UTILIZING STANDARDIZED ASSESSMENTS TO INFORM THE SERVICE PLANNING


































































- Slides: 66

UTILIZING STANDARDIZED ASSESSMENTS TO INFORM THE SERVICE PLANNING PROCESS: PART 1 - inter. RAI

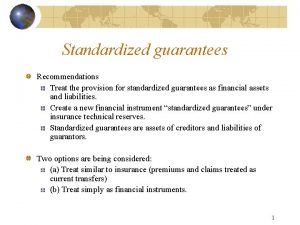
BACKGROUND • inter. RAI has developed Clinical Assessment Protocols (CAPs) for use with their assessment instruments. • This presentation is an introduction to using the assessment results as a guide for development of a service plan with the individual being assessed. It will not cover CAPs intended for inpatient settings only. • We won’t go through all the slides during the presentation. The slides provide a high-level summary of the CAPs, which are detailed in manuals available from inter. RAI. • More information can be found at www. inter. RAI. org, including the purchase of the manuals, both electronic and print versions.

• CAPs were developed as part of a multiyear, international collaborative research • • • effort based on best practice guidelines and extensive analyses of inter. RAI assessment results. CAPs are triggered for at least two types of individuals: • Those likely to experience improvements in a particular domain with appropriate support • Those at elevated risk of further setbacks if action is not taken Decision-making should be collaborative and inclusive of the individual’s perspective and should aim to enhance the individual’s quality of life and independence as fully as possible. Use the team process to identify priorities for goals of care. An individual’s priorities may be identified through a CAP or through other means. The CAPs aim to link the assessment findings to interventions, services, and support strategies that have been demonstrated to be effective.

TRIGGERS BASED ON MH SCALES AND ALGORITHMS • Items on the inter. RAI assessments have been organized into various • • scales. Some of the CAPs are triggered by how an individual’s results score on these scales. Some scales are straight-forward and easy to calculate. Some algorithms are complex and use a variety of scales. IACP has developed a spreadsheet for each inter. RAI (CMH and Ch. YMH) that helps in calculating the scale and algorithm results and identifying triggers for individuals being assessed.

ENTER SCORES FOR IDENTIFIED ITEMS (SAMPLE) Item C 1 a C 1 b C 1 d C 1 g C 1 h C 1 l C 1 aa C 1 cc C 1 ff C 2 C 3 D 5 a D 5 b H 1 a H 2 e I 1 Score Notes Record the Capacity score Do not enter if score is "8"

RESULTS (EXAMPLES) Scale Aggressive Behavior Scale ADL Heirarchy Anhedonia CAGE Cognitive Performance Scale Communication Depression Rating Scale Depression Severity Index IADL Capacity Scale Mania Pain Positive Symptoms Scale (short) Positive Symptoms Scale (long) Risk of Harm to Others Self-Care Index Severity of Self-harm Score Interpretation of Score 0 No signs of aggression 0 No Anhedonia 0 0 No communication issues 0 No depression 0 High capacity for independent functioning 0 Infrequent or no signs of mania 0 No pain 0 No positive symptoms

COMPONENTS OF EACH CAP • • • Issue Statement Goals of Care CAP Triggers CAP Guidelines Additional Resources

ISSUES COVERED BY inter. RAI CMH CAPs Safety Social Life Economic Issues Autonomy Health Promotion

SAFETY CAPs HARM TO OTHERS CAP SUICIDALITY AND PURPOSEFUL SELF-HARM CAP SELF-CARE CAP

HARM TO OTHERS CAP • Issue: Violent or aggressive behavior may be associated with biological, psychological, social, and environmental risk factors. Key issue is difficulty regulating or coping with emotions like anger, impulsivity, fear, or distress. • Goals of Care: Ensure safety; prevent escalation or reoccurrence; ID factors that contribute; ID interventions; implement therapeutic interventions; reduce future risk; prevent institutionalization or criminal justice involvement; promote safe community integration. • Triggers: High Risk – RHO Scale 5 or 6; Moderate Risk – RHO Scale 3 or 4 OR violent indications in last 7 days; No Trigger – RHO Scale 0 -2 and no violent indications in last 7 days. • Guidelines: Consider acuity, nature of harm, and contributing factors; 2 stages of intervention – respond to immediate incidents and guidelines for prevention; manual has specific suggestions for interventions. • Additional Resources: 3 articles published 2003 -2006

SUICIDALITY AND PURPOSEFUL SELF-HARM CAP • Issue: Intentional behavior aimed at ending one’s life or not; often treated with equal importance despite the intended outcome, but treatment options may differ. Risk factors for suicide are identified in manual. • Goals of Care: Attend to immediate safety needs; approach nonjudgmentally; assess risk for suicide; ID contributing factors; ID and implement interventions; reduce risk of repeated attempts; support recovery; support family and others. • • Triggers: High Risk – So. S Scale 5 or 6; Moderate Risk – So. S Scale 4; No Trigger – So. S Scale 0 -3 • Additional Resources: 3 articles 2003 -2008 Guidelines: Address safety issues; ascertain history of attempts; determine plan/preparations for suicide; presences of mood disorders; role of family and other informal supports; document level of risk and plans for treatment/prevention; interventions.

SELF-CARE CAP • Issue: Ability to carry out Activities of Daily Living (ADLs) and Independent Activities of Daily Living (IADLs), as well as self-directed treatment-related activities. Balance optimizing self-determination with responsibility to protect from harm. • Goals of Care: Ensure safety from harm; alleviate MH symptoms; provide support and care for basic functioning; promote independence in self-care; build on strengths and ID emerging opportunities; ID and address underlying barriers to recovery of self-care. • • Triggers: High Risk – SCI Scale 6; Moderate Risk – SCI Scale 2 -5; No Trigger –SCI Scale 0 -1. • Additional Resources: 3 publications 1997 -2008 Guidelines: ID and assist with ADL/IADL difficulties; build on strengths and engage informal support network; address any living environment issues; address any legal justice system contact.

SOCIAL LIFE CAPs SOCIAL RELATIONSHIPS CAP INFORMAL SUPPORT CAP INTERPERSONAL CONFLICT CAP TRAUMATIC LIFE EVENTS CAP CRIMINAL ACTIVITY CAP

SOCIAL RELATIONSHIPS CAP • Issue: Engagement in social relationships is both a dimension of recovery and a predictor of outcomes. This CAP aims to address factors leading to disruption in social relationships that may result in isolation. It points to shared experiences of the individual, the informal network, and the community. • Goals of Care: ID and address symptoms that isolate; ID and respond to causes of difficulties; strengthen social skills; provide opportunities to experience safe and supportive interactions; support meaningful social connections; reduce impact of adverse experiences, foster community integration. • Triggers: See scoring spreadsheet: Reduce Social Isolation and Family Dysfunction; Improve Close Friendships and Family Functioning; No Trigger • Guidelines: Readiness to change and self-efficacy; understanding possibilities; history of substance abuse; physical health affecting participation level; communication and problemsolving skills; any abusive relationships; problematic former relationships; role of external factors; awareness of community supports; family education; therapy programs. • Additional Resources: 5 publications 1995 - 2006

INFORMAL CAP • Issue: An informal social. SUPPORT support network may provide a buffer against adverse life events and stressful living conditions, and may contribute to a person’s overall sense of well-being. Increasing informal supports may reduce loneliness and social isolation, improve psychosocial functioning, and reduce MH symptoms. • Goals of Care: ID and link with informal supports; mobilize formal resources when no informal supports; stabilize and increase informal supports; rebuild or strengthen family and friendship relationships, where appropriate; enhance sense of well-being, belonging, and overall quality of life. • Triggers: See scoring spreadsheet: Address Need for Functional Support Related to Physical Disability or Cognitive Impairment; Address Need for Support Related to Mental Health Symptoms; No Trigger • Guidelines: Social skills training; ID and address potential barriers to informal support; address conflict or dysfunction in the social network; enhance informal network; change attitudes or beliefs; incorporate family or friends into treatment; consider family interventions • Additional Resources: 2 publications 2000 - 2006

INTERPERSONAL CONFLICT CAP • Issue: The focus of this CAP is to address interpersonal relationships that have, or have the potential for, anger issues related to interpersonal conflict. • Goals of Care: Prevent escalation of the conflict; reduce intensity and number of individuals involved; ID and alleviate underlying causes; ID patterns of emotional responses; develop coping strategies and interpersonal social skills. • Triggers: See scoring spreadsheet: Reduce Widespread Conflict; Reduce Conflict Within Specific Relationships; No Trigger • Guidelines: Determine nature of interpersonal conflict; ID factors that may be contributing to the conflict; assess the potential that the hostility may intensify to ensure safety of the individual and others; address the concern with the individual; pharmacological treatment; skills training; cognitive impairment; substance use; physical symptoms; role of family; personality traits. • Additional Resources: 4 publications 1993 - 2005

TRAUMATIC LIFE EVENTS CAP • Issue: Most people who experience a traumatic life event recover without serious problems. Some develop acute stress disorder (lasting 2 -4 weeks) or post-traumatic stress disorder (lasting 3 -6 months or becoming chronic). • Goals of Care: Ensure safe and secure environment; reduce crisis-related symptoms; treat co-morbid disorders; address underlying symptoms; support healthy self-care; increase individual’s understanding of feelings; prevent or reduce trauma-related conditions; protect against relapse and prevent future abuse; restore family relationships where appropriate. • • Triggers: Address Immediate Safety Concerns; Reduce Impact of Prior Events; No Trigger • Additional Resources: 8 publications 2004 - 2008 Guidelines: Obtain historical information; safety; emotional numbing; hypervigilance; comorbid disorders; aggressive behaviors; military exposure; specific therapeutic interventions; target trauma-related symptom reduction as the major clinical outcome

CRIMINAL ACTIVITY CAP • Issue: If present, it’s important to consider safety and security, proceedings or restrictions that may be in effect, and the effect of criminal activity on treatment/recovery. Often is related to troubled relationships, abuse, victimization, unemployment, insecure housing, and poverty. Recovery plan focus is on preventing further involvement. • Goals of Care: Ensure safety and security; address MH symptoms; address criminogenic needs; minimize the risk of involvement in criminal activity. • • Triggers: Reduce Risk of Violent or Nonviolent Criminal Behavior; No Trigger • Additional Resources: 5 publication 1998 - 2006 Guidelines: Conduct further evaluation regarding the nature of the activity, its origins, and risks to others; monitor and control as needed; evaluate and treat MH symptoms; evaluate and intervene predisposition to ongoing criminal involvement; minimize risk of involvement in future criminal activity.

ECONOMIC ISSUES CAPs PERSONAL FINANCES CAP EDUCATION AND EMPLOYMENT CAP

PERSONAL FINANCES CAP • Issue: Economic hardship may result from a point-in-time loss of income or may be a persistent problem. May be related to unemployment, substance abuse, gambling, or exploitation by family. Severe cognitive impairment may affect ability to manage finances. May lead to unstable or unsafe housing, inadequate nutrition, depression, and reduced social participation. • Goals of Care: ID barriers to income security; establish short-term support as needed; assist in securing an income and stable housing; ensure that property and finances are secure from abuse; ensure any problems related to substance use or gambling are addressed. • • Triggers: Economic Hardship; Inability to Manage Finances; No Trigger • Additional Resources: 6 publications 1994 - 2007 Guidelines: Ensure safety and security; ID causes of and address consequences of financial issues; income; employment; housing and living arrangements; nutritional status; substance use; health conditions, problem gambling; support sound financial decision-making; ID any financial abuse.

EDUCATION EMPLOYMENT CAP • Issue: This CAP focuses AND on assisting individuals to access, return to, or maintain employment, education, or other meaningful activity as critical steps in recovery, successful rehabilitation, and community integration. Benefits can address emotional, economic, and relational issues. • Goals of Care: ID strengths and preferences; eliminate barriers to meaningful engagement; reduce risks associated with unemployment or dropping out of school; find meaningful involvement; help the individual develop an increased sense of self-esteem and self-worth; broaden the individual’s social network. • Triggers: Reduce the Risk of Unemployment or Dropping Out of School; Support Employment or Educational Participation; No Trigger • Guidelines: Use strengths-based approach to ID skills and characteristics; help ID barriers to achieving vocational goals; determine functional or physical limitations in performance of daily tasks; help ID personal occupational goals; determine readiness for employment and literacy skills; support MH needs; determine services to support the individual; ID any need for education; explore volunteering • Additional Resources: 7 publications 2001 - 2007

AUTONOMY CAPs CONTROL INTERVENTIONS CAP (in-patient only) MEDICATION MANAGEMENT AND ADHERENCE CAP REHOSPITALIZATION CAP

MEDICATION & ADHERENCE CAP • Issue: The primary MGMT concern of this CAP is the clinical benefit derived from the medication and not merely the issue of adherence. Considerations include overall response to the medication; any adverse side effects; therapeutic effectiveness; and the individual’s values, preferences, choices, barriers, and specific functioning levels. • Goals of Care: Stabilize medical and MH concerns; eliminate or reduce concerns about medication; implement a medication regimen that increases likelihood of adherence; support safe use and independent management of medication with assistance as needed; reduce the risk of relapse and hospital admissions. • Triggers: Problems with Medication Management and Adherence Related to Cognitive Deficits and Positive Symptoms; Having Previously Stopped Taking Medication Due to Side Effects; No Trigger • Guidelines: Assess nonadherence for nature, contributing factors, and specific issues; implement interventions that are psycho-affective, educational, behavioral, cognitive, socioenvironmental, or legal. • Additional Resources: 8 publications 2000 - 2008

REHOSPITALIZATION CAP • Issue: Rehospitalization might increase a sense of stigmatization and reduce the individual’s confidence regarding recovery. May result from MH symptoms, lack of informal supports, functional deficits, or poor quality of care. • Goals of Care: Minimize specific MH symptoms; develop and implement a recovery support plan and crisis-management plan; engage in a coordinated and comprehensive MH program; maintain community residence. • Triggers: High Risk – 3+ hospitalizations in 2 years and one additional characteristic; Moderate Risk – 1 -2 hospitalizations in 2 years and one additional characteristic; No Trigger • Guidelines: Perform a comprehensive review of MH status, MH services and interventions, characteristics of the individual’s environment and community; ID challenges, MH issues, social and family ties, community support, and past hospitalizations; address challenges and unresolved issues, ensure a personal safety plan, arrange community supports and services, promote psycho-education, address social environment issues. • Additional Resources: 2 publications 1998 - 1999

HEALTH PROMOTION CAPs SMOKING CAP SUBSTANCE USE CAP WEIGHT MANAGEMENT CAP EXERCISE CAP SLEEP DISTURBANCE CAP PAIN CAP FALLS CAP

SMOKING CAP • Issue: Leading worldwide cause of preventable illness and premature mortality. Addictive so there are withdrawal symptoms. Sometimes is a form of self-medication. • Goals of Care: Manage smoking withdrawal symptoms; education about benefits of smoking cessation; promote willingness and readiness for smoking cessation; reduce or stop smoking. • Triggers: Manage Withdrawal Symptoms; Encourage Smoking Cessation or Reduction; No Trigger • Guidelines: Encourage sustained abstinence; strategies to encourage and support tobacco cessation or reduction; strategies for those not willing or ready to change behavior; considerations of the environment and other treatment considerations. • Additional Resources: 8 publications 2006 - 2009

SUBSTANCE USE CAP • Issue: When combined with mental illness, substance use can interfere with participation in a rehab or recovery program and can reduce the effectiveness of treatments and interventions. Includes the misuse of prescribed and over-the-counter medications. Consider social and behavioral indicators of problematic use. • Goals of Care: Determine readiness to change behaviors; help develop a recovery path to decrease or eliminate problematic substance use; prevent adverse effects of substance use and withdrawal; provide education; strengthen social ties and remove social and economic barriers • Triggers: Current Problematic Substance Use; Prior History of Problematic Substance Use; No Trigger • Guidelines: Assess for withdrawal symptoms, degree of dependency and patterns of use; evaluate motivation for change; evaluate social, economic, psychological, and medical issues; referral to specialist or program, harm reduction, involvement of others, education. • Additional Resources: 4 publications 1986 - 2006

WEIGHT MANAGEMENT CAP • Issue: Weight management can be complex and multifactorial. Obesity can have profound effects on physical health, self-esteem, well-being, and quality of life. This CAP IDs factors associated with unhealthy weights and offers interventions to reduce the effects of altered body composition. • Goals of Care: ID underlying causes of problems; address acute MH and medical conditions that complicate weight management; review impact and appropriateness of medication; provide education and counseling around healthy eating and lifestyles; achieve and maintain a health weight. • • Triggers: Body Composition; Problematic Eating Behaviors; No Trigger • Additional Resources: 5 publications 2004 - 2009 Guidelines: ID and address any acute MH symptoms and immediate health concerns to ensure safety; review eating patterns, medications and patterns of physical activity; ID potential lifestyle changes; evaluate role of financial resources, medication side effects, MH and substance use; determine readiness to change behaviors; promote peer support.

EXERCISE CAP • Issue: Physical exercise is important for optimal health and functioning. This CAP identifies individuals who are physically inactive and aims to assist them in modifying factors that prevent achieving an appropriate level of exercise. • Goals of Care: ID and understand the reasons for low physical activity; increase knowledge and confidence in exercise; establish a fitness program; increase hours of physical activity; improve energy level, confidence, self-awareness, and overall sense of well-being. • Triggers: Increase Physical Activity Among Individuals Capable of Being Active; Increase Physical Activity but Consider Limitations of a Health Condition; No Trigger • Guidelines: Address personal choices; ID causes and consequences of physical inactivity; address nutrition; consider MH issues as a cause of inactivity; aging and physical comorbidities; substance use and co-morbid disorders; sleep deprivation; medication side effects; physical fitness programs; walking; behavior modification; intervention and support. • Additional Resources: 2 publications 2001 - 2009

SLEEP DISTURBANCE CAP • Issue: Sleep disturbance impairs quality of life as well as many areas of physical function. This CAP aims to ID factors to consider in any situation where sleeping problems arise. The reciprocal relationship between sleep disturbance and health can result in a rapid downward spiral in the individual’s mental and physical well-being, if not addressed. • Goals of Care: Address underlying causes of the sleep disturbance; decrease frequency and severity of interrupted sleep; improve the quality and quantity of sleep; prevent relapse of sleep problems; reverse insomnia-related morbidities; reduce the risk of accidental injury. • Triggers: Current Sleep Disturbance and Severe Cognitive Impairment; Current Sleep Disturbance and No Worse Than Moderate Cognitive Impairment; No Trigger • Guidelines: Consider nature of the sleep disturbance and potential causes of sleep disturbances; ID potential interventions, e. g. , sleep hygiene, behavioral therapies, complementary and alternative therapies, oral appliances, respiratory equipment, sleep disorder surgery; sleep medications. • Additional Resources: 3 publications 1993 - 2010

PAIN CAP • Issue: Reported pain should be considered an important quality-of-life problem that should always be given a high priority in plan development. It is the physical and emotional response to pain and its associated consequences that varies from person to person, not the pain per se. Work with the individual and family members to ID approaches to control the impact of pain. • Goals of Care: ID the etiology of the pain and manage it with the most effective treatment modalities; assess risk for and minimize or prevent adverse outcomes related to use of pain medication; increase the individual’s understanding of the relationship of pain to somatic and psychological problems; monitor response to treatment and adverse effects. • Triggers: High Priority – pain that is severe, horrible, or excruciating; Moderate Priority – daily mild or moderate pain; No Trigger • Guidelines: Ensure there is not an acute medical condition causing the pain; consider comorbid physical health problems or psychopathology; conduct a thorough assessment of the pain; ID and implement pharmacological or nonpharmacological pain management interventions; evaluate ongoing effectiveness of interventions. • Additional Resources: 5 publications 1999 - 2007

FALLS CAP • Issue: While typically an issue for older adults, recent studies have shown psychotropic medications to be associated with an increased risk of falls even in younger individuals. Effectively addressing any risk of falls is an important priority in supporting an individual’s autonomy and community integration. • Goals of Care: Minimize the impact of risk factor falls; prevent future falls; reduce fear of falling as a barrier to physical activity and community engagement. • • Triggers: High Risk – multiple prior falls; Moderate Risk – one previous fall; No Trigger • Additional Resources: 4 publications 2001 - 2010 Guidelines: Initial priority is improving safety; understand previous falls; review medications; assess physical performance; ID any vision problems; ID any neurological and cognitive problems; review any cardiorespiratory problems; ID any environmental factors

ISSUES COVERED BY inter. RAI Ch. YMH CAPs Safety Family Life & Social Integration Functional Status Health Promotion Services & Supports

SAFETY CAPs CONTROL INTERVENTIONS CAP (in-patient only) CRIMINALITY PREVENTION CAP HARM TO OTHERS CAP HAZARDOUS FIRE INVOLVEMENT CAP SEXUAL BEHAVIOR CAP SUCIDALITY & PURPOSEFUL SELF-HARM CAP TRAUMATIC LIFE EVENTS CAP

CRIMINALITY PREVENTION CAP • Issue: Adults who commit serious offenses often had early childhood experiences that placed them at risk for criminal involvement. Risk factors for involvement in criminality encompass multiple domains – individual, family and societal. • Goals of Care: Help the individual envision a life without criminal involvement; address individual risk and protective factors; promote academic success and community and school involvement; strengthen the individual’s social skills and encourage positive peer relationships; aid caregivers in adequately monitoring and supervising the individual. • • Trigger: Any expressions supportive of criminal activity, stealing, or violence to others • Additional Resources: 5 resources 2010 - 2013 Guidelines: Refer for treatment if serious psychiatric symptoms are evident; refer to protective services if there are signs of abuse, neglect, lack of supervision, or exposure to family violence; use other CAPs if violent, aggressive or inappropriate sexual behaviors are present; gain an understanding of behaviors, background, and motivations; engage the individual and caregivers; facilitate support from community and school resources; specific strategies for stealing and gang participation; refer to evidence-based care.

HARM TO OTHERS CAP • Issue: Individual, social, family, and environment factors are associated with harmful behaviors. With age, harmful behaviors tend to become more calculative and planned. Physical aggression generally provokes immediate concern and is one of the most common reasons for young individuals to be referred for MH services. • Goals of Care: Ensure safety; prevent escalation or recurrence of harm; minimize the need for control intervention; reduce the risk of harm to others. • Triggers: Immediate Intervention – CY-RHO 5 -6 or CY-RHO 3 -4 and Impulsivity >1; Prevention – CY-RHO 3 -4 and Impulsivity 0 -1; No Trigger • Guidelines: Interventions for acute physical aggression to ensure immediate safety of all concerned; debriefing; assessment of incident; assessment of harmful behavior; treatment planning; cognitive-behavioral psychosocial interventions; strategies to address proactive aggression; strategies to address reactive aggression; involvement of family • Additional Resources: 4 publications 2010

HAZARDOUS FIRE INVOLVEMENT CAP • Issue: Includes any unsanctioned or unsafe fire-related behavior. Early identification and treatment may prevent devastating consequences. • Goals of Care: Eliminate, decrease, or prevent hazardous fire setting; enhance the individual’s fire safety knowledge and skills; engage support to ensure safety in the home and community. • Triggers: High Risk – engaged in activity in last year and has >1 identified risk factor; Moderate Risk – engaged in activity in last year and has 1 identified risk factor; Low Risk – engaged in activity in last year with no additional risk factor; No Trigger • Guidelines: Evaluate the incident; consider interventions based on the identified risk; support caregivers to encourage safety at home or in residential facilities; engage the individual; use evidence-based care. • Additional Resources: 4 publications 2004 - 2012

SEXUAL BEHAVIOR CAP • Issue: Distinguish problematic, potentially harmful sexual behavior by children and youth from developmentally appropriate curiosity. In may cases problematic behavior can be redirected with clear and direct instruction. Help the individual understand what is respectful and appropriate. • Goals of Care: Establish appropriate limits and boundaries; ensure that the individual understands rules and appropriate behavior for age, development, and culture; provide opportunities for the individual to practice newly acquired appropriate and socially acceptable behaviors; foster support and safety within the home, peer group, and community. • • Trigger: Engagement in one or more of five identified situations • Additional Resources: 5 publications 2010 - 2012 Guidelines: Ensure safety; respond to the behavior appropriately; report any harm by the individual; assess for history of being sexually abused; ID and understand the reasons for the behavior through a professional assessment; implement individualized, developmentally sensitive interventions; promote health sexual development.

SUICIDALITY & suicidal PURPOSEFUL SELF-HARM CAP • Issue: In general, and self-harming behaviors can be differentiated according to lethality, repetition, and intent. Suicidal behaviors tend to involve more lethal methods, occur less frequently, and are associated with a higher desire to end life. The most common reason for self-harming behavior is to alleviate negative affect or arousal. • Goals of Care: Attend to immediate safety needs; reduce the risk of repeated attempts; support recovery through school, family, and community support services; support family and other members of the social network who are distressed by the attempts. • Triggers: High Risk – CY-So. S Scale 5 -6; Moderate Risk – CY-So. S Scale 3 -4 and Impulsivity >1; No Trigger • Guidelines: If high risk, treat immediately in hospital and ensure immediate safety; if moderate risk, consider hospitalization depending on circumstances; physical and psychological assessments; determine details of the suicide plan; evaluate additional risk factors; ID and implement psychological, pharmacological, and social interventions; ID strategies to prevent further attempts • Additional Resources: 5 publications 2011 - 2013

TRAUMATIC LIFE EVENTS CAP • Issue: Traumatic life events can have debilitating consequences. More complex forms of traumatic stress responses can occur when there is a history of chronic trauma. If left untreated, problems such as attachment and relational difficulties, dissociation, emotional numbness, and depression can worsen over time. • Goals of Care: Alleviate risk of further trauma or abuse by ensuring a safe environment with knowledgeable and sensitive caregivers; reduce crisis-related symptoms; address underlying MH symptoms; prevent or reduce secondary conditions; strengthen family relationships, where appropriate. • Triggers: Address Immediate Safety Concerns; Reduce the Impact of Prior Traumatic Life Events; No Trigger • Guidelines: Ensure safety; provide trauma-informed care; refer to specialized care; be aware of stress responses; stabilization and containment; engage the individual’s support system; manage behavioral symptoms; refer to therapy from individuals with appropriate training and experience. • Additional Resources: 6 publications 2010 - 2013

FAMILY LIFE & SOCIAL INTEGRATION CAPs ATTACHMENT CAP CAREGIVER DISTRESS CAP INTERPERSONAL CONFLICT CAP PARENTING CAP SOCIAL & PEER RELATIONSHIPS CAP

ATTACHMENT CAP • Issue: Attachment is a key developmental goal in early childhood and refers to the drive for a young child to be close to a caregiver for safety, protection, and regulation. Once attachments have been formed, the child can use the caregiver as a secure base to explore the environment and as a source of support and comfort when distressed. Children with disorganized attachment patterns are particularly at high risk for adjustment difficulties and psychopathology. • • Goals of Care: Help the caregiver establish a secure and trusting relationship with the child. • Guidelines: Assess by gathering history, interviewing caregivers, and observing the child’s interactions with the caregiver and an unfamiliar adult; ID interventions and caregiver strategies; refer to qualified therapeutic resources; avoid coercive strategies. • Additional Resources: 4 publications 2011 - 2013 Trigger: Age 11 and younger who have experienced any of 9 identified situations and have at least one identified comfort-seeking difficulty.

CAREGIVER DISTRESS CAP • Issue: Caregivers experiencing stress, serious mental illness, drug or alcohol abuse, or highintensity marital discord have a reduced ability to respond sensitively and lead to a heightened sensitivity to distress, externalizing disorders, internalizing disorders, impairments in psychosocial functioning, and delinquent behaviors. • Goals of Care: Improve the caregiver’s capacity to manage stress; facilitate access to appropriate treatment for the caregiver. • • Trigger: Caregivers who demonstrate at least two of eight identified indicators of distress • Additional Resources: 4 publications 2010 - 2012 Guidelines: Explore with the caregiver the current situation and strategies for resolving; encourage treatment for any mental illness or substance abuse; determine if there are financial concerns; address conflict between caregivers; consider family-related issues.

INTERPERSONAL CONFLICT CAP • Issue: Interpersonal conflict is a natural and common consequence of social interaction. Common and less severe types of conflict serve an important purpose in the socialization of young people and the maintenance of the family system. Destructive conflict within the family is linked to negative child and youth outcomes. Conflict can occur within and outside the family. • Goals of Care: Reduce the frequency and intensity of conflict; ID and address emotional response patterns that contribute to interpersonal conflict; increase the young person’s conflict management, emotional regulation, and social skills; enhance the individual’s and family’s capacity for conflict resolution. • Triggers: Based on domains of Family, Friends and Peers, and Other Relationships. Reduce Widespread Conflict – one or more indicators from at least two of the domains; Reduce Conflict Within a Specific Domain – one or more indicators in one domain; No Trigger • Guidelines: Short-term interventions are generally ineffective; consider cultural issues; assess the nature of the conflict; ID underlying issues that fuel the conflict; involve caregivers; provide skill-building opportunities; promote stress management; consider medications; assess for behavioral or physical illness; ID strategies to reduce conflict; increase family wellness. • Additional Resources: 4 publications 2011 - 2012

PARENTING CAP • Issue: A young person’s emotional or behavioral challenges can be a driving force leading to inappropriate or ineffective parenting. Negative parenting can worsen the young person’s MH symptoms. Educating caregivers and providing effective strategies for managing behavioral symptoms can improve the dynamics of the relationship. • Goals of Care: Aid caregivers to develop realistic expectations in light of individual needs; equip caregivers with strategies to manage behavioral symptoms of the young person’s MH condition; enhance caregivers’ sense of confidence in parenting abilities. • • Trigger: Caregivers who demonstrate more than one of six identified concerns • Additional Resources: 3 publications 2010 - 2011 Guidelines: Consider if concerns rise to the level needing protective services; consider cultural beliefs; ID practical strategies to educate and inform caregivers; ID strategies for the caregiver to provide support to the individual; ID strategies to prevent problematic behavior; ID strategies for responding to behavioral symptoms; ID strategies for the caregiver to help the individual deal with anxiety.

SOCIAL & PEER RELATIONSHIPS CAP • Issue: Positive peer relationships are essential to increase self-esteem, prevent victimization, promote the development of important social skills, and to protect from the effects of problematic family relationships. • Goals of Care: Alleviate isolating behaviors and symptoms; reduce factors that contribute to problematic social and peer relationships and develop strategies for dealing with difficult peer situations; strengthen the young person’s social skills, promote maintenance of health peer relationships. • Triggers: Reduce Social Withdrawal or Isolation – more than one of seven identified indicators; Reduce Maladaptive or Antisocial Peer Interactions – at least one of two identified indicators; No Trigger • Guidelines: Assess for risk factors; ID strategies to address extreme shyness, unsociable individuals, peer rejection and victimization, bullying, antisocial peers; refer to effective therapeutic interventions. • Additional Resources: 6 publications 2003 - 2012

FUNCTIONAL STATUS CAPs COMMUNICATION CAP LIFE SKILLS CAP

COMMUNICATION CAP • Issue: Communication includes understanding others and sending messages with motor movements. Communication difficulties can interfere with social and emotional development and can have far-reaching consequences on MH and academic achievement. • Goals of Care: Enhance ability to express oneself and understand others in various contexts and settings; engage the social network to understand support communication development. • • Trigger: Difficulties in at least one of two types of communication • Additional Resources: 4 publications 2010 - 2013 Guidelines: Comprehensive evaluation in consultation with appropriate specialists; address speech and language issues; ID interventions that are appropriate for current levels of communication; address associated physical and MH issues; support majority language learning while respecting first language and culture

LIFE SKILLS CAP • Issue: Children and youth must master life skills to maintain health and safety as they progress into adulthood. This includes activities of daily living and instrumental activities of daily living. Caregiver training is an essential component of intervention. • Goals of Care: Enhance the young person’s life skills; promote independence with adequate caregiver support consistent with developmental level and family’s culture. • Triggers: ADL Assistance – age 6 -18 requiring physical assistance with more than one ADL; IADL Assistance – age 12 -18 requiring at least extensive assistance for more than one IADL; No Trigger • Guidelines: Consider enhancing life skills regardless of physical or cognitive limitations; use specialized therapies and strategies as needed; assess capacity and performance; ID limiting factors and barriers; compare to typical ADL/IADL development; develop a step-by-step plan; enlist caregivers • Additional Resources: 6 publications 2010 - 2012

HEALTH PROMOTION CAPs CAFFEINE USE CAP GAMBLING CAP MEDICATION ADHERENCE CAP MEDICATION REVIEW CAP PHYSICAL ACTIVITY CAP SLEEP DISTURBANCE CAP STRENGTHS CAP SUBSTANCE USE CAP TOBACCO AND NICOTINE USE CAP VIDEO GAMING CAP WEIGHT MANAGEMENT CAP

CAFFEIN USE CAP • Issue: High levels of caffeine pose a threat to healthy brain development and physical growth by impeding regular sleeping and eating patterns. It has a negative impact on behavior and academic and athletic achievement, and is related to decreased attention, inappropriate conduct, aggression, unpredictability, sensation seeking, and risky behaviors. • Goals of Care: Reduce excessive use of caffeine; address toxic effects associated with excessive intake; manage caffeine withdrawal symptoms; support willingness and readiness for caffeine use reduction. • Trigger: consumption of three or more caffeinated beverages or energy drinks in a single day within the last three days. • Guidelines: Assess for caffeine-related issues; address toxic effects of excessive caffeine intake; manage withdrawal symptoms; encourage reduction of use; ID and implement appropriate strategies; maintain reduced intake. • Additional Resources: 5 publications 2009 - 2012

GAMBLING CAP • Issue: Gambling addiction in adulthood often begins in adolescence or earlier. Children and youth with gambling problems often have parents who gamble excessively. • Goals of Care: Reduce, minimize, or curtail gambling; address the impact in affected areas of the individual’s life. • Trigger: Children and youth who have gambled excessively or uncontrollably in the last 90 days • Guidelines: ID gambling patterns and related concerns; set goals; ID and address barriers; ID coping strategies for the individual to use; support caregivers and family members; assist in development of positive relationships and finding alternative leisure activities; help manage withdrawal symptoms; ID ways to maintain abstinence from gambling. • Additional Resources: 5 publications 2010 - 2014

MEDICATION ADHERENCE CAP • Issue: Adherence to a medication regimen is essential for therapeutic effectiveness. Successful adherence is achieved by understanding the needs, values, habits, and abilities of the individual and caregivers directly involved in daily care. Includes both underdosing and overdosing. • Goals of Care: Ensure the individual and caregiver understand the rationale for all prescribed medications, the regimen, and the possible side effects; improve adherence in collaboration with the prescriber, individual, and caregivers. • • Trigger: Presence of at least one of three identified situations • Additional Resources: 5 publications 2010 - 2014 Guidelines: Safety and well-being of the individual is the highest priority; ID factors that contribute to non-adherence; ID strategies to enhance adherence, including education, collaborative decision making, and behavioral, socio-environmental, socio-culturally modified, or legal interventions; evaluate effectiveness of interventions.

MEDICATION REVIEW CAP • Issue: Periodic medication review is an essential component of any pharmacological treatment plan. A full review is indicated when there are issues of actual and possible side effects or MH deterioration. • • Goals of Care: Reach optimal therapeutic effectiveness while minimizing side effects. • Guidelines: A team approach with the prescriber is essential; review all medication and other medicinal products; address adverse effects; assess therapeutic effects; encourage ongoing monitoring and follow-up. • Additional Resources: 3 publications 2010 - 2012 Trigger: Discontinuance of psychotropic meds in the last 90 days due to side effects OR 80100% adherence with a deterioration or one of a list of eight side effects

PHYSICAL ACTIVITY CAP • Issue: Physical activity is an essential component of a healthy lifestyle. International guidelines recommend that young people engage in at least one hour of physical activity per day. • • • Goals of Care: Increase physical activity to at least one hour per day. • Additional Resources: 3 publications 2010 - 2012 Trigger: less than one hour of physical activity in the last 3 days Guidelines: Complete a full health assessment prior to starting a program; conduct a lifestyle assessment; ID and address barriers; with the individual create a comprehensive physical activity plan that is flexible and focused on the individual’s preferences and abilities; support the physical activity plan.

SLEEP DISTURBANCE CAP • Issue: Sleep disturbances in children and youth are often related to environmental conditions, but also can be related to physiological, behavioral, or psychological factors. Sleep disturbances can affect quality of life and daytime functioning. • Goals of Care: Assess situational variables and environmental factors and the need for intervention or referral for specialized services; ensure that appropriate routines to contribute to sleep quality are in place; treat sleep problems with the aim of optimizing the duration and quality of sleep. • • Trigger: >1 of six identified concerns in the last three days • Additional Resources: 5 publications 2007 - 2010 Guidelines: Assess issues related to the sleep disturbance, including its effects; implement a recommended two step process for intervention; ID any conditions requiring specialized treatment; address any special considerations needed to address special populations

STRENGTHS CAP • Issue: Strengths are defined as personal traits and abilities that serve a protective function. Success in achieving goals generally happens when an individual is able to draw on strengths. It is important to help children and youth develop and use strengths in order for them to achieve continued growth, success, and positive treatment outcomes. • Goals of Care: Develop personal strengths in the individual; encourage use of strengths as a tool for success. • • Trigger: <2 of four identified potential personal strengths • Additional Resources: 4 publications 2010 - 2012 Guidelines: Foster notable talents; increase positive outlook; enhance adaptability to change; develop problem-solving skills.

SUBSTANCE USE CAP • Issue: Substance use among children and youth is a major public health concern world-wide and is one of the most cited reasons for mental health admissions. Any use by young individuals is generally considered detrimental. It is important to consider the social environment that promotes or facilitates substance use. • Goals of Care: Reduce substance use and engage the individual in treatment; help the individual to develop a substance use recovery path; manage withdrawal symptoms. • • Trigger: Presence of at least one of three identified situations • Additional Resources: 4 publications 2010 - 2011 Guidelines: Refer to emergency services, if needed; address cultural issues; ID patterns of substance use, social context, co-morbid conditions, and medical considerations; ID and implement interventions for detox, treatment, and recovery; guide the individual; engage the family, where appropriate.

TOBACCO AND NICOTINE USE CAP • Issue: About half of children and youth who use tobacco products will form long-term nicotine addictions. Up to 90% of adult tobacco users became addicted to nicotine as youth. Tobacco use rates for children and youth have declined internationally, but use by those receiving inpatient psychiatric care remains high. The mean age for smoking initiation in young people with MH problems is 11 years, with weekly smoking habits forming by age 12. • Goals of Care: Promote willingness and readiness to cease tobacco use; manage nicotine withdrawal symptoms; foster social supports to sustain abstinence from tobacco. • • Trigger: occasional use of nicotine products or usual use of nicotine products daily • Additional Resources: 5 publications 2010 - 2013 Guidelines: Assess amount of use and likelihood of withdrawal; manage withdrawal symptoms; evaluate the individual’s knowledge of risks; provide education; address barriers to cessation; prevent long-term tobacco use; reduce or cease daily tobacco use; relapse prevention.

VIDEO GAMING CAP • Issue: Excessive video gaming over time can impact self-care, friendships, relationships, sleep, and academic achievement. Intervention is needed if the activity interferes with the individual’s daily function, impairing social relationships, family life, or school performance. • Goals of Care: Reduce the amount of video gaming both in daily individual sessions and total time played weekly; address the impact of reducing problem video gaming in the affected areas of the individual’s life. • Triggers: Severe Risk – negligible participation in self-care, social or household activities, or work/school; Moderate Risk – reduced attention to these activities; No Trigger • Guidelines: ID video gaming patterns and related concerns; ID coping strategies; engage and support caregivers; manage withdrawal from video gaming. • Additional Resources: 6 publications 2010 - 2013

WEIGHT MANAGEMENT CAP • Issue: A variety of factors complicate weight management for children and youth with MH conditions, including medication side effects, sedentary lifestyle, poor diet, and problematic eating behaviors. Eating disorders have the highest associated mortality among mental health disorders. • Goals of Care: ID and address underlying causes of problematic eating behaviors and weight -management difficulties; review the impact and appropriateness of medications related to weight; enhance the individual’s ability to live a healthy lifestyle; promote self-esteem and a realistic body image. • Triggers: For Weight Concerns – expressed concern of weight gain, weight loss, or failure to gain weight in the last 90 days; Due to Problematic Eating Behavior – presence of at least one of three identified situations; No Trigger • Guidelines: Address medical safety and healthy lifestyle change; assess issues related to weight concerns; ID interventions to promote healthy weight management; engage family support; assess problematic eating behaviors; ID interventions to address eating behaviors. • Additional Resources: 4 publications 2007 - 2013

SERVICES AND SUPPORTS CAPs EDUCATION CAP INFORMAL SUPPORT CAP READMISSION CAP SUPPORT SYSTEMS FOR DISCHARGE CAP (inpatient only) TRANSITIONS CAP

EDUCATION CAP • Issue: The decision to drop out of school is the result of risk factors in all life domains. Poor school performance is a risk factor for mental health concerns, and mental health conditions can greatly affect academic achievement. Success in education improves future socioeconomic status and is instrumental in the development of positive relationships, friendships, a sense of belonging, and purpose. • Goals of Care: Reduce the risks associate with dropping out of school; foster a sense of academic or vocational motivation, competency, and autonomy; enhance meaningful engagement in school or vocational training; engage the individual’s social network to support success. • Triggers: Risk of Dropping Out of School – at least one of six identified risk factors; Disrupted Education – current disrupted education and no employment arrangement; No Trigger • Guidelines: Evaluate and develop goals; ID and address barriers; promote school engagement; improve motivation; engage caregivers; assess supportiveness of school; explore alternative education programs; consider employment. • Additional Resources: 3 publications 2010 - 2011

INFORMAL SUPPORT CAP • Issue: Informal support from extended family and friends for crisis management, financial assistance, emotional support, and child care/youth supervision reduces the strain caregivers feel and promotes better outcomes for the individual. • Goals of Care: ID and link the individual and caregivers with available sources of informal support; strengthen informal support systems; support the informal support. • Trigger: individuals whose family needs but does not have informal supports for >1 of 5 identified areas of need • Guidelines: Support the individual and caregivers and possibly engage formal supports; suggestions are given for crisis situations, emotional support, support for financial problems, child care/youth supervision, and respite care. • Additional Resources: 3 publications 2011

READMISSION CAP • Issue: Among children and youth with previous psychiatric admissions, readmission rates are as high as 65%. The majority of readmissions occur within three months of discharge. A number of factors across multiple domains predict psychiatric readmission. A successful post-discharge plan requires active engagement of the individual, family, school, and other community resources and supports, with continued MH and supportive care. • Goals of Care: Prevent psychiatric readmissions; ensure timely and comprehensive transition to post-discharge services; engage the individual and family in a coordinated and comprehensive mental health care plan. • Trigger: one of 3 identified categories related to hospitalizations and/or inter. RAI scale scores • Guidelines: Discharge planning with community partners; crisis planning; plan for immediacy of post-discharge services and continuity of care; address family involvement and living environment. • Additional Resources: 4 publications 2010 - 2013

TRANSITIONS CAP • Issue: While not always possible, individuals who are prepared and equipped to deal with transitions will adapt more effectively. It is important to consider both the individual’s feelings about the change and how adaptable he or she might be. Moving from children’s services to adult mental health services is a particularly difficult transition. • Goals of Care: Facilitate supports around the individual and family for a smooth transition; enhance the individual’s coping and self-advocacy skills to successfully manage the transition; enhance the family’s capacity to support and advocate for the individual during the transition. • • Trigger: any transition from one setting to another • Additional Resources: 5 publications 2011 - 2013 Guidelines: Assess the individual’s experience, willingness, and preparedness for change; construct a transition plan as early as possible; ID and address barriers to a successful transition; engage caregivers; engage the individual; ID specific strategies for specific transitions.
 Tuning out dull topics
Tuning out dull topics Open field tackling drills
Open field tackling drills Formal vs informal assessment
Formal vs informal assessment General revision of assessments and property classification
General revision of assessments and property classification Performance assessment examples
Performance assessment examples Premarital tests or assessments
Premarital tests or assessments Formative assessments in physical education
Formative assessments in physical education Slidetodoc.com
Slidetodoc.com Mlpp assessments
Mlpp assessments 6 assessments for dols
6 assessments for dols Irip
Irip Formal and informal test
Formal and informal test Eccentric viewing techniques occupational therapy
Eccentric viewing techniques occupational therapy What are the elpac levels
What are the elpac levels Cte technical skills assessments.azed.gov/student
Cte technical skills assessments.azed.gov/student Creative arts, grade 8
Creative arts, grade 8 What does olivia mean
What does olivia mean Types of authentic assessment
Types of authentic assessment Characteristics of psychological assessment
Characteristics of psychological assessment Impromptu reading plus comprehension questions
Impromptu reading plus comprehension questions Physical education assessments examples
Physical education assessments examples Apm testing florida
Apm testing florida Sat subscores
Sat subscores Lausd interim assessments
Lausd interim assessments Aware online testing neisd
Aware online testing neisd Placement diagnostic formative summative
Placement diagnostic formative summative Writing analytical assessments in social work
Writing analytical assessments in social work Vdoe algebra readiness
Vdoe algebra readiness Informative assesment
Informative assesment Incas assessment
Incas assessment What is physical fitness test in mapeh
What is physical fitness test in mapeh Florida assessments for instruction in reading
Florida assessments for instruction in reading Ddi assessments
Ddi assessments Aimsweb reading
Aimsweb reading Writing assessment strategies
Writing assessment strategies Iowa staewide assessment of student progress
Iowa staewide assessment of student progress Glba risk assessment template
Glba risk assessment template Thereselleraccount
Thereselleraccount Ricas accommodations
Ricas accommodations What are the features of performance based assessment
What are the features of performance based assessment Osde assessments
Osde assessments Next generation assessments
Next generation assessments Kentucky assessments biology
Kentucky assessments biology What are the characteristics of a holistic assessment
What are the characteristics of a holistic assessment Formative evaluation
Formative evaluation Anet interim assessments
Anet interim assessments Rhode island comprehensive assessments system
Rhode island comprehensive assessments system Michigan literacy progress profile
Michigan literacy progress profile Common core ela assessments
Common core ela assessments Fors-online.org.uk
Fors-online.org.uk Datarich student assessments
Datarich student assessments Assessments that favor one group over another are
Assessments that favor one group over another are Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worms-breton
Tư thế worms-breton Hát lên người ơi
Hát lên người ơi Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết