Communityacquired respiratory infections and cardiovascular complications what did



- Slides: 46
Community-acquired respiratory infections and cardiovascular complications: what did we know and what have we learned from the European Respiratory Society (ERS) and American Thoracic Society (ATS) meetings in 2020? Ronald Grossman MD, FRCPC Professor of Medicine University of Toronto MA-PFM-AI-SG-0008 -1 , October 2020 G. GM. AVE. 09. 2010. 0020 1

G. GM. AVE. 09. 2010. 0020 INCIDENCE: HEART COMPLICATIONS 2
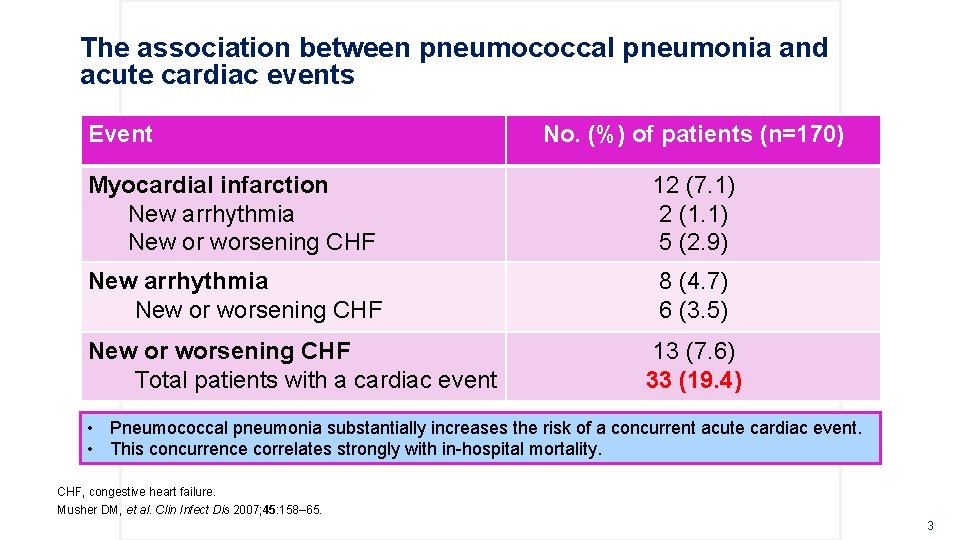
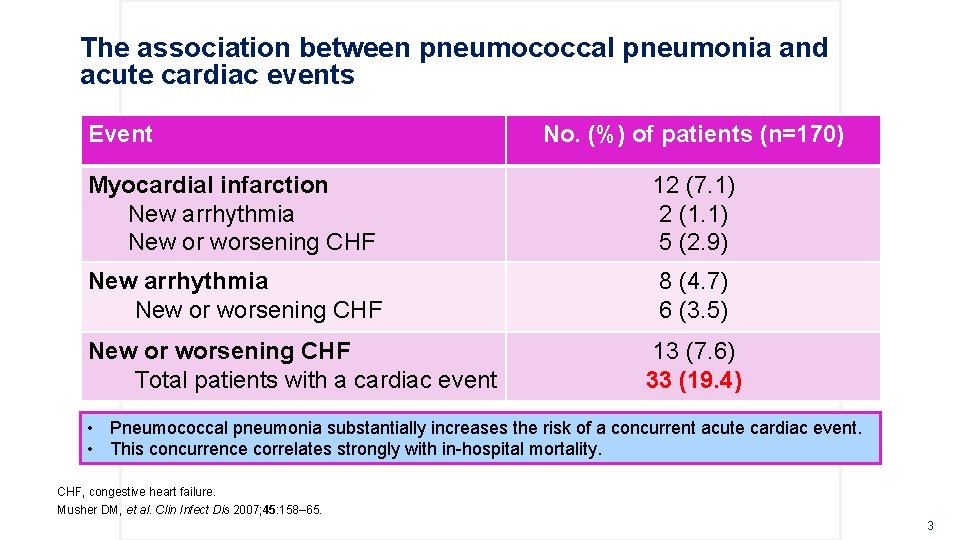
The association between pneumococcal pneumonia and acute cardiac events Event No. (%) of patients (n=170) Myocardial infarction New arrhythmia New or worsening CHF 12 (7. 1) 2 (1. 1) 5 (2. 9) New arrhythmia New or worsening CHF 8 (4. 7) 6 (3. 5) New or worsening CHF Total patients with a cardiac event 13 (7. 6) 33 (19. 4) • Pneumococcal pneumonia substantially increases the risk of a concurrent acute cardiac event. • This concurrence correlates strongly with in-hospital mortality. CHF, congestive heart failure. Musher DM, et al. Clin Infect Dis 2007; 45: 158– 65. G. GM. AVE. 09. 2010. 0020 3
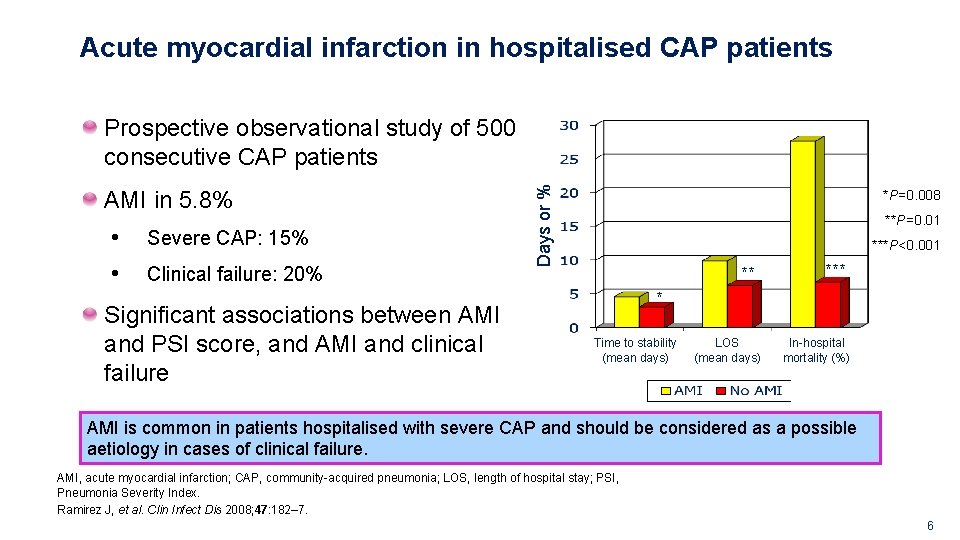
Acute myocardial infarction in hospitalised CAP patients Prospective observational study of 500 consecutive CAP patients enrolled in the CAPO study cohort June 2001 – March 2006 Conducted at VA Medical Center of Louisville, KY, USA CAP, community-acquired pneumonia; CAPO, Community-Acquired Pneumonia Organization. Ramirez J, et al. Clin Infect Dis 2008; 47: 182– 7. G. GM. AVE. 09. 2010. 0020 4
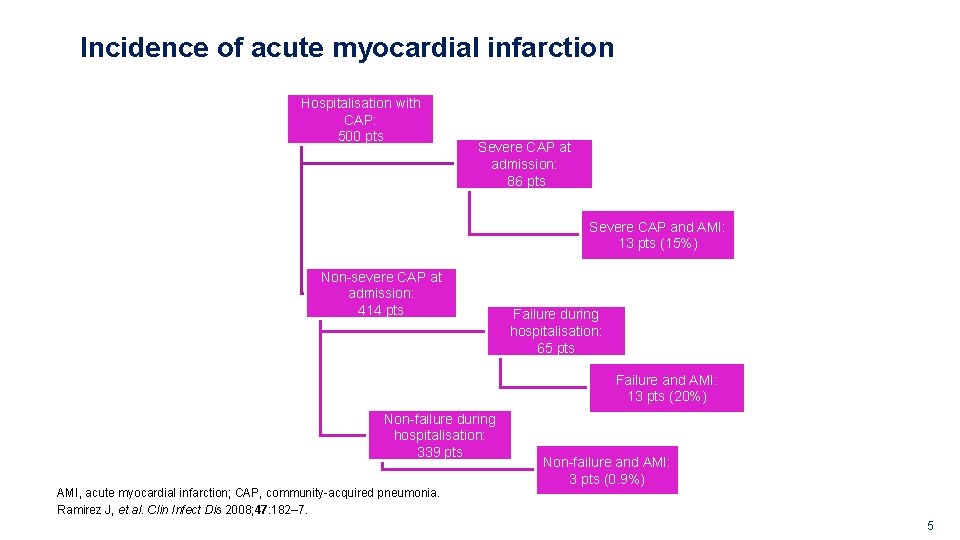
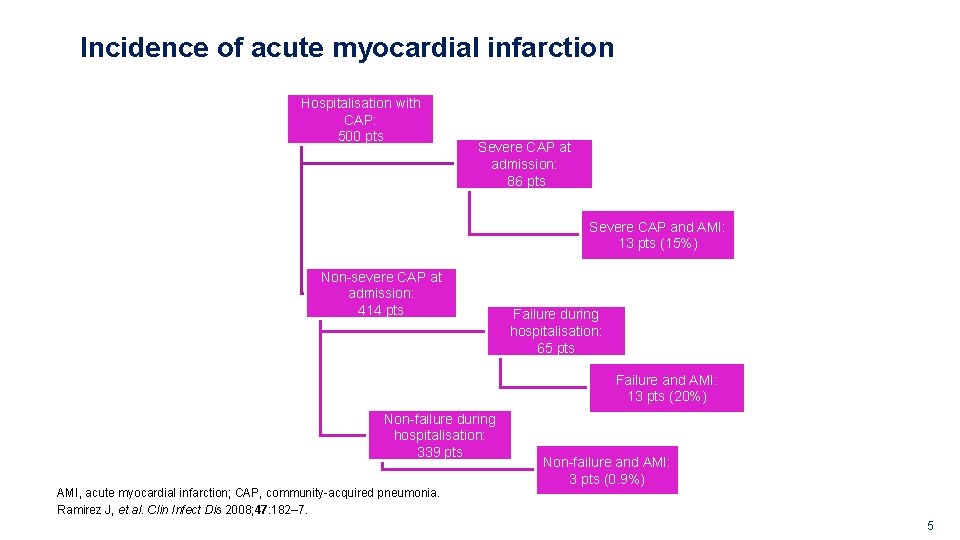
Incidence of acute myocardial infarction Hospitalisation with CAP: 500 pts Severe CAP at admission: 86 pts Severe CAP and AMI: 13 pts (15%) Non-severe CAP at admission: 414 pts Failure during hospitalisation: 65 pts Failure and AMI: 13 pts (20%) Non-failure during hospitalisation: 339 pts AMI, acute myocardial infarction; CAP, community-acquired pneumonia. Ramirez J, et al. Clin Infect Dis 2008; 47: 182– 7. G. GM. AVE. 09. 2010. 0020 Non-failure and AMI: 3 pts (0. 9%) 5
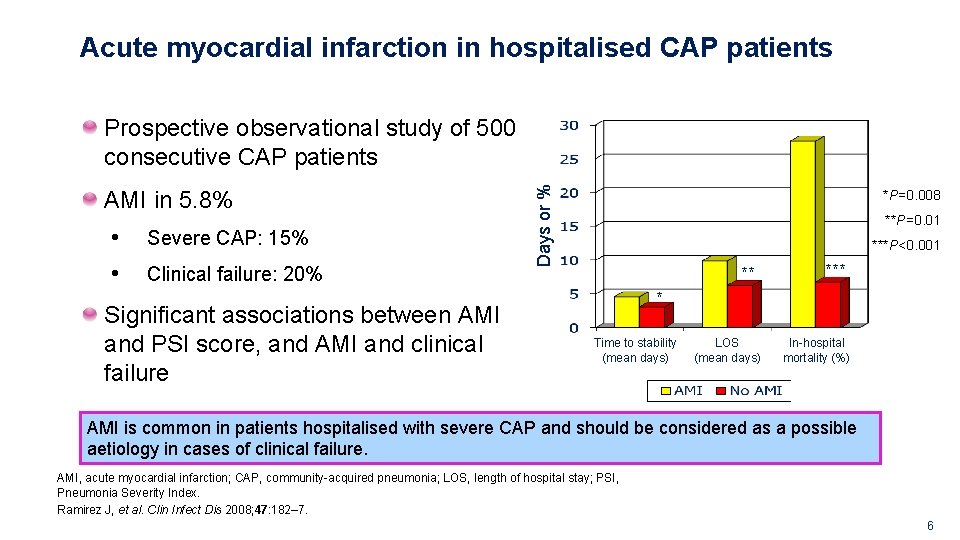
Acute myocardial infarction in hospitalised CAP patients AMI in 5. 8% • • Severe CAP: 15% Clinical failure: 20% Significant associations between AMI and PSI score, and AMI and clinical failure Days or % Prospective observational study of 500 consecutive CAP patients *P=0. 008 **P=0. 01 ***P<0. 001 ** * Time to stability (mean days) LOS (mean days) In-hospital mortality (%) AMI is common in patients hospitalised with severe CAP and should be considered as a possible aetiology in cases of clinical failure. AMI, acute myocardial infarction; CAP, community-acquired pneumonia; LOS, length of hospital stay; PSI, Pneumonia Severity Index. Ramirez J, et al. Clin Infect Dis 2008; 47: 182– 7. G. GM. AVE. 09. 2010. 0020 6
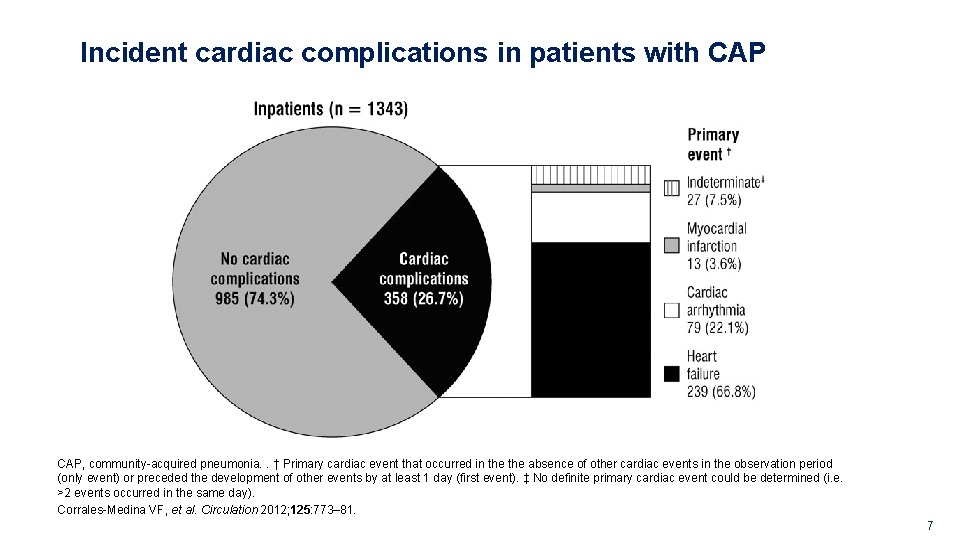
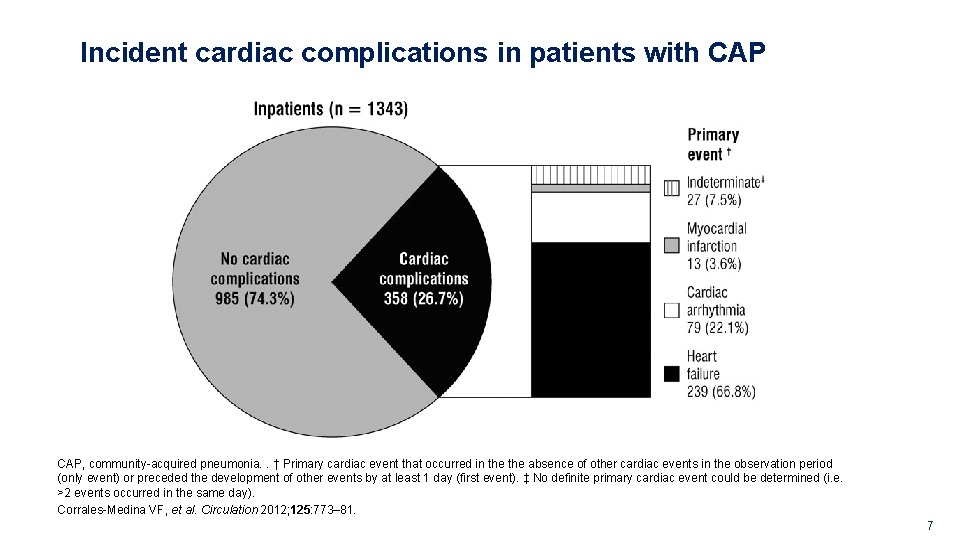
Incident cardiac complications in patients with CAP, community-acquired pneumonia. . † Primary cardiac event that occurred in the absence of other cardiac events in the observation period (only event) or preceded the development of other events by at least 1 day (first event). ‡ No definite primary cardiac event could be determined (i. e. >2 events occurred in the same day). Corrales-Medina VF, et al. Circulation 2012; 125: 773– 81. G. GM. AVE. 09. 2010. 0020 7
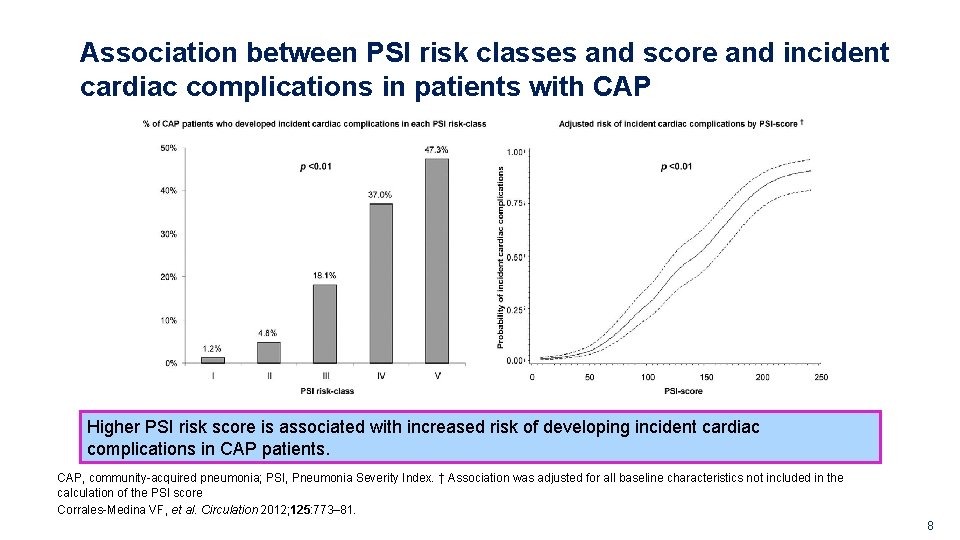
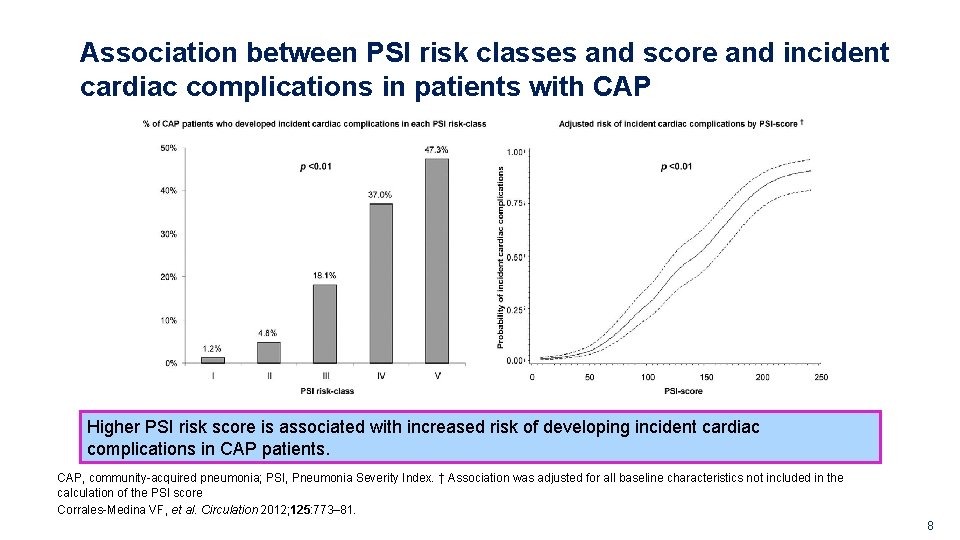
Association between PSI risk classes and score and incident cardiac complications in patients with CAP Higher PSI risk score is associated with increased risk of developing incident cardiac complications in CAP patients. CAP, community-acquired pneumonia; PSI, Pneumonia Severity Index. † Association was adjusted for all baseline characteristics not included in the calculation of the PSI score Corrales-Medina VF, et al. Circulation 2012; 125: 773– 81. G. GM. AVE. 09. 2010. 0020 8
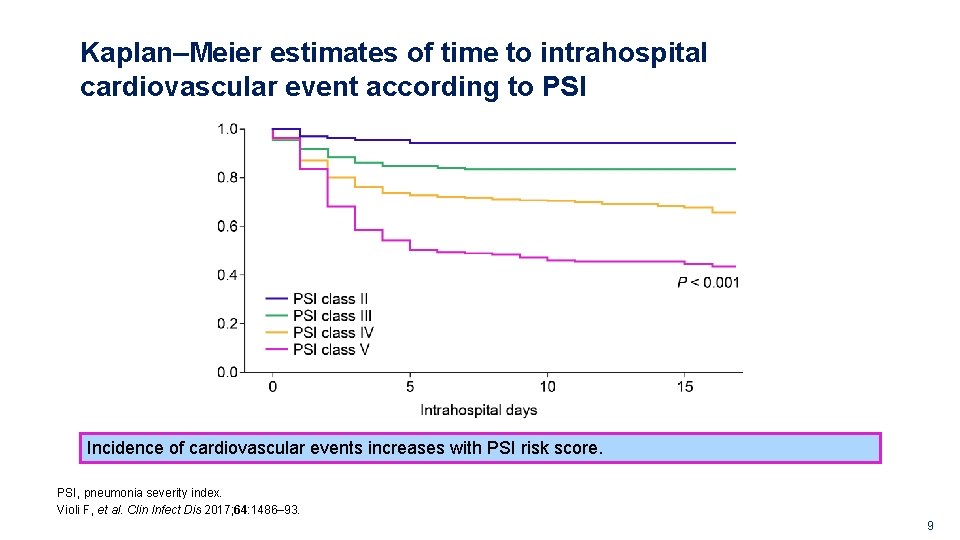
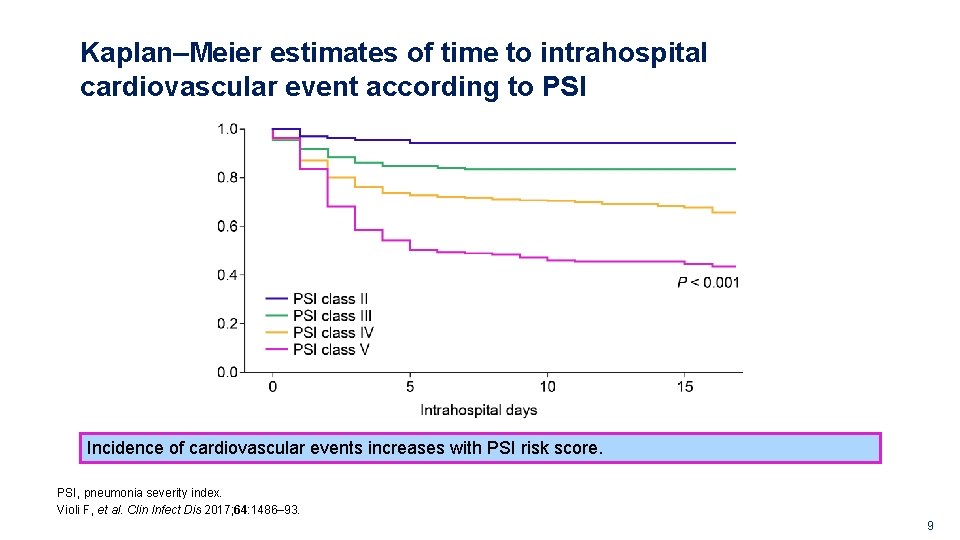
Kaplan–Meier estimates of time to intrahospital cardiovascular event according to PSI Incidence of cardiovascular events increases with PSI risk score. PSI, pneumonia severity index. Violi F, et al. Clin Infect Dis 2017; 64: 1486– 93. G. GM. AVE. 09. 2010. 0020 9
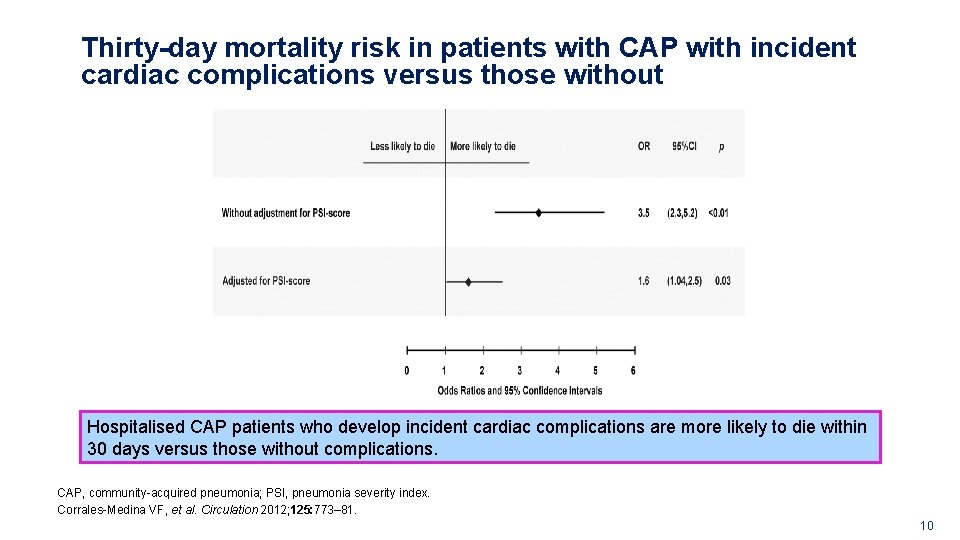
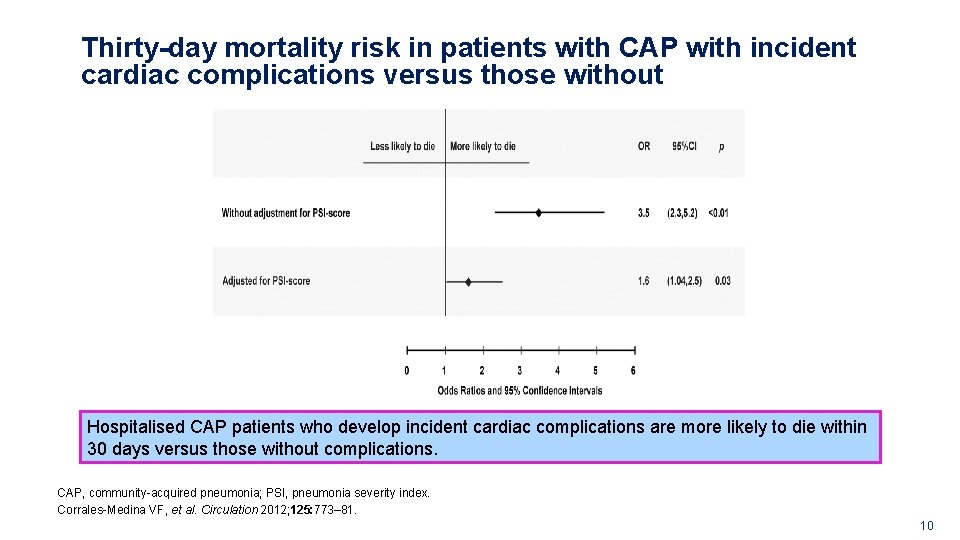
Thirty-day mortality risk in patients with CAP with incident cardiac complications versus those without Hospitalised CAP patients who develop incident cardiac complications are more likely to die within 30 days versus those without complications. CAP, community-acquired pneumonia; PSI, pneumonia severity index. Corrales-Medina VF, et al. Circulation 2012; 125: 773– 81. G. GM. AVE. 09. 2010. 0020 10
Risk factors for cardiovascular events in hospitalised patients with CAP Secondary analysis of the Community-Acquired Pneumonia Organization (CAPO) database on CAP, a multicentre, retrospective, international cohort study of inpatients from 80 centres in 13 countries Of 3068 patients with CAP, 376 (12%) presented with at least one CVE upon admission or developed an event during hospitalisation CAP, community-acquired pneumonia; CVE, cardiovascular event. Griffin AT, et al. Int J Infect Dis 2013; 17: e 1125– 9. G. GM. AVE. 09. 2010. 0020 11
Risk factors for cardiovascular events in hospitalised patients with CAP 435 events occurred in total During admission, 28% of the CVE group died compared with 8% of the non-CVE group (P<0. 001) Cumulatively at 28 days, 36% of the total CVE group died compared with 10% in the comparison group (P<0. 001) CAP, community-acquired pneumonia; CVE, cardiovascular events. Griffin AT, et al. Int J Infect Dis 2013; 17: e 1125– 9. G. GM. AVE. 09. 2010. 0020 12
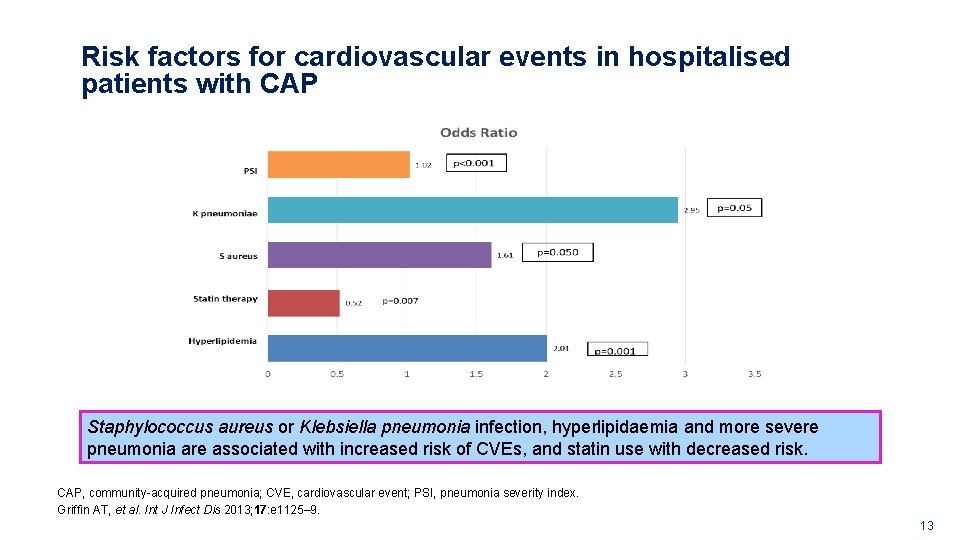
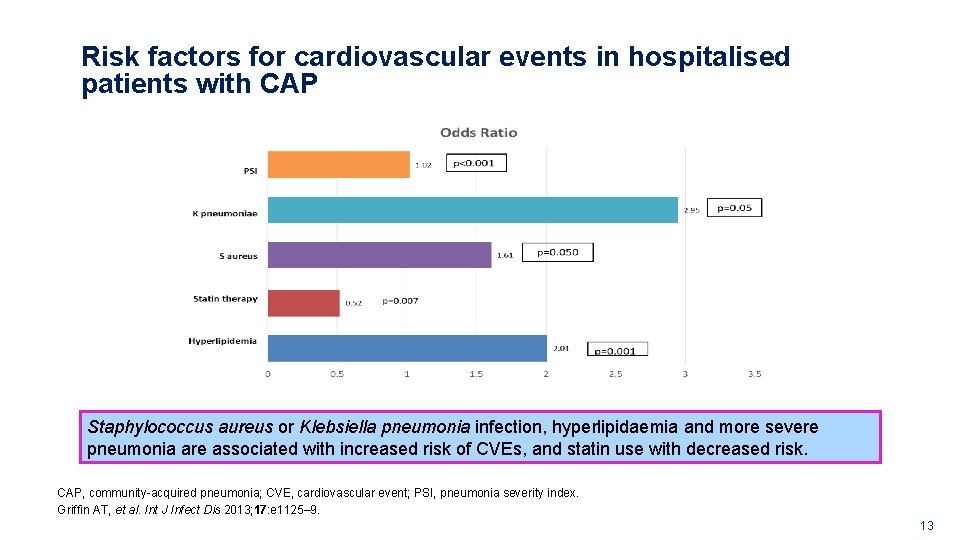
Risk factors for cardiovascular events in hospitalised patients with CAP Staphylococcus aureus or Klebsiella pneumonia infection, hyperlipidaemia and more severe pneumonia are associated with increased risk of CVEs, and statin use with decreased risk. CAP, community-acquired pneumonia; CVE, cardiovascular event; PSI, pneumonia severity index. Griffin AT, et al. Int J Infect Dis 2013; 17: e 1125– 9. G. GM. AVE. 09. 2010. 0020 13
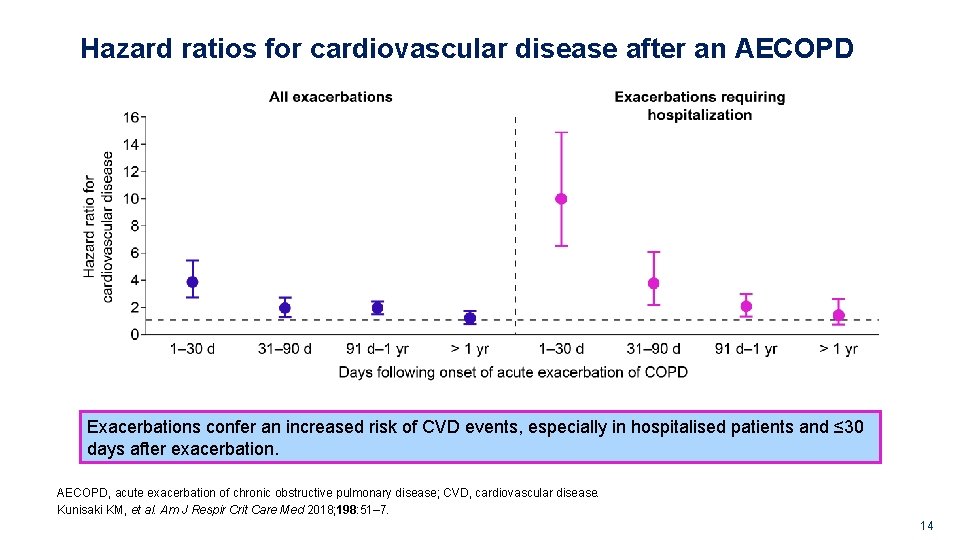
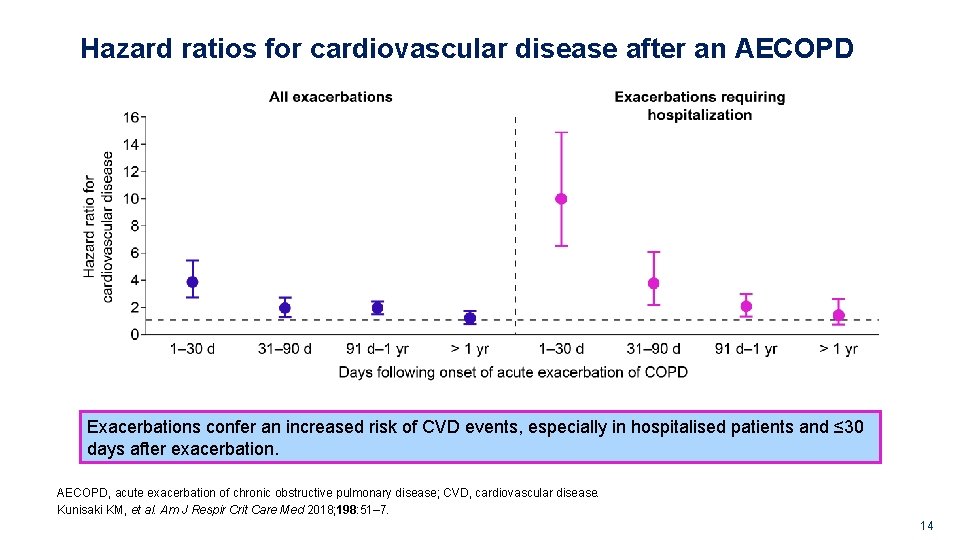
Hazard ratios for cardiovascular disease after an AECOPD Exacerbations confer an increased risk of CVD events, especially in hospitalised patients and ≤ 30 days after exacerbation. AECOPD, acute exacerbation of chronic obstructive pulmonary disease; CVD, cardiovascular disease. Kunisaki KM, et al. Am J Respir Crit Care Med 2018; 198: 51– 7. G. GM. AVE. 09. 2010. 0020 14
Cardiovascular complications of influenza Myocarditis • Reported in approximately 0. 4– 13% of hospitalised adult patients with documented influenza • Cellular infiltration and myocyte necrosis have been found in 30– 50% of patients at autopsy despite cardiac involvement not being clinically suspected Ischaemic heart disease • Temporal association between the circulation of influenza viruses and an increase in hospitalisations and deaths due to ischaemic heart disease • A significant increase in the number of IHD deaths has also been detected during epidemic periods IHD, ischaemic heart disease. Sellers SA, et al. Influenza Other Respir Viruses 2017; 11: 372– 93. G. GM. AVE. 09. 2010. 0020 15
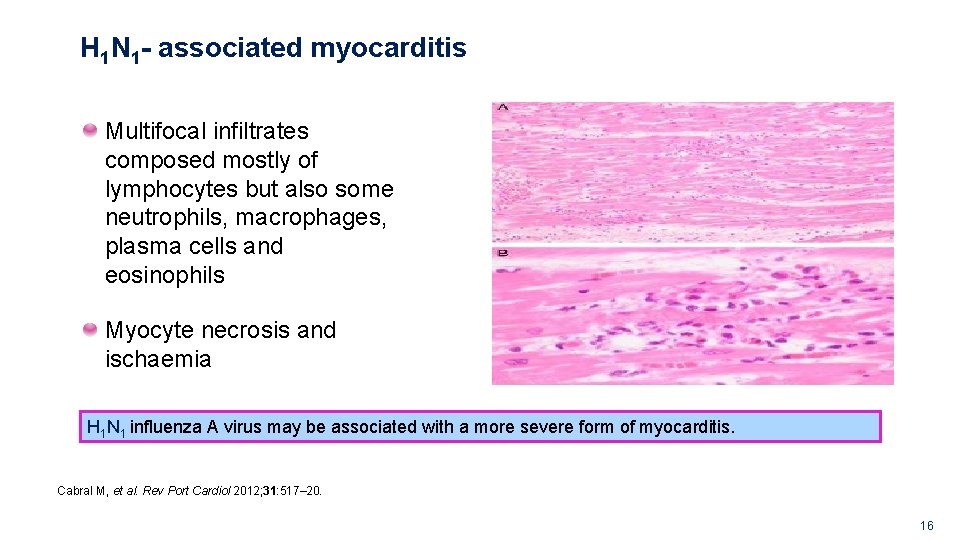
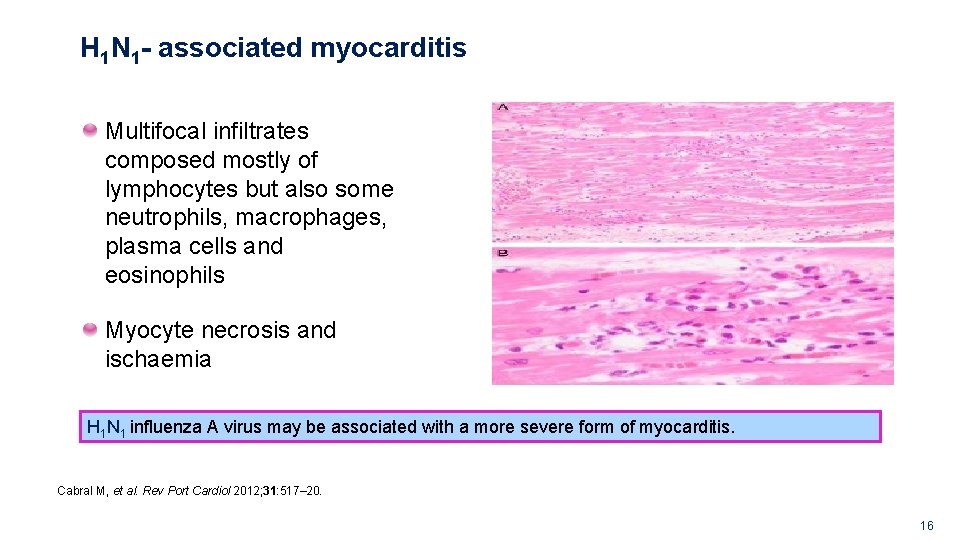
H 1 N 1 - associated myocarditis Multifocal infiltrates composed mostly of lymphocytes but also some neutrophils, macrophages, plasma cells and eosinophils Myocyte necrosis and ischaemia H 1 N 1 influenza A virus may be associated with a more severe form of myocarditis. Cabral M, et al. Rev Port Cardiol 2012; 31: 517– 20. G. GM. AVE. 09. 2010. 0020 16
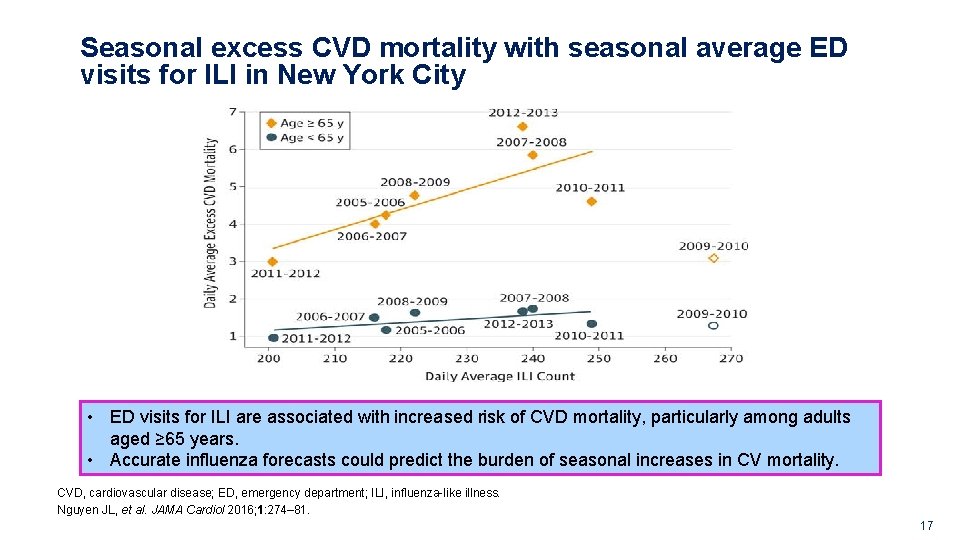
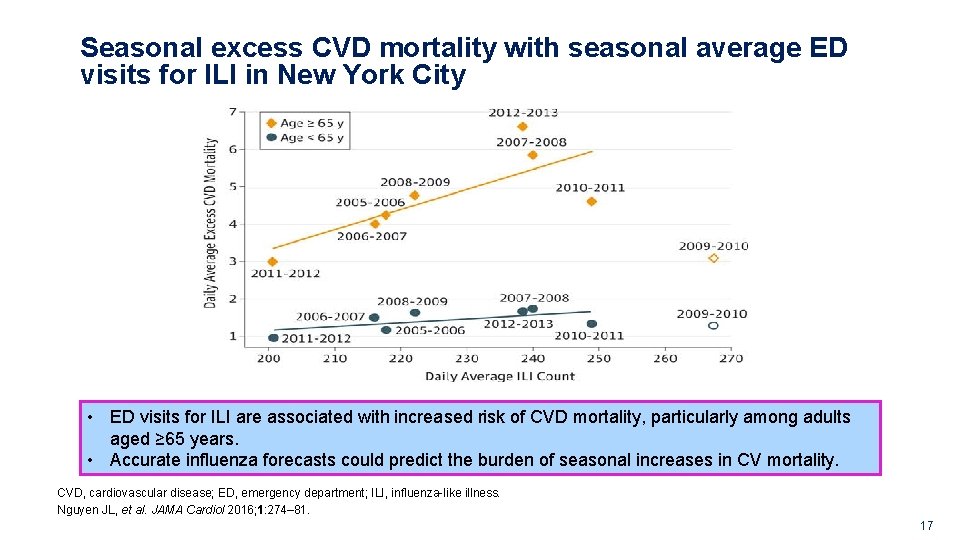
Seasonal excess CVD mortality with seasonal average ED visits for ILI in New York City • ED visits for ILI are associated with increased risk of CVD mortality, particularly among adults aged ≥ 65 years. • Accurate influenza forecasts could predict the burden of seasonal increases in CV mortality. CVD, cardiovascular disease; ED, emergency department; ILI, influenza-like illness. Nguyen JL, et al. JAMA Cardiol 2016; 1: 274– 81. G. GM. AVE. 09. 2010. 0020 17
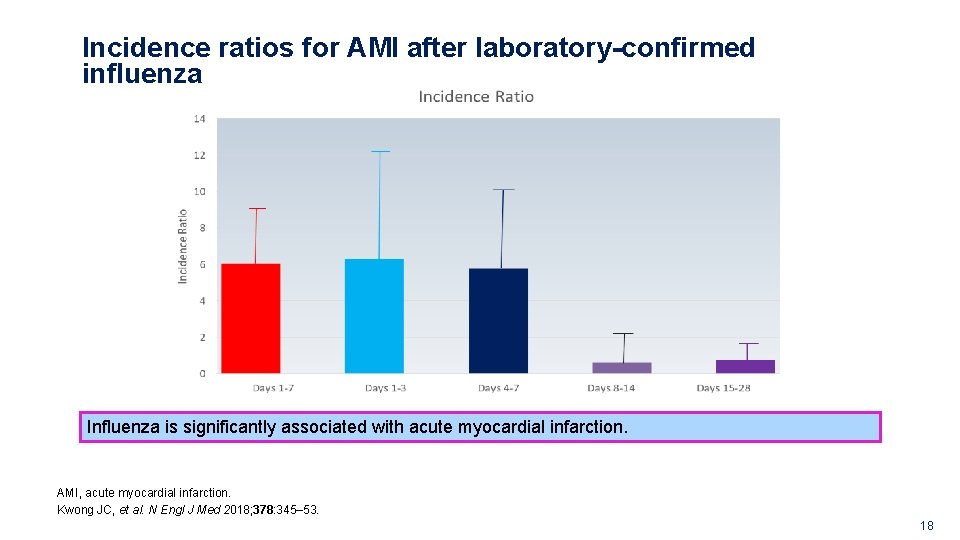
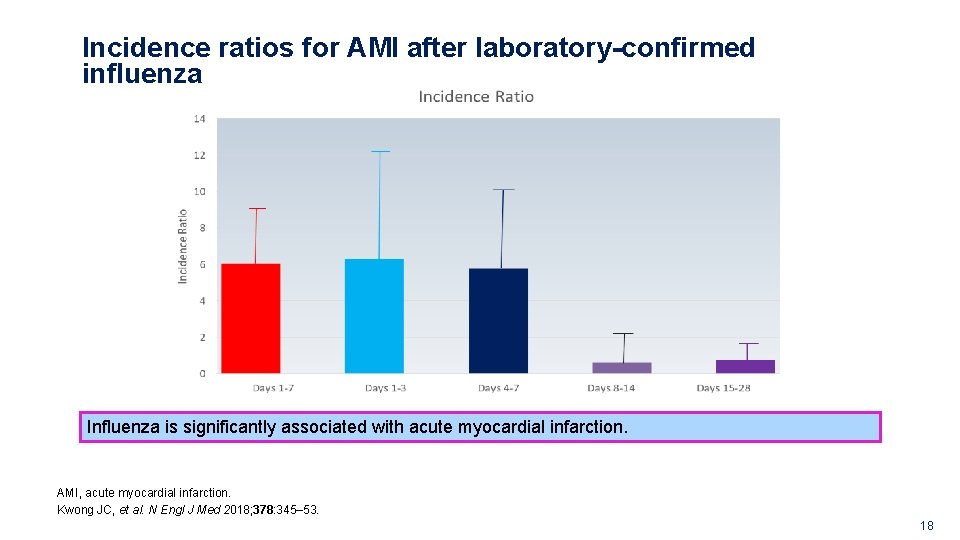
Incidence ratios for AMI after laboratory-confirmed influenza Influenza is significantly associated with acute myocardial infarction. AMI, acute myocardial infarction. Kwong JC, et al. N Engl J Med 2018; 378: 345– 53. G. GM. AVE. 09. 2010. 0020 18
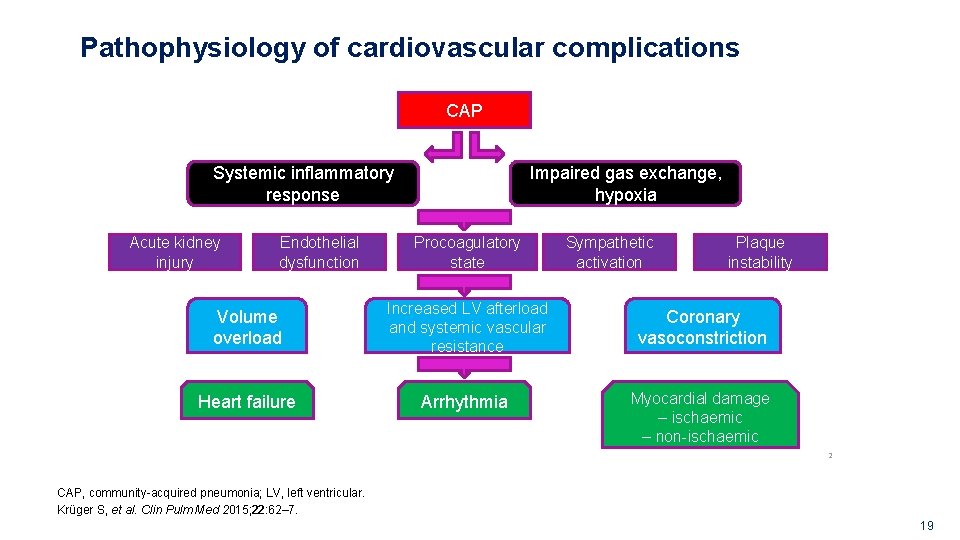
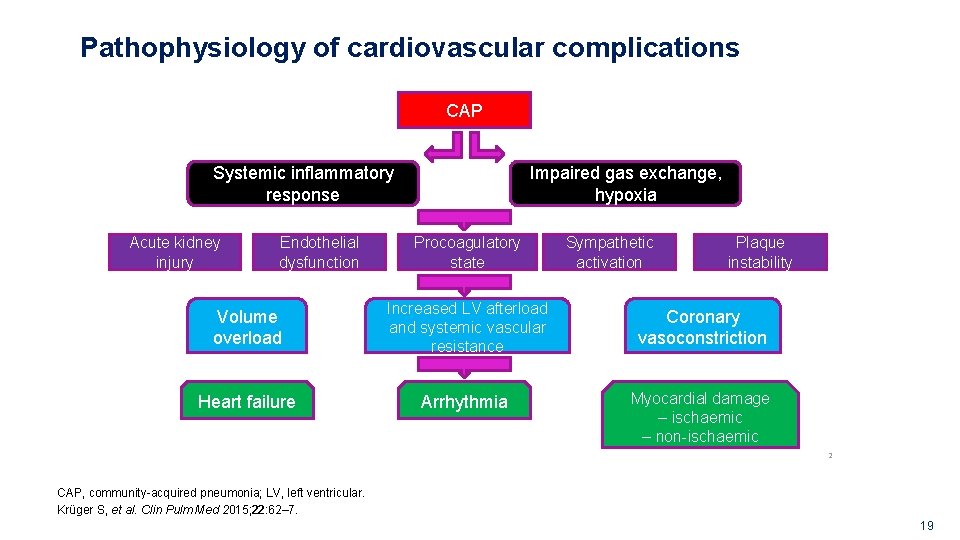
Pathophysiology of cardiovascular complications CAP Systemic inflammatory response Acute kidney injury Endothelial dysfunction Impaired gas exchange, hypoxia Procoagulatory state Sympathetic activation Plaque instability Volume overload Increased LV afterload and systemic vascular resistance Coronary vasoconstriction Heart failure Arrhythmia Myocardial damage – ischaemic – non-ischaemic 2 CAP, community-acquired pneumonia; LV, left ventricular. Krüger S, et al. Clin Pulm Med 2015; 22: 62– 7. G. GM. AVE. 09. 2010. 0020 19
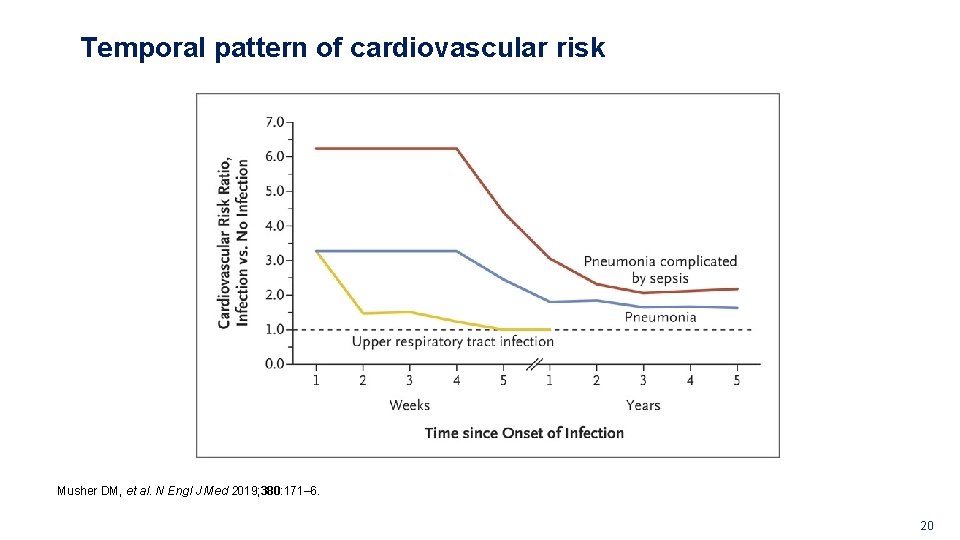
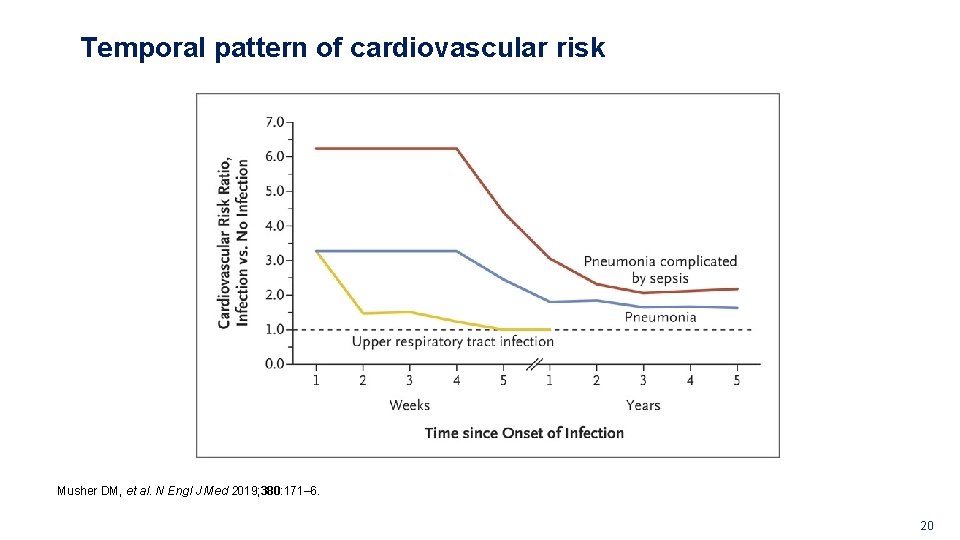
Temporal pattern of cardiovascular risk Musher DM, et al. N Engl J Med 2019; 380: 171– 6. G. GM. AVE. 09. 2010. 0020 20
G. GM. AVE. 09. 2010. 0020 LONG-TERM IMPLICATIONS 21
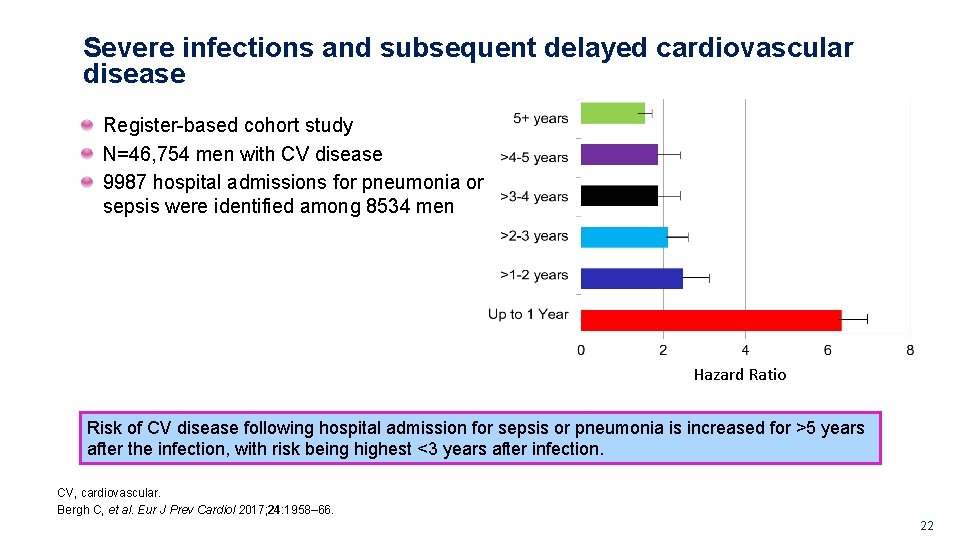
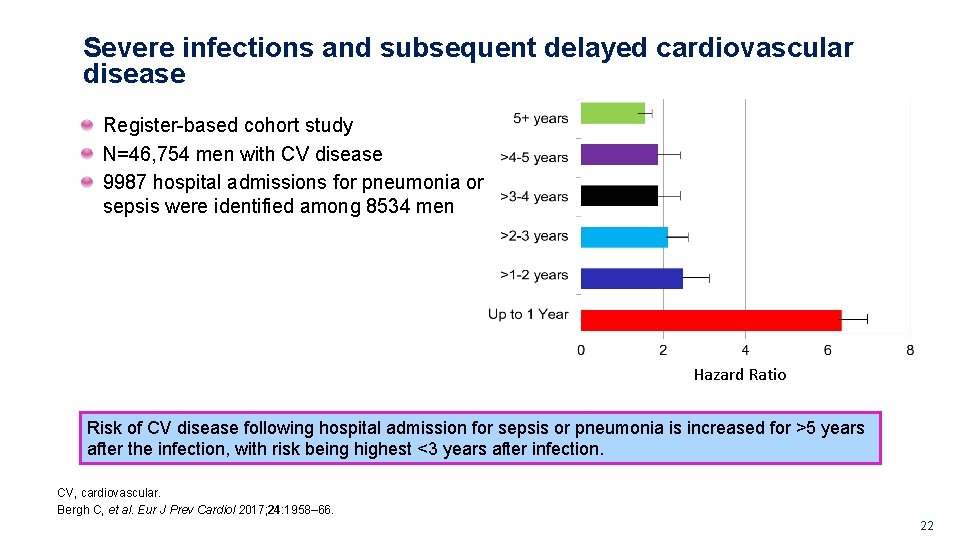
Severe infections and subsequent delayed cardiovascular disease Register-based cohort study N=46, 754 men with CV disease 9987 hospital admissions for pneumonia or sepsis were identified among 8534 men Hazard Ratio Risk of CV disease following hospital admission for sepsis or pneumonia is increased for >5 years after the infection, with risk being highest <3 years after infection. CV, cardiovascular. Bergh C, et al. Eur J Prev Cardiol 2017; 24: 1958– 66. G. GM. AVE. 09. 2010. 0020 22
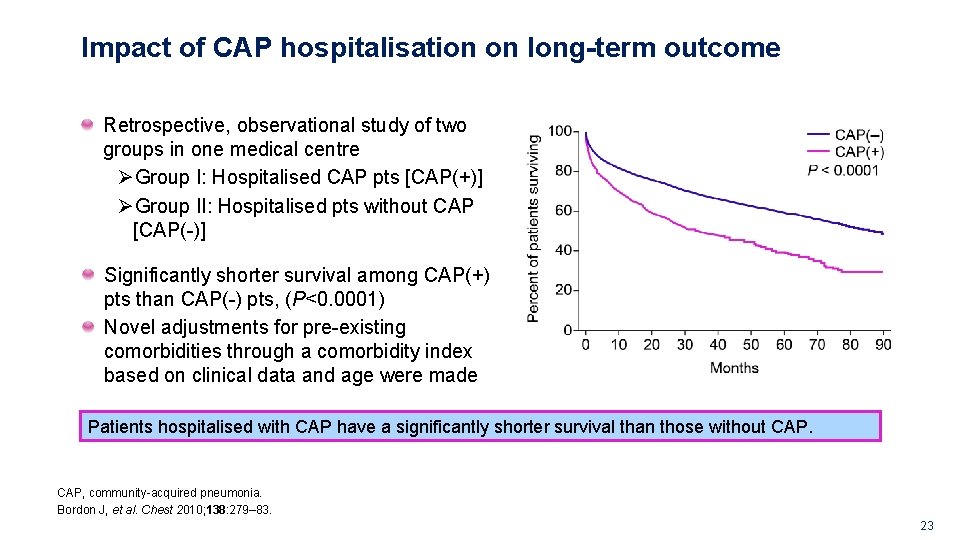
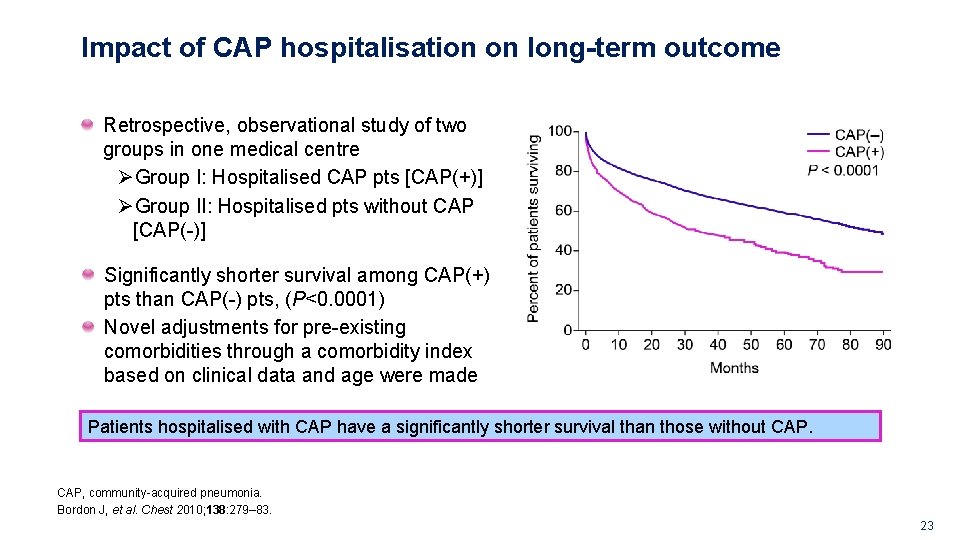
Impact of CAP hospitalisation on long-term outcome Retrospective, observational study of two groups in one medical centre ØGroup I: Hospitalised CAP pts [CAP(+)] ØGroup II: Hospitalised pts without CAP [CAP(-)] Significantly shorter survival among CAP(+) pts than CAP(-) pts, (P<0. 0001) Novel adjustments for pre-existing comorbidities through a comorbidity index based on clinical data and age were made Patients hospitalised with CAP have a significantly shorter survival than those without CAP, community-acquired pneumonia. Bordon J, et al. Chest 2010; 138: 279– 83. G. GM. AVE. 09. 2010. 0020 23
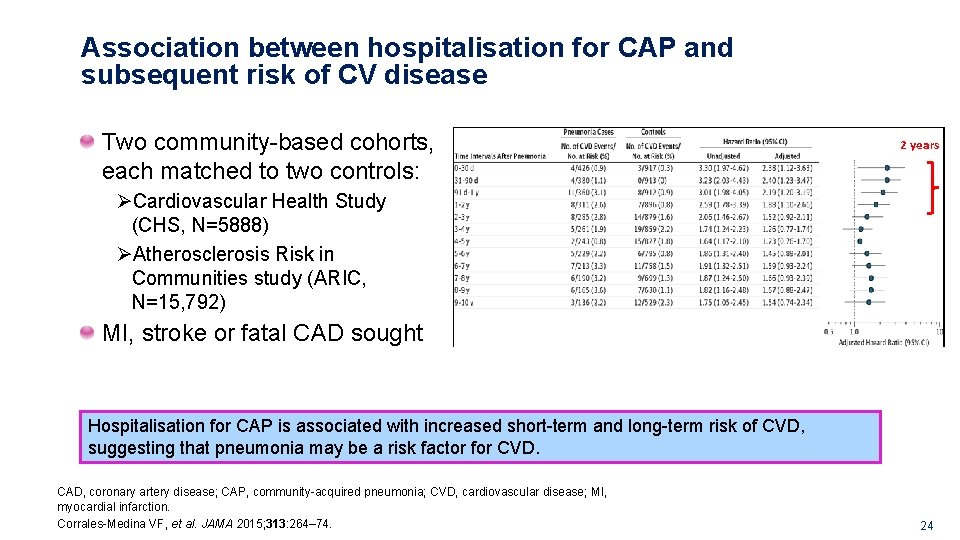
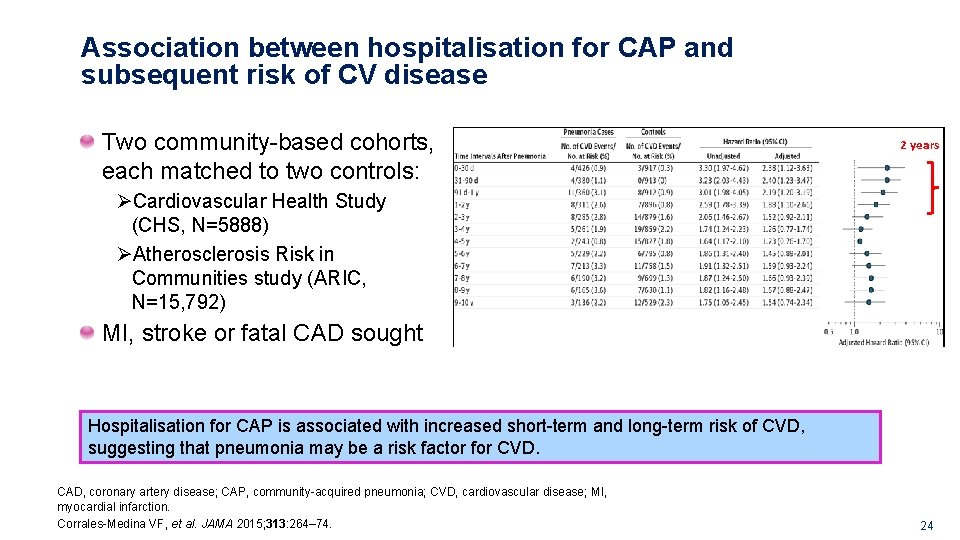
Association between hospitalisation for CAP and subsequent risk of CV disease Two community-based cohorts, each matched to two controls: 2 years ØCardiovascular Health Study (CHS, N=5888) ØAtherosclerosis Risk in Communities study (ARIC, N=15, 792) MI, stroke or fatal CAD sought Hospitalisation for CAP is associated with increased short-term and long-term risk of CVD, suggesting that pneumonia may be a risk factor for CVD. CAD, coronary artery disease; CAP, community-acquired pneumonia; CVD, cardiovascular disease; MI, myocardial infarction. Corrales-Medina VF, et al. JAMA 2015; 313: 264– 74. G. GM. AVE. 09. 2010. 0020 24
G. GM. AVE. 09. 2010. 0020 WHAT IS THE MECHANISM? 25
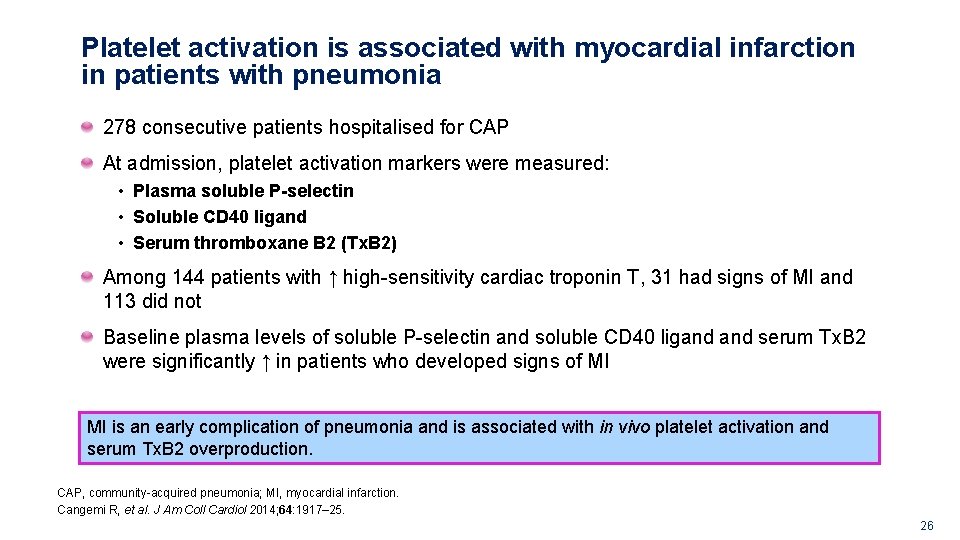
Platelet activation is associated with myocardial infarction in patients with pneumonia 278 consecutive patients hospitalised for CAP At admission, platelet activation markers were measured: • Plasma soluble P-selectin • Soluble CD 40 ligand • Serum thromboxane B 2 (Tx. B 2) Among 144 patients with ↑ high-sensitivity cardiac troponin T, 31 had signs of MI and 113 did not Baseline plasma levels of soluble P-selectin and soluble CD 40 ligand serum Tx. B 2 were significantly ↑ in patients who developed signs of MI MI is an early complication of pneumonia and is associated with in vivo platelet activation and serum Tx. B 2 overproduction. CAP, community-acquired pneumonia; MI, myocardial infarction. Cangemi R, et al. J Am Coll Cardiol 2014; 64: 1917– 25. G. GM. AVE. 09. 2010. 0020 26
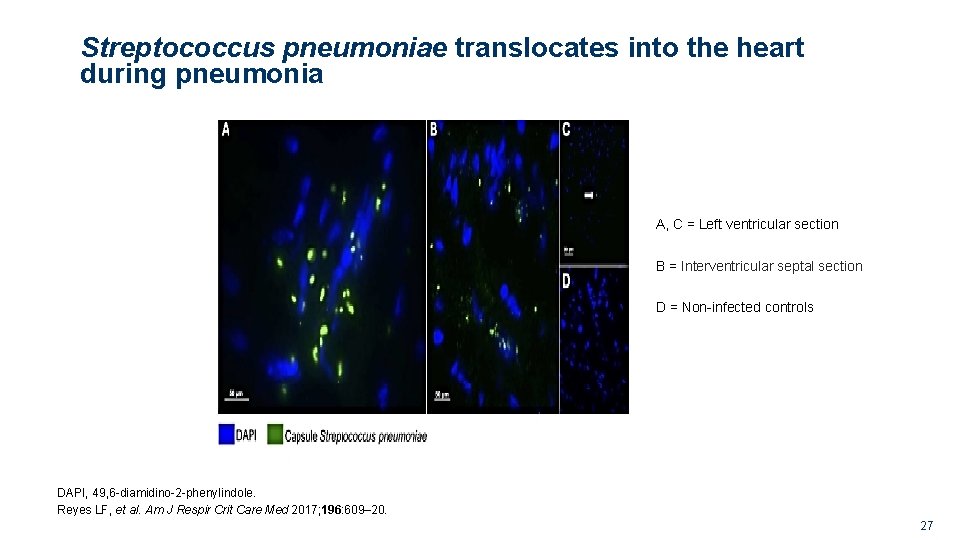
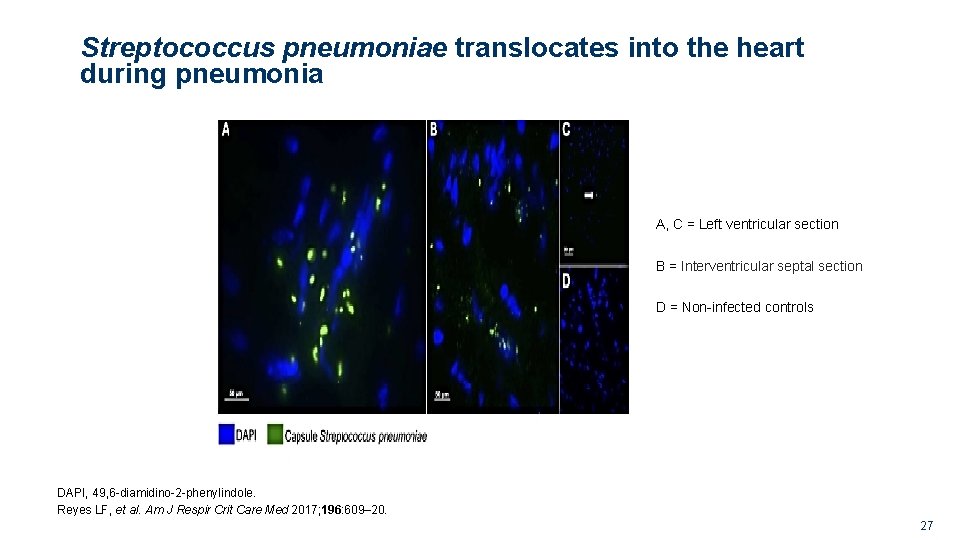
Streptococcus pneumoniae translocates into the heart during pneumonia A, C = Left ventricular section B = Interventricular septal section D = Non-infected controls DAPI, 49, 6 -diamidino-2 -phenylindole. Reyes LF, et al. Am J Respir Crit Care Med 2017; 196: 609– 20. G. GM. AVE. 09. 2010. 0020 27

Cardiac microlesion in a human after death from IPD Microlesion formation may contribute to the acute and long-term adverse cardiac events seen in humans with IPD, invasive pneumococcal disease. Brown AO, et al. PLo. S Pathog 2014; 10: e 1004383. G. GM. AVE. 09. 2010. 0020 28
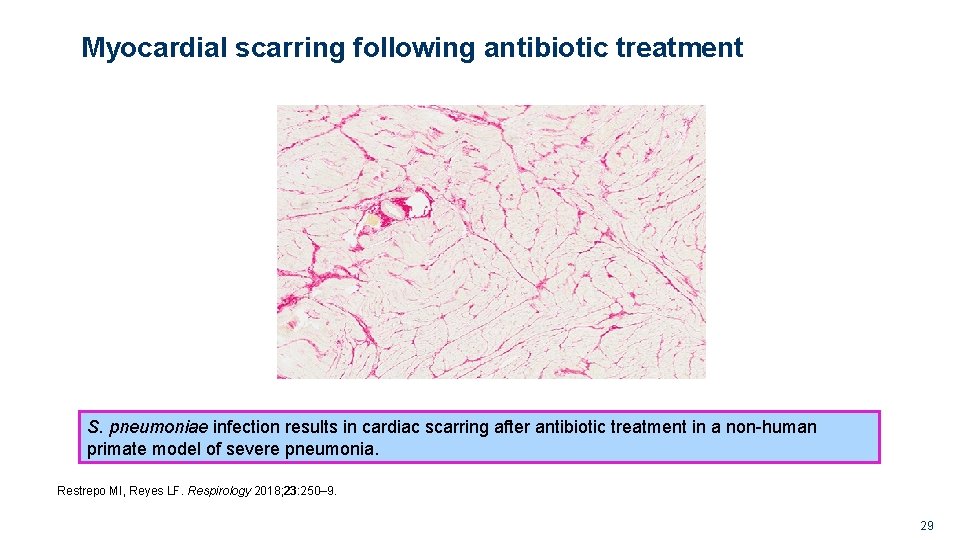
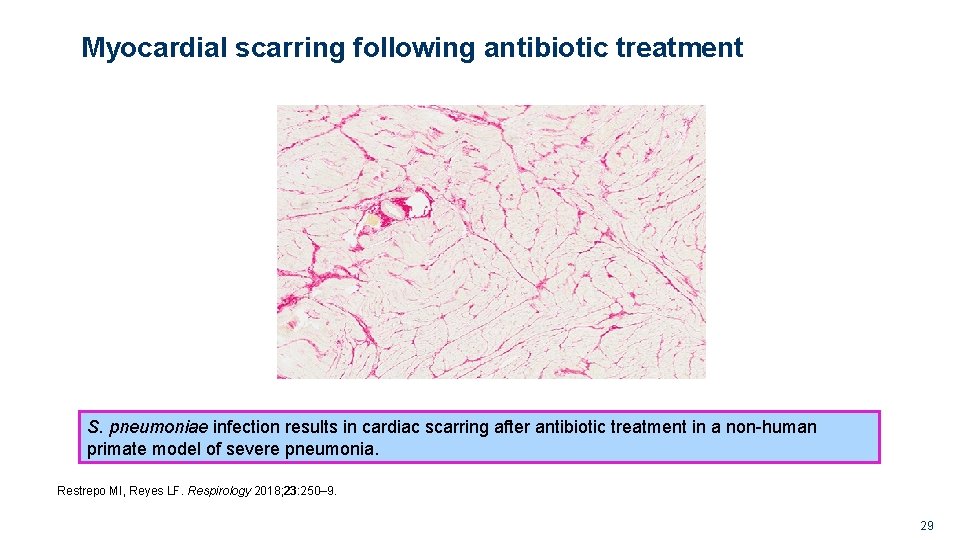
Myocardial scarring following antibiotic treatment S. pneumoniae infection results in cardiac scarring after antibiotic treatment in a non-human primate model of severe pneumonia. Restrepo MI, Reyes LF. Respirology 2018; 23: 250– 9. G. GM. AVE. 09. 2010. 0020 29
Potential mechanisms of S. pneumoniae toxicity Invade the myocardium and form microlesions Induce ion flow disturbances and electrophysiological abnormalities Kill cardiomyocytes in a pneumolysin-dependent manner Generate enlargement and instability of atherosclerotic plaques Provoke necroptosis in cardiomyocytes and macrophages infiltrating the heart Promote platelet activation After antibiotic treatment, inducing heart scarring Restrepo MI, Reyes LF. Respirology 2018; 23: 250– 9. G. GM. AVE. 09. 2010. 0020 30
G. GM. AVE. 09. 2010. 0020 NEW STUDIES AT ERS AND ATS 31
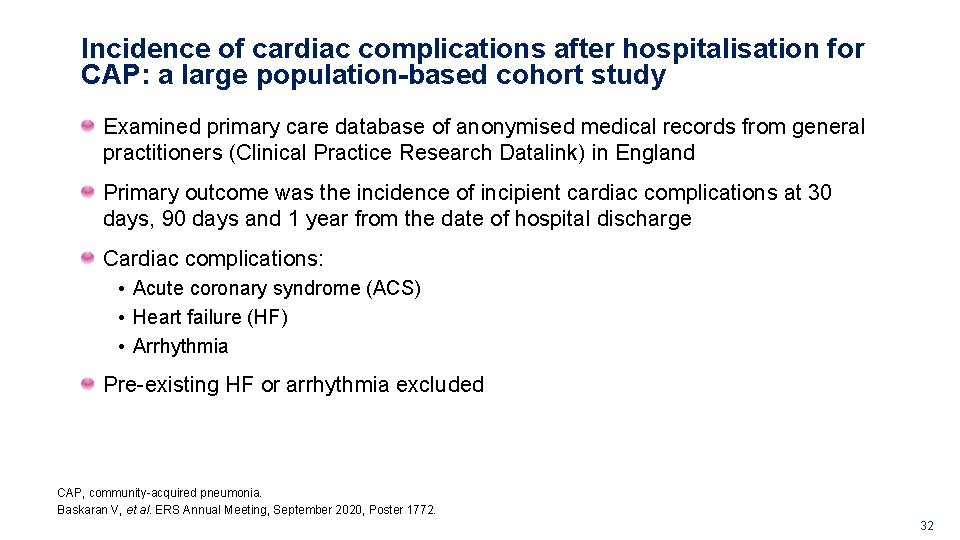
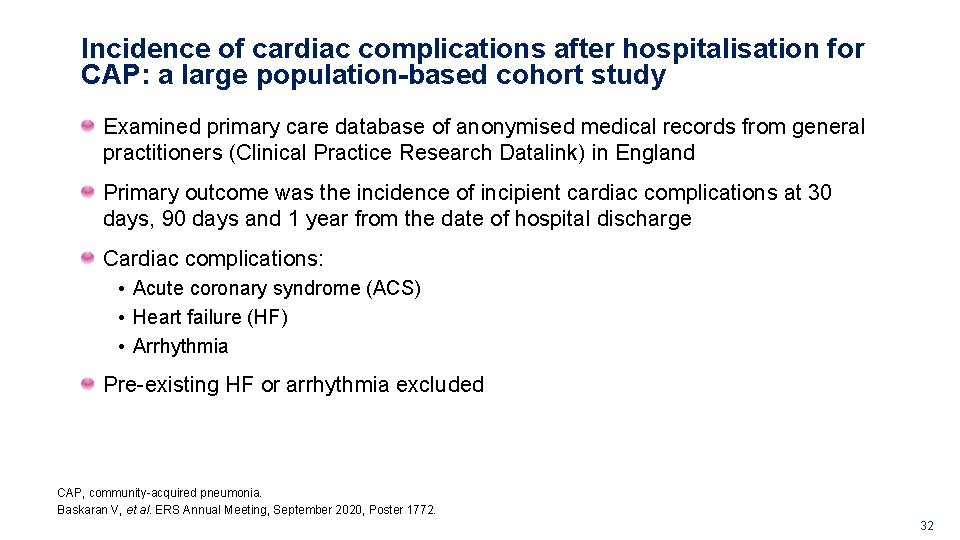
Incidence of cardiac complications after hospitalisation for CAP: a large population-based cohort study Examined primary care database of anonymised medical records from general practitioners (Clinical Practice Research Datalink) in England Primary outcome was the incidence of incipient cardiac complications at 30 days, 90 days and 1 year from the date of hospital discharge Cardiac complications: • Acute coronary syndrome (ACS) • Heart failure (HF) • Arrhythmia Pre-existing HF or arrhythmia excluded CAP, community-acquired pneumonia. Baskaran V, et al. ERS Annual Meeting, September 2020, Poster 1772. G. GM. AVE. 09. 2010. 0020 32
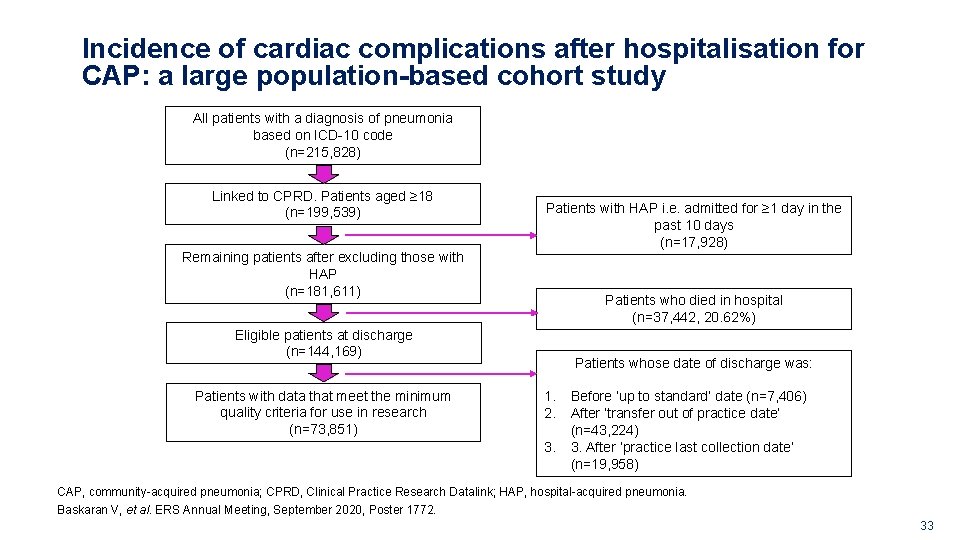
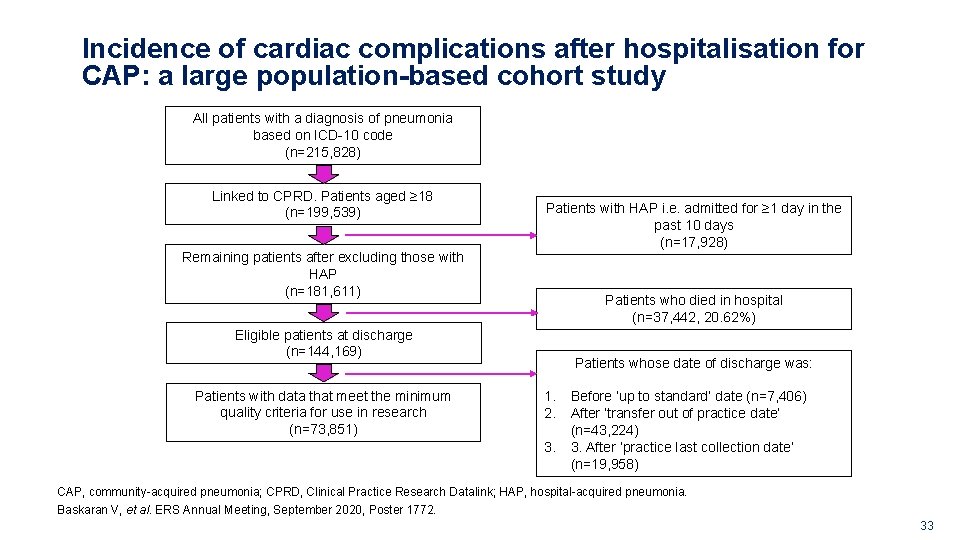
Incidence of cardiac complications after hospitalisation for CAP: a large population-based cohort study All patients with a diagnosis of pneumonia based on ICD-10 code (n=215, 828) Linked to CPRD. Patients aged ≥ 18 (n=199, 539) Remaining patients after excluding those with HAP (n=181, 611) Patients with HAP i. e. admitted for ≥ 1 day in the past 10 days (n=17, 928) Patients who died in hospital (n=37, 442, 20. 62%) Eligible patients at discharge (n=144, 169) Patients with data that meet the minimum quality criteria for use in research (n=73, 851) Patients whose date of discharge was: 1. 2. 3. Before ‘up to standard’ date (n=7, 406) After ‘transfer out of practice date’ (n=43, 224) 3. After ‘practice last collection date’ (n=19, 958) CAP, community-acquired pneumonia; CPRD, Clinical Practice Research Datalink; HAP, hospital-acquired pneumonia. Baskaran V, et al. ERS Annual Meeting, September 2020, Poster 1772. G. GM. AVE. 09. 2010. 0020 33
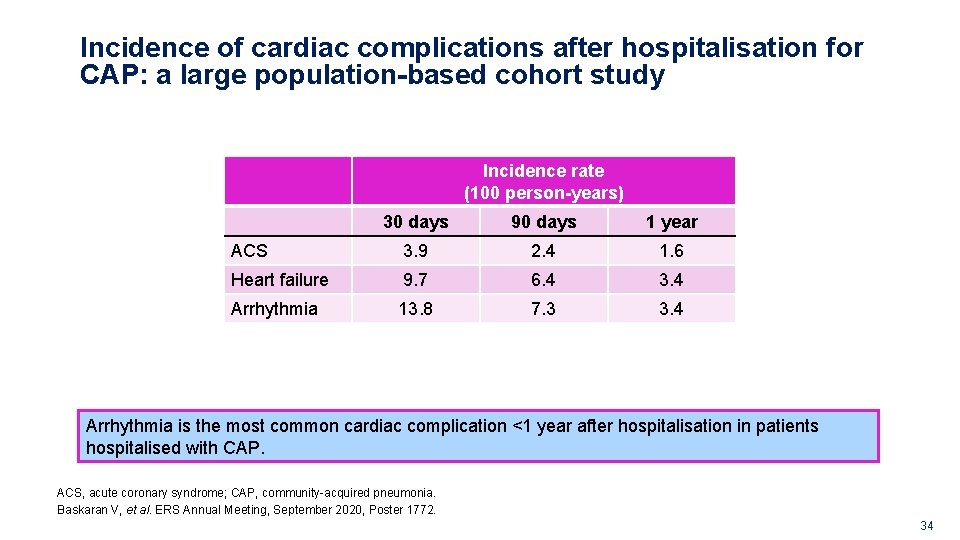
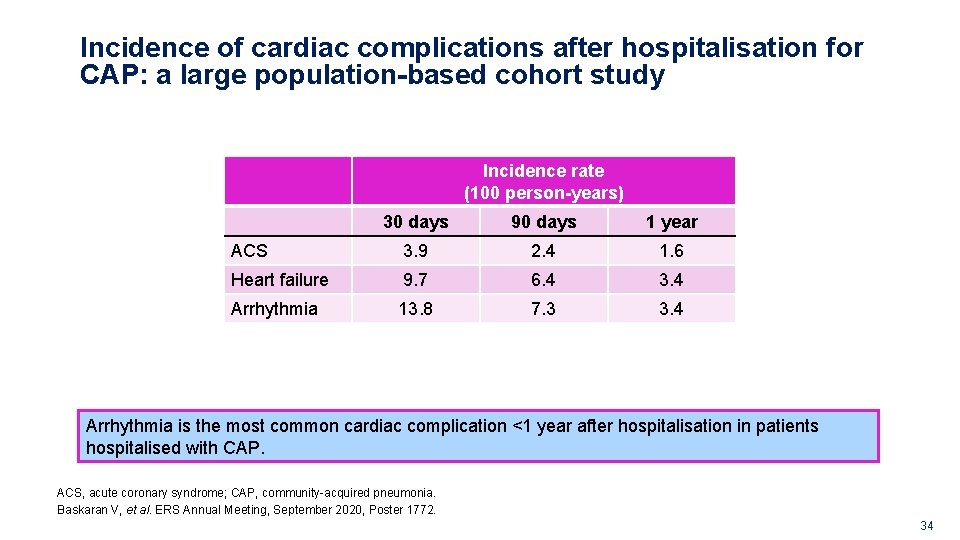
Incidence of cardiac complications after hospitalisation for CAP: a large population-based cohort study Incidence rate (100 person-years) 30 days 90 days 1 year ACS 3. 9 2. 4 1. 6 Heart failure 9. 7 6. 4 3. 4 Arrhythmia 13. 8 7. 3 3. 4 Arrhythmia is the most common cardiac complication <1 year after hospitalisation in patients hospitalised with CAP. ACS, acute coronary syndrome; CAP, community-acquired pneumonia. Baskaran V, et al. ERS Annual Meeting, September 2020, Poster 1772. G. GM. AVE. 09. 2010. 0020 34
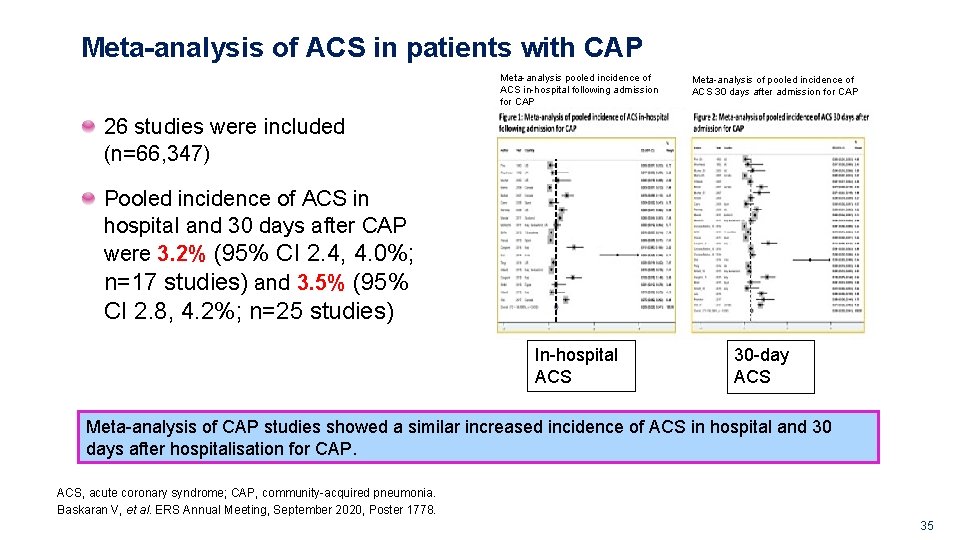
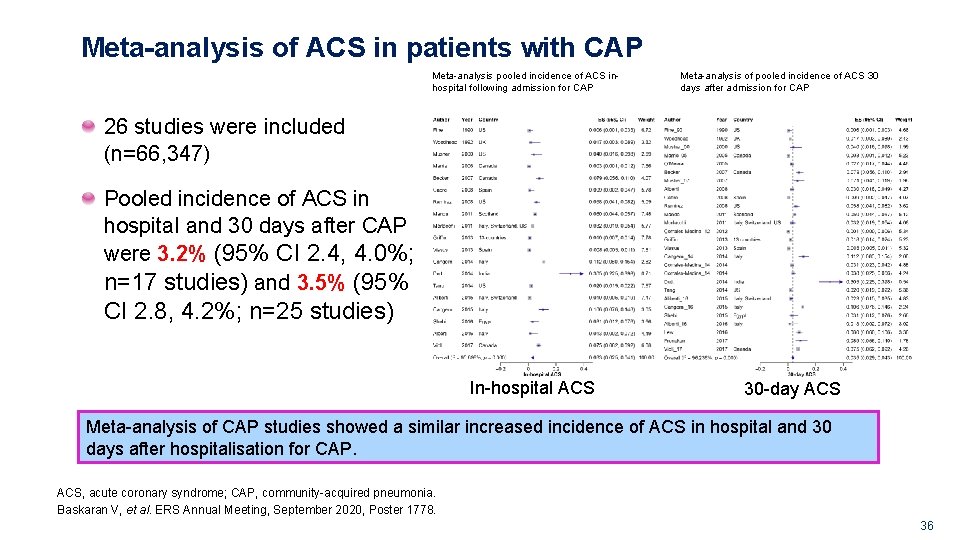
Meta-analysis of ACS in patients with CAP Meta-analysis pooled incidence of ACS in-hospital following admission for CAP Meta-analysis of pooled incidence of ACS 30 days after admission for CAP 26 studies were included (n=66, 347) Pooled incidence of ACS in hospital and 30 days after CAP were 3. 2% (95% CI 2. 4, 4. 0%; n=17 studies) and 3. 5% (95% CI 2. 8, 4. 2%; n=25 studies) In-hospital ACS 30 -day ACS Meta-analysis of CAP studies showed a similar increased incidence of ACS in hospital and 30 days after hospitalisation for CAP. ACS, acute coronary syndrome; CAP, community-acquired pneumonia. Baskaran V, et al. ERS Annual Meeting, September 2020, Poster 1778. G. GM. AVE. 09. 2010. 0020 35
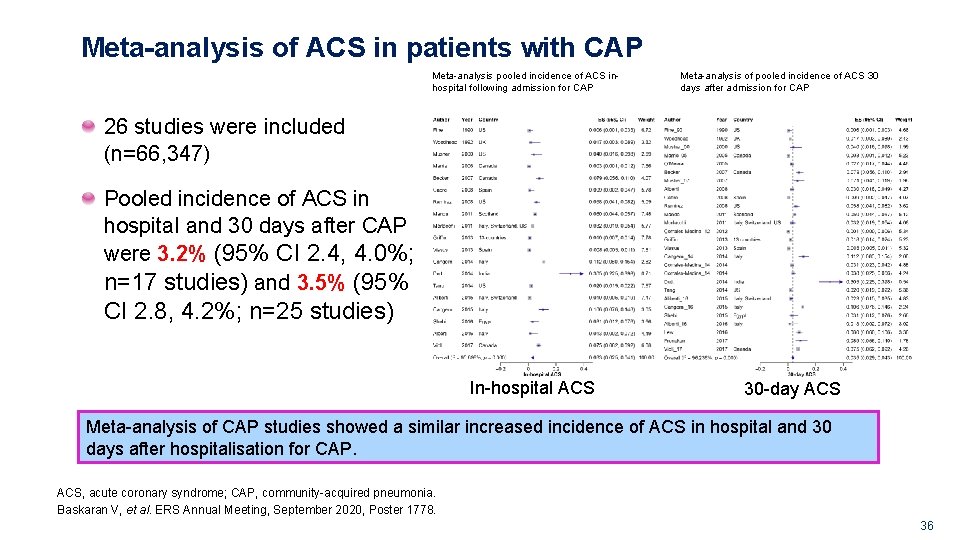
Meta-analysis of ACS in patients with CAP Meta-analysis pooled incidence of ACS inhospital following admission for CAP Meta-analysis of pooled incidence of ACS 30 days after admission for CAP 26 studies were included (n=66, 347) Pooled incidence of ACS in hospital and 30 days after CAP were 3. 2% (95% CI 2. 4, 4. 0%; n=17 studies) and 3. 5% (95% CI 2. 8, 4. 2%; n=25 studies) In-hospital ACS 30 -day ACS Meta-analysis of CAP studies showed a similar increased incidence of ACS in hospital and 30 days after hospitalisation for CAP. ACS, acute coronary syndrome; CAP, community-acquired pneumonia. Baskaran V, et al. ERS Annual Meeting, September 2020, Poster 1778. G. GM. AVE. 09. 2010. 0020 36
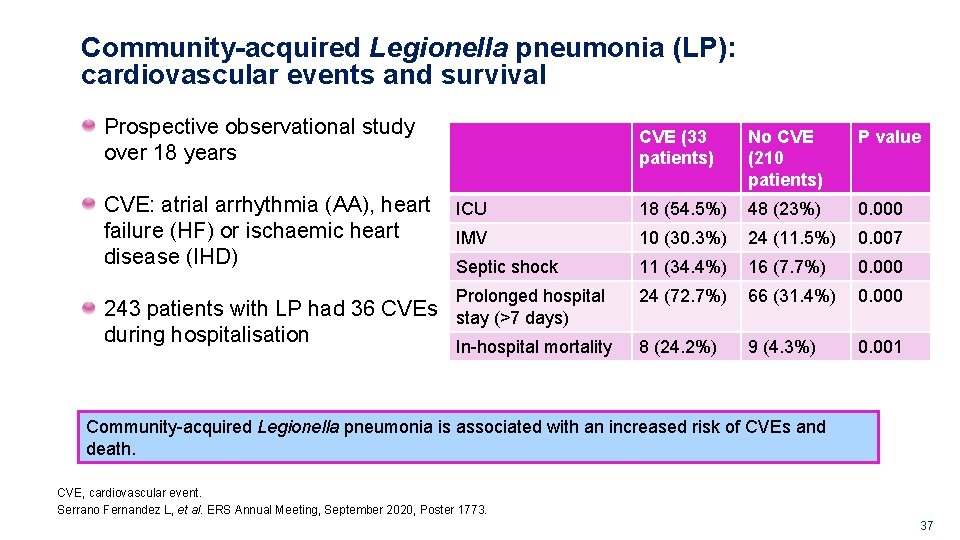
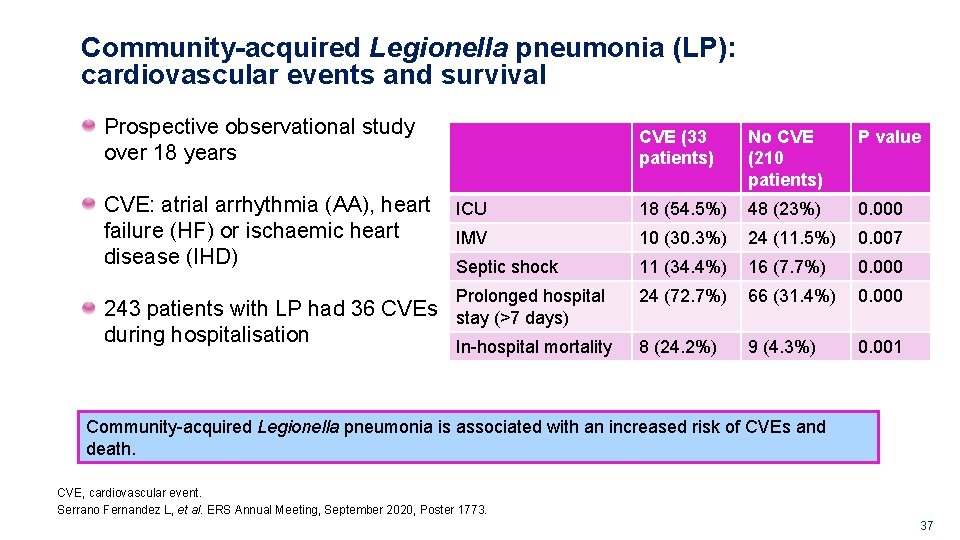
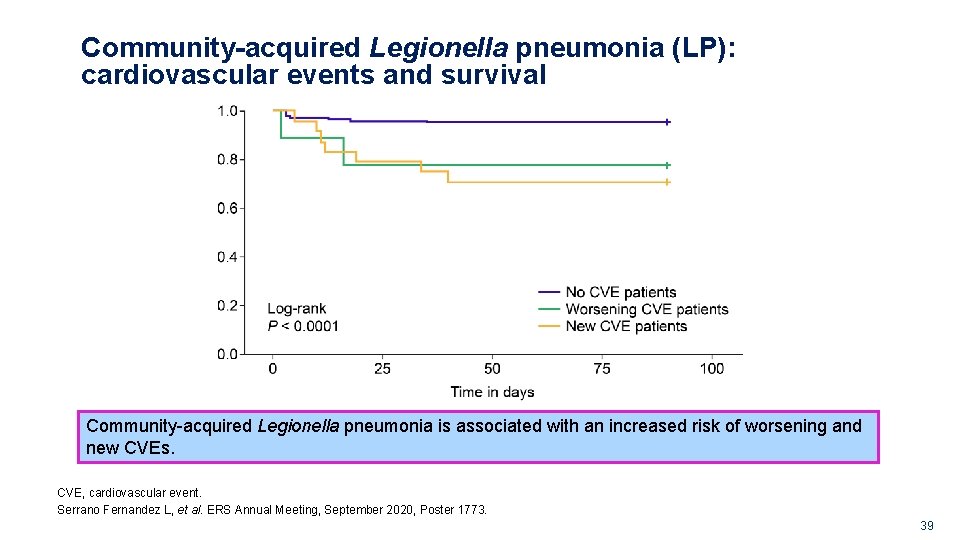
Community-acquired Legionella pneumonia (LP): cardiovascular events and survival Prospective observational study over 18 years CVE: atrial arrhythmia (AA), heart failure (HF) or ischaemic heart disease (IHD) CVE (33 patients) No CVE (210 patients) P value ICU 18 (54. 5%) 48 (23%) 0. 000 IMV 10 (30. 3%) 24 (11. 5%) 0. 007 Septic shock 11 (34. 4%) 16 (7. 7%) 0. 000 Prolonged hospital 24 (72. 7%) 66 (31. 4%) 0. 000 8 (24. 2%) 9 (4. 3%) 0. 001 243 patients with LP had 36 CVEs stay (>7 days) during hospitalisation In-hospital mortality Community-acquired Legionella pneumonia is associated with an increased risk of CVEs and death. CVE, cardiovascular event. Serrano Fernandez L, et al. ERS Annual Meeting, September 2020, Poster 1773. G. GM. AVE. 09. 2010. 0020 37
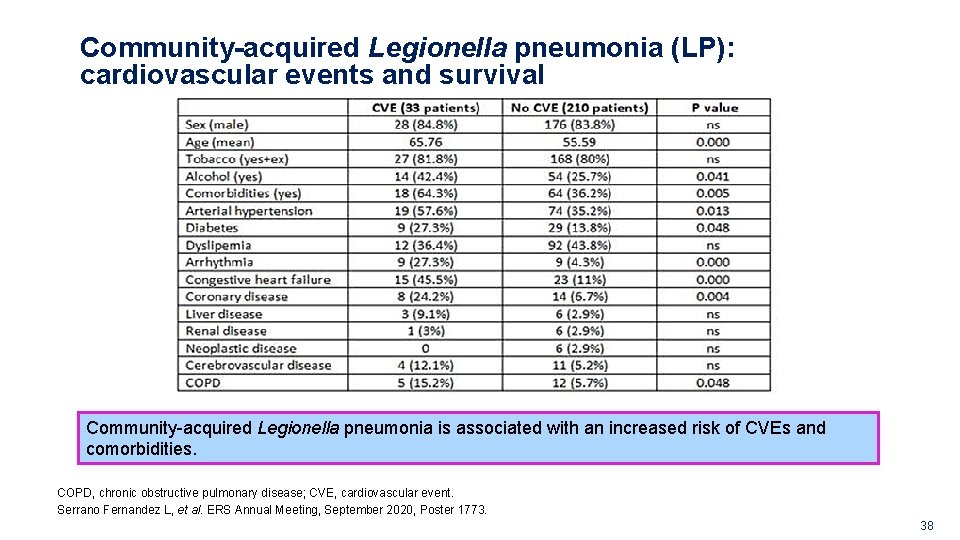
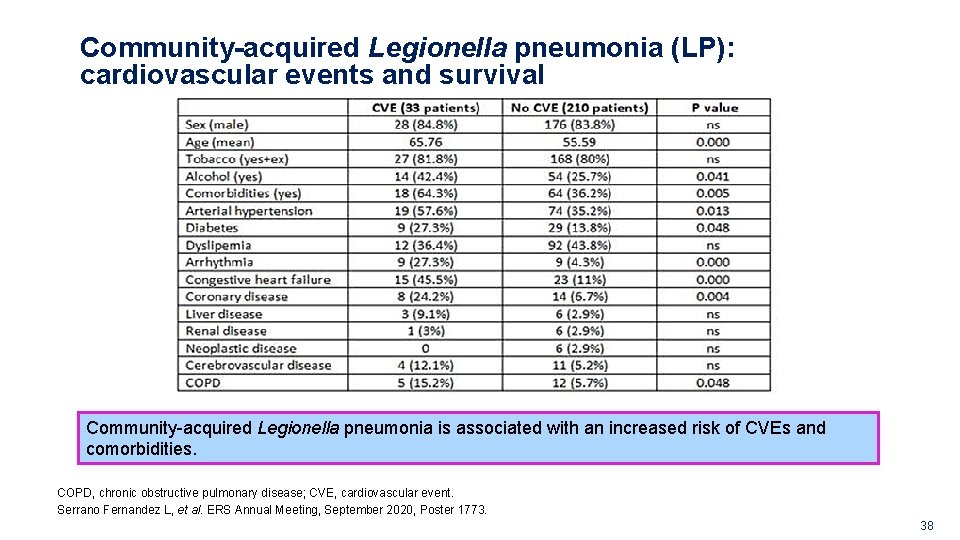
Community-acquired Legionella pneumonia (LP): cardiovascular events and survival Community-acquired Legionella pneumonia is associated with an increased risk of CVEs and comorbidities. COPD, chronic obstructive pulmonary disease; CVE, cardiovascular event. Serrano Fernandez L, et al. ERS Annual Meeting, September 2020, Poster 1773. G. GM. AVE. 09. 2010. 0020 38
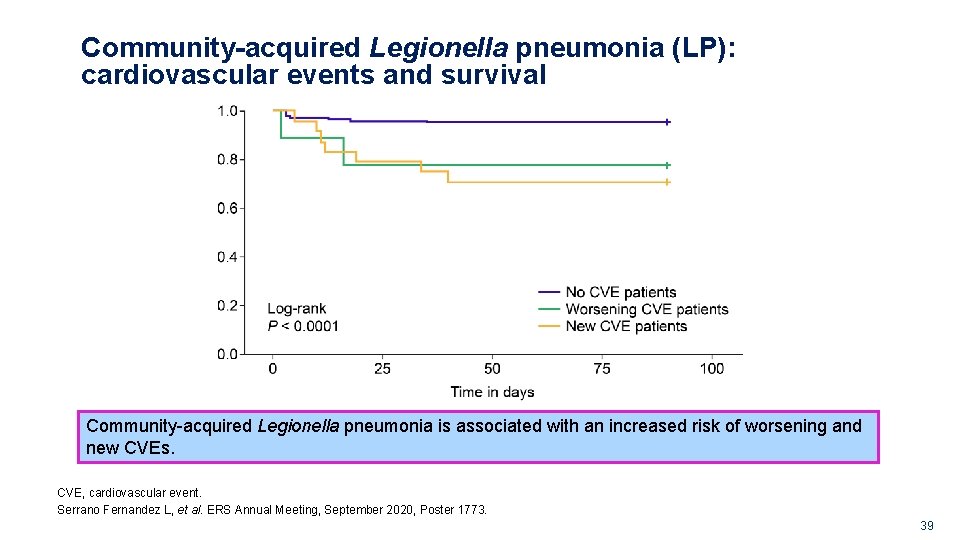
Community-acquired Legionella pneumonia (LP): cardiovascular events and survival Community-acquired Legionella pneumonia is associated with an increased risk of worsening and new CVEs. CVE, cardiovascular event. Serrano Fernandez L, et al. ERS Annual Meeting, September 2020, Poster 1773. G. GM. AVE. 09. 2010. 0020 39
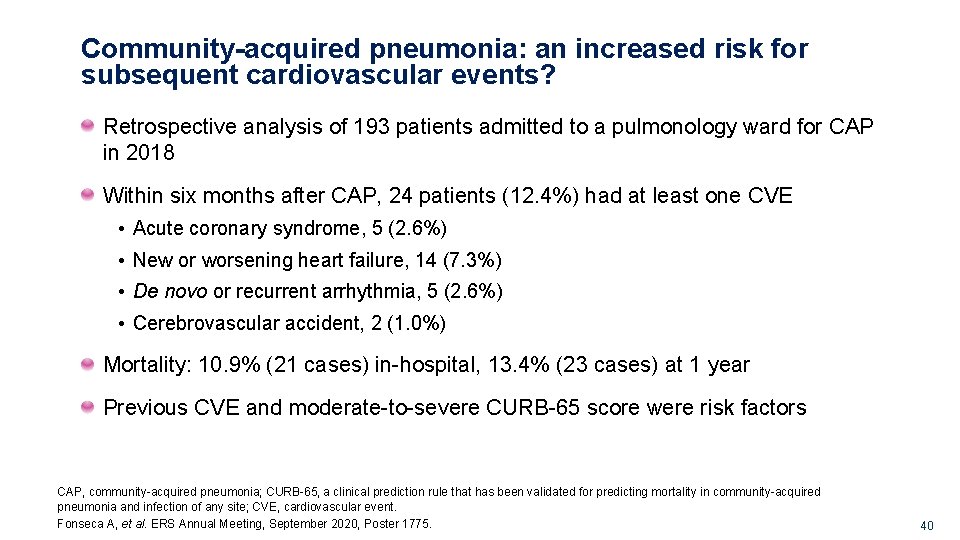
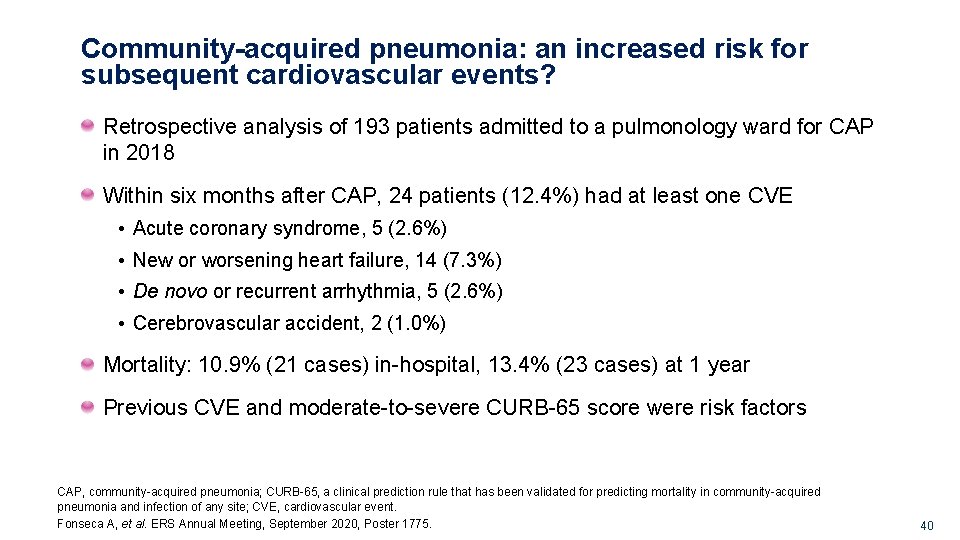
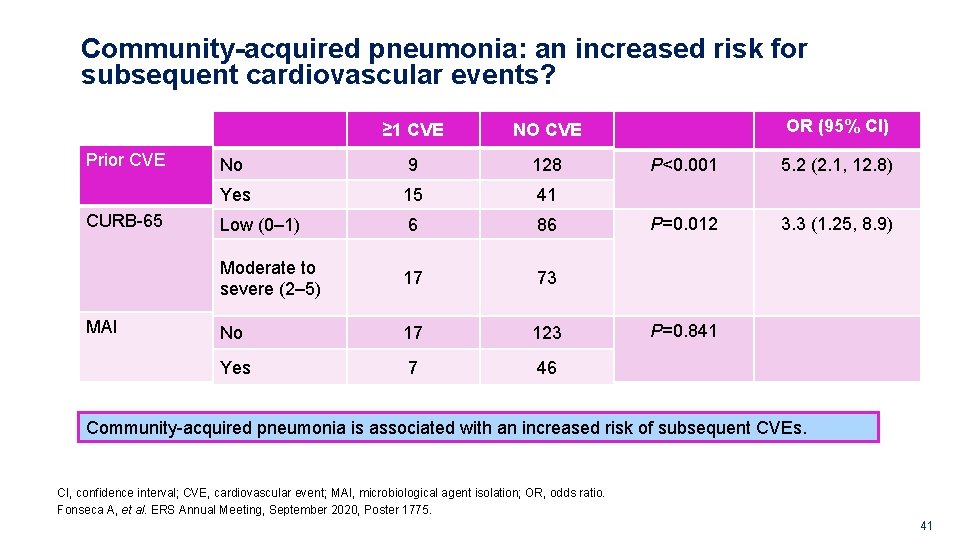
Community-acquired pneumonia: an increased risk for subsequent cardiovascular events? Retrospective analysis of 193 patients admitted to a pulmonology ward for CAP in 2018 Within six months after CAP, 24 patients (12. 4%) had at least one CVE • Acute coronary syndrome, 5 (2. 6%) • New or worsening heart failure, 14 (7. 3%) • De novo or recurrent arrhythmia, 5 (2. 6%) • Cerebrovascular accident, 2 (1. 0%) Mortality: 10. 9% (21 cases) in-hospital, 13. 4% (23 cases) at 1 year Previous CVE and moderate-to-severe CURB-65 score were risk factors CAP, community-acquired pneumonia; CURB-65, a clinical prediction rule that has been validated for predicting mortality in community-acquired pneumonia and infection of any site; CVE, cardiovascular event. Fonseca A, et al. ERS Annual Meeting, September 2020, Poster 1775. G. GM. AVE. 09. 2010. 0020 40
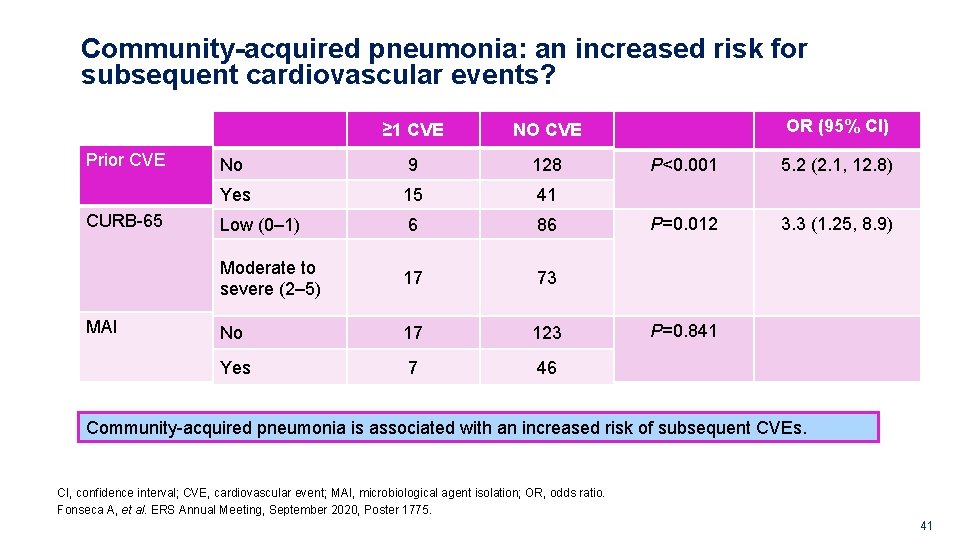
Community-acquired pneumonia: an increased risk for subsequent cardiovascular events? Prior CVE CURB-65 MAI ≥ 1 CVE NO CVE No 9 128 Yes 15 41 Low (0– 1) 6 86 Moderate to severe (2– 5) 17 73 No 17 123 Yes 7 46 OR (95% CI) P<0. 001 5. 2 (2. 1, 12. 8) P=0. 012 3. 3 (1. 25, 8. 9) P=0. 841 Community-acquired pneumonia is associated with an increased risk of subsequent CVEs. CI, confidence interval; CVE, cardiovascular event; MAI, microbiological agent isolation; OR, odds ratio. Fonseca A, et al. ERS Annual Meeting, September 2020, Poster 1775. G. GM. AVE. 09. 2010. 0020 41
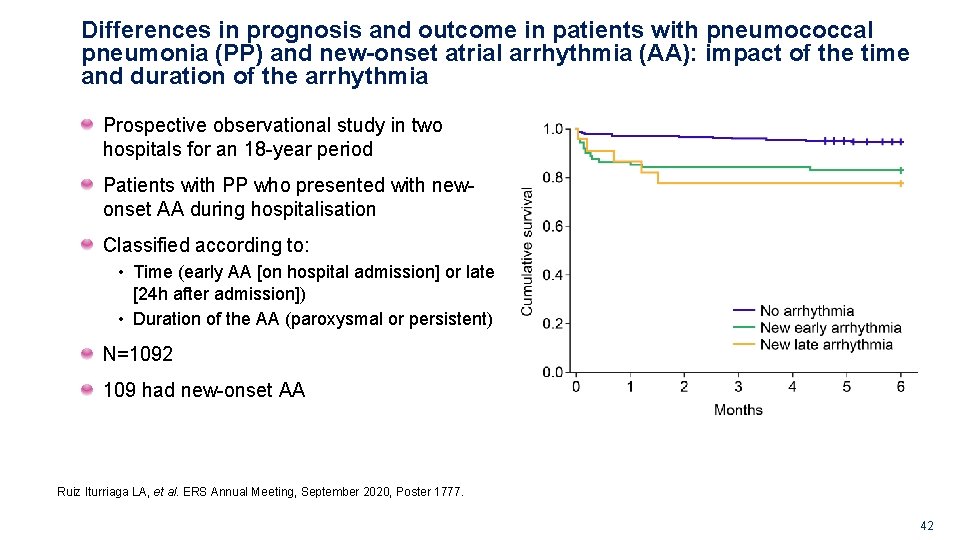
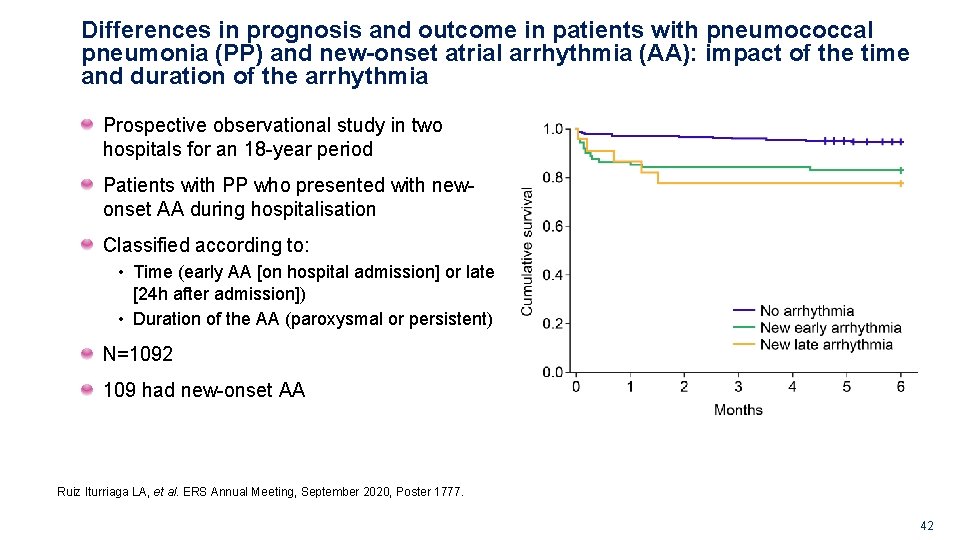
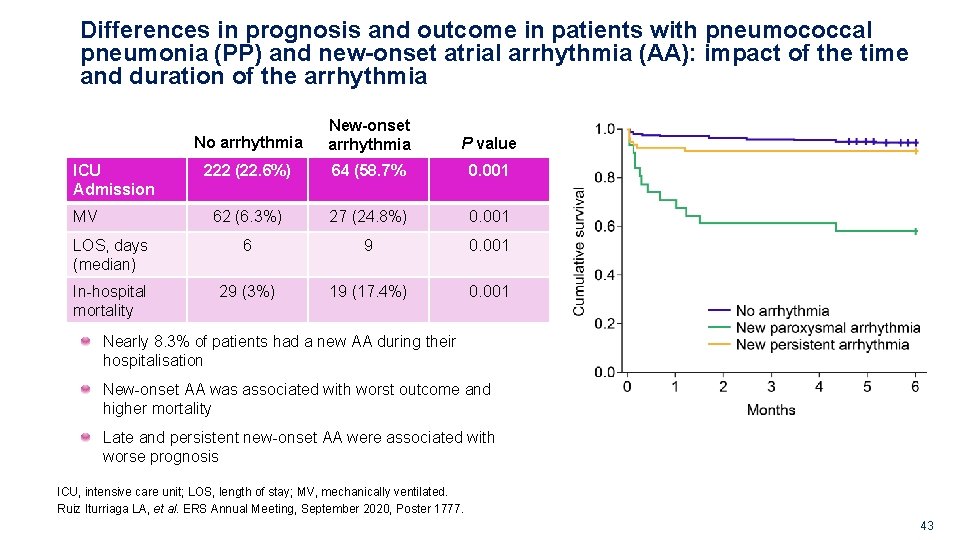
Differences in prognosis and outcome in patients with pneumococcal pneumonia (PP) and new-onset atrial arrhythmia (AA): impact of the time and duration of the arrhythmia Prospective observational study in two hospitals for an 18 -year period Patients with PP who presented with newonset AA during hospitalisation Classified according to: • Time (early AA [on hospital admission] or late [24 h after admission]) • Duration of the AA (paroxysmal or persistent) N=1092 109 had new-onset AA Ruiz Iturriaga LA, et al. ERS Annual Meeting, September 2020, Poster 1777. G. GM. AVE. 09. 2010. 0020 42
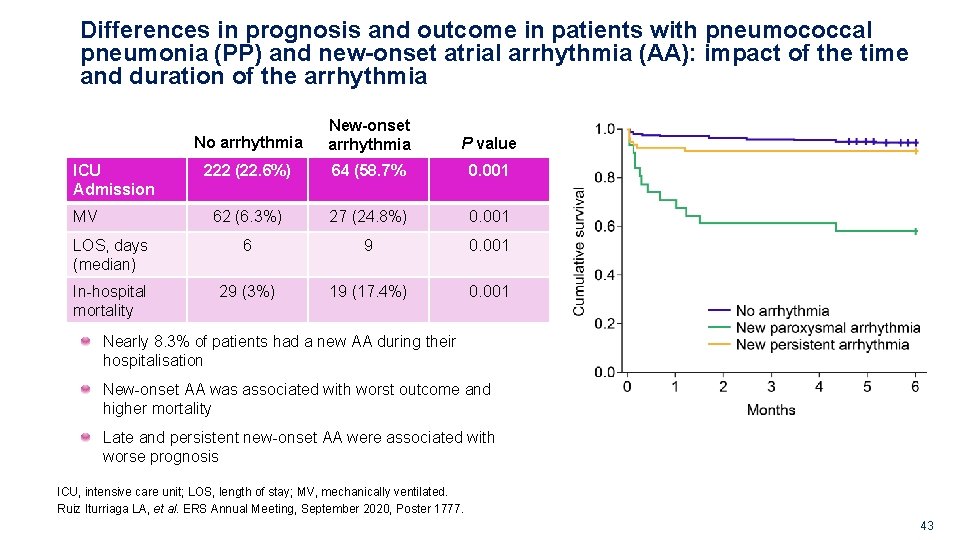
Differences in prognosis and outcome in patients with pneumococcal pneumonia (PP) and new-onset atrial arrhythmia (AA): impact of the time and duration of the arrhythmia No arrhythmia New-onset arrhythmia P value 222 (22. 6%) 64 (58. 7% 0. 001 62 (6. 3%) 27 (24. 8%) 0. 001 LOS, days (median) 6 9 0. 001 In-hospital mortality 29 (3%) 19 (17. 4%) 0. 001 ICU Admission MV Nearly 8. 3% of patients had a new AA during their hospitalisation New-onset AA was associated with worst outcome and higher mortality Late and persistent new-onset AA were associated with worse prognosis ICU, intensive care unit; LOS, length of stay; MV, mechanically ventilated. Ruiz Iturriaga LA, et al. ERS Annual Meeting, September 2020, Poster 1777. G. GM. AVE. 09. 2010. 0020 43

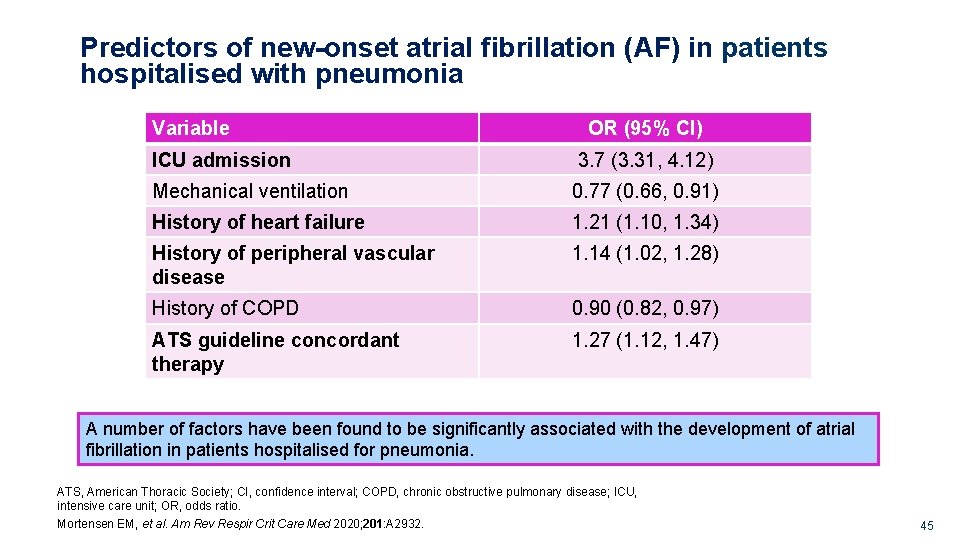
Predictors of new-onset atrial fibrillation (AF) in patients hospitalised with pneumonia Retrospective cohort study using US Department of Veterans Affairs (VA) national data including patients >65 years hospitalised with pneumonia in fiscal years 2002– 2007 Primary outcome was an incident diagnosis of AF within 30 days of admission Patients with previous diagnosis of AF were excluded 38, 679 patients analysed 2690 (7%) had a new diagnosis of AF within 30 days of admission A clinically significant number of patients hospitalised for pneumonia have incident atrial fibrillation. Mortensen EM, et al. Am Rev Respir Crit Care Med 2020; 201: A 2932. G. GM. AVE. 09. 2010. 0020 44
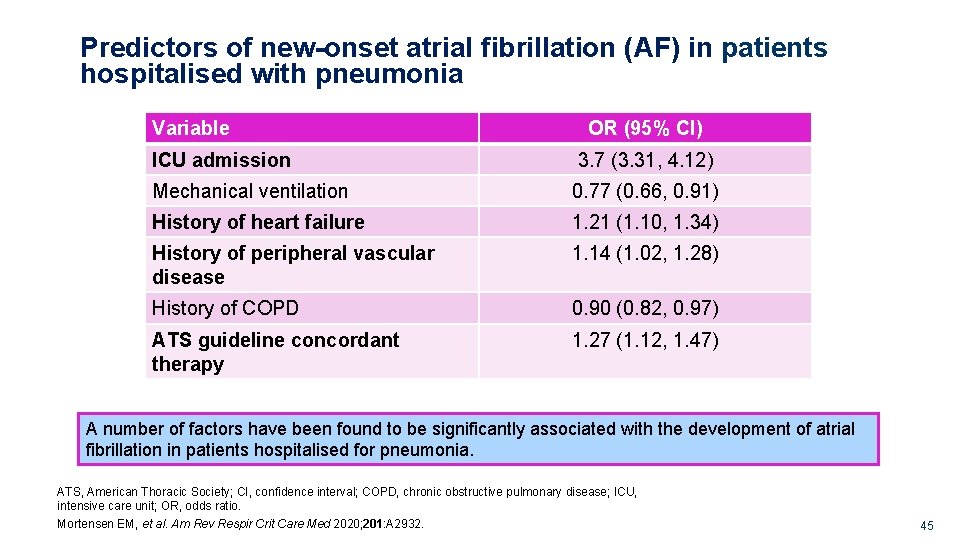
Predictors of new-onset atrial fibrillation (AF) in patients hospitalised with pneumonia Variable OR (95% CI) ICU admission 3. 7 (3. 31, 4. 12) Mechanical ventilation 0. 77 (0. 66, 0. 91) History of heart failure 1. 21 (1. 10, 1. 34) History of peripheral vascular disease 1. 14 (1. 02, 1. 28) History of COPD 0. 90 (0. 82, 0. 97) ATS guideline concordant therapy 1. 27 (1. 12, 1. 47) A number of factors have been found to be significantly associated with the development of atrial fibrillation in patients hospitalised for pneumonia. ATS, American Thoracic Society; CI, confidence interval; COPD, chronic obstructive pulmonary disease; ICU, intensive care unit; OR, odds ratio. Mortensen EM, et al. Am Rev Respir Crit Care Med 2020; 201: A 2932. G. GM. AVE. 09. 2010. 0020 45
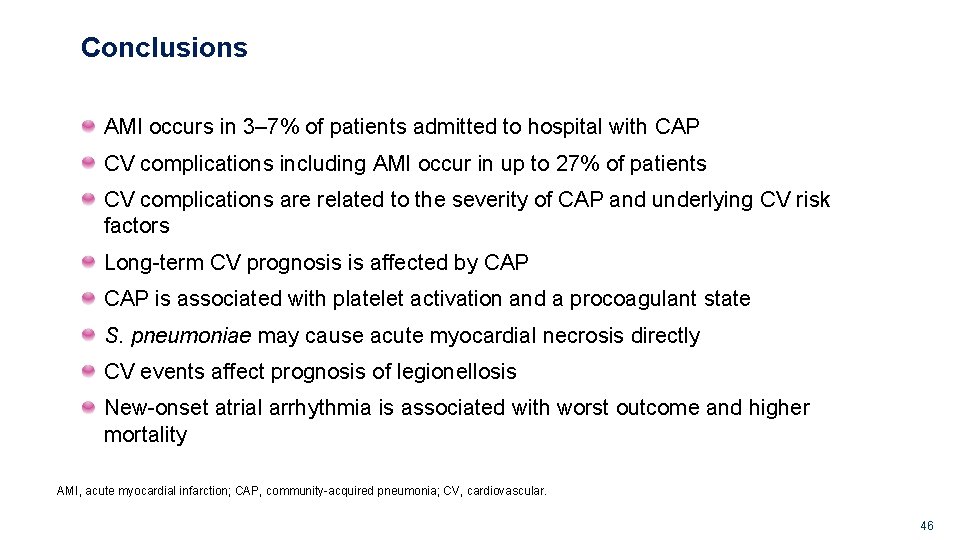
Conclusions AMI occurs in 3– 7% of patients admitted to hospital with CAP CV complications including AMI occur in up to 27% of patients CV complications are related to the severity of CAP and underlying CV risk factors Long-term CV prognosis is affected by CAP is associated with platelet activation and a procoagulant state S. pneumoniae may cause acute myocardial necrosis directly CV events affect prognosis of legionellosis New-onset atrial arrhythmia is associated with worst outcome and higher mortality AMI, acute myocardial infarction; CAP, community-acquired pneumonia; CV, cardiovascular. G. GM. AVE. 09. 2010. 0020 46
 Complications of respiratory failure
Complications of respiratory failure Respiratory zone and conducting zone
Respiratory zone and conducting zone A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Understanding the mirai botnet
Understanding the mirai botnet Bone and joint infections
Bone and joint infections Methotrexate and yeast infections
Methotrexate and yeast infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Opportunistic infections
Opportunistic infections Opportunistic infections
Opportunistic infections Storch infections
Storch infections Storch infections
Storch infections Infections opportunistes digestives
Infections opportunistes digestives Bacterial vaginosis
Bacterial vaginosis Postpartum infections
Postpartum infections Genital infections
Genital infections Genital infections
Genital infections Phagocytr
Phagocytr Acute gingival infections
Acute gingival infections Early and late complications of blood transfusion
Early and late complications of blood transfusion Blood transfusion complications
Blood transfusion complications What is an short story
What is an short story Elements of a setting
Elements of a setting Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Cardiovascular system diseases and disorders chapter 8
Cardiovascular system diseases and disorders chapter 8 Thyroid
Thyroid Eswl complications
Eswl complications Complications c section
Complications c section Duodenal switch complications
Duodenal switch complications Complications of shigellosis
Complications of shigellosis Double tracheostomy tube
Double tracheostomy tube Bronchial asthma
Bronchial asthma Who stroke definition
Who stroke definition Thoracentesis indications
Thoracentesis indications Complications of eclampsia
Complications of eclampsia Labor induction methods
Labor induction methods Post dated pregnancy complications
Post dated pregnancy complications Stitches after birth pictures
Stitches after birth pictures Complications of blood transfusion
Complications of blood transfusion Bronchoscopy complications
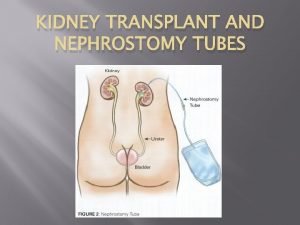
Bronchoscopy complications Nephrostomy tube complications
Nephrostomy tube complications Herpes zoster
Herpes zoster Bronchoscopy complications
Bronchoscopy complications Jim simm
Jim simm Deviated septum
Deviated septum Dialysis purpose
Dialysis purpose Phlegmasia alba dolens definition
Phlegmasia alba dolens definition Complications of cirrhosis
Complications of cirrhosis