The physiology of edema DR JOEL SOLORZANO Edema

- Slides: 27
The physiology of edema. DR JOEL SOLORZANO
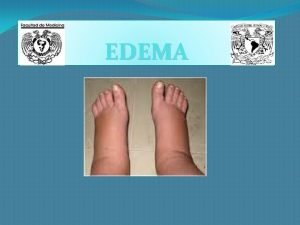
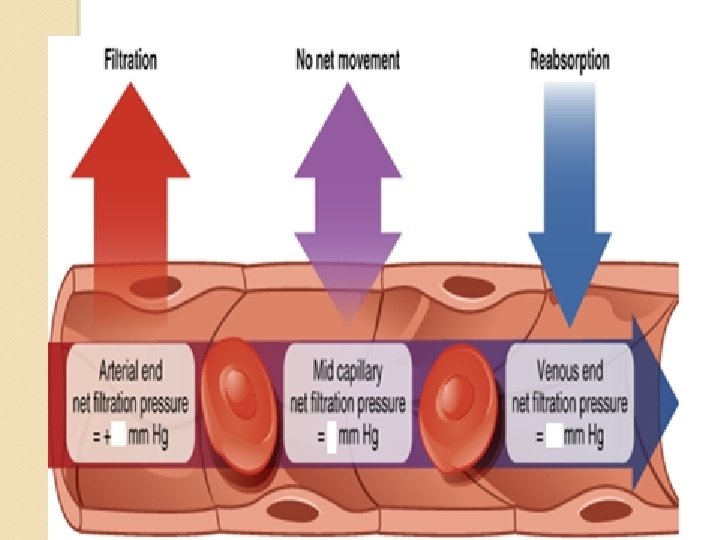
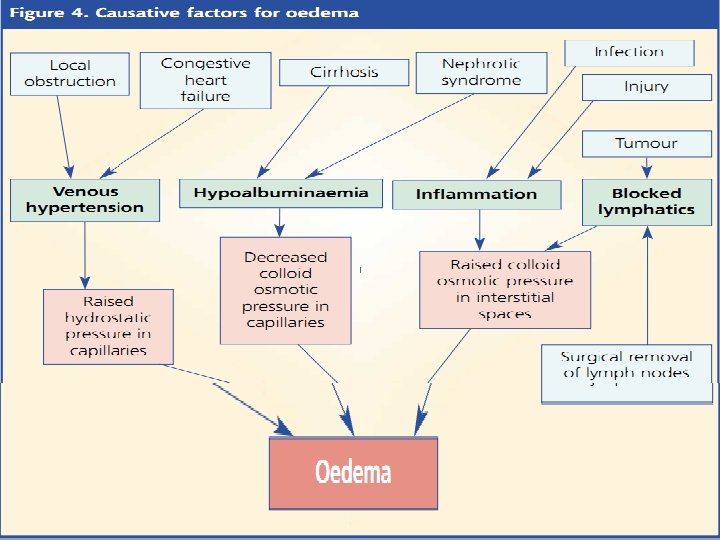
Edema: • The abnormal accumulation of fluid in a specific organ vs generalized. • In capillary: Balance between hydrostatic pressure and oncotic (colloid osmotic) pressure.
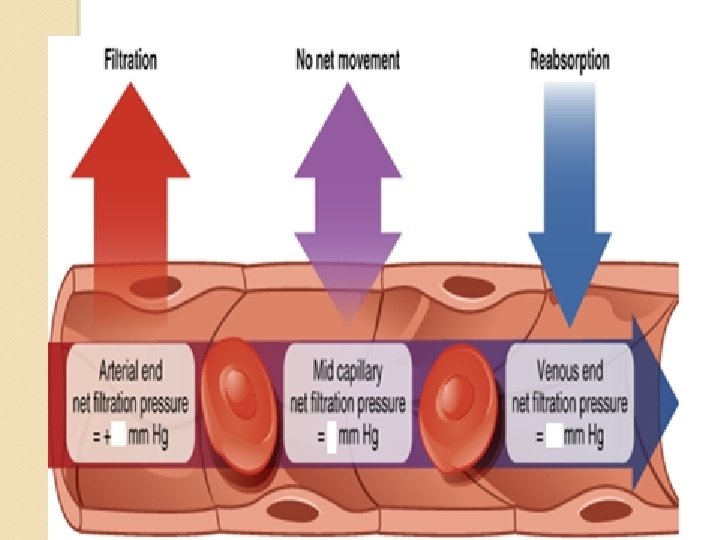
Hydrostatic pressure: • Intra-capillary vs interstitial • Capillary pressures vary: • Nail bed capillaries: 32 mm. Hg at arteriolar end and 15 mm. Hg at venous end. Mean 25 mm. Hg. • Hydrostatic pressure gradient: • Intra-capillary hydrostatic pressure – interstitial fluid hydrostatic pressure
Interstitial hydrostatic pressure: • Varies from one organ to another: • Subcutaneous tissue: Subatmospheric (-2 mm. Hg) • Liver, kidney: + • Brain: As high as 6 mm. Hg
Oncotic pressure: • Capillary wall usually impermeable to plasma proteins and other colloids. • Only water and small solutes cross capillary wall. • Crystalloids vs colloids
• These colloids exert an osmotic pressure of about 25 mm. Hg. • The colloid osmotic pressure due to the plasma colloids=oncotic pressure.
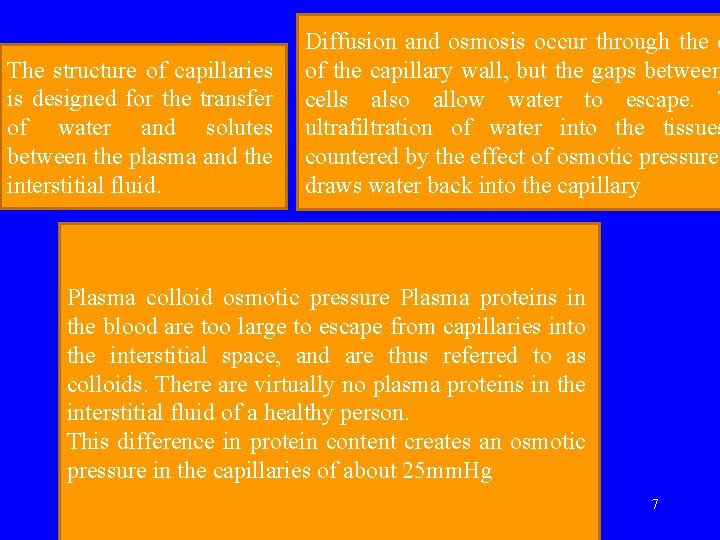
The structure of capillaries is designed for the transfer of water and solutes between the plasma and the interstitial fluid. Diffusion and osmosis occur through the c of the capillary wall, but the gaps between cells also allow water to escape. T ultrafiltration of water into the tissues countered by the effect of osmotic pressure draws water back into the capillary Plasma colloid osmotic pressure Plasma proteins in the blood are too large to escape from capillaries into the interstitial space, and are thus referred to as colloids. There are virtually no plasma proteins in the interstitial fluid of a healthy person. This difference in protein content creates an osmotic pressure in the capillaries of about 25 mm. Hg 7
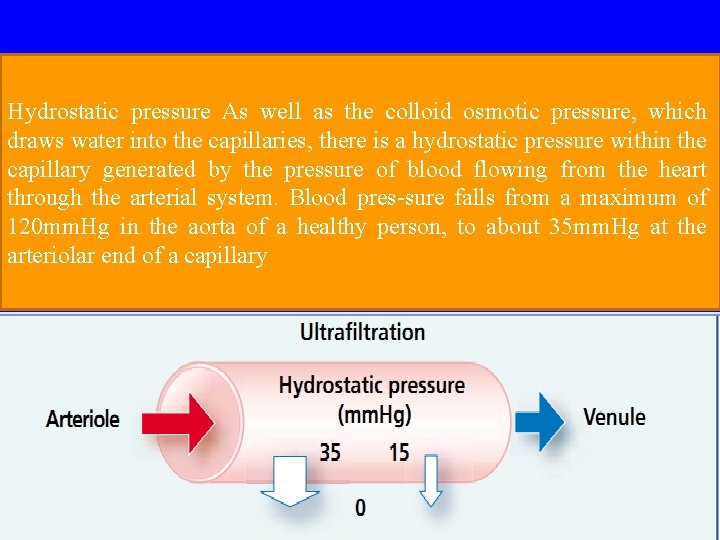
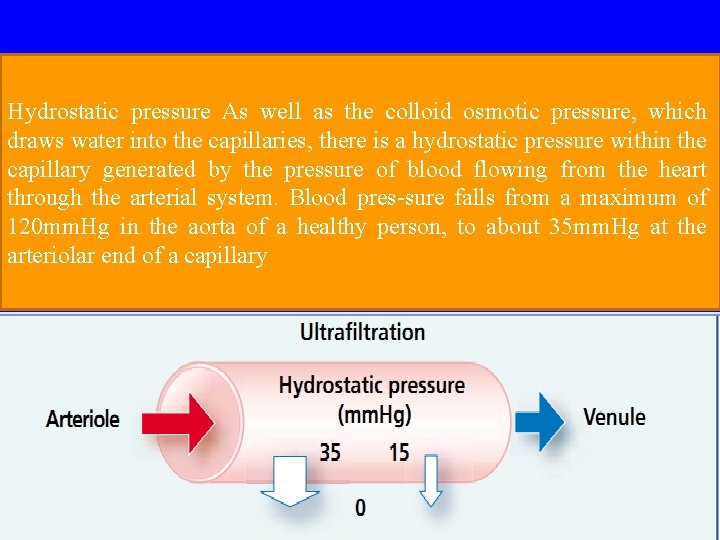
Hydrostatic pressure As well as the colloid osmotic pressure, which draws water into the capillaries, there is a hydrostatic pressure within the capillary generated by the pressure of blood flowing from the heart through the arterial system. Blood pres-sure falls from a maximum of 120 mm. Hg in the aorta of a healthy person, to about 35 mm. Hg at the arteriolar end of a capillary 8
9
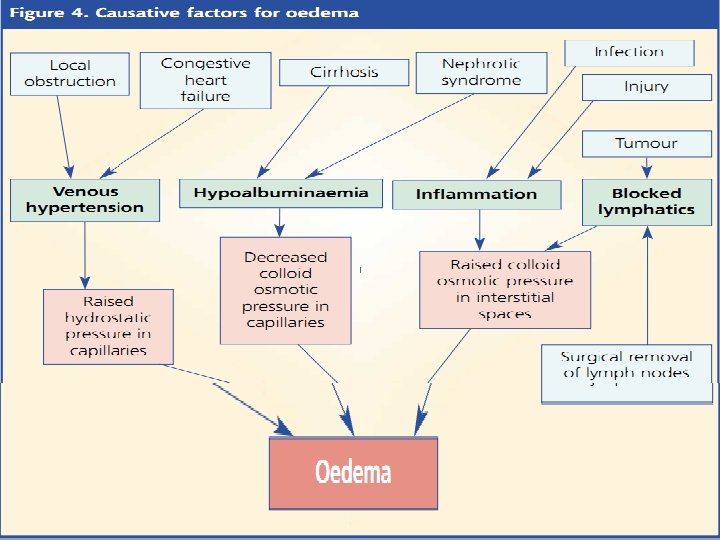
Edema: • Due to disturbance in hydrostatic and/or oncotic pressure between intra-capillary and interstitial component.
Organ specific: • Brain: Cerebral edema • Lung: Intra-alveolar=pulmonary edema, intra-pleural=pleural effusion • Peritoneum=ascites • Severe generalized edema=anasarca
Reduced oncotic pressure: • Reduction in production of colloids--plasma proteins. • Liver failure • Malnutrition
• Increase in loss of colloids--- plasma proteins. • Nephrotic syndrome • Catabolic states
Increase capillary hydrostatic pressure: • Venous end: Heart failure, deep venous thrombosis, superior vena cava obstruction etc. • Arterial end: Pre-capillary dilatation. Calcium channel blockers.
Increased interstitial oncotic pressure: • Lymphatic obstruction: • Primary vs secondary group.
Capillary leaks: • Result of capillary damage: • Pleura: Infections, tumors • Alveoli: Inhalation of noxious substance, eg chlorine gas etc
Diverse causes of edema: • Anaemia • Hypothyroidism

Hormones involved in edema: • Renin angiotensin aldosterone system: secondary hyperaldosteronism • ADH (Vasopressin) • ANP
Clinical physiological approach to edema: • Hypervolemia: • Vs • Normovolemia:
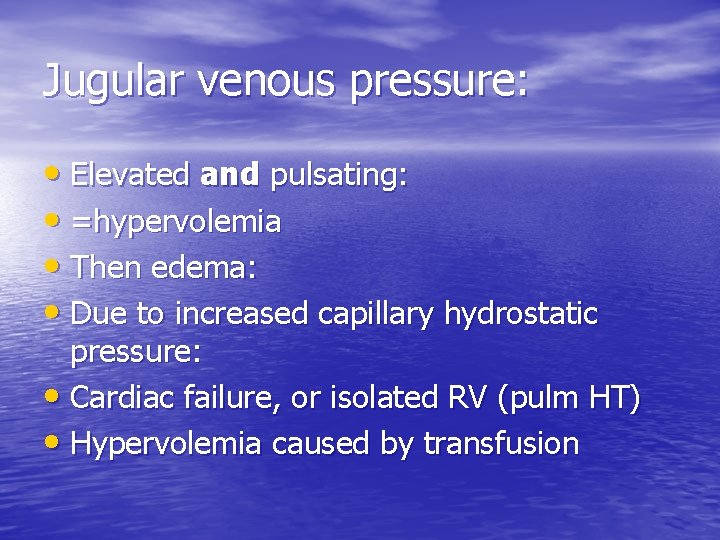
Jugular venous pressure: • Elevated and pulsating: • =hypervolemia • Then edema: • Due to increased capillary hydrostatic pressure: • Cardiac failure, or isolated RV (pulm HT) • Hypervolemia caused by transfusion
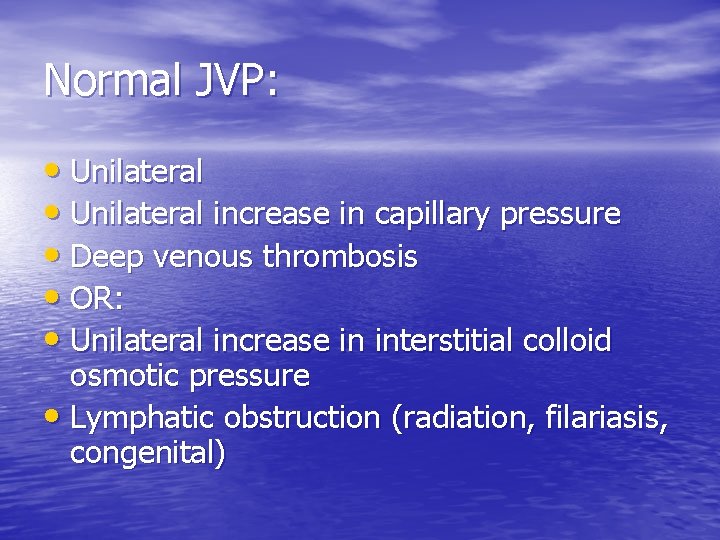
Normal JVP: • Unilateral increase in capillary pressure • Deep venous thrombosis • OR: • Unilateral increase in interstitial colloid osmotic pressure • Lymphatic obstruction (radiation, filariasis, congenital)
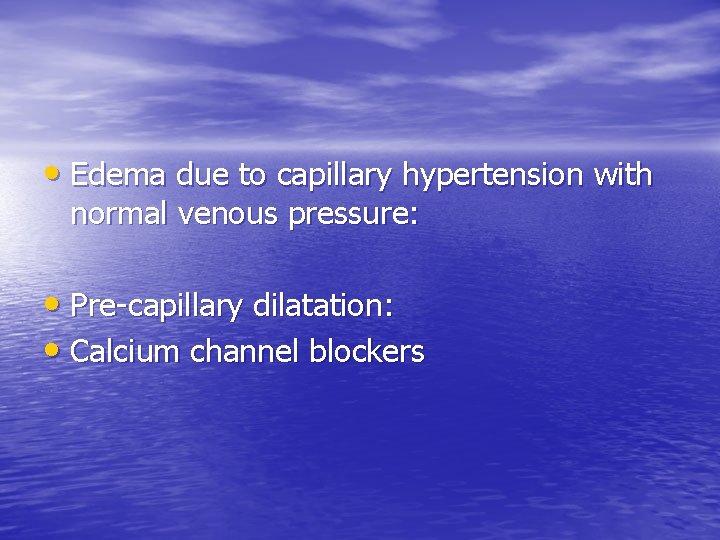
• Edema due to capillary hypertension with normal venous pressure: • Pre-capillary dilatation: • Calcium channel blockers
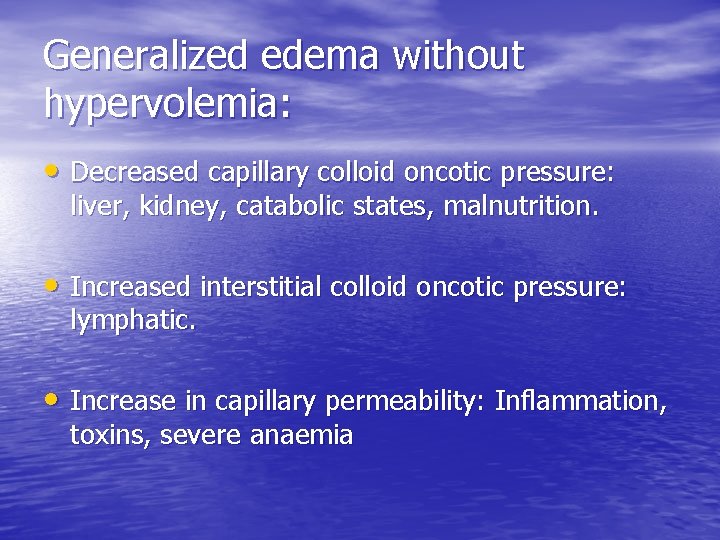
Generalized edema without hypervolemia: • Decreased capillary colloid oncotic pressure: liver, kidney, catabolic states, malnutrition. • Increased interstitial colloid oncotic pressure: lymphatic. • Increase in capillary permeability: Inflammation, toxins, severe anaemia
Pressure changes in the heart: • Atria: Study curve in Ganong: jugular venous pressure curve, also known as flobogram, indicative of pressure changes in superior vena cava/ right atrium. • 3 waves in the curve:
• a-wave: atrial systole • c-wave: bulging of tricuspid valve into R atrium • v-wave: rise in atrial pressure, just before tricuspid valve opens during diastole. • Clinical application of these 3 waves:
• Sinus rhythm or not. • Pulmonary hypertension • 3`rd degree heart block • Patency between SVC and RA • Tricuspid regurgitation and stenosis
 Super coffee franquicia
Super coffee franquicia Tanya solorzano
Tanya solorzano Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan điện thế nghỉ
điện thế nghỉ Fecboak
Fecboak Một số thể thơ truyền thống
Một số thể thơ truyền thống Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Hệ hô hấp
Hệ hô hấp Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Các số nguyên tố
Các số nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy ưu thế lai là gì
ưu thế lai là gì Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Tư thế ngồi viết
Tư thế ngồi viết Thẻ vin
Thẻ vin Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Gấu đi như thế nào
Gấu đi như thế nào Tư thế ngồi viết
Tư thế ngồi viết V cc
V cc Thể thơ truyền thống
Thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Hổ đẻ mỗi lứa mấy con
Hổ đẻ mỗi lứa mấy con Ng-html
Ng-html