Common Parathyroid Disorders in Children Dr Sarar Mohamed










- Slides: 47
. Common Parathyroid Disorders in Children Dr Sarar Mohamed FRCPCH (UK), MRCP (UK), CCST (Ire), CPT (Ire), DCH (Ire), MD Consultant Paediatric Endocrinologist & Metabolic Physician Associate Professor of Pediatrics King Saud University

Agenda • Calcium homeostasis • Causes of hypocalcaemia • Rickets • hypercalcaemia .
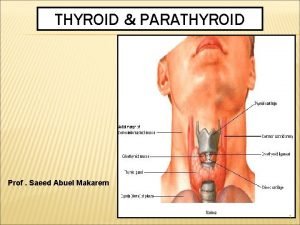
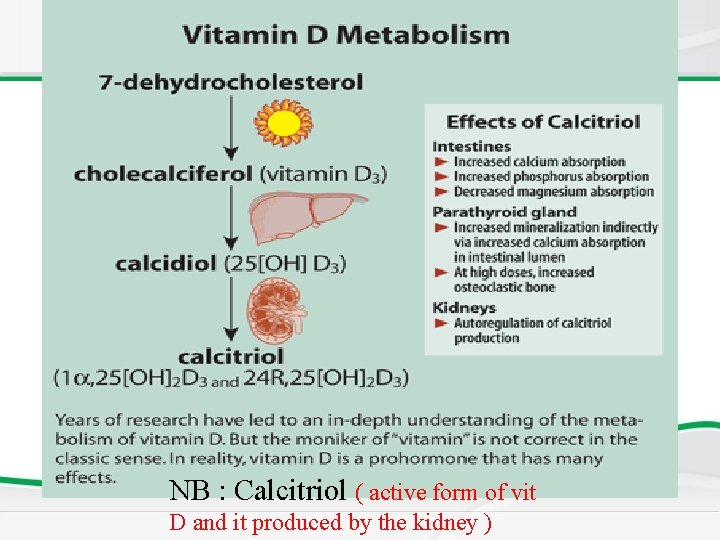
Key-players of calcium metabolism • Calcium & Phosphates • Parathyroid hormone (PTH). • Cholecalciferol (Vit. D 3) and Calcitriol ( active form of vit D and it produced by the kidney ) • Estrogen and other Sex hormones. ( in adults only ) • Calcitonin.

PARATHYROID HORMONE Function of PTH 1 -raises the level of calcium in the blood 2 -decreases levels of blood phosphate. 3 -Partially antagonistic to calcitonin
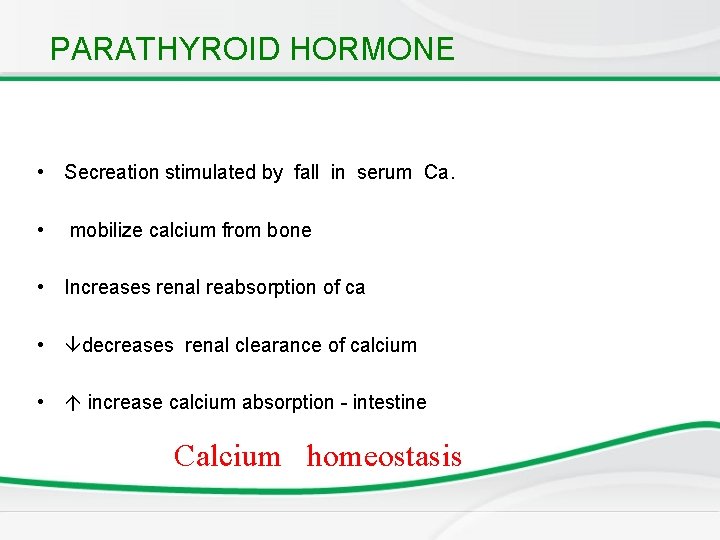
PARATHYROID HORMONE • Secreation stimulated by fall in serum Ca. • mobilize calcium from bone • Increases renal reabsorption of ca • decreases renal clearance of calcium • increase calcium absorption - intestine Calcium homeostasis
Vitamin D • Fat soluble ‘vitamin’ • Synthesised in skin • Food sources include fish oils
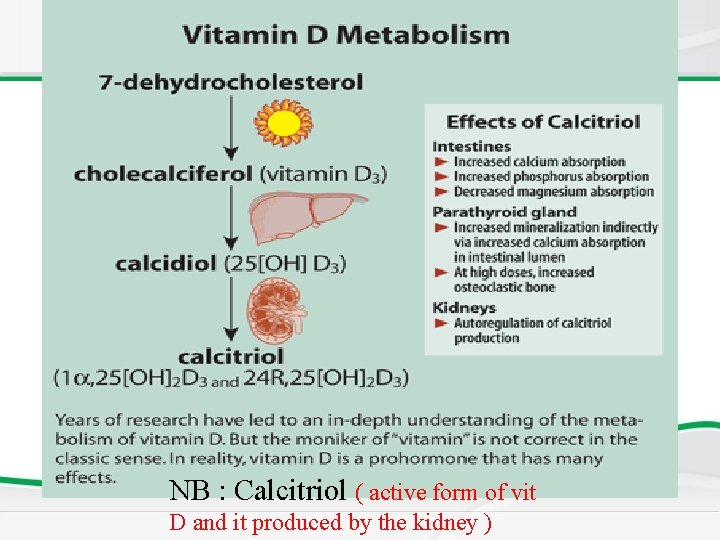
NB : Calcitriol ( active form of vit D and it produced by the kidney )
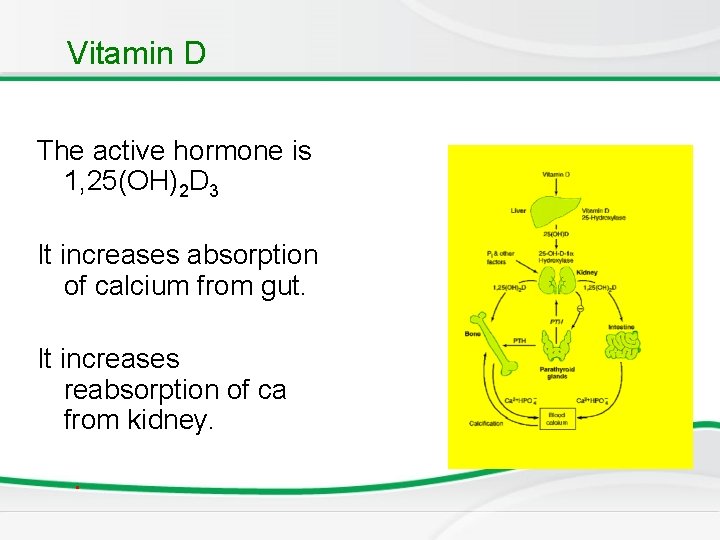
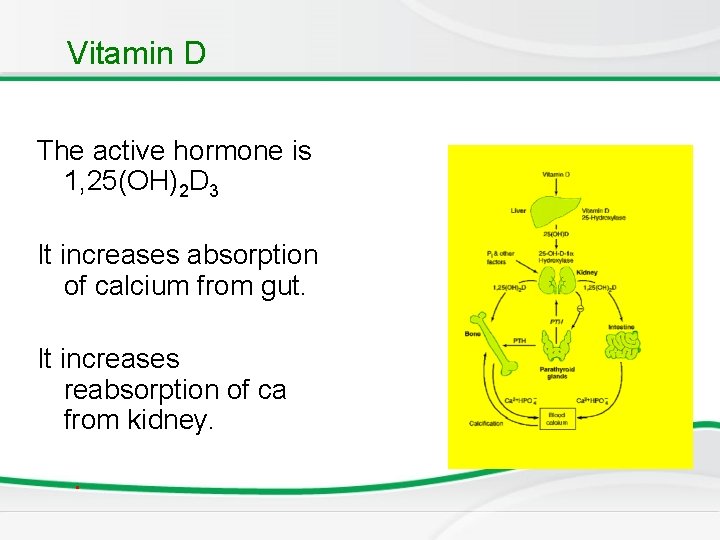
Vitamin D The active hormone is 1, 25(OH)2 D 3 It increases absorption of calcium from gut. It increases reabsorption of ca from kidney. .
Calcitonin • It is a calcium lowering hormone • Secreted by Thyroid C cells Anti - PTH
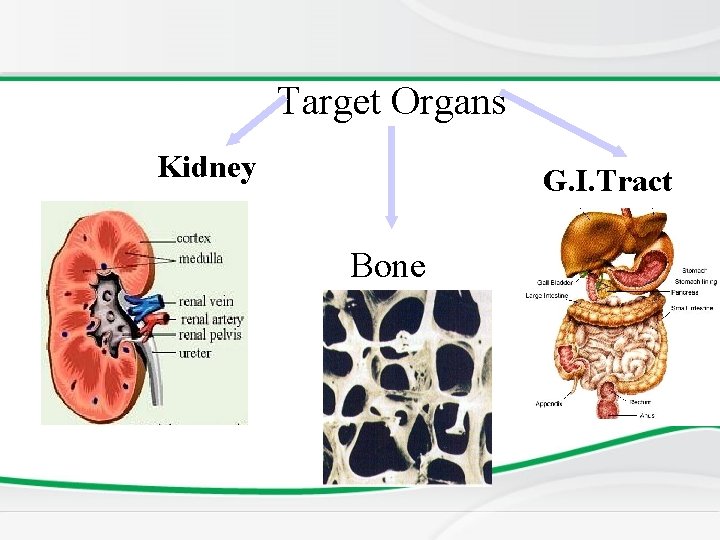
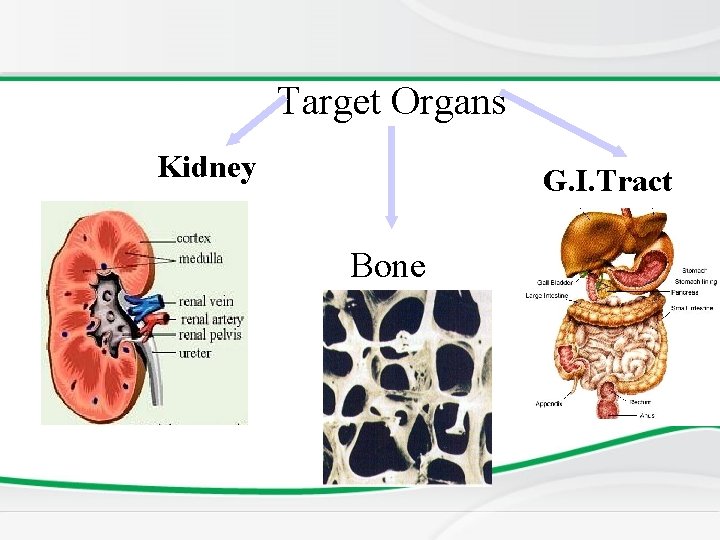
Target Organs Kidney G. I. Tract Bone
Dysfunction of parathyroid Gland - MCQ 1. Too little parathyroid hormone – hypoparahypothyroidism causes low serum calcium and high phosphate 2. Too much parathyroid hormone– hyperparahyperthyroidism causes high calcium and low phosphate.
Newborn Screening Hyperparathyroidism • Main symptom is hypercalcemia, and hypophosphatemia also occurs but not always. • Pseudohypoparathyroidism ﻣﻬﻢ • Normal or elevated PTH (intact pituitary function), the problem is that end organ is resistant. • Leading to decreased calcium and increased phosphate levels with normal ALP. • Clinical presentation: short stature, and obese. • Radiology: x-ray shows short 4 th metacarpal and delayed development. • Occur in End organ insensitivity occur in obese childrens
Calcium profile • To diagnose a metabolic bone disease – – – calcium Phosphate Alkaline phosphatase Parathyroid hormone Vitamin D Urinary calcium and phospherus
Newborn Screening • Elevated ALP on calcium profile, think of rickets. • For vitamin D deficiency, measure the 25 hydroxy-cholecalciferol (which is normally formed in the liver). • Prolonged breast feeding without supplementation can lead to nutritional deficiency in the infants.
Causes of hypocalcaemia • • . Rickets Hypopararthyroidism Psuedohypopararthyroidism Familial hypocalcaemia Renal failure Drugs: phenytoin Maternal diabetes: newborn to diabetic mothers have decreased insulin, hyperglycemia, and pancreatic atrophy. Insulin is required for PTH. This condition subsides with time and patient is taken for counseling. • Prematurity • Di. Goerge syndrome CATCH 22 – – – Cardiac abnormality (tertaolgy of Fallot). Abnormal facies. Thymus aplasia. Cleft palate. Hypoparathyroidism/hypocalceamia.
ﺍﻭﻻ : Rickets • Reduced mineralization of bone matrix due to calcium deficiency. Rickets results when the osteoid does not have mineral. This can also happen quickly, depending on the severity of mineral deficiency. In adolescents or adults it is called osteomalacia because they are not growing bones. Calcium deficiency/Vit D deficiency
Newborn Screening • Commonest cause of vitamin D deficiency is decreased sun exposure overall, but in infancy it is mainly from diet; therefore, if patient is on breast milk switch to supplement. • All types of rickets leads to decreased phosphate level except renal rickets because of renal failure (renal osteodystrophy).
Etiology : Deficiency of Vit. D • Dietary lack of the vitamin like in baby who is breastfeeding dependant - MCQ ﻣﻬﻤﻪ • Insufficient ultraviolet skin exposure • Malabsorption of fats and fat-soluble vitamins- A, D, E, & K. • Abnormal metabolism of vitamin D chronic renal failure. .
Rickets: Non renal causes – • • • Nutritional Intestinal – malabsorption Hepatobiliary Metabolic – anticonvulsant therapy Rickets of prematurity (happens in the first weeks of life).
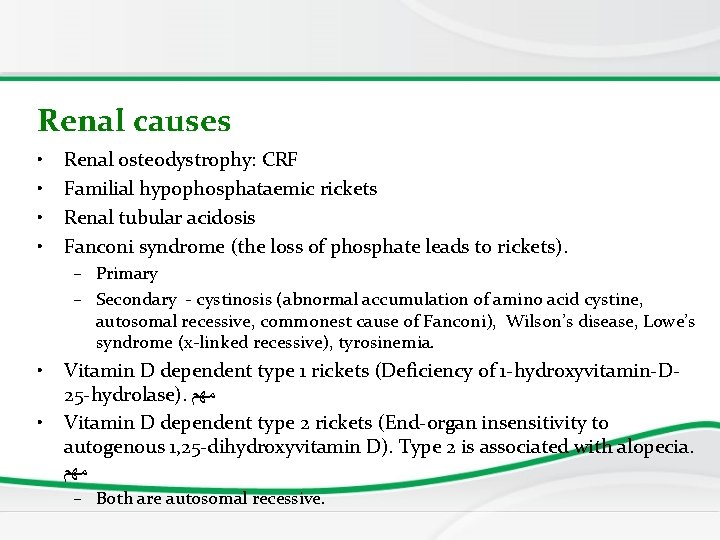
Renal causes • • Renal osteodystrophy: CRF Familial hypophosphataemic rickets Renal tubular acidosis Fanconi syndrome (the loss of phosphate leads to rickets). – Primary – Secondary - cystinosis (abnormal accumulation of amino acid cystine, autosomal recessive, commonest cause of Fanconi), Wilson’s disease, Lowe’s syndrome (x-linked recessive), tyrosinemia. • • Vitamin D dependent type 1 rickets (Deficiency of 1 -hydroxyvitamin-D 25 -hydrolase). ﻣﻬﻢ Vitamin D dependent type 2 rickets (End-organ insensitivity to autogenous 1, 25 -dihydroxyvitamin D). Type 2 is associated with alopecia. ﻣﻬﻢ – Both are autosomal recessive.
Rickets: Effect at growth end plate • Inadequate growth plate mineralization. • Defective calcification in the interstitial regions. • The growth plate increases in thickness. • The columns of cartilage cells are disorganized. • Hereditary type is associated with short stature.
Rickets • Cupping of the epiphyses. • Bones incapable of withstanding mechanical stresses and lead to bowing deformities. • Eventual length of the long bones is diminished (short stature).
Age of presentation • VITAMIN D DEFICIENCY RICKETS (nutritional) – 6 to 18 months (first 2 years of life). • NON NUTRITIONAL RICKETS – Beyond this age group. • VITAMIN D DEPENDENT RICKETS – Presents early in life.
Skeletal manifestations of Rickets • Craniotaes (depression when pressing on the skull ping ball sign) • Delayed closure of anterior fontanelle • Frontal and parietal bossing • Delayed eruption of primary teeth • Chest for rickets Rosary (increase in size of costo-chondoral junction)

Skeletal manifestations EXTREMITIES – Enlargement of long bones around wrists and ankles due to increased size of distal bones (radius and ulna) Bow legs, knock knees Green stick fractures


Extra – skeletal manifestations SEIZURES AND TETANY – Secondary to hypocalcaemia HYPOTONIA AND DELAYED MOTOR DEVELOPMENT In rickets developing during infancy.

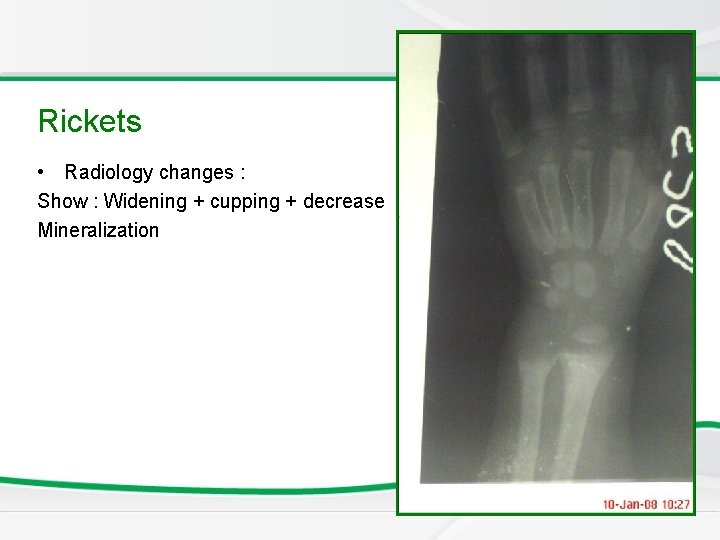
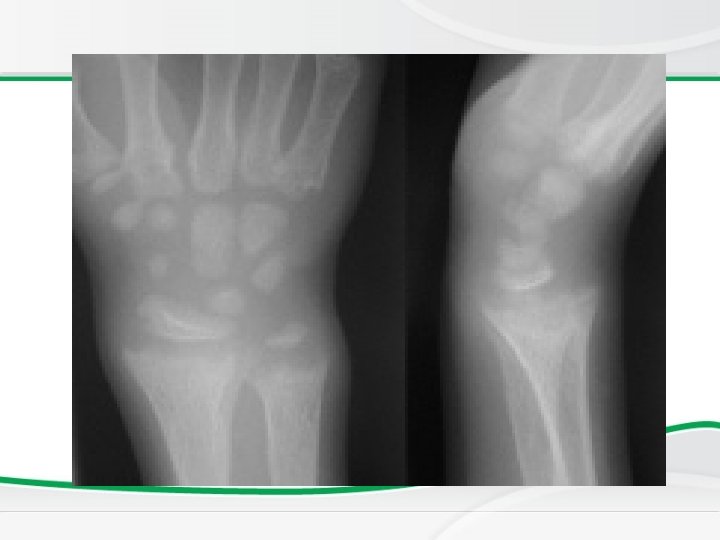
Investigations • BASIC INVESTIGATIONS TO CONFIRM RICKETS • • Low or normal serum Ca Low phosphorus (very early on in the disease may be normal) High alkaline phosphatase X rays of ends of long bones at knees or wrists – Shows Widening, fraying, cupping of the distal ends of shaft. • Vit D level low • Parathyroid hormone high is secondary due to hypocalcemia ﻣﻬﻢ
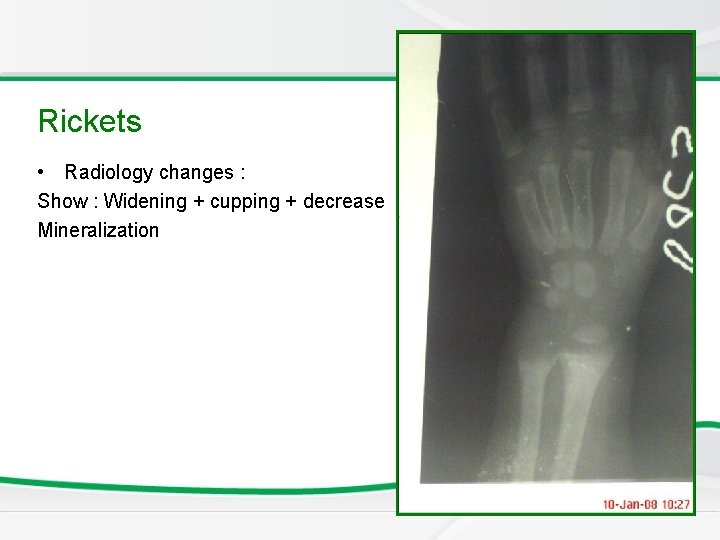
Newborn Screening Rickets • Radiology changes : Show : Widening + cupping + decrease Mineralization
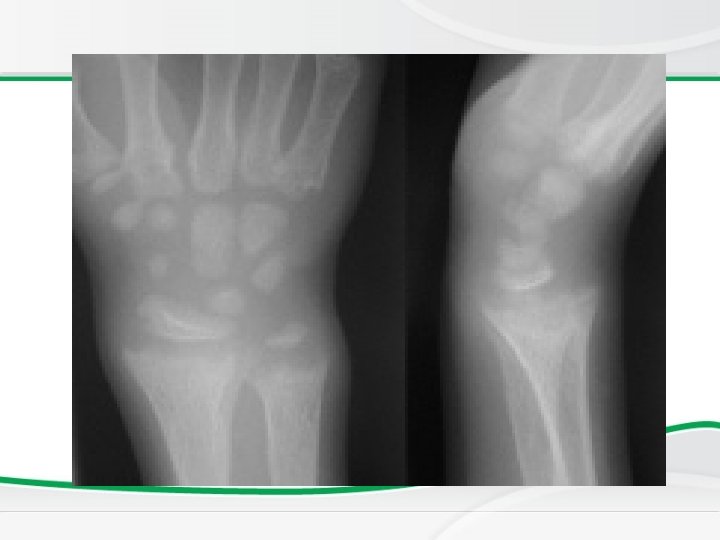
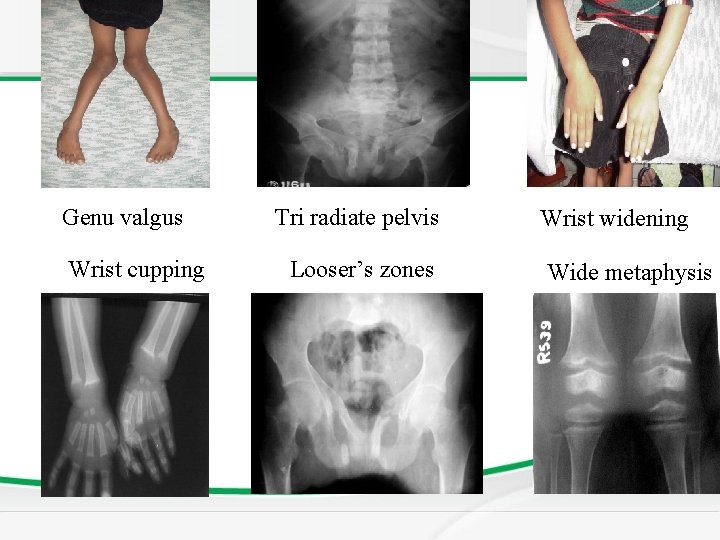
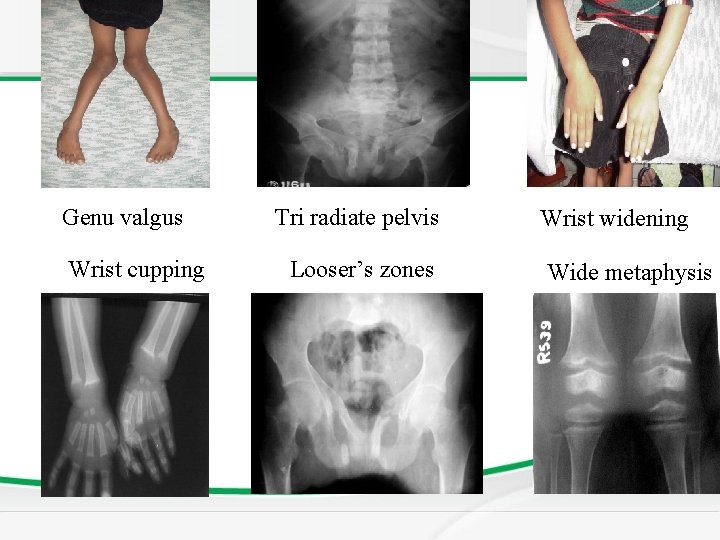
Genu valgus Wrist cupping Tri radiate pelvis Looser’s zones Wrist widening Wide metaphysis
Vitamin D Resistant Rickets ( X linked hypocalcemia ) • In the renal tubular disorders, rickets develops in the presence of normal intestinal function and are not cured by normal doses of vitamin D. • Resistant or refractory rickets. • Commonest is x-linked hypophosphatemic rickets • Short stature and late presentation. ﻣﻬﻤﻪ • Vitamin D is normal but the pathology is in the kidney because it can not absorb phosphate Defective final conversion of Vit. D in to active form or End organ insensitivity.
Newborn Screening • Rickets is a clinical diagnosis, whereas vitamin D deficiency is a biochemical one.

Vitamin D Resistant Rickets

Vitamin D Resistant Rickets
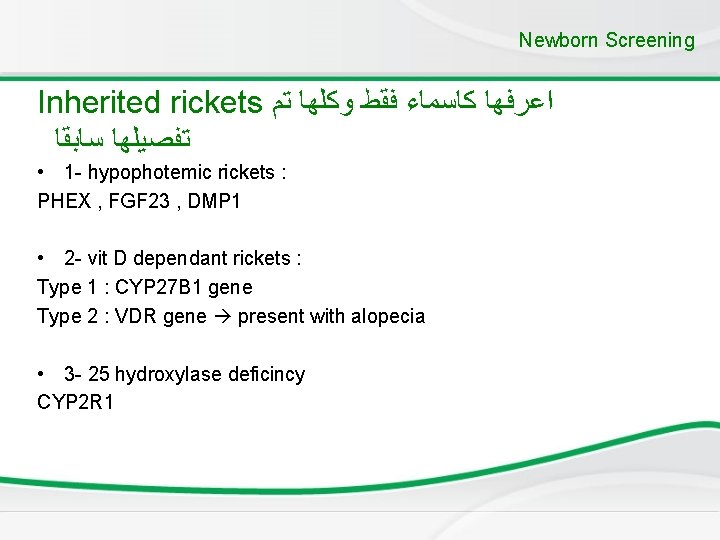
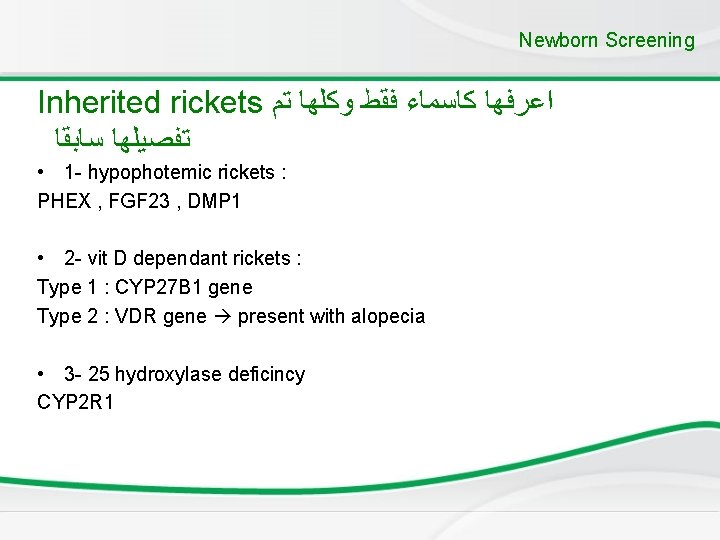
Newborn Screening Inherited rickets ﺍﻋﺮﻓﻬﺎ ﻛﺎﺳﻤﺎﺀ ﻓﻘﻂ ﻭﻛﻠﻬﺎ ﺗﻢ ﺗﻔﺼﻴﻠﻬﺎ ﺳﺎﺑﻘﺎ • 1 - hypophotemic rickets : PHEX , FGF 23 , DMP 1 • 2 - vit D dependant rickets : Type 1 : CYP 27 B 1 gene Type 2 : VDR gene present with alopecia • 3 - 25 hydroxylase deficincy CYP 2 R 1
Treatment of Rickets • Vitamin D supplement – Nutritional (commonest) we give vitamin D 3. – Resistant rickets is treated by the active form of vitamin D. • Type and dose depends on underlying cause of Rickets
Causes of hypercalcaemia • Hyperparathyroidism • Vitamin D intoxicity • William syndrome • Familial hypocalcuric hypercalcaemia: calcium is not excreted. • malignancy .
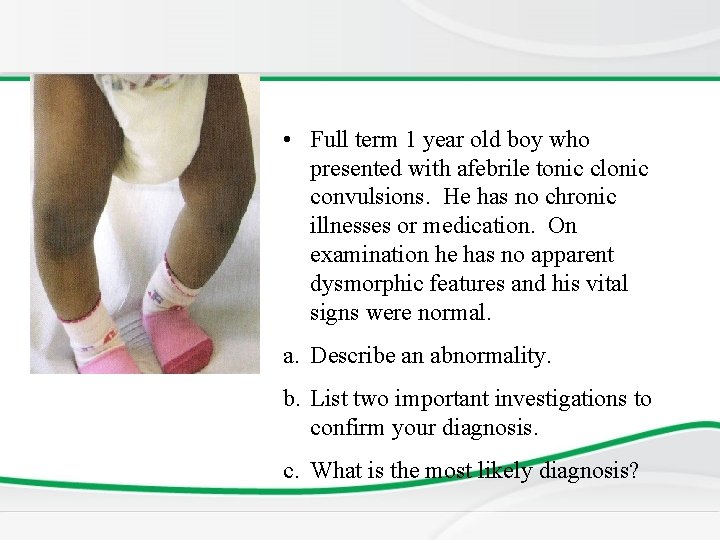
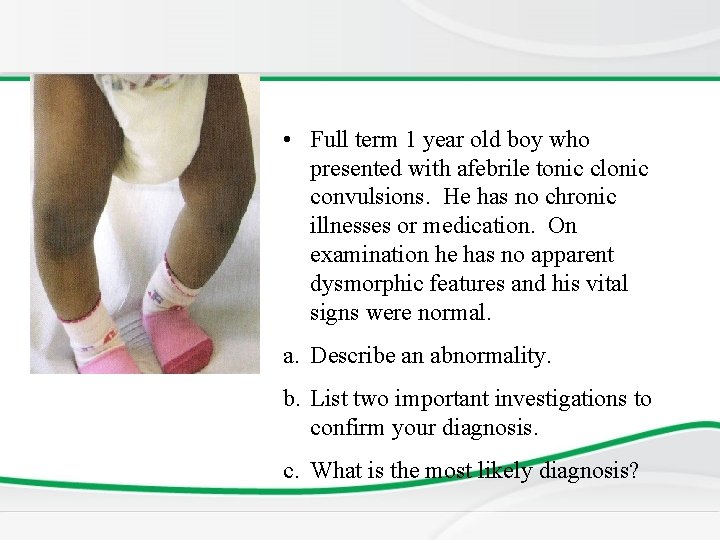
• Full term 1 year old boy who presented with afebrile tonic clonic convulsions. He has no chronic illnesses or medication. On examination he has no apparent dysmorphic features and his vital signs were normal. a. Describe an abnormality. b. List two important investigations to confirm your diagnosis. c. What is the most likely diagnosis?
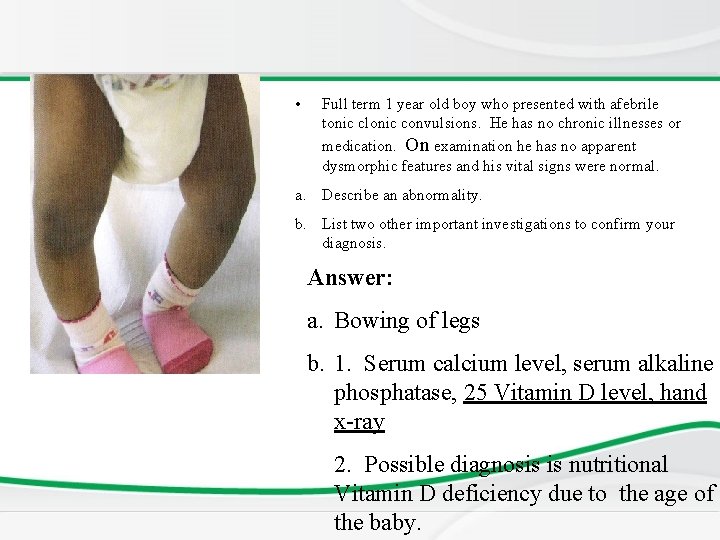
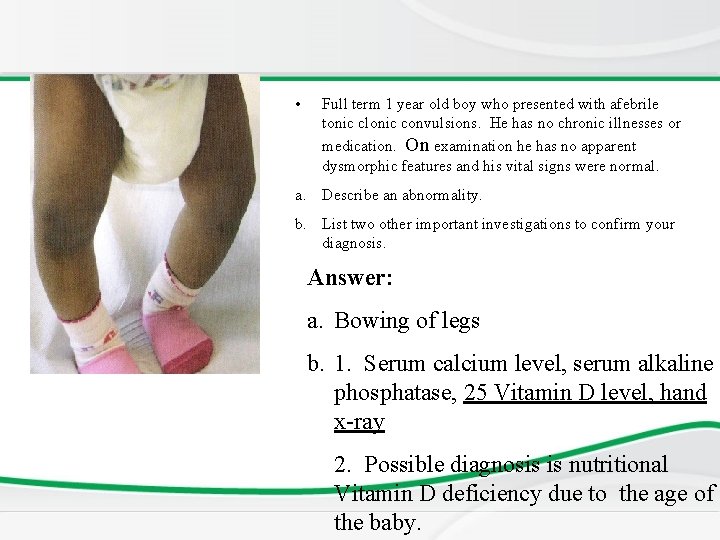
• Full term 1 year old boy who presented with afebrile tonic clonic convulsions. He has no chronic illnesses or medication. On examination he has no apparent dysmorphic features and his vital signs were normal. a. Describe an abnormality. b. List two other important investigations to confirm your diagnosis. Answer: a. Bowing of legs b. 1. Serum calcium level, serum alkaline phosphatase, 25 Vitamin D level, hand x-ray 2. Possible diagnosis is nutritional Vitamin D deficiency due to the age of the baby.
Data interpretation. An obese 2 year old girl was found to be hypocalcemic and did not respond to vitamin D. These results were found. Plasma Calcuim 1. 2 mmol/L , Plasma phosphate 2. 8 mmol/L ( N- 0. 8 -1. 4) Alkaline Phosphatase 300 1 u/L Urea 4 mmol/L Magnesium 0. 7 mmol/L Parathyroid hormone 20 mg/ml ( n <1) What is the most likely diagnosis? Psudohyperparathyrodism what may radiological exams of hand reveal? Shorting of the 4 th metacarbal bone ﻋﻼﻣﻪ ﻣﻤﻴﺰﻩ
Newborn Screening • This is a case of pseudohypoparathyroidism. What makes it more likely is that the ALP, urea is normal (excluding both renal and non-renal causes of rickets) and only calcium is low with high PTH.

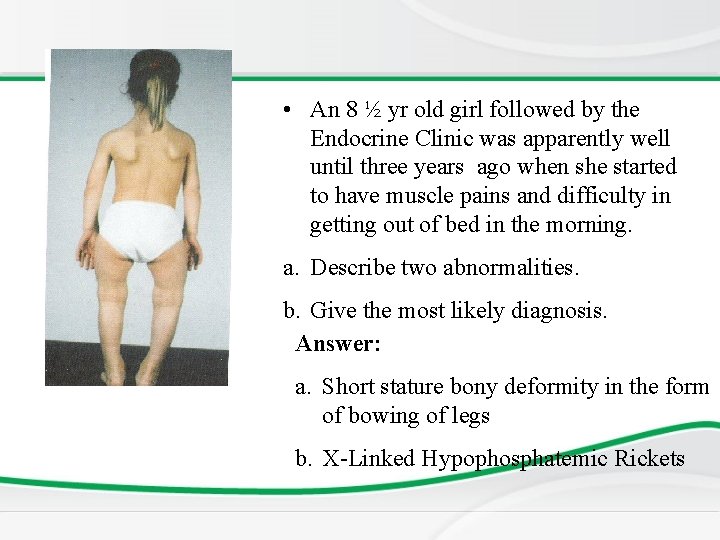
• An 8 ½ yr old girl followed by the Endocrine Clinic was apparently well until three years ago when she started to have muscle pains and difficulty in getting out of bed in the morning. a. Describe two abnormalities. b. Give the most likely diagnosis.
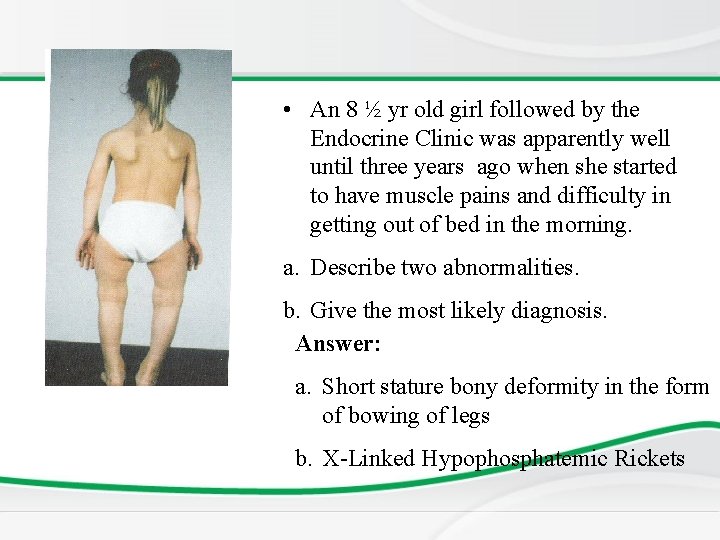
• An 8 ½ yr old girl followed by the Endocrine Clinic was apparently well until three years ago when she started to have muscle pains and difficulty in getting out of bed in the morning. a. Describe two abnormalities. b. Give the most likely diagnosis. Answer: a. Short stature bony deformity in the form of bowing of legs b. X-Linked Hypophosphatemic Rickets

n a Th ! u o y k
 Fahri sarar
Fahri sarar Describe how to conduct nail and skin analysis
Describe how to conduct nail and skin analysis Hyoparathyroidism
Hyoparathyroidism Parathyroid hormone pathway
Parathyroid hormone pathway Pth vs calcitonin
Pth vs calcitonin Parathyroid
Parathyroid Thyroid scan
Thyroid scan Fourth pharyngeal pouch
Fourth pharyngeal pouch True capsule of thyroid gland
True capsule of thyroid gland Parathyroid gland chief cell
Parathyroid gland chief cell Nerve supply of parathyroid gland
Nerve supply of parathyroid gland Hypophseal
Hypophseal Histological structure of parathyroid gland
Histological structure of parathyroid gland Surfaces of thyroid gland
Surfaces of thyroid gland Parathyroid hormone and calcitonin
Parathyroid hormone and calcitonin Mohamed hmiden
Mohamed hmiden Omar requirements
Omar requirements Mohamed taamouti
Mohamed taamouti Power rating
Power rating Dr mohamed bashar shala
Dr mohamed bashar shala Discovering computer
Discovering computer Mohamed younis umbc
Mohamed younis umbc Soumia ecrit en arabe
Soumia ecrit en arabe Mohamed akel
Mohamed akel Mohamed akel
Mohamed akel Dr qazi omar
Dr qazi omar Dr elsayed mohamed
Dr elsayed mohamed Mohamed younis umbc
Mohamed younis umbc Dr mohamed nasr
Dr mohamed nasr Parallel computing nyu
Parallel computing nyu Mohamed bouhicha
Mohamed bouhicha Dr alboushi
Dr alboushi Mohamed el merouani
Mohamed el merouani Fahma mohamed
Fahma mohamed Mohamed younis umbc
Mohamed younis umbc Bani hashim family tree
Bani hashim family tree Mohamed akel
Mohamed akel Professor nasser mohamed
Professor nasser mohamed Mohamed younis umbc
Mohamed younis umbc Mohamed kossentini
Mohamed kossentini Al fayed
Al fayed Mohamed merchant
Mohamed merchant Abdelrahman mohamed
Abdelrahman mohamed Mohamed salah
Mohamed salah Mohamed seghir nekkache
Mohamed seghir nekkache Riham mohamed aly
Riham mohamed aly Mohamed fayad sjsu
Mohamed fayad sjsu Mr mohamed chafik el idrissi
Mr mohamed chafik el idrissi