Figure 18 26 Figure 18 27 a Figure













- Slides: 117
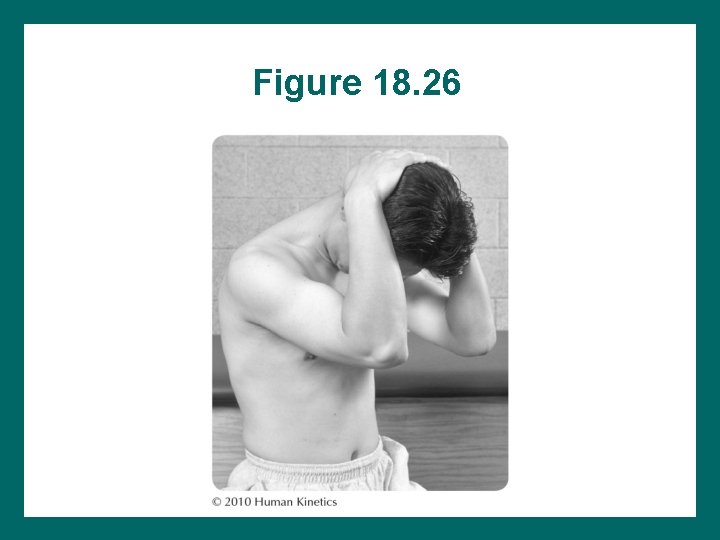
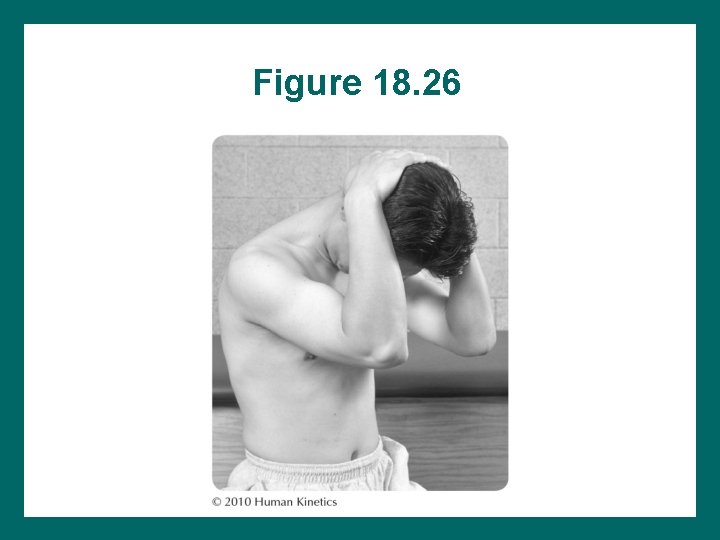
Figure 18. 26
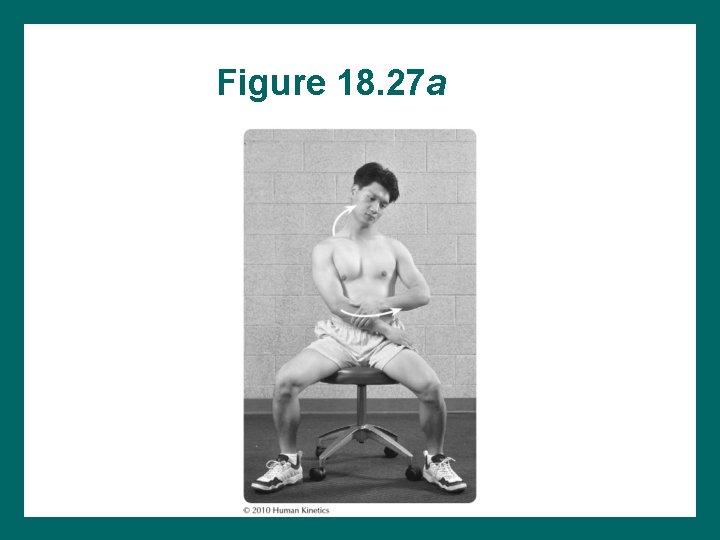
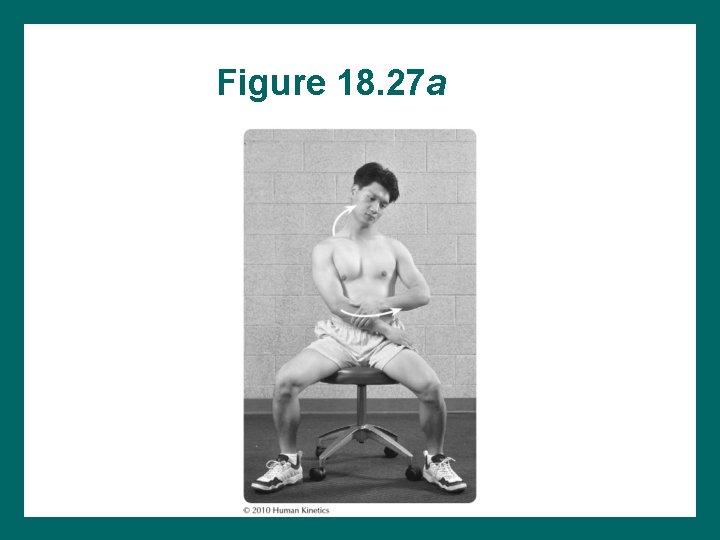
Figure 18. 27 a
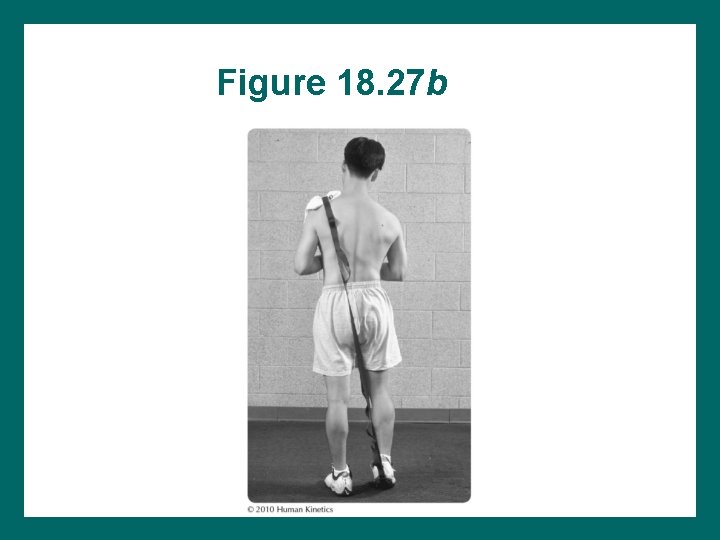
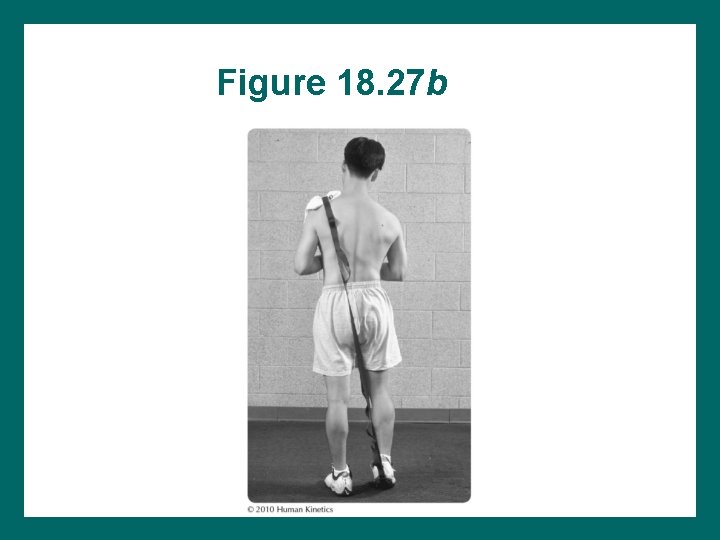
Figure 18. 27 b
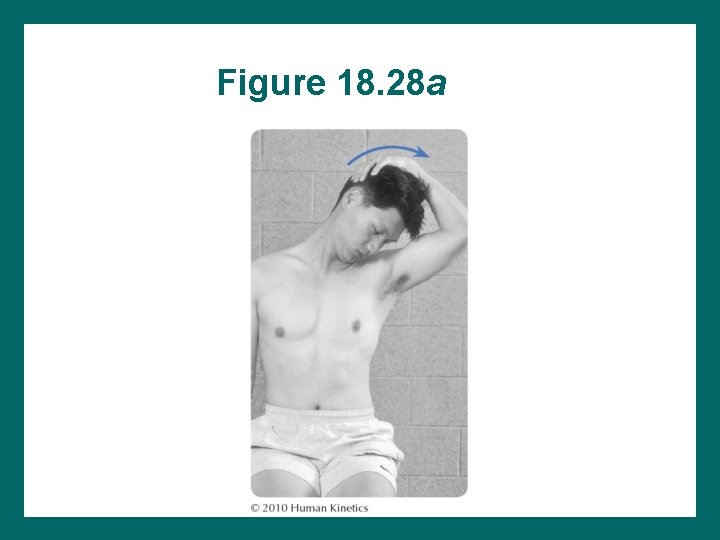
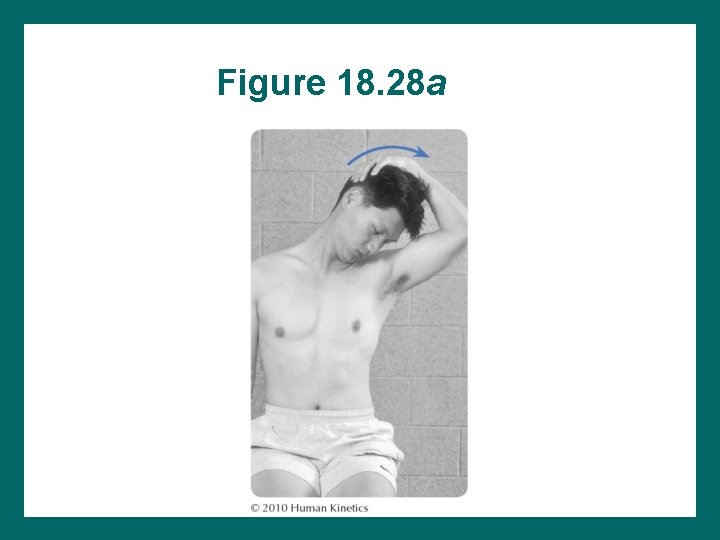
Figure 18. 28 a
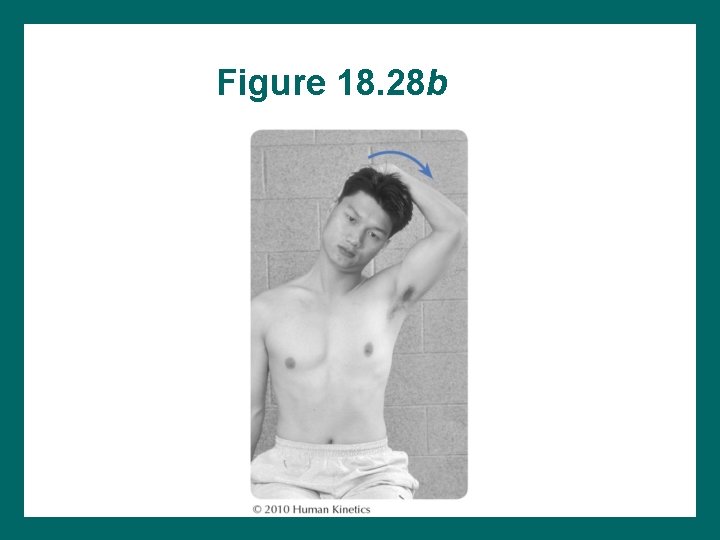
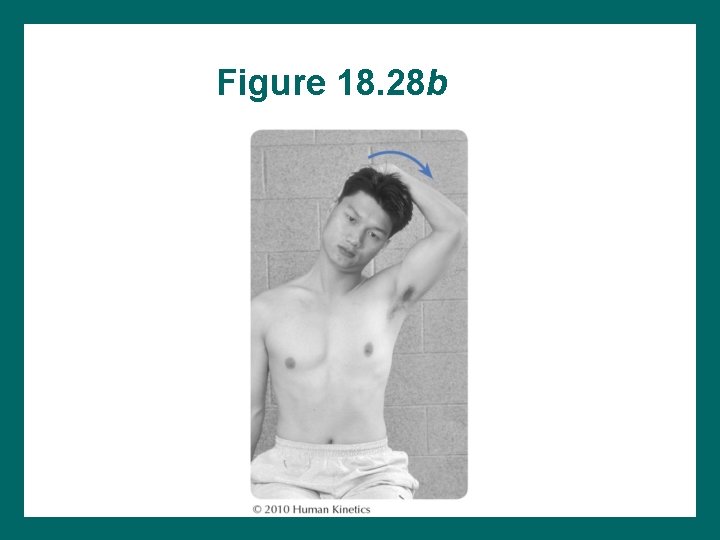
Figure 18. 28 b
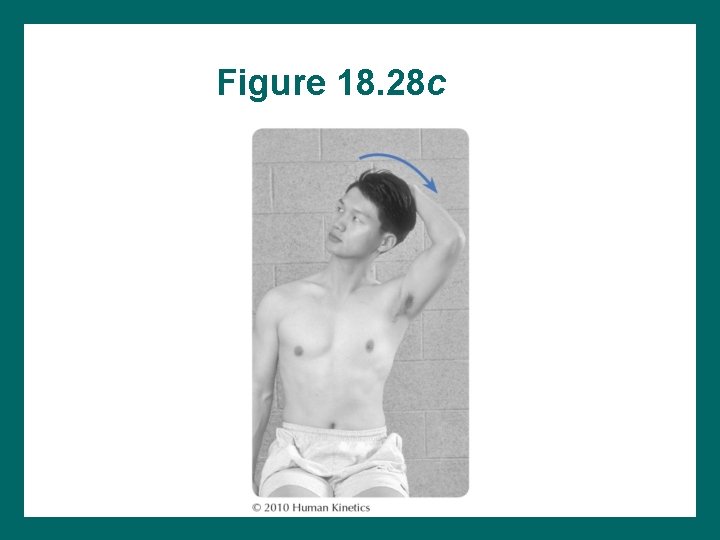
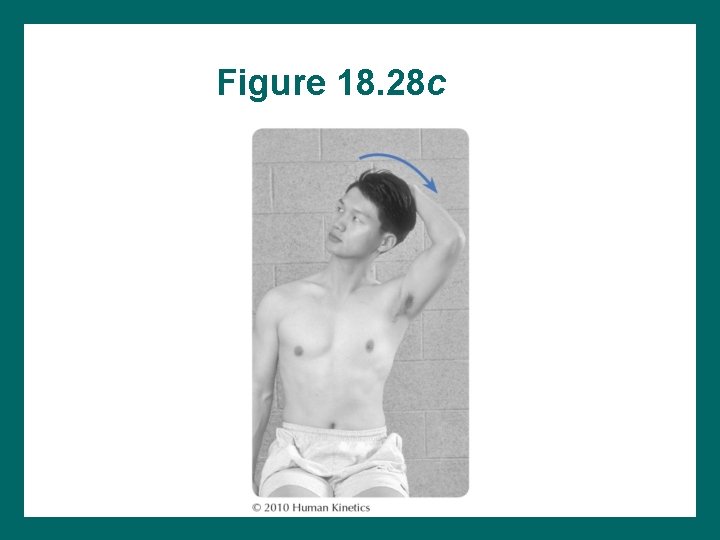
Figure 18. 28 c
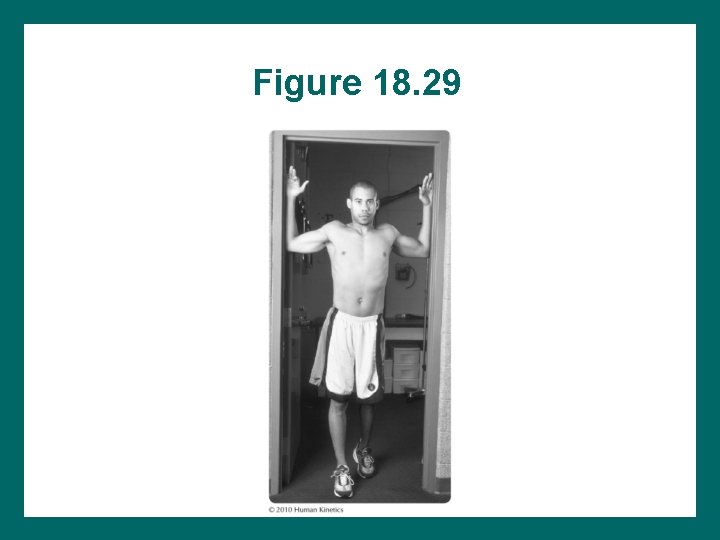
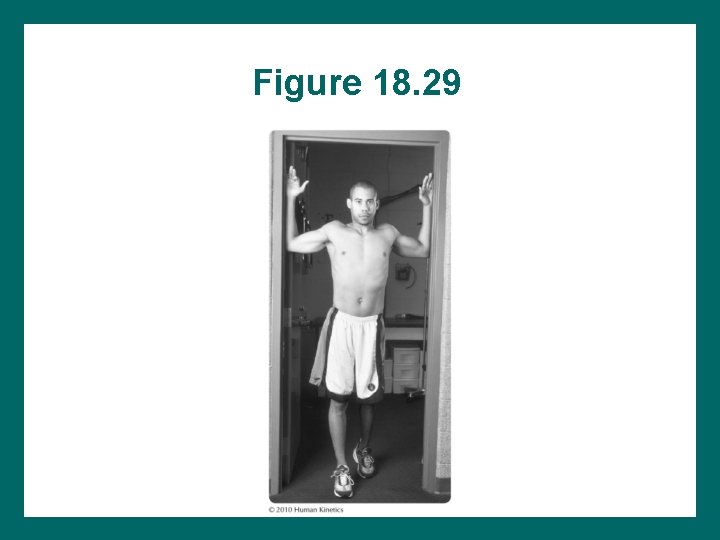
Figure 18. 29
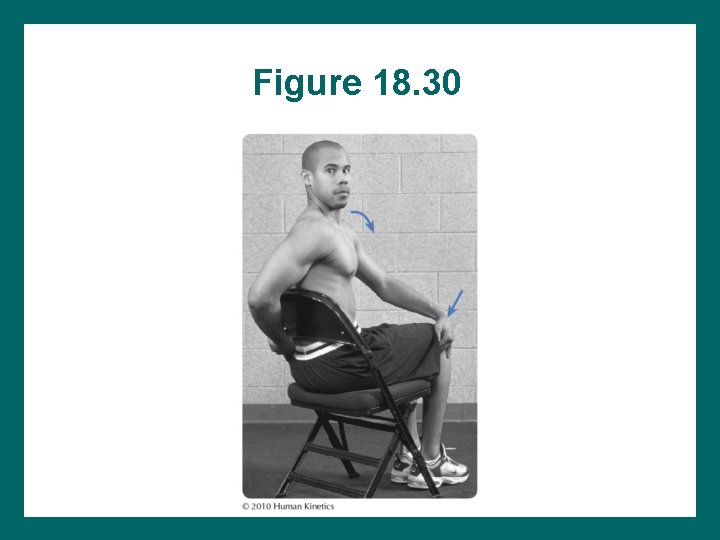
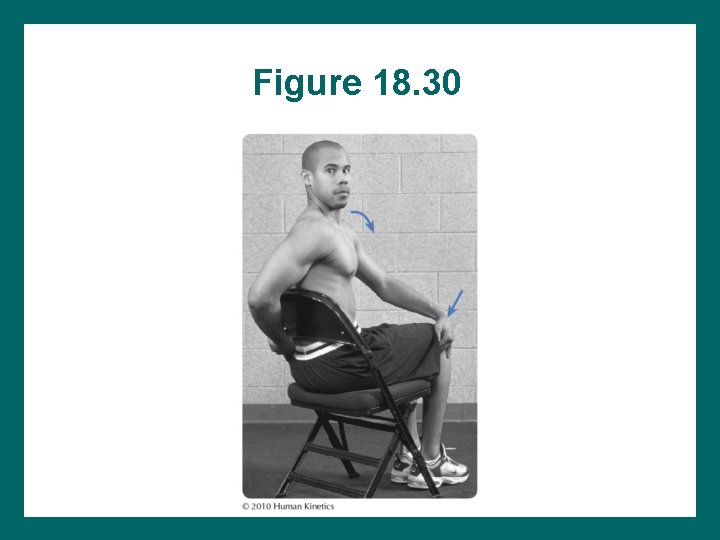
Figure 18. 30
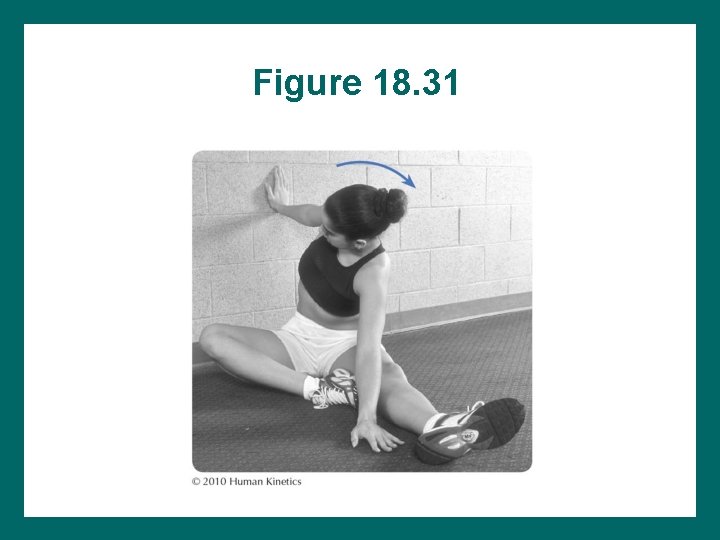
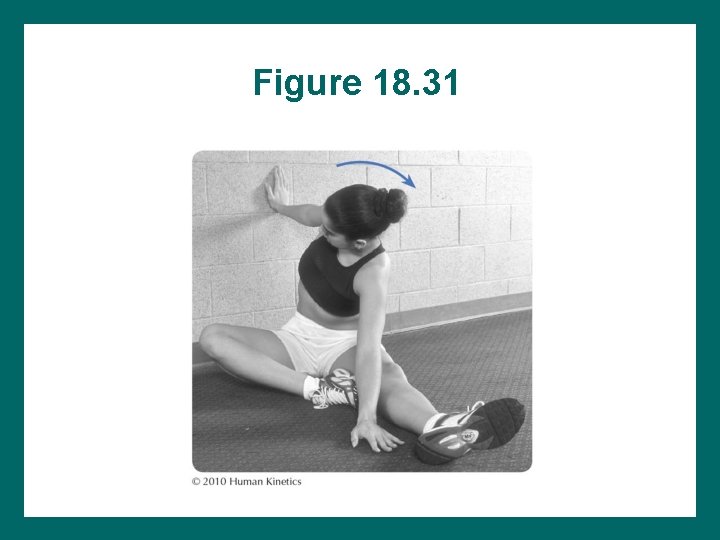
Figure 18. 31
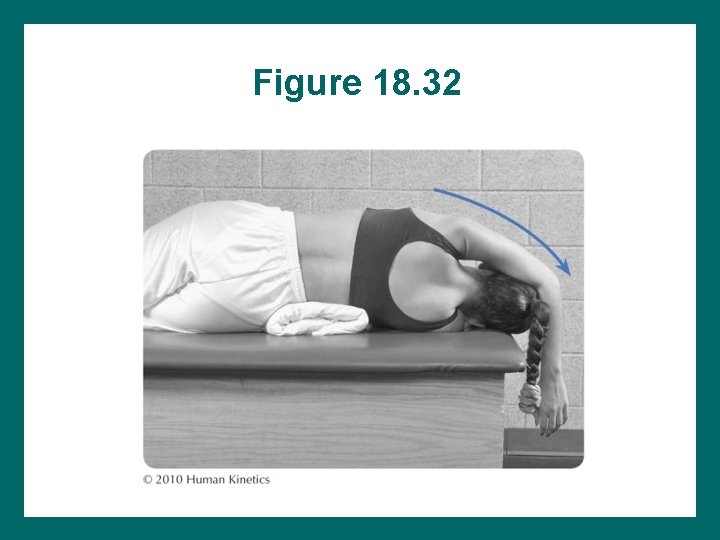
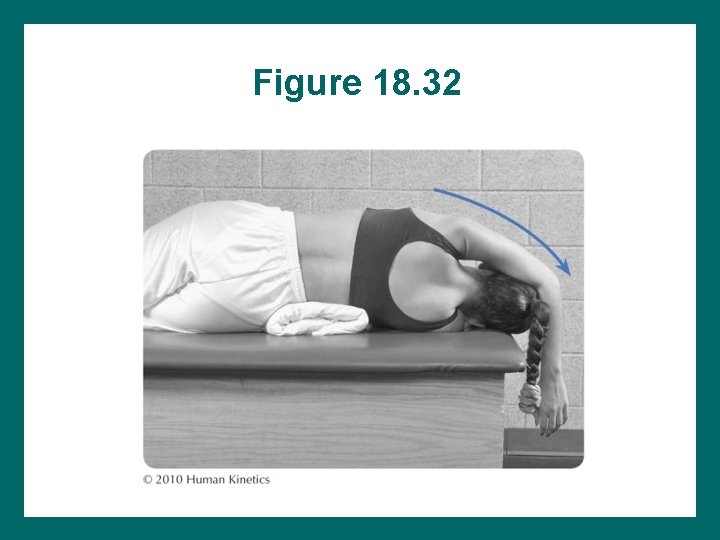
Figure 18. 32
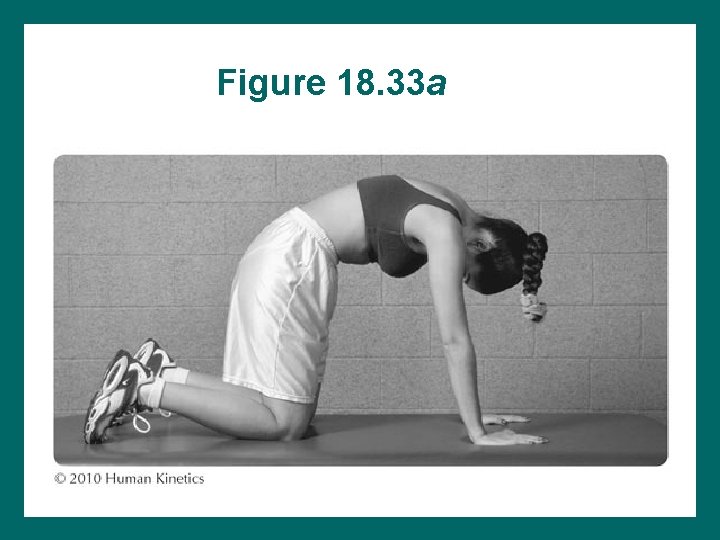
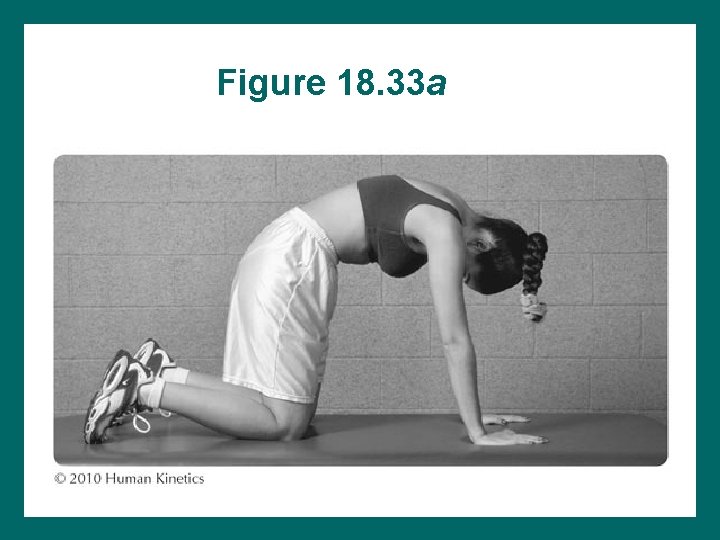
Figure 18. 33 a
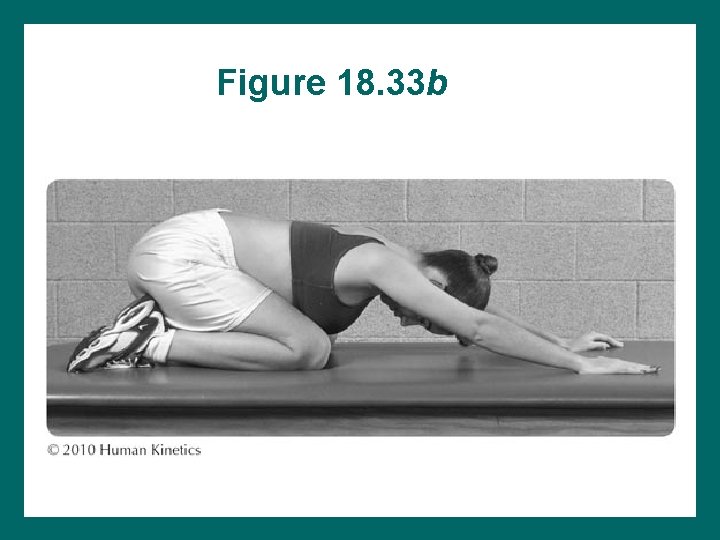
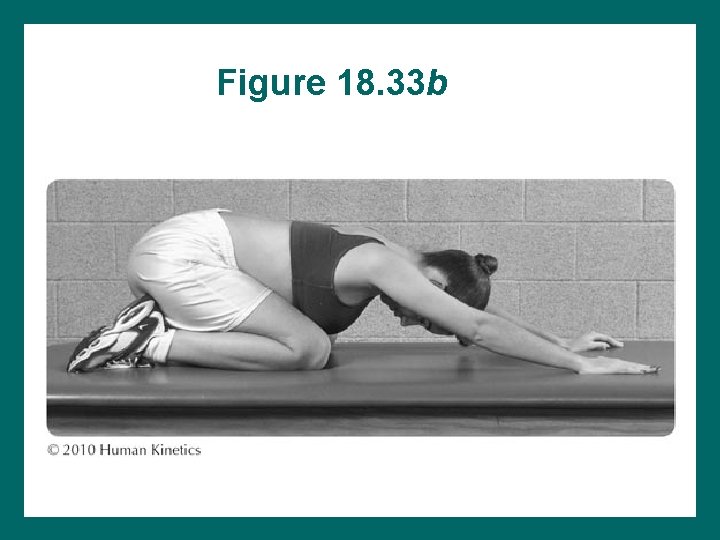
Figure 18. 33 b
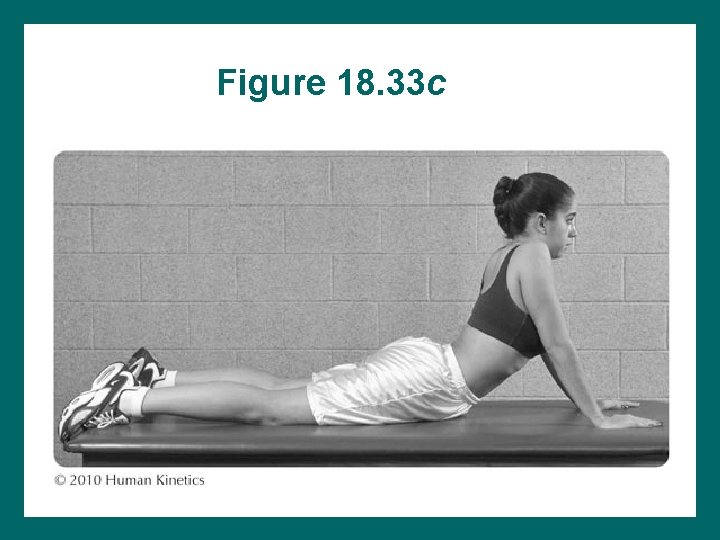
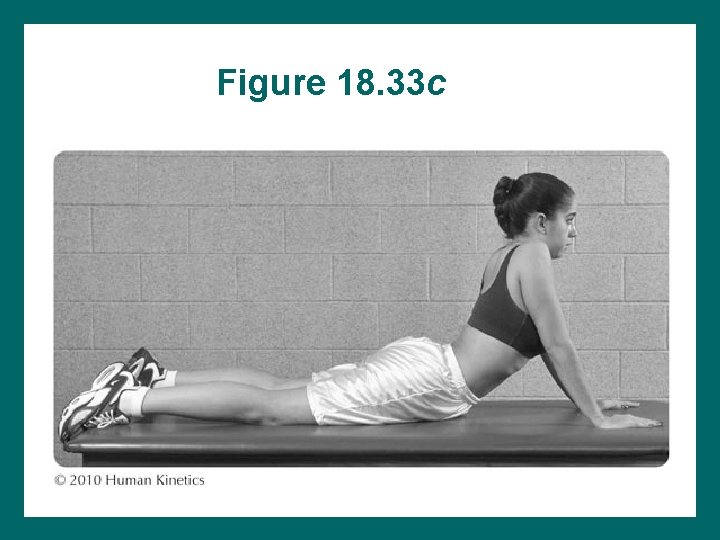
Figure 18. 33 c
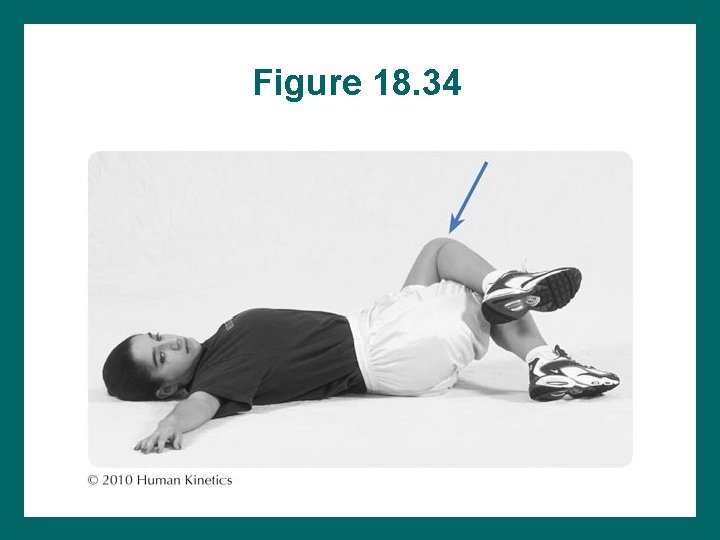
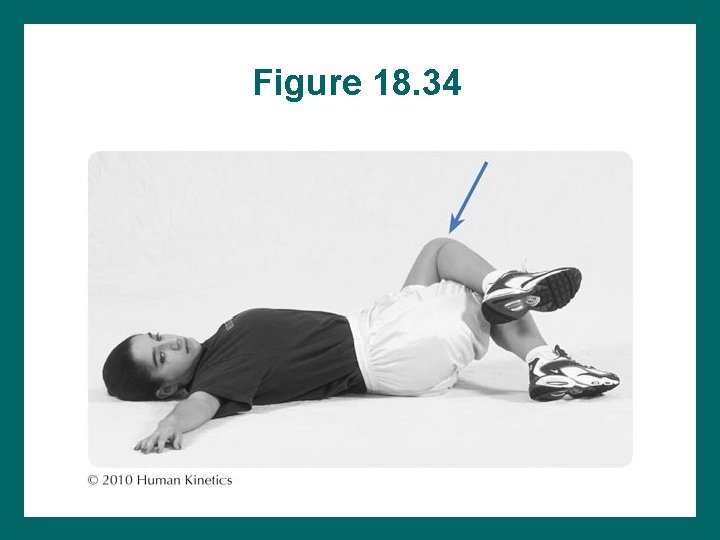
Figure 18. 34
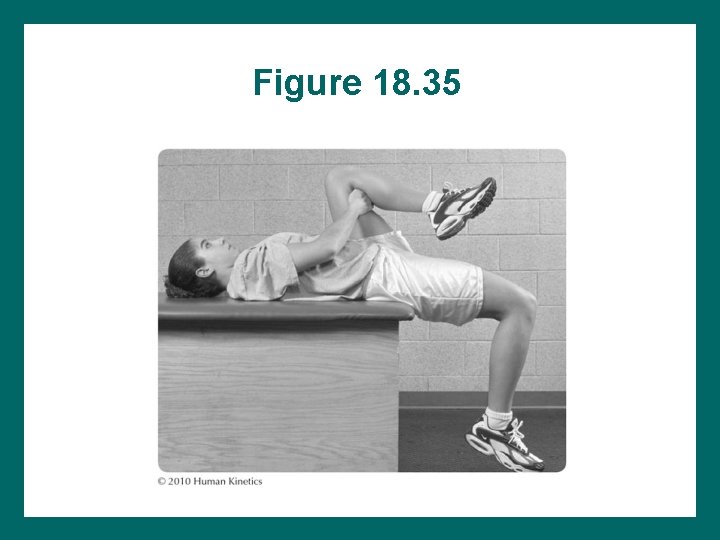
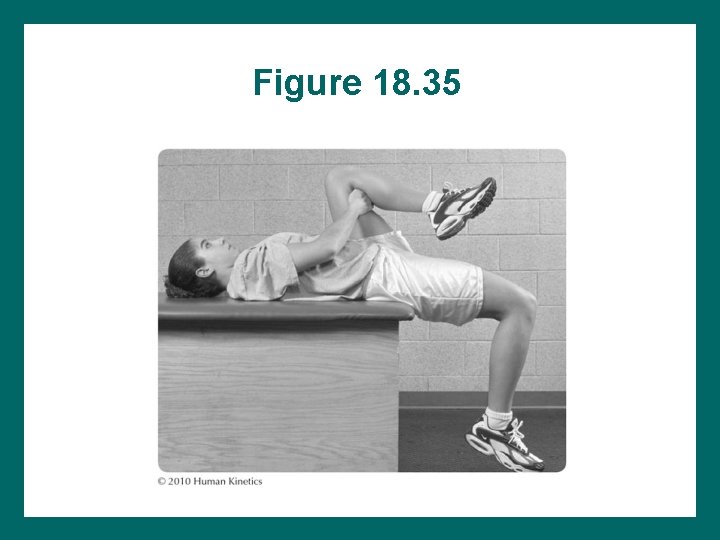
Figure 18. 35
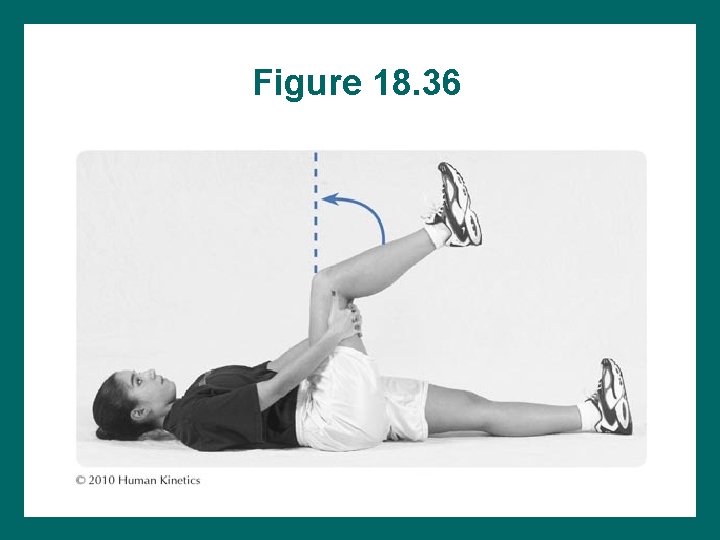
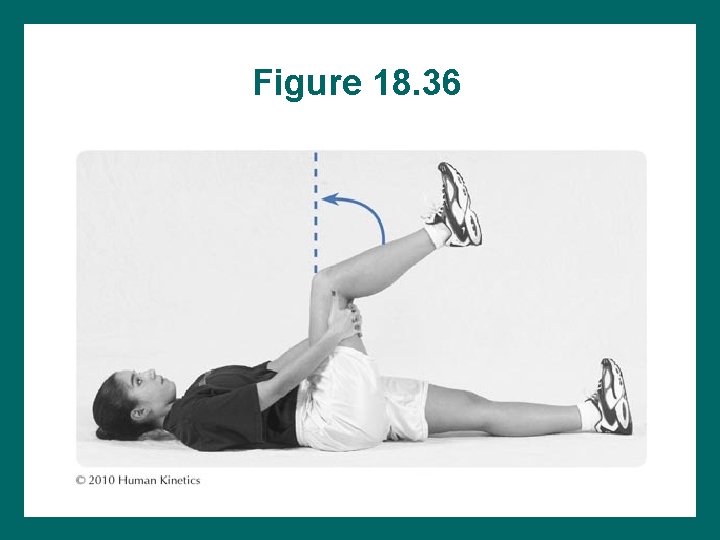
Figure 18. 36
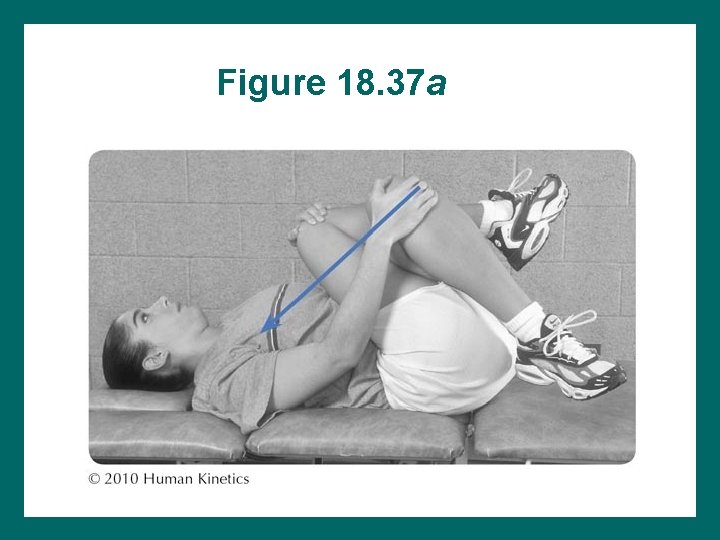
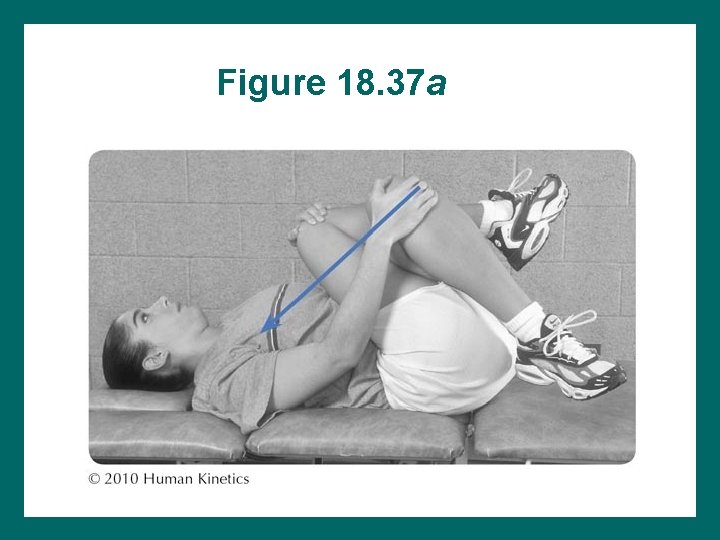
Figure 18. 37 a
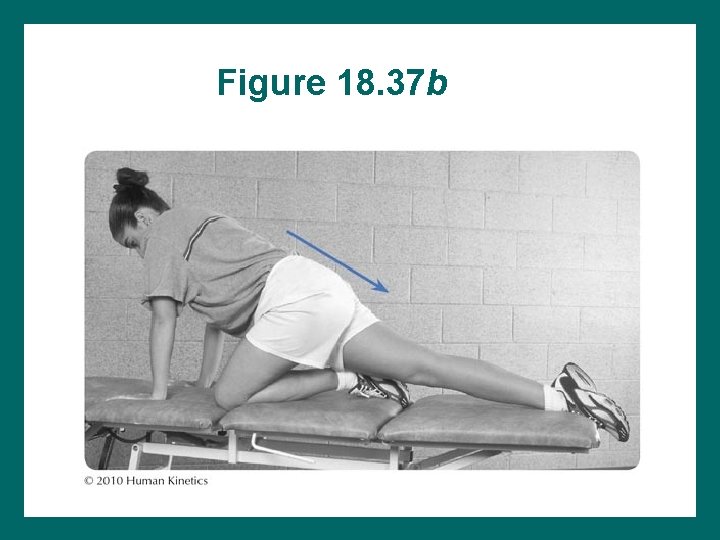
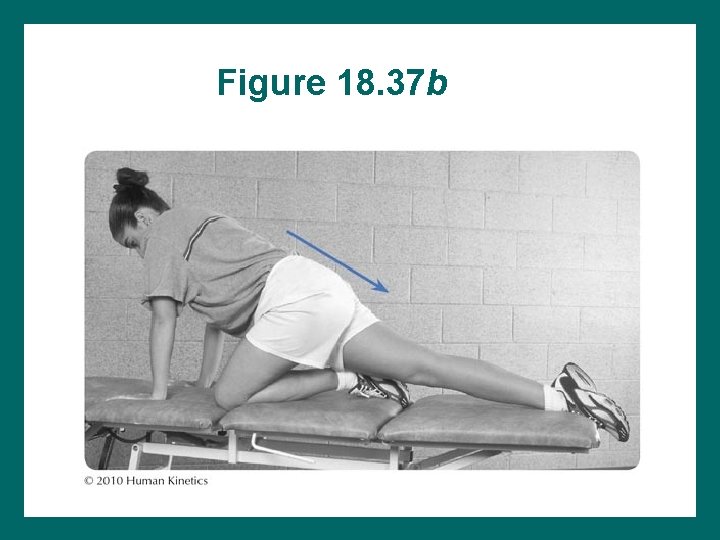
Figure 18. 37 b

Figure 18. 38
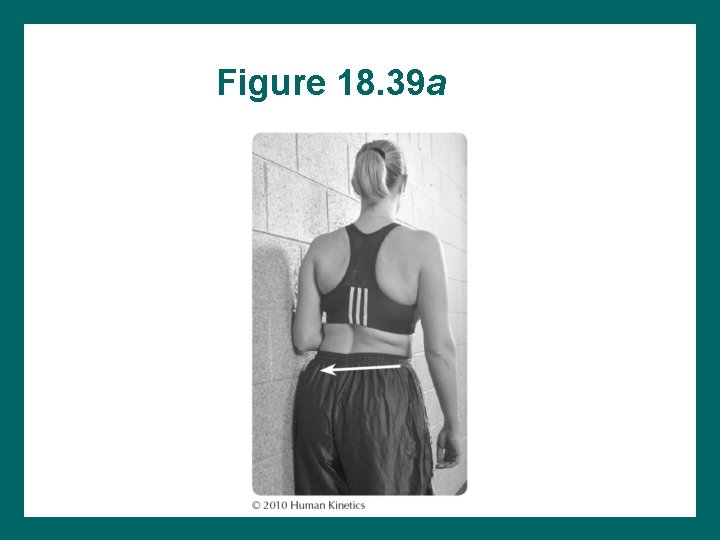
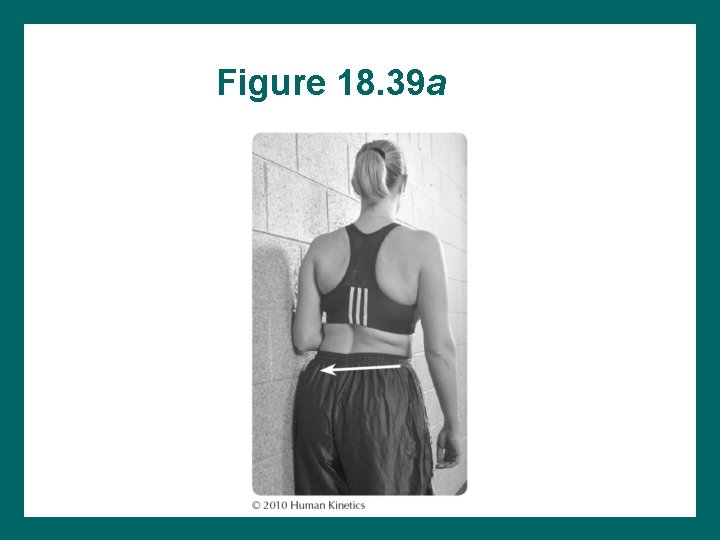
Figure 18. 39 a

Figure 18. 39 b
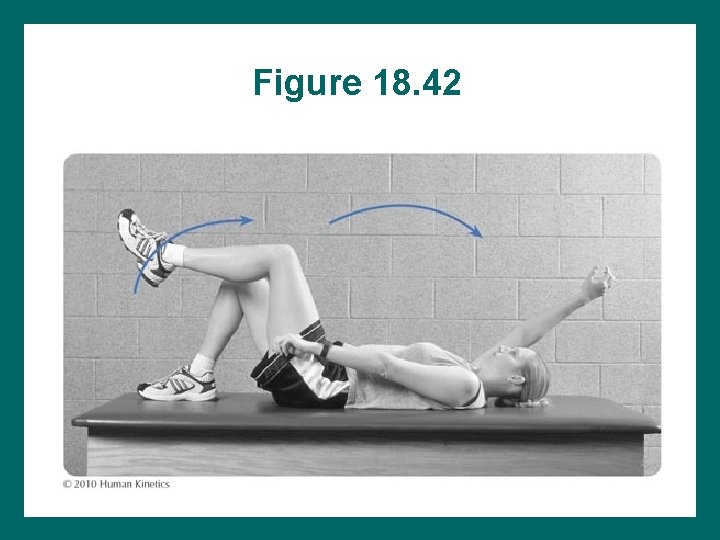
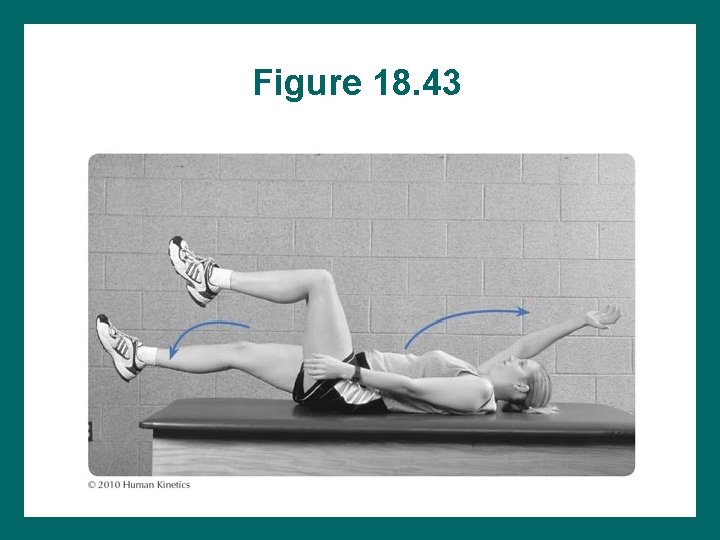
Dead Bug Exercises • Not all back patients need to do dead bug exercises. • Difficulty with these exercises means poor stabilization. • Exercises should be part of the program until performed correctly. • Only the extremities move during exercise.
Dead Bug Exercise Substitutions • • Hips are allowed to roll. Patient rolls from side to side. Lumbar spine moves. Abdominal and gluteal muscles do not remain tense. • Pelvic neutral is not maintained.

Dead Bug Exercise Progression 1. Trunk stabilization in supine with arm or leg movement, then both 2. Trunk stabilization in quadruped with arm or leg movement, then both 3. Trunk stabilization in standing with arm or leg movement, then both 4. Trunk stabilization during functional activities

Figure 18. 40
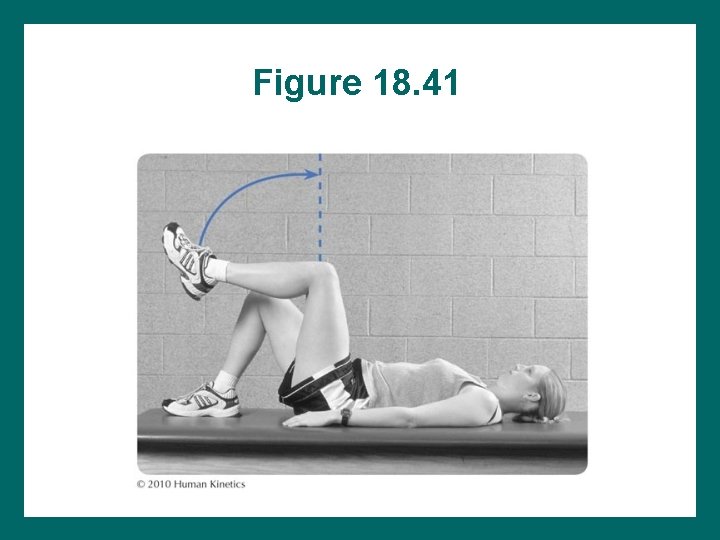
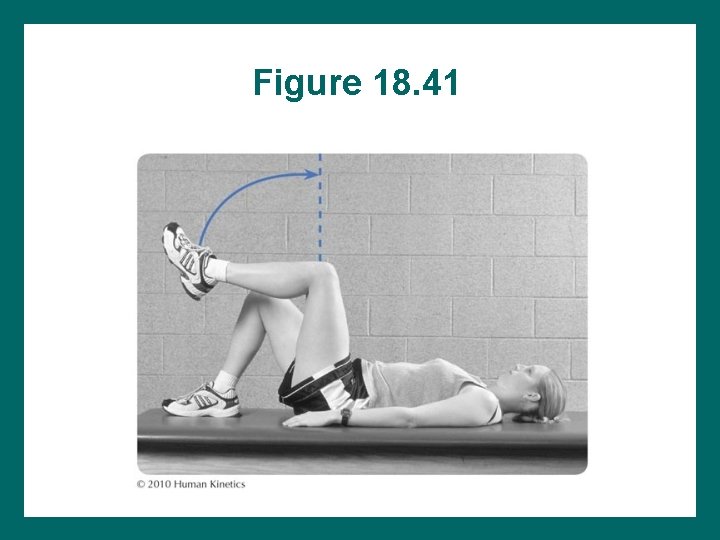
Figure 18. 41
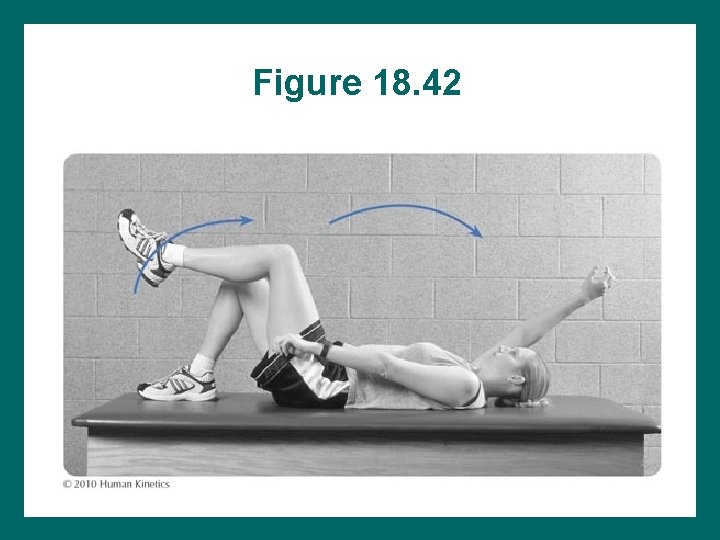
Figure 18. 42
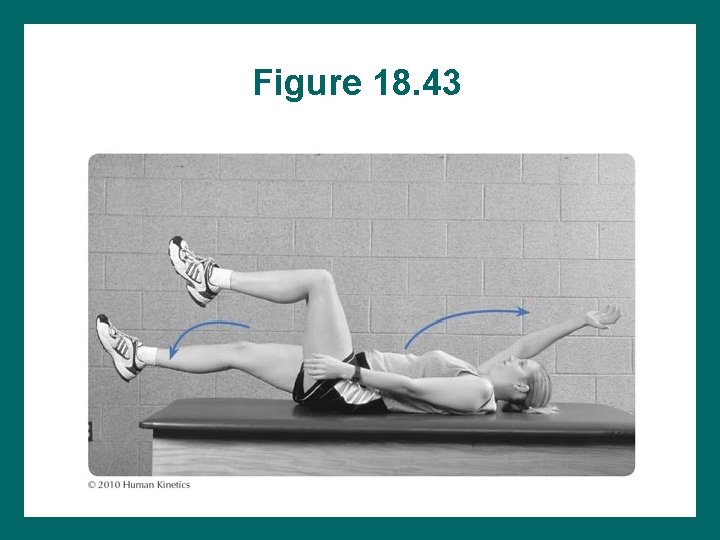
Figure 18. 43

Figure 18. 44
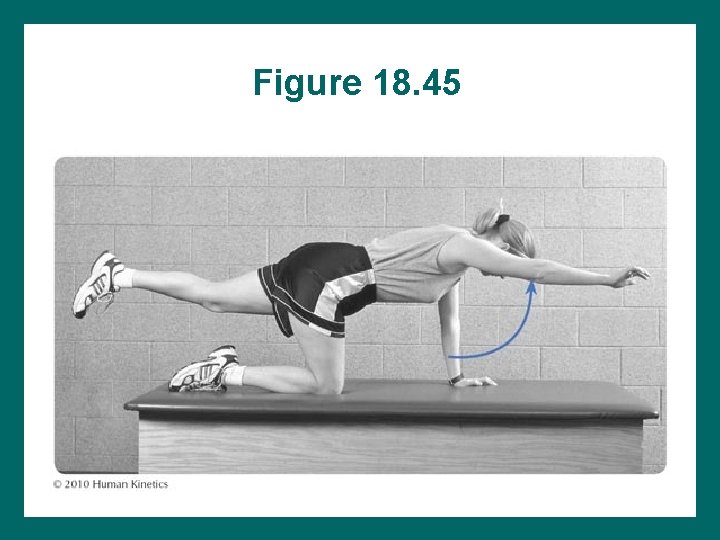
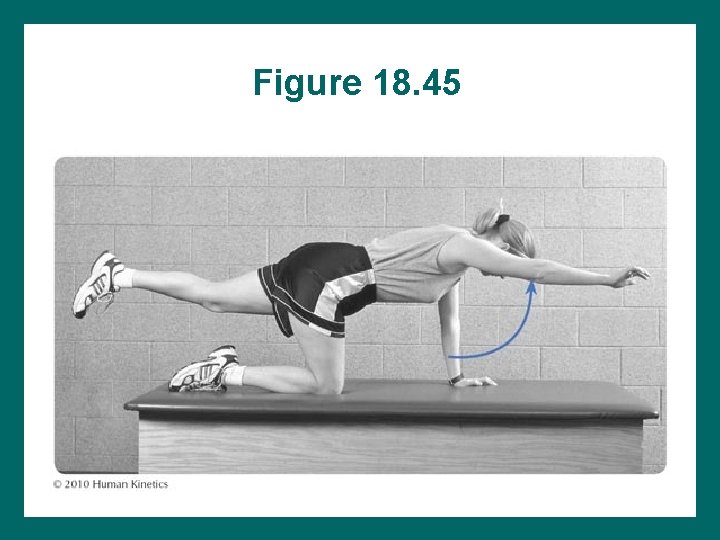
Figure 18. 45

Core Stability Also known as: • Pelvic stability • Spinal stability • Trunk stability • Lumbar stability
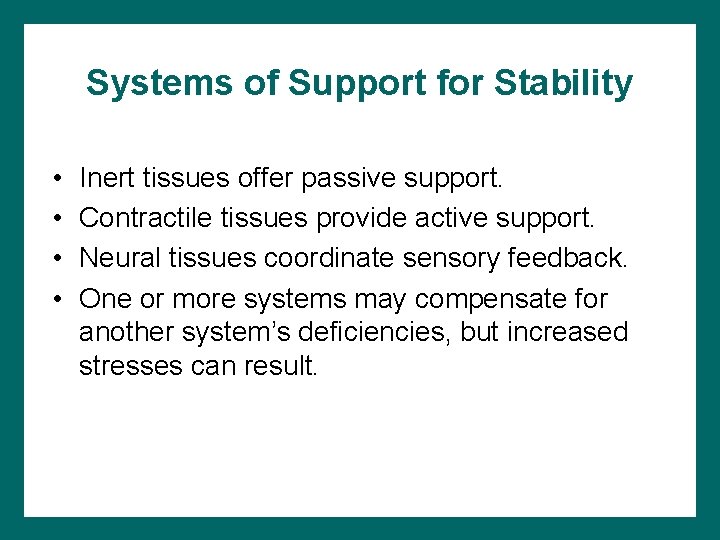
Systems of Support for Stability • • Inert tissues offer passive support. Contractile tissues provide active support. Neural tissues coordinate sensory feedback. One or more systems may compensate for another system’s deficiencies, but increased stresses can result.
Added Sources of Stabilization • • Thoracolumbar fascia Quadratus lumborum Latissimus dorsi Gluteus maximus and medius
Stabilization of Lumbar Spine Abdominal muscles – Superficial (rectus abdominis): prime movers of trunk flexion, not stabilizers – Deep (transverse abdominis): primary stabilizers • Not often well conditioned • Primary stabilizers of trunk during overhead and lower-limb activity • Assistance from obliques
Stabilization • Spine patients should be assessed for posture • Stabilization requires strength of: – – Transverse abdominis Internal obliques Core muscles Multifidus Lateral and posterior hip muscles
Pelvic Stabilization • During sports: abdominal muscles and back extensors—essential for trunk stabilization to serve as base of support for arm and leg movement • In rehab: trunk stability before trunk muscle performance

Other Factors • Just as trunk stabilization serves as a platform for arm and leg activities, hip stabilization serves as a platform for trunk movement. • Consider hip extensors, abductors, and adductors in rehab.
Lumbar Neutral • Refers to overall movement of the lumbar spine, not movement between vertebrae • Lumbar neutral = midway between full flexion and full extension via anterior-posterior pelvic tilting • Basic to stabilization – Places minimal stress on tissues – Best position from which trunk functions
Finding Pelvic Neutral • • • Start in sitting, supine, or standing. Fingers on anterior superior iliac spine (ASIS). Roll pelvis as far as possible forward. Roll pelvis as far as possible backward. Rock from each extreme to find the middle of the motion.
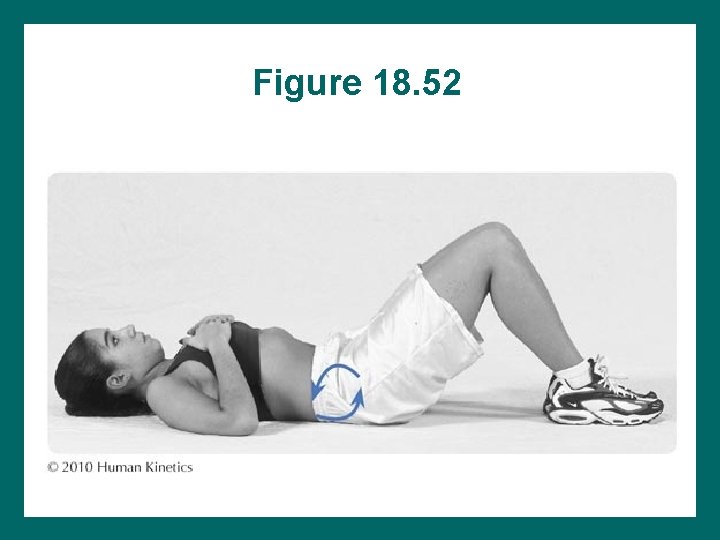
First Exercise to Hold Pelvic Neutral • Start in supine hooklying position. • Place blood pressure cuff under lower lumbar spine. • Find pelvic neutral. • Inflate cuff to 40 mm. Hg. • Tighten gluteal muscles. • Tighten abdominal muscles. • Cuff inflation should remain steady throughout exercises
Exercise Cues to Facilitate Multifidus • Keep pelvic neutral position. • Tighten pelvic floor muscles: Tighten as if stopping urination midflow.
Exercise Cues to Facilitate Transverse Abdominis • Pull navel to spine. • Keep pelvic neutral position. • Place hand on ASIS or sternum or belly for feedback. • Pull in stomach harder as arm or leg moves away from body’s center. • Stop when position is lost.
Early Exercise • Start with feet off floor, hips and knees flexed. • Lower one foot, then the other. • Gradually land foot away from buttock.
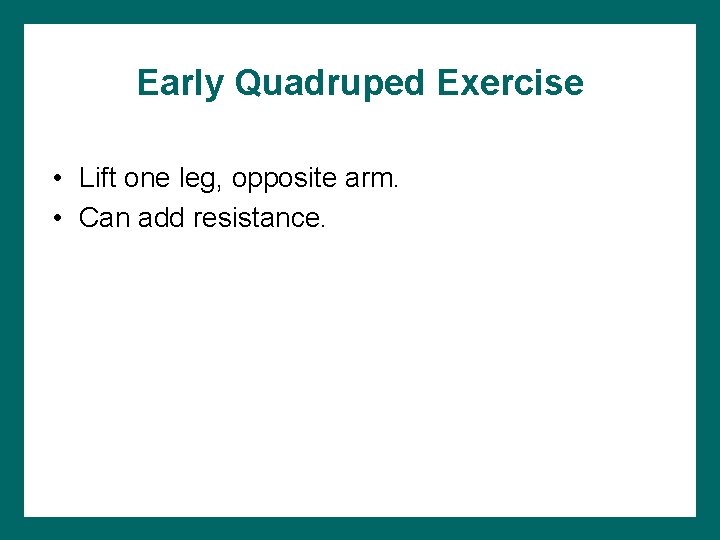
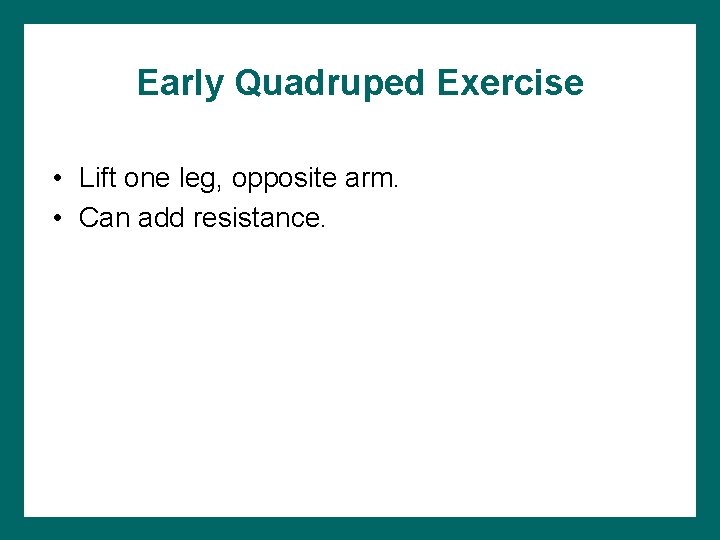
Early Quadruped Exercise • Lift one leg, opposite arm. • Can add resistance.
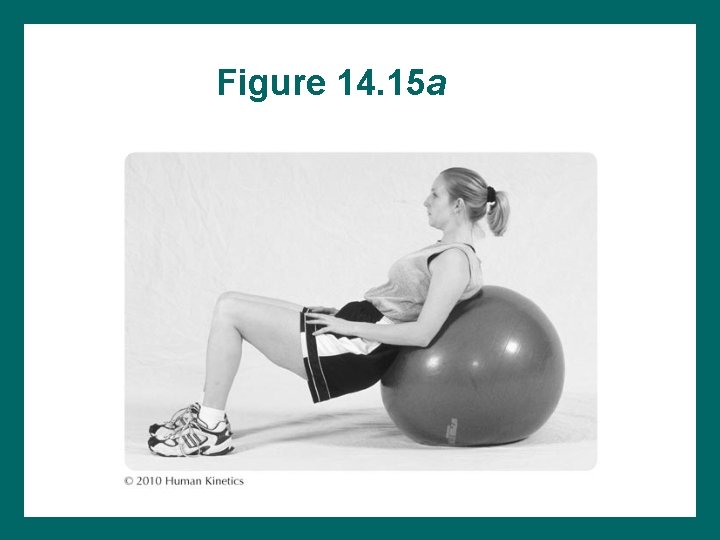
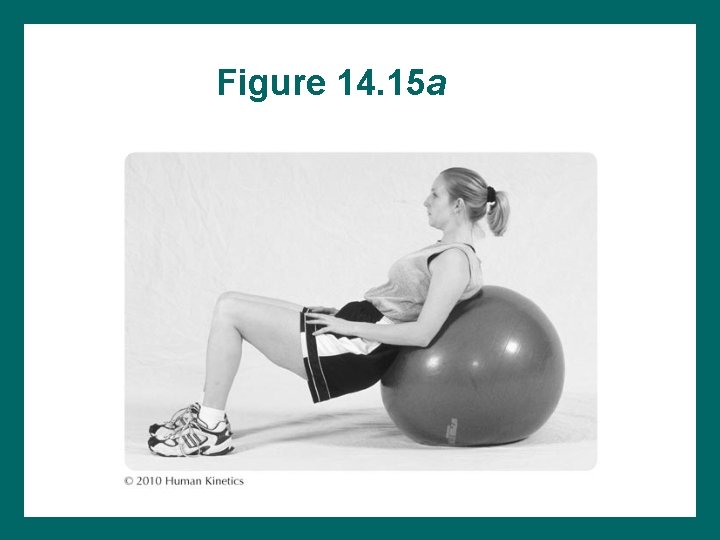
Figure 14. 15 a
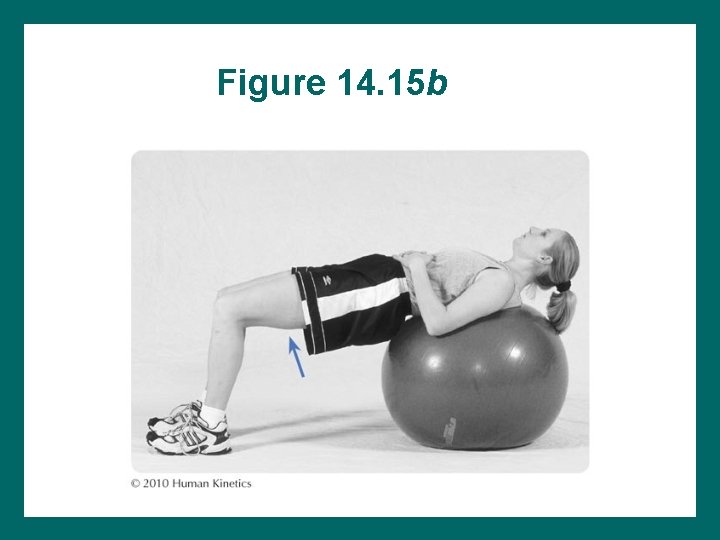
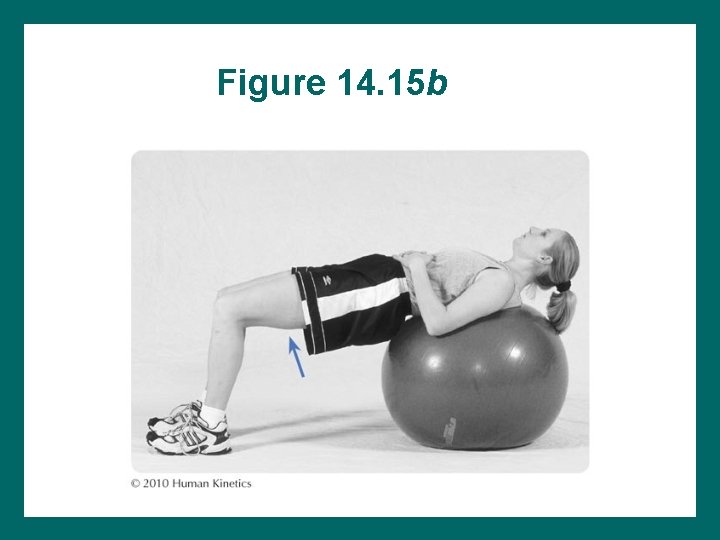
Figure 14. 15 b
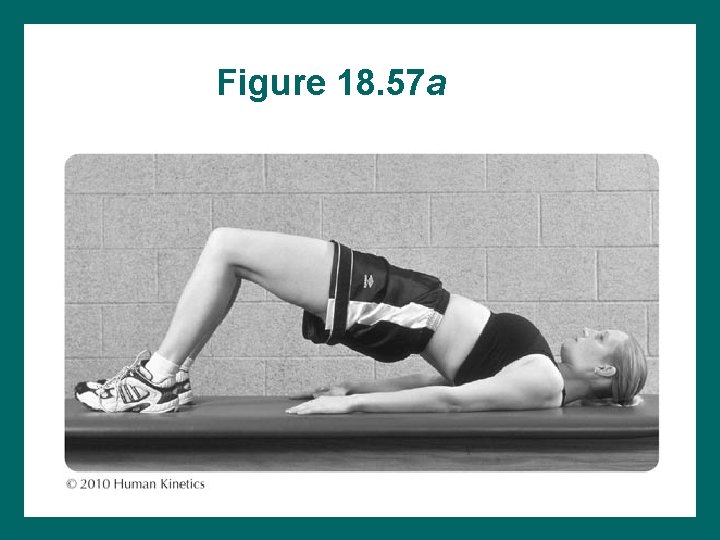
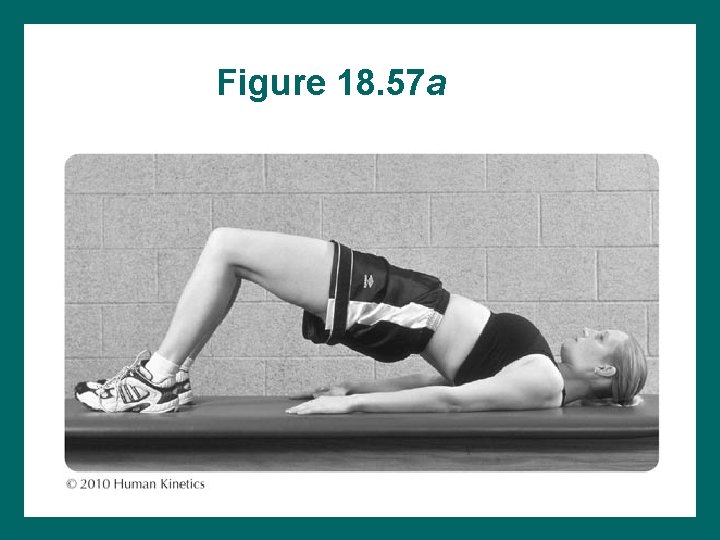
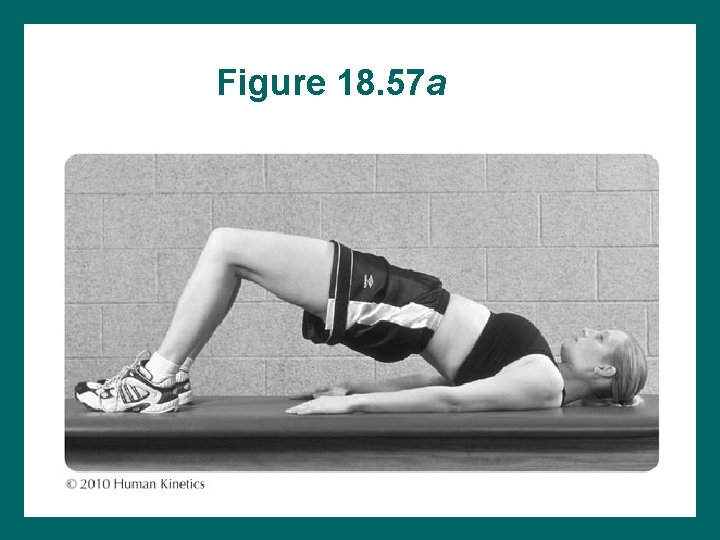
Figure 18. 57 a
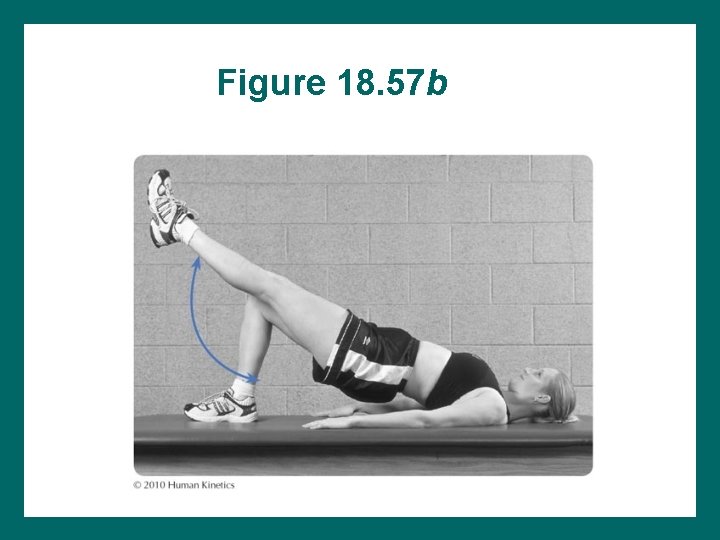
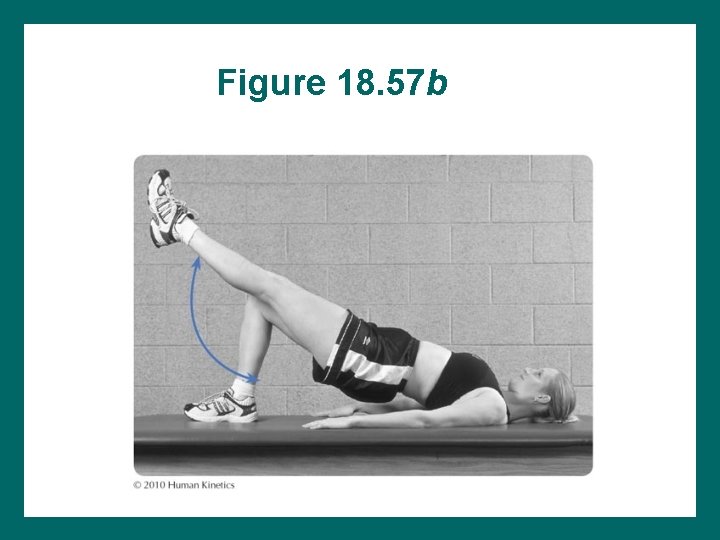
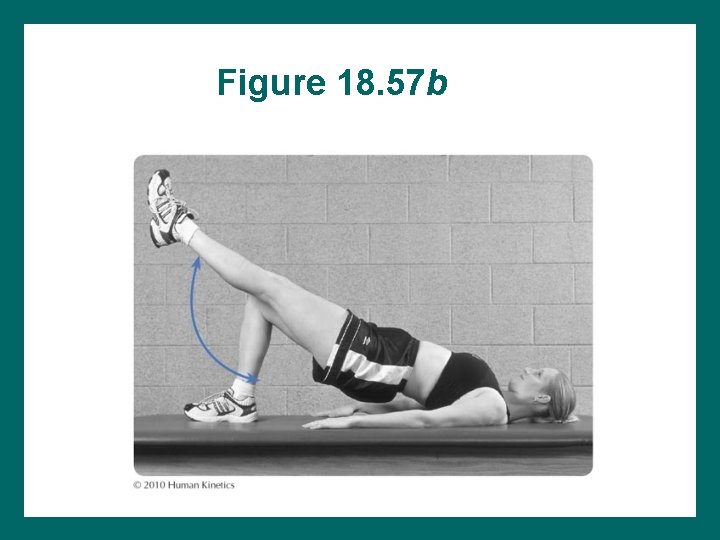
Figure 18. 57 b
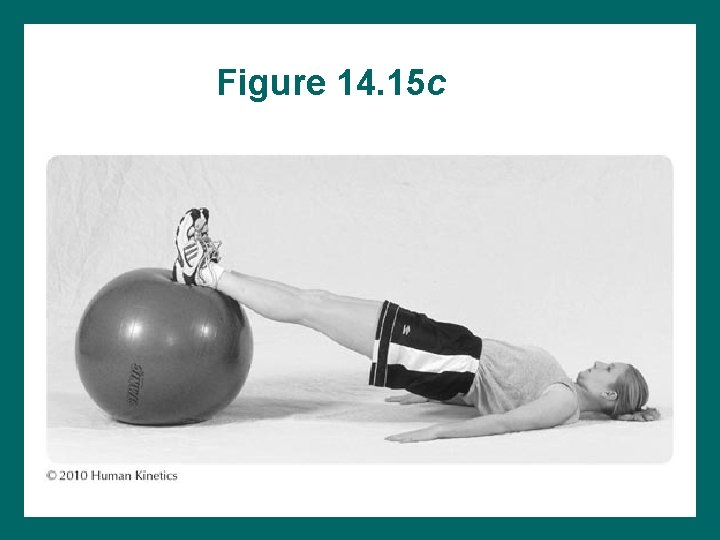
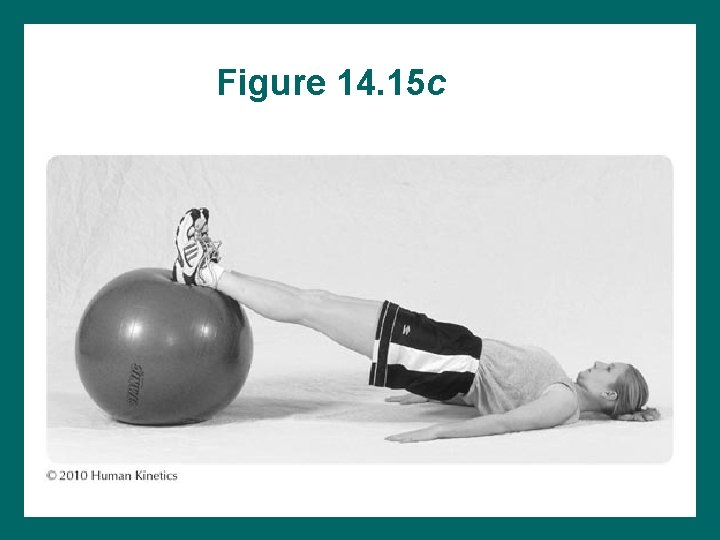
Figure 14. 15 c
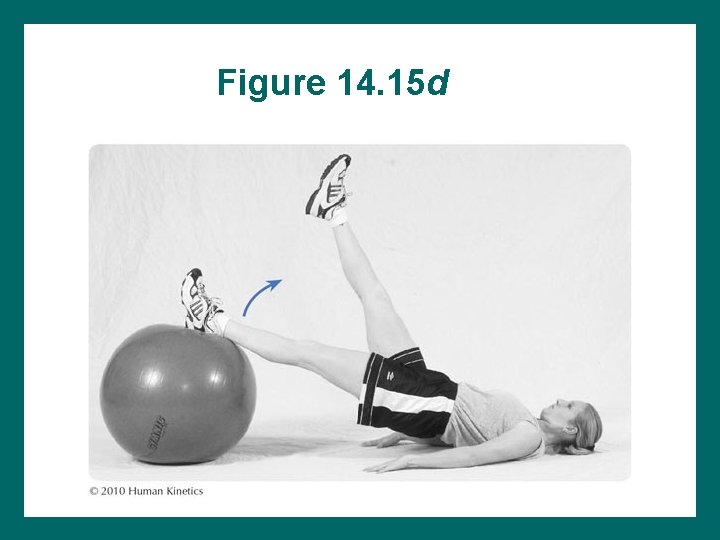
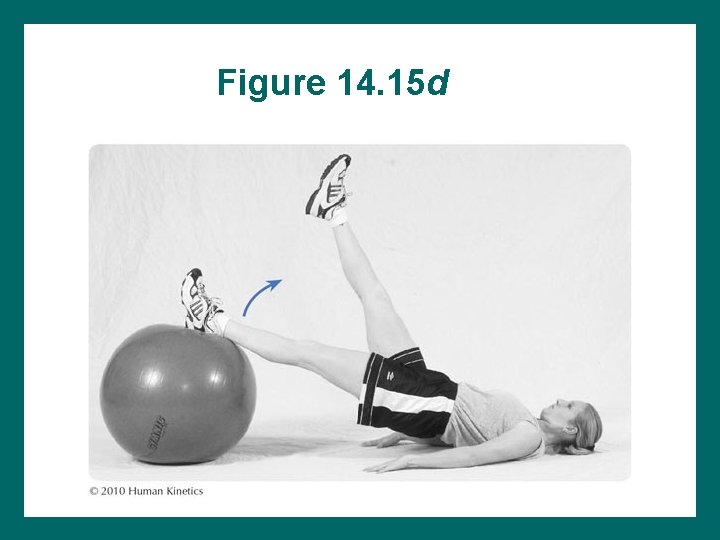
Figure 14. 15 d
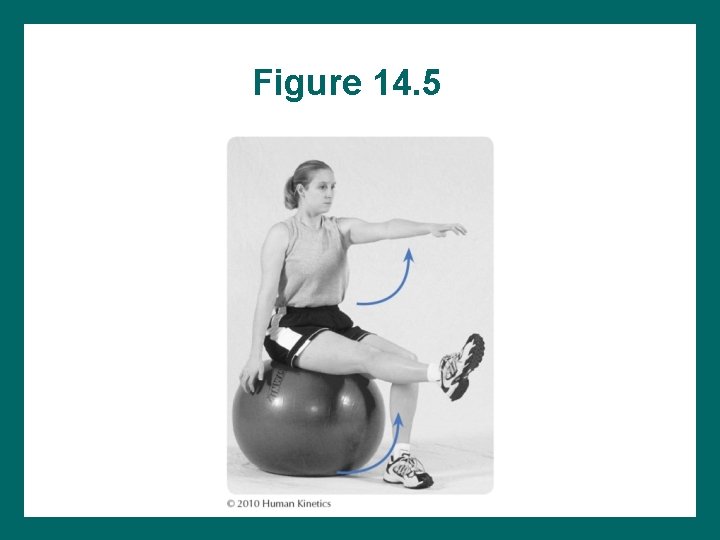
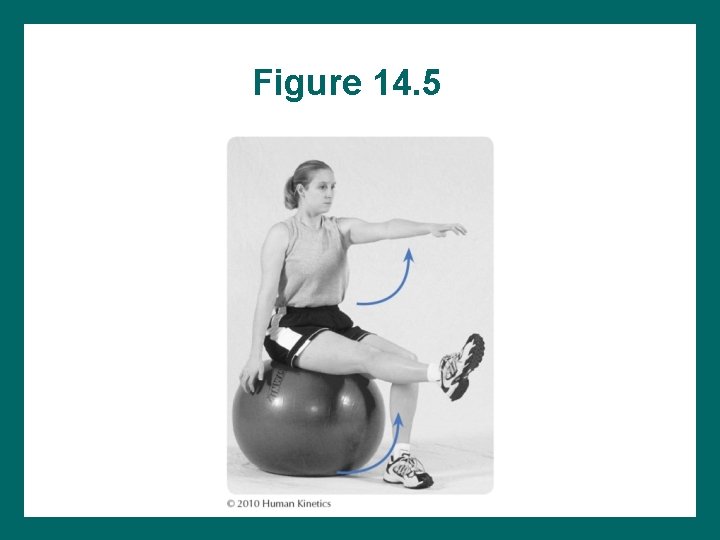
Figure 14. 5
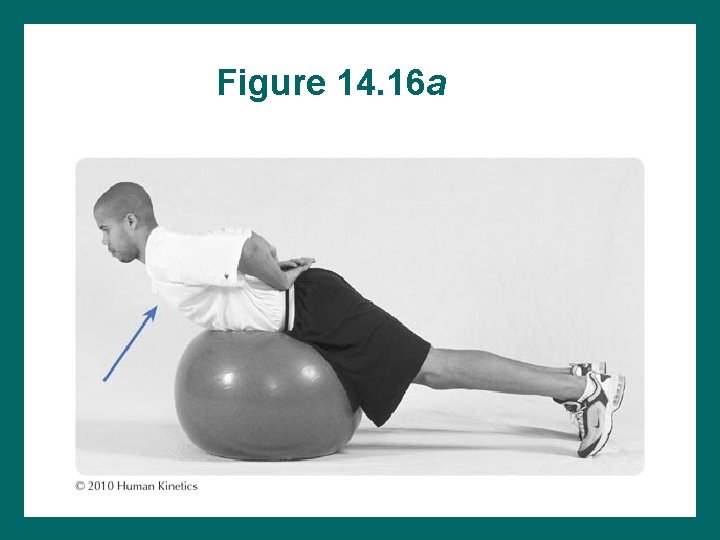
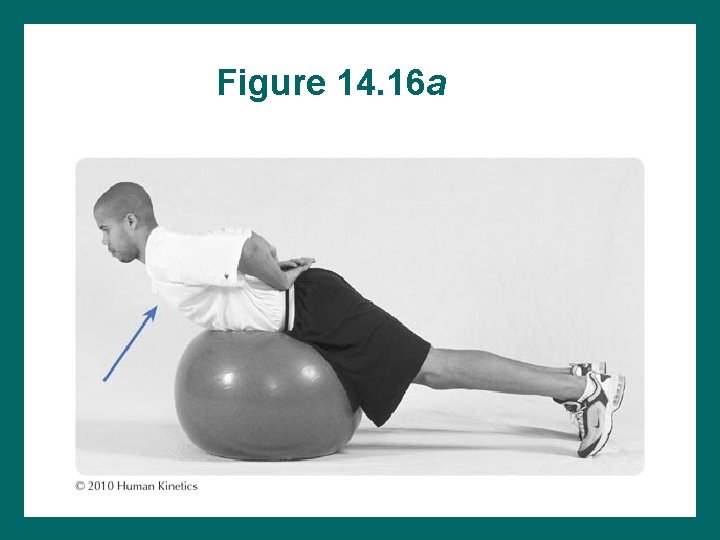
Figure 14. 16 a
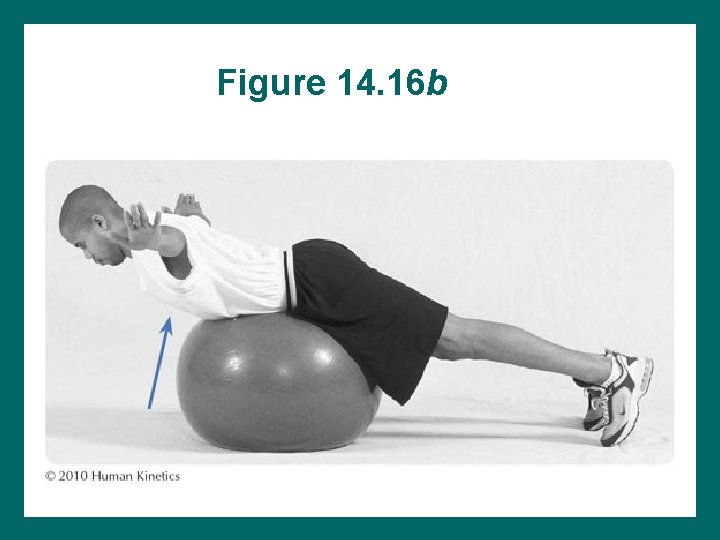
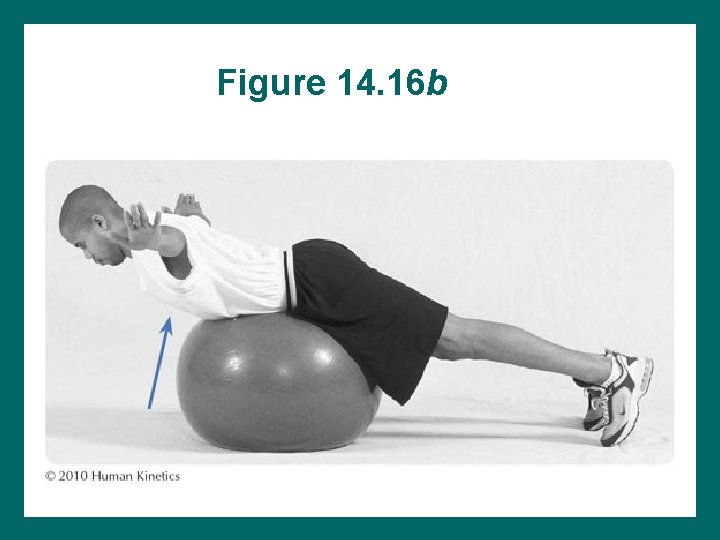
Figure 14. 16 b
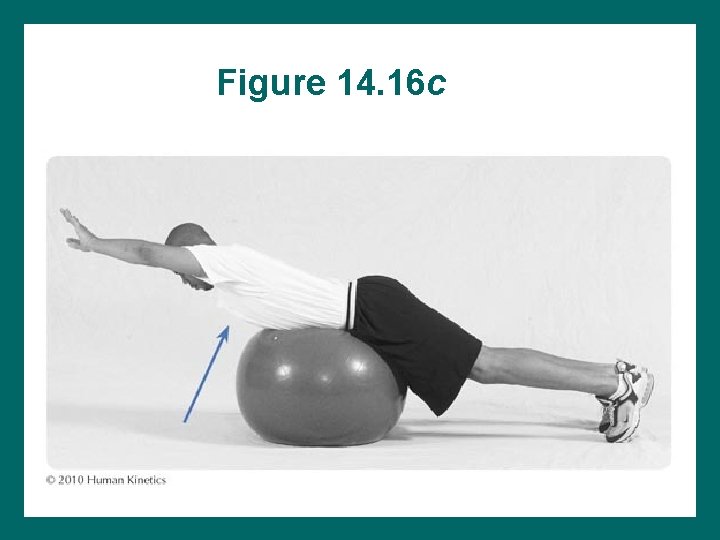
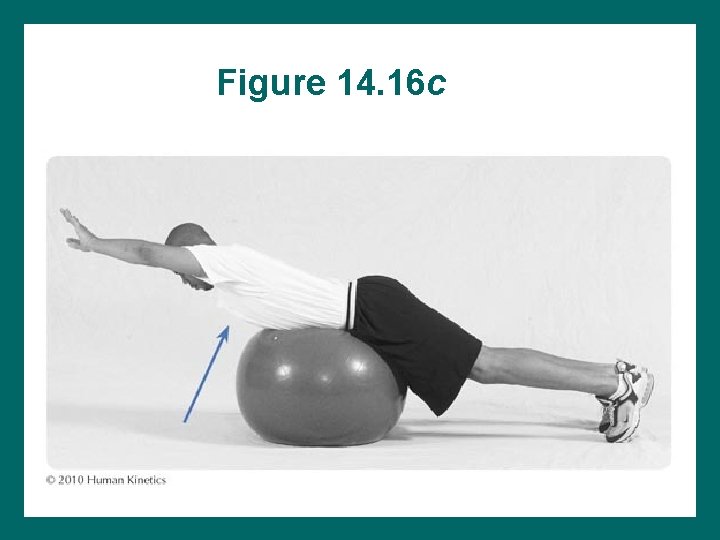
Figure 14. 16 c
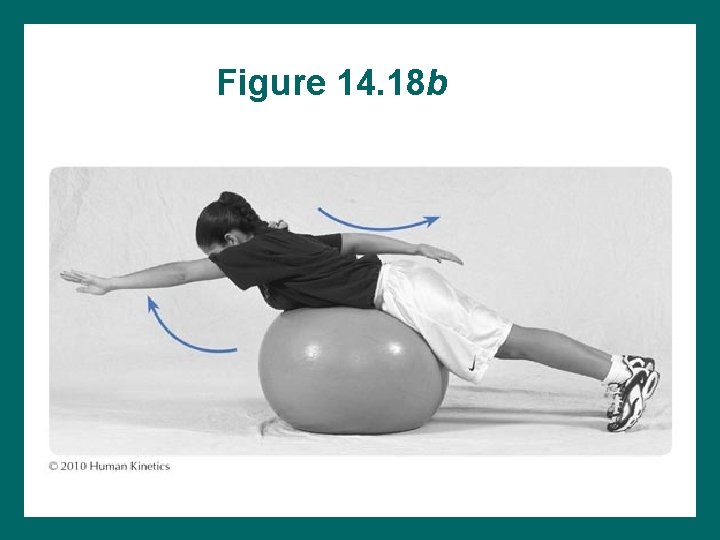
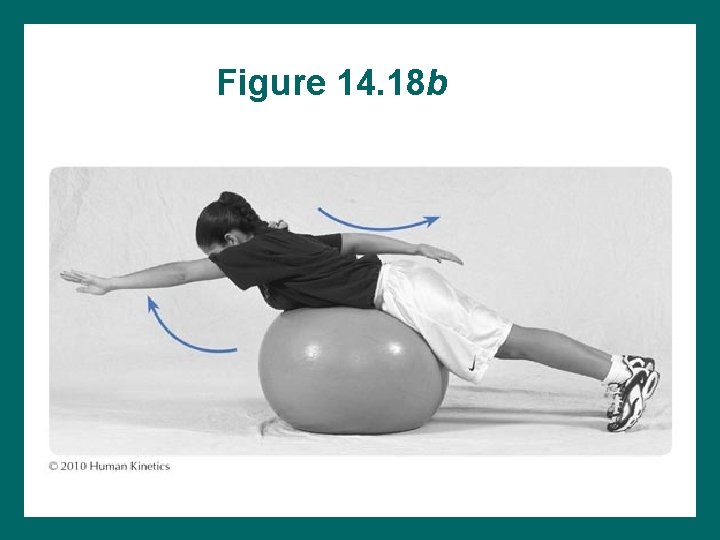
Figure 14. 18 b
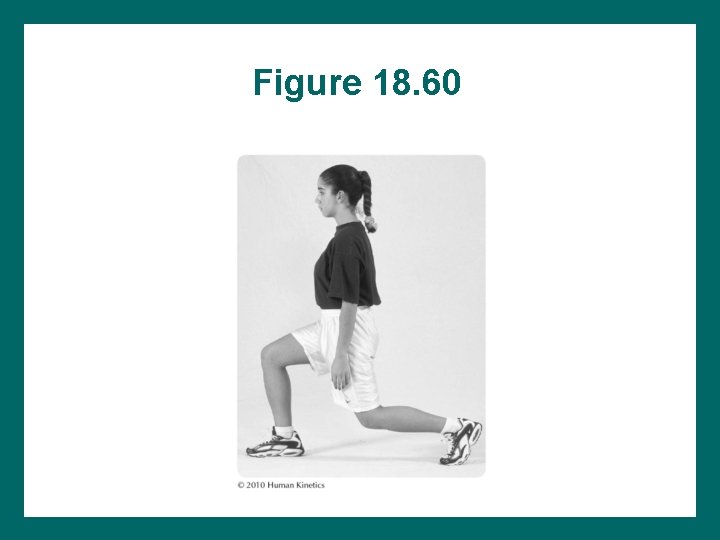
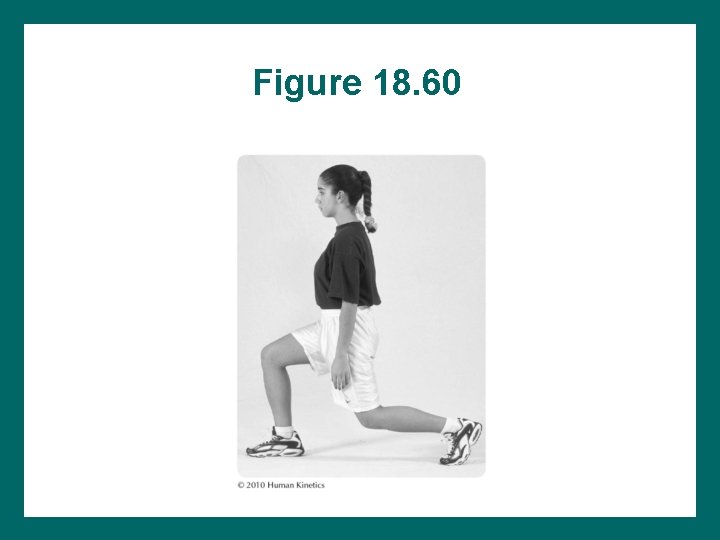
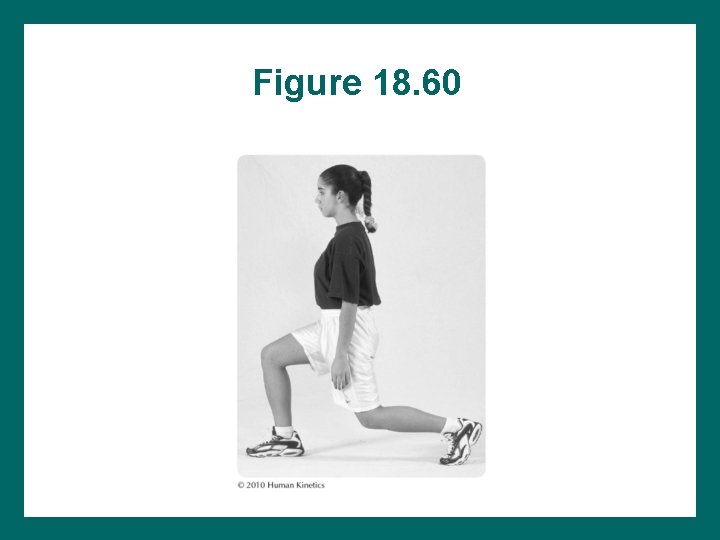
Figure 18. 60
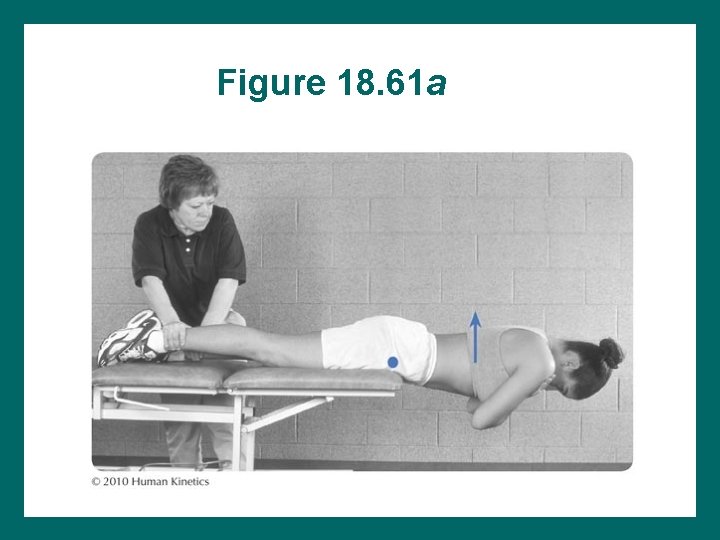
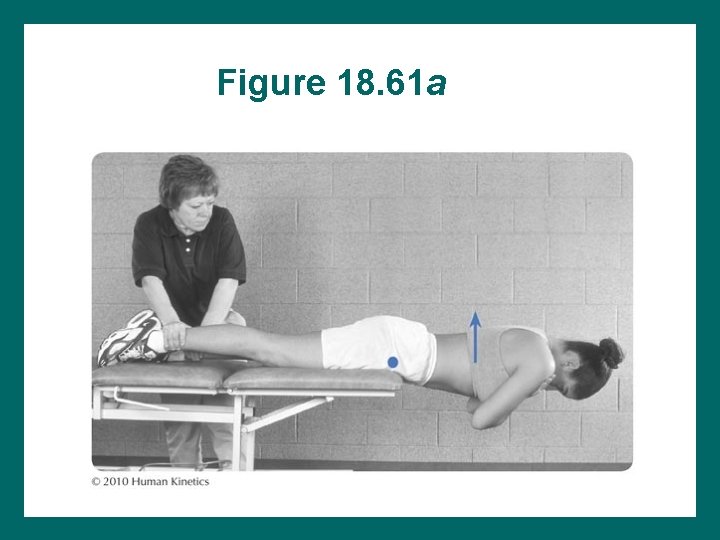
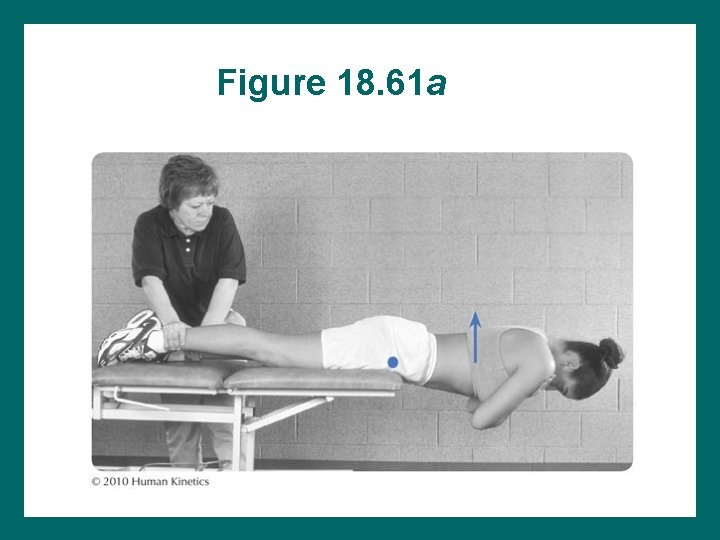
Figure 18. 61 a
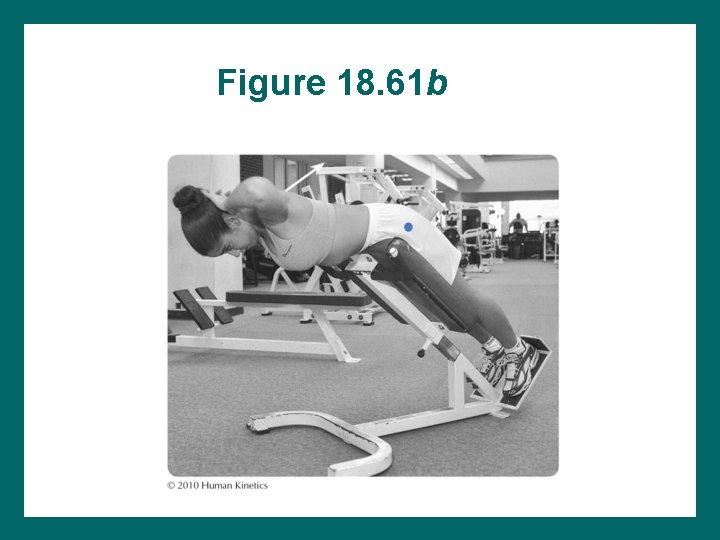
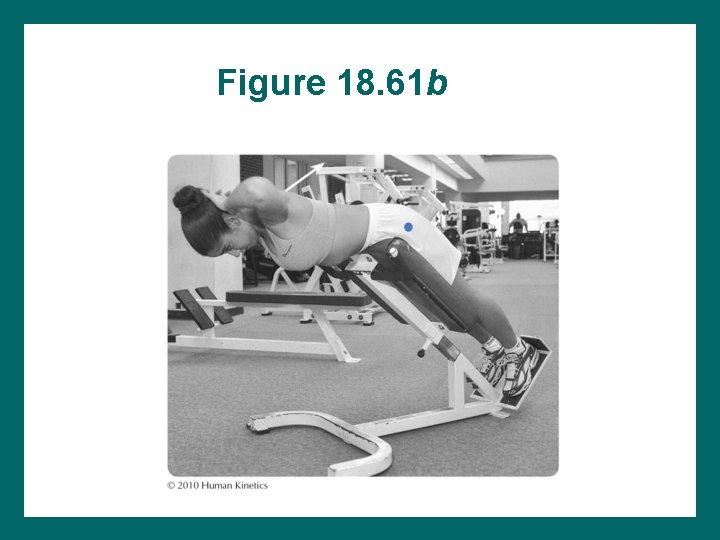
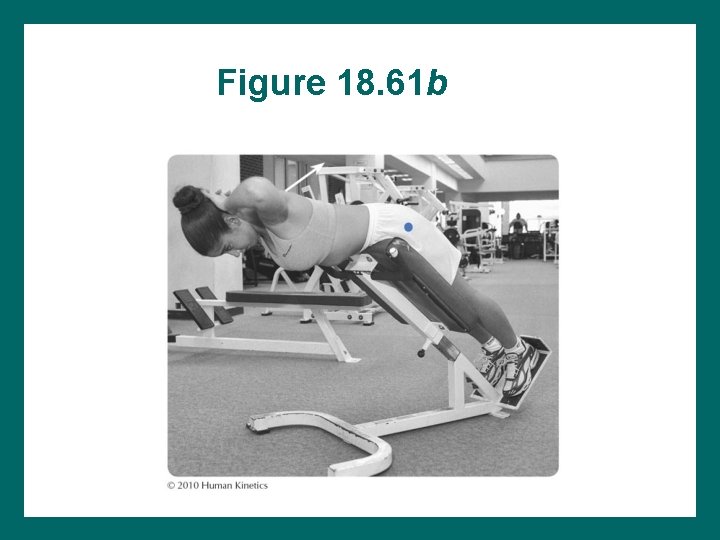
Figure 18. 61 b
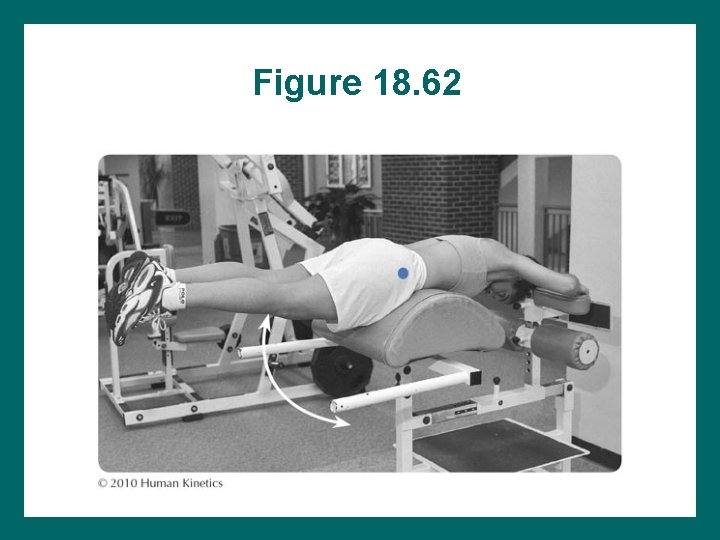
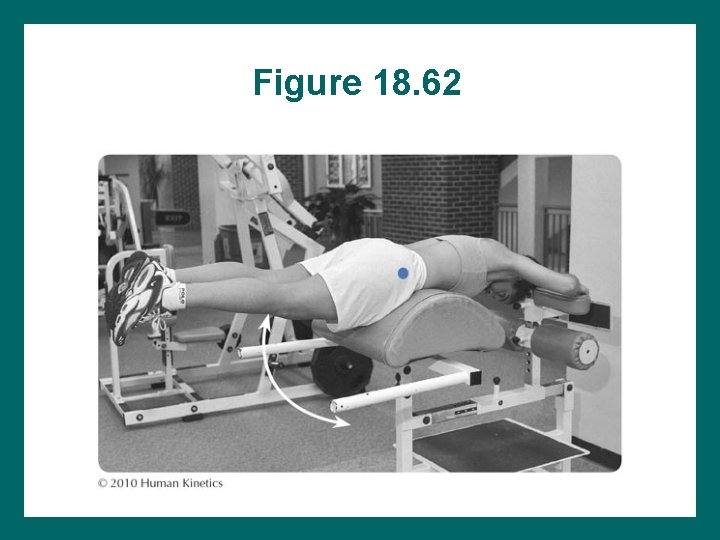
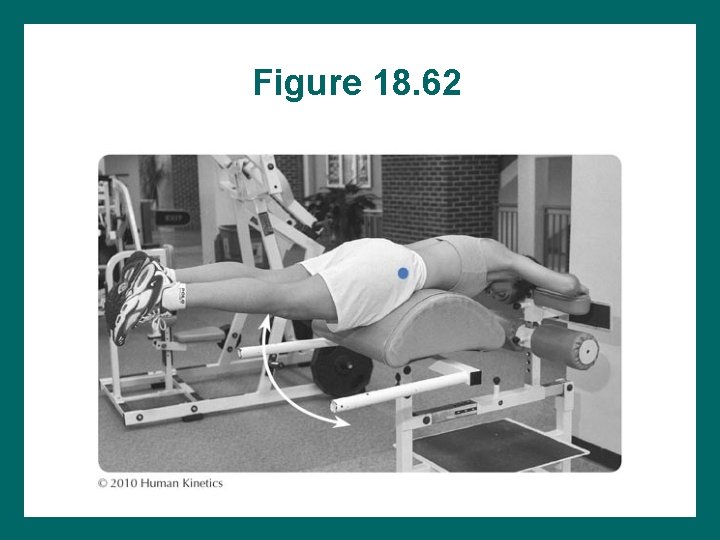
Figure 18. 62
Additional Advanced Stabilization Exercises • • Seated stick motion on Swiss ball Prone stick motion on Swiss ball Jumping activities in pelvic neutral Kicking in pelvic neutral – Without pulley/Thera-Band™ resistance – With pulley/Thera-Band™ resistance • Walking running in pelvic neutral
Functional Activities • • • Sit-to-stand Bending Lifting Kicking: rotation from hips, not back Stair climbing Sport activities
Strengthening Exercises • • Aquatic exercises Swiss ball exercises Foam roller exercises Resistance exercises – – – Rubber tubing and bands Dumbbells Pulleys Machines Medicine balls
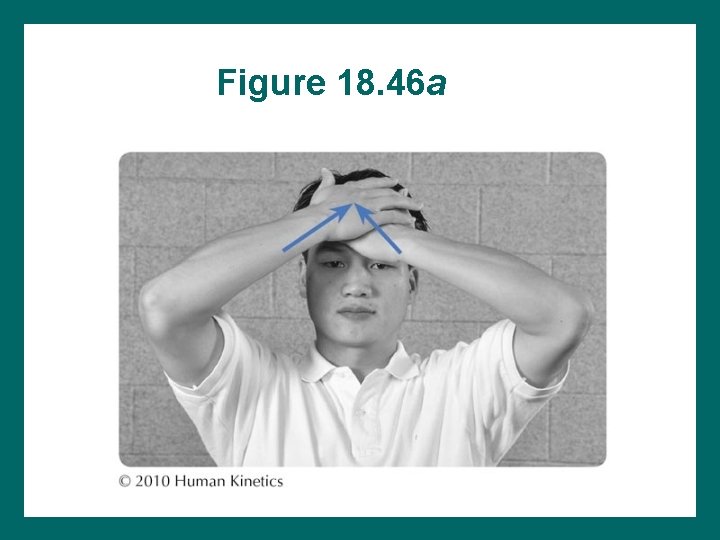
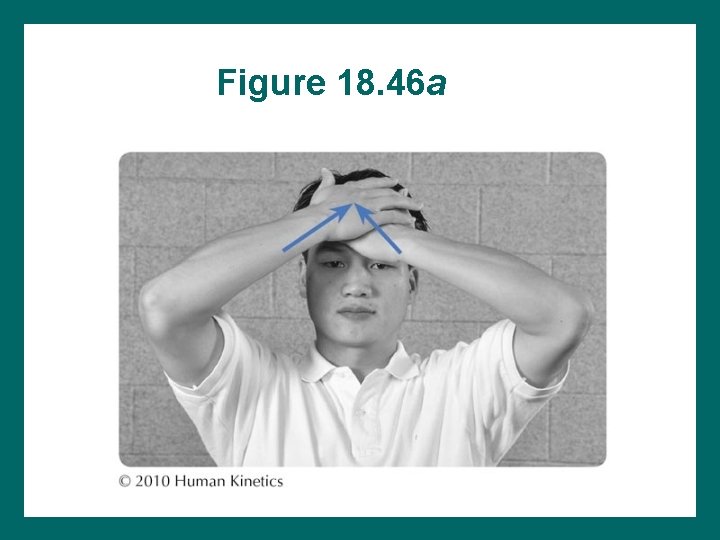
Figure 18. 46 a
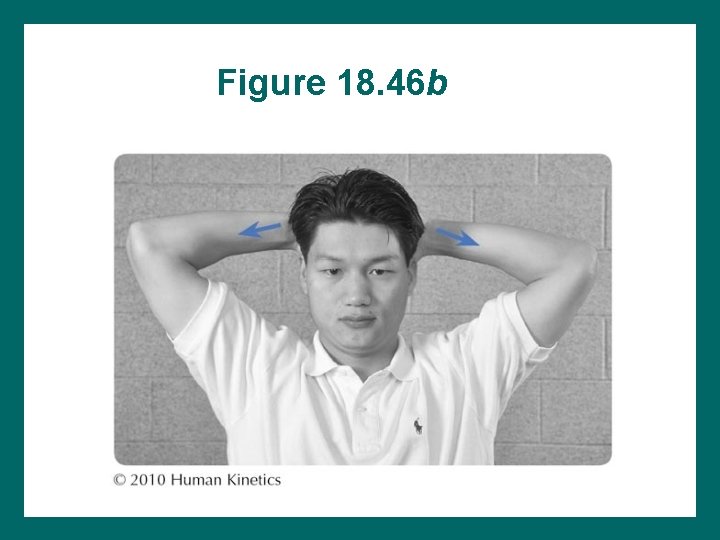
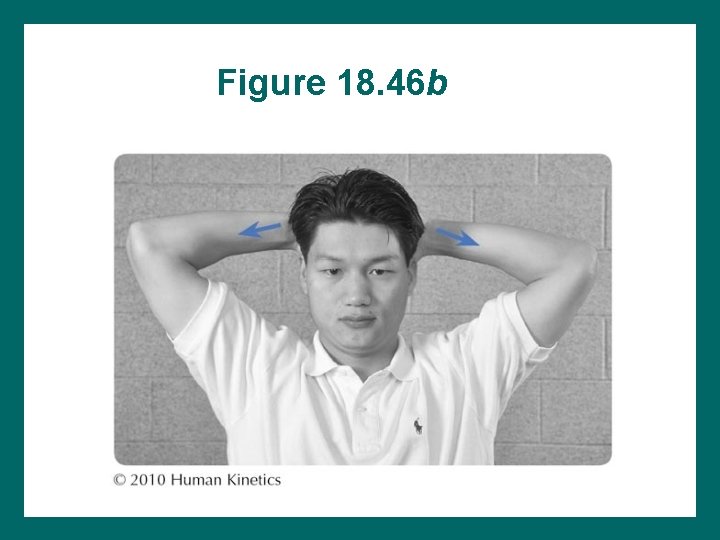
Figure 18. 46 b
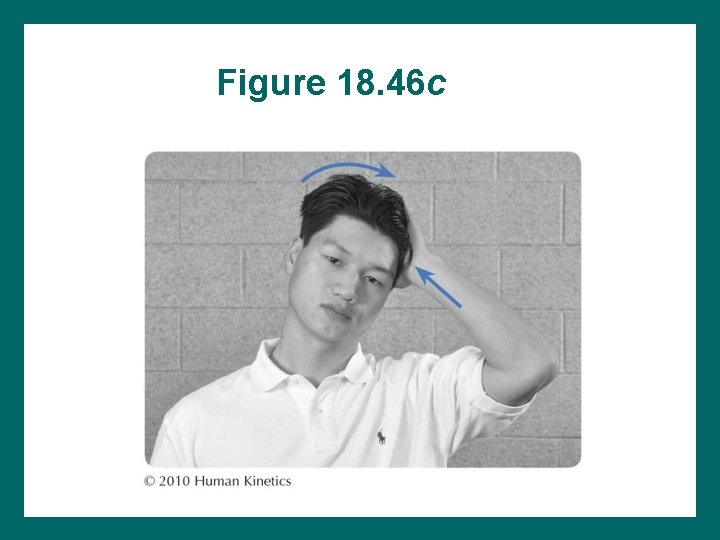
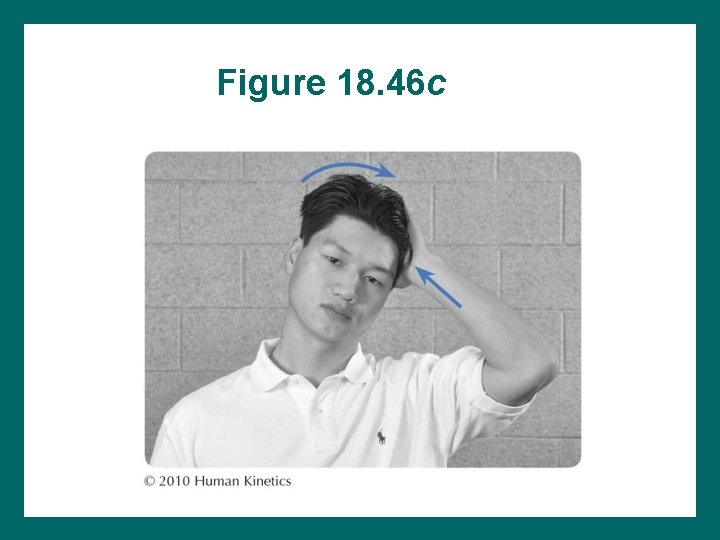
Figure 18. 46 c
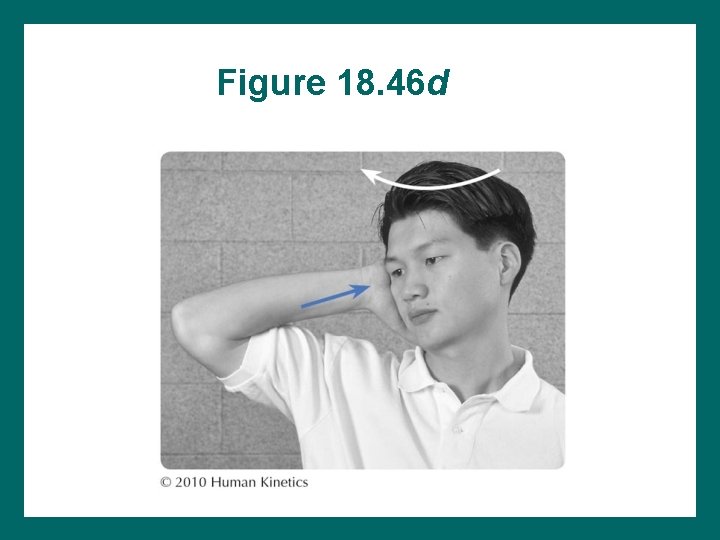
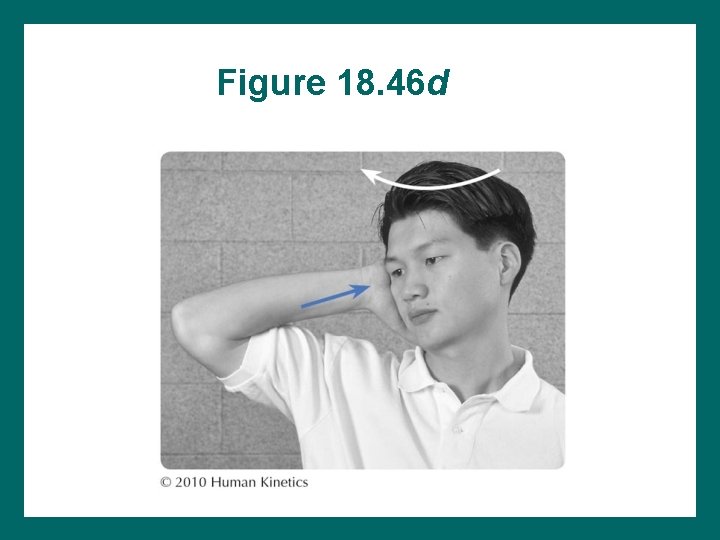
Figure 18. 46 d

Figure 18. 47
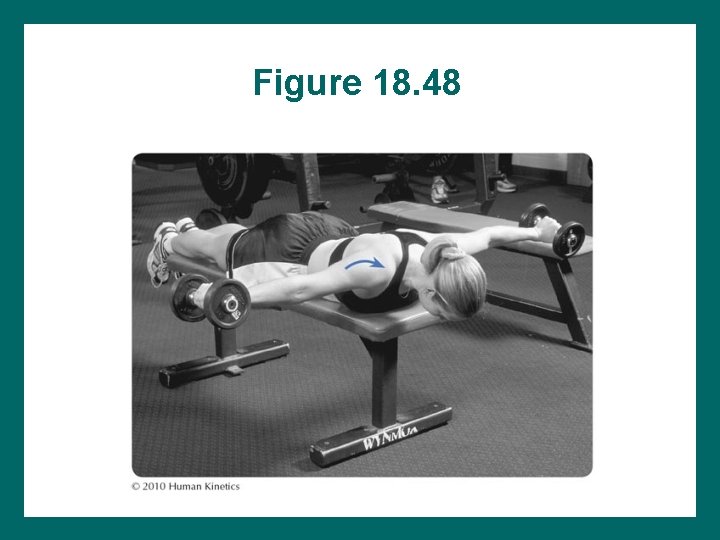
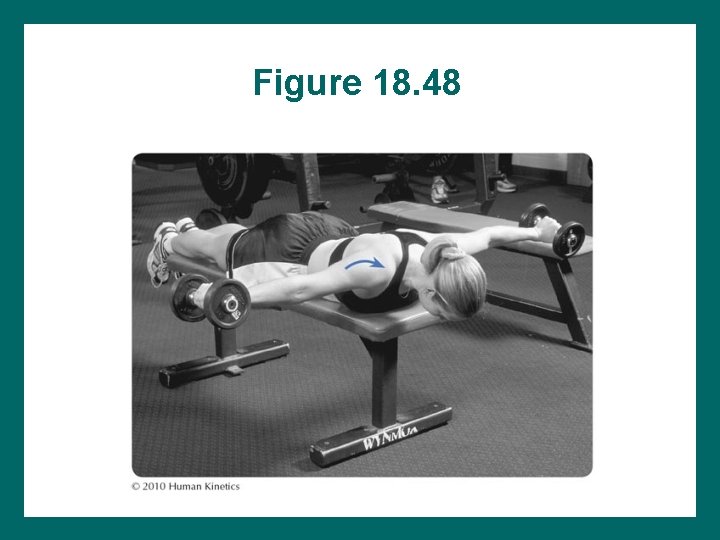
Figure 18. 48

Figure 18. 49
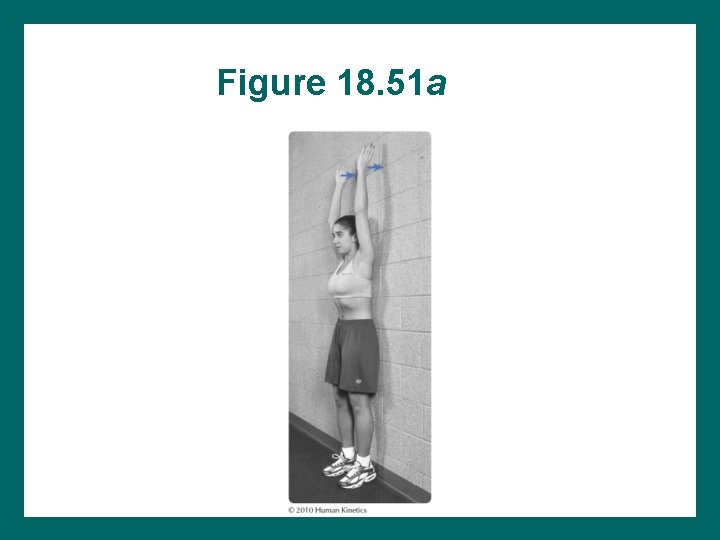
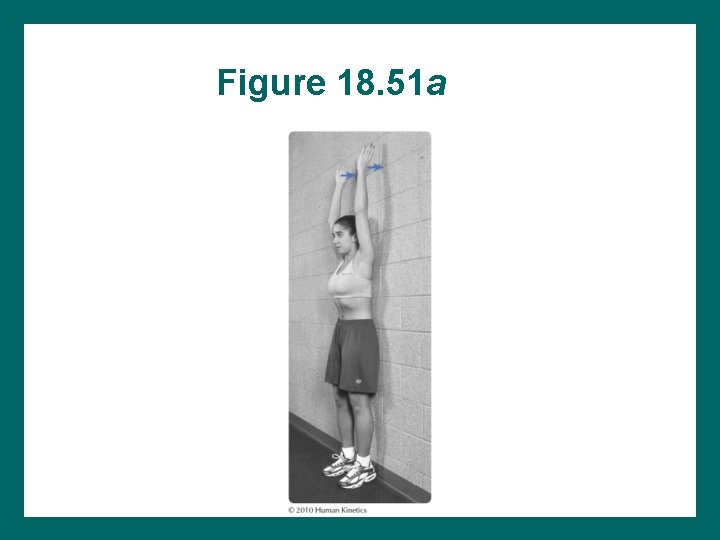
Figure 18. 51 a
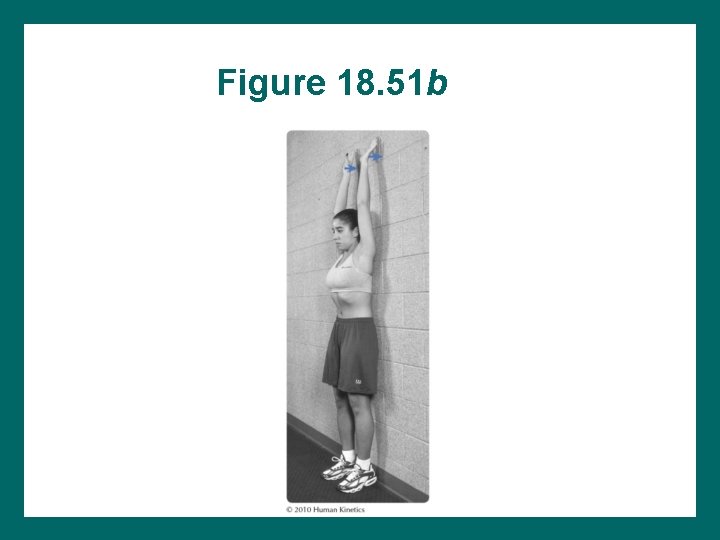
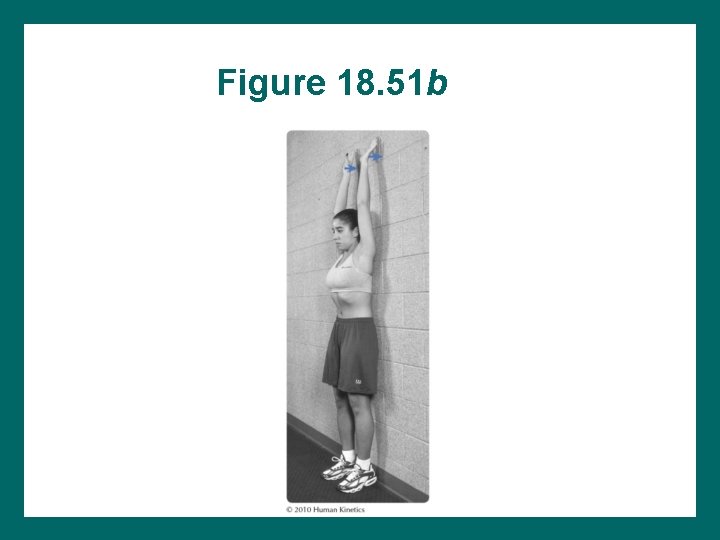
Figure 18. 51 b
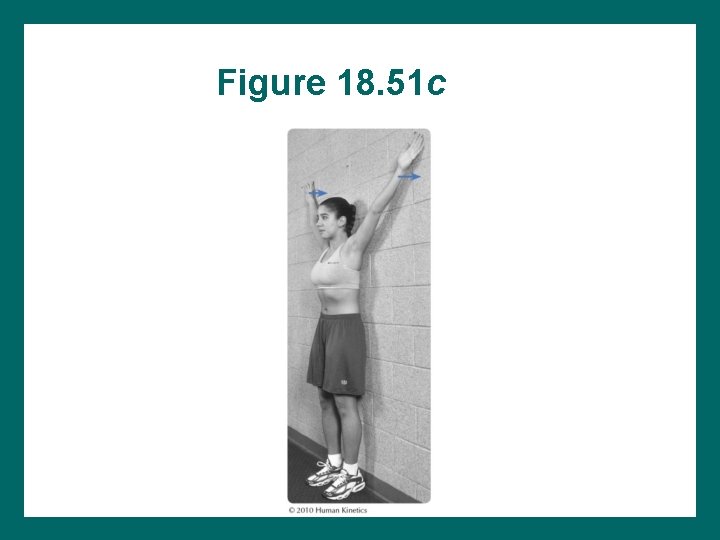
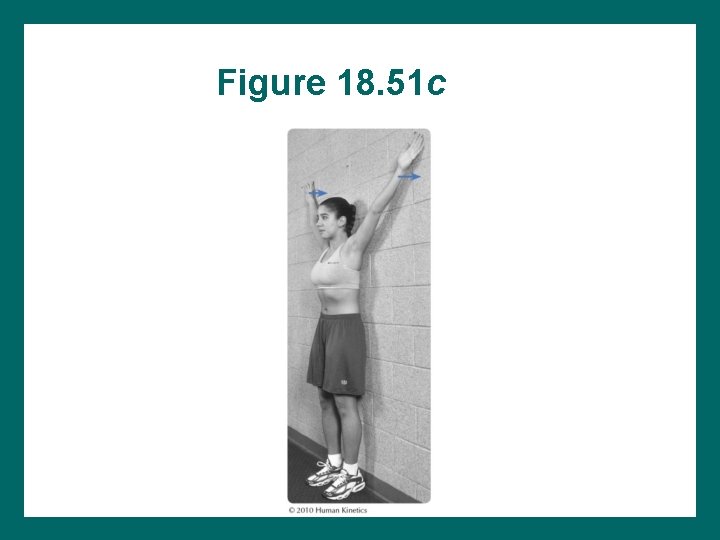
Figure 18. 51 c

Figure 18. 51 d
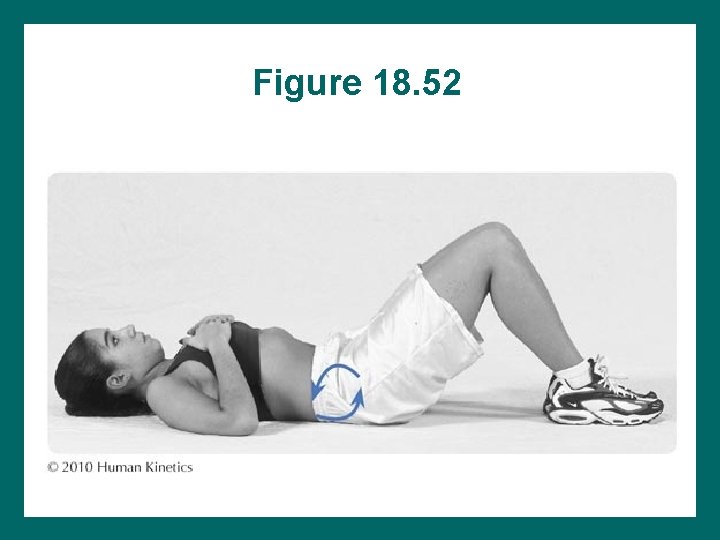
Figure 18. 52
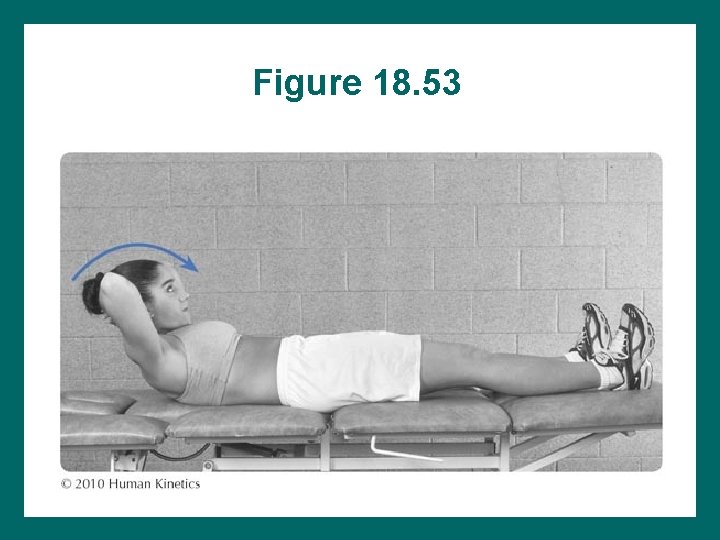
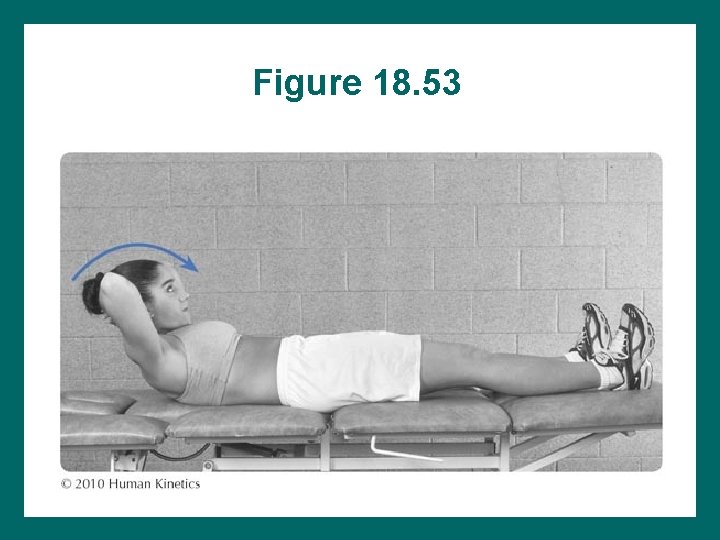
Figure 18. 53
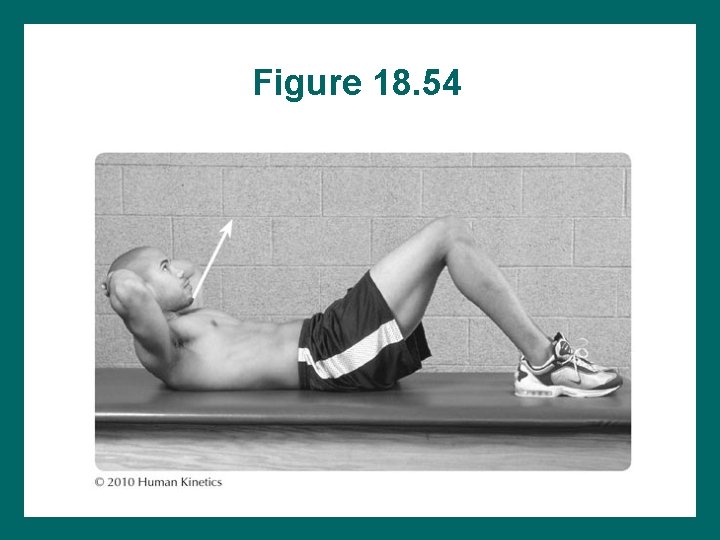
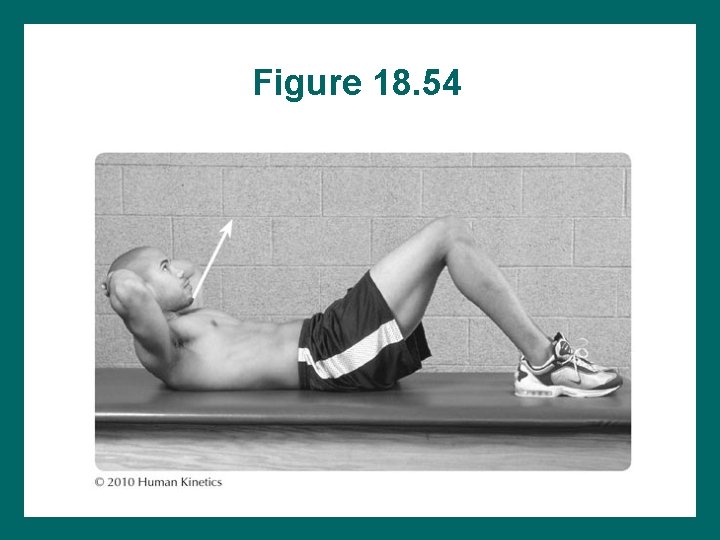
Figure 18. 54
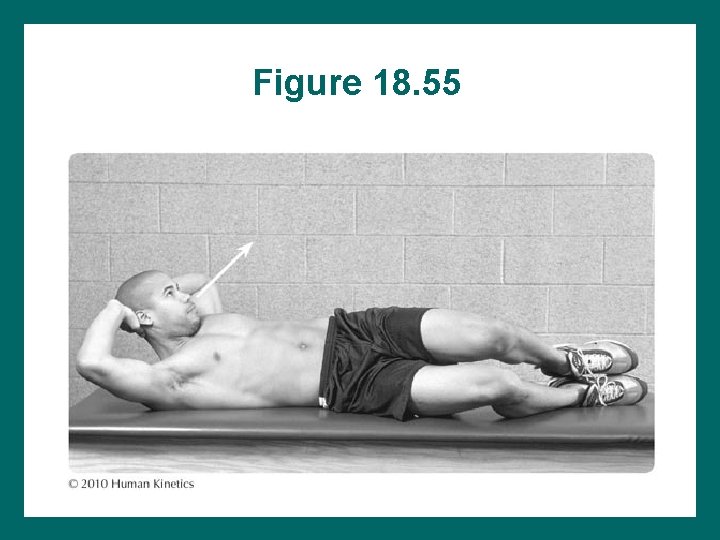
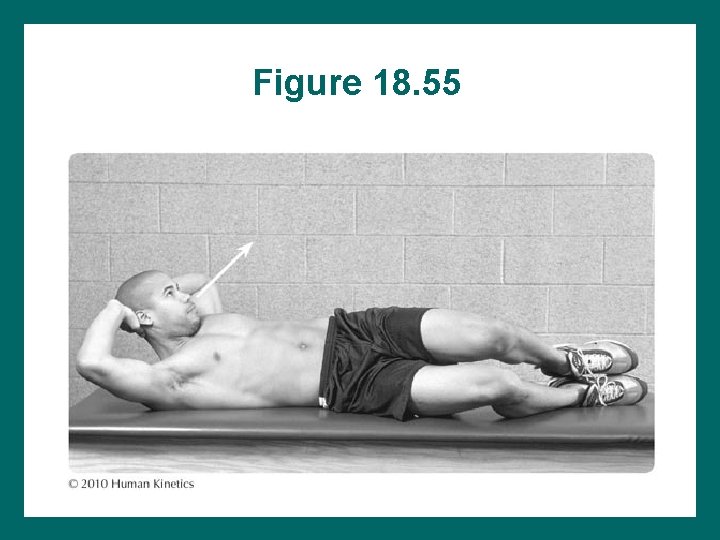
Figure 18. 55
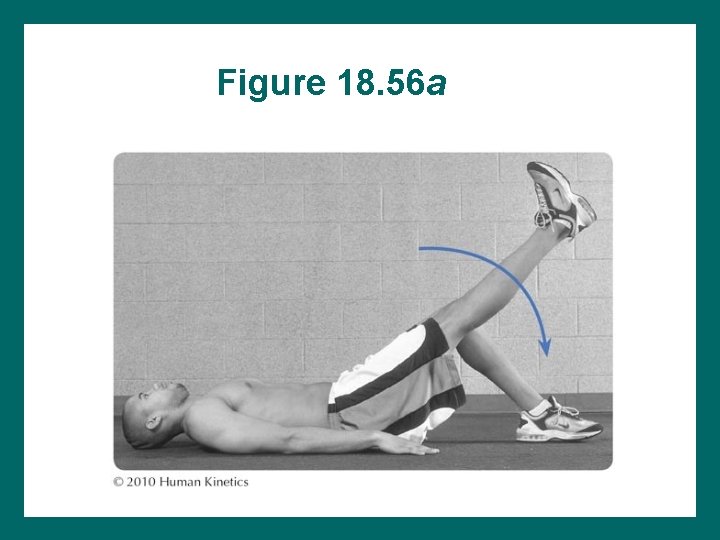
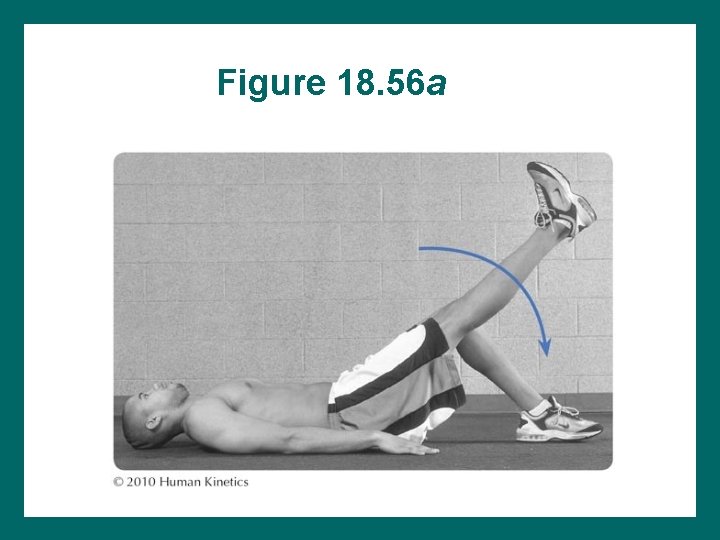
Figure 18. 56 a
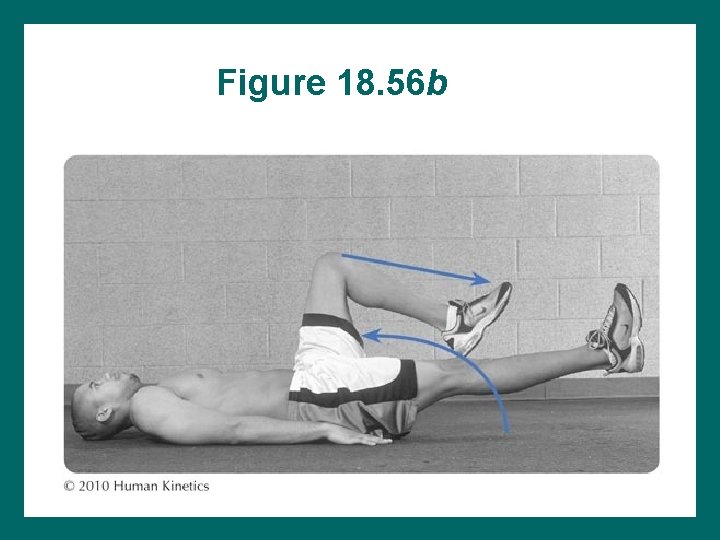
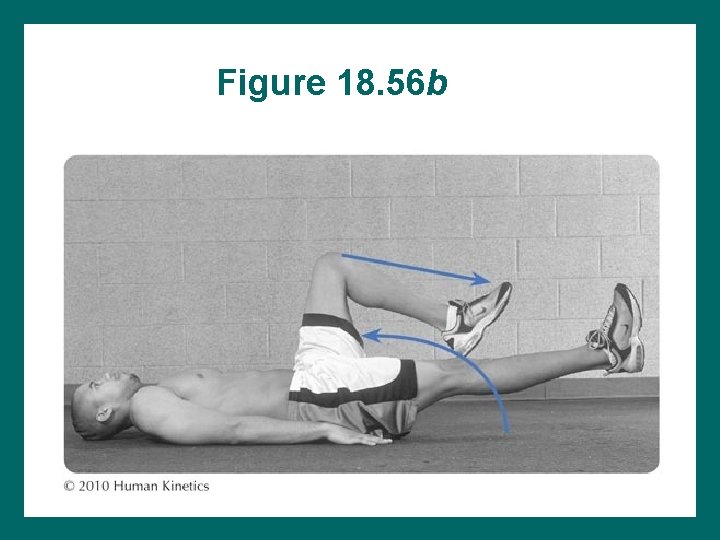
Figure 18. 56 b
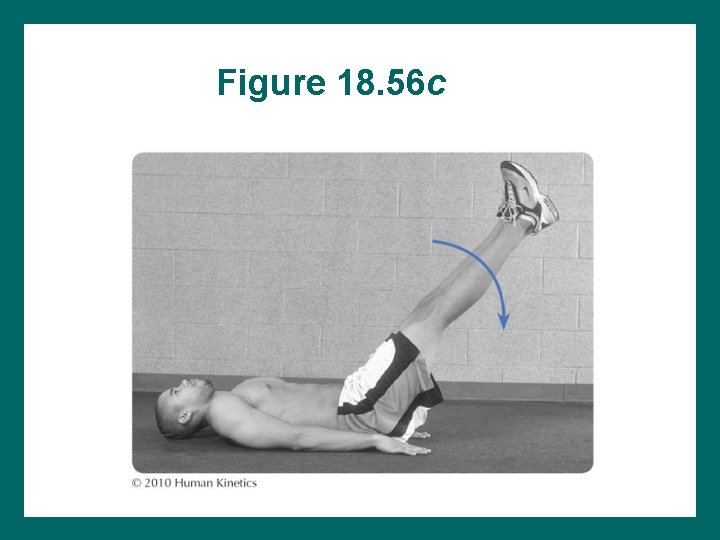
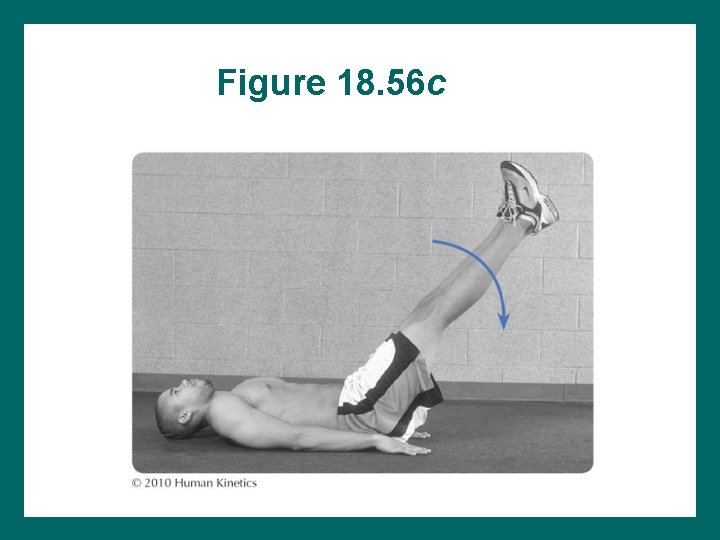
Figure 18. 56 c

Figure 18. 56 d
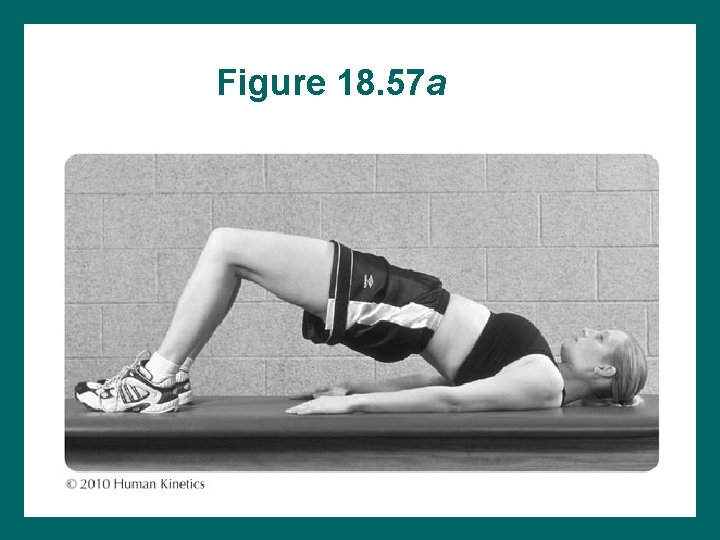
Figure 18. 57 a
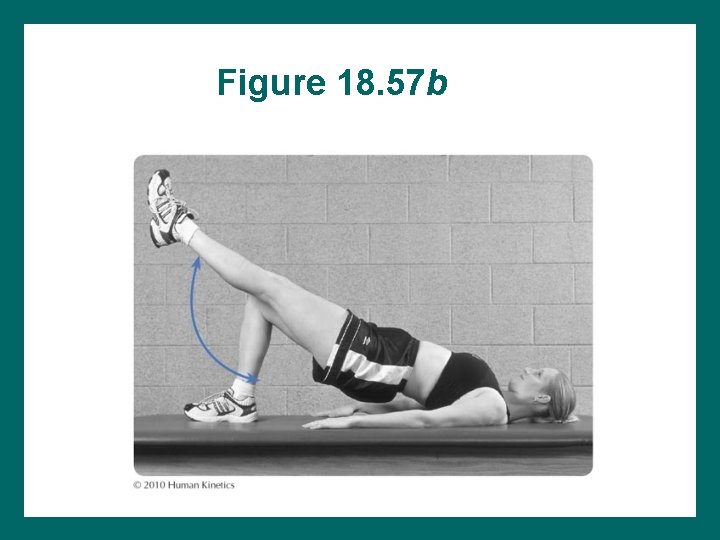
Figure 18. 57 b
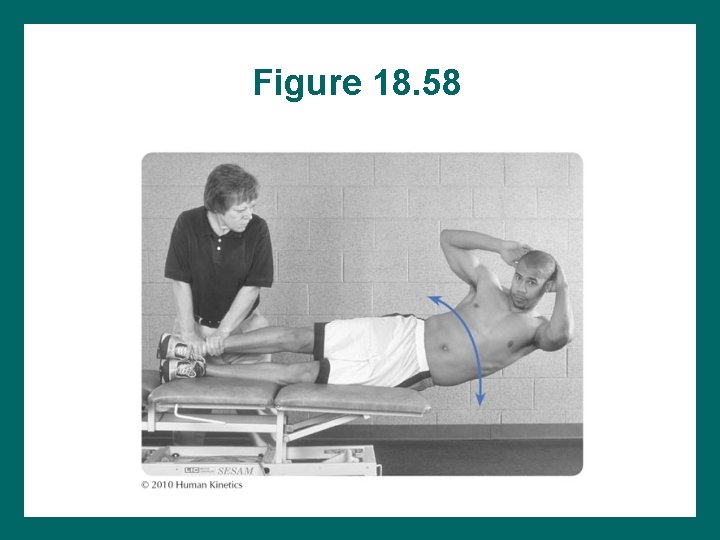
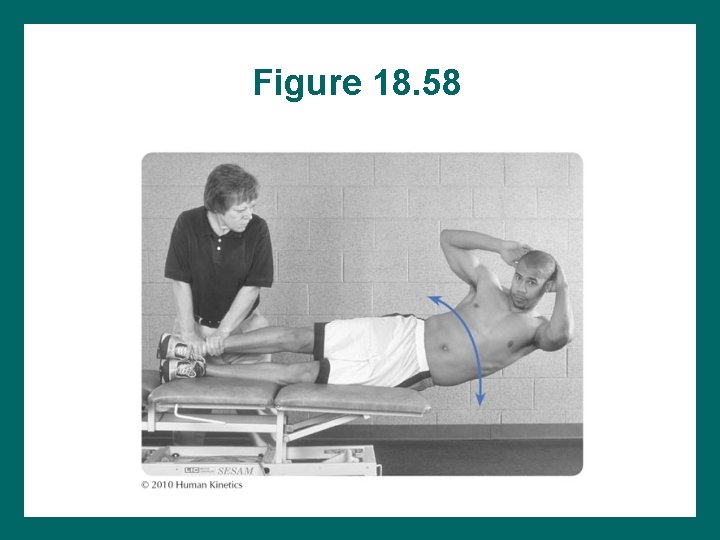
Figure 18. 58
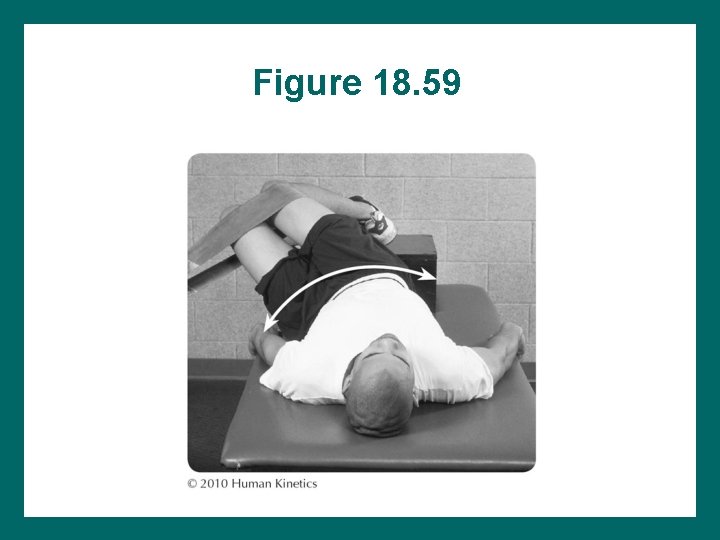
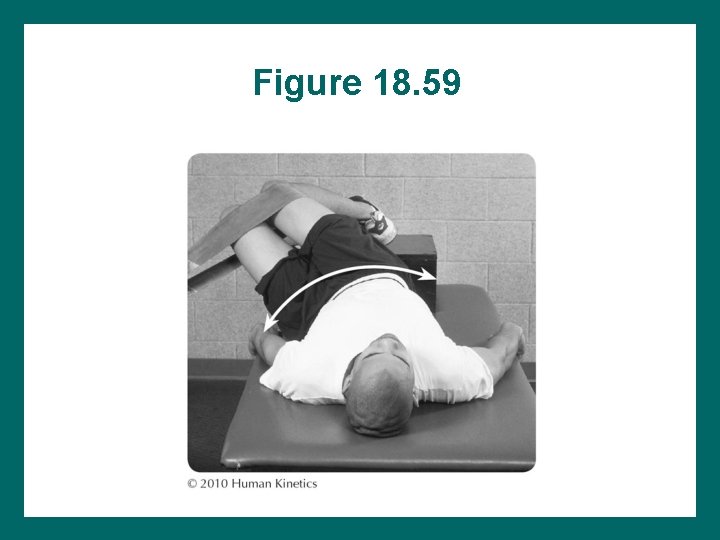
Figure 18. 59
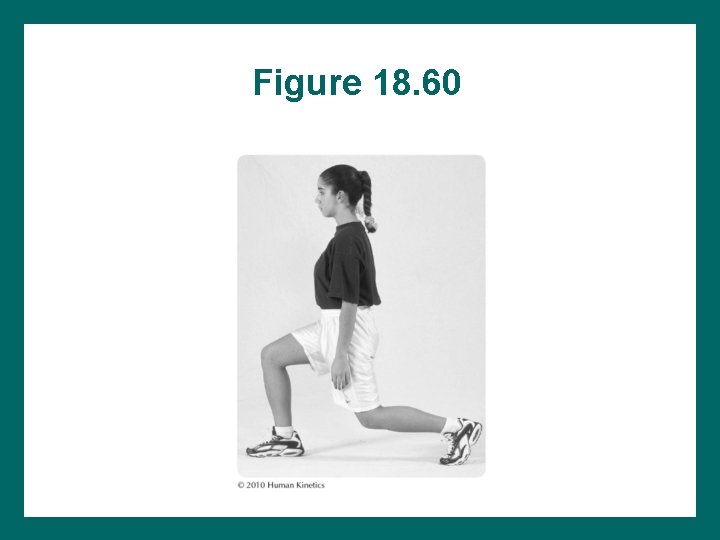
Figure 18. 60
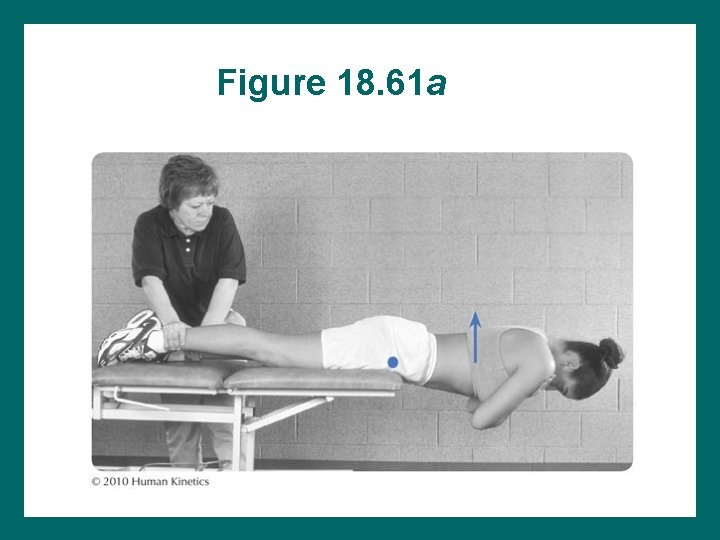
Figure 18. 61 a
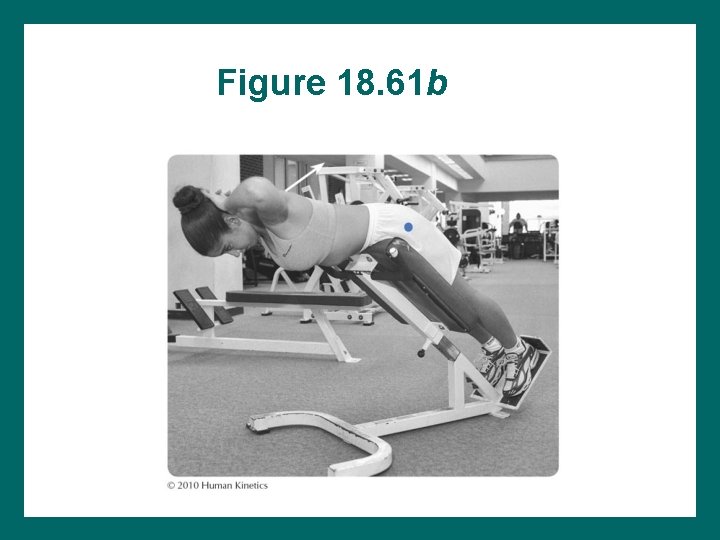
Figure 18. 61 b
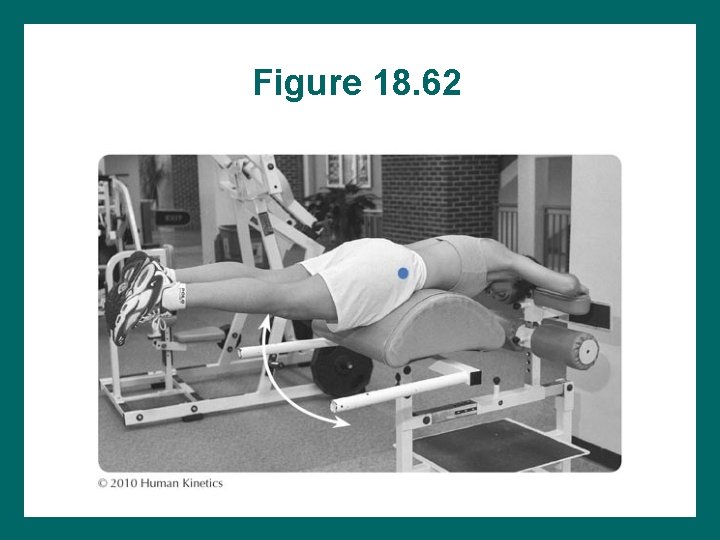
Figure 18. 62
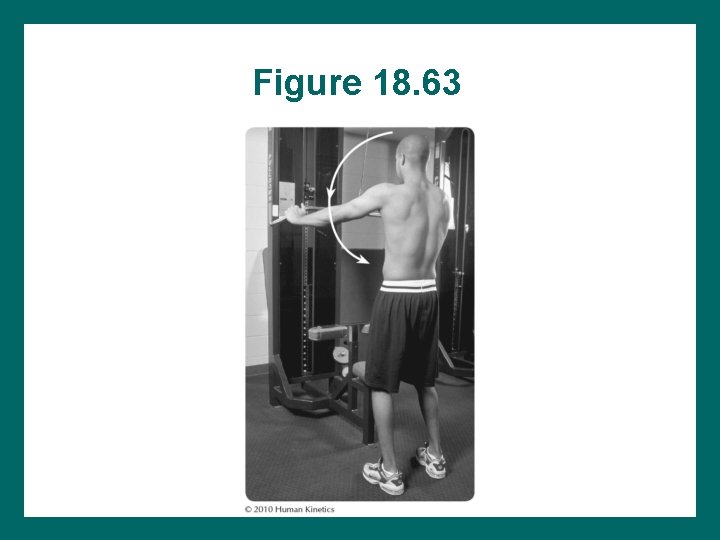
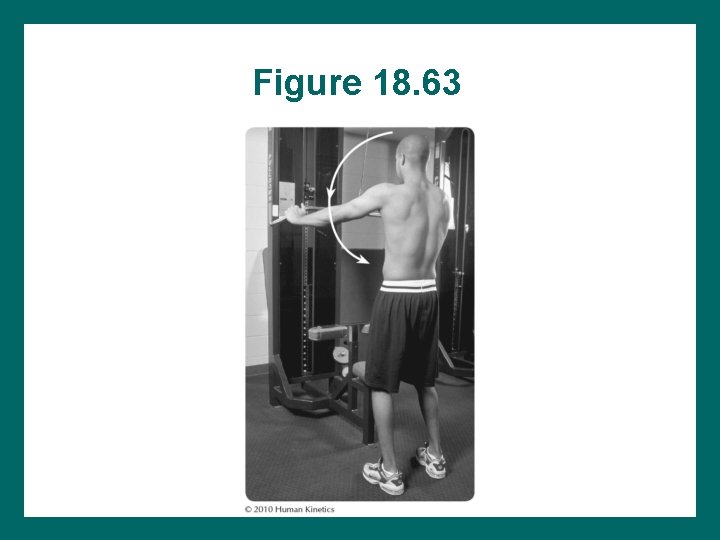
Figure 18. 63
Coordination Agility Functional Activities • Coordination work is started once strength gains are made. • Trunk rotation, plyometrics, and multiplane movements are included. • Pelvic stability must be maintained throughout activity.
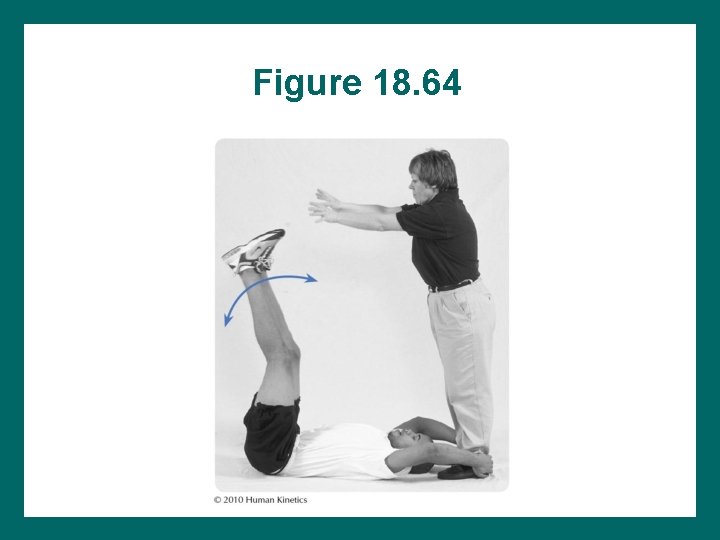
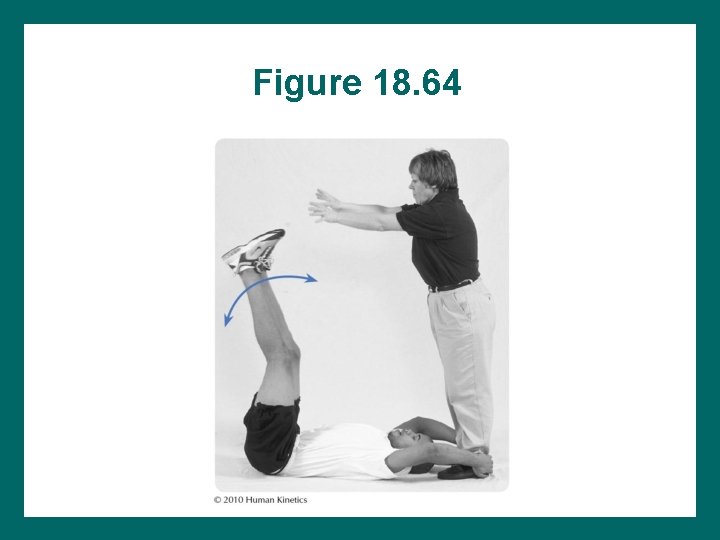
Figure 18. 64
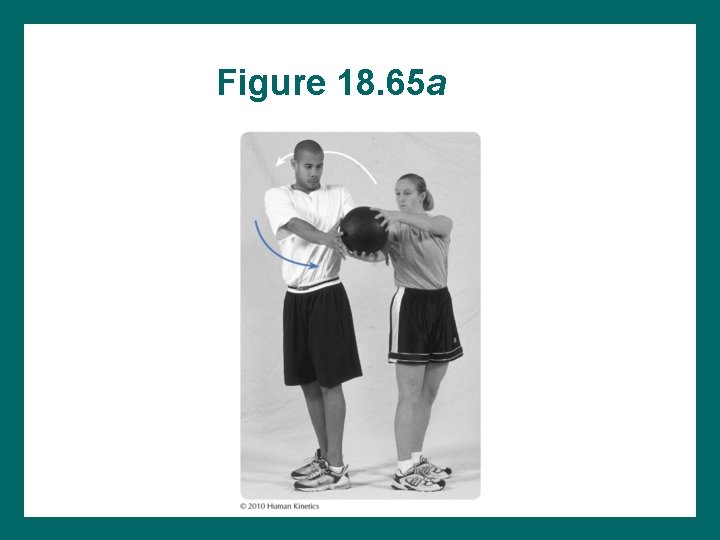
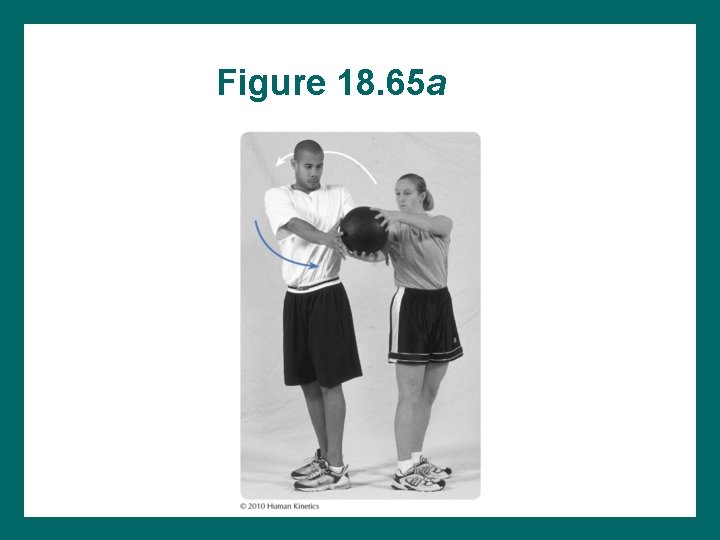
Figure 18. 65 a
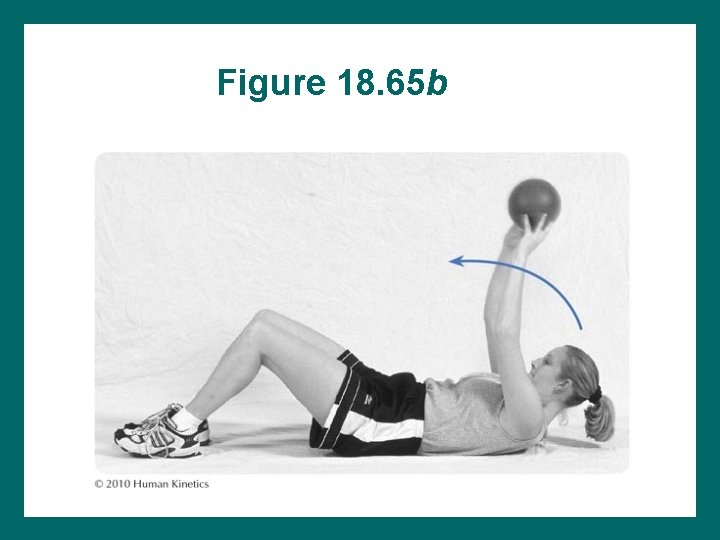
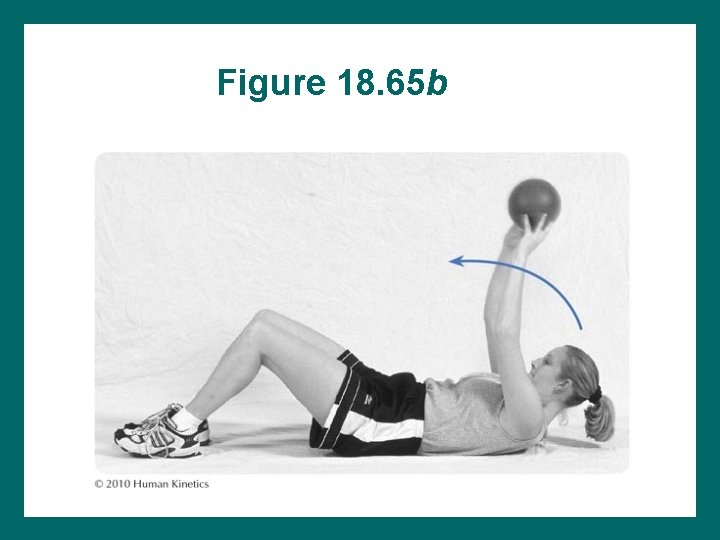
Figure 18. 65 b
Specific Treatment Application Guidelines for Spinal Injuries • Modalities • Early: – – Pelvic neutral, stabilization, and body mechanics Dead bug exercises Pool exercises Trunk flexibility and strengthening • Later: – What do you think some possible guidelines are? Why?
Sprains and Strains • • Cause: ? (Identify possibilities) Signs and symptoms (S/S): (Identify these) Treat pain and spasm first. Use soft-tissue and joint mobilizations. Correct posture and body mechanics. Begin strengthening after spasm is relieved. Emphasize trunk stabilizers and gluteals.
Spondylosis • Degeneration of the disc spaces between the vertebrae • Commonly associated with osteoarthritis
Spondylolysis Stress fracture to the pars interarticularis – Common in football players, weightlifters, and divers – Also referred to as “scottie dog fracture”
Spondylolisthesis Forward slippage of one vertebra in relation to another
Spondylosis, Spondylolysis, Spondylolisthesis • Cause: ? (identify these) • S/S: ? (identify these, based on your knowledge) • Involve lower lumbar spine • Are irritated with extension • Patient should avoid hyperextension motions. • Patient must be taught to maintain posterior pelvic tilt. • Patient must maintain posterior pelvic stability and strengthen abdominal muscles.

Referred Lower-Extremity Pain • Symptoms down the leg do not necessarily mean a disc problem, but this is a possibility • Facet injuries, muscle spasm, and active trigger points • Differential diagnosis before treatment is performed
Disc Lesions • Cause: ? (Identify these) • S/S: ? (Identify these) • Avoid forward bending, side-bending, and twisting. • Maintain pelvic neutral. • If sciatic pain worsens, reevaluate treatment.
Disc Lesions and Sciatica Program considerations: • Centralization of pain • If sciatic pain worsens, must reevaluate the most recently performed exercises for possible incorrect execution and for appropriateness • Patients who have undergone microdiscectomies start treatment about 1 week postoperatively and follow a course of treatment similar to that for patients who have not had surgical correction.

Pathology: Facet Injury Locked facet – Open – Closed
Facet: Positional Dysfunction • • • = Position the facet is held in following trauma. Motion restriction: What the facet can’t do. Is always contralateral to a motion restriction. Restriction can occur in flexion or extension. Facet in flexion = open (facet surfaces are apart). Facet in extension = closed (facet surfaces are together).
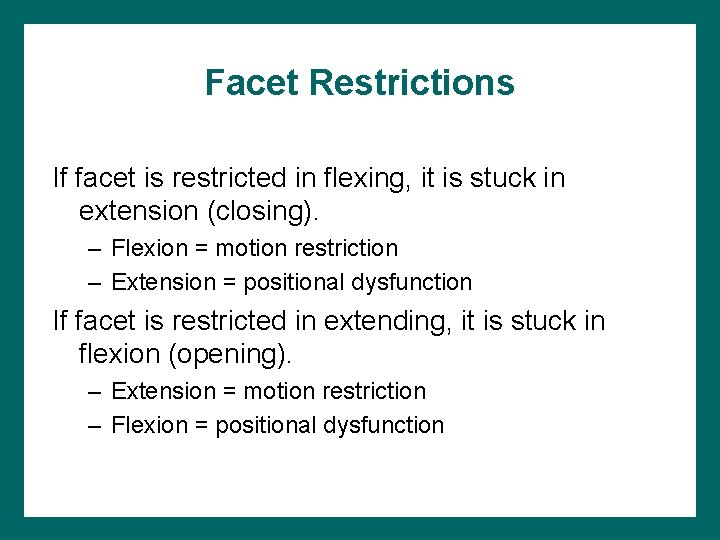
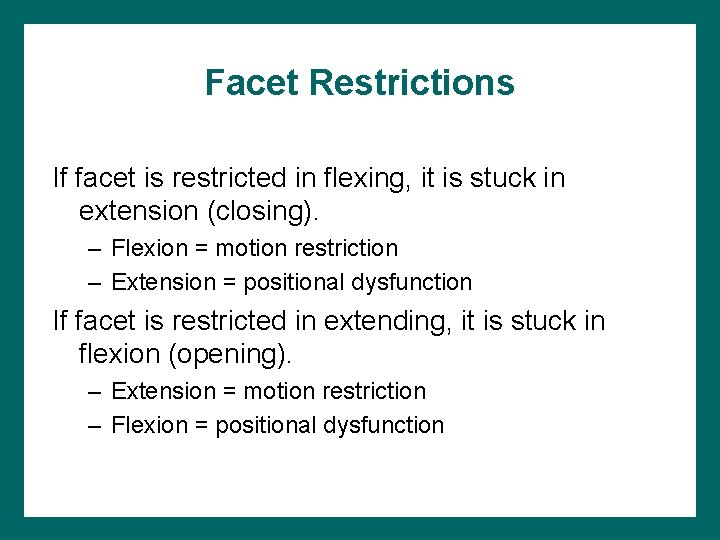
Facet Restrictions If facet is restricted in flexing, it is stuck in extension (closing). – Flexion = motion restriction – Extension = positional dysfunction If facet is restricted in extending, it is stuck in flexion (opening). – Extension = motion restriction – Flexion = positional dysfunction
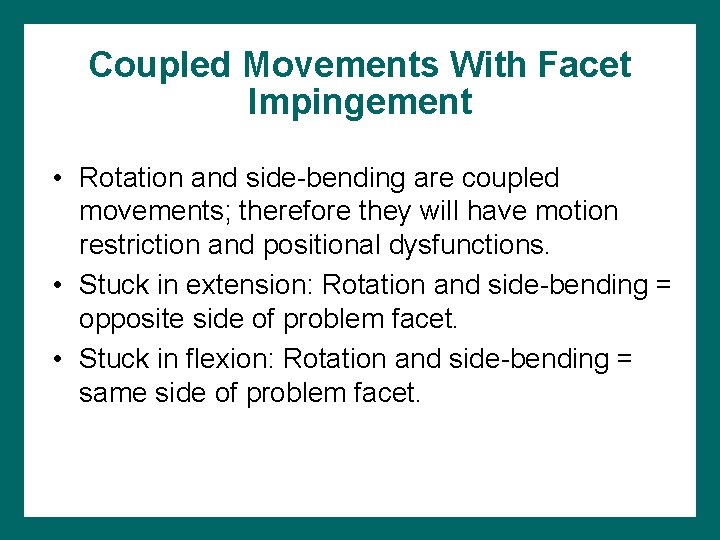
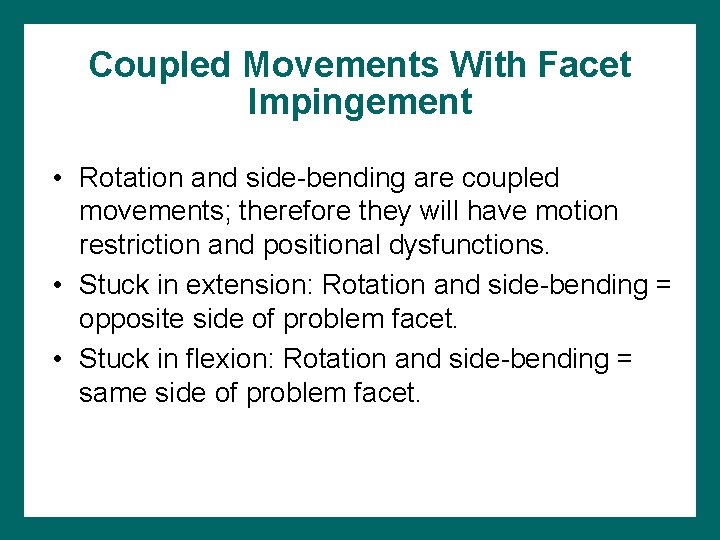
Coupled Movements With Facet Impingement • Rotation and side-bending are coupled movements; therefore they will have motion restriction and positional dysfunctions. • Stuck in extension: Rotation and side-bending = opposite side of problem facet. • Stuck in flexion: Rotation and side-bending = same side of problem facet.
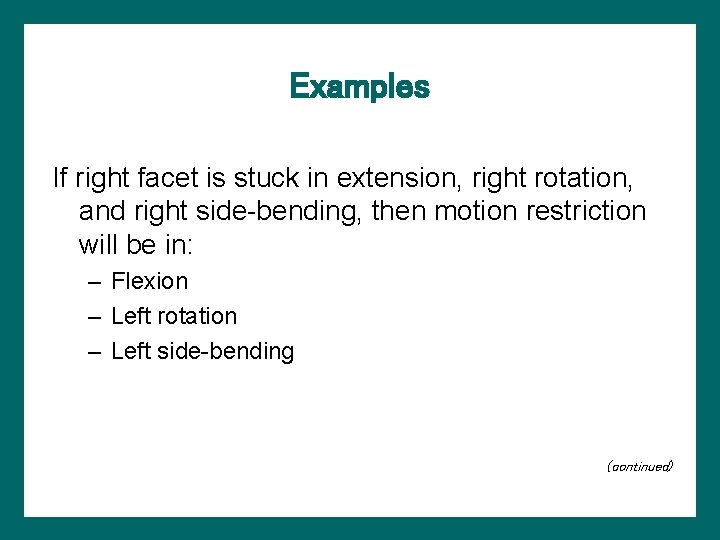
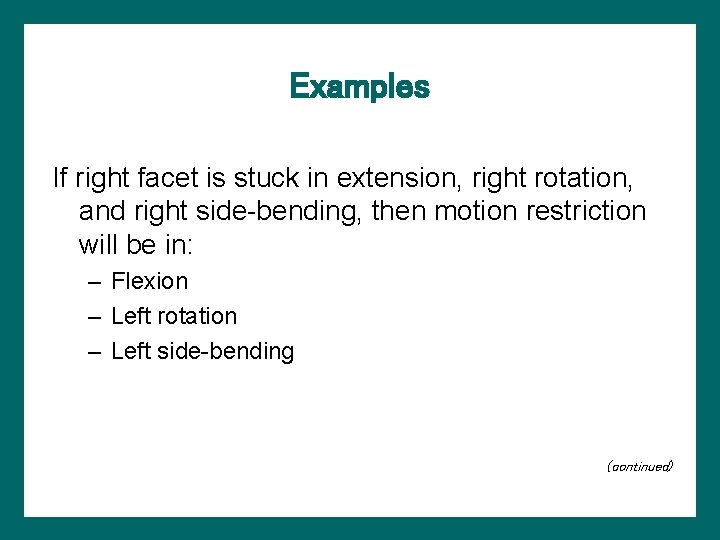
Examples If right facet is stuck in extension, right rotation, and right side-bending, then motion restriction will be in: – Flexion – Left rotation – Left side-bending (continued)
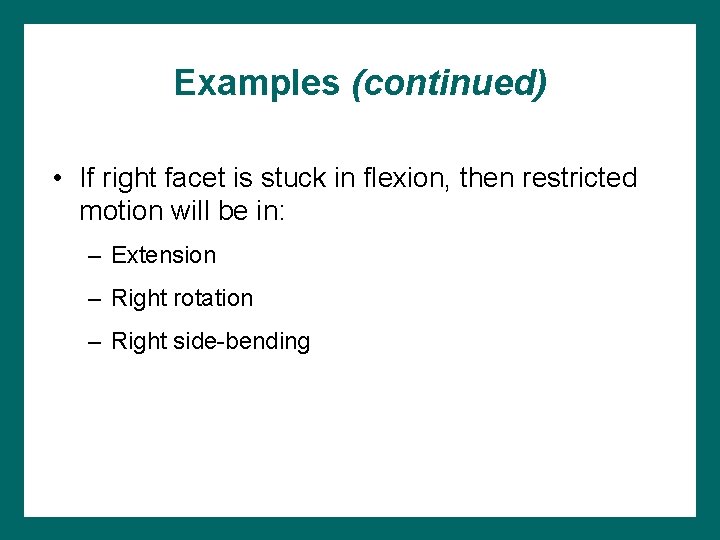
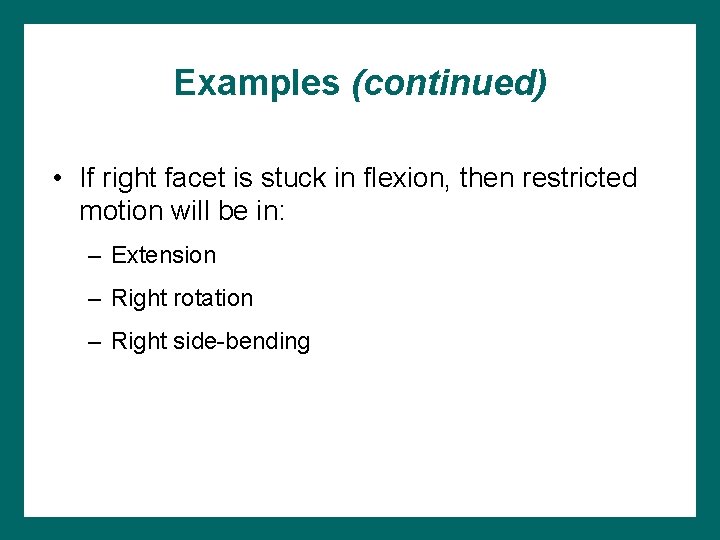
Examples (continued) • If right facet is stuck in flexion, then restricted motion will be in: – Extension – Right rotation – Right side-bending
Facet Injury: S/S • Radiating facet pain can mimic dermatomal distribution into the lower extremity. • Palpation of the specific spinous process causes tenderness.
Facet Injury: Causes • Impingement – Facet joint capsule and synovium impinged between joint surfaces – From sudden extension, side-bending, or rotation that may seem minor • Sprain – Trauma more profound – Tissue injury greater
Facet Impingement: Rx • Gentle ROM in pain-free range with gradual progression into painful ranges with traction • Avoid painful motions initially • Posteroanterior mobilizations on painful side
Facet Sprain: Rx • More conservative approach • Modalities; cervical collar • Gentle range of motion in pain-free range and joint mobilization following modalities to relieve muscle spasm, pain, edema
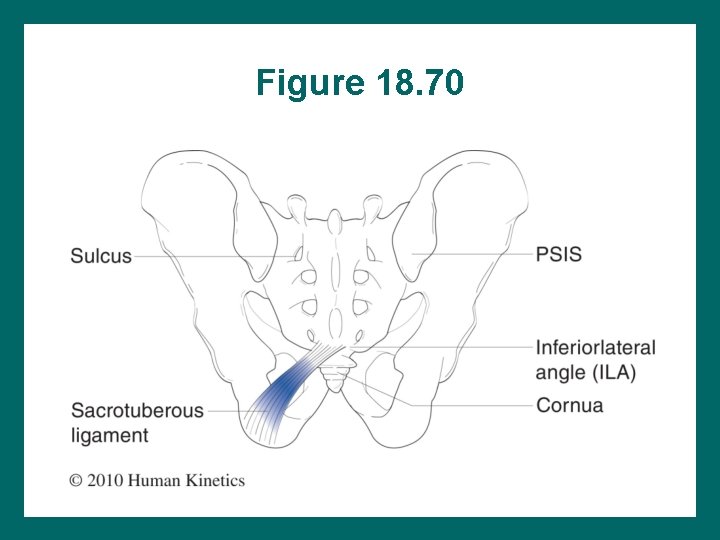
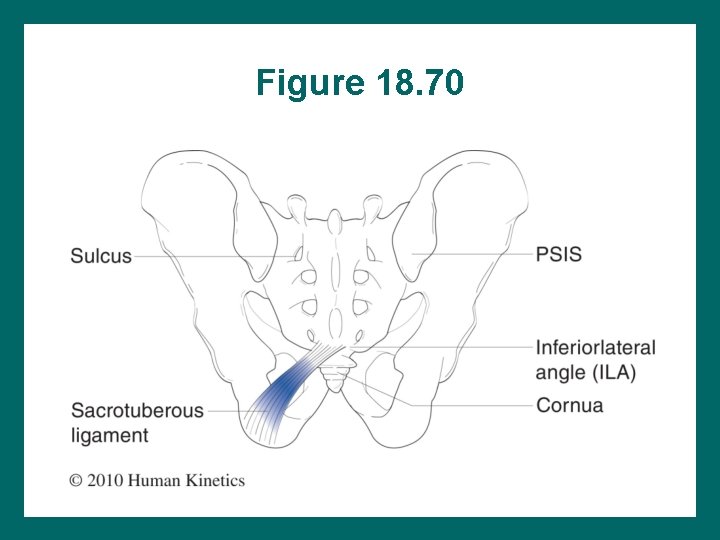
Figure 18. 70
Sacroilium Sacroiliac ring: – Sacrum – Two SI joints – Two hemipelvises • Ilium • Pubis • Ischium – Pubic symphysis joint (continued)
Sacroilium (continued) • Pelvic ring transfers weight bidirectionally. • Pelvic ring strength is directly related to fit and stability of sacrum. • Sacrum (anchored by sacroiliac joints) = keystone of pelvic ring.
Sacrum • Auricular surface • Thicker cartilage on sacrum • Transitions from puberty to adulthood: – Smooth to rough surface – Synovial to modified amphiarthroidal joint – Degenerates with age