Radiation Injury Critical Care Acute radiation syndrome ARS
- Slides: 17
Radiation Injury: Critical Care Acute radiation syndrome (ARS) is an acute illness caused by irradiation of the whole body (or a significant portion of it). In general, the higher the dose the greater the severity of early effects and the greater the possibility of late effects. Depending on dose, the following syndromes can manifest:
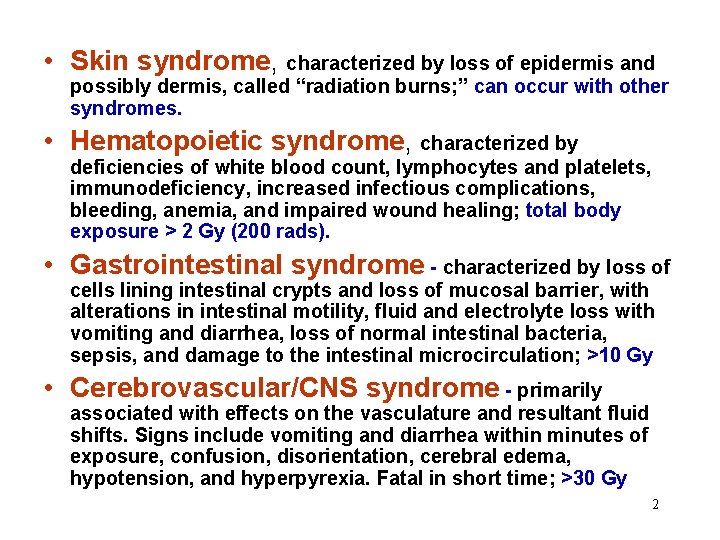
• Skin syndrome, characterized by loss of epidermis and possibly dermis, called “radiation burns; ” can occur with other syndromes. • Hematopoietic syndrome, characterized by deficiencies of white blood count, lymphocytes and platelets, immunodeficiency, increased infectious complications, bleeding, anemia, and impaired wound healing; total body exposure > 2 Gy (200 rads). • Gastrointestinal syndrome - characterized by loss of cells lining intestinal crypts and loss of mucosal barrier, with alterations in intestinal motility, fluid and electrolyte loss with vomiting and diarrhea, loss of normal intestinal bacteria, sepsis, and damage to the intestinal microcirculation; >10 Gy • Cerebrovascular/CNS syndrome - primarily associated with effects on the vasculature and resultant fluid shifts. Signs include vomiting and diarrhea within minutes of exposure, confusion, disorientation, cerebral edema, hypotension, and hyperpyrexia. Fatal in short time; >30 Gy 2
Acute Radiation Syndrome: Exposure Less Than 2 Gy (200 rad) Nausea and vomiting due to radiation are seldom experienced unless exposure is at least 0. 75 Gy. Patients without symptoms in 24 hours will most certainly have had less than 0. 75 Gy of whole-body exposure. Hospitalization is generally unnecessary if exposure is less than 2 Gy (200 rads). Management of ARS (dose less than 2 Gy): • Observation and frequent CBC with differential. • Outpatient management may be appropriate. • Provide instructions regarding home care. 3
Acute Radiation Syndrome: Exposure Greater than 2 Gy (200 rads) • Prevention and treatment of infections. • Stimulation of hematopoiesis (use of growth factors, i. e. , GCSF, GMCSF, interleukin 11). • Stem cell transfusions: cord blood, peripheral blood, or bone marrow. Platelet transfusions if bleeding occurs or if platelet count too low. • Psychological support. • Observe carefully for erythema, hair loss, skin injury, mucositis, parotitis, weight loss, and/or FEVER. • Consultation with experts in radiation accident management is encouraged. 4
Hematopoietic Syndrome: • Prodromal phase: nausea, vomiting and anorexia within a few hours at the higher dose levels, lasts 24 to 48 hours • Latent Phase: lasts a few days to 2 -3 weeks depending on dose. Exhibits lymphocyte depression, and gradual decline of neutrophil and platelet counts • Bone Marrow Depression Phase: Infection and hemorrhage can occur when white cell and platelet become critically low • Depending on exposure, Hematopoietic support can become critical within several days to three weeks 5
Chernobyl: A Harsh Lesson • At Chernobyl, some victims received bone marrow that was HLA matched or partially matched. However, donor marrows were difficult to obtain in adequate numbers. • After exposure to between 2 to 16 Gy, 28 of 34 service personnel died of acute bone-marrow failure, GVHD, or gastro-intestinal infection. • Human umbilical cord blood, now considered an excellent source of hematopoietic stem cells, was not used at Chernobyl. 6
Bone Marrow Transplantation: practical limitations and clinical hurdles • Finding matched donors for numerous casualties on short notice • Rejection of donor marrow by residual immune functions • Graft Versus Host Disease (GVHD): transplanted cells attack the host • Increased risk of infection through immunosuppression. 7
Cord Blood for Hematopoietic Syndrome: Benefits • • • Greater genetic diversity and availability Reduced need for HLA-matching Less prone to GVHD, or host rejection Reduced need for immunosuppression Extensive clincial experience (for hematopoietic restoration following radiation and/or chemo for cancer) • Easy to collect, analyze, store, and use 8
Unique Points Single units of cord blood engraft more slowly than bone marrow from an HLA-matched bone marrow donor, however… • Cord blood’s speed of engraftment and event-free success is directly related to the number of transplanted nucleated cells. • Pooling unmatched units of cord blood increases densities of nucleated blood cells, primitive (Berashis) stem cells, CD 34, CD 117, and GPA cells, and increases mitotic activity • Without raising risks of rejection, pooling unmatched cord blood substancially reduces reactivity of CB responder cells to fresh allogenic CB stimulator cells, likewise reducing CB responder cell reactivity to host stimulator cells (GVHD) • In addition to offering replacement of hematopoietic systems destroyed by radiation, cord blood-derived hematopoietic cells co-exist with surviving marrow cells, encouraging endogenous hematopoietic recovery, while providing transitional support 9
Human evidence suggestive of the previous points “Four patients with advanced solid tumors were treated by means of high-dose chemotherapy and HLA-mismatched and unrelated multi-cord blood transfusion. Of these patients, three achieved complete remission and one achieved a partial remission. Little or no graft vs. host disease (GVHD) was observed. These results suggest the possibility that HLA-mismatched and unrelated multi-cord blood transfusion may engraft with little or no GVHD and hasten recovery from marrow suppression. ” Shen B. -J. et. al. , Blood Cells Volume 20, Issue 2 -3 , 1994, Pages 285 -292 10
Cord Blood –Treated Radiation Casualty Japanese Tokaimura Facility “Although the transplanted cord blood cells engrafted, the patient’s bone marrow functions eventually returned two months later. During this period, there existed a mixed chimerism between donor cells and recipient cells. ” From: Radiation-Accident Preparedness: The Clinical Care of Victims, Fourth International REAC/TS Conference on the Medical Basis for Radiation Accident Preparedness, March 2001, Orlando FL 11
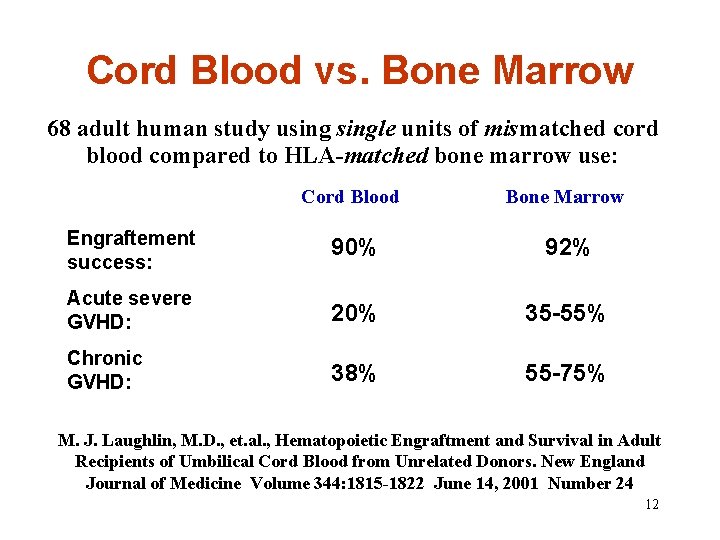
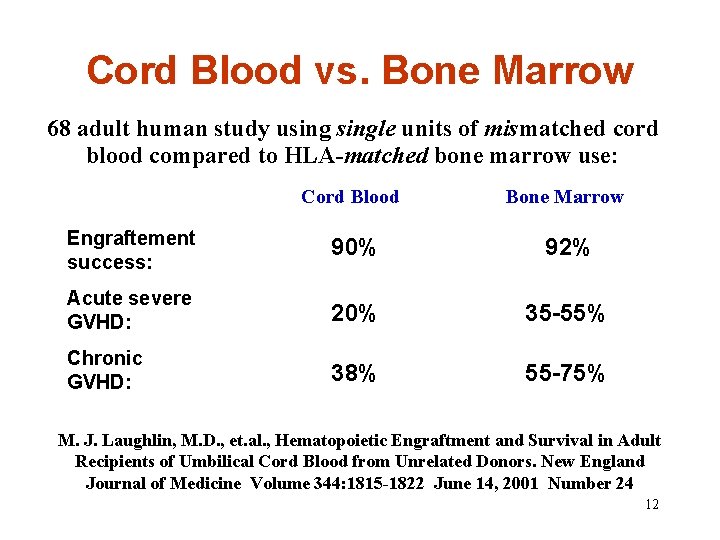
Cord Blood vs. Bone Marrow 68 adult human study usingle units of mismatched cord blood compared to HLA-matched bone marrow use: Cord Blood Bone Marrow Engraftement success: 90% 92% Acute severe GVHD: 20% 35 -55% Chronic GVHD: 38% 55 -75% M. J. Laughlin, M. D. , et. al. , Hematopoietic Engraftment and Survival in Adult Recipients of Umbilical Cord Blood from Unrelated Donors. New England Journal of Medicine Volume 344: 1815 -1822 June 14, 2001 Number 24 12
In Conclusion: “In the event of large-scale exposure, some persons are likely to be exposed to a dose of total-body radiation (approximately 6 to 15 Gy) that would result in death from bone marrow failure without other lifethreatening complications. The only effective treatment for bone marrow failure caused by lethal doses of radiation is hematopoieticcell transplantation. ” Continued… 13
“Units of cryopreserved umbilical-cord blood can be identified in registries and made available for transplantation within days. When umbilical-cord blood is used, less stringent HLA matching is required. A bank of approximately 200, 000 units could provide 90 percent of the population with cord blood matched at four or five of six HLA loci — the type of matches most commonly used in cord-blood transplantation. ” Continued… 14
“Shortening the turnaround time for searching donor registries, providing an umbilical-cord–blood bank of appropriate size, and developing a consortium of transplantation programs should be part of the plan for national preparedness for radiological disaster. ” Stephen J. Forman, M. D. Lawrence D. Petz, M. D. Major Radiation Exposure, Letters; New England Journal of Medicine, Volume 347: 944 -947 September 19, 2002 Number 12 15
Referenced Literature: Ricks RC, Berger ME, O’Hara FM Jr. , Radiation-Accident Preparedness: The Clinical Care of Victims, Fourth International REAC/TS Conference on the Medical Basis for Radiation Accident Preparedness, March 2001, Orlando FL Rubinstein, et. al. , Outcomes among 562 Recipients of Placental-Blood Transplants from unrelated donors. New England Journal of Medicine, Vol. 339, Nov. 26 th, 1998, no. 22 1565 -77 Laughlin, et. al. , Hematopoietic Engraftment and survival in adult recipients of umbilical cord blood from unrelated donors. New England Journal of Medicine Volume 344: 1815 -1822 June 14, 2001 Number 24 Ende, et. al. , Potential effectiveness of stored cord blood (non-frozen) for emergency use. The Journal of Emergency Medicine Vol 14, no. 6, pp 673 -677 (1996) Ende, et. al. , Pooled umbilical cord blood as a possible universal donor for marrow reconstitution and use in nuclear accidents. Life Sciences 69 (2001) 1531 -1539` Shen et. al. , Unrelated, HLA-mismatched multiple human umbilical cord blood transfusion in four cases with advanced solid tumors: Initial studies. Blood Cells Volume 20, Issue 2 -3 , 1994, Pages 285 -292 16
Ende et. al. , The feasibility of using blood bank-stored (4°C) cord blood, unmatched for HLA for marrow transplantation. Am J. Clin. Pathol. (1999) 111; 6: 773 -781. Gluckman, Hematopoietic Stem-Cell Transplants using umbilical-cord blood, The New England Journal of Medicine, Vol. 344, No. 24; June 14, 2001, pg. 1860 -61 Ende, et. al. , Murine survival of lethal irradiation with the use of human umbilical cord blood. Life Sci. 51: 1249 -1253. (1992) Ende, N. Use of human umbilical cord blood for stem-cell transplantation (HLAmatched, unmatched. Clinical, ethical, and legal aspects). In: Hematopoietic Stem Cells. (1995) Edited by: D. Levitt and Mertelsmann. 333 -347. Ende et. al. , The effect of human cord blood on SJL/J mice after chemoablation and irradiation and its possible clinical significance Immunological Investigations Volume 24, Issue 6 , November 1995, Pages 999 -1012 Gluckman et. al. , Clinical applications of stem cell transfusion from cord blood and rationale for cord blood banking Bone Marrow Transplantation Volume 9, Supplement 1 , 1992, Pages 114 -117 Guidance for Radiation Accident Management: Radiation Emergency Assistance Center/Training Site REAC/TS 17
 Pagwash
Pagwash Acute radiation syndrome
Acute radiation syndrome Critical semi critical and non critical instruments
Critical semi critical and non critical instruments Semi-critical
Semi-critical Examples of intentional injury
Examples of intentional injury Aki aki aki
Aki aki aki Acute coronary syndrome
Acute coronary syndrome Firas mussa
Firas mussa Primary secondary and tertiary care
Primary secondary and tertiary care Nursing care plan for head injury slideshare
Nursing care plan for head injury slideshare Acute care collaboration
Acute care collaboration Rcp acute care toolkit
Rcp acute care toolkit Hepatitis a incubation period
Hepatitis a incubation period Critical reading meaning
Critical reading meaning Poema ars
Poema ars A.r.s. § 33-1324
A.r.s. § 33-1324 Vojtina jelentése
Vojtina jelentése Urbs declinazione
Urbs declinazione