Stem Cell A cell with a unique capacity

- Slides: 41
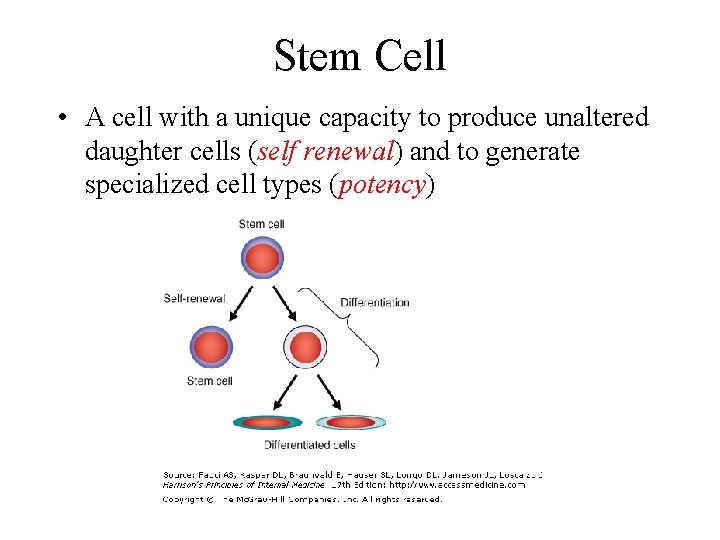
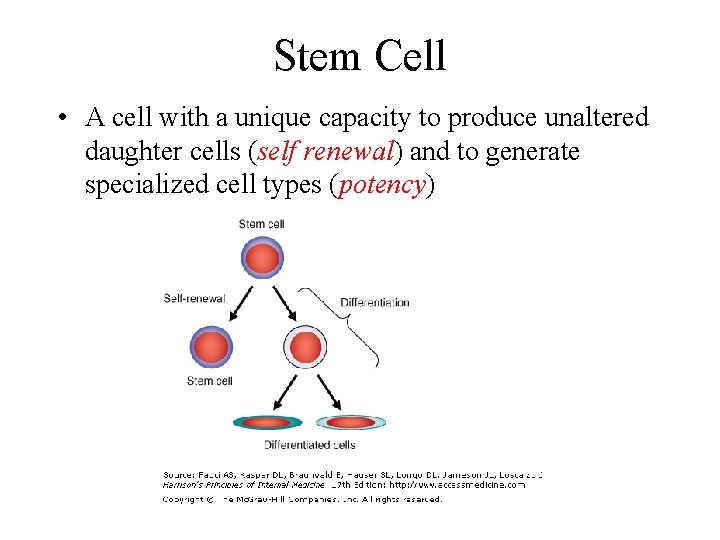
Stem Cell • A cell with a unique capacity to produce unaltered daughter cells (self renewal) and to generate specialized cell types (potency)
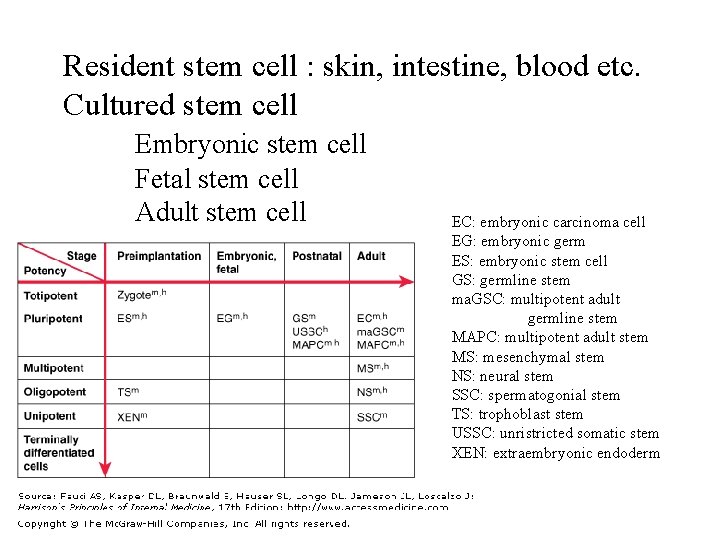
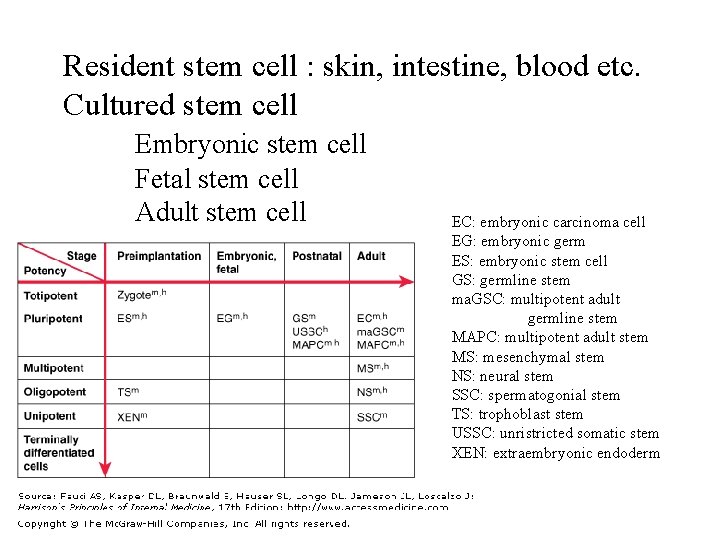
Resident stem cell : skin, intestine, blood etc. Cultured stem cell Embryonic stem cell Fetal stem cell Adult stem cell EC: embryonic carcinoma cell EG: embryonic germ ES: embryonic stem cell GS: germline stem ma. GSC: multipotent adult germline stem MAPC: multipotent adult stem MS: mesenchymal stem NS: neural stem SSC: spermatogonial stem TS: trophoblast stem USSC: unristricted somatic stem XEN: extraembryonic endoderm
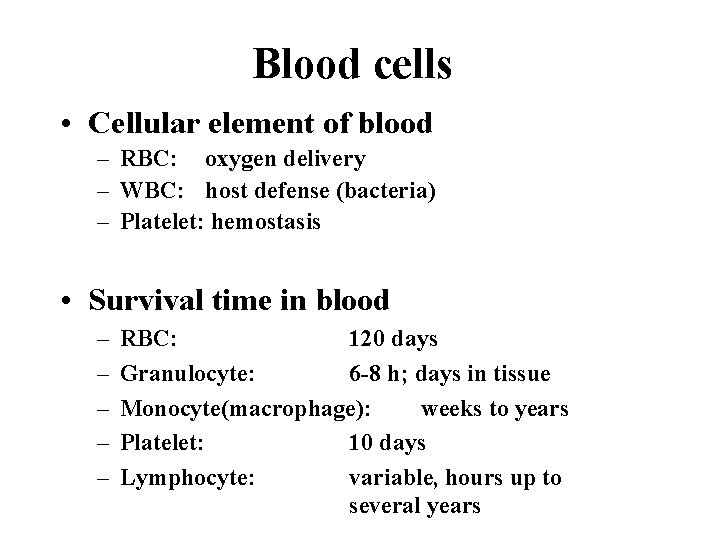
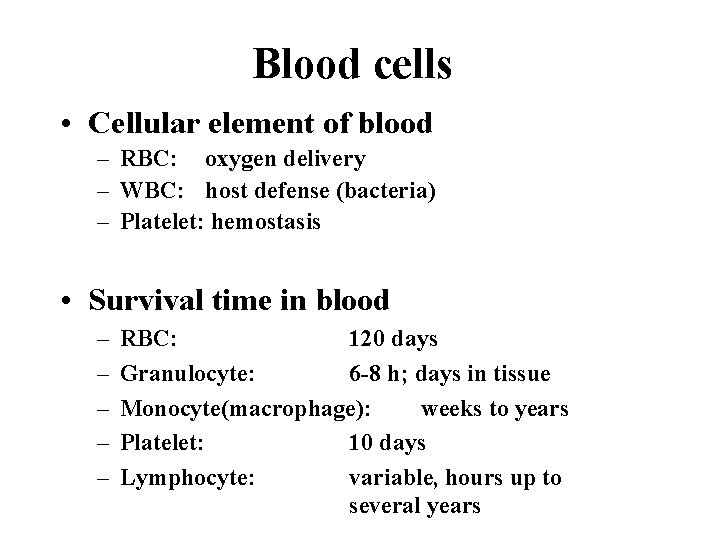
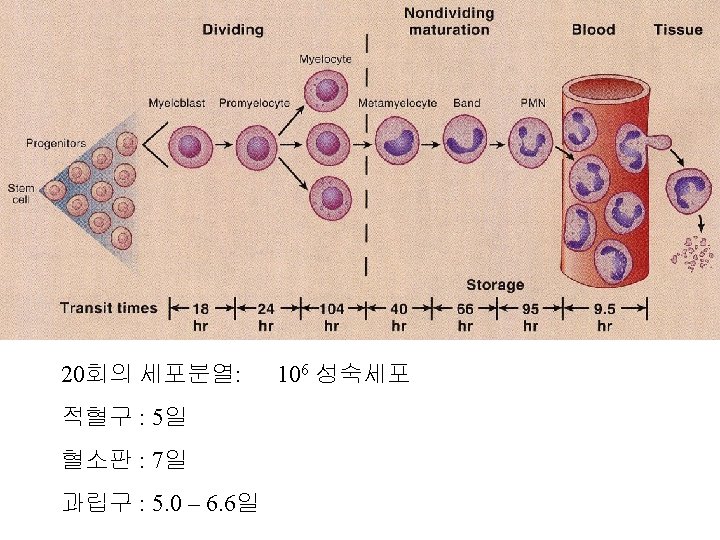
Blood cells • Cellular element of blood – RBC: oxygen delivery – WBC: host defense (bacteria) – Platelet: hemostasis • Survival time in blood – – – RBC: 120 days Granulocyte: 6 -8 h; days in tissue Monocyte(macrophage): weeks to years Platelet: 10 days Lymphocyte: variable, hours up to several years
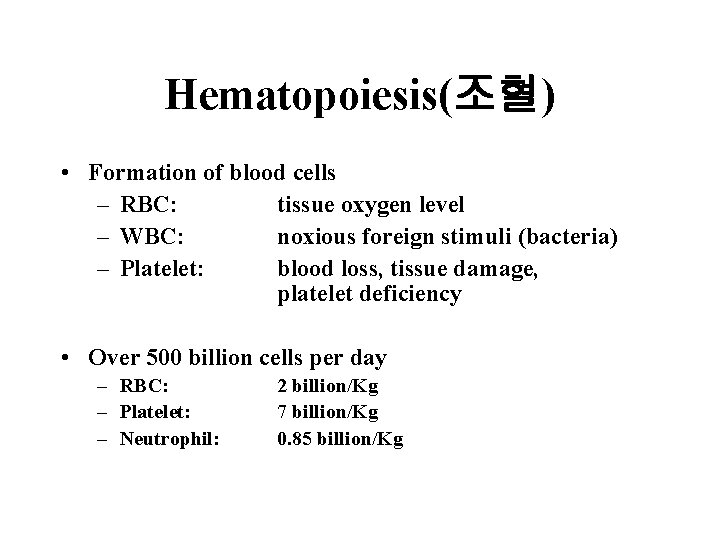
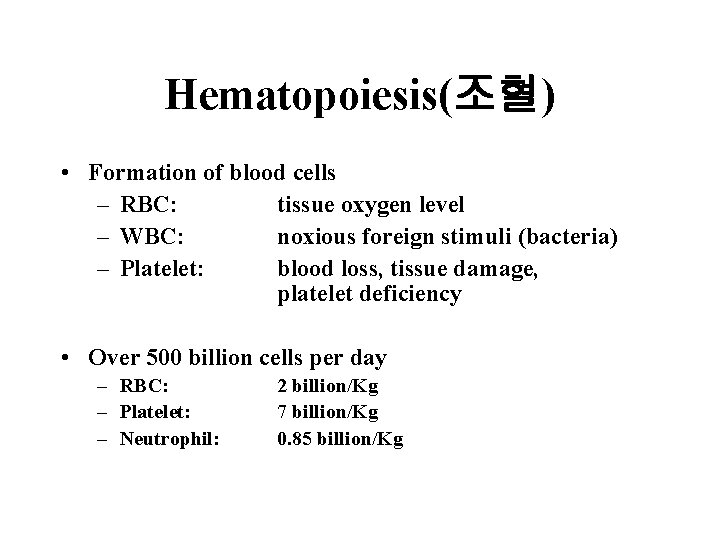
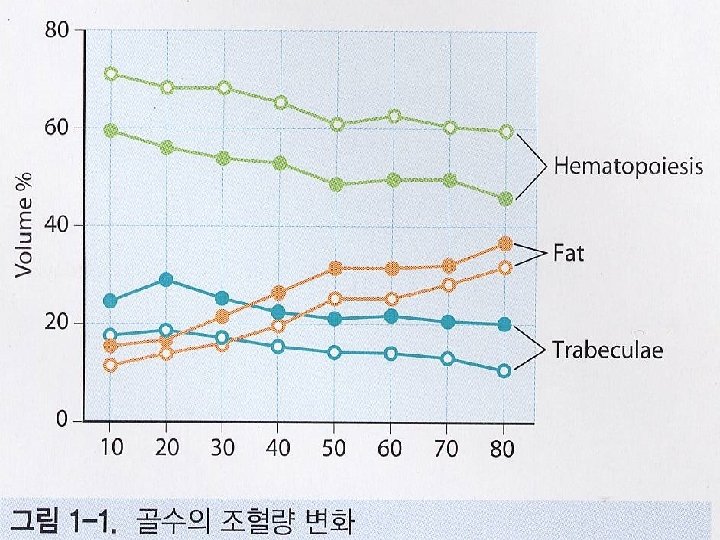
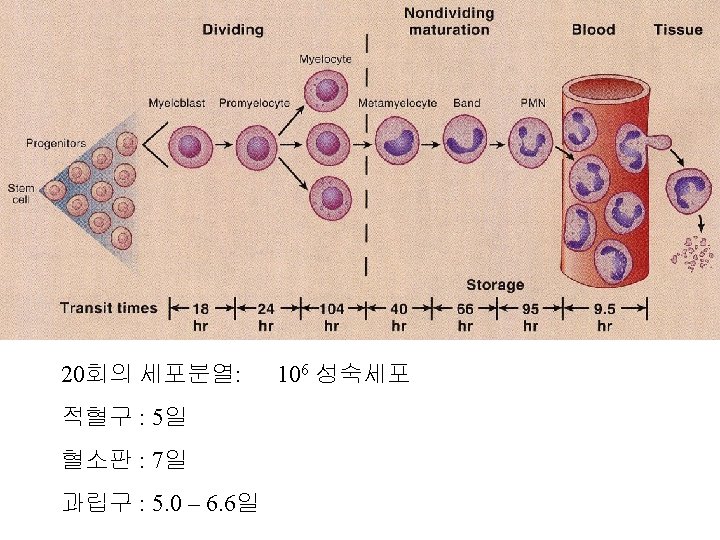
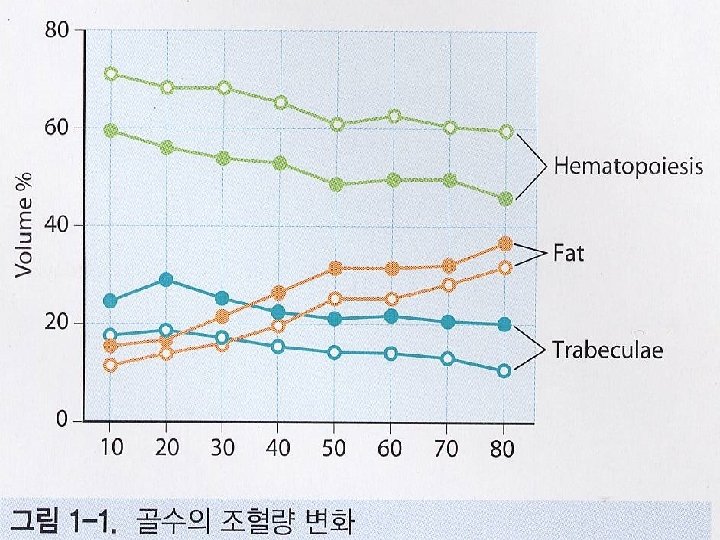
Hematopoiesis(조혈) • Formation of blood cells – RBC: tissue oxygen level – WBC: noxious foreign stimuli (bacteria) – Platelet: blood loss, tissue damage, platelet deficiency • Over 500 billion cells per day – RBC: – Platelet: – Neutrophil: 2 billion/Kg 7 billion/Kg 0. 85 billion/Kg
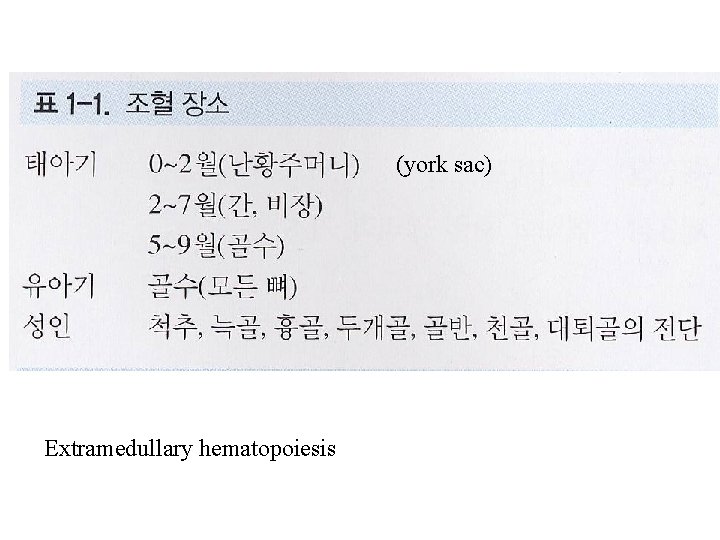
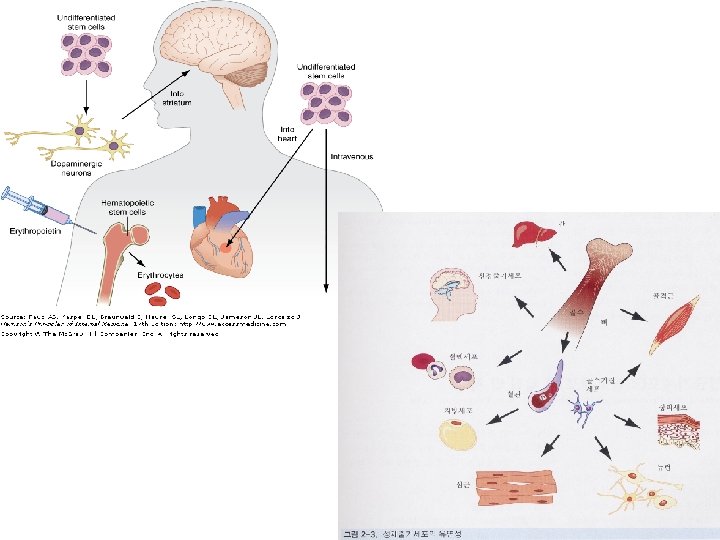
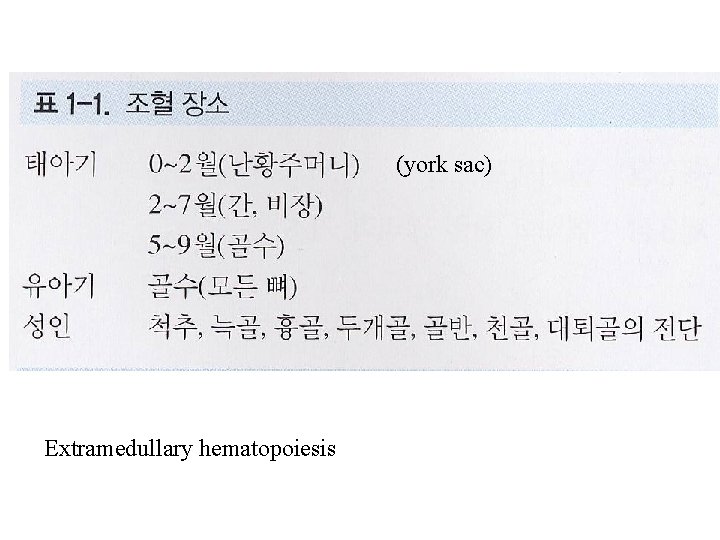
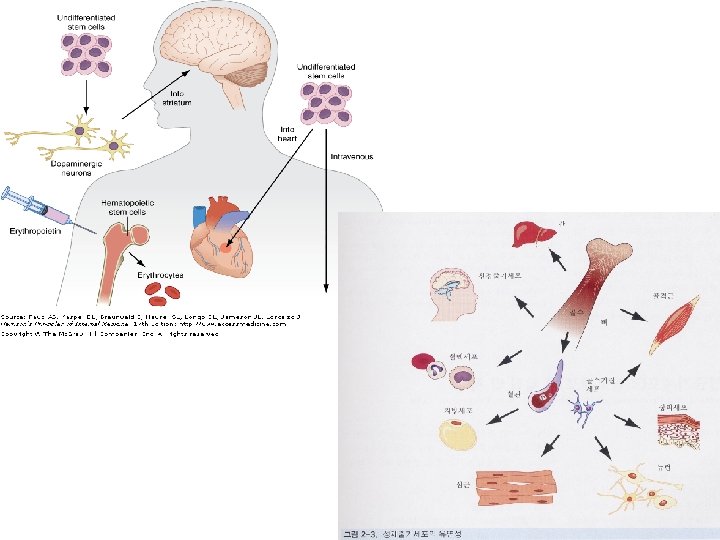
(york sac) Extramedullary hematopoiesis
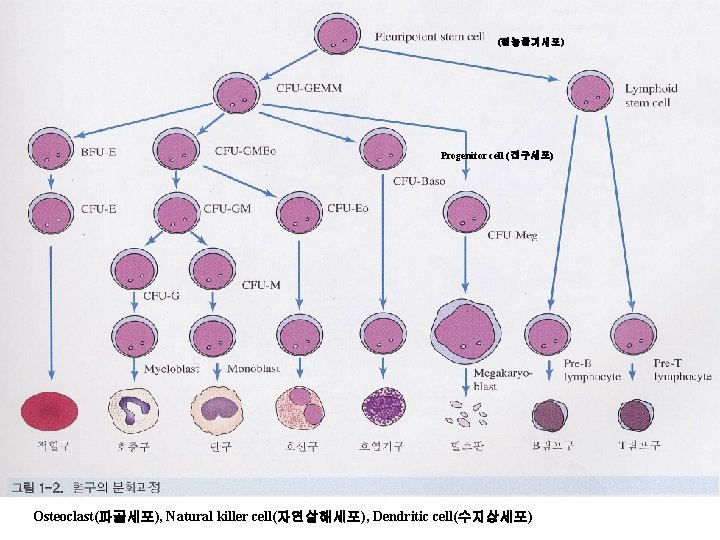
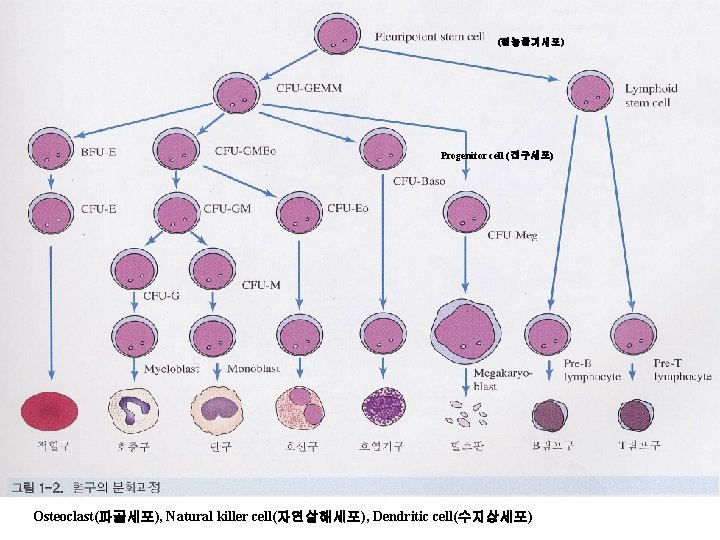
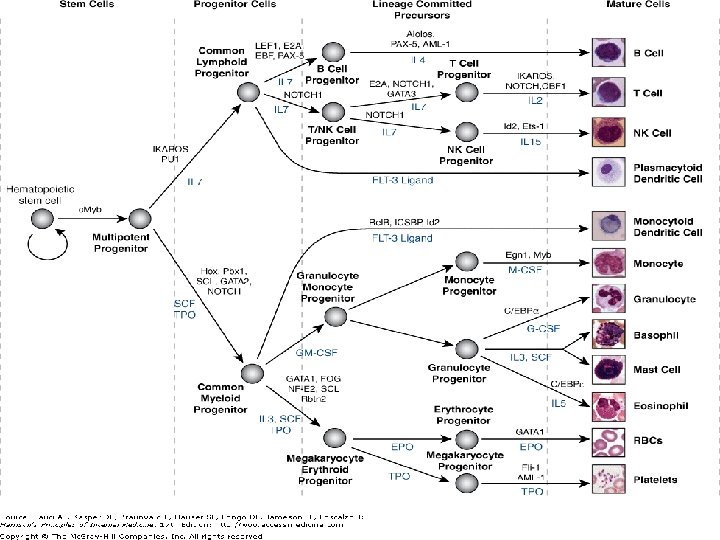
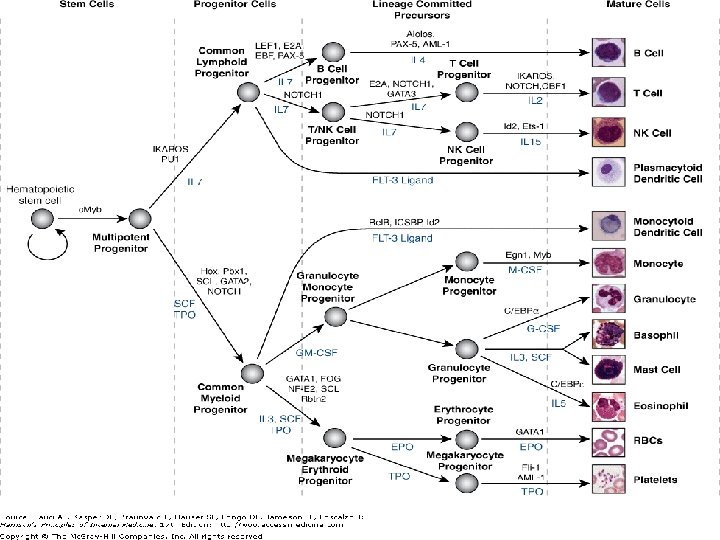
(원능줄기세포) Progenitor cell (전구세포) Osteoclast(파골세포), Natural killer cell(자연살해세포), Dendritic cell(수지상세포)
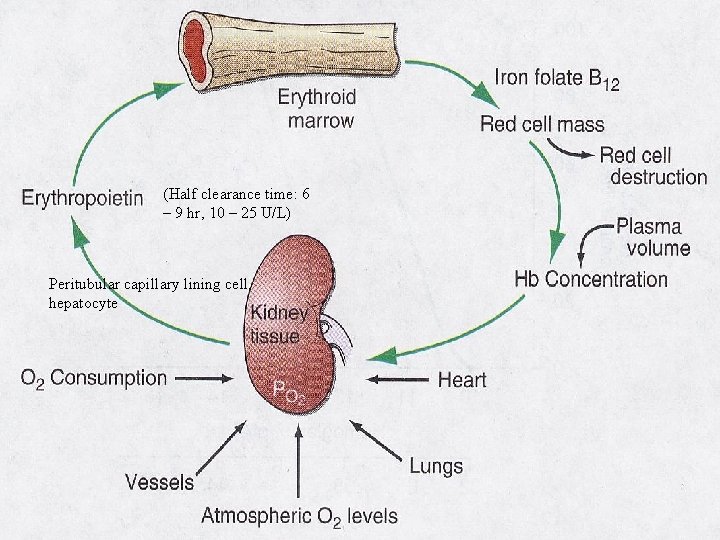
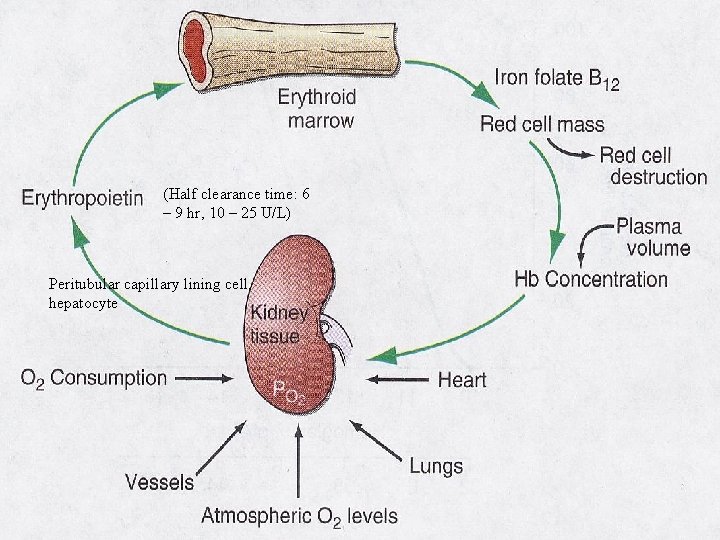
(Half clearance time: 6 – 9 hr, 10 – 25 U/L) Peritubular capillary lining cell, hepatocyte
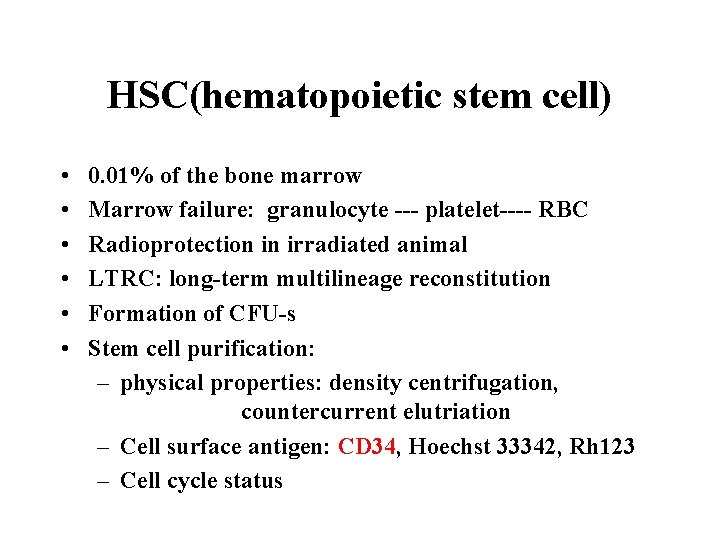
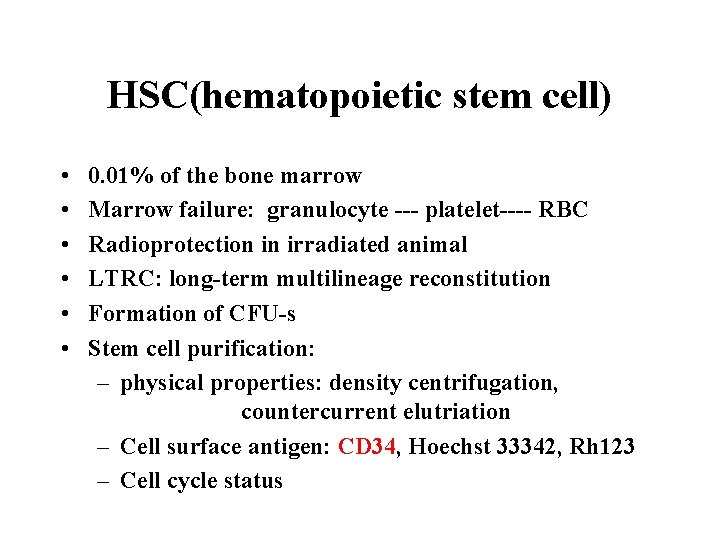
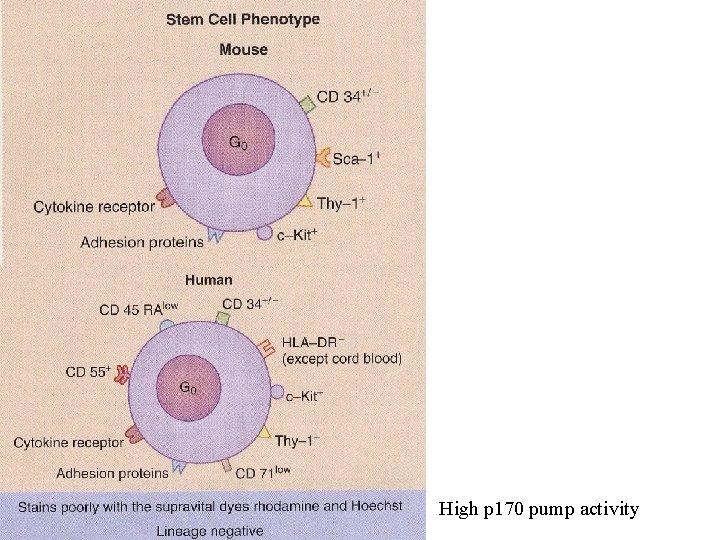
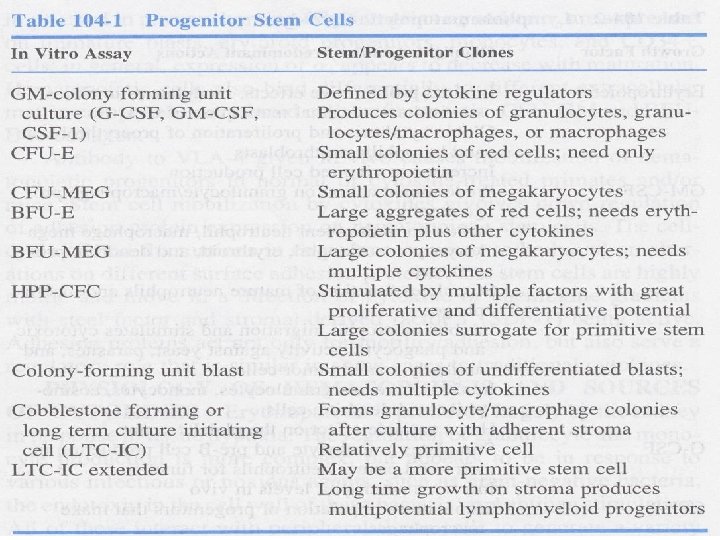
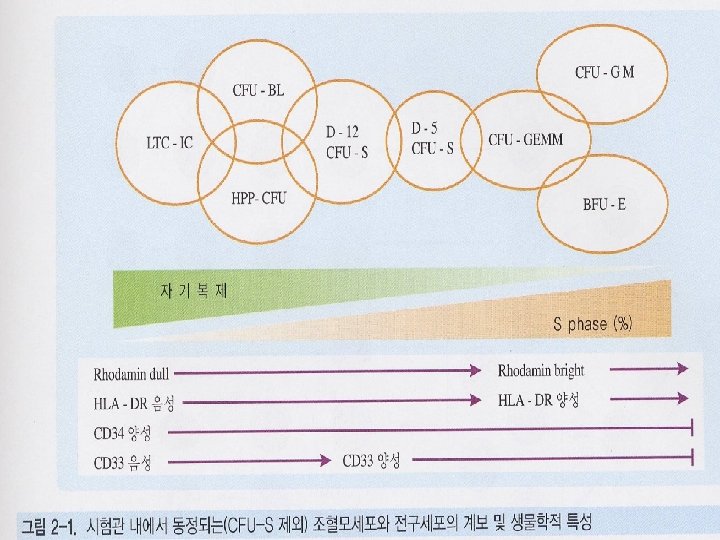
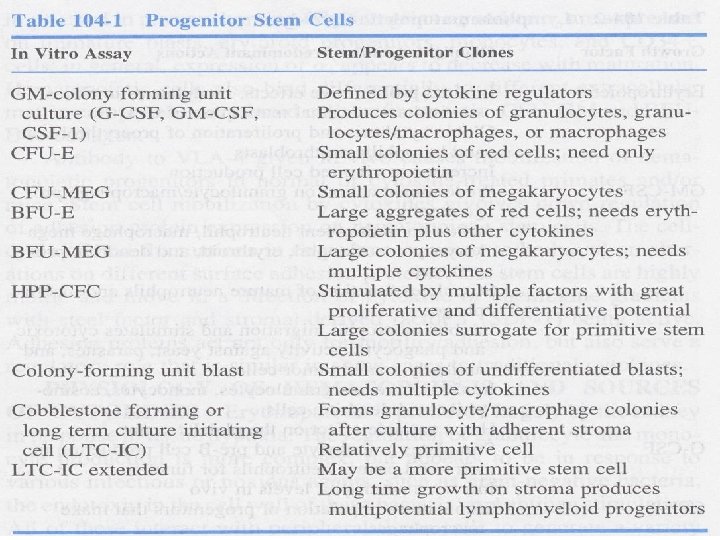
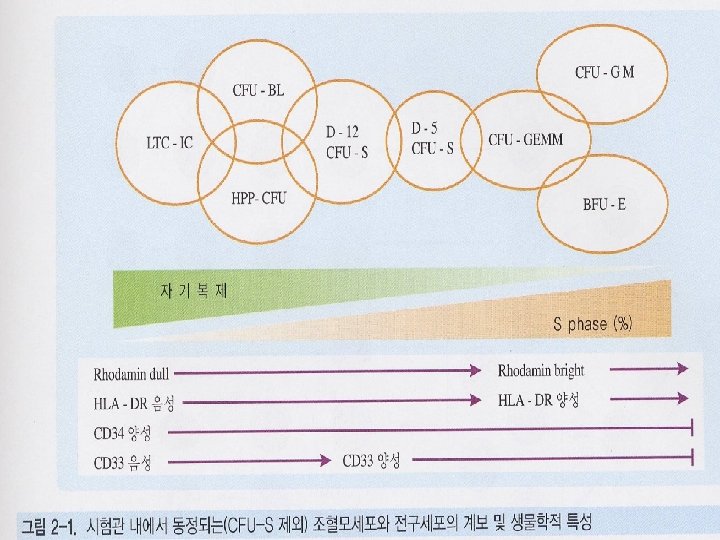
HSC(hematopoietic stem cell) • • • 0. 01% of the bone marrow Marrow failure: granulocyte --- platelet---- RBC Radioprotection in irradiated animal LTRC: long-term multilineage reconstitution Formation of CFU-s Stem cell purification: – physical properties: density centrifugation, countercurrent elutriation – Cell surface antigen: CD 34, Hoechst 33342, Rh 123 – Cell cycle status
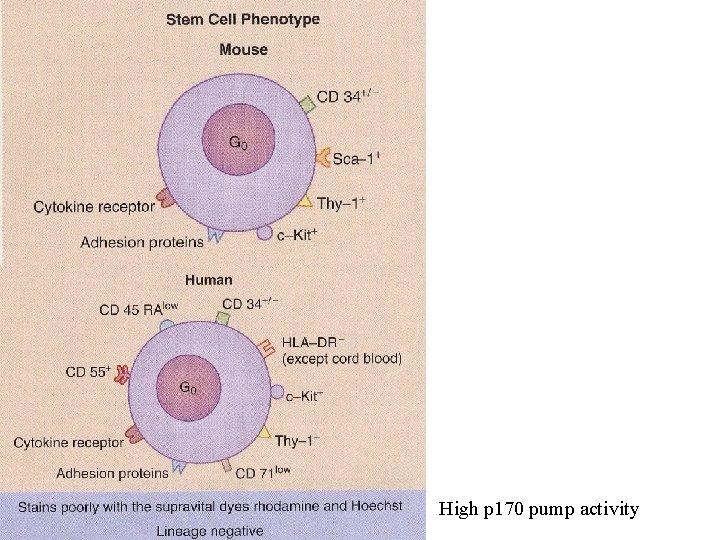
High p 170 pump activity
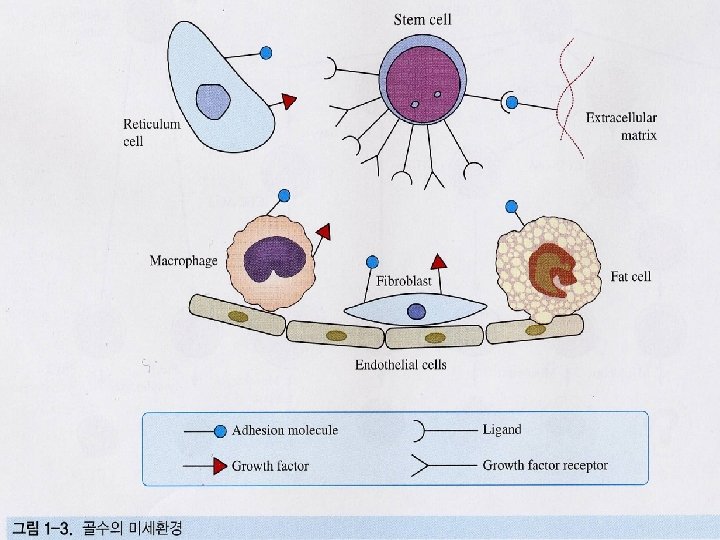
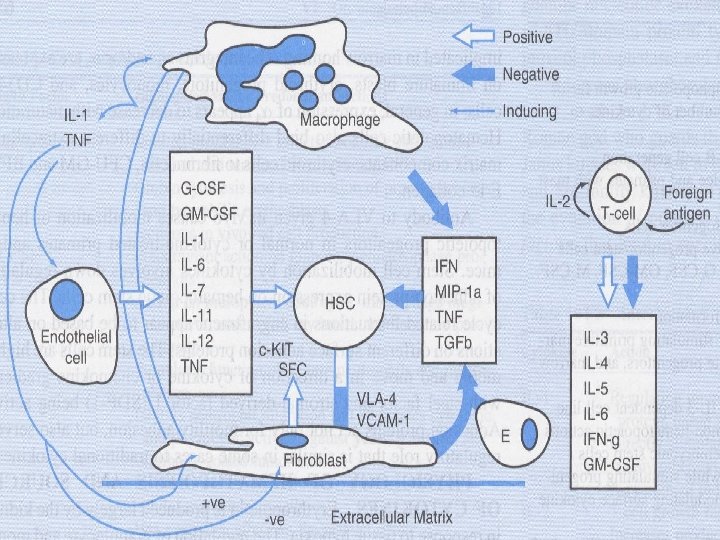
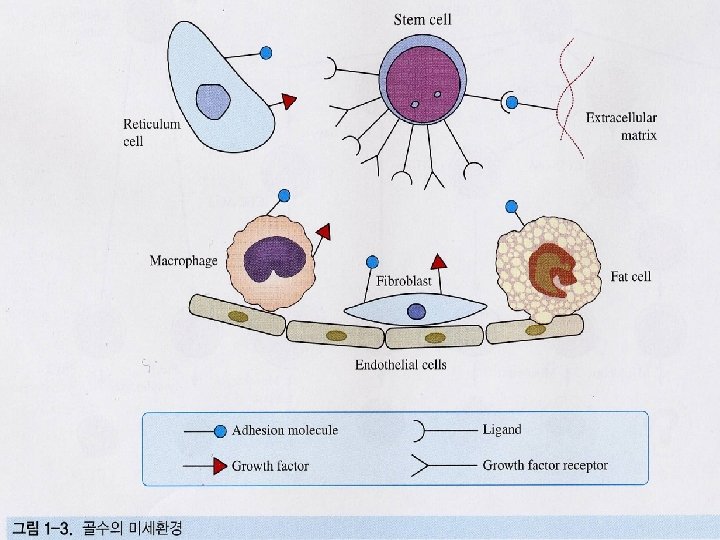
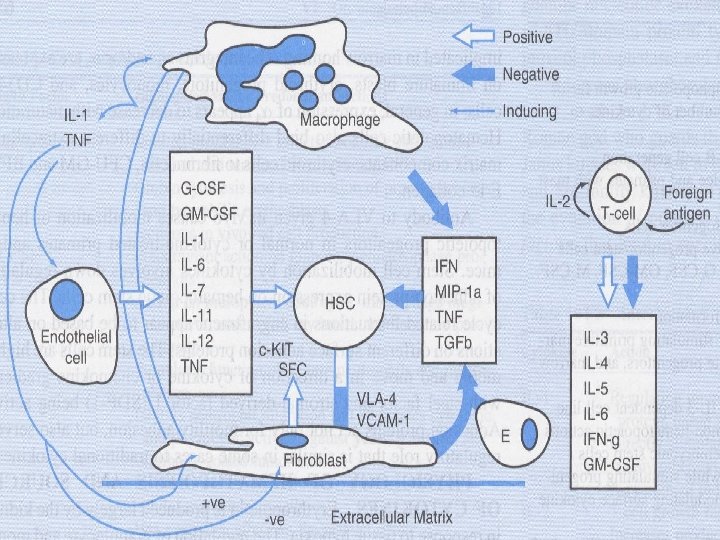
Hematopoietic microenvironment • Specific positional effect: product of microenvironment • adipocytes, fibroblastoid cells, reticulo-endotheloid cells, macrophages, T-cells • Cell adhesion molecules, cytokines • Extracellular matrix: collagens, laminin, fibronectin, proteoglycan
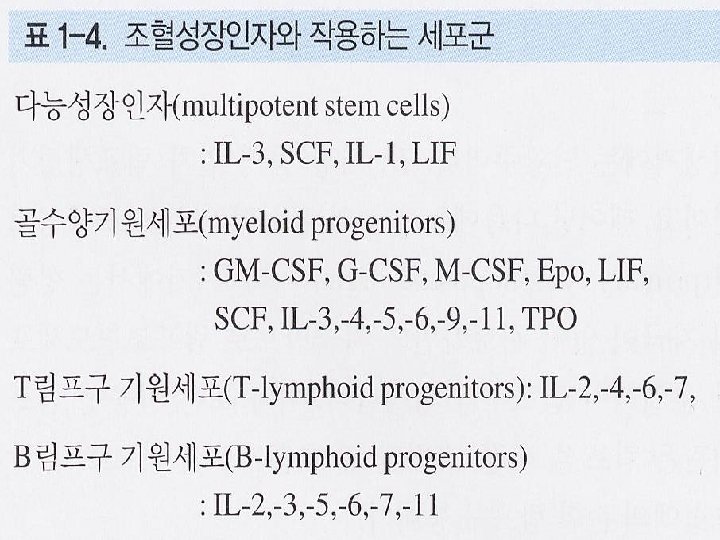
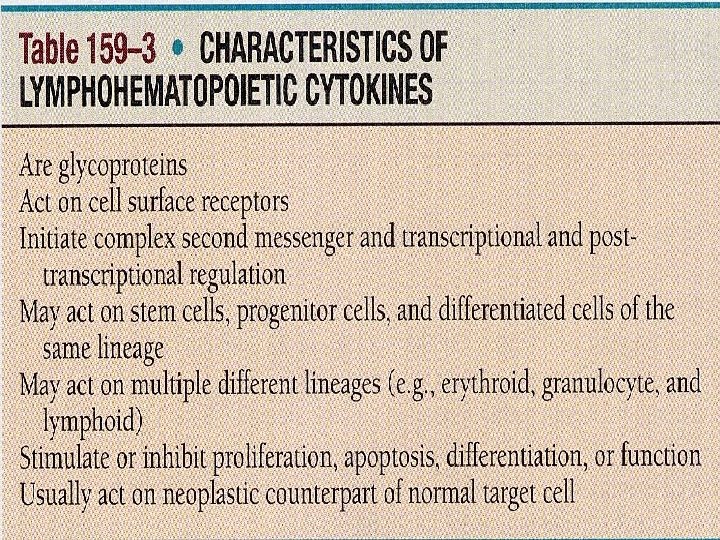
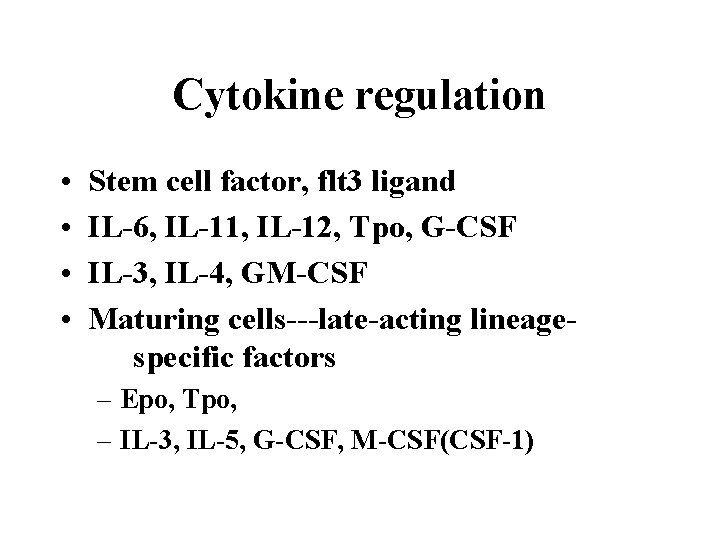
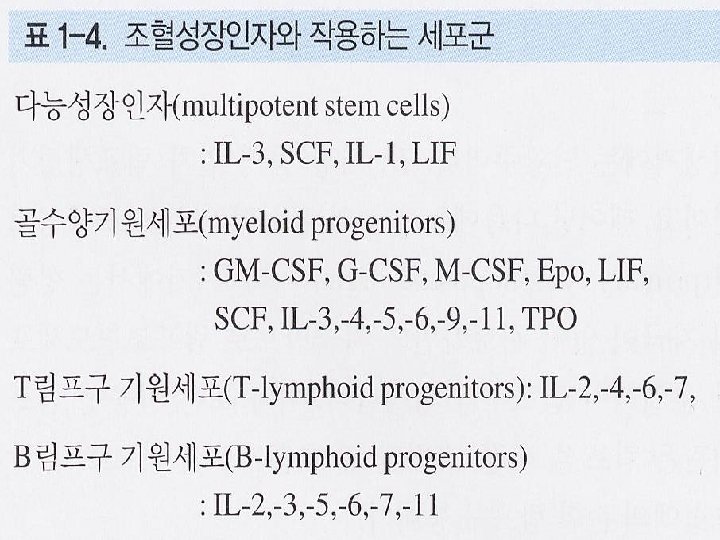
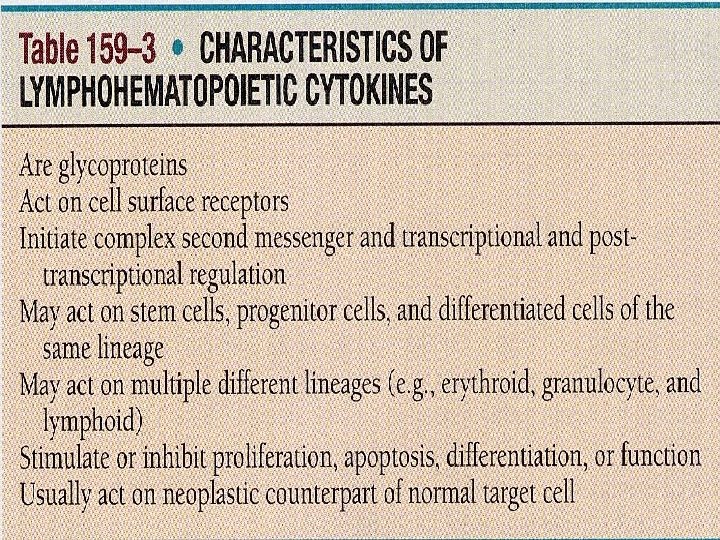
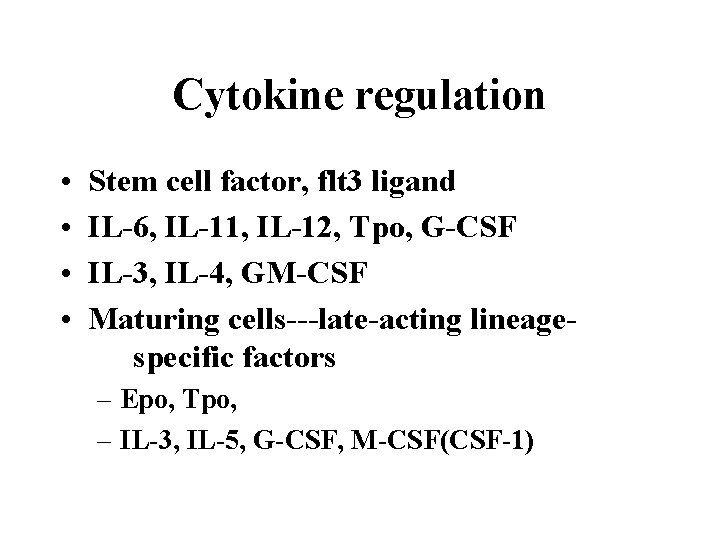
Cytokine regulation • • Stem cell factor, flt 3 ligand IL-6, IL-11, IL-12, Tpo, G-CSF IL-3, IL-4, GM-CSF Maturing cells---late-acting lineagespecific factors – Epo, Tpo, – IL-3, IL-5, G-CSF, M-CSF(CSF-1)
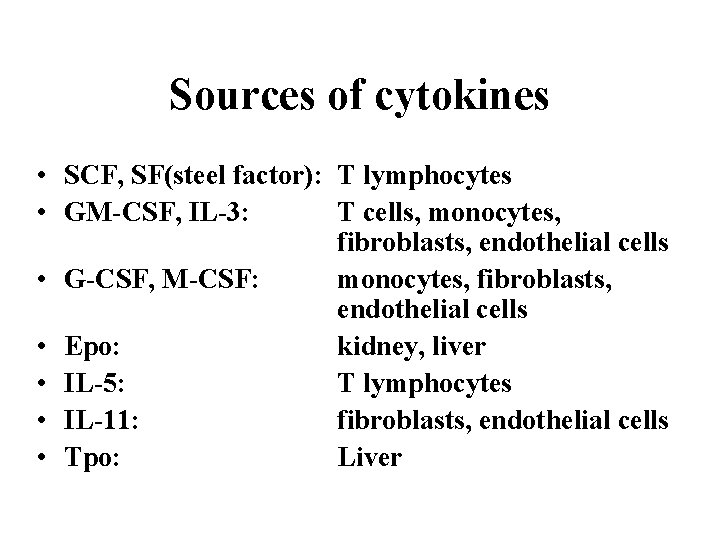
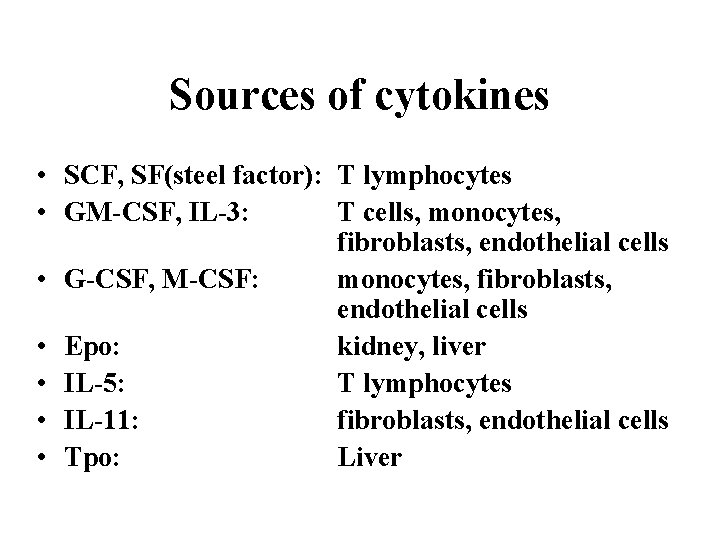
Sources of cytokines • SCF, SF(steel factor): T lymphocytes • GM-CSF, IL-3: T cells, monocytes, fibroblasts, endothelial cells • G-CSF, M-CSF: monocytes, fibroblasts, endothelial cells • Epo: kidney, liver • IL-5: T lymphocytes • IL-11: fibroblasts, endothelial cells • Tpo: Liver
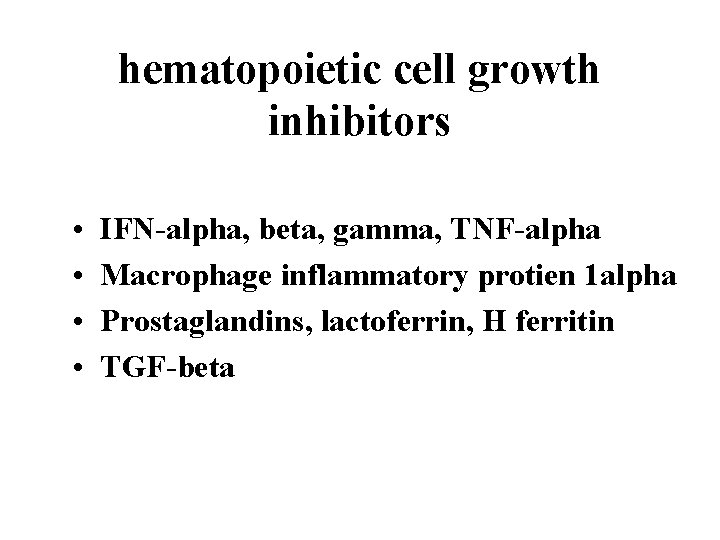
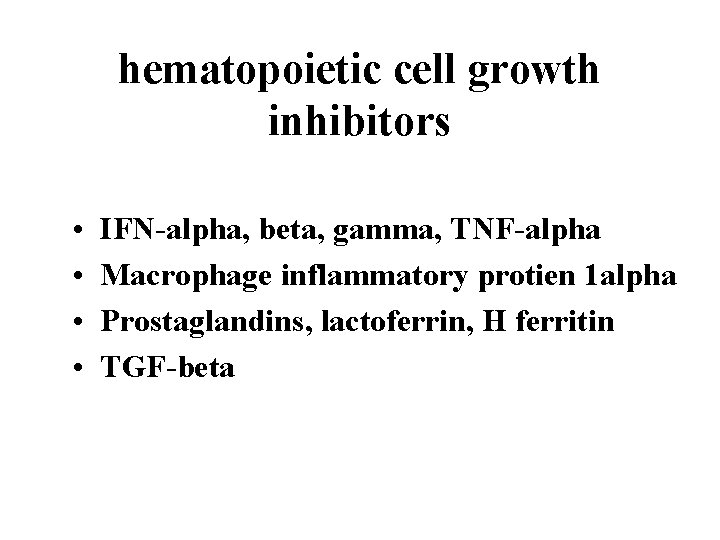
hematopoietic cell growth inhibitors • • IFN-alpha, beta, gamma, TNF-alpha Macrophage inflammatory protien 1 alpha Prostaglandins, lactoferrin, H ferritin TGF-beta
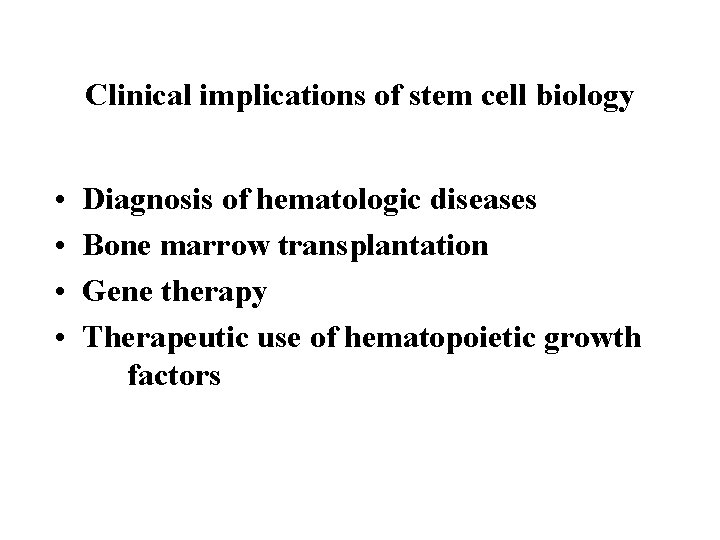
Clinical implications of stem cell biology • • Diagnosis of hematologic diseases Bone marrow transplantation Gene therapy Therapeutic use of hematopoietic growth factors
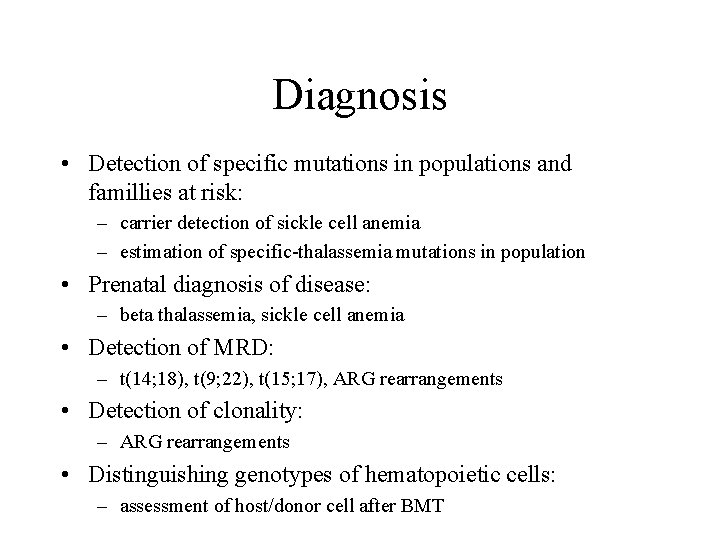
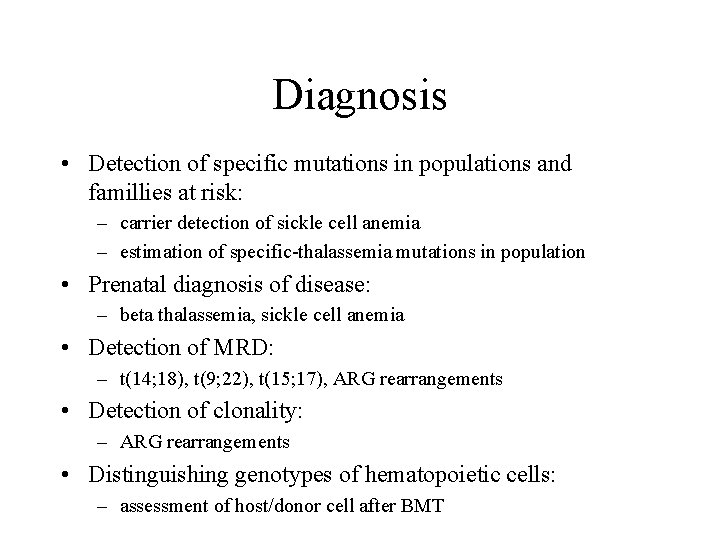
Diagnosis • Detection of specific mutations in populations and famillies at risk: – carrier detection of sickle cell anemia – estimation of specific-thalassemia mutations in population • Prenatal diagnosis of disease: – beta thalassemia, sickle cell anemia • Detection of MRD: – t(14; 18), t(9; 22), t(15; 17), ARG rearrangements • Detection of clonality: – ARG rearrangements • Distinguishing genotypes of hematopoietic cells: – assessment of host/donor cell after BMT
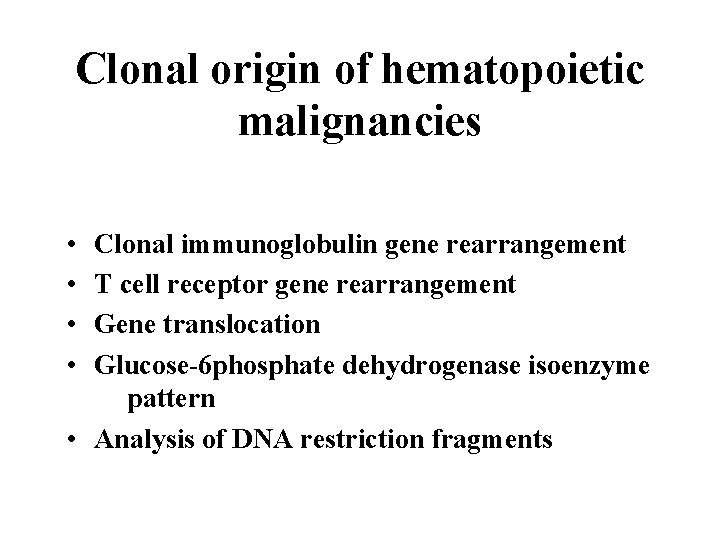
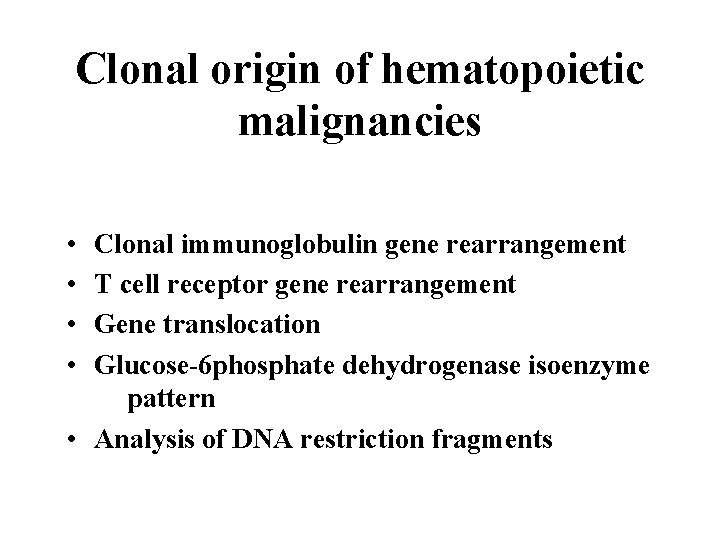
Clonal origin of hematopoietic malignancies • • Clonal immunoglobulin gene rearrangement T cell receptor gene rearrangement Gene translocation Glucose-6 phosphate dehydrogenase isoenzyme pattern • Analysis of DNA restriction fragments
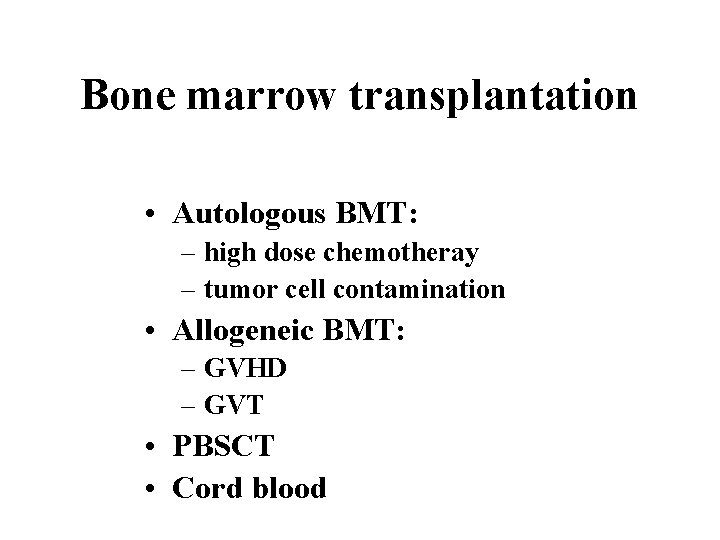
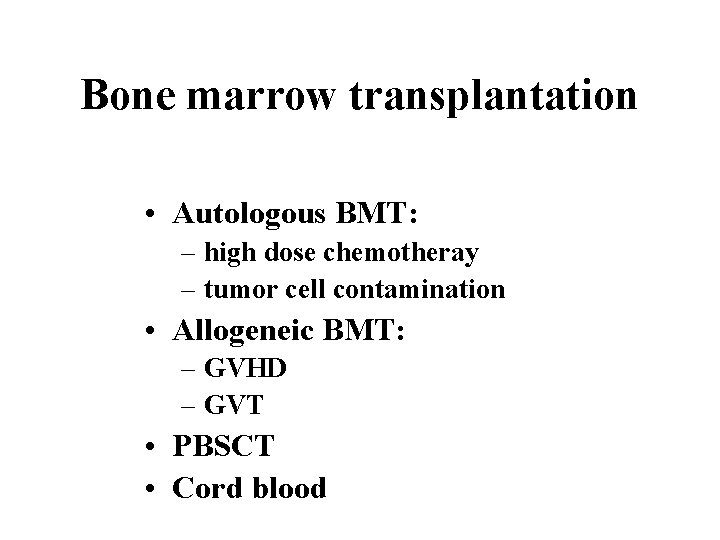
Bone marrow transplantation • Autologous BMT: – high dose chemotheray – tumor cell contamination • Allogeneic BMT: – GVHD – GVT • PBSCT • Cord blood
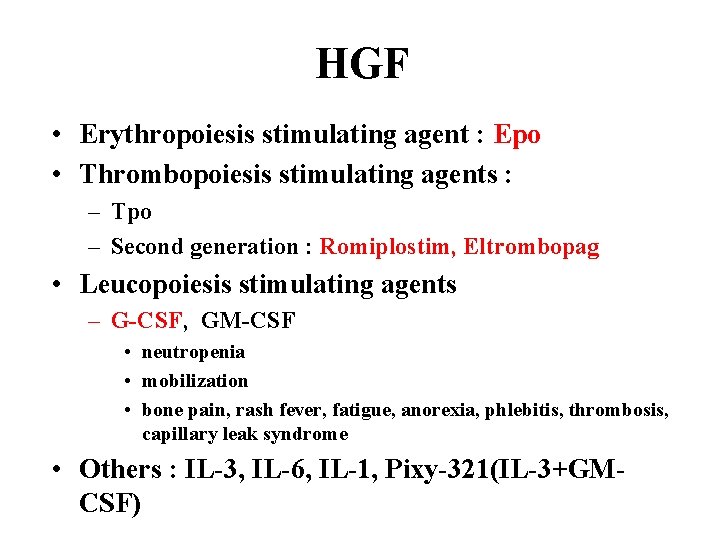
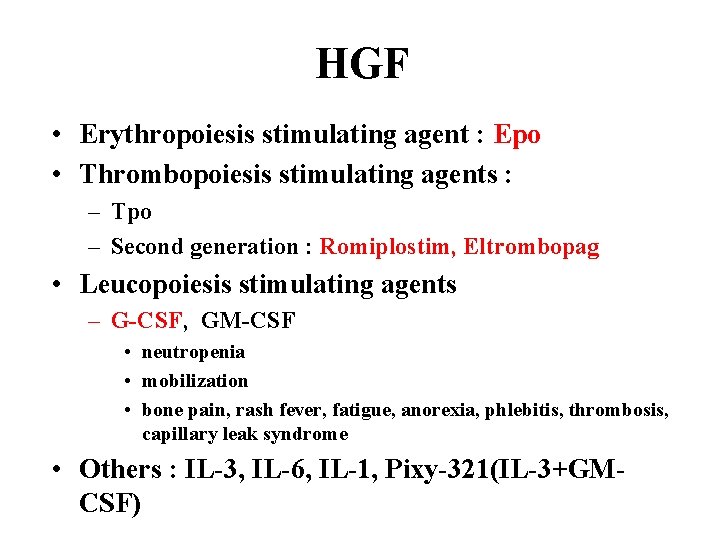
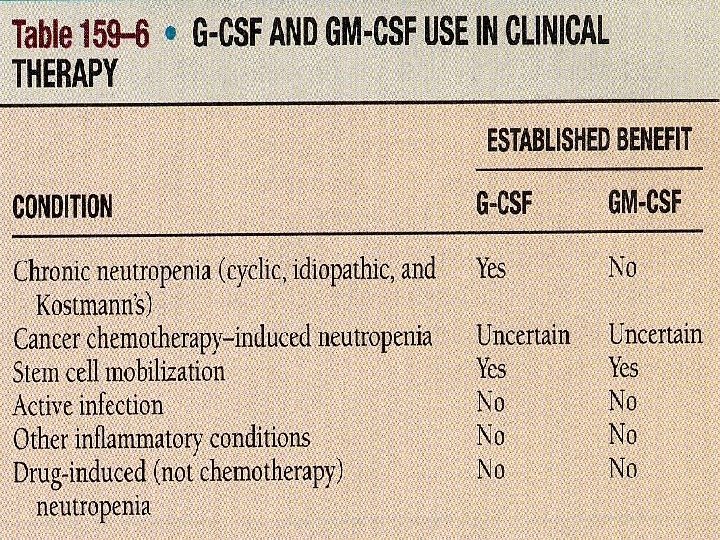
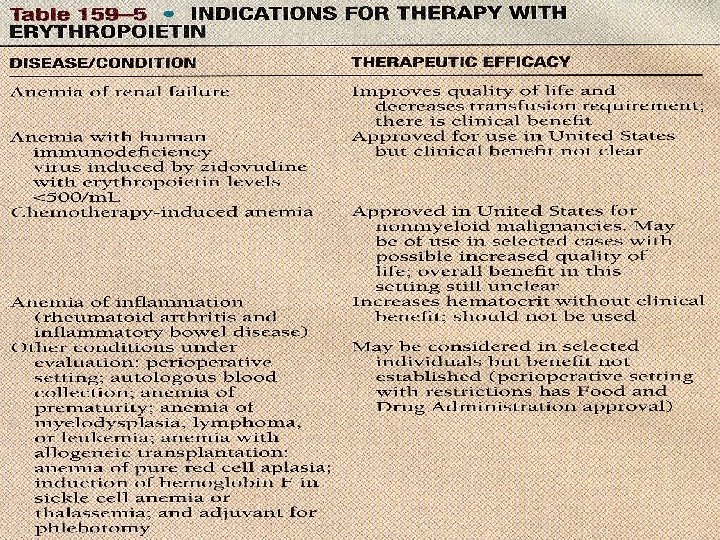
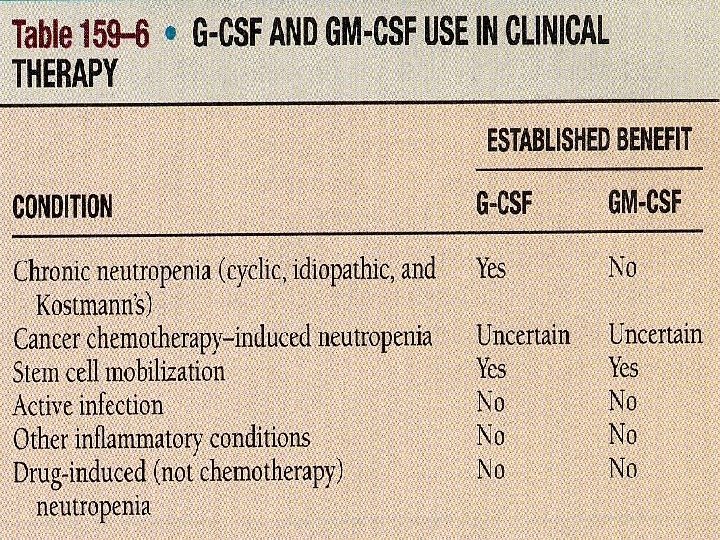
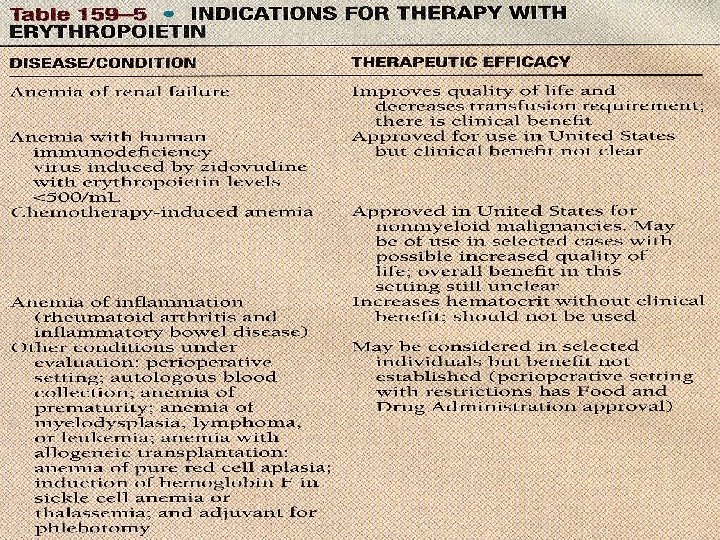
HGF • Erythropoiesis stimulating agent : Epo • Thrombopoiesis stimulating agents : – Tpo – Second generation : Romiplostim, Eltrombopag • Leucopoiesis stimulating agents – G-CSF, GM-CSF • neutropenia • mobilization • bone pain, rash fever, fatigue, anorexia, phlebitis, thrombosis, capillary leak syndrome • Others : IL-3, IL-6, IL-1, Pixy-321(IL-3+GMCSF)
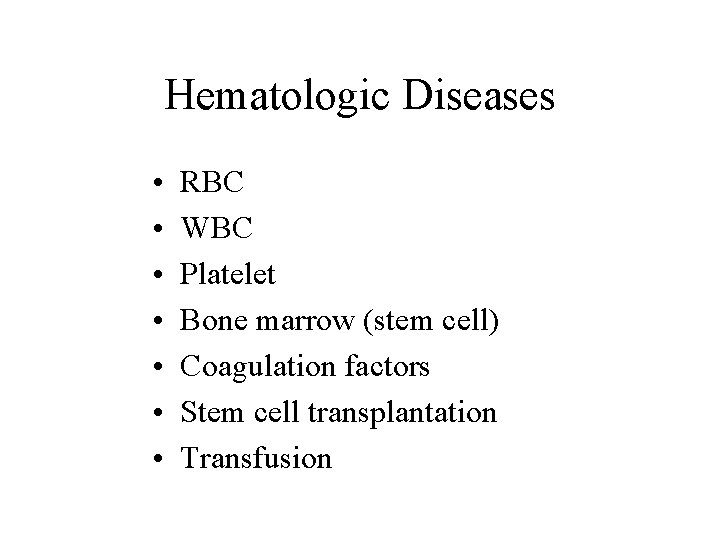
Hematologic Diseases • • RBC WBC Platelet Bone marrow (stem cell) Coagulation factors Stem cell transplantation Transfusion
Erythroid • Anemia – Production defect – Destruction – Loss – Functional defect • Erythrocytosis – Primary – Secondary
WBC • Leucocytosis – Primary – Secondary • Leucopenia – Neutropenia – Lymphopenia • Functional defect
Platelets • Thrombocytosis – Primary – Secondary • Thrombocytopenia – Production – Destruction • Functional defects

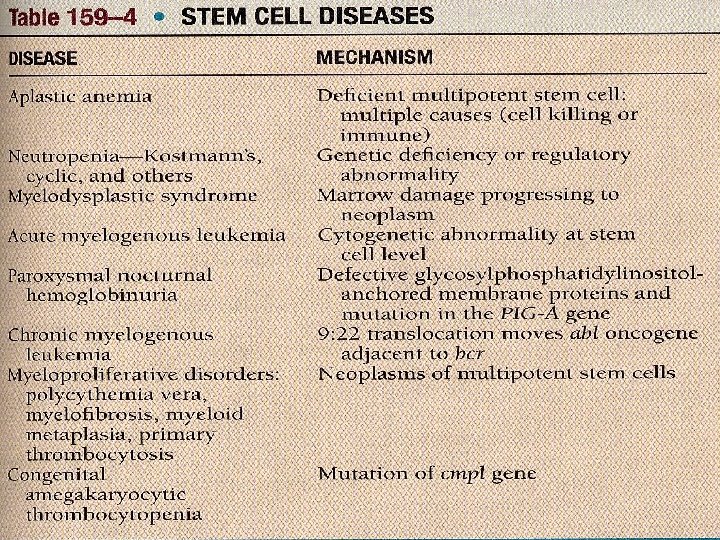
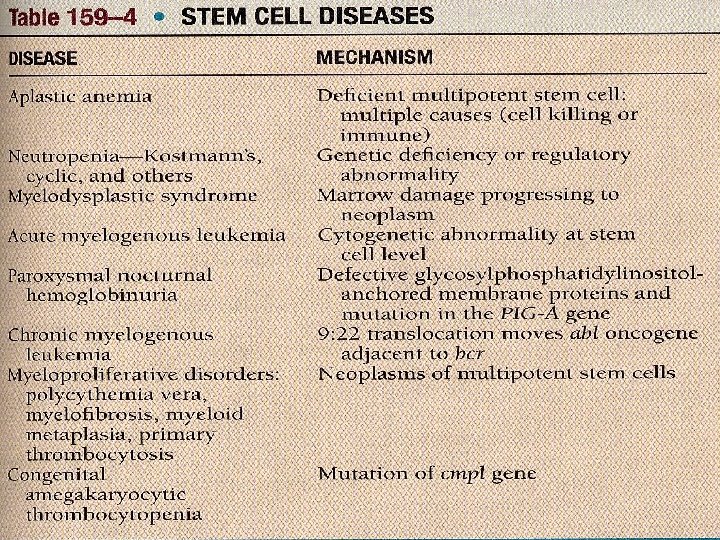
Bone marrow (Stem cell) • Primary – Clonal disease • Malignant : myeloid, lymphoid • Non-malignant : – Non-clonal • Secondary – Drug – Myelophthisia – Idiopathic
Others • Coagulation factors – Deficiency : • Congenital • Acquired – Thrombosis • Stem cell transplantation – Allogeneic – Autologous • Transfusion