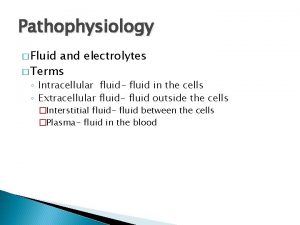
Edema Excess fluid in the tissues Intracellular Edema
- Slides: 14
Edema • Excess fluid in the tissues Ø Intracellular Edema Ø Extracellular Edema
Intracellular Edema 1) Hyponatremia (2) Depression of the metabolic systems of the tissues (3) Lack of adequate nutrition to the cells 4) Intracellular edema can also occur in inflamed tissues. Inflammation usually increases cell membrane permeability
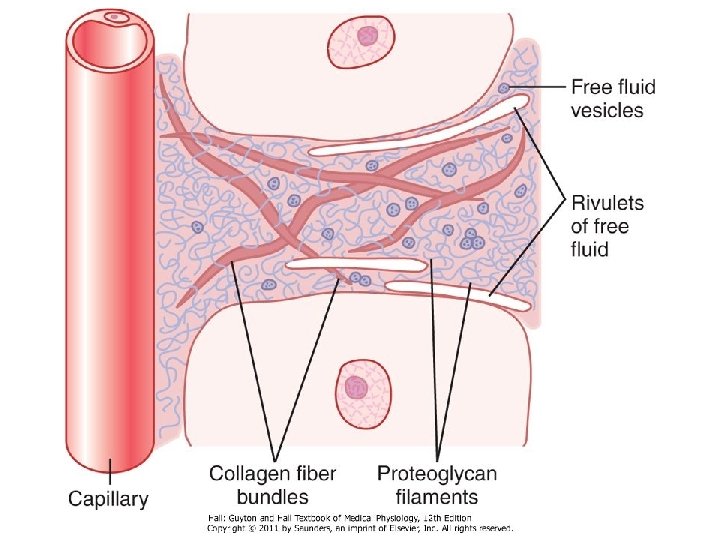
Extracellular Edema • Excess fluid accumulation in the extracellular spaces qabnormal leakage of fluid from the plasma to the interstitial spaces across the capillaries q failure of the lymphatics to return fluid from the interstitium back into the blood called lymphedema
Capillary Filtration
Factors That Can Increase Capillary Filtration • Increased capillary filtration coefficient • Increased capillary hydrostatic pressure. • Decreased plasma colloid osmotic pressure
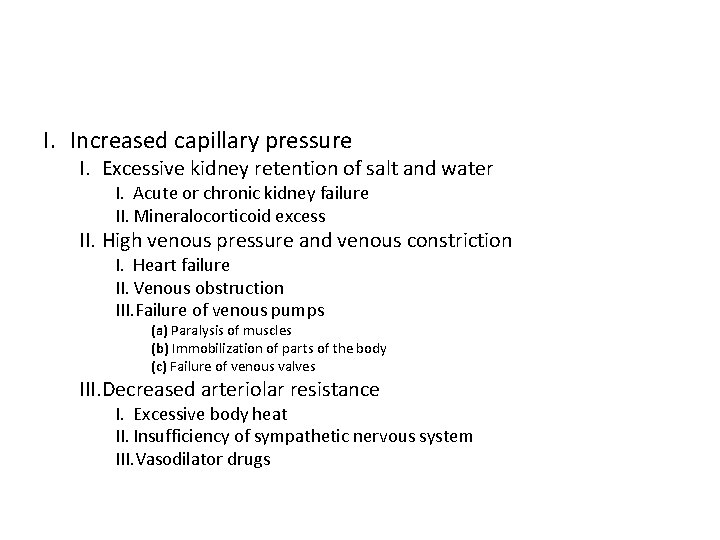
I. Increased capillary pressure I. Excessive kidney retention of salt and water I. Acute or chronic kidney failure II. Mineralocorticoid excess II. High venous pressure and venous constriction I. Heart failure II. Venous obstruction III. Failure of venous pumps (a) Paralysis of muscles (b) Immobilization of parts of the body (c) Failure of venous valves III. Decreased arteriolar resistance I. Excessive body heat II. Insufficiency of sympathetic nervous system III. Vasodilator drugs
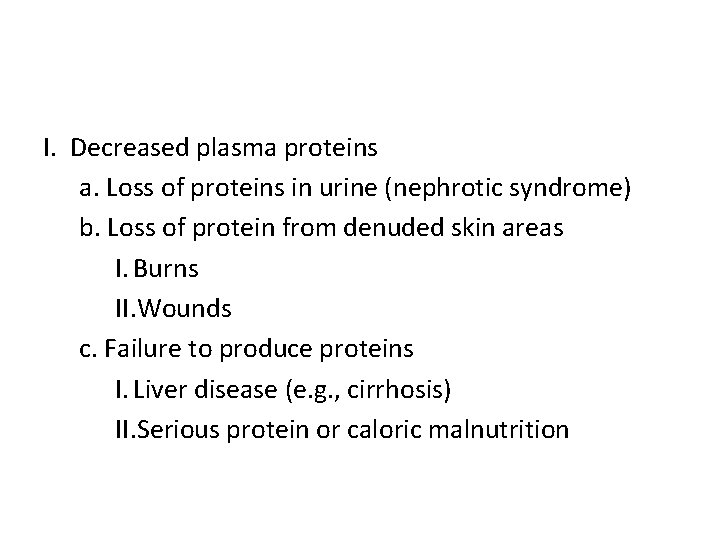
I. Decreased plasma proteins a. Loss of proteins in urine (nephrotic syndrome) b. Loss of protein from denuded skin areas I. Burns II. Wounds c. Failure to produce proteins I. Liver disease (e. g. , cirrhosis) II. Serious protein or caloric malnutrition
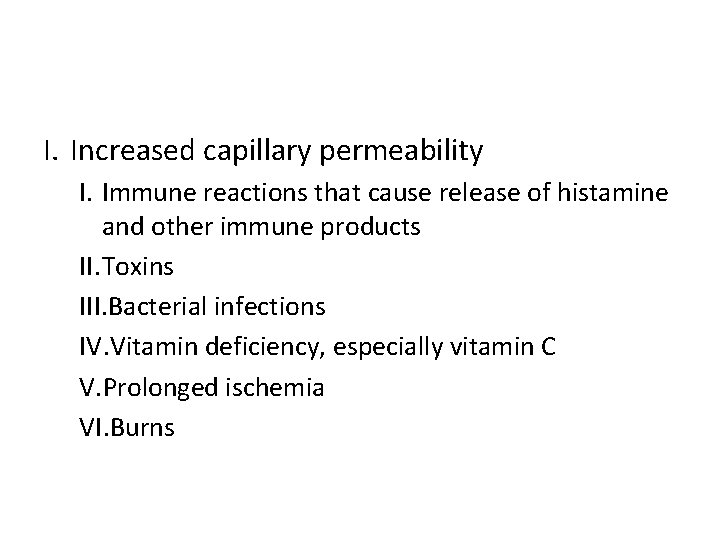
I. Increased capillary permeability I. Immune reactions that cause release of histamine and other immune products II. Toxins III. Bacterial infections IV. Vitamin deficiency, especially vitamin C V. Prolonged ischemia VI. Burns
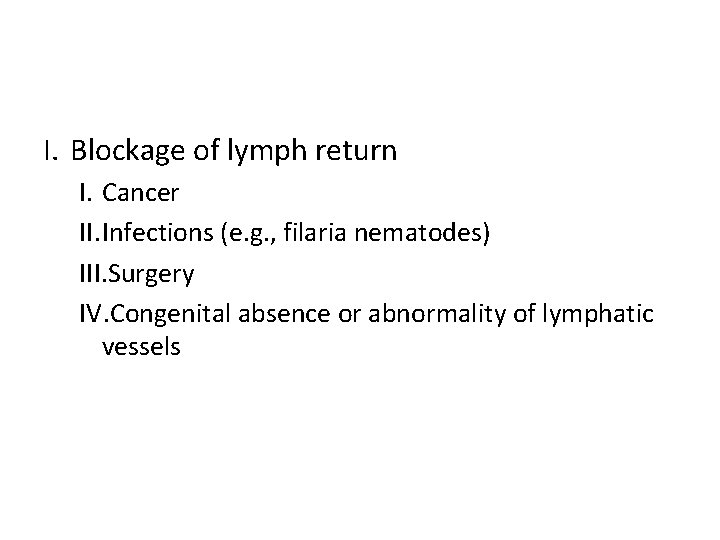
I. Blockage of lymph return I. Cancer II. Infections (e. g. , filaria nematodes) III. Surgery IV. Congenital absence or abnormality of lymphatic vessels
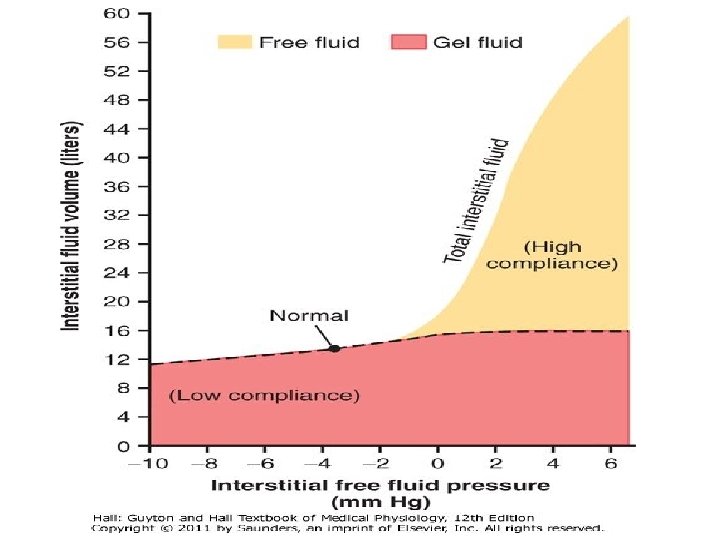
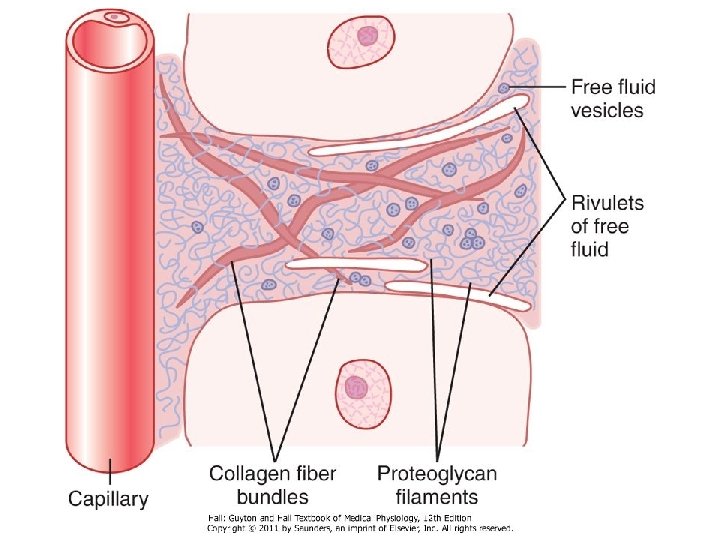
Safety Factors That Normally Prevent Edema (1) low compliance of the interstitium when interstitial fluid pressure is in the negative pressure range (2) the ability of lymph flow to increase 10 - to 50 -fold (3) washdown of interstitial fluid protein concentration which reduces interstitial fluid colloid osmotic pressure
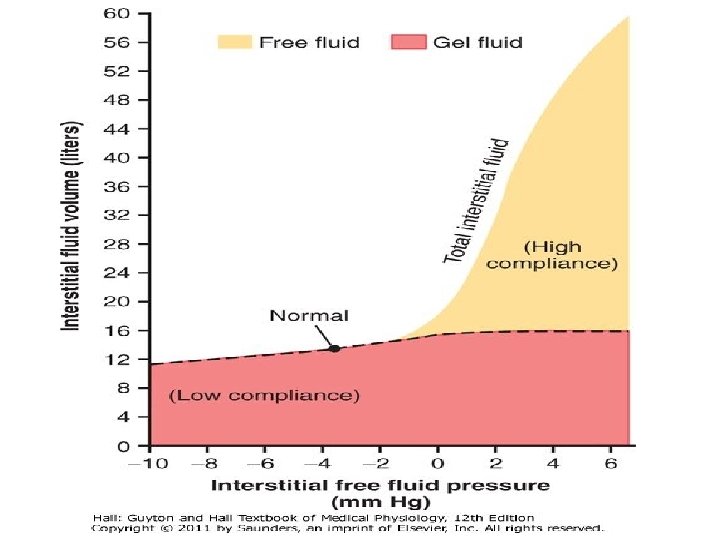
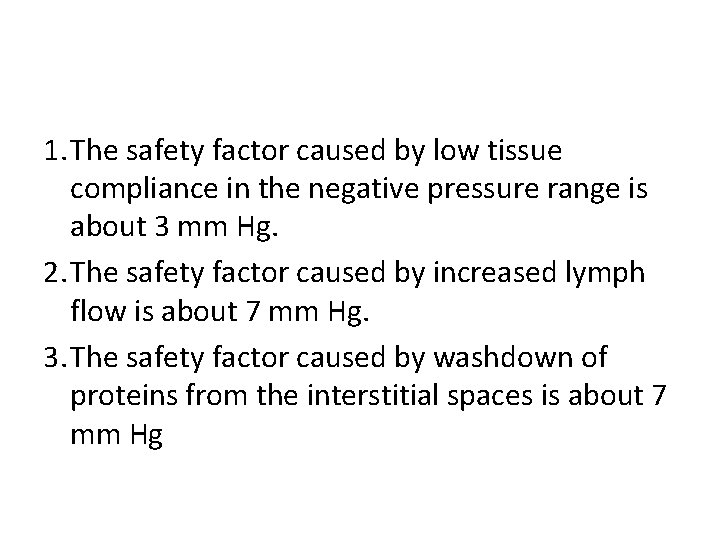
1. The safety factor caused by low tissue compliance in the negative pressure range is about 3 mm Hg. 2. The safety factor caused by increased lymph flow is about 7 mm Hg. 3. The safety factor caused by washdown of proteins from the interstitial spaces is about 7 mm Hg
• The total safety factor against edema is about 17 mm Hg • This means that the capillary pressure in a peripheral tissue could theoretically rise by 17 mm Hg before marked edema would occur
 Fluid compartments in the body
Fluid compartments in the body Eisonophil
Eisonophil Body tissues chapter 3 cells and tissues
Body tissues chapter 3 cells and tissues Stained cheek cell
Stained cheek cell Chapter 3 cells and tissues body tissues
Chapter 3 cells and tissues body tissues Body tissues chapter 3 cells and tissues
Body tissues chapter 3 cells and tissues Ecf icf and interstitial fluid
Ecf icf and interstitial fluid Intracellular extracellular fluid
Intracellular extracellular fluid Intracellular hormone binding
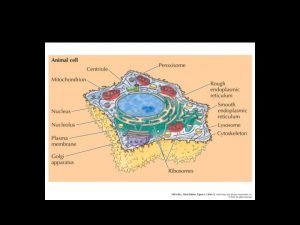
Intracellular hormone binding Intracellular structure
Intracellular structure Interstitial vs intracellular
Interstitial vs intracellular Intracellular receptors
Intracellular receptors Youtube.com
Youtube.com Intracellular and extracellular
Intracellular and extracellular Intracellular proteins
Intracellular proteins