URINARY TRACT INFECTION introduction UTI is considered the








- Slides: 64
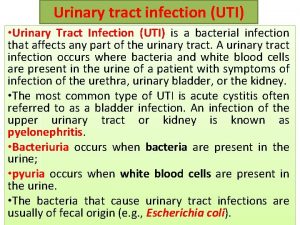
URINARY TRACT INFECTION
introduction • UTI is considered the most common bacterial infection • Almost half of all women will experience a UTI during their lifetime • The prevalence of bacteriuria is more in female when compared with male • The incidence of bacteriuria increase with increasing age, institutionalization or hospitalization. • Catheter associated UTI is the most common nosocomial infection
• Once the patient has UTI he or she is likely to develop subsequent infection • The probability of recurrent UTI increase with number of previous infection and inversely related with the time between infections the • short nature of the female urethra combined with its close proximity to the vagina and rectum predispose women to more frequent UTIs when compared with men.
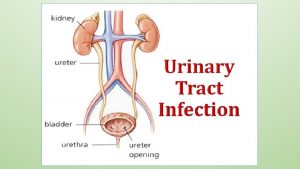
Definitions • UTI : -inflammatory response of urothelium to bacterial invasion • Bacteriuria: presence of bacteria in the urine, which is normally free of bacteria which could be colonization or infection or contamination of abacteriuric specimen • Significant bacteriuria is a term used to describe the number of bacteria in specimen that usually exceed the number of contamination , this number depend on method of collection, presence of symptom …
• Colonization(asymptomatic bacteriuria): urinary growth of bacteria without symptom, no inflammatory response • We usually do not screen or manage except in pregnancy or before urological intervention • Pyuria: is the presence of WBC in urine which indicate inflammatory response to bacteria , or stone , foreign body , TB, tumor (sterile pyuria)
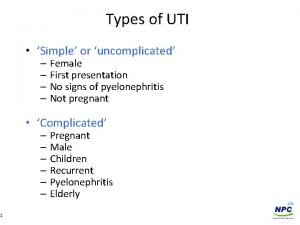
classification • UTI could be classified according to the site • Like cystitis, pyelonephritis , urethritis , prostatitis , epididymitis • UTI could also be classified into: • Complicated UTI: UTI occurs in presence of underlying anatomical or functional abnormalities, the host is compromised , bacteria more virulent, majority are male, these factors increase the chance of acquiring bacteria and decrease the efficacy of therapy
• Uncomplicated: infection in healthy patient with structurally and functionally normal urinary tract the majority are female and respond to short course of cheap antibiotic, the bacteria is easily eradicated by short course of inexpensive oral antibiotic • Example of complicated UTI: infection in pregnancy, immuncompromised patient like DM, PTN on catheter, stone or BPH, neurogenic bladder, decrease renal concentrating ability
• UTI could be classified according to relation to other UTI • Isolated UTI: - UTI occur in individual who has never UTI, or has one remote infection • Recurrent UTI: -more than 2 infections in 6 months or 3 infections in 12 months, with documented successful resolution of the previous infection, can be due to 1 - reinfection : reintroduction of bacteria into urinary tract from outside 2 -bacterial persistence: the same bacteria reemerging from a focus within urinary tract like infected stone or infected prostate.
3 -Unresolved infection: - has not responded to antimicrobial therapy UTI also could be classified into Outpatient : in ptn who are not hospitalized or institutionalized at the time when they got infected Nosocomial: in ptn who are hospitalized or institutionalized usually caused by resistant microorganism
bacterial entery • Most bacteria enter the urinary tract from bowl reservoir via ascent through urethra to bladder, Most cases of pyelonephritis are caused by the ascent of bacteria from the bladder through the ureter and into the renal parenchyma (ascending route). • Other modes of bacterial entry are uncommon causes of UTI. Hematogenous spread can occur in immunocompromised patients and in neonates. Staphylococcus aureus, Candida species, and Mycobacterium tuberculosis are common pathogens that travel through the blood to infect the urinary tract.
virulence factor • limited number of E coli are responsible for infection • Theses bacteria have factor that facilitate the adhesion and colonization and invasion of urinary tract example of these virulence factors • 1 -pili which mediate The adherence of E. coli to epithelial cells by binding to specific receptor on the surface epithelium. There is two types of pili • Type 1 pili (mannose sensitive): which help the adherence to bladder mucosa.
• Type P pili (mannose resistance): these pili confer tropism to kidney , found in most pyelonephritis associated e coli • Mannose resistant means that mediate hemagglutination of human RBC and not affected by mannose. • Most uropathogenic E coli have both types of pili , Evidence of phase variation of bacterial pili in vivo

• 2 -Hemolysin: which initiates tissue invasion and makes iron available for the infecting pathogens. • 3 -K antigen: which protects the invading bacteria from phagocytosis by neutrophils
Host defense factor normal flora of vaginal introitus like lactobacilli and coagulase negative staph , corynebacteria form barrier against colonization and compete for nutrient, lactobacilli metabolize glycogen into Lactic acid and so drop the vaginal PH. urine : osmolarity and Ph and urea concentration • Tamm horsfall protein: kidney derived protein that attach to the pili and so prevent them from binding to urothelial receptor
• mechanical flushing of urine: Consequently, any anatomic or functional abnormalities of the urinary tract that impede urinary flow can increase the host’s susceptibility to UTI. • The epithelium lining the urinary tract not only provides a physical barrier to infection but also has the capacity to recognize bacteria in order to activate host defenses • bladder mucosal exfoliation and immune response
microbiology • E coli is the most common cause of UTI (85% of community and 50% of hospital acquired UTI • Other gram negative enterobacteriaceae like proteus and kleibsella. • Gram positive such as E fecalis and staph saprophyticus • Nosocomial infection E coli , klebsiella, pseudomonas aeruginosa , staph aureus
Urine collection methods • Presumptive diagnosis of UTI is made by direct and indirect analysis of urine and is confirmed by urine culture. • Most often, the urine is obtained from voided specimen(midstream urine sample) • In children who are not toilet-trained, a urine collection device, such as a bag, is placed over the genitalia, and the urine is cultured from the bagged specimen.
• These two methods of urine collection are easy to obtain, but the risk of contamination is higher • Suprapubic aspiration avoids potential contamination; however, because of its invasiveness, it is rarely used except in selected patients • Urine obtained from a urinary catheter is less invasive than a suprapubic aspiration and is less likely to be contaminated than that obtained from a voided specimen. If a patient has an indwelling catheter, a urine specimen should be obtained from the collection port on the catheter.
Urinalysis and culture • microscopic analysis of urine for WBC, RBC, and bacteria • The finding of bacteria in urine under microscope is found in more than 90% of infection with counts of 10^5 colony forming unit • But in infection with lower colony count it is not sensitive • The false positive result may be seen in contamination
• Bacteriuria has sensitivity of 50% and specifity of 90% • Pyuria has 90% sensitivity and 50% specifity, the low specifity of pyuria occure because many disease can cause the presence of WBC in urine • Microscopic hematuria is found in 50% of cystitis and uncommon in other dysuria syndrome
• Dipstick test: biochemical and enzymatic test using special strip of paper that is dipped into urine sample, the strip has many parts saturated with chemicals react with compounds present in urine • Gram negative bacteria reduce nitrate to nitrite, and WBC secrete leukocyte esterase, both nitrite and leukocyte esterase could be detected by dipstick test

• Urine culture and sensitivity • It can take up to 3– 4 days to receive results with the antibiotic sensitivities • The number of colonies is counted and adjusted per milliliter of urine (CFU/m. L). Defining the CFU/m. L that represents clinically significant infection can be difficult. It is dependent on the method of collection, the sex of the patient, and the type of bacteria isolated and presence of symptom.
Antimicrobial therapy • The type of antibiotic and duration of treatment depend on the most likely pathogen, whether the infection is complicated or not and the cost of drug and it, s side effect and the patient (allergies, underlying diseases, age, previous antibiotic therapy, other medications currently taken, outpatient vs inpatient status, pregnancy)
• Fluoroquinolones have a broad spectrum of activity, especially against Gram-negative bacteria, and so ideal for empirical therapy, • it inhibit DNA gyrase • it is contraindicated in children and adolescent and pregnant because it affects cartilage development • fluoroquinolones are relatively expensive. Adverse reactions are infrequent and include mild gastrointestinal effects, dizziness, It may cause achilles tendon rupture
Aminoglycosides(gentamycin): inhibit protein synthesis, it is the first choice in complicated UTI (febrile UTI). in patient who requires IV antibiotics It may cause nephrotoxicity and ototoxicity Nitrofurantoin : damage bacterial DNA, it is rapidly excreted in urine but demonstrates poor tissue penetration. For this reason, it should not be used for complicated UTI, pyelonephritis, or prostatitis. It is contraindicated in ptn with G 6 PD deficiency
• Cotrimoxazole: TMP-SMX It interferes with the bacterial metabolism of folate. Adverse reaction include hypersensitivity reactions, rashes, thrombocytopenia. TMP-SMX should not be used in patients who have a folic acid deficiency state, glucose-6 -phosphate dehydrogenase deficiency, or acquired immunodeficiency syndrome (AIDS), or in pregnant patients. • It is inexpensive medication
• Cephalosporines: inhibit cell wall synthesis , Third and fourth-generation cephalosporins have broader coverage against Gram-negative bacteria but less against Gram-positive bacteria • Adverse reactions include hypersensitivity and gastrointestinal upset
• Keflex is a common first-line empiric agent in children based on sensitivity profiles for most uropathogens and has the added benefit that it can be utilized in children less than 2 months of age, it is first generation cephalosporin and orally used • in children with febrile UTI/pyelonephritis, oral third-generation cephalosporins such as cefixime have been shown to be safe and effective
Cystitis • Infection or inflammation of UB • The presenting symptoms include frequency, dysuria, urgency. Foul-smelling urine, suprapubic pain and hematuria may develop, Fever and systemic symptoms are rare • E. coli causes most of the acute cystitis • Staph saprophyticus is the second most common cause in young female(commensal organism in skin)
• bladder pain: (suprapubic pain), usually secondary to overdistension(AUR)or inflammation, • Inflammatory condition of bladder usually cause intermittent suprapubic discomfort • Strangury: sharp stabbing suprapubic pain at the end of voiding in ptn with cystitis • Constant suprapubic pain that not associated with lower abdominal swelling is rarely of urological origin • Slowly progressive bladder distention frequently cause no pain

• Cystitis must be differentiated from other infection in which dysuria may be the most prominent symptom including : • Urethritis : the dysuria is sub acute in onset, and associate with discharge, or history of new or multiple sexual partners, other irritative symptom are found but less pronounced • Vaginitis : vaginal discharge and multiple sexual partener, other irritative symptom not usually found
• Non-infectious condition of the bladder such as interstitial cystitis , urinary bladder stone , and carcinoma in situ may be associated with these symptoms
• The appropriate antibiotic should be chosen based on local resistance • For young female with uncomplicated cystitis there is no need of urine culture except if atypical presentation or no response to drugs • Management of acute cystitis consists of a short course of oral antibiotics. TMP-SMX, nitrofurantoin, and fluoroquinolones have excellent activity against most pathogens that cause cystitis.
• In case of recurrent cystitis extensive radiological evaluation is needed • Management of recurrent cystitis, depends on its cause. Surgical removal of the infected source (such as urinary calculi) is needed to treat bacterial persistence • In most cases of bacterial reinfection, medical management with prophylactic antibiotics is indicated. Low-dose continuous prophylactic antibiotic has been shown to reduce the relative risk for recurrence.
• Treatment: -General measures : -increase fluid intake, avoid constipation in female, voiding before and after intercourse and wiping from front to back -Alternatives to antibiotic therapy in the treatment of recurrent cystitis/UTI include intravaginal estriol , lactobacillus vaginal suppositories (Reid and Burton, 2002), and cranberry juice taken orally. or
• When the recurrent cystitis/UTI is related to sexual activity, frequent emptying of the bladder and a single dose of antibiotic taken within 2 hours of sexual intercourse can significantly reduce the incidence of recurrent infection
Pyelonephritis • Inflammation of kidney and renal pelvis, diagnosis is usually made clinically. • • Presents with fever, flank pain, nausea, vomiting and symptoms of lower UTI P/E- renal angle tenderness Lab- leukocytosis , urine test ( positive for UTI) and culture Radiology: In patients with acute pyelonephritis, renal ultrasonography is important to rule out concurrent urinary tract obstruction but cannot reliably detect inflammation or infection of the kidney. CT scan is not necessary unless the diagnosis is unclear or the patient is not responding after 48– 72 hours of culture specific antibiotic therapy. Acute bacterial infection causes constriction of peripheral arterioles and reduces perfusion of the affected renal segments. Perfusion defects,

• Management: in complicated infection and in patient who have toxicity due to associated septicemia, hospitalization is indicated with IV antibiotic(gentamycin and ampicillin) or third generation cephalosporin • If no response to management within 2 -3 days we do ct with contrast to exclude underlying obstruction or complicated pyelonephritis

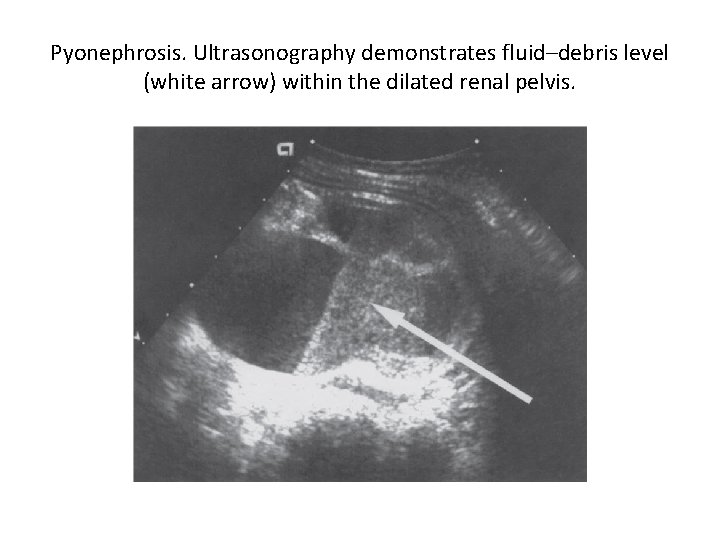
Other kidney infections 1 -pyonephrosis and infective hydronephrosis: -pus in renal pelvis and calyces Infected HN: bacterial infection of hydronephrotic kidney Pyonephrosis: infected HN associate with parenchymal destruction Patients with pyonephrosis are usually very ill, with high fever, chills, and flank pain Need drainage with jj stent or nehrostomy and iv antibiotic

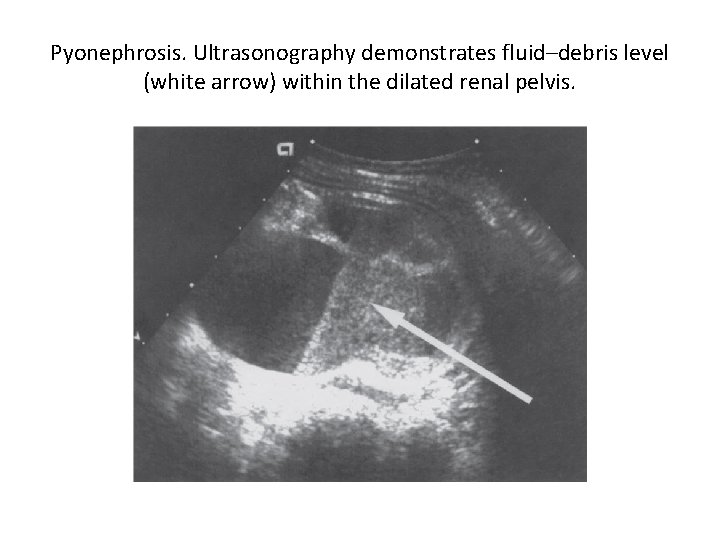
Pyonephrosis. Ultrasonography demonstrates fluid–debris level (white arrow) within the dilated renal pelvis.
2 -Renal Abscesses: -result from a severe infection that leads to liquefaction of renal tissue; this area is subsequently form abscess which can rupture into the perinephric space forming perinephric abscesses. Renal abscess could arise from gram negative bacteria in conjunction with some other underlying urinary tract abnormalities, such as stones or obstruction, and mostly involve the cortico-medullary junction Or arise from hematogenous spread of staphylococci, particularly from infected skin lesions, less common and usually involve the renal cortex, Patients with diabetes, those undergoing hemodialysis, or intravenous drug abusers have been at high risk
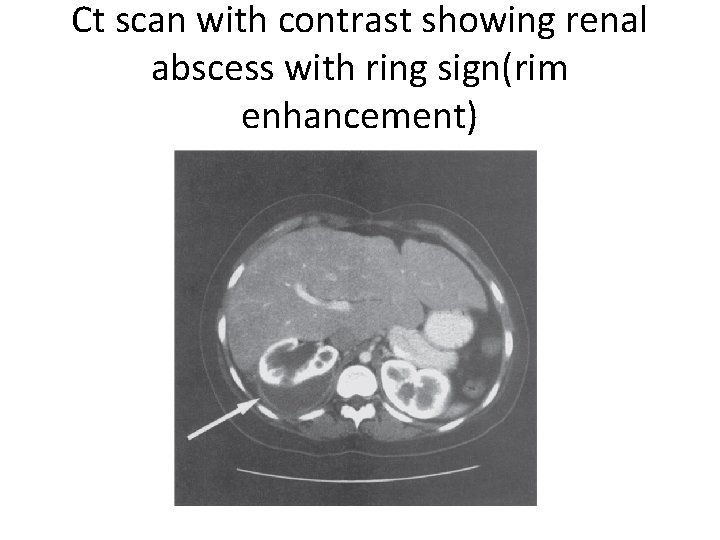
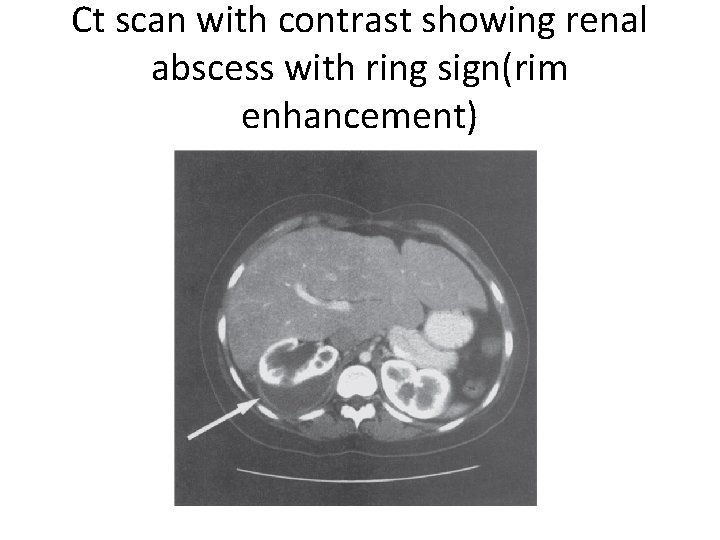
Ct scan with contrast showing renal abscess with ring sign(rim enhancement)
• The most common presenting symptoms in patients with renal/perinephric abscesses include fever, flank or abdominal pain, chills, and dysuria. Many of the symptoms have lasted for more than 2 weeks • The appropriate management of renal abscess must first include appropriate antibiotic therapy, percutaneous drainage under CT scan or ultrasound guidance, drainage of obstruction if found.
3 - emphysematous pyelonephritis: - severe acute necrotizing pyelonephritis, and associate with gas within and around the kidney. About 95% of patients with emphysematous pyelonephritis have diabetes; female: male ratio 6: 1 other contributing factors upper urinary tract obstruction and renal impairement
• Patients with emphysematous pyelonephritis present with fever, flank pain, and vomiting that fails initial management • Gas overlying the affected kidney may be seen on a plain abdominal radiograph (kidneys, ureters, bladder [KUB]) or CT scan (more sensitive) • Management: with parenteral antibiotics. Tx , percutaneous drainage, blood sugar control and transfer to icu, if not improved then emergency nephrectomy needed • high mortality rate reach about 40%


4 -xanthogranulomatous pyelonephritis: -chronic destructive infection of the kidney The affected kidney is almost always hydronephrotic and obstructed. In most cases, Unilateral Severe inflammation and necrosis obliterate the kidney parenchyma. Characteristically, foamy lipid-laden histiocytes (xanthoma cells) are Present. typical symptom include chronic flank pain fever malaise and weight loss
• CT is probably the most useful radiologic technique in evaluating patients with xanthogranulomatous pyelonephritis. Fifty to 80 percent of patients show the classic triad of unilateral renal enlargement with little or no function and a large calculus in the renal pelvis • Although review of the literature shows Proteus to be the most common organism involved with xanthogranulomatous pyelonephritis, E. coli is also common.
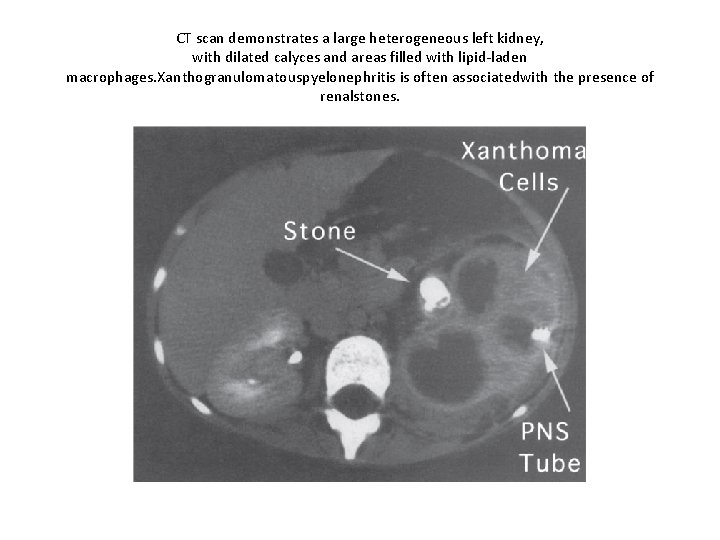
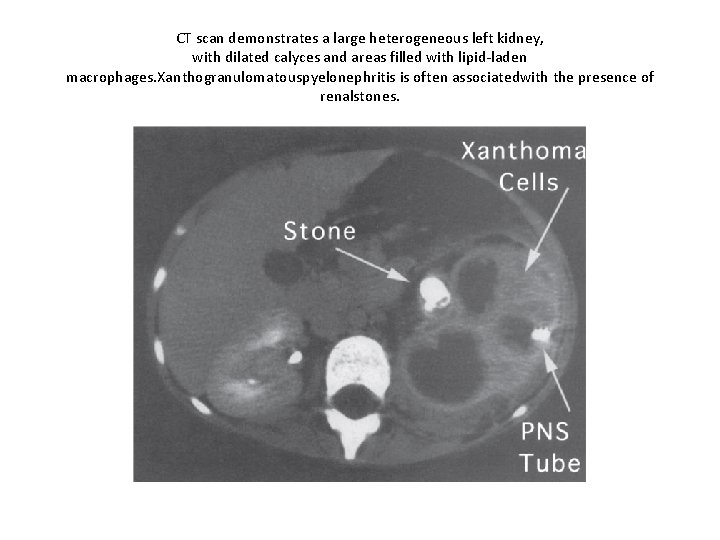
CT scan demonstrates a large heterogeneous left kidney, with dilated calyces and areas filled with lipid-laden macrophages. Xanthogranulomatouspyelonephritis is often associatedwith the presence of renalstones.
- Kidney becomes grossly enlarged, difficult to distinguish from RCC radiologically ( most cases Dx for presumed RCC)
5 - chronic pyelonephritis: - Renal scarring may or may not related to previous infection - Usually due to reflux nephropathy - Scars best diagnosed by …DMSA scan. .
Prostatitis • Infection or inflammation of prostate • NIH classification: 1 - acute bacterial 2 -chronic bacterial: presence of bacteria in prostatic fluid in the absence of a concomitant UTI or significant systemic signs. 3 a-chronic non bacterial inflammatory: no bacteria but there is WBC in prostatic fluid 3 b-chronic non bacterial non inflammatory: no bacteria and no WBC 4 -histological prostatitis ( asymptomatic) diagnosed in Bx
Acute prostatitis • Patients with acute bacterial prostatitis usually present with an abrupt onset of constitutional (fever, chills, malaise, arthralgia, myalgia, lower back/rectal/perineal pain) and urinary symptoms (frequency, urgency, dysuria). They may also present with urinary retention due to swelling of the prostate or obstructive symptoms
• Digital rectal examination reveals a tender, enlarged gland that is irregular and warm and soft in consistency • Serum blood analysis typically demonstrates leukocytosis. Prostate-specific antigen levels are often elevated. • at the onset of acute prostatitis, prostatic massage is seldom suggested because the prostate is quite tender and the massage may lead to bacteremia. Similarly, urethral catheterization should be avoided.
• Urinary retention secondary to acute prostatitis should be managed with a suprapubic catheter because transurethral catheterization or instrumentation is contraindicated • If there is prostatic abscess, transurethral drainage of abscess could be done
Chronic bacterial prostatitis • Most patients with chronic bacterial prostatitis typically present with dysuria, urgency, frequency, nocturia, and low back/ perineal pain. These patients usually are afebrile and commonly have a history of recurrent or relapsing UTI, • digital rectal examination of the prostate is often normal; occasionally, tenderness • Diagnosis is made after identification of bacteria from prostate express secretion or urine specimen after a prostatic massage,
• Management: Using fluoroquinolones, some patients may respond after 4– 6 weeks of treatment, but relapse is not uncommon, requiring the duration of antibiotic therapy to be extended to 3– 4 months
Chronic non bacterial prostatitis • The predominant symptom in all these studies was pain, which was most commonly localized to the perineum, suprapubic area, and penis but can also occur in the testes, groin, or low back. Pain during or after ejaculation is one of the most prominent, important, and bothersome features in many patients • Irritative or obstructive voiding symptom
• antibiotics, α-adrenergic blockers, antiinflammatory agents, may be used for management of CPPS
• Segmented urine culture: -urine localization test 1 - VB 1 : -first 10 ml of voided urine, if positive urethritis 2 -VB 2: -mid urine, if positive cystitis. 3 -EPS: -Prostate massage secretions, positive in prostatitis 4 - VB 3: - first 10 ml of voided urine post prostate massage, positive in prostatitis
 Urinary tract infection
Urinary tract infection Complicated urinary tract infection
Complicated urinary tract infection Urinary tract infection in pregnancy ppt
Urinary tract infection in pregnancy ppt Urised otc
Urised otc What causes uti
What causes uti Histological structure of kidney
Histological structure of kidney Urethra
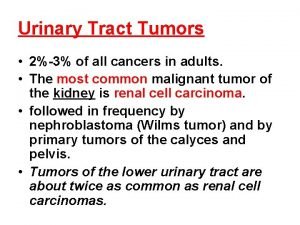
Urethra Tumor in the urinary tract
Tumor in the urinary tract Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Lrti
Lrti Sexually transmitted diseases
Sexually transmitted diseases Extrapyramidal vs pyramidal
Extrapyramidal vs pyramidal Dorsal reticulospinal tract
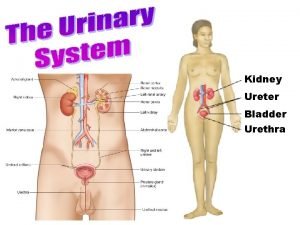
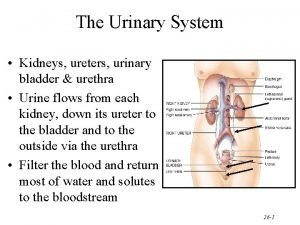
Dorsal reticulospinal tract Urinary system introduction
Urinary system introduction Peylonephritis
Peylonephritis Hominem uti hominem educare oportet
Hominem uti hominem educare oportet Sbar model communication
Sbar model communication Prokov dóra
Prokov dóra Uti discharge pictures
Uti discharge pictures Im safe checklist
Im safe checklist Bso uti pilot
Bso uti pilot Uti swatantra
Uti swatantra Sidcs
Sidcs Urinary
Urinary Uti and pancreatitis
Uti and pancreatitis Uti upper and lower
Uti upper and lower Finale in latino esempi
Finale in latino esempi Utiitsl objection menu
Utiitsl objection menu Uti posidetis juris
Uti posidetis juris Risk factors uti
Risk factors uti Ua uti results
Ua uti results Penicinilase
Penicinilase Uti causes
Uti causes Uti discharge pictures
Uti discharge pictures Cost of macrobid
Cost of macrobid Complicated vs uncomplicated uti
Complicated vs uncomplicated uti Utiitsl psa login
Utiitsl psa login Curarização em uti
Curarização em uti Urinary
Urinary Length of male urethra
Length of male urethra Ureter blood supply
Ureter blood supply Glomerular filtration
Glomerular filtration Trigone of bladder
Trigone of bladder Hyperproteinuria definition
Hyperproteinuria definition Urinary system interesting facts
Urinary system interesting facts Nursing care bundle
Nursing care bundle Urogenital papilla fetal pig
Urogenital papilla fetal pig Chapter 30 the urinary system workbook answers
Chapter 30 the urinary system workbook answers Chapter 22 urinary elimination
Chapter 22 urinary elimination Kidney pyramid labeled
Kidney pyramid labeled Lesson 14.2 male and female urinary structures
Lesson 14.2 male and female urinary structures Order of urine flow through kidney
Order of urine flow through kidney Urinary bladder
Urinary bladder Sustenocytes
Sustenocytes Chapter 25 urinary catheters
Chapter 25 urinary catheters Chapter 24 urinary elimination
Chapter 24 urinary elimination Chapter 22 urinary elimination
Chapter 22 urinary elimination Chapter 20 urinary/excretory system
Chapter 20 urinary/excretory system _____ is difficulty in starting a urinary stream.
_____ is difficulty in starting a urinary stream. Urinary system model
Urinary system model Urinary system model
Urinary system model Nephroureterectomy
Nephroureterectomy Alimentary canal
Alimentary canal Urinary system powerpoint
Urinary system powerpoint Proximal convoluted tubule histology
Proximal convoluted tubule histology