THYROID DISORDERS DR SULEMAN DOSANI Anatomy of Thyroid







- Slides: 54
THYROID DISORDERS DR SULEMAN DOSANI
Anatomy of Thyroid gland • The thyroid gland weighs approximately 20 g and is composed of two lobes joined by an isthmus. • The gland is closely affixed to the anterior and lateral aspects of the trachea with the upper border of the isthmus located just below the cricoid cartilage. ( C 5 -T 1) • A pair of parathyroid glands are located on the posterior aspect of each lobe.
Blood Supply: Ø superior thyroid artery, a branch of external carotid artery, and Ø inferior thyroid artery- thyrocervical trunk Venous drainage: Ø superior thyroid veins- internal jugular vein, Ø Middle thyroid vein- internal jugular vein, Ø Inferior thyroid veins- left brachio - cephalic vein.

Nerve Supply : Ø sympathetic nerve input from superior cervical ganglion and cervicothoracic ganglion of sympathetic trunk Ø Parasympathetic nerve input from superior laryngeal nerve and recurrent laryngeal nerve.

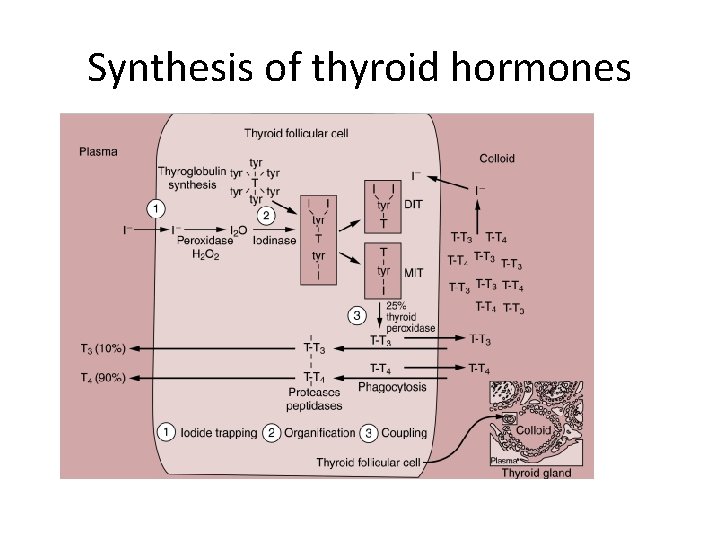
Synthesis of thyroid hormones • Trapping of iodide • Oxidation • Organification • Coupling
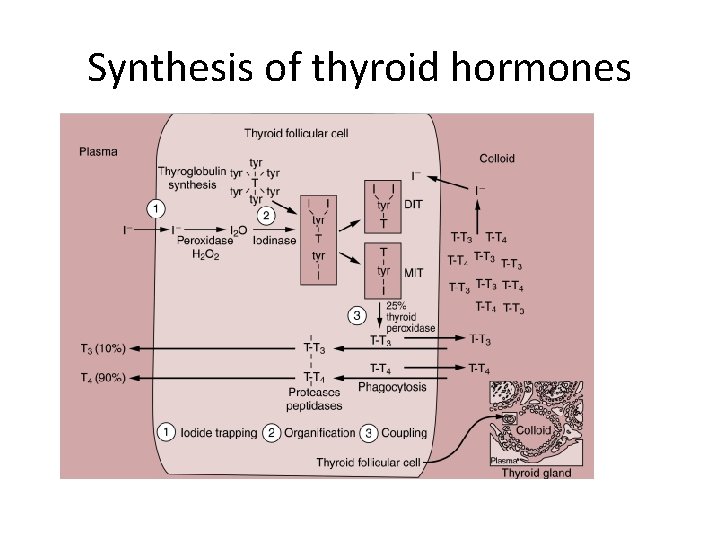
Synthesis of thyroid hormones
• Active hormones are released into the circulation, while unused iodotyrosines in the colloid undergo deiodination to yield free iodide for reuse. • The T 4/T 3 ratio of secreted hormones is 10/1. • Daily secretion of T 4 is approximately 80 to 100 μg. • Upon entering the blood, T 4 and T 3 bind reversibly to three major proteins: thyroxine binding globulin (80% of binding), prealbumin (10%– 15%), and albumin (5%– 10%).
• Only the small amount of free fraction of hormone, however, is biologically active. • The remainder serves as a metabolically inert reservoir. • The elimination half-life (T 1/2) of T 4 is 7 to 8 days and the T 1/2 of T 3 is 3 days. • Although only 10% of thyroid hormone secretion is T 3, T 3 is three to four times more active than T 4
• The majority of T 3 (75%) is derived from monodeiodination of T 4 in the periphery. • Ninty percent of thyroid hormone bound intracellularly is T 3 and 10% is T 4 • Deiodination pathways account for approximately 70% of the metabolism of T 3 and T 4. • T 3 and T 4 are also conjugated in the liver with glucuronic acid and excreted into the bile
Ø Regulation of Thyroid Secretion • Thyroid function is regulated primarily by variations in the circulating level of pituitary TSH. • TSH secretion is increased by the hypothalamic hormone thyrotropin-releasing hormone (TRH) and inhibited in a negative feedback fashion by circulating free T 4 and T 3. • TSH secretion is also inhibited by stress, and in experimental animals it is increased by cold and decreased by warmth
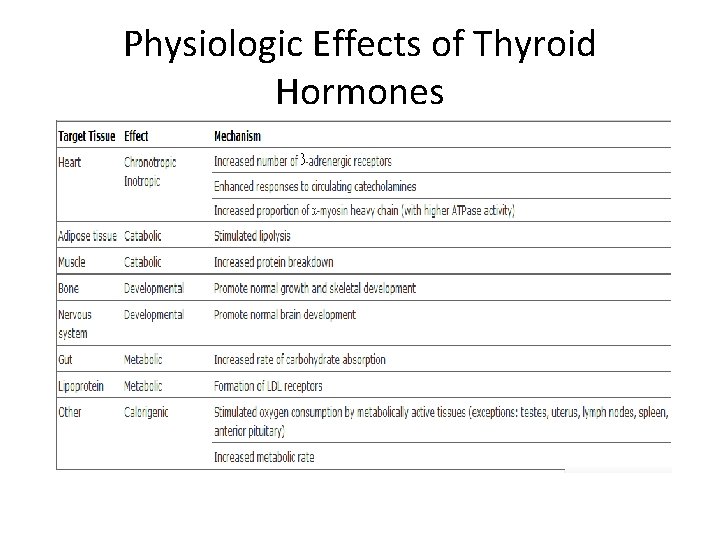
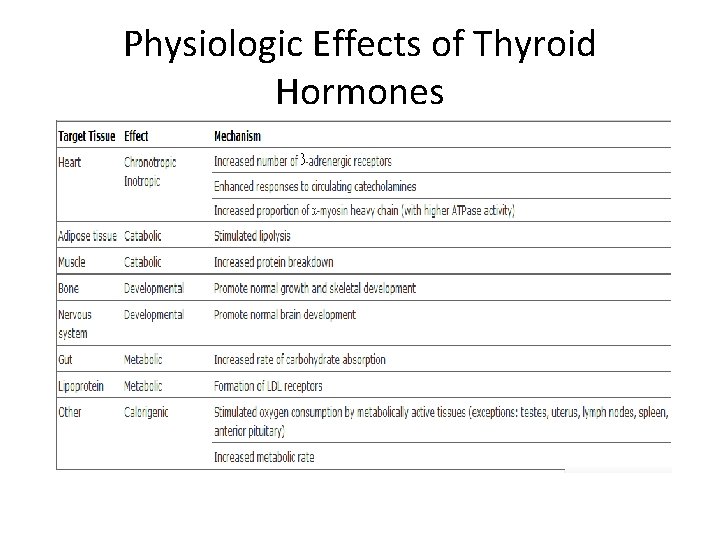
Physiologic Effects of Thyroid Hormones
Tests of Thyroid Function 1. Serum Thyroxine • The serum T 4 assay is the standard screening test for evaluation of thyroid gland function. • The total T 4 is elevated in approximately 90% of patients with hyperthyroidism, and it is low in 85% of those who are hypothyroid. • The serum T 4 concentration is influenced by thyroid hormone protein binding capacity.
• An increase or decrease in TBG levels or in protein binding may therefore alter the total T 4 but not the concentration of the free T 4. • Because of the effect of TBG on circulating total T 4, T 4 levels should never be used alone to evaluate thyroid disease. • Elevations in the TBG concentration are the most common cause of hyperthyroxinemia in euthyroid patients.
2. Serum Tri-iodothyronine: • Serum T 3 levels are often determined to detect disease in patients with clinical evidence of hyperthyroidism in the absence of elevations of T 4. • T 3 concentrations may be depressed by factors that impair the peripheral conversion of T 4 to T 3 (sick euthyroid syndrome).
• In 50% of hypothyroid patients, the serum T 3 concentration is low; in the remaining 50%, it is normal. 3. Thyroid-Stimulating Hormone: • It is often higher than 20 m. U/L in primary hypothyroidism. • Current assays are sensitive enough to diagnose hyperthyroidism by depressed levels of TSH.
• A condition characterized by elevated TSH and normal T 4 may represent subclinical hypothyroidism. • A low TSH level in a clinically hypothyroid patient indicates disease at the pituitary or hypothalamic level. • Starvation, fever, stress, corticosteroids, and T 3 or T 4 can all depress TSH levels.
4. THBR : Thyroid Hormone Binding Ratio • Measures the uptake of T 3/T 4 tracer by thyroid binding globulin in a given serum sample • Normal THBR is 24%-39% • Hyperthyroidism - increase • Hypothyroidism – decrease • It is directly proportional to the fraction of F T 4, and inversely proportional to the TBG binding sites.
5. Radioactive iodine uptake test : • I 123, I 131 or technetium-99 are used. • The percentage of tracer taken up by the thyroid in 24 hrs is measured. • Normal range – 10 -25% • The test is done to confirm hyperthyroidism where the uptake is high. 6. Thyroid scans : using I 123 or technetium 99 • Warm - normal
• Hot - hyperfunctioning (hyperthyroid) • Cold - hypofunctioning (hypothyroid and malignancy). 7. USG – to determine whether a lesion is cystic, solid or mixed. OTHER: • detection of serum antimicrosomal antibodies, anti thyroglobulin antibodies, long acting thyroid stimulator, thyroid stimulating thyroglobulins.
Hyperthyroidism • Hyperthyroidism results from the exposure of tissues to excessive amounts of thyroid hormone. • The most common etiology is the multinodular diffuse goiter of Graves' disease. • This typically occurs between the ages of 20 and 40 years, and is predominant in women.
causes 1. • • • 2. • Primary: Grave’s ds, MNG, Single toxic nodule Thyroiditis Thyroid ca. Secondary: Excess TSH: Pituitary tumor 3. • • • Iatrogenic : drugs Thyroxin Iodides Amiodarone
Clinical features • General : weight loss, tremors, heat intolerence, sweating, goitre, apathy, fatigue. • CVS: increased CO with tachycardia, arrhythmias (commonly atrial) and palpitations, a hyperdynamic circulation, increased myocardial contractility and cardiomegaly. • Respiratory : Dyspnea • GIT: diarrhea, N & V • CNS: anxiety, Irritability, insomnia. • Neuromuscular : proximal neuropathy, muscle weakness. • Ophthalmic: lid lag, lid retraction, reduced blinking, exophthalmos, corneal ulceration. • Reproductive : amenorrhea, oligomenorrhe a, infertility.

• A hyperdynamic circulation characterized by tachycardia, tachyarrythmias and increased CO suggests excessive activity of the SNS and a compensatory attempt to eliminate heat. • The sensitivity of Beta-receptors is increased in hyperthyroid patients. • The PP is increased due to increase in sys BP and a decrease in diastolic BP due to vasodilation.
• Circulating plasma catacholamines levels are normal but thyroid hormones increases the sensitivity to catacholamines.
Treatment A. Anti–thyroid drugs: PTU 200 to 300 mg orally every 8 to 12 hours Methimazole as 10 to 20 mg orally 12 hours. • A euthyroid state in 6 to 8 weeks. • Once euthyroidism is achieved, the dose is reduced and continued for 6 to 12 months and in some cases for 24 months. • S/E: Agranulocytosis, Hepatotoxicity, Arthritis, Skin ulceration, Vasculitis, Teratogenicity.
B. Iodides: • Iodide in high concentration inhibits release of hormones from the hyperfunctioning gland. • It is usually reserved for preparing hyperthyroid patients for surgery, managing patients with actual or impending thyroid storm, or treating patients with severe thyrocardiac disease.
• High concentrations of iodide reduces gland size and possibly a decrease in vascularity. • Administered orally as an SSKI (saturated solution of potassium iodide) solution, 5 drops orally every 8 hours for 10 to 14 days. • Lugol’s iodine 8 drops, 4 times a days • The radiographic contrast dye ipodate sodium or iopanoic acid (0. 5– 3. 0 g every day) demonstrates beneficial effects (Inhibits 5’ deiodinase) inhibits conversion of T 4 to T 3 & also inhibits release from gland
• Lithium carbonate 300 mg orally every 6 hours C. β-Adrenergic antagonists : • Propranolol 40 to 80 mg orally every 6 to 8 hours, • esmolol, metoprolol, and atenolol are effective • For emergency use, IV propranolol in 0. 21. 0 mg boluses followed by an infusion or an IV esmolol 0. 5 mg/kg bolus followed by an infusion is titrated to restore a normal heart rate.
D. Radioactive 131 I therapy: Standard doses deliver approximately 8500 c. Gy( centigray ) rad to the thyroid and destroy the follicular cells. • The remission rate is 80% to 98%. • A major disadvantage of therapy is that 40% to 70% of treated patients become hypothyroid within 10 years.
E. Surgery (i. e. , subtotal thyroidectomy or total thyroidectomy) results in prompt control of disease and a lower incidence of hypothyroidism (10%– 30%) than radioactive iodine. Ø Hyperthyroidism in pregnancy: • PTU 200 mg/day (Agranulocytosis & aplastic anemia) • Inhibits thyroperoxidase (TPO oxidizes iodide to iodine) • Methimazole- aplastic cutis and choanal atresia • Radioactive therapy and iodine therapy- C/I
Hypothyroidism • Hypothyroidism or myxedema is a relatively common disease affecting 0. 5% to 0. 8% of the adult population. • Primary hypothyroidism results in a decreased production of thyroid hormones despite adequate or increased levels of TSH and accounts for 95% of all cases. • Secondary hypothyroidism due to hypothalamic or pituitary disease accounts for 5%.
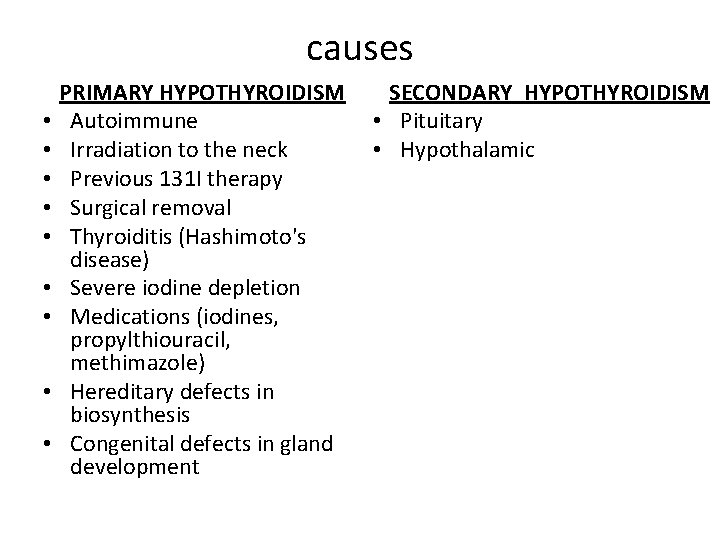
causes • • • PRIMARY HYPOTHYROIDISM Autoimmune Irradiation to the neck Previous 131 I therapy Surgical removal Thyroiditis (Hashimoto's disease) Severe iodine depletion Medications (iodines, propylthiouracil, methimazole) Hereditary defects in biosynthesis Congenital defects in gland development SECONDARY HYPOTHYROIDISM • Pituitary • Hypothalamic
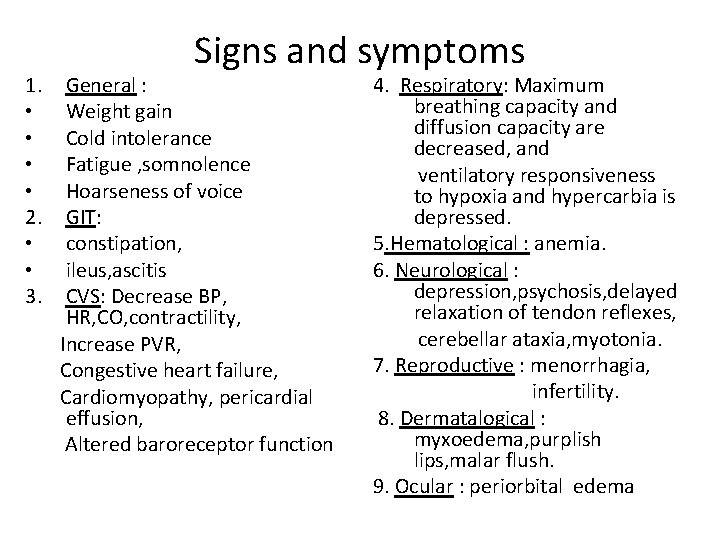
1. • • 2. • • 3. Signs and symptoms General : Weight gain Cold intolerance Fatigue , somnolence Hoarseness of voice GIT: constipation, ileus, ascitis CVS: Decrease BP, HR, CO, contractility, Increase PVR, Congestive heart failure, Cardiomyopathy, pericardial effusion, Altered baroreceptor function 4. Respiratory: Maximum breathing capacity and diffusion capacity are decreased, and ventilatory responsiveness to hypoxia and hypercarbia is depressed. 5. Hematological : anemia. 6. Neurological : depression, psychosis, delayed relaxation of tendon reflexes, cerebellar ataxia, myotonia. 7. Reproductive : menorrhagia, infertility. 8. Dermatalogical : myxoedema, purplish lips, malar flush. 9. Ocular : periorbital edema
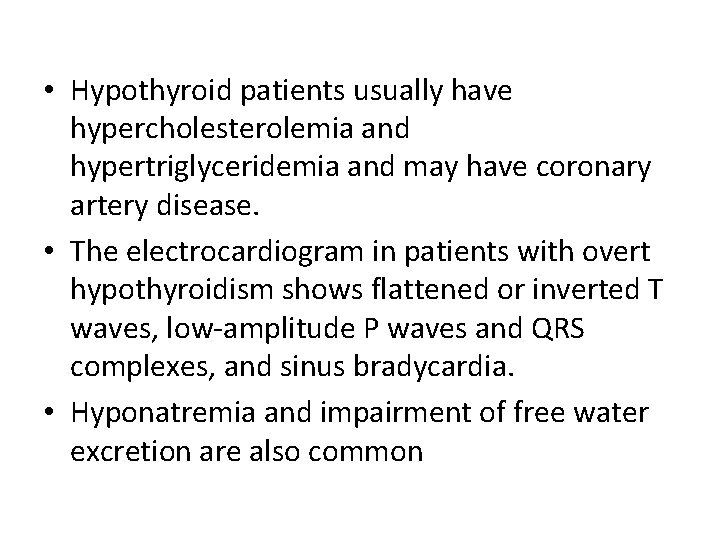
• Hypothyroid patients usually have hypercholesterolemia and hypertriglyceridemia and may have coronary artery disease. • The electrocardiogram in patients with overt hypothyroidism shows flattened or inverted T waves, low-amplitude P waves and QRS complexes, and sinus bradycardia. • Hyponatremia and impairment of free water excretion are also common
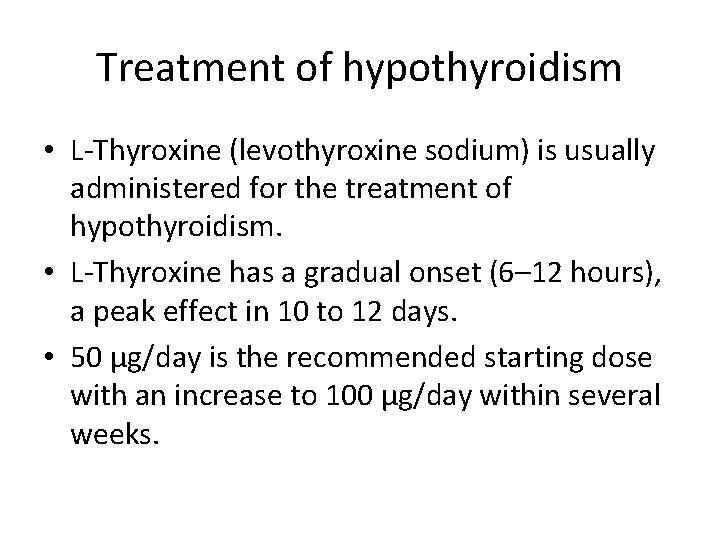
Treatment of hypothyroidism • L-Thyroxine (levothyroxine sodium) is usually administered for the treatment of hypothyroidism. • L-Thyroxine has a gradual onset (6– 12 hours), a peak effect in 10 to 12 days. • 50 μg/day is the recommended starting dose with an increase to 100 μg/day within several weeks.
• For the elderly or patients with coronary artery disease, 25 μg/day increasing monthly by 25 -μg increments is recommended until euthyroidism is achieved. • Other alternative preparations include thyroid extract USP, I-triiodothyronine T 3 (liothyronine sodium), and liotrix, a combination of T 4 and T 3 in a 4: 1 ratio.
Myxedema Coma • Myxedema coma is a rare severe form of hypothyroidism characterized by delirium or unconsciousness, hypoventilation, hypothermia , bradycardia, hypotension, and a severe dilutional hyponatremia. • It is a medical emergency with a mortality rate greater than 50% and requires immediate aggressive treatment.
• Diagnosis based on characteristic clinical syndrome in a patient with hypothyroidism • Laboratory role is to confirm that patient is hypothyroid & also look for treatable complications like hypoventilation, hypoglycemia, & hyponatremia • Sub normal serum free thyroxine index or serum FT 4 concentration & elevated TSH
Clinical features of myxedema coma • • • Mental obtundation Course, dry skin Myxedema facies Hypothermia Hypoglycemia Bradycardia & hypotension Atonic GI tract Atonic bladder Pleural, pericardial & peritoneal effusions

• Infection, trauma, cold, and central nervous system depressants predispose hypothyroid patients to myxedema coma. • This is the one indication for intravenous thyroxine. • I-Thyroxine in a 300 -500 -μg loading dose followed by a maintenance dose of 50 to 200 μg/day or I-triiodothyronine in a 25 - to 50 -μg loading dose followed by a maintenance infusion is recommended. • I-Triiodothyronine has a more rapid onset and may be preferred.
• Intravenous hydration with glucose-containing saline solutions, temperature regulation, correction of electrolyte imbalances, and stabilizing the cardiac and pulmonary systems are necessary. • Mechanical ventilation is frequently necessary. • Intravenous hydrocortisone 100 to 300 mg/day is also prescribed to treat possible adrenal insufficiency (AI), a common sequelae of hypothyroidism.
Euthyroid sick syndrome • It occurs in critically ill patients with significant non thyroidal illness who demonstrate abnormal thyroid function tests. • These tests demonstrate low levels of T 3 and T 4 and a normal TSH. • As illness increases in severity, the T 3 and T 4 levels decrease further. • It may be a physiologic response to stress, and it can be induced by surgery. • No treatment for thyroid function is necessary.
Thyroid storm • It is an abrupt exacerbation of hyperthyroidism caused by excessive release of thyroid hormones into the circulation • Predisposing factors: • Medical factors Ø Infection, fever, uncontrolled toxicity Ø Improper treatment Ø Pregnancy Ø Anxious and nervous patients before surgery
• Surgical factors: Ø Too much handling of gland before surgery Ø Rough handling of gland during surgery. • It occurs most commonly in the post-op period. • Patients present with extreme anxiety, fever, tachycardia, cardiovascular instability, and altered consciousness, psychosis, seizures, GI disturbances like N/V, abd pain, jaundice etc. ,
Ø Hyperthermia Ø Tachycardia Ø Hypertension Ø High output failure and then to low output failure Ø Arrhythmia( AF) Ø Flushing /sweating Ø Increased Et. Co 2 Ø Hypo/hyperglycemia

Ø Treatment : § Increase the inspired O 2 concentration § Surface cooling-sponging, ice packs, iced IV fluids. § propranolol, labetalol, or esmolol titrated to decrease heart rate to less than 90 bpm. § dexamethasone 2 mg every 6 hours or cortisol 100 to 200 mg every 8 hours
• Antithyroid drugs (PTU 200– 400 mg every 8 hours) may be administered through a nasogastric tube, orally, or rectally. • If circulatory shock is present, an intravenous direct vasopressor (phenylephrine) is indicated. • β-adrenergic blocker or digitalis is recommended for atrial fibrillation accompanied by a fast ventricular response. • Serum thyroid hormone levels generally return to normal within 24 to 48 hours and recovery occurs within 1 week. • Unfortunately, the mortality rate for thyroid storm remains surprisingly high at approximately 20%.


THANK YOU
 Hussein suleman
Hussein suleman Suleman ahmer
Suleman ahmer Reporaproblem
Reporaproblem Uct computer
Uct computer Hussein suleman
Hussein suleman Hussein suleman
Hussein suleman Thyroid anatomy
Thyroid anatomy Thyroid anatomy
Thyroid anatomy Anxiety disorders def
Anxiety disorders def Multipath model of anxiety disorders
Multipath model of anxiety disorders Neurobehavioral disorders list
Neurobehavioral disorders list Chapter 11 childhood and neurodevelopmental disorders
Chapter 11 childhood and neurodevelopmental disorders Psychiatric nursing theories
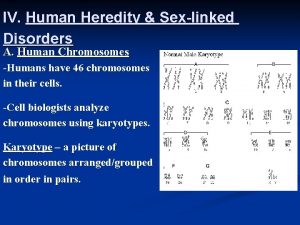
Psychiatric nursing theories Sex linked disorders
Sex linked disorders The uk national disorders
The uk national disorders Lrrk
Lrrk Chapter 15 anxiety and obsessive-compulsive disorders
Chapter 15 anxiety and obsessive-compulsive disorders Neurocognitive disorder
Neurocognitive disorder Chapter 5 mental and emotional problems answer key
Chapter 5 mental and emotional problems answer key Neurosis disorder
Neurosis disorder Physiological disorders of onion
Physiological disorders of onion Chapter 29 endocrine and metabolic disorders
Chapter 29 endocrine and metabolic disorders Cluster b personality traits
Cluster b personality traits Cluster c personality disorders
Cluster c personality disorders National iodine deficiency disorders control programme
National iodine deficiency disorders control programme Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases Disorders of the nervous system
Disorders of the nervous system Body dysmorphia irvine
Body dysmorphia irvine Mcq on phenylketonuria
Mcq on phenylketonuria Acupuncture for eating disorders
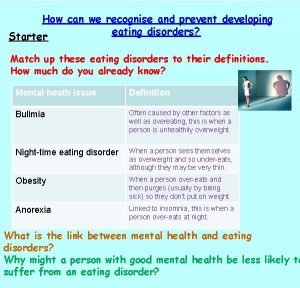
Acupuncture for eating disorders How to spot eating disorders
How to spot eating disorders Using karyotypes to diagnose genetic disorders
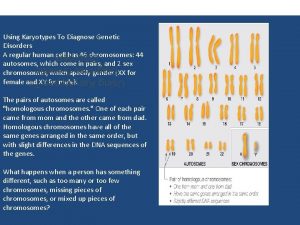
Using karyotypes to diagnose genetic disorders Somatoform disorder nursing diagnosis
Somatoform disorder nursing diagnosis Sleep disorders
Sleep disorders Edema heart
Edema heart Chapter 47 urinary and reproductive disorders
Chapter 47 urinary and reproductive disorders Cluster b personality disorder
Cluster b personality disorder Edema lesion
Edema lesion Eating disorder in which people overeat compulsively
Eating disorder in which people overeat compulsively Chapter 18 psychological disorders
Chapter 18 psychological disorders Unit 14 physiological disorders
Unit 14 physiological disorders Recognize developmental disorders of the dentition
Recognize developmental disorders of the dentition Assistive technology for emotional and behavioral disorders
Assistive technology for emotional and behavioral disorders Freud anorexia
Freud anorexia Orotic aciduria
Orotic aciduria Mental health disorders
Mental health disorders Chapter 46 digestive and endocrine disorders
Chapter 46 digestive and endocrine disorders Personality disorders dsm 5
Personality disorders dsm 5 Squamous cell carcinoma
Squamous cell carcinoma Chapter 14 psychological disorders
Chapter 14 psychological disorders Karla homulka
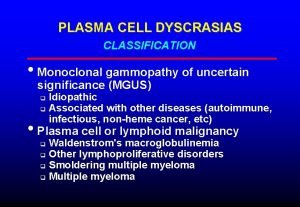
Karla homulka Waldenstrom macroglobulinemia mnemonic
Waldenstrom macroglobulinemia mnemonic Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Congenital voice disorders
Congenital voice disorders Milady nail diseases and disorders
Milady nail diseases and disorders