Dr Hlya KANKAYA Coronary artery disease CAD Coronary






- Slides: 48
Dr. Hülya KANKAYA
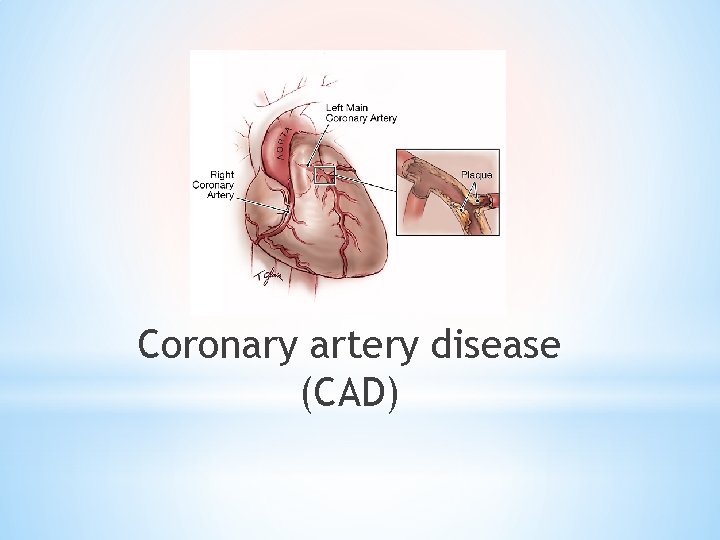
Coronary artery disease (CAD)
* * Coronary artery disease (CAD) is the most common type of heart disease. * Coronary artery disease (CAD) is the single most common cause of death in the developed world, responsible for about 1 in every 5 deaths. Chronic coronary artery disease (CAD) is estimated to affect 16. 8 million people in the United States; of these, * 9. 8 million have angina pectoris * nearly 8 million have had a myocardial infaction (MI)
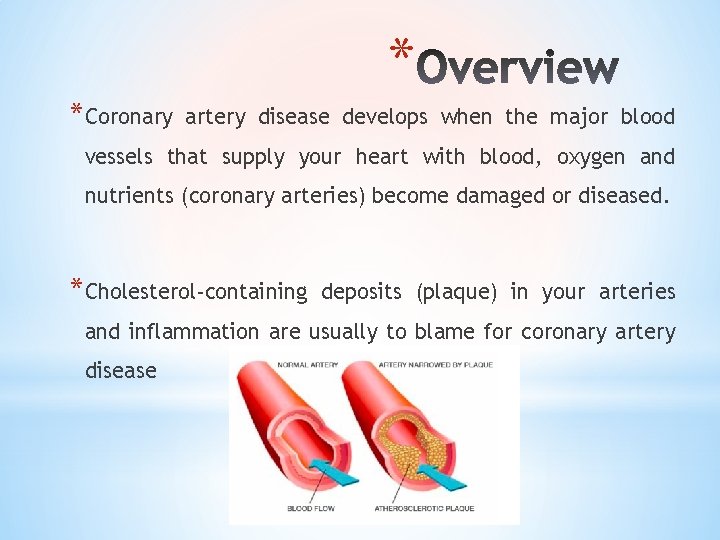
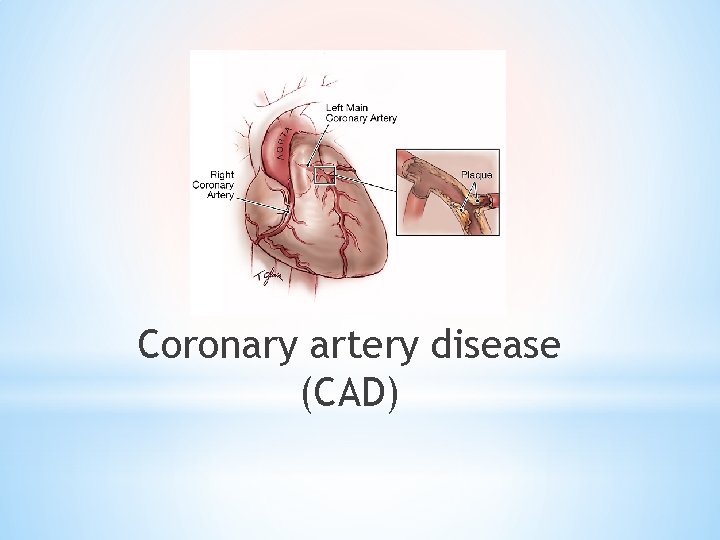
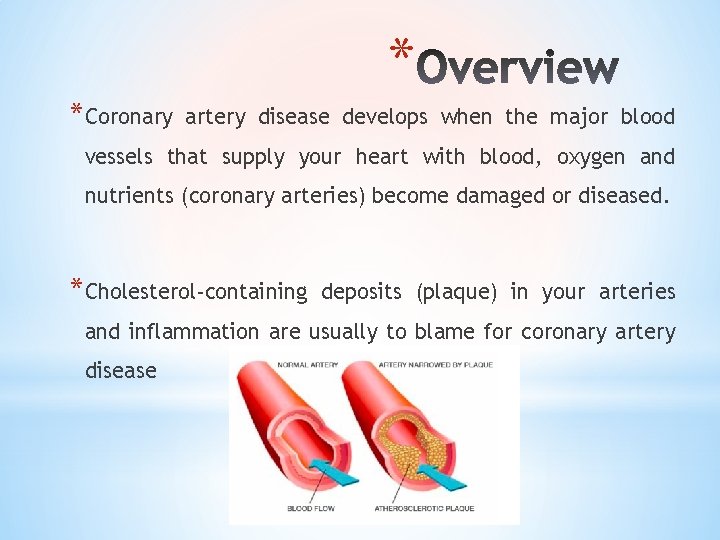
* *Coronary artery disease develops when the major blood vessels that supply your heart with blood, oxygen and nutrients (coronary arteries) become damaged or diseased. *Cholesterol-containing deposits (plaque) in your arteries and inflammation are usually to blame for coronary artery disease
*Coronary artery disease (CAD) causes impaired blood flow in the arteries that supply blood to the heart.
*The most common cause of CAD is vascular injury with cholesterol plaque buildup in the arteries, known as atherosclerosis. *Reduced blood flow occurs when one or more of these arteries becomes partially or completely blocked.

* CAD happens when the arteries that supply blood to heart muscle become hardened and narrowed. This is due to the buildup of cholesterol and other material, called plaque, on their inner walls. * This buildup is called atherosclerosis. * As it grows, less blood can flow through the arteries. As a result, the heart muscle can't get the blood or oxygen it needs. * This can lead to chest pain (angina) or a heart attack. * Most heart attacks happen when a blood clot suddenly cuts off the hearts' blood supply, causing permanent heart damage.
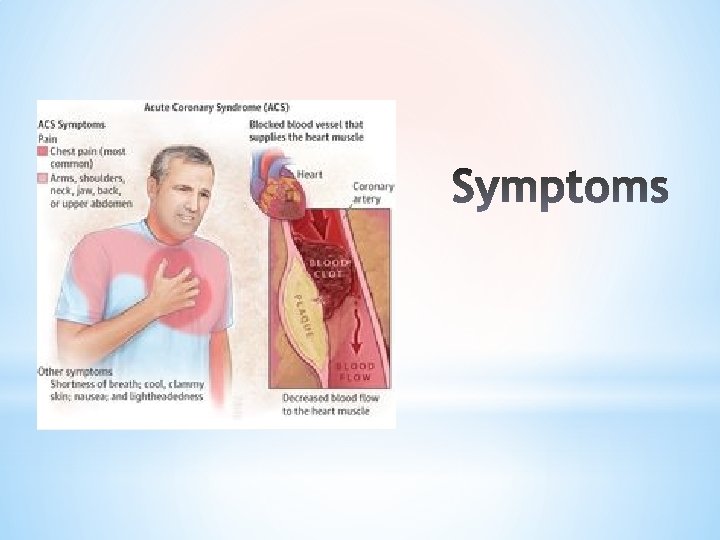
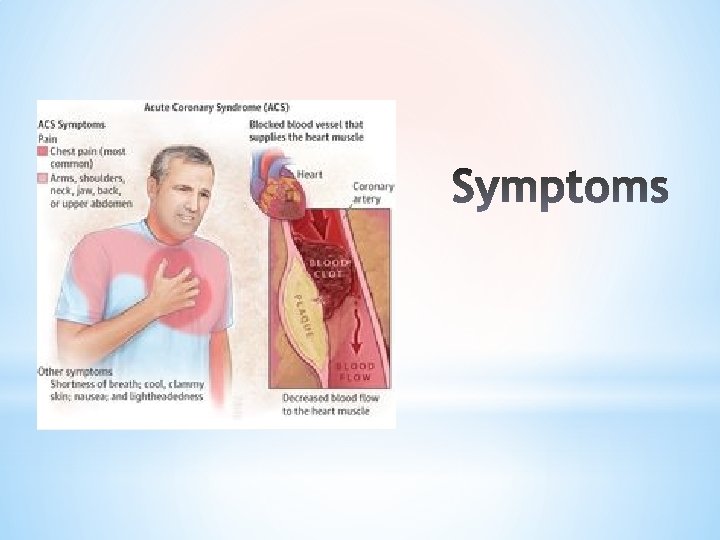
*At first, the decreased blood flow may not cause any coronary artery disease symptoms. *As plaque continues to build up in the coronary arteries, however, maybe to develop coronary artery disease signs and symptoms.
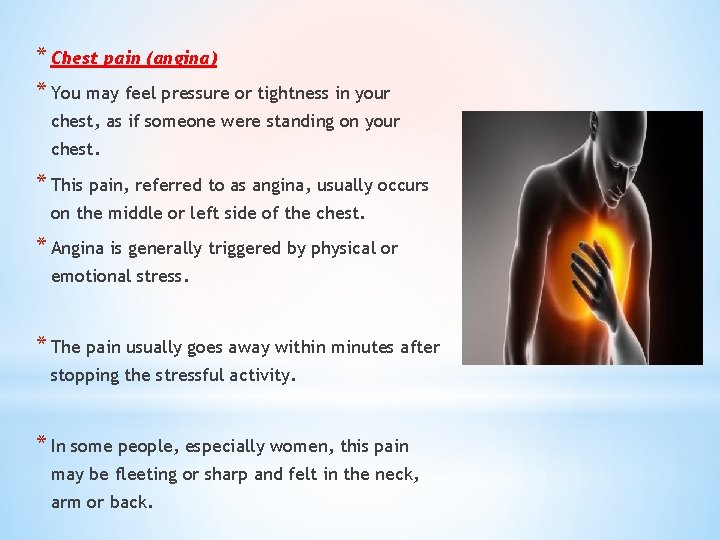
* Chest pain (angina) * You may feel pressure or tightness in your chest, as if someone were standing on your chest. * This pain, referred to as angina, usually occurs on the middle or left side of the chest. * Angina is generally triggered by physical or emotional stress. * The pain usually goes away within minutes after stopping the stressful activity. * In some people, especially women, this pain may be fleeting or sharp and felt in the neck, arm or back.
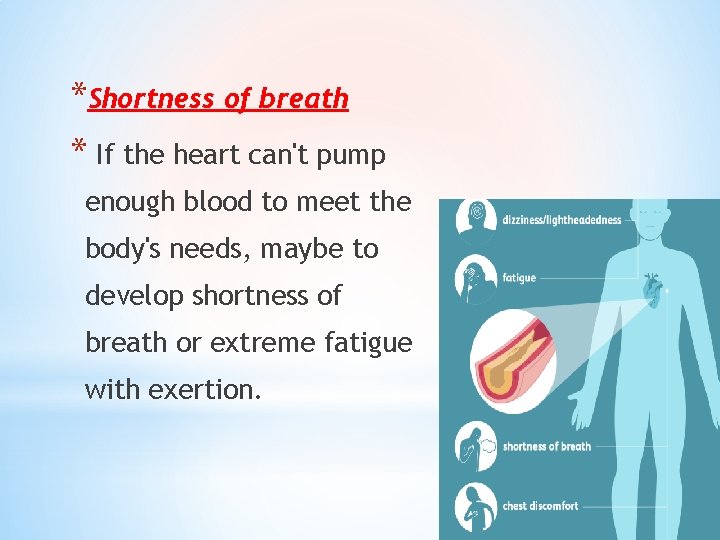
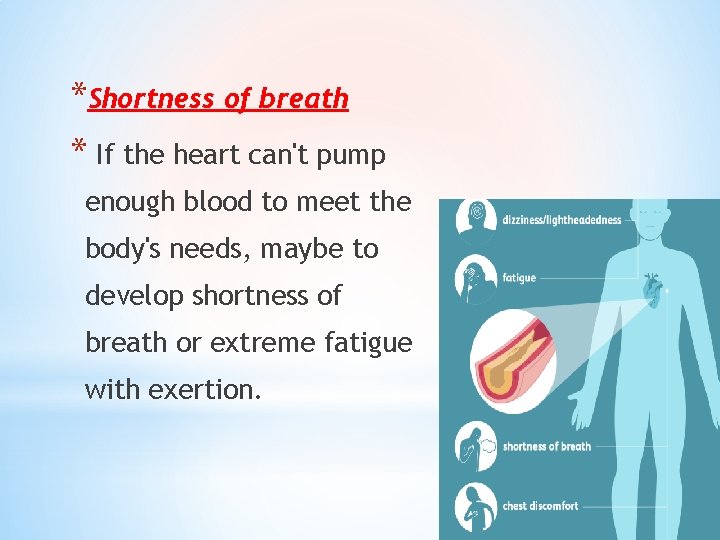
*Shortness of breath * If the heart can't pump enough blood to meet the body's needs, maybe to develop shortness of breath or extreme fatigue with exertion.
*Heart attack *A completely blocked coronary artery will cause a heart attack. *The classic signs and symptoms of a heart attack include crushing pressure in the chest and pain in the shoulder or arm, sometimes with shortness of breath and sweating. *Excessive weight *Genetic factors *Certain occupations which lead to injury and overuse of joints *Increasing age
*Women are somewhat more likely than men are to experience less typical signs and symptoms of a heart attack, such as neck or jaw pain. *Sometimes a heart attack occurs without any apparent signs or symptoms.

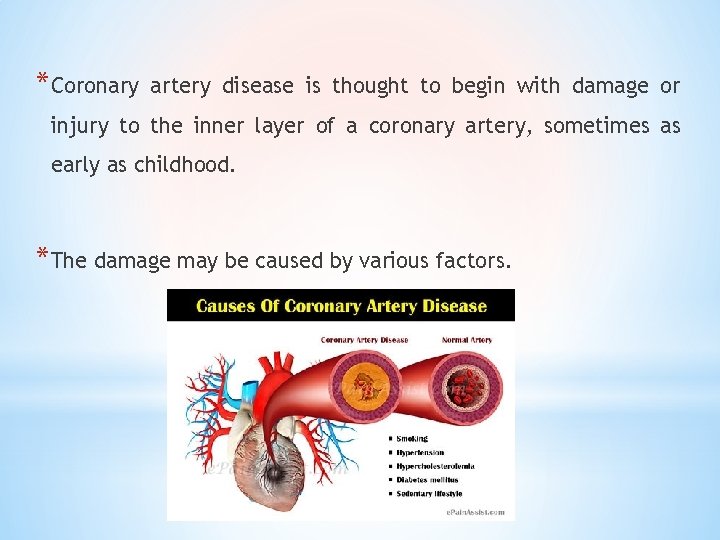
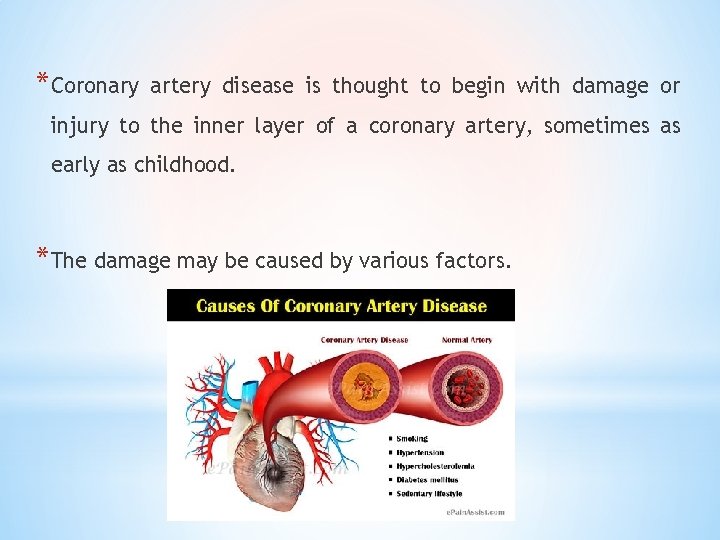
*Coronary artery disease is thought to begin with damage or injury to the inner layer of a coronary artery, sometimes as early as childhood. *The damage may be caused by various factors.
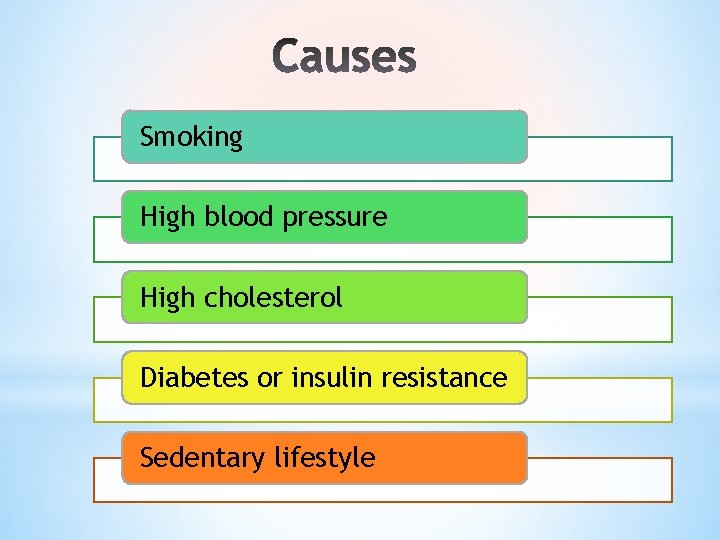
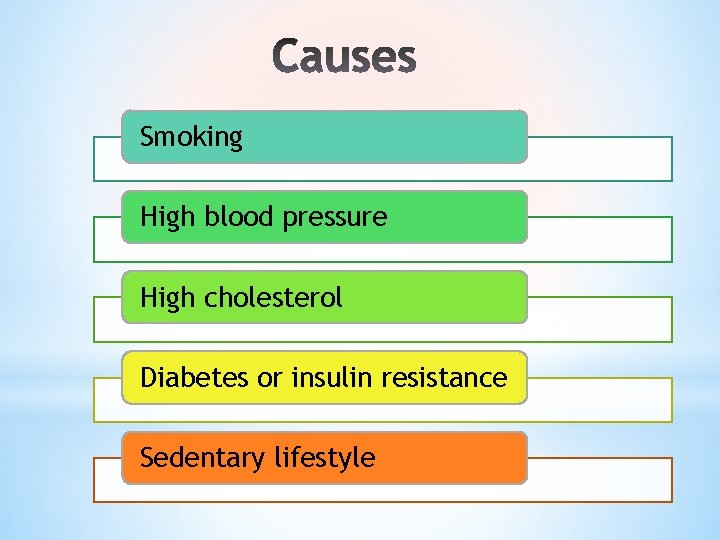
Smoking High blood pressure High cholesterol Diabetes or insulin resistance Sedentary lifestyle
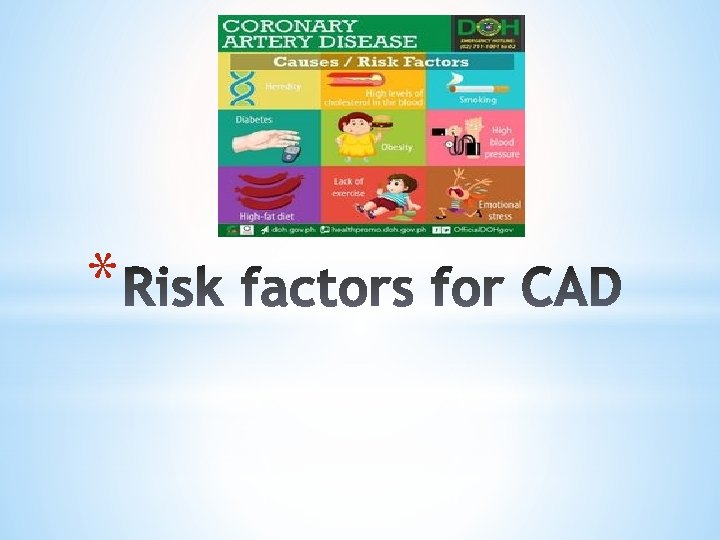
* The most important indicators for cardiac risk are those of a person's personal health history. These include: * Age * Sex * Family history * Weight * Cigarette smoking * Blood pressure * High blood cholesterol levels * Diet, obesity * Exercise, physical activity * Diabetes * High stress

* high blood pressure * high blood cholesterol levels * tobacco smoking * insulin resistance/hyperglycemia/diabetes mellitus * obesity * inactivity * unhealthy eating habits * obstructive sleep apnea * emotional stress * excessive alcohol consumption * history of preeclampsia during pregnancy
*The risk for CAD also increases with age. *Based on age alone as a risk factor, men have a greater risk for the disease beginning at age 45 and women have a greater risk beginning at age 55. *The risk for coronary artery disease is also higher if you have a family history of the disease.
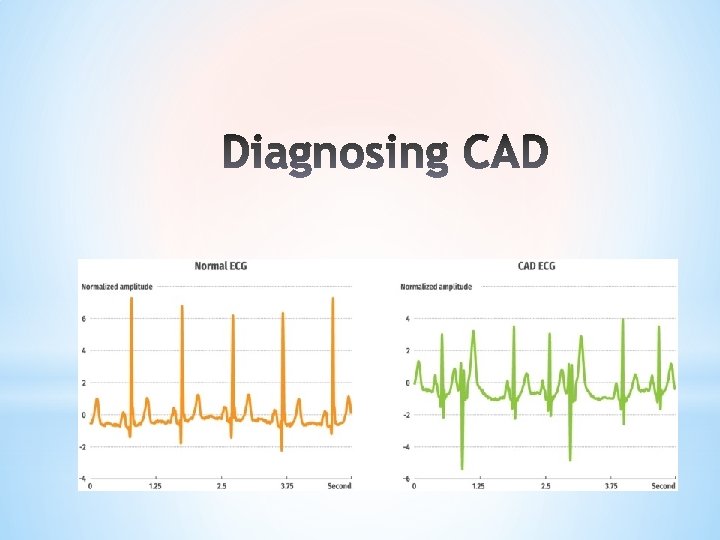
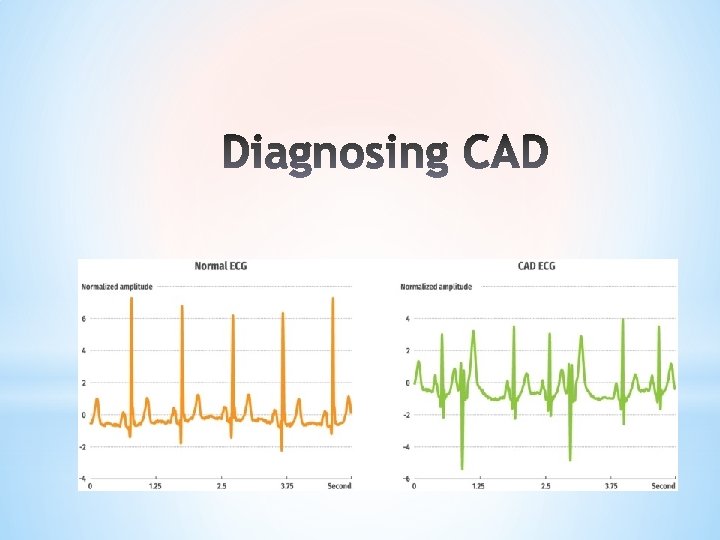
*Diagnosing CAD requires a review of your medical history, a physical examination, and other medical testing.
*Electrocardiogram *Echocardiogram *Stress test *Cardiac catheterization (left heart catheterization) *Heart CT scan
*Some other tests that may be used to assess cardiac risk include: *High-sensitivity C-reactive protein (hs-CRP) *Lipoprotein A (Lp(a)) *Urine albumin (microalbumin) *Cystatin C *Fibrinogen

*It’s important to reduce or control the risk factors and seek treatment to lower the chance of a heart attack or stroke, if it is diagnosed with CAD. *Treatment also depends on the current health condition, risk factors, and overall wellbeing.
*Lifestyle changes can also reduce your risk of heart disease and stroke. *quit smoking tobacco *reduce or stop the consumption of alcohol *exercise regularly *lose weight to a healthy level *eat a healthy diet (low in fat, low in sodium)
*If the condition doesn’t improve with lifestyle changes and medication, the doctor may recommend a procedure to increase blood flow to the heart. These procedures may be: *balloon angioplasty *coronary artery bypass graft surgery *enhanced external counterpulsation
Medical Management of Coronary Artery Disease
*Medications may be needed to help the heart work more efficiently and receive more oxygen-rich blood. *Nitroglycerin
*Nitroglycerin is the most common vasodilator used for acute cases of angina. *It works to dilate or widen the coronary arteries, increasing blood flow to the heart muscle and to relax the veins, lessening the amount of blood that returns to the heart from the body. *This combination of effects decreases the amount of work for the heart.
Nitroglycerin comes in tablet or spray form. *Nitroglycerin must be kept in a dark container. *Keep it away from heat or moisture. *Check the expiration date on the container. *Once the container is opened, it must be replaced every 6 months.
If Angina Occurs. . * If you have been prescribed nitroglycerin and experience angina, stop what you are doing and rest. * Take one nitroglycerin tablet and let it dissolve under your tongue, or if using the spray form, spray it under your tongue. * Wait 5 minutes. * If you still have angina after 5 minutes, call 112 to get emergency help.
*For patients diagnosed with chronic stable angina: *If you experience angina, take one nitroglycerin tablet and let it dissolve under your tongue, repeating every 5 minutes for up to 3 tablets spanning 15 minutes. *If you still have angina after taking 3 doses of nitroglycerin, call 112 to get emergency help.
Use of Aspirin with unstable chest pain: *After you call 1 -1 -2, if you do not have a history of aspirin allergy or bleeding, emergency personnel may advise that you chew one full (325 mg) aspirin slowly. *It's especially effective if taken within 30 minutes of the onset of symptoms.

Chest pain (angina) *When the coronary arteries narrow, the heart may not receive enough blood when demand is greatest — particularly during physical activity. *This can cause chest pain (angina) or shortness of breath.
Heart attack * If a cholesterol plaque ruptures and a blood clot forms, complete blockage of the heart artery may trigger a heart attack. * The lack of blood flow to the heart may damage the heart muscle. * The amount of damage depends in part on how quickly you receive treatment.
Heart failure *If some areas of the heart are chronically deprived of oxygen and nutrients because of reduced blood flow, or if the heart has been damaged by a heart attack, the heart may become too weak to pump enough blood to meet the body's needs. *This condition is known as heart failure.
Abnormal heart rhythm (arrhythmia) *Inadequate blood supply to the heart or damage to heart tissue can interfere with the heart's electrical impulses, causing abnormal heart rhythms.

*The same lifestyle habits that can help treat coronary artery disease can also help prevent it from developing in the first place. *Leading a healthy lifestyle can help keep your arteries strong and clear of plaque.
To improve your heart health; * Stop smoking * Control conditions such as high blood pressure, high cholesterol and diabetes * Stay physically active * Eat a low-fat, low-salt diet that's rich in fruits, vegetables and whole grains * Maintain a healthy weight * Reduce and manage stress
* *Acute Pain *Deficient Knowledge *Anxiety *Risk for Decreased Cardiac Output *Other Possible Nursing Care Plans
* * Instruct patient to notify nurse immediately when chest pain occurs. * Assess and document patient response to medication. * Identify precipitating event, if any: frequency, duration, intensity, and location of pain * Observe for associated symptoms: dyspnea, nausea and vomiting, dizziness, palpitations, desire to micturate. * Evaluate reports of pain in jaw, neck, shoulder, arm, or hand (typically on left side). * Place patient at complete rest during anginal episodes. * Elevate head of bed if patient is short of breath. * Monitor heart rate and rhythm. * Monitor vital signs every 5 min during initial anginal attack. * Stay with patient who is experiencing pain or appears anxious. * Maintain quiet, comfortable environment. Restrict visitors as necessary. * Provide light meals. Have patient rest for 1 hr after meals. * Provide supplemental oxygen as indicated.
* * Discuss pathophysiology of condition. Stress need for preventing and managing anginal attacks. * Review significance of cholesterol levels and differentiate between LDL and HDL factors. Emphasize importance of periodic laboratory measurements. * Encourage avoidance of situations that may precipitate anginal episode (stress, intense physical exertion, large heavy meals especially during bedtime, exposure to extreme temperatures). * Assist patient and/or SO to identify sources of physical and emotional stress and discuss ways that they can be avoided. * Review importance of weight control, cessation of smoking, dietary changes, and exercise. * Encourage patient to follow prescribed reconditioning program; caution to avoid exhaustion.
* *Explain purpose of tests and procedures: stress testing. *Promote expression of feelings and fears. Let patient/SO know these are normal reactions. *Encourage family and friends to treat patient as before. *Tell patient the medical regimen has been designed to limit future attacks and increase cardiac stability. *Administer sedatives, tranquilizers, as indicated.
* * Maintain bed or chair rest in position of comfort during acute episodes. * Monitor vital signs and cardiac rhythm. * Auscultate breath sounds and heart sounds. Listen for murmurs. * Provide for adequate rest periods. Perform self-care activities, as indicated. * Stress importance of avoiding straining down, especially during defecation. * Evaluate mental status, noting development of confusion, disorientation. * Note skin color and presence and quality of pulses * Administer supplemental oxygen as needed.
 Coronary artery disease
Coronary artery disease Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Aortic sinus
Aortic sinus Right atrioventricular valve
Right atrioventricular valve Coronary heart disease
Coronary heart disease Branches of sma
Branches of sma Hemodinamik bozukluklar nedir
Hemodinamik bozukluklar nedir Cad ekg
Cad ekg Lökosit ekstravazasyonu
Lökosit ekstravazasyonu Hülya kankaya
Hülya kankaya Kompleman sistemi
Kompleman sistemi Bharathi viswanathan
Bharathi viswanathan Annulus of vieussens
Annulus of vieussens Dr eter
Dr eter Heart sounds location
Heart sounds location Mesa coronary calcium score
Mesa coronary calcium score Worm like amphibian
Worm like amphibian Coronary perfusion pressure
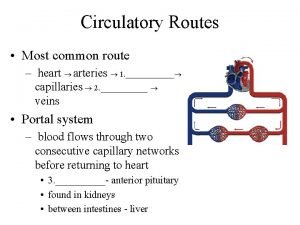
Coronary perfusion pressure Pulmonary trunk
Pulmonary trunk Cardiovascular system crash course
Cardiovascular system crash course Anemia or hypoproteinemia will ______ blood viscosity.
Anemia or hypoproteinemia will ______ blood viscosity. Global registry of acute coronary events
Global registry of acute coronary events Left lung
Left lung Coronary personality
Coronary personality Cag spider view
Cag spider view Acute coronary syndrome
Acute coronary syndrome Anterior aortic sinus
Anterior aortic sinus Papyrus covered stent
Papyrus covered stent Cardiac output animation
Cardiac output animation Ischemic heart disease classification
Ischemic heart disease classification Coronary sinusoids
Coronary sinusoids Coronary calcium score guidelines
Coronary calcium score guidelines Mesa coronary calcium score
Mesa coronary calcium score Coronary ligament
Coronary ligament Coronary steal
Coronary steal Lig hepatoduodenal
Lig hepatoduodenal Coronary sulcus
Coronary sulcus Coronary circulation of heart
Coronary circulation of heart Pk papyrus covered coronary stent system
Pk papyrus covered coronary stent system Coronary groove of heart
Coronary groove of heart Qfr coronary
Qfr coronary Superadded changes in coronary atherosclerosis
Superadded changes in coronary atherosclerosis Coronary blood flow
Coronary blood flow Concepto de cetoacidosis diabetica
Concepto de cetoacidosis diabetica Cad 2002
Cad 2002 Cad has productivity in many firms
Cad has productivity in many firms Wild cad
Wild cad Cadcam orthotics
Cadcam orthotics Cad ingegneria aerospaziale sapienza
Cad ingegneria aerospaziale sapienza