ADVERSE NEURAL TISSUE TENSION The Manual Therapy Institute







- Slides: 60
ADVERSE NEURAL TISSUE TENSION The Manual Therapy Institute
Anatomy & Physiology
Going back to Anatomy…
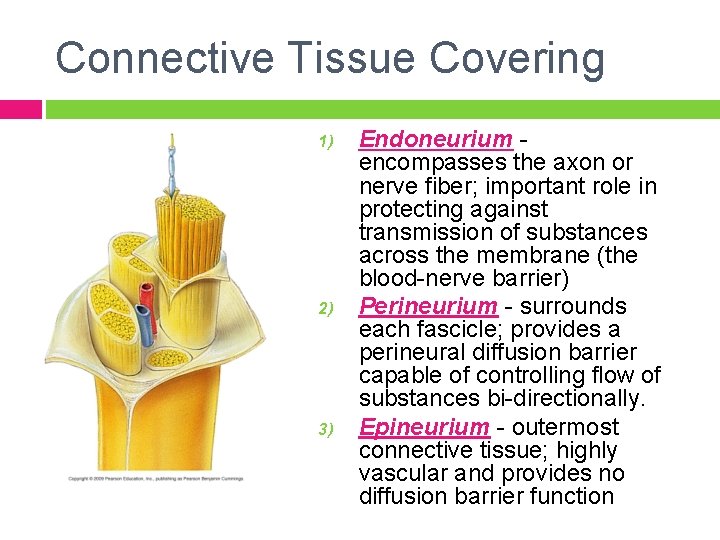
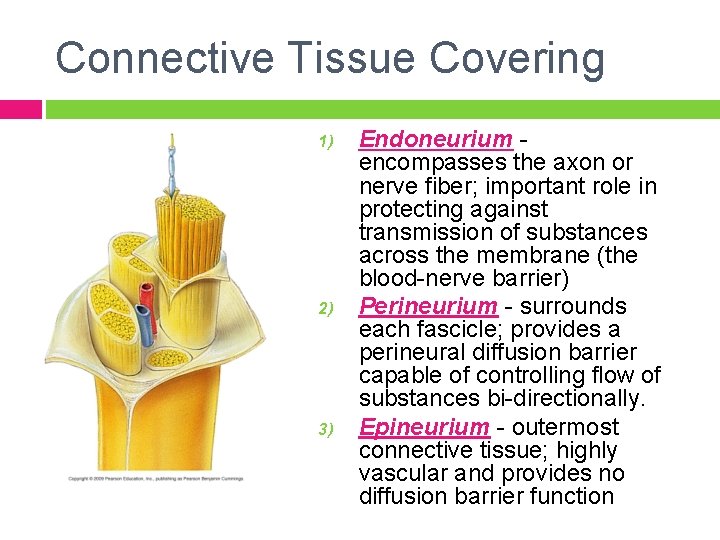
Connective Tissue Covering 1) 2) 3) Endoneurium encompasses the axon or nerve fiber; important role in protecting against transmission of substances across the membrane (the blood-nerve barrier) Perineurium - surrounds each fascicle; provides a perineural diffusion barrier capable of controlling flow of substances bi-directionally. Epineurium - outermost connective tissue; highly vascular and provides no diffusion barrier function


Nerve Nutrition Bi-directional Nutritional Flow (Axoplasmic Flow): � Antegrade Flow: � Fast 400 mm day, carries substances used in the transmission of impulses (neurotransmitters and transmitter vesicles) Slow 1 -6 mm/day, carries substances needed for the maintenance of the structure of the axon Retrograde Flow: 200 mm/day, responsible for carrying extracellular materials from the nerve terminal and trophic messages about the status of the nerve and the target tissues Nutritional Requirements – 20% of O 2 consumption while only composing 2% of total body weight
Continuity of Central & Peripheral Nerves The system is considered continuous in three ways: 1) the connective tissues are continuous 2) the neurons are interconnected electrically 3) the system is continuous chemically. Any stresses that are imposed on the peripheral nervous system are conveyed to the central nervous system, and the reverse holds true.
Nerve Innervation The connective tissues of the peripheral nerves, nerve roots and autonomic nervous system have a source of intrinsic innervation = nervi nervorum Free nerve endings have been found in the: 1. 2. 3. Perineurium Epineurium Endoneurium
MOI’s & Examination of the Peripheral Nerve
Dysfunctions of Peripheral Nerves • • Motor Problems – motor neuron (body, axon, motor end plate, muscle fiber). Signs: • • distal weakness decreased DTR’s myotomal patterns Sensory Problems – sensory neuron (cell body in ganglion, axon, sensory receptor). Reports: tingling, burning, dysesthesias, paresthesias; dermatome pattern. Mixed Nerves – both ANS – sweating and/or vascular control; skin changes
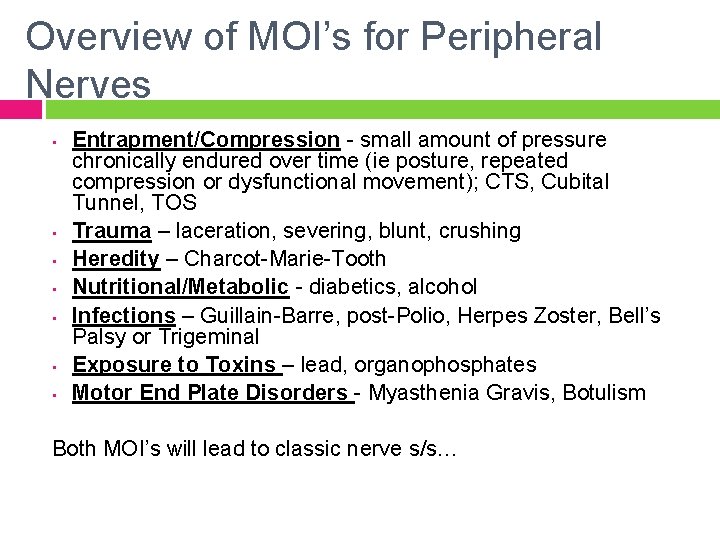
Overview of MOI’s for Peripheral Nerves • • Entrapment/Compression - small amount of pressure chronically endured over time (ie posture, repeated compression or dysfunctional movement); CTS, Cubital Tunnel, TOS Trauma – laceration, severing, blunt, crushing Heredity – Charcot-Marie-Tooth Nutritional/Metabolic - diabetics, alcohol Infections – Guillain-Barre, post-Polio, Herpes Zoster, Bell’s Palsy or Trigeminal Exposure to Toxins – lead, organophosphates Motor End Plate Disorders - Myasthenia Gravis, Botulism Both MOI’s will lead to classic nerve s/s…
Systemic Risk Factors Create an “at risk” environment for the neural tissue. Be mindful of theses conditions, and whether they are under control…
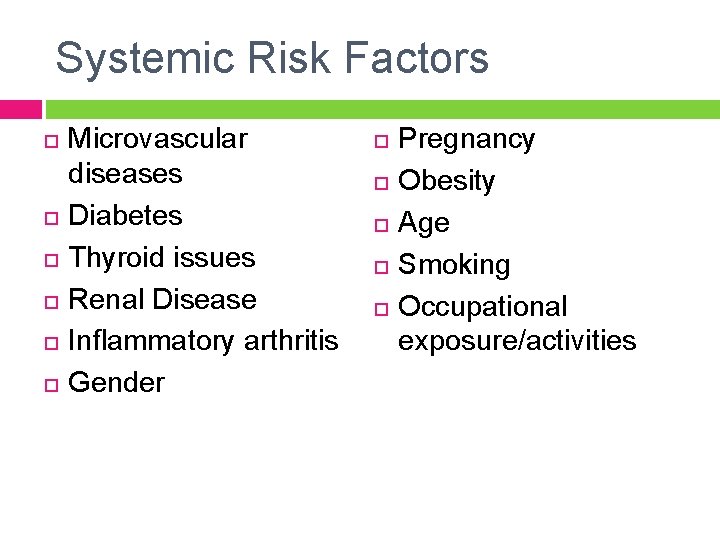
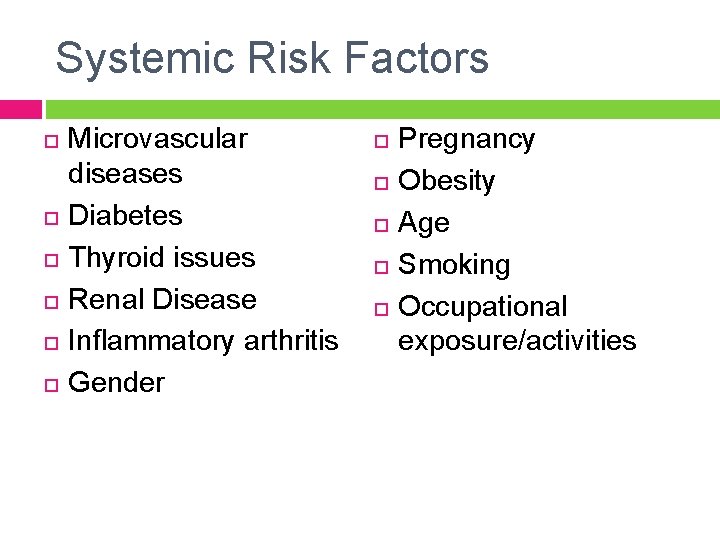
Systemic Risk Factors Microvascular diseases Diabetes Thyroid issues Renal Disease Inflammatory arthritis Gender Pregnancy Obesity Age Smoking Occupational exposure/activities
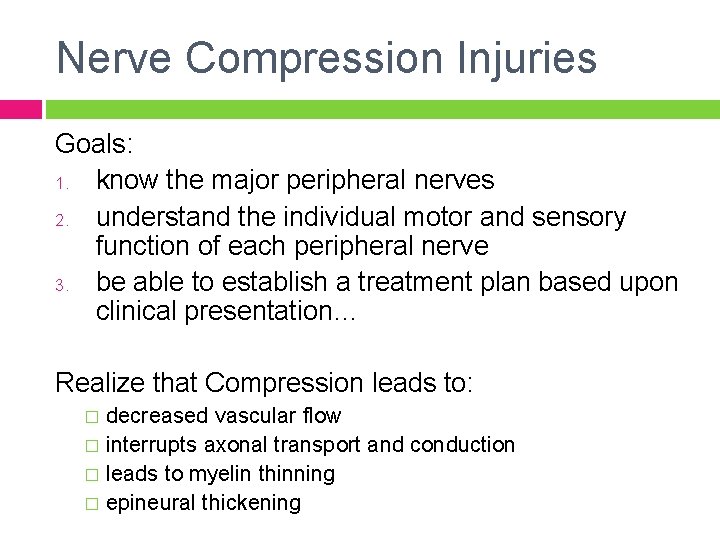
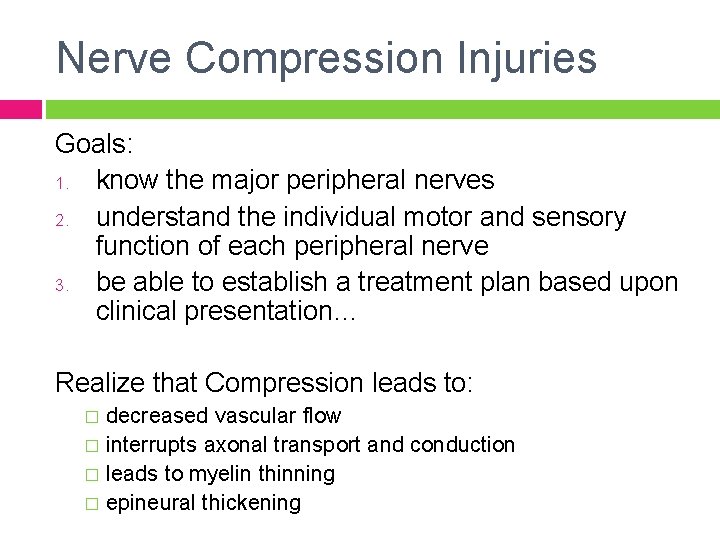
Nerve Compression Injuries Goals: 1. know the major peripheral nerves 2. understand the individual motor and sensory function of each peripheral nerve 3. be able to establish a treatment plan based upon clinical presentation… Realize that Compression leads to: decreased vascular flow � interrupts axonal transport and conduction � leads to myelin thinning � epineural thickening �
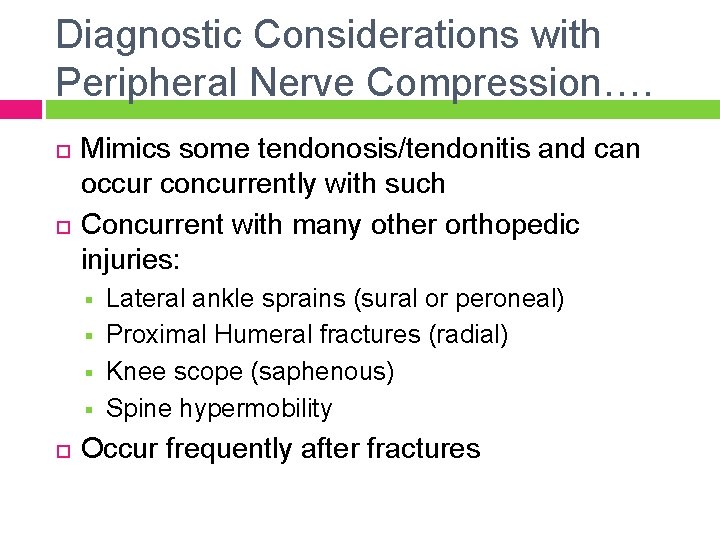
Diagnostic Considerations with Peripheral Nerve Compression…. Mimics some tendonosis/tendonitis and can occur concurrently with such Concurrent with many other orthopedic injuries: § § Lateral ankle sprains (sural or peroneal) Proximal Humeral fractures (radial) Knee scope (saphenous) Spine hypermobility Occur frequently after fractures
Examination Considerations Pt. Hx, physical exam and laboratory data assist in diagnosis and locating lesion. However, no one test is 100% specific or sensitive (so look at multiple pieces of the puzzle…)
Nerve Compression Diagnostic Procedures Pt. History Motor Exam – myotomal as well as specific to suspected peripheral nerve Sensory Exam – dermatomal as well as specific peripheral nerve NTPT (neural tissue provocation testing) Provocative Testing (ie Tinel’s, Phalen’s, Roo’s) Physical findings - atrophy, clawing, etc. Body diagrams EMG/NCV studies
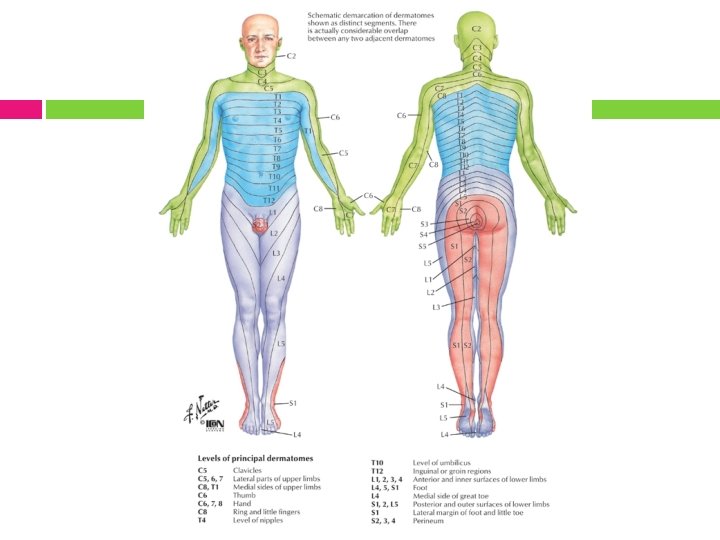

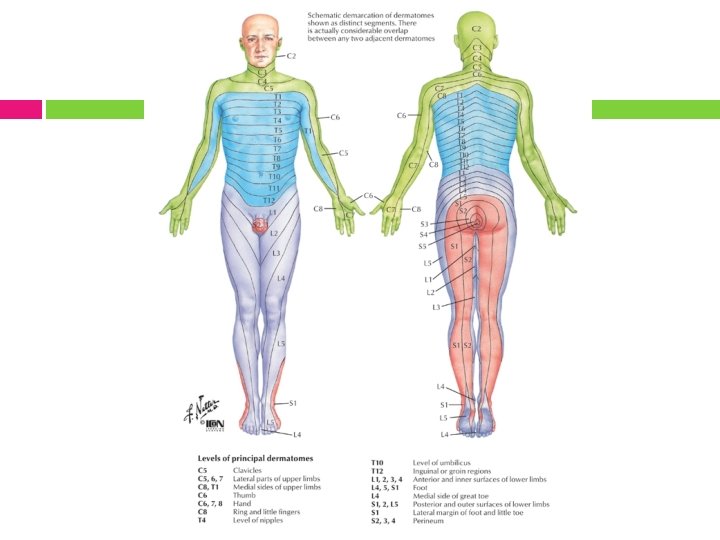
Dermatomal Key Points
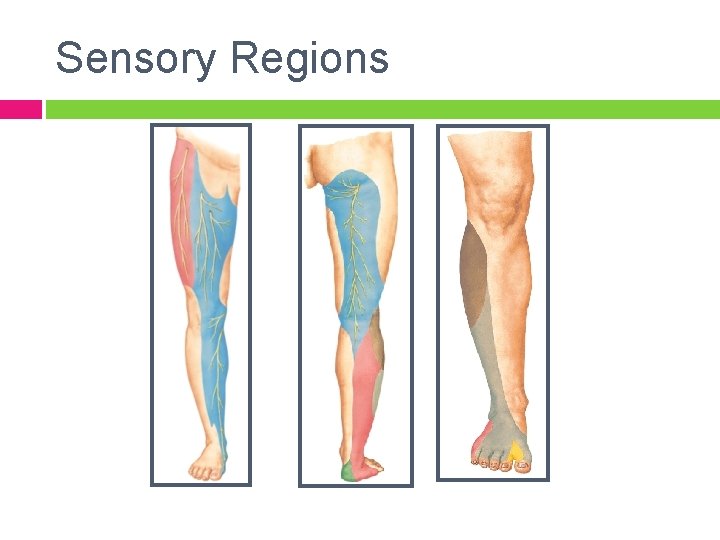
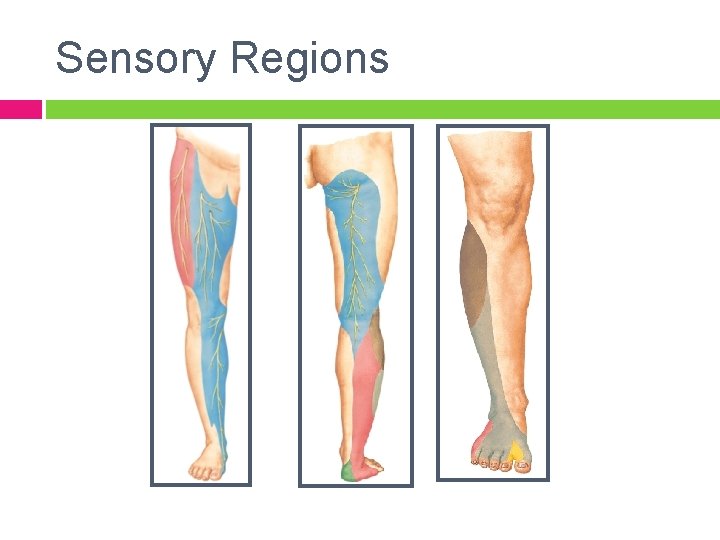
Sensory Regions
Examination Note: Always consider proximal points of compression…. Be mindful that initial changes may be transient, but if situation persists or worsen, the changes can become permanent with fibrosis. Localization and correct diagnosis allow for appropriate intervention planning. Based on peripheral nerve anatomical organization, which is affected first - motor or sensory?
Sidenote on EMG/NCV Sometimes the only objective measure Can localize lesion by “inching” Not always positive in early stages Operator dependent Assists in diagnosis and allows measurement of progression/resolution
Adverse Neural Tissue Tension Never-ending Acronyms: ANTT = Adverse Neural Tissue Tension ULTT = Upper Limb Tension Testing NTPT = Neural Tissue Provocation Testing
Important Concepts Initially may not suspect ANTT with straight forward orthopedic conditions tend to develop gradually as a secondary result from injury The nerve as a source of pain Concept of AIG = abnormal impulse generating site
AIG’s Coined by David Butler When a peripheral nerve is injured, it can develop the ability to repeatedly & spontaneously generate its own impulse
Main Characteristics of AIG’s Mechano-sensitivity: stimulated by mechanical stimuli (movement, touch, etc) Spontaneous Activity Susceptible Sites = area of myelin damage or regenerating axon sprouts
When to suspect ANTT? When not responding as should within the expected time frame Describes in terms consistent with ANTT “burning”, “crawling”, “electrical”, “ants on me”, “pulling”, bizarre sounding things like “warm water” Worsening despite objective improvement of ROM, strength, etc
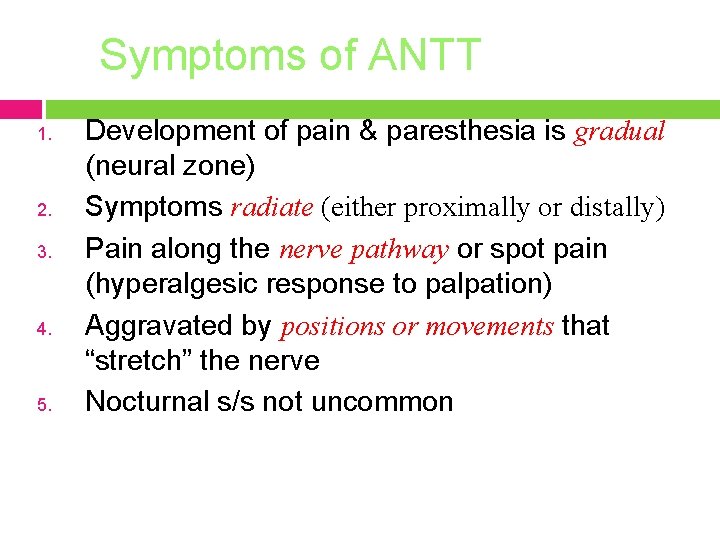
Symptoms of ANTT 1. 2. 3. 4. 5. Development of pain & paresthesia is gradual (neural zone) Symptoms radiate (either proximally or distally) Pain along the nerve pathway or spot pain (hyperalgesic response to palpation) Aggravated by positions or movements that “stretch” the nerve Nocturnal s/s not uncommon
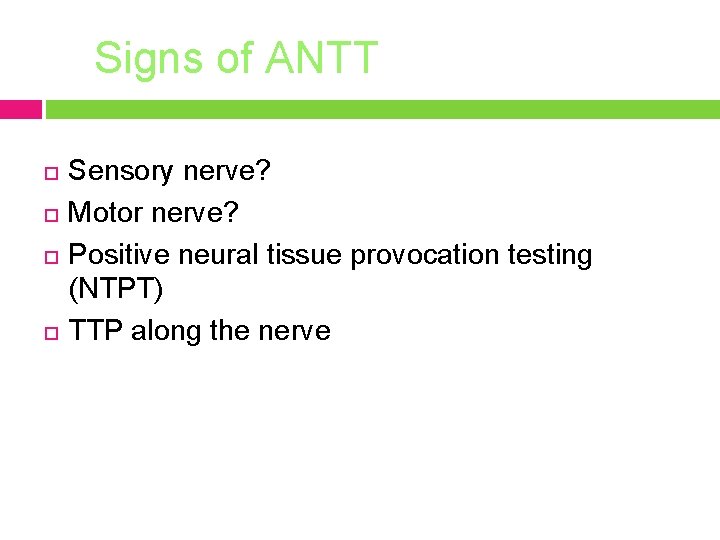
Signs of ANTT Sensory nerve? Motor nerve? Positive neural tissue provocation testing (NTPT) TTP along the nerve
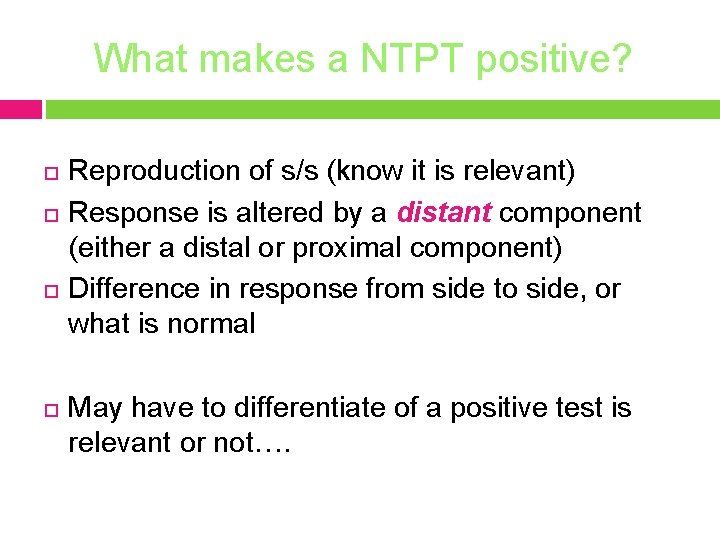
What makes a NTPT positive? Reproduction of s/s (know it is relevant) Response is altered by a distant component (either a distal or proximal component) Difference in response from side to side, or what is normal May have to differentiate of a positive test is relevant or not….
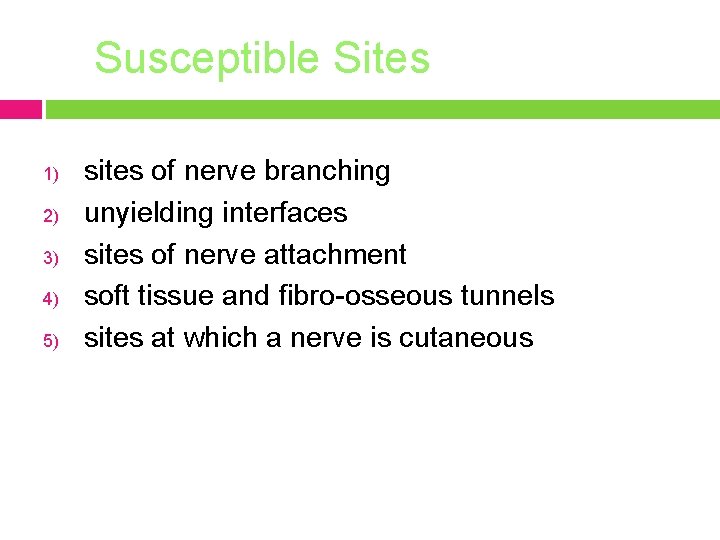
Susceptible Sites 1) 2) 3) 4) 5) sites of nerve branching unyielding interfaces sites of nerve attachment soft tissue and fibro-osseous tunnels sites at which a nerve is cutaneous
Common MOI’s External forces – ie casts, belts, walking boots, ill-fitting shoes Internal forces – ie swelling, bone spur Chronic repeated microtrauma – ie posture Double crush – ie ask about old injuries proximal & distal to site
Double Crush Proteins and cell bodies travel distally while waste products travel proximally thru axonal transport systems. Disruption causes decreased threshold for s/s or AIG’s elsewhere along the nerve. Either site may be asymptomatic without the second insult. What does this tell you must be done on evaluation?
ANTT Differential Diagnosis Lumbar Radiculopathies: Pain with cough, sneeze, Valsalva? Well delineated area of sensory change? Partial weakness, decreased reflexes? Electrodiagnostic testing? What is the key to differential diagnosis of ANTT and lumbar root?
The Key… Identify a different peripheral nerve with the major contribution from the same root level as the suspected nerve Or test a more proximal branch originating from the same peripheral nerve Then compare motor and sensory function

Common LE Entrapments
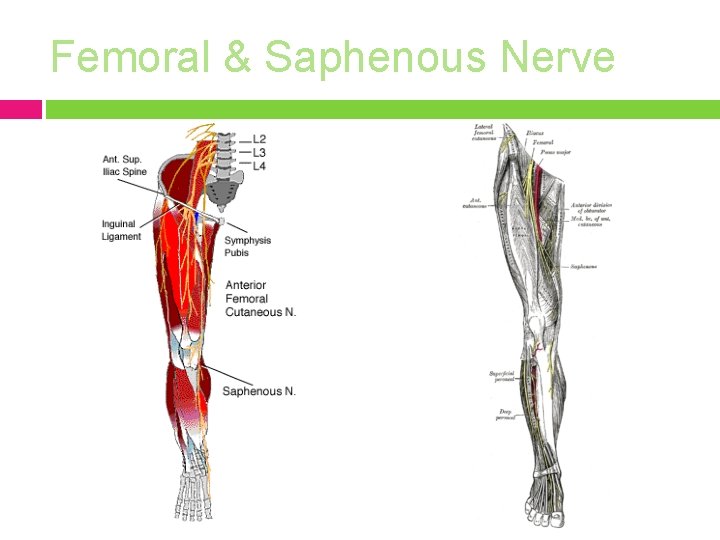
Femoral Nerve MOI: pelvic fracture, scarring after abdominal surgery, tumors, inguinal hernias S/S: most pronounced at the knee, knee buckling may occur Local tenderness in the groin, pain and paresthesiae over the anteromedial surface of the thigh and the medial surface of the leg. Decreased sensation over anteromedial thigh, weakness of quadriceps (compensated for by hyper extending the leg in standing and walking) and sartorius, decreased patellar tendon reflex. Increased pain at endrange hip flexion and hip extension. Positive neural tension signs. Radiculopathy? What level? Will present with anterior tib and adductor weakness. R/O: hip arthritis and psoas strain
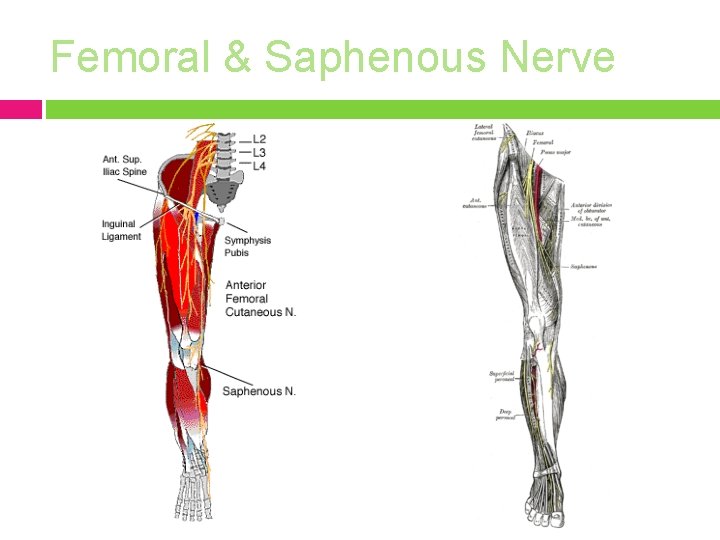
Femoral & Saphenous Nerve
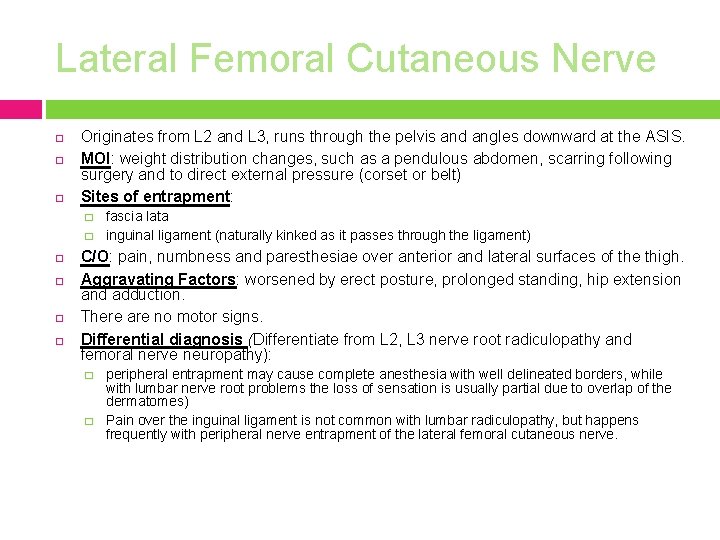
Lateral Femoral Cutaneous Nerve Originates from L 2 and L 3, runs through the pelvis and angles downward at the ASIS. MOI: weight distribution changes, such as a pendulous abdomen, scarring following surgery and to direct external pressure (corset or belt) Sites of entrapment: � � fascia lata inguinal ligament (naturally kinked as it passes through the ligament) C/O: pain, numbness and paresthesiae over anterior and lateral surfaces of the thigh. Aggravating Factors: worsened by erect posture, prolonged standing, hip extension and adduction. There are no motor signs. Differential diagnosis (Differentiate from L 2, L 3 nerve root radiculopathy and femoral nerve neuropathy): � � peripheral entrapment may cause complete anesthesia with well delineated borders, while with lumbar nerve root problems the loss of sensation is usually partial due to overlap of the dermatomes) Pain over the inguinal ligament is not common with lumbar radiculopathy, but happens frequently with peripheral nerve entrapment of the lateral femoral cutaneous nerve.
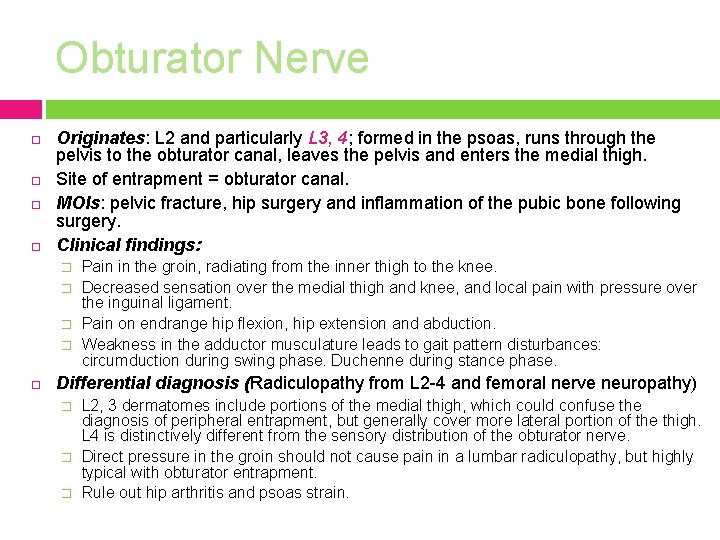
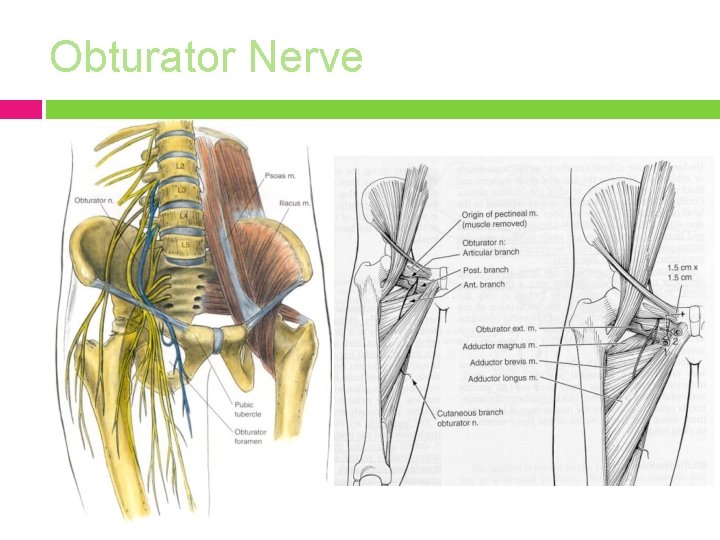
Obturator Nerve Originates: L 2 and particularly L 3, 4; formed in the psoas, runs through the pelvis to the obturator canal, leaves the pelvis and enters the medial thigh. Site of entrapment = obturator canal. MOIs: pelvic fracture, hip surgery and inflammation of the pubic bone following surgery. Clinical findings: � � Pain in the groin, radiating from the inner thigh to the knee. Decreased sensation over the medial thigh and knee, and local pain with pressure over the inguinal ligament. Pain on endrange hip flexion, hip extension and abduction. Weakness in the adductor musculature leads to gait pattern disturbances: circumduction during swing phase. Duchenne during stance phase. Differential diagnosis (Radiculopathy from L 2 -4 and femoral nerve neuropathy) � � � L 2, 3 dermatomes include portions of the medial thigh, which could confuse the diagnosis of peripheral entrapment, but generally cover more lateral portion of the thigh. L 4 is distinctively different from the sensory distribution of the obturator nerve. Direct pressure in the groin should not cause pain in a lumbar radiculopathy, but highly typical with obturator entrapment. Rule out hip arthritis and psoas strain.
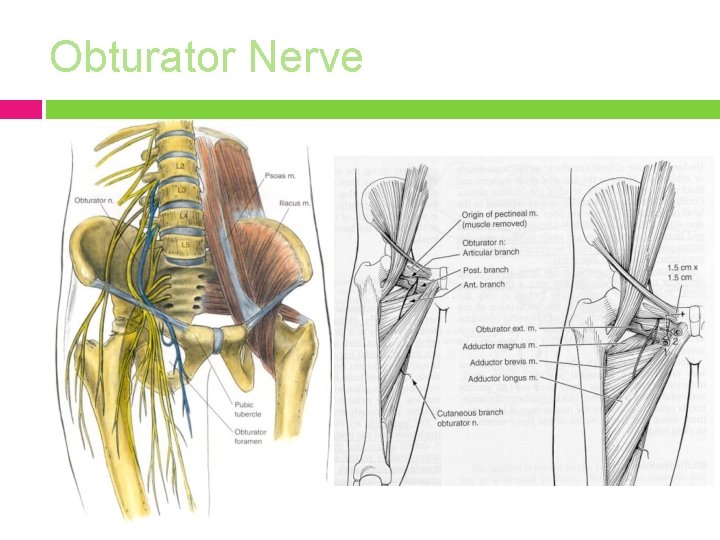
Obturator Nerve
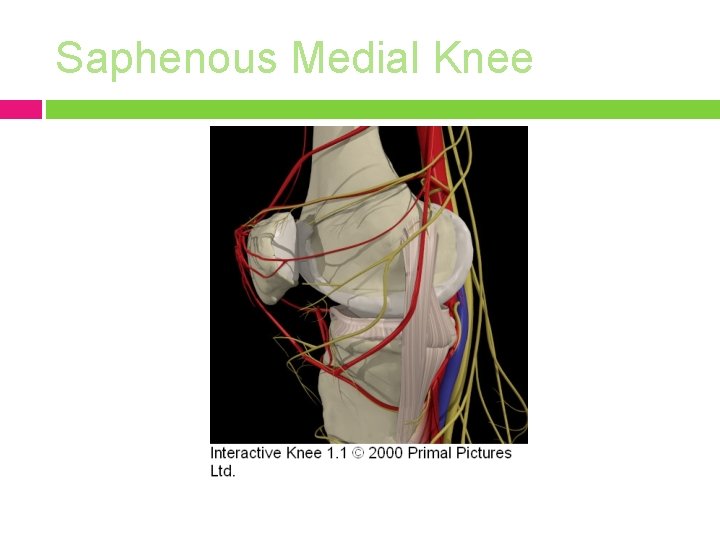
Saphenous MOI: knee arthroscopy, medial meniscal repair, trauma
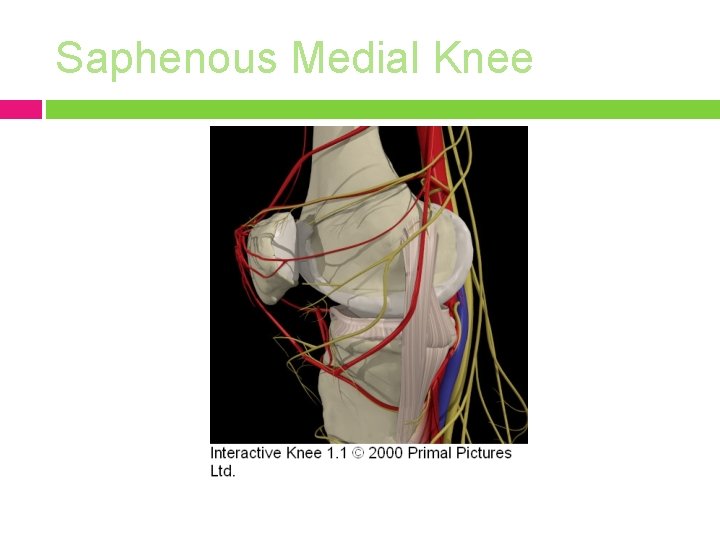
Saphenous Medial Knee
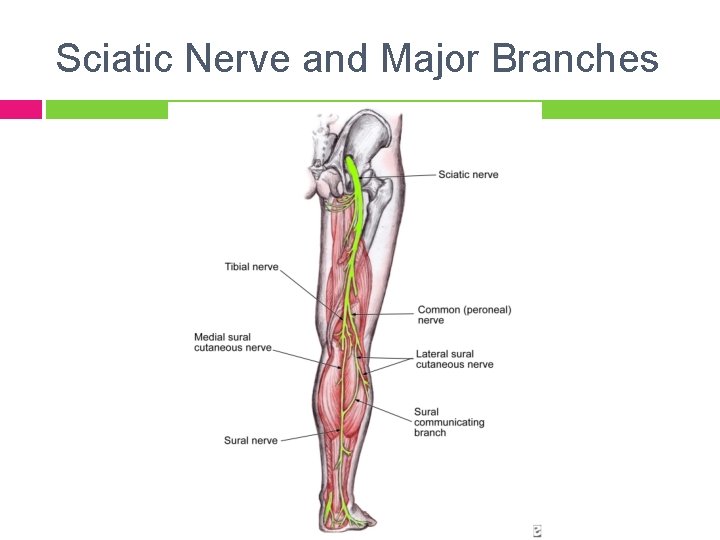
Sciatic MOI: sacral dysfunction with piriformis spasm, thick wallets, scarring from hip surgery, injections, gluteal or pelvic tumors Key: glutei help differential from radiculopathy Caution: Neurodynamic testing will give the same result as for radiculopathy
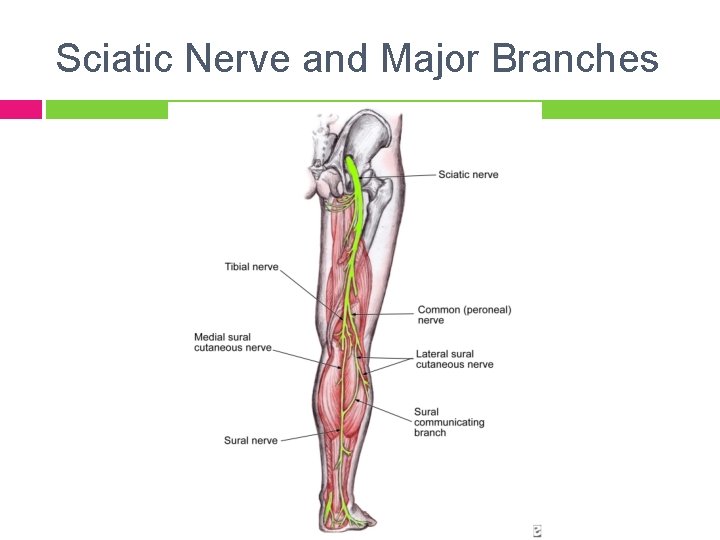
Sciatic Nerve and Major Branches
LE Nerves Commonly Involved Tibial: MOI: plantar fascitis, eversion sprains, “joggers” foot
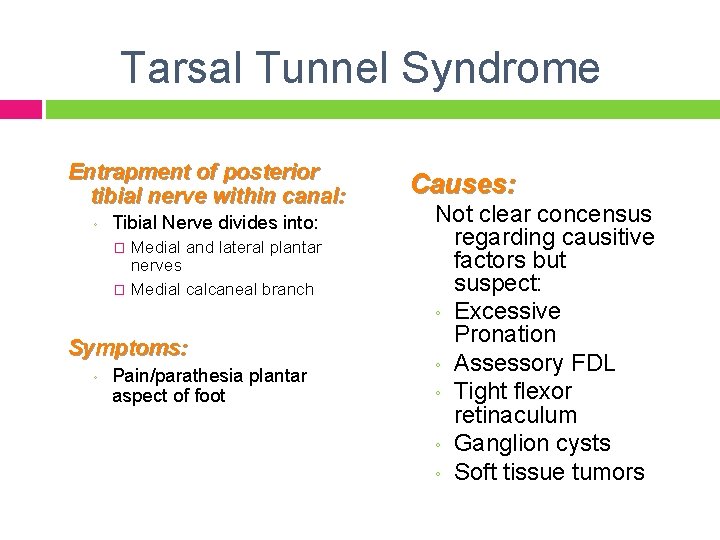
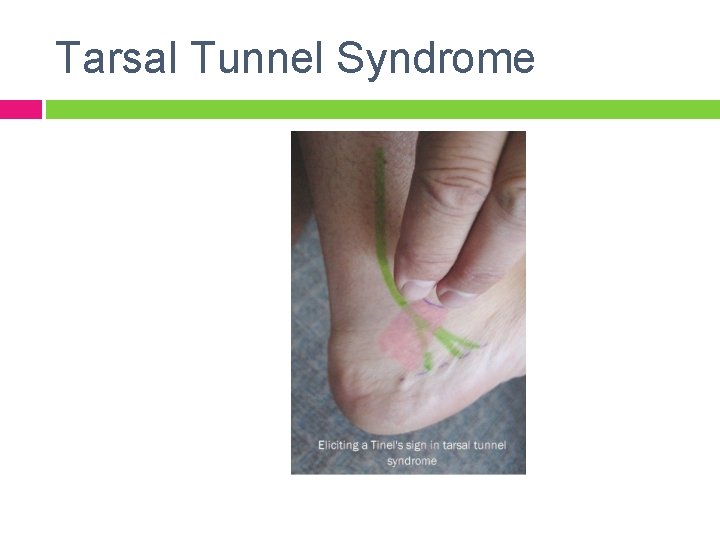
Tarsal Tunnel Syndrome Entrapment of posterior tibial nerve within canal: ◦ Tibial Nerve divides into: Medial and lateral plantar nerves � Medial calcaneal branch � Symptoms: ◦ Pain/parathesia plantar aspect of foot Causes: Not clear concensus regarding causitive factors but suspect: ◦ Excessive Pronation ◦ Assessory FDL ◦ Tight flexor retinaculum ◦ Ganglion cysts ◦ Soft tissue tumors
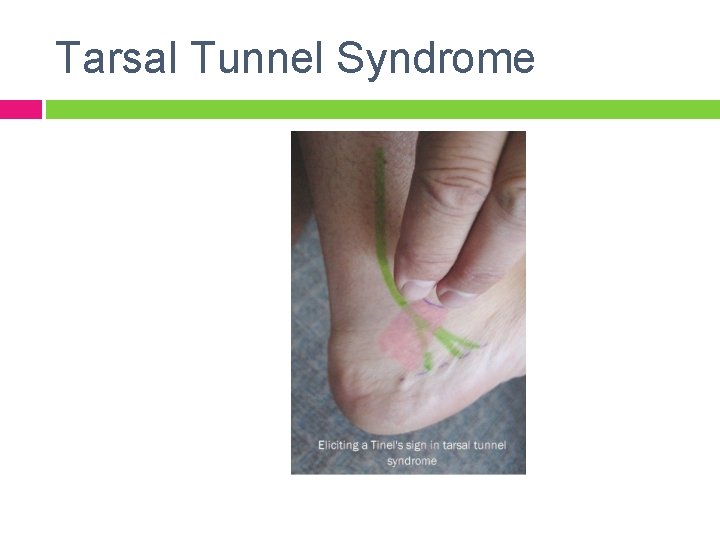
Tarsal Tunnel Syndrome
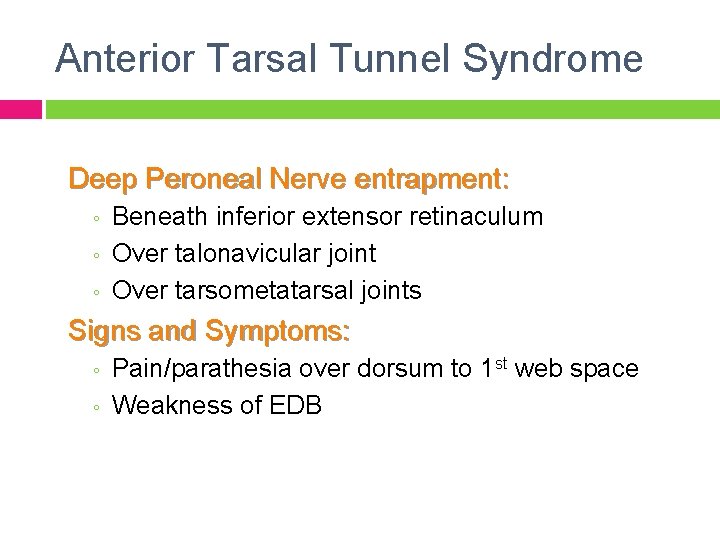
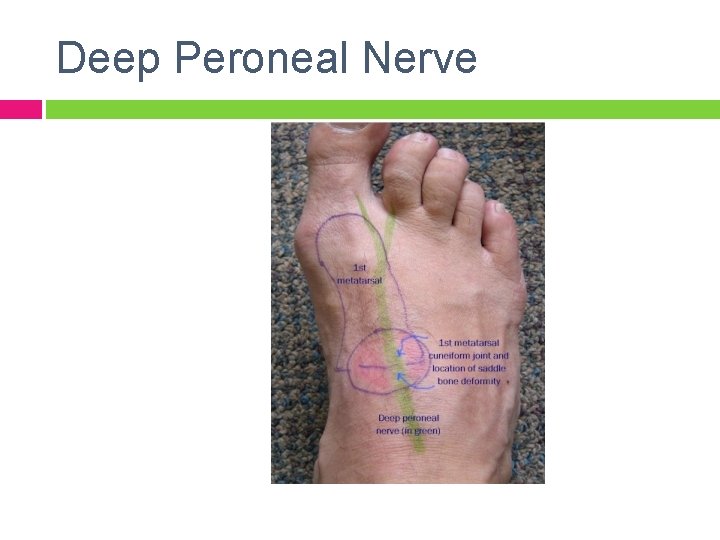
Anterior Tarsal Tunnel Syndrome Deep Peroneal Nerve entrapment: ◦ ◦ ◦ Beneath inferior extensor retinaculum Over talonavicular joint Over tarsometatarsal joints Signs and Symptoms: ◦ ◦ Pain/parathesia over dorsum to 1 st web space Weakness of EDB
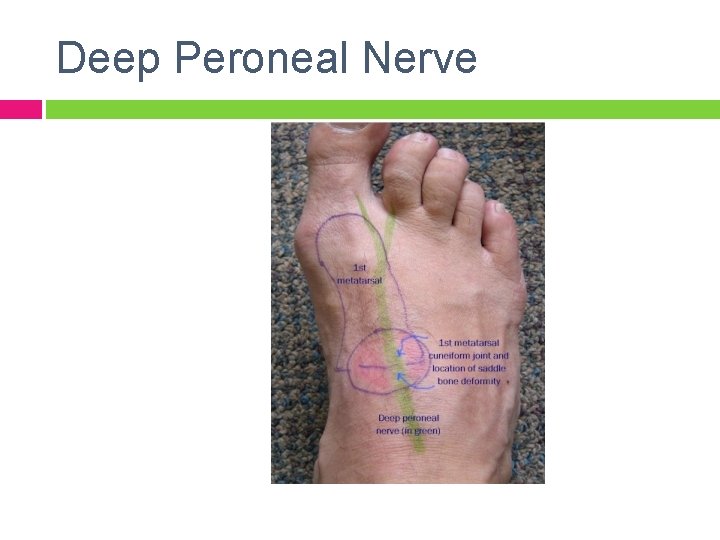
Deep Peroneal Nerve
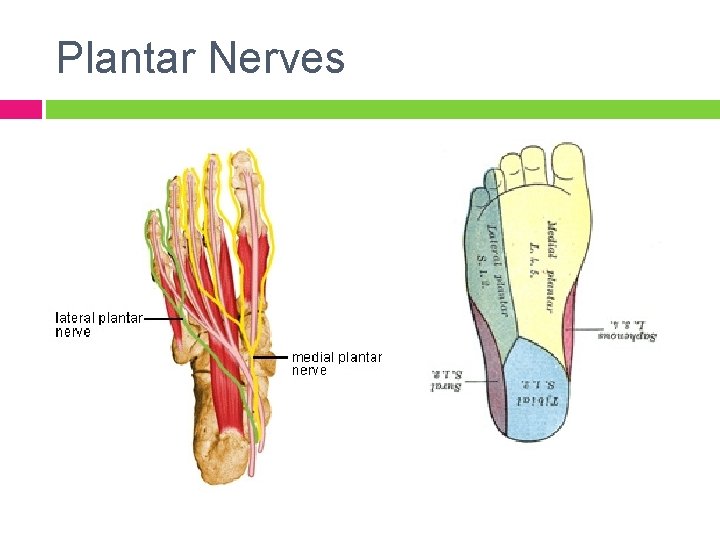
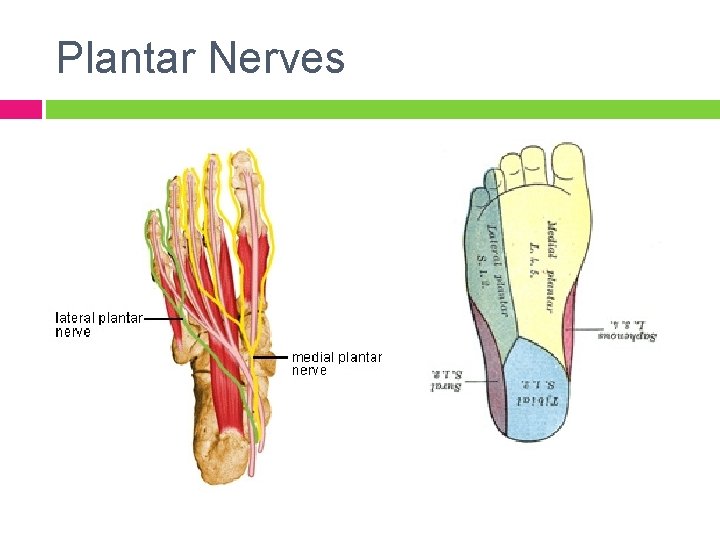
Plantar Nerves
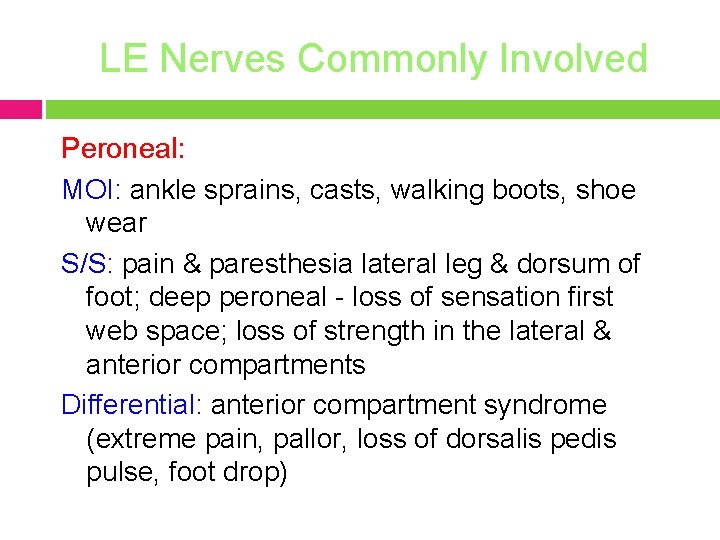
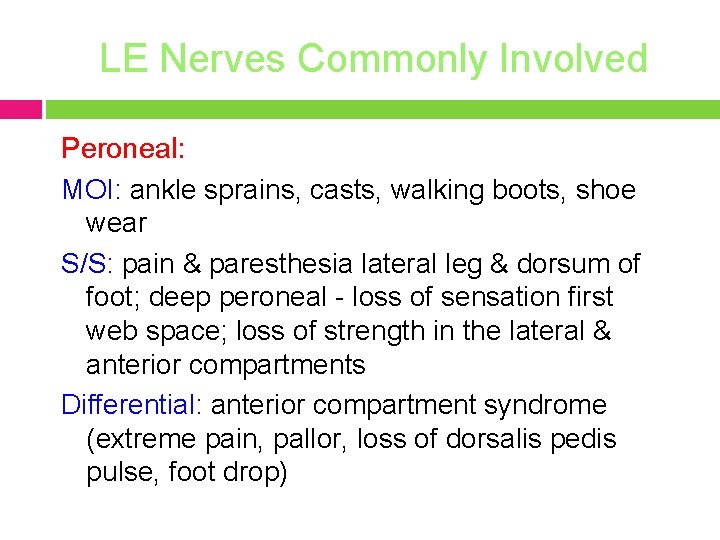
LE Nerves Commonly Involved Peroneal: MOI: ankle sprains, casts, walking boots, shoe wear S/S: pain & paresthesia lateral leg & dorsum of foot; deep peroneal - loss of sensation first web space; loss of strength in the lateral & anterior compartments Differential: anterior compartment syndrome (extreme pain, pallor, loss of dorsalis pedis pulse, foot drop)


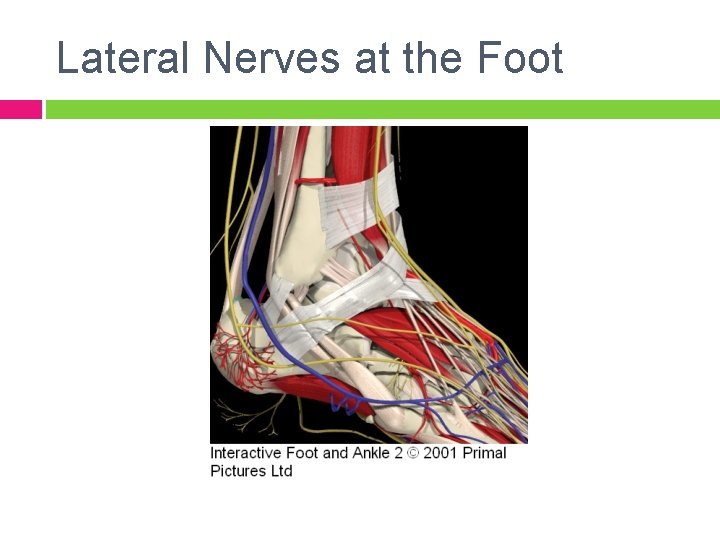
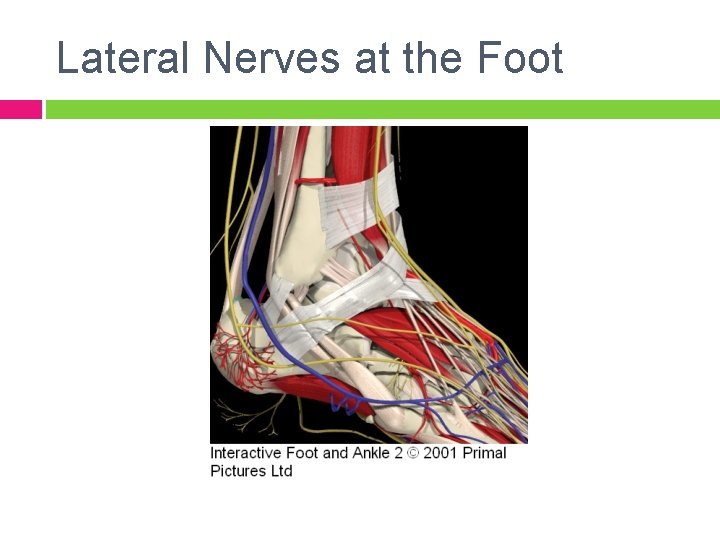
Lateral Nerves at the Foot
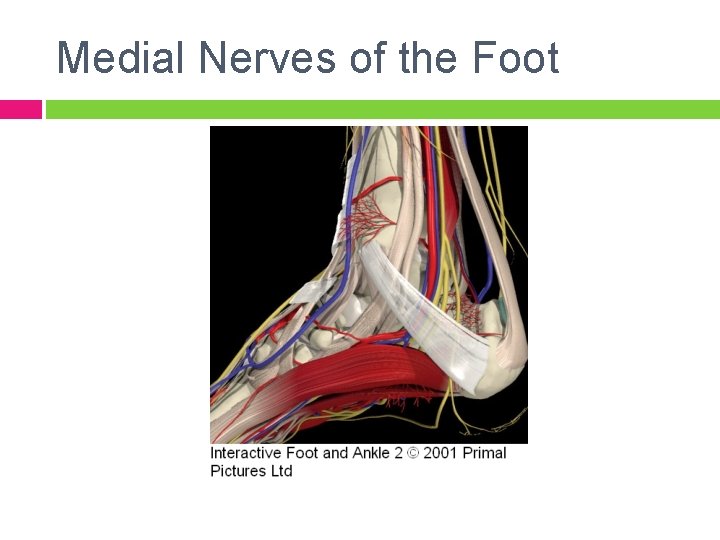
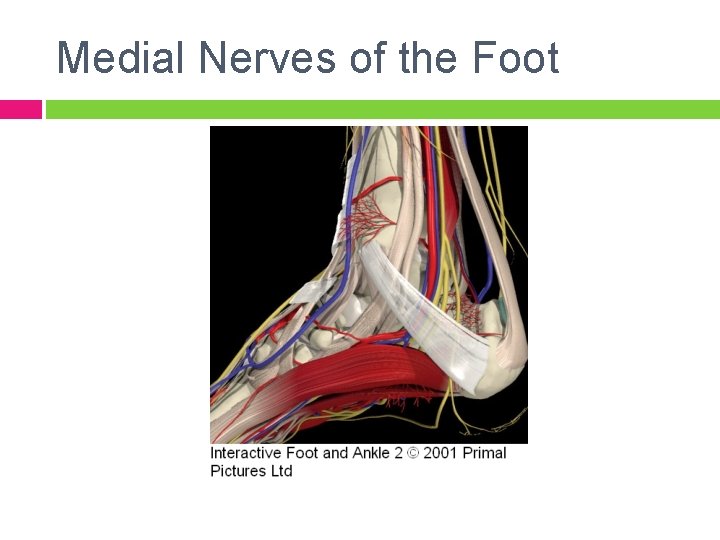
Medial Nerves of the Foot
Adverse Neural Tissue Tensioning Provocative Testing Positive: 1. 2. 3. Different from uninvolved LE Reproduction of s/s Changes with “remote” component Caution! Assessment of irritability is key, as well as severity. Irritability guides the nerve glide prescription related to intensity…
Principles of Management of ANTT Intensity directly related to the level of irritability present – greater the irritability the less intense the glide (ie NOT into s/s) Neurological s/s (ie tingling, numbness) should NOT persist after gliding technique or should be improved Choose one component motion of the testing position to utilize as the “gliding force” Either “floss” or “glide” – either one works Ask regarding s/s after each treatment and document changes across the course of treatment Any worsening at all need to be immediately reported to the PT – pt. education…

Guidelines for Prescription Educate pt on condition and goals of treatment Emphasize NOT to push treatment – MUST be gentle ALWAYS start with assisting to ensure perfect form and determine response; when pt masters, give nerve glides as HEP. 1. Intensity & Duration: § § Initially: Perform 20 -30 glides just out of s/s Progress to: glides with minimum s/s at the end of the “glide” only 2. Frequency: § § Initially: 1 x day, determine response Progress to: Gradually build up to 3 x-5 x day if appropriate response achieved.
 Spin coat
Spin coat Transference meaning in psychology
Transference meaning in psychology Interfacial tension vs surface tension
Interfacial tension vs surface tension Connective tissue
Connective tissue Psychodynamic and humanistic therapies have in common
Psychodynamic and humanistic therapies have in common Bioness integrated therapy system occupational therapy
Bioness integrated therapy system occupational therapy Humanistic therapies aim to boost
Humanistic therapies aim to boost Perforation plates
Perforation plates American institute for cognitive therapy
American institute for cognitive therapy Fraunhofer institute for cell therapy and immunology
Fraunhofer institute for cell therapy and immunology Feminist therapy institute
Feminist therapy institute Manual circumlaryngeal techniques
Manual circumlaryngeal techniques Mst analytical process
Mst analytical process History of manual therapy
History of manual therapy Functional manual therapy
Functional manual therapy Intramuscular manual therapy
Intramuscular manual therapy Aps therapy user manual
Aps therapy user manual Labelling in tissue processing
Labelling in tissue processing Aip style manual
Aip style manual Adverse reaction definition
Adverse reaction definition Near miss examples ppt
Near miss examples ppt Adverse selection
Adverse selection Adverse selection
Adverse selection Adverse reaction definition
Adverse reaction definition Adverse reaction definition
Adverse reaction definition Adverse events in hospital
Adverse events in hospital Ir adverse event
Ir adverse event Puerperal sepsis
Puerperal sepsis What is adverse selection
What is adverse selection Effects of paracetamol
Effects of paracetamol Loop diuretics adverse effects
Loop diuretics adverse effects Paracetamol adverse effects
Paracetamol adverse effects Dpp-4 inhibitors side effects
Dpp-4 inhibitors side effects Adverse selection
Adverse selection Adr adverse drug reaction
Adr adverse drug reaction Furosemide side effects
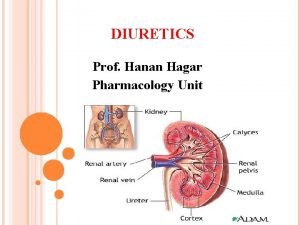
Furosemide side effects Classification of diuretics
Classification of diuretics Hayanil tab
Hayanil tab Adverse treatment
Adverse treatment To give yourself more time for the ipde process at night,
To give yourself more time for the ipde process at night, Driving in adverse conditions
Driving in adverse conditions Adverse selection
Adverse selection Adverse event adalah
Adverse event adalah Teratogenic drugs mnemonic
Teratogenic drugs mnemonic Beta blocker examples
Beta blocker examples Beta blocker moa
Beta blocker moa Alpha blockers classification
Alpha blockers classification Adverse effect of alpha blockers
Adverse effect of alpha blockers Adverse childhood experiences study
Adverse childhood experiences study Adverse yaw
Adverse yaw Adverse childhood experiences study
Adverse childhood experiences study Adverse event
Adverse event Novartis adverse event reporting
Novartis adverse event reporting Mhmr of tarrant county
Mhmr of tarrant county Adverse
Adverse Adverse yaw
Adverse yaw Unanticipated problem vs adverse event
Unanticipated problem vs adverse event Adverse event crf
Adverse event crf Schoolsworkpro
Schoolsworkpro Slidetodoc.com
Slidetodoc.com Adverse selection
Adverse selection