Living with Heart Failure Ayesha Hasan MD FACC






- Slides: 47

Living with Heart Failure Ayesha Hasan MD, FACC Advanced Heart Failure and Transplantation Program Medical Director Cardiac Transplant Program Contact information: 614 -293 -6081 (heart failure office)
What is Heart Failure? Heart failure is NOT a heart attack Heart failure means the heart is: Weakened § Cannot pump enough blood to supply the body’s needs § . . . It does not mean the heart has stopped working!
Heart Failure is Very Common § Heart failure affects nearly 5 million Americans § § 50% men and 50% women An estimated ½ million new cases are diagnosed each year Expected to rise to 750, 000 new cases by 2040 § Related to aging population, better treatment of heart disease and risk factors, awareness § § Over one million heart failure hospitalizations annually Rising over past few decades § Accounts for over 20% admissions in people 65 and over §
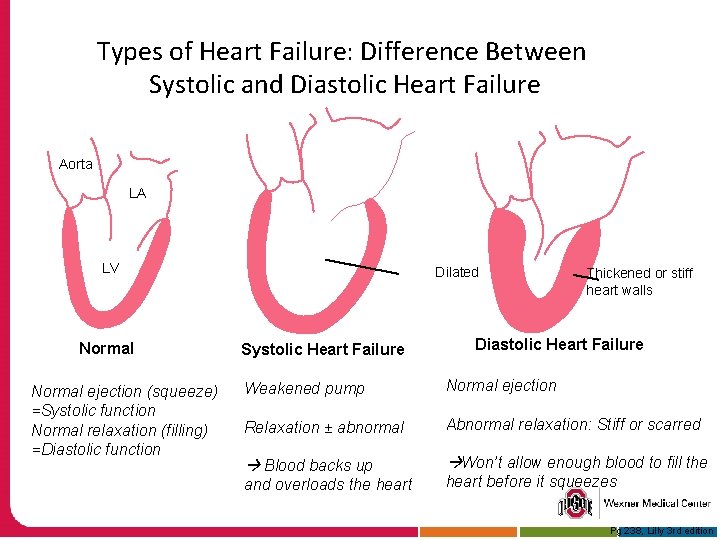
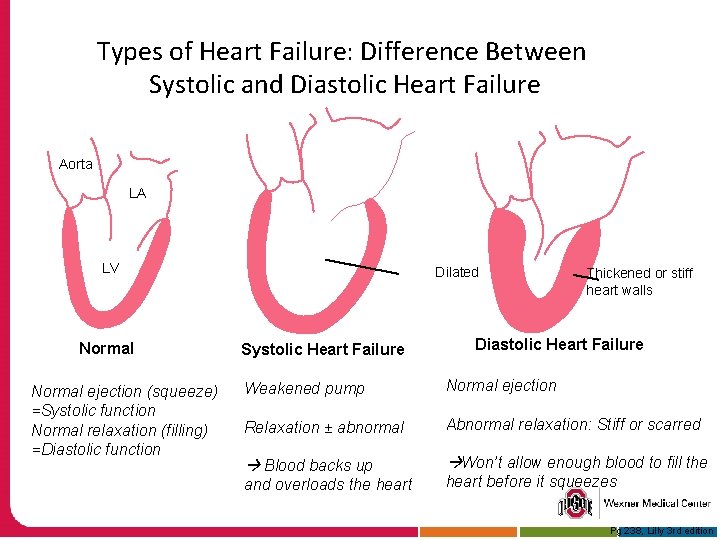
Types of Heart Failure: Difference Between Systolic and Diastolic Heart Failure Aorta LA LV Normal ejection (squeeze) =Systolic function Normal relaxation (filling) =Diastolic function Dilated Systolic Heart Failure Thickened or stiff heart walls Diastolic Heart Failure Weakened pump Normal ejection Relaxation ± abnormal Abnormal relaxation: Stiff or scarred Blood backs up Won’t allow enough blood to fill the and overloads the heart before it squeezes Pg 238, Lilly 3 rd edition
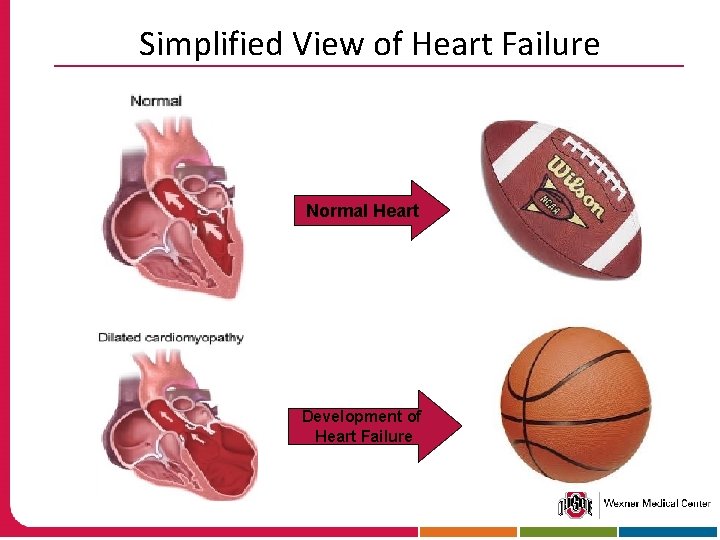
Simplified View of Heart Failure Normal Heart Development of Heart Failure
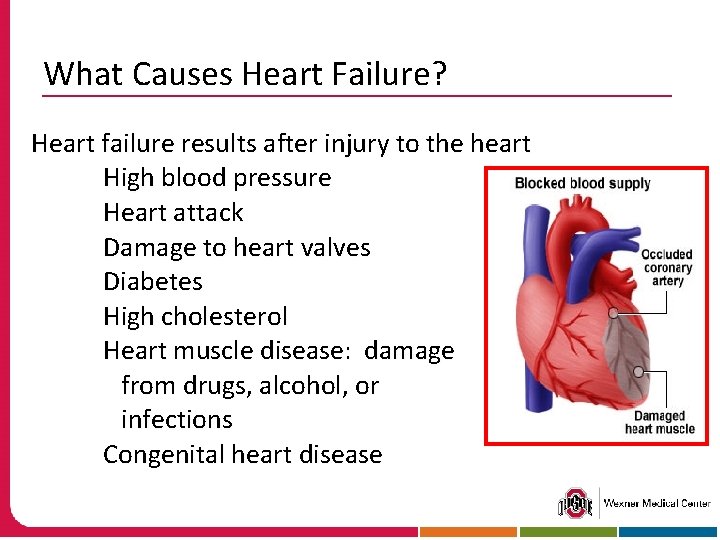
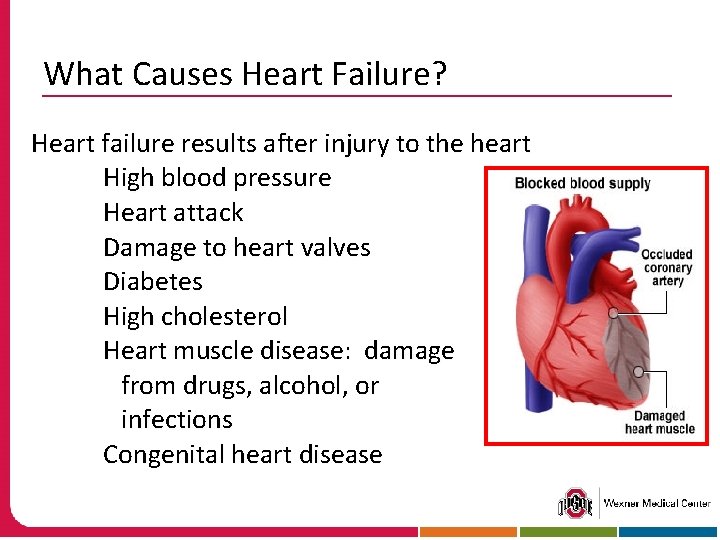
What Causes Heart Failure? Heart failure results after injury to the heart High blood pressure Heart attack Damage to heart valves Diabetes High cholesterol Heart muscle disease: damage from drugs, alcohol, or infections Congenital heart disease
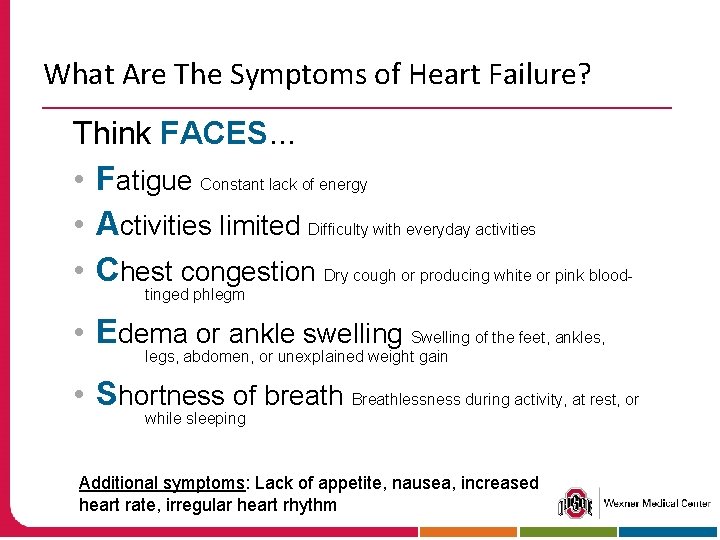
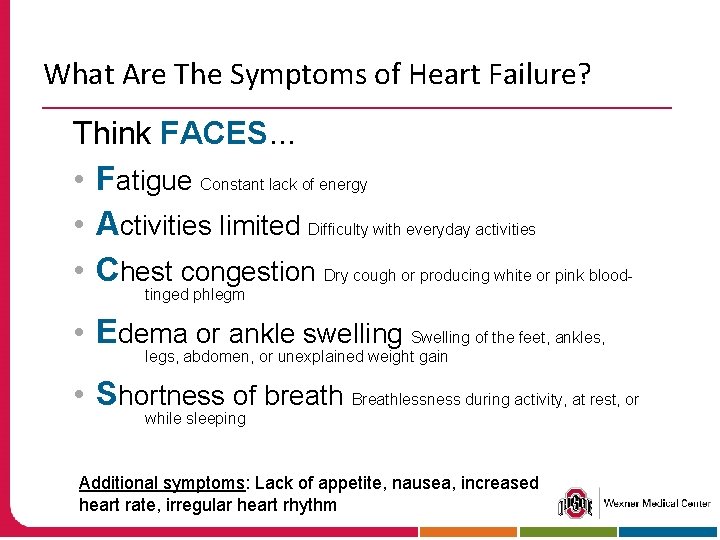
What Are The Symptoms of Heart Failure? Think FACES. . . • Fatigue Constant lack of energy • Activities limited Difficulty with everyday activities • Chest congestion Dry cough or producing white or pink bloodtinged phlegm • Edema or ankle swelling Swelling of the feet, ankles, legs, abdomen, or unexplained weight gain • Shortness of breath Breathlessness during activity, at rest, or while sleeping Additional symptoms: Lack of appetite, nausea, increased heart rate, irregular heart rhythm

How Severe is A Patient’s Heart Failure? § We measure the “ejection fraction” by echo § The fraction of blood that the heart pumps with every beat § We assess the patient’s symptoms § No or mild symptoms § Do symptoms limit activity? If so, how much?
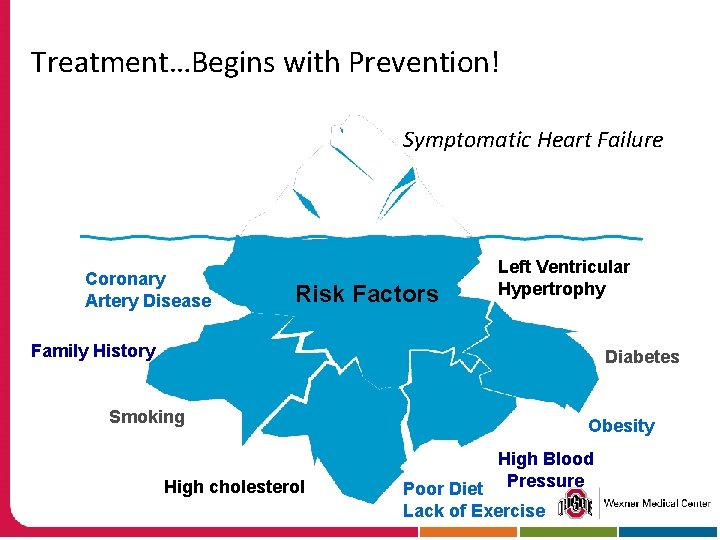
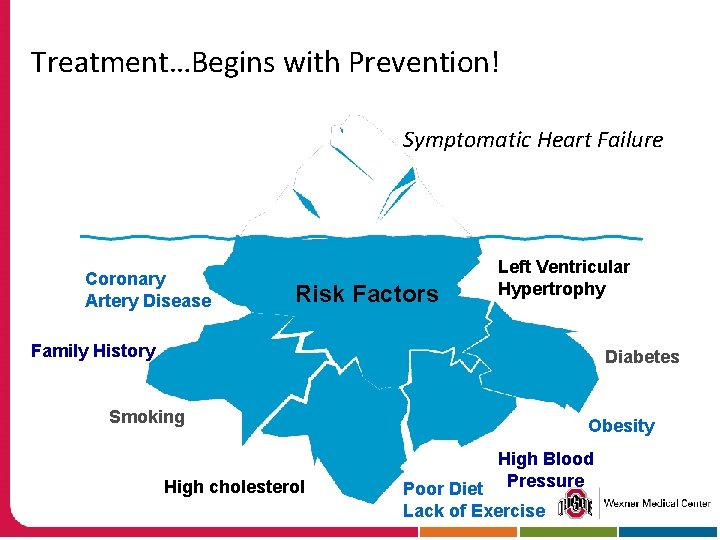
Treatment…Begins with Prevention! Symptomatic Heart Failure Coronary Artery Disease Risk Factors Left Ventricular Hypertrophy Family History Diabetes Smoking High cholesterol Obesity High Blood Poor Diet Pressure Lack of Exercise
How Do We Treat Heart Failure? Lifestyle Changes § Quit smoking § Monitor diet: low-fat, low sodium § Exercise regularly § Lose weight § Avoid alcohol § Limit caffeine intake
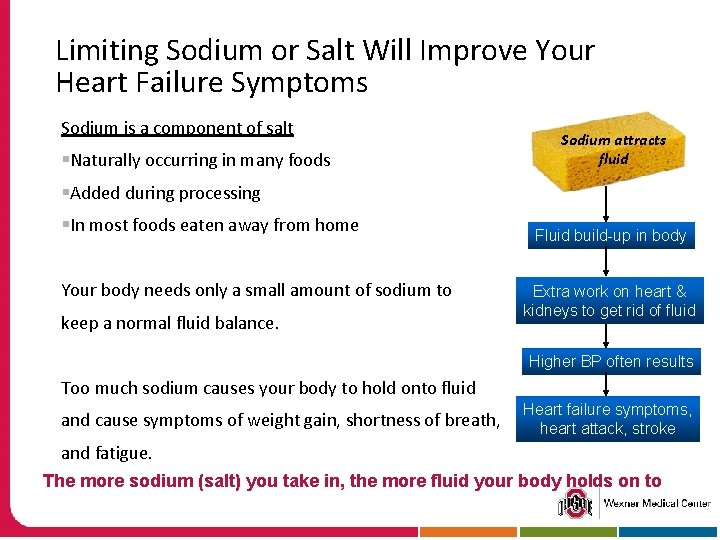
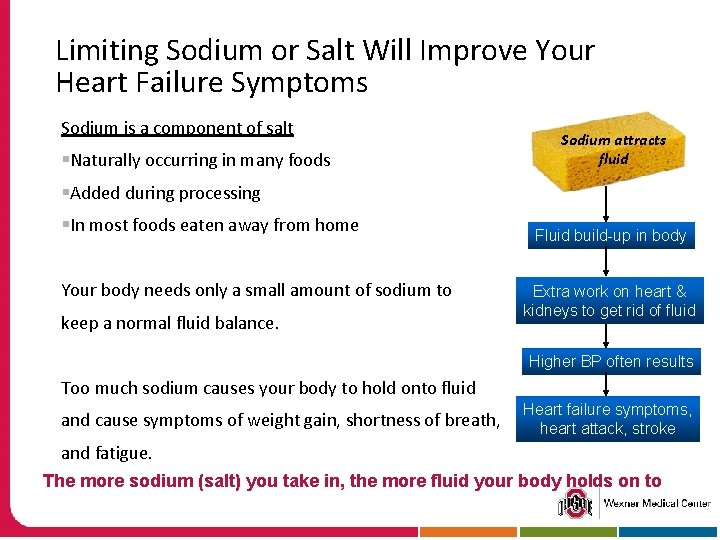
Limiting Sodium or Salt Will Improve Your Heart Failure Symptoms Sodium is a component of salt §Naturally occurring in many foods Sodium attracts fluid §Added during processing §In most foods eaten away from home Your body needs only a small amount of sodium to keep a normal fluid balance. Fluid build-up in body Extra work on heart & kidneys to get rid of fluid Higher BP often results Too much sodium causes your body to hold onto fluid and cause symptoms of weight gain, shortness of breath, Heart failure symptoms, heart attack, stroke and fatigue. The more sodium (salt) you take in, the more fluid your body holds on to
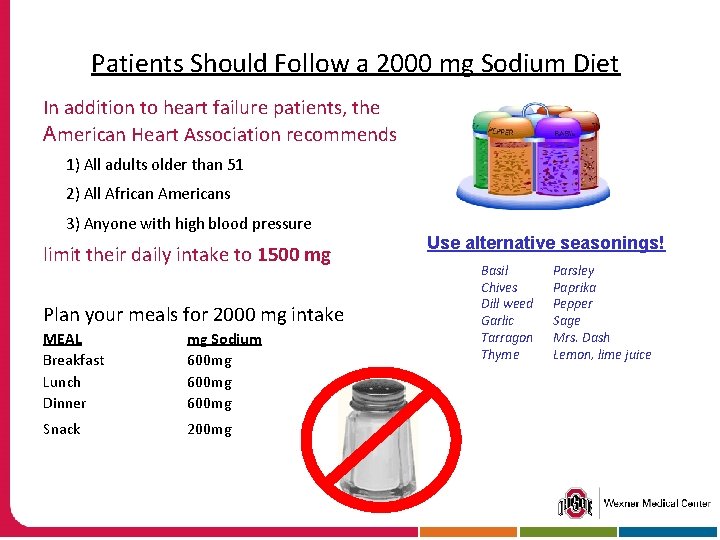
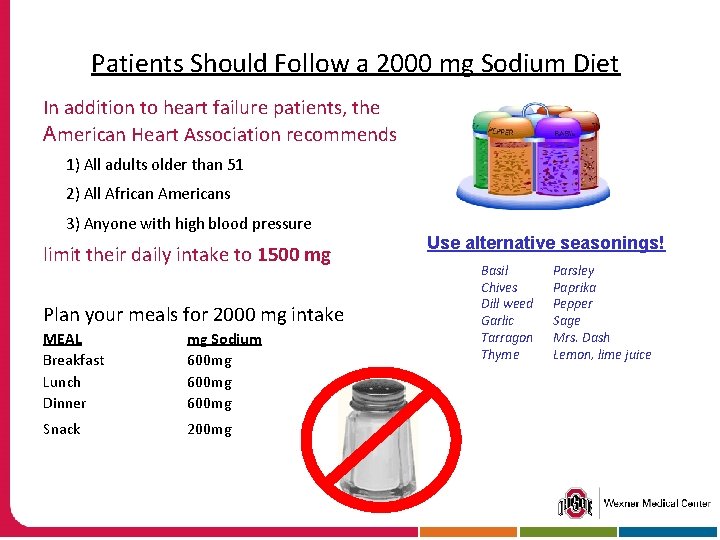
Patients Should Follow a 2000 mg Sodium Diet In addition to heart failure patients, the American Heart Association recommends 1) All adults older than 51 2) All African Americans 3) Anyone with high blood pressure limit their daily intake to 1500 mg Plan your meals for 2000 mg intake MEAL Breakfast Lunch Dinner mg Sodium 600 mg Snack 200 mg Use alternative seasonings! Basil Chives Dill weed Garlic Tarragon Thyme Parsley Paprika Pepper Sage Mrs. Dash Lemon, lime juice
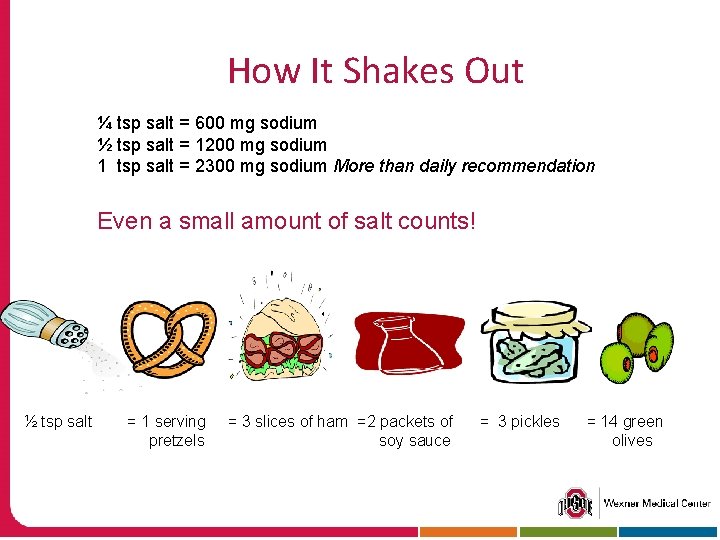
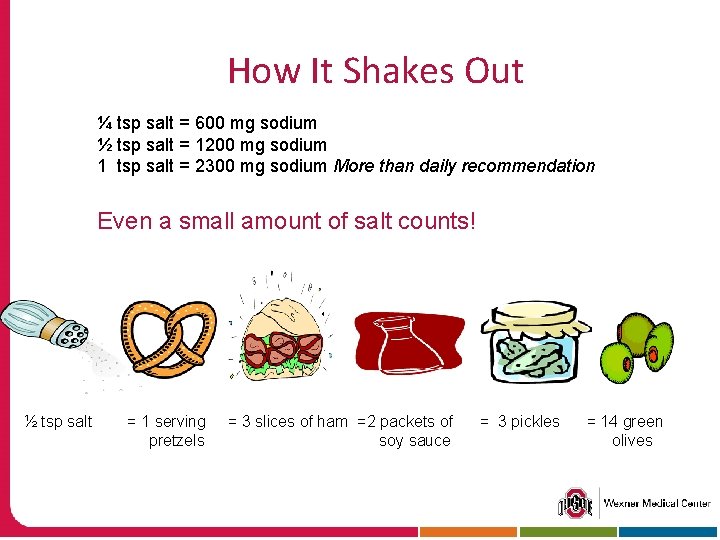
How It Shakes Out ¼ tsp salt = 600 mg sodium ½ tsp salt = 1200 mg sodium 1 tsp salt = 2300 mg sodium More than daily recommendation Even a small amount of salt counts! ½ tsp salt = 1 serving pretzels = 3 slices of ham =2 packets of soy sauce = 3 pickles = 14 green olives
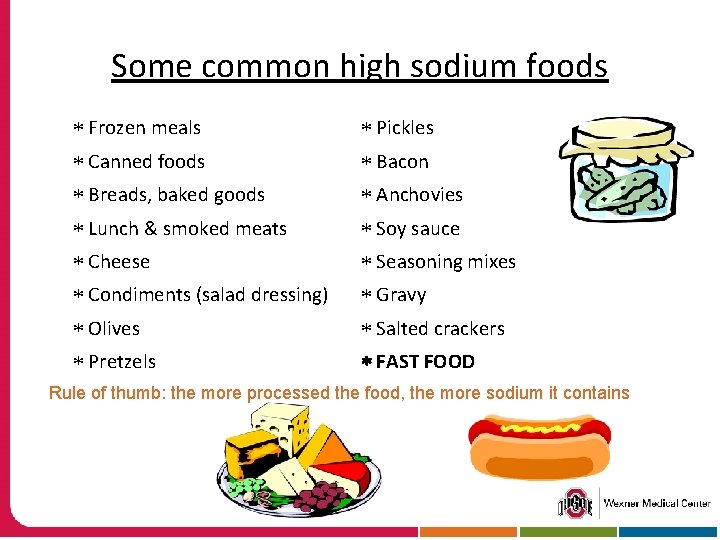
Some common high sodium foods Frozen meals Pickles Canned foods Bacon Breads, baked goods Anchovies Lunch & smoked meats Soy sauce Cheese Seasoning mixes Condiments (salad dressing) Gravy Olives Salted crackers Pretzels FAST FOOD Rule of thumb: the more processed the food, the more sodium it contains
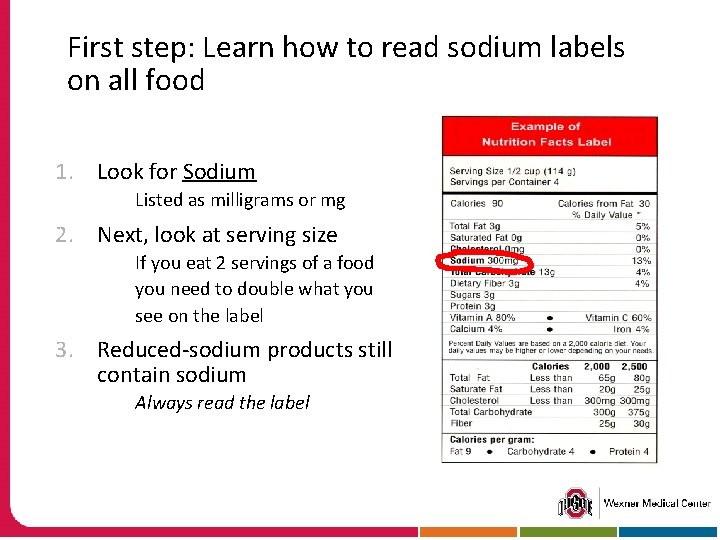
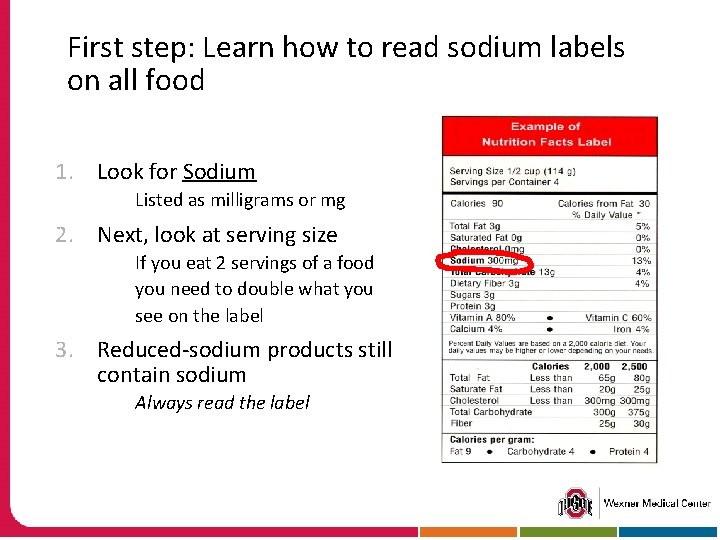
First step: Learn how to read sodium labels on all food 1. Look for Sodium Listed as milligrams or mg 2. Next, look at serving size If you eat 2 servings of a food you need to double what you see on the label 3. Reduced-sodium products still contain sodium Always read the label
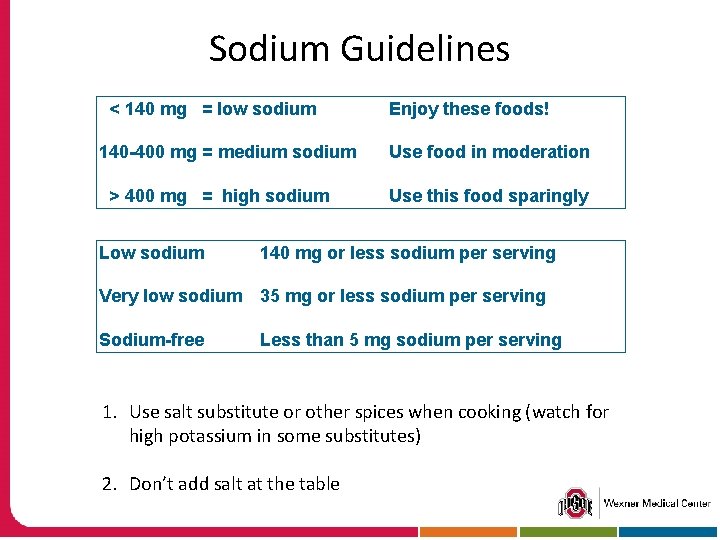
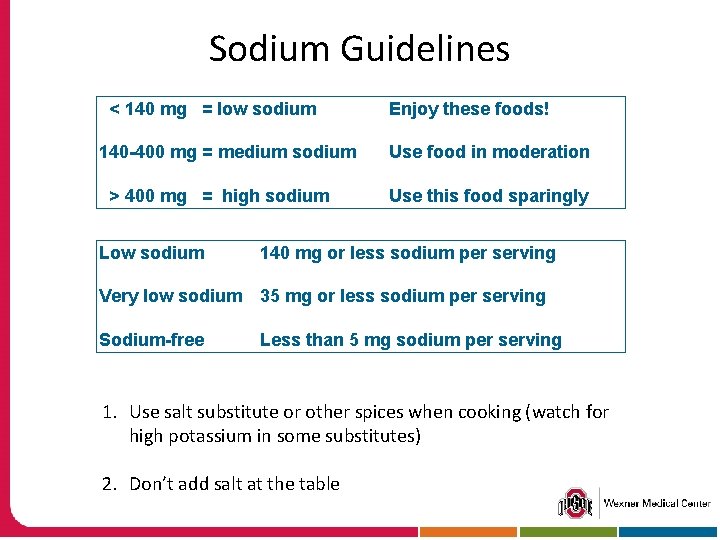
Sodium Guidelines < 140 mg = low sodium 140 -400 mg = medium sodium > 400 mg = high sodium Enjoy these foods! Use food in moderation Use this food sparingly Low sodium 140 mg or less sodium per serving Very low sodium 35 mg or less sodium per serving Sodium-free Less than 5 mg sodium per serving 1. Use salt substitute or other spices when cooking (watch for high potassium in some substitutes) 2. Don’t add salt at the table
Fluid intake & Daily Weights Limiting fluid intake: important in managing heart failure REMEMBER: Anything liquid at room temperature is considered a fluid Daily weights: every morning at the same time using the same scale Keep track of daily weights REMEMBER: You might not see swelling until you are 8 -15# up
Exercise: Get Off the Couch!
Exercise Will Improve Your Quality of Life § Pick a simple aerobic activity that you enjoy § Start slowly and increase gradually § Need to move large muscle groups § Walking is a great first choice § Resume activities you stopped (gardening, bowling, fishing) § Work your way up to 30 minutes most days § Doesn’t have to be 30 minutes in a row § Warm up and cool down § Check with your physician first if § You are really out of shape, uncertain about your abilities, or have shortness of breath with very mild activity
Exercising & Precautions § Find an indoor location along with a partner § Build muscle (stretching, elastic bands, light weights) § Overexertion § Shortness of breath that prevents you from completing a sentence or doesn’t get better with rest § Dizziness, chest pain, nausea, vomiting, severe sweating, unusual fatigue (extreme)
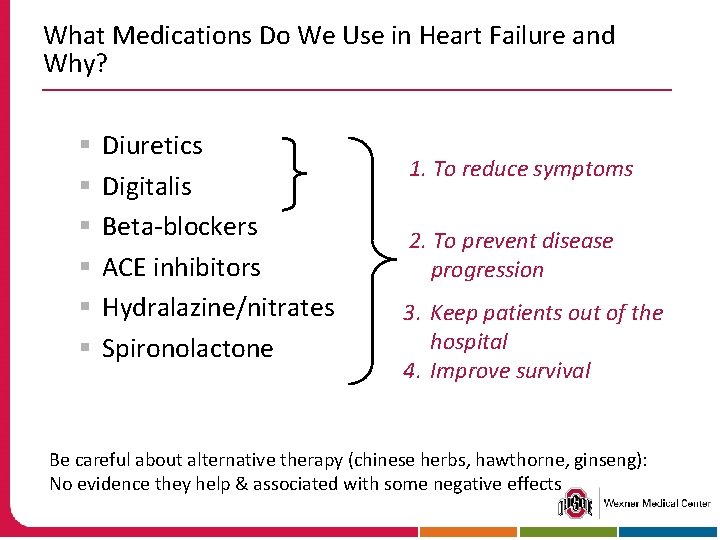
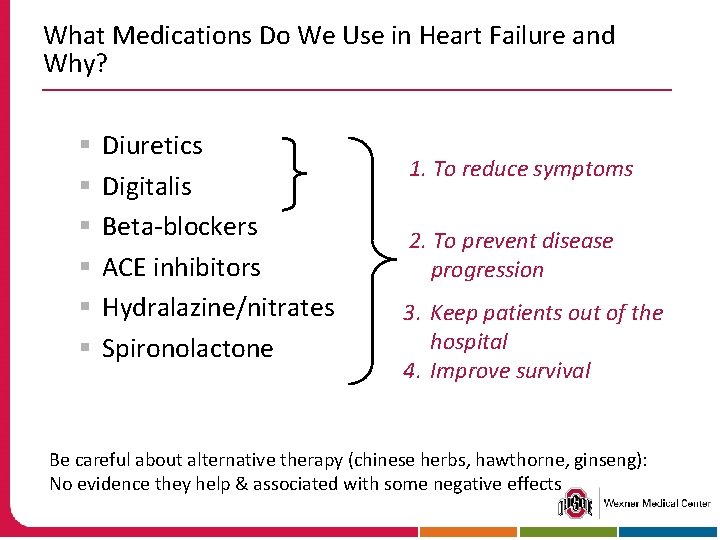
What Medications Do We Use in Heart Failure and Why? § § § Diuretics Digitalis Beta-blockers ACE inhibitors Hydralazine/nitrates Spironolactone 1. To reduce symptoms 2. To prevent disease progression 3. Keep patients out of the hospital 4. Improve survival Be careful about alternative therapy (chinese herbs, hawthorne, ginseng): No evidence they help & associated with some negative effects
Why Do We Use These Treatments? Heart failure limits a patient's ability to perform the routine activities of daily living…
Diuretics, ACE Inhibitors Reduce the number of sacks on the wagon (or load on the heart)
ß-Blockers Limit the speed, thus saving energy

Spironolactone, Cardiac Resynchronization Therapy Increase the heart’s efficiency
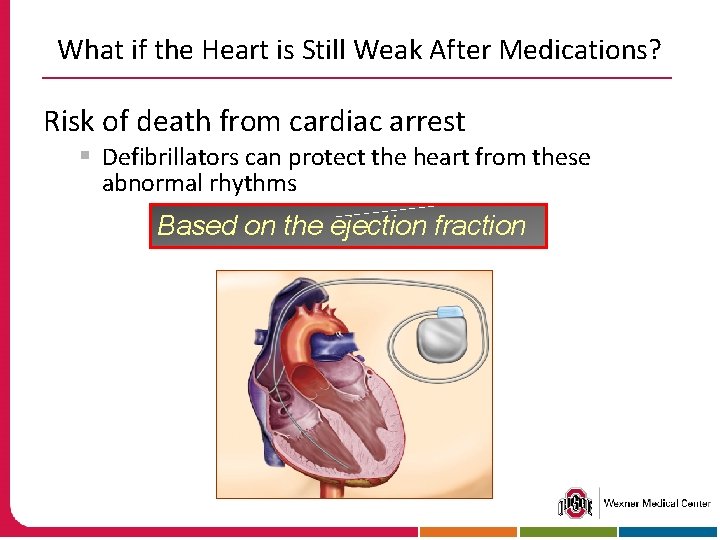
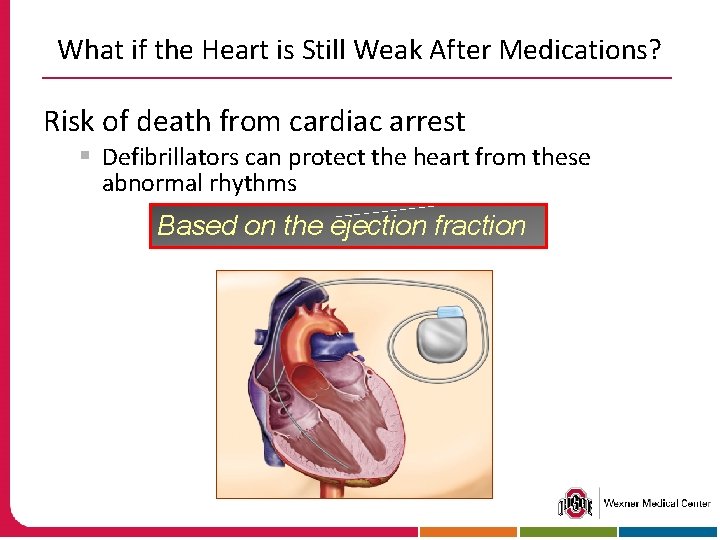
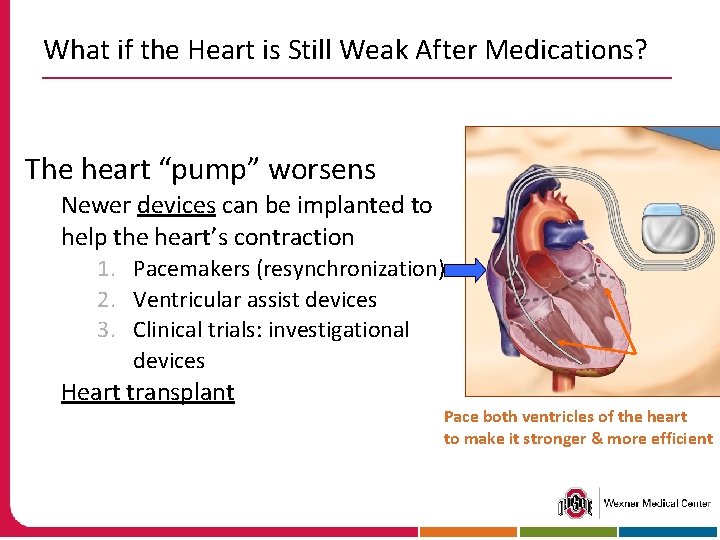
What if the Heart is Still Weak After Medications? Risk of death from cardiac arrest § Defibrillators can protect the heart from these abnormal rhythms Based on the ejection fraction
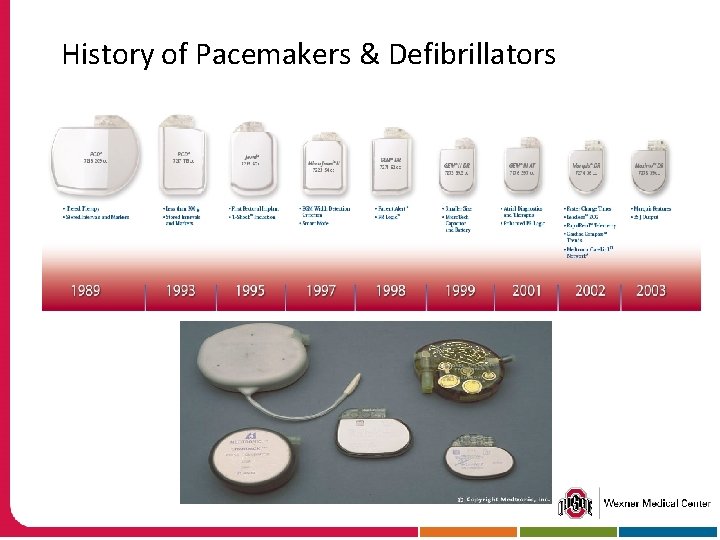
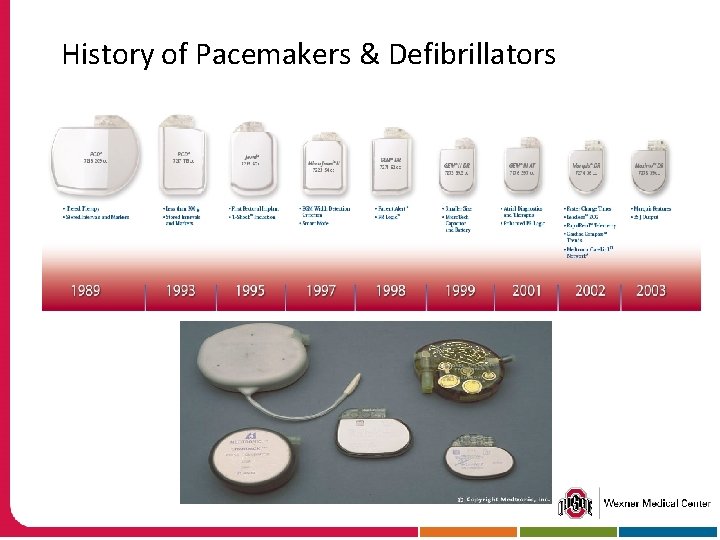
History of Pacemakers & Defibrillators
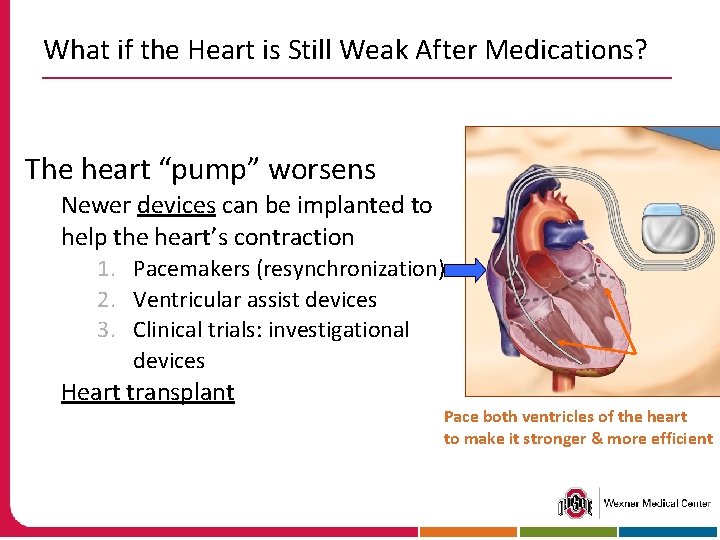
What if the Heart is Still Weak After Medications? The heart “pump” worsens Newer devices can be implanted to help the heart’s contraction 1. Pacemakers (resynchronization) 2. Ventricular assist devices 3. Clinical trials: investigational devices Heart transplant Pace both ventricles of the heart to make it stronger & more efficient
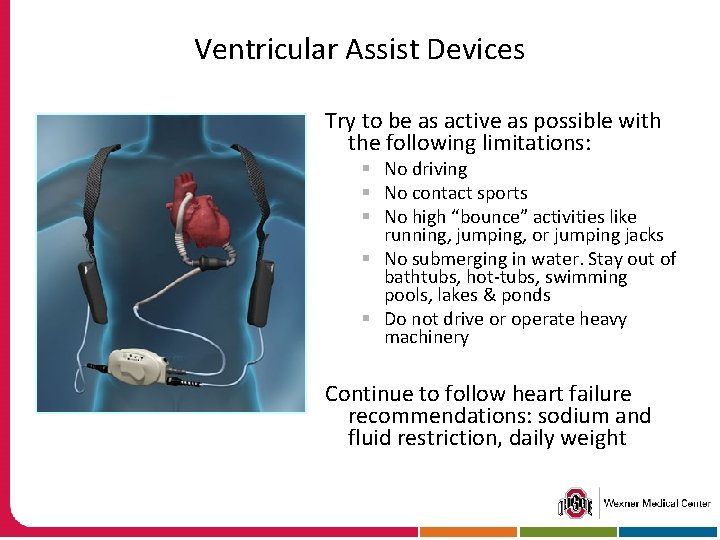
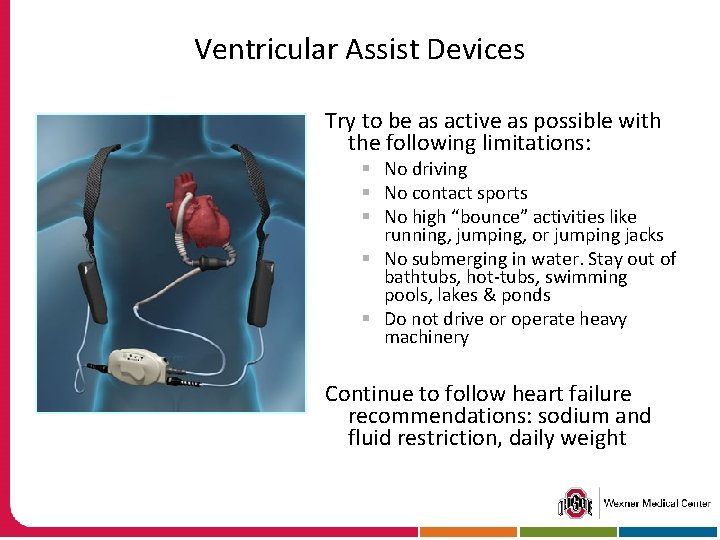
Ventricular Assist Devices Try to be as active as possible with the following limitations: § No driving § No contact sports § No high “bounce” activities like running, jumping, or jumping jacks § No submerging in water. Stay out of bathtubs, hot-tubs, swimming pools, lakes & ponds § Do not drive or operate heavy machinery Continue to follow heart failure recommendations: sodium and fluid restriction, daily weight
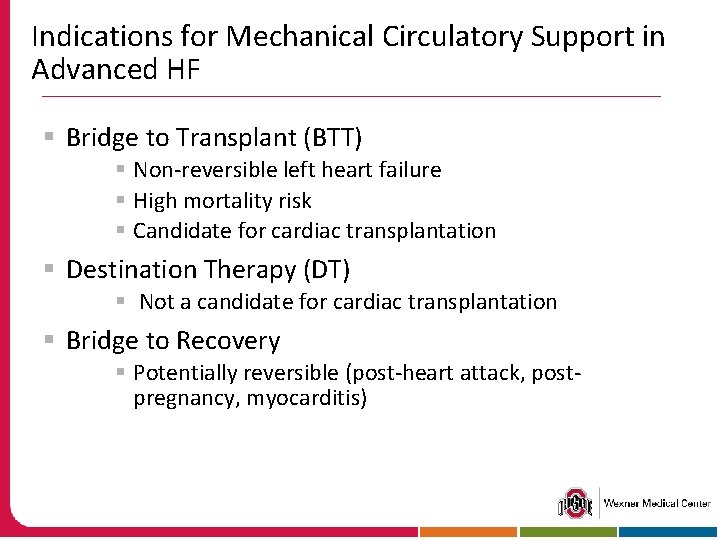
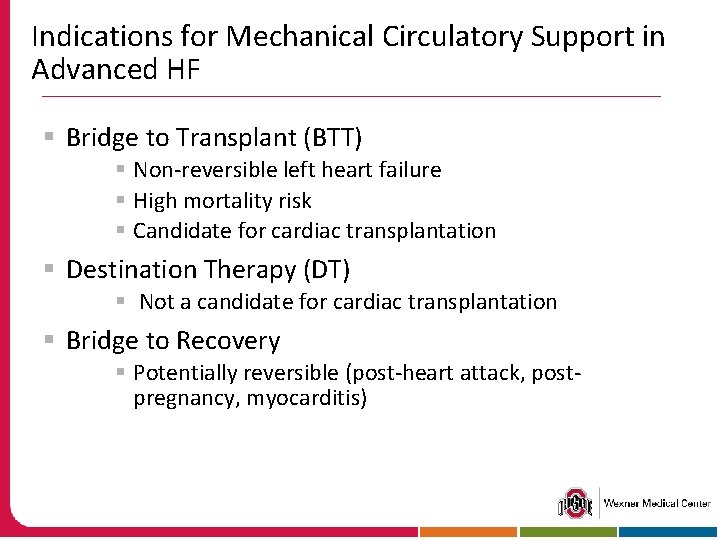
Indications for Mechanical Circulatory Support in Advanced HF § Bridge to Transplant (BTT) § Non-reversible left heart failure § High mortality risk § Candidate for cardiac transplantation § Destination Therapy (DT) § Not a candidate for cardiac transplantation § Bridge to Recovery § Potentially reversible (post-heart attack, postpregnancy, myocarditis)
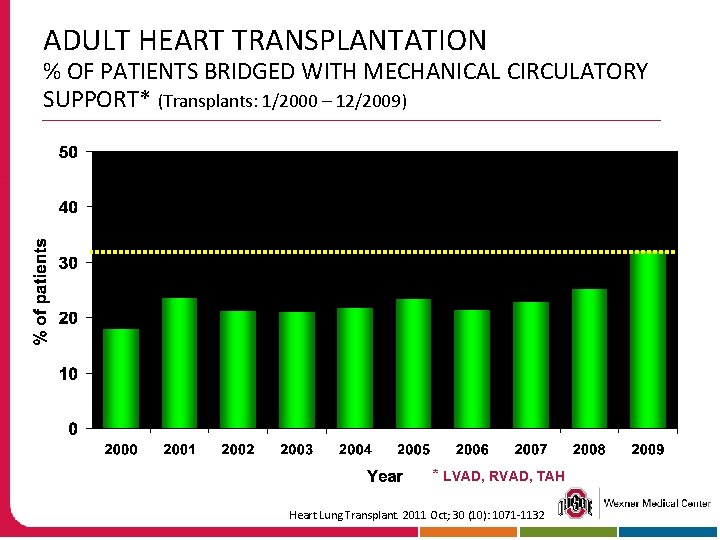
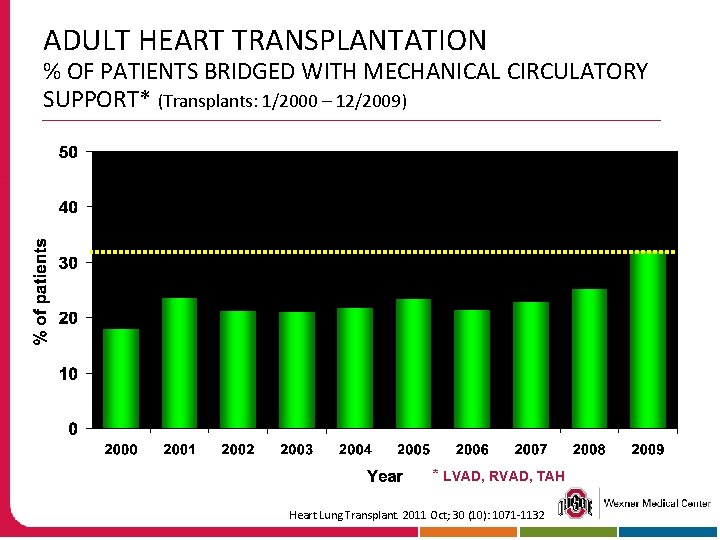
ADULT HEART TRANSPLANTATION % OF PATIENTS BRIDGED WITH MECHANICAL CIRCULATORY SUPPORT* (Transplants: 1/2000 – 12/2009) * LVAD, RVAD, TAH Heart Lung Transplant. 2011 Oct; 30 (10): 1071 -1132
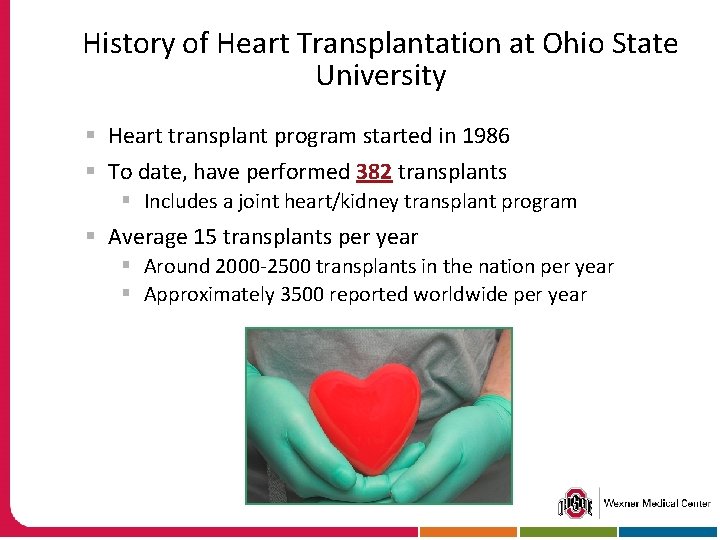
History of Heart Transplantation at Ohio State University § Heart transplant program started in 1986 § To date, have performed 382 transplants § Includes a joint heart/kidney transplant program § Average 15 transplants per year § Around 2000 -2500 transplants in the nation per year § Approximately 3500 reported worldwide per year
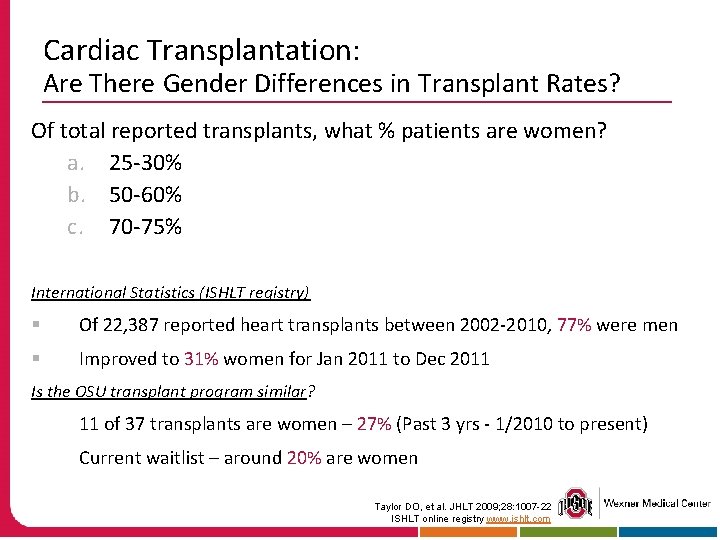
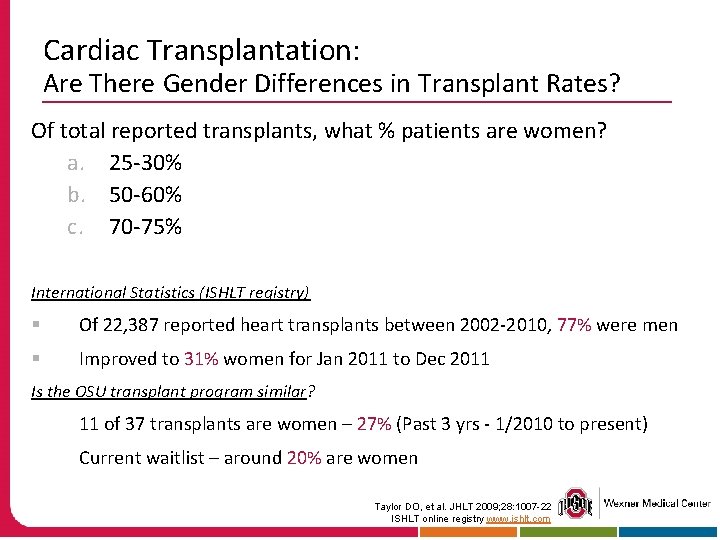
Cardiac Transplantation: Are There Gender Differences in Transplant Rates? Of total reported transplants, what % patients are women? a. 25 -30% b. 50 -60% c. 70 -75% International Statistics (ISHLT registry) § Of 22, 387 reported heart transplants between 2002 -2010, 77% were men § Improved to 31% women for Jan 2011 to Dec 2011 Is the OSU transplant program similar? 11 of 37 transplants are women – 27% (Past 3 yrs - 1/2010 to present) Current waitlist – around 20% are women Taylor DO, et al. JHLT 2009; 28: 1007 -22 ISHLT online registry www. ishlt. com
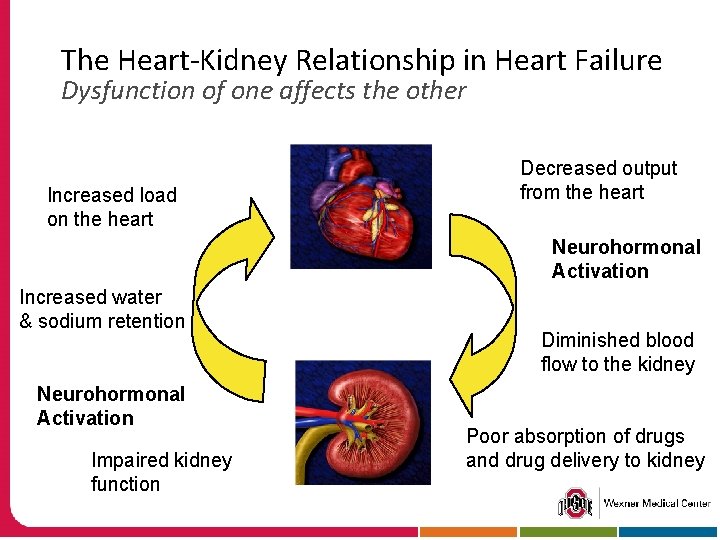
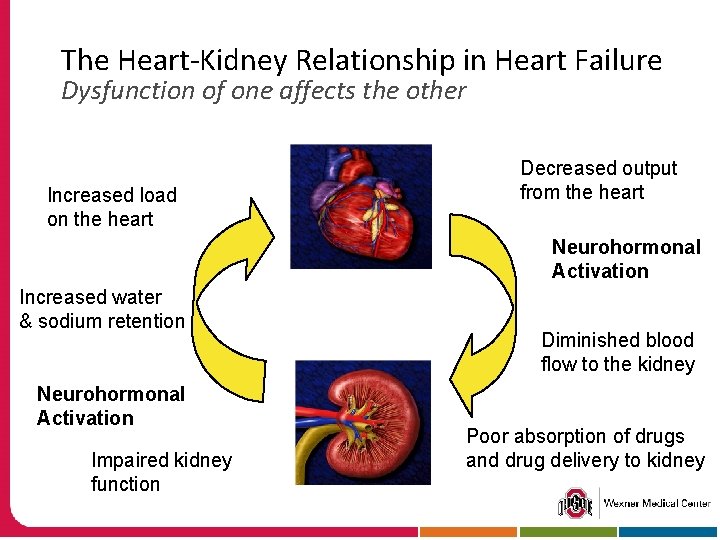
The Heart-Kidney Relationship in Heart Failure Dysfunction of one affects the other Increased load on the heart Decreased output from the heart Neurohormonal Activation Increased water & sodium retention Neurohormonal Activation Impaired kidney function Diminished blood flow to the kidney Poor absorption of drugs and drug delivery to kidney
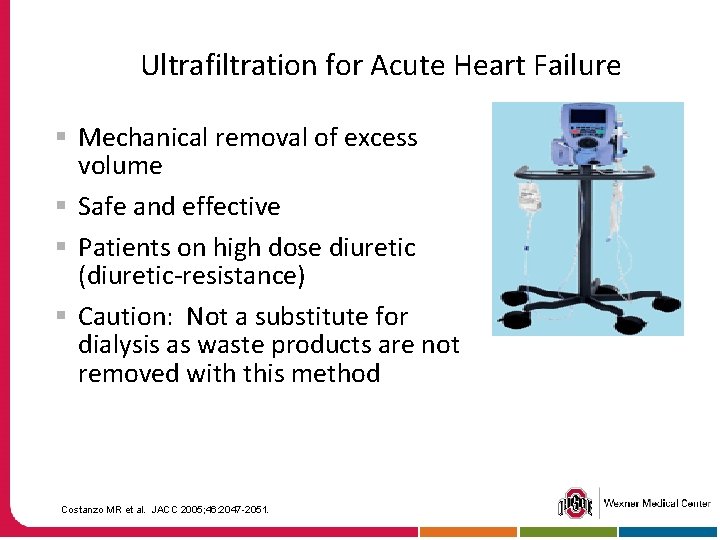
Ultrafiltration for Acute Heart Failure § Mechanical removal of excess volume § Safe and effective § Patients on high dose diuretic (diuretic-resistance) § Caution: Not a substitute for dialysis as waste products are not removed with this method Costanzo MR et al. JACC 2005; 46: 2047 -2051.
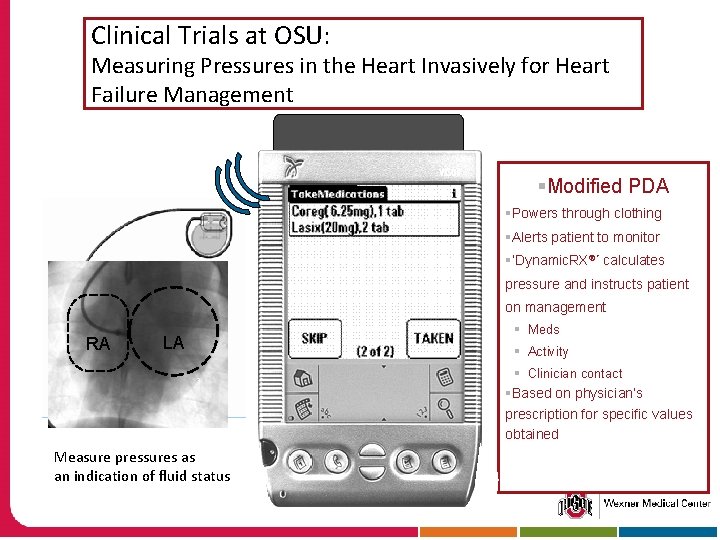
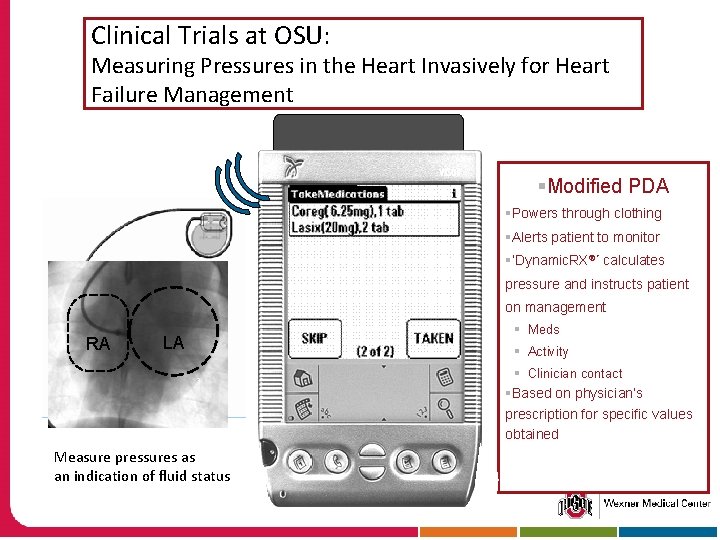
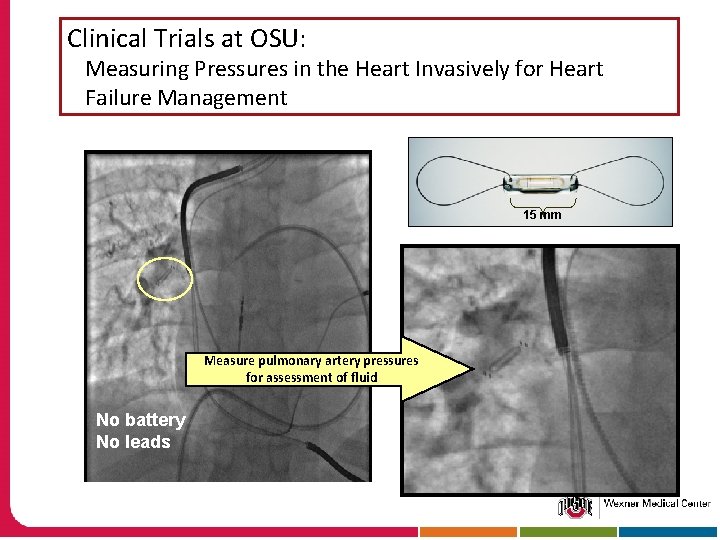
Clinical Trials at OSU: Measuring Pressures in the Heart Invasively for Heart Failure Management Left Atrial Pressure Sensor §Modified PDA §Powers through clothing §Alerts patient to monitor §‘Dynamic. RX®’ calculates pressure and instructs patient on management RA LA § Meds § Activity § Clinician contact §Based on physician’s prescription for specific values obtained Measure pressures as an indication of fluid status
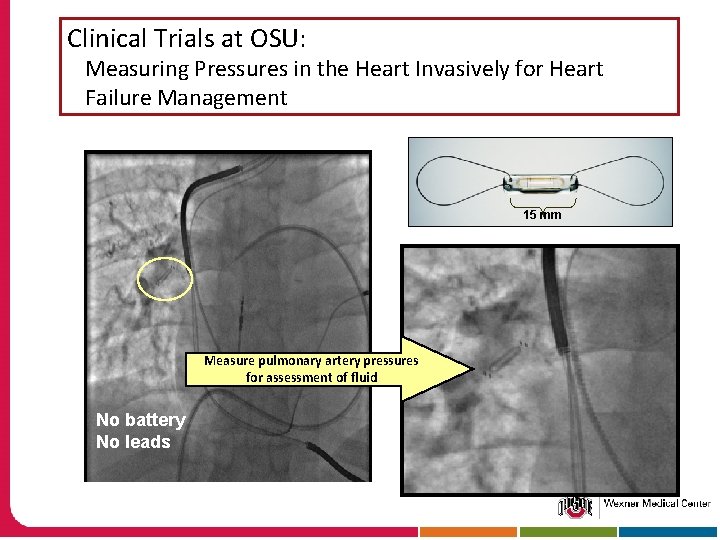
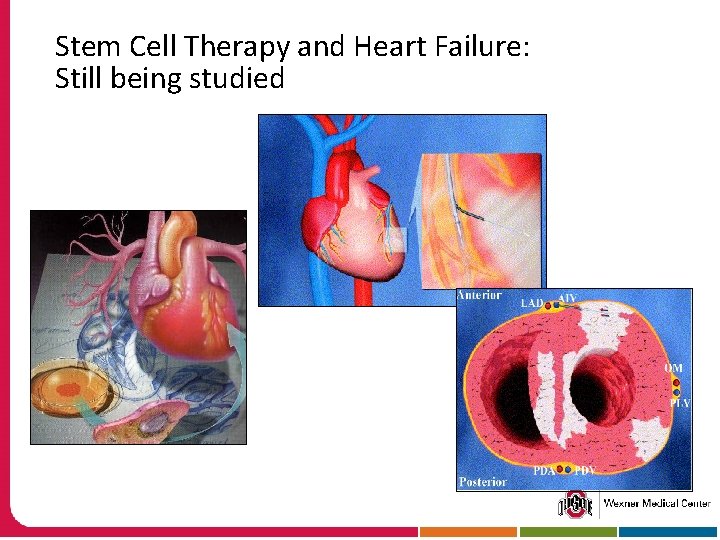
Clinical Trials at OSU: Measuring Pressures in the Heart Invasively for Heart Failure Management 15 mm Measure pulmonary artery pressures for assessment of fluid No battery No leads
Stem Cell Therapy and Heart Failure: Still being studied

Sleep Apnea and Heart Failure People with heart failure have a high risk for sleep apnea If not treated, sleep apnea can cause: § § § Drop in oxygen levels The heart rate to speed up A rise in the blood pressure Changes to the heart rhythm Stroke Heart attack or an episode of heart failure Normal breathing pattern Central sleep apnea: no breathing (apnea) alternates with rapid breathing
Friends and Family § Emotional support helps a patient have a more positive outlook on life § Allow the patient to make decisions regarding health care and lifestyle behaviors § Positive reinforcement § Discuss fears about heart failure § Discuss advanced care planning § Don’t forget to take care of yourself: eat healthy, exercise, sleep
Advanced Care Planning § Not giving up § Focus is on caring for the patient in a way that meets your wishes § Key is communication § Goal is to reduce stress on the patient § Consists of § § § Advanced care directive Do-not-resuscitate order Power of attorney Living will Financial plan

Advanced Care Planning § Palliative care § Support program that focuses on comfort and reducing symptoms, pain. The disease is no longer responsive to curative treatment. § Hospice care § Support program for the patient and family through the dying process. Focus is also comfort and to help with bereavement. § Nurses, chaplains, therapists, bereavement counselors, social workers and physicians
Conclusion: Call your healthcare provider for these symptoms. . . § A change in shortness of breath, fatigue, or swelling § Requiring more pillows than usual to sleep comfortably at night or needing to sleep in a recliner § Chest pain § Near fainting or fainting § Weight gain of 2 lbs in one day or 5 lbs in one week
Conclusion: Living with Heart Failure § See your physician regularly § Weigh yourself daily & call your RN/MD if gaining § Limit salt and fluid intake § Exercise at a level recommended by your physician § Avoid smoking § Keep your flu and pneumonia vaccines current § Take your medications § Take an active role in managing your health!
For More Information About Heart Failure… The Heart Failure Society of America via their website: Patients and caregivers– www. abouthf. org

 Ayesha hasan md
Ayesha hasan md Failure to sense
Failure to sense Pacer failure to sense
Pacer failure to sense Brittle vs ductile fracture
Brittle vs ductile fracture Dr ayesha anwar
Dr ayesha anwar Ayesha samad
Ayesha samad Umer zeeshan ijaz
Umer zeeshan ijaz Dr ayesha ghous pasha
Dr ayesha ghous pasha Halstead ligament
Halstead ligament Dr ayesha batool
Dr ayesha batool Edema assessment
Edema assessment Chlorpromide
Chlorpromide Congestive heart failure zones for management
Congestive heart failure zones for management Classification of ejection fraction
Classification of ejection fraction Cor pulmonale
Cor pulmonale Heart failure complications
Heart failure complications Acute vs chronic heart failure
Acute vs chronic heart failure Diabetes and heart failure
Diabetes and heart failure Lmnop heart failure
Lmnop heart failure Heart failure defined
Heart failure defined Heart failure cells are seen in lungs
Heart failure cells are seen in lungs Chapter 24 heart failure drugs
Chapter 24 heart failure drugs Right vs left-sided heart failure chart
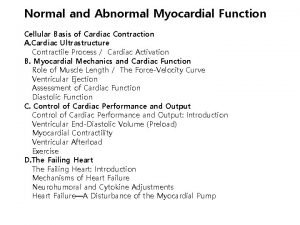
Right vs left-sided heart failure chart Compensatory mechanisms of heart failure
Compensatory mechanisms of heart failure Keith rn heart failure case study
Keith rn heart failure case study Causes of cardiomegaly in child
Causes of cardiomegaly in child Heart failure forward vs backward
Heart failure forward vs backward Heart failure
Heart failure Apetm
Apetm Lvedp normal range
Lvedp normal range Ecg findings of heart failure
Ecg findings of heart failure Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Is mold living or nonliving
Is mold living or nonliving Living non living dead
Living non living dead The smallest living unit of all living things is
The smallest living unit of all living things is Difference between living and non living organisms
Difference between living and non living organisms Heart dullness
Heart dullness Sheep heart anatomy
Sheep heart anatomy Hrt to hrt merrylands
Hrt to hrt merrylands Voorwoord bachelorproef
Voorwoord bachelorproef Hasan oben pullu
Hasan oben pullu Seorang pedagang membeli 1 kodi mainan seharga 280
Seorang pedagang membeli 1 kodi mainan seharga 280 Hasan irfan khan
Hasan irfan khan Hasan
Hasan Hasan cesur
Hasan cesur Sudden painless loss of vision
Sudden painless loss of vision Ahmad makki hasan
Ahmad makki hasan Gastrectomy anesthesia considerations
Gastrectomy anesthesia considerations