Endocrine Part Duex Adrenal Disorders 2016 Adrenal Hormones














- Slides: 42

Endocrine Part Duex Adrenal Disorders 2016
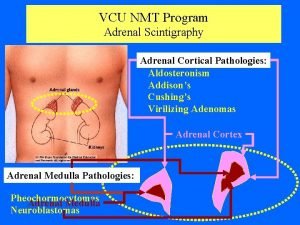
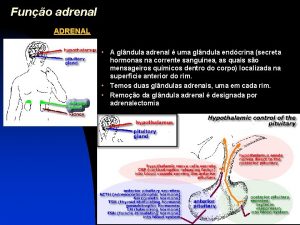
Adrenal Hormones • Located on top of the kidneys • Gland has 3 zones – Aldosterone • Cortex • Inhibits Na excretion
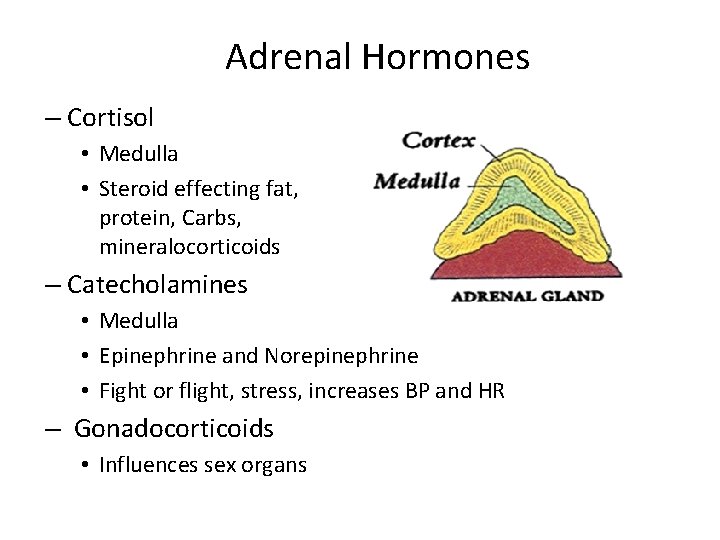
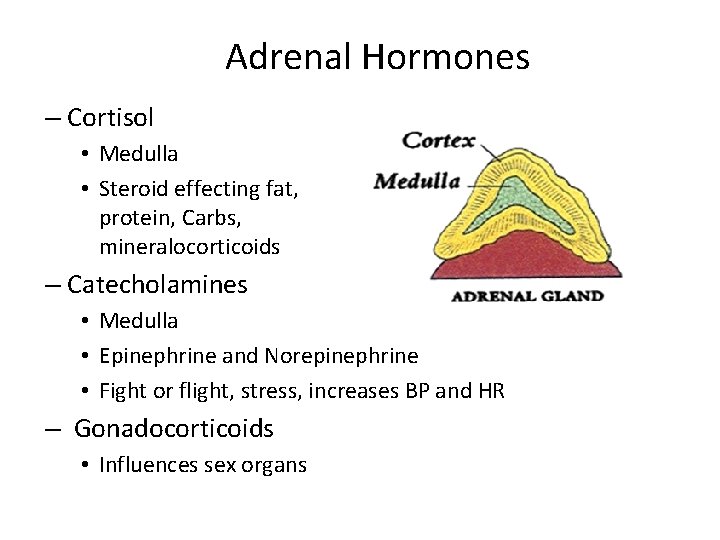
Adrenal Hormones – Cortisol • Medulla • Steroid effecting fat, protein, Carbs, mineralocorticoids – Catecholamines • Medulla • Epinephrine and Norepinephrine • Fight or flight, stress, increases BP and HR – Gonadocorticoids • Influences sex organs
Cortisol is a hormone produced by the cortex – the outer layer – of the adrenal glands. – Steroid hormone that helps the body react to physical and emotional stress, regulate blood pressure, and metabolize food. – Normally secreted in a diurnal pattern, with levels highest in the morning (8 AM) and lowest around midnight. – Production of cortisol is controlled through a feedback system. • When cortisol levels are low, the hypothalamus, a gland located in the lower portion of the brain, produces corticotropin releasing hormone (CRH). • This stimulates the pituitary gland, located below it, to produce adrenocorticotropin hormone (ACTH), which then stimulates the adrenal glands to produce and release cortisol. • When cortisol levels are high, production of CRH and ACTH are normally inhibited. This diurnal pattern changes in people who work alternate shifts and sleep at different times during the day.
Cushing's Syndrome caused by abnormally high levels of cortisol • Can affect anyone, but it is most frequently seen in adults between the ages of 20 to 50 and is more common in women than men. • Rarely, a patient may have an inherited gene mutation that increases her risk of developing tumors throughout the endocrine system
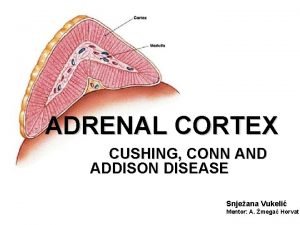
Disorders of the Adrenal Gland Cushing’s Syndrome • Condition from excessive secretion of corticosteroids (particularly glucocoticoid cortisol) • Primary cause: – Adrenocortical tumors or hyperplasia • Secondary cause: – Cushing’s disease-caused by functioning pituitary or non-pituitary neoplasm secreting ACTH-causing increased secretion of glucocorticoids • Iatrogenic: – caused by prolonged use of corticosteroids

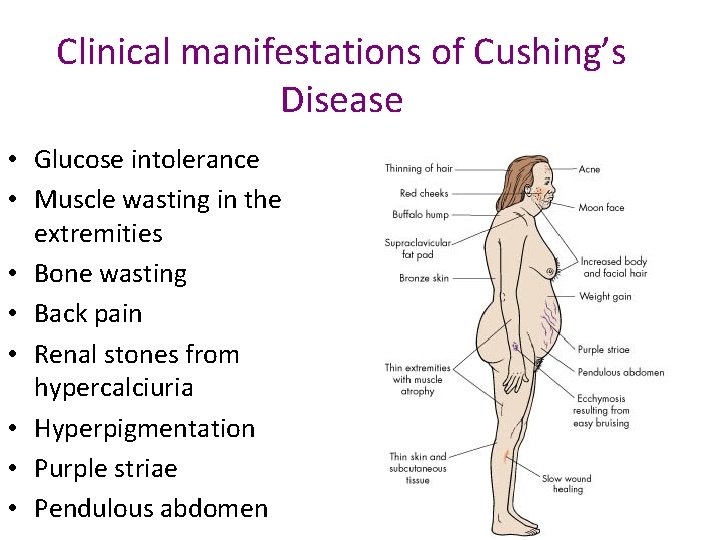
Clinical Manifestations of Hypercortisol Function • Caused by increased hypercortisolism • Weight gain • Accumulation of adipose in trunk (truncal obesity), facial (moon face), and cervical areas (buffalo hump) • Sodium and water retention because of mineralcorticoid effects

There are several causes of Cushing’s syndrome: • Ingestion of exogenous steroids • A pituitary tumor that produces ACTH (also called Cushing’s disease) • Primary overproduction of cortisol by the adrenal gland due to an adrenal tumor or to adrenal hyperplasia • Tumor outside of the hypothalamic-pituitary axis that produces ACTH (ectopic ACTH production)


Disorders of the Adrenal Gland Cushing’s Syndrome If your patient stops their high-dose steroid abruptly!
Disorders of the Adrenal Gland Cushing’s Syndrome • Assessment Findings – Muscle weakness, fatigue – Obese trunk with thin arms and legs, moon face, buffalo hump, pendulous abdomen – Irritability, depression, frequent mood swings – Purple striae on trunk, acne, thin skin – Signs of Masculinization in women – Mental dysfunction, decreased libido – Osteoporosis, decreased resistance to infection – Hypertension, edema

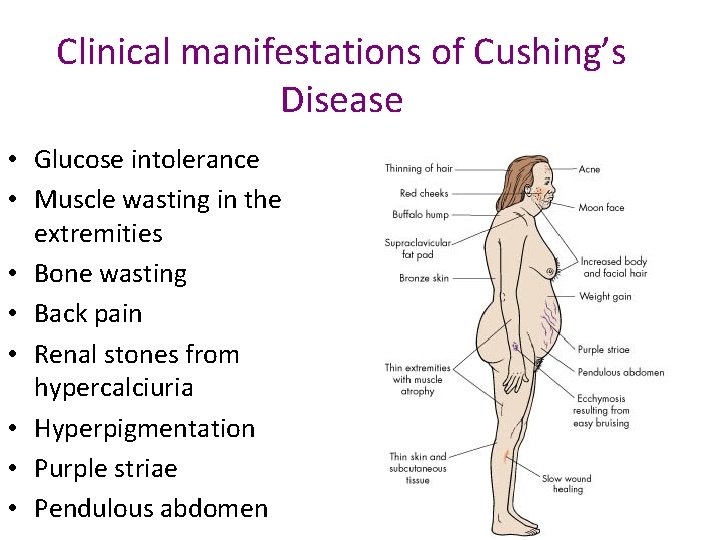
Clinical manifestations of Cushing’s Disease • Glucose intolerance • Muscle wasting in the extremities • Bone wasting • Back pain • Renal stones from hypercalciuria • Hyperpigmentation • Purple striae • Pendulous abdomen

Disorders of the Adrenal Gland Cushing’s Syndrome • Diagnostic Test – Cortisol levels increased – Slight hypernatremia – Hypokalemia – Hyperglycemia

How is Cushing's syndrome diagnosed? • The Dexamethasone-CRH Test – Some individuals have high cortisol levels, but do not develop the progressive effects of Cushing's syndrome, such as muscle weakness, fractures and thinning of the skin. – These individuals may have Pseudo Cushing's syndrome, which was originally described in people who were depressed or drank excess alcohol, but is now known to be more common. – Pseudo Cushing's does not have the same long-term effects on health as Cushing's syndrome and does not require treatment directed at the endocrine glands. – Developed to distinguish between the conditions rapidly, so that Cushing's patients can receive prompt treatment. Elevations of cortisol during this test suggest Cushing's syndrome.

How is Cushing's syndrome diagnosed? • 24 -Hour Urinary Free Cortisol Level – Most specific diagnostic test. – Patient's urine is collected over a 24 -hour period and tested for the amount of cortisol. – Levels higher than 50– 100 micrograms a day for an adult suggest Cushing's syndrome. • Dexamethasone Suppression Test – Helps to distinguish patients with excess production of ACTH due to pituitary adenomas from those with ectopic ACTH-producing tumors. – Patients are given dexamethasone, a synthetic glucocorticoid, by mouth every 6 hours for 4 days. – Patients are given an injection of CRH, the corticotropin-releasing hormone which causes the pituitary to secrete ACTH. – Patients with pituitary adenomas usually experience a rise in blood levels of ACTH and cortisol. This response is rarely seen in patients with ectopic ACTH syndrome and practically never in patients with cortisol-secreting adrenal tumors.
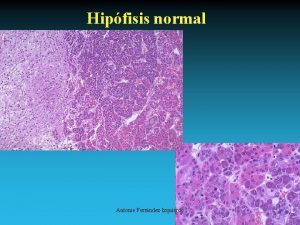
How is Cushing's syndrome diagnosed? • CRH Stimulation Test (continued) – For the first 2 days, low doses of dexamethasone are given, and for the last 2 days, higher doses are given. – 24 hour urine collections are made before dexamethasone is administered and on each day of the test. Since cortisol and other glucocorticoids signal the pituitary to lower secretion of ACTH, the normal response after taking dexamethasone is a drop in blood and urine cortisol levels. • Direct Visualization of the Endocrine Glands (Radiologic Imaging) – Imaging tests reveal the size and shape of the pituitary and adrenal glands and help determine if a tumor is present. – CT (computerized tomography) scan – MRI (magnetic resonance imaging).
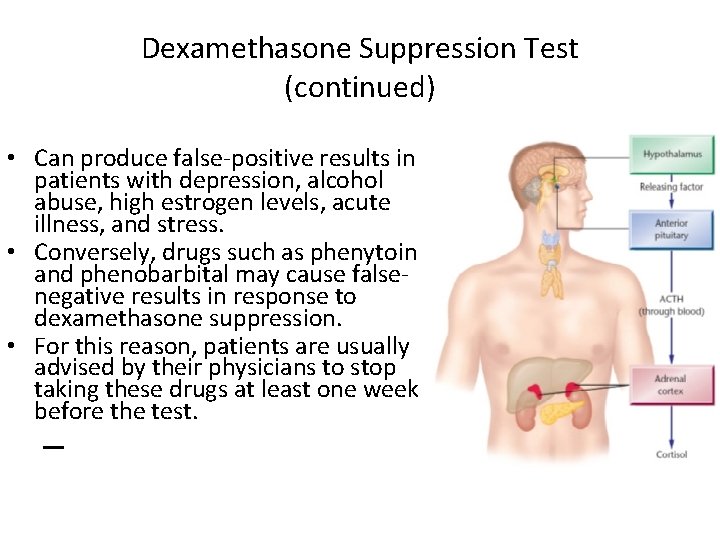
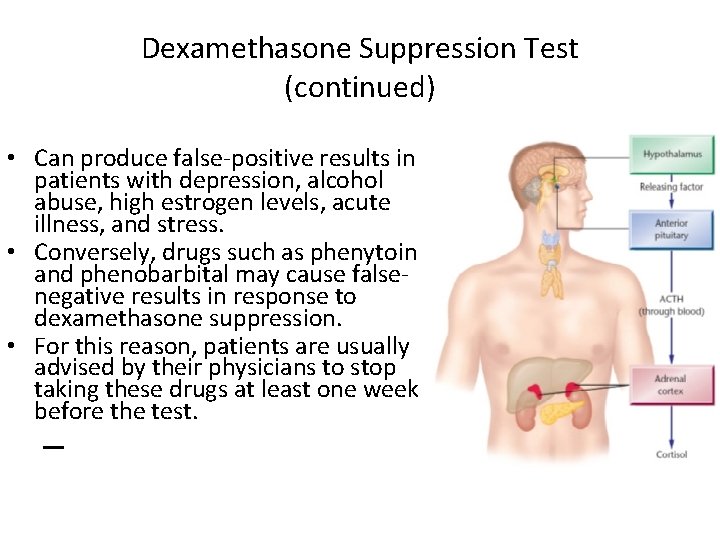
Dexamethasone Suppression Test (continued) • Can produce false-positive results in patients with depression, alcohol abuse, high estrogen levels, acute illness, and stress. • Conversely, drugs such as phenytoin and phenobarbital may cause falsenegative results in response to dexamethasone suppression. • For this reason, patients are usually advised by their physicians to stop taking these drugs at least one week before the test. –

Dexamethasone Suppression Test Procedure 1. Administration of 1. 0 mg dexamethasone orally at 11 p. m 2. Samples for plasma cortisol measurement are collected the following day at 4 p. m and 11 p. m. * * * there is no special patient preparation * * * - if either the 4 p. m of the 11 p. m sample shows a total cortisol level greater than 5. 0 ug/d. L the test is considered positive of endogenous depression. - a rise in the 4 p. m value above the 5. 0 ug/d. L cutoff is termed early escape a strong degree of resistance to suppression of cortisol synthesis by dexamethasone.
Normal Results • Cortisol levels should decrease after you receive dexamethasone. • Low dose: • Overnight: 8 a. m. plasma cortisol <> • High dose: • Overnight: > 50% reduction in plasma cortisol
How is Cushing's syndrome diagnosed? • Petrosal Sinus Sampling – This test is not always required, but in many cases, it is the best way to separate pituitary from ectopic causes of Cushing's syndrome. – Samples of blood are drawn from the petrosal sinuses, veins which drain the pituitary, by introducing catheters through a vein in the upper thigh/groin region, with local anesthesia and mild sedation. – X-rays are used to confirm the correct position of the catheters. – Often CRH, the hormone which causes the pituitary to secrete ACTH, is given during this test to improve diagnostic accuracy. – Levels of ACTH in the petrosal sinuses are measured and compared with ACTH levels in a forearm vein. – ACTH levels higher in the petrosal sinuses than in the forearm vein indicate the presence of a pituitary adenoma; similar levels suggest ectopic ACTH syndrome.
How is Cushing's syndrome diagnosed? • Direct Visualization of the Endocrine Glands (Radiologic Imaging) – Imaging tests reveal the size and shape of the pituitary and adrenal glands and help determine if a tumor is present. – CT (computerized tomography) scan – MRI (magnetic resonance imaging).
Disorders of the Adrenal Gland Cushing’s Syndrome – Management • Surgery is uses when etiology is primary tumor. • Replacement hormones are necessary following surgery • Medical management may include diet therapy and radiation
How is Cushing's syndrome treated? • Treatment depends on the specific reason for cortisol excess and may include surgery, radiation, chemotherapy or the use of cortisol-inhibiting drugs. • If the cause is long-term use of glucocorticoid hormones to treat another disorder, the doctor will gradually reduce the dosage to the lowest dose adequate for control of that disorder. • Once control is established, the daily dose of glucocorticoid hormones may be doubled and given on alternate days to lessen side effects.
How is Cushing's syndrome treated? • Ectopic ACTH Syndrome – Overproduction of cortisol caused by ectopic ACTH syndrome, it is necessary to eliminate all of the cancerous tissue that is secreting ACTH. – The choice of cancer treatment—surgery, radiotherapy, chemotherapy, immunotherapy, or a combination of these treatments—depends on the type of cancer and how far it has spread. – Since ACTH-secreting tumors (for example, small cell lung cancer) may be very small or widespread at the time of diagnosis, cortisolinhibiting drugs, like mitotane, are an important part of treatment. – In some cases, if pituitary surgery is not successful, surgical removal of the adrenal glands (bilateral adrenalectomy) may take the place of drug therapy.
How is Cushing's syndrome treated? Pituitary Adenomas • Several therapies are available to treat the ACTH-secreting pituitary adenomas of Cushing's disease. • Using a special microscope and very fine instruments, the surgeon approaches the pituitary gland through a nostril or an opening made below the upper lip. • Because this is an extremely delicate procedure, patients are often referred to centers specializing in this type of surgery.
How is Cushing's syndrome treated? Pituitary Adenomas • The success, or cure, rate of this procedure is over 80 percent when performed by a surgeon with extensive experience. • If surgery fails, or only produces a temporary cure, surgery can be repeated, often with good results. • After curative pituitary surgery, the production of ACTH drops two levels below normal. • This is a natural, but temporary, drop in ACTH production, and patients are given a synthetic form of cortisol (such as hydrocortisone or prednisone). • Most patients can stop this replacement therapy in less than a year.

Disorders of the Adrenal Gland Cushing’s Syndrome • Nursing Interventions – Maintain muscle tone • Provide ROM exercises • Assist with ambulation – Prevent accidents or falls and provide adequate rest – Protect client from exposure to infection – Maintain skin integrity • Provide meticulous skin care • Prevent tearing of skin; use paper tape if necessary
Disorders of the Adrenal Gland Cushing’s Syndrome • Nursing Interventions (continued) – Minimize stress in the environment – Monitor vital signs; observe for hypertension, edema – Measure I&O and daily weights – Provide diet low in calories and sodium and high in protein, potassium, calcium, and vitamin D – Monitor urine for glucose and acetone; administer insulin if ordered – Provide psychologic support and acceptance – Prepare client for hypophysectomy or radiation if condition is caused by a pituitary tumor.

Disorders of the Adrenal Gland Cushing’s Syndrome • Nursing Interventions (continued) • Prepare client for an adrenalectomy if condition is caused by an adrenal tumor or hyperplasia – Provide client teaching and discharge planning concerns • • Diet modifications Importance of adequate rest Need to avoid stress and infection Change in medication regimen – Alternate day therapy or reduced dosage if cause of the condition is prolonged corticosteroid therapy – Adding Imuran (azathioprine)-chemotherapeutic agent could decrease steroid use
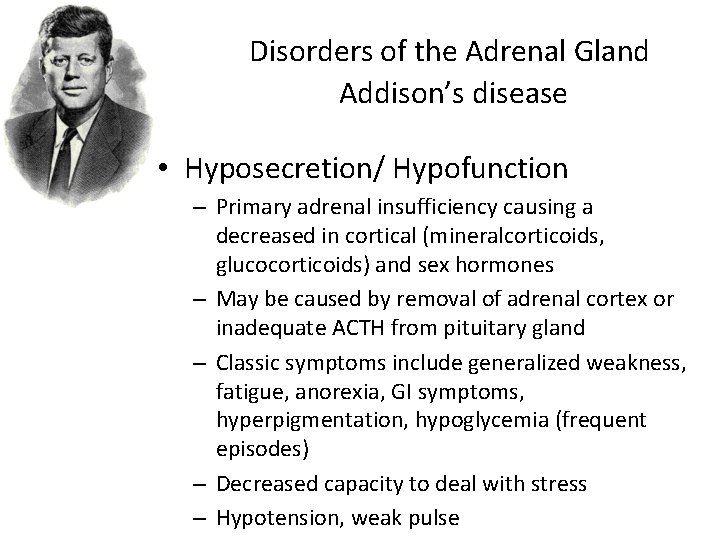
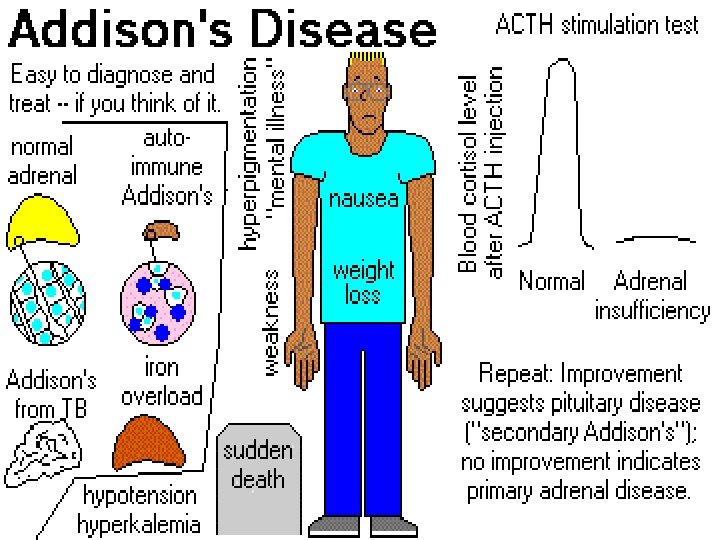
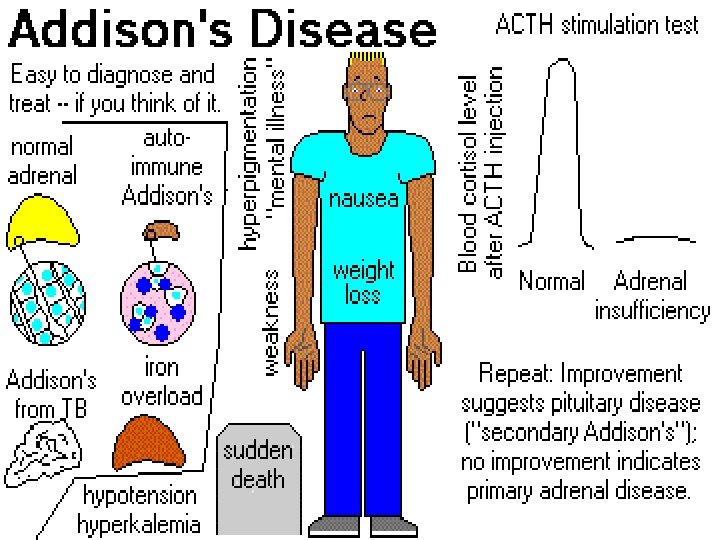
Disorders of the Adrenal Gland Addison’s disease • Hyposecretion/ Hypofunction – Primary adrenal insufficiency causing a decreased in cortical (mineralcorticoids, glucocorticoids) and sex hormones – May be caused by removal of adrenal cortex or inadequate ACTH from pituitary gland – Classic symptoms include generalized weakness, fatigue, anorexia, GI symptoms, hyperpigmentation, hypoglycemia (frequent episodes) – Decreased capacity to deal with stress – Hypotension, weak pulse
Disorders of the Adrenal Gland Addison’s disease • Diagnostic Studies – Low cortisol levels – Hyponatremia – Hyperkalemia – Hypoglycemia

Disorders of the Adrenal Gland Addison’s Disease Nursing interventions – Administer hormone replacement therapy as ordered • Clucocorticoids (cortisone, hydrocortisone): to stimulate diurnal rhythm of cortisol release, give 2/3 of dose in early morning and 1/3 of dose in afternoon • Mineralcorticoids: fludrocortisone acetate (Florinef) • Monitor vital signs • Decrease stress in the environment • Prevent exposure to infection • Provide rest periods; prevent fatigue • Monitor I and O
Disorders of the Adrenal Gland Addison’s disease • Nursing interventions (continued) – Weigh daily – Provide small, frequent feedings of diet high in carbohydrates, sodium and protein to prevent hypoglycemia and hyponatremia and provide proper nutrition The nineteenth century British physician Thomas Addison (1793 -1860) was the first to relate the symptoms of Addison's Disease to problems with the adrenal glands.
Disorders of the Adrenal Gland Addison’s disease • Nursing interventions (continued) • Provide client teaching and discharge planning concerning: – Disease process; signs of adrenal insufficiency – Use of prescribed medications for lifelong replacement therapy; never omit medications – Need to avoid stress, trauma and infections, and to notify physician if these occur as medication may need to be adjusted – Stress management techniques – Diet modification (high in protein, carbos, and sodium) – Use of salt tablets (if prescribed) or ingestion of the GOOD STUFF! Like potato chips! If having increased sweating. – Importance of alternating regular exercise with rest periods – Avoidance of strenuous exercise especially in hot weather
Disorders of the Adrenal Gland Addison’s disease • Adrenal Crisis • Severe exacerbation of Addison’s Disease • Acute adrenal insufficiency • Seen with severe stress or illness; may show acute hypotension, confusion, nausea/vomiting, and signs of shock • Management – Hormonal replacement – cortisol to be given with careful monitoring of patient. Hydrocortisone 100 -200 mg/day in times of stress – Patient education for patient needing long-term replacement therapy. Special attention for measures to be taken at times of physical or emotional stress

Disorders of the Adrenal Gland Addison’s disease • Adrenal Crisis - Nursing Interventions – Administer IV fluids (D 5 NS) as ordered to treat vascular collapse – Administer IV glucocorticoids (hydrocortisone-Solu. Cortef – and vasopressors as ordered – If crisis precipitated by infection, administer antibiotics as ordered – Maintain strict bed rest and eliminate all forms of stressful stimuli – Monitor vital signs, I and O, daily weights – Protect patient from infection – Provide teaching and discharge planning same as Addison’s Disease
Disorders of the Adrenal Gland • Disorders related to hypersecretion of epinephrine and norepinephrine – Most commonly cause by rare tumor known as a pheochromocytoma, usually stemming from medulla – Excessive secretion of epinephrine and norepinephrine cause severe hypertension, headache, nervousness, perspiration, tachycardia, and often hyperglycemia, dilation of pupils, cold extremities – Acute attacks of hypertension also may cause blurry vision, vertigo, and dyspnea • Diagnostic Tests – Increased plasma and urine catecholamines – Elevated glucose – Presence of tumor on x-ray
Disorders related to hypersecretion of epinephrine and norepinephrine • Management – Treatment of choice of pheochromocytoma is surgical removal of actual tumor – Antihypertensive medication, such as adrenergic-blocking agents, may be useful in controlling blood pressure – Nursing Interventions – Monitor VS, especially BP – Administer meds for HTN as prescribed – Promote rest; decrease stress – Monitor urine and serum levels – Provide well-balanced meals-no stimulants – Once adrenalectomy watch for shock (drastic drop in catecholamines) may need vasopressor therapy – Provide teaching
 Adrenal gland
Adrenal gland Hormones
Hormones Chapter 45 hormones and the endocrine system
Chapter 45 hormones and the endocrine system Chapter 46 digestive and endocrine disorders
Chapter 46 digestive and endocrine disorders Chapter 29 endocrine and metabolic disorders
Chapter 29 endocrine and metabolic disorders Zona reticularis gonadocorticoids
Zona reticularis gonadocorticoids Cat dissection labeled
Cat dissection labeled Visceral autonomic nervous system
Visceral autonomic nervous system Adrenal medulla cortex
Adrenal medulla cortex Summary of adrenal gland
Summary of adrenal gland Peptit ve protein yapılı hormonlar
Peptit ve protein yapılı hormonlar Addison's vs conn's
Addison's vs conn's Adrenal sympathetic pathway
Adrenal sympathetic pathway Hiperplasia adrenal congênita não clássica
Hiperplasia adrenal congênita não clássica Adrenal gland regions
Adrenal gland regions Site:slidetodoc.com
Site:slidetodoc.com Neural plate formation
Neural plate formation Objectives for stress management
Objectives for stress management Adrenal gland epithelium
Adrenal gland epithelium Medulla
Medulla Betoderm
Betoderm Adrenal bez histolojisi
Adrenal bez histolojisi Adrenal bez embriyolojisi
Adrenal bez embriyolojisi Adrenal nervous system
Adrenal nervous system Adrenal cortex and medulla
Adrenal cortex and medulla Costan mefenamic acid
Costan mefenamic acid Adrenal tumour
Adrenal tumour Psödohermafrodit
Psödohermafrodit Histology thyroid gland
Histology thyroid gland Adrenal cortex develops from
Adrenal cortex develops from Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics Adrenal drugs pharmacology
Adrenal drugs pharmacology Cetosis e hipotiroidismo
Cetosis e hipotiroidismo Human body
Human body Adrenal yetmezlik acilci
Adrenal yetmezlik acilci Adrenal glands
Adrenal glands Adrenal cushing
Adrenal cushing Arritimias
Arritimias Ectocrine
Ectocrine Adrenal bezin hipofonksiyonu sonucu gelişen tablo
Adrenal bezin hipofonksiyonu sonucu gelişen tablo The adrenal medullae secrete
The adrenal medullae secrete Adrenal sympathetic pathway
Adrenal sympathetic pathway Relation of suprarenal gland
Relation of suprarenal gland