INTRO TO ACLS Department of Emergency Medicine University

- Slides: 53
INTRO TO ACLS Department of Emergency Medicine University of Manitoba Zoe Oliver, Cheryl ffrench, Shai Harel, Hareishun Shanmuganathan, Katie Sullivan
OBJECTIVES 1. Approach to the first three minutes of a code 2. Primer on the rest….
ACLS Clinical Rotation Resus Day Intro Lecture

Part 1: He Looks Dead Katie is a third year medical student on her Ortho rotation. She is pre-rounding on her patients in the morning. Pitfall: Started CPR before checking responsiveness
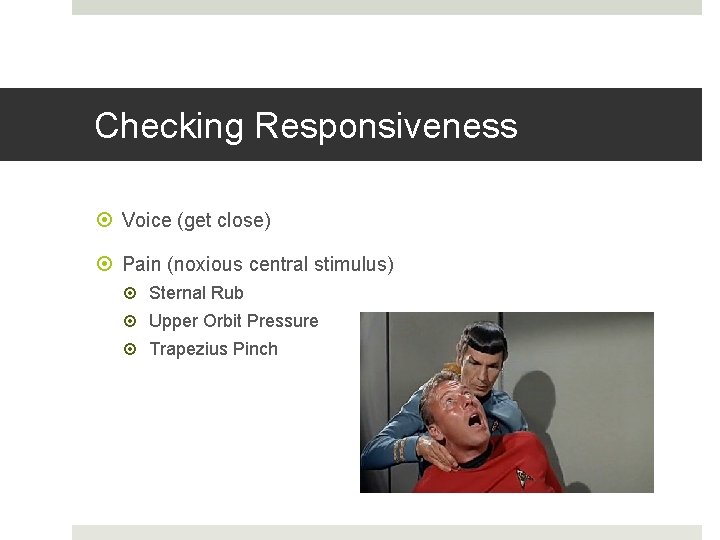
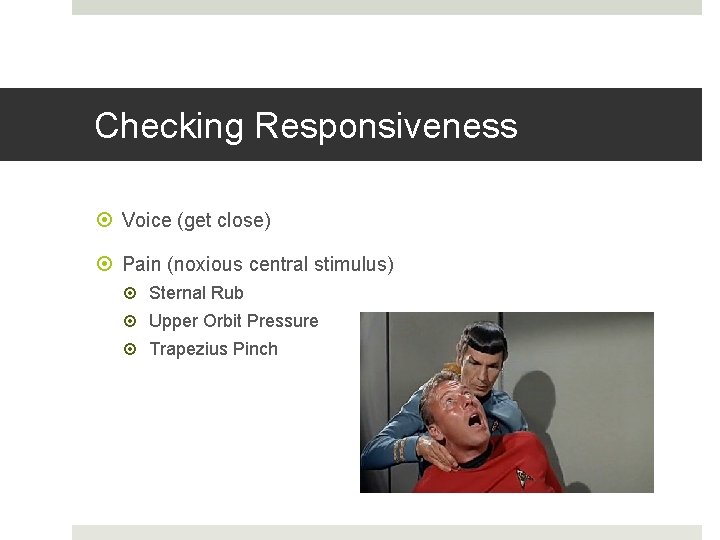
Checking Responsiveness Voice (get close) Pain (noxious central stimulus) Sternal Rub Upper Orbit Pressure Trapezius Pinch
Part 2 – He Is Dead Katie is a third year medical student on her Ortho rotation. She is pre-rounding on her patients in the morning. Pitfall: Didn’t call for help
Calling for help Check which room you’re in Go into hallway and look for nurse Get someone to check the code status No one there? Go to phone and dial ‘ 55’ for an emergency line Code Blue vs. Medical 25 vs. Code 88
Part 3 – How was your Weekend? Katie and Shai are third year med students prerounding on their Ortho rotation. They enter a four bed room together. Katie’s patient, “doesn’t look right”. Pitfall: Didn’t activate BLS
Activating the BLS Primary Survey A B C (D)
BLS Primary Survey • • Airway Breathing Circulation Defibrillation Simple interventions
Part 4 – He’s Not Perking Up Pitfall: Katie and Shai decide to activate BLS. Didn’t open airway Gave inadequate breaths Radial pulse check
Airway Primary
Breathing • Give 2 breaths • NO response? 1 breath / 5 seconds and CPR Primary
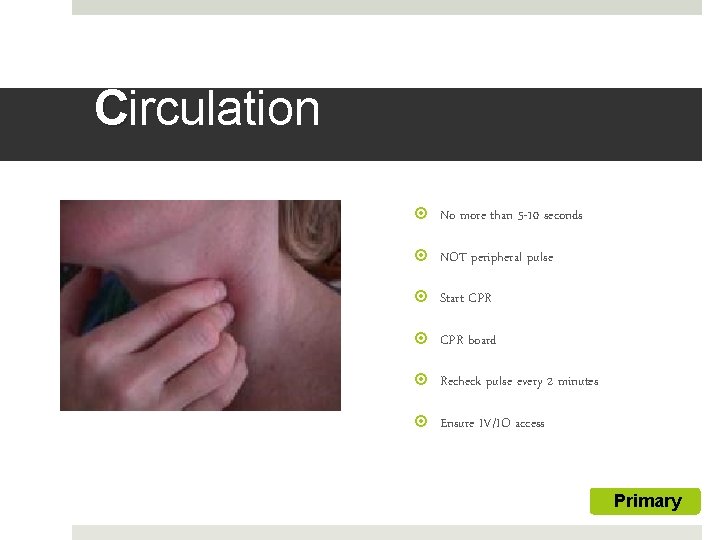
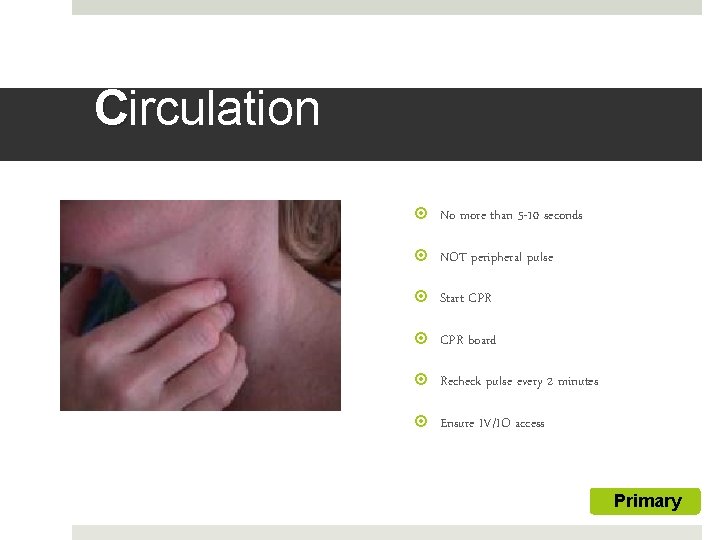
Circulation No more than 5 -10 seconds NOT peripheral pulse Start CPR board Recheck pulse every 2 minutes Ensure IV/IO access Primary
Part 5: The Team Will be Here Soon Previous scenario continues Ward resident Hareishun runs into the room… Pitfall: Too many CPR interruptions
CPR board 100 compressions/minute 30: 2 breaths Hard and fast
Parts 1 -5: The Replay
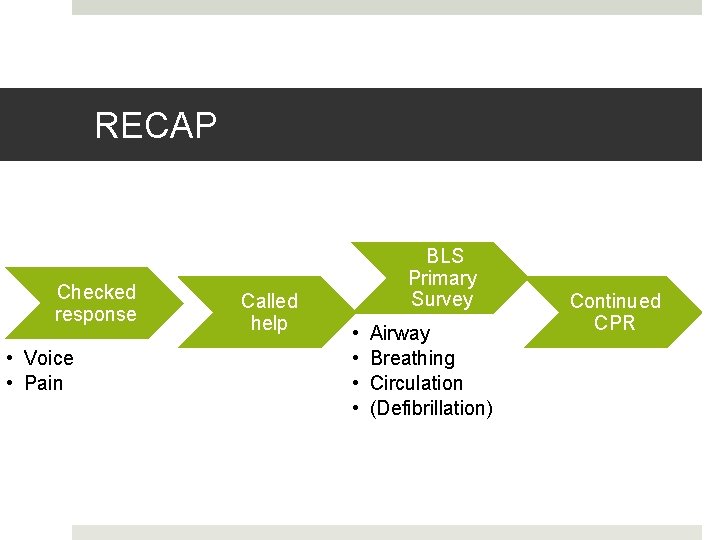
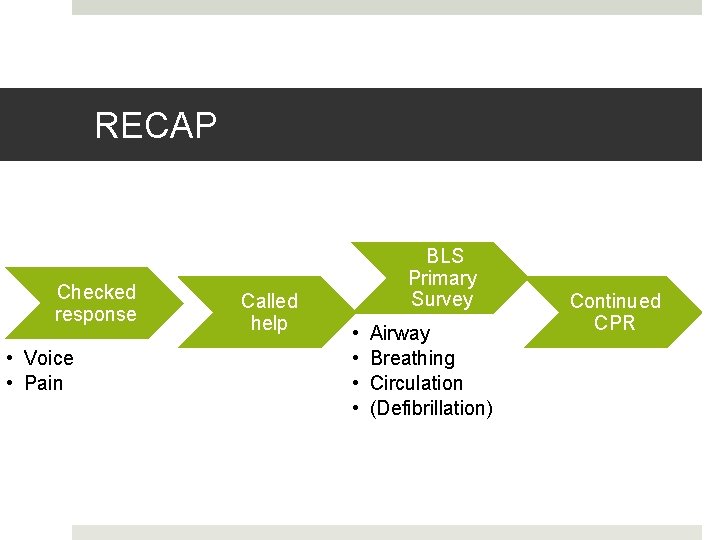
RECAP Checked response • Voice • Pain Called help BLS Primary Survey • • Airway Breathing Circulation (Defibrillation) Continued CPR
Who’s on the code team? • Code team leader • More doctors if they happen to be around • Nurses • Record keeper, someone to give meds • RT • Orderly • CPR
How does the code team work? • Code team leader: • • • Makes it clear who is in charge Call for quiet if there’s too much noise Stands at pt’s side, hand on pulse (femoral) If possible, delegate tasks to others Closed-loop communication Maintain sense of ‘big picture’
What the team leader will ask you…. Patient name, age, reason for admission Past medical history CODE STATUS Time of arrest, events leading up
What next? Repeat the BLS Primary Survey Can now do ‘D’ A B C D
Defibrillation In hospital: will not have AED immediately available At casino: No pulse power-on AED and follow voice prompts Apply pads Administer shock as directed
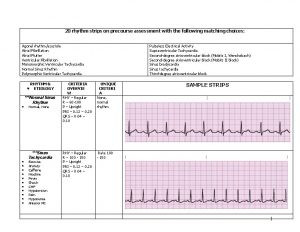
D: Rhythm Recognition Once you know the rhythm, you can follow the algorithm Today: Non-Perfusing Rhythms
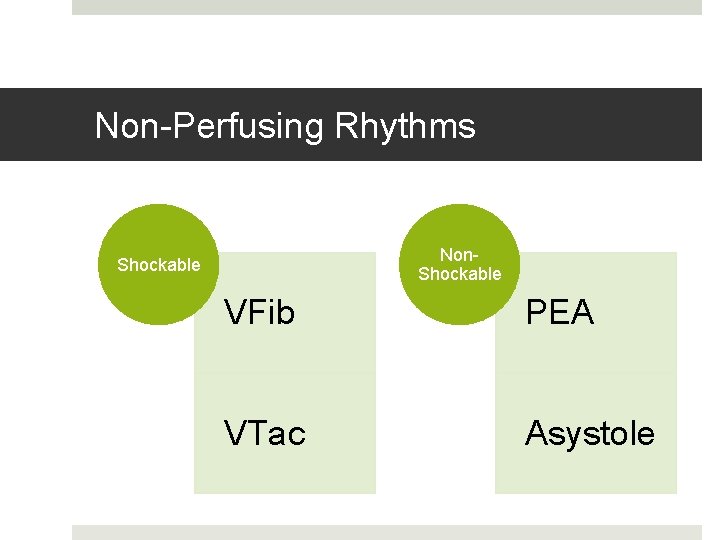
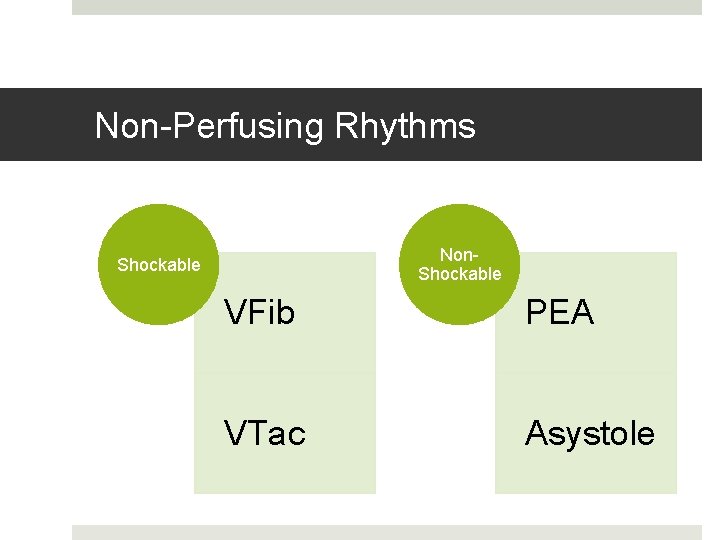
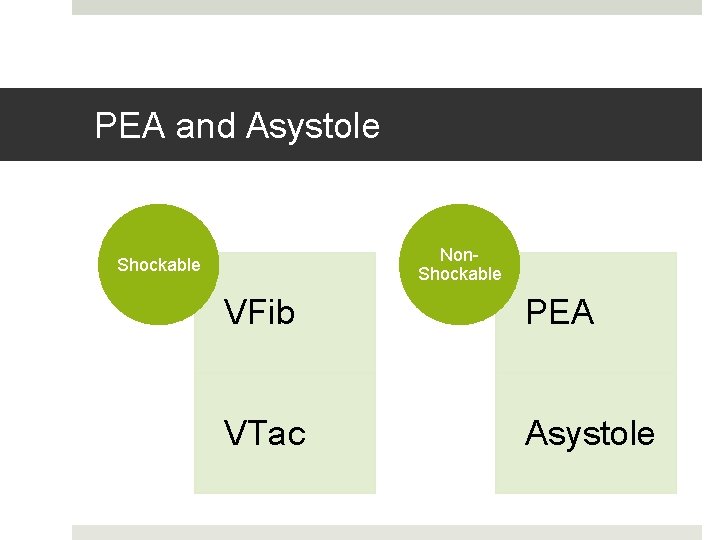
Non-Perfusing Rhythms Non. Shockable VFib PEA VTac Asystole
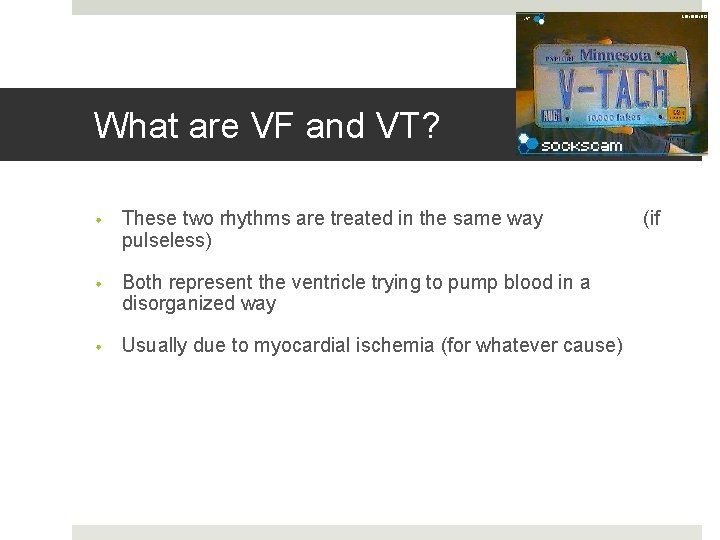
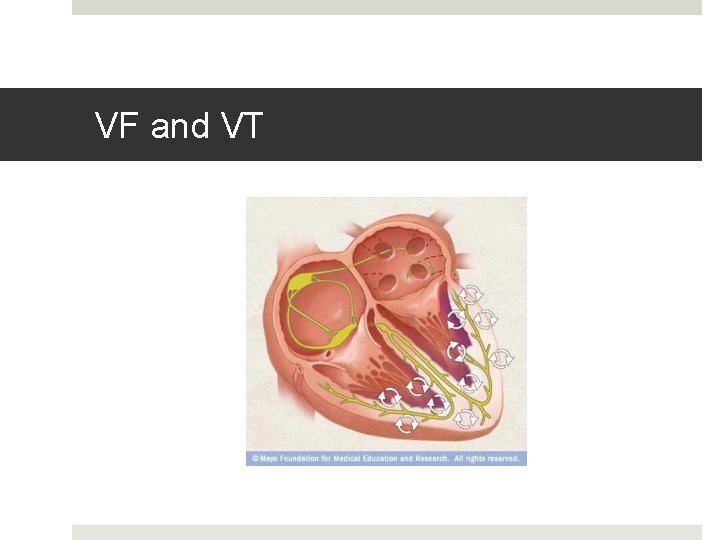
What are VF and VT? • These two rhythms are treated in the same way pulseless) • Both represent the ventricle trying to pump blood in a disorganized way • Usually due to myocardial ischemia (for whatever cause) (if
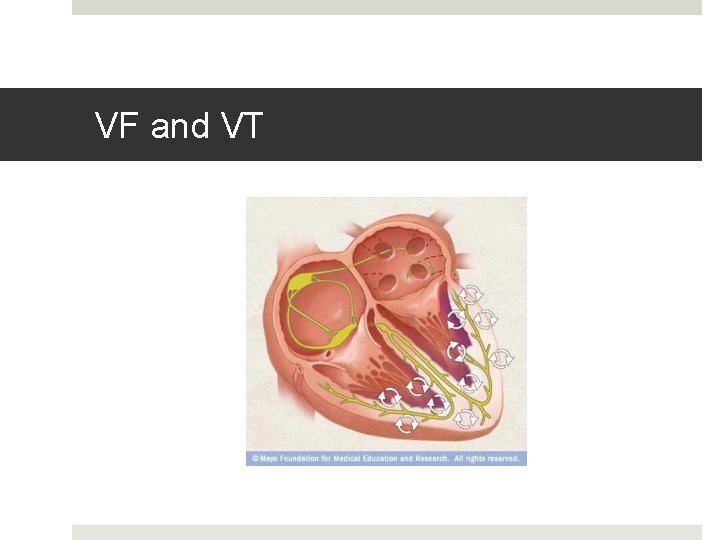
VF and VT
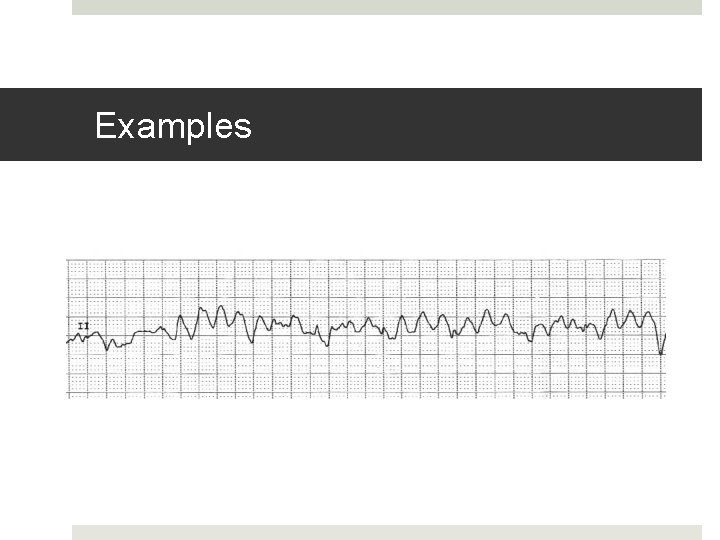
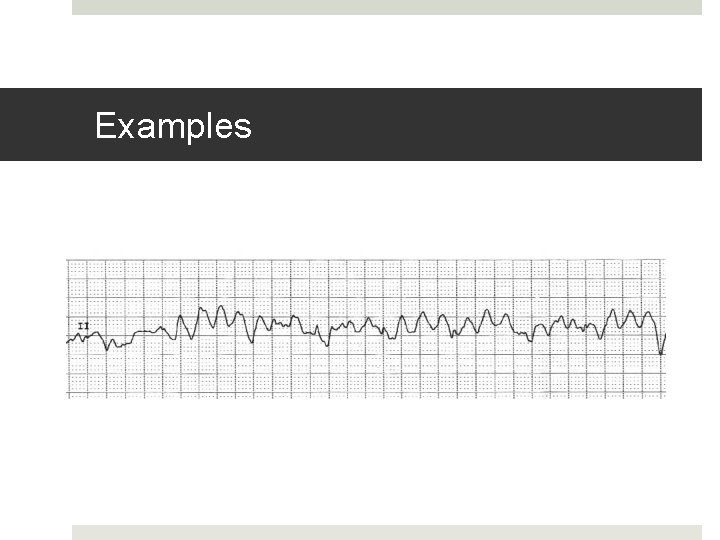
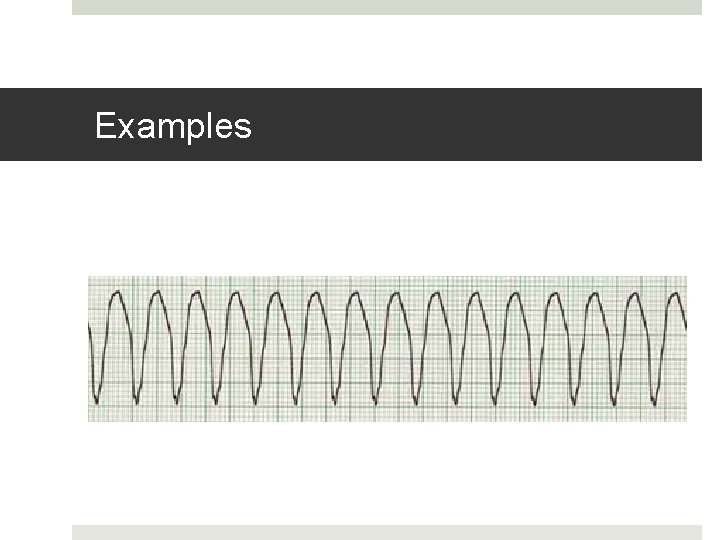
Examples
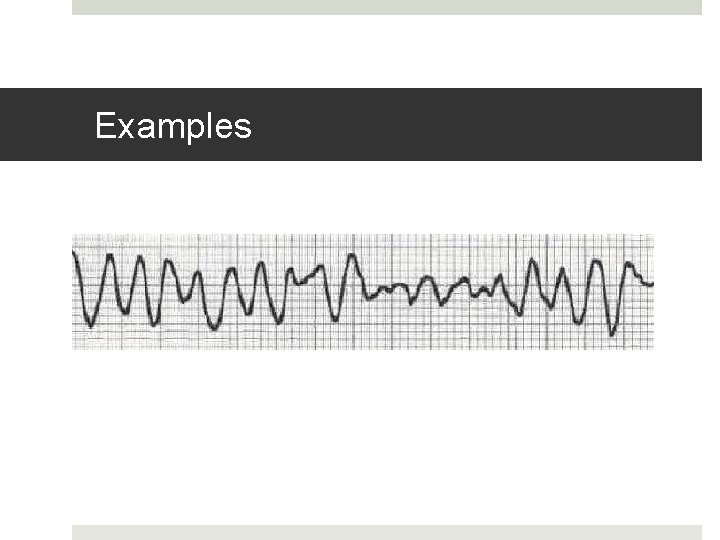
Examples
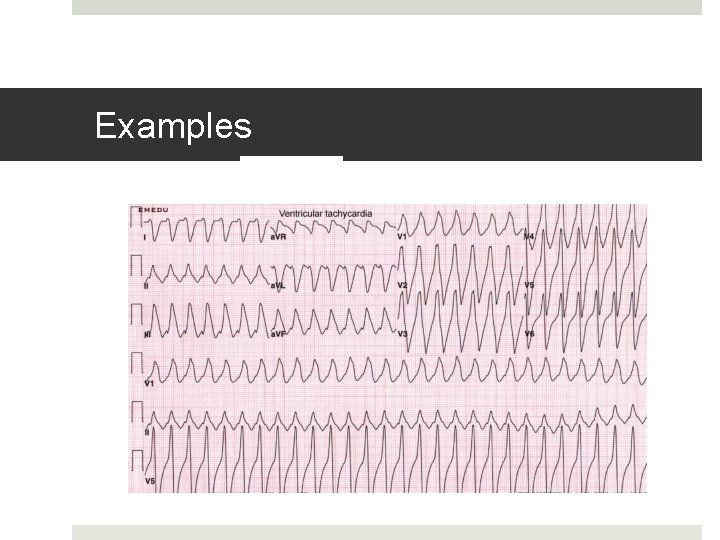
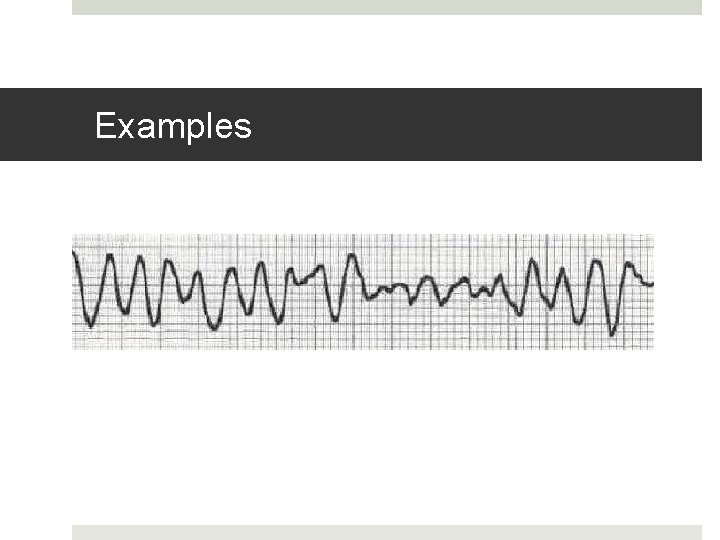
Examples
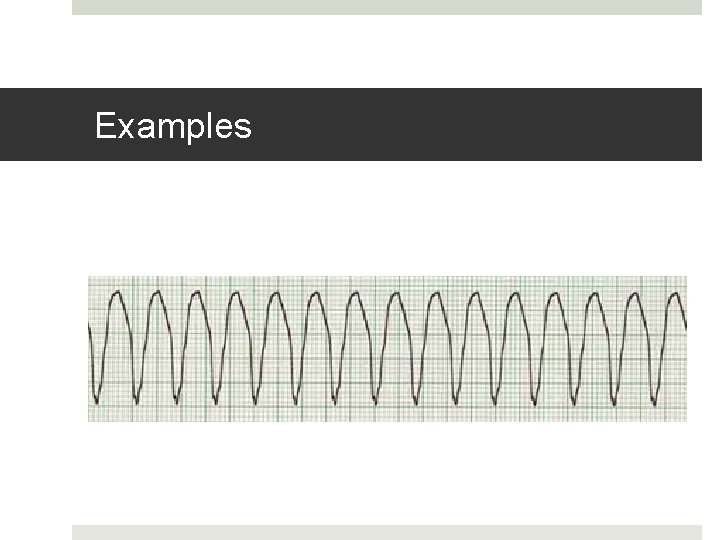
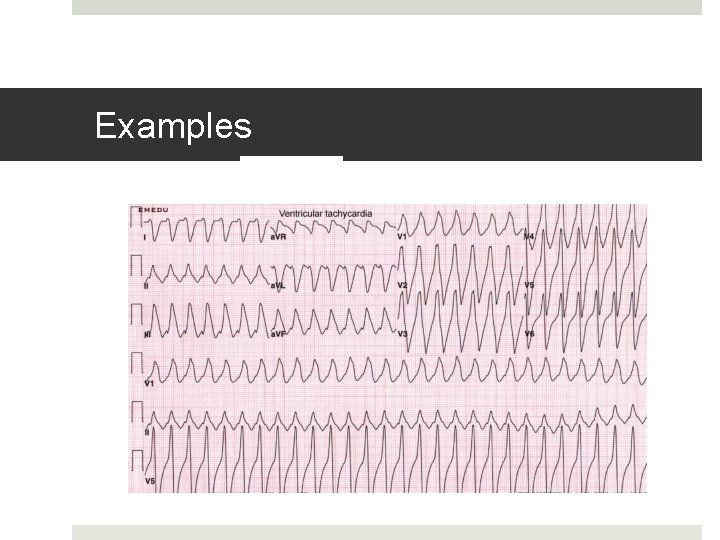
Examples
Defibrillators 101
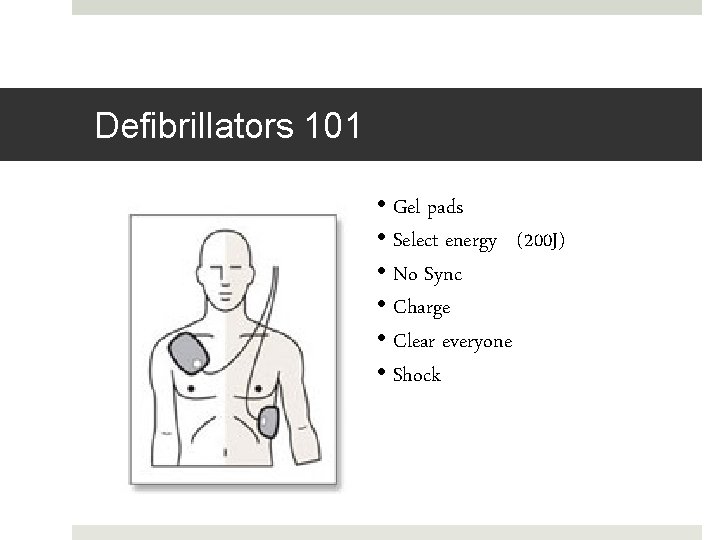
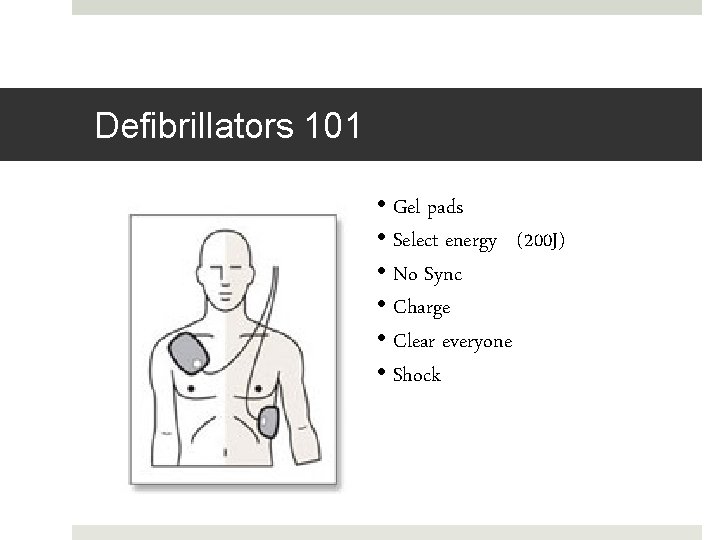
Defibrillators 101 • Gel pads • Select energy (200 J) • No Sync • Charge • Clear everyone • Shock
Putting it together • You’ve found an unresponsive patient • Called a code • Did as much of the BLS primary survey as you could • Code team has arrived and repeated the primary survey, including defibrillation if needed
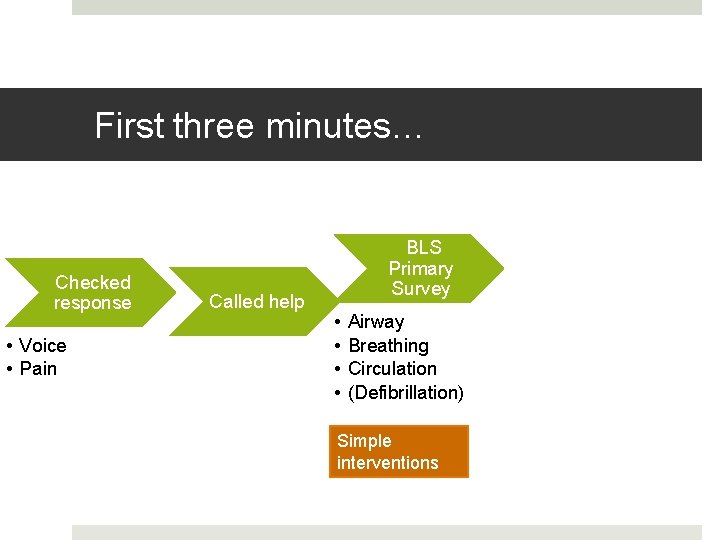
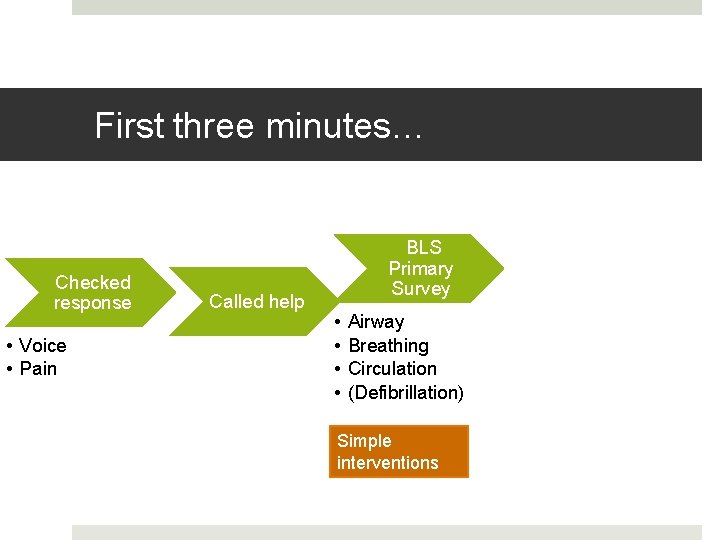
First three minutes… Checked response • Voice • Pain Called help BLS Primary Survey • • Airway Breathing Circulation (Defibrillation) Simple interventions
OBJECTIVES 1. Approach to the first three minutes of a code 2. Primer on the rest….
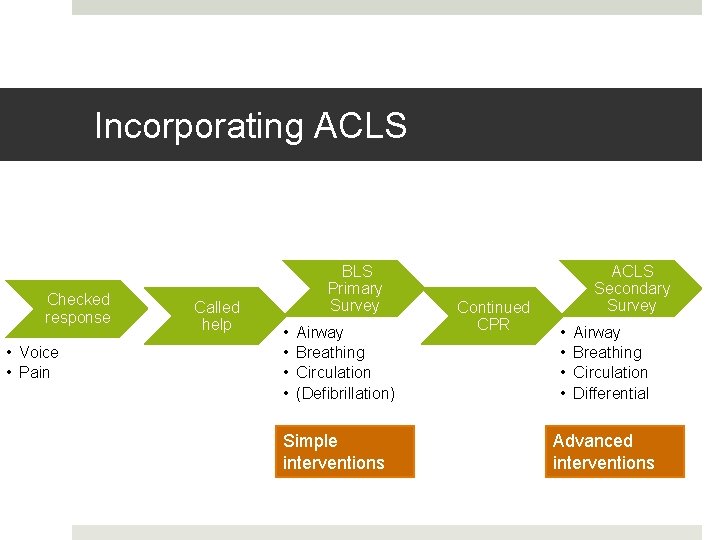
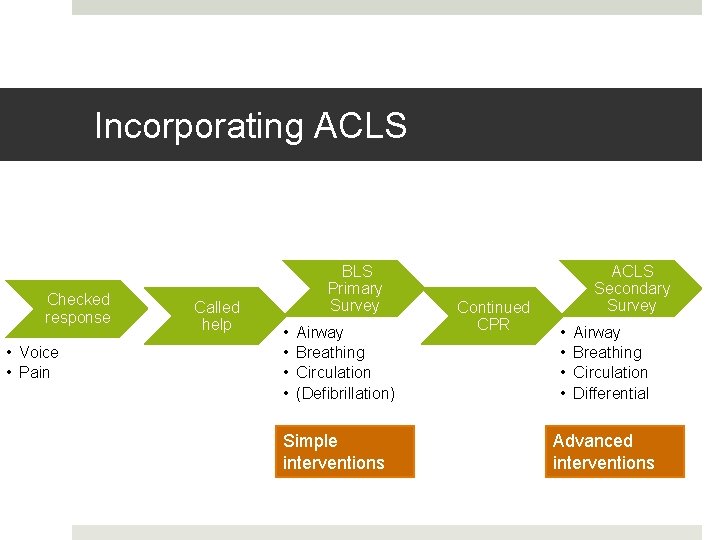
Incorporating ACLS Checked response • Voice • Pain Called help BLS Primary Survey • • Airway Breathing Circulation (Defibrillation) Simple interventions Continued CPR ACLS Secondary Survey • • Airway Breathing Circulation Differential Advanced interventions
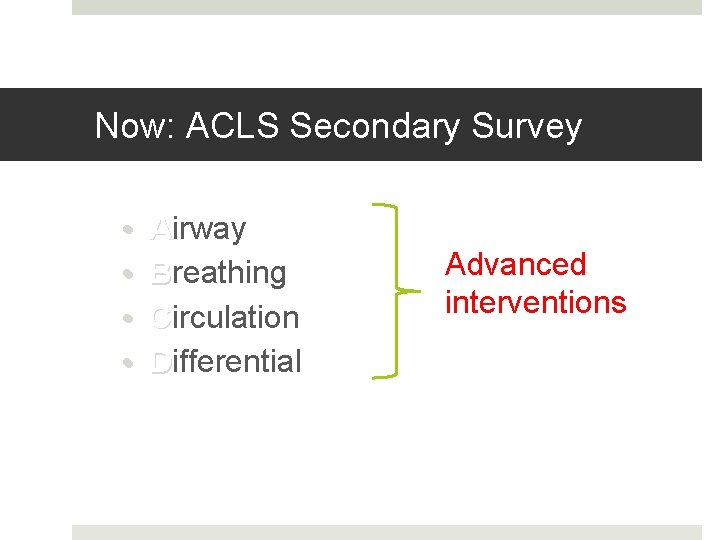
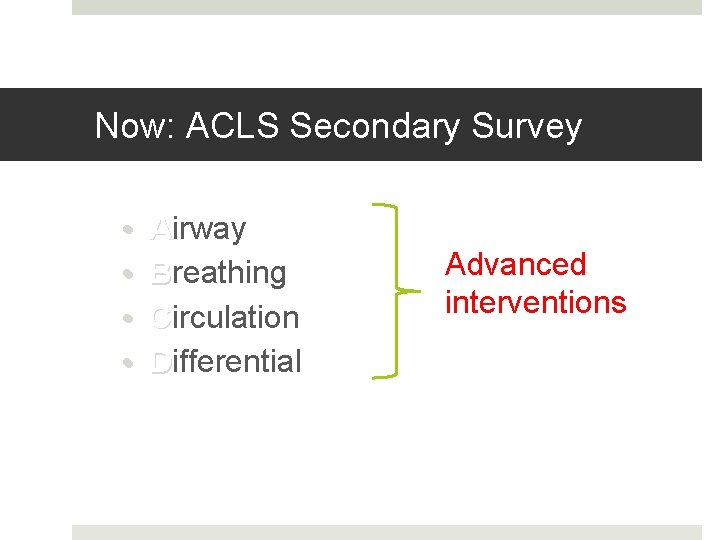
Now: ACLS Secondary Survey • • Airway Breathing Circulation Differential Advanced interventions
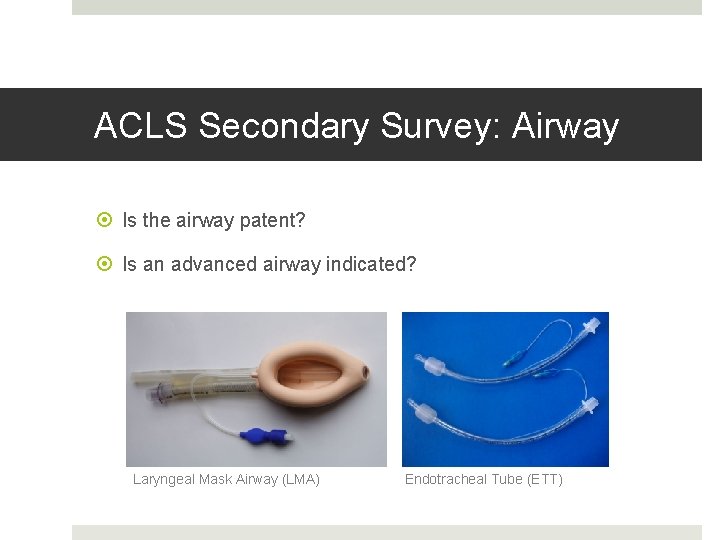
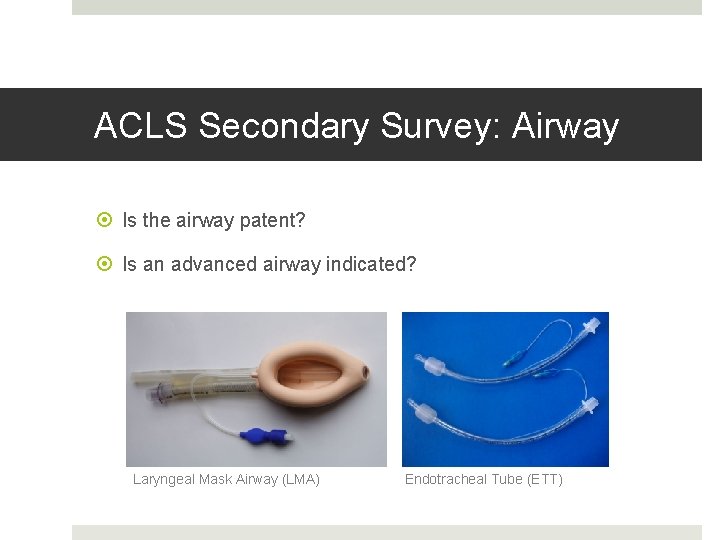
ACLS Secondary Survey: Airway Is the airway patent? Is an advanced airway indicated? Laryngeal Mask Airway (LMA) Endotracheal Tube (ETT)
ACLS Secondary Survey: Breathing Is the airway in the right place? Is the tube secure? Are we monitoring O 2 and CO 2?
ACLS Secondary Survey: Circulation What is/was the rhythm? Is there IV access? Is fluid needed? Are drugs needed?
ACLS Secondary Survey: Differential Why did the patient arrest? Is there a reversible cause for the arrest?
Part 6: Dream Team Code
PEA and Asystole Non. Shockable VFib PEA VTac Asystole
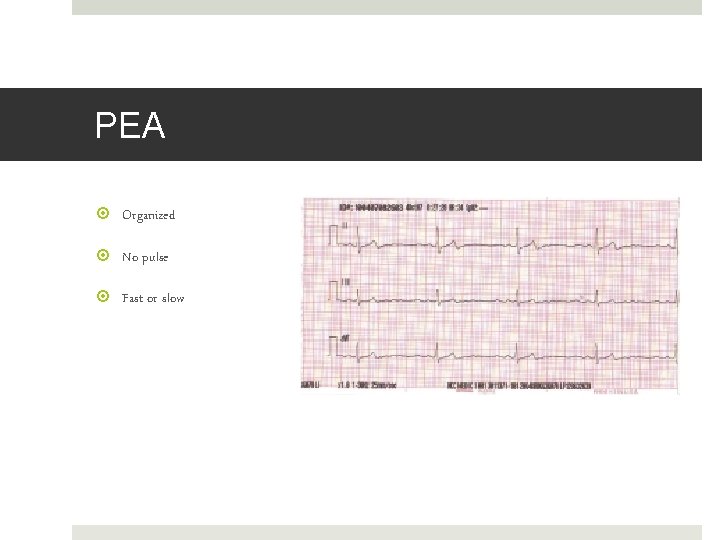
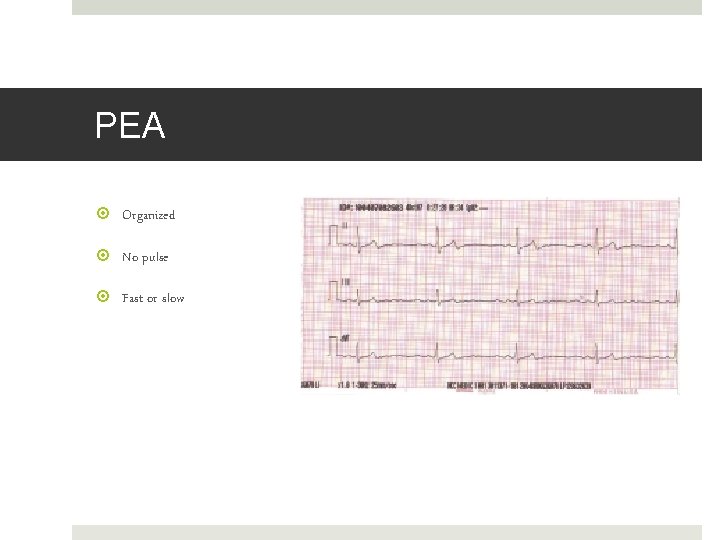
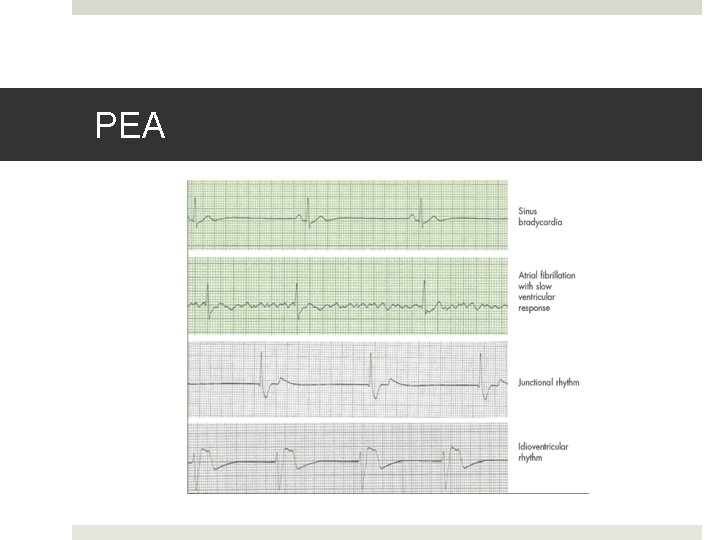
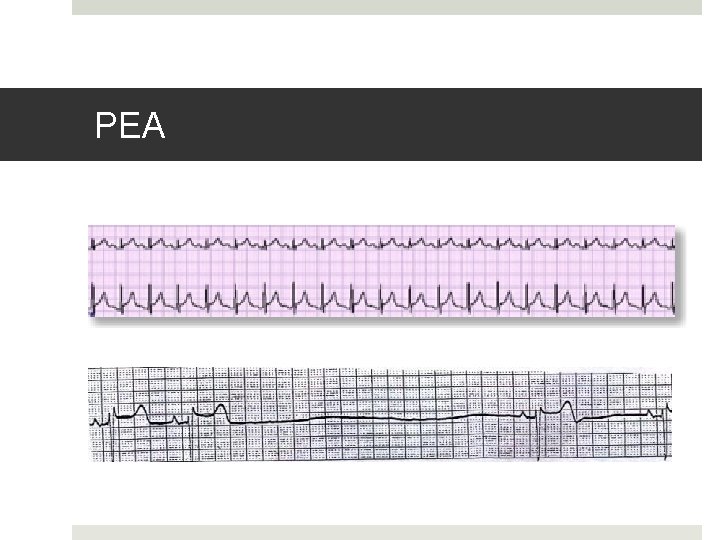
PEA Organized No pulse Fast or slow
PEA
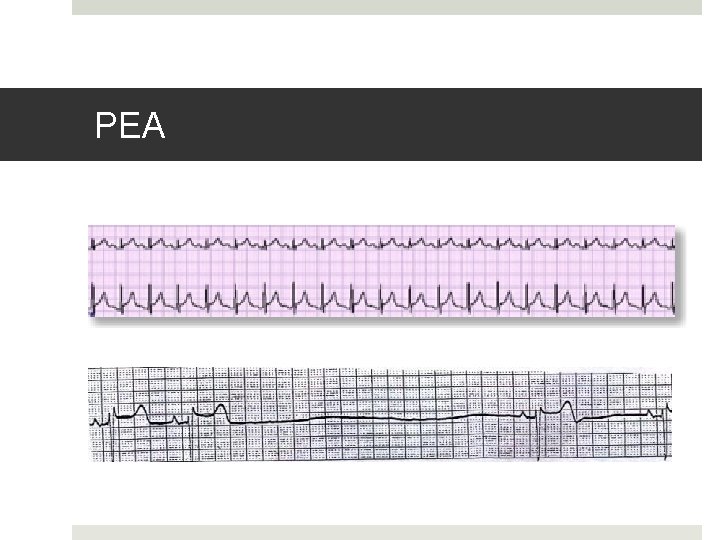
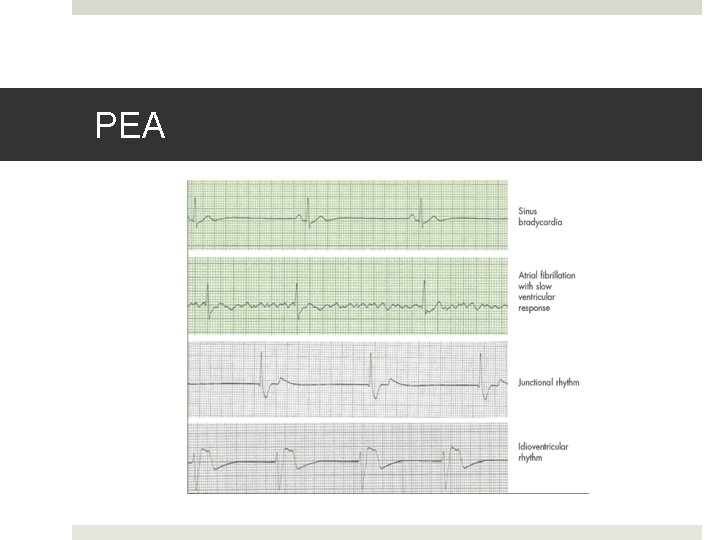
PEA
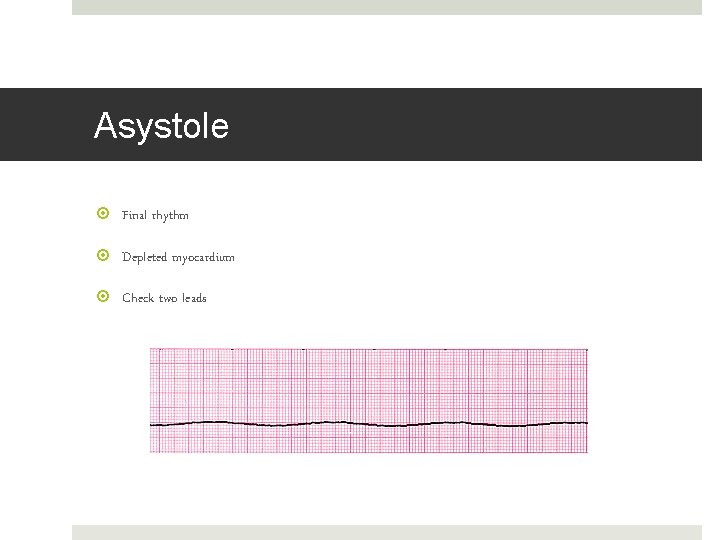
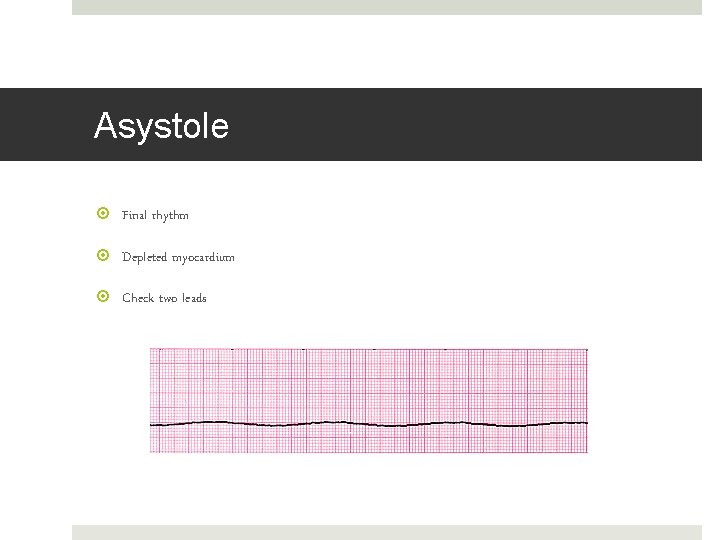
Asystole Final rhythm Depleted myocardium Check two leads
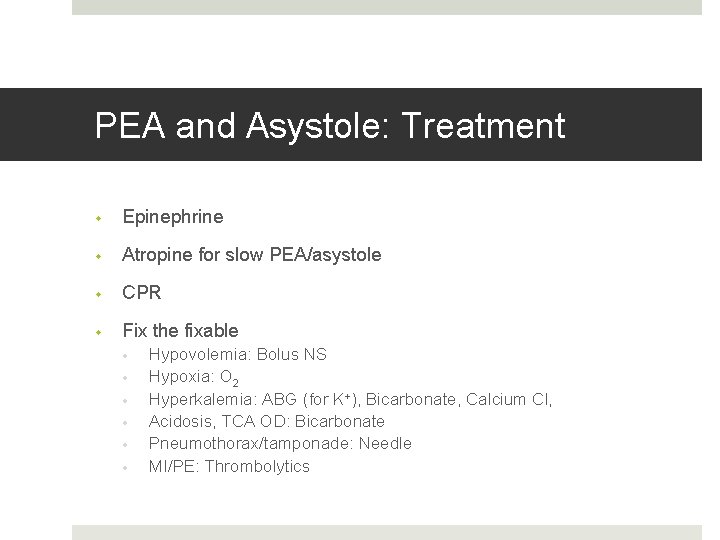
PEA and Asystole: Treatment • Epinephrine • Atropine for slow PEA/asystole • CPR • Fix the fixable • • • Hypovolemia: Bolus NS Hypoxia: O 2 Hyperkalemia: ABG (for K+), Bicarbonate, Calcium Cl, Acidosis, TCA OD: Bicarbonate Pneumothorax/tamponade: Needle MI/PE: Thrombolytics
Part 7: An hour later…. . The Dream Team is still at it: Switch to the other side of the flowchart
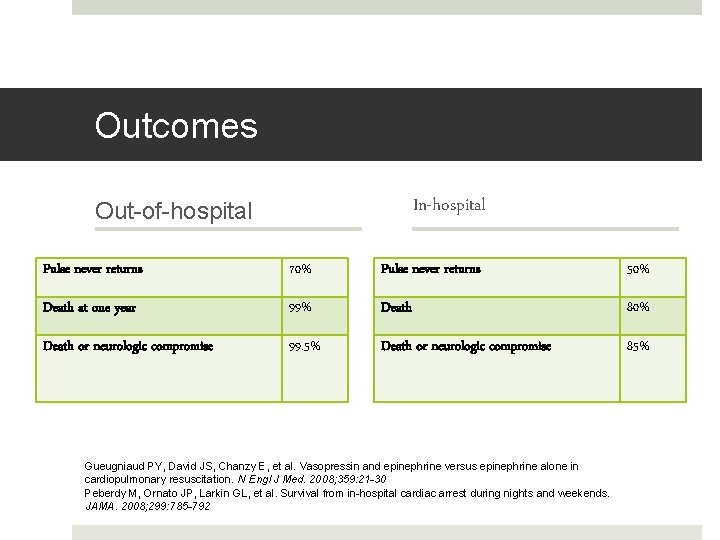
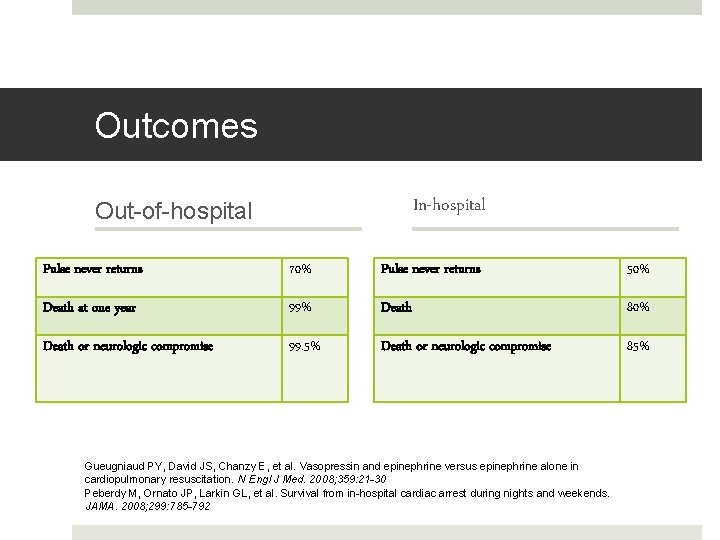
Outcomes In-hospital Out-of-hospital Pulse never returns 70% Pulse never returns 50% Death at one year 99% Death 80% Death or neurologic compromise 99. 5% Death or neurologic compromise 85% Gueugniaud PY, David JS, Chanzy E, et al. Vasopressin and epinephrine versus epinephrine alone in cardiopulmonary resuscitation. N Engl J Med. 2008; 359: 21 -30 Peberdy M, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008; 299: 785 -792
Questions?
 University of arizona emergency medicine
University of arizona emergency medicine Cmc vellore emergency medicine
Cmc vellore emergency medicine Emergency medicine case presentation
Emergency medicine case presentation Dutch north sea emergency medicine conference
Dutch north sea emergency medicine conference Unm internal medicine residency
Unm internal medicine residency Emergency department nursing orientation manual
Emergency department nursing orientation manual Whittington urgent care centre
Whittington urgent care centre Emergency care harrow
Emergency care harrow Sfgh emergency department
Sfgh emergency department Department of medicine solna
Department of medicine solna Mcgill medicine supporting documents
Mcgill medicine supporting documents Indikasi nasopharyngeal airway
Indikasi nasopharyngeal airway Abcd acls
Abcd acls Atenolol to carvedilol conversion chart
Atenolol to carvedilol conversion chart Acls rhythm recognition
Acls rhythm recognition Acls flowsheet
Acls flowsheet Acls bradycardia algorithm
Acls bradycardia algorithm Acls ventricular tachycardia
Acls ventricular tachycardia Agonal rhythm asystole strip
Agonal rhythm asystole strip Acls 123
Acls 123 Algoritmo als 2020
Algoritmo als 2020 H's and t's acls
H's and t's acls Acls guidelines
Acls guidelines Acls algorithmus tachykardie
Acls algorithmus tachykardie Business services
Business services 6h 6t acls
6h 6t acls Aesp acls
Aesp acls 4h 4t
4h 4t Acls ettc
Acls ettc Postparo fases
Postparo fases What is acls
What is acls Tulane university emergency management
Tulane university emergency management Victor babeş university of medicine and pharmacy
Victor babeş university of medicine and pharmacy Hubert kairuki memorial university faculty of medicine
Hubert kairuki memorial university faculty of medicine Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Lincoln memorial university college of veterinary medicine
Lincoln memorial university college of veterinary medicine King saud university college of medicine
King saud university college of medicine King saud university college of medicine
King saud university college of medicine King saud university college of medicine
King saud university college of medicine Applied medical sciences
Applied medical sciences Uw integrative medicine
Uw integrative medicine Victor babeş university of medicine and pharmacy
Victor babeş university of medicine and pharmacy Victor babes university of medicine
Victor babes university of medicine Semmelweis university faculty of medicine
Semmelweis university faculty of medicine King saud university college of medicine
King saud university college of medicine Faculty of veterinary medicine cairo university logo
Faculty of veterinary medicine cairo university logo Veterinary university brno
Veterinary university brno Slu family medicine residency
Slu family medicine residency Hacettepe university faculty of medicine
Hacettepe university faculty of medicine Enteroclysis vs barium follow-through
Enteroclysis vs barium follow-through Dorsocranially
Dorsocranially Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Midwestern university college of dental medicine
Midwestern university college of dental medicine Seoul national university medical school
Seoul national university medical school