Lower Urinary tract infection Dr AMMAR FADIL UTI
- Slides: 39
Lower Urinary tract infection Dr. AMMAR FADIL
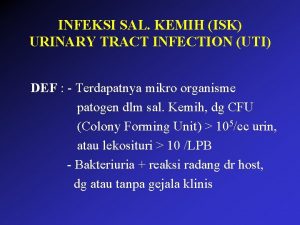
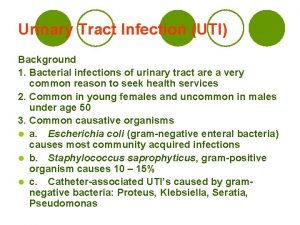
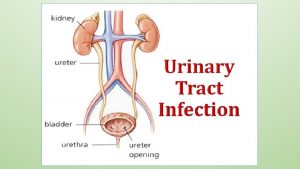
UTI • Urinary tract infection (UTI) is a term that is applied to a variety of clinical conditions ranging from cystitis to severe infection of the kidney with resultant sepsis. 2
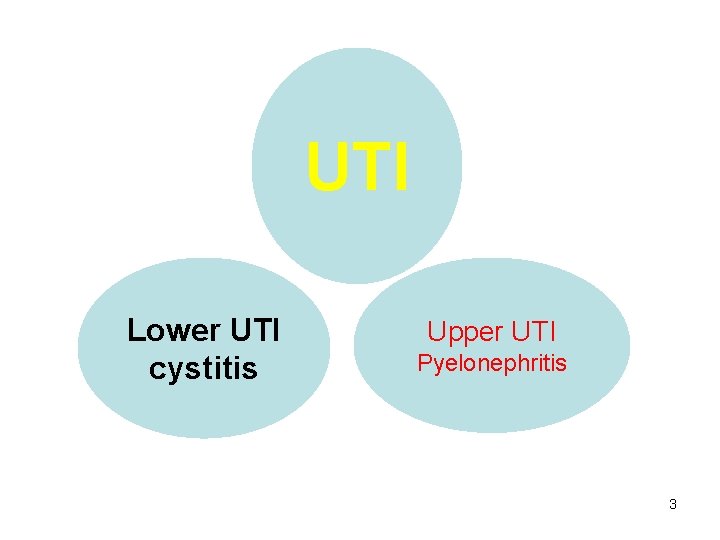
UTI Lower UTI cystitis Upper UTI Pyelonephritis 3
UTI May also be classified as 1. Isolated UTI a single episode of lower tract infection occurs frequently in females and is rarely complicated. 2. Recurrent UTI is >2 infections in 6 months, or 3 within 12 months. 4
Predisposing causes of urinary tract infection • Incomplete emptying of the bladder, bladder outflow obstruction, bladder diverticulum, neurogenic bladder • A calculus, foreign body or neoplasm. • Incomplete emptying of the upper tract, dilatation of the ureters associated with pregnancy, or vesicoureteric reflux VUR. 5
• Oestrogen deficiency, which may give rise to lowered local resistance. • Colonisation of the perineal skin by strains of Escherichia coli expressing molecules that facilitate adherence to mucosa • Diabetes. • Immunosuppression 6
Acute cystitis • urinary infection of the lower urinary tract, principally the bladder. • Acute cystitis. ♂ < ♀ • The primary mode of infection is ascending from the periurethral / vaginal and fecal flora. • The diagnosis is made clinically. 7
PRESENTATION • There is frequent voiding of small volumes, dysuria, urgency, suprapubic pain, hematuria. • 50% of women will have an episode of cystitis in their lifetime – Fever and systemic symptoms are rare. 8
INVESTIGATIONS • Urinalysis WBCs in the urine & hematuria may be present. • Urine culture is required to confirm the diagnosis & identify the causative organism. • However, when the clinical picture & urinalysis are suggestive of the Dx of acute cystitis, urine culture may not be needed. 9
RADIOGRAPHIC IMAGING • In uncomplicated infection of the bladder, radiologic evaluation is often not necessary • recurrent UTI, Fever, UTI in children • US • VCUG 10
Treatment • Management for acute cystitis consists of a short course of oral antibiotics. – TMP SMX – Nitrofurantoin – Quinolones Short oral course 3 -5 d ♀ Days for ♂ & child 7 d 11
Honeymoon Cystitis • Is the term for a UTI that often occurs after sexual activity. Sexual activity can push infecting bacteria into the urethra resulting in an infection. 12
• Recurrent UTI may be due to – Reinfection (i. e. , infection by a different bacteria) or – Bacterial persistence (infection by the same organism). Bacterial persistence is caused by – the presence of bacteria within calculi (e. g. , struvite calculi) – – antimicrobial resistance, patient noncompliance with therapy 13
Recurrent UTI 1. Bacterial persistence presence of bacteria within a site in the urinary tract, leads to repeat episodes of infection. • Such sites include Ø urolithiasis anywhere in the urinary tract, Ø chronic bacterial prostatitis, Ø obstructed or atrophic kidney 14
The recurrent UTIs will not resolve until this underlying problem has been addressed and corrected. e. g. surgical removal of the infected source (such as urinary calculi) 15
Recurrent UTI 2. Reinfections usually occur after a prolonged interval (months) from the previous infection and are often caused by a different organism than the previous infecting bacterium 16
MANAGEMENT • renal ultrasound, CT scan, cystoscopy) to evaluate for a potential source of bacterial persistence. • In the absence of finding an underlying functional or anatomic abnormality, they can be managed in one of the following ways. 17
• Low-dose antibiotic prophylaxis trimethoprim, nitrofurantoin, low-dose cephalexin, and the fluoroquinolones appear to have minimal adverse effects on the fecal and vaginal flora. • Prophylactic therapy requires only a small dose of an antimicrobial agent, generally given at bedtime for 3 to 6 months 18
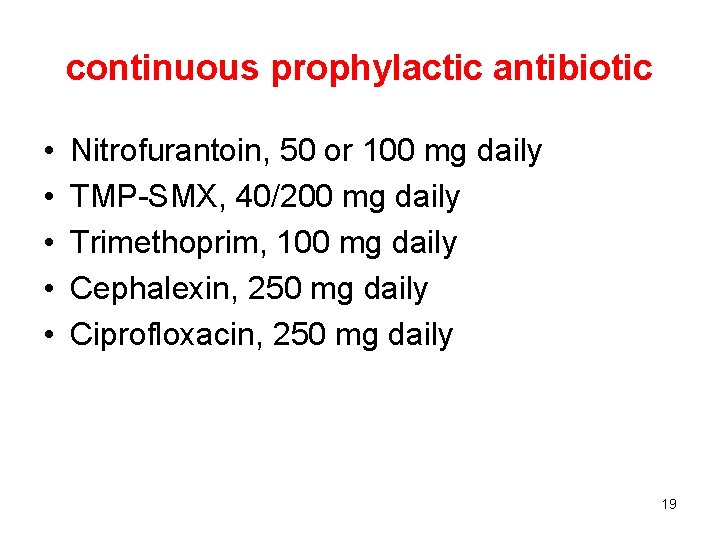
continuous prophylactic antibiotic • • • Nitrofurantoin, 50 or 100 mg daily TMP-SMX, 40/200 mg daily Trimethoprim, 100 mg daily Cephalexin, 250 mg daily Ciprofloxacin, 250 mg daily 19
Recurrent cystitis/ UTI • ♀with reinfection do not usually have an underlying functional or anatomical abnormality. But have higher adherence of bacteria to their mucosal cells compared to women who never had UTI. • ♂ with reinfection may have underlying bladder outlet obstruction (due to prostate enlargement or urethral stricture), which makes them more likely to develop a repeated infection. 20
Other Measures in women – When the recurrent cystitis/UTI is related to sexual activity frequent emptying of the bladder after coitus. – either CPA or post intercourse prophylaxis can significantly reduce the incidence of recurrent infection • Yogurt applied to the vulva and vagina can help restore normal vaginal flora, • Cranberry taken orally 21
Infection in pregnancy • The incidence of asymptomatic bacteriuria in pregnant women is twice as high as in nonpregnant women. • Simple uncomplicated infection can be treated following urine culture with an antibiotic that is not contraindicated in pregnancy, such as cephalosporin or ampicillin. • Pyelonephritis need I. V ABS and close observation. 22
Antibiotics in urology • TMP SMX: – highly effective against many uropathogenes except pseudomonas & entreococcus. – interfere with bacterial metabolism of folate. SE: rash, GIT upset, leukopenia. CI: G 6 PD, pregnant 23
Quinolones • Ciprofloxacin, levofloxacin • broad spectrum, interfere with bacterial DNA. Adverse reactions include tendon damage, arthropathy in children CI: children & pregnant 24
Nitrofurantoin has good activity against most gram –ve except Pseudomonas & proteus. It inhibit bacterial enzymes & DNA activity. SE: polyneuropathy, hepatotoxicity. • Aminoglycosides used for complicated UTI. When combined with ampicilline act against enterococci 25
Cephalosporine Have good activity against most uropathogene. 1 st generation gram positive & E. Coli. 2 nd generation anaerobic & H. influenze. 3 rd generation ceftriaxone , cefotaxim boader coverage against G –ve less against G+ve 4 th generation cefepim oral 3 rd cefixime effective in febrile UTI in children 26
Penicillin • Are ineffective against uropathogene. • Ampicilline & amoxicilline have good activity against uropathogene but G-ve bacteria quickly develop resistance. • Addition of B lactamase inhibitor such as clavulanic acid makes combination more active against G-ve bacteria. 27
Schistosomiasis (bilharziasis) • Urinary schistosomiasis is caused by the Schistoma haematobium. It is endemic in Iraq, Egypt, and the Middle East. • Fresh water bulinus snails release the infective form of the parasite (cercariae), which can penetrate skin, and migrate to the liver (as schistosomules), where they mature. 28
• Adult flukes couple, migrate to vesical veins, and lay eggs , which leave the body by penetrating the bladder and entering the urine. The disease has two stages: • active (when adult worms are actively laying eggs) • inactive (when the adult has died, and there is a reaction to the remaining eggs). The development of squamous cell carcinoma of the bladder is result of the chronic inflammation. 29
Clinical features Swimmer’s itch. • Active inflammation results in hematuria, frequency, and terminal dysuria. 30
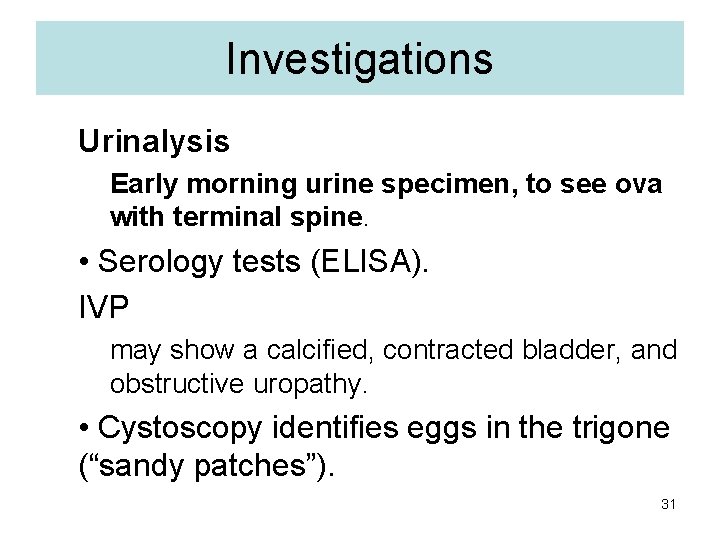
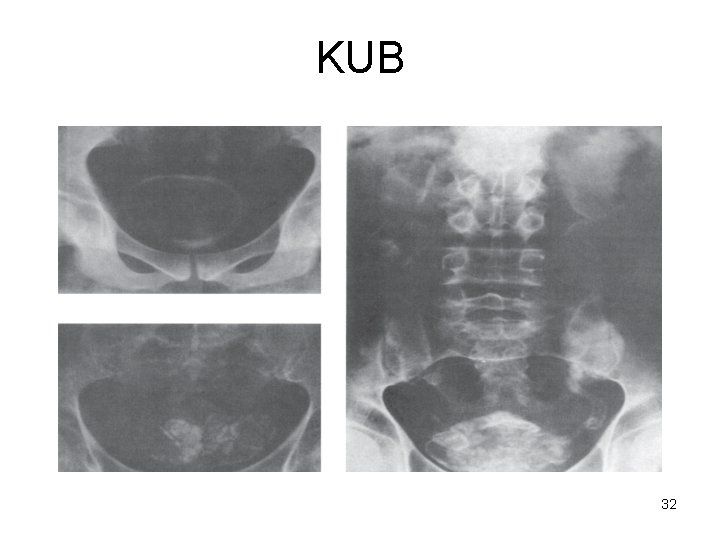
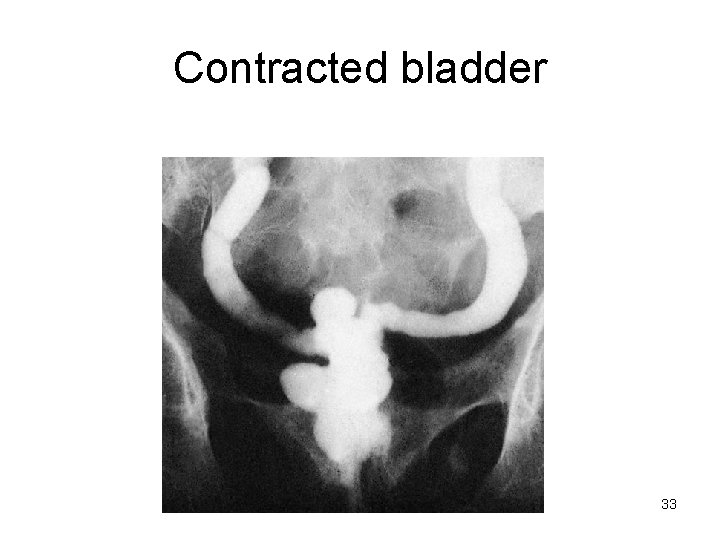
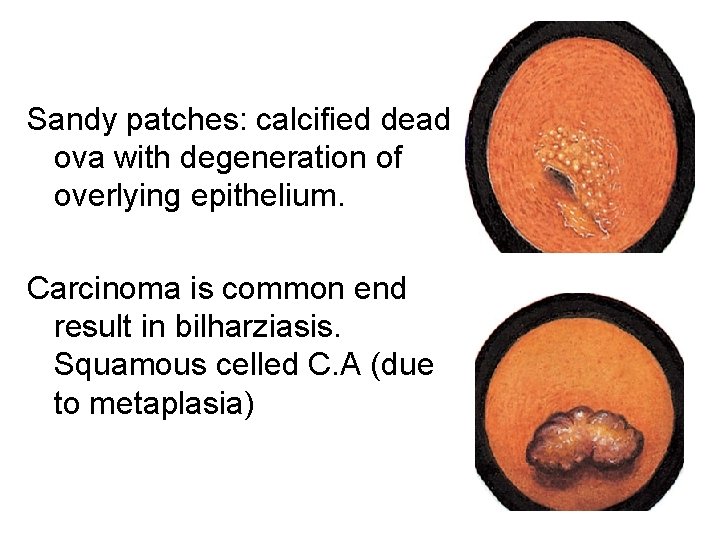
Investigations Urinalysis Early morning urine specimen, to see ova with terminal spine. • Serology tests (ELISA). IVP may show a calcified, contracted bladder, and obstructive uropathy. • Cystoscopy identifies eggs in the trigone (“sandy patches”). 31
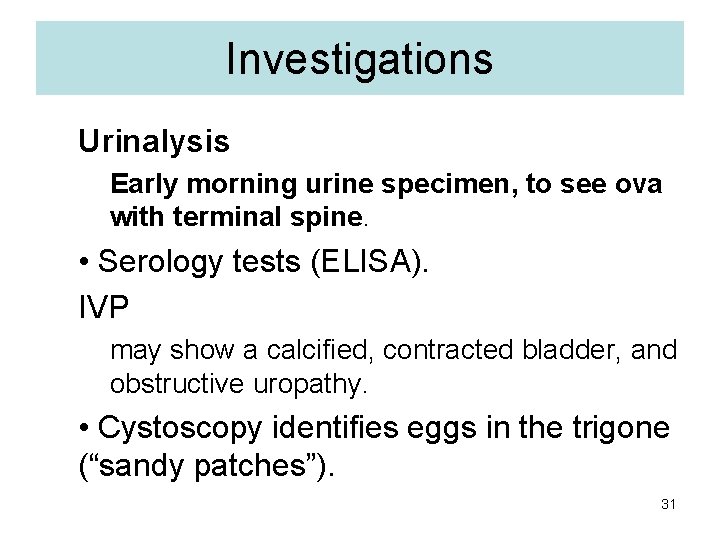
KUB 32
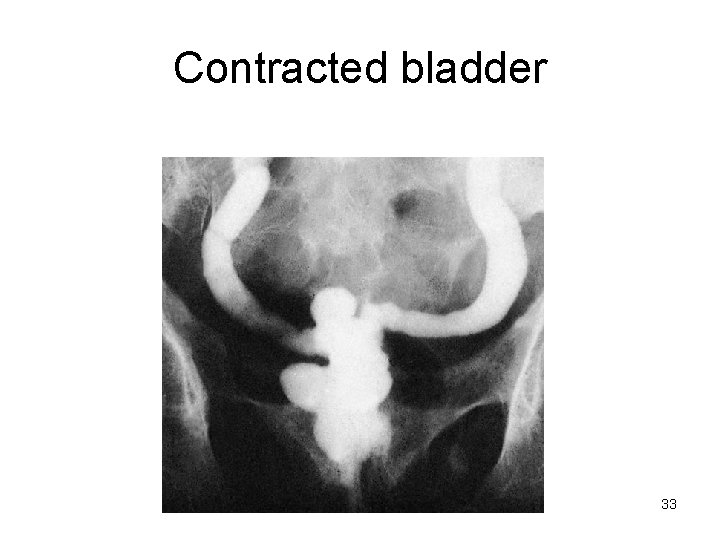
Contracted bladder 33
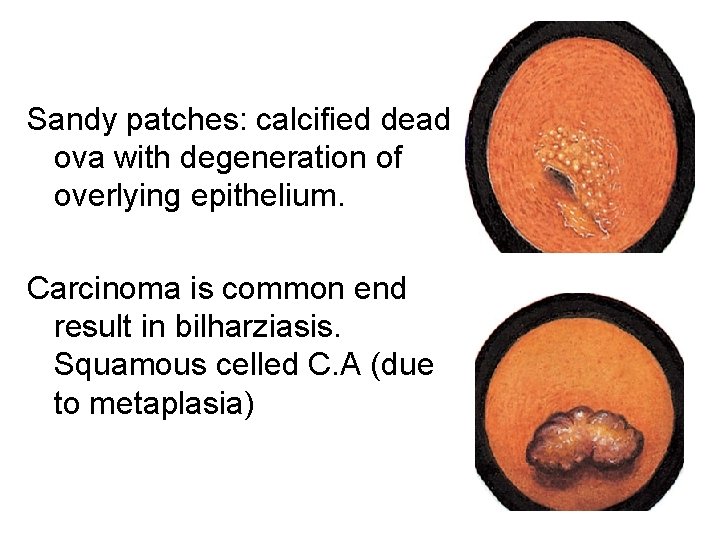
Sandy patches: calcified dead ova with degeneration of overlying epithelium. Carcinoma is common end result in bilharziasis. Squamous celled C. A (due to metaplasia) 34
Complication Chronic infection can lead to obstructive uropathy, ureteric stenosis, renal failure, and bladder contraction. The most significant and concerning complication is the development of squamous cell carcinoma of the bladder that often presents at an advanced stage. 35
Interstitial cystitis/ BPS • Interstitial cystitis (IC). this is confined to women, also known as painful bladder syndrome of unknown etiology • IC is characterized by daytime & night time urinary frequency, urgency, suprapubic pain, no identifiable pathological cause. urinary tract infection are absent. 36
Interstitial cystitis/BPS IC is a diagnosis of exclusion. Urine culture Cystoscopy: characteristic ulcer is found in the fundus. Bladder biopsy 37
treatment • Oral : Amitriptyline, Pentosanpolysulphate, cimitidine • Intravesical: onabotulinum toxin A plus Hydrostatic dilatation under anaesthesia may give relief for some months. 38
• Recurrent UTI due to reinfection treated by lowdose continuous prophylactic antibiotic has been shown to reduce the recurrences of UTI by 95% compared to placebo. 39
 Uti symptoms men
Uti symptoms men Complicated urinary tract infection
Complicated urinary tract infection Urinary tract infection in pregnancy ppt
Urinary tract infection in pregnancy ppt Urised otc
Urised otc Urinary tract infection
Urinary tract infection Uti upper and lower
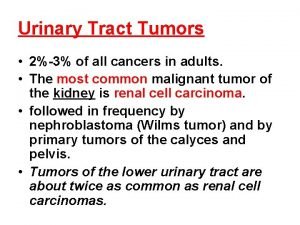
Uti upper and lower Tumor in the urinary tract
Tumor in the urinary tract Urinary tract obstruction
Urinary tract obstruction Urethra
Urethra Nursing management of reproductive tract infection
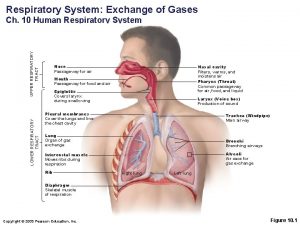
Nursing management of reproductive tract infection Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Conclusion of respiratory tract infection
Conclusion of respiratory tract infection Extrapyramidal vs pyramidal
Extrapyramidal vs pyramidal Dorsal reticulospinal tract
Dorsal reticulospinal tract Lower respiratory tract
Lower respiratory tract Upper and lower respiratory system
Upper and lower respiratory system Structure of the upper respiratory system
Structure of the upper respiratory system Ammar yaseen
Ammar yaseen Hany ammar
Hany ammar Type trophique
Type trophique Fadıl tunçel
Fadıl tunçel How do you spell colleague
How do you spell colleague Dr ammar attiya
Dr ammar attiya Ammar mirascija
Ammar mirascija Ammar pronunciation
Ammar pronunciation Fadıl yıldız
Fadıl yıldız Schéma de construction ciseau
Schéma de construction ciseau Hany ammar
Hany ammar Brahim el fadil
Brahim el fadil Zookeeper ammar
Zookeeper ammar Brahim el fadil
Brahim el fadil Kevin gimpel
Kevin gimpel Hany ammar
Hany ammar Low dose naltrexone walgreens
Low dose naltrexone walgreens Vcayco
Vcayco Utiitsl objection menu
Utiitsl objection menu Sbar examples in business
Sbar examples in business Bactrim for uti
Bactrim for uti Bso uti pilot
Bso uti pilot Complicated vs uncomplicated uti
Complicated vs uncomplicated uti