Chapter 48 Skin Integrity and Wound Care Scientific





- Slides: 62
Chapter 48 Skin Integrity and Wound Care
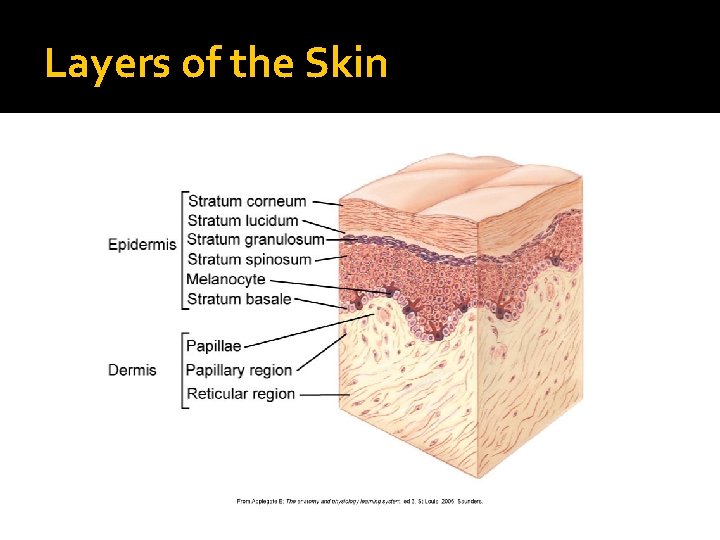
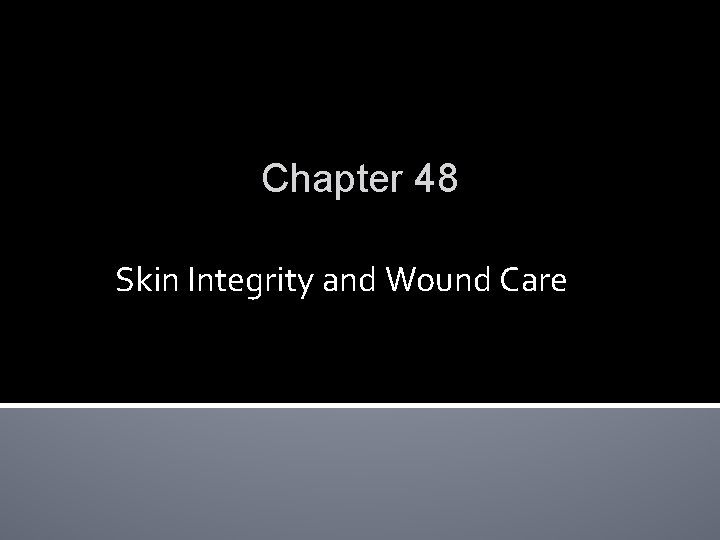
Scientific Knowledge Base: Skin �Dermal-epidermal junction Separates dermis and epidermis �Epidermis Top layer of skin �Dermis Inner layer of skin Collagen
Layers of the Skin
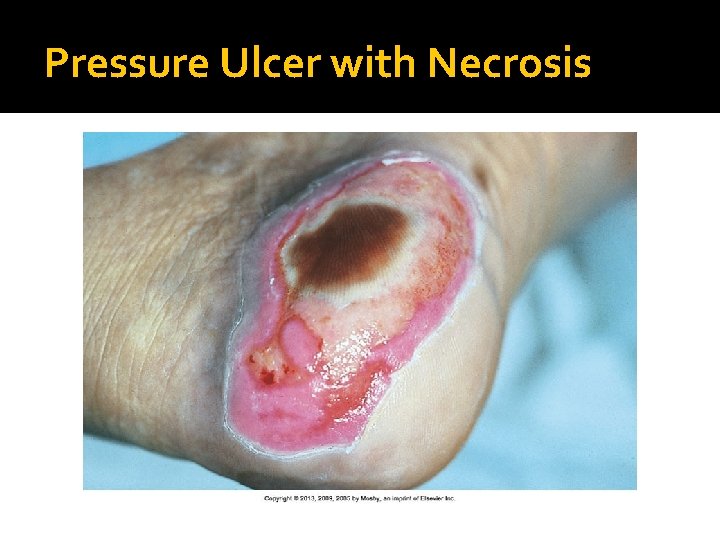
Pressure Ulcers �Pressure ulcer Pressure sore, decubitus ulcer, or bed sore �Pathogenesis Pressure intensity ▪ Tissue ischemia ▪ Blanching Pressure duration Tissue tolerance
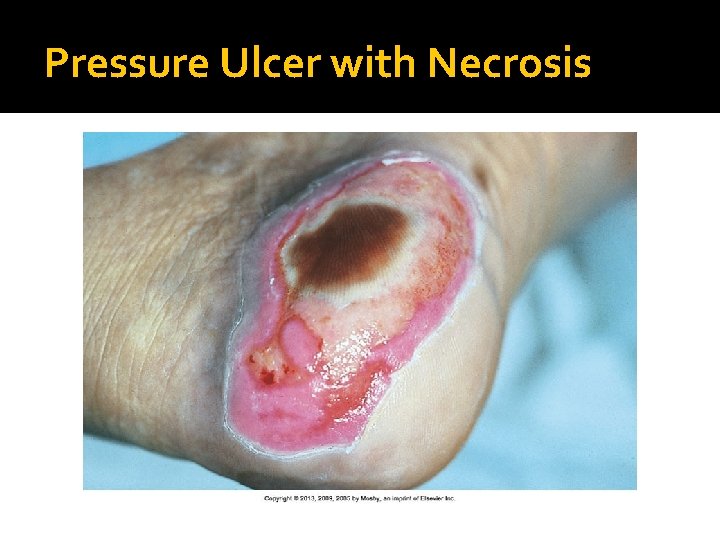
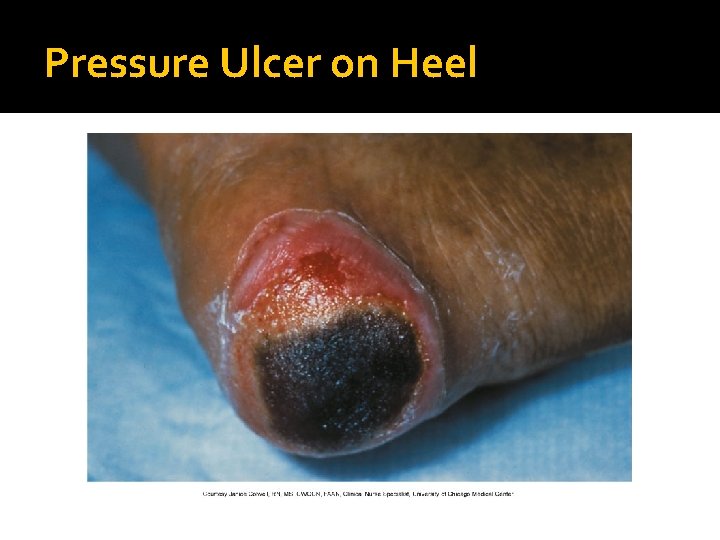
Pressure Ulcer with Necrosis
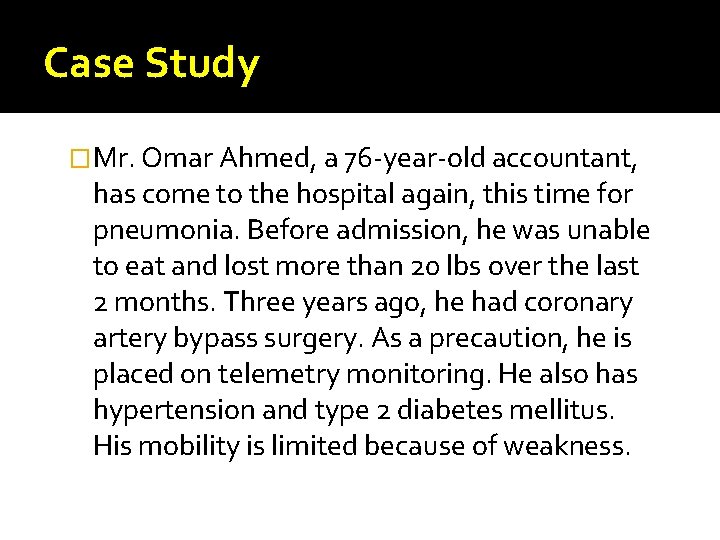
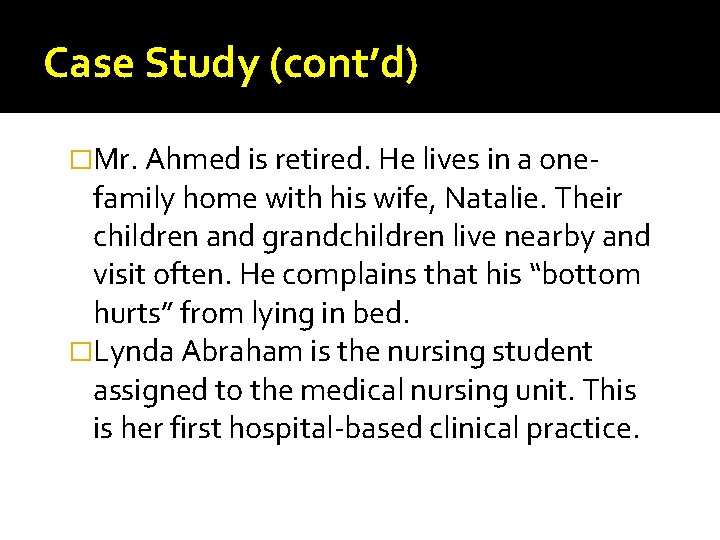
Case Study �Mr. Omar Ahmed, a 76 -year-old accountant, has come to the hospital again, this time for pneumonia. Before admission, he was unable to eat and lost more than 20 lbs over the last 2 months. Three years ago, he had coronary artery bypass surgery. As a precaution, he is placed on telemetry monitoring. He also has hypertension and type 2 diabetes mellitus. His mobility is limited because of weakness.
Case Study (cont’d) �Mr. Ahmed is retired. He lives in a one- family home with his wife, Natalie. Their children and grandchildren live nearby and visit often. He complains that his “bottom hurts” from lying in bed. �Lynda Abraham is the nursing student assigned to the medical nursing unit. This is her first hospital-based clinical practice.
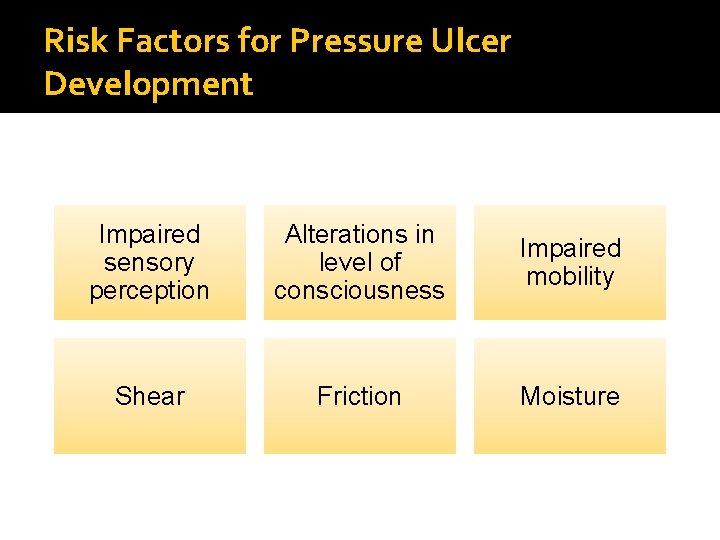
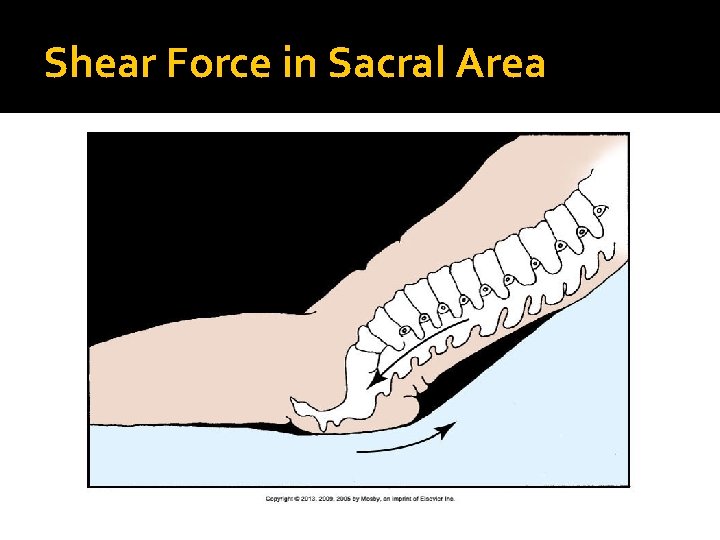
Risk Factors for Pressure Ulcer Development Impaired sensory perception Alterations in level of consciousness Impaired mobility Shear Friction Moisture
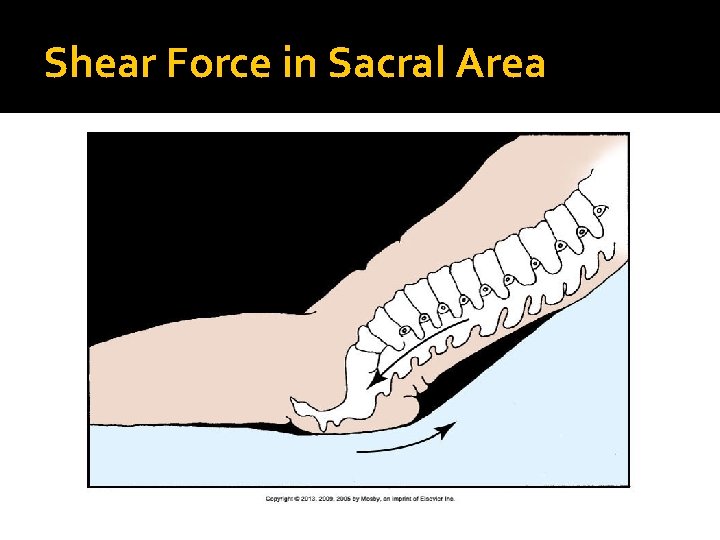
Shear Force in Sacral Area
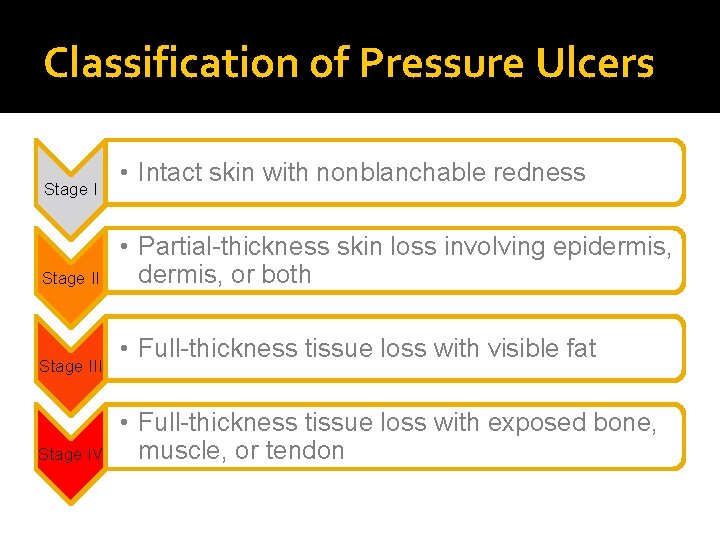
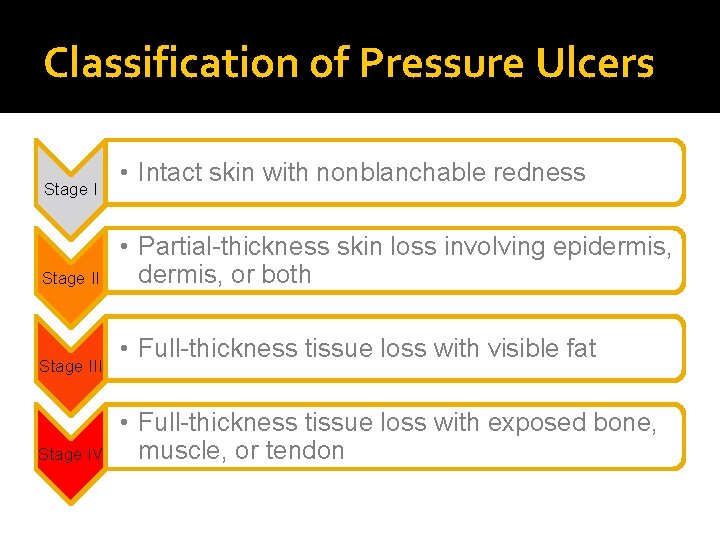
Classification of Pressure Ulcers Stage III Stage IV • Intact skin with nonblanchable redness • Partial-thickness skin loss involving epidermis, or both • Full-thickness tissue loss with visible fat • Full-thickness tissue loss with exposed bone, muscle, or tendon
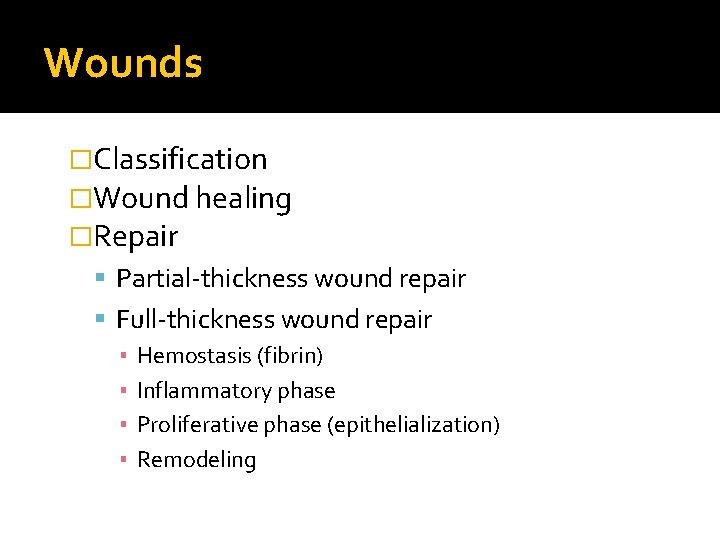
Wounds �Classification �Wound healing �Repair Partial-thickness wound repair Full-thickness wound repair ▪ Hemostasis (fibrin) ▪ Inflammatory phase ▪ Proliferative phase (epithelialization) ▪ Remodeling

Wound Colors
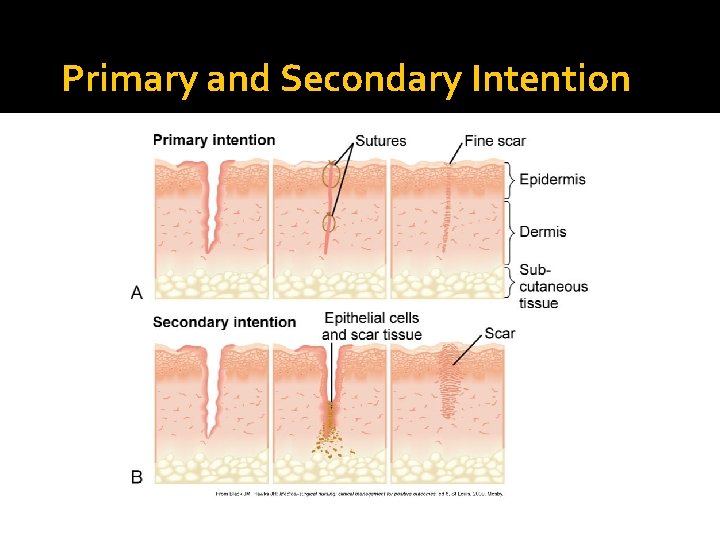
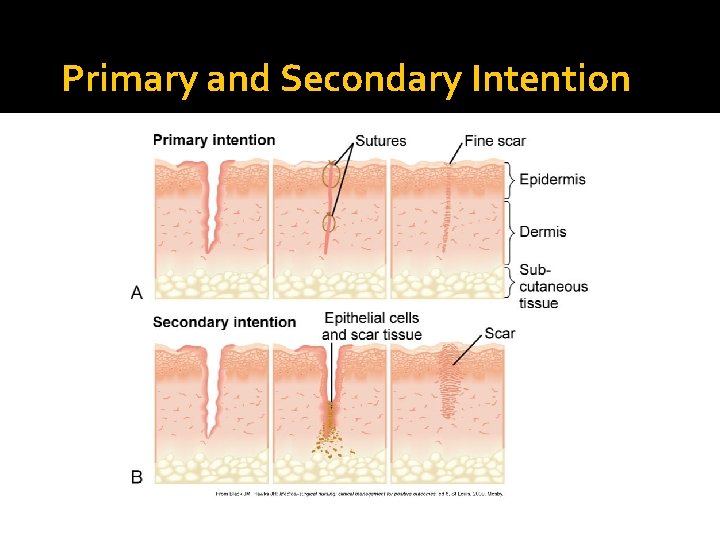
Primary and Secondary Intention
Complications of Wound Healing Hemorrhage Hematoma Infection Dehiscence Evisceration
Nursing Knowledge Base �Prediction and prevention of pressure ulcers Risk assessment ▪ Braden scale Sensory perception, moisture, activity, mobility, nutrition, and friction and shear Prevention ▪ Economic consequences
Factors Influencing Pressure Ulcer Formation and Wound Healing �Nutrition �Tissue perfusion �Infection �Age �Psychosocial impact of wounds
Assessment �Skin �Pressure ulcers Predictive measures Mobility Nutritional status Body fluids Pain
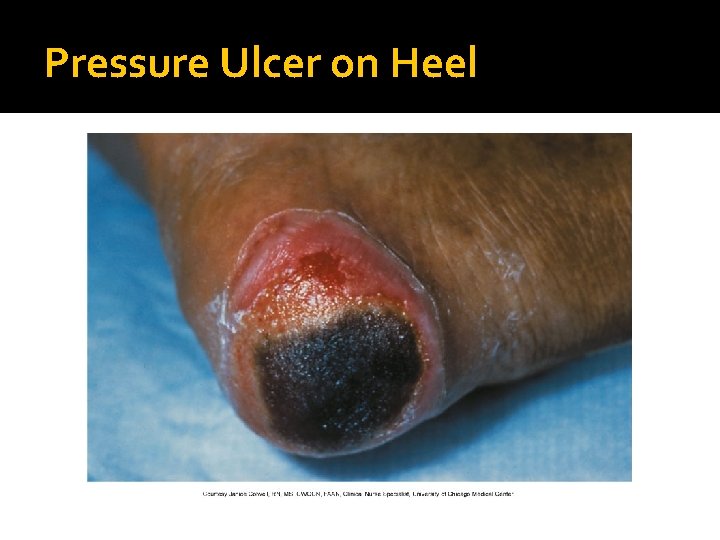
Pressure Ulcer on Heel
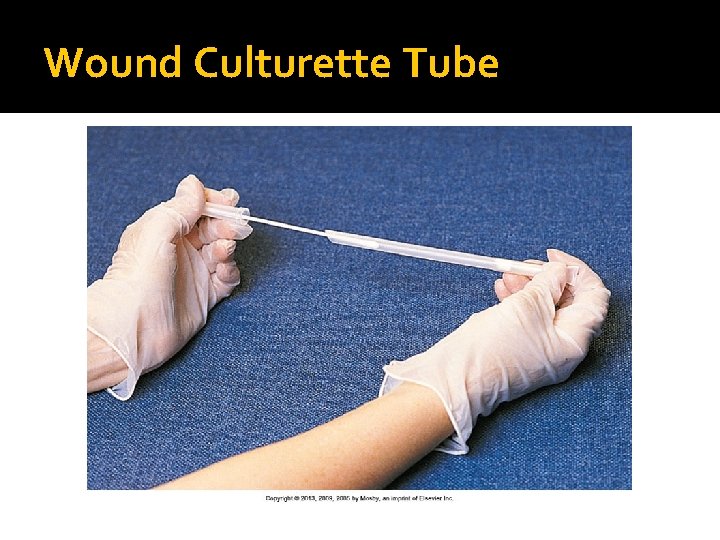
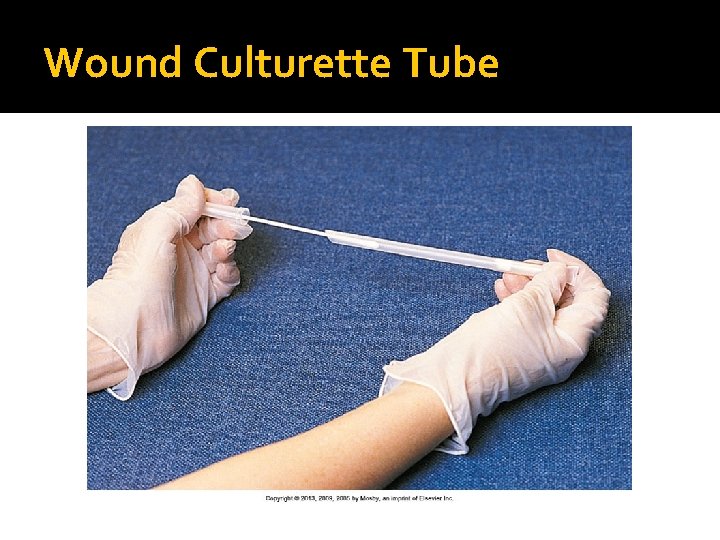
Assessment �Wounds Emergency setting Stable setting Wound appearance Character of wound drainage Drains Wound closures Palpation of wound Wound cultures
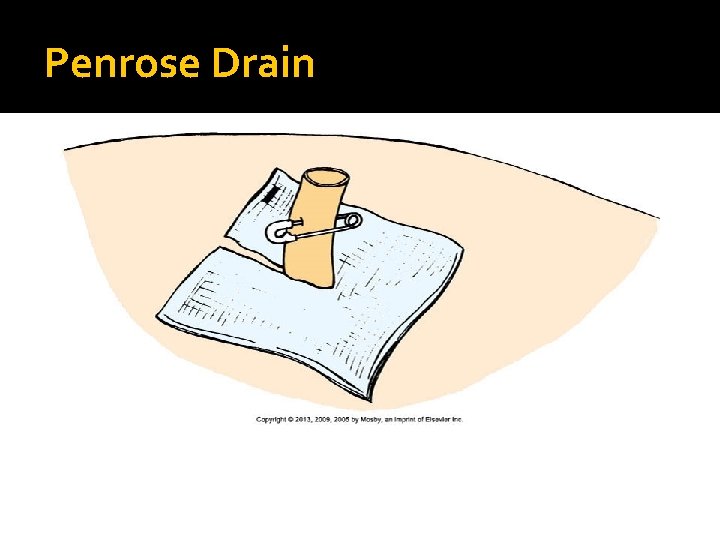
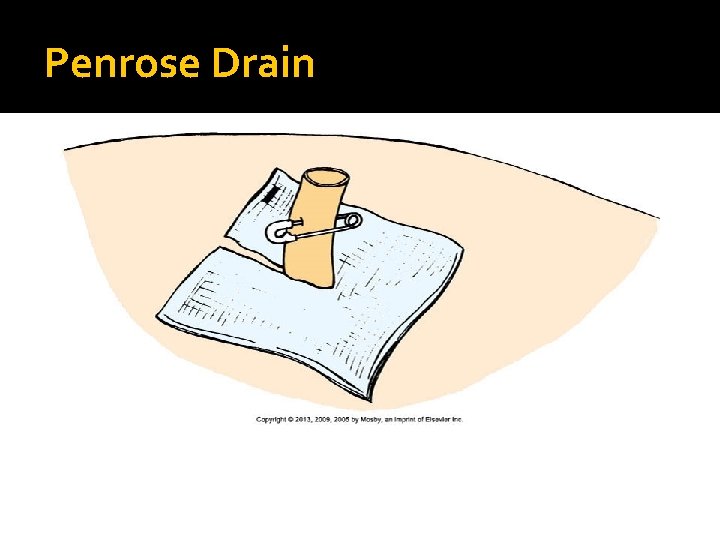
Penrose Drain
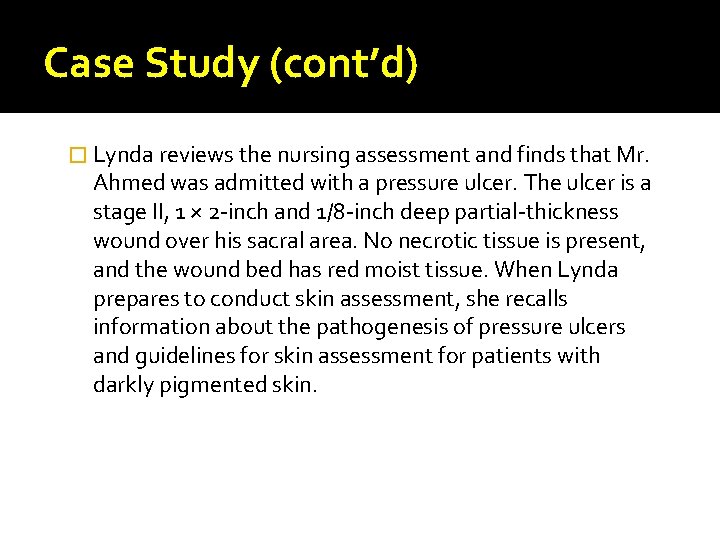
Case Study (cont’d) � Lynda reviews the nursing assessment and finds that Mr. Ahmed was admitted with a pressure ulcer. The ulcer is a stage II, 1 × 2 -inch and 1/8 -inch deep partial-thickness wound over his sacral area. No necrotic tissue is present, and the wound bed has red moist tissue. When Lynda prepares to conduct skin assessment, she recalls information about the pathogenesis of pressure ulcers and guidelines for skin assessment for patients with darkly pigmented skin.
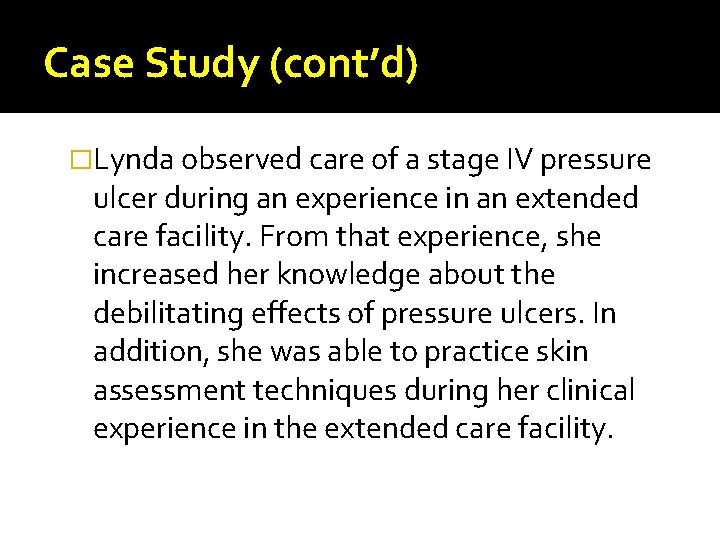
Case Study (cont’d) �Lynda observed care of a stage IV pressure ulcer during an experience in an extended care facility. From that experience, she increased her knowledge about the debilitating effects of pressure ulcers. In addition, she was able to practice skin assessment techniques during her clinical experience in the extended care facility.
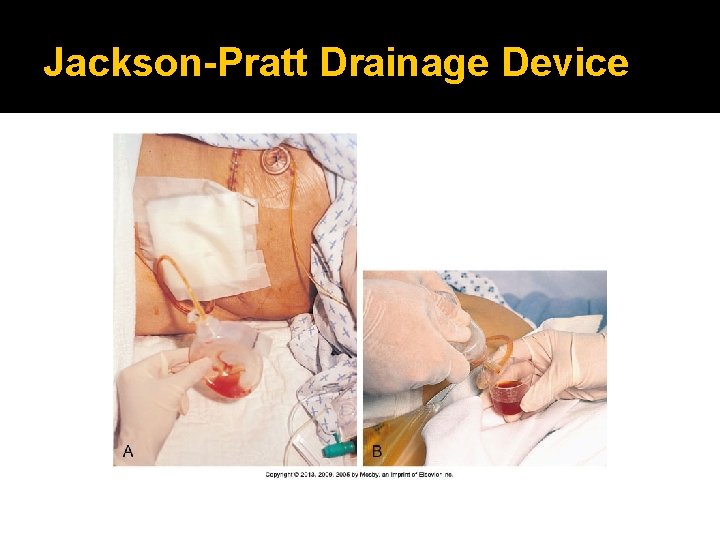
Jackson-Pratt Drainage Device
Wound Culturette Tube
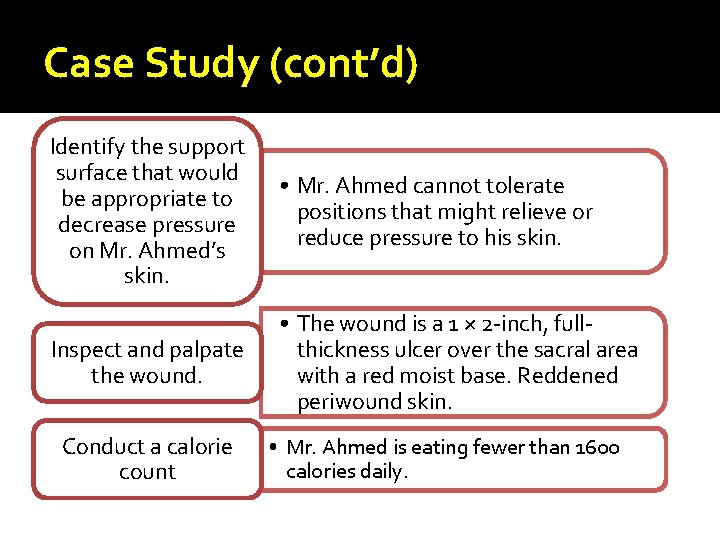
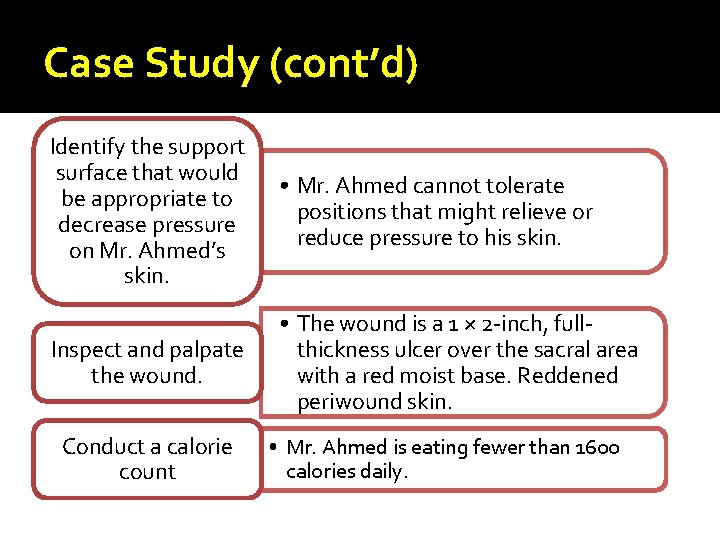
Case Study (cont’d) Identify the support surface that would be appropriate to decrease pressure on Mr. Ahmed’s skin. • Mr. Ahmed cannot tolerate positions that might relieve or reduce pressure to his skin. Inspect and palpate the wound. • The wound is a 1 × 2 -inch, fullthickness ulcer over the sacral area with a red moist base. Reddened periwound skin. Conduct a calorie count • Mr. Ahmed is eating fewer than 1600 calories daily.
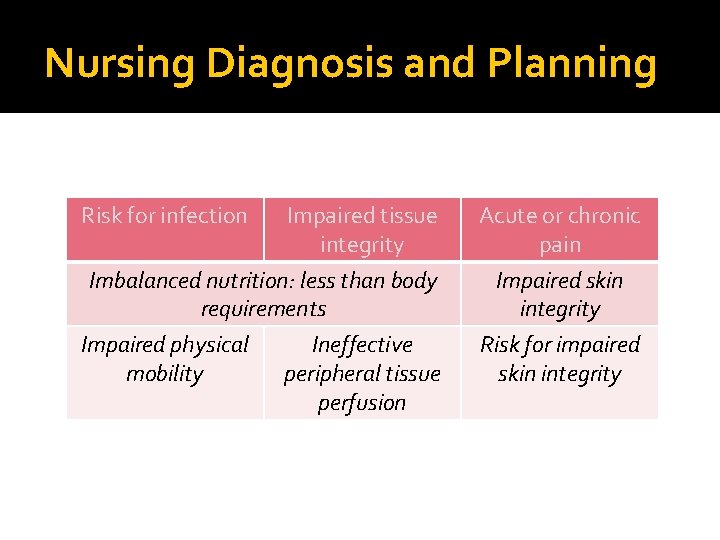
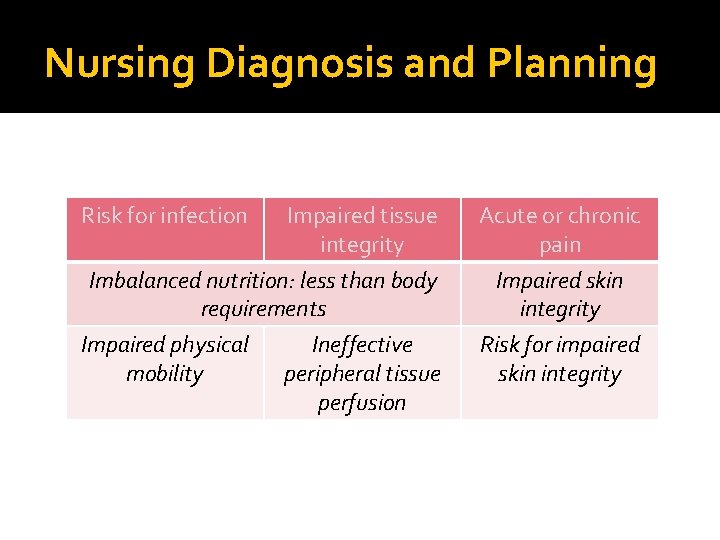
Nursing Diagnosis and Planning Risk for infection Impaired tissue integrity Acute or chronic pain Imbalanced nutrition: less than body requirements Impaired physical Ineffective mobility peripheral tissue perfusion Impaired skin integrity Risk for impaired skin integrity
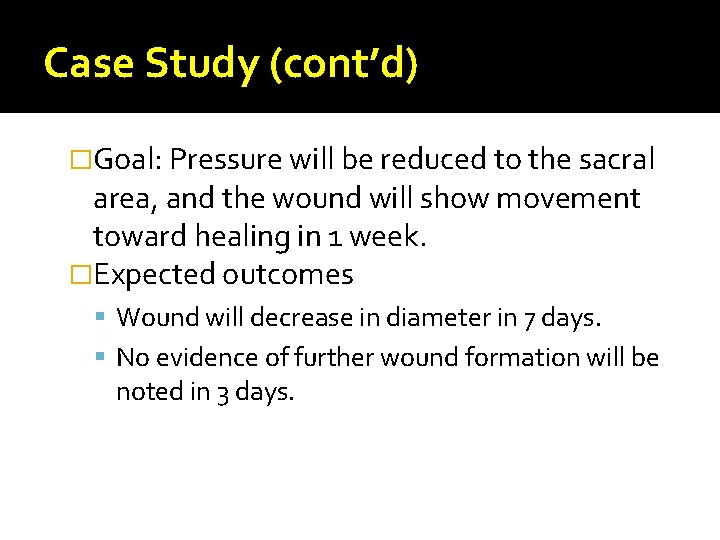
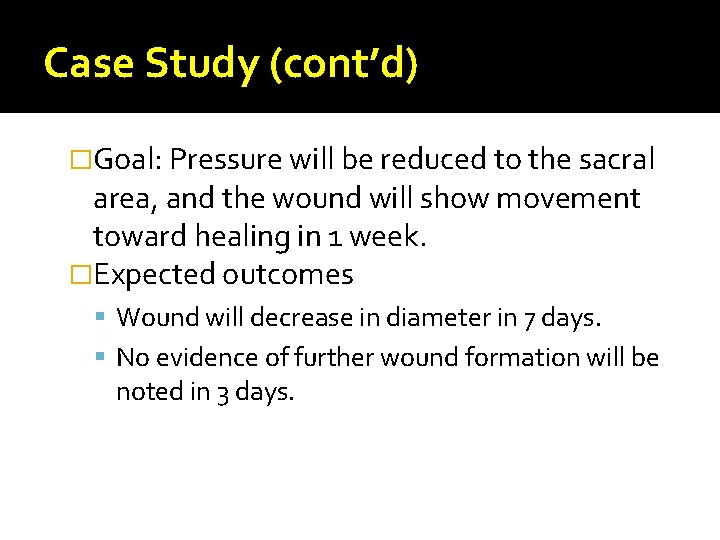
Case Study (cont’d) �Goal: Pressure will be reduced to the sacral area, and the wound will show movement toward healing in 1 week. �Expected outcomes Wound will decrease in diameter in 7 days. No evidence of further wound formation will be noted in 3 days.
Quick Quiz! 1. The nursing assistant asks you the difference between a wound that heals by primary or secondary intention. You will reply that a wound heals by primary intention when the skin edges A. Are approximated. B. Migrate across the incision. C. Appear slightly pink. D. Slightly overlap each other.
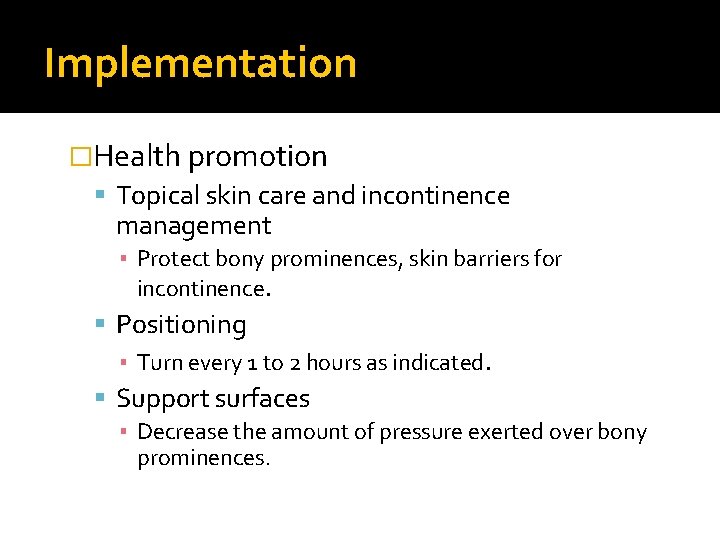
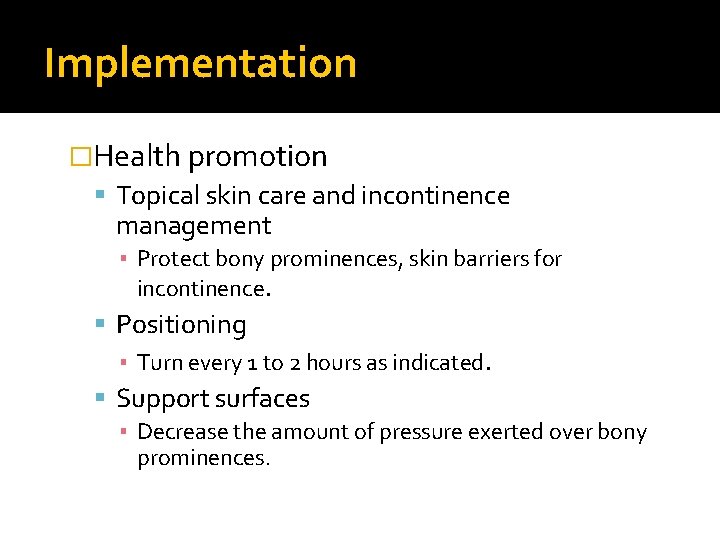
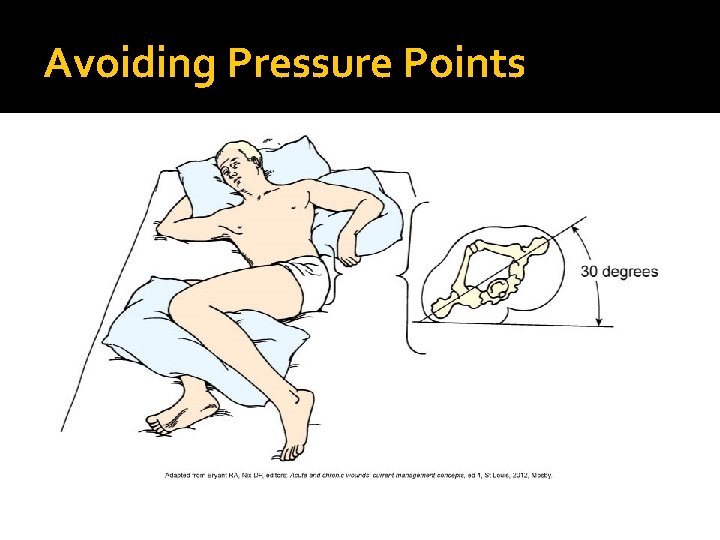
Implementation �Health promotion Topical skin care and incontinence management ▪ Protect bony prominences, skin barriers for incontinence. Positioning ▪ Turn every 1 to 2 hours as indicated. Support surfaces ▪ Decrease the amount of pressure exerted over bony prominences.
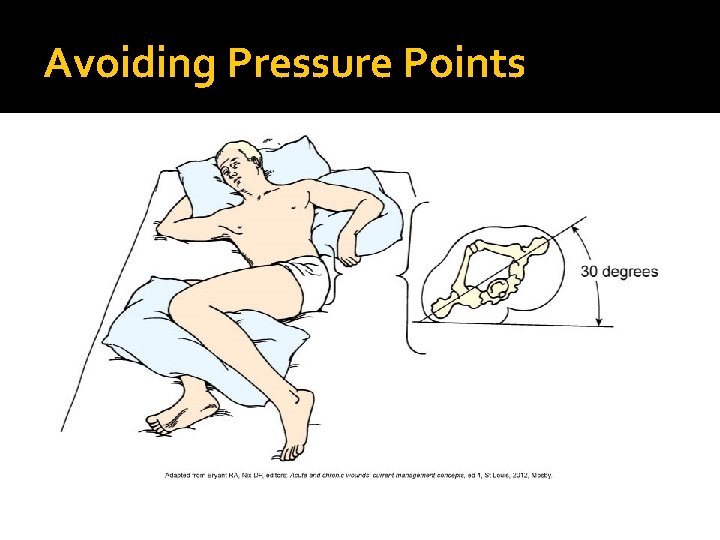
Avoiding Pressure Points
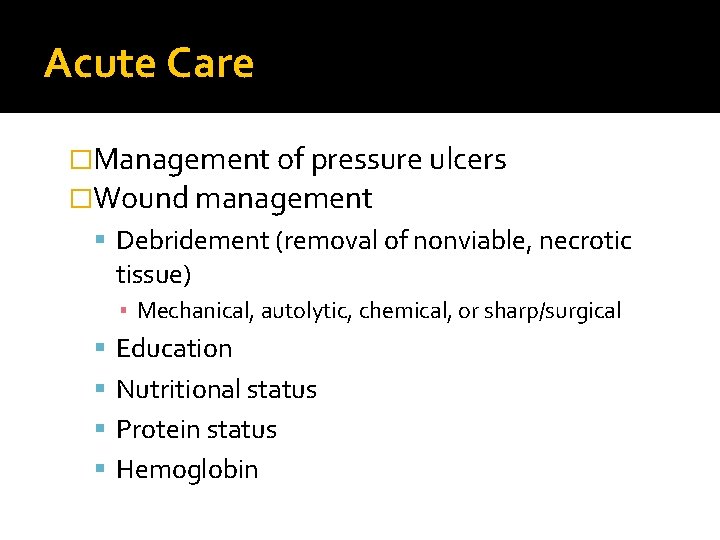
Acute Care �Management of pressure ulcers �Wound management Debridement (removal of nonviable, necrotic tissue) ▪ Mechanical, autolytic, chemical, or sharp/surgical Education Nutritional status Protein status Hemoglobin
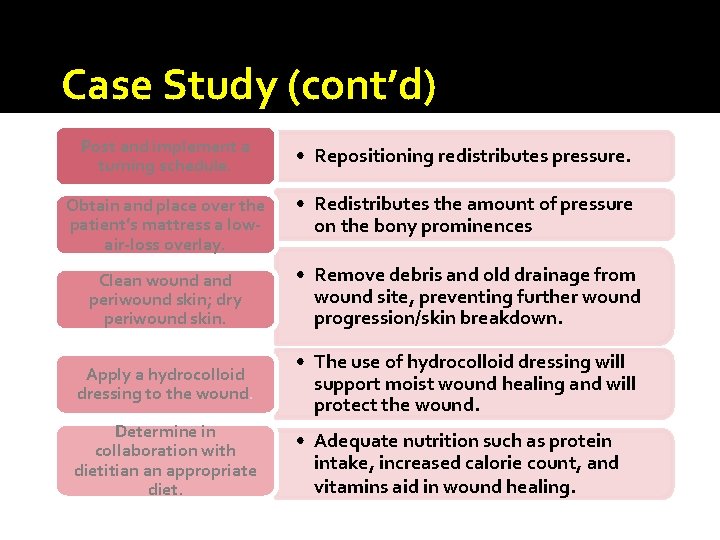
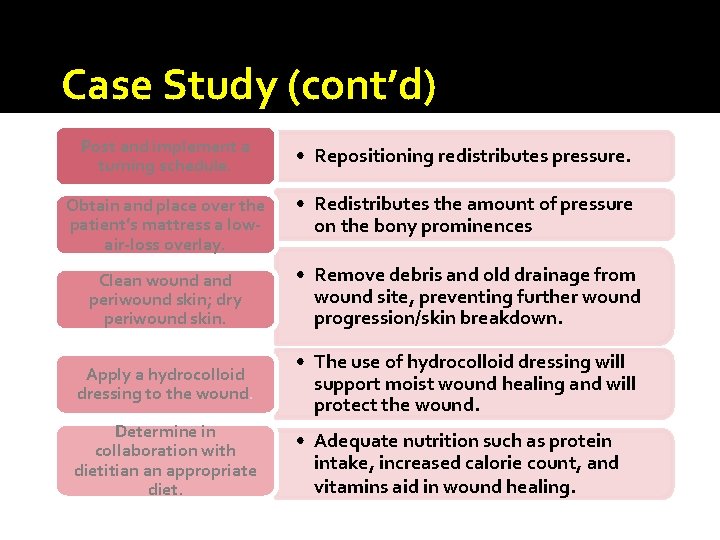
Case Study (cont’d) Post and implement a turning schedule. • Repositioning redistributes pressure. Obtain and place over the patient’s mattress a lowair-loss overlay. • Redistributes the amount of pressure on the bony prominences Clean wound and periwound skin; dry periwound skin. • Remove debris and old drainage from wound site, preventing further wound progression/skin breakdown. Apply a hydrocolloid dressing to the wound. • The use of hydrocolloid dressing will support moist wound healing and will protect the wound. Determine in collaboration with dietitian an appropriate diet. • Adequate nutrition such as protein intake, increased calorie count, and vitamins aid in wound healing.
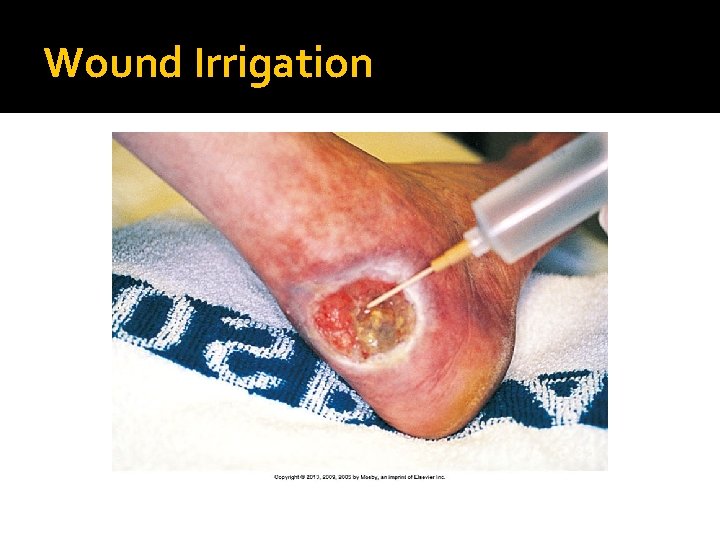
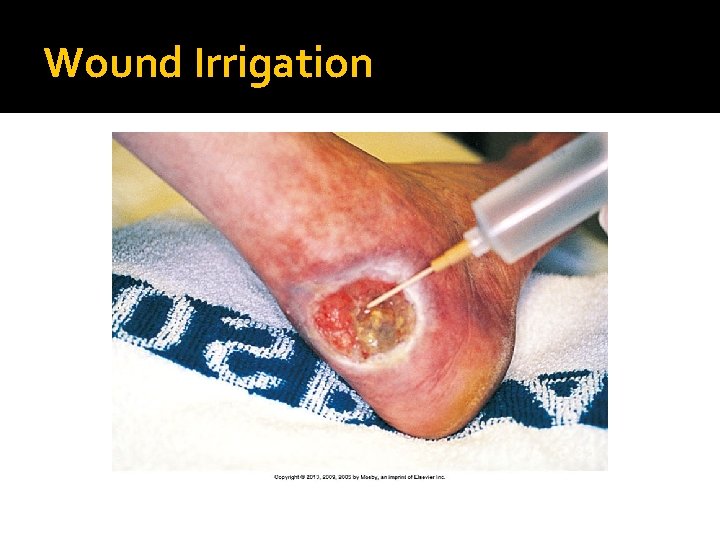
Wound Irrigation
First Aid for Wounds �Hemostasis Control bleeding. ▪ Allow puncture wounds to bleed. ▪ Do not remove a penetrating object. Bandage �Cleaning Gentle Normal saline �Protection
Purposes of Dressings �Protect a wound from microorganism contamination �Aid in hemostasis �Promote healing by absorbing drainage and debriding a wound �Support or splint the wound site �Protect patients from seeing the wound (if perceived as unpleasant) �Promote thermal insulation of the wound surface
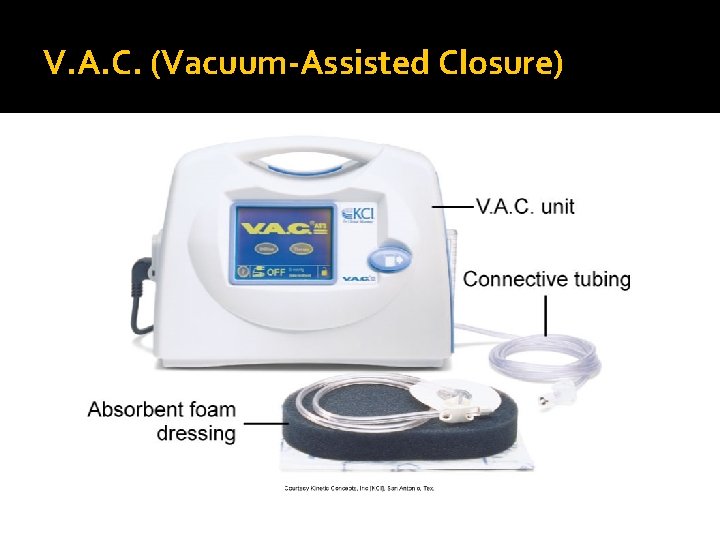
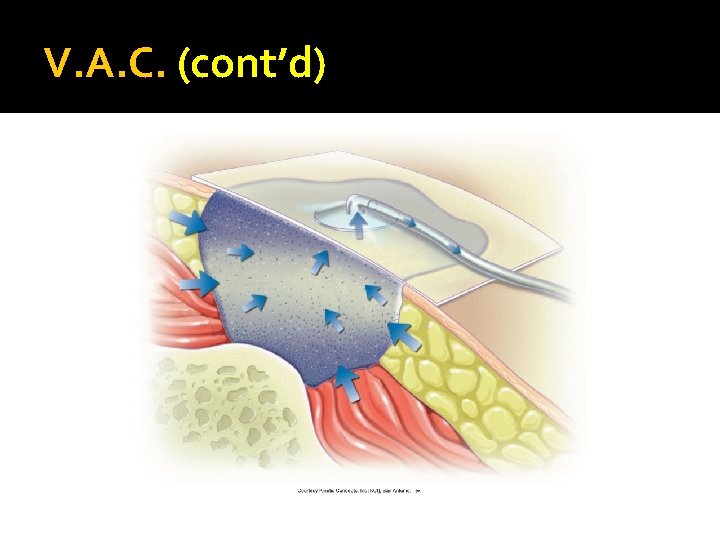
Dressings �Dry or moist Gauze �Film dressing �Hydrocolloid—protects the wound from surface contamination �Hydrogel—maintains a moist surface to support healing �Wound vacuum assisted closure (V. A. C. )— uses negative pressure to support healing

Transparent film dressing
Dressings (cont’d) �Changing Know type of dressing, placement of drains, and equipment needed. �Prepare the patient for a dressing change Evaluate pain. Describe procedure steps. Gather supplies. Recognize normal signs of healing. Answer questions about the procedure or wound.
During a Dressing Change �Assess the skin beneath the tape. �Perform thorough hand hygiene before and after wound care. �Wear sterile gloves before directly touching an open or fresh wound. �Remove or change dressings over closed wounds when they become wet or if the patient has signs or symptoms of infection, and as ordered.
Dressings �Packing a wound Assess size, depth, and shape �Securing Tape, ties, or binders �Comfort measures Carefully remove tape. Gently clean the wound. Administer analgesics before dressing change.
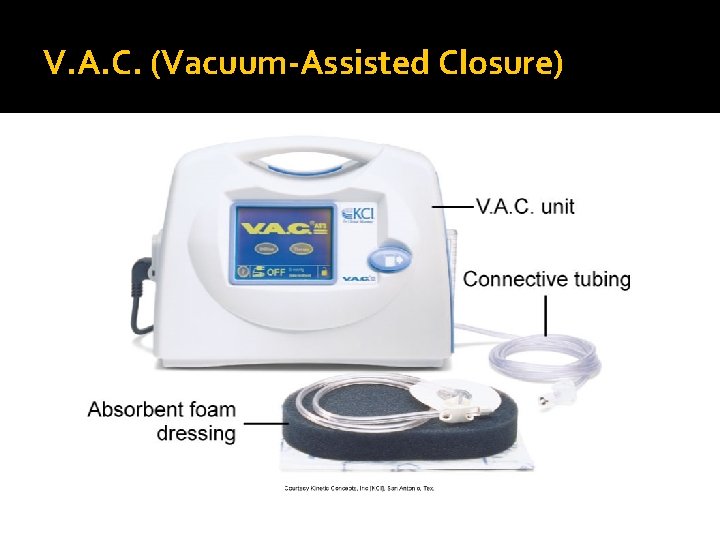
V. A. C. (Vacuum-Assisted Closure)
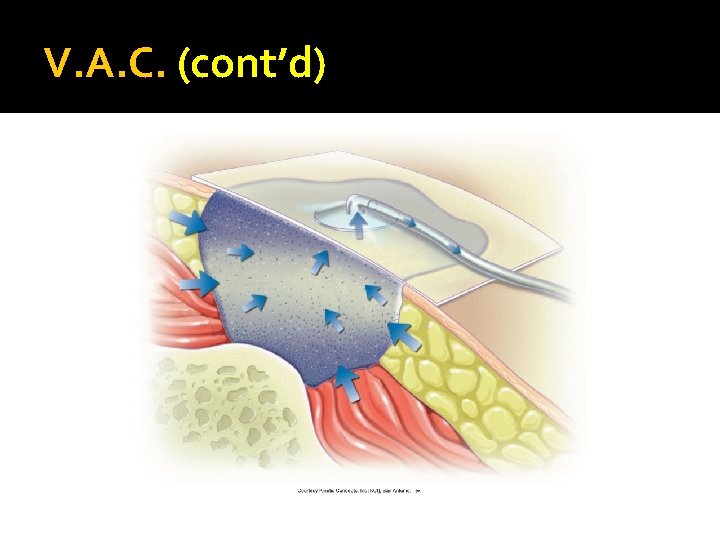
V. A. C. (cont’d)

Before and After V. A. C. Therapy
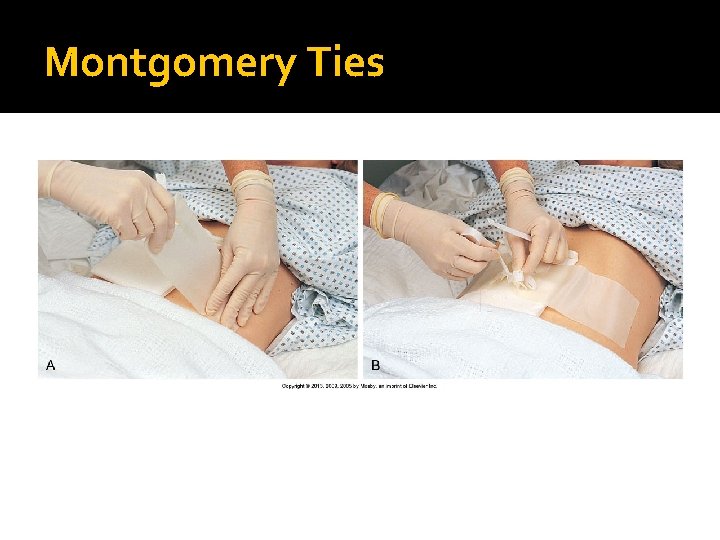
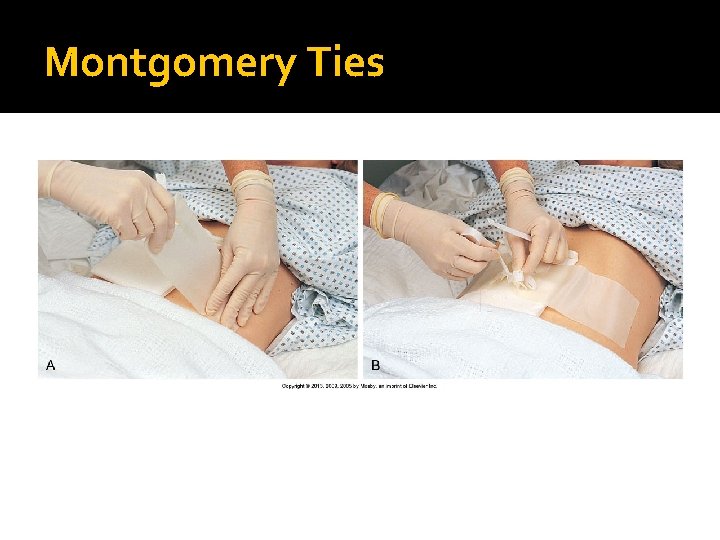
Montgomery Ties
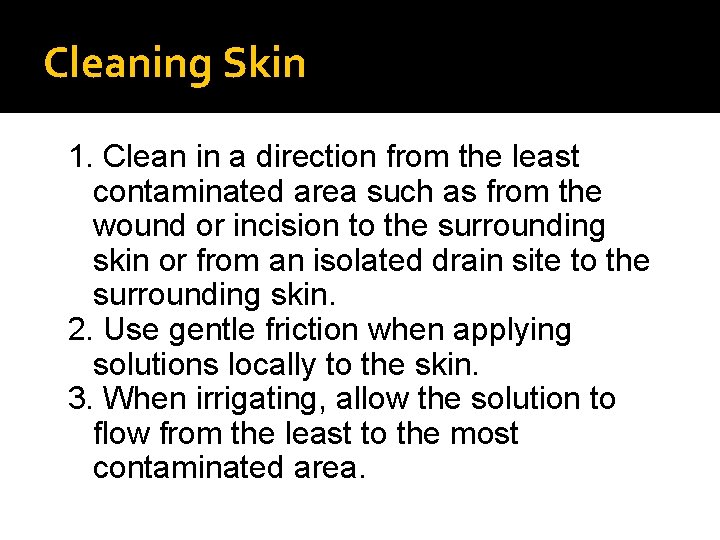
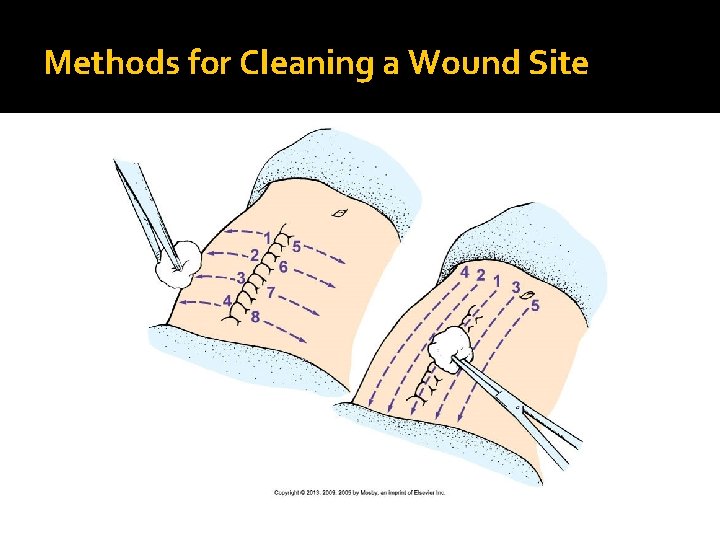
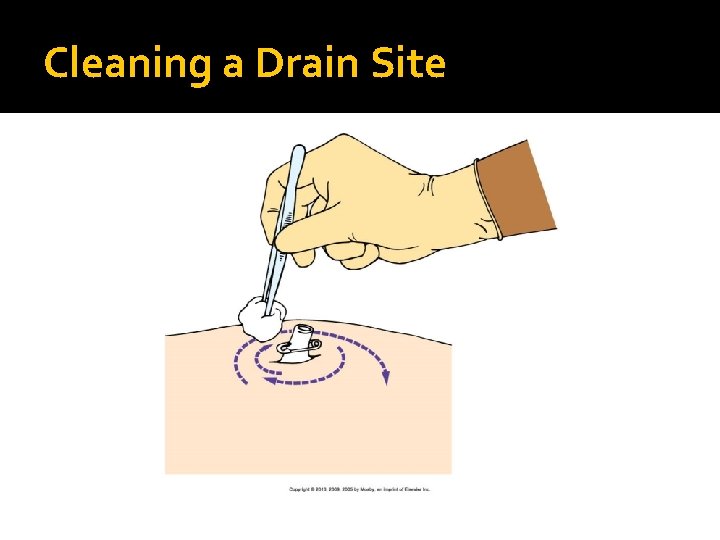
Cleaning Skin 1. Clean in a direction from the least contaminated area such as from the wound or incision to the surrounding skin or from an isolated drain site to the surrounding skin. 2. Use gentle friction when applying solutions locally to the skin. 3. When irrigating, allow the solution to flow from the least to the most contaminated area.

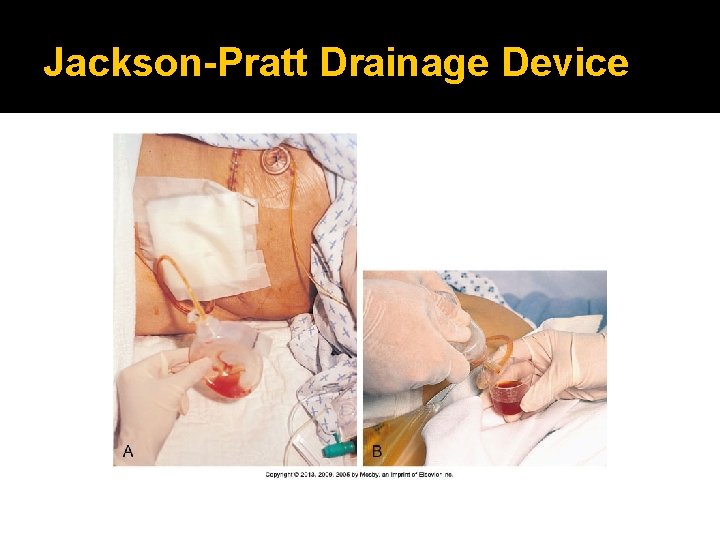
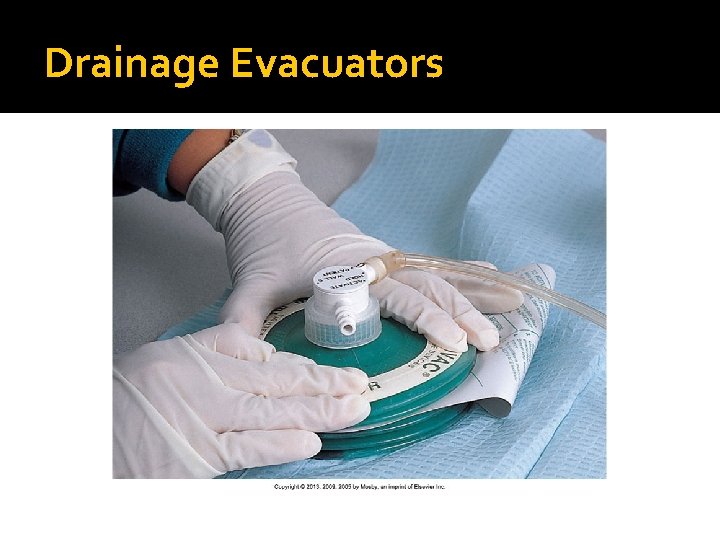
Cleaning Skin and Drain Sites Cleaning Irrigation Apply noncytotoxic solution. To remove exudates, use sterile technique with 35 -m. L syringe and 19 -gauge needle. Suture Care Drainage Evacuators Consult health care facility policy. Portable units exert a safe, constant, low-pressure vacuum to remove and collect drainage.
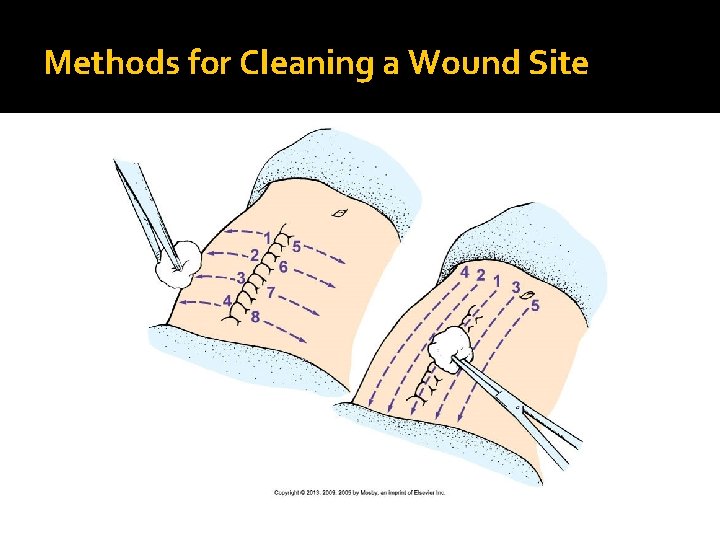
Methods for Cleaning a Wound Site
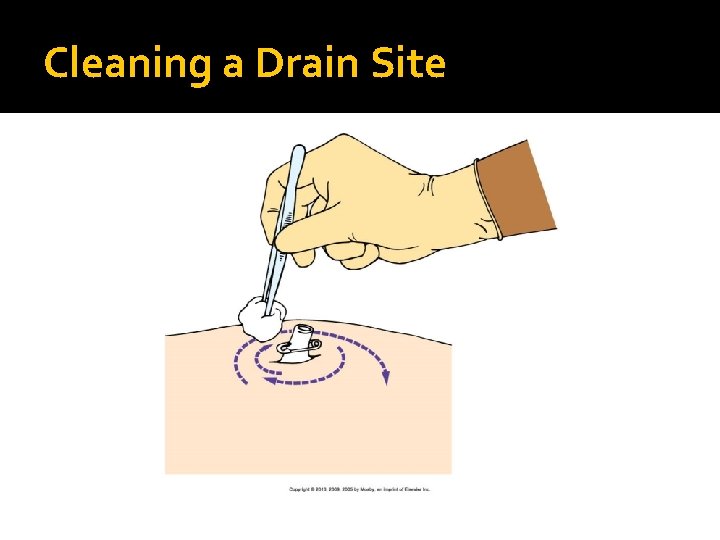
Cleaning a Drain Site

Staples and Remover
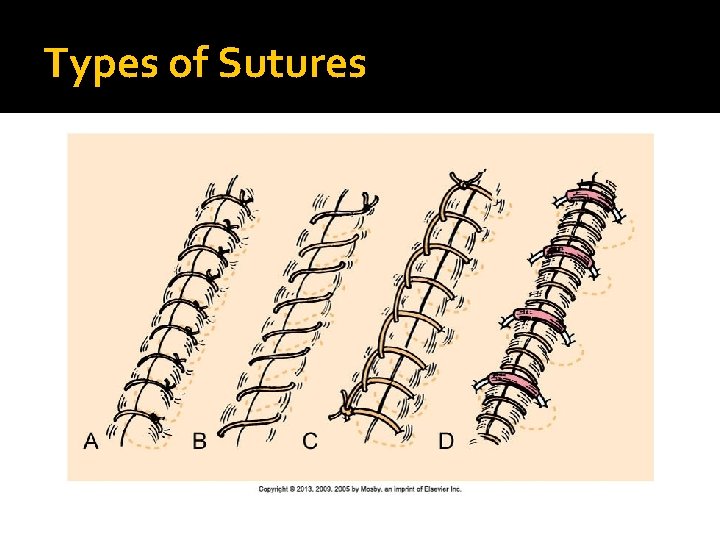
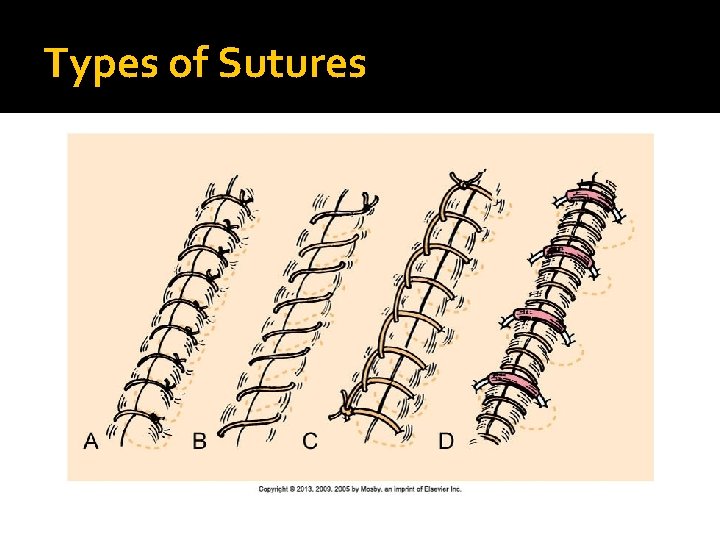
Types of Sutures
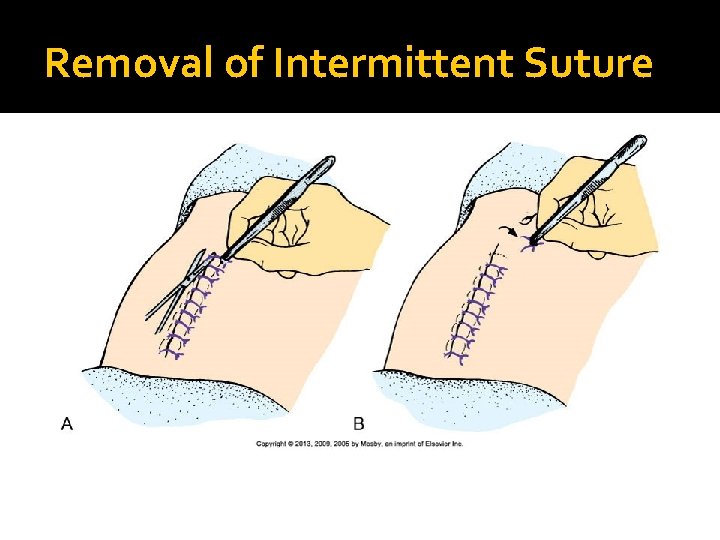
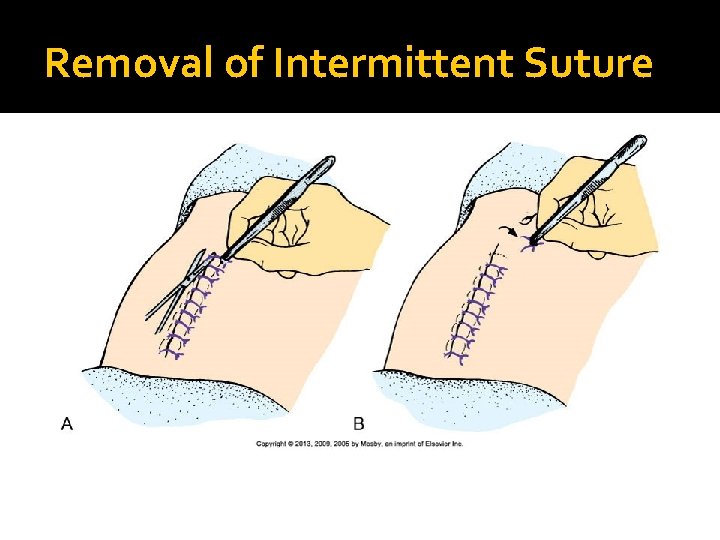
Removal of Intermittent Suture
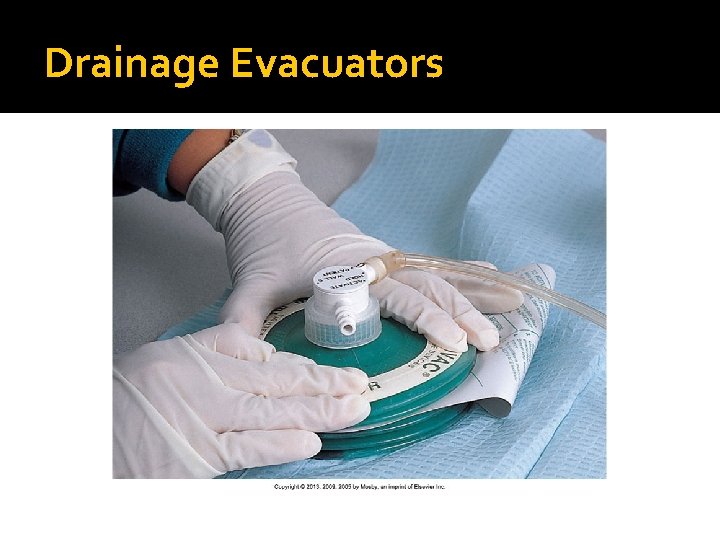
Drainage Evacuators
Quick Quiz! 2. A postoperative patient arrives at an ambulatory care center and states, “I am not feeling good. ” Upon assessment, you note an elevated temperature. An indication that the wound is infected would be A. It has no odor. B. A culture is negative. C. The edges reveal the presence of fluid. D. It shows purulent drainage coming from the incision site.
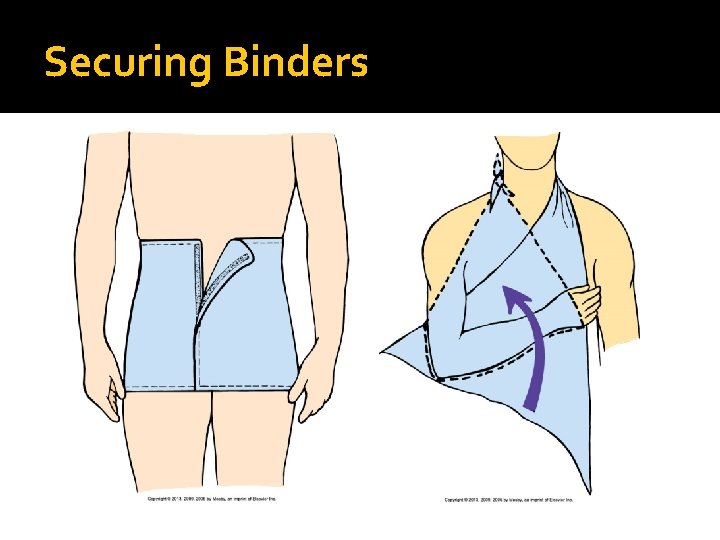
Bandages and Binders �Functions: create pressure, immobilize and/or support a wound, reduce or prevent edema, secure a splint, secure dressings �Bandages Rolled gauze, elasticized knit, elastic webbing, flannel, and muslin �Binder application Breast, abdominal, sling
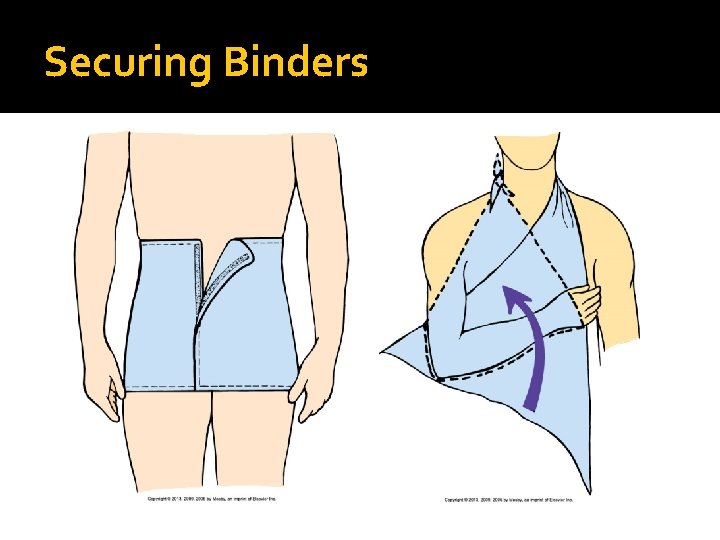
Securing Binders
Case Study (cont’d) �In preparation for her husband’s discharge, Mrs. Ahmed is interested in learning how to change Mr. Ahmed’s pressure ulcer dressing. Lynda develops a teaching plan to include Mrs. Ahmed, with the outcome goal that “At the end of the teaching session, Mrs. Ahmed will perform an acceptable return demonstration of dressing application. ” �What teaching and evaluation strategies would be appropriate?
Heat and Cold Therapy �Assessment for temperature tolerance Assess the skin and skin integrity. Assess the patient’s response to stimuli. Assess the equipment being used. Identify any contraindications. �Bodily responses to heat and cold �Local effects of heat and cold �Factors influencing heat and cold tolerance �Application of heat and cold therapies
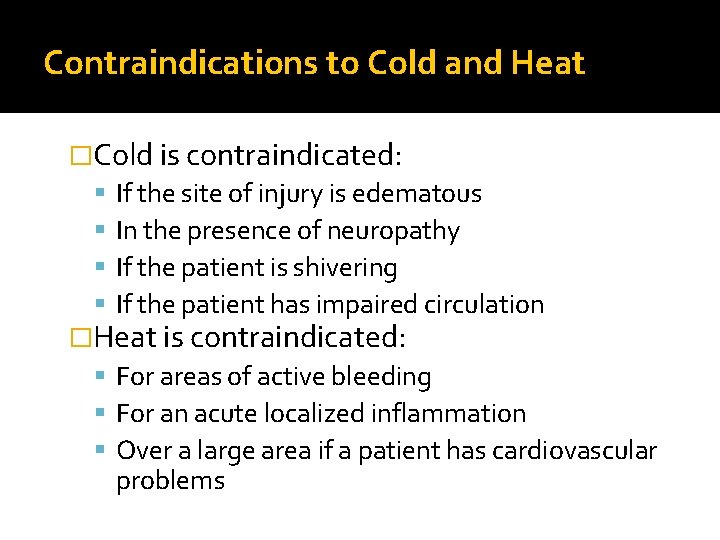
Contraindications to Cold and Heat �Cold is contraindicated: If the site of injury is edematous In the presence of neuropathy If the patient is shivering If the patient has impaired circulation �Heat is contraindicated: For areas of active bleeding For an acute localized inflammation Over a large area if a patient has cardiovascular problems
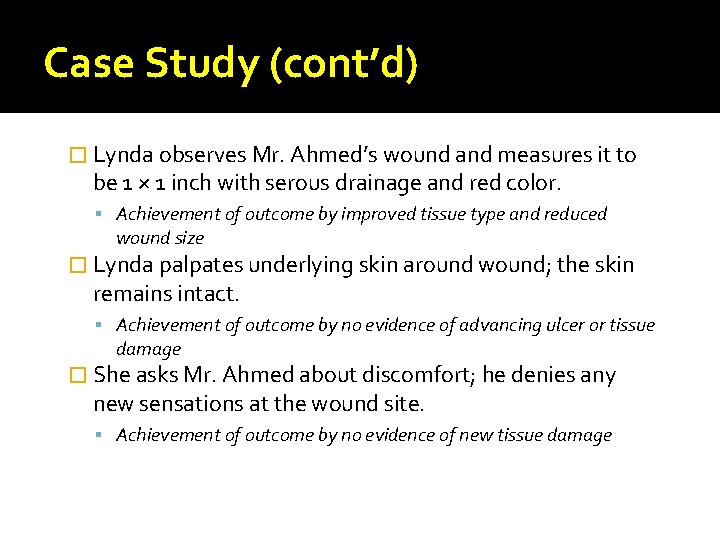
Case Study (cont’d) � Lynda observes Mr. Ahmed’s wound and measures it to be 1 × 1 inch with serous drainage and red color. Achievement of outcome by improved tissue type and reduced wound size � Lynda palpates underlying skin around wound; the skin remains intact. Achievement of outcome by no evidence of advancing ulcer or tissue damage � She asks Mr. Ahmed about discomfort; he denies any new sensations at the wound site. Achievement of outcome by no evidence of new tissue damage
Quick Quiz! 3. A surgical wound requires a Hydrogel dressing. The primary advantage of this type of dressing is that it provides A. An absorbent surface to collect wound drainage. B. Decreased incidence of skin maceration. C. Protection from the external environment. D. Moisture needed for wound healing.
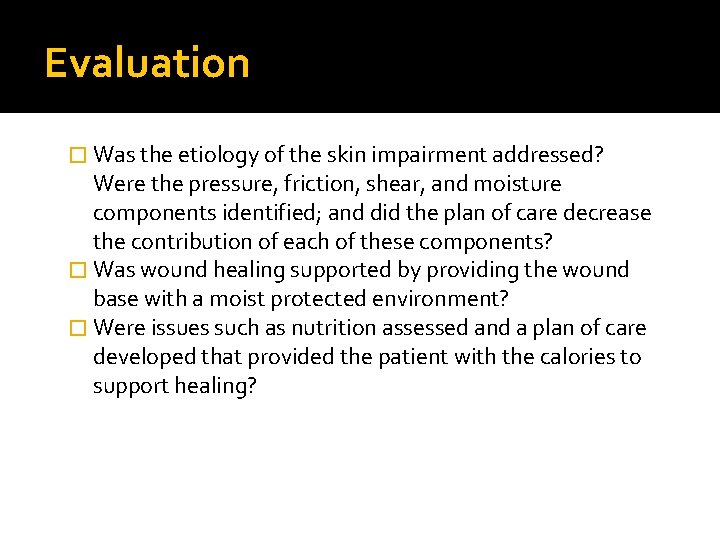
Evaluation � Was the etiology of the skin impairment addressed? Were the pressure, friction, shear, and moisture components identified; and did the plan of care decrease the contribution of each of these components? � Was wound healing supported by providing the wound base with a moist protected environment? � Were issues such as nutrition assessed and a plan of care developed that provided the patient with the calories to support healing?
Case Study (cont’d) � Lynda Abraham has completed her clinical experience with Mr. Ahmed. His pressure ulcer is still present, but it is reduced in size and demonstrates progress toward healing. No other sites of nonblanchable erythema were noted, and the rest of his skin remains intact. Lynda taught Mrs. Ahmed how to assess her husband’s skin for signs of increased risk for or further breakdown. Lynda, with the help of her instructor, devised a plan of care for the home, and they are meeting with the home care nurse today when she visits Mr. Ahmed at the hospital.