Histology of the male reproductive system Testis gonad
- Slides: 40
Histology of the male reproductive system
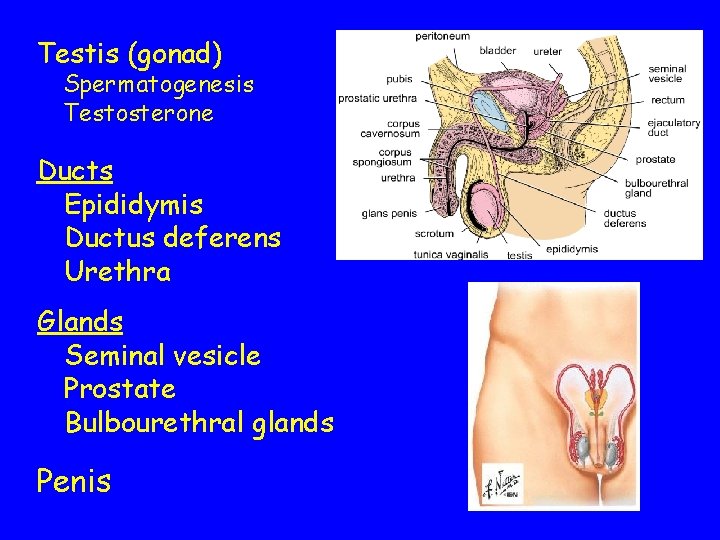
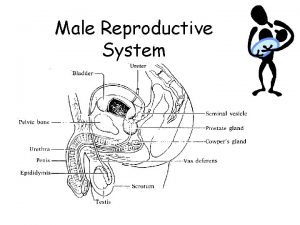
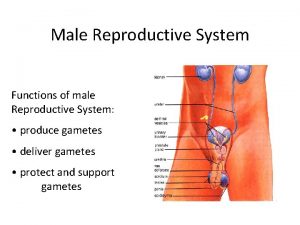
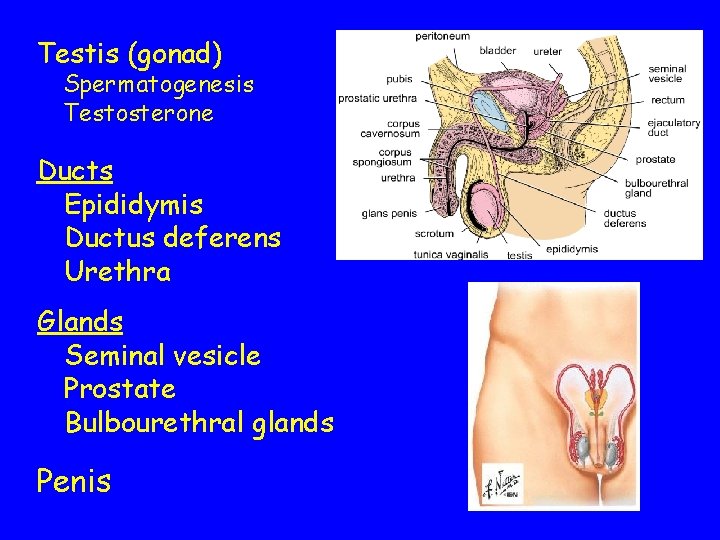
Testis (gonad) Spermatogenesis Testosterone Ducts Epididymis Ductus deferens Urethra Glands Seminal vesicle Prostate Bulbourethral glands Penis
Testis
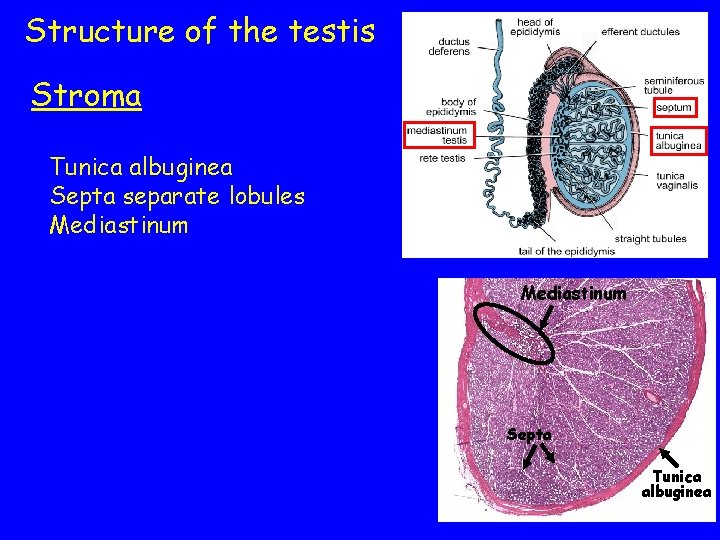
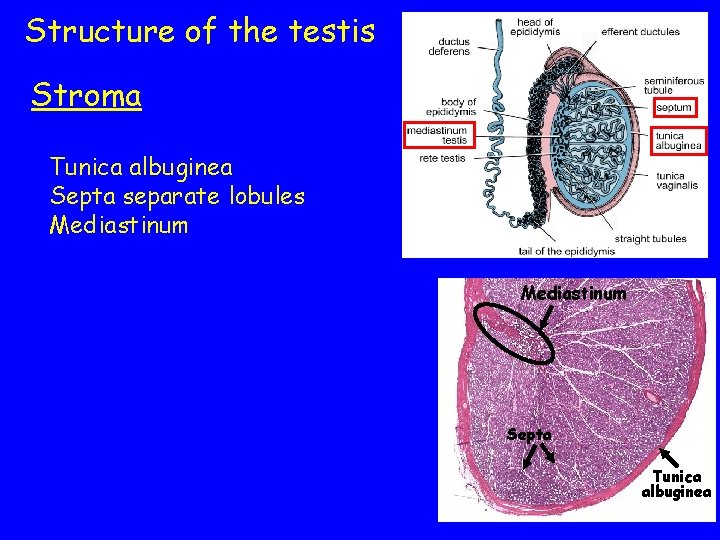
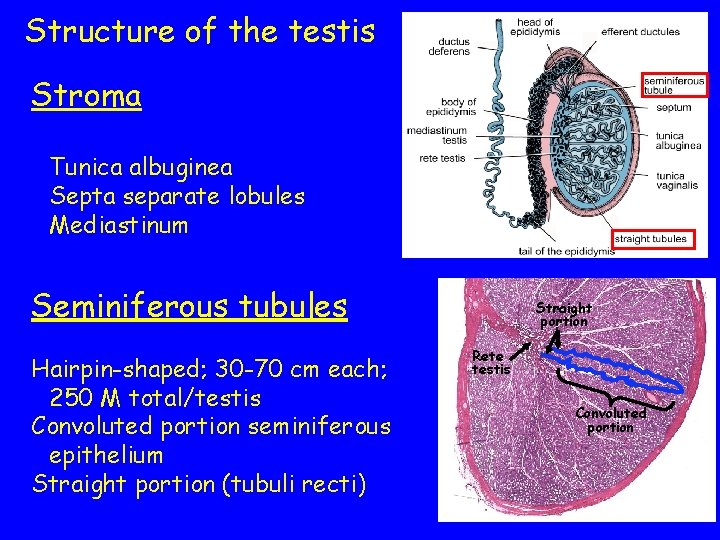
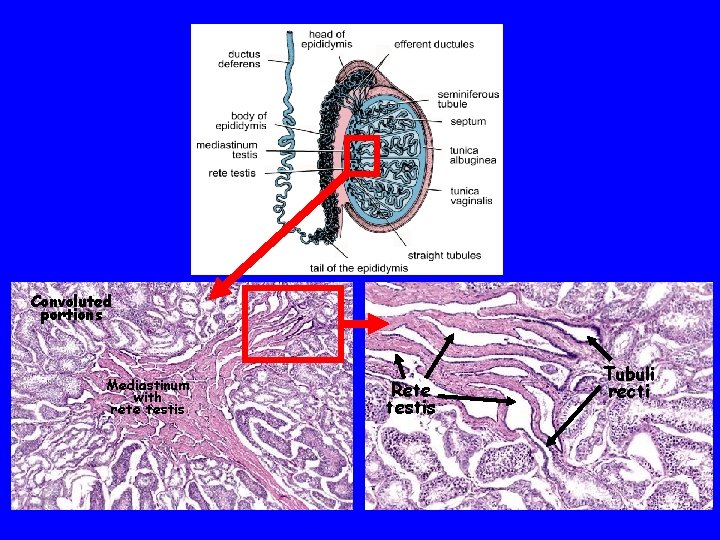
Structure of the testis Stroma Tunica albuginea Septa separate lobules Mediastinum Seminiferous tubules Hairpin-shaped; 30 -70 cm each; 250 M total/testis Convoluted portion seminiferous epithelium Straight portion (tubuli recti) Mediastinum Septa Tunica albuginea
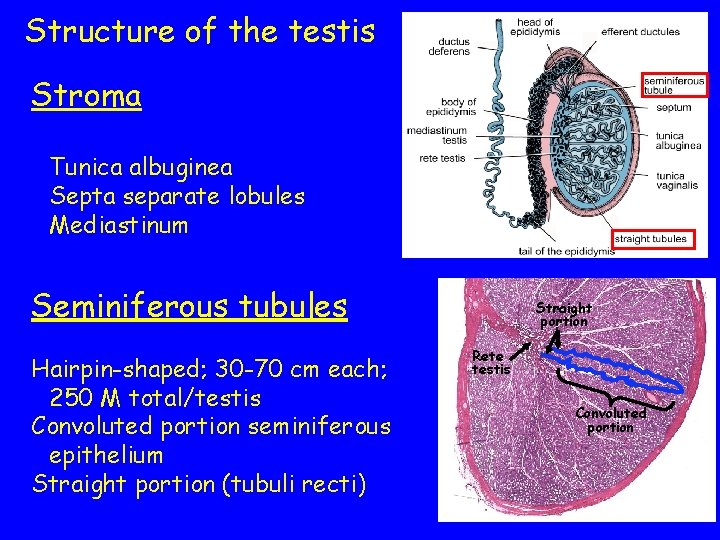
Structure of the testis Stroma Tunica albuginea Septa separate lobules Mediastinum Seminiferous tubules Hairpin-shaped; 30 -70 cm each; 250 M total/testis Convoluted portion seminiferous epithelium Straight portion (tubuli recti) Straight portion Rete testis Convoluted portion
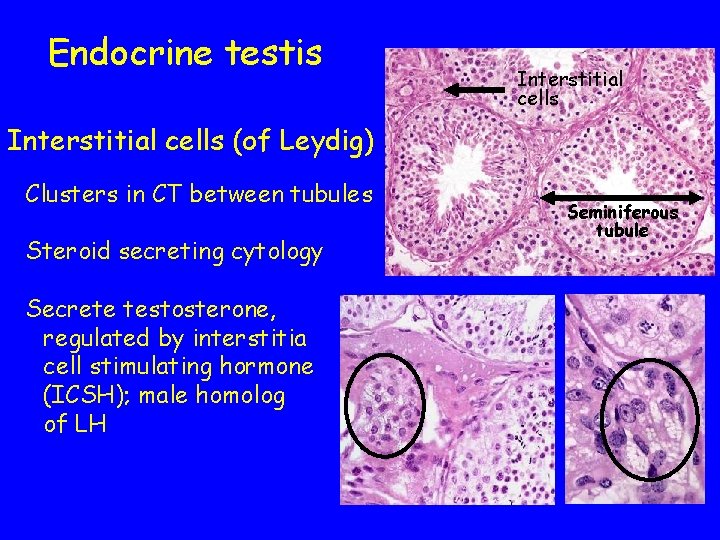
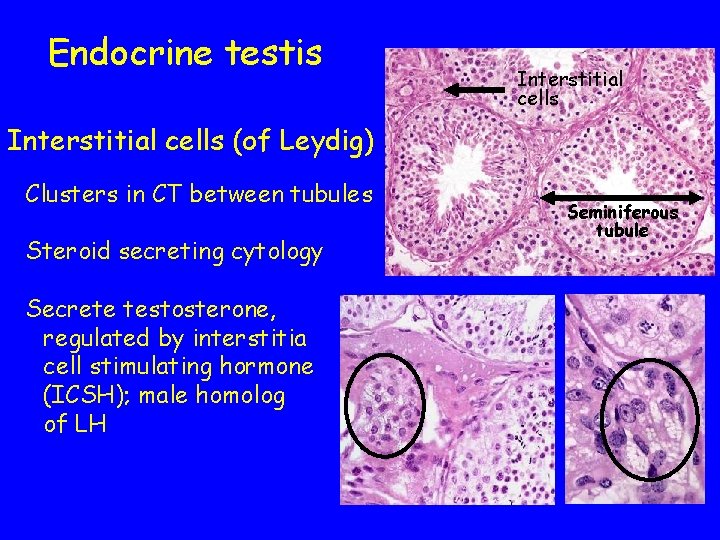
Endocrine testis Interstitial cells (of Leydig) Clusters in CT between tubules Steroid secreting cytology Secrete testosterone, regulated by interstitia cell stimulating hormone (ICSH); male homolog of LH Seminiferous tubule
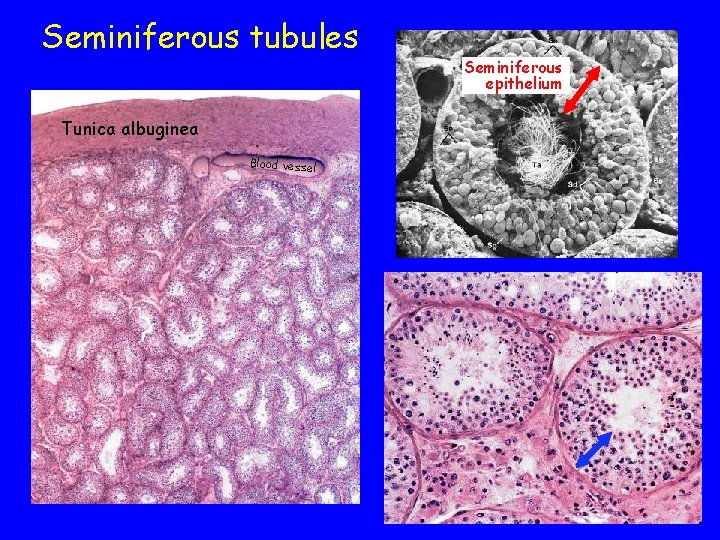
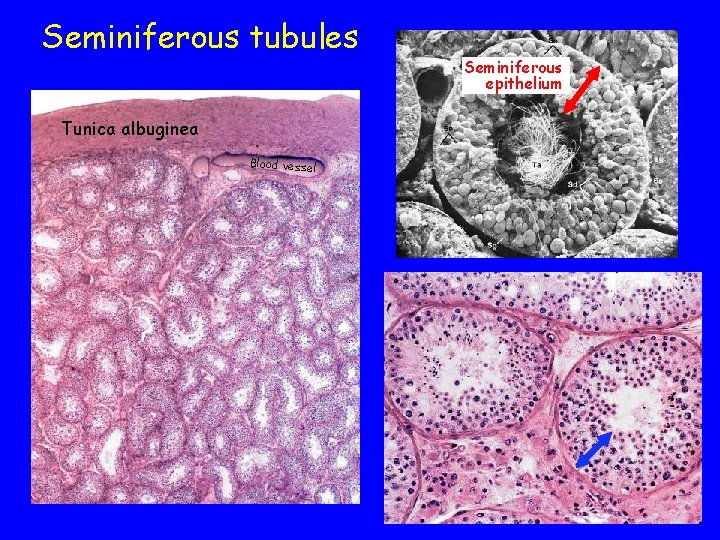
Seminiferous tubules Tunica albuginea Blood vessel Seminiferous epithelium
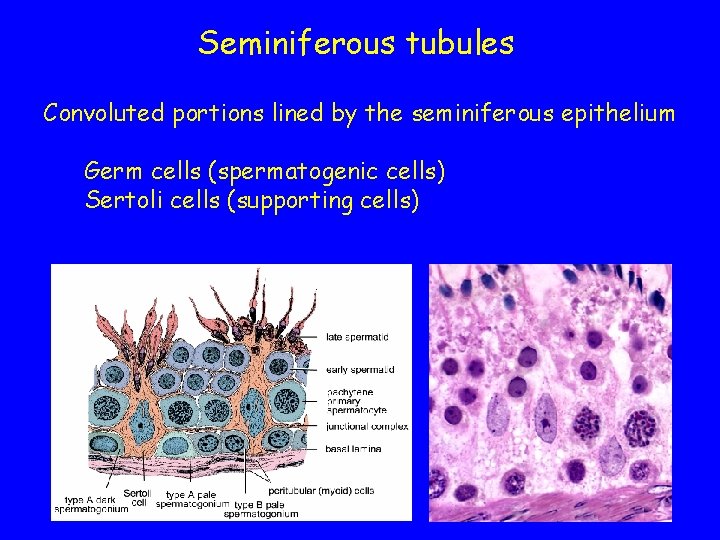
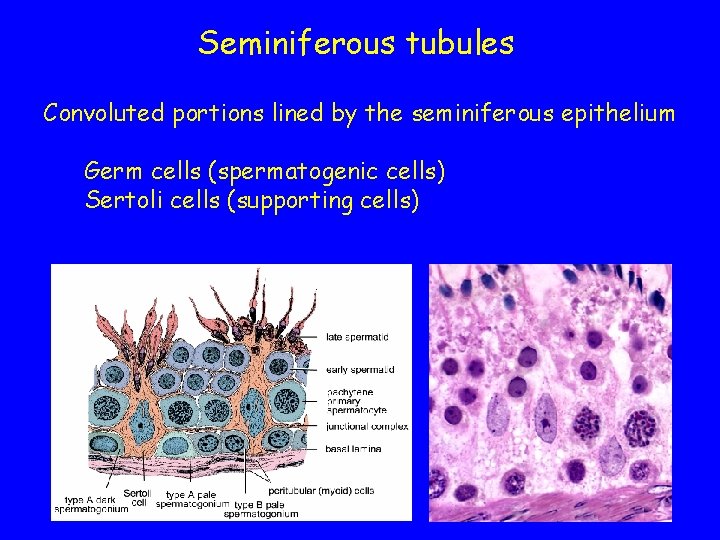
Seminiferous tubules Convoluted portions lined by the seminiferous epithelium Germ cells (spermatogenic cells) Sertoli cells (supporting cells)
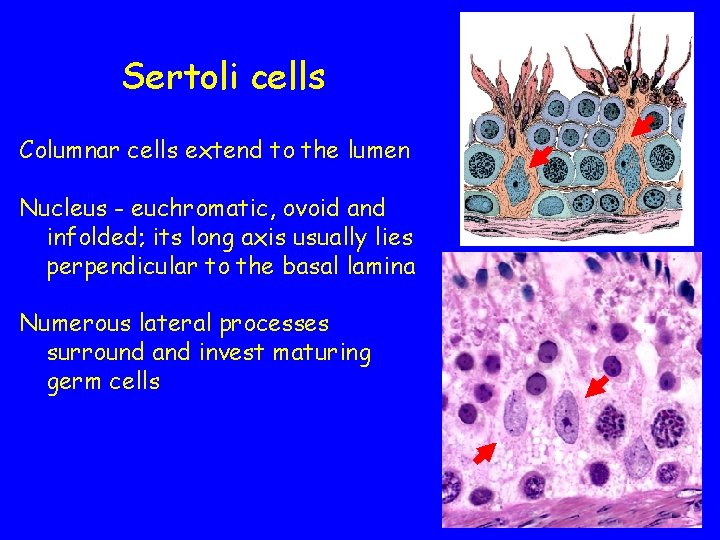
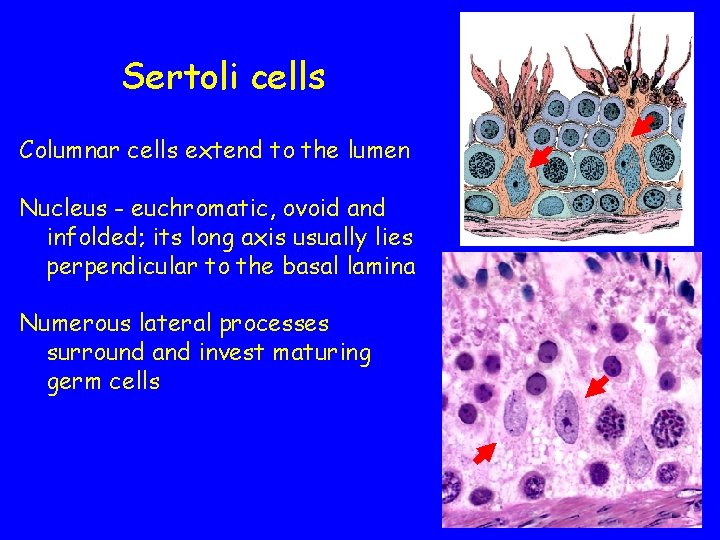
Sertoli cells Columnar cells extend to the lumen Nucleus - euchromatic, ovoid and infolded; its long axis usually lies perpendicular to the basal lamina Numerous lateral processes surround and invest maturing germ cells
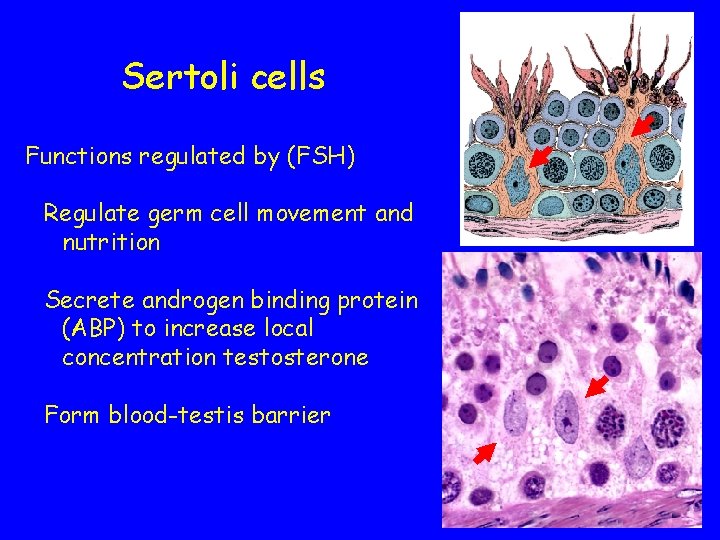
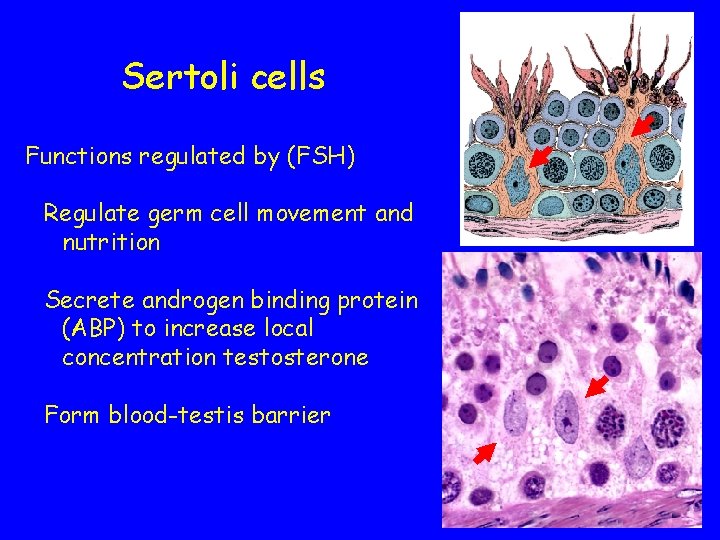
Sertoli cells Functions regulated by (FSH) Regulate germ cell movement and nutrition Secrete androgen binding protein (ABP) to increase local concentration testosterone Form blood-testis barrier
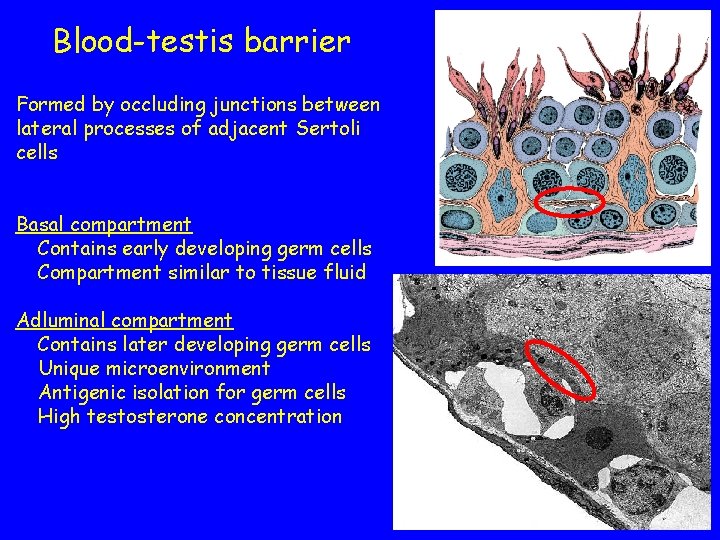
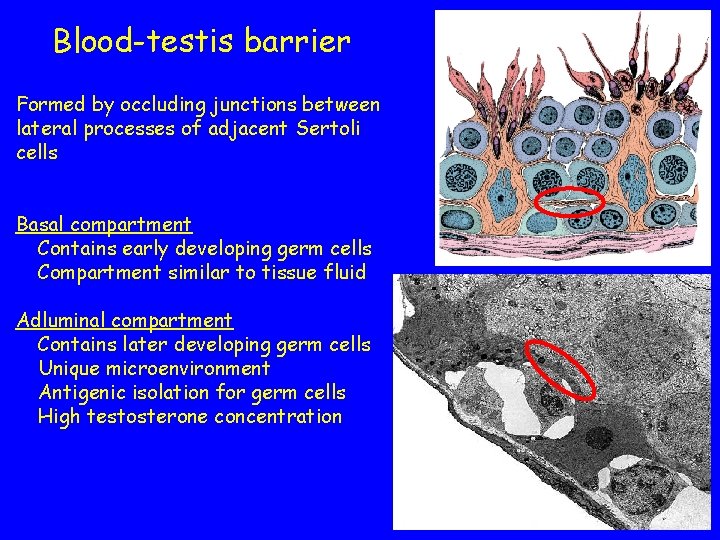
Blood-testis barrier Formed by occluding junctions between lateral processes of adjacent Sertoli cells Basal compartment Contains early developing germ cells Compartment similar to tissue fluid Adluminal compartment Contains later developing germ cells Unique microenvironment Antigenic isolation for germ cells High testosterone concentration
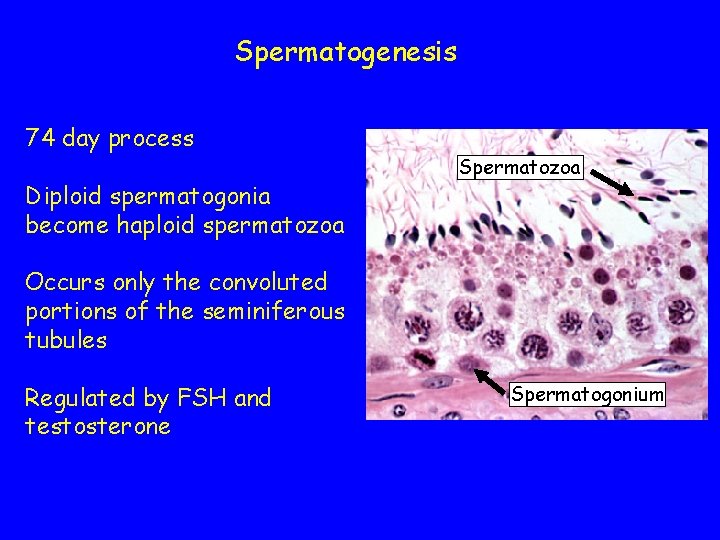
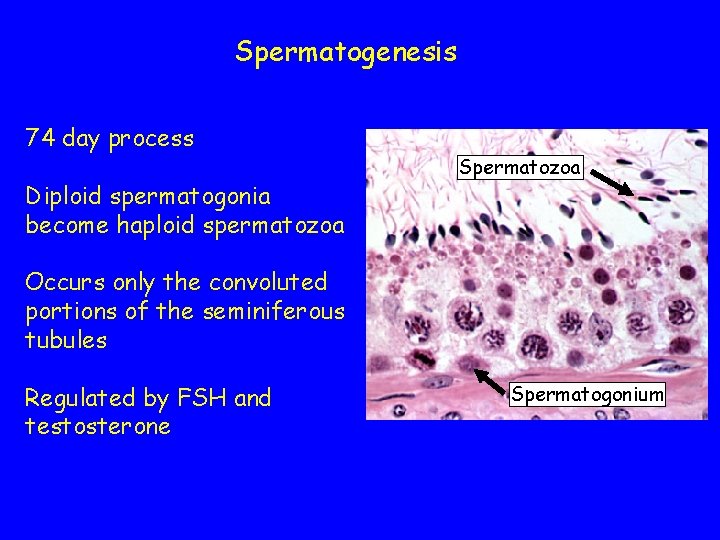
Spermatogenesis 74 day process Diploid spermatogonia become haploid spermatozoa Spermatozoa Occurs only the convoluted portions of the seminiferous tubules Regulated by FSH and testosterone Spermatogonium
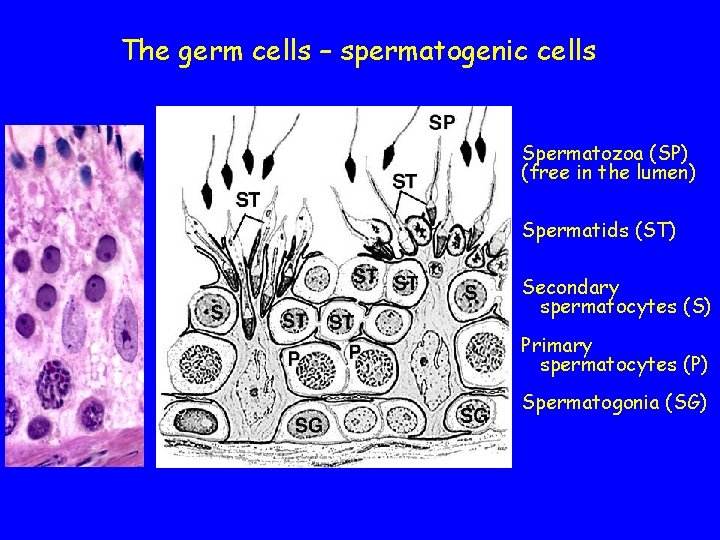
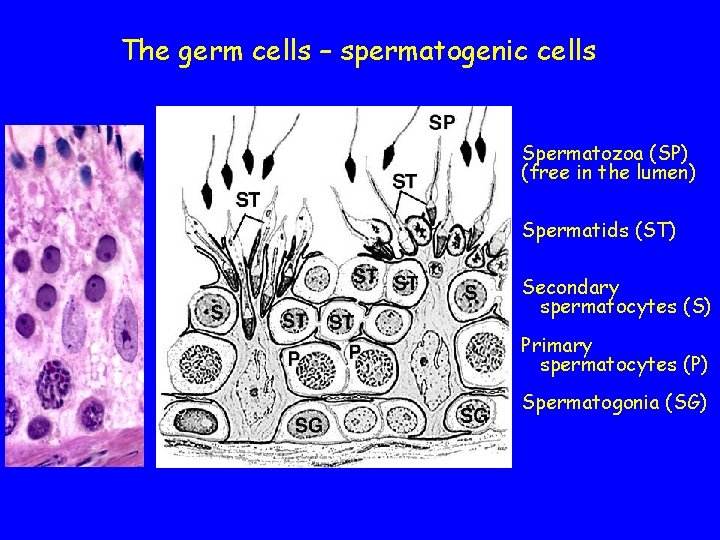
The germ cells – spermatogenic cells Spermatozoa (SP) (free in the lumen) Spermatids (ST) Secondary spermatocytes (S) Primary spermatocytes (P) Spermatogonia (SG)
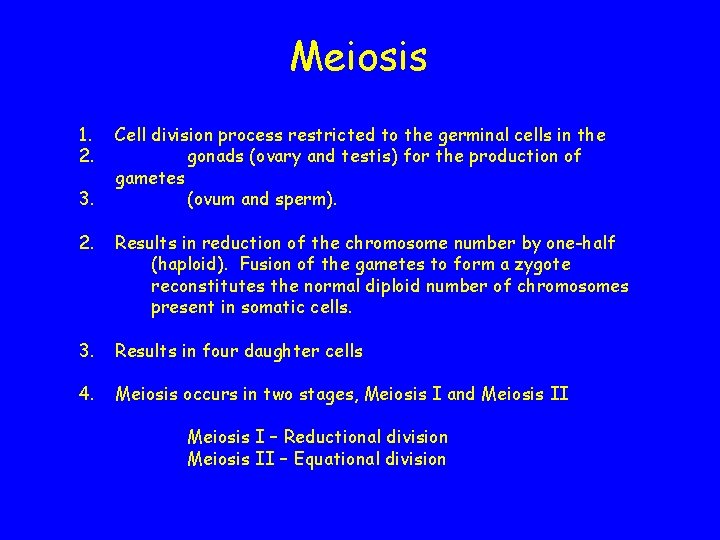
Meiosis 1. 2. 3. Cell division process restricted to the germinal cells in the gonads (ovary and testis) for the production of gametes (ovum and sperm). 2. Results in reduction of the chromosome number by one-half (haploid). Fusion of the gametes to form a zygote reconstitutes the normal diploid number of chromosomes present in somatic cells. 3. Results in four daughter cells 4. Meiosis occurs in two stages, Meiosis I and Meiosis II Meiosis I – Reductional division Meiosis II – Equational division
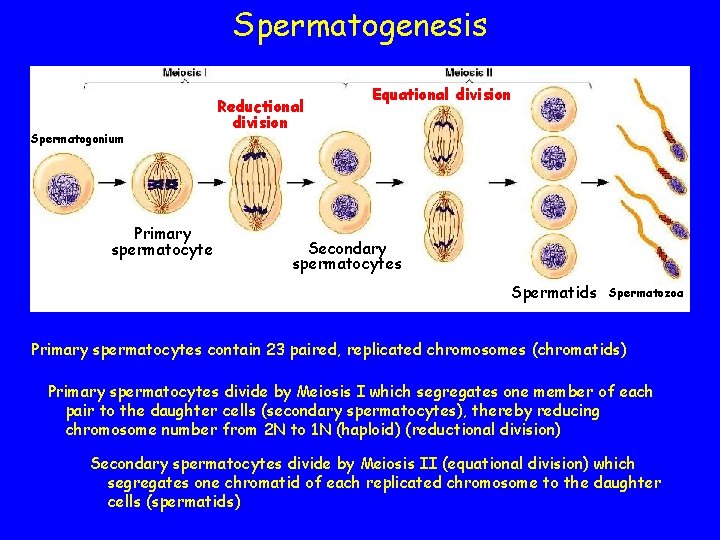
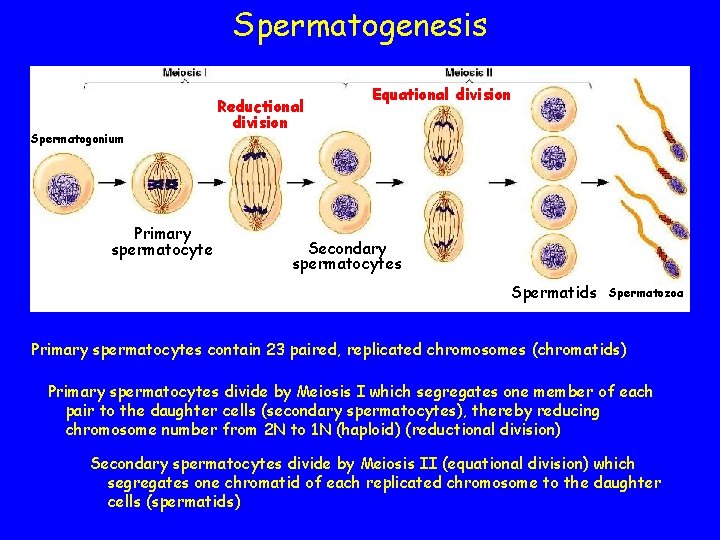
Spermatogenesis Spermatogonium Primary spermatocyte Reductional division Equational division Secondary spermatocytes Spermatids Spermatozoa Primary spermatocytes contain 23 paired, replicated chromosomes (chromatids) Primary spermatocytes divide by Meiosis I which segregates one member of each pair to the daughter cells (secondary spermatocytes), thereby reducing chromosome number from 2 N to 1 N (haploid) (reductional division) Secondary spermatocytes divide by Meiosis II (equational division) which segregates one chromatid of each replicated chromosome to the daughter cells (spermatids)
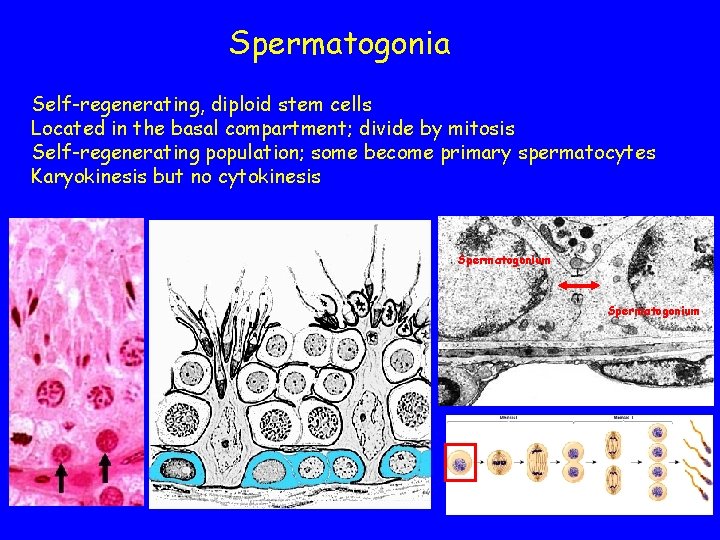
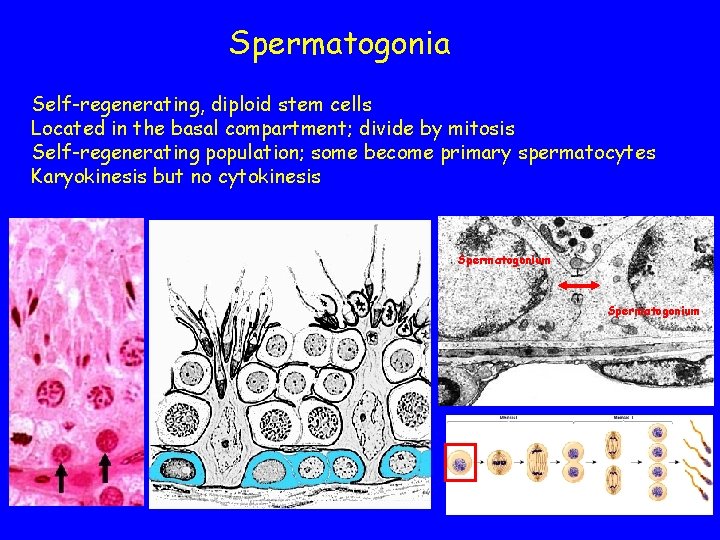
Spermatogonia Self-regenerating, diploid stem cells Located in the basal compartment; divide by mitosis Self-regenerating population; some become primary spermatocytes Karyokinesis but no cytokinesis Spermatogonium
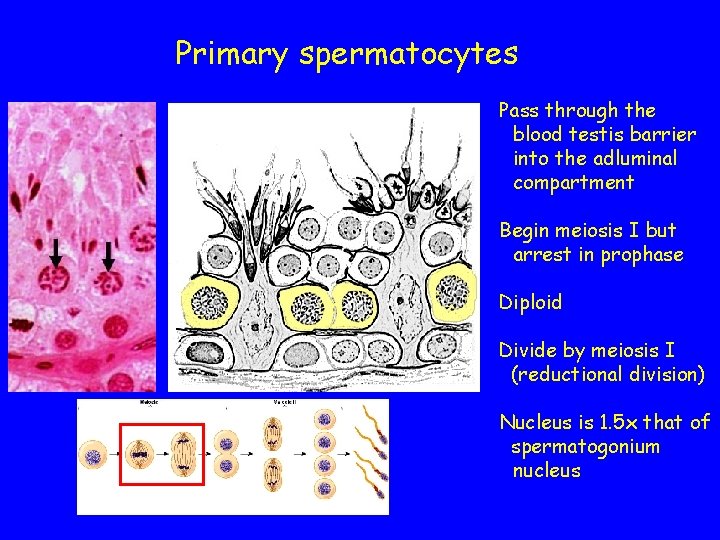
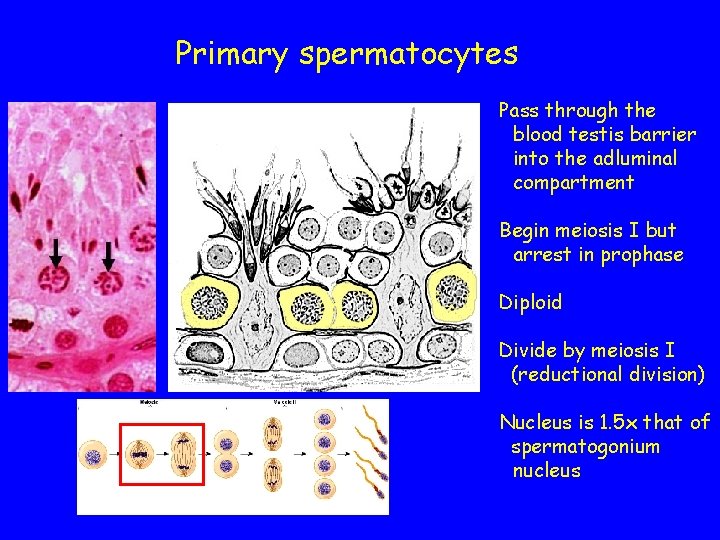
Primary spermatocytes Pass through the blood testis barrier into the adluminal compartment Begin meiosis I but arrest in prophase Diploid Divide by meiosis I (reductional division) Nucleus is 1. 5 x that of spermatogonium nucleus
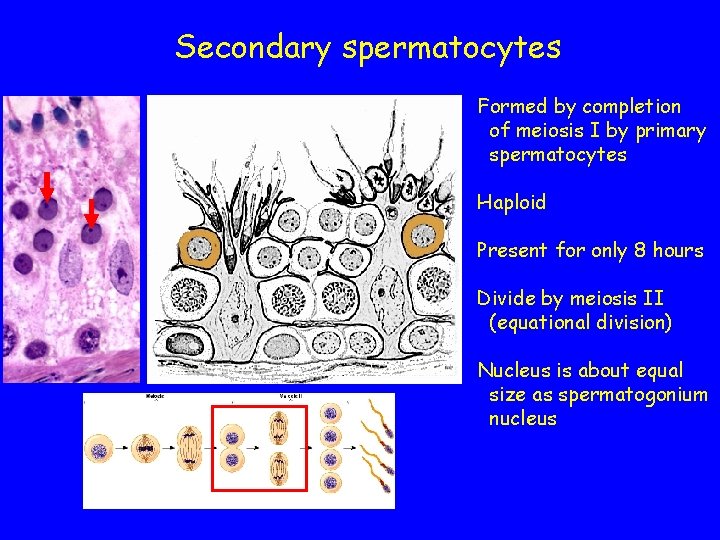
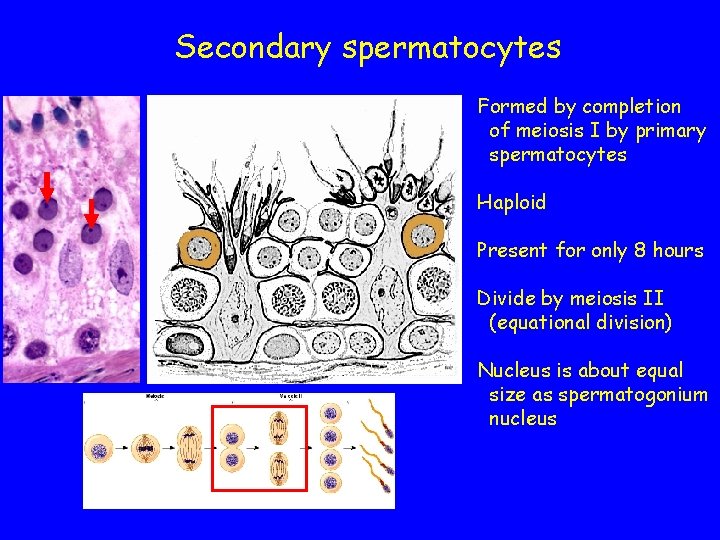
Secondary spermatocytes Formed by completion of meiosis I by primary spermatocytes Haploid Present for only 8 hours Divide by meiosis II (equational division) Nucleus is about equal size as spermatogonium nucleus
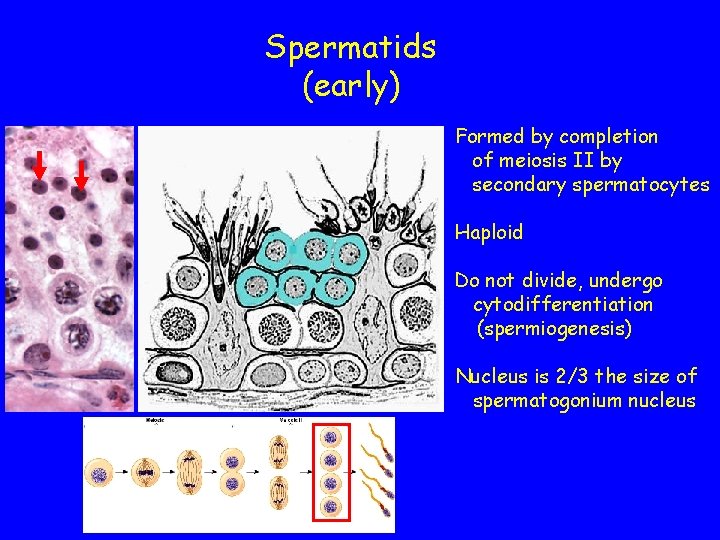
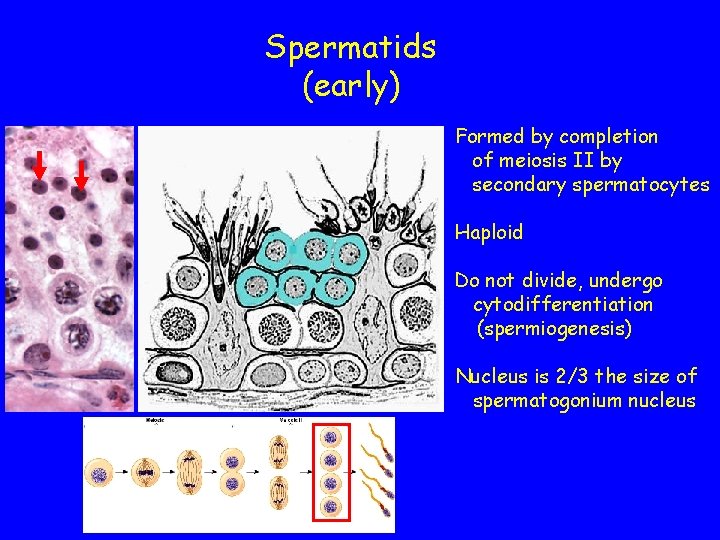
Spermatids (early) Formed by completion of meiosis II by secondary spermatocytes Haploid Do not divide, undergo cytodifferentiation (spermiogenesis) Nucleus is 2/3 the size of spermatogonium nucleus
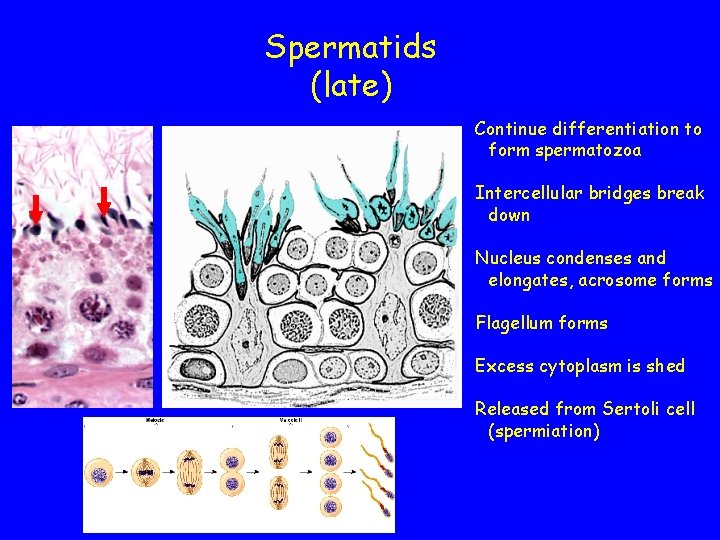
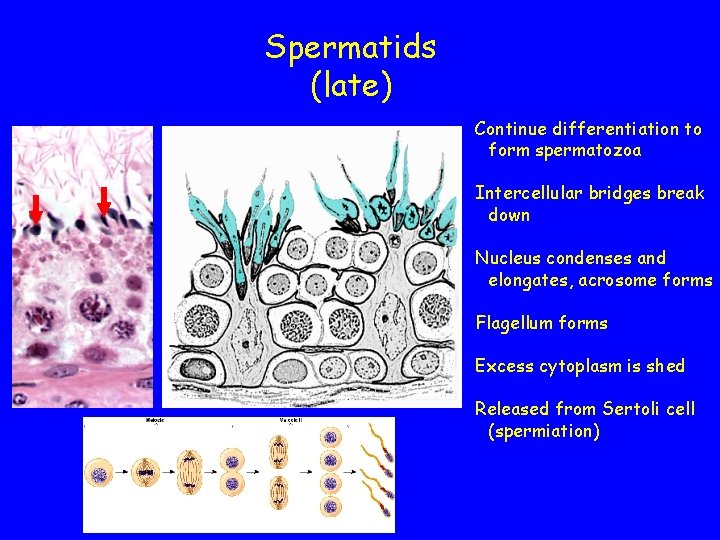
Spermatids (late) Continue differentiation to form spermatozoa Intercellular bridges break down Nucleus condenses and elongates, acrosome forms Flagellum forms Excess cytoplasm is shed Released from Sertoli cell (spermiation)
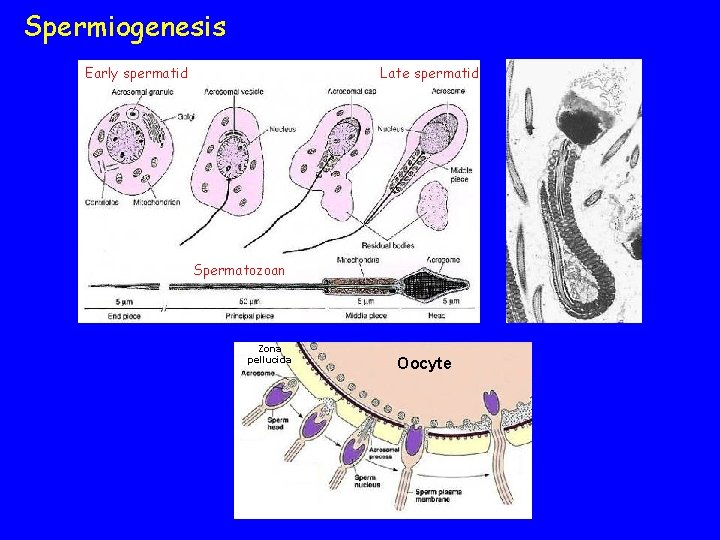
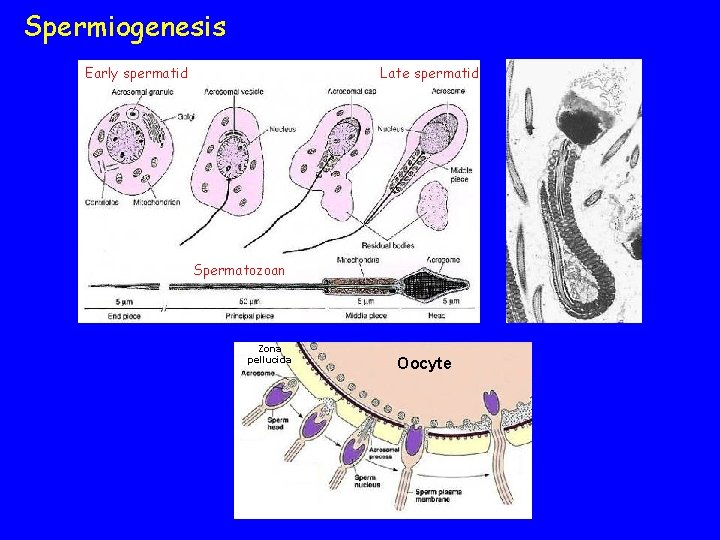
Spermiogenesis Early spermatid Late spermatid Spermatozoan Zona pellucida Oocyte
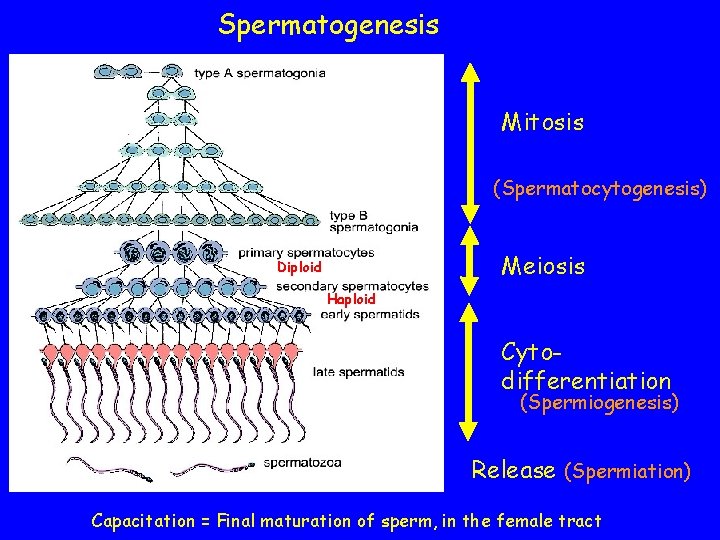
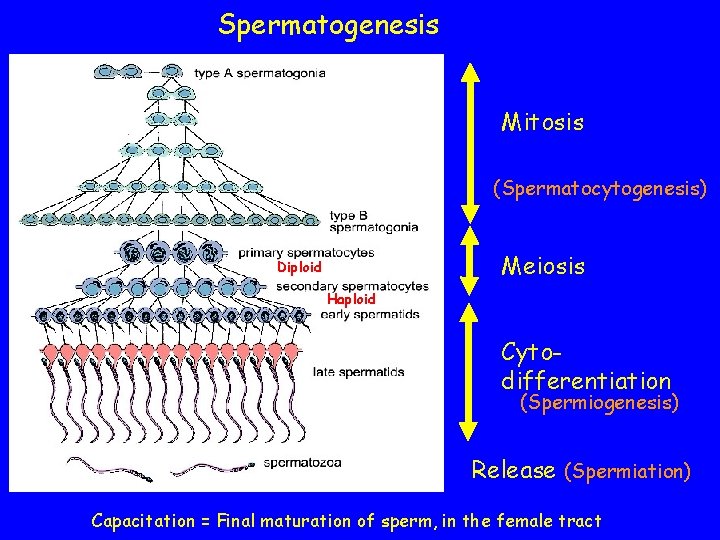
Spermatogenesis Mitosis (Spermatocytogenesis) Meiosis Diploid Haploid Cytodifferentiation (Spermiogenesis) Release (Spermiation) Capacitation = Final maturation of sperm, in the female tract
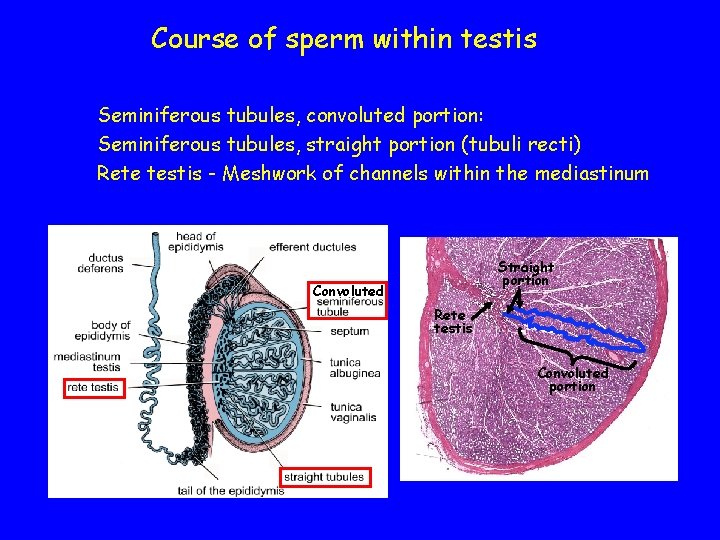
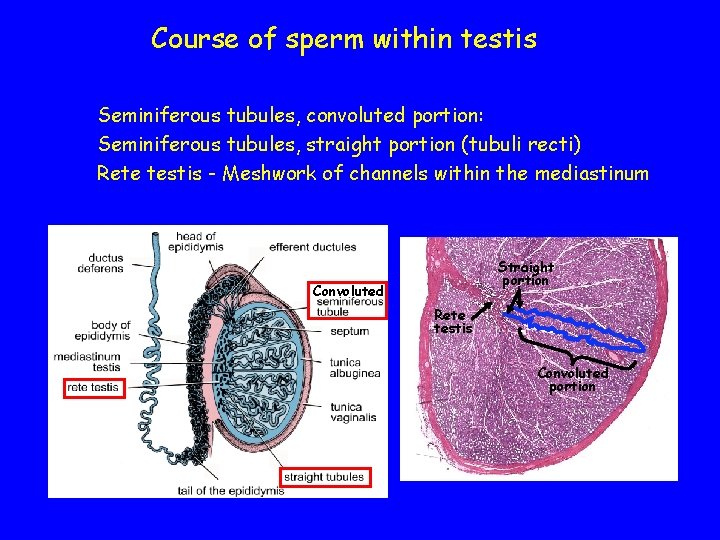
Course of sperm within testis Seminiferous tubules, convoluted portion: Seminiferous tubules, straight portion (tubuli recti) Rete testis - Meshwork of channels within the mediastinum Straight portion Convoluted Rete testis Convoluted portion
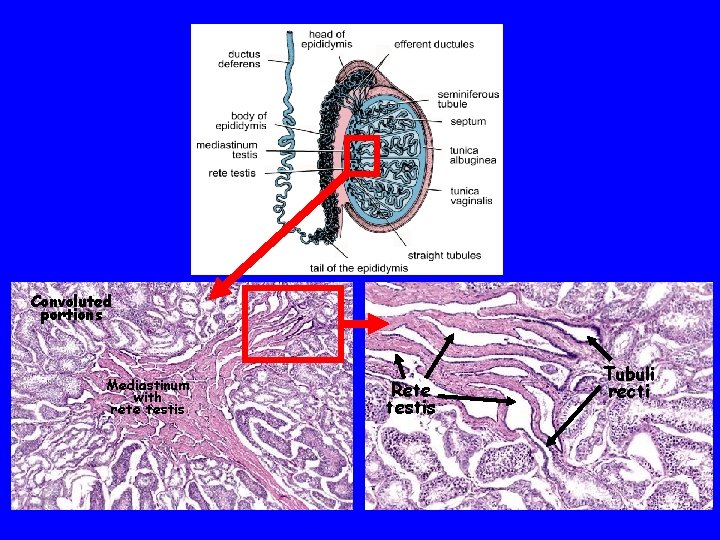
Convoluted portions Mediastinum with rete testis Rete testis Tubuli recti
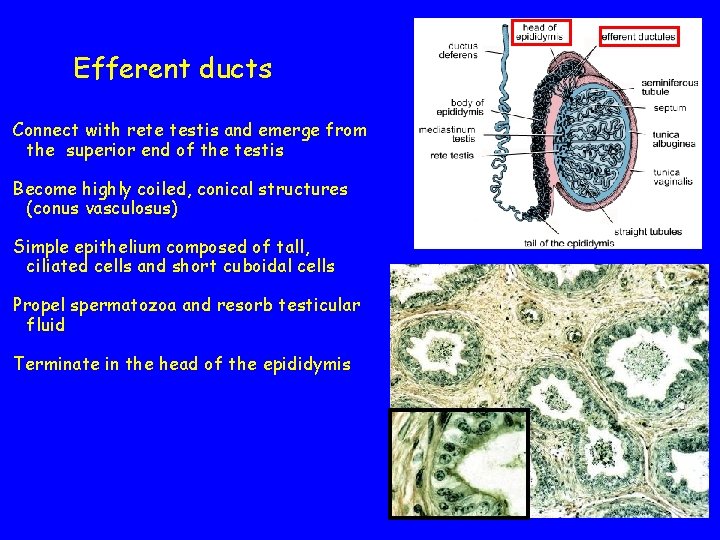
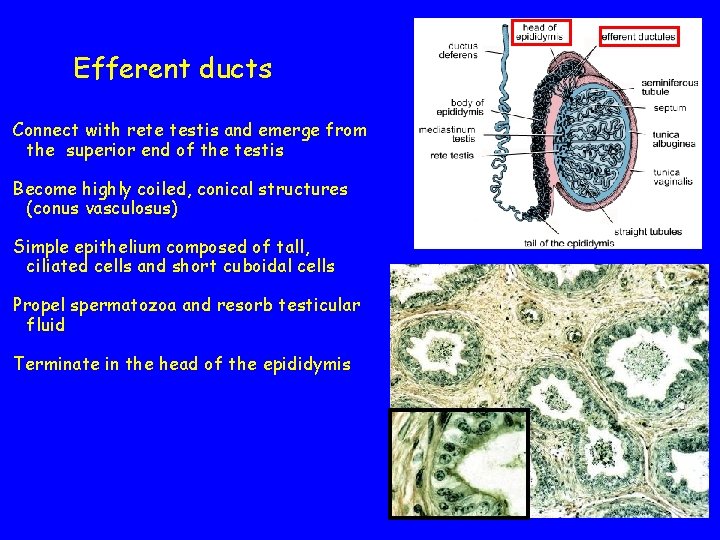
Efferent ducts Connect with rete testis and emerge from the superior end of the testis Become highly coiled, conical structures (conus vasculosus) Simple epithelium composed of tall, ciliated cells and short cuboidal cells Propel spermatozoa and resorb testicular fluid Terminate in the head of the epididymis
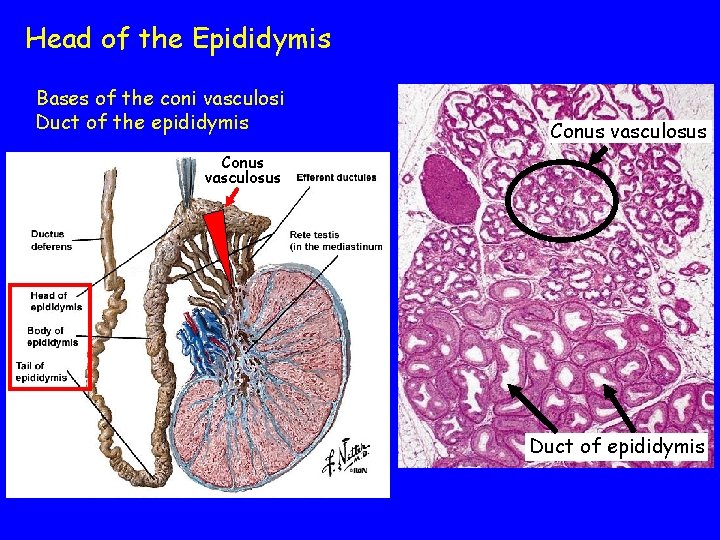
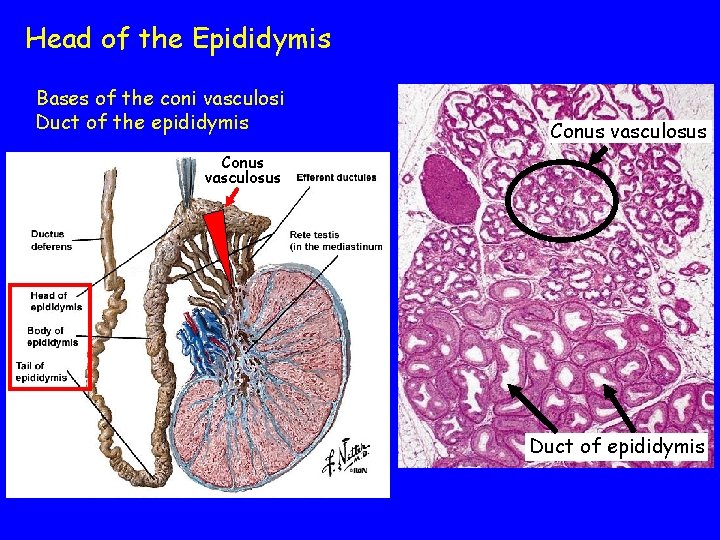
Head of the Epididymis Bases of the coni vasculosi Duct of the epididymis Conus vasculosus Duct of epididymis
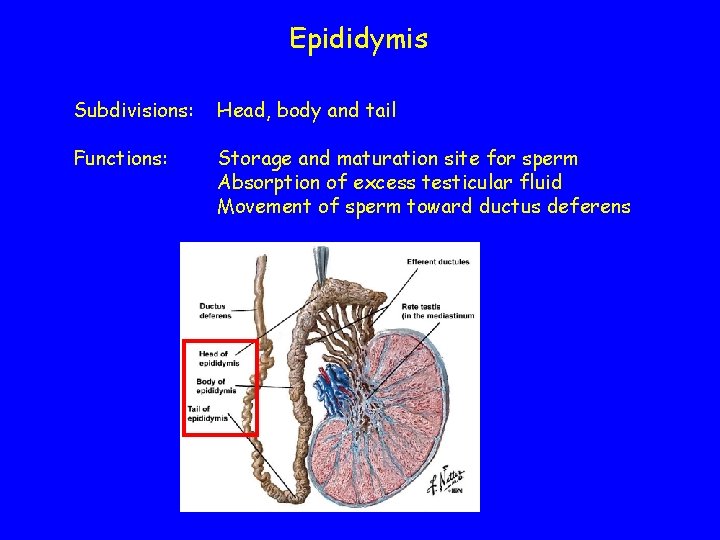
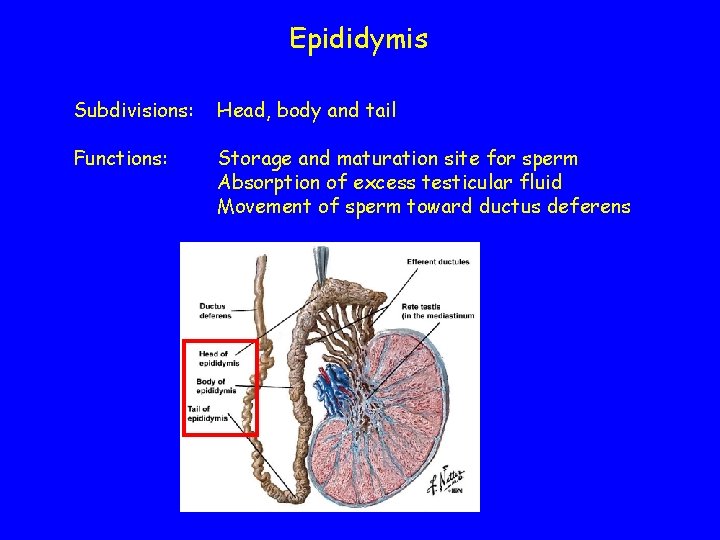
Epididymis Subdivisions: Head, body and tail Functions: Storage and maturation site for sperm Absorption of excess testicular fluid Movement of sperm toward ductus deferens
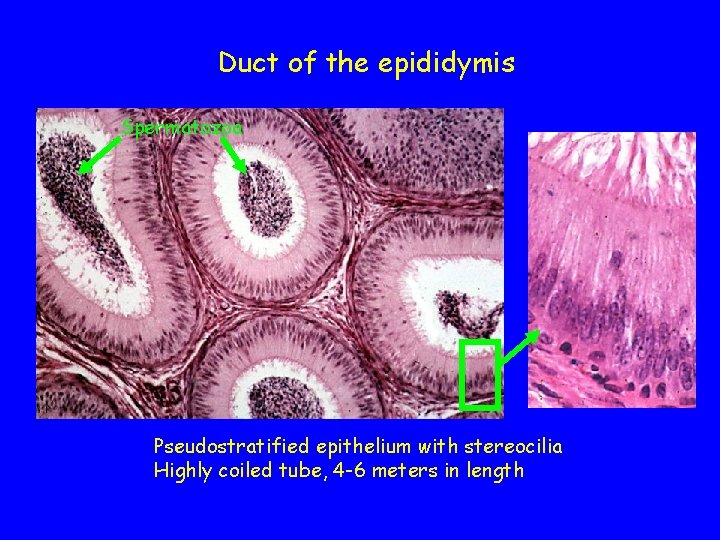
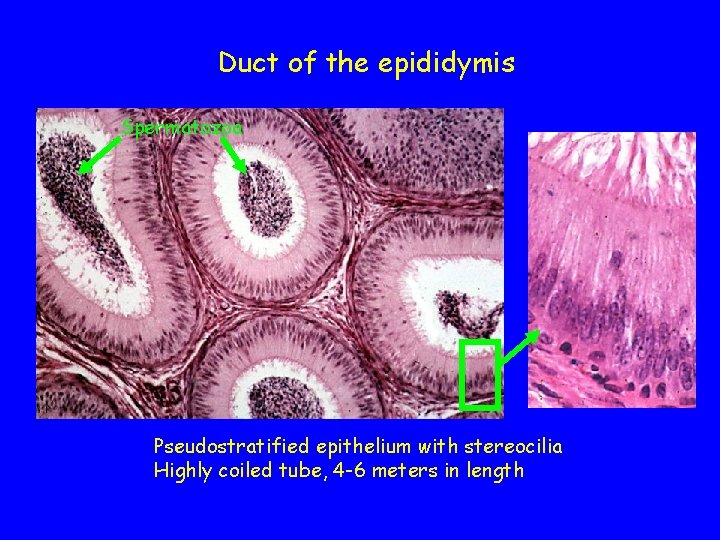
Duct of the epididymis Spermatozoa Pseudostratified epithelium with stereocilia Highly coiled tube, 4 -6 meters in length
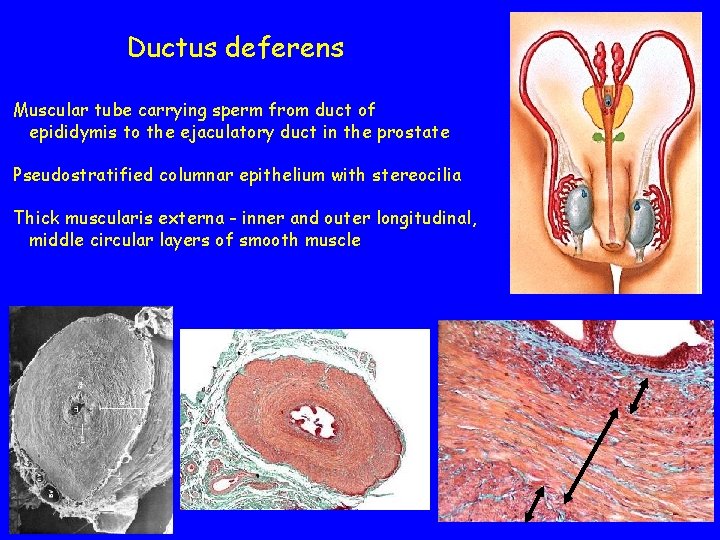
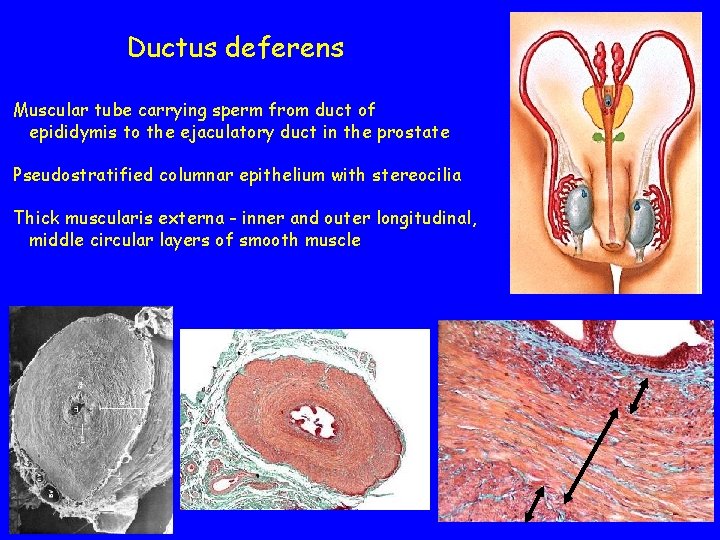
Ductus deferens Muscular tube carrying sperm from duct of epididymis to the ejaculatory duct in the prostate Pseudostratified columnar epithelium with stereocilia Thick muscularis externa - inner and outer longitudinal, middle circular layers of smooth muscle
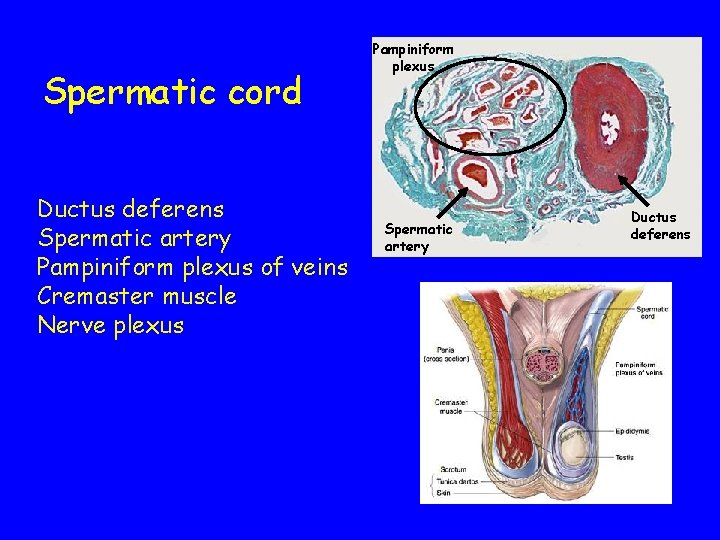
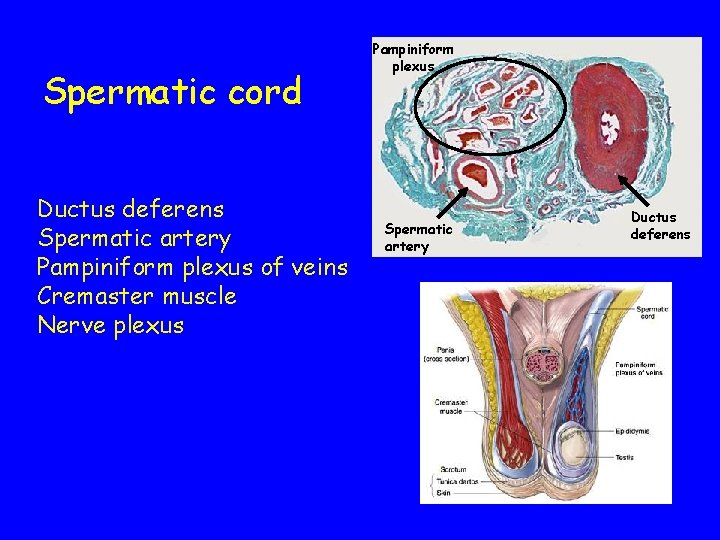
Spermatic cord Ductus deferens Spermatic artery Pampiniform plexus of veins Cremaster muscle Nerve plexus Pampiniform plexus Spermatic artery Ductus deferens
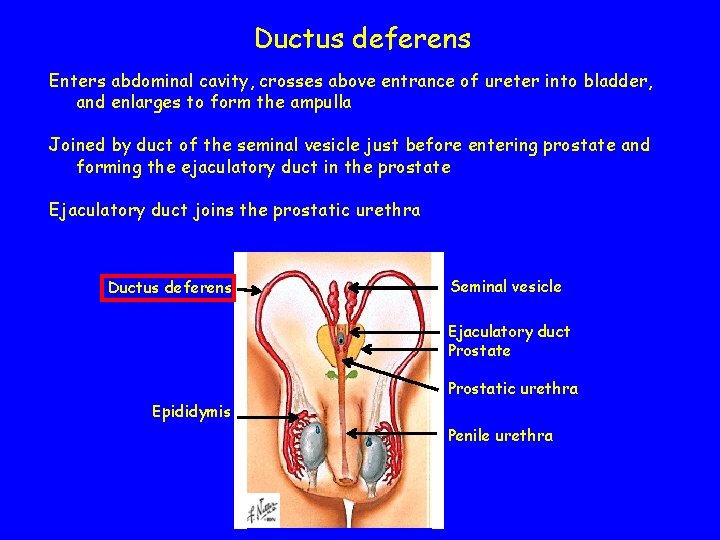
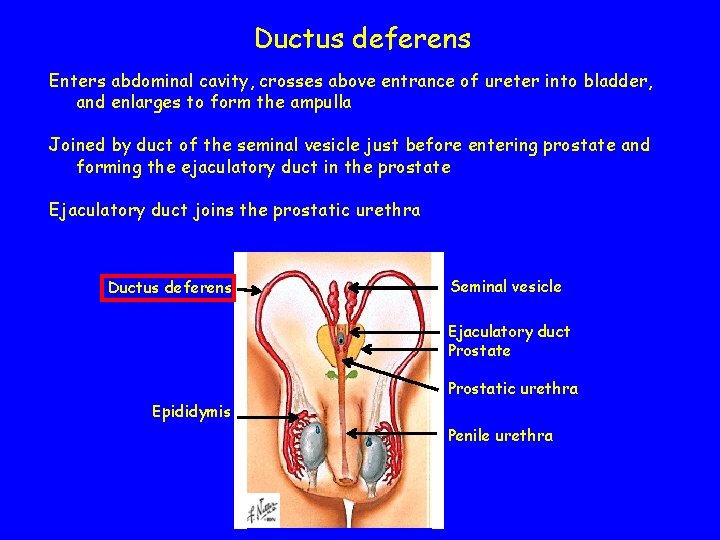
Ductus deferens Enters abdominal cavity, crosses above entrance of ureter into bladder, and enlarges to form the ampulla Joined by duct of the seminal vesicle just before entering prostate and forming the ejaculatory duct in the prostate Ejaculatory duct joins the prostatic urethra Ductus deferens Seminal vesicle Ejaculatory duct Prostate Prostatic urethra Epididymis Penile urethra
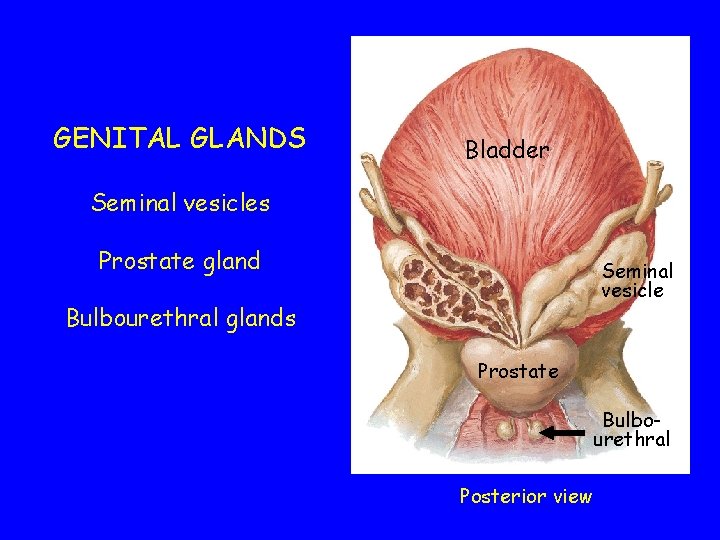
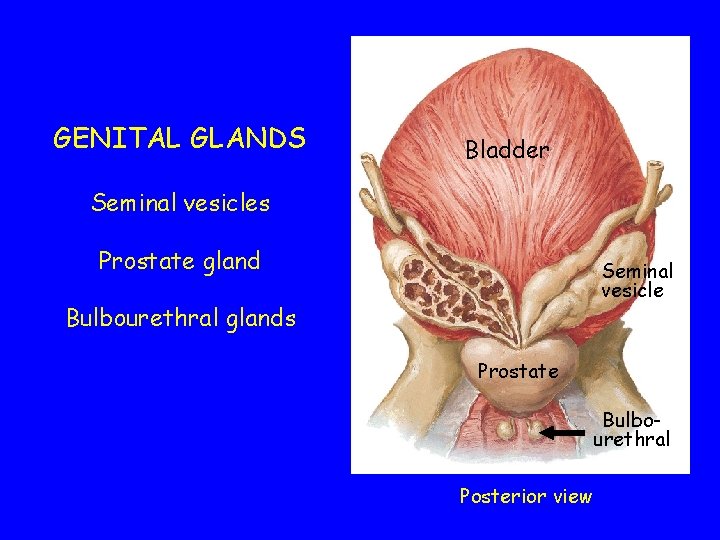
GENITAL GLANDS Bladder Seminal vesicles Prostate gland Seminal vesicle Bulbourethral glands Prostate Bulbourethral Posterior view
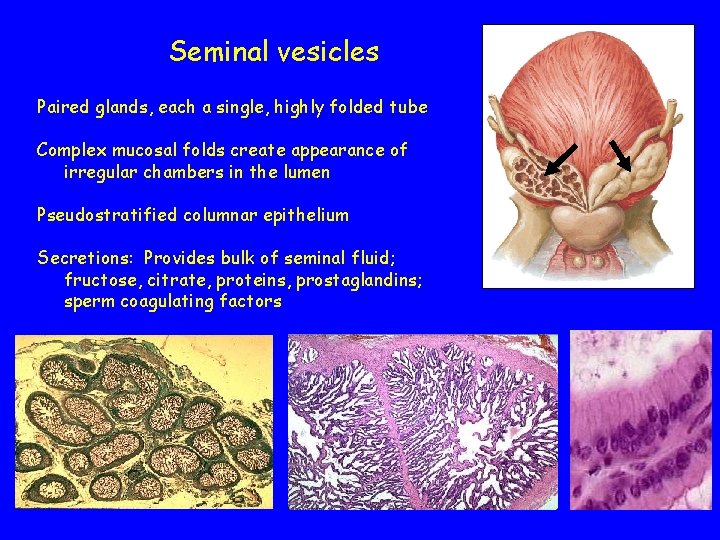
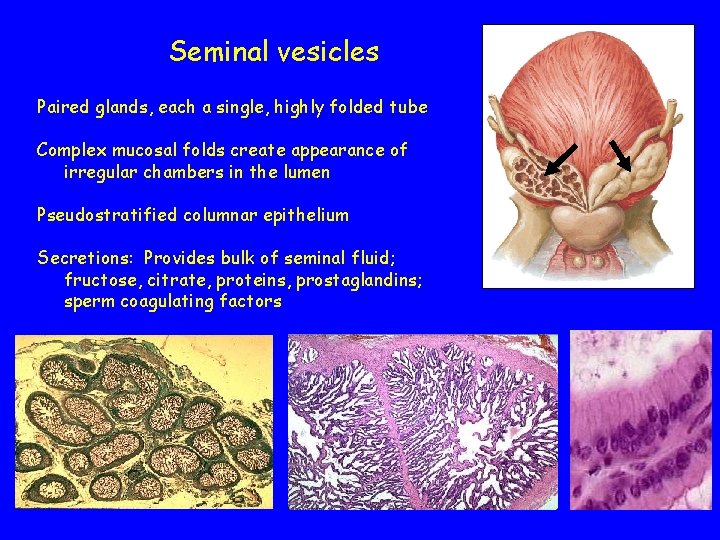
Seminal vesicles Paired glands, each a single, highly folded tube Complex mucosal folds create appearance of irregular chambers in the lumen Pseudostratified columnar epithelium Secretions: Provides bulk of seminal fluid; fructose, citrate, proteins, prostaglandins; sperm coagulating factors
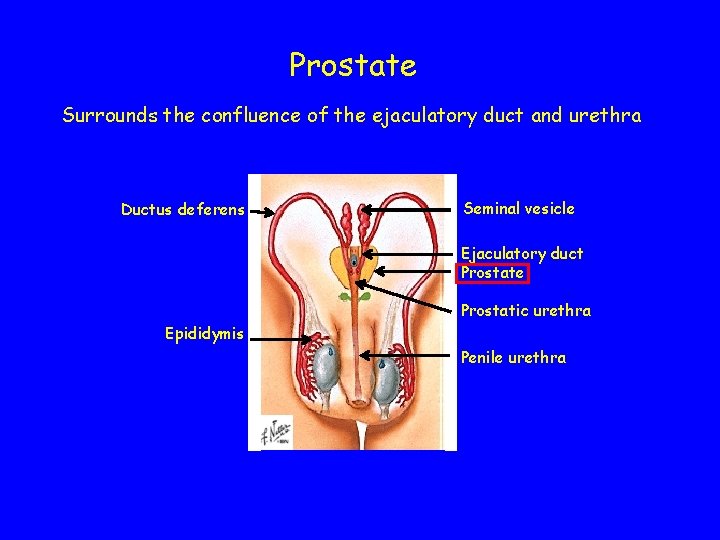
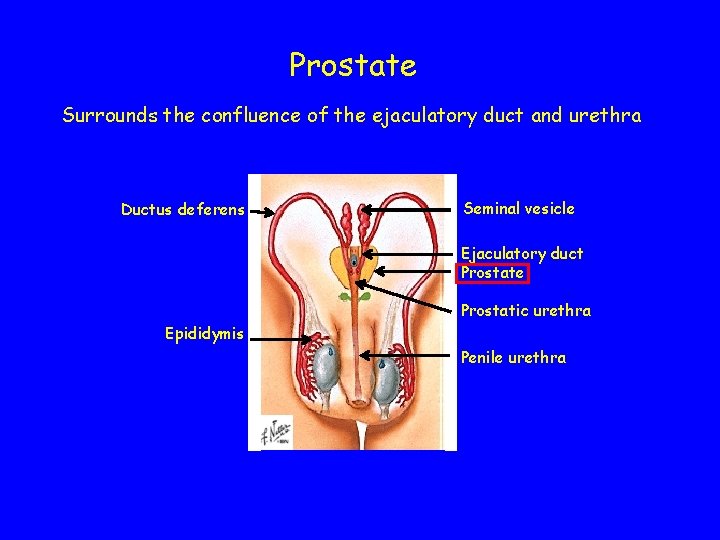
Prostate Surrounds the confluence of the ejaculatory duct and urethra Ductus deferens Seminal vesicle Ejaculatory duct Prostate Prostatic urethra Epididymis Penile urethra
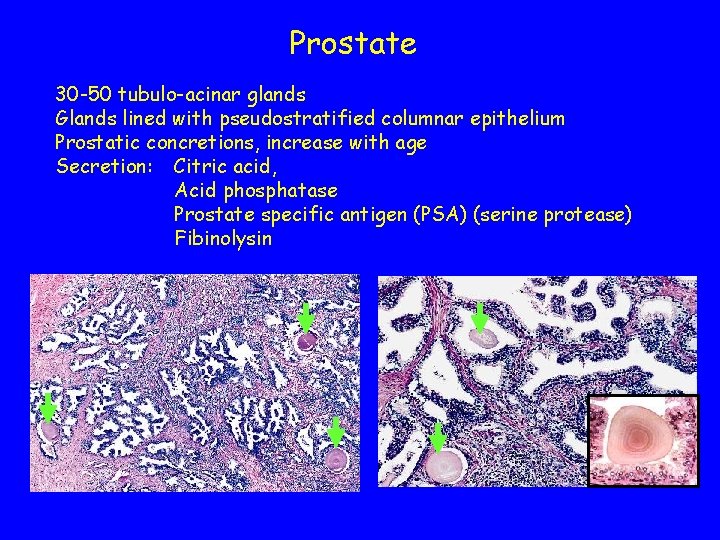
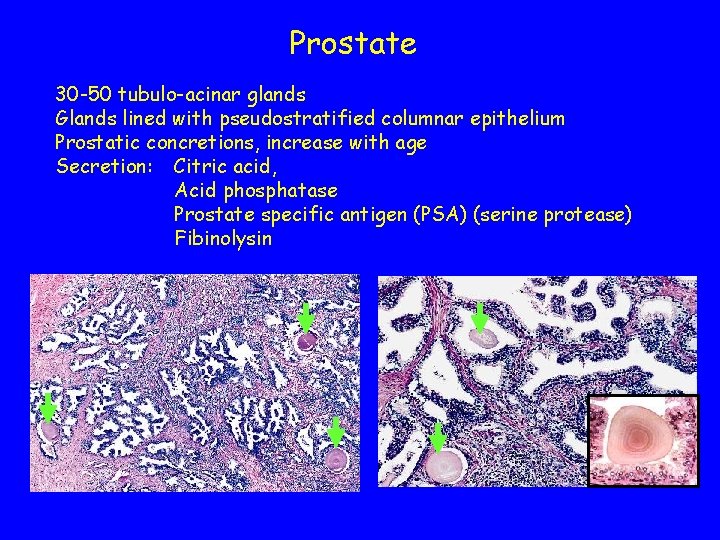
Prostate 30 -50 tubulo-acinar glands Glands lined with pseudostratified columnar epithelium Prostatic concretions, increase with age Secretion: Citric acid, Acid phosphatase Prostate specific antigen (PSA) (serine protease) Fibinolysin
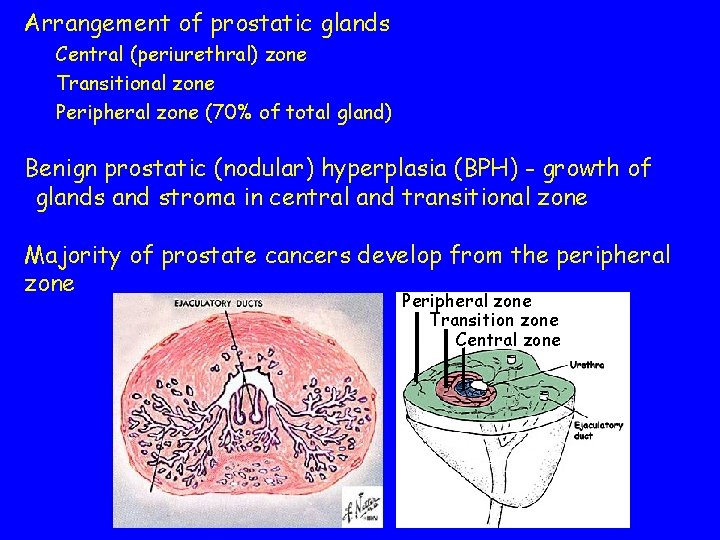
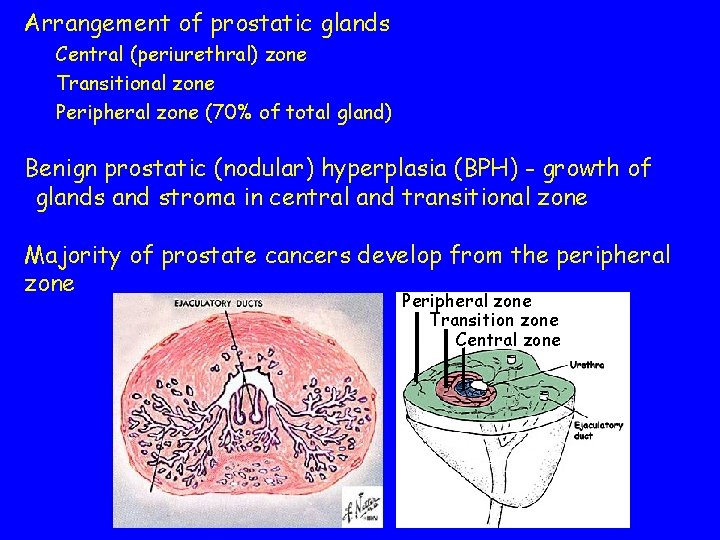
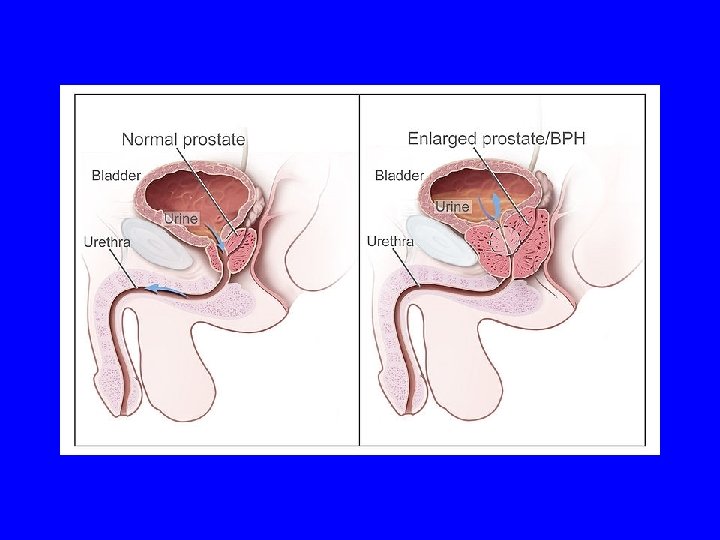
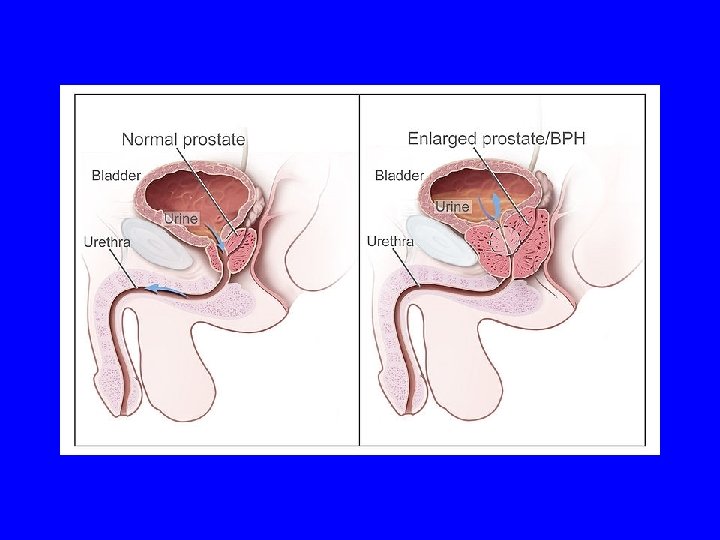
Arrangement of prostatic glands Central (periurethral) zone Transitional zone Peripheral zone (70% of total gland) Benign prostatic (nodular) hyperplasia (BPH) - growth of glands and stroma in central and transitional zone Majority of prostate cancers develop from the peripheral zone Peripheral zone Transition zone Central zone
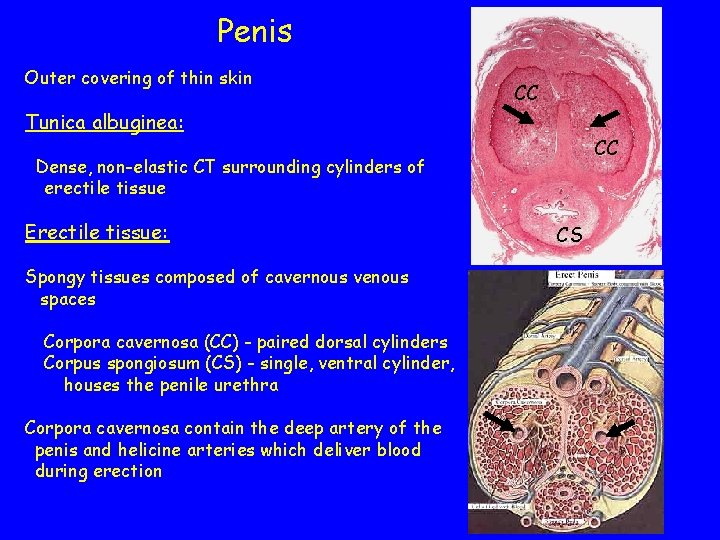
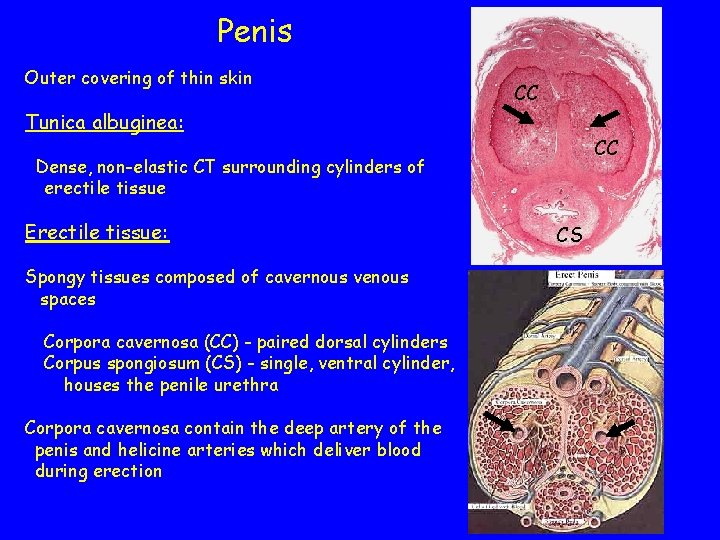
Penis Outer covering of thin skin CC Tunica albuginea: CC Dense, non-elastic CT surrounding cylinders of erectile tissue Erectile tissue: Spongy tissues composed of cavernous venous spaces Corpora cavernosa (CC) - paired dorsal cylinders Corpus spongiosum (CS) - single, ventral cylinder, houses the penile urethra Corpora cavernosa contain the deep artery of the penis and helicine arteries which deliver blood during erection CS
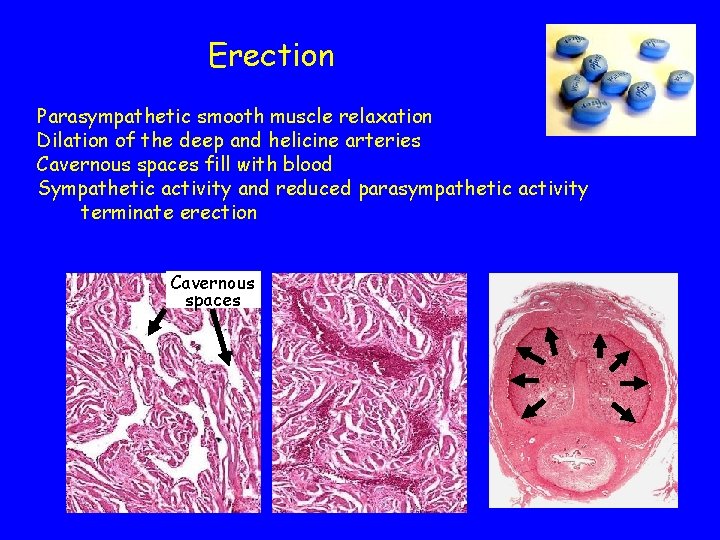
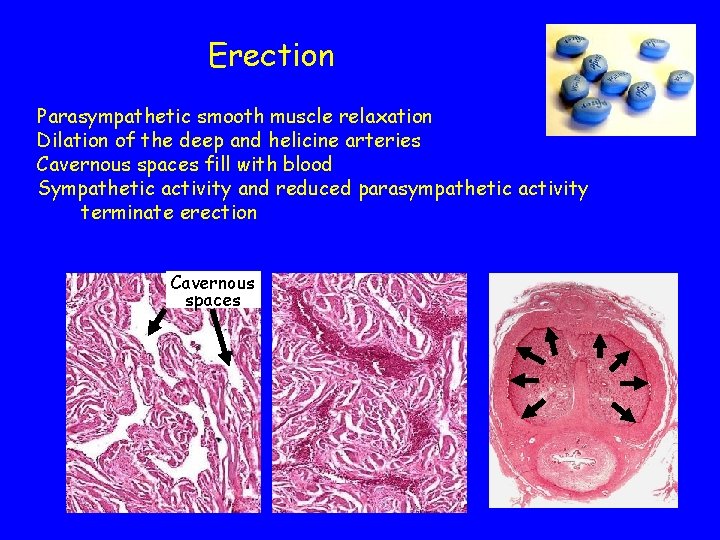
Erection Parasympathetic smooth muscle relaxation Dilation of the deep and helicine arteries Cavernous spaces fill with blood Sympathetic activity and reduced parasympathetic activity terminate erection Cavernous spaces
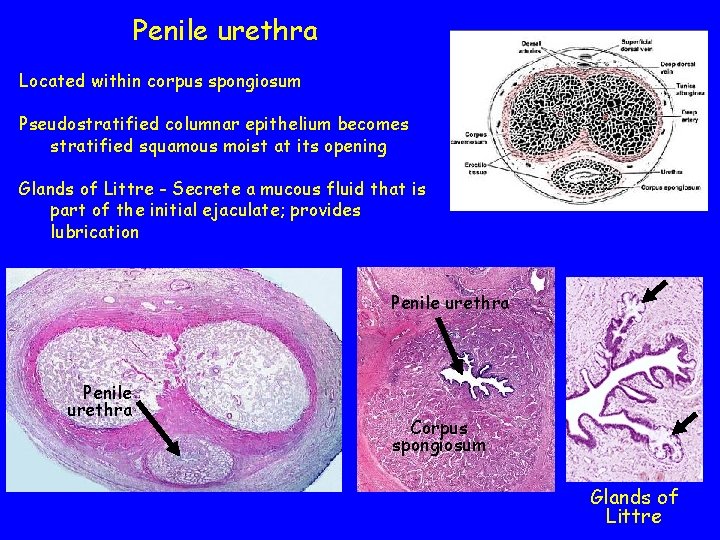
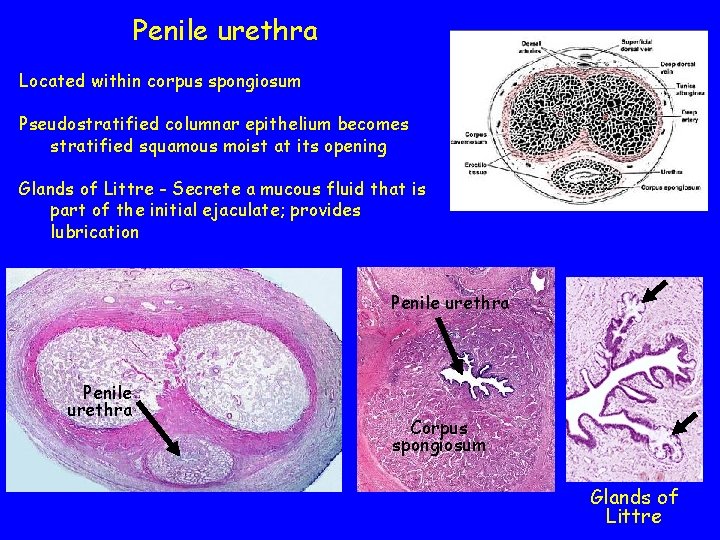
Penile urethra Located within corpus spongiosum Pseudostratified columnar epithelium becomes stratified squamous moist at its opening Glands of Littre - Secrete a mucous fluid that is part of the initial ejaculate; provides lubrication Penile urethra Corpus spongiosum Glands of Littre
 Testes
Testes Gonads glands
Gonads glands Function of vagina
Function of vagina Function of reproductive system
Function of reproductive system Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Anatomy of the reproductive system exercise 42
Anatomy of the reproductive system exercise 42 Lymphatic drainage of breast
Lymphatic drainage of breast Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Female and male reproductive system
Female and male reproductive system Male reproductive system diagram
Male reproductive system diagram Luteinizing hormone in male reproductive system
Luteinizing hormone in male reproductive system Human reproductive system
Human reproductive system Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Male reproductive system information
Male reproductive system information Where is semen stored
Where is semen stored Male cow reproductive system diagram
Male cow reproductive system diagram Male anatomy front view
Male anatomy front view Asexual reproduction
Asexual reproduction Disease traductor
Disease traductor Anatomy of fish reproductive system
Anatomy of fish reproductive system Female reproductive system
Female reproductive system Male fetal pig reproductive system labeled
Male fetal pig reproductive system labeled Female part of a flower
Female part of a flower Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Primary sex organ of the male reproductive system? *
Primary sex organ of the male reproductive system? * Lesson 20.2 the male reproductive system
Lesson 20.2 the male reproductive system Cow male reproductive system
Cow male reproductive system Figure 28-2 the female reproductive system
Figure 28-2 the female reproductive system Colon function in male reproductive system
Colon function in male reproductive system Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Similarities between male and female reproductive system
Similarities between male and female reproductive system Female reproductive system label
Female reproductive system label Pathway of semen
Pathway of semen Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Plants reproductive system
Plants reproductive system Reproductive system summary
Reproductive system summary Anatomy of female genital tract ppt
Anatomy of female genital tract ppt Tunica albuginea
Tunica albuginea Note on male reproductive system
Note on male reproductive system Does meiosis occur in humans
Does meiosis occur in humans Path of male reproductive system
Path of male reproductive system