Perioperative and Postoperative Nursing NURS 230Spring 2014 History



- Slides: 47
Perioperative and Postoperative Nursing NURS 230/Spring 2014
History of Surgical Nursing • Association of peri. Operative Registered Nurses (AORN) – Established in 1956 – Focus on clinical practice, professional practice, administrative practice, patient outcomes, and quality improvement • Ambulatory surgery – Hospital-based or freestanding – Many laparoscopic surgeries, such as gallbladder removal (cholecystectomy)
Classification of Surgery • Seriousness – Major or minor • Urgency – Elective, urgent, emergency • Purpose – Diagnostic, ablative, palliative, reconstructive/restorative, procurement for transplant, constructive, or cosmetic • Moribound: at the point of death • American Society of Peri. Anesthesia Nurses (ASPAN)
Nursing Process: Preoperative Surgical Phase Assessment Diagnosis Planning Implementation Evaluation
Assessment/Pre-op phase • Nursing history • Medical history – Past illnesses, surgeries, and reasons for surgery • Risk factors – Age, nutrition, obesity, sleep apnea, immunocompetence, fluid and electrolyte imbalance, and pregnancy
Risk Factors Age Nutrition Obesity Sleep apnea Immunocompetence Fluid and electrolyte imbalance Pregnancy
Assessment (cont’d) • Perceptions and knowledge • Medication history – Prescription – Over the counter – Herbs – Street drugs • Allergies – Drugs, latex, food, and contact
Assessment/Pre-op phase • Smoking – Cigarettes or packs per day • Alcohol ingestion and substance use/abuse – Use per day or week • Support sources – Family, friends, home environment
Assessment/ Pre-op Phase • • • Occupation Preoperative pain assessment Emotional health Self-concept Body image Culture
Physical Examination • • General survey Head and neck Integument Thorax and lungs Heart and vascular system Abdomen Neurological Diagnostic screenings
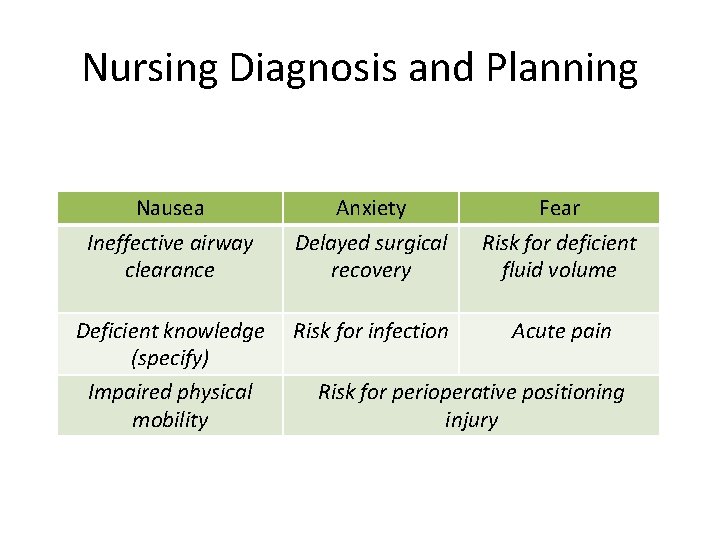
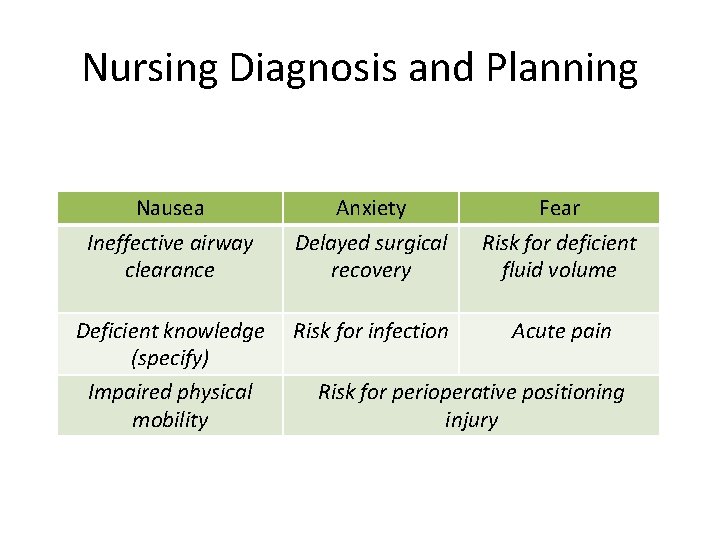
Nursing Diagnosis and Planning Nausea Ineffective airway clearance Anxiety Delayed surgical recovery Fear Risk for deficient fluid volume Deficient knowledge (specify) Impaired physical mobility Risk for infection Acute pain Risk for perioperative positioning injury
Implementation • Informed consent: legal issue • Preoperative teaching: – Reasons for preoperative Instructions and exercises; time of surgery – Postoperative unit and location of family during surgery and recovery; anticipated postoperative monitoring and therapies – Surgical procedures and postoperative treatment; postoperative activity resumption – Patient verbalizes pain relief measures. – Patient expresses feelings regarding surgery.
Acute Care • Physical preparation – Maintaining normal fluid and electrolyte balance – Reducing risk of surgical site infection – Preventing bladder and bowel incontinence – Promoting rest and comfort
Acute Care (cont’d) • Preparation on day of surgery – Hygiene – Hair and cosmetics – Removal of prostheses – Safeguarding valuables – Preparing the bowel and bladder – Vital signs – Documentation – Other procedures – Administering preoperative medications – Eliminating wrong site and wrong procedure surgery
Eliminating wrong site and wrong procedure surgery The three principles of The Joint Commission (TJC) protocol to avoid wrong site and wrong procedure surgery include the following: (1)Preoperative verification that ensures that all relevant documents (e. g. , consent forms, allergies, medical history, physical assessment findings) and results of laboratory tests and diagnostic studies are available before the start of the procedure, and that the type of surgery scheduled is consistent with the patient’s expectations (2) Marking of the operative site with indelible ink to mark left and right distinction, multiple structures (e. g. , fingers), and levels of the spine (3) “Time out” just before the start of the procedure for final verification of correct patient, procedure, and site, and any implants – make sure you watch the you tube videos at the end of this ppt
Preoperative Evaluation • Evaluate whether the patient’s expectations were met with respect to surgical preparation. • During evaluation, include a discussion of any misunderstandings, so patient concerns can be clarified. • When patients have expectations about pain control, this is a good time to reinforce how pain will be managed after surgery.
Day of Surgery • • • Physical preparation Hygiene Vital signs Documentation Preoperative meds Surgical time out

Intraoperative Surgical Phase • Transport to the operating room • Preoperative (holding) area – IV placement – Anesthesia assessment • Admission to the operating room • Nursing process – Assessment – Nursing diagnosis – Planning
Intraoperative Implementation • Physical preparation – Monitoring – Graded compression stockings Latex sensitivity/allergy Introduction of anesthesia Positioning the patient for surgery Documentation of intraoperative care
Introduction of Anesthesia • General – Loss of all sensation and consciousness – Induction, maintenance, and emergence • Regional – Loss of sensation in one area of the body • Local – Loss of sensation at a site • Conscious sedation/moderate sedation – Used for procedures that do not require complete anesthesia
Intraoperative Evaluation • The circulating nurse conducts an ongoing evaluation to ensure that interventions such as patient position are implemented correctly during the intraoperative phase of surgery. – Circulating nurse – Scrub nurse • Evaluate the patient’s ongoing clinical status. Continuously monitor vital signs and intake and output.
Quick Quiz! 1. When conducting preoperative patient and family teaching, you demonstrate proper use of the incentive spirometer. You know that the patient understands the need for this intervention when the patient states, “I use this device to A. Help my cough reflex. ” B. Expand my lungs after surgery. ” C. Increase my lung capacity. ” D. Drain excess fluid from my lungs. ”
Postoperative Surgical Phase • Immediate postoperative recovery (phase 1) – Arrival – Hand-off: OR to PACU – Systems assessment – Discharge and hand-off: PACU to Acute Care
Postoperative Surgical Phase • Recovery in ambulatory surgery (phase 2) – Postanesthesia recovery score for ambulatory patients (PARSAP) – Observation – Discharge • Postoperative convalescence
Postoperative Convalescence: Assessment • Airway and respiration • Circulation • Temperature control – Malignant hyperthermia (covered at the end of this PPT) • Fluid and electrolyte balance • Neurological functions
Postoperative Assessment • • Skin integrity and condition of the wound Metabolism Genitourinary function Gastrointestinal function – Paralytic ileus • Comfort
Postoperative Implementation • Maintaining respiratory function – Start pulmonary intervention early. • Preventing circulatory complications – Foster circulation. • Achieving rest and comfort – Administer pain medications.
Postoperative Nursing Diagnosis and Planning • Determine status of preoperative diagnosis. • Revise or resolve preoperative diagnosis; identify relevant new diagnoses. • Goals and outcomes: – Patient’s incision remains closed and intact. – Patient’s incision remains free of infectious drainage. – Patient remains afebrile. • Setting priorities • Teamwork and collaboration
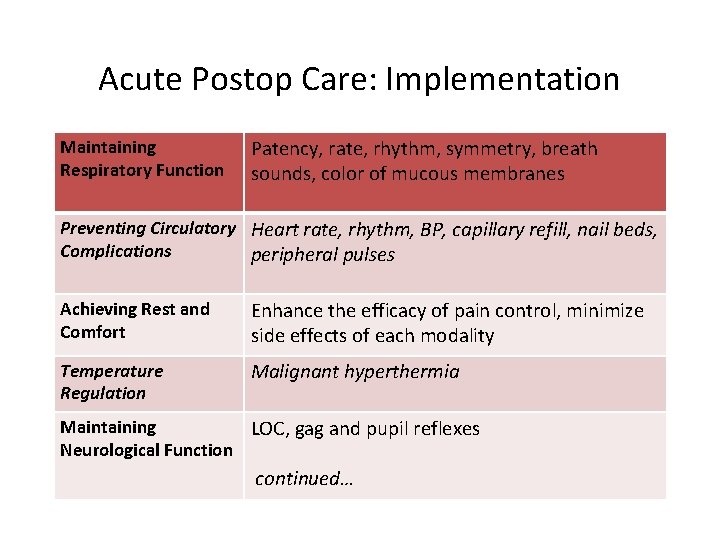
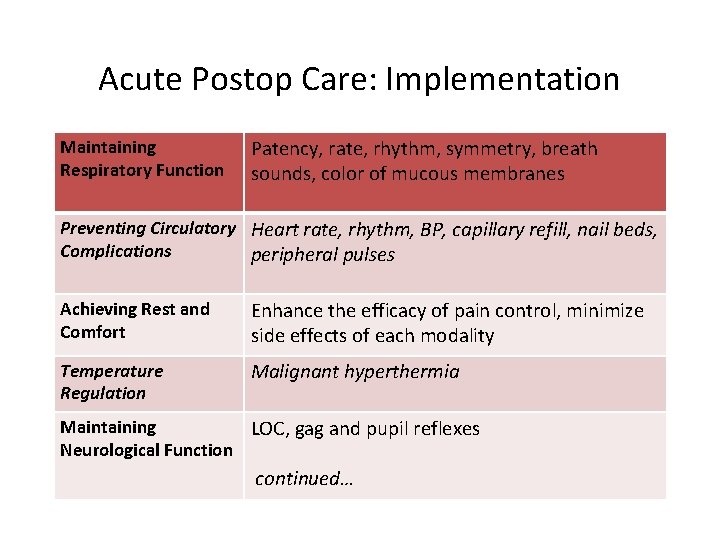
Acute Postop Care: Implementation Maintaining Respiratory Function Patency, rate, rhythm, symmetry, breath sounds, color of mucous membranes Preventing Circulatory Heart rate, rhythm, BP, capillary refill, nail beds, Complications peripheral pulses Achieving Rest and Comfort Enhance the efficacy of pain control, minimize side effects of each modality Temperature Regulation Malignant hyperthermia Maintaining LOC, gag and pupil reflexes Neurological Function continued…
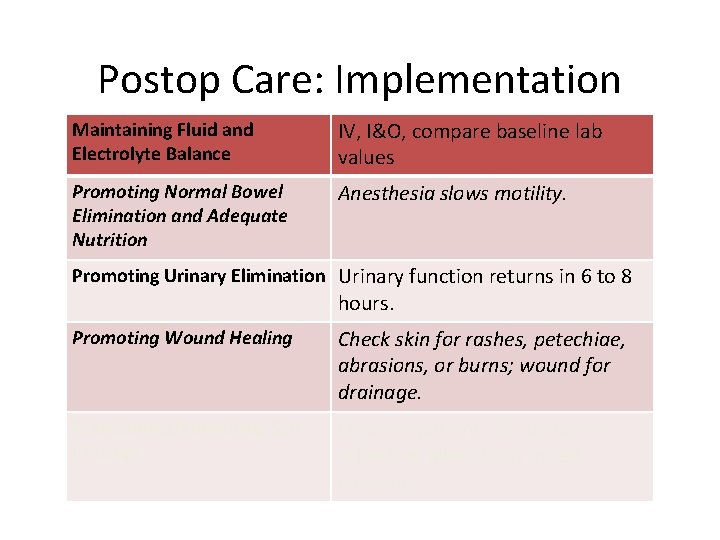
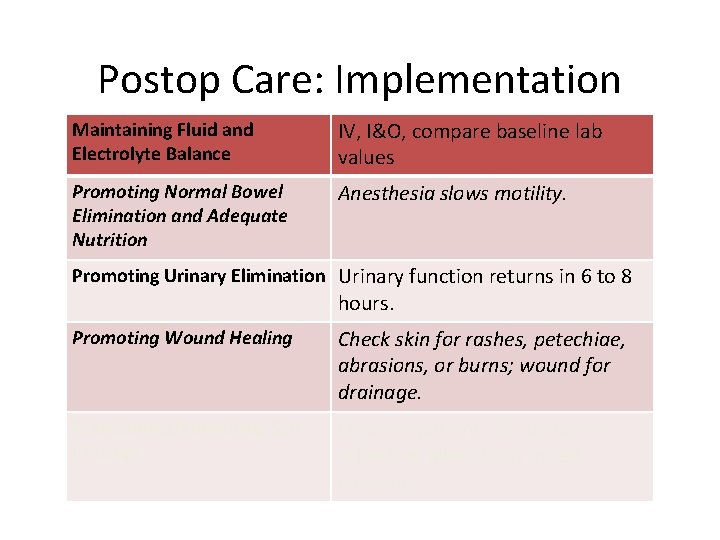
Postop Care: Implementation Maintaining Fluid and Electrolyte Balance IV, I&O, compare baseline lab values Promoting Normal Bowel Elimination and Adequate Nutrition Anesthesia slows motility. Promoting Urinary Elimination Urinary function returns in 6 to 8 hours. Promoting Wound Healing Check skin for rashes, petechiae, abrasions, or burns; wound for drainage. Maintaining/Enhancing Self. Concept Observe patients for behaviors reflecting alterations in selfconcept.
Quick Quiz! 2. Postoperatively, the nurse instructs the patient to perform leg exercises every hour to A. Maintain muscle tone. B. Assess range of motion. C. Exercise fatigued muscles. D. Increase venous return.
Implementation: Restorative and Continuing Care • Preparation for discharge – Continue wound care. – Follow diet or activity restrictions. – Continue medication therapy. – Watch for complications. • Some patients need home care after discharge; others require discharge to a skilled nursing facility.
Evaluation • Examples of evaluation questions: – “Are you satisfied with the way we are managing your pain? ” – “Do you feel you have learned enough to be able to follow your diet at home? ” – “Are you having any ongoing issues, questions, or concerns that we can address for you at this time? ” • Evaluate whether the patient and the family have learned self-care measures.
Final Checklist…. KNOW THIS! • http: //www. youtube. com/watch? v=IAvwx. KJVI DE
Final Time-Out • http: //www. youtube. com/watch? v=RJzd. BF 7 I 6 w&feature=related
Postoperative Pulmonary Complications • 5 - 10% all surgical patients • 9 - 40% after abdominal surgery • Wong et al. Factors associated with postoper. pulmonary complications in patients with severe COPD. Anesthesia Analgesia 1995; 80: 276 -284.
The most important and morbid postoperative pulmonary complications 1. Atelectasis 2. Pneumonia 3. Respiratory failure 4. Exacerbation of underlying chronic lung disease

Breathing and Coughing Exercises • The sitting position gives the best lung expansion for coughing and deep breathing exercises • Inhale through the nose and exhale through the mouth with pursed lips • Hold breath for three seconds and cough • Cough and deep breathe q 2 h while awake
DVT/VTE Risk Factors: • • • Age 40 -60 years Age > 60 (count as 2 factors) History of DVT or PE (count as 5 factors) Malignancy Obesity (>120 % of BW) Previous or present immobilization (>72 hrs) Anticipated immobilization/bed confinement >72 hrs Major Surgery Paralysis Trauma Indwelling central venous catheter • • • Severe COPD Pregnancy, or post partum < 1 month (tendency to bleed) Inflammatory bowel disease Severe sepsis Hypercoagulable state (clot to easily) Nephrotic Syndrome (kidney failure) Current or previous estrogen use w/in last 5 days Leg ulcers, edema, or stasis (varicose veins) History of MI History of CHF (congestive heart failure) History of Stroke

6 W’s of Post-Operative Fever • Wind: the pulmonary system is the primary source of fever in the first 48 hours. • Wound: there might be an infection at the surgical site. • Water: check intravenous access site for signs of phlebitis. • Walk: deep venous thrombosis can develop due to pelvic pooling or restricted mobility related to pain and fatigue. • Whiz: a urinary tract infection is possible if urinary catheterization was required. • Wonder drugs: drug fevers (anesthesia, heparin, antibiotics, anticonvulsants).
BIG, Bad , Ugly
Malignant Hyperthermia • Rare genetic disorder manifests after treatment of with anesthetic agents: succinylcholine and halothane • Onset is usually in 1 hour of the administration of anesthesia, rarely delayed up to 10 hours • ½ of cases are inherited in as Autosomal Dominant • In the presence of anesthetic agents uncontrolled Ca ++ efflux from the SR tetany, ↑ and heat production
Malignant Hyperthermia • Early clinical findings in malignant hyperthermia include muscle rigidity (especially masseter (jaw) stiffness), tachycardia, increased CO 2 production, and skin cyanosis with mottling (purple and blue) • Marked hyperthermia (up to 45ºC [113ºF]) occurs minutes to hours later; core body temperature tends to rise 1ºC every 5 to 60 minutes. • Hypotension
Management: Malignant hyperthermia • Dantrolene administration is the mainstay of treatment of malignant hyperthermia, and should be initiated as soon as the diagnosis is suspected. • Since the introduction of dantrolene, the mortality of this syndrome has fallen from close to 70 percent to less than 10 percent. • Dantrolene is a nonspecific muscle relaxant that acts by blocking the release of calcium from the SR decreases the myoplasmic concentration of free calcium and diminishes the myocyte hypermetabolism that causes clinical symptoms. • Most effective when given early in the illness (ie, before hyperthermia occurs), when maximal calcium can be retained within the muscle • A 2 mg/kg IV bolus is given and should be repeated every 5 minutes until symptoms abate up to a maximum dose of 10 mg/kg. • This may be repeated every 10 to 15 hours. After an initial response, the drug should be continued orally at a dose of 4 to 8 mg/kg per day, in four divided doses, for three days.
 5 nursing diagnosis of cataract
5 nursing diagnosis of cataract Perioperative nurse definition
Perioperative nurse definition Perioperative phases
Perioperative phases Perioperative case study nursing
Perioperative case study nursing What is a good pico question
What is a good pico question Nurs 425
Nurs 425 Nurs 425
Nurs 425 Intraoperative care definition
Intraoperative care definition Rumus postoperative death rate
Rumus postoperative death rate Postoperative shock
Postoperative shock Ccs perioperative guidelines
Ccs perioperative guidelines Staffing and nursing care delivery models
Staffing and nursing care delivery models Nursing diagnosis ocd
Nursing diagnosis ocd Nursing interventions for neonatal abstinence syndrome
Nursing interventions for neonatal abstinence syndrome Nursing process in psychiatric nursing
Nursing process in psychiatric nursing History of nursing in sudan
History of nursing in sudan Cc hpi
Cc hpi West african college of nursing lagos
West african college of nursing lagos First psychiatric nurse in india
First psychiatric nurse in india History of emergency nursing
History of emergency nursing History also history physical
History also history physical Principles of social services and wellbeing act wales
Principles of social services and wellbeing act wales Social services and wellbeing (wales) act 2014 easy read
Social services and wellbeing (wales) act 2014 easy read Veterinary nurse conduct and discipline rules 2014
Veterinary nurse conduct and discipline rules 2014 Cooper and schindler
Cooper and schindler Features of rte
Features of rte Difference between beftn and npsb
Difference between beftn and npsb Teacher twins 2014
Teacher twins 2014 Who traditional medicine strategy 2014–23
Who traditional medicine strategy 2014–23 Teacher twins@2014
Teacher twins@2014 Ddb board regulation #1 s. 2014
Ddb board regulation #1 s. 2014 Ieee 519
Ieee 519 Ccot essay
Ccot essay Pnp delinquency report system
Pnp delinquency report system Hawking
Hawking 2014 special olympics
2014 special olympics Agosto 2014
Agosto 2014 Sfc2014 login
Sfc2014 login Orden 3814/2014
Orden 3814/2014 Trados studio 2014
Trados studio 2014 Riverbed gartner
Riverbed gartner Enade 2014
Enade 2014 Enade 2014
Enade 2014 Determining proportionality with tables
Determining proportionality with tables Acsm 2014
Acsm 2014 Gred spm
Gred spm Siklus pengelolaan aset pada pp 27 tahun 2017
Siklus pengelolaan aset pada pp 27 tahun 2017 Patientlagen 2014:821
Patientlagen 2014:821