Common Parathyroid Disorders in Children Dr Sarar Mohamed






- Slides: 41
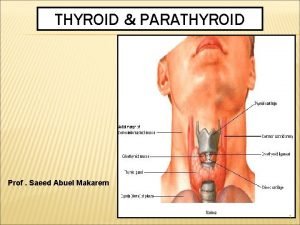
. Common Parathyroid Disorders in Children Dr Sarar Mohamed FRCPCH (UK), MRCP (UK), CCST (Ire), CPT (Ire), DCH (Ire), MD Consultant Paediatric Endocrinologist & Metabolic Physician Associate Professor of Pediatrics King Saud University
Agenda • Calcium homeostasis • Causes of hypocalcaemia • Rickets • hypercalcaemia .
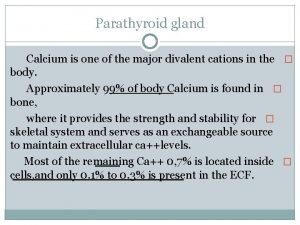
Key-players of calcium metabolism • • • Calcium & Phosphates Parathyroid hormone (PTH). Cholecalciferol (Vit. D 3) and Calcitriol Estrogen and other Sex hormones. Calcitonin.
PARATHYROID HORMONE Function of PTH 1 -raises the level of calcium in the blood 2 -decreases levels of blood phosphate. 3 -Partially antagonistic to calcitonin
PARATHYROID HORMONE • Secreation stimulated by fall in serum Ca. • mobilize calcium from bone • Increases renal reabsorption of ca • � decreases renal clearance of calcium • �increase calcium absorption - intestine Calcium homeostasis
Vitamin D • Fat soluble ‘vitamin’ • Synthesised in skin • Food sources include fish oils

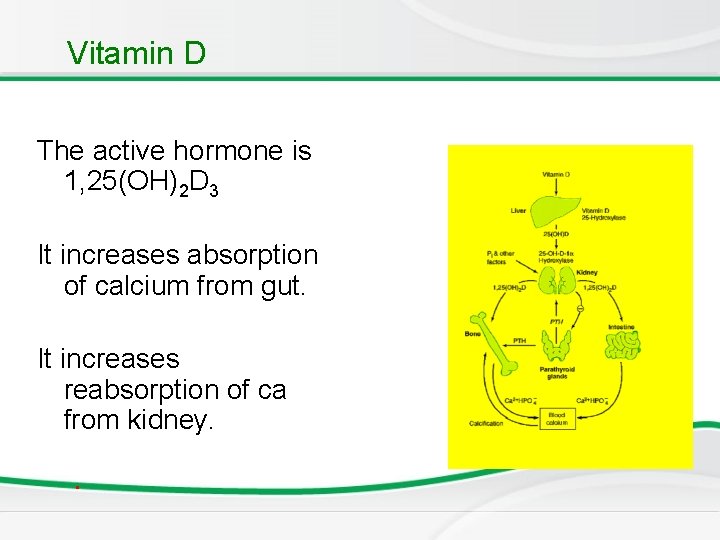
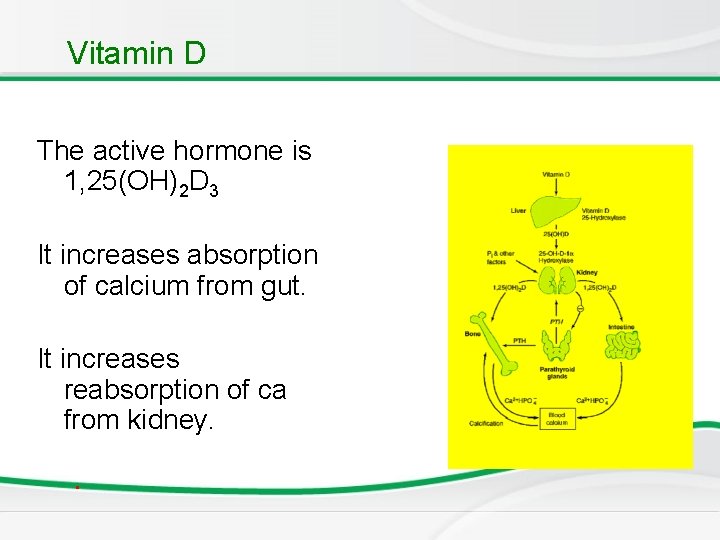
Vitamin D The active hormone is 1, 25(OH)2 D 3 It increases absorption of calcium from gut. It increases reabsorption of ca from kidney. .
Calcitonin • It is a calcium lowering hormone • Secreted by Thyroid C cells Anti - PTH
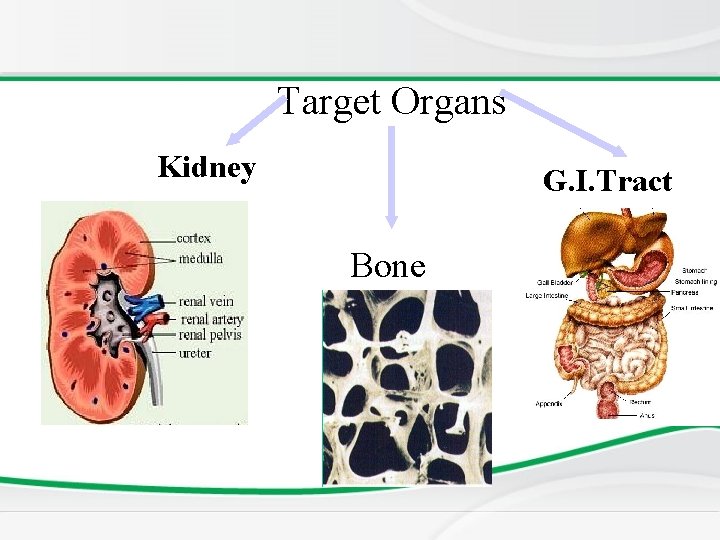
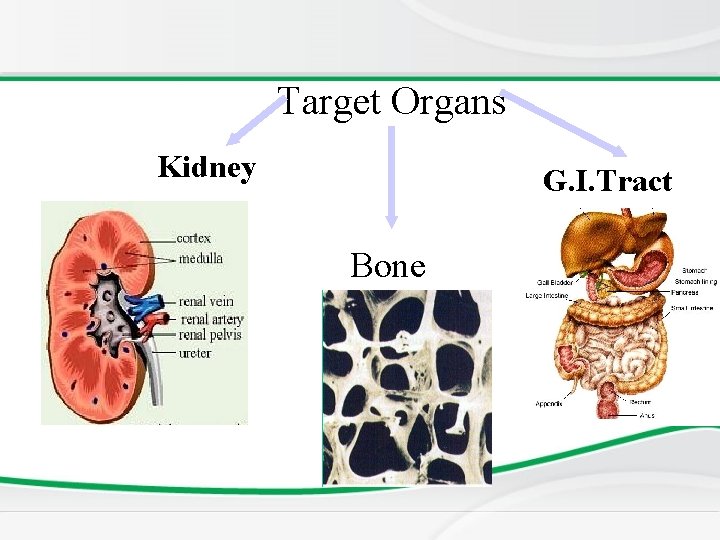
Target Organs Kidney G. I. Tract Bone
Dysfunction of parathyroid Gland 1. Too little parathyroid hormone – hypoparahypothyroidism causes low serum calcium and high phosphate 2. Too much parathyroid hormone– hyperparahyperthyroidism causes high calcium and low phosphate
Calcium profile • To diagnose a metabolic bone disease – – – calcium Phosphate Alkaline phosphatase Parathyroid hormone Vitamin D Urinary calcium and phospherus
Causes of hypocalcaemia • • • Rickets Hypopararthyroidism Psuedohypopararthyroidism Familial hypocalcaemia Renal failure Drugs: phenytoin Maternal diabetes Premarurity Di. Goerge syndrome .
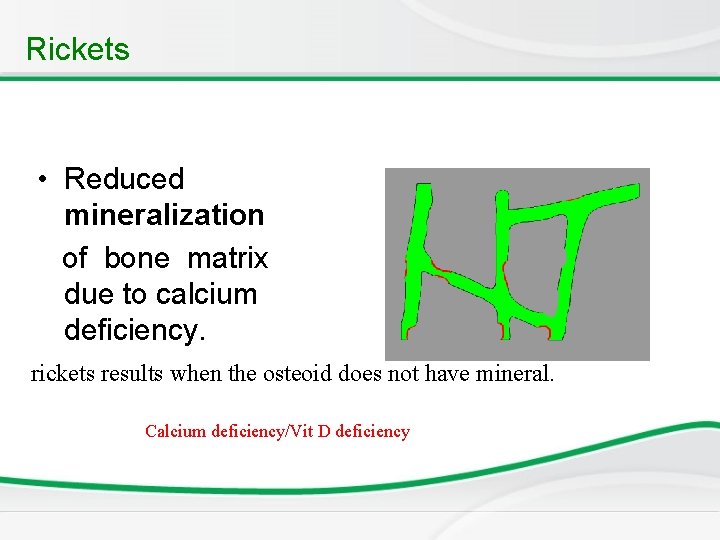
Rickets • Reduced mineralization of bone matrix due to calcium deficiency. rickets results when the osteoid does not have mineral. Calcium deficiency/Vit D deficiency
Deficiency of Vit. D • Dietary lack of the vitamin • Insufficient ultraviolet skin exposure • Malabsorption of fats and fat-soluble vitamins- A, D, E, & K. • Abnormal metabolism of vitamin D chronic renal failure. .
Rickets: Non renal causes – • • • Nutritional Intestinal – malabsorption Hepatobiliary Metabolic – anticonvulsant therapy Rickets of prematurity
Renal causes • Renal osteodystrophy: CRF Familial hypophosphataemic rickets Renal tubular acidosis Fanconi syndrome Primary Secondary - cystinosis, wilsons disease, lowe syndrome, tyrosinemia Vitamin D dependent type 1 rickets Vitamin D dependent type 2 rickets
Rickets: Effect at growth end plate • Inadequate growth plate mineralization. • Defective calcification in the interstitial regions • The growth plate increases in thickness. • The columns of cartilage cells are disorganized.
Rickets v Cupping of the epiphyses. v Bones incapable of withstanding mechanical stresses and lead to bowing deformities. v Eventual length of the long bones is diminished. ( short stature)
Age of presentation • VITAMIN D DEFICIENCY RICKETS – 6 to 18 months. • NON NUTRITIONAL RICKETS Beyond this age group.
Skeletal manifestations of Rickets • • • Craniotaes Delayed closure of anterior fontanelle Frontal and parietal bossing Delayed eruption of primary teeth Rosary

Skeletal manifestations EXTREMITIES – Enlargement of long bones around wrists and ankles Bow legs, knock knees green stick fractures


Extra – skeletal manifestations SEIZURES AND TETANY – Secondary to hypocalcaemia HYPOTONIA AND DELAYED MOTOR DEVELOPMENT In rickets developing during infancy.
Investigations, • BASIC INVESTIGATIONS TO CONFIRM RICKETS • • Low or normal serum Ca Low phospherus High alkaline phosphatase X rays of ends of long bones at knees or wrists – Shows Widening, fraying, cupping of the distal ends of shaft. • Vit D level low • Parathyroid hormone high
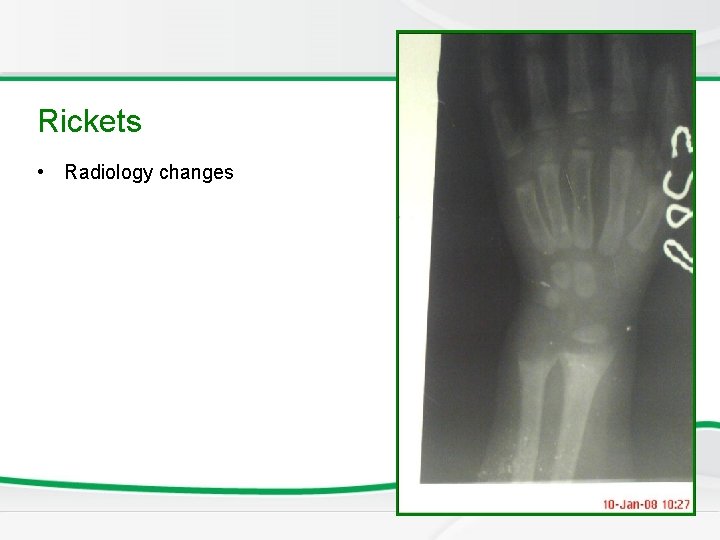
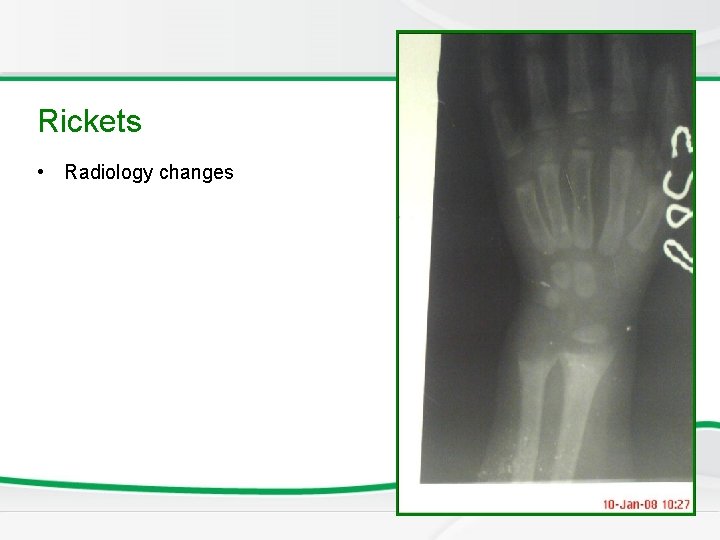
Newborn Screening Rickets • Radiology changes

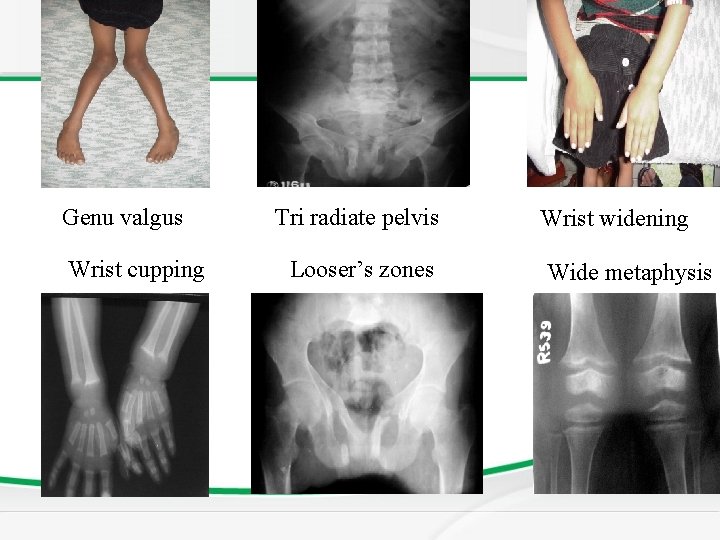
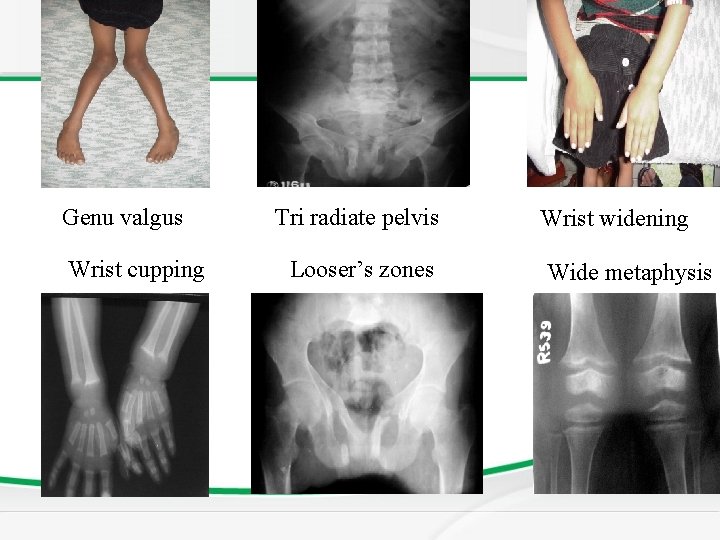
Genu valgus Wrist cupping Tri radiate pelvis Looser’s zones Wrist widening Wide metaphysis
Vitamin D Resistant Rickets • In the renal tubular disorders, rickets develops in the presence of normal intestinal function and are not cured by normal doses of vitamin D. • Resistant or refractory rickets. Defective final conversion of Vit. D in to active form or End organ insensitivity.
Vitamin D Resistant Rickets
Vitamin D Resistant Rickets
Treatment of Rickets • Vitamin D supplement • Type and dose depends on underline cause of Rickets
Causes of hypercalcaemia • Hyperparathyroidism • Vitamin D intoxicity • William syndrome • Familial hypocalcuric hypercalcaemia • malignancy .
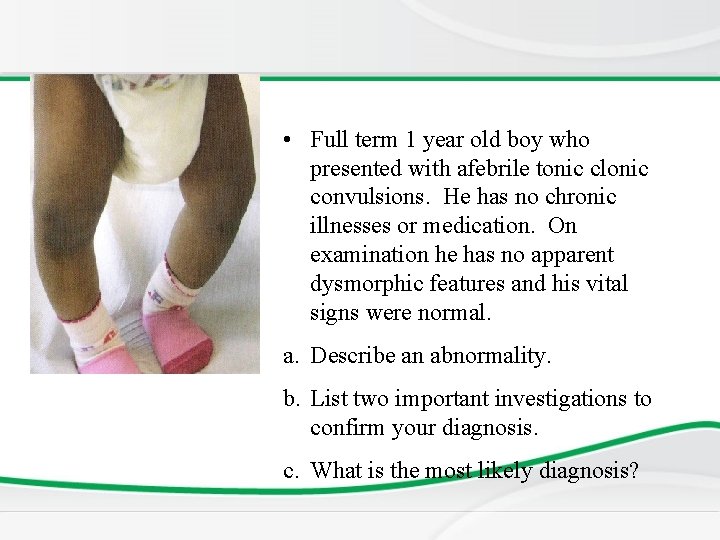
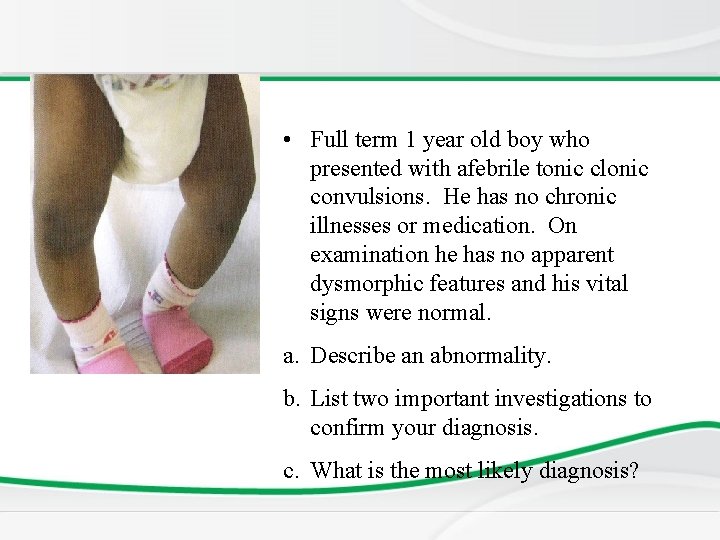
• Full term 1 year old boy who presented with afebrile tonic clonic convulsions. He has no chronic illnesses or medication. On examination he has no apparent dysmorphic features and his vital signs were normal. a. Describe an abnormality. b. List two important investigations to confirm your diagnosis. c. What is the most likely diagnosis?
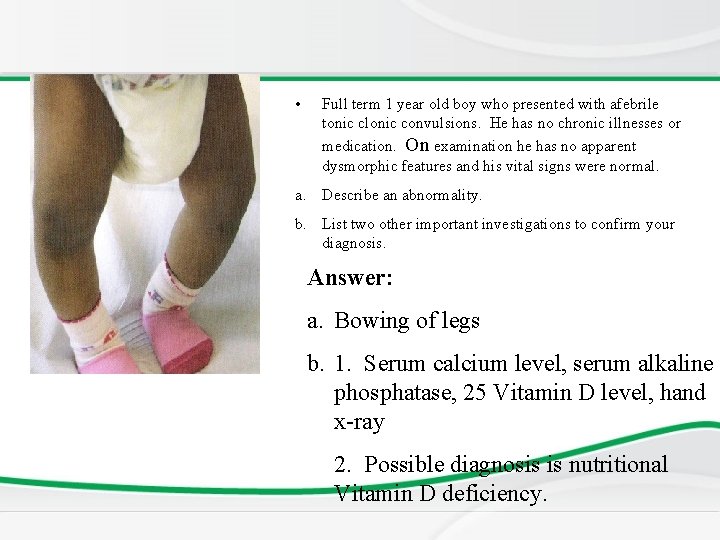
• Full term 1 year old boy who presented with afebrile tonic clonic convulsions. He has no chronic illnesses or medication. On examination he has no apparent dysmorphic features and his vital signs were normal. a. Describe an abnormality. b. List two other important investigations to confirm your diagnosis. Answer: a. Bowing of legs b. 1. Serum calcium level, serum alkaline phosphatase, 25 Vitamin D level, hand x-ray 2. Possible diagnosis is nutritional Vitamin D deficiency.
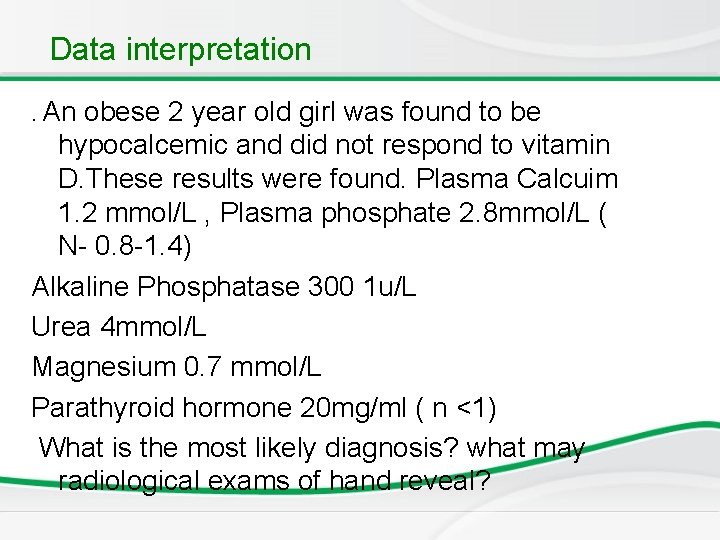
Data interpretation. An obese 2 year old girl was found to be hypocalcemic and did not respond to vitamin D. These results were found. Plasma Calcuim 1. 2 mmol/L , Plasma phosphate 2. 8 mmol/L ( N- 0. 8 -1. 4) Alkaline Phosphatase 300 1 u/L Urea 4 mmol/L Magnesium 0. 7 mmol/L Parathyroid hormone 20 mg/ml ( n <1) What is the most likely diagnosis? what may radiological exams of hand reveal?
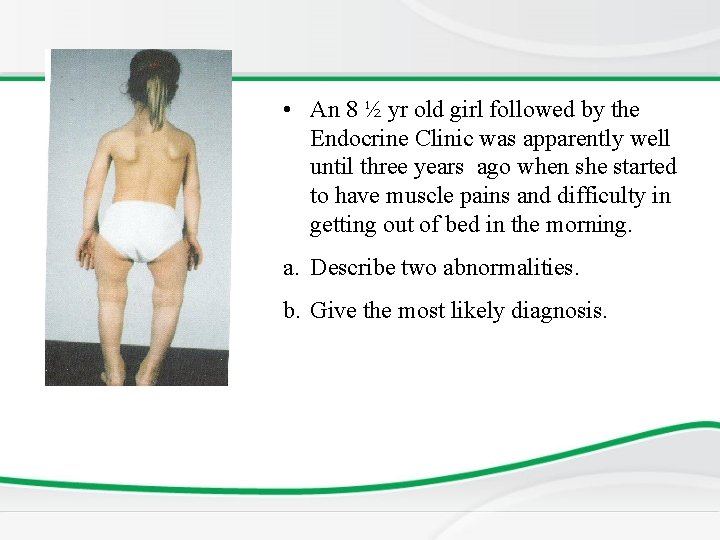
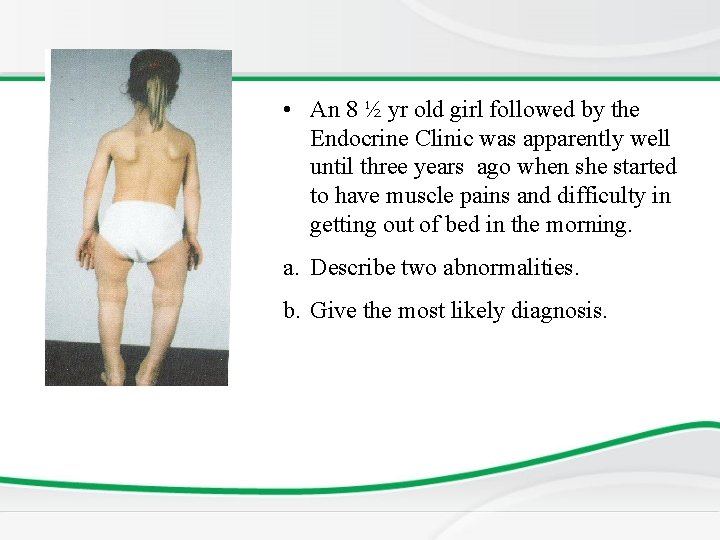
• An 8 ½ yr old girl followed by the Endocrine Clinic was apparently well until three years ago when she started to have muscle pains and difficulty in getting out of bed in the morning. a. Describe two abnormalities. b. Give the most likely diagnosis.
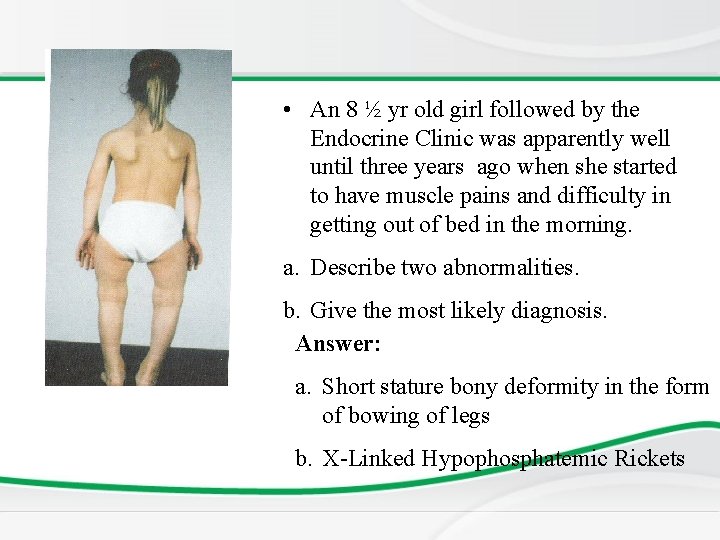
• An 8 ½ yr old girl followed by the Endocrine Clinic was apparently well until three years ago when she started to have muscle pains and difficulty in getting out of bed in the morning. a. Describe two abnormalities. b. Give the most likely diagnosis. Answer: a. Short stature bony deformity in the form of bowing of legs b. X-Linked Hypophosphatemic Rickets

n a Th ! u o y k
 Fahri sarar
Fahri sarar In what situation should a nail service be performed
In what situation should a nail service be performed Parathyroid gland chief cell
Parathyroid gland chief cell Parathyroid innervation
Parathyroid innervation Hypophseal
Hypophseal Histological structure of parathyroid gland
Histological structure of parathyroid gland Parathyroid gland chief cell
Parathyroid gland chief cell Parathyroid hormone and calcitonin
Parathyroid hormone and calcitonin Parathormone function
Parathormone function Phycatri
Phycatri Calcitonin vs pth
Calcitonin vs pth Parathyroid
Parathyroid Shrsies
Shrsies 3rd pharyngeal pouch
3rd pharyngeal pouch Isthmus size
Isthmus size Nyu parallel computing
Nyu parallel computing Dr mohamed eldeib
Dr mohamed eldeib Mohamed homayed
Mohamed homayed Mohamed younis umbc
Mohamed younis umbc Mohamed samir design
Mohamed samir design Mohamed akel
Mohamed akel Mohamed akel
Mohamed akel Dr. mohammad diab
Dr. mohammad diab Abukar mohamed
Abukar mohamed Mohamed dahoui
Mohamed dahoui Omar requirements
Omar requirements Mohamed hmiden
Mohamed hmiden Henintsoa georges
Henintsoa georges Mohamed
Mohamed Dr mohamed bashar shala
Dr mohamed bashar shala Muhamed computer technology
Muhamed computer technology Mohamed younis umbc
Mohamed younis umbc Mohamed hassoun
Mohamed hassoun Hassan fareed physics
Hassan fareed physics Mohamed akel
Mohamed akel Yahye mohamed omar
Yahye mohamed omar Dr elsayed mohamed
Dr elsayed mohamed Mohamed younis umbc
Mohamed younis umbc Dr mohamed nasr
Dr mohamed nasr Parallel computing nyu
Parallel computing nyu Bouhicha mohamed
Bouhicha mohamed Dr alboushi
Dr alboushi