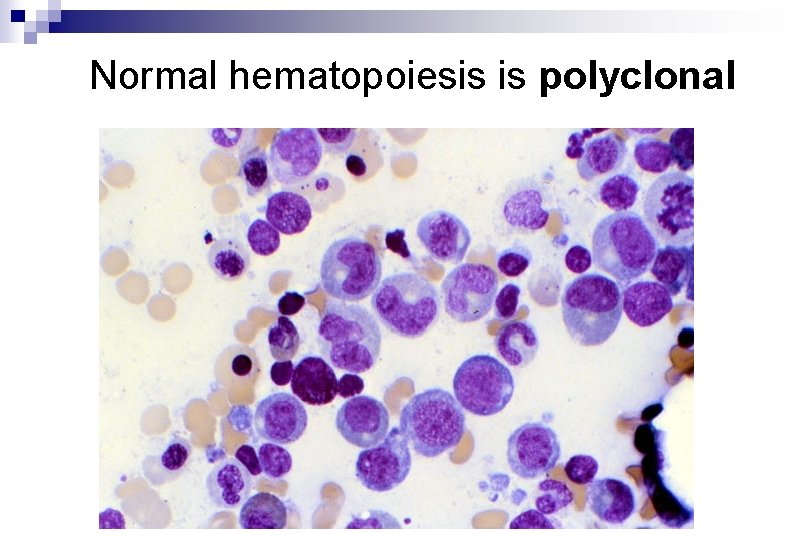
Normal hematopoiesis is polyclonal
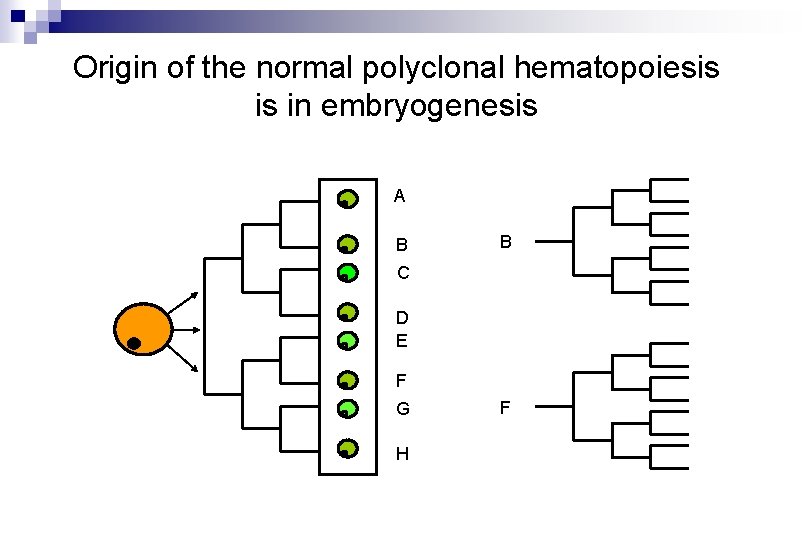
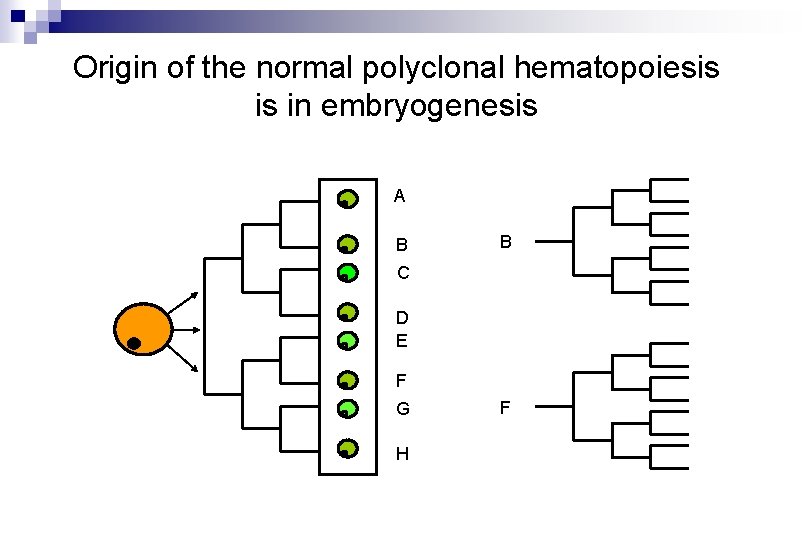
Origin of the normal polyclonal hematopoiesis is in embryogenesis A B B C D E F G H F
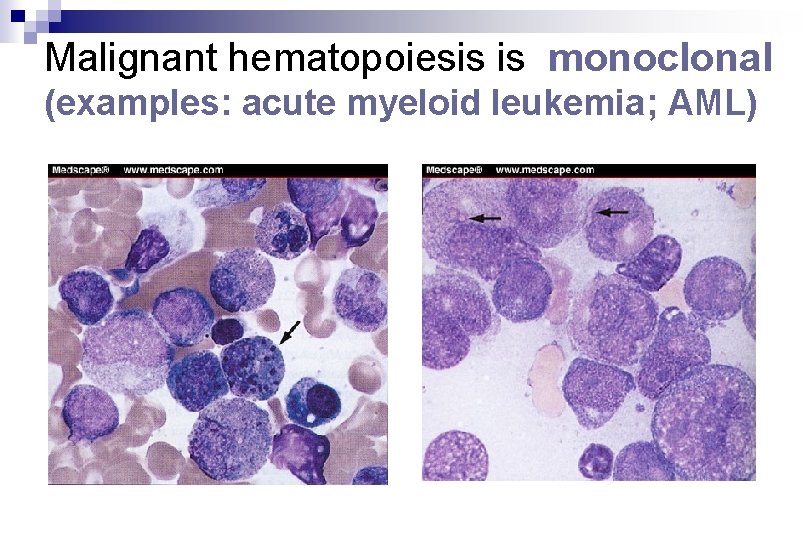
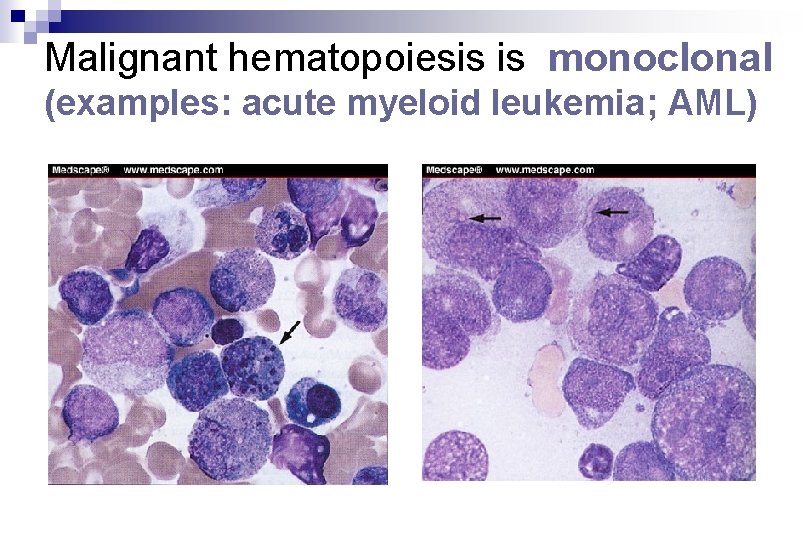
Malignant hematopoiesis is monoclonal (examples: acute myeloid leukemia; AML)
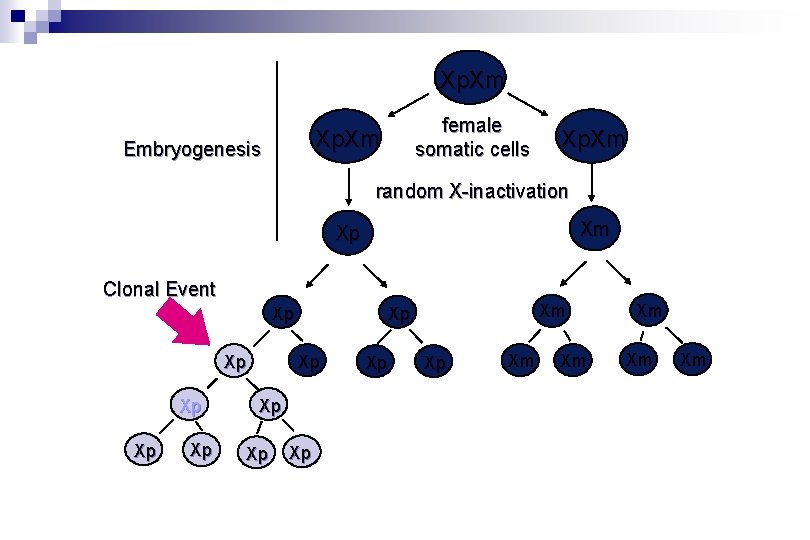
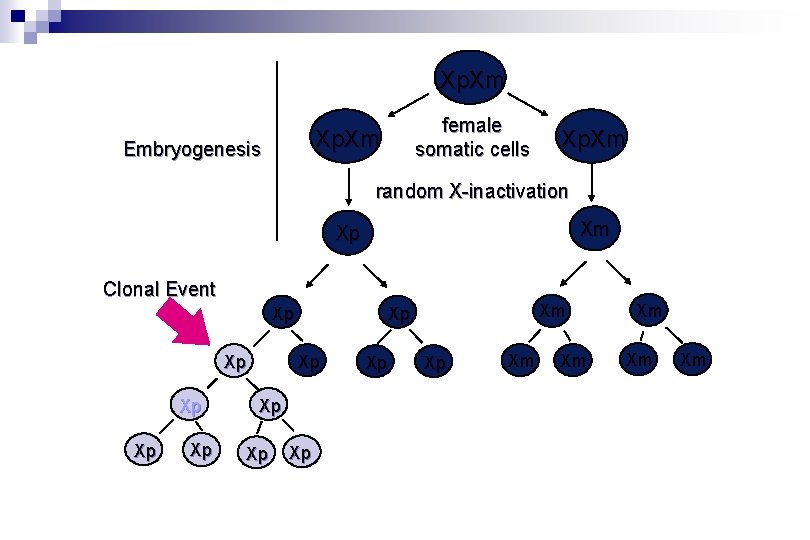
Xp. Xm female somatic cells Xp. Xm Embryogenesis Xp. Xm random X-inactivation Xm Xp Clonal Event Xp Xp Xm Xp Xp Xm Xm Xm

Malignant monoclonal hematopoiesis is caused by mutations (F´cell clone) A B B C D E F G H F´
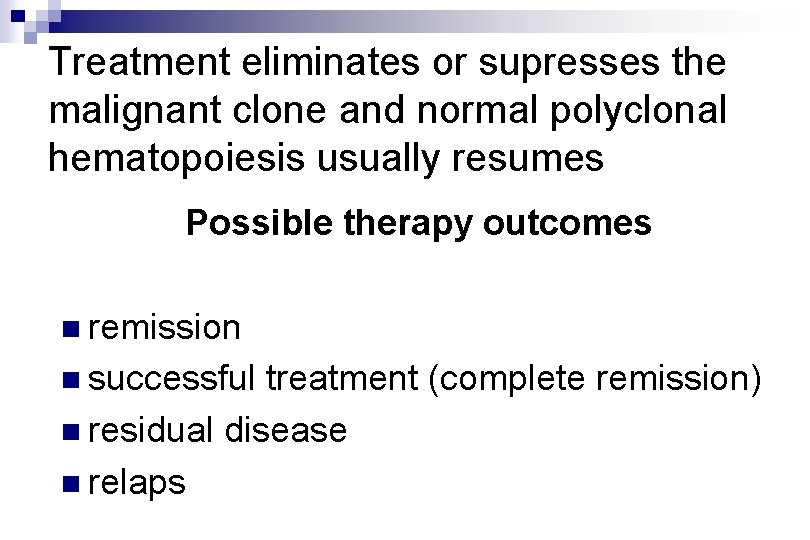
Treatment eliminates or supresses the malignant clone and normal polyclonal hematopoiesis usually resumes Possible therapy outcomes n remission n successful treatment (complete remission) n residual disease n relaps
A pathological dominant clone may start from a mutated hematopoietic stem cell but not necessarily. A mutated progenitor cell may be a source of a dominant malignant clone as well.
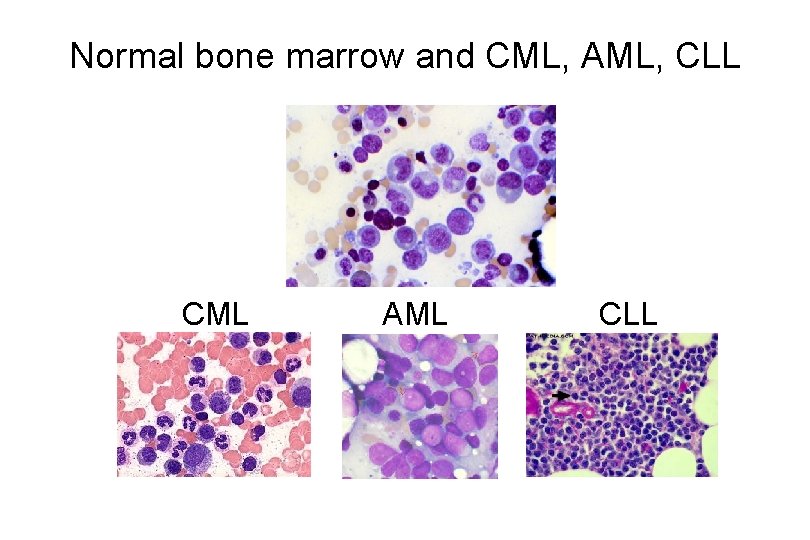
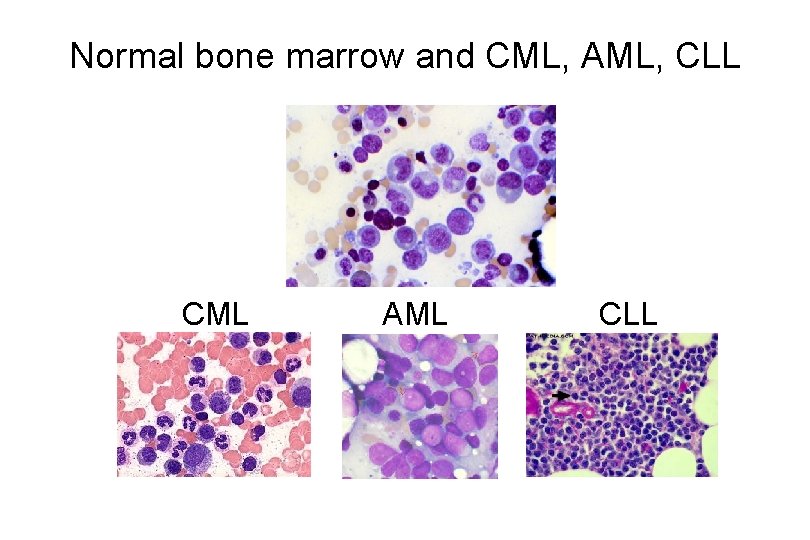
Normal bone marrow and CML, AML, CLL CML AML CLL
Chronic myeloproliferative disorders
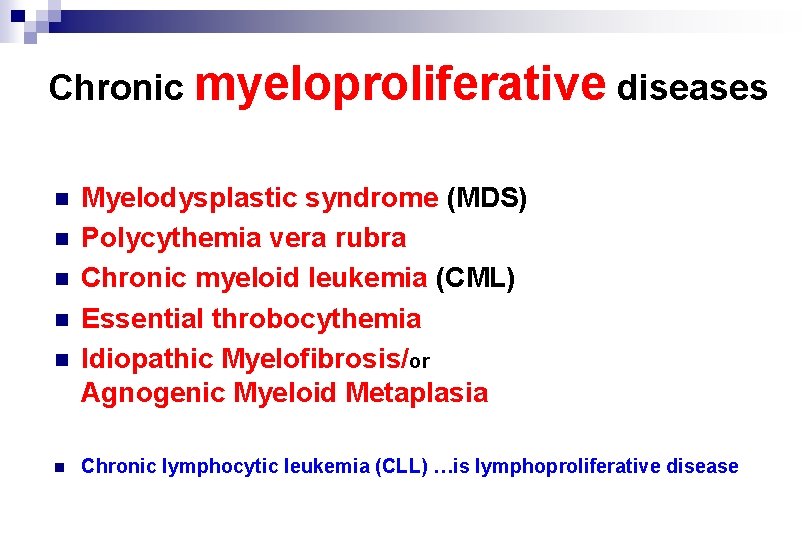
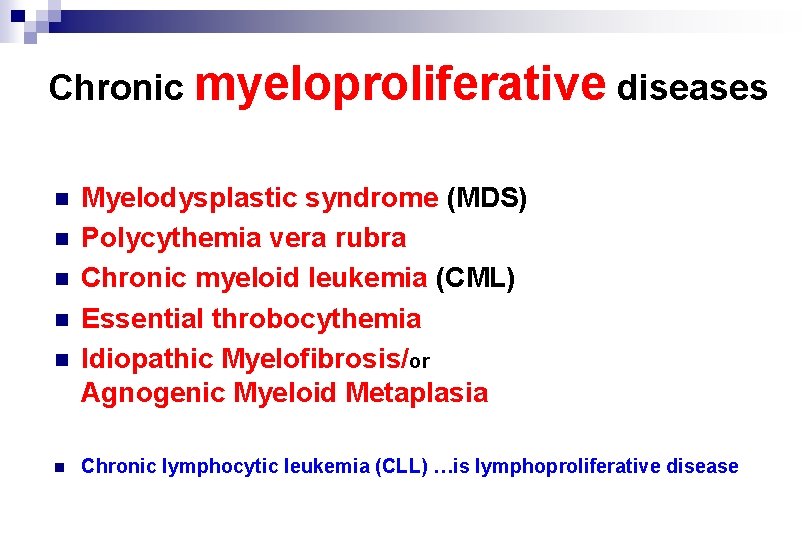
Chronic myeloproliferative diseases n n n Myelodysplastic syndrome (MDS) Polycythemia vera rubra Chronic myeloid leukemia (CML) Essential throbocythemia Idiopathic Myelofibrosis/or Agnogenic Myeloid Metaplasia Chronic lymphocytic leukemia (CLL) …is lymphoproliferative disease
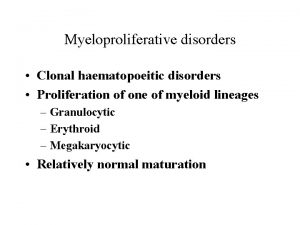
Myeloproliferative Disorders
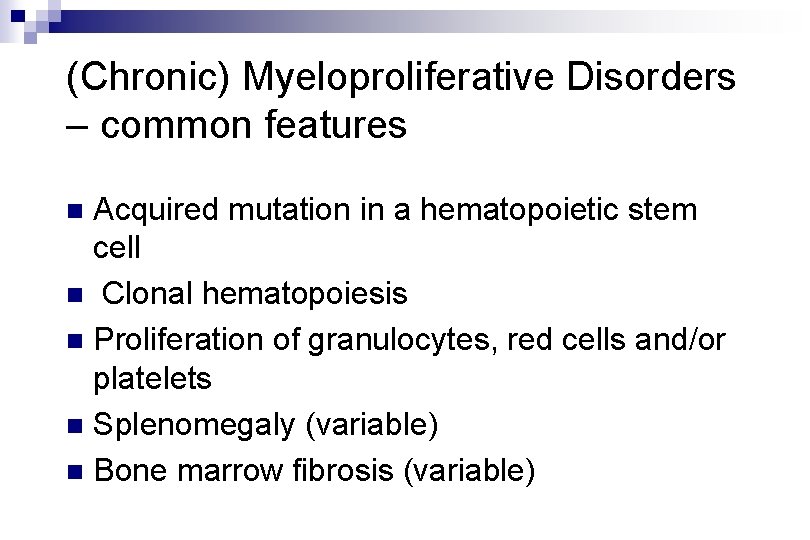
(Chronic) Myeloproliferative Disorders – common features Acquired mutation in a hematopoietic stem cell n Clonal hematopoiesis n Proliferation of granulocytes, red cells and/or platelets n Splenomegaly (variable) n Bone marrow fibrosis (variable) n

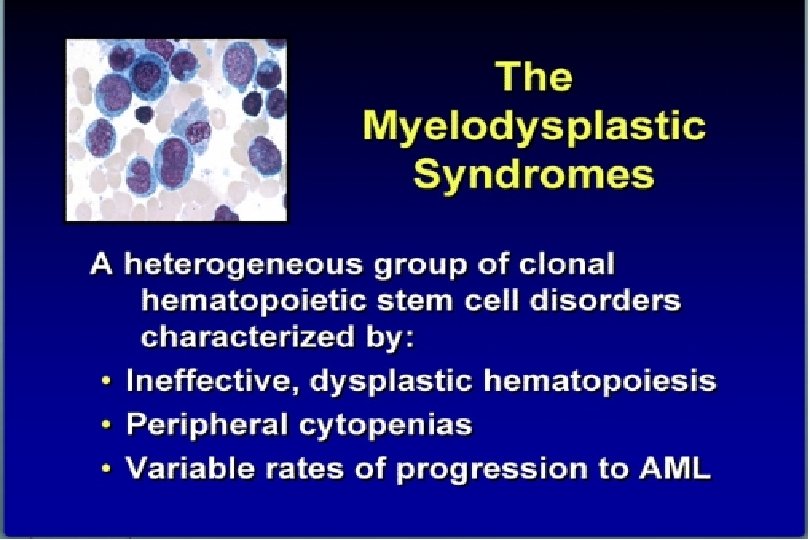
Myelodysplastic syndrome (MDS)
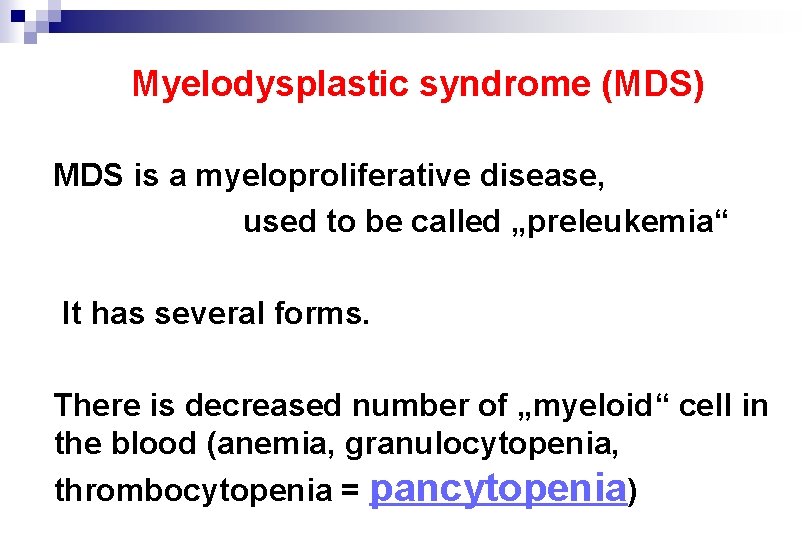
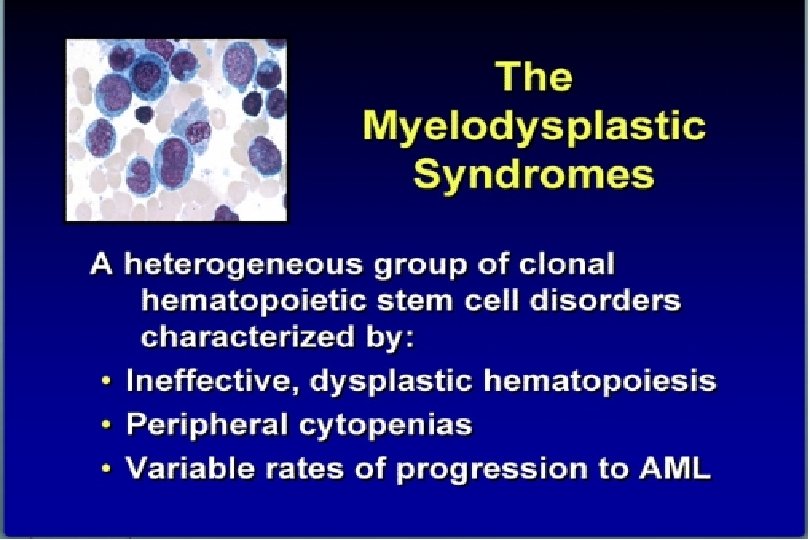
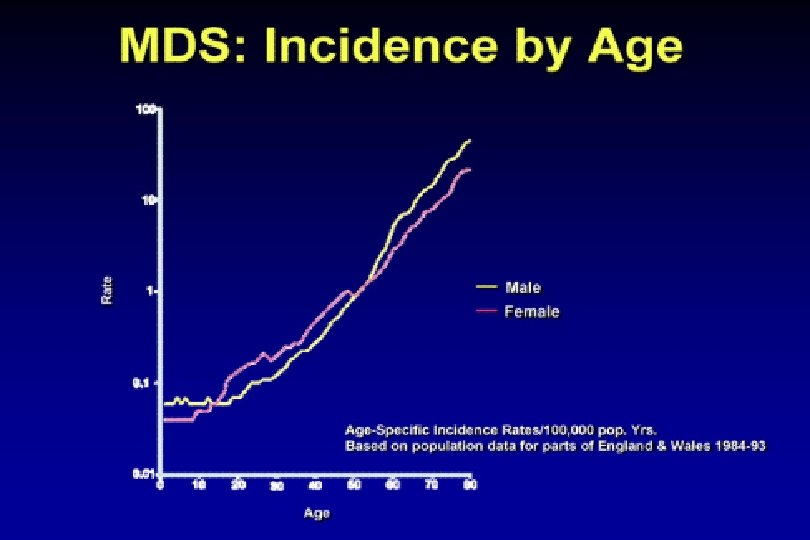
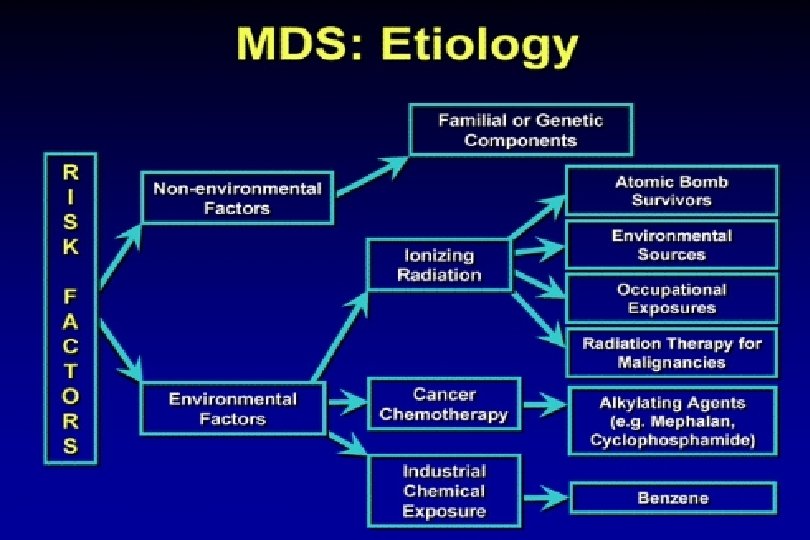
Myelodysplastic syndrome (MDS) MDS is a myeloproliferative disease, used to be called „preleukemia“ It has several forms. There is decreased number of „myeloid“ cell in the blood (anemia, granulocytopenia, thrombocytopenia = pancytopenia)
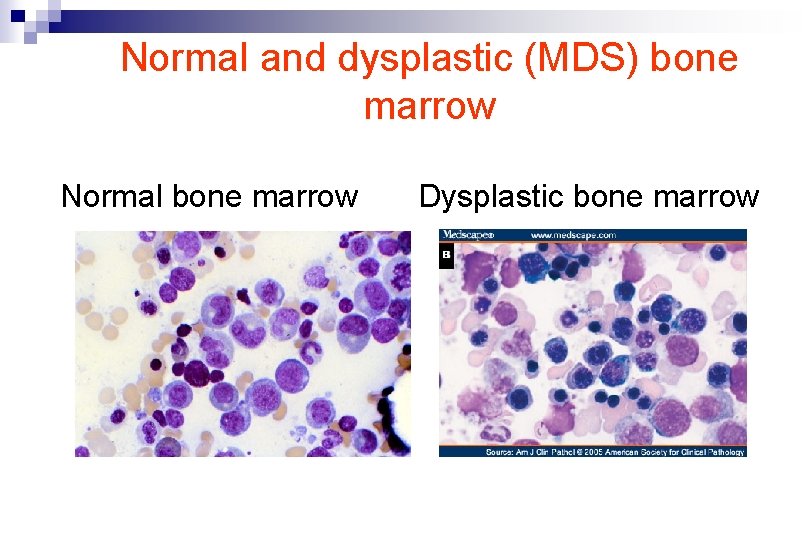
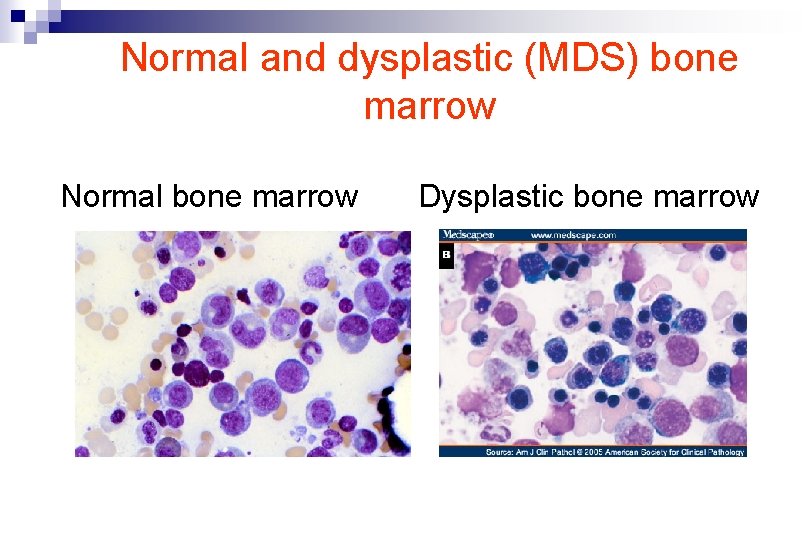
Normal and dysplastic (MDS) bone marrow Normal bone marrow Dysplastic bone marrow
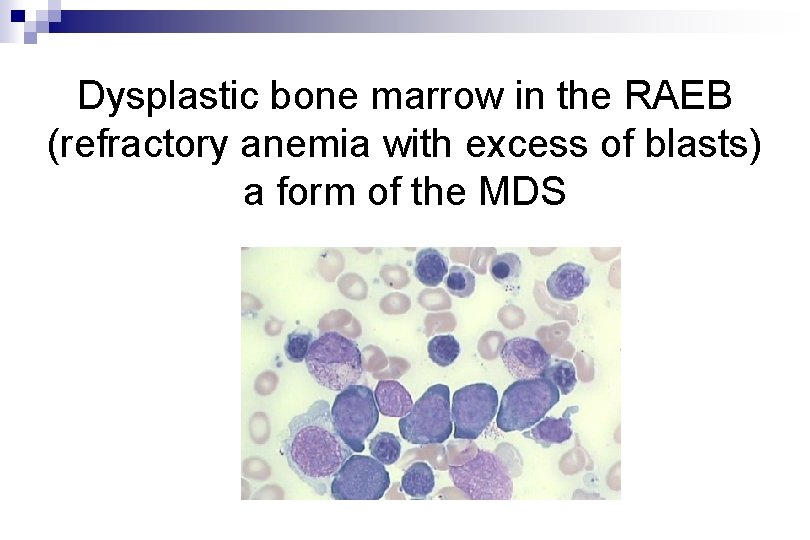
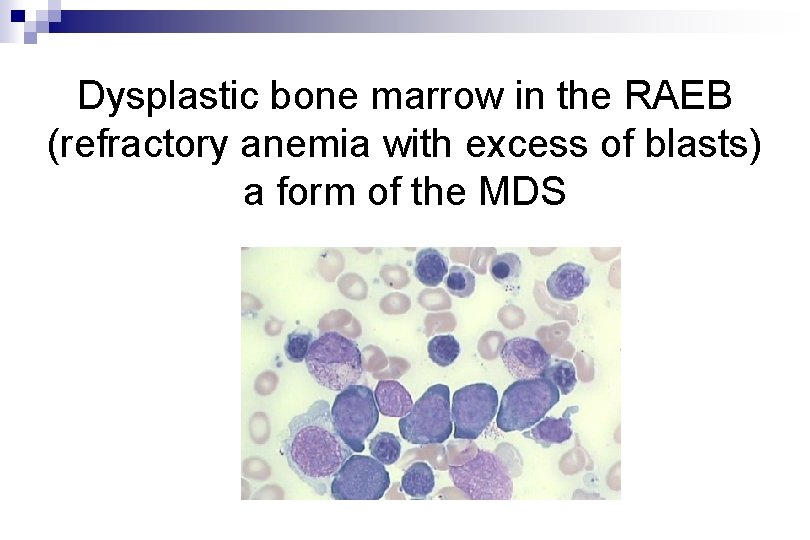
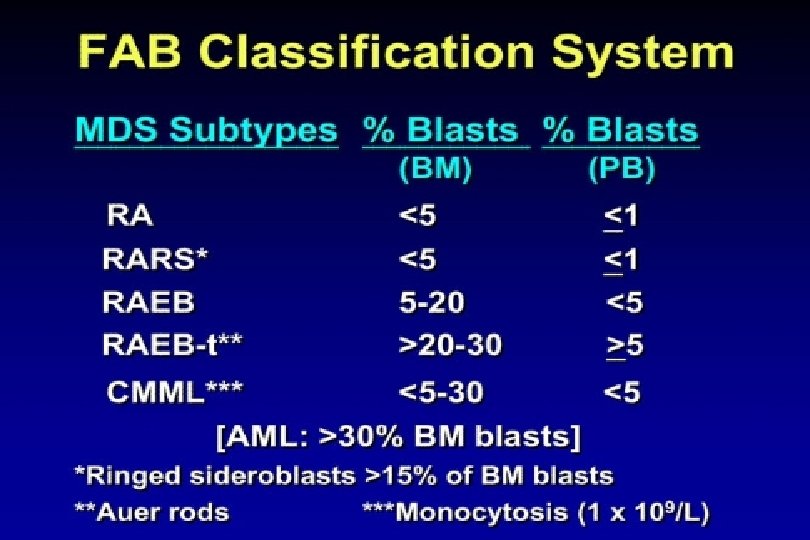
Dysplastic bone marrow in the RAEB (refractory anemia with excess of blasts) a form of the MDS
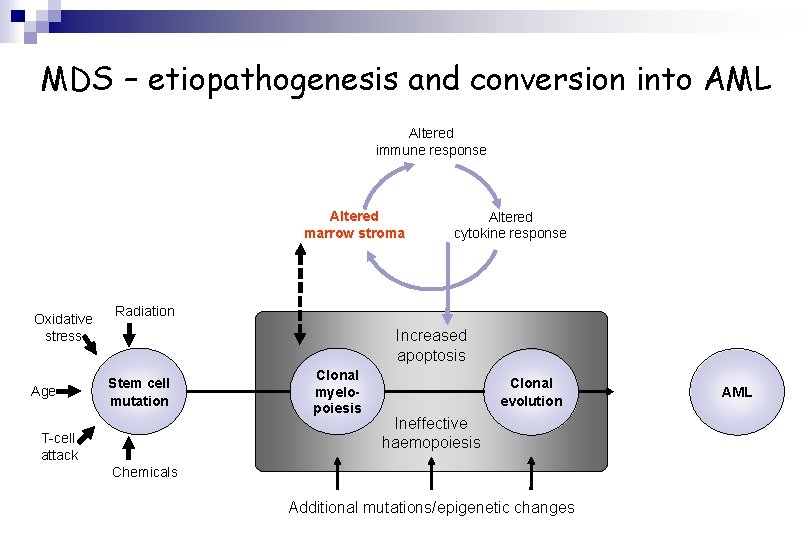
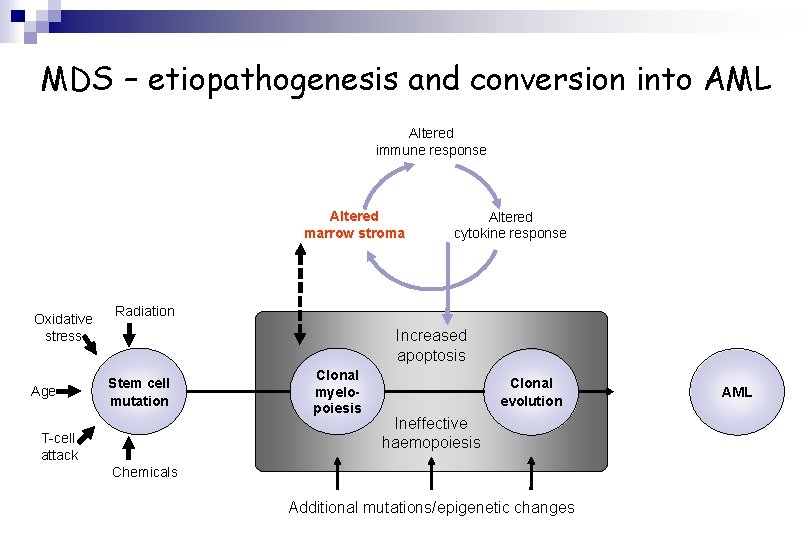
MDS – etiopathogenesis and conversion into AML Altered immune response Altered marrow stroma Oxidative stress Age Altered cytokine response Radiation Increased apoptosis Stem cell mutation T-cell attack Clonal myelopoiesis Clonal evolution Ineffective haemopoiesis Chemicals Additional mutations/epigenetic changes AML
Polycythemia vera rubra („primary polycythemia“, Disease Vasquez-Osler)
Polycythemias Hct 43% 53%
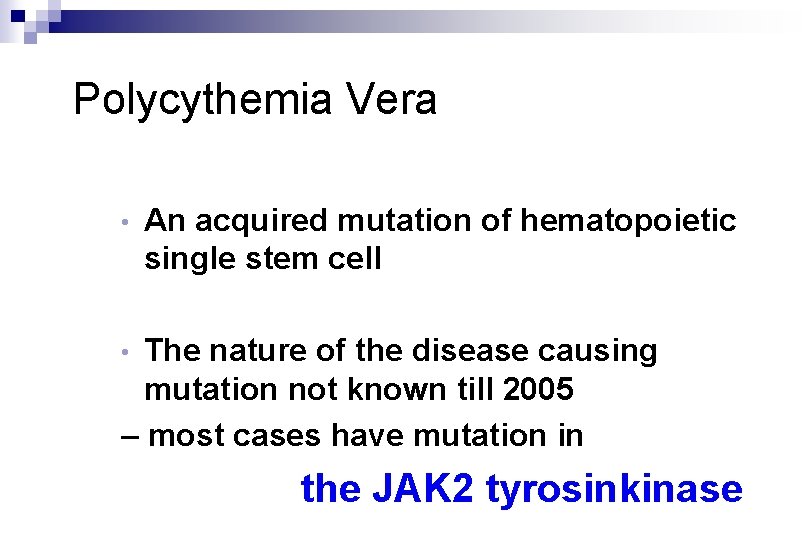
Polycythemia Vera • An acquired mutation of hematopoietic single stem cell The nature of the disease causing mutation not known till 2005 – most cases have mutation in • the JAK 2 tyrosinkinase
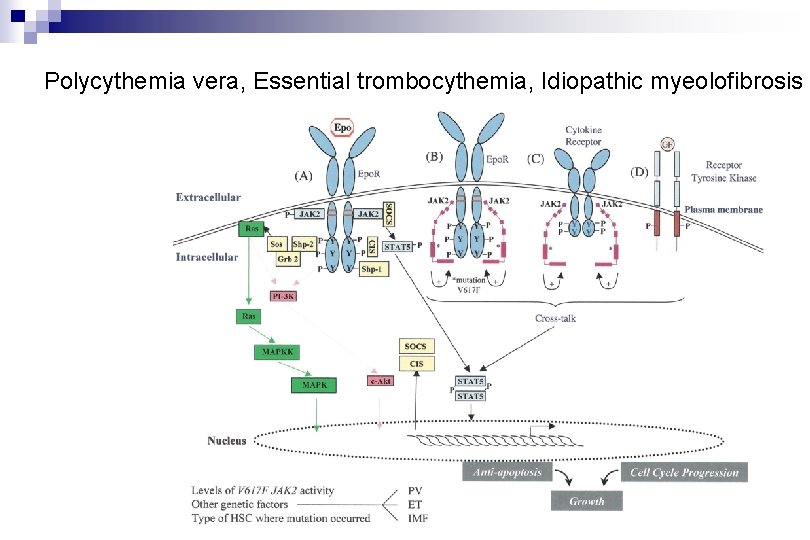
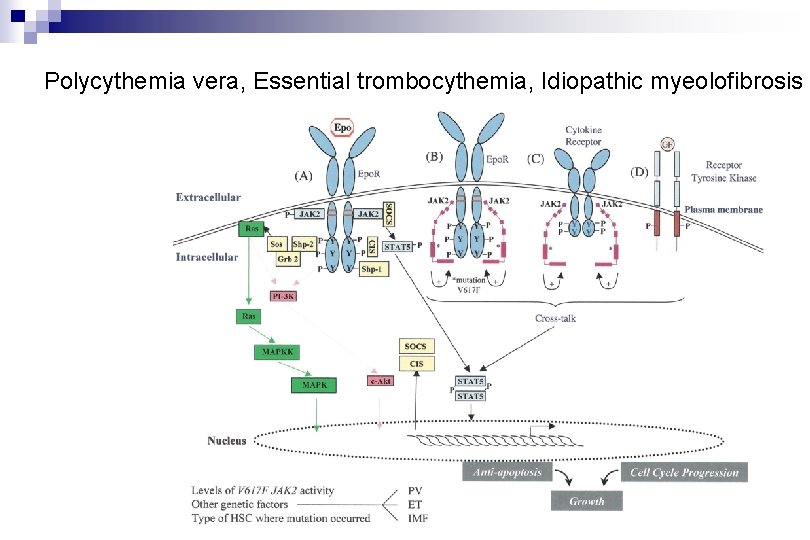
Polycythemia vera, Essential trombocythemia, Idiopathic myeolofibrosis
Frequency, % Incidence of Polycythemia Vera Age
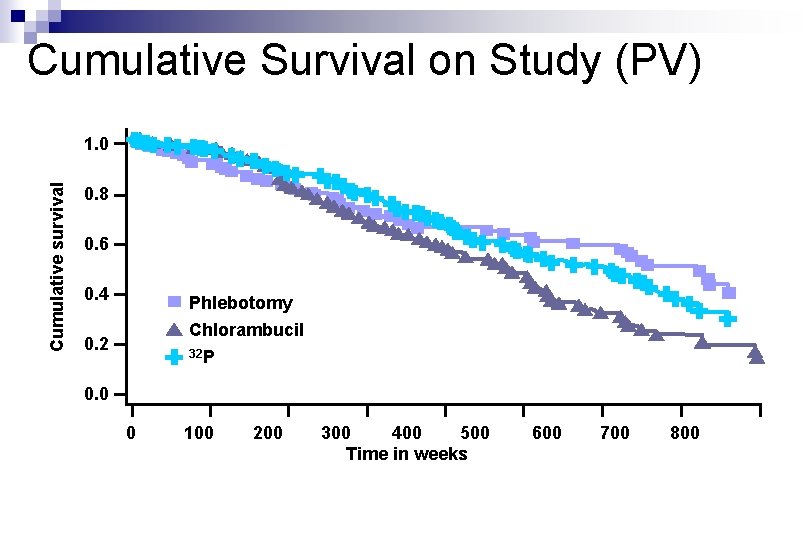
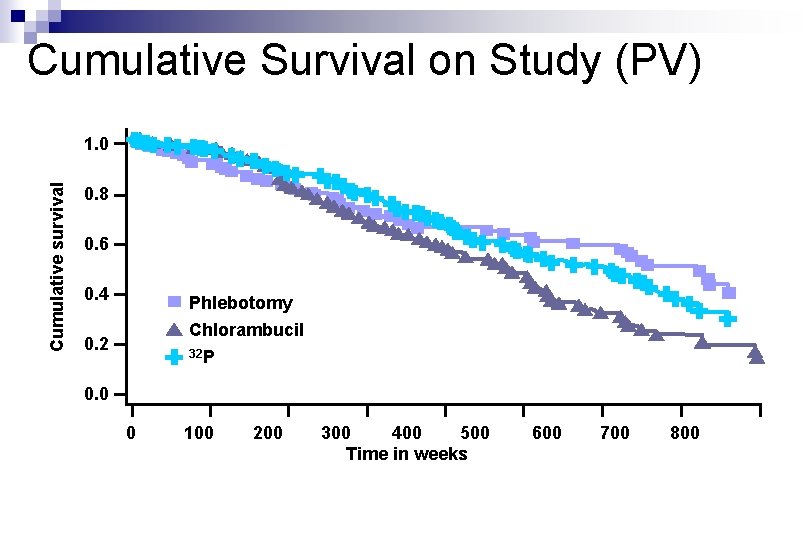
Cumulative Survival on Study (PV) Cumulative survival 1. 0 0. 8 0. 6 0. 4 Phlebotomy Chlorambucil 0. 2 32 P 0. 0 0 100 200 300 400 500 Time in weeks 600 700 800
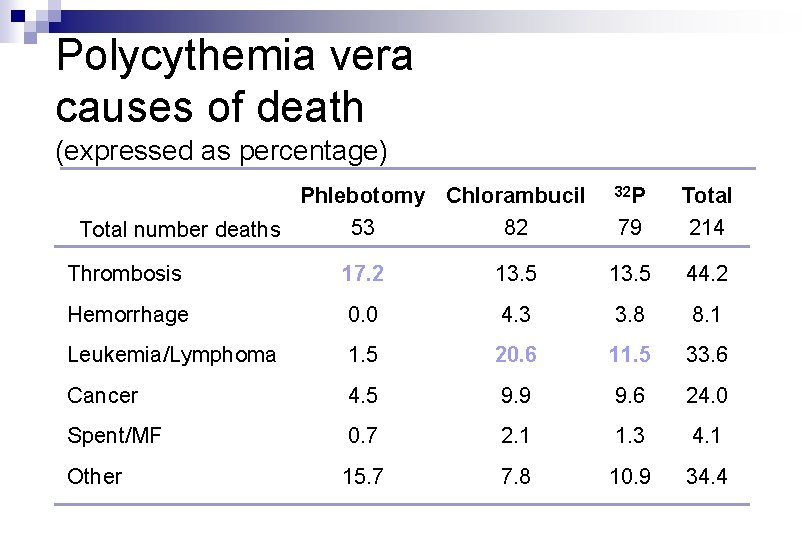
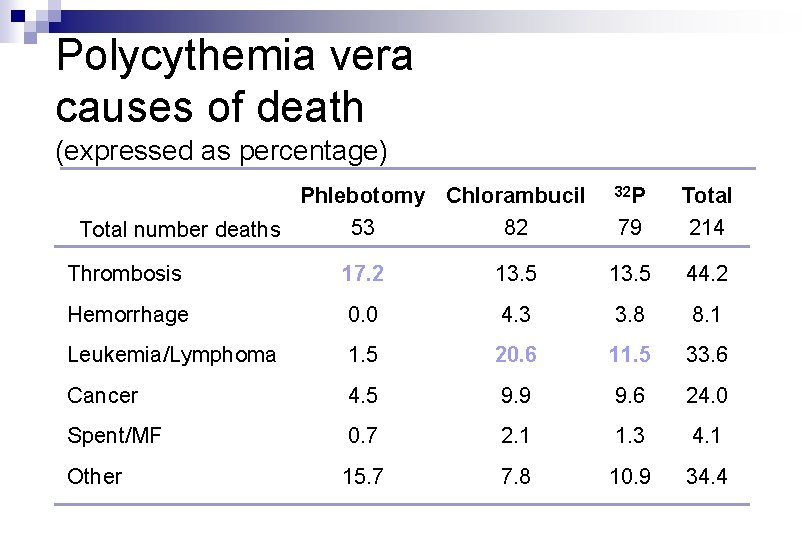
Polycythemia vera causes of death (expressed as percentage) Phlebotomy Chlorambucil 53 82 Total number deaths 32 P 79 Total 214 Thrombosis 17. 2 13. 5 44. 2 Hemorrhage 0. 0 4. 3 3. 8 8. 1 Leukemia/Lymphoma 1. 5 20. 6 11. 5 33. 6 Cancer 4. 5 9. 9 9. 6 24. 0 Spent/MF 0. 7 2. 1 1. 3 4. 1 Other 15. 7 7. 8 10. 9 34. 4
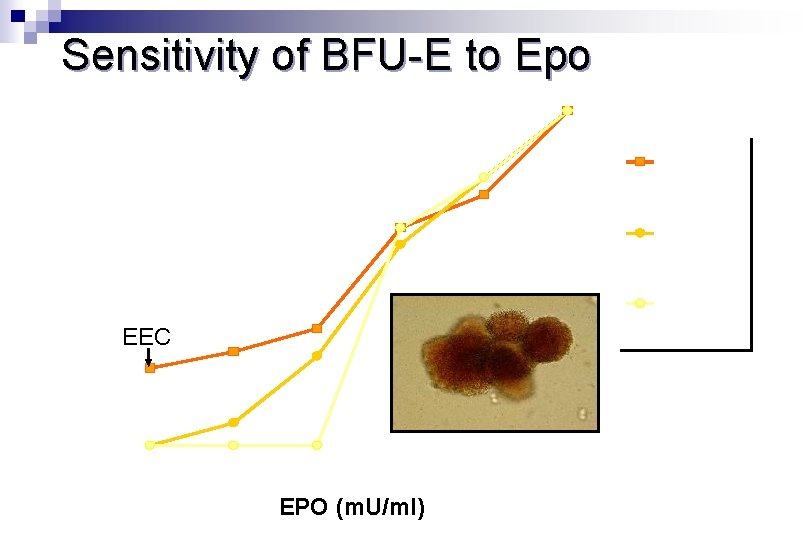
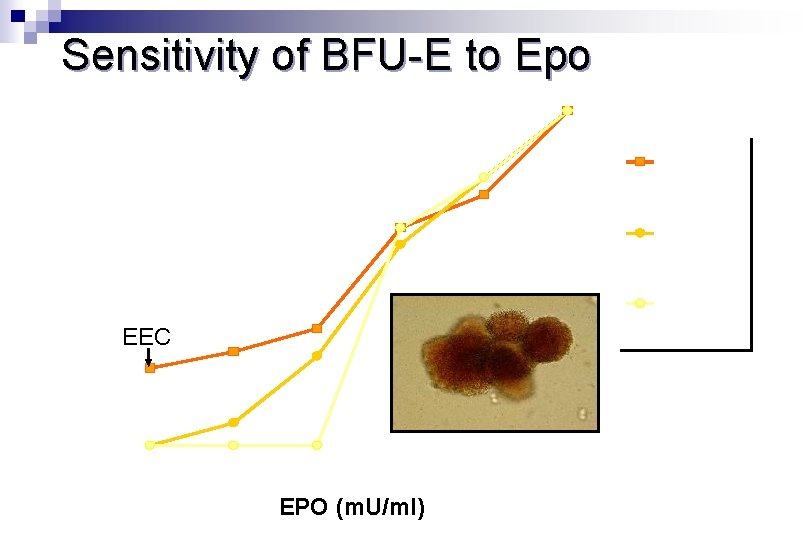
Sensitivity of BFU-E to Epo 100% PV (EEC) 75% PFCP 50% Normal EEC 25% 0% 0 30 60 125 EPO (m. U/ml) 250 3000
Essential thrombocytemia
Essential Thrombocythemia n Platelet count in excess of 600, 000 per mm 3 n Marked megakaryocytic hyperplasia n Abundant platelet clumps
Essential Thrombocythemia n No cytogenetic abnormalities n Splenomegaly seen in fewer than 50% n Morbidity: Thrombotic and/or bleeding problems
Essential Thrombocythemia n No cytogenetic abnormalities n The same mutation in the JAK 2 kinase as causes Polycythemia vera is present in some patients
Idiopathic Myelofibrosis/ Agnogenic Myeloid Metaplasia
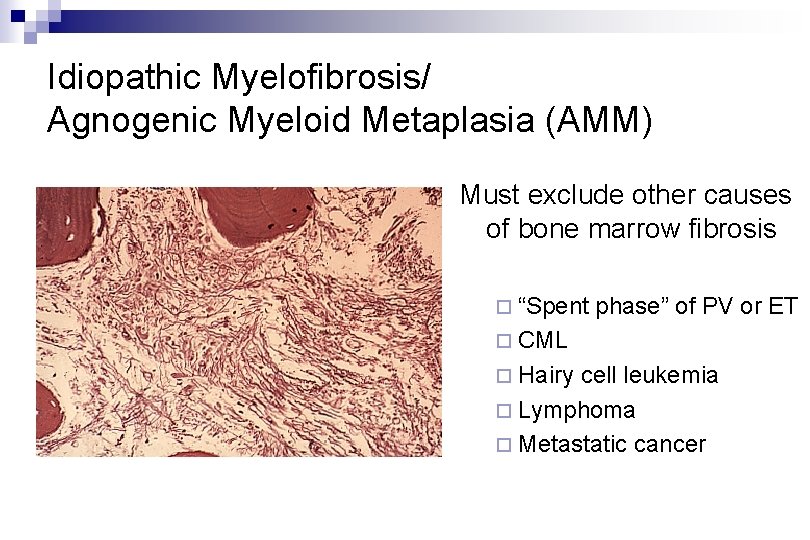
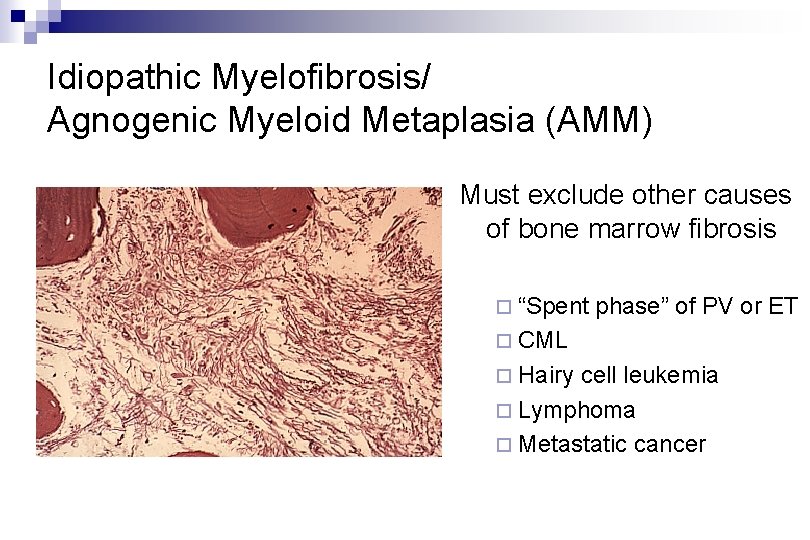
Idiopathic Myelofibrosis/ Agnogenic Myeloid Metaplasia (AMM) Must exclude other causes of bone marrow fibrosis ¨ “Spent phase” of PV or ET ¨ CML ¨ Hairy cell leukemia ¨ Lymphoma ¨ Metastatic cancer
Chronic myleoid leukemia (CML)
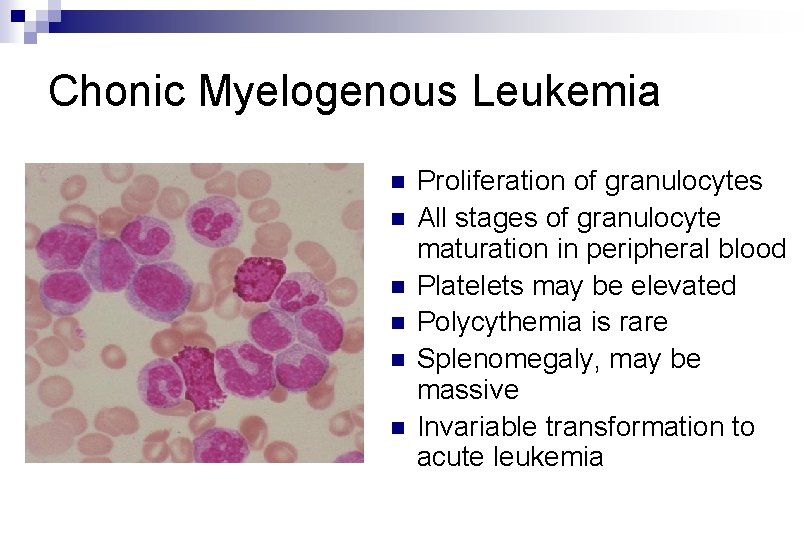
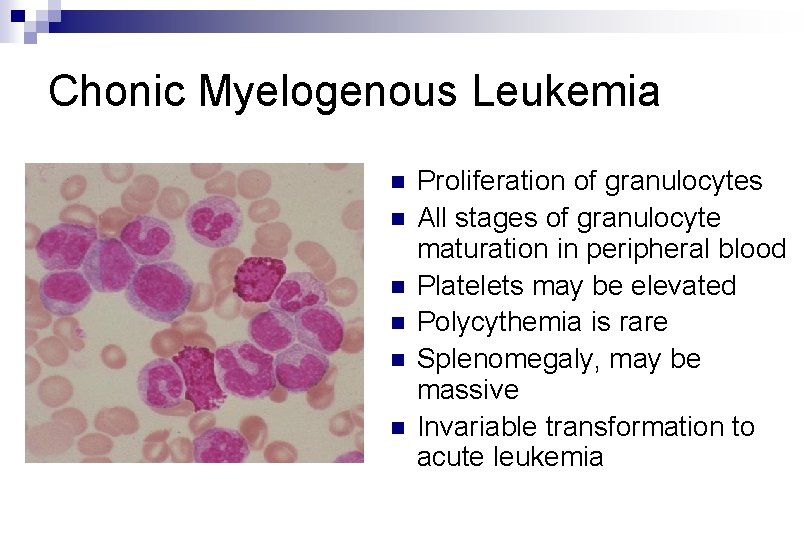
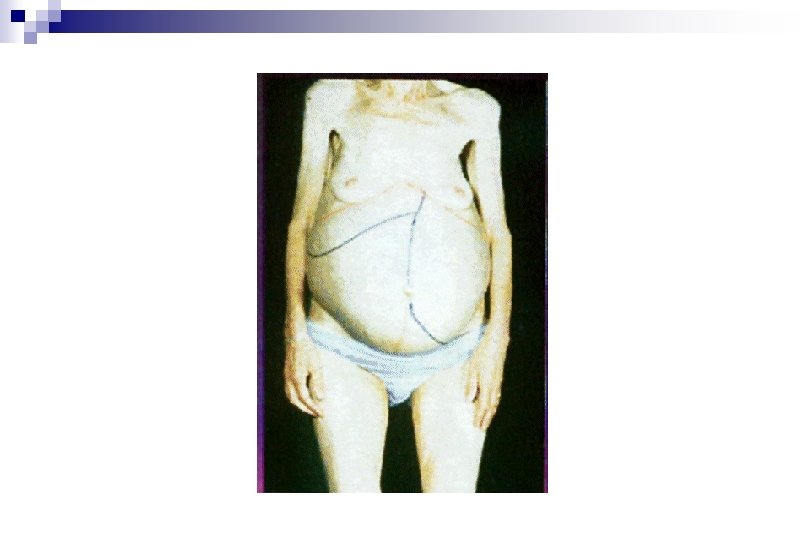
Chonic Myelogenous Leukemia n n n Proliferation of granulocytes All stages of granulocyte maturation in peripheral blood Platelets may be elevated Polycythemia is rare Splenomegaly, may be massive Invariable transformation to acute leukemia
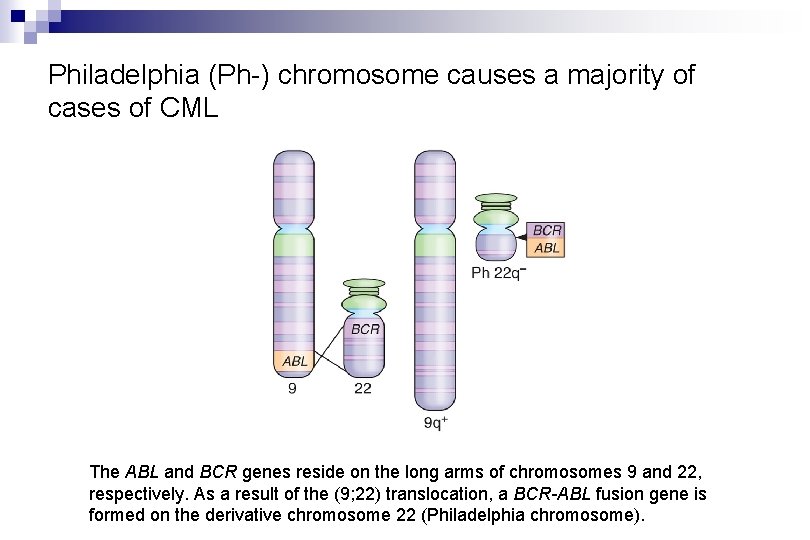
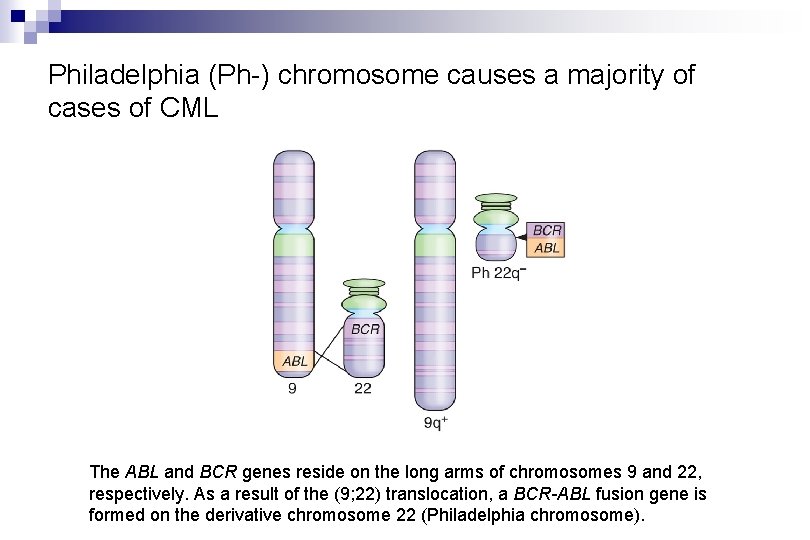
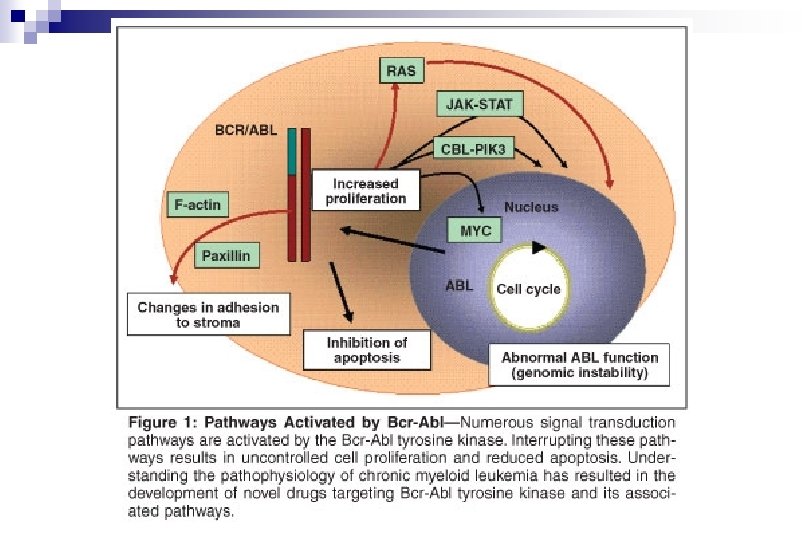
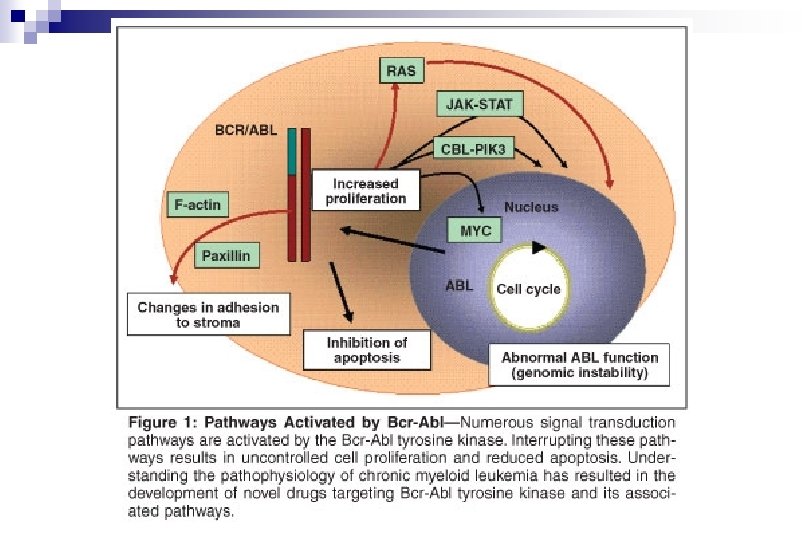
Philadelphia (Ph-) chromosome causes a majority of cases of CML The ABL and BCR genes reside on the long arms of chromosomes 9 and 22, respectively. As a result of the (9; 22) translocation, a BCR-ABL fusion gene is formed on the derivative chromosome 22 (Philadelphia chromosome).
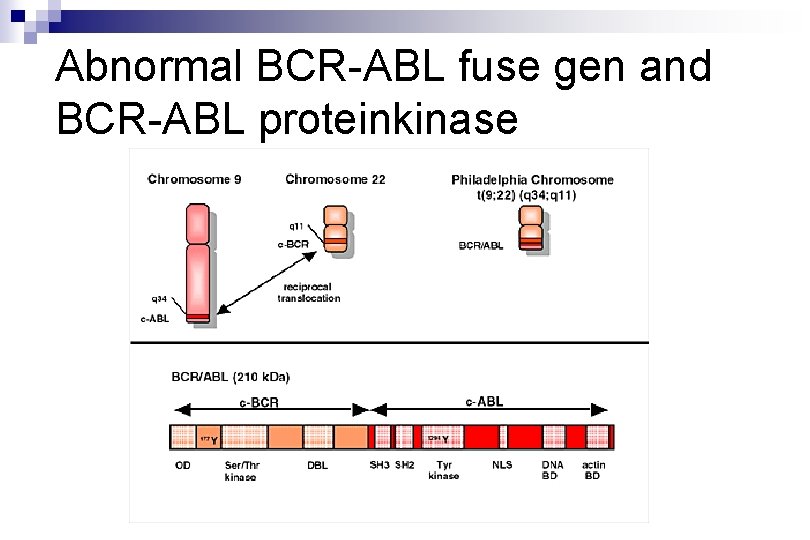
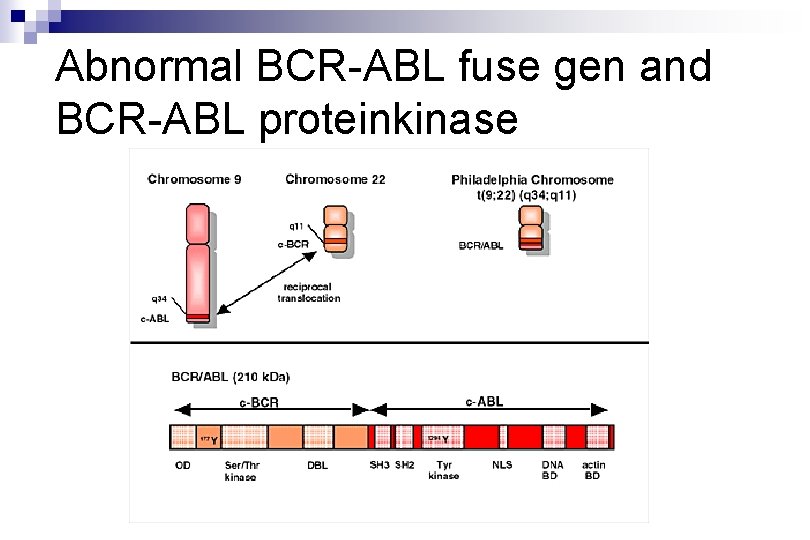
Abnormal BCR-ABL fuse gen and BCR-ABL proteinkinase
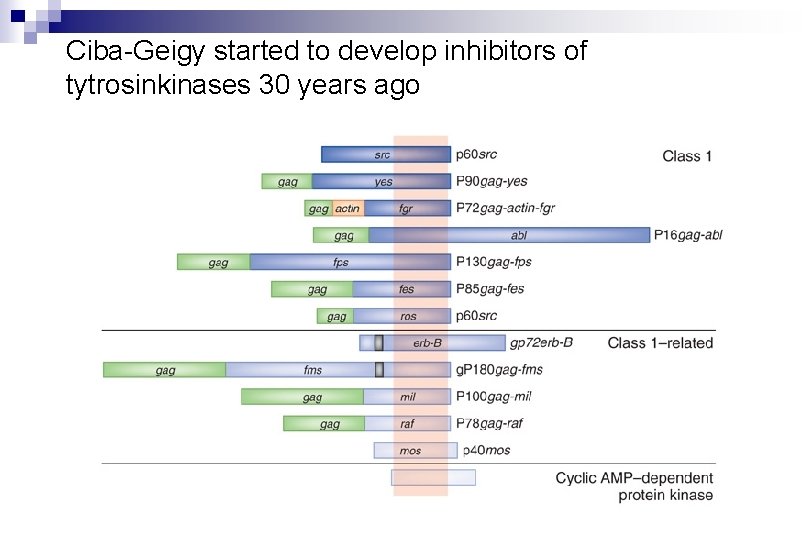
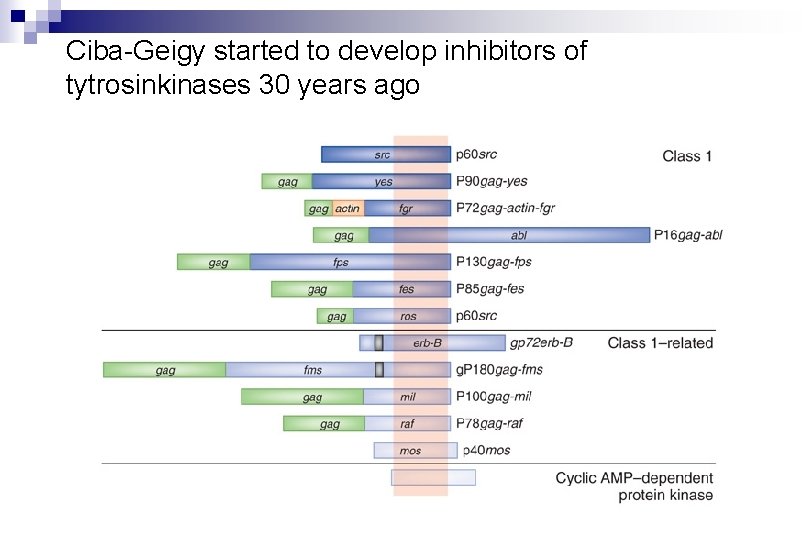
Ciba-Geigy started to develop inhibitors of tytrosinkinases 30 years ago
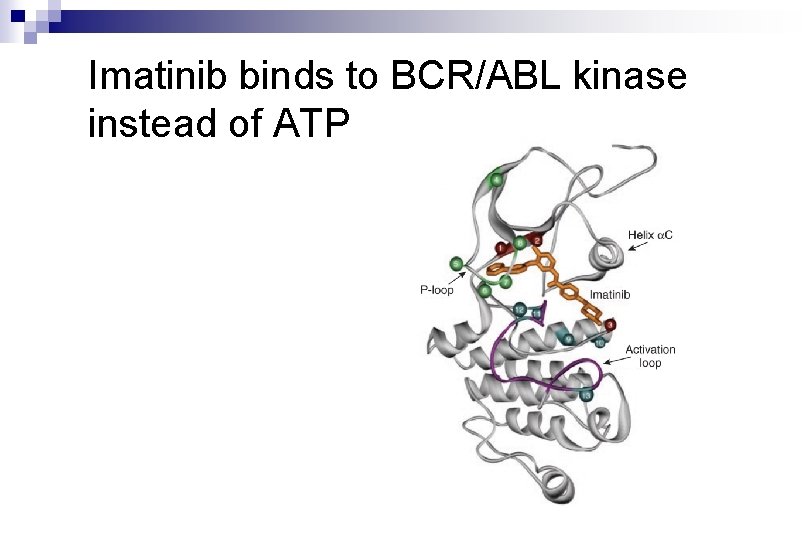
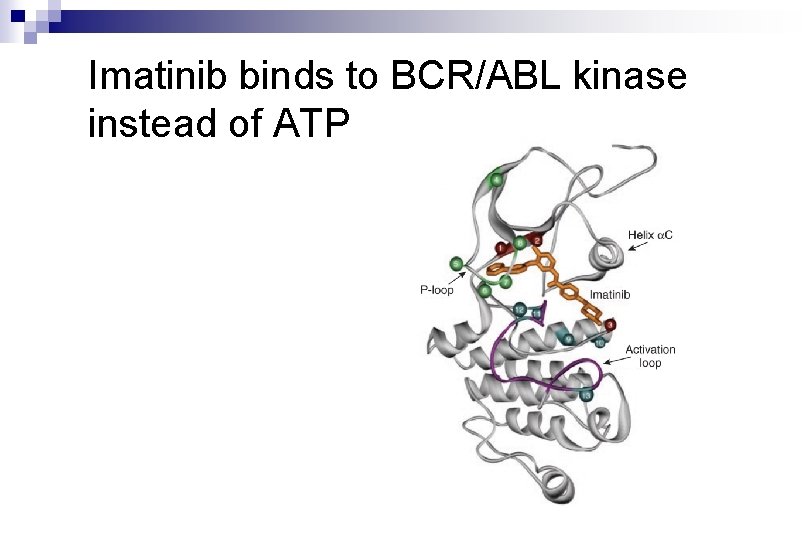
Imatinib binds to BCR/ABL kinase instead of ATP
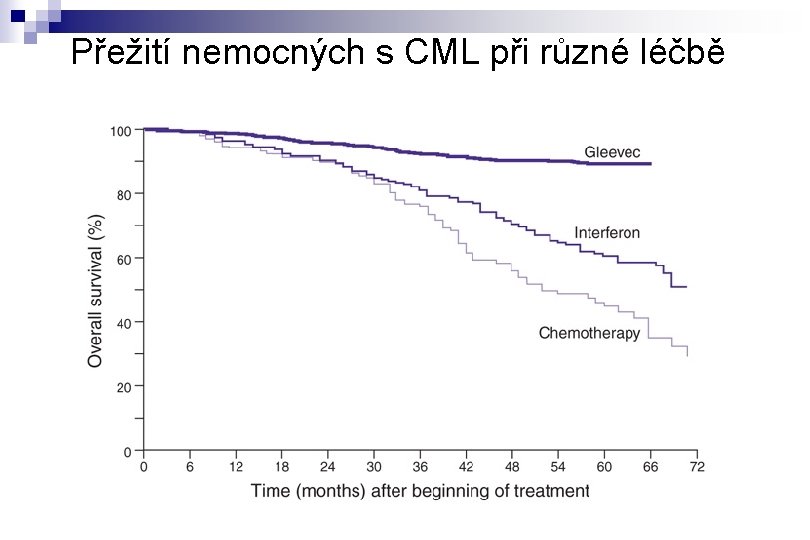
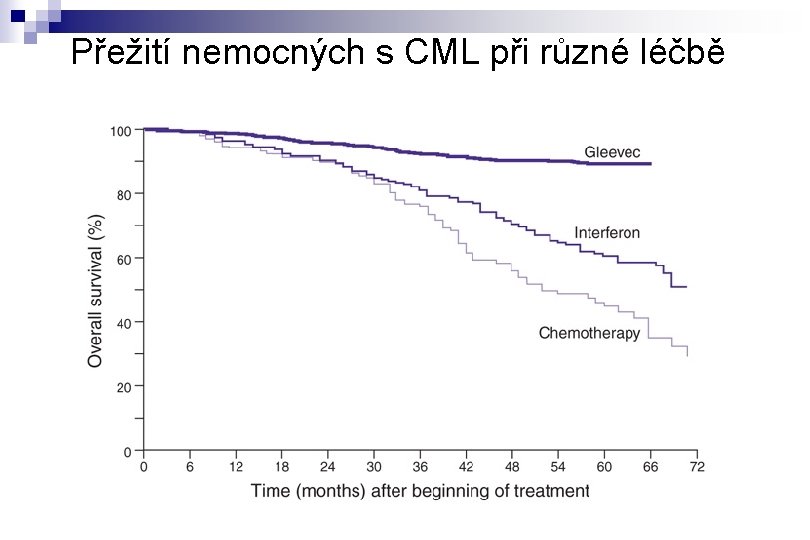
Přežití nemocných s CML při různé léčbě
„Targeted“ therapy – aimed at the biological cause of a disease Imatinibem (Gleevec) suppresses cells belonging to mutated tumor clone – but does not get rid-off the body of the cause (all mutated cells).
Lasker prize for clinical research 2009 Brian J. Druker Nicholas Lydon Charles L. Sawyers
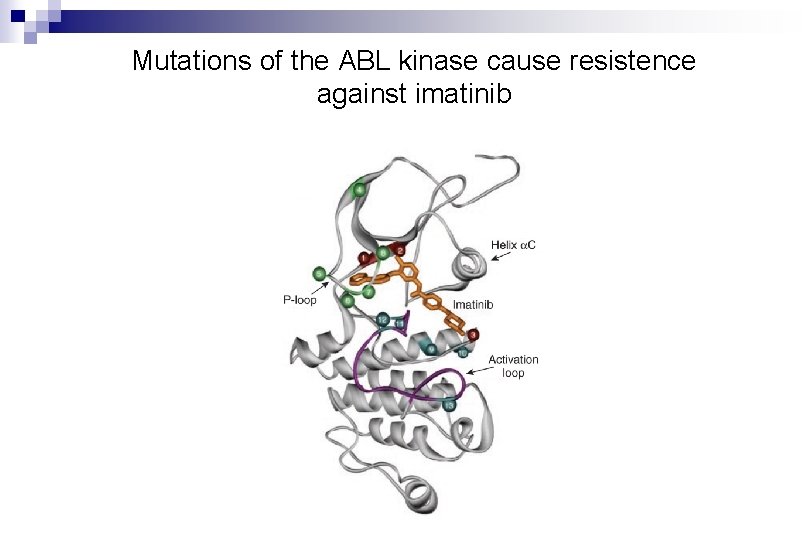
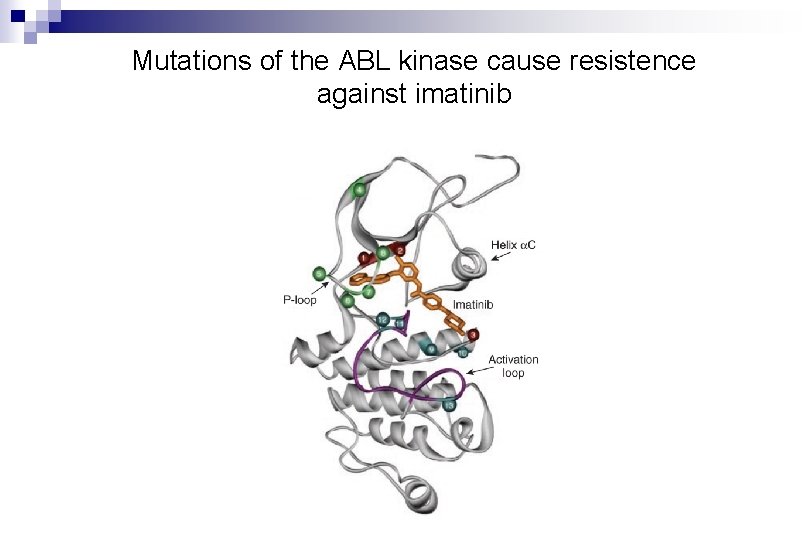
Mutations of the ABL kinase cause resistence against imatinib
Possible outcomes of CML complete remission n residual disease n relaps n resistance to therapy n blastic conversion (AML) n
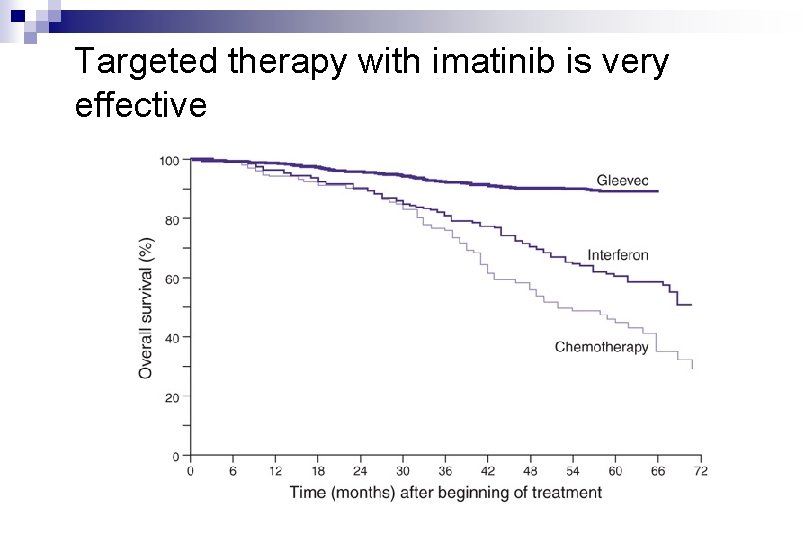
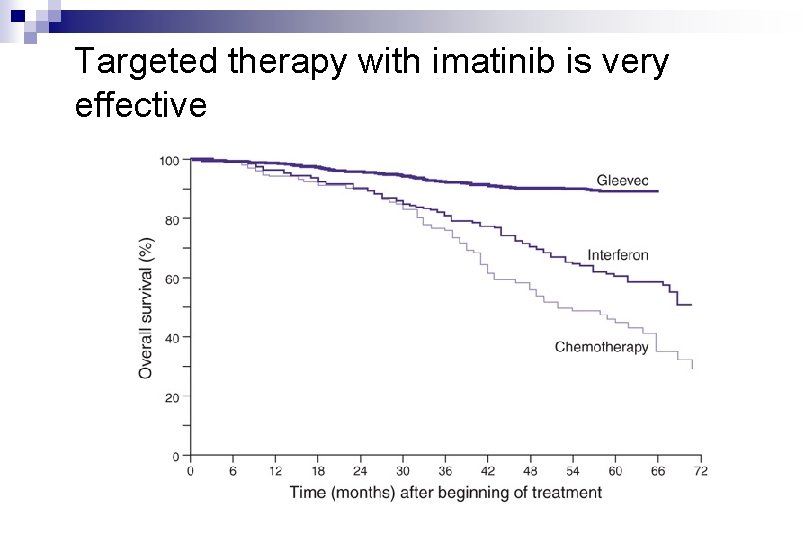
Targeted therapy with imatinib is very effective
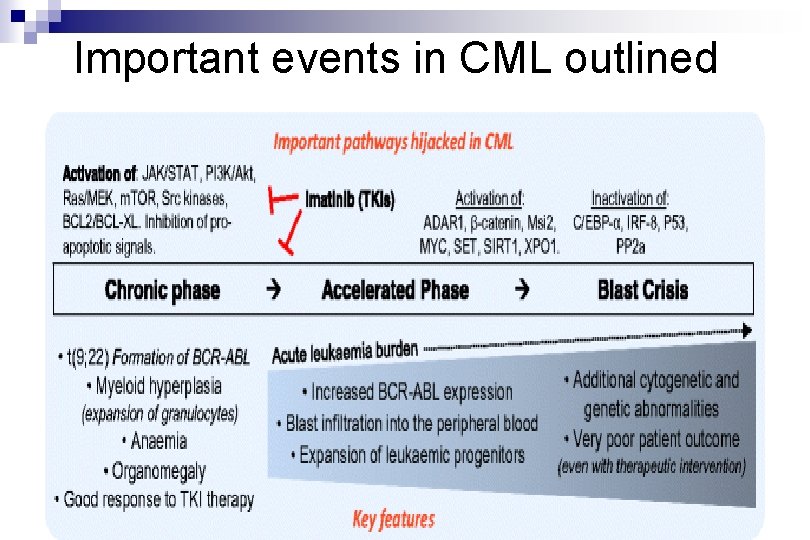
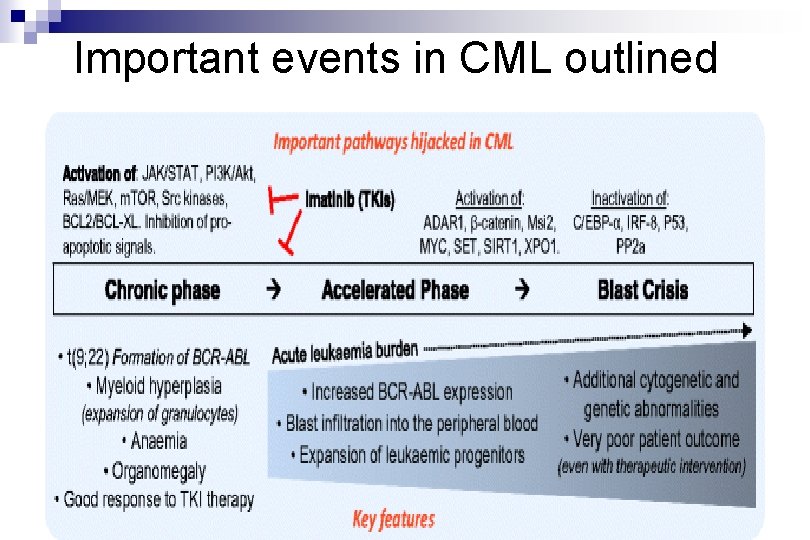
Important events in CML outlined
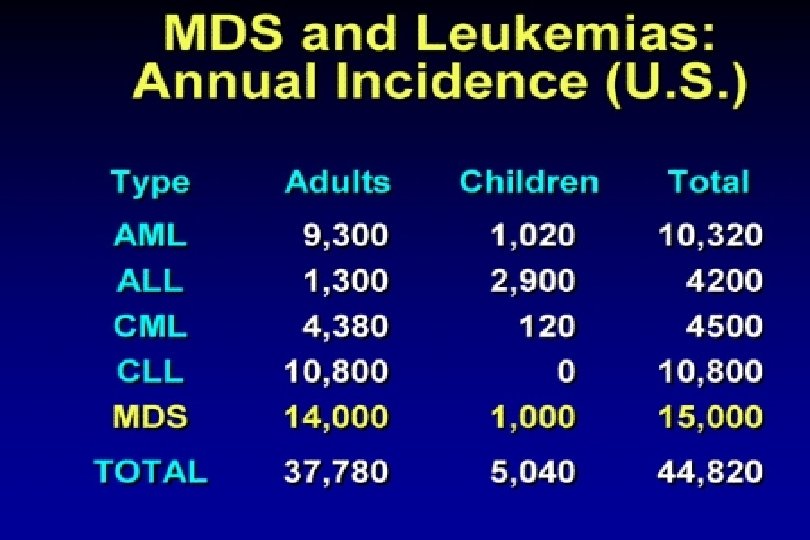
Acute myeloproliferative diseases n Acute myeloid leukemia (AML), several forms (myelogenous, myeloblastic are synonyms to myeloid) n Acute lymphocytic leukemia (ALL) … is lymphoproliferative disease (lymphoblastic is a synonym to lymphocytic)
Acute myleoid leukemia (AML)
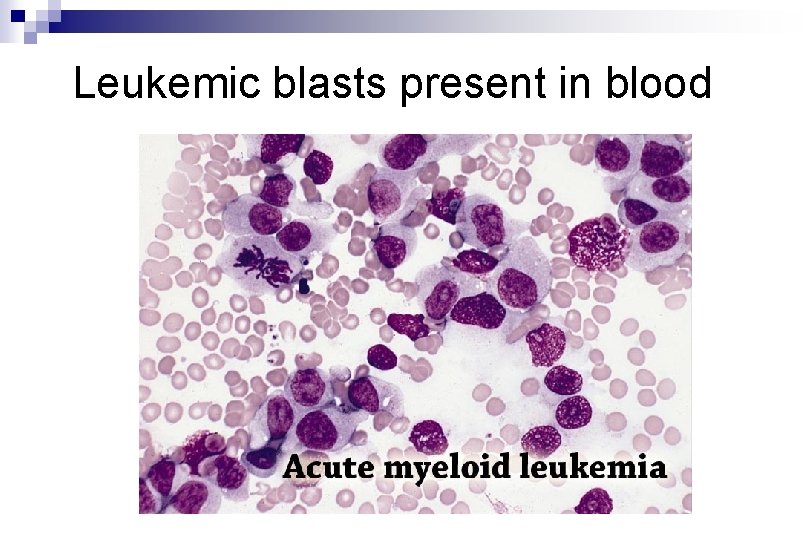
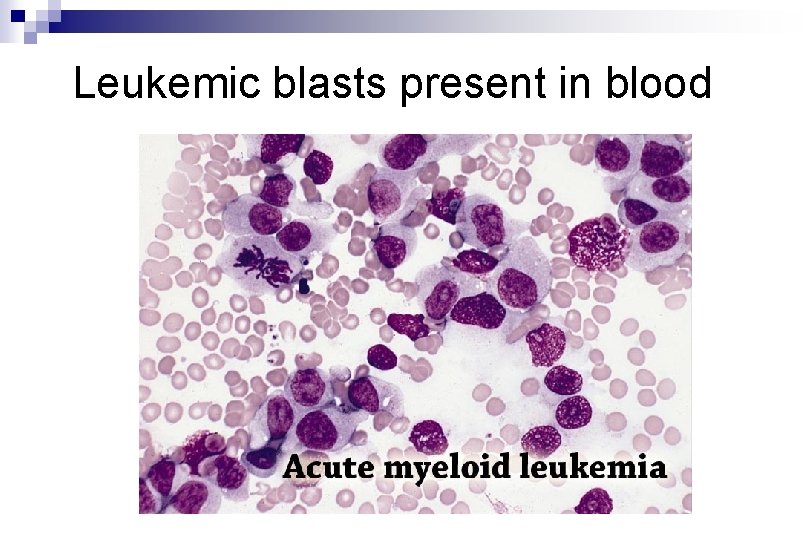
Leukemic blasts present in blood
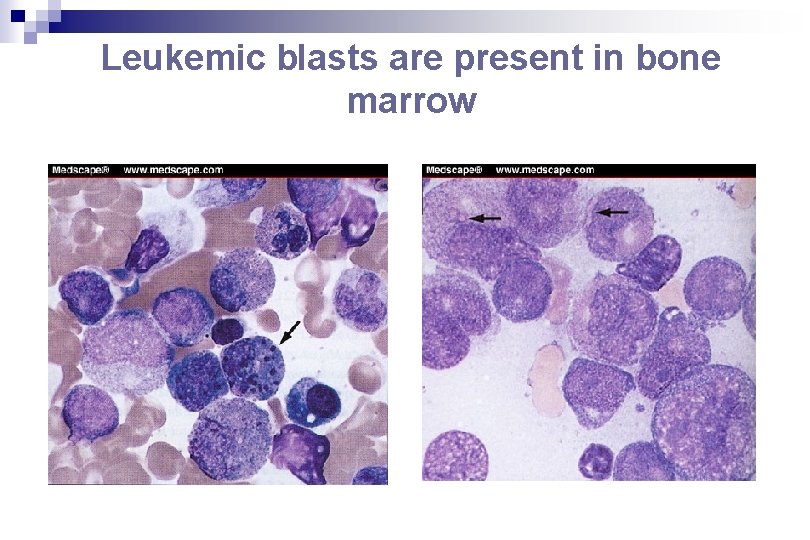
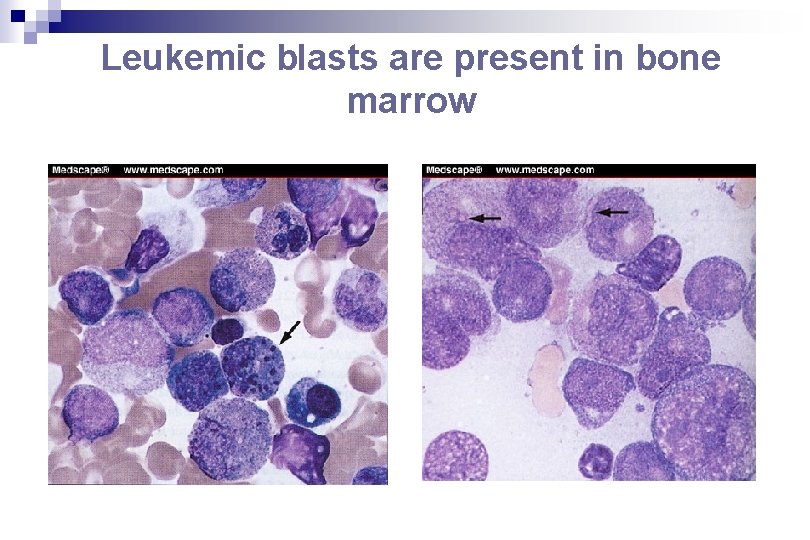
Leukemic blasts are present in bone marrow
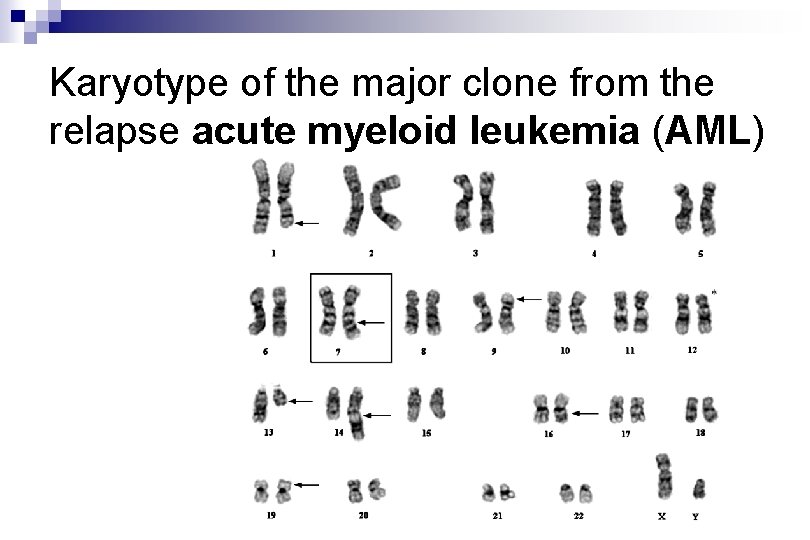
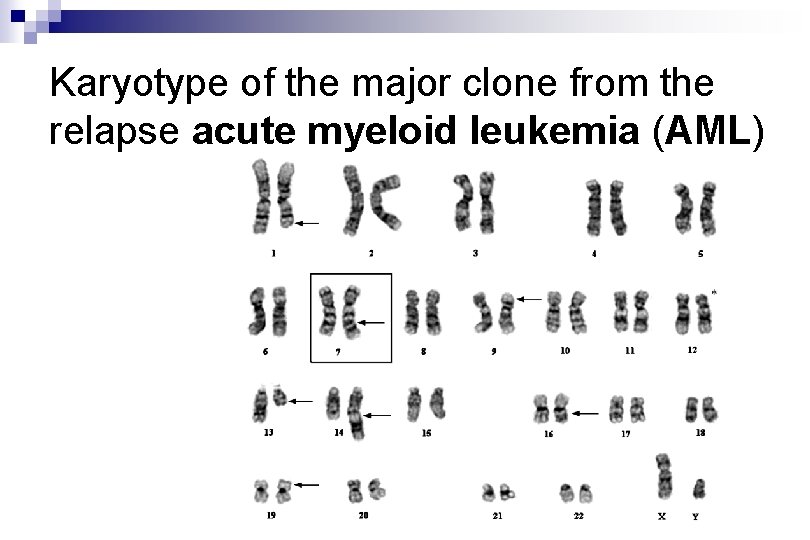
Karyotype of the major clone from the relapse acute myeloid leukemia (AML)
Acute Myeloid Leukemia (AML) - 8 clinical forms
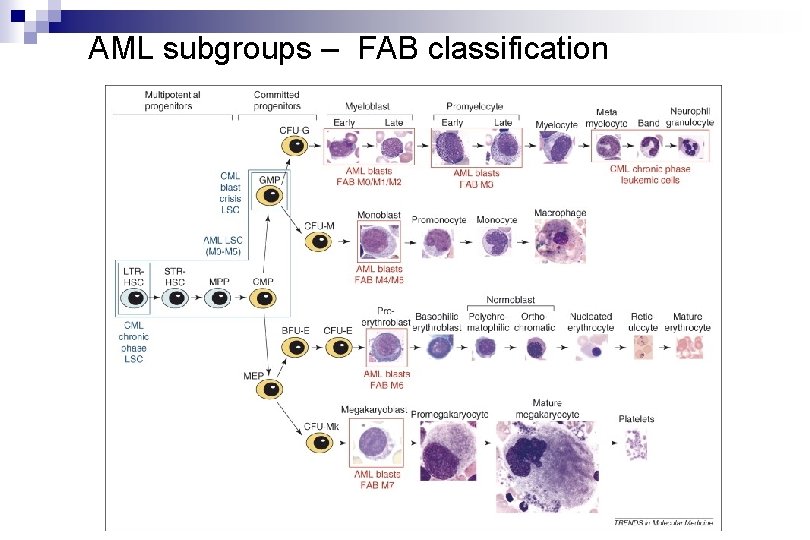
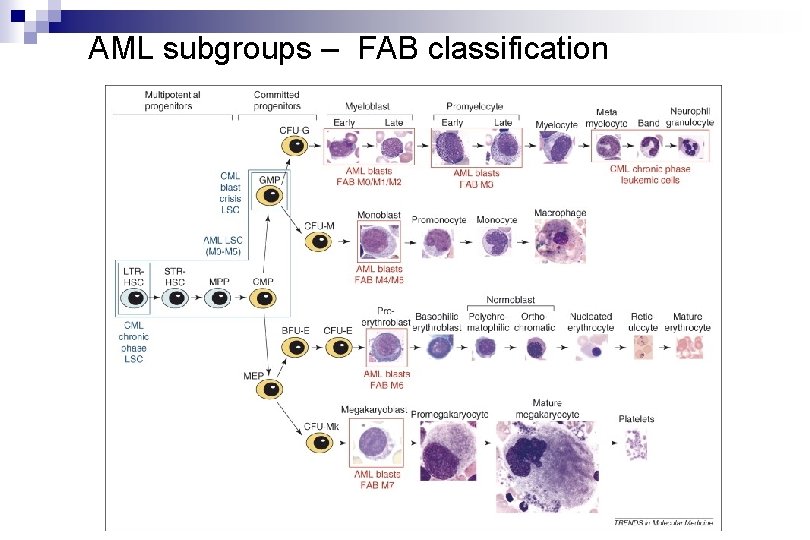
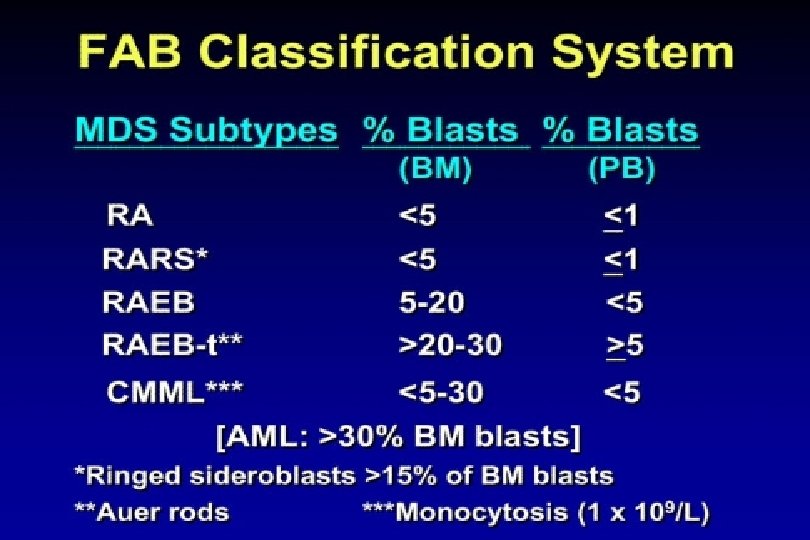
AML subgroups – FAB classification
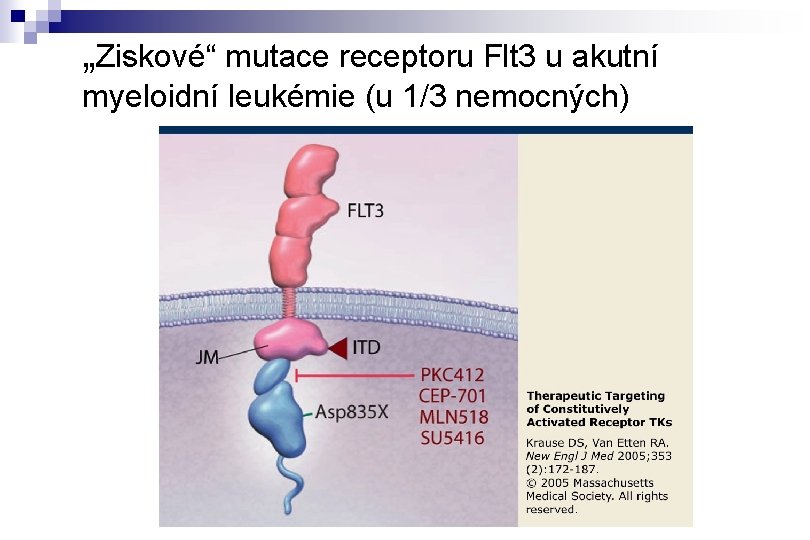
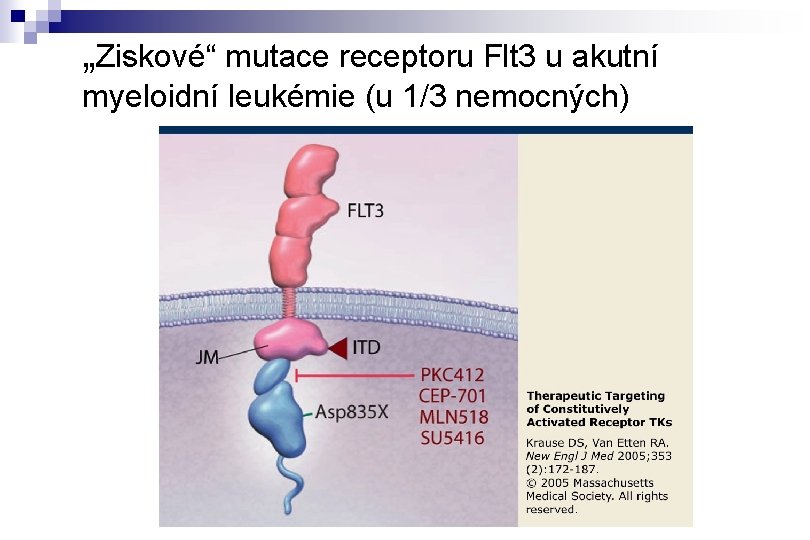
„Ziskové“ mutace receptoru Flt 3 u akutní myeloidní leukémie (u 1/3 nemocných)
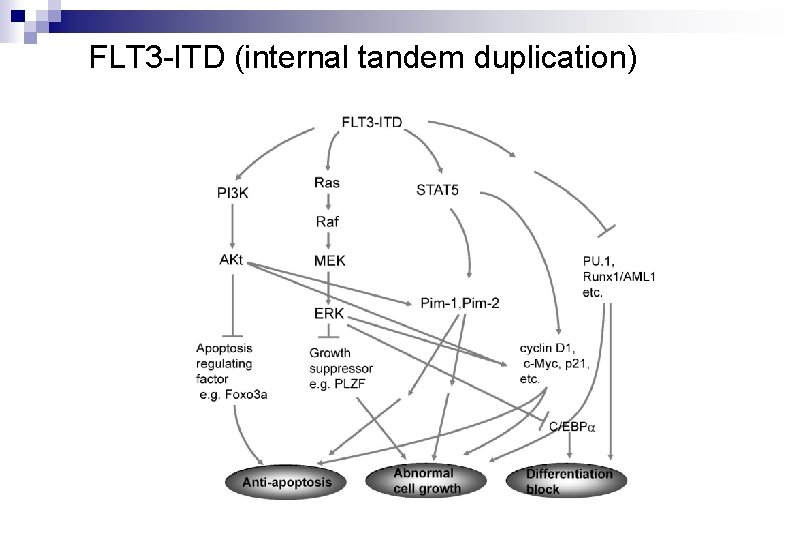
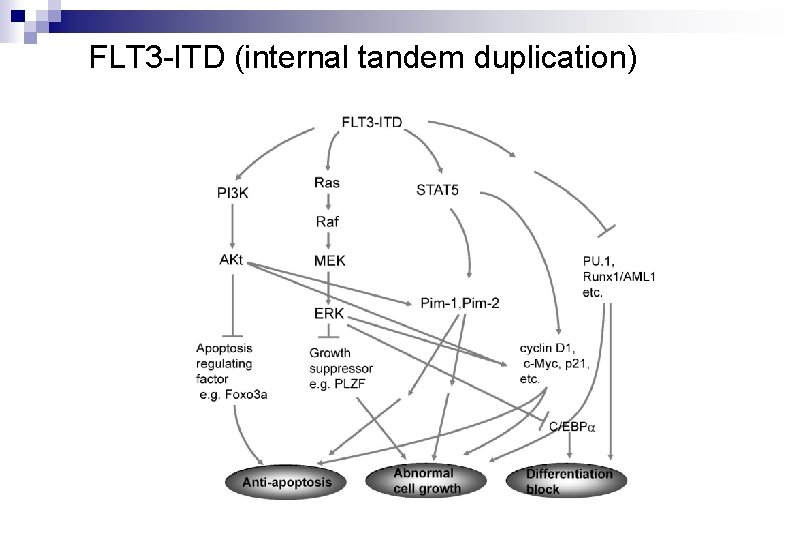
FLT 3 -ITD (internal tandem duplication)
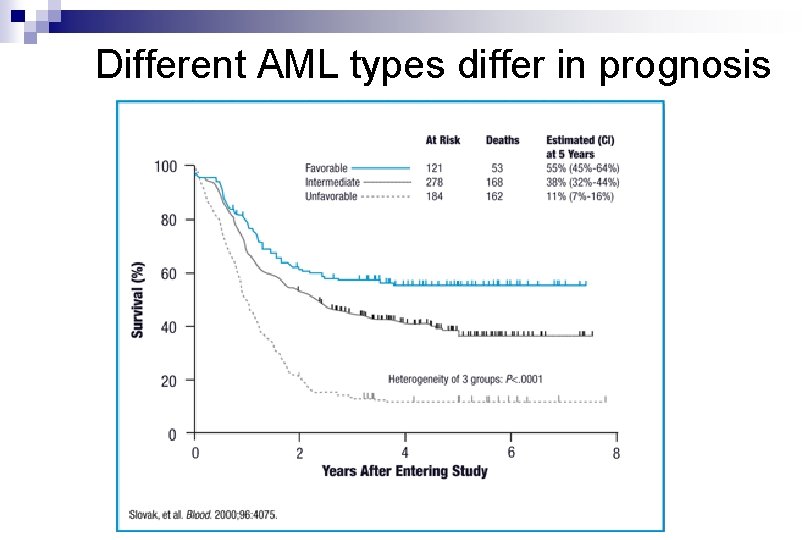
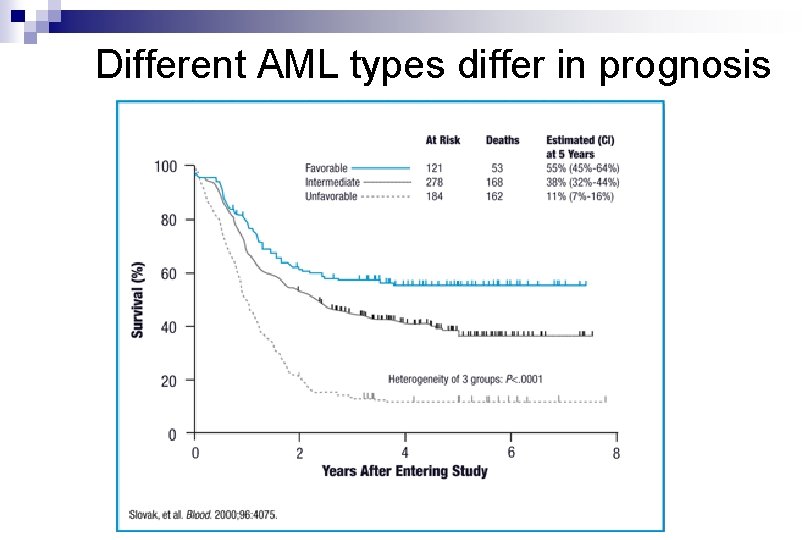
Different AML types differ in prognosis
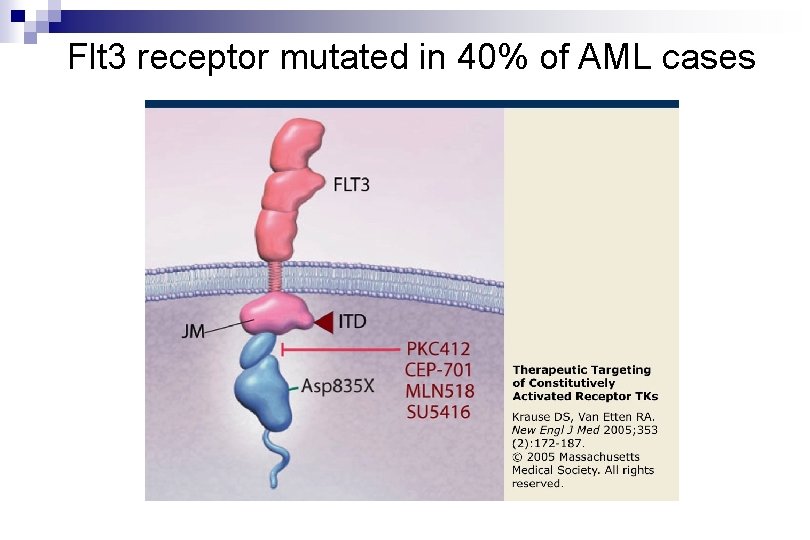
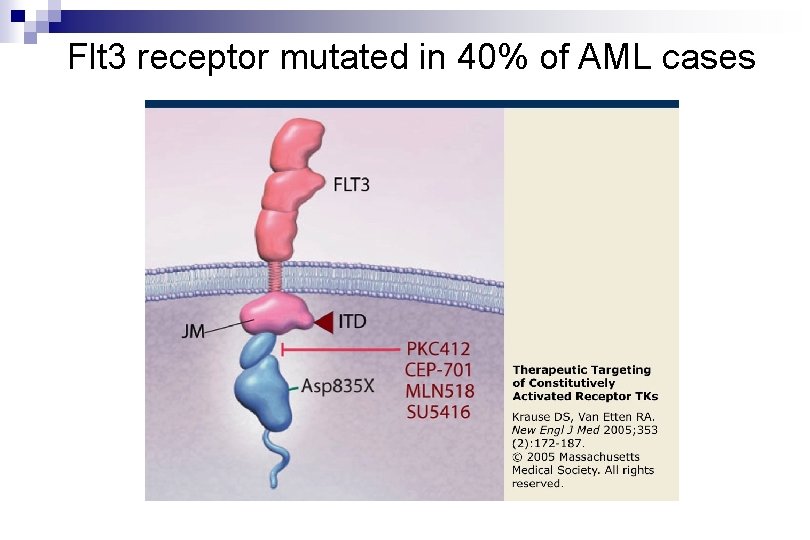
Flt 3 receptor mutated in 40% of AML cases
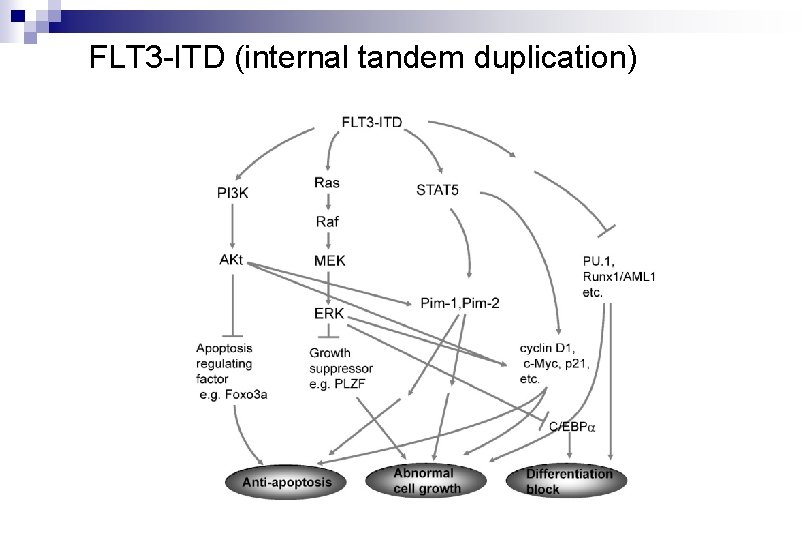
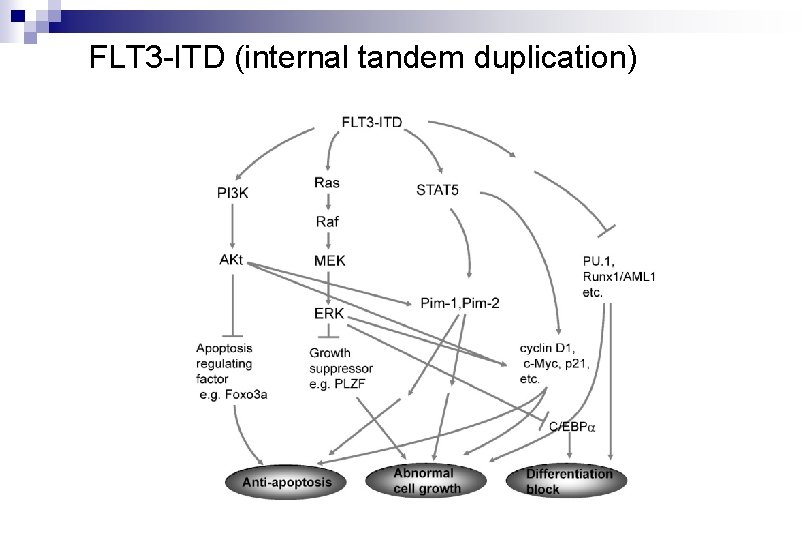
FLT 3 -ITD (internal tandem duplication)
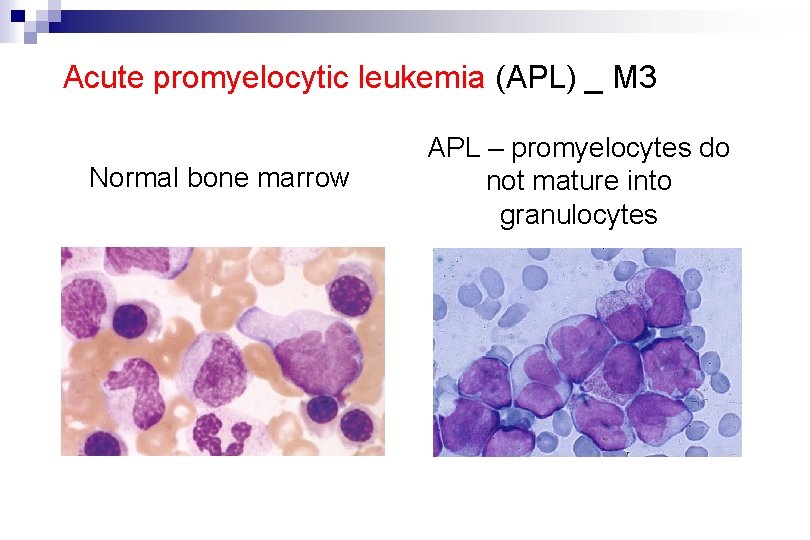
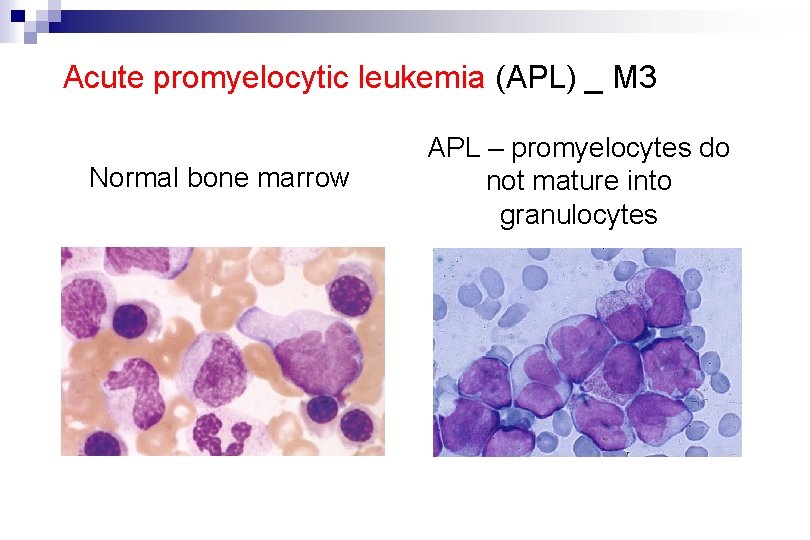
Acute promyelocytic leukemia (APL) _ M 3 Normal bone marrow APL – promyelocytes do not mature into granulocytes
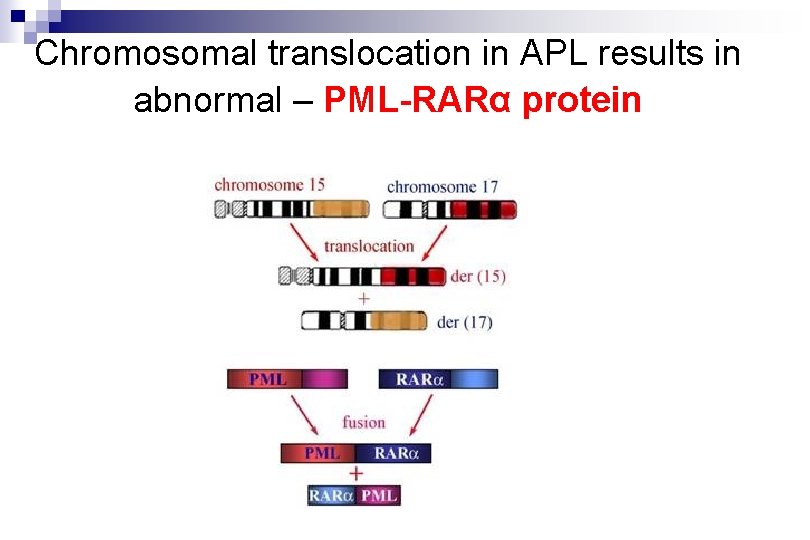
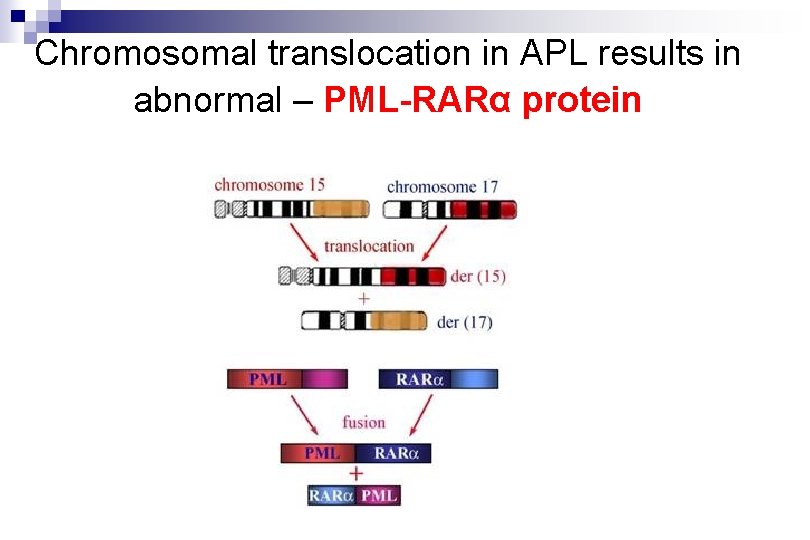
Chromosomal translocation in APL results in abnormal – PML-RARα protein
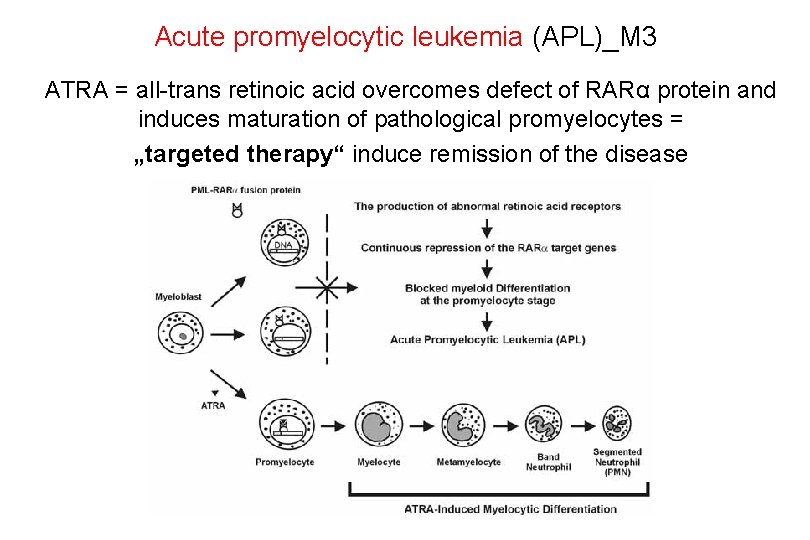
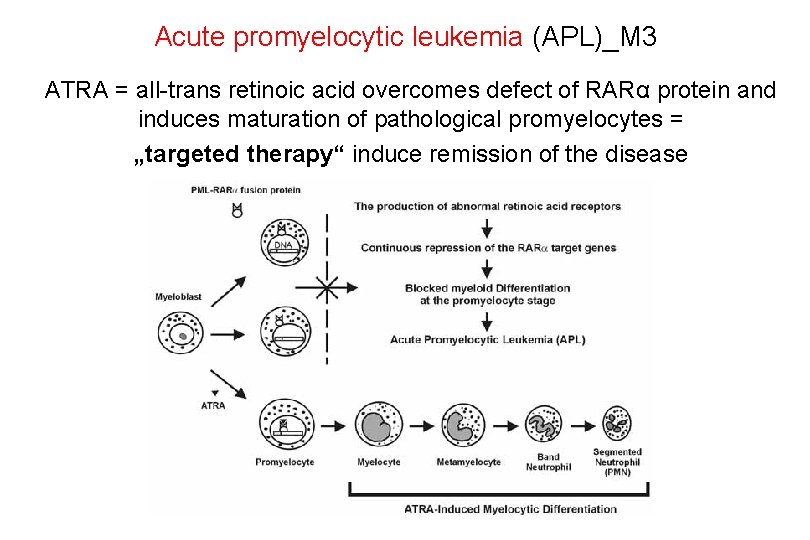
Acute promyelocytic leukemia (APL)_M 3 ATRA = all-trans retinoic acid overcomes defect of RARα protein and induces maturation of pathological promyelocytes = „targeted therapy“ induce remission of the disease
Transplantation of hematopoietic stem cells („Bone Marrow Transplantation“) is the only „causative therapy“ for AML
END OF THE LECTURE
 What is myeloproliferative disorder
What is myeloproliferative disorder Scheme of postembryonic hematopoiesis - lymphocytopoiesis
Scheme of postembryonic hematopoiesis - lymphocytopoiesis Entrocyte
Entrocyte Mapc cells
Mapc cells Polycythemia
Polycythemia Nature reviews immunology
Nature reviews immunology Myeloid metaplasia
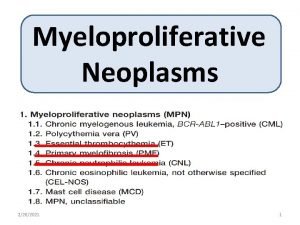
Myeloid metaplasia Myeloproliferative neoplams
Myeloproliferative neoplams Drugs causing leukocytosis
Drugs causing leukocytosis 2282021
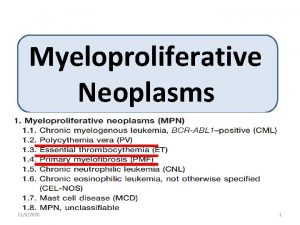
2282021 Myeloproliferative neoplasm
Myeloproliferative neoplasm Myeloproliferative disease
Myeloproliferative disease Hypertensive urgency vs emergency
Hypertensive urgency vs emergency Calcium channel blockers examples
Calcium channel blockers examples Malignant neoplasm of the blood-forming organs
Malignant neoplasm of the blood-forming organs Malignant neuroleptic syndrome
Malignant neuroleptic syndrome Neoplasia
Neoplasia Neuroleptic malignant syndrome
Neuroleptic malignant syndrome Histological features of malignant cells
Histological features of malignant cells Malignant mesothelioma
Malignant mesothelioma Malignant hypertension management
Malignant hypertension management Nail body
Nail body Cachexia
Cachexia Hypertensive encephalopathy
Hypertensive encephalopathy Perdida de polaridad celular
Perdida de polaridad celular Peter hino md
Peter hino md Catatonic behavior example
Catatonic behavior example Malignant hypertension ppt
Malignant hypertension ppt Background
Background Benign vs malignant
Benign vs malignant Adenocarcinoma
Adenocarcinoma Kitwoods flower model
Kitwoods flower model Emanuel onica
Emanuel onica Emanuel komnen
Emanuel komnen Egg för emanuel
Egg för emanuel Emanuel lehman
Emanuel lehman Elektro emanuel
Elektro emanuel Emanuel kittl
Emanuel kittl Ziekte van asherman
Ziekte van asherman Emanuel kanti
Emanuel kanti Rebecca gerstein
Rebecca gerstein Bernstein memory of paper
Bernstein memory of paper Handlungskompetenzorientierung
Handlungskompetenzorientierung Emanuel dohi
Emanuel dohi Evanyely zamorano
Evanyely zamorano Francois emanuel fodere
Francois emanuel fodere Liceul teologic baptist emanuel
Liceul teologic baptist emanuel George washington crossing the delaware painting
George washington crossing the delaware painting Emanuel timoni
Emanuel timoni Rebekah emanuel
Rebekah emanuel Emanuel coman tcd
Emanuel coman tcd Emanuel leutze westward the course of empire
Emanuel leutze westward the course of empire Dileme etice in cercetare
Dileme etice in cercetare Separacion entre viguetas
Separacion entre viguetas Chapter 18 eating and feeding disorders
Chapter 18 eating and feeding disorders Cluster b personality disorders
Cluster b personality disorders Mild neurocognitive disorder
Mild neurocognitive disorder Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Disorder of skin and subcutaneous tissue adalah
Disorder of skin and subcutaneous tissue adalah Cluster c
Cluster c Chapter 47 urinary and reproductive disorders
Chapter 47 urinary and reproductive disorders Icd x anxiety disorders
Icd x anxiety disorders Ap psychology chapter 15 psychological disorders
Ap psychology chapter 15 psychological disorders Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Managing weight and eating behaviors
Managing weight and eating behaviors Salivary gland disorders classification
Salivary gland disorders classification Egodystonic
Egodystonic Looney tunes speech impediments
Looney tunes speech impediments Dissociative disorders
Dissociative disorders Unit 14 physiological disorders
Unit 14 physiological disorders The flinders model
The flinders model Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 Body fluid
Body fluid In fruit flies white eyes is a sex linked recessive trait
In fruit flies white eyes is a sex linked recessive trait Mnt for eating disorders
Mnt for eating disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Sleep disorders
Sleep disorders Purine disorders
Purine disorders Schizoid personality disorder
Schizoid personality disorder