Failure to Thrive Premi Suresh MD FAAP Learning





















- Slides: 57
Failure to Thrive Premi Suresh, MD, FAAP
Learning Objectives The participant will be able to… • Review use of growth charts. • Know how failure to thrive is identified. • Be familiar with the three broad categories of causes of Failure to Thrive (FTT). • List ways in which FTT could result from abuse and neglect. • Learn strategies for management of children with FTT.
Background • Failure to Thrive (FTT) is a common problem in pediatric populations • Accounts for 1 -5% of referrals to children’s hospitals/tertiary care centers • May be under diagnosed • 20 -50% may not be picked up by physician
Background • In low-income countries, poverty is the most common cause of Failure to Thrive; however, medical providers, social services and law enforcement must learn about the entire family to see if this child – for any reason – was not given food that was given to others in the family.

GROWTH CHARTS

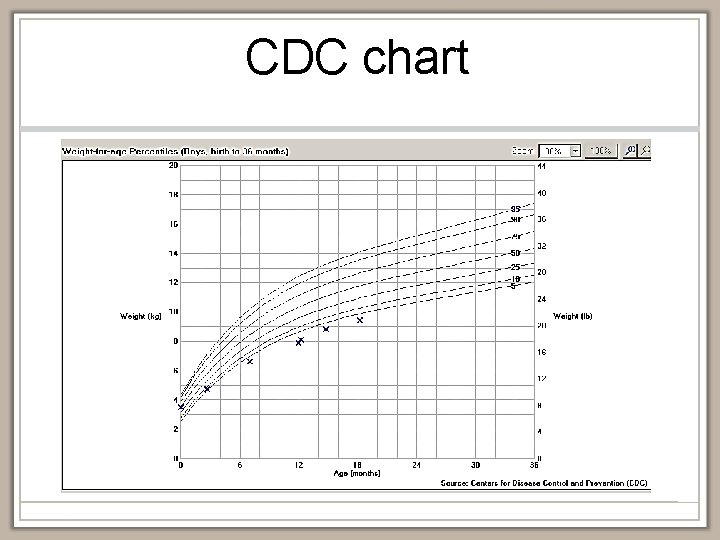
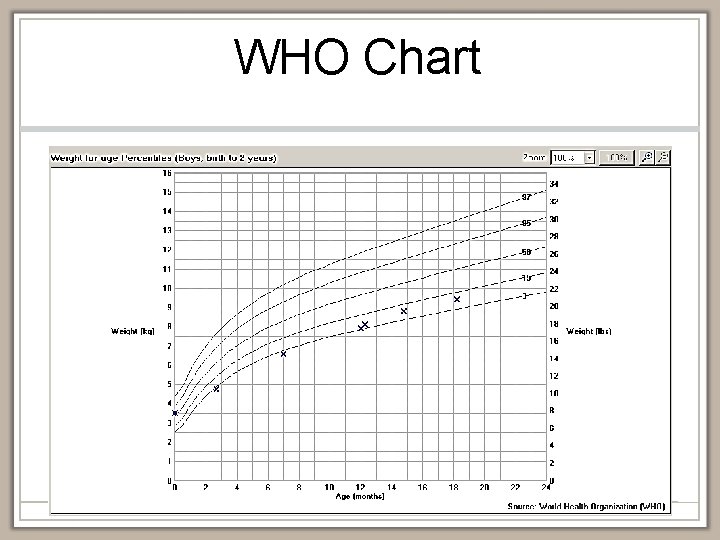
Growth Charts • U. S. Centers for Disease Control (CDC) • Growth reference • How children grow in the U. S. • World Health Organization (WHO) • Growth standard • How children should grow in ideal conditions • Recommended for use in children under 2
CDC or WHO? • WHO growth chart may be better for children under 2 years old • WHO more appropriate for exclusively breastfed infant • WHO may take into account cultural differences • Still no consensus among providers
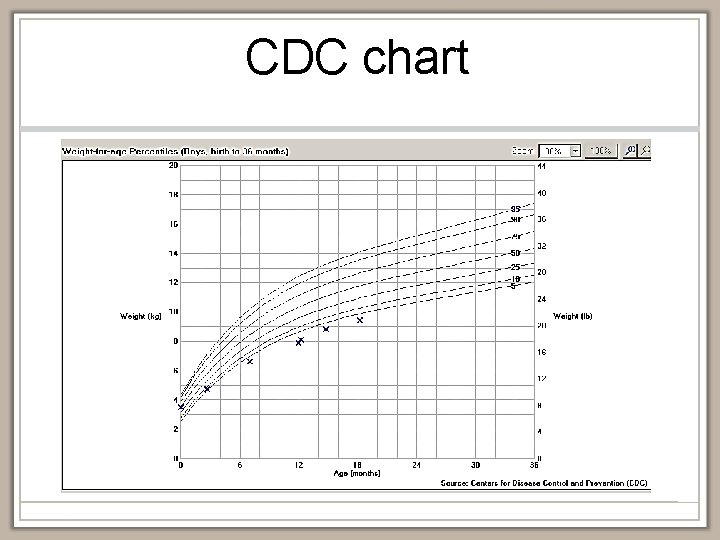
CDC chart
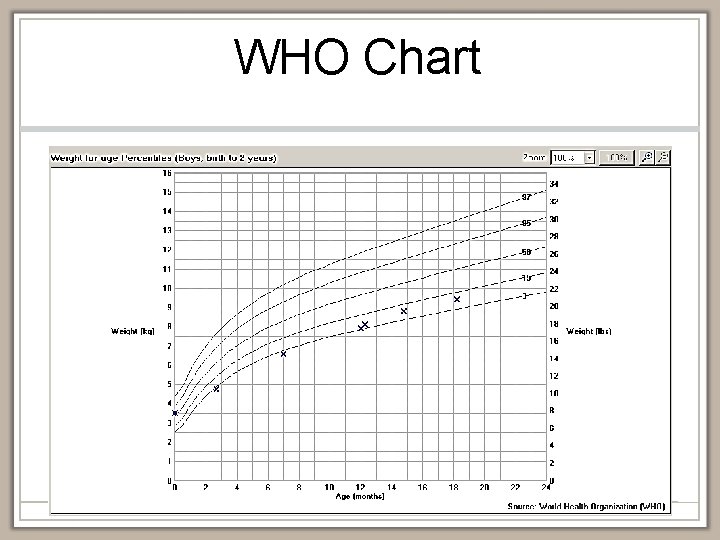
WHO Chart
FAILURE TO THRIVE
Failure to Thrive • Not a diagnosis - a description • Inadequate nutrition to sustain normal growth and development • Significantly prolonged cessation of appropriate weight gain compared with recognized norms for age/gender after having achieved stable pattern
Criteria • Weight curve crossing 2 major percentile lines on growth chart after achieving stable pattern • Weight for age or weight for height more than 2 standard deviations below mean for gender/age


Weight for Height

Thomas
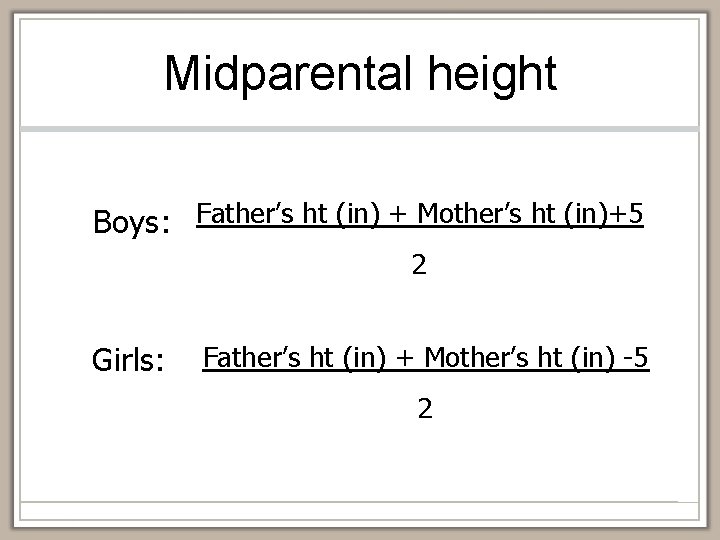
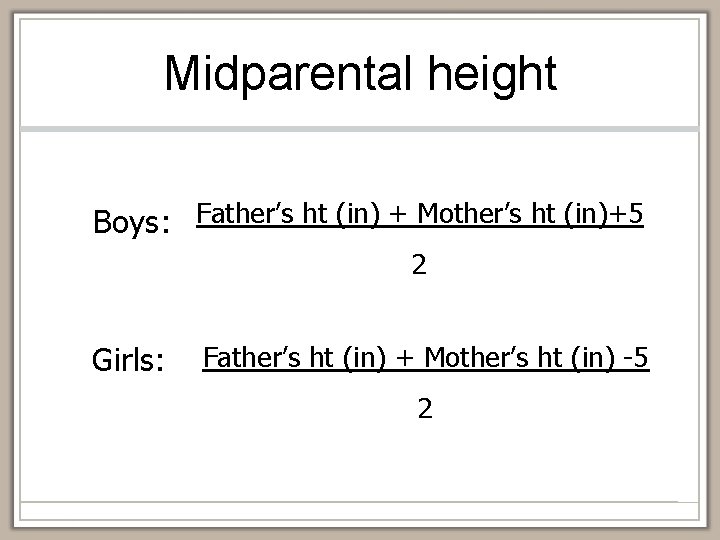
Midparental height Boys: Father’s ht (in) + Mother’s ht (in)+5 2 Girls: Father’s ht (in) + Mother’s ht (in) -5 2


Organic vs. Non-Organic • Not a helpful distinction • Both overlap • Too simplistic • Malnutrition causes growth failure

Causes of FTT • Inadequate calories • Inability to utilize calories • Increased caloric needs More than one of these causes can overlap!!
Normal Growth Food (calories) Waste Metabolism Growth

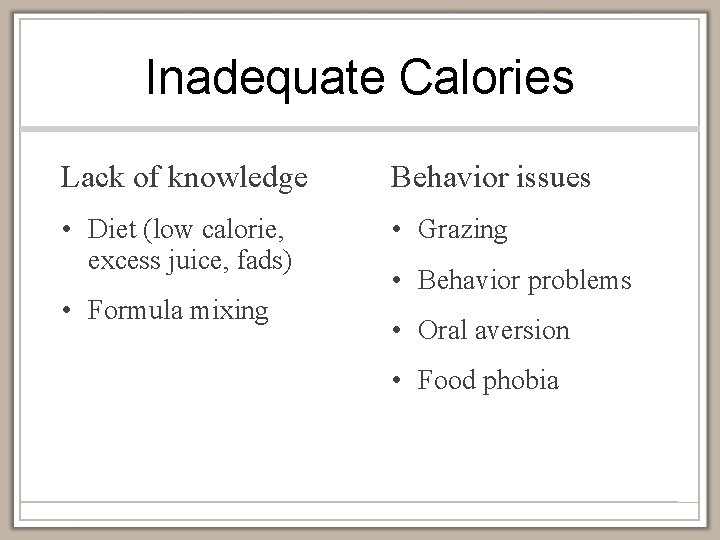
Inadequate Calories • Lack of knowledge • Behavior • Psychosocial • Anatomic
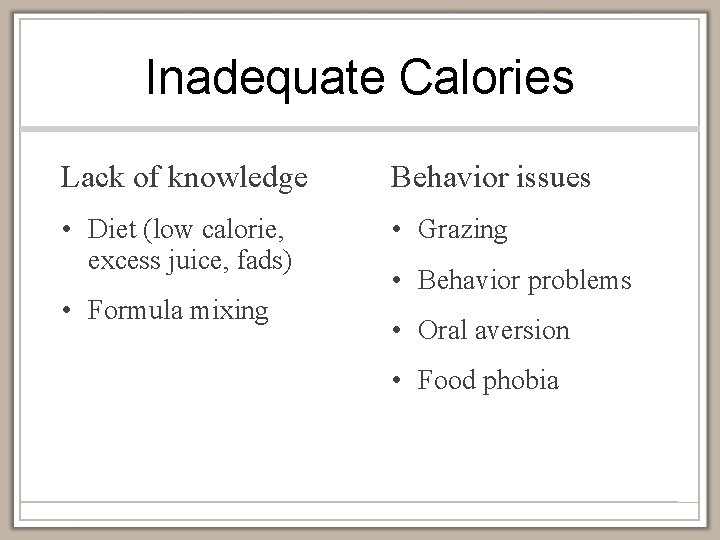
Inadequate Calories Lack of knowledge Behavior issues • Diet (low calorie, excess juice, fads) • Grazing • Formula mixing • Behavior problems • Oral aversion • Food phobia
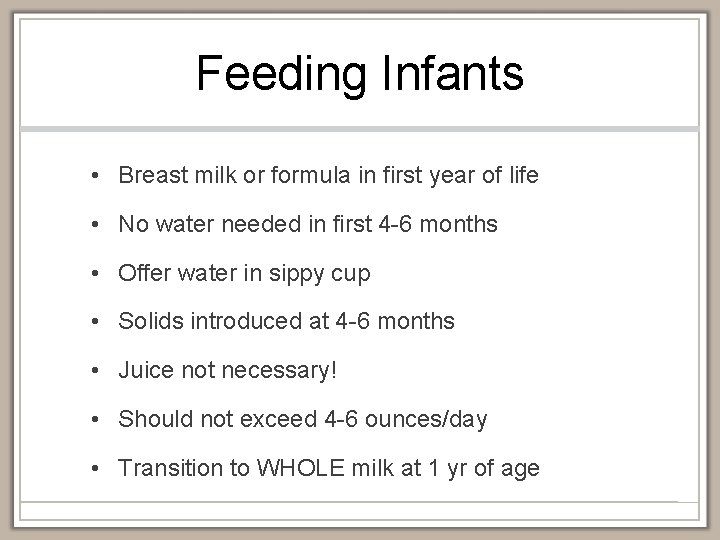
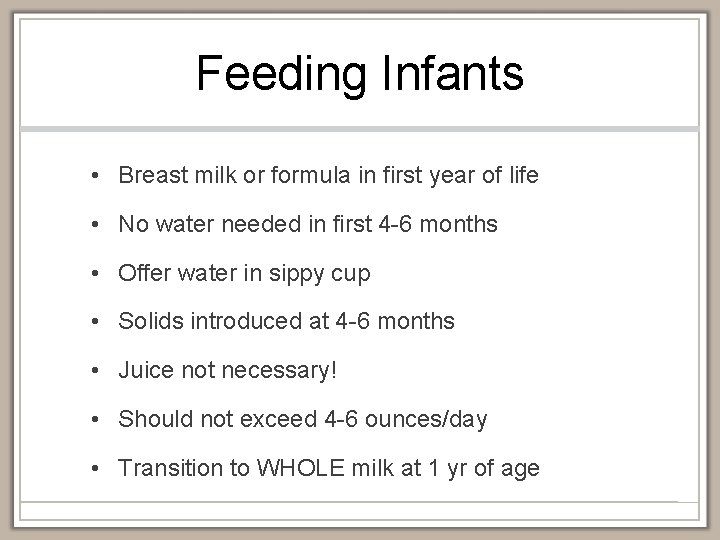
Feeding Infants • Breast milk or formula in first year of life • No water needed in first 4 -6 months • Offer water in sippy cup • Solids introduced at 4 -6 months • Juice not necessary! • Should not exceed 4 -6 ounces/day • Transition to WHOLE milk at 1 yr of age
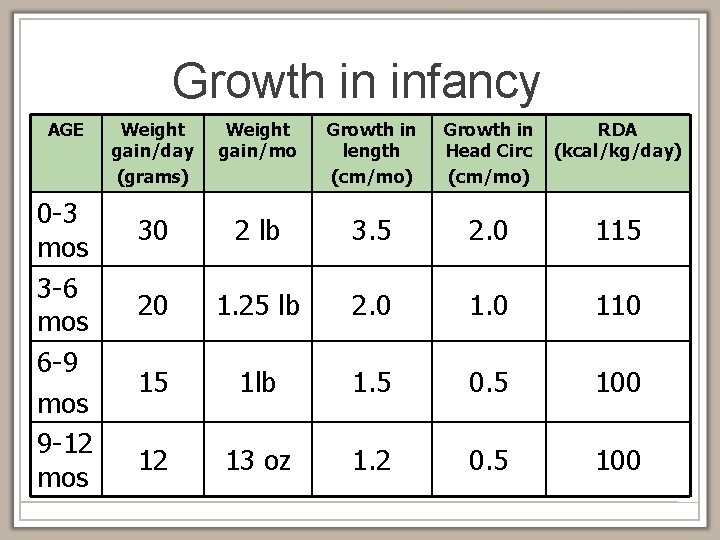
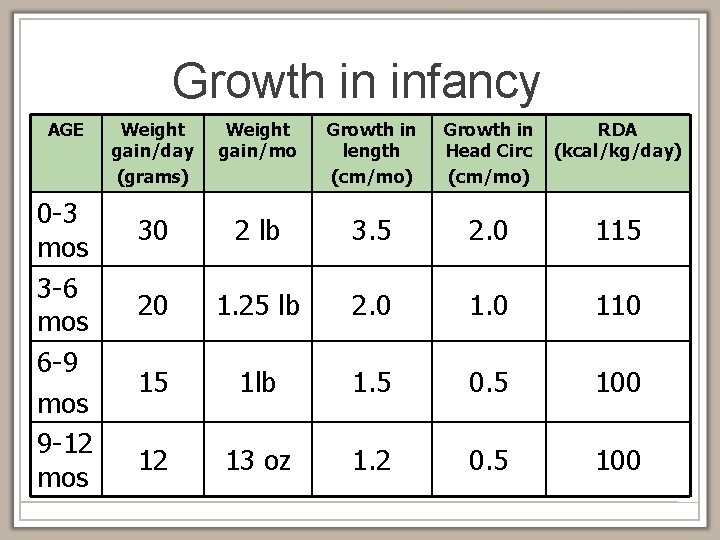
Growth in infancy AGE 0 -3 mos 3 -6 mos 6 -9 mos 9 -12 mos Weight gain/day (grams) Weight gain/mo Growth in length (cm/mo) Growth in Head Circ (cm/mo) RDA (kcal/kg/day) 30 2 lb 3. 5 2. 0 115 20 1. 25 lb 2. 0 110 15 1 lb 1. 5 0. 5 100 12 13 oz 1. 2 0. 5 100
Caloric intake • Breastmilk and Standard Infant formula have 20 calories per oz • Formula should be mixed 1 scoop to 2 oz water • There are special formulas with higher calories per oz
Toddlers • Growth less rapid • Can become picky • Food “jags” • Bottle should be discontinued • Self feeding encouraged • Avoid battles over food
Stop Grazing • Offer 3 meals and 3 snacks per day • Separate meals and snacks by 2 -2. 5 hours • Only water between meals and snacks • Meals and snacks should be offered at a table or highchair and should last 20 -25 minutes • Solid foods should be offered before liquids

Inadequate Calories Psychosocial • Poverty/financial • Formula mixing • Abuse/neglect/IPV • Parental mental health issues • Parental eating disorders

Inadequate Calories Anatomic • Congenital anomalies • Oromotor dysfunction • Dental caries • Gastroesophageal reflux • Obstruction (i. e. pyloric stenosis)
Malabsorption • Milk protein allergy • Cystic fibrosis • Pancreatic insufficiency Inability to Utilize Calories • Biliary atresia • Short gut or necrotizing enterocolitis Improper utilization • Inflammatory bowel disease • Inborn errors of metabolism • Chronic diarrhea • Storage disorders • Disaccharidase deficiency • Growth hormone deficiency

Increased Caloric Needs • Prematurity • Cancer • Recurrent infection • Kidney problems • Renal tubular acidosis, chronic renal failure • Cardiac disorders • Congenital heart disease, heart failure • Pulmonary disorders • Chronic lung disease, poorly controlled asthma • Chronic liver disease • Obstructive sleep apnea • Chronic infection (HIV, Tuberculosis)
Case Scenario • Pt is a 2 yr 5 mo male brought to the Hospital after being found unresponsive at home. Doctors found the patient’s abdomen was abnormally large, his legs were extremely swollen and face and arms appeared malnourished and gaunt. Doctors report that patient has been found to have a large abdominal tumor. Per mother’s report patient has been “unwell” for several months.

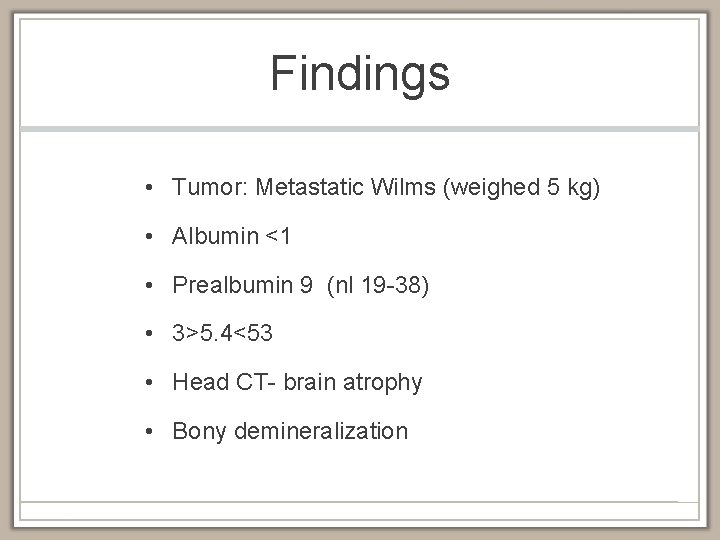
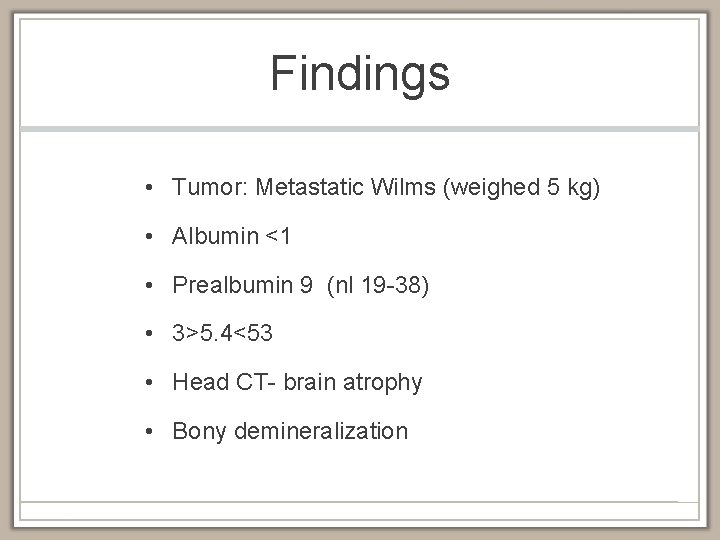
Findings • Tumor: Metastatic Wilms (weighed 5 kg) • Albumin <1 • Prealbumin 9 (nl 19 -38) • 3>5. 4<53 • Head CT- brain atrophy • Bony demineralization


Is this patient failing to thrive?
Causes of FTT • Inadequate calories • Inability to utilize calories • Increased caloric needs More than one of these causes can overlap!!

CHILD ABUSE CAUSES OF FTT
Child abuse causing FTT • Neglect • Pediatric Condition Falsification • Other- effects of physical abuse, sexual abuse
Case Scenario Patient is a 2 month old male. Mother took him to the primary doctor for immunizations. Doctor became concerned because the baby was very small and considered to be failure to thrive. Baby’s birth weight was 6 lbs, 6 oz ( 3. 3 Kg). At 1 month of age baby weighed 7 lbs, 6 oz. At today’s 2 month visit, baby weighed 7 lbs 5 oz. Mother told doctors that she gives the baby 32 oz of formula per day which the doctors said was an appropriate amount. Nurses report that mother is not engaged in the child’s care and sleeps most of the time. Nursing staff had to wake mother to participate in diaper changes and feedings.
Child Abuse Causing FTT • Neglect • • • Food withholding Caregiver mental health issues Caregiver substance abuse Poor attachment Domestic violence Lack of follow through/medical neglect

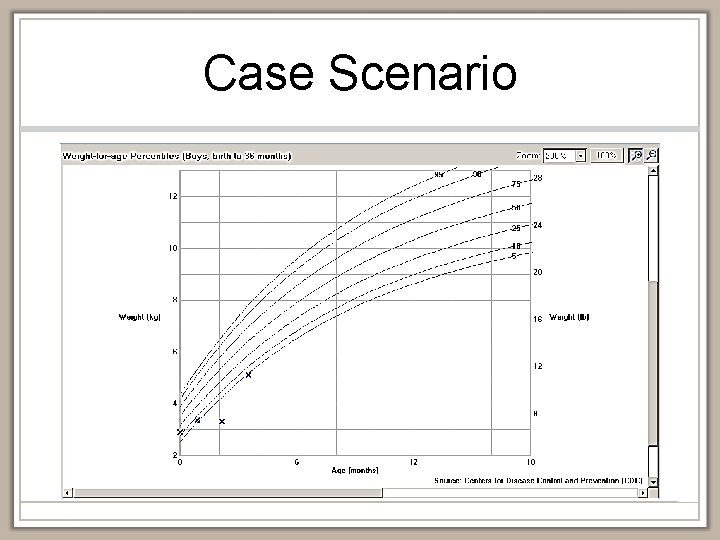
Case Scenario

Case Scenario
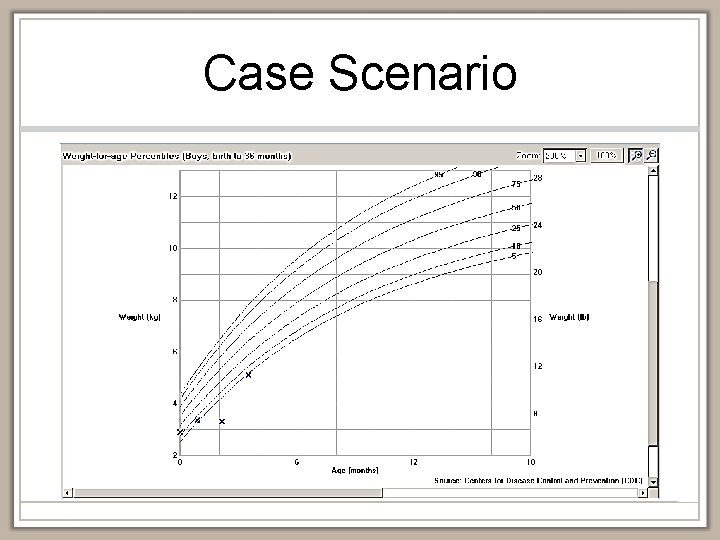
Case Scenario
Case Scenario Patient is a 12 month old female with failure to thrive. Hospital physicians are concerned because child appears to be normal, eat well and gain weight while in the hospital. However, child’s primary physician is worried that the child has an underlying medical condition. She frequently has diarrhea and has days where she vomits with every meal. The child has had numerous medical lab tests and imaging studies that have not determined what is causing her vomiting and diarrhea. Mother brings the child to all appointments and seems very appropriate and engaged in child’s care.

Child Abuse Causing FTT • Fabricated or Induced Illness (Medical Child Abuse or Pediatric Condition Falsification • Induced FTT • Giving the child laxatives, ipecac, etc • Fabricated symptoms • Reporting symptoms that child not experiencing • Leads to further workup, tests
Child Abuse Causing FTT Pediatric condition falsification (PCF) • Caregivers typically present well • May be extremely attentive • “Model” caregivers • Will be opposite of caregivers who are neglecting the child
Child Abuse Causing FTT • Physical/Sexual abuse • Could cause behavioral symptoms that lead to failure to thrive • Food refusal • Vomiting • Can co-exist with neglect
Evaluation & Management • History • Physical exam • Laboratory testing • Treatment

History • Prenatal/Birth • Development • Medical history • Family history • Surgical history • Social history • Medications • Diet history • Allergies • Three day food diary • Symptoms
Physical Exam • Weight, head circumference • Same scale best • Standing height after 2 years of age • Complete physical exam • Observe parent-child interaction • Observe feeding • Signs of neglect • Hygiene, teeth, diaper area
Laboratory Studies • Focused lab evaluation • Common labs include: • • • Complete blood count Electrolytes Urinalysis Thyroid studies Sweat test (cystic fibrosis) • Majority of time, labs unhelpful
Treatment: Aimed at Cause of FTT • Dietary changes • Increase calories • Behavioral changes • Scheduled, structured mealtimes • Home visitation • Document weight, check in with family, observe home dynamics • Hospitalization • Severe cases, suspected abuse, failure of outpatient treatment

Multidisciplinary Teams • Best way to address FTT • Medical Provider • Dietician • Social Worker • Visiting nurse • Occupational therapy • Developmental specialist
Outcomes • Depends on case • Prognosis on growth typically good; however 2560% may remain small • Cognitive deficits, learning disability, behavioral problems seen in follow up • Hard to tease out affects of FTT because of comorbidities
References • Kleinman R, Pediatric Nutrition Handbook 6 th edition. American Academy of Pediatrics; 2009. • Reece R, Christian C, eds. Child Abuse, Medical Diagnosis and Management. 3 rd edition. American Academy of Pediatrics; 2009. • Block, BW, Krebs, NF, et al. Failure to Thrive as a Manifestation of Child Neglect. Pediatrics 2005; 116: 1234 -1237. • Krugman, SD, Dubowitz, H. Failure to Thrive. Amer Fam Phys 2003; 68(5): 879 -884 • Bools, C. Fabricated or Induced Illness in a Child by a Carer: A Reader. Radcliffe Publishing, Oxford 2007