Approach to a thyroid nodule Anatomy of the
- Slides: 50
Approach to a thyroid nodule
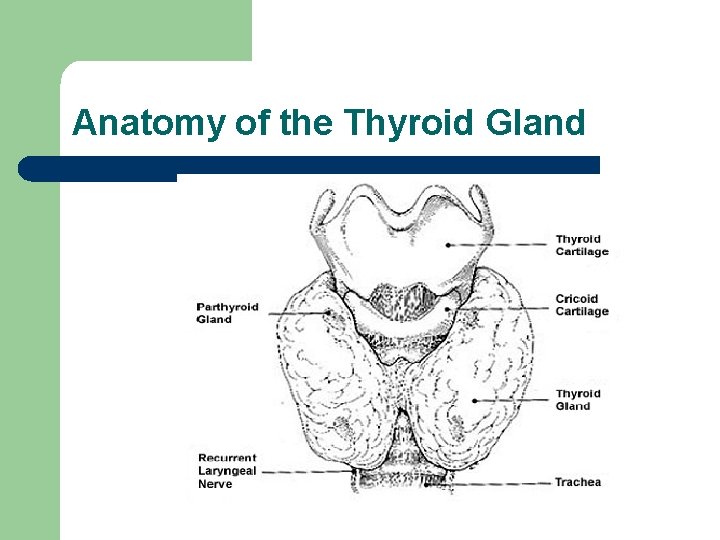
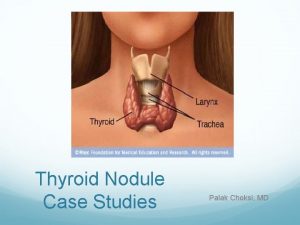
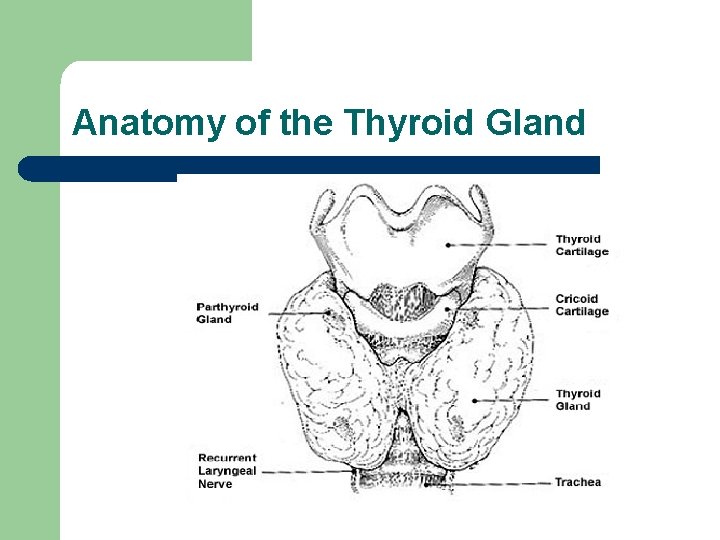
Anatomy of the Thyroid Gland
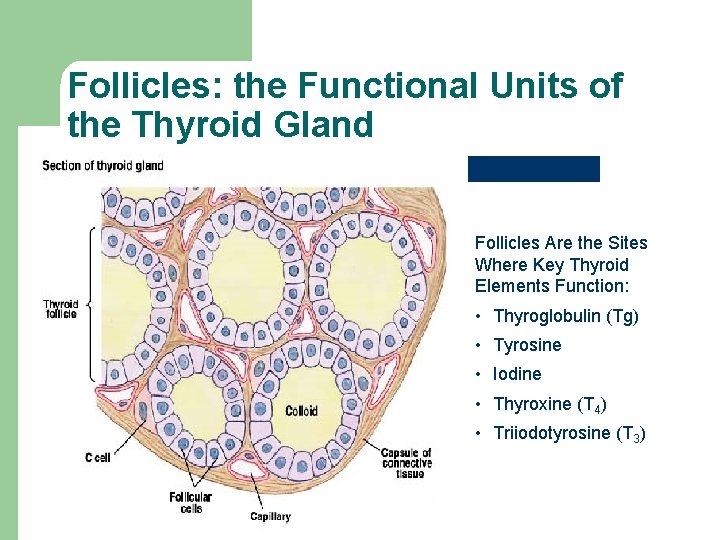
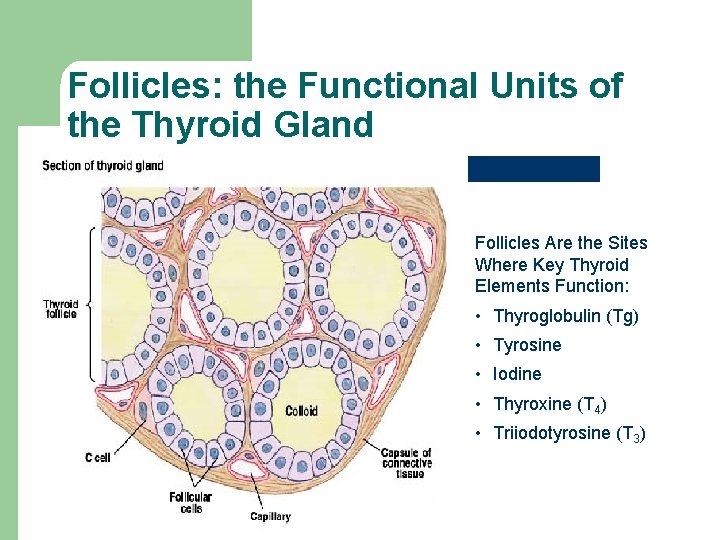
Follicles: the Functional Units of the Thyroid Gland Follicles Are the Sites Where Key Thyroid Elements Function: • Thyroglobulin (Tg) • Tyrosine • Iodine • Thyroxine (T 4) • Triiodotyrosine (T 3)
Thyroid Hormones l l l Thyroid pro-hormone is stored as thryoglobulin as an extracellular colloid T 3 and T 4 can cross lipid membranes readily (secretion and uptake) T 3 and T 4 are small, hydrophobic and circulate bound to Thyroxine-binding globulin (TBG)
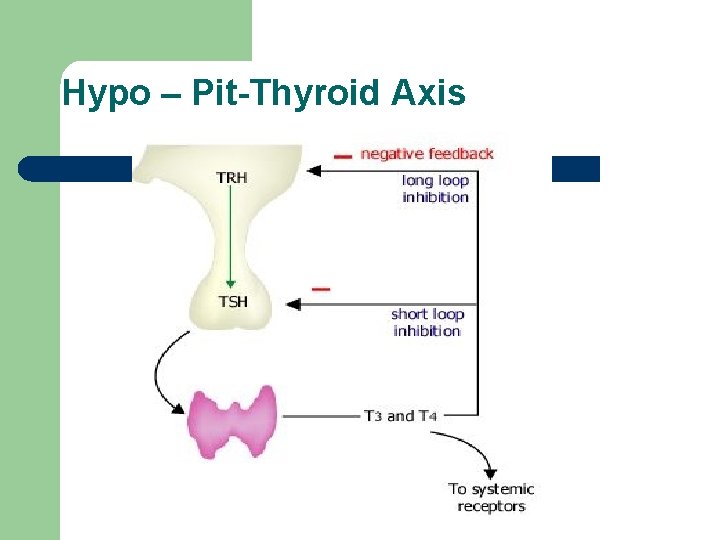
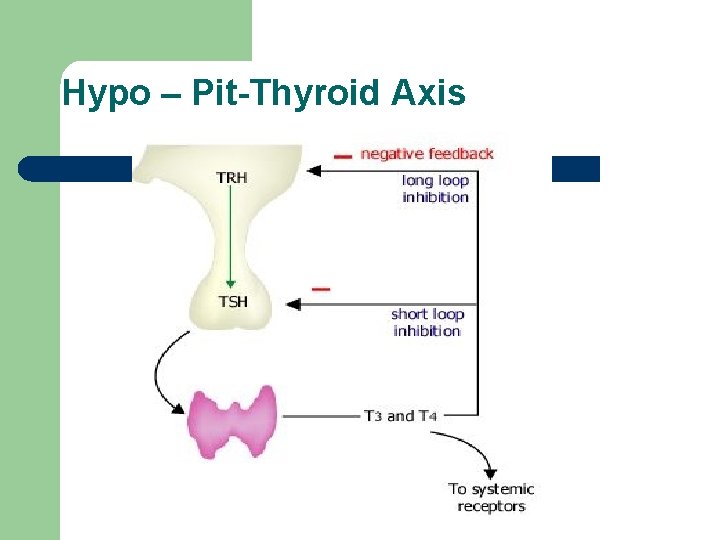
Hypo – Pit-Thyroid Axis
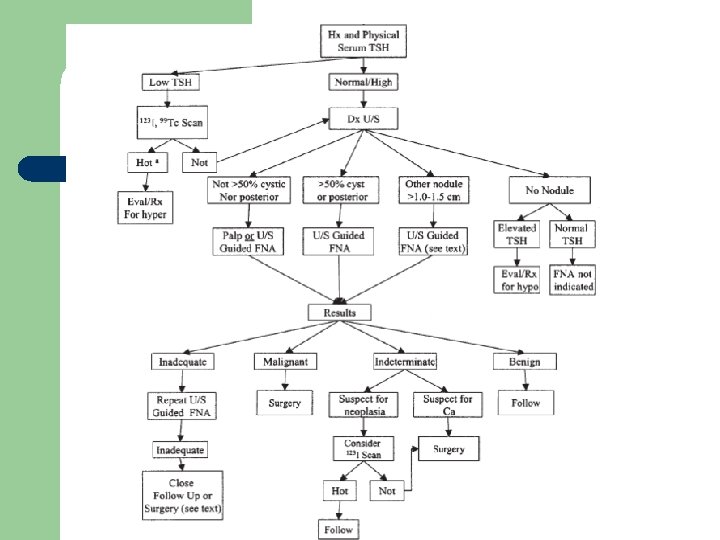
Approach l Clinical. l Biochemical. l Radiological. l Histopathological.
Clincal l History taking. l Physical examination.
History l l l Profile. Mass in ant. neck (onset, duration, pain, course, trauma…. ) Assessment of function( Symptoms of thyrotxicosis or hypothyroidism) Risk factors for malignancy. Review of Systems, medical hx. , past hx, drug hx, social hx.
Symptoms of thyrotoxicosis l nervousness, tremors, sweating, heat intolerance, palpitations, wt loss despite normal or increased appetite, amenorrhea, weakness.
Hypothyroidism l. Lethargy, hoarseness, hearing loss, thick and dry skin, constipation, cold intolerance, stiff gate, weight gain.
Risk factors for malignancy Age sex occupation family hx Painless Hoarseness Hx of irradiation hard, LN enlargement residency, . . . . etc.
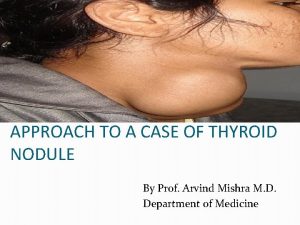
Physical Exam l Swelling in the anatomical site of thyroid. l Moves with swallowing
Goitre l Diffuse l Nodular -Solitary nodule -Multinodular goitre
l Anatomical dx includes retrosternal extension below sternocledomastoid
Solitary Noudule l Neoplastic l Non neoplastic
Non Neoplastic l Cyst: degenerative, Hemorrhagic, Hydatid… Surgery is indicated after second recurrence. l Solid : Part of Multinodular Goiter.
Neoplastic l Benign: Follicular adenoma l Malignant: Wide spectrum of behaviour
Papillary Ca l l l l Most common, Best prognosis 10 year survival around 85 % At younger age group. Spreads by lymphatics. Can be multifocal. Can be familial. Usually sensitive to RAI
Follicular Ca l l l 10 y survival around 60 %. Associated with iodine deficiency. Usually monofocal. Haematogenous spread. Diagnosed by capsular and vascular infiltration. Sensitive to RAI.
Medullary Ca l l l From Parafollicular cells. 10 year survival 25 -30% Can be Familial or Sporadic. Can be part of MEN 2. Does not uptake RAI.
Anaplastic l l Around 1 % Very aggressive tumor. The worst prognosis Survival is usually less than 6 months
Fibrolymphovasclar tumors l Haemangioma, Lymphoma, Fibroma, …. . l Secondary Metastases.
Biochemical l Thyroid function tests: T 3, T 4, TSH. l Antithyroid Antibodies: antithyroglobulin, antimicrosomal antibodies.
Imaging Assessment l Ultrasound. l Computerized tomographic scan. l Magnetic resonance scan. l Radioactive Iodine scan.
Pathological Dx l Fine Needle Aspiration. l Surgery for definitive biopsy.
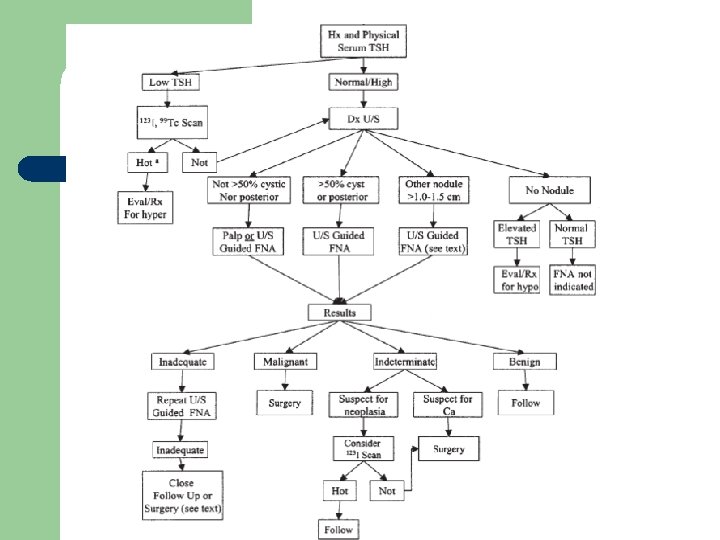
Ultrasound l One nodule or more l Cystic or solid l Presence or abecence of features of malignancy Cervical LN enlargement l
Features of malignancy in U/S l Microcalcification. l Hypoechoeic nodules. l Increased vascularity. l Interupted hallo sign
U/S guided FNA l Prefered if - > 50 % cystic leision. - located posteriorly.
Serum Thyroglobulin l Increases in most thyroid pathologies. l Not specific as a diagnostic tool. l For follow up only.
Serum Calcitonin l l Contraversy about its importance as a diagnostic tool. if >100 pg/ml can suggest medullary Ca.
Benign FNA l - Risk of false neg. Up to 5%. papable >U/S guided(0. 6%). Repeat examination or U/S 6 -18 m interval Growth>20%, or more than 2 mm in two dimensions repeat FNA preferably U/S guided.
Medical Treatment l No data to suggest that TSH suppression will cause a change in thyroid nodule size in Iodine sufficient area. l Not recomended.
Children l Should be evaluated as adults.
Pregnancy l l Thyroid scan should be delayed till delivery. If operation is to be done 12 -24 wks GA. After that should be postponed till delivery. (studies: delay less than one year will not affect the eventual prognosis)
Treatment l Goals: 1 -to remove the primary tumour and its local extension. 2 -to minimize treatment related morbidity. 3 -to permit accurate staging. 4 -fascilitate postop. Radioactive Iodine ttt. 5 -fascilitate long term postop. Surveilance 6 -minimize disease reccurence and mets.
Total Thyroidectomy l 1 - FNA papillary, medullary. 2 - nodule > 4 cm and atypia. 3 - hx. Of irradiation or positive family hx. 4 - bilateral nodules. 5 - regional LN or distant metastases. 6 - patient preferance for one stage. 7 - relative indication age >45
Lobectomy l Soitary nodule+indetermined pathology FNA+ patient preferance.
Central LN Dissection – l CLN are most common site of recurrence. Routine CLN dissection is indicated in medullary Ca. , no consensus in papillary Ca.
Lateral Neck Dissection Levels II, IV and V Done only with biopsy proven metastases after clinical or sonographic suspicion
Completion Thyroidectomy l l To allow resection of multicentric disease. Allow radioactive Iodine diagnostic scan and treatment. Studies: same surgical risk as one stage surgery. (small tumours<1 cm, intrathyroid, node neg. , low risk group) can be managed without completion.
Postoperative Radioactive Iodine Ablation l l Prepared with L-thyroxin withdrawal for 4 wks, or replace it with T 3 for 2 -4 wks then withdraw it for 2 wks. TSH > 30, to increase avidity. The minimal activity should be used 30 -100 mci. Higher dose 100 -200, in residual disease or aggressive pathology(tall cell, columnar, insular)
l Recombinant human thyrotropin(rh. TSH) can be used in patients who cannot tolerate stopping thyroxin. Needs stopping thyroxin for one day only. l Approved in Europe but still not in USA. l
Whole body scan l Usually done week after ablation therapy. l 10 -26% metastatic foci.
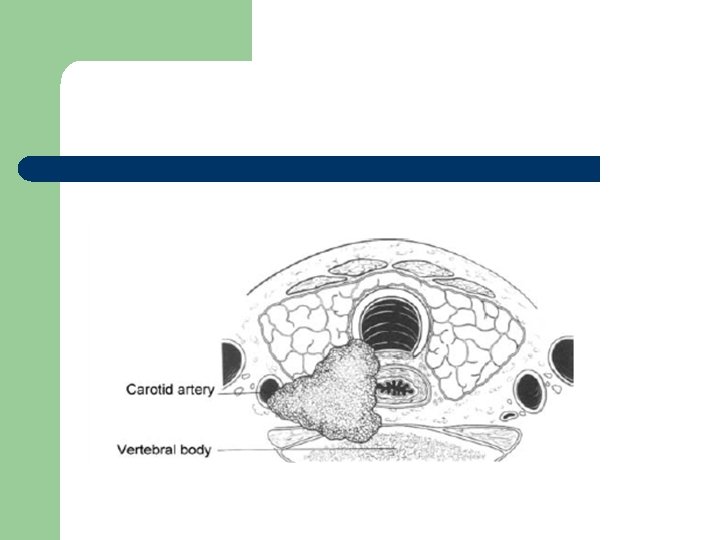
External Beam Radiotherapy l Indications - age > 45 and extrathyroid extension and high likelyhood of microscopic residual tumour. -gross residual and further surgery or radioactive iodine treatment is ineffective.
Chemotherapy l NO role for chemotherapy in differentiated thyroid Ca. l Some studies: Adriamycin can act as a radiation sensitizer for external beam radiotherapy.
TSH Suppression Therapy l Differntiated thyroid Ca have TSH receptors on cellular membrane. High risk patients < 0. 1 mu/l l Low risk patients l 0. 1 - 0. 5 mu/l
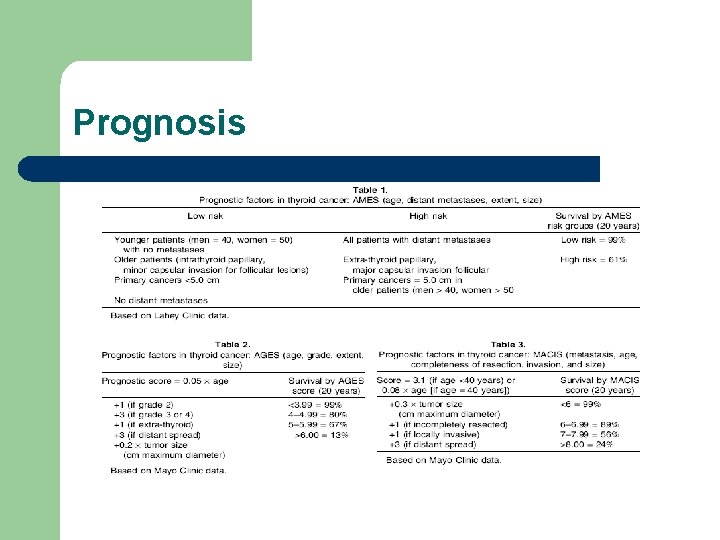
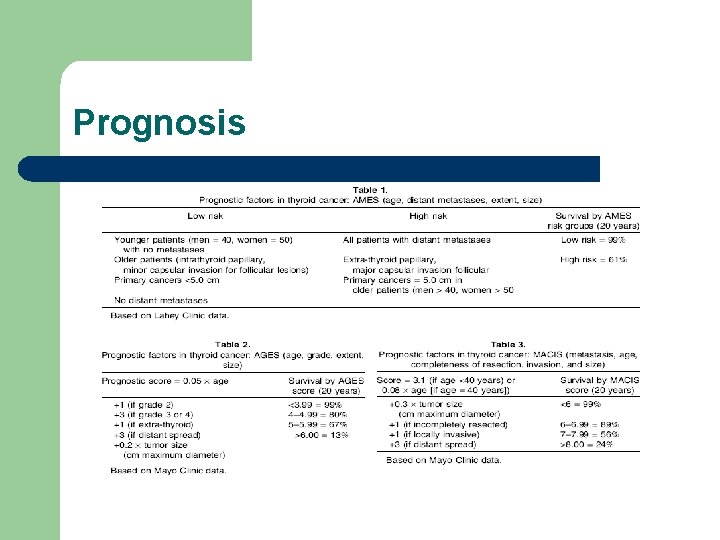
Prognosis
Follow Up l l l Every 6 -12 months. Physical examination and cervical U/S Thyroglobulin and calcitonin. In borderline Tgn stimulation by withdrawing thyroxin or rh. TSH. If positive whole body scan
 Riedel's thyroiditis
Riedel's thyroiditis Thyroid isotope scan
Thyroid isotope scan Thyroid nodule
Thyroid nodule Hyperparathyreosis
Hyperparathyreosis Hot thyroid nodule
Hot thyroid nodule Anatomy and physiology
Anatomy and physiology Thyroid anatomy
Thyroid anatomy Muscularis mucosa
Muscularis mucosa Philtrum
Philtrum Nodule isoéchogène tirads 3
Nodule isoéchogène tirads 3 Floccular nodule lobe
Floccular nodule lobe Nodule de sœur marie-joseph scanner
Nodule de sœur marie-joseph scanner Hypothyrodic
Hypothyrodic Les critères de jones
Les critères de jones Histology of large intestine
Histology of large intestine épaississement septal pulmonaire
épaississement septal pulmonaire Lepidique
Lepidique Esophageal varices
Esophageal varices Thyroid cancer: a case-based approach
Thyroid cancer: a case-based approach Traditional approach of development
Traditional approach of development Multiple approach avoidance
Multiple approach avoidance Deep learning approach and surface learning approach
Deep learning approach and surface learning approach Origins of vc and datagram networks
Origins of vc and datagram networks Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Theoretical models of counseling
Theoretical models of counseling Research approach meaning
Research approach meaning Waterfall vs shower approach
Waterfall vs shower approach Sơ đồ cơ thể người
Sơ đồ cơ thể người Tư thế ngồi viết
Tư thế ngồi viết đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Bổ thể
Bổ thể Glasgow thang điểm
Glasgow thang điểm ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Tư thế ngồi viết
Tư thế ngồi viết Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Phép trừ bù
Phép trừ bù Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Hươu thường đẻ mỗi lứa mấy con
Hươu thường đẻ mỗi lứa mấy con đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi