Common Adrenal Disorders in Children Dr Sarar Mohamed








- Slides: 56
. Common Adrenal Disorders in Children Dr Sarar Mohamed FRCPCH (UK), MRCP (UK), CCST (Ire), CPT (Ire), DCH (Ire), MD Consultant Paediatric Endocrinologist & Metabolist Associate Professor of Pediatrics King Saud University
Agenda • • • Physiology of adrenal Causes of adrenal insufficiency Addison Disease Adrenal crisis Congenital adrenal hyperplasia Cushing Syndrome .


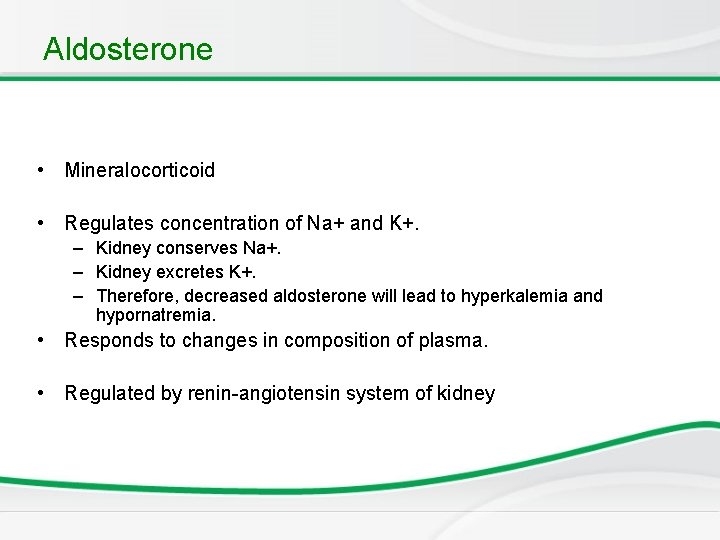
Aldosterone • Mineralocorticoid • Regulates concentration of Na+ and K+. – Kidney conserves Na+. – Kidney excretes K+. – Therefore, decreased aldosterone will lead to hyperkalemia and hypornatremia. • Responds to changes in composition of plasma. • Regulated by renin-angiotensin system of kidney
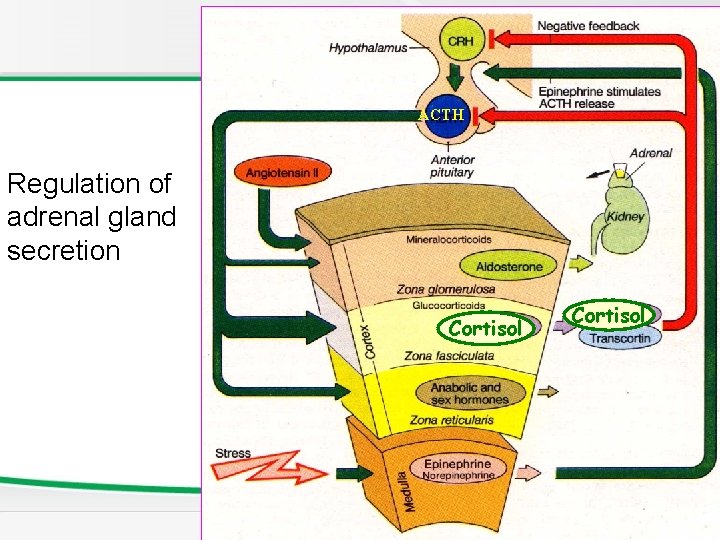
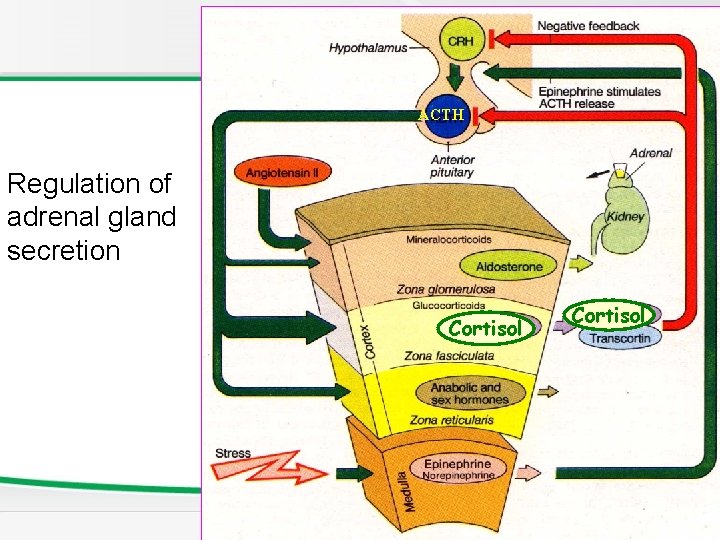
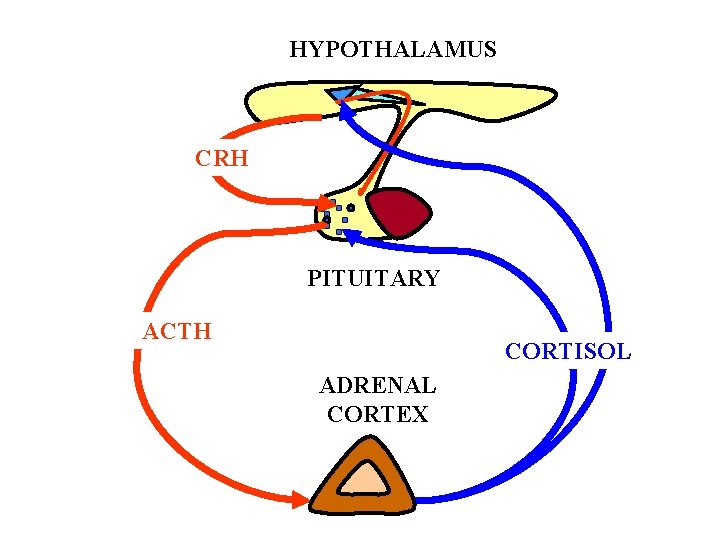
ACTH Regulation of adrenal gland secretion Cortisol
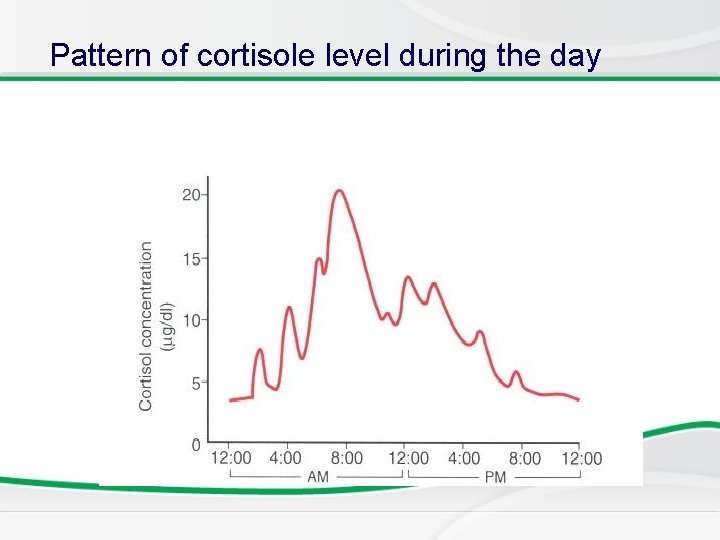
Aldosterone is regulated by the renin angiotensin system while cortisol is regulated by the hypothalamic pituitary axis. Random cortisol measurement is not useful, ACTH stimulating test to stimulate the adrenals must be done to measure it. If it’s still low after stimulation, then it suggests adrenal insuffeciency.
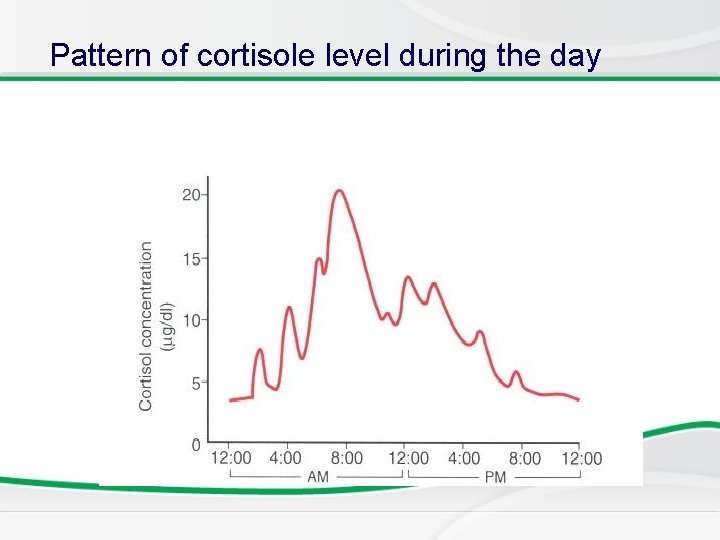
Pattern of cortisole level during the day
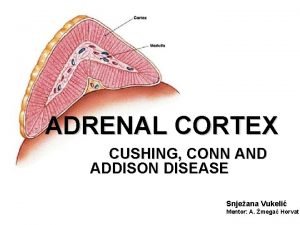
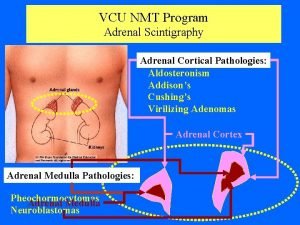
. Adrenal Dysfunction Decrease function Increase function • Adrenal insufficiency • Low cortisol, aldestrone Eg Addison disease • Cushing syndrome High Cortisol • Hyperaldosteronism High aldestrone • Pheochromocytoma High catecholamine
Causes of Adrenal insufficiency 1. Congenital adrenal hyperplasia 2. Addison disease most common cause and it’s acquired. 3. Infection (TB, sepsis) 4. Adrenoleukodystrophy very rare. .
Addison disease 1. 2. 3. 4. 5. 6. 7. Autoimmune Isolated or associated with other autoimmune disease Presents with tiredness, weight loss, skin pigmentation Hypotension, hyponatremia, hyperkalemia Aldestrone & cortisol low, high ACTH, high renin Low sodium , high potasium ACTH stimulation test: diagnostic test by giving synthetic ACTH (IV or IM) and measuring the serum cortisol at 30 and 60 minutes. In normal individuals the baseline cortisol should be doubled after the test whereas in adrenal insufficiency, the baseline (which is low) is only increased to 25% after the test. 8. Adrenal antibodies 9. Treatment : cortisol + aldosterone .

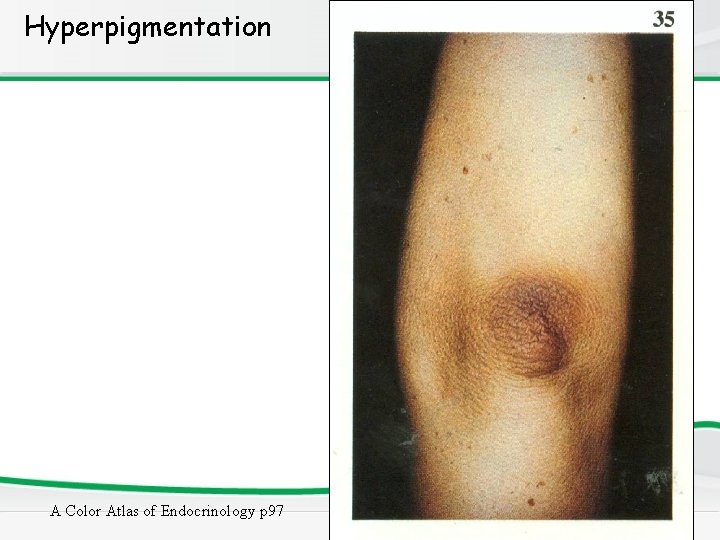
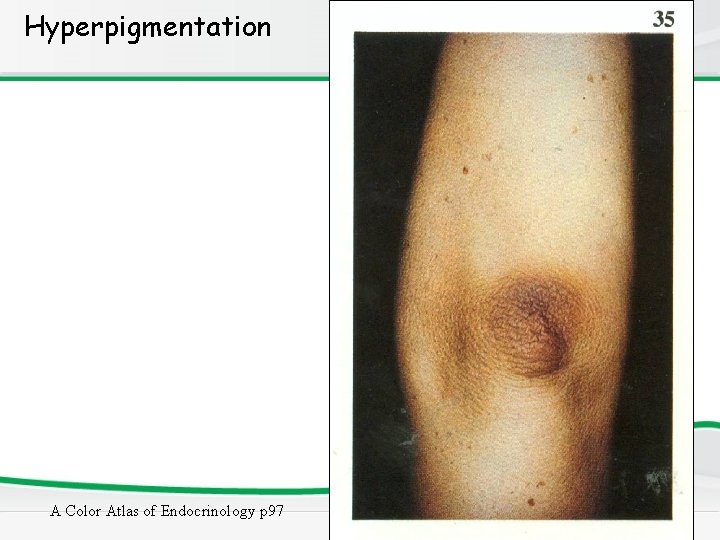
Hyperpigmentation A Color Atlas of Endocrinology p 97
Addisonian crisis • Life threatening complication • Severe vomiting and diarrhoea followed by dehydration • Low blood pressure and shock • Hypoglycemia • Loss of consciousness • Treatment: IV fluids + IV hydrocortisone
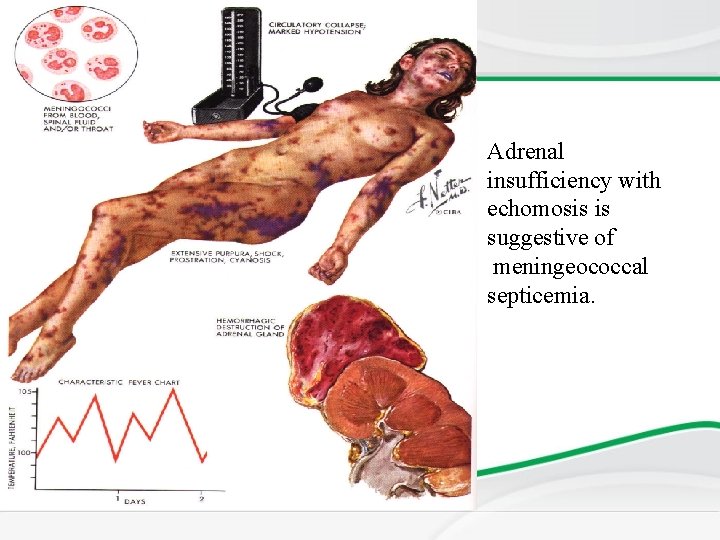
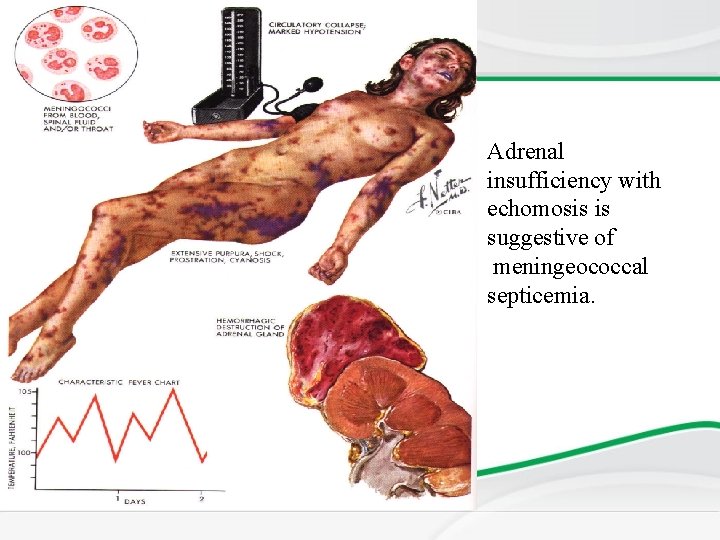
Adrenal insufficiency with echomosis is suggestive of meningeococcal septicemia.
Congenital Adrenal Hyperplasia • Family of inherited disorders of adrenal synthesis • Autosomal Recessive (M=F) • Each disorder results from a deficiency of one of the five enzymes necessary for steroid synthesis • 21 -hydroxylase is the commonest form (90– 95% of CAH cases)
Steroid biosynthetic enzymes 1) Cholesterol side chain cleavage= desmolase) 2) 3 -Hydoxysteroid dehydrogenase 3) 17 hydroxylase 4) 21 -Hydroxylase 5) 11 -Hydroxylase
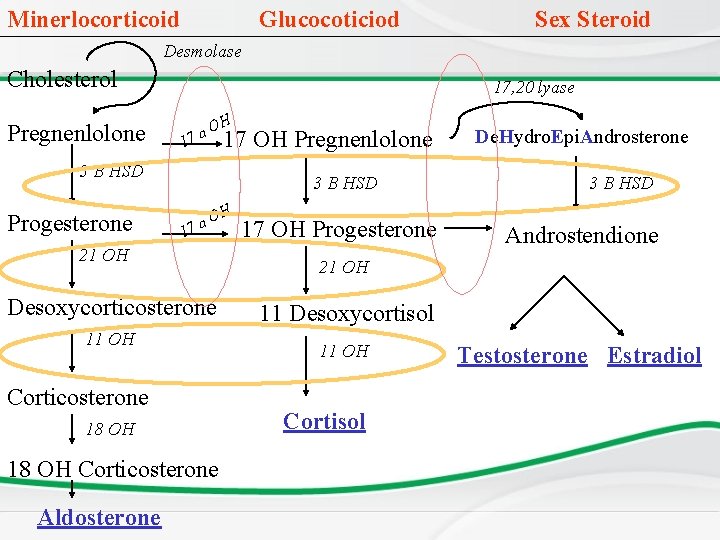
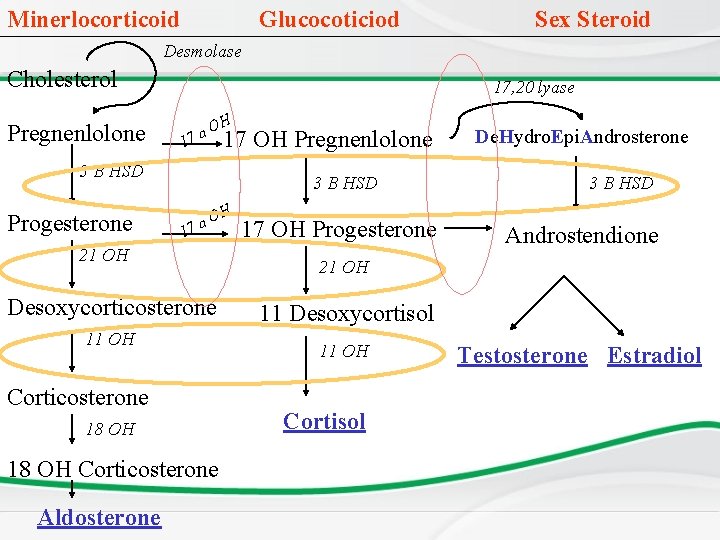
Minerlocorticoid Glucocoticiod Sex Steroid Desmolase Cholesterol Pregnenlolone 17, 20 lyase 1 O 7 a H 17 OH Pregnenlolone 3 B HSD Progesterone 3 B HSD 1 O 7 a 21 OH Desoxycorticosterone 11 OH Corticosterone 18 OH Corticosterone Aldosterone H 17 OH Progesterone De. Hydro. Epi. Androsterone 3 B HSD Androstendione 21 OH 11 Desoxycortisol 11 OH Cortisol Testosterone Estradiol
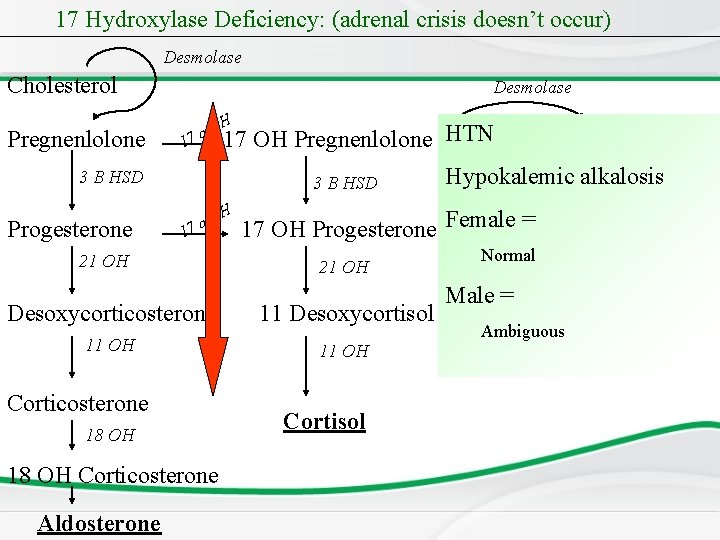
Desmolase is the first step in the pathway and if deficient all three • pathways will be stopped. Only female genitalia because no androgens at all. 3 BHSD deficiency: all 3 enzymes will be absent but will also present • with ambiguous genitalia because of high levels of DHEA 17 a. OH: cortisol androgens are deficient and males will present with • ambiguous genitalia. Aldosterone is present; therefore, they will not develop adrenal crisis and will have hypertension due to the excess aldosterone levels.
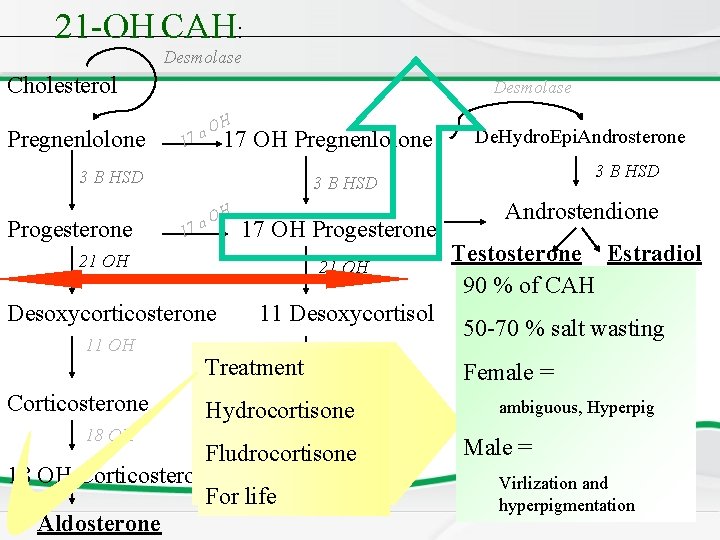
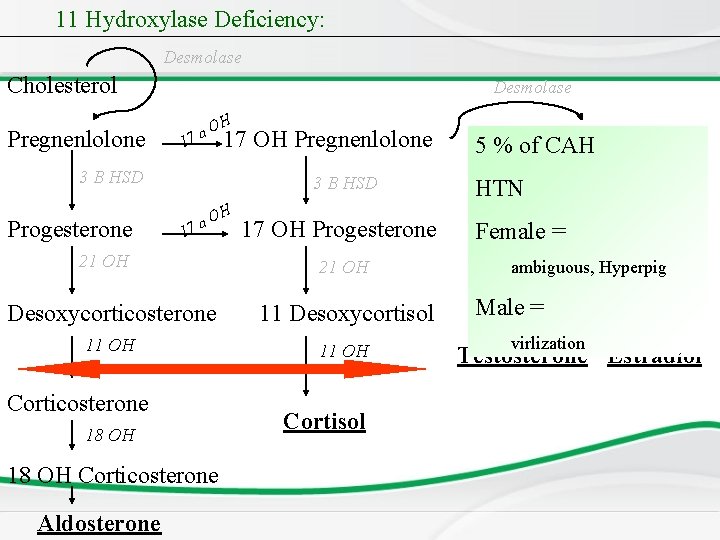
21 a. OH: is the commonest cause of CAH, both cortisol and aldosterone • will be missing, the pathway will be shifted to the production of androgens which will be manifested as ambiguous genitalia in females and hyper-pigmentation and virilization in males. 11 a. OH: both cortisol and aldosterone will be deficient, but there will be • accumulation of the Desoxycorticosterone which has an aldosterone like activity, therefore they will present hypertension, hypernatremia and hypokalemia), but it similar to 21 OH in that they both present with ambiguous genitalia and low cortisol levels. Hypertension is only present in 11 And 17 OH deficiency. •
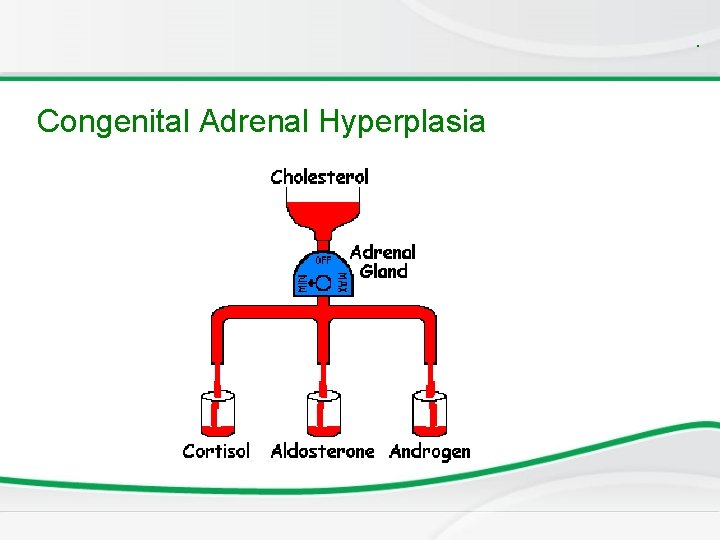
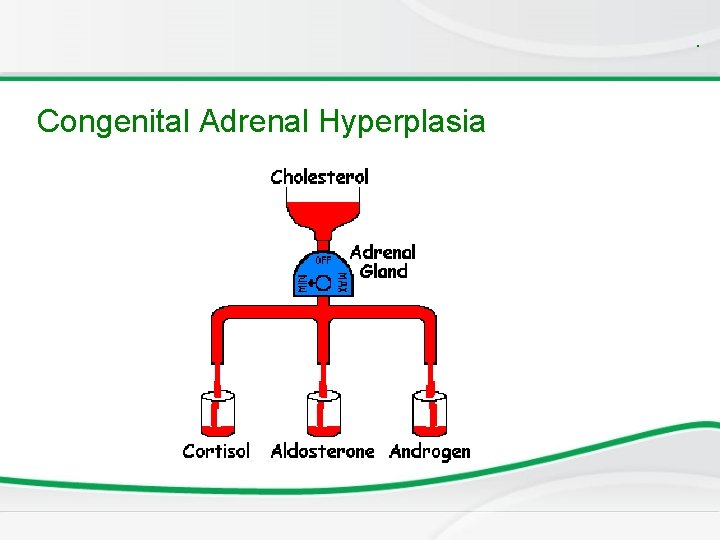
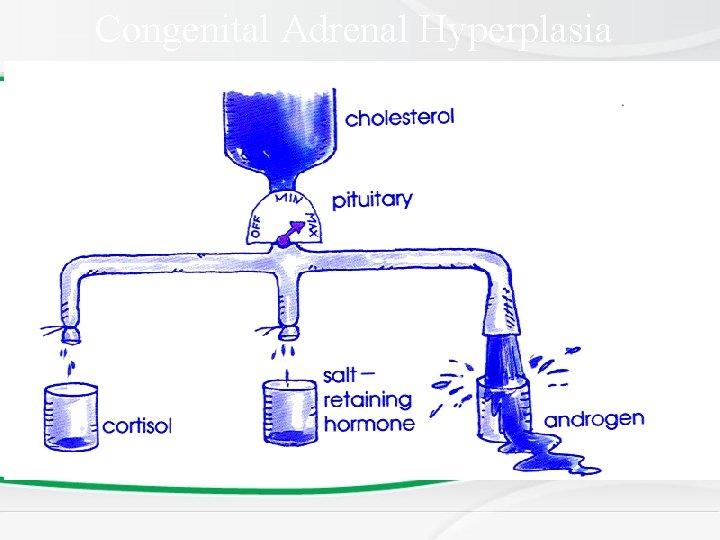
. Congenital Adrenal Hyperplasia
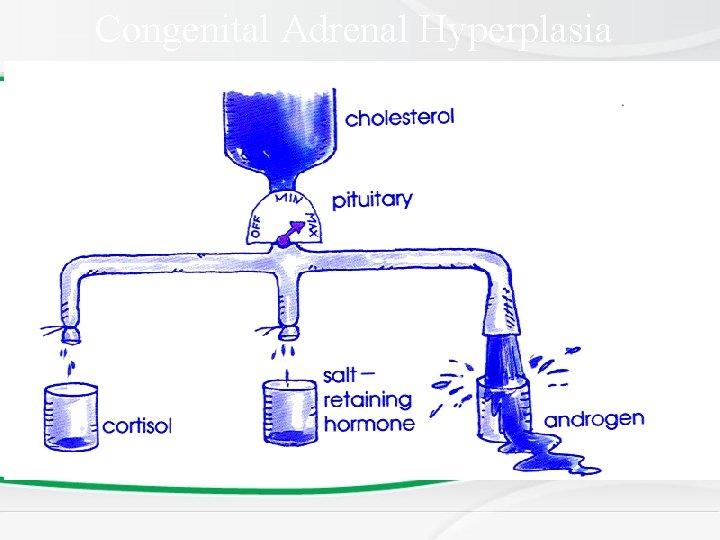
Congenital Adrenal Hyperplasia
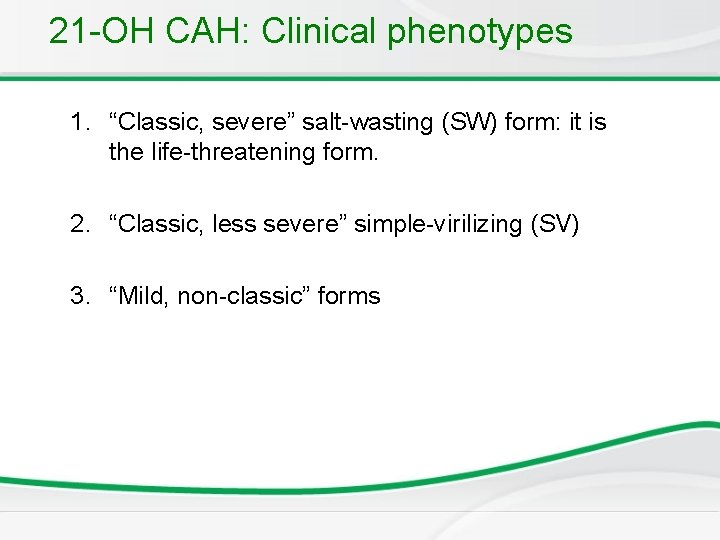
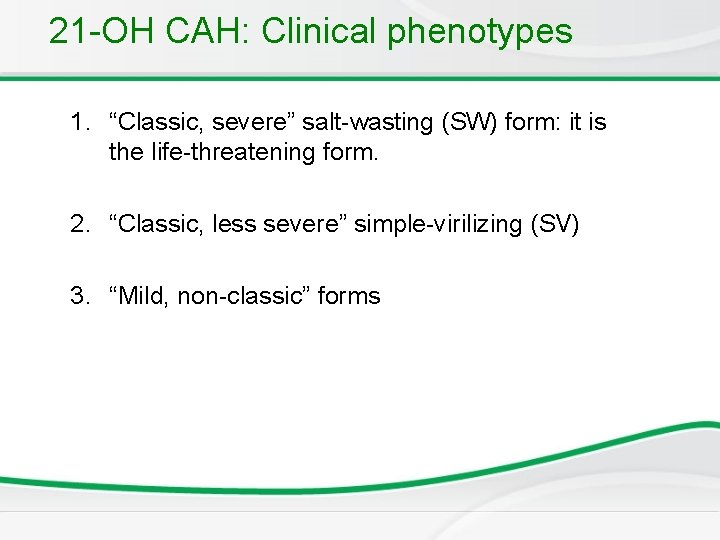
21 -OH CAH: Clinical phenotypes 1. “Classic, severe” salt-wasting (SW) form: it is the life-threatening form. 2. “Classic, less severe” simple-virilizing (SV) 3. “Mild, non-classic” forms
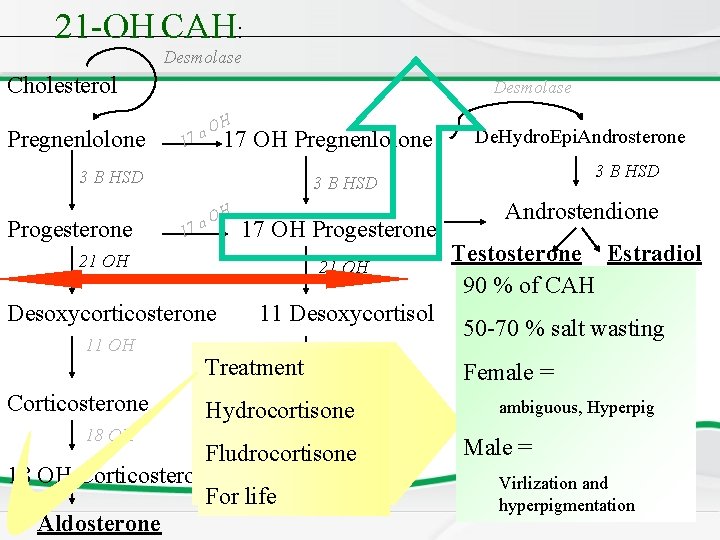
21 -OH CAH: Desmolase Cholesterol Pregnenlolone Desmolase 1 O 7 a H 17 OH Pregnenlolone 3 B HSD Progesterone 3 B HSD 1 O 7 a H 17 OH Progesterone 21 OH Desoxycorticosterone 11 Desoxycortisol 11 OH Corticosterone De. Hydro. Epi. Androsterone Treatment Hydrocortisone Cortisol 18 OH Fludrocortisone 18 OH Corticosterone For life Aldosterone Androstendione Testosterone Estradiol 90 % of CAH 50 -70 % salt wasting Female = ambiguous, Hyperpig Male = Virlization and hyperpigmentation
Salt wasting form • Salt wasting form • • • – Adrenal crisis in the 1 st-4 th weeks of life, peaking at 3 rd – Poor feeding, vomiting, diarrhea, FTT Dehydration Shock Electrolytes imbalance – Hyponatremia – Hyperkalaemia Hypoglycemia Hyperpigementations – If untreated circulatory collapse shock death – Permanent brain injury due to shock and hypoglycemia lower IQ
Simple virilizing form 21 -OH CAH • Simple virilizing form – No adrenal-insufficiency symptoms unless subjected to severe stress but exhibit virilization – Girls present with ambiguous genitalia at birth – Males usually not diagnosed until later (virilization, precocious, growth acceleration) – Advanced skeletal age diagnosed late short adult stature
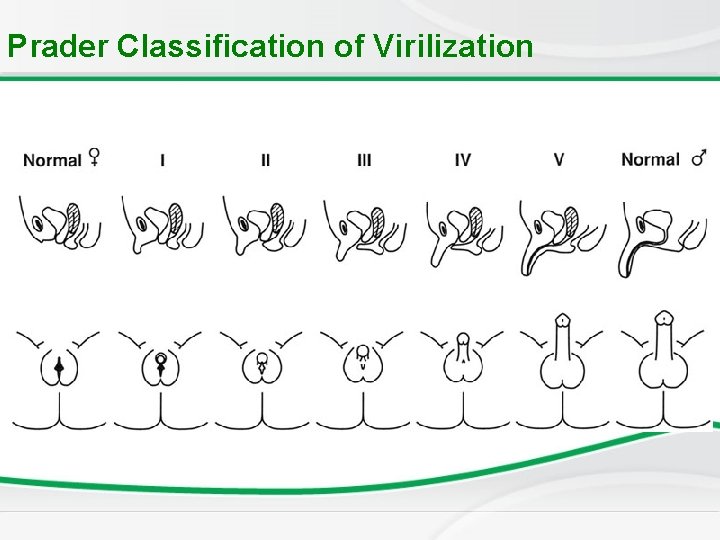
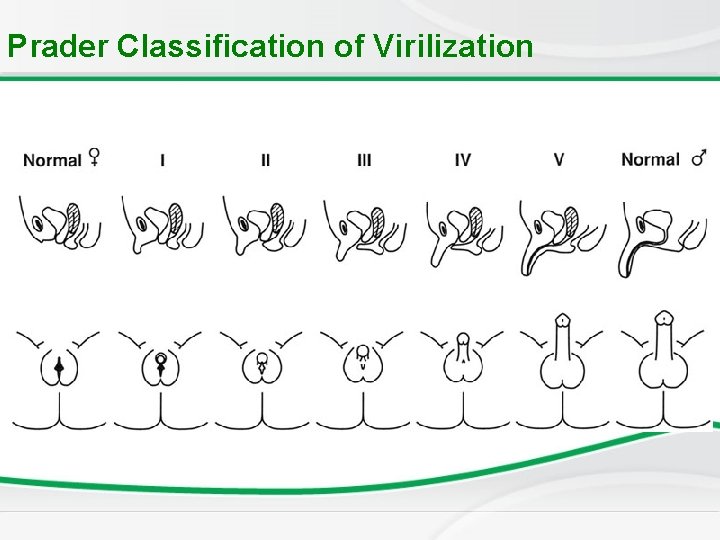
Prader Classification of Virilization
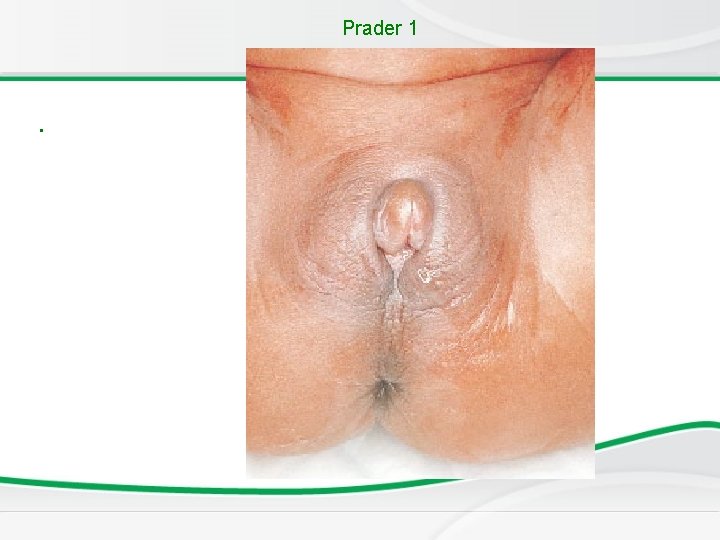
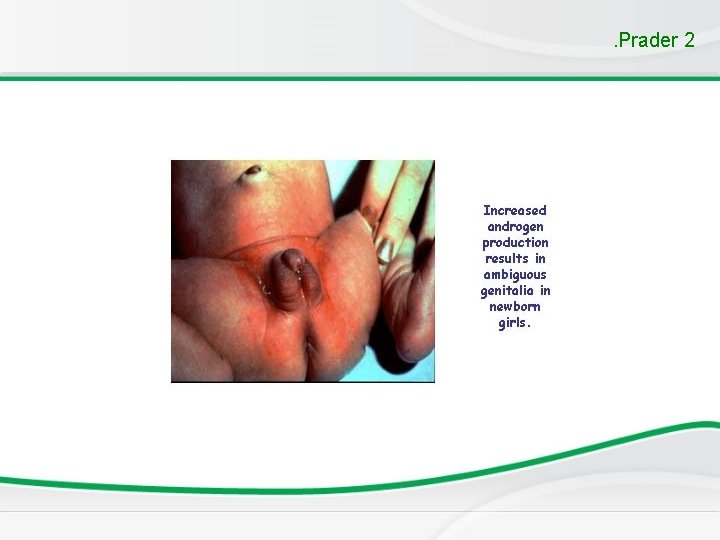
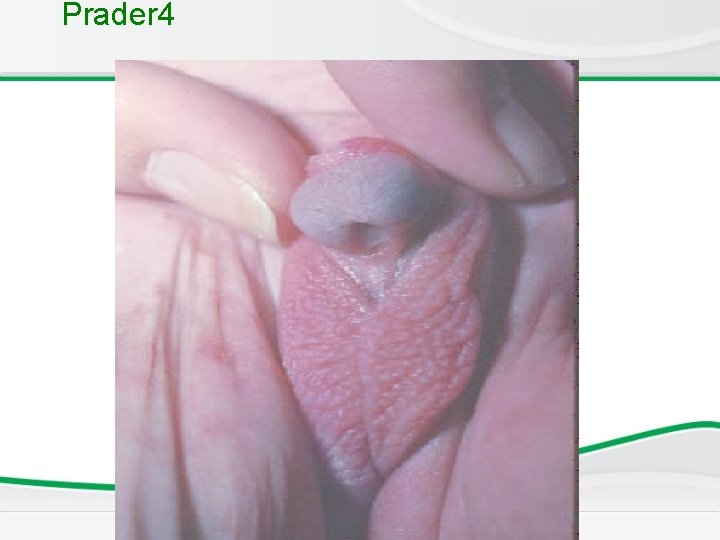
Newborn Screening • Type 1: increase in the size of the clitoris. • Type 2: more increase in the size of the clitoris. • Type 3: one opening, the vagina and clitoris opens in the same opening. • Type 4: one opening and more increase in the size, starts looking as a penis. • Type 5: looks like male genitalia with no testis.
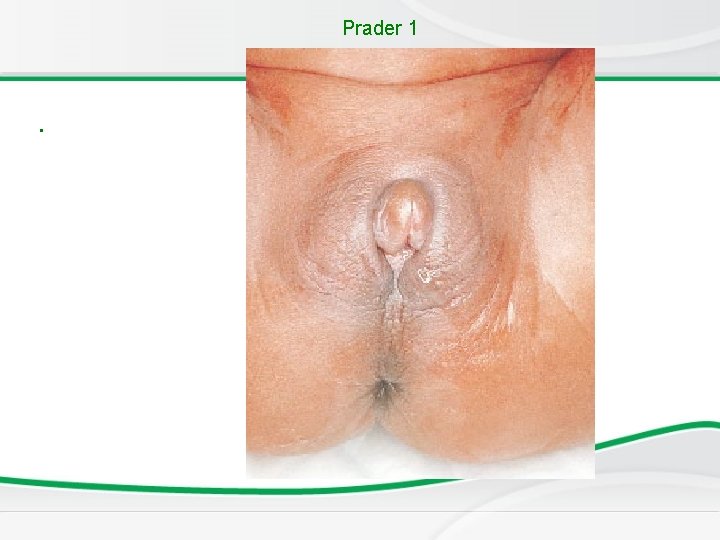
Prader 1 .
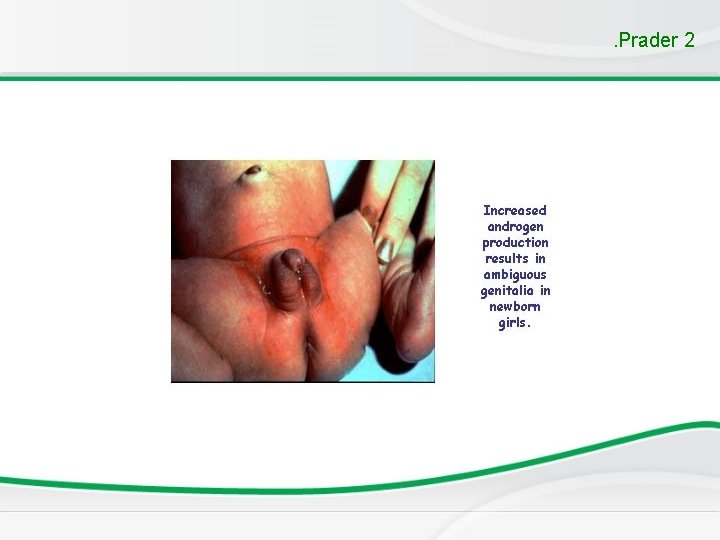
. Prader 2
Prader 3 • .
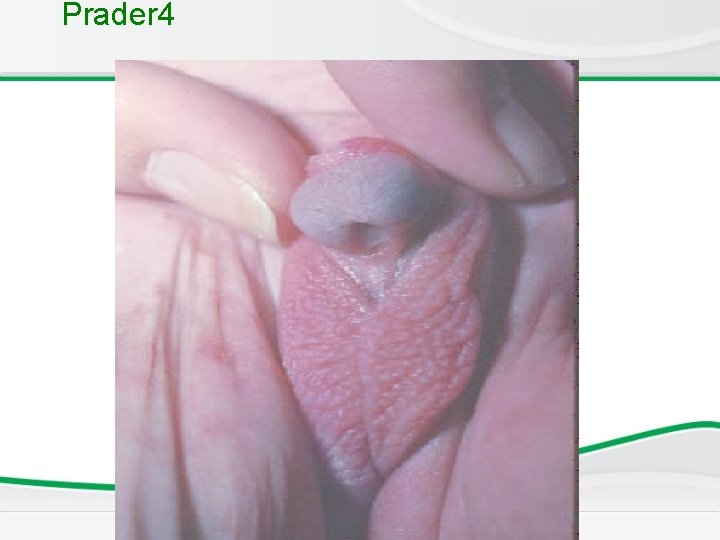
Prader 4

Prader 5
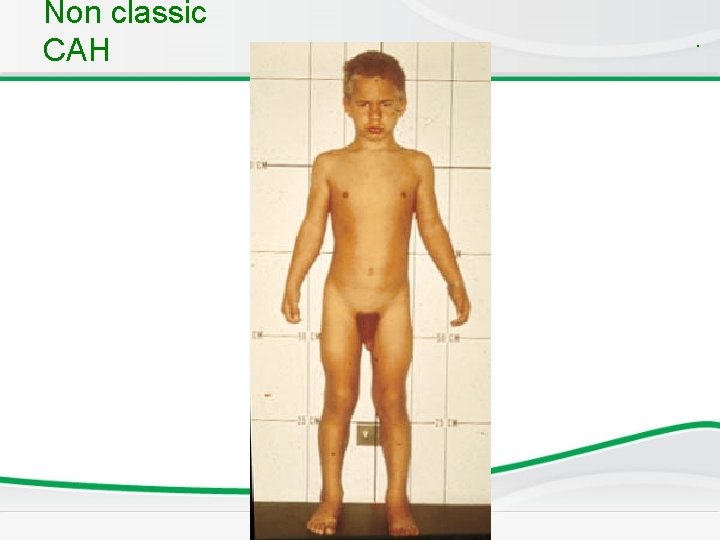
Nonclassical CAH q. Residual enzyme activity. q. Non-salt losing CAH q. Presents late in childhood with precocious pubic hair and/or clitoromegaly and accelerated growth. q. Present in adolescence or adulthood with varying virilizing symptoms ranging from oligomenorrhea to hirusutism and infertility.
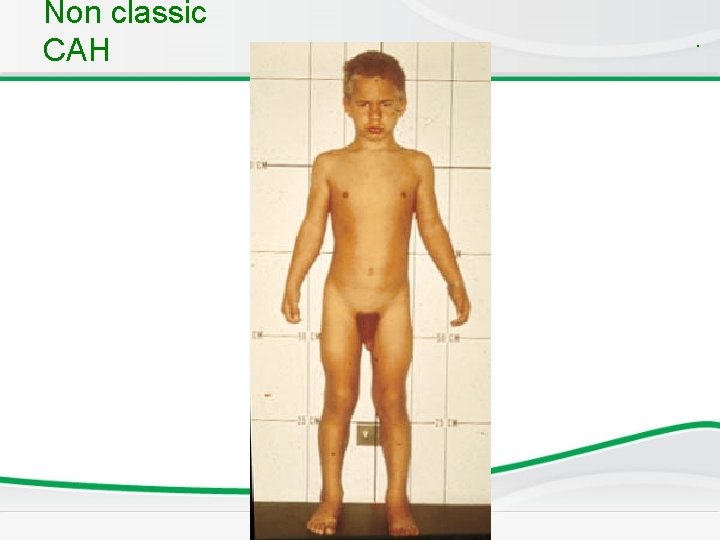
Non classic CAH .
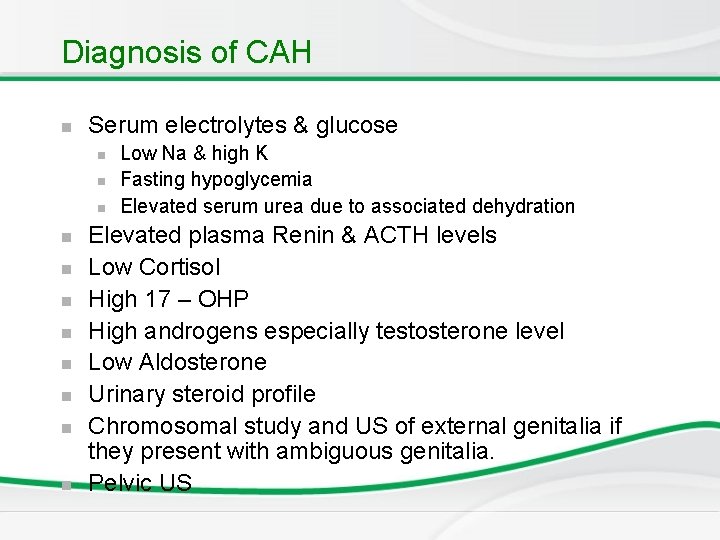
Diagnosis of CAH n Serum electrolytes & glucose n n n Low Na & high K Fasting hypoglycemia Elevated serum urea due to associated dehydration Elevated plasma Renin & ACTH levels Low Cortisol High 17 – OHP High androgens especially testosterone level Low Aldosterone Urinary steroid profile Chromosomal study and US of external genitalia if they present with ambiguous genitalia. Pelvic US
Management • Hydrocortisone • Fludrocortisone 0. 05 - 0. 2 mg/day • Triple dose of hydrocortisone and mineralcorticoids during stress or very sick. • During adrenal crisis intravenous hydrocortisone and IV fluid • Surgery for female external genitalia can be done in the 1 st year of life. • Antenatal diagnosis and treatment
Newborn screening for CAH • Neonatal screening by filter paper on 3 rd day of life • 17 Hydroxyprogestrone blood level (17 OHP) .
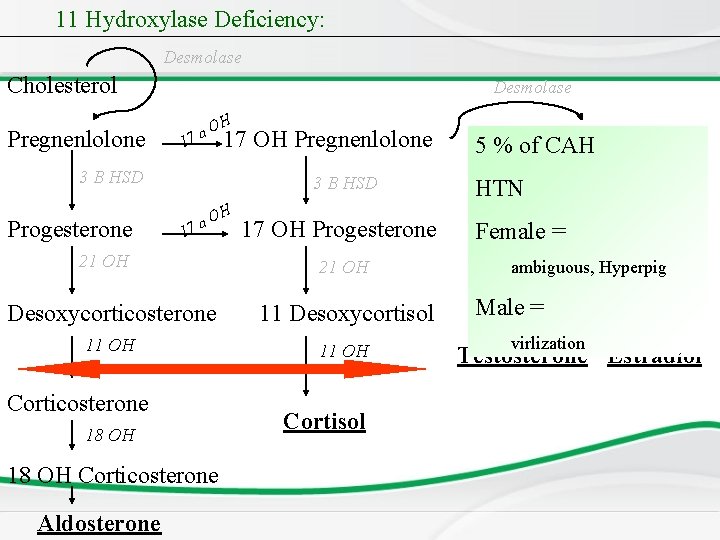
11 Hydroxylase Deficiency: Desmolase Cholesterol Pregnenlolone Desmolase 1 O 7 a H 17 OH Pregnenlolone 3 B HSD Progesterone 3 B HSD 1 O 7 a 21 OH H 17 OH Progesterone 21 OH Desoxycorticosterone 11 Desoxycortisol 11 OH Corticosterone 18 OH Corticosterone Aldosterone Cortisol De. Hydro. Epi. Androsterone 5 % of CAH HTN 3 B HSD Female = Androstendione ambiguous, Hyperpig Male = virlization Testosterone Estradiol
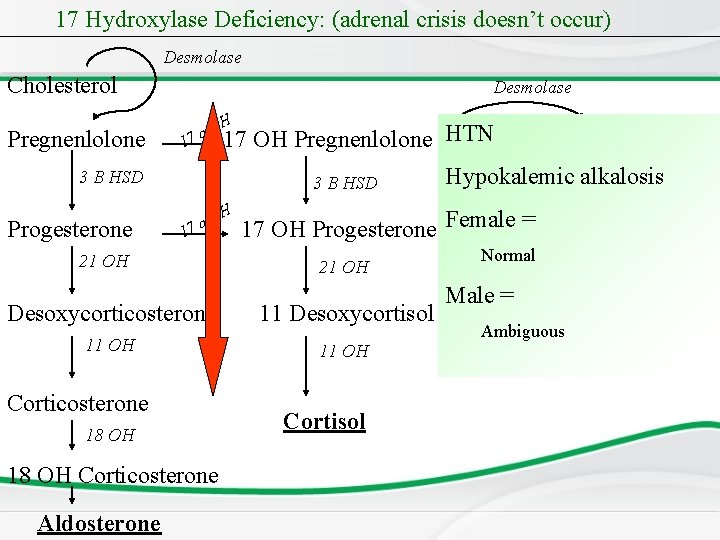
17 Hydroxylase Deficiency: (adrenal crisis doesn’t occur) Desmolase Cholesterol Pregnenlolone Desmolase 1 O 7 a H De. Hydro. Epi. Androsterone 17 OH Pregnenlolone HTN 3 B HSD Progesterone 3 B HSD 1 O 7 a 21 OH H 17 OH Progesterone Female = Androstendione Normal 21 OH Desoxycorticosterone 11 Desoxycortisol 11 OH Corticosterone 18 OH Corticosterone Aldosterone Hypokalemic alkalosis 3 B HSD Cortisol Male = Ambiguous Testosterone Estradiol
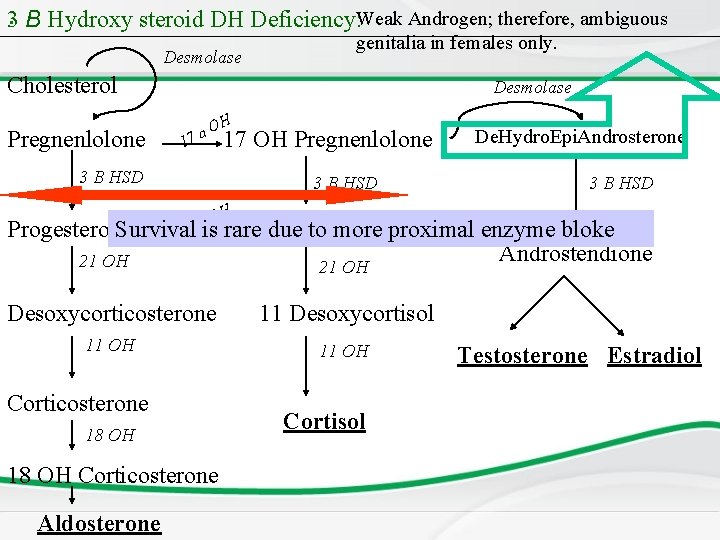
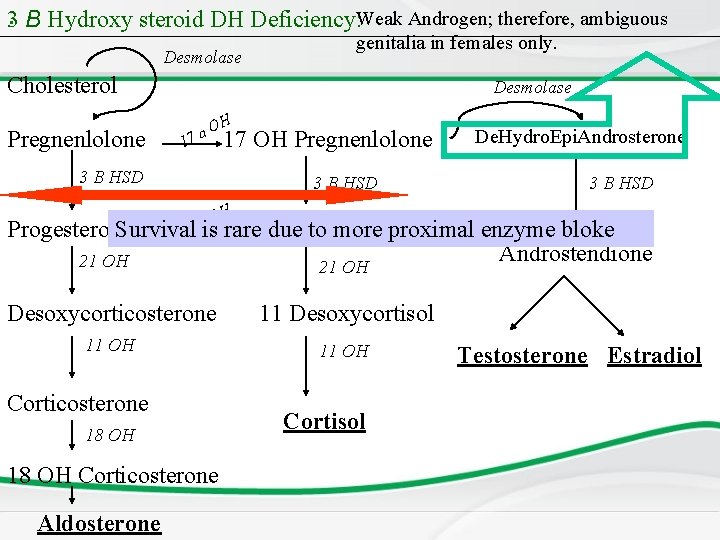
3. B Hydroxy steroid DH Deficiency: Weak Androgen; therefore, ambiguous Desmolase genitalia in females only. Cholesterol Pregnenlolone Desmolase 1 O 7 a H 17 OH Pregnenlolone 3 B HSD O 7 a De. Hydro. Epi. Androsterone 3 B HSD H Progesterone Survival 17 due OH to Progesterone more proximal enzyme bloke 1 is rare Androstendione 21 OH Desoxycorticosterone 11 Desoxycortisol 11 OH Corticosterone 18 OH Corticosterone Aldosterone Cortisol Testosterone Estradiol
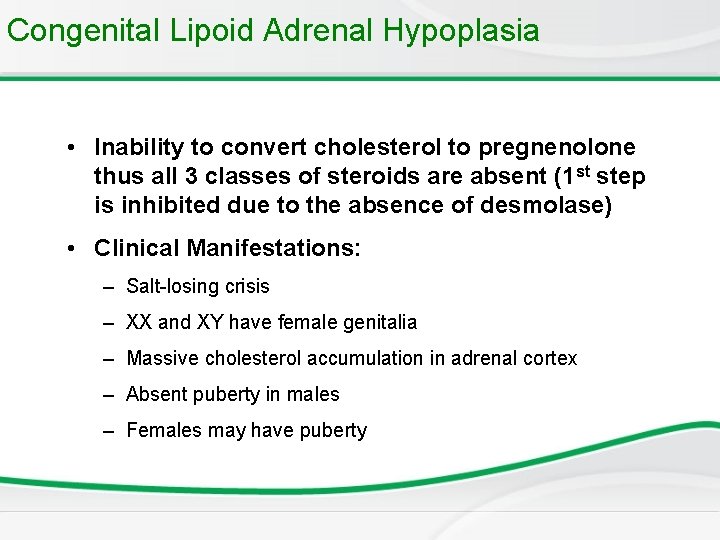
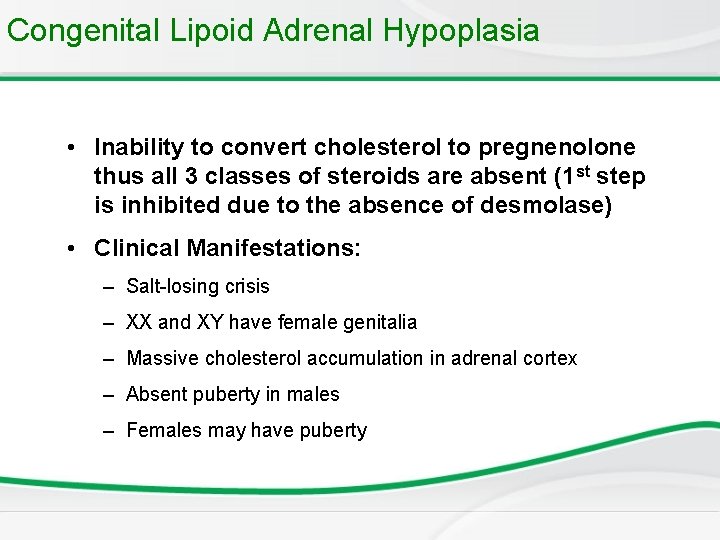
Congenital Lipoid Adrenal Hypoplasia • Inability to convert cholesterol to pregnenolone thus all 3 classes of steroids are absent (1 st step is inhibited due to the absence of desmolase) • Clinical Manifestations: – Salt-losing crisis – XX and XY have female genitalia – Massive cholesterol accumulation in adrenal cortex – Absent puberty in males – Females may have puberty
Harvey Williams Cushing (1869 -1939)
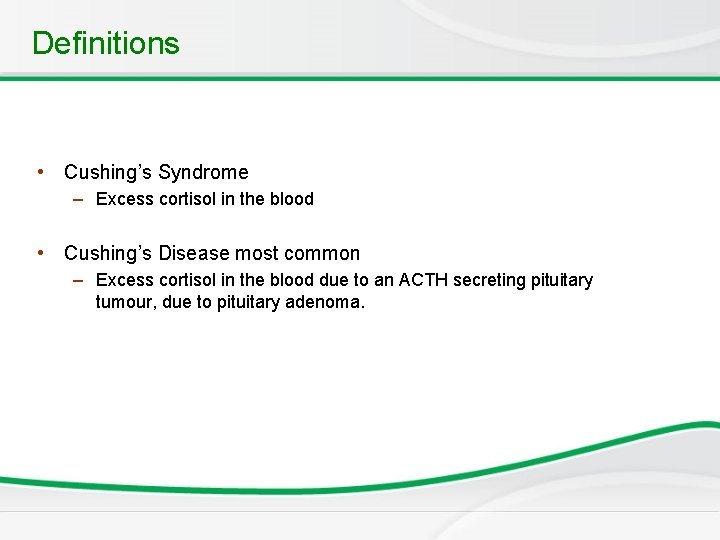
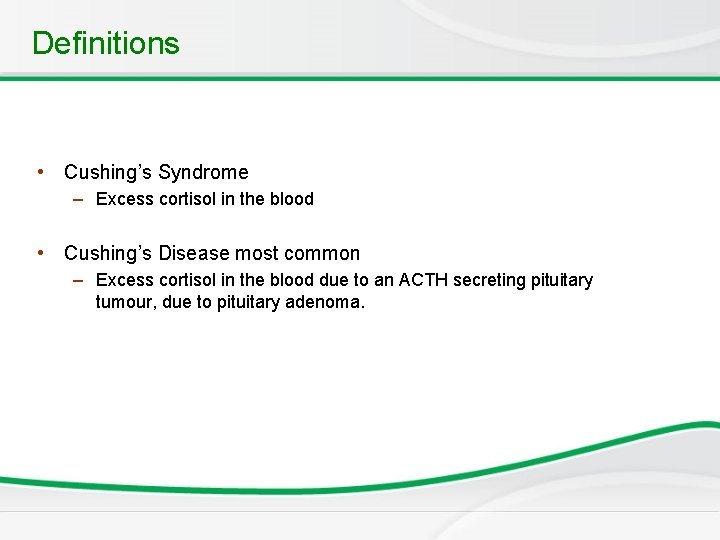
Definitions • Cushing’s Syndrome – Excess cortisol in the blood • Cushing’s Disease most common – Excess cortisol in the blood due to an ACTH secreting pituitary tumour, due to pituitary adenoma.
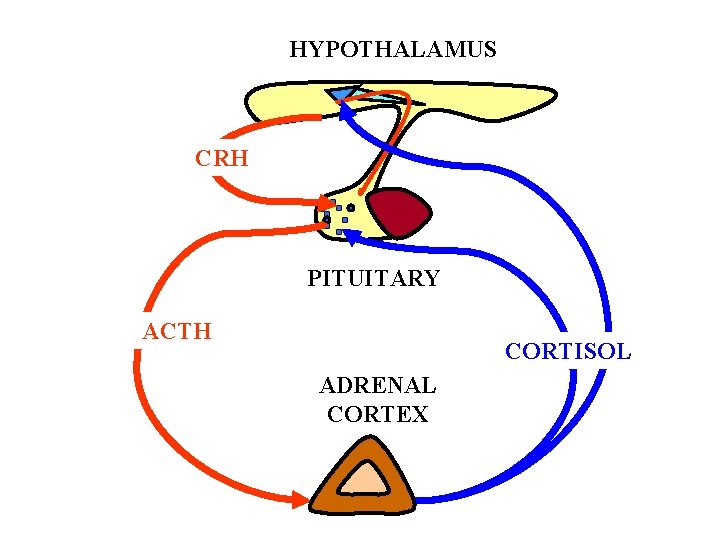
HYPOTHALAMUS CRH PITUITARY ACTH CORTISOL ADRENAL CORTEX
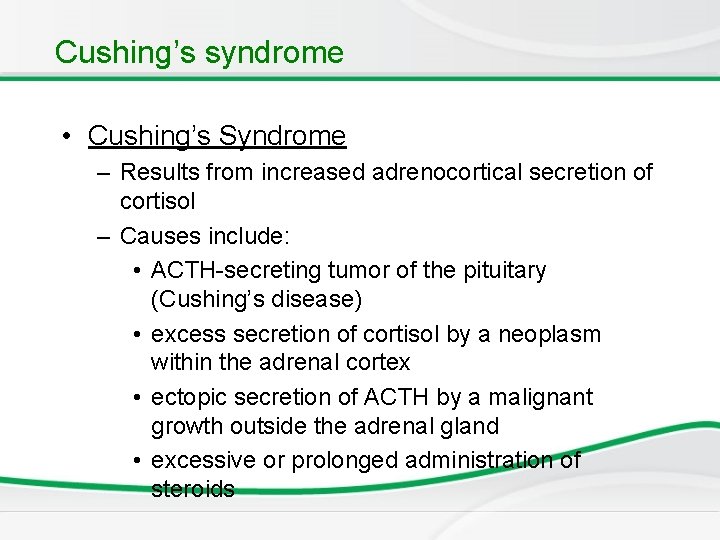
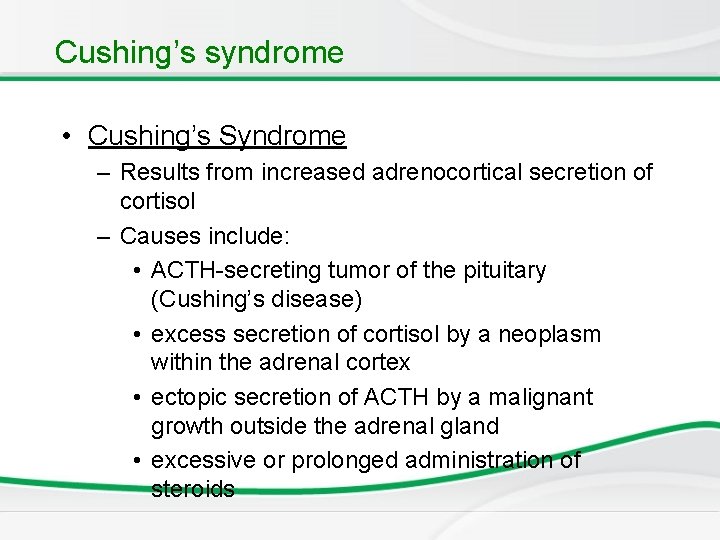
Cushing’s syndrome • Cushing’s Syndrome – Results from increased adrenocortical secretion of cortisol – Causes include: • ACTH-secreting tumor of the pituitary (Cushing’s disease) • excess secretion of cortisol by a neoplasm within the adrenal cortex • ectopic secretion of ACTH by a malignant growth outside the adrenal gland • excessive or prolonged administration of steroids

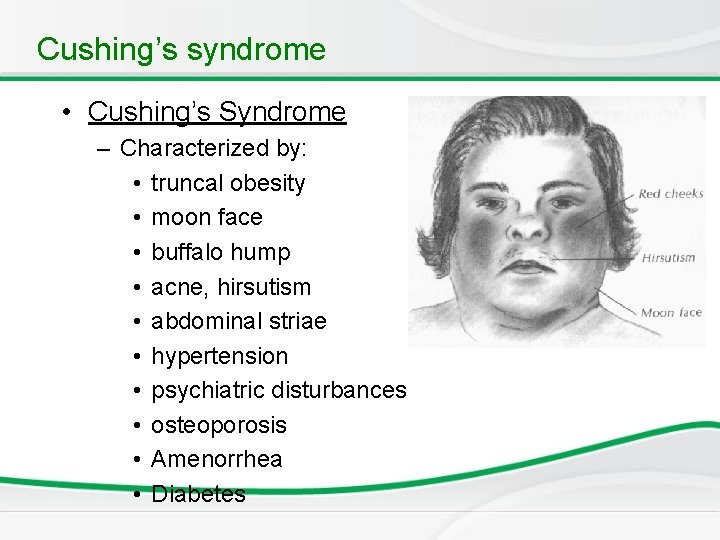
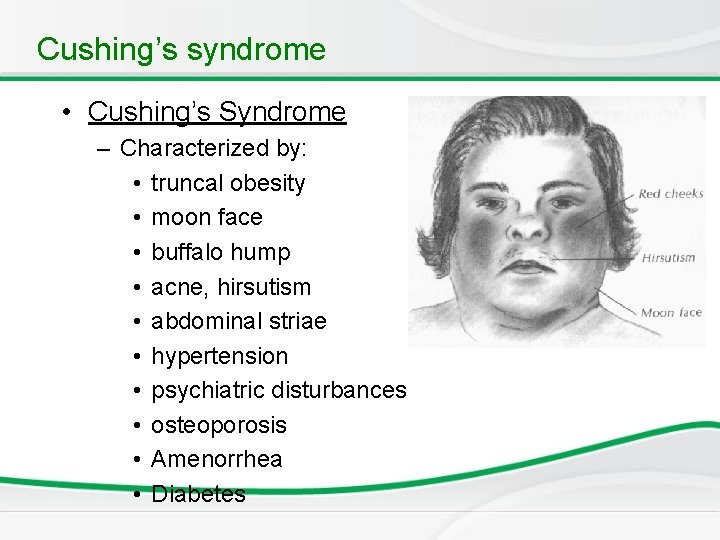
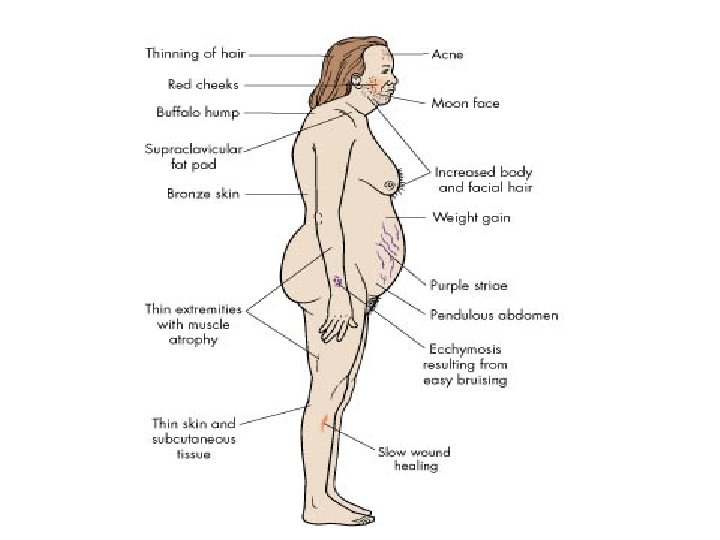
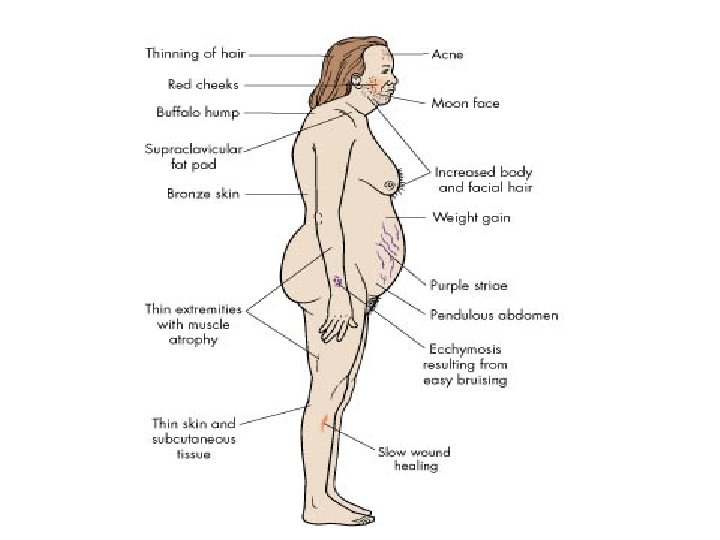
Cushing’s syndrome • Cushing’s Syndrome – Characterized by: • truncal obesity • moon face • buffalo hump • acne, hirsutism • abdominal striae • hypertension • psychiatric disturbances • osteoporosis • Amenorrhea • Diabetes
www. saadmedical. com


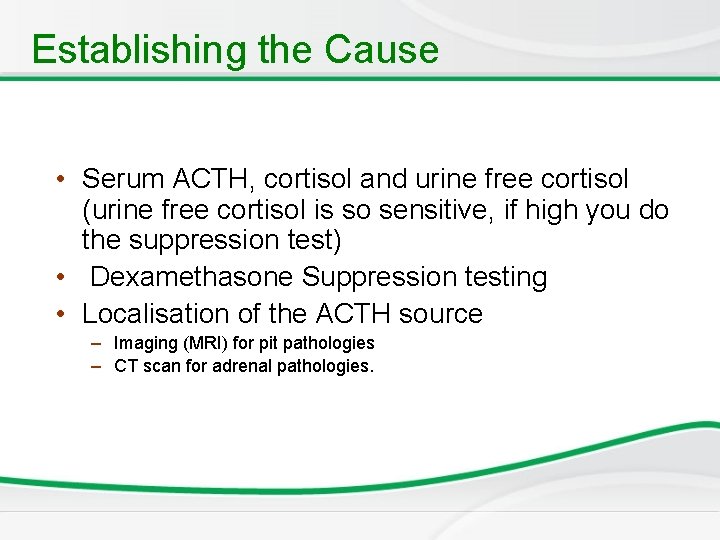
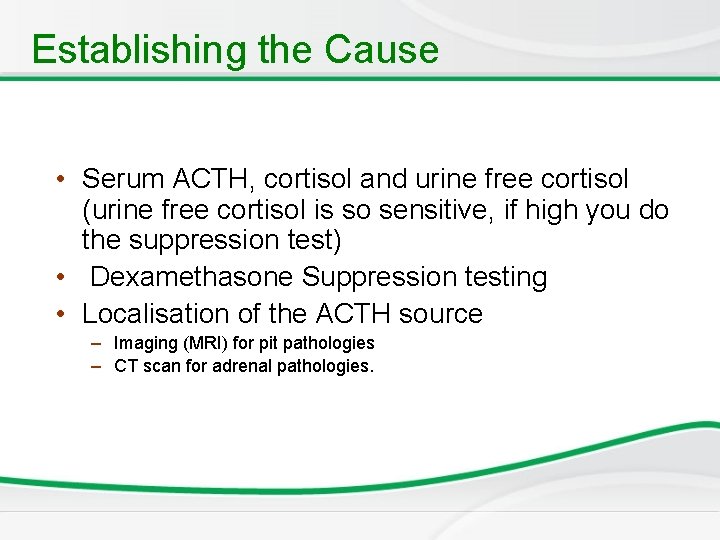
Establishing the Cause • Serum ACTH, cortisol and urine free cortisol (urine free cortisol is so sensitive, if high you do the suppression test) • Dexamethasone Suppression testing • Localisation of the ACTH source – Imaging (MRI) for pit pathologies – CT scan for adrenal pathologies.
. Treatment of Cushing’s syndrome • Treatment of underline cause • Surgery for neoplasia
Data interpretation A 2 week old infant presents to hospital with 1 week history of persistent vomiting and lethargy. On examination the infant is 10% dehydrated and unwell. He has normal male genitalia and both gonads are palpable blood results are: Sodium 115 mmol/L Glucose 3. 8 mmol/L; hypoglycemic <2. 7 mmol/L Potassium 7. 2 mmol? L What two investigations would be most likely to confirm the diagnosis? How do you treat?
Newborn Screening • This case could be CAH or hyponatremic dehydration, so now we added the presence of hyperpigmentation to the scenario to confirm CAH. • The most important 2 investigations are: A. 17 hydroxyprogesterone as a screening test, it will be high (blockage of 21 OH will lead to its accumulation of substrate before. B. ACTH stimulation test to confirm the diagnosis. • DNA study (CYP 21) for 21 OH deficiency is done at the end. • Treatment: I. V fluid and I. V hydrocortisone for the treatment of the crisis, and replacement of cortisol and aldosterone for life. • Not addisons because it doesn’t present in the first few months of life.

 Fahri sarar
Fahri sarar In what situation should nail service not be performed
In what situation should nail service not be performed Kolekalsiferol
Kolekalsiferol Hypothalamus
Hypothalamus Dr wilson adrenal rebuilder side effects
Dr wilson adrenal rebuilder side effects Conn's syndrome
Conn's syndrome Adrenal sympathetic pathway
Adrenal sympathetic pathway Caso clínico sop
Caso clínico sop Virilisation in females
Virilisation in females Nursing management of adrenal tumor
Nursing management of adrenal tumor Adrenal hormone pathway
Adrenal hormone pathway What causes addisons disease
What causes addisons disease Cells of adrenal gland
Cells of adrenal gland Thyroiditis
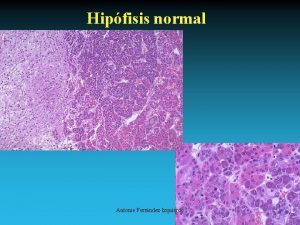
Thyroiditis Adrenal bez histolojisi
Adrenal bez histolojisi Adrenal bez embriyolojisi
Adrenal bez embriyolojisi Chromaffin cells
Chromaffin cells Peptit ve protein yapılı hormonlar
Peptit ve protein yapılı hormonlar Adrenal gland epithelium
Adrenal gland epithelium Summary of adrenal gland
Summary of adrenal gland Adrenal gland
Adrenal gland Adrenal tumour
Adrenal tumour Adrenogenital sendrom
Adrenogenital sendrom Adrenal cortex develops from
Adrenal cortex develops from Coelomic epithelium
Coelomic epithelium Objective of stress management
Objective of stress management Oktay eray
Oktay eray Adrenal glands
Adrenal glands Adrenal cushing
Adrenal cushing Arritimias
Arritimias Ectocrine
Ectocrine Adrenal cortex and medulla
Adrenal cortex and medulla Human body systems images
Human body systems images Levotironina
Levotironina Adrenal sympathetic pathway
Adrenal sympathetic pathway Mineralocorticoid function
Mineralocorticoid function Relations of suprarenal gland
Relations of suprarenal gland Adrenal gland hormone
Adrenal gland hormone Adrenal drugs pharmacology
Adrenal drugs pharmacology Hipogonadismo secundario
Hipogonadismo secundario Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics Acth stimulation test
Acth stimulation test Hymen
Hymen Non classical adrenal hyperplasia
Non classical adrenal hyperplasia Non classical adrenal hyperplasia
Non classical adrenal hyperplasia Adrenal bezin hipofonksiyonu sonucu gelişen tablo
Adrenal bezin hipofonksiyonu sonucu gelişen tablo The suprarenal (adrenal) medullae secrete
The suprarenal (adrenal) medullae secrete Zona reticularis gonadocorticoids
Zona reticularis gonadocorticoids Cricoid cartilage
Cricoid cartilage Adrenal gland regions
Adrenal gland regions Autonomic nervous system visceral
Autonomic nervous system visceral Adrenal medulla cortex
Adrenal medulla cortex Iszlám padisahja 2. mohamed
Iszlám padisahja 2. mohamed Mohamed merchant
Mohamed merchant Nyu parallel computing
Nyu parallel computing Abdelrahman mohamed
Abdelrahman mohamed Mohamed homayed
Mohamed homayed