Classification and management of wound principle of wound

- Slides: 53
Classification and management of wound, principle of wound healing, haemorrhage and bleeding control 1 GYÖRGYI SZABÓ ASSISTANT PROFESSOR DEPARTMENT OF SURGICAL RESEARCH AND TECHNIQUES Basic Surgical Techniques, Faculty of Medicine, 3 rd year 2021/13 Academic Year, Second Semester
2 WOUND
What is a wound? 3 It is a circumscribed injury which is caused by an external force and it can involve any tissue or organ. surgical, traumatic It can be mild, severe, or even lethal. Simple wound Compound wound Acute Chronic
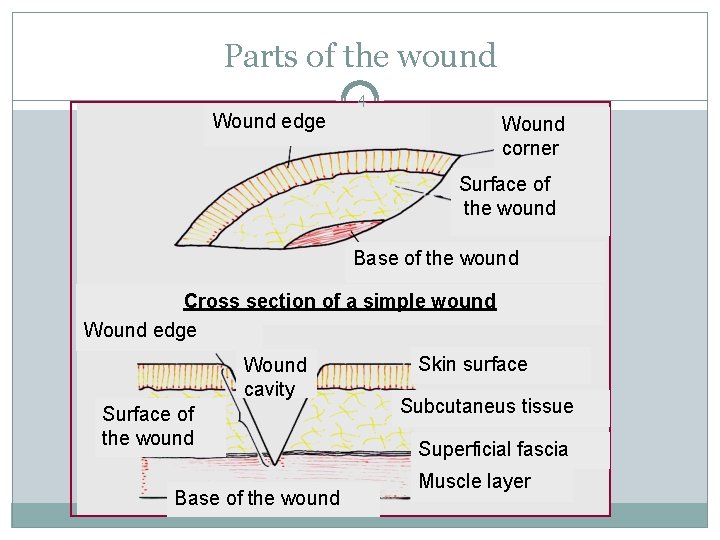
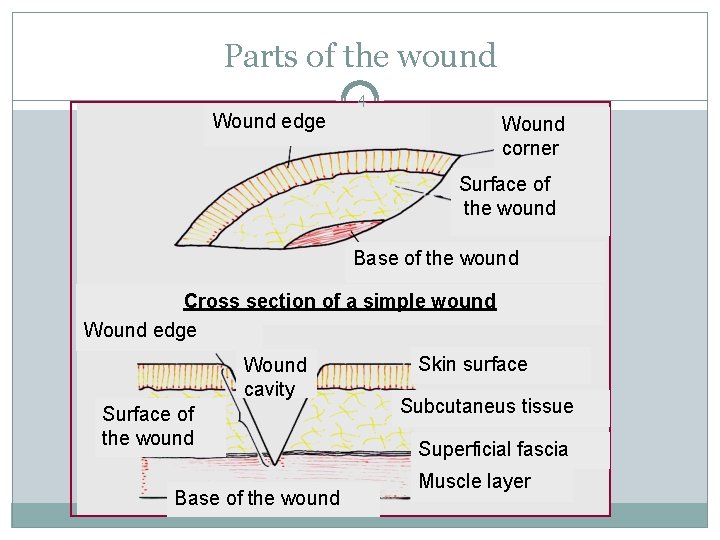
Parts of the wound 4 Wound edge Wound corner Surface of the wound Base of the wound Cross section of a simple wound Wound edge Wound cavity Surface of the wound Base of the wound Skin surface Subcutaneus tissue Superficial fascia Muscle layer
The ABCDE in the injured assessment 5 The mnemonic ABCDE is used to remember the order of assessment with the purpose to treat first that kills first. A: Airway and C-spine stabilization B: Breathing C: Circulation D: Disability E: Environment and Exposure
Wound management - anamnesis 6 When and where was the wound occured? Alcohol and drug consumption What did caused the wound? The circumstances of the injury Other diseases eg. diabetes mellitus, tumour, atherosclesosis, allergy The state of patient’s vaccination against Tetanus Prevention of rabies The applied first-aid
Classification of the accidental wounds 1. Based on the origine 7 � I. Mechanical: 1. Abraded wound (vulnus abrasum) 2. Puncured wound (v. punctum) 3. Incised wound (v. scissum) 4. Cut wound (v. caesum) 5. Crush wound (v. contusum) 6. Torn wound (v. lacerum) 7. Bite wound (v. morsum) 8. Shot wound (v. sclopetarium) � II. Chemical: 1. Acid 2. Base � III. Wounds caused by radiation � IV. Wounds caused by thermal forces: 1. Burning 2. Freezing � V. Special
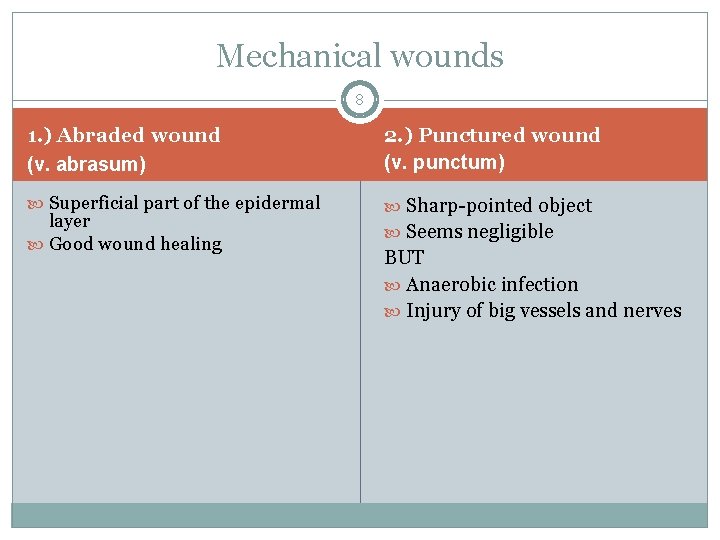
Mechanical wounds 8 1. ) Abraded wound (v. abrasum) 2. ) Punctured wound (v. punctum) Superficial part of the epidermal Sharp-pointed object layer Good wound healing Seems negligible BUT Anaerobic infection Injury of big vessels and nerves
Mechanical wounds 9 3. ) Incised wound (v. scissum) 4. ) Cut wound (v. caesum) Sharp object + blunt additional Best healing force Edges - uneven
Mechanical wounds 10 5. ) Crush wound (v. contusum) Blunt force Pressure injury Edges – uneven and torn Bleeding 6. ) Torn wound (v. lacerum) Great tearing or pulling Incomplete amputation (v. lacerocontusum)
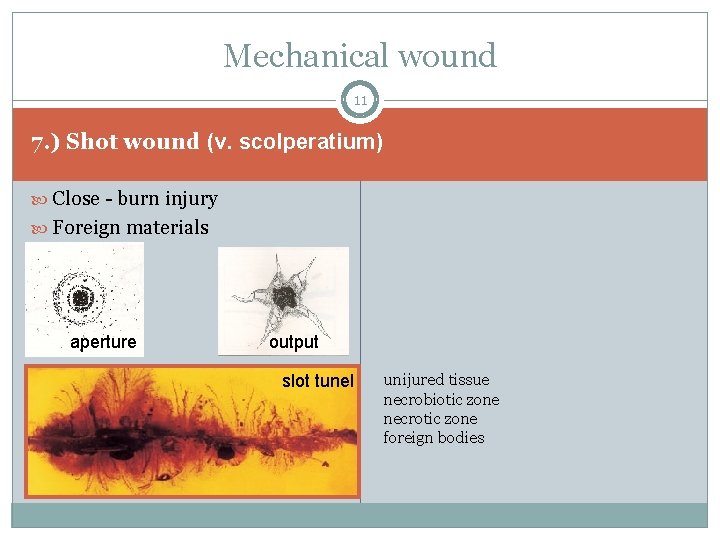
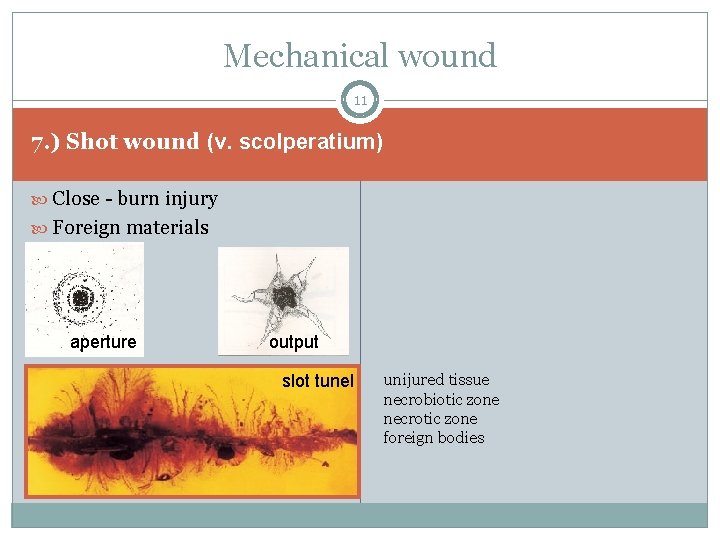
Mechanical wound 11 7. ) Shot wound (v. scolperatium) Close - burn injury Foreign materials aperture output slot tunel unijured tissue necrobiotic zone necrotic zone foreign bodies
Mechanical wounds 12 8. ) Bite wound (v. morsum) Ragged wound Crushed tissue Torn Infection Bone fracture Prevention of rabies Tetanus profilaxis
The direction of the flap 13 Distal Proximal The wound healing is good
Chemical wounds 14 1. ) Acid 2. ) Base in small concentration – irritate in large concentration – colliquative necrosis coagulation necrosis
Wounds caused by radiation 15 Symptoms and severity depend on: Amount of radiation Length of exposure Body part that was exposed Symptoms may occur immediately, after a few days, or even as long as months. What part of the body is most sensitive during radiation sickness? bone marrow gastrointestinal tract
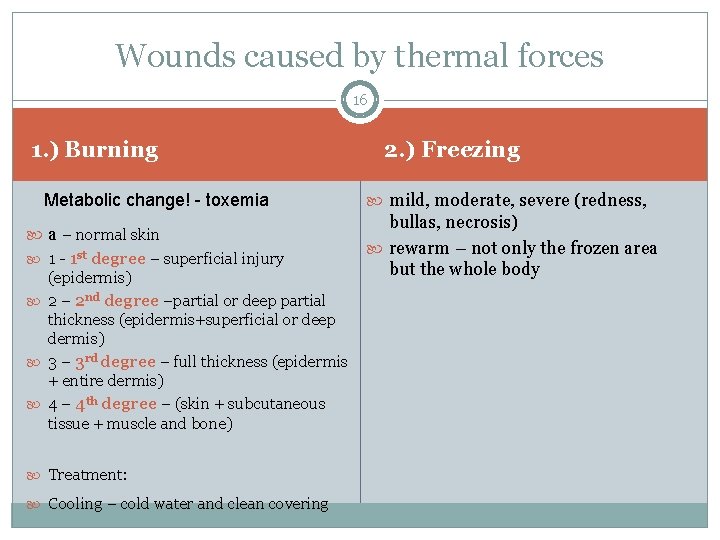
Wounds caused by thermal forces 16 1. ) Burning Metabolic change! - toxemia a – normal skin 1 - 1 st degree – superficial injury (epidermis) 2 – 2 nd degree –partial or deep partial thickness (epidermis+superficial or deep dermis) 3 – 3 rd degree – full thickness (epidermis + entire dermis) 4 – 4 th degree – (skin + subcutaneous tissue + muscle and bone) Treatment: Cooling – cold water and clean covering 2. ) Freezing mild, moderate, severe (redness, bullas, necrosis) rewarm – not only the frozen area but the whole body
Special wounds 17 Exotic, poisonous animals Toxins, venom - toxicologist Skin necrosis
Classification of the wounds 2. According to the bacterial contamination 18 Clean wound Clean-contaminated wound Contaminated wound Heavily contaminated wound
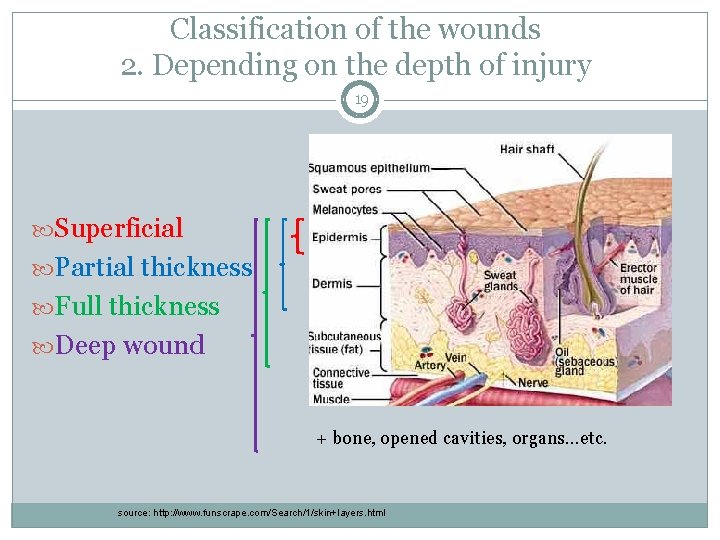
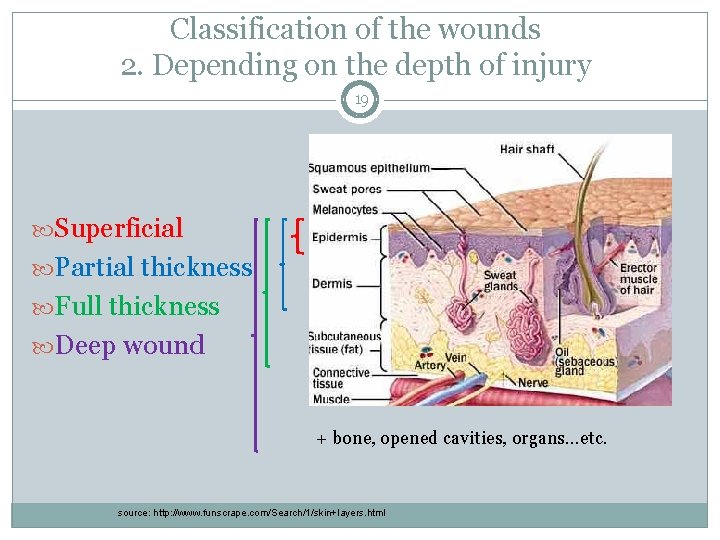
Classification of the wounds 2. Depending on the depth of injury 19 Superficial Partial thickness Full thickness Deep wound + bone, opened cavities, organs…etc. source: http: //www. funscrape. com/Search/1/skin+layers. html
Wound management - history 20 Ancient Egypt – lint (fibrous base-wound site closure), animal grease (barrier) and honey (antibiotic) „closing the wound preserved the soul” Greeks – acute wound= „fresh” wound; chronic wound = „non-healing” wound maintaining wound-site moisture Ambroise Paré – hot oil of roses and turpentine, ligature of arteries instead of cauterization Lister pretreated surgical gauze – Robert Wood Johnson 1870 s; gauze and wound dressings treated with iodide
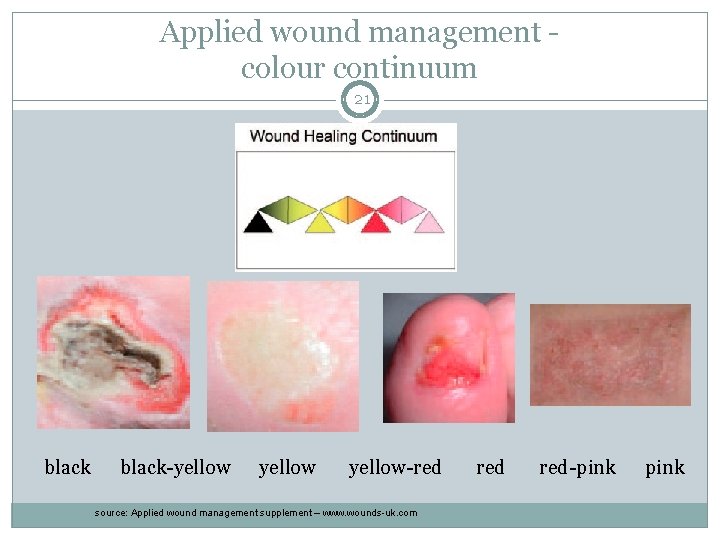
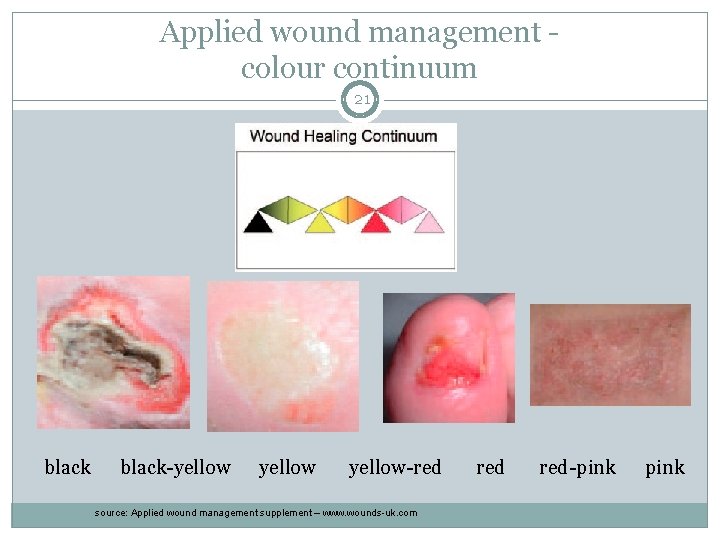
Applied wound management colour continuum 21 black-yellow-red source: Applied wound management supplement – www. wounds-uk. com red-pink
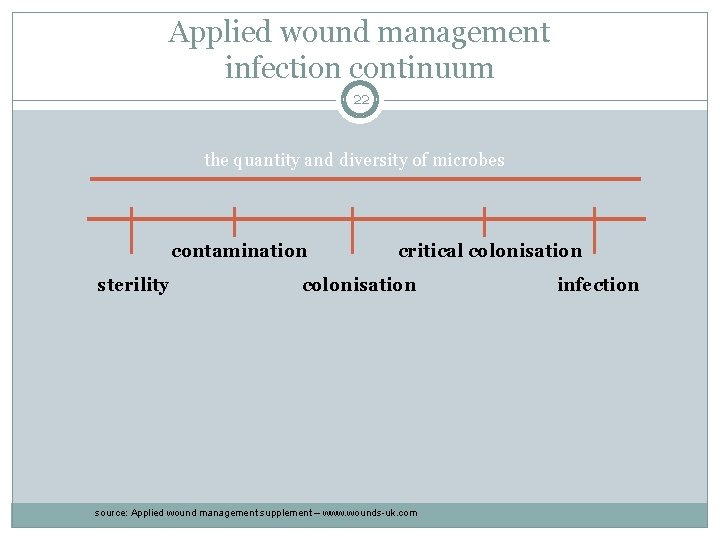
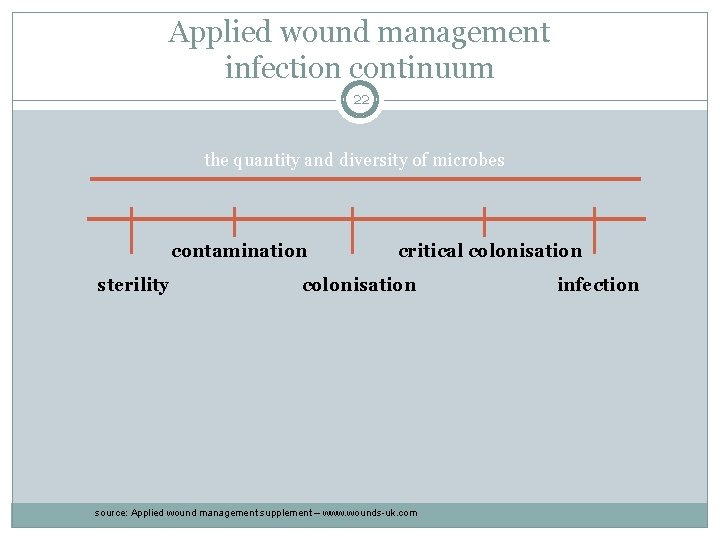
Applied wound management infection continuum 22 the quantity and diversity of microbes contamination sterility critical colonisation source: Applied wound management supplement – www. wounds-uk. com infection
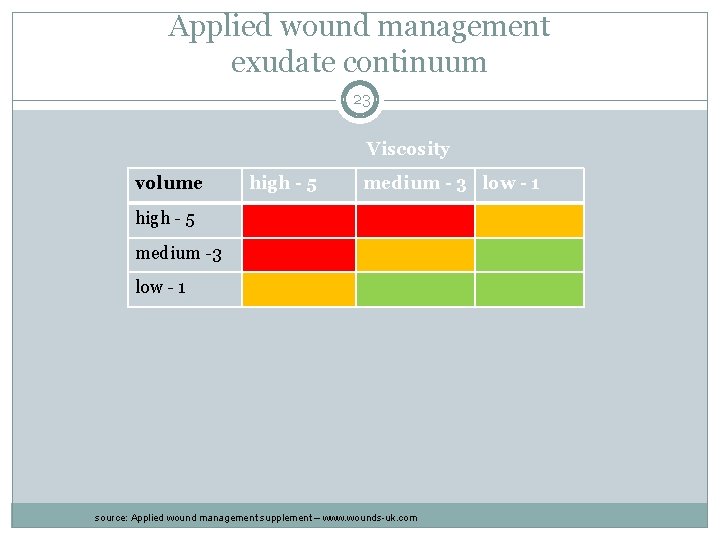
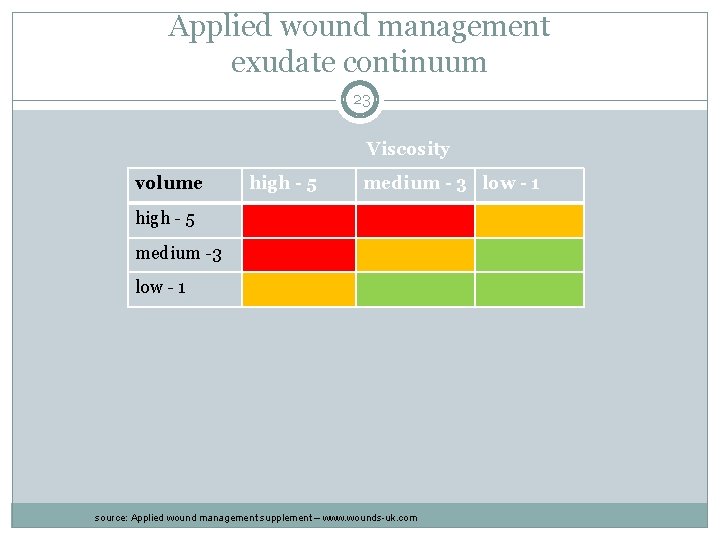
Applied wound management exudate continuum 23 Viscosity volume high - 5 medium - 3 low - 1 high - 5 medium -3 low - 1 source: Applied wound management supplement – www. wounds-uk. com
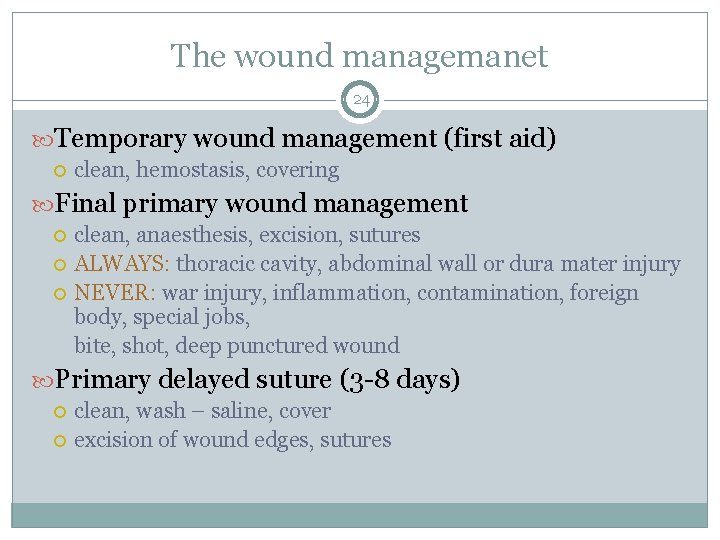
The wound managemanet 24 Temporary wound management (first aid) clean, hemostasis, covering Final primary wound management clean, anaesthesis, excision, sutures ALWAYS: thoracic cavity, abdominal wall or dura mater injury NEVER: war injury, inflammation, contamination, foreign body, special jobs, bite, shot, deep punctured wound Primary delayed suture (3 -8 days) clean, wash – saline, cover excision of wound edges, sutures
The wound managemanet 25 Early secondary wound closure (2 weeks) after inflammation, necrosis – proliferation anesthesia, refresh wound edges, suturing and draining Late secondary wound closure (4 -6 weeks) anesthesis, scar excision, suturing, draining greater defect – plastic surgery
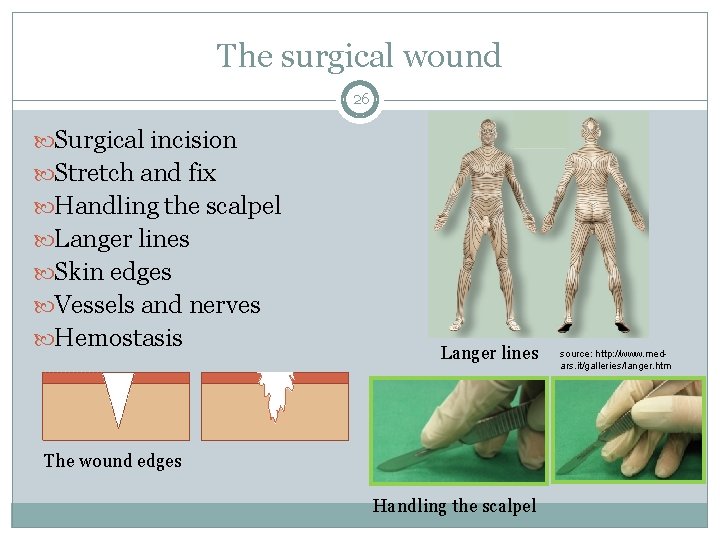
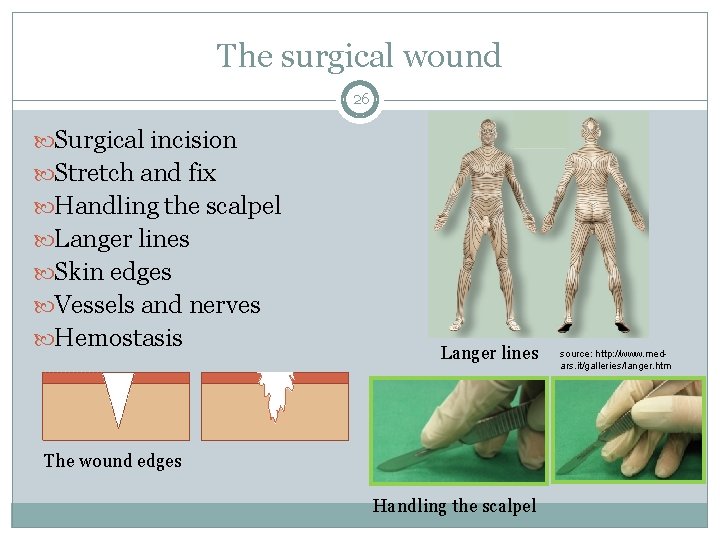
The surgical wound 26 Surgical incision Stretch and fix Handling the scalpel Langer lines Skin edges Vessels and nerves Hemostasis Langer lines The wound edges Handling the scalpel source: http: //www. medars. it/galleries/langer. htm
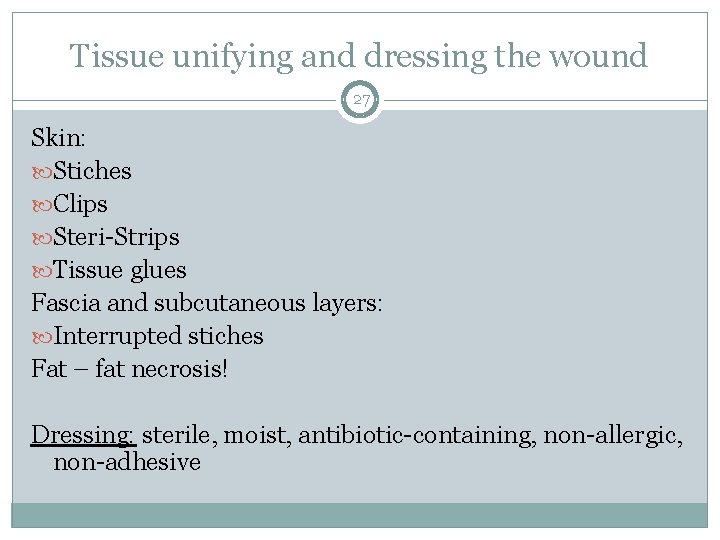
Tissue unifying and dressing the wound 27 Skin: Stiches Clips Steri-Strips Tissue glues Fascia and subcutaneous layers: Interrupted stiches Fat – fat necrosis! Dressing: sterile, moist, antibiotic-containing, non-allergic, non-adhesive
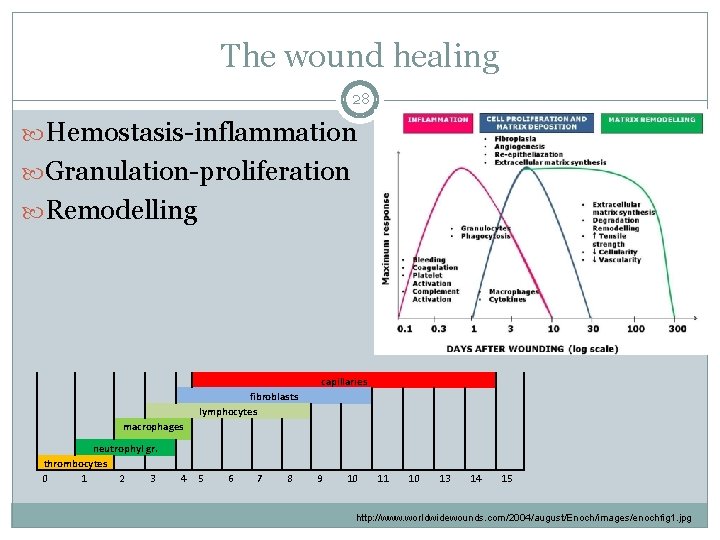
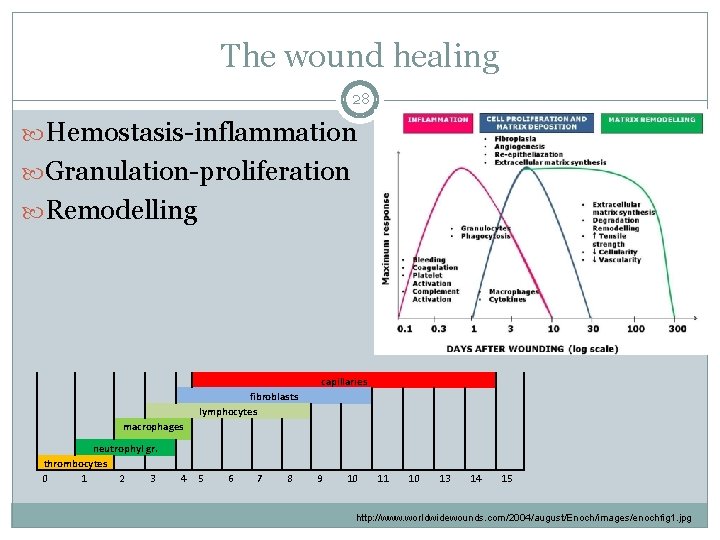
The wound healing 28 Hemostasis-inflammation Granulation-proliferation Remodelling capillaries fibroblasts lymphocytes macrophages neutrophyl gr. thrombocytes 0 1 2 3 4 5 6 7 8 9 10 11 10 13 14 15 http: //www. worldwidewounds. com/2004/august/Enoch/images/enochfig 1. jpg
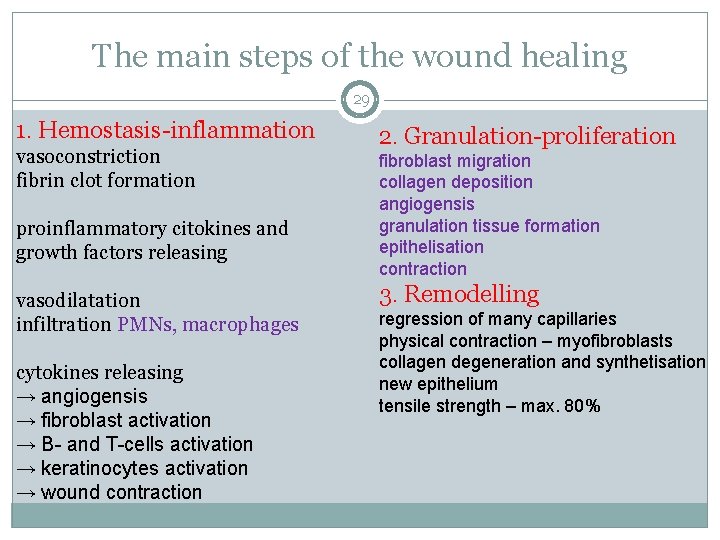
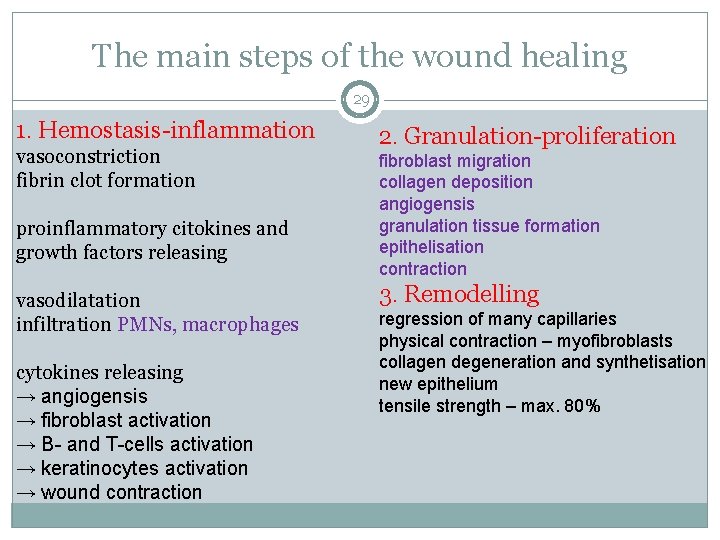
The main steps of the wound healing 29 1. Hemostasis-inflammation vasoconstriction fibrin clot formation proinflammatory citokines and growth factors releasing vasodilatation infiltration PMNs, macrophages cytokines releasing → angiogensis → fibroblast activation → B- and T-cells activation → keratinocytes activation → wound contraction 2. Granulation-proliferation fibroblast migration collagen deposition angiogensis granulation tissue formation epithelisation contraction 3. Remodelling regression of many capillaries physical contraction – myofibroblasts collagen degeneration and synthetisation new epithelium tensile strength – max. 80%
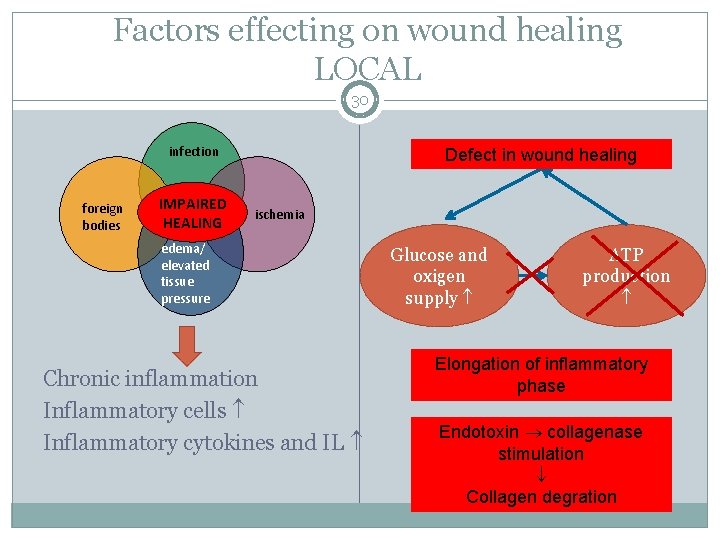
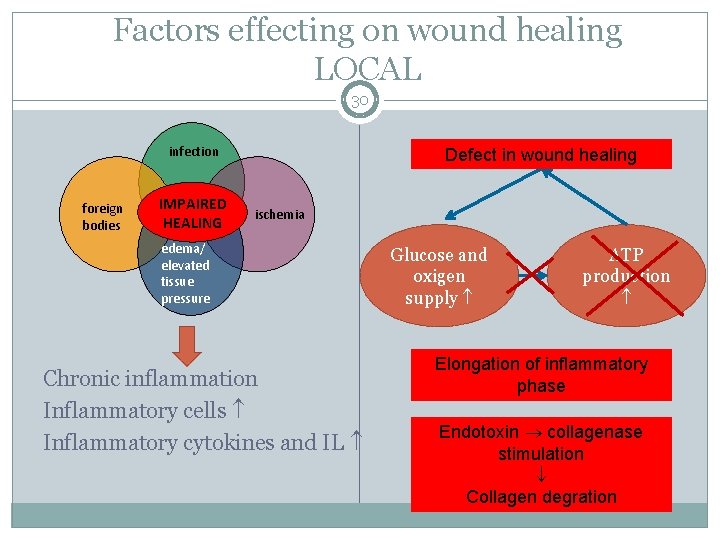
Factors effecting on wound healing LOCAL 30 infection foreign bodies IMPAIRED HEALING Wound Defect healing in wound needs healing energy ischemia edema/ elevated tissue pressure Chronic inflammation Inflammatory cells Inflammatory cytokines and IL Glucose and oxigen supply ATP production Elongation of inflammatory phase Endotoxin collagenase stimulation Collagen degration
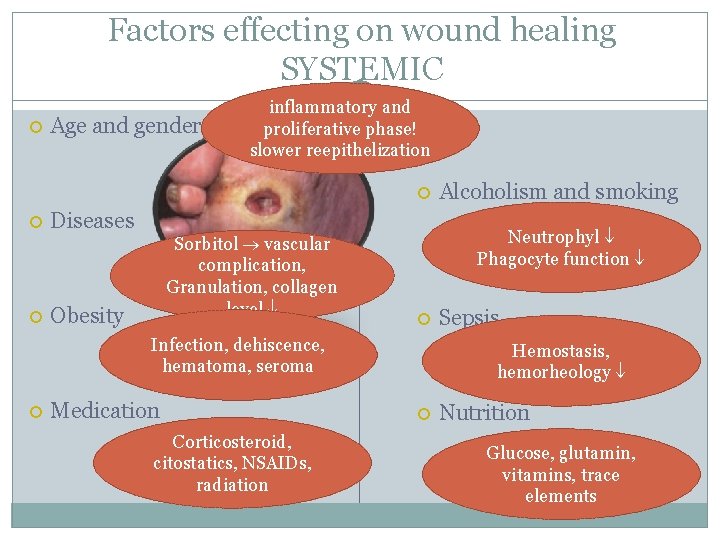
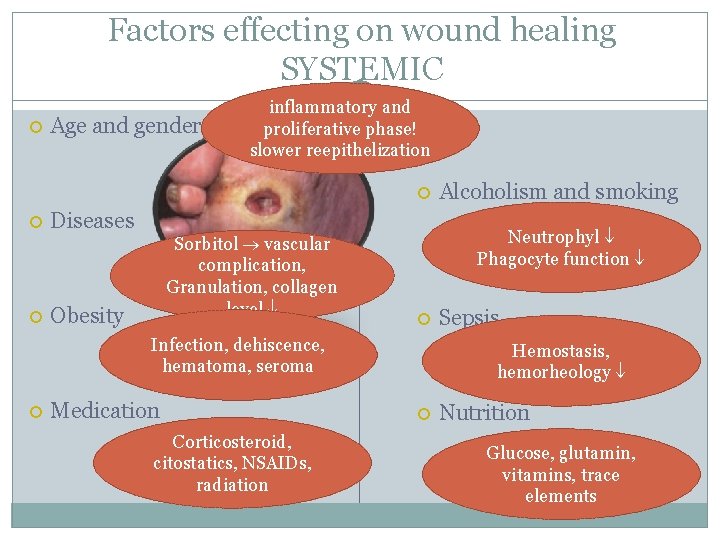
Factors effecting on wound healing SYSTEMIC Age and gender 31 inflammatory and proliferative phase! slower reepithelization Diseases Sorbitol vascular complication, diabetes Granulation, collagen level Obesity Neutrophyl Phagocyte function Infection, dehiscence, hematoma, seroma Medication Corticosteroid, citostatics, NSAIDs, radiation Alcoholism and smoking Sepsis Hemostasis, hemorheology Nutrition Glucose, glutamin, vitamins, trace elements
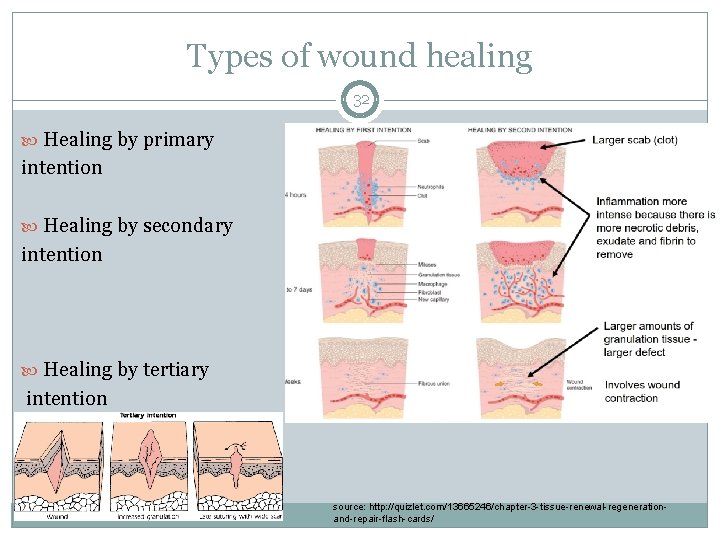
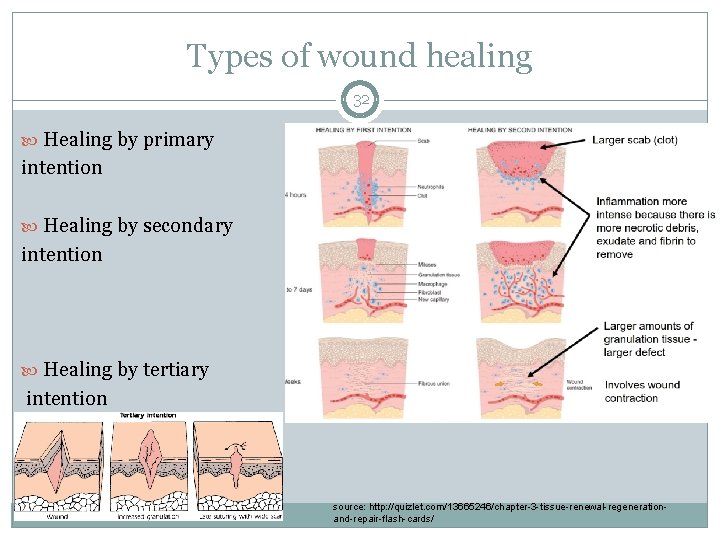
Types of wound healing 32 Healing by primary intention Healing by secondary intention Healing by tertiary intention source: http: //quizlet. com/13665246/chapter-3 -tissue-renewal-regenerationand-repair-flash-cards/

Complications of wound healing I. Early complications 33 Seroma Hematoma Wound disruptin Superficial wound infection Deep wound infection Mixed wound infection
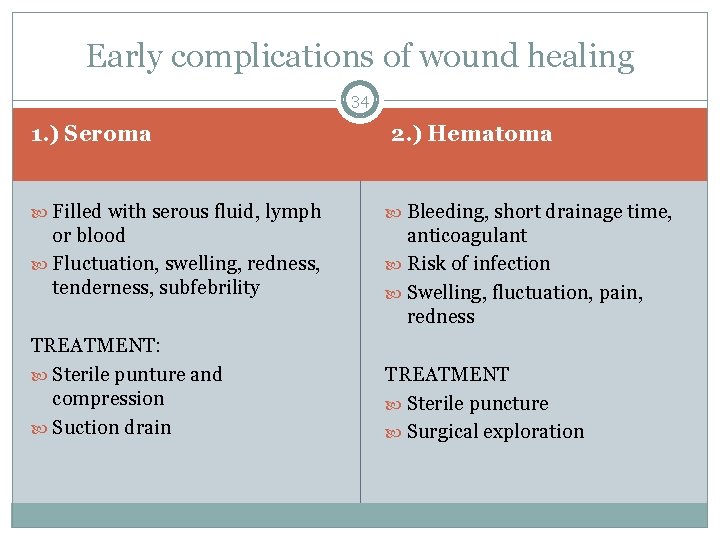
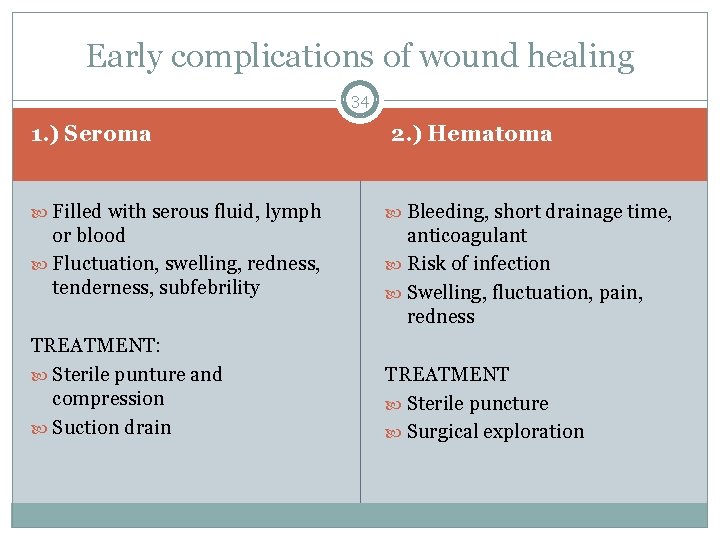
Early complications of wound healing 34 1. ) Seroma 2. ) Hematoma Filled with serous fluid, lymph Bleeding, short drainage time, or blood Fluctuation, swelling, redness, tenderness, subfebrility anticoagulant Risk of infection Swelling, fluctuation, pain, redness TREATMENT: Sterile punture and compression Suction drain TREATMENT Sterile puncture Surgical exploration
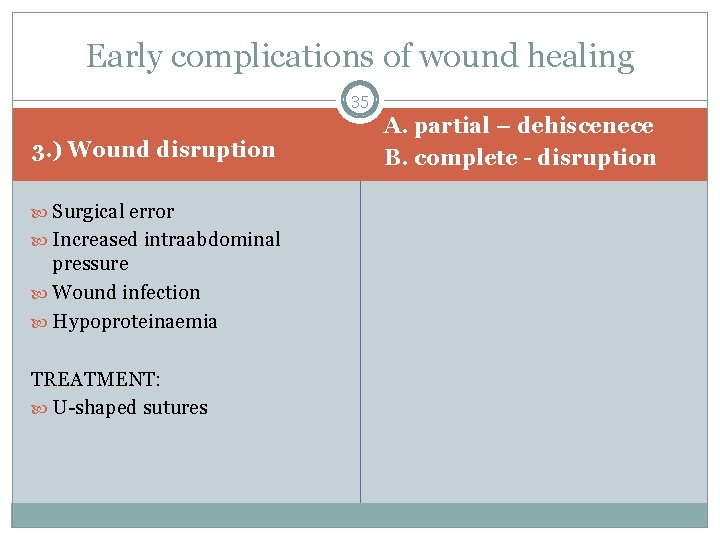
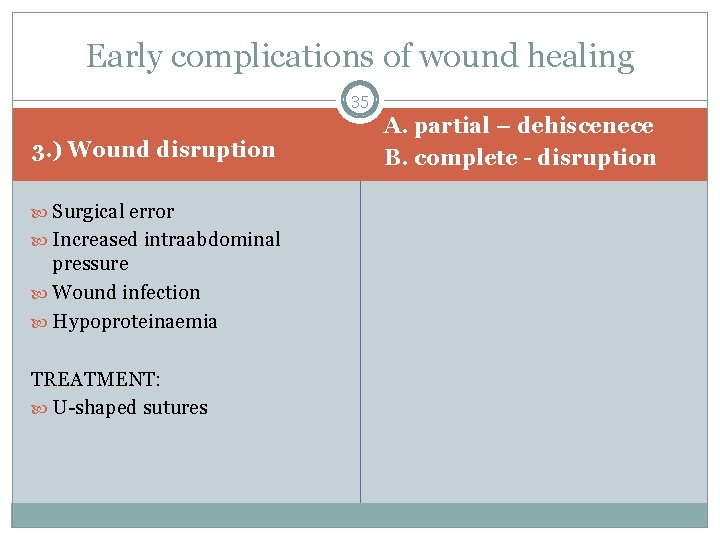
Early complications of wound healing 35 3. ) Wound disruption Surgical error Increased intraabdominal pressure Wound infection Hypoproteinaemia TREATMENT: U-shaped sutures A. partial – dehiscenece B. complete - disruption
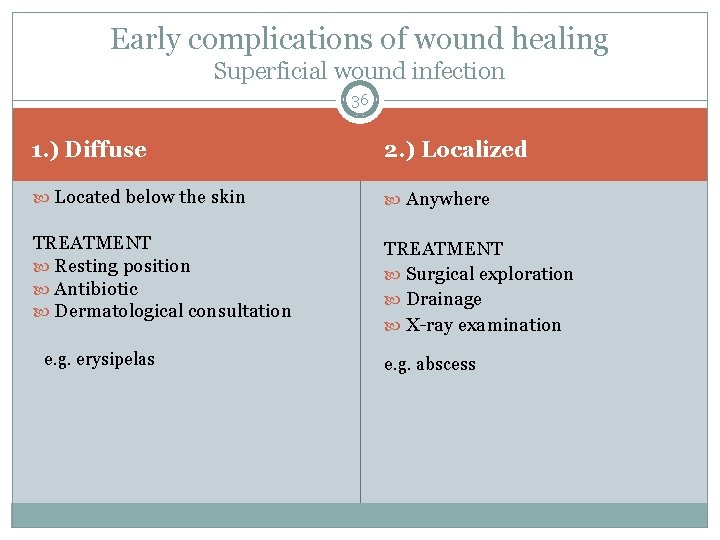
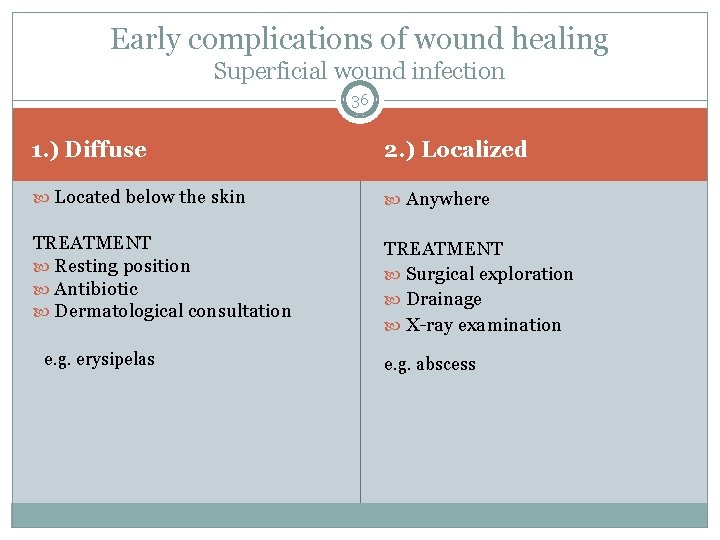
Early complications of wound healing Superficial wound infection 36 1. ) Diffuse 2. ) Localized Located below the skin Anywhere TREATMENT Resting position Antibiotic Dermatological consultation TREATMENT Surgical exploration Drainage X-ray examination e. g. erysipelas e. g. abscess
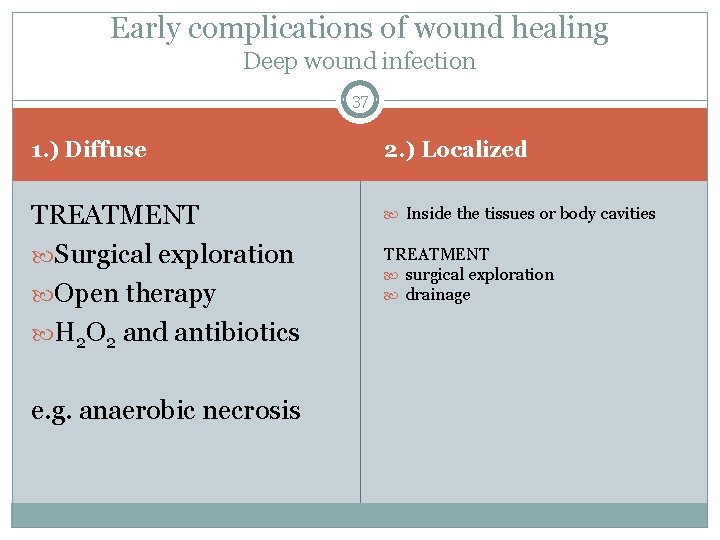
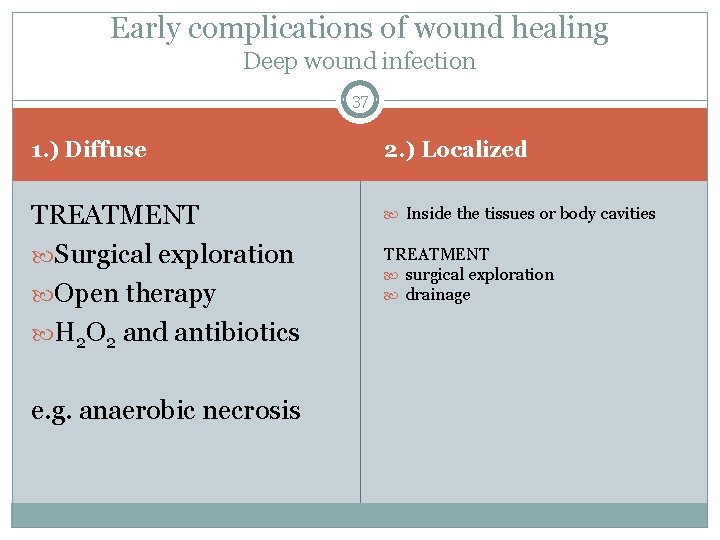
Early complications of wound healing Deep wound infection 37 1. ) Diffuse 2. ) Localized TREATMENT Surgical exploration Open therapy H 2 O 2 and antibiotics Inside the tissues or body cavities e. g. anaerobic necrosis TREATMENT surgical exploration drainage
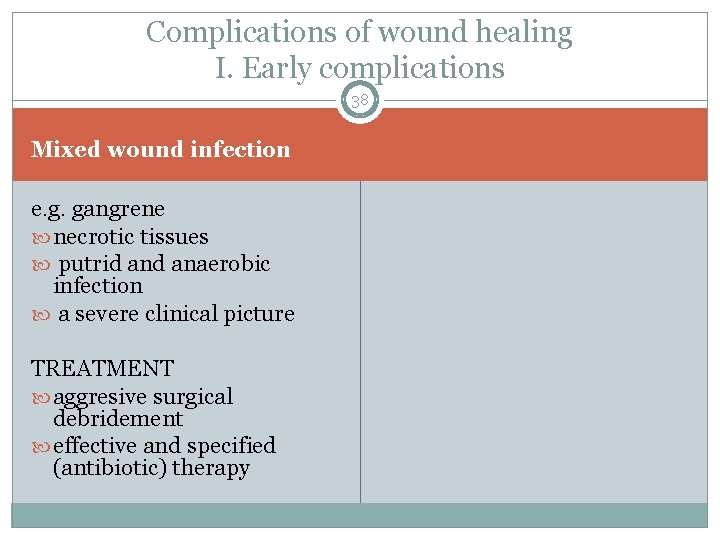
Complications of wound healing I. Early complications 38 Mixed wound infection e. g. gangrene necrotic tissues putrid anaerobic infection a severe clinical picture TREATMENT aggresive surgical debridement effective and specified (antibiotic) therapy
Complications of wound healing II. Late complications 39 Hyperthrophic scar Keloid formation Necrosis Inflammatory infiltration Abscesses Foreign body containing abscesses
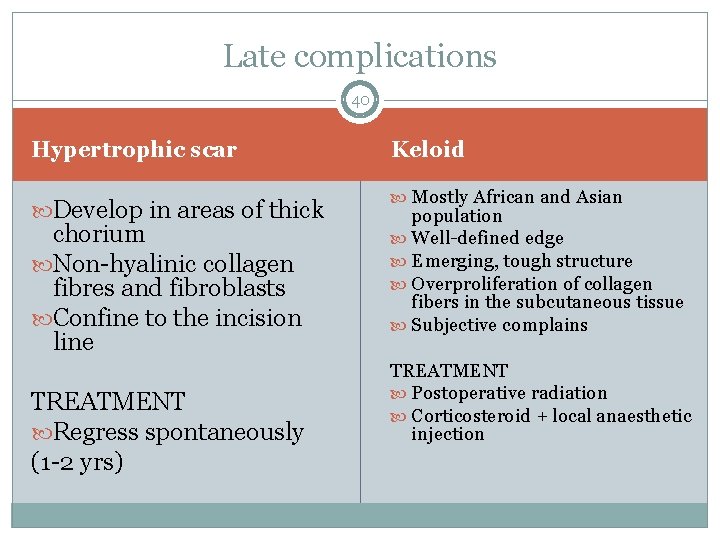
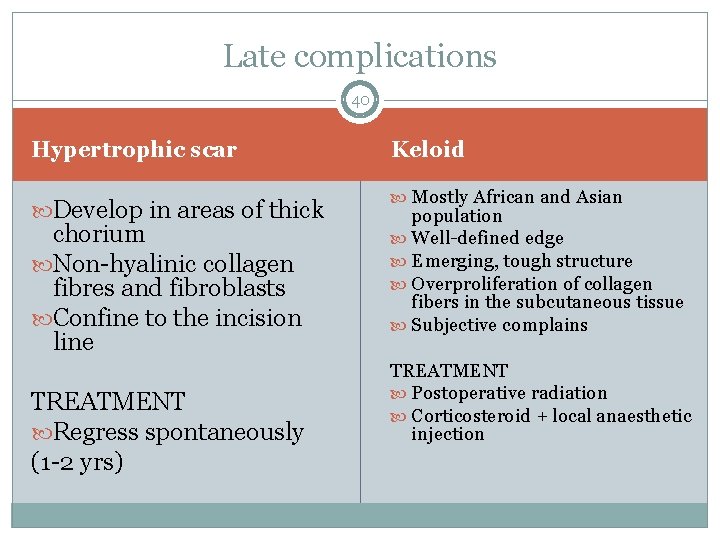
Late complications 40 Hypertrophic scar Develop in areas of thick chorium Non-hyalinic collagen fibres and fibroblasts Confine to the incision line TREATMENT Regress spontaneously (1 -2 yrs) Keloid Mostly African and Asian population Well-defined edge Emerging, tough structure Overproliferation of collagen fibers in the subcutaneous tissue Subjective complains TREATMENT Postoperative radiation Corticosteroid + local anaesthetic injection
41 BLEEDING AND HEMOSTASIS
Bleeding 42 Anatomical Arterial – bright red, pulsate Venous – dark red, continuous Diffuse Capillary – can become serious Parenchymal
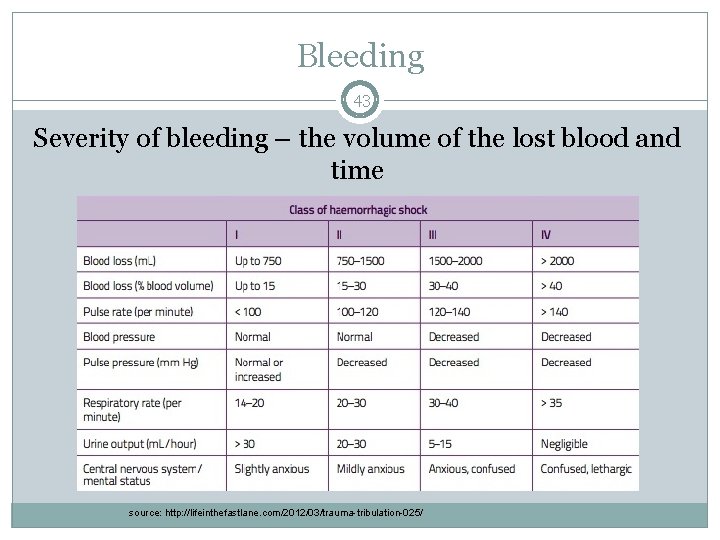
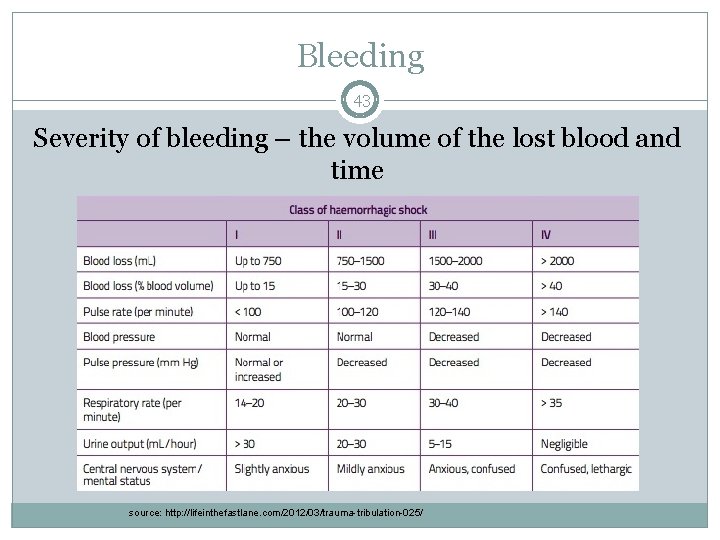
Bleeding 43 Severity of bleeding – the volume of the lost blood and time source: http: //lifeinthefastlane. com/2012/03/trauma-tribulation-025/
The direction of hemorrage 44 External Internal In a luminar organ (hematuria, hemoptoe, melena) In body cavities (intracranial, hemothorax, hemascos, hemopericardium, hemarthros) Among the tissues (hematoma, suffusion)
Bleeding 45 Preoperative hemorrhage Prehospital care! – maintenance of the airways, ventillation and circulation bandages, direct pressure, turniquets Intraoperative hemorrhage anatomical and/or diffuse depending on the surgeon, the surgery, position, the size of the vessel, pressure in the vessel ANESTHESIA! Postoperative bleeding ineffective local hemostasis, undetected hemostatic defect, consumptive coagulopathy or fibrinolysis
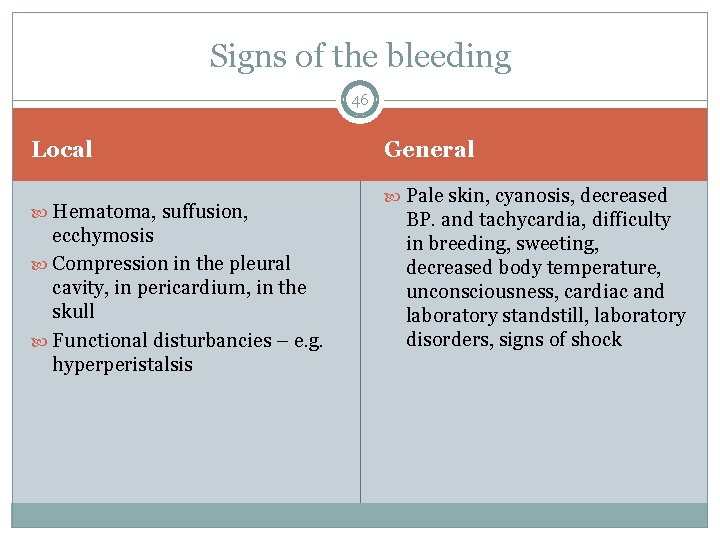
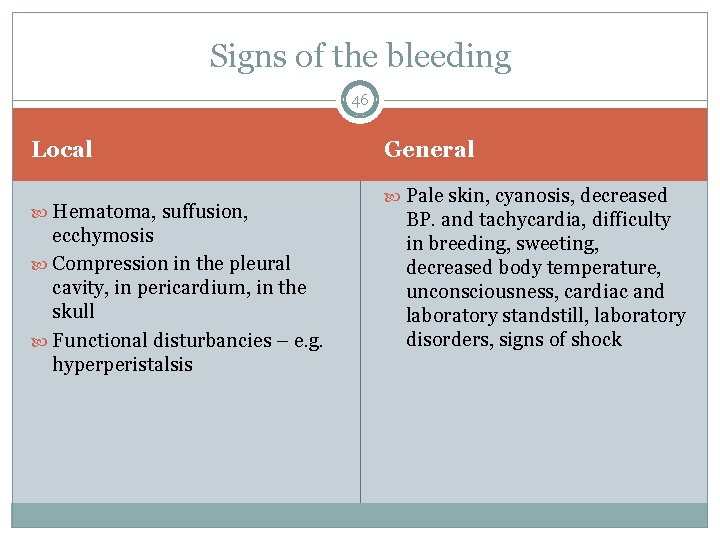
Signs of the bleeding 46 Local Hematoma, suffusion, ecchymosis Compression in the pleural cavity, in pericardium, in the skull Functional disturbancies – e. g. hyperperistalsis General Pale skin, cyanosis, decreased BP. and tachycardia, difficulty in breeding, sweeting, decreased body temperature, unconsciousness, cardiac and laboratory standstill, laboratory disorders, signs of shock
Surgical hemostasis 47 Aim – to prevent the flow of blood from the incised or transected vessels Mechanical methods Thermal methods Chemical and biological methods
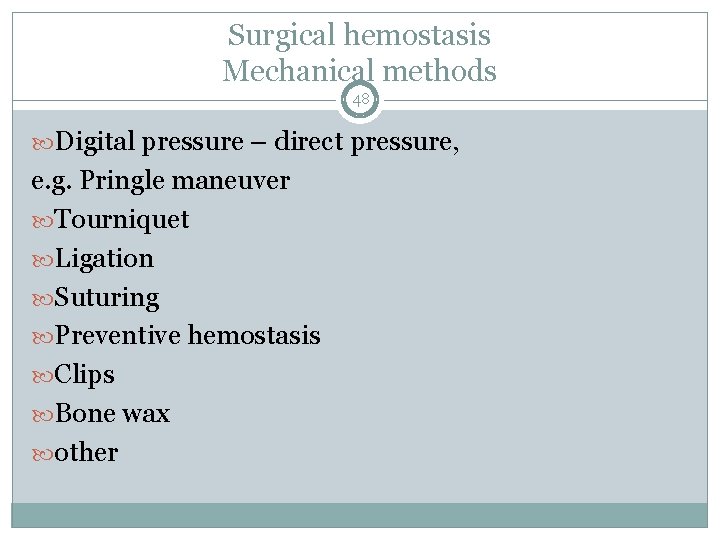
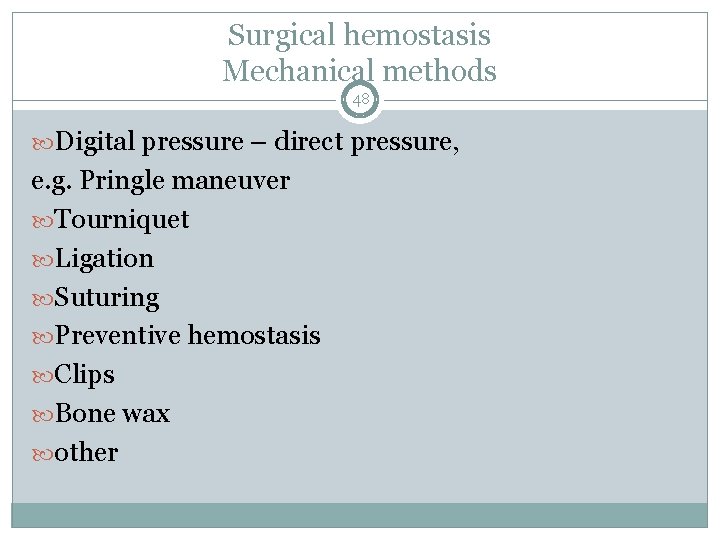
Surgical hemostasis Mechanical methods 48 Digital pressure – direct pressure, e. g. Pringle maneuver Tourniquet Ligation Suturing Preventive hemostasis Clips Bone wax other
Thermal methods 49 Low temperature Hypothermia – eg. stomach bleeding Cryosurgery dehidratation and denaturation of fatty tissue decreases the cell metabolism vasoconstriction
Thermal methods 50 High temperature Electrosurgery – electrocauterization Monopolar diathermy Bipolar diathermy Laser surgery coagulation and vaporization for fine tissues
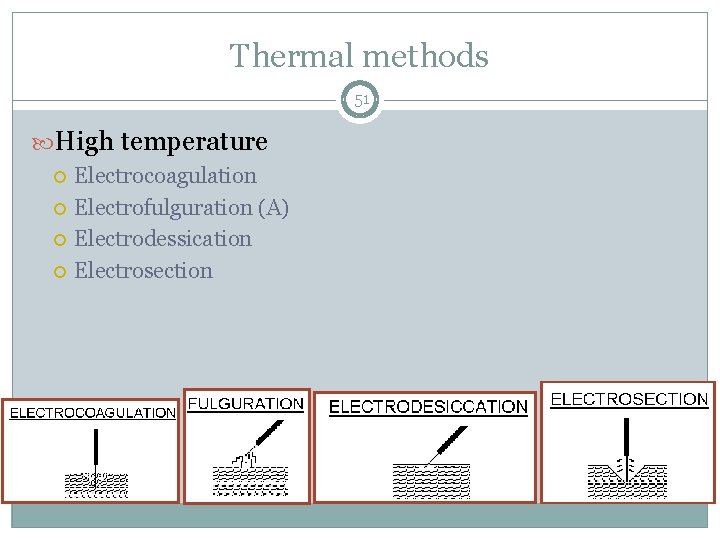
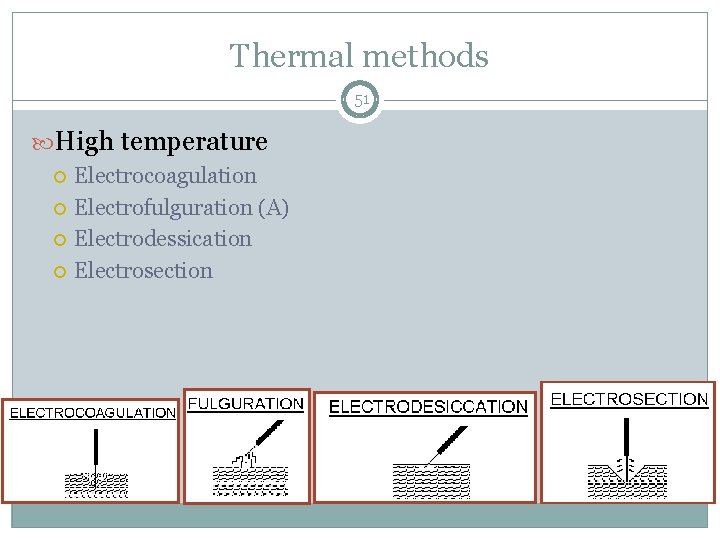
Thermal methods 51 High temperature Electrocoagulation Electrofulguration (A) Electrodessication Electrosection
Hemostasis with chemical and biological methods 52 vasoconstriction coagulation hygroscopic effect Absorbable collagen Absorbable gelatin Microfibrillar collagen Oxidized celluloze Oxytocin Epinephrine Thrombin Hemcon Quik. Clot
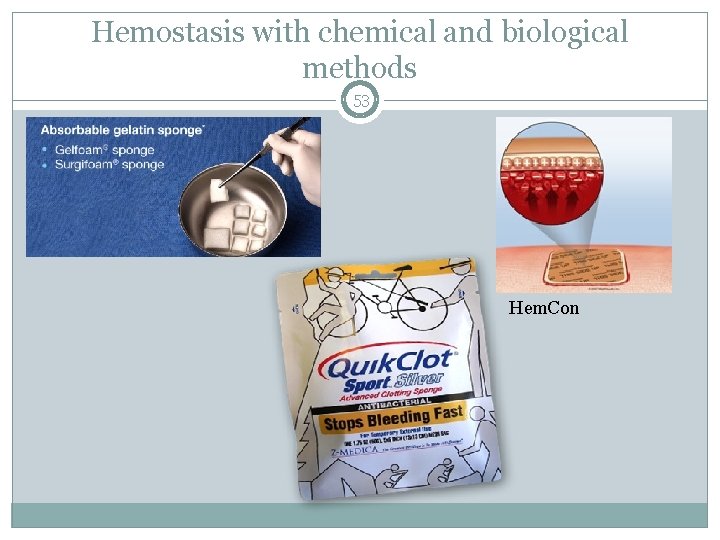
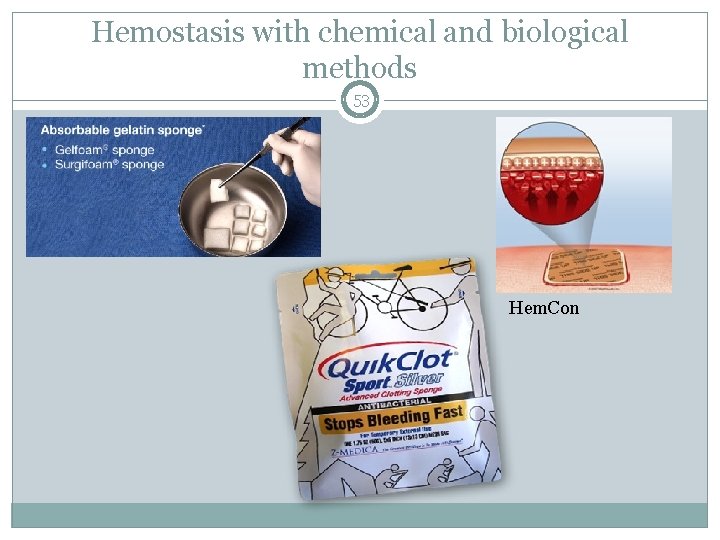
Hemostasis with chemical and biological methods 53 Hem. Con
 Types of wound classification
Types of wound classification Wound classification surgery
Wound classification surgery Utsa wound classification
Utsa wound classification Texas wound classification system
Texas wound classification system Utsa wound classification
Utsa wound classification Classification of tabulation
Classification of tabulation Systemic factors that influence wound healing
Systemic factors that influence wound healing Serosanguineous vs serous
Serosanguineous vs serous Chapter 48 skin integrity and wound care
Chapter 48 skin integrity and wound care Tidy and untidy wound
Tidy and untidy wound A wind up toy is fully wound and at rest
A wind up toy is fully wound and at rest Copyright
Copyright Wedge shaped wound
Wedge shaped wound Wolters kluwer
Wolters kluwer Top management and middle management
Top management and middle management Management pyramid
Management pyramid Basic concepts of management
Basic concepts of management Lazy vs eager
Lazy vs eager Traditional classification vs modern classification
Traditional classification vs modern classification Type of wound
Type of wound Wound tracking software
Wound tracking software Wound infection continuum
Wound infection continuum Incised wound
Incised wound Ryb color code wound care
Ryb color code wound care An inclined plane wound around a post
An inclined plane wound around a post Chapter 20 hunger games questions
Chapter 20 hunger games questions Doylestown wound care center
Doylestown wound care center Jacob's ladder wound closure
Jacob's ladder wound closure Watch simple machine
Watch simple machine Inclined plane wrapped around a post
Inclined plane wrapped around a post Shasta regional wound center
Shasta regional wound center Wound bed preparation adalah
Wound bed preparation adalah Ws of post op fever
Ws of post op fever Swallow tail in laceration
Swallow tail in laceration It is a type of inclined plane that is wound around a post
It is a type of inclined plane that is wound around a post Billiard ball phenomenon
Billiard ball phenomenon Amulet of wound closure
Amulet of wound closure Wound certificate means
Wound certificate means Clean incised wound heals by
Clean incised wound heals by Jackson's thermal wound theory
Jackson's thermal wound theory Loyal retainers archetype
Loyal retainers archetype Contaminated wound
Contaminated wound Wound dehiscence
Wound dehiscence Obici physical therapy
Obici physical therapy Wound healing nutrition handout
Wound healing nutrition handout Mrsa wound
Mrsa wound Medical terms that sound alike
Medical terms that sound alike Bevelling cut wound
Bevelling cut wound Types of inflammation
Types of inflammation Augusta health wound clinic
Augusta health wound clinic Conclusion of the skin
Conclusion of the skin Tension pneumothorax vs simple pneumothorax
Tension pneumothorax vs simple pneumothorax Iad wound
Iad wound Apci lng process schematic
Apci lng process schematic