Doc it was a nightmare CCM Interhospital Grand


- Slides: 53
"Doc, it was a nightmare!" CCM Inter-hospital Grand Round 15 th March, 2011 Ruttonjee Hospital Raymond Tso
Mr. L � 58 year old waiter with good past health �Presented to AED at 2: 48 am with some palpitation starting 3 hours ago �Palpitation was associated with sweating and dull backache �Denies any dyspnea or chest pain �Active smoker with 60 pack year, social drinker, denies IV drug use �No family history of CAD �Allergic to penicillin
General Exam • Vitals: � Afebrile; BP 97/67 mm. Hg; Pulse 107/min; Sa. O 2 94 % on 2 L O 2 via NC • PE: � Gen: pale looking, lying in bed appear anxious; no JVD � Chest: mild rales at base bilaterally � CVS: Tachycardiac, normal S 1 &2, no murmur appreciated � Abd: soft, non-tender, non-distended � Ext: no peripheral edema, no pulse delay, no needle marking at arms or groins
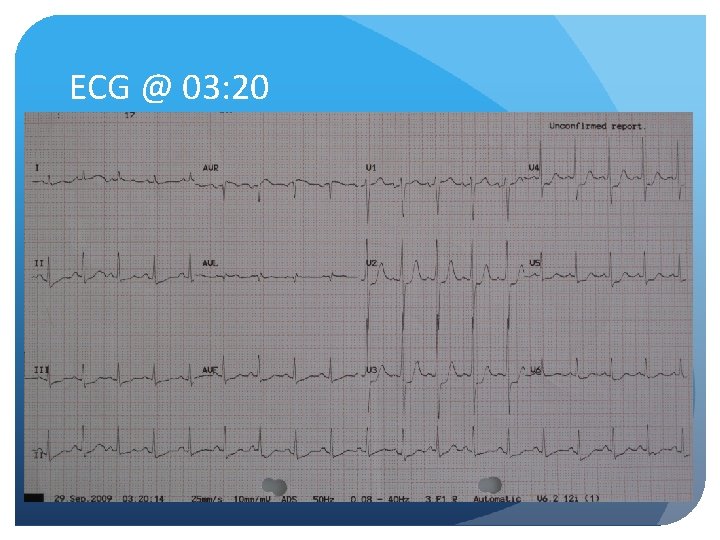
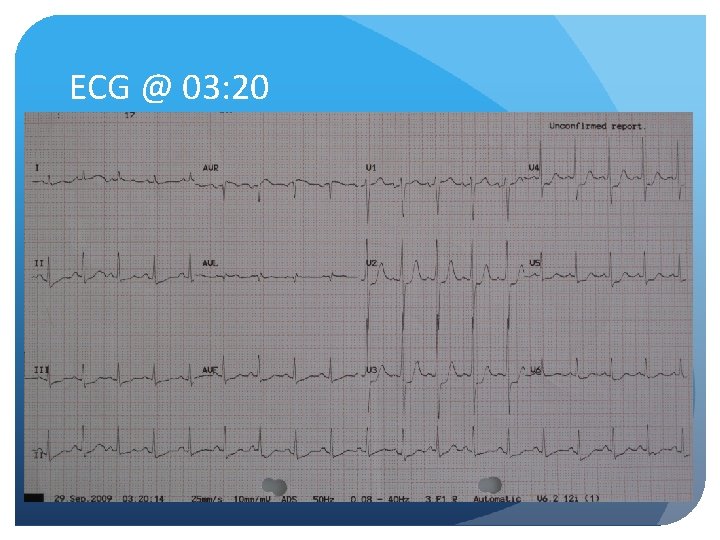
ECG @ 03: 20
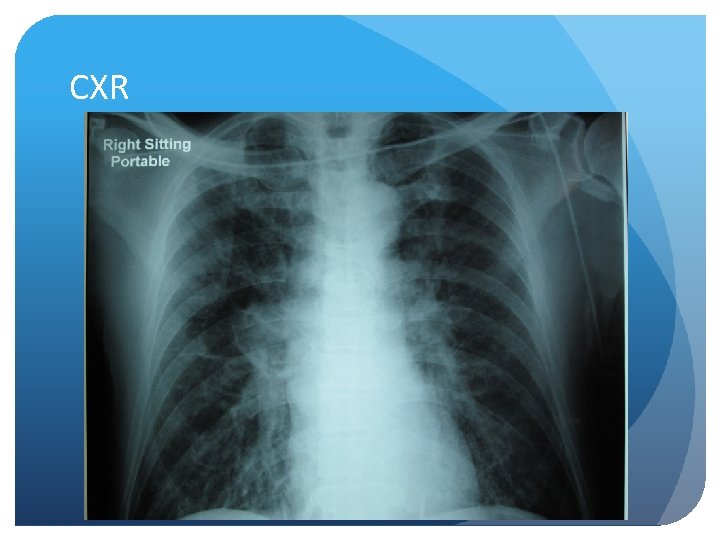
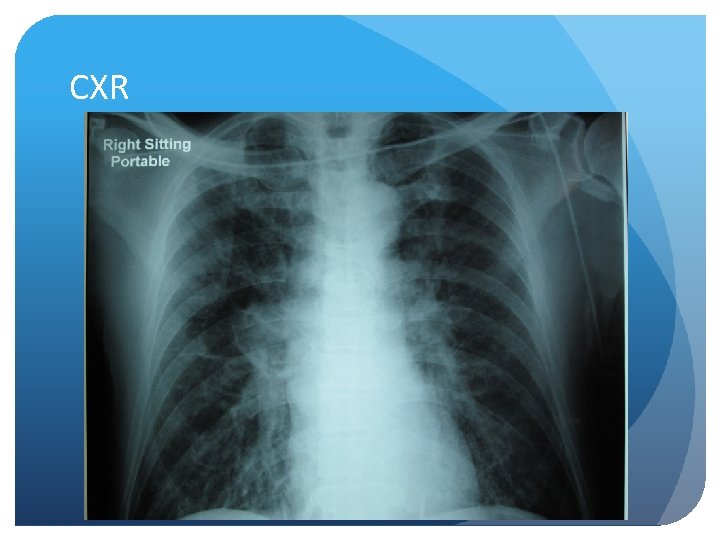
CXR
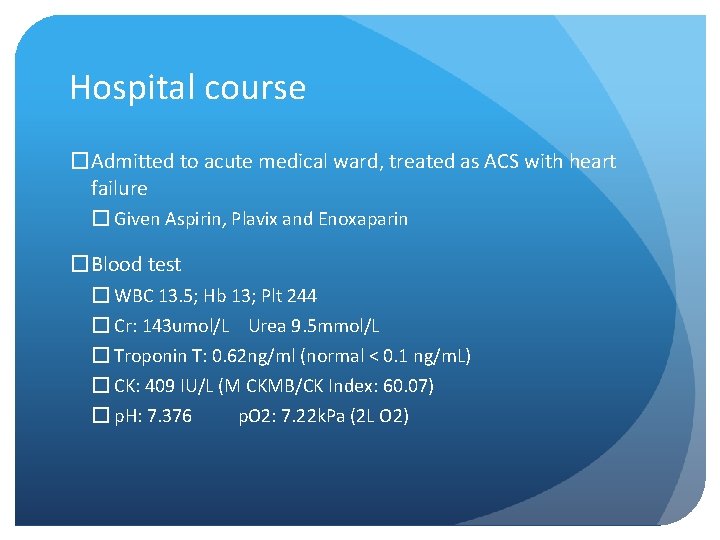
Hospital course �Admitted to acute medical ward, treated as ACS with heart failure � Given Aspirin, Plavix and Enoxaparin �Blood test � WBC 13. 5; Hb 13; Plt 244 � Cr: 143 umol/L Urea 9. 5 mmol/L � Troponin T: 0. 62 ng/ml (normal < 0. 1 ng/m. L) � CK: 409 IU/L (M CKMB/CK Index: 60. 07) � p. H: 7. 376 p. O 2: 7. 22 k. Pa (2 L O 2)
Hospital course �Condition partially improved �Palpitation subsided without any back discomfort � BP 114/78; HR 72 � Sa. O 2 > 95% with 2 L NC O 2
Hospital course �Developed sudden deterioration 4 hours after admission � Desaturation requiring 100% O 2 mask � Dopamine infusion was started � BP 103/72; HR 110; � Still able to reveal no chest pain
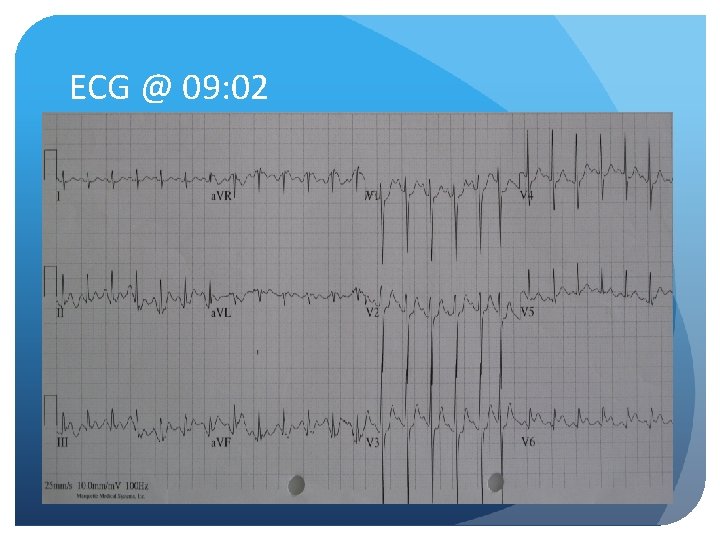
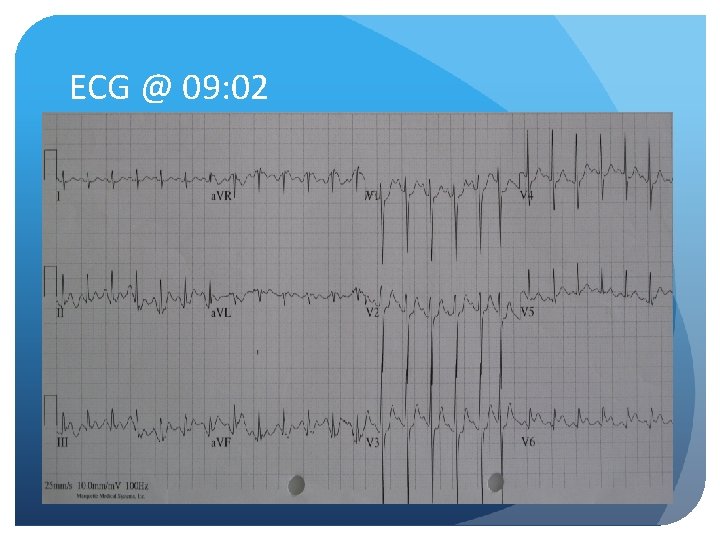
ECG @ 09: 02
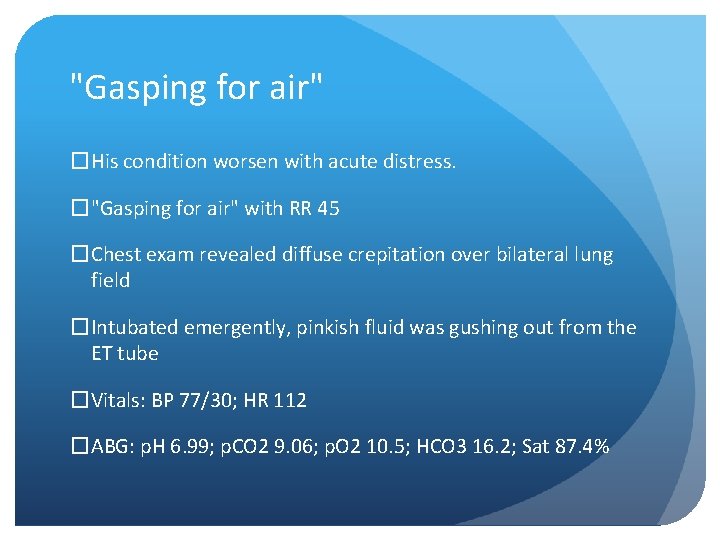
"Gasping for air" �His condition worsen with acute distress. �"Gasping for air" with RR 45 �Chest exam revealed diffuse crepitation over bilateral lung field �Intubated emergently, pinkish fluid was gushing out from the ET tube �Vitals: BP 77/30; HR 112 �ABG: p. H 6. 99; p. CO 2 9. 06; p. O 2 10. 5; HCO 3 16. 2; Sat 87. 4%
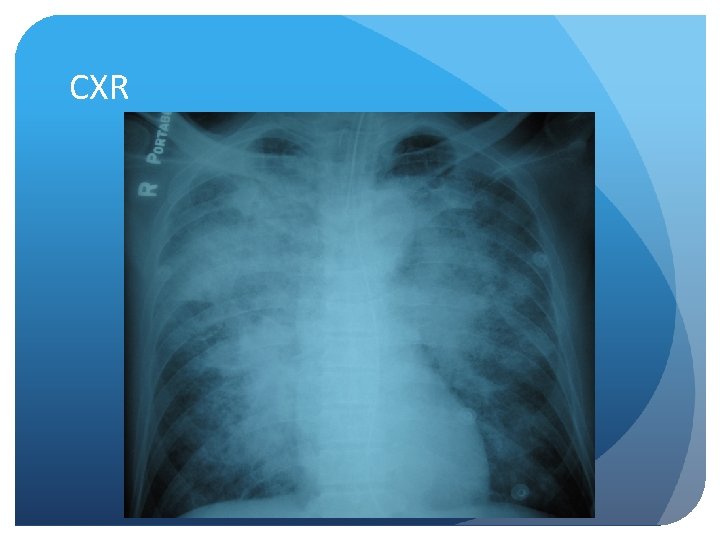
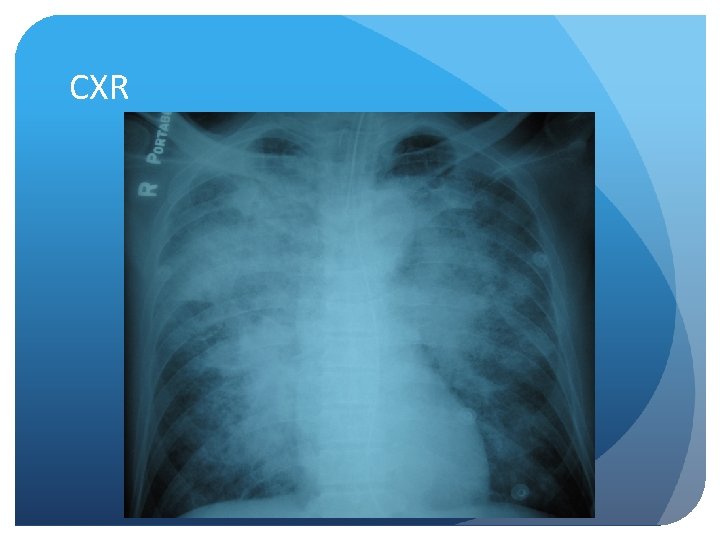
CXR
Case Summary � 59 yo male with smoking history admitted for palpitation and dull back pain �NSTEMI was diagnosed, treated with triple therapy then developed sudden onset of dyspnea and desaturation �Clinically in profound cardiogenic shock requiring inotropic and ventilatory support �Transferred to our Cardiac and Intensive Care Unit
What would you do next? �Extra dose of Lasix �Increase inotropes �Insertion of Swan Ganz catheter �Contrast CT �Echocardiography �Emergency coronary angiogram ± PCI �None of the above �All of the above
Cardiogenic Shock �<10% of AMI �Mortality 50 -60% �Etiology: � Extensive myocardial damage (>40% of LV) � Rupture of ventricular septum � Rupture of papillary muscle � Free wall rupture with tamponade � Right ventricular infarction � Marked reduction of preload (e. g. hypovolemia)
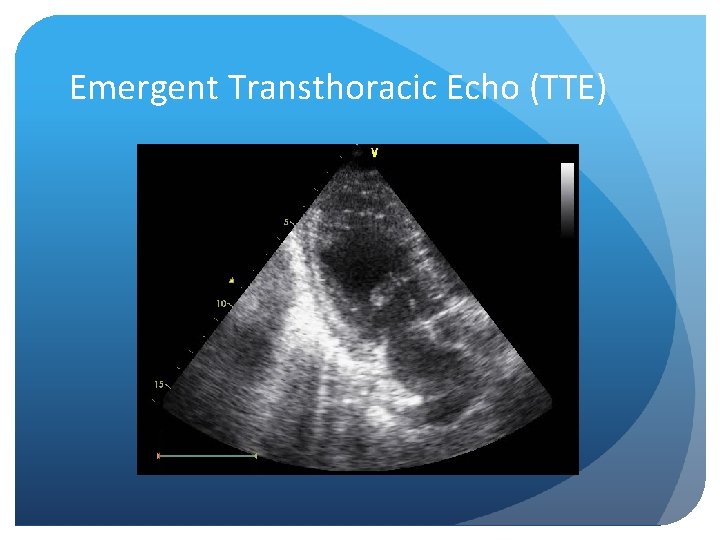
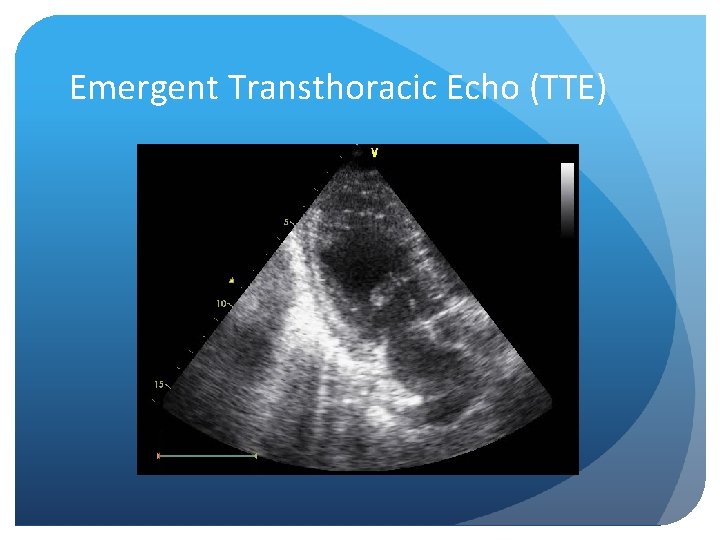
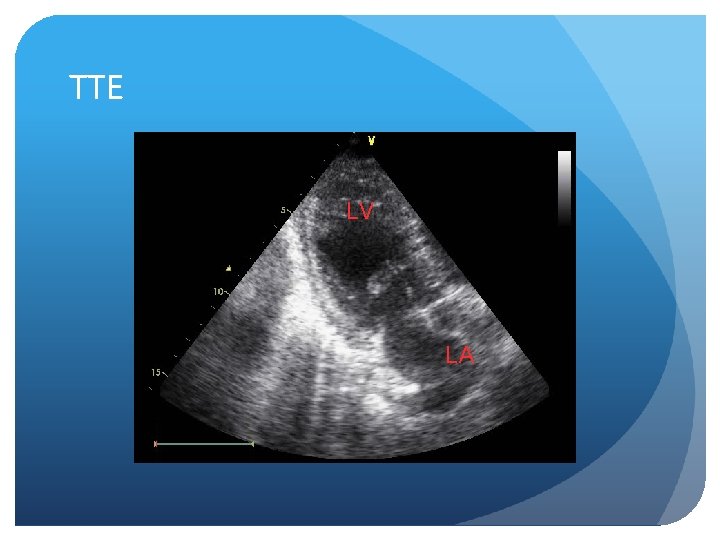
Emergent Transthoracic Echo (TTE)
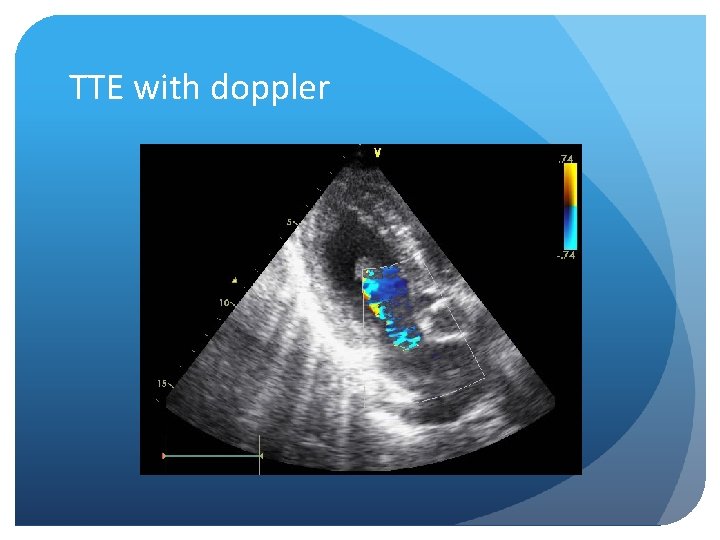
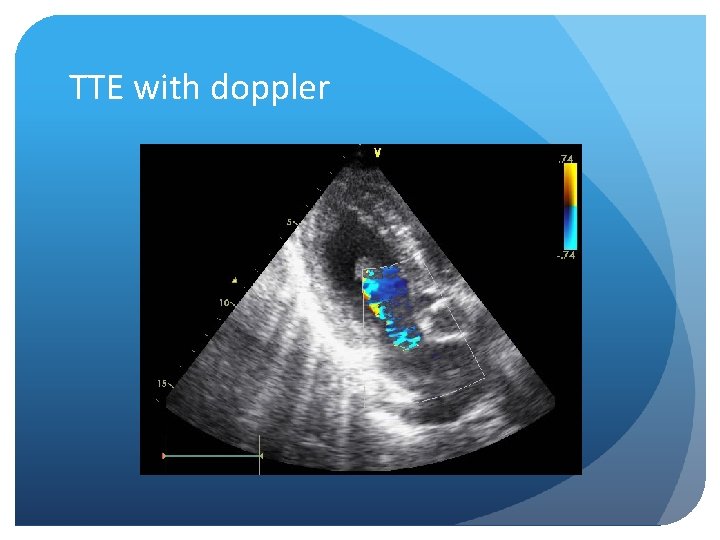
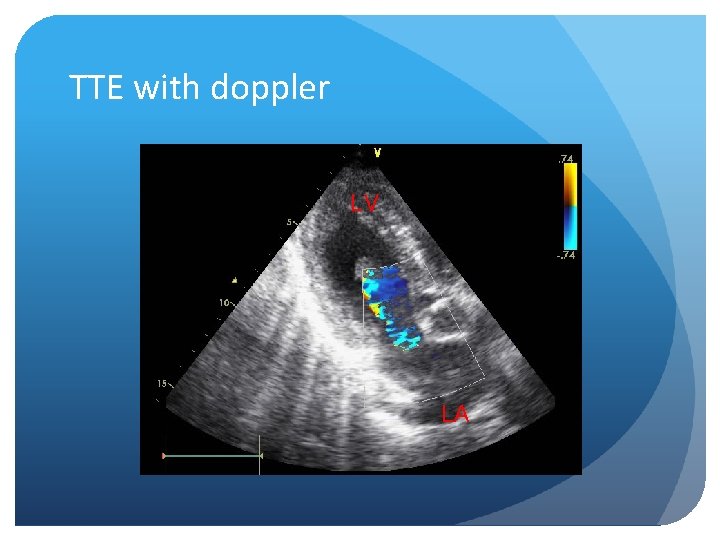
TTE with doppler
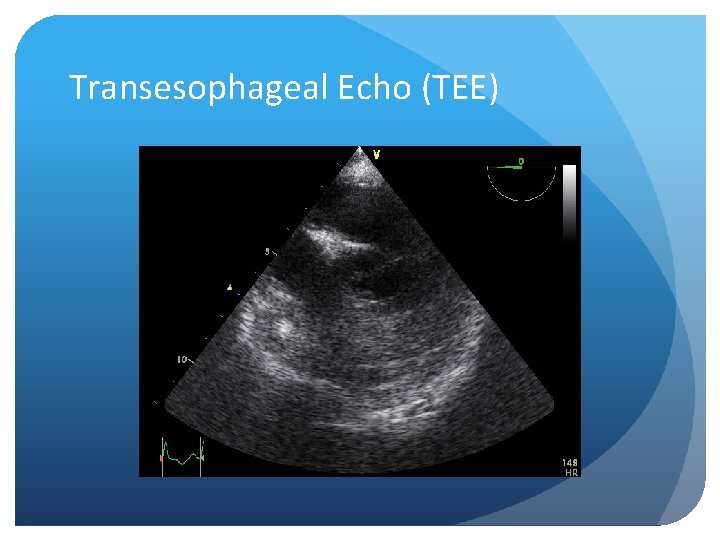
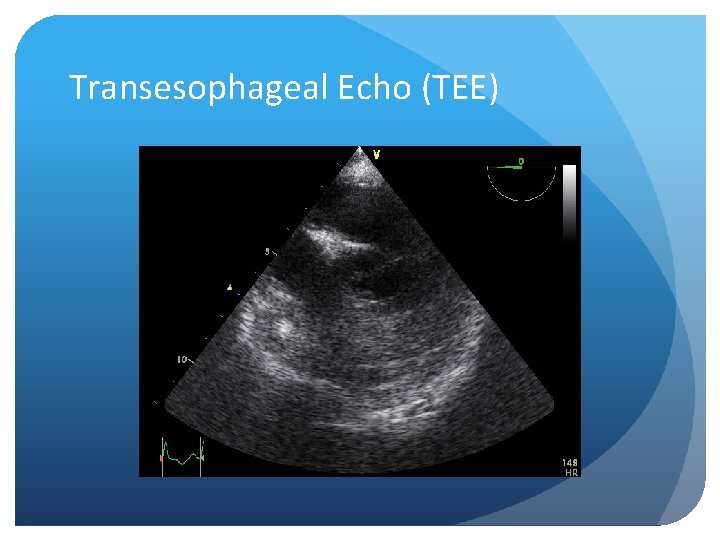
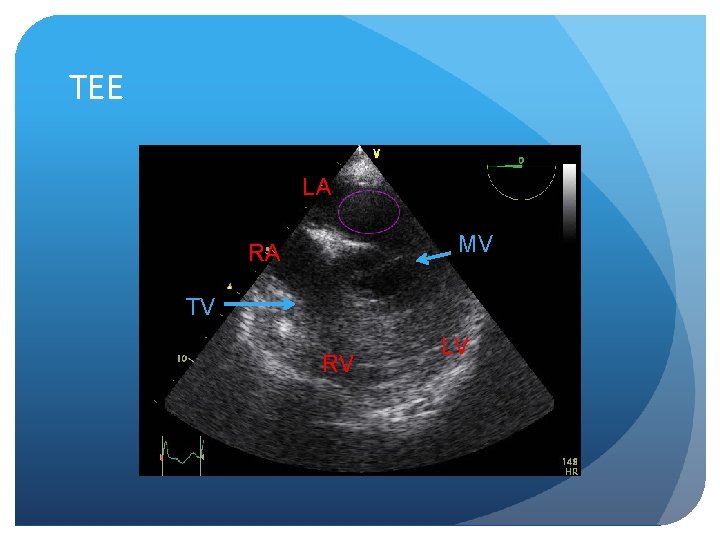
Transesophageal Echo (TEE)

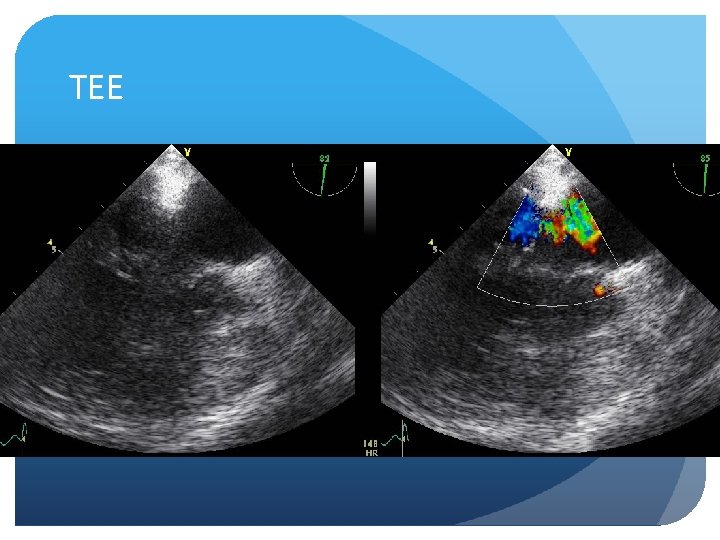
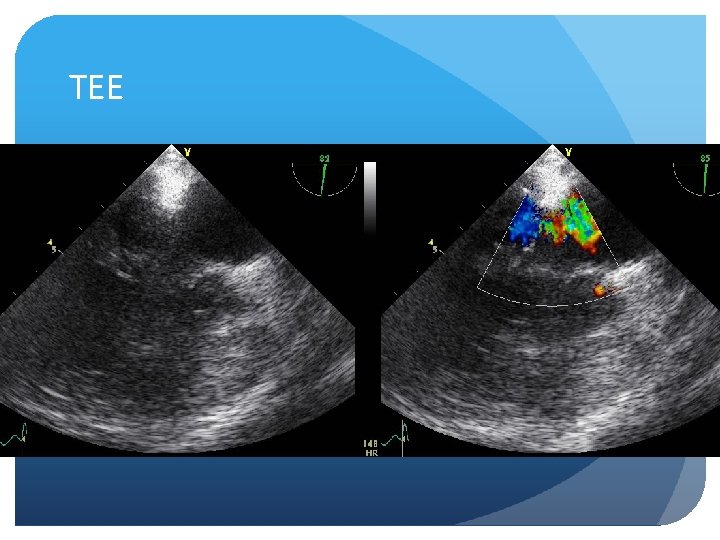
TEE

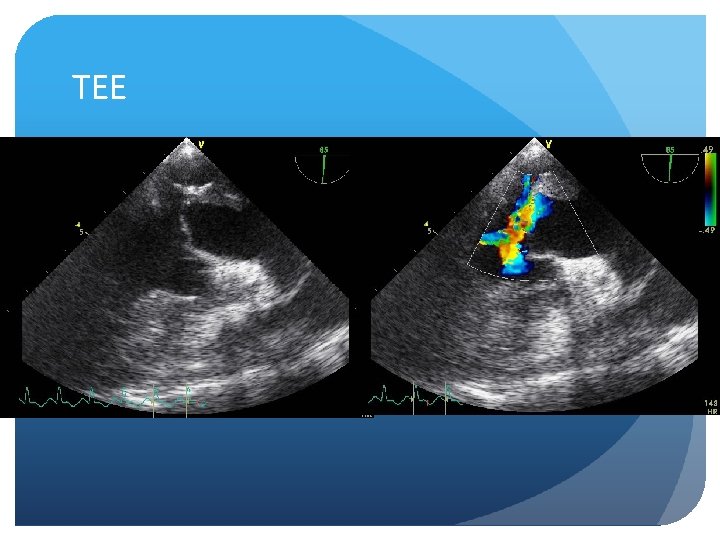
TEE
TEE
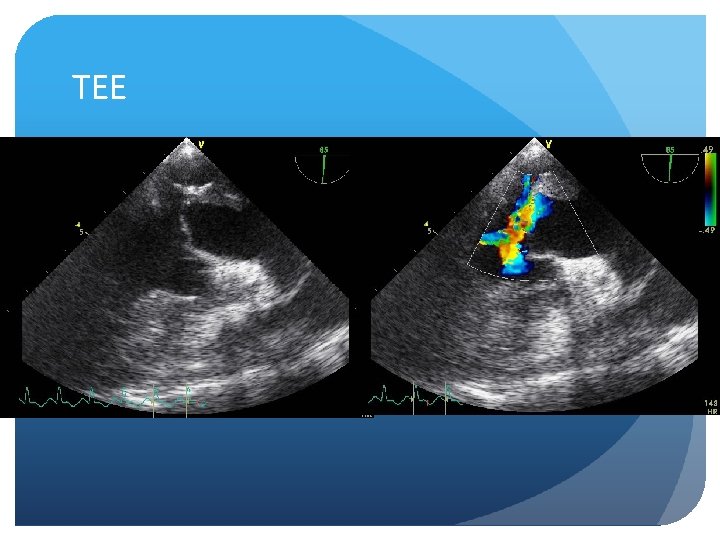
TEE
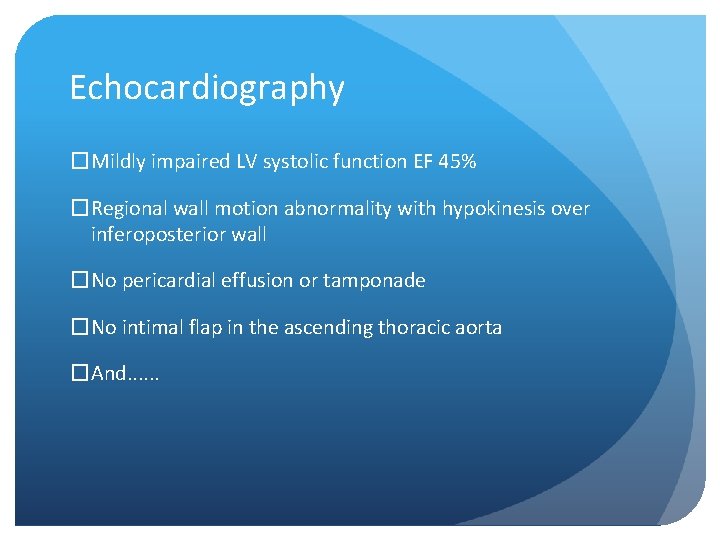
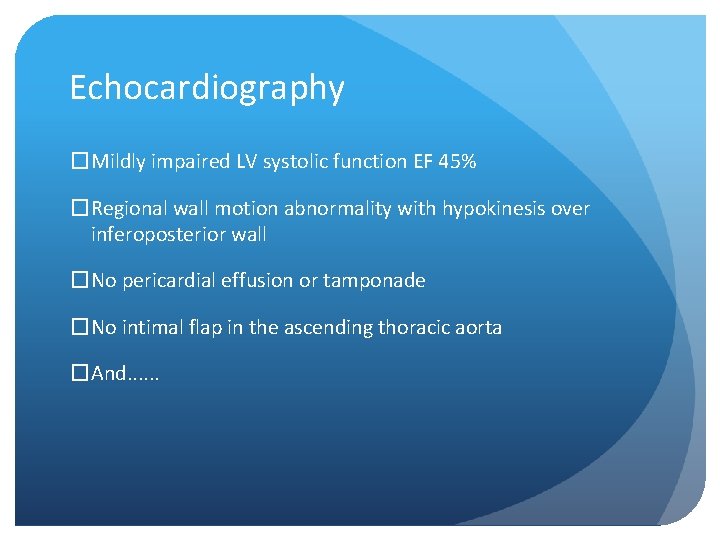
Echocardiography �Mildly impaired LV systolic function EF 45% �Regional wall motion abnormality with hypokinesis over inferoposterior wall �No pericardial effusion or tamponade �No intimal flap in the ascending thoracic aorta �And. . .
What is the echo diagnosis? �Endocarditis with vegetation attached to mitral valve leaflet �Atrial myxoma �Left atrial mural thrombus �Large pulmonary embolism �Papillary muscle rupture �Cordae tendinae rupture �Artifact
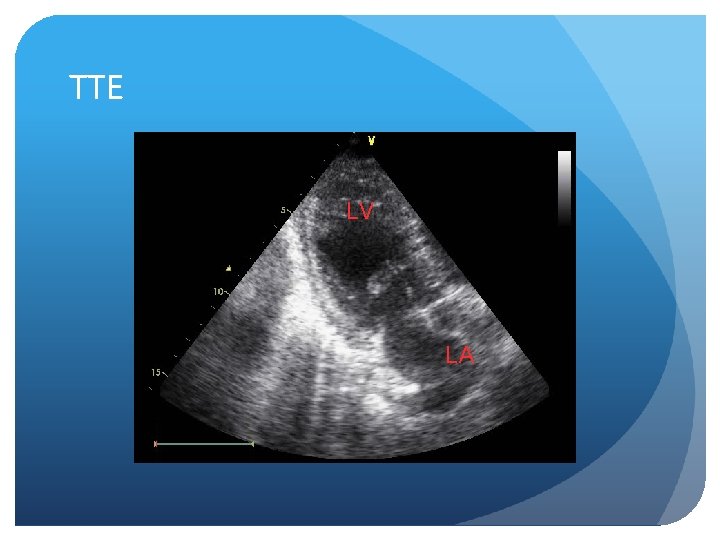
TTE LV LV LA LA
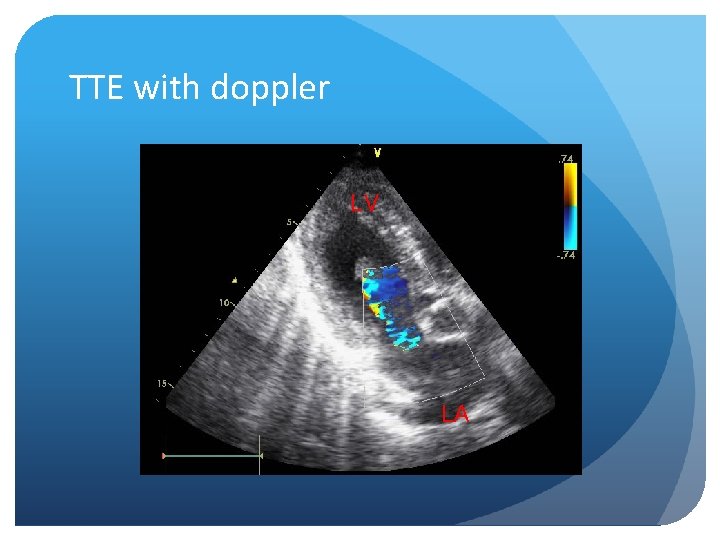
TTE with doppler LV LA
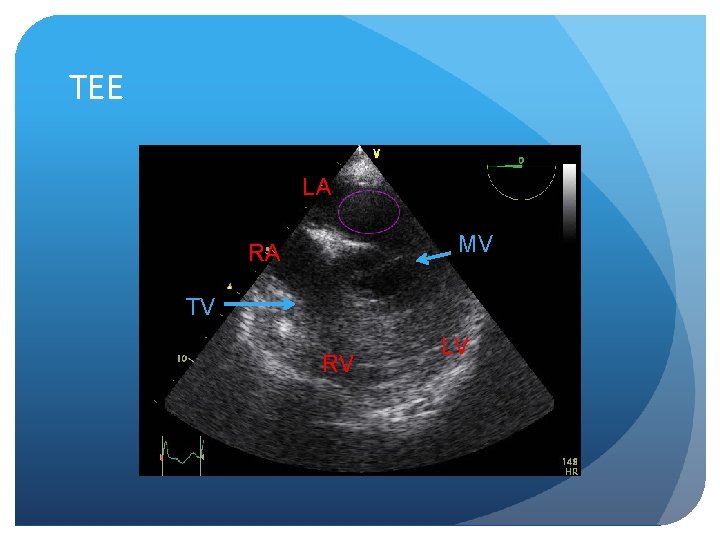
TEE LA MV RA TV RV LV
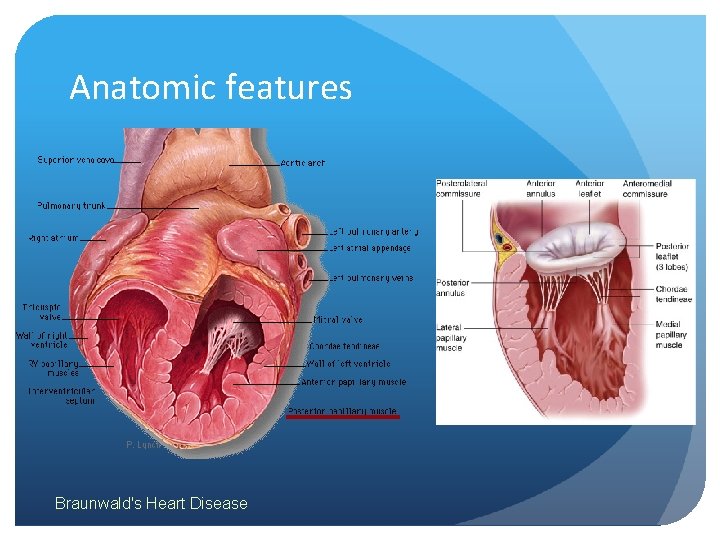
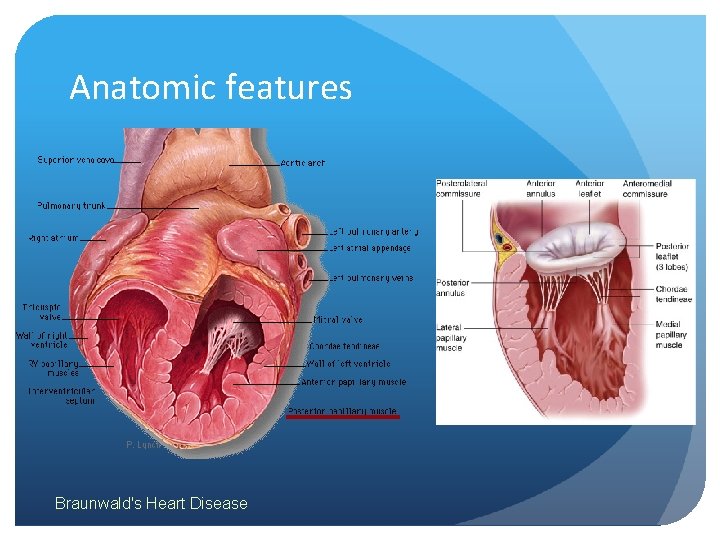
Anatomic features Braunwald's Heart Disease
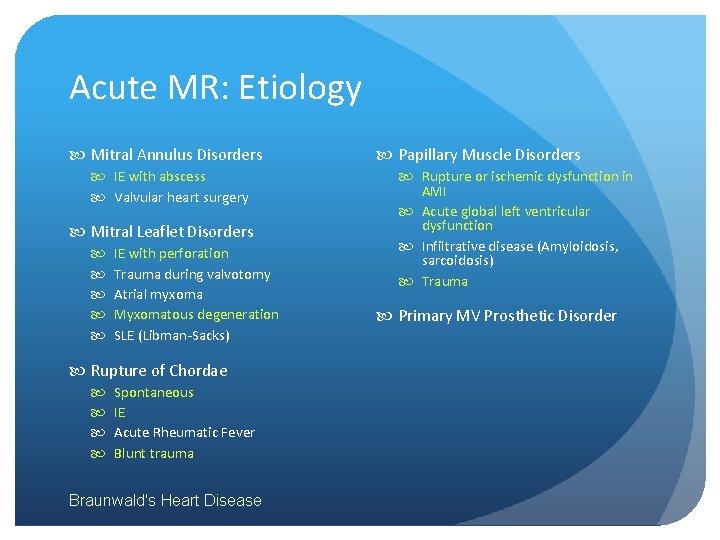
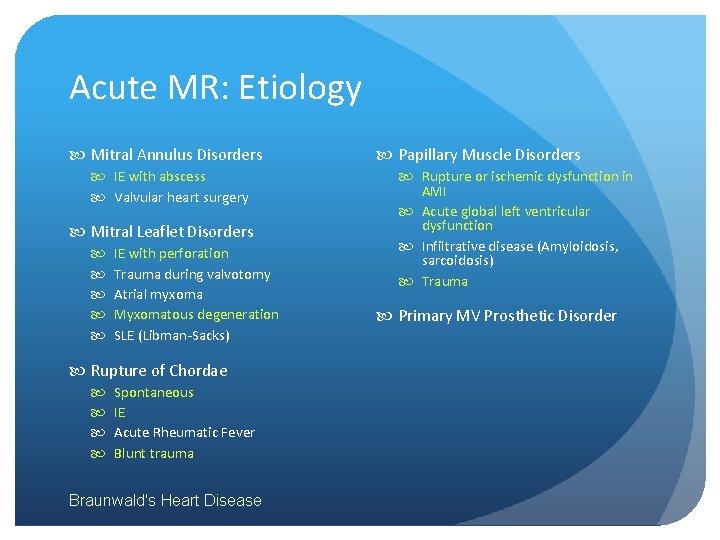
Acute MR: Etiology Mitral Annulus Disorders IE with abscess Valvular heart surgery Mitral Leaflet Disorders IE with perforation Trauma during valvotomy Atrial myxoma Myxomatous degeneration SLE (Libman-Sacks) Rupture of Chordae Spontaneous IE Acute Rheumatic Fever Blunt trauma Braunwald's Heart Disease Papillary Muscle Disorders Rupture or ischemic dysfunction in AMI Acute global left ventricular dysfunction Infiltrative disease (Amyloidosis, sarcoidosis) Trauma Primary MV Prosthetic Disorder
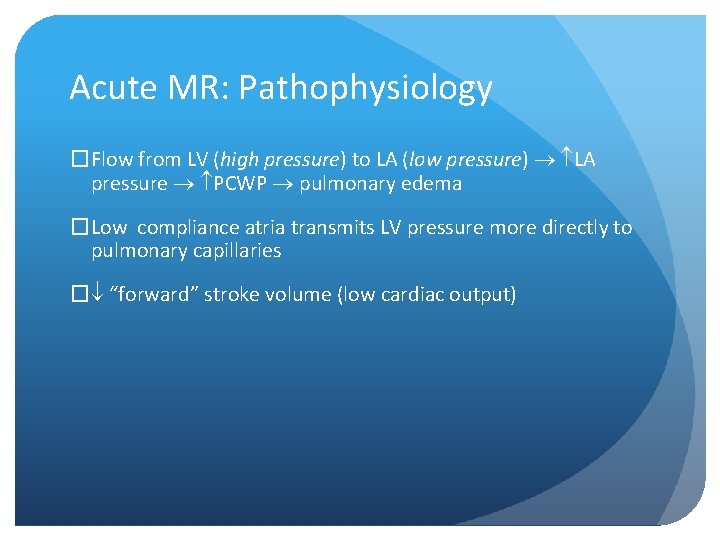
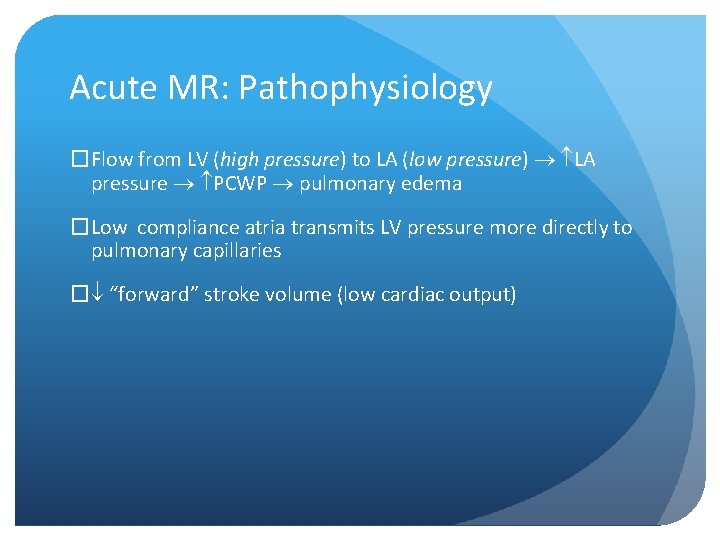
Acute MR: Pathophysiology �Flow from LV (high pressure) pressure to LA (low pressure) pressure LA pressure PCWP pulmonary edema �Low compliance atria transmits LV pressure more directly to pulmonary capillaries � “forward” stroke volume (low cardiac output)
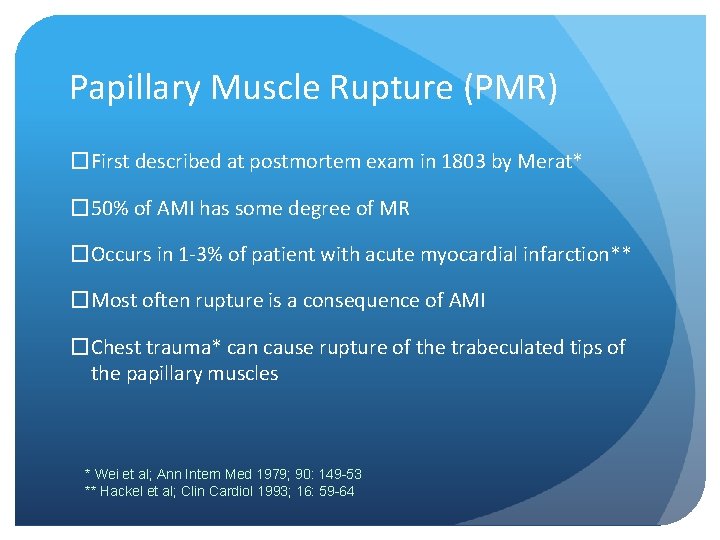
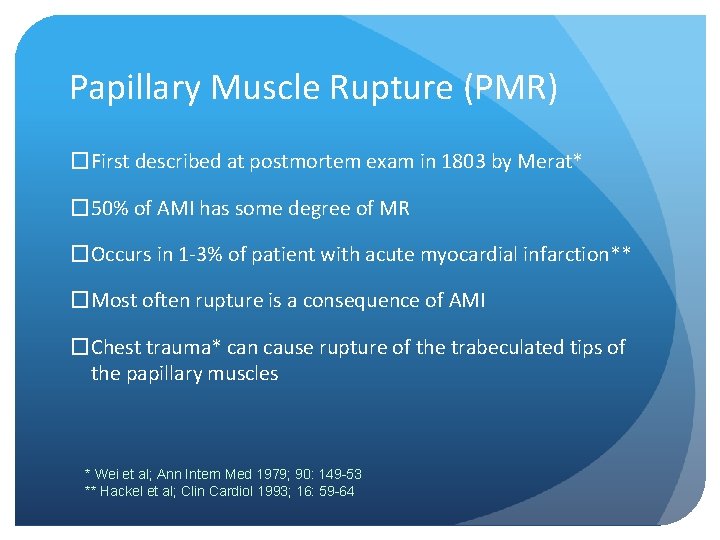
Papillary Muscle Rupture (PMR) �First described at postmortem exam in 1803 by Merat* � 50% of AMI has some degree of MR �Occurs in 1 -3% of patient with acute myocardial infarction** �Most often rupture is a consequence of AMI �Chest trauma* can cause rupture of the trabeculated tips of the papillary muscles * Wei et al; Ann Intern Med 1979; 90: 149 -53 ** Hackel et al; Clin Cardiol 1993; 16: 59 -64
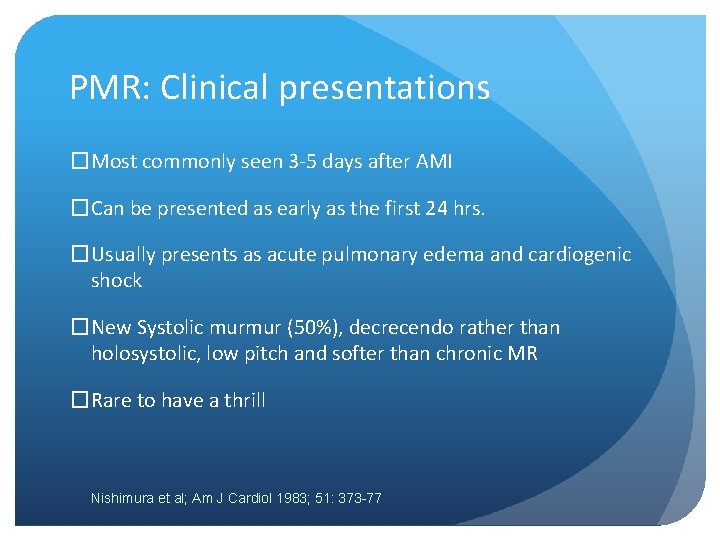
PMR: Clinical presentations �Most commonly seen 3 -5 days after AMI �Can be presented as early as the first 24 hrs. �Usually presents as acute pulmonary edema and cardiogenic shock �New Systolic murmur (50%), decrecendo rather than holosystolic, low pitch and softer than chronic MR �Rare to have a thrill Nishimura et al; Am J Cardiol 1983; 51: 373 -77
PMR: ECG changes �ECG can be diagnostic of AMI with ST elevation, but can be ST depression only or non-specific changes � 21/22 patients with papillary muscle rupture have inferior ECG changes* *Kishon et al; Mayo Clin Proc 1992; 67: 1023 -30
PMR: Diagnostic clues �Acute pulmonary edema + first AMI + inferior/posterior location + well-preserved LV systolic function �Physical sign of JVD in 50% patients � 2 D echocardiography with Doppler is the diagnostic of choice �TEE* is highly diagnostic if TTE is suboptimal in defining the abnormal mitral valve and the MR * Zota et al; Clin Cardiol 1993; 16: 665 -70
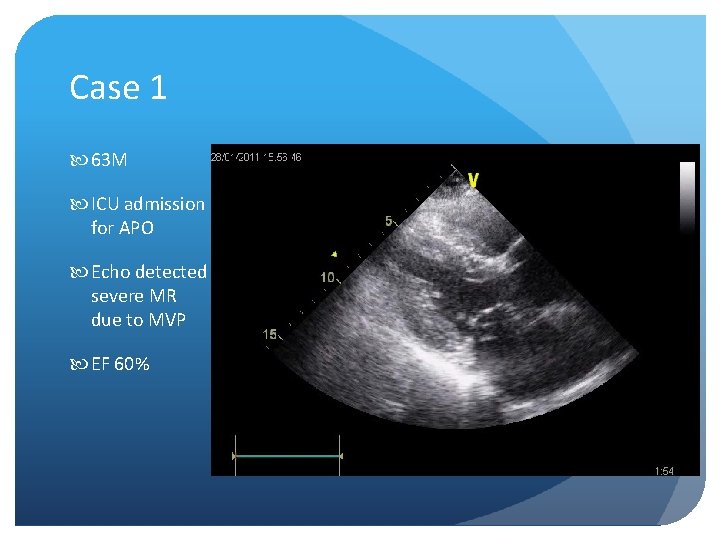
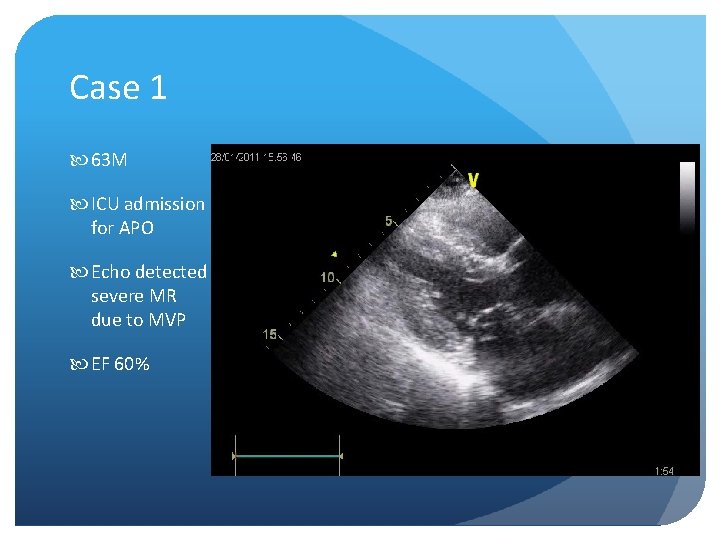
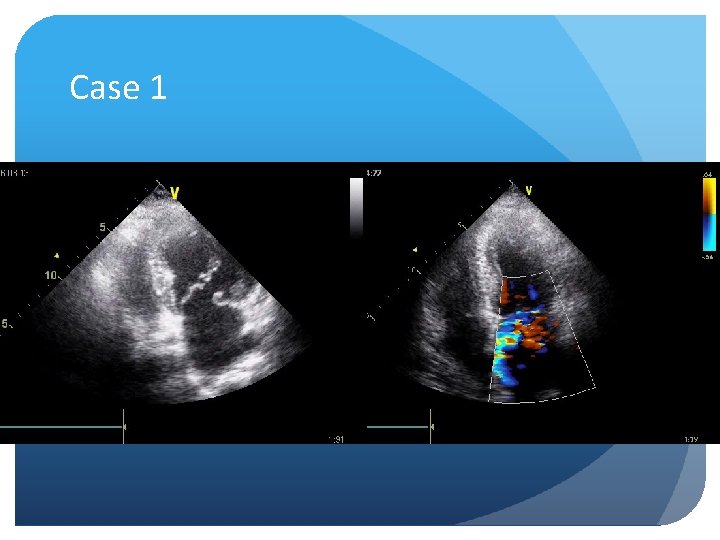
Case 1 63 M ICU admission for APO Echo detected severe MR due to MVP EF 60%
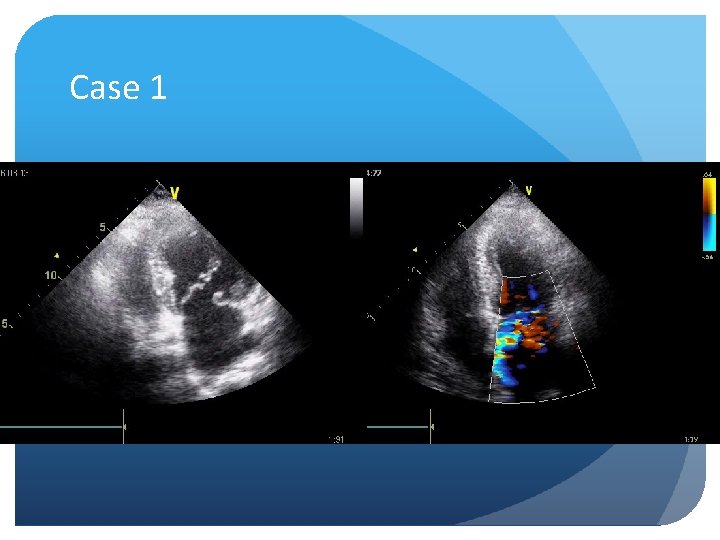
Case 1
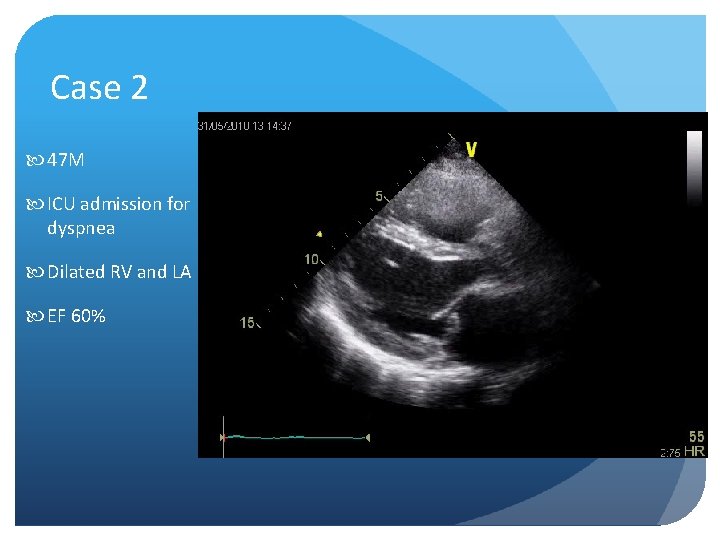
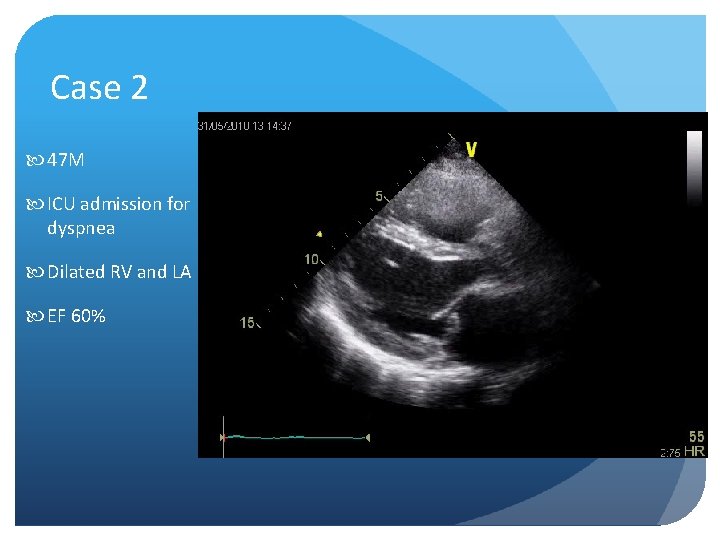
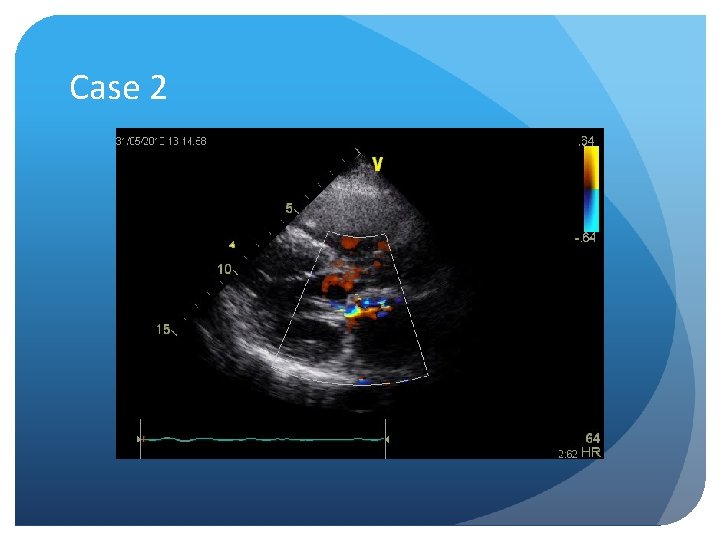
Case 2 47 M ICU admission for dyspnea Dilated RV and LA EF 60%
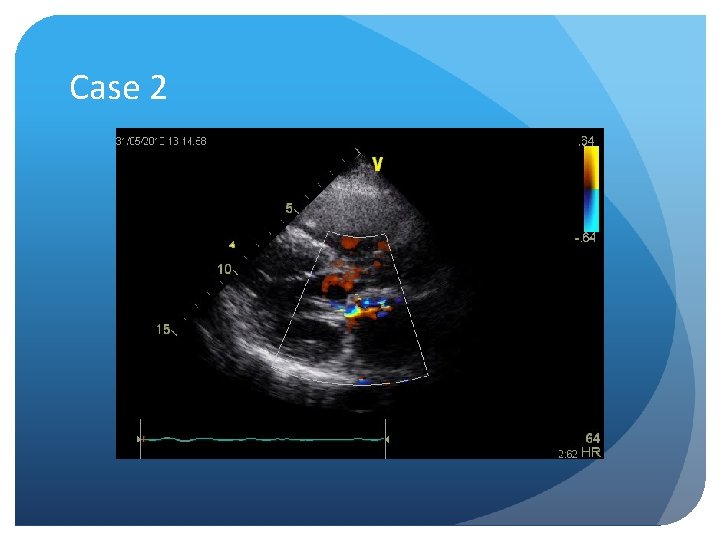
Case 2
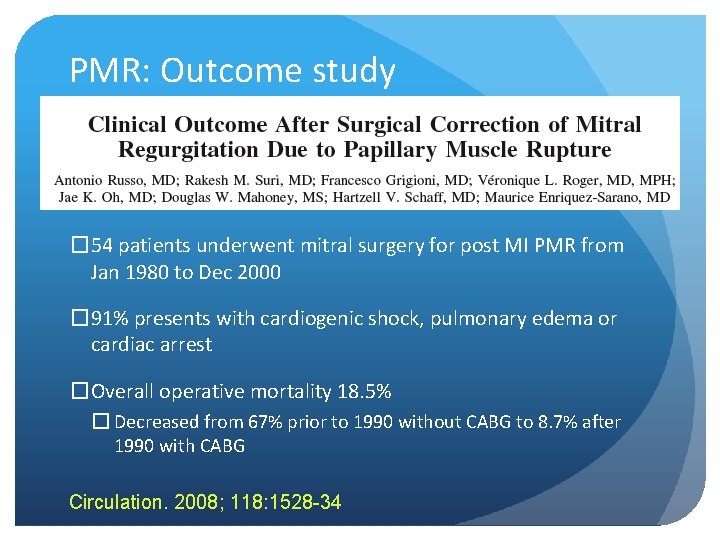
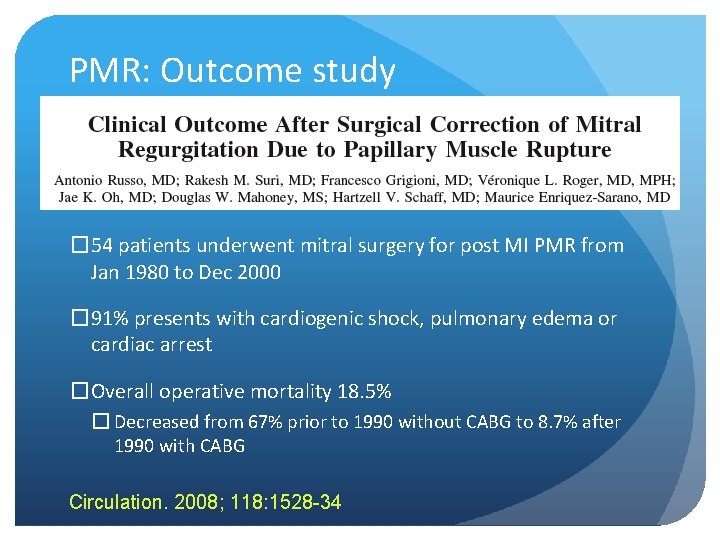
PMR: Outcome study � 54 patients underwent mitral surgery for post MI PMR from Jan 1980 to Dec 2000 � 91% presents with cardiogenic shock, pulmonary edema or cardiac arrest �Overall operative mortality 18. 5% � Decreased from 67% prior to 1990 without CABG to 8. 7% after 1990 with CABG Circulation. 2008; 118: 1528 -34
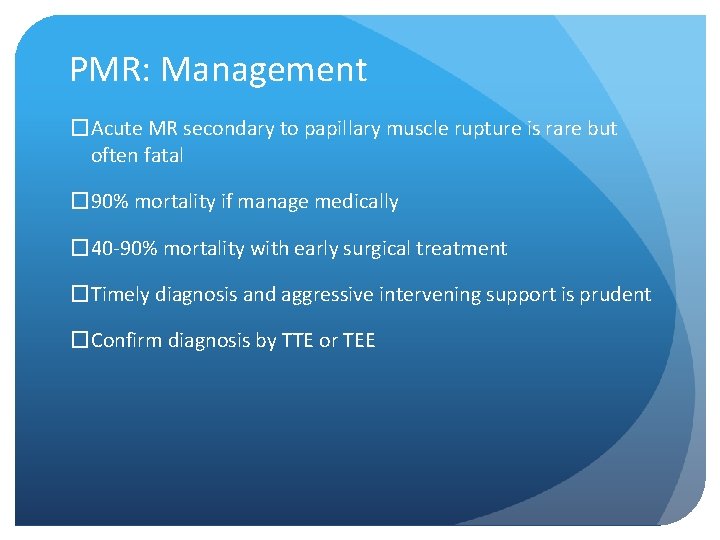
PMR: Management �Acute MR secondary to papillary muscle rupture is rare but often fatal � 90% mortality if manage medically � 40 -90% mortality with early surgical treatment �Timely diagnosis and aggressive intervening support is prudent �Confirm diagnosis by TTE or TEE
PMR: Management �Vasodilators (IV NTG or NTP) to reduce afterload (if SBP>90) is the main stay of treatment �Judicious use of Inotropic agents if SBP<90 �IABP placement helps stabilizing the patient �Emergent Mitral valve replacement and coronary grafting
Hospital course �Patient remain hypotensive despite inotropic support �CPR required while placing IABP and blood pressure restored �With triple inotropes on board, patient was transported to QMH Cardiothoracic unit
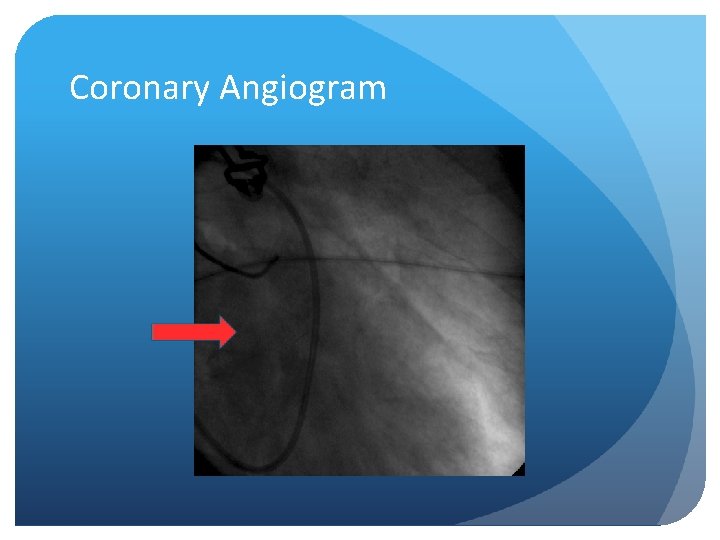
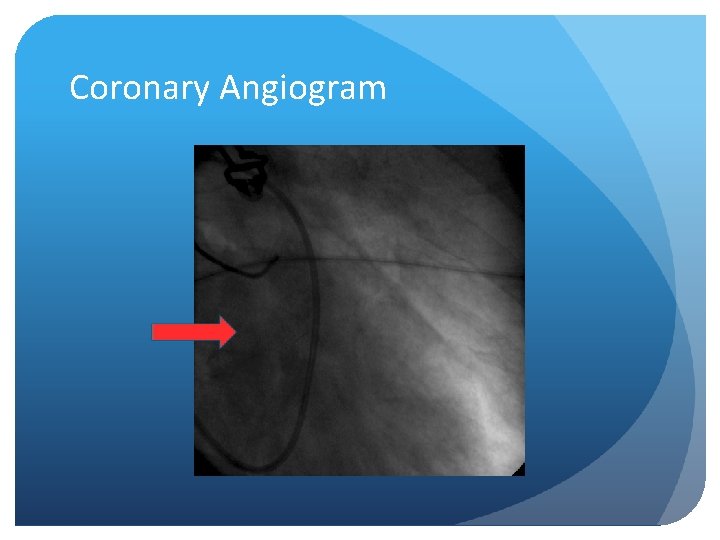
Coronary Angiogram
Coronary Angiogram
QMH Hospital course �Emergency operation was performed on the same day �MVR (SJM 25#) and �CABG (SVG to LCx) �Intraoperative finding revealed complete prolapse of MV due to rupture of a large posteromedial papillary muscle (0. 8 x 1. 5 cm) �Pathology report showed necrotic cardiac muscle cell consistent with infarction
Intra-op Photo
Hospital course �IABP weaned off on post operation D 3 �Tracheostomy performed on D 8 �Transferred back to RH ICU on D 9 �Weaned off ventilator on D 16 �Underwent rehabilitation in cardiac ward �Discharged home on D 32
Pearls in the diagnosis! �Clinical � Absence of murmur in acute MR � Shock �ECG � Non-specific changes �Echo � TTE vs. TEE
Take home message �Suspect mechanical complication of AMI such as papillary muscle rupture in patients with acute pulmonary edema or cardiogenic shock �Especially patient with AMI and preserved systolic LV function �Absence of a murmur does not exclude the diagnosis �If TTE fails to confirm the diagnosis, a TEE should be done
Take home message �Coronary angiogram should be performed whenever patient condition allows to assess the coronary artery status for concomitant CABG during MVR �Temporary stabilization with vasodilators, inotropes and IABP are important to bridge over preoperatively �Emergent mitral valve replacement and coronary artery grafting is the definitive treatment
“Thanks Doc, it was a nightmare, I finally pull through with your prompt diagnosis and emergent treatment!” • Well • Asymptomatic • ADL Independent • Working part-time as a waiter
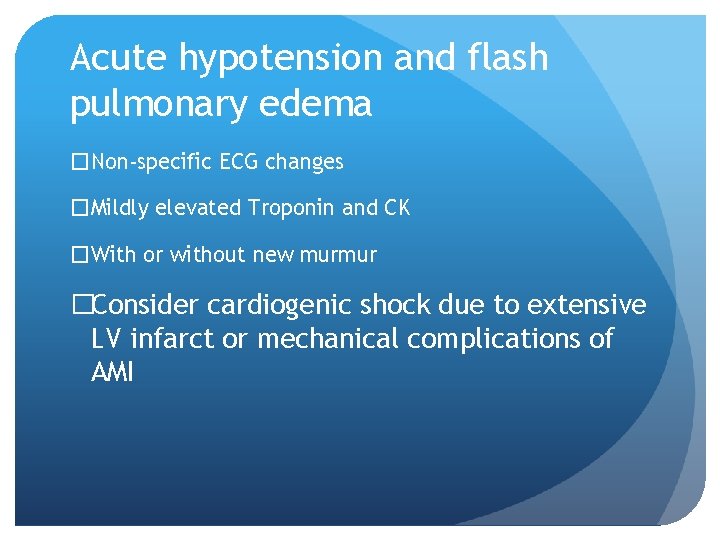
Acute hypotension and flash pulmonary edema �Non-specific ECG changes �Mildly elevated Troponin and CK �With or without new murmur �Consider cardiogenic shock due to extensive LV infarct or mechanical complications of AMI
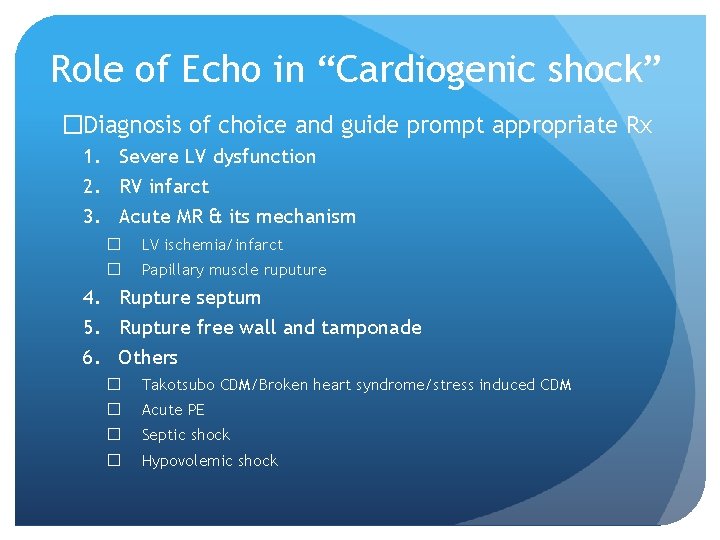
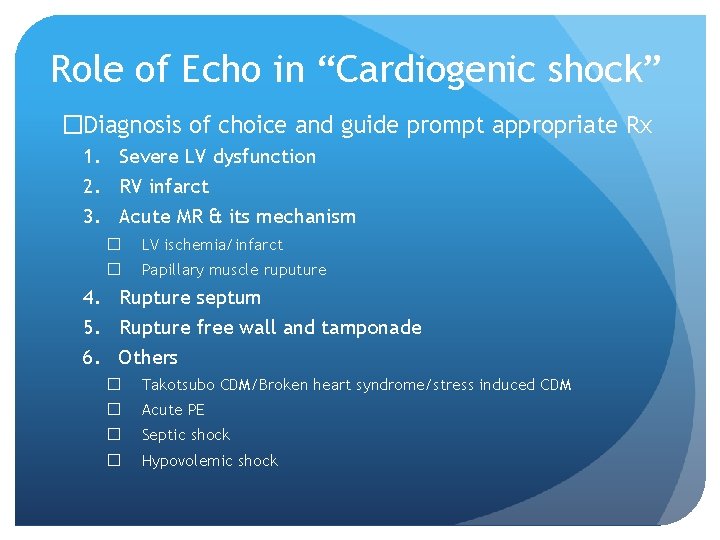
Role of Echo in “Cardiogenic shock” �Diagnosis of choice and guide prompt appropriate Rx 1. Severe LV dysfunction 2. RV infarct 3. Acute MR & its mechanism � LV ischemia/infarct � Papillary muscle ruputure 4. Rupture septum 5. Rupture free wall and tamponade 6. Others � Takotsubo CDM/Broken heart syndrome/stress induced CDM � Acute PE � Septic shock � Hypovolemic shock
Thank you Special thanks to Dr. YK Lau
 Transportasi pasien gawat darurat
Transportasi pasien gawat darurat Interhospital
Interhospital Ccm crm
Ccm crm Ccm eligibility
Ccm eligibility Ccm exemple
Ccm exemple Model ccm
Model ccm Ccm
Ccm Continuous control monitoring definition
Continuous control monitoring definition Enterprise ccm
Enterprise ccm Ccm tutorials
Ccm tutorials Bhutan ccm
Bhutan ccm Ccm certification construction
Ccm certification construction Nightmare on elms street
Nightmare on elms street Night terror vs nightmare
Night terror vs nightmare Zog's nightmare
Zog's nightmare Running children in a nightmare heat
Running children in a nightmare heat Carsonian nightmare
Carsonian nightmare A free bird leaps
A free bird leaps Third world
Third world Nightmare.js
Nightmare.js Jane eyre foreshadowing
Jane eyre foreshadowing Nightmare over the atlantic
Nightmare over the atlantic Daydream island nightmare
Daydream island nightmare Fannie mae homepath nightmare
Fannie mae homepath nightmare Nightmare best friend
Nightmare best friend Nightmare waiting list cartoon
Nightmare waiting list cartoon What event happened first in my shopping norte's nightmare
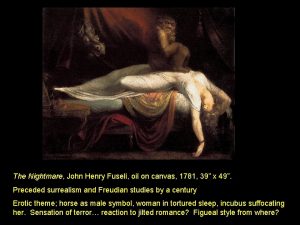
What event happened first in my shopping norte's nightmare John henry fuseli
John henry fuseli Symbolic archetype
Symbolic archetype Gossip girl every parent's nightmare
Gossip girl every parent's nightmare Carsonian nightmare
Carsonian nightmare Joint hospital surgical grand round
Joint hospital surgical grand round Tows matrix of coca cola
Tows matrix of coca cola Joint hospital surgical grand round
Joint hospital surgical grand round Et moi je suis avec vous tous les jours
Et moi je suis avec vous tous les jours Grand solutions international
Grand solutions international Grand vin de reignac 2010
Grand vin de reignac 2010 Ie matrix
Ie matrix Grand somsa yakkasaroy
Grand somsa yakkasaroy Grand barbados beach resort
Grand barbados beach resort Grand banks earthquake of 1929
Grand banks earthquake of 1929 Grand fermage lactalis
Grand fermage lactalis Grand forks personals
Grand forks personals Grand solutions guidelines
Grand solutions guidelines Il pleuvait fort sur la grand route
Il pleuvait fort sur la grand route Grand oiseau blanc
Grand oiseau blanc Contoh grand theory
Contoh grand theory Sydekick grand haven
Sydekick grand haven Master choa kok sui son
Master choa kok sui son Suggest grand
Suggest grand Plus grand tableau du monde
Plus grand tableau du monde Grand canonical ensemble
Grand canonical ensemble Politics of strategy choice
Politics of strategy choice Grand blanc high school staff
Grand blanc high school staff