Coronary Artery Disease and Acute Coronary Syndrome Description
- Slides: 41
Coronary Artery Disease and Acute Coronary Syndrome
Description • Coronary Artery Disease (CAD) – A type of blood vessel disorder that is included in the general category of atherosclerosis
Description • Atherosclerosis – Can occur in any artery in the body – Atheromas (fatty deposits) • Preference for the coronary arteries
Description • Atherosclerosis – Terms to describe the disease process: • Arteriosclerotic heart disease (ASHD) • Cardiovascular heart disease (CHD) • Ischemic heart disease (IHD) • CAD
Description • Cardiovascular diseases are the major cause of death in the US and Canada • Heart attacks are still the leading cause of all cardiovascular disease deaths and deaths in general
Etiology and Pathophysiology • Atherosclerosis is the major cause of CAD – Characterized by a focal deposit of cholesterol and lipids, primarily within the intimal wall of the artery
Etiology and Pathophysiology • Endothelial lining altered as a result of chemical injuries – Hyperlipidemia – Hypertension
Etiology and Pathophysiology • Bacteria and/or viruses may have role in damaging endothelium by causing local inflammation • C-reactive protein (CRP) – Nonspecific marker of inflammation – Increased in many patients with CAD – Chronic exposure to CRP triggers the rupture of plaques
Etiology and Pathophysiology • Endothelial alteration – Platelets are activated – Growth factor stimulates smooth muscle proliferation – Cell proliferation entraps lipids, which calcify over time and form an irritant to the endothelium on which platelets adhere and aggregate
Etiology and Pathophysiology • Endothelial alteration – Thrombin is generated – Fibrin formation and thrombi occur
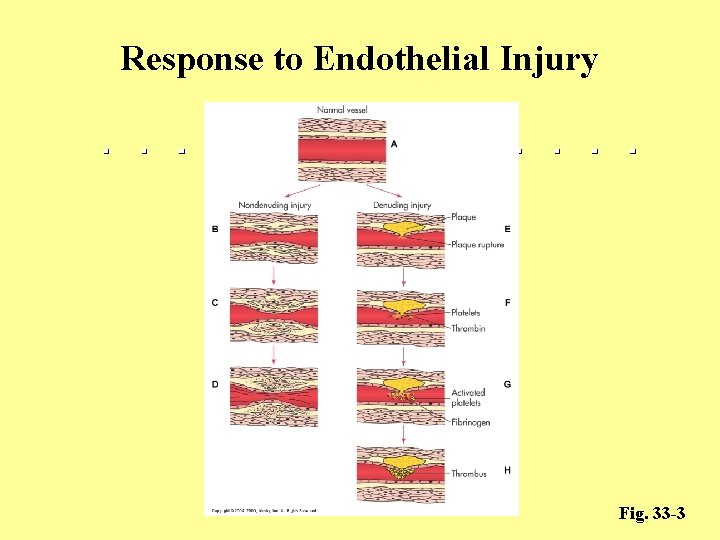
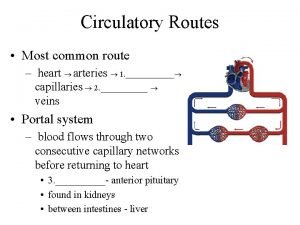
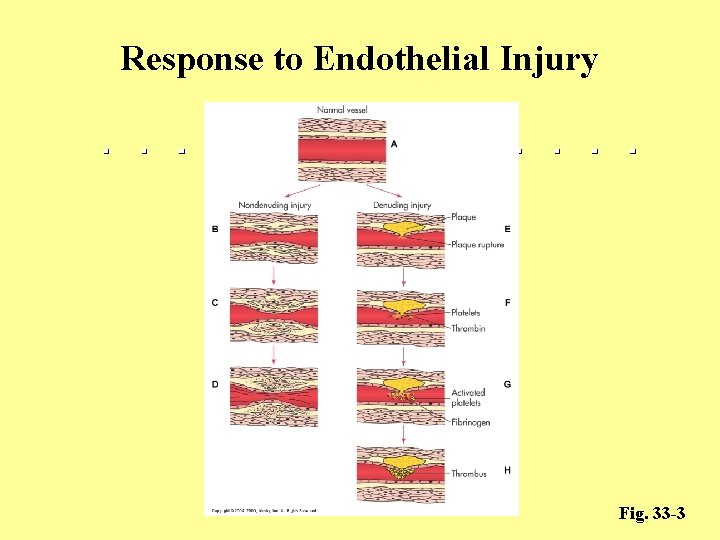
Response to Endothelial Injury Fig. 33 -3
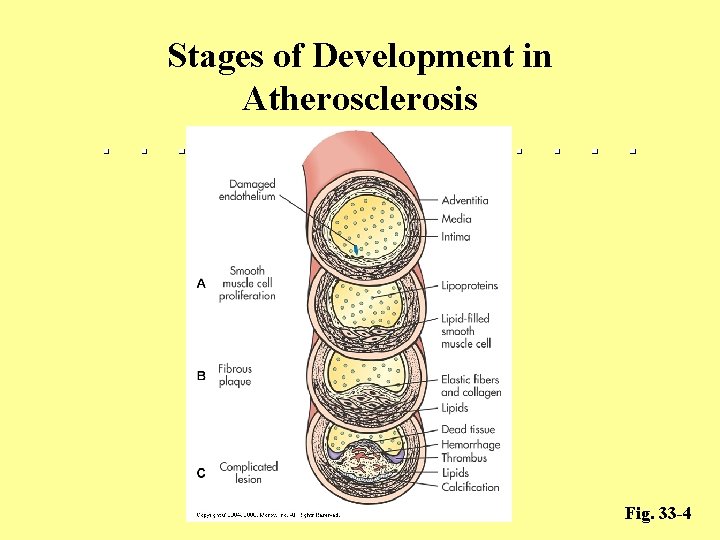
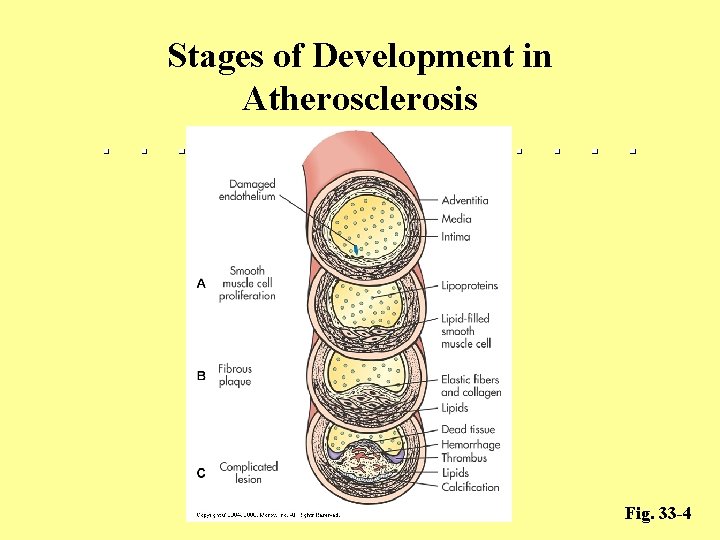
Stages of Development in Atherosclerosis Fig. 33 -4
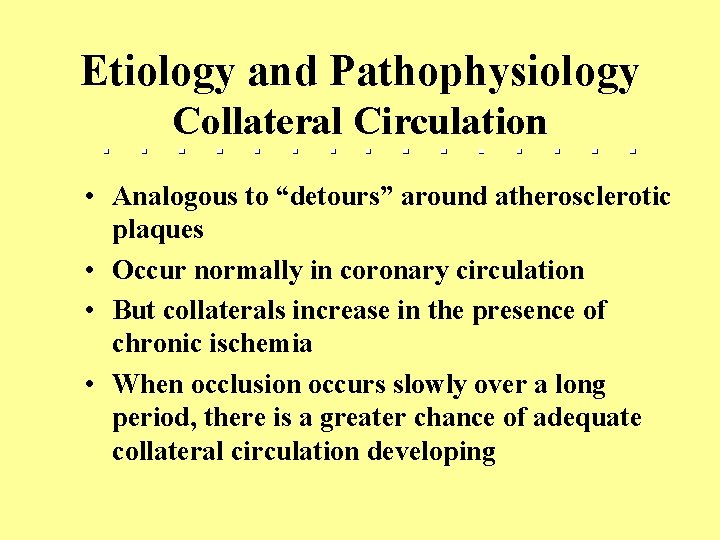
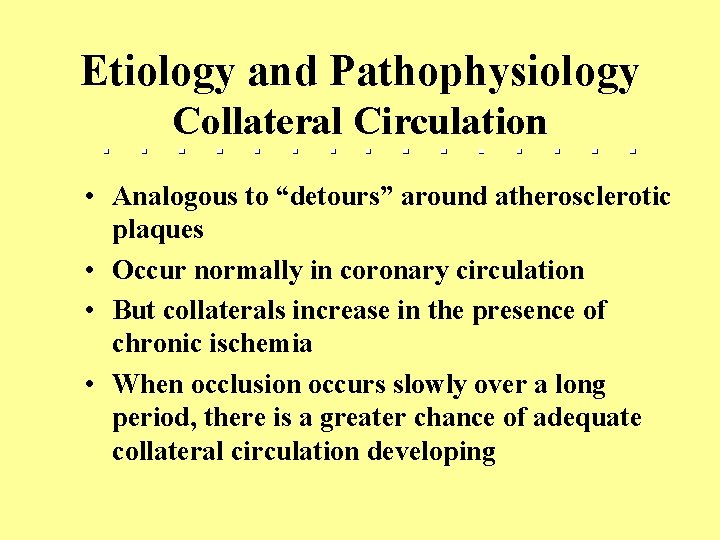
Etiology and Pathophysiology Collateral Circulation • Analogous to “detours” around atherosclerotic plaques • Occur normally in coronary circulation • But collaterals increase in the presence of chronic ischemia • When occlusion occurs slowly over a long period, there is a greater chance of adequate collateral circulation developing
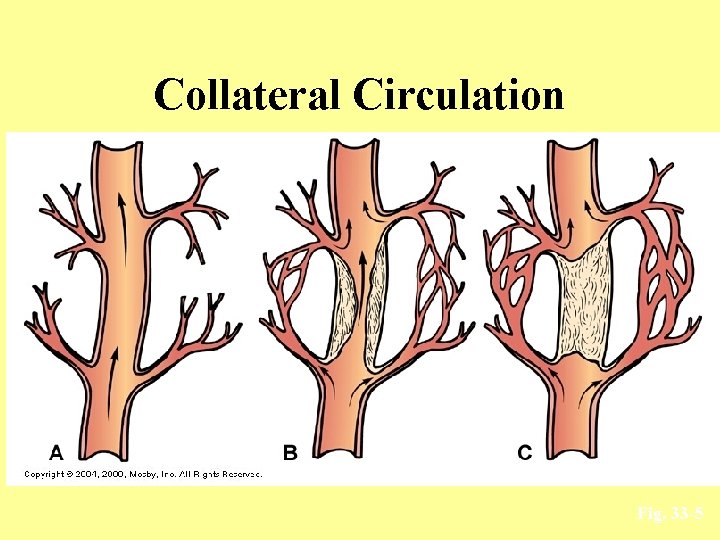
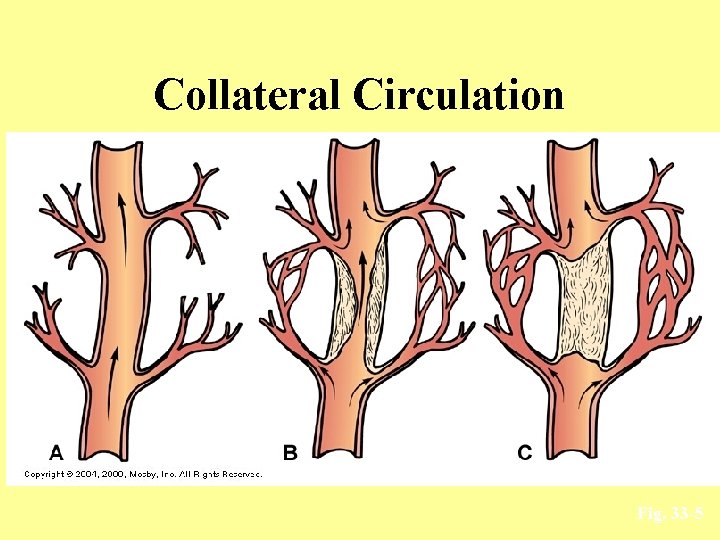
Collateral Circulation Fig. 33 -5
Risk Factors for Coronary Artery Disease • Risk factors can be divided: – Unmodifiable risk factors – Modifiable risk factors
Risk Factors for Coronary Artery Disease • Unmodifiable risk factors: – Age – Gender – Ethnicity – Genetic predisposition
Risk Factors for Coronary Artery Disease • Modifiable risk factors: – Elevated serum lipids – Hypertension – Smoking – Obesity – Physical inactivity – Diabetes mellitus – Stressful lifestyle
Risk Factors for Coronary Artery Disease • Health Promotion – Identification of high-risk persons – Management of high-risk persons • Risk factor modification – Physical fitness – Health education in schools – Nutrition (weight control, ↓ fat, ↓ chol intake) – Cholesterol-lowering medications
Types of Angina • Results when the lack of oxygen supply is temporary and reversible • Types of Angina – Stable Angina – Prinzmetal Angina – Unstable Angina
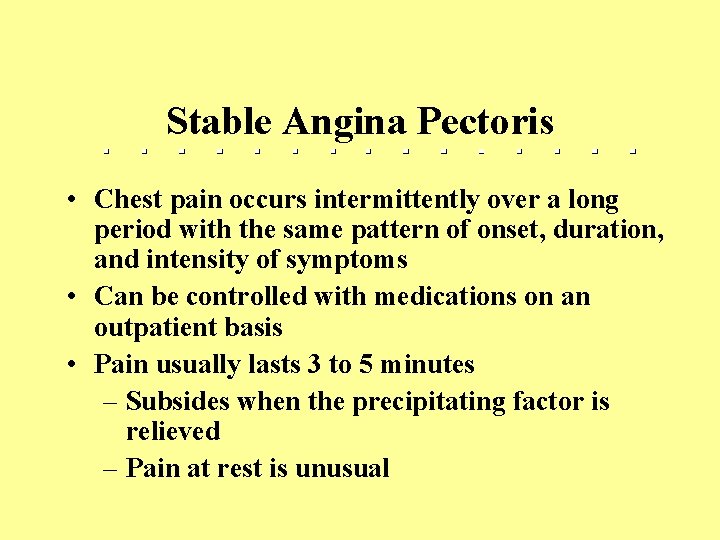
Stable Angina Pectoris • Chest pain occurs intermittently over a long period with the same pattern of onset, duration, and intensity of symptoms • Can be controlled with medications on an outpatient basis • Pain usually lasts 3 to 5 minutes – Subsides when the precipitating factor is relieved – Pain at rest is unusual
Silent Ischemia
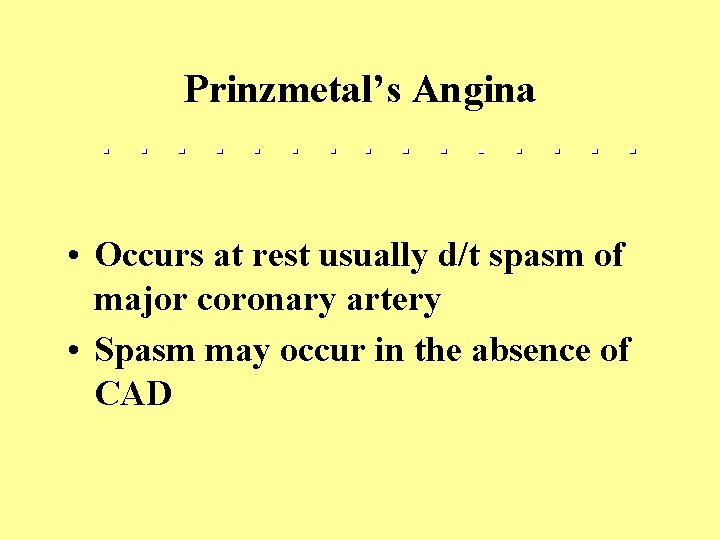
Prinzmetal’s Angina • Occurs at rest usually d/t spasm of major coronary artery • Spasm may occur in the absence of CAD
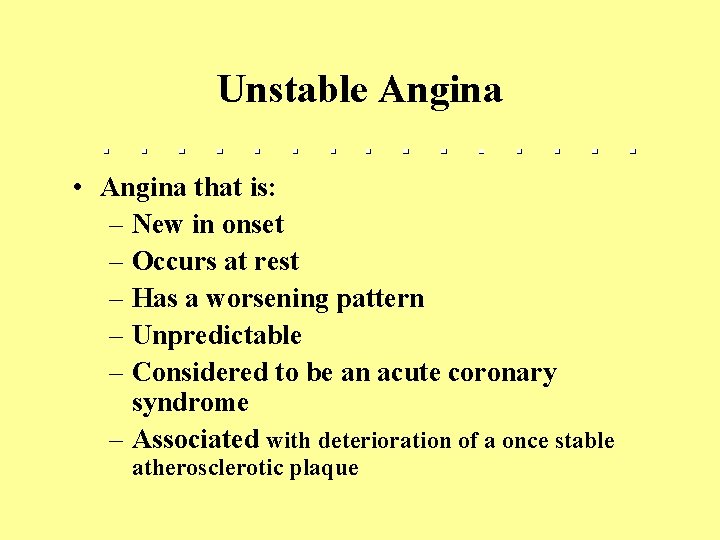
Unstable Angina • Angina that is: – New in onset – Occurs at rest – Has a worsening pattern – Unpredictable – Considered to be an acute coronary syndrome – Associated with deterioration of a once stable atherosclerotic plaque
Clinical Manifestations Angina • Chest pain or discomfort (d/t ischemia) – A strange feeling, pressure, or ache in the chest – Constrictive, squeezing, heaving, choking, or suffocating sensation – Indigestion, burning
However • Up to 80% of patients with myocardial ischemia are asymptomatic • Associated with diabetes mellitus and hypertension
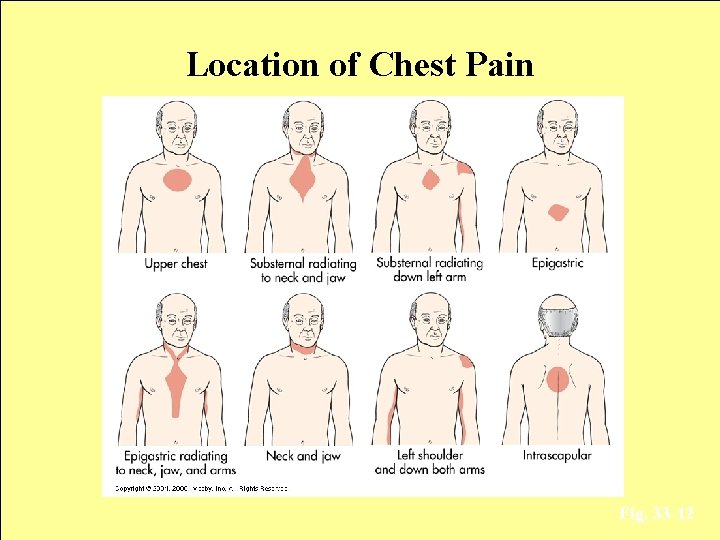
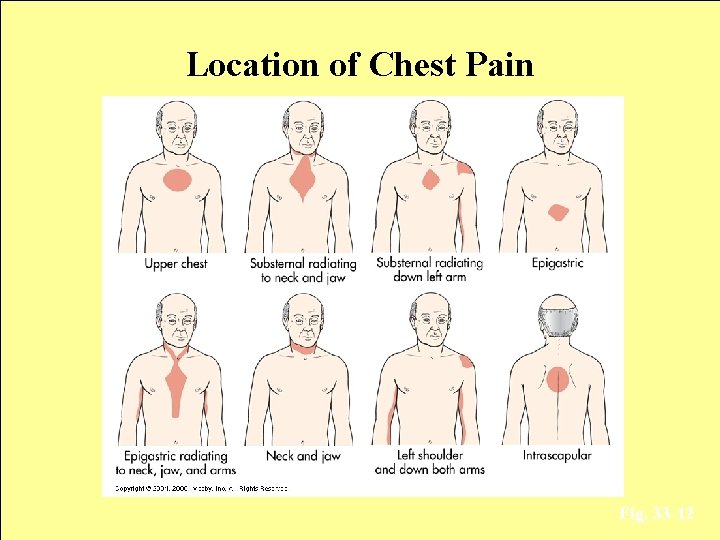
Location of Chest Pain Fig. 33 -12
Diagnostic Studies Angina • • ECG Coronary angiography Cardiac markers (CK MB, Troponin) Treadmill exercise testing (stress test) Serum lipid levels C-reactive protein (CRP) Nuclear imaging
Collaborative Care Angina • Treatment for stable angina: – oxygen demand and/or oxygen supply – Nitrate therapy – Stent placement
Collaborative Care Angina • Treatment for stable angina: – Percutaneous coronary intervention – Atherectomy – Laser angioplasty – Myocardial revascularization (CABG)
Collaborative Care Angina • Drug Therapy – Antiplatelet aggregation therapy • Aspirin: drug of choice (for MI prevention) • First line of treatment for angina
Collaborative Care Angina • Drug Therapy – Nitrates • 1 st line therapy for treatment of acute anginal symptoms • Dilation of vessels
Collaborative Care Angina • Drug Therapy – -Adrenergic blockers – Calcium channel blockers
Collaborative Care Angina • Percutaneous coronary intervention – Surgical intervention alternative – Performed with local anesthesia – Ambulatory 24 hours after the procedure
Collaborative Care Angina • Stent placement – Used to treat abrupt or threatened abrupt closure and restenosis following PCI
Collaborative Care Angina • Atherectomy – The plaque is shaved off using a type of rotational blade – Decreases the incidence of abrupt closure as compared with PCI
Collaborative Care Angina • Laser angioplasty – Performed with a catheter containing fibers that carry laser energy – Used to precisely dissolve the blockage
Collaborative Care Angina • Myocardial revascularization (CABG) – Primary surgical treatment for CAD – Patient with CAD who has failed medical management or has advanced disease is considered a candidate
Clinical Manifestations Myocardial Infarction • Pain – Severe, immobilizing chest pain not relieved by rest, position change, or nitrate administration • The hallmark of an MI
Clinical Manifestations • Acute Coronary Syndrome (ACS) – Develops when the oxygen supply is prolonged and not immediately reversible
Clinical Manifestations • ACS encompasses: – Unstable angina – Myocardial infarction (MI)
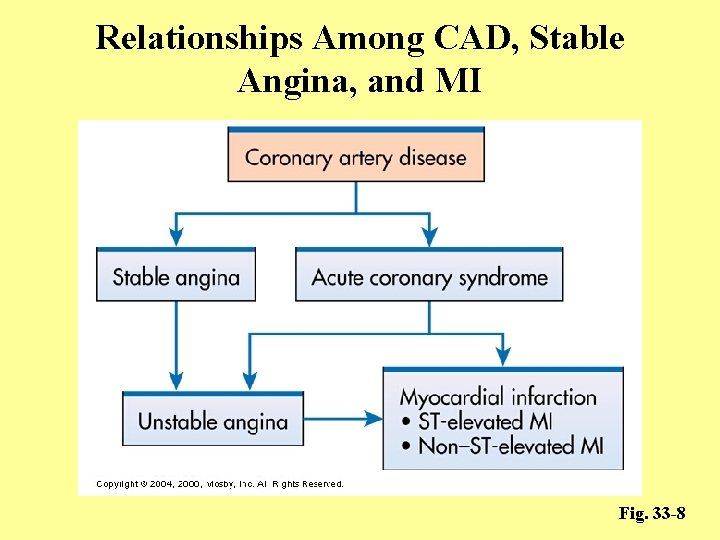
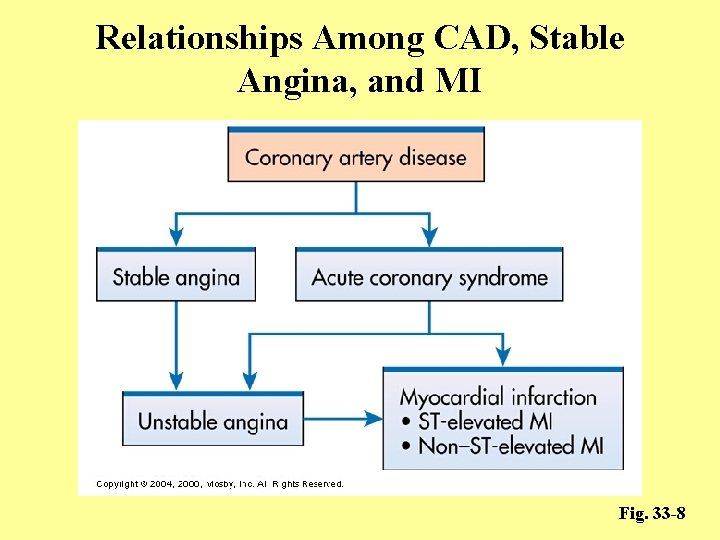
Relationships Among CAD, Stable Angina, and MI Fig. 33 -8
 Coronary artery disease
Coronary artery disease Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Acute coronary syndrome
Acute coronary syndrome Global registry of acute coronary events
Global registry of acute coronary events Sircumflex
Sircumflex Right atrioventricular valve
Right atrioventricular valve Mesenteric artery origin
Mesenteric artery origin Coronary heart disease
Coronary heart disease Coronary steal syndrome
Coronary steal syndrome Antianginal drugs classification
Antianginal drugs classification An acute highly contagious viral disease
An acute highly contagious viral disease Acute radiation syndrome
Acute radiation syndrome Acute aortic syndrome
Acute aortic syndrome Communicable disease and non communicable disease
Communicable disease and non communicable disease Nursing diagnosis of adrenal tumor
Nursing diagnosis of adrenal tumor Coronary sulcus
Coronary sulcus Trabeculae carinae
Trabeculae carinae Coronary personality
Coronary personality Chordae tendineae
Chordae tendineae Ali sepahdari
Ali sepahdari Cardiac plexus
Cardiac plexus Coronary perfusion pressure
Coronary perfusion pressure Crux cordis
Crux cordis Great cardiac vein
Great cardiac vein Pk papyrus covered coronary stent system
Pk papyrus covered coronary stent system Worm like amphibian
Worm like amphibian Intracapsular but extrasynovial
Intracapsular but extrasynovial Coronary blood flow
Coronary blood flow Anemia or hypoproteinemia will ______ blood viscosity.
Anemia or hypoproteinemia will ______ blood viscosity. Mesa coronary calcium score
Mesa coronary calcium score Ischemic heart disease
Ischemic heart disease Com
Com Cardiac cycle animation
Cardiac cycle animation Coronary circulation of heart
Coronary circulation of heart Mesa coronary calcium score
Mesa coronary calcium score Spider view cag
Spider view cag Coronary calcium score guidelines
Coronary calcium score guidelines Qfr coronary
Qfr coronary Coronary sinus
Coronary sinus Pk papyrus stent
Pk papyrus stent Sinusoid anatomy
Sinusoid anatomy Dr eter
Dr eter