PNEUMONIA LECTURER INTERNAL MEDICINE JOEL SOLORZANO ROMERO CONTROL



![CRB 65 score for mortality risk assessment in primary care[a] CRB 65 score is CRB 65 score for mortality risk assessment in primary care[a] CRB 65 score is](https://slidetodoc.com/presentation_image_h/fde6774ee55e6117cfa7d047d979fe35/image-24.jpg)

- Slides: 38
PNEUMONIA LECTURER. INTERNAL MEDICINE. JOEL SOLORZANO ROMERO
CONTROL QUESTION • Which one of the following is a predictor of poor outcome in patients with infective endocarditis? • A. Insulin-dependent diabetes mellitus • B. Renal failure • C. Echocardiographic evidence of peri-annular complications • D. Staphylococcus aureus in blood cultures • E. All the above
OUTLINES – Definition – Classification of pneumonia – Mode of transmission – Predisposing factors – Pathophysiology – Clinical manifestations – Diagnostic tests – Medical management – Preventive measures – Prognosis – Complications
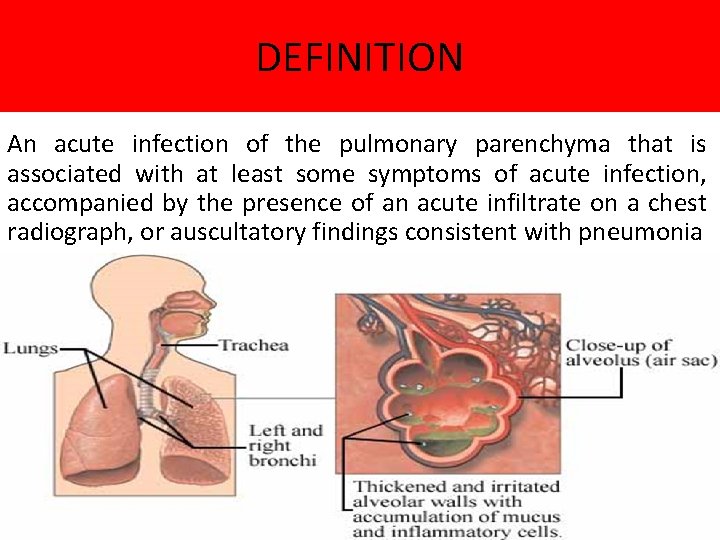
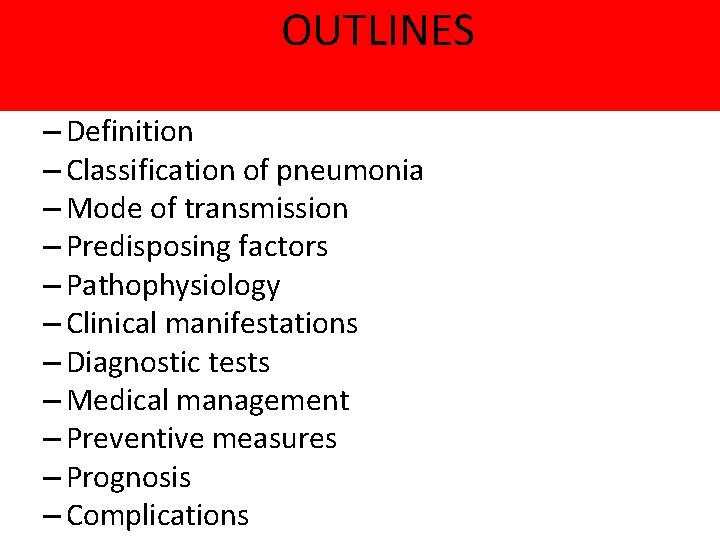
DEFINITION An acute infection of the pulmonary parenchyma that is associated with at least some symptoms of acute infection, accompanied by the presence of an acute infiltrate on a chest radiograph, or auscultatory findings consistent with pneumonia
CLASIFICATION: ACCORDING TO CAUSES Bacterial (the most common cause of pneumonia) Viral pneumonia Fungal pneumonia Chemical pneumonia (ingestion of kerosene or inhalation of irritating substance) • Inhalation pneumonia (aspiration pneumonia) • •
ACCORDING TO AREAS INVOLVED Lobar pneumonia; if one or more lobe is involved Broncho-pneumonia; the pneumonic process has originated in one or more bronchi and extends to the surrounding lung tissue. Intersticial
ACCORDING CLINICAL PICTURES • TYPICAL • ATYPICAL
OTHERS DEFINITION Community-acquired pneumonia Pneumonia that is acquired outside hospital. Pneumonia that develops in a nursing home resident is included in this definition. Hospital-acquired pneumonia: Pneumonia that develops 48 hours or more after hospital admission and that was not incubating at hospital admission. VAP: Ventilator-associated pneumonia ≥ 48 h from endotracheal intubation HCAP: Healthcare-associated pneumonia Long-term care facility (NH), hemodialysis, outpatient chemo, wound care, etc.
PREDISPOSING FACTORS • Immuno-suppresed patients • Cigarette smoking • Difficult swallowing (due to stroke, dementia, parkinsons disease, or other neurological conditions) • Impaired consciousness ( loss of brain function due to dementia, stroke, or other neurological conditions)
PREDISPOSING FACTORS • Chronic lung disease (COPD, bronchostasis) • Frequent suction • Other serious illness such as heart disease, liver cirrhosis, and DM
PATHOPHYSIOLOGY Inhalation, aspiration and hematogenous spread are the 3 main mechanisms by which bacteria reaches the lungs The agents reach the alveoli and lead to inflammation and pouring of an exudates into the air spaces. WBCs migrates to alveoli, the alveoli become more thick due to its filling consolidation, involved areas by inflammation are not adequately ventilated, due to secretion and edema. This will lead to partial occlusion of alveoli and bronchi causing a decrease in alveolar oxygen content.


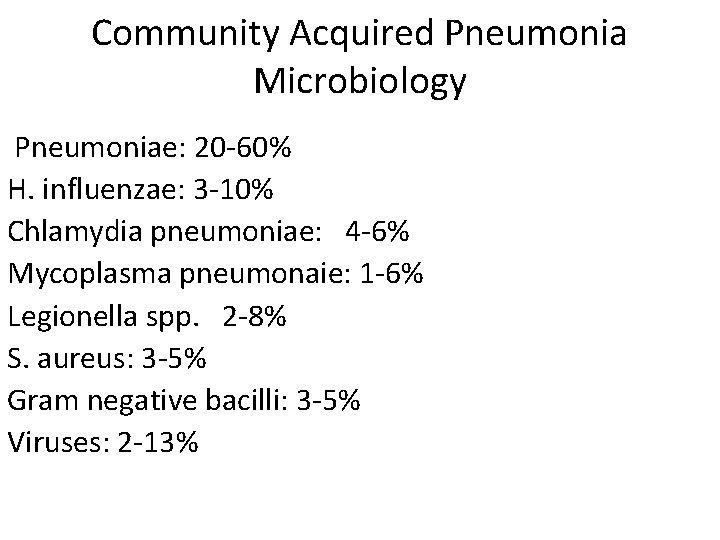
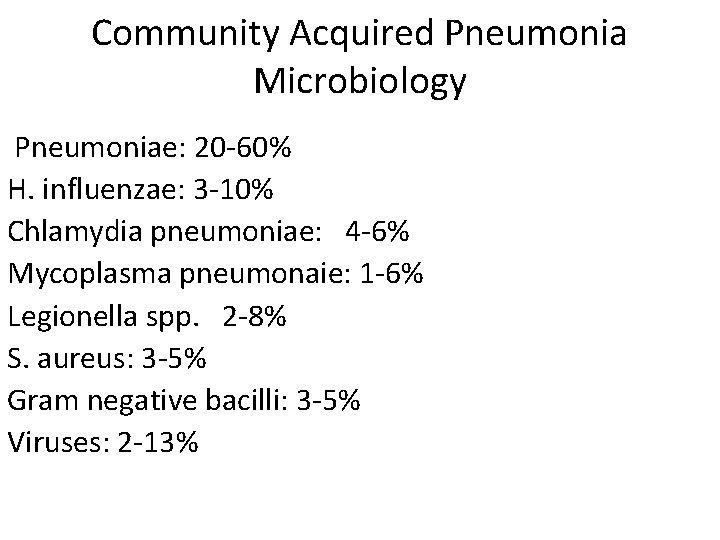
Community Acquired Pneumonia Microbiology Pneumoniae: 20 -60% H. influenzae: 3 -10% Chlamydia pneumoniae: 4 -6% Mycoplasma pneumonaie: 1 -6% Legionella spp. 2 -8% S. aureus: 3 -5% Gram negative bacilli: 3 -5% Viruses: 2 -13%
MOST COMMON CAUSE OF CAP About 2/3 of CAP are due to S. pneumoniae These are gram positive diplococci Typical symptoms (e. g. malaise, shaking chills fever, rusty sputum, pleuritic chest pain, cough) Lobar infiltrate on CXR May be Immuno suppressed host 25% will have bacteremia – serious effects
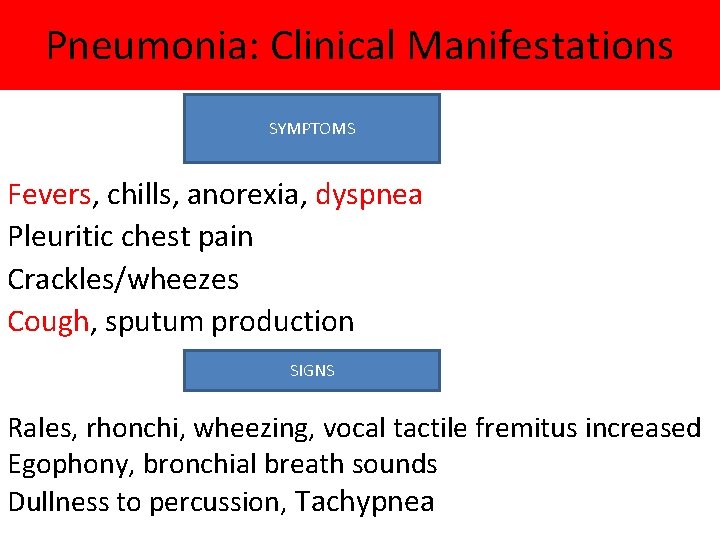
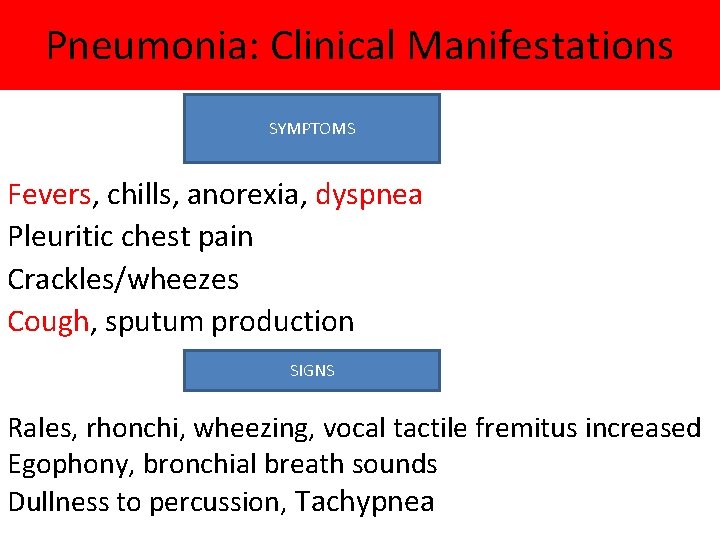
Pneumonia: Clinical Manifestations SYMPTOMS Fevers, chills, anorexia, dyspnea Pleuritic chest pain Crackles/wheezes Cough, sputum production SIGNS Rales, rhonchi, wheezing, vocal tactile fremitus increased Egophony, bronchial breath sounds Dullness to percussion, Tachypnea
Atypical Pneumonia • Commonly associated with milder Sx’s: subacute onset, non-productive cough, no focal infiltrate on CXR, headache, sore throat, diarrhea
OTHER AGENTS Anaerobes Aspiration-prone Pt, putrid sputum, dental disease Gram negative Klebsiella - alcoholics Branhamella catarrhalis - sinus disease, otitis, COPD H. influenza
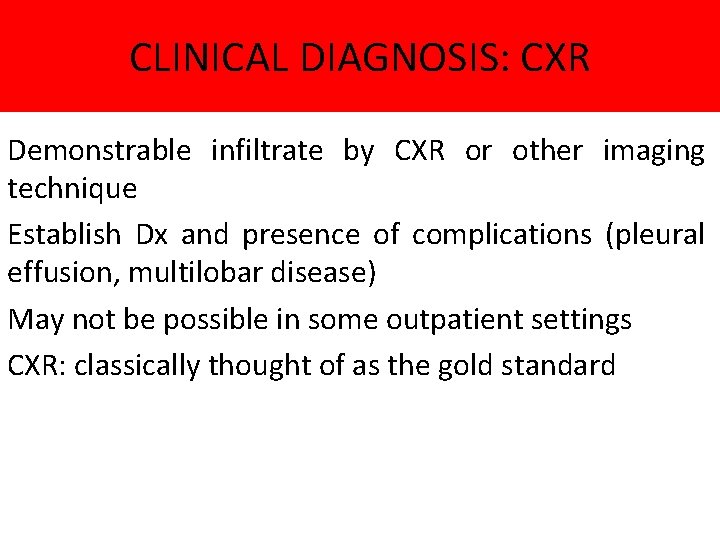
CLINICAL DIAGNOSIS: CXR Demonstrable infiltrate by CXR or other imaging technique Establish Dx and presence of complications (pleural effusion, multilobar disease) May not be possible in some outpatient settings CXR: classically thought of as the gold standard

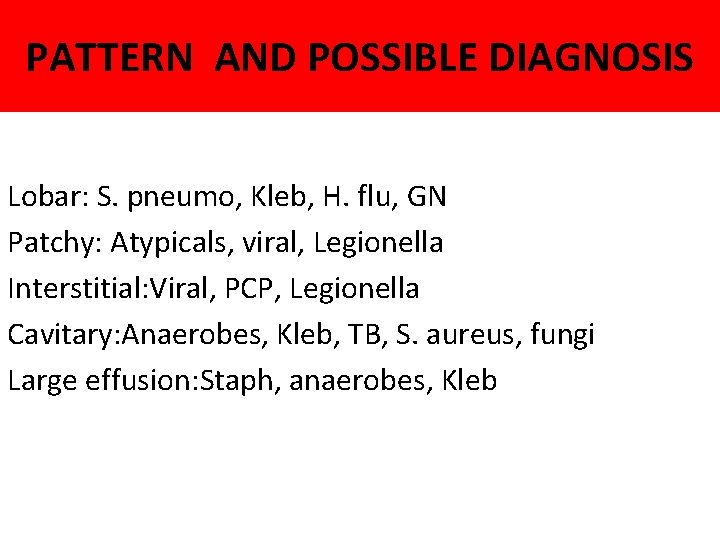
PATTERN AND POSSIBLE DIAGNOSIS Lobar: S. pneumo, Kleb, H. flu, GN Patchy: Atypicals, viral, Legionella Interstitial: Viral, PCP, Legionella Cavitary: Anaerobes, Kleb, TB, S. aureus, fungi Large effusion: Staph, anaerobes, Kleb
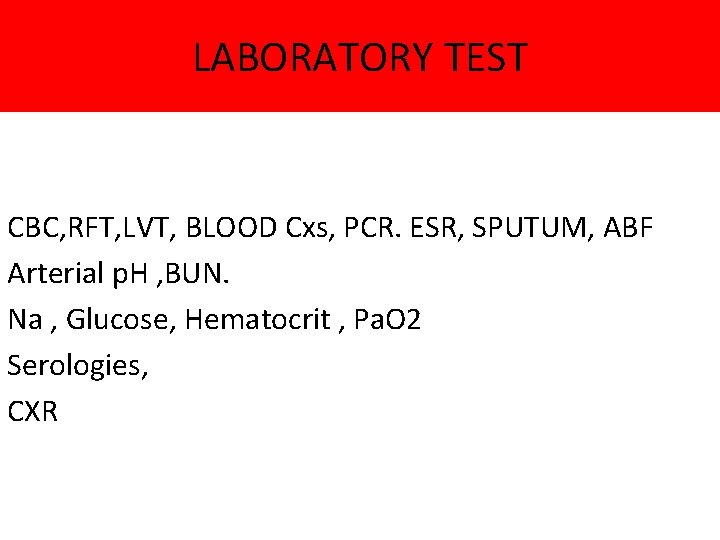
LABORATORY TEST CBC, RFT, LVT, BLOOD Cxs, PCR. ESR, SPUTUM, ABF Arterial p. H , BUN. Na , Glucose, Hematocrit , Pa. O 2 Serologies, CXR
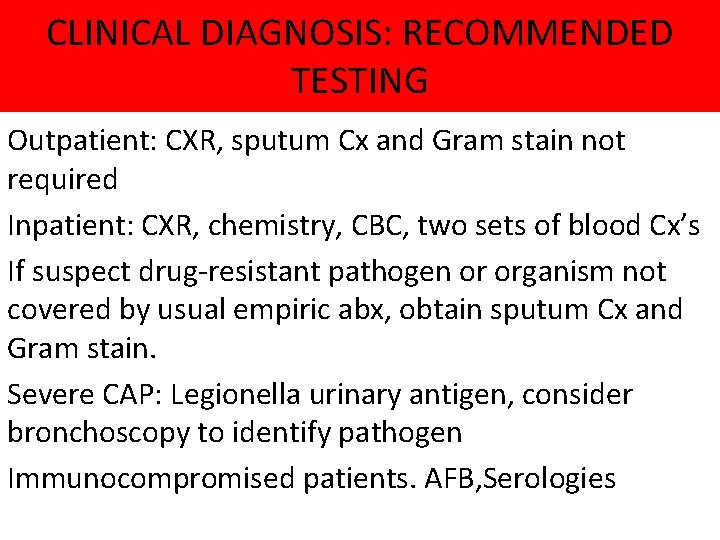
CLINICAL DIAGNOSIS: RECOMMENDED TESTING Outpatient: CXR, sputum Cx and Gram stain not required Inpatient: CXR, chemistry, CBC, two sets of blood Cx’s If suspect drug-resistant pathogen or organism not covered by usual empiric abx, obtain sputum Cx and Gram stain. Severe CAP: Legionella urinary antigen, consider bronchoscopy to identify pathogen Immunocompromised patients. AFB, Serologies
![CRB 65 score for mortality risk assessment in primary carea CRB 65 score is CRB 65 score for mortality risk assessment in primary care[a] CRB 65 score is](https://slidetodoc.com/presentation_image_h/fde6774ee55e6117cfa7d047d979fe35/image-24.jpg)
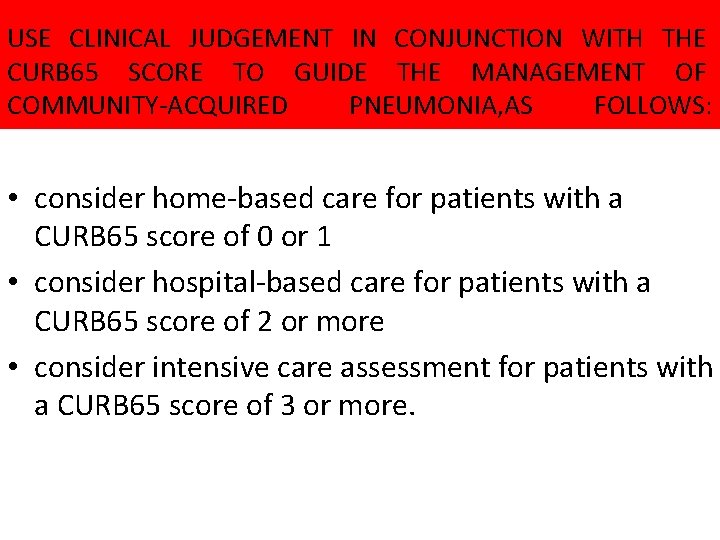
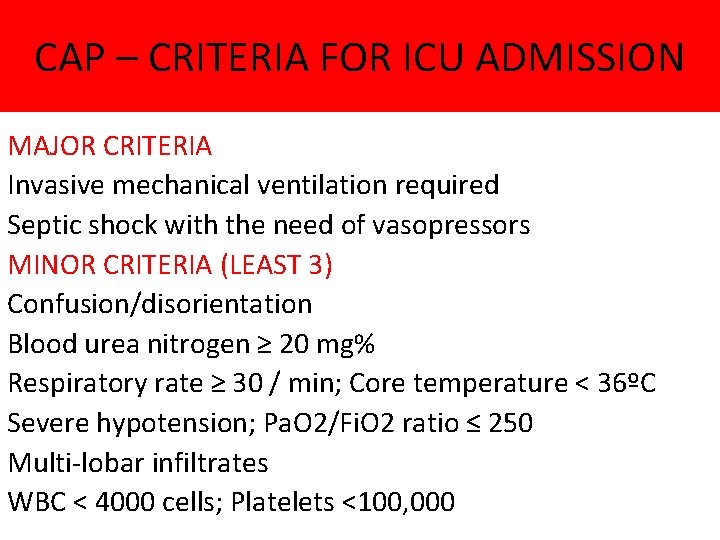
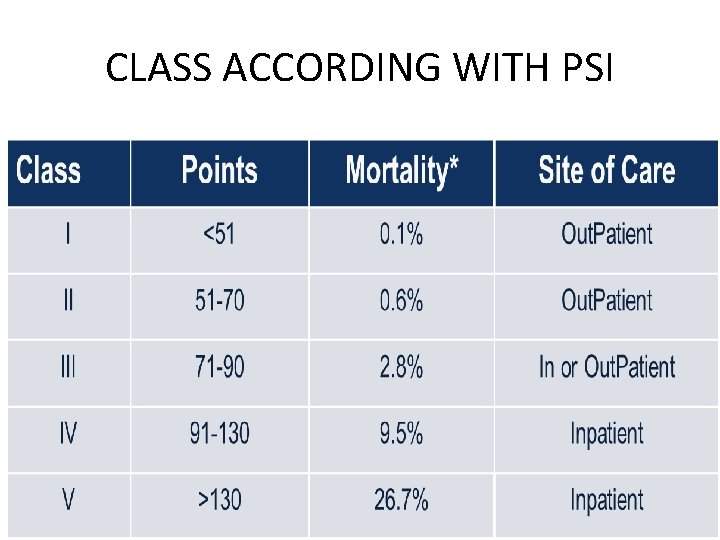
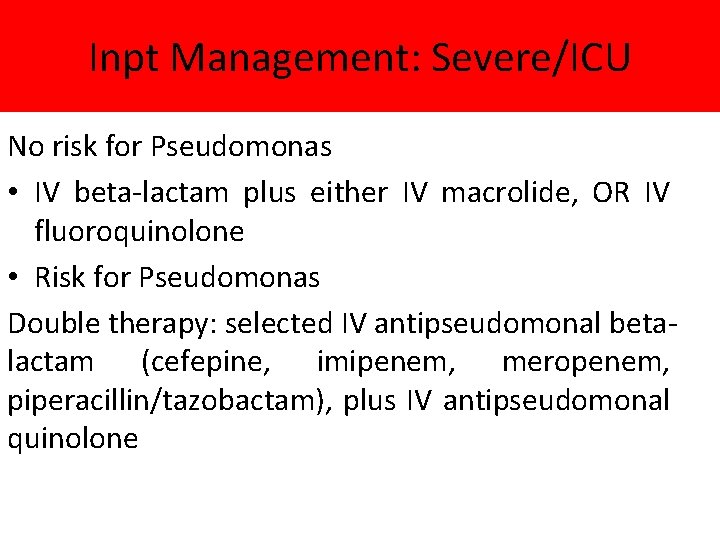
CRB 65 score for mortality risk assessment in primary care[a] CRB 65 score is calculated by giving 1 point for each of the following prognostic features: • confusion (abbreviated Mental Test score 8 or less, or new disorientation in person, place or time) • raised respiratory rate (30 breaths per minute or more) • low blood pressure (diastolic 60 mm. Hg or less, or systolic less than 90 mm. Hg) • age 65 years or more. Patients are stratified for risk of death as follows: 0: low risk (less than 1% mortality risk) 1 or 2: intermediate risk (1 -10% mortality risk) 3 or 4: high risk (more than 10% mortality risk).
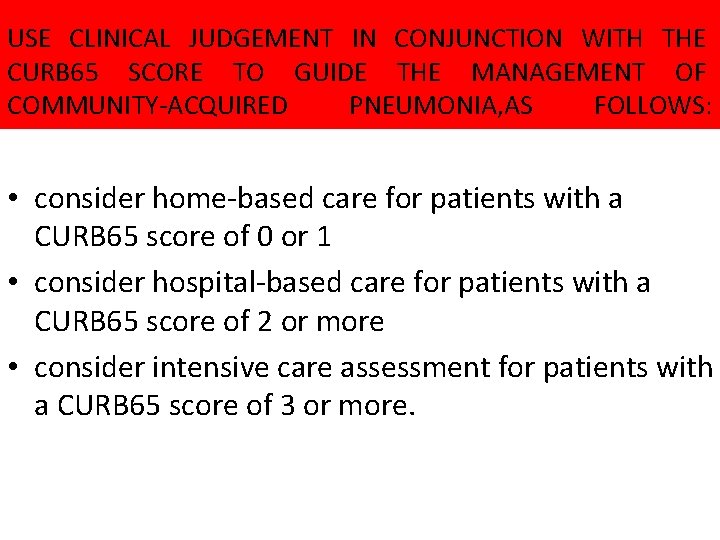
USE CLINICAL JUDGEMENT IN CONJUNCTION WITH THE CURB 65 SCORE TO GUIDE THE MANAGEMENT OF COMMUNITY-ACQUIRED PNEUMONIA, AS FOLLOWS: • consider home-based care for patients with a CURB 65 score of 0 or 1 • consider hospital-based care for patients with a CURB 65 score of 2 or more • consider intensive care assessment for patients with a CURB 65 score of 3 or more.

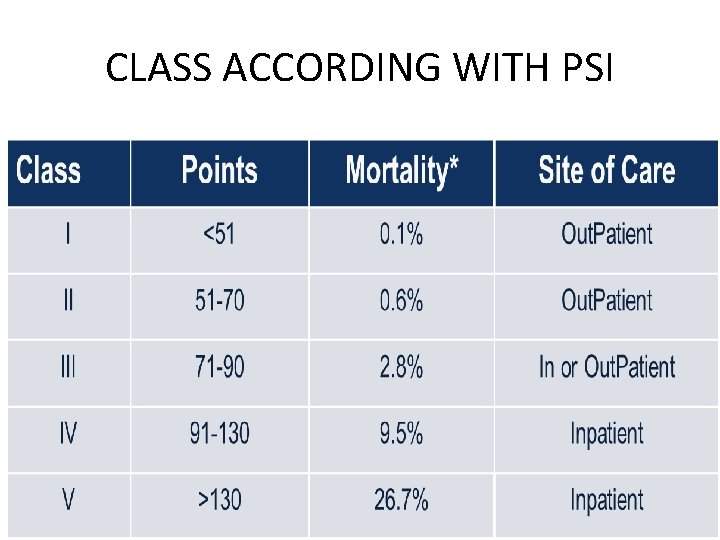
CLASS ACCORDING WITH PSI
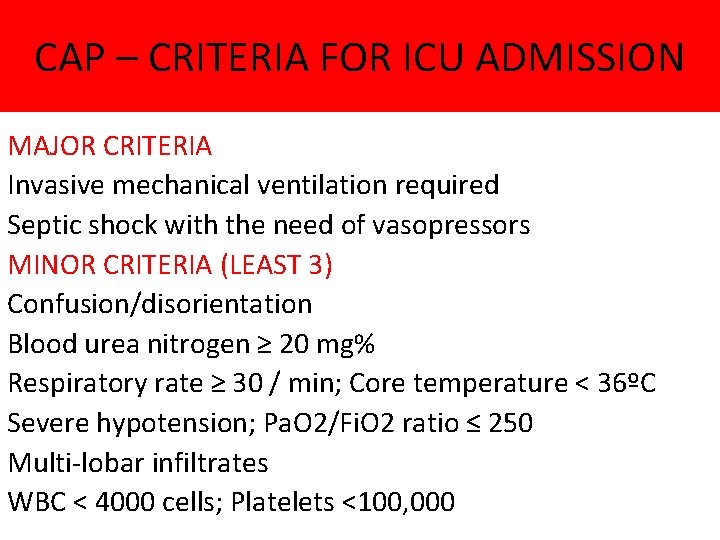
CAP – CRITERIA FOR ICU ADMISSION MAJOR CRITERIA Invasive mechanical ventilation required Septic shock with the need of vasopressors MINOR CRITERIA (LEAST 3) Confusion/disorientation Blood urea nitrogen ≥ 20 mg% Respiratory rate ≥ 30 / min; Core temperature < 36ºC Severe hypotension; Pa. O 2/Fi. O 2 ratio ≤ 250 Multi-lobar infiltrates WBC < 4000 cells; Platelets <100, 000
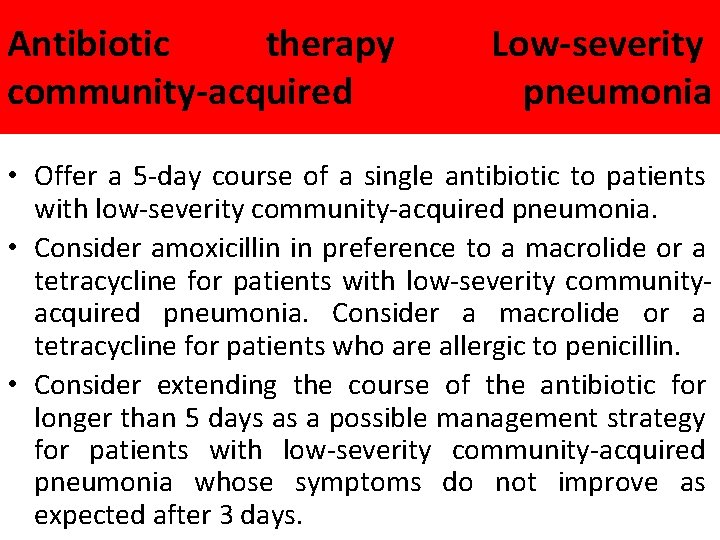
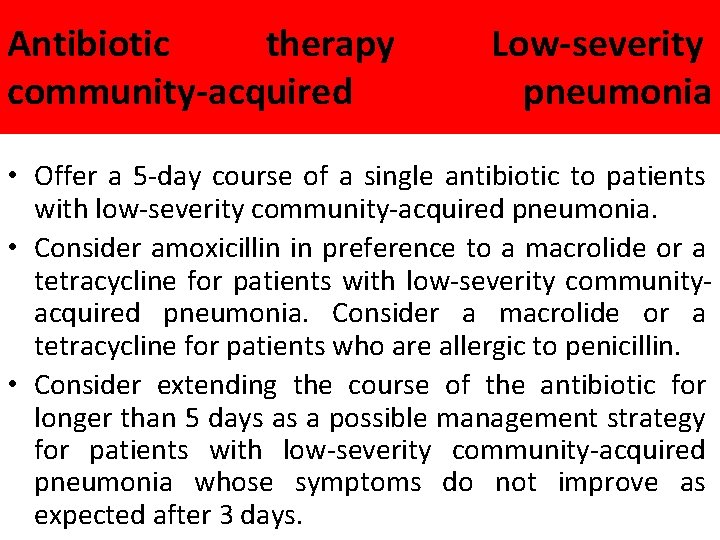
Antibiotic therapy community-acquired Low-severity pneumonia • Offer a 5 -day course of a single antibiotic to patients with low-severity community-acquired pneumonia. • Consider amoxicillin in preference to a macrolide or a tetracycline for patients with low-severity communityacquired pneumonia. Consider a macrolide or a tetracycline for patients who are allergic to penicillin. • Consider extending the course of the antibiotic for longer than 5 days as a possible management strategy for patients with low-severity community-acquired pneumonia whose symptoms do not improve as expected after 3 days.
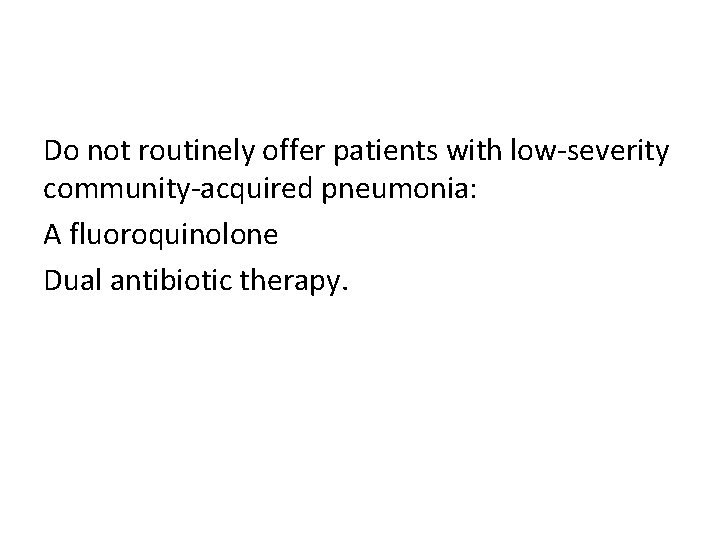
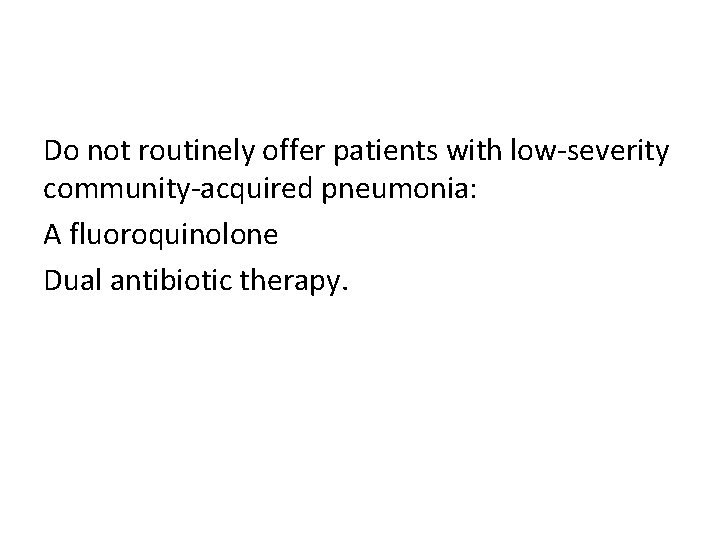
Do not routinely offer patients with low-severity community-acquired pneumonia: A fluoroquinolone Dual antibiotic therapy.
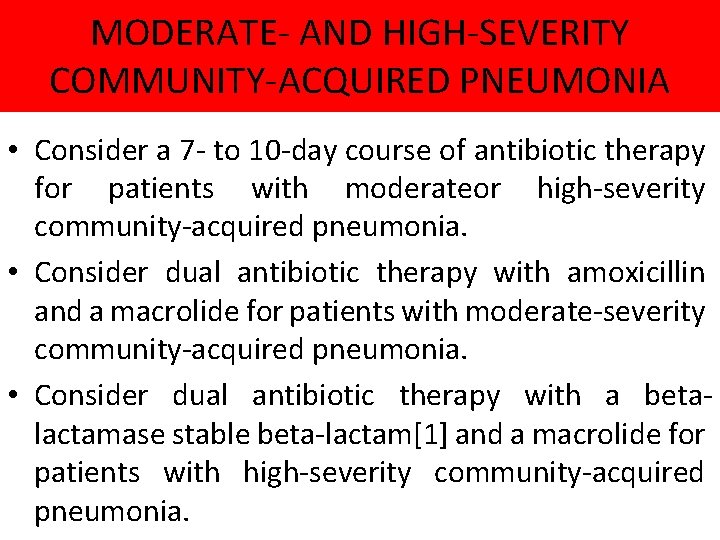
MODERATE- AND HIGH-SEVERITY COMMUNITY-ACQUIRED PNEUMONIA • Consider a 7 - to 10 -day course of antibiotic therapy for patients with moderateor high-severity community-acquired pneumonia. • Consider dual antibiotic therapy with amoxicillin and a macrolide for patients with moderate-severity community-acquired pneumonia. • Consider dual antibiotic therapy with a betalactamase stable beta-lactam[1] and a macrolide for patients with high-severity community-acquired pneumonia.
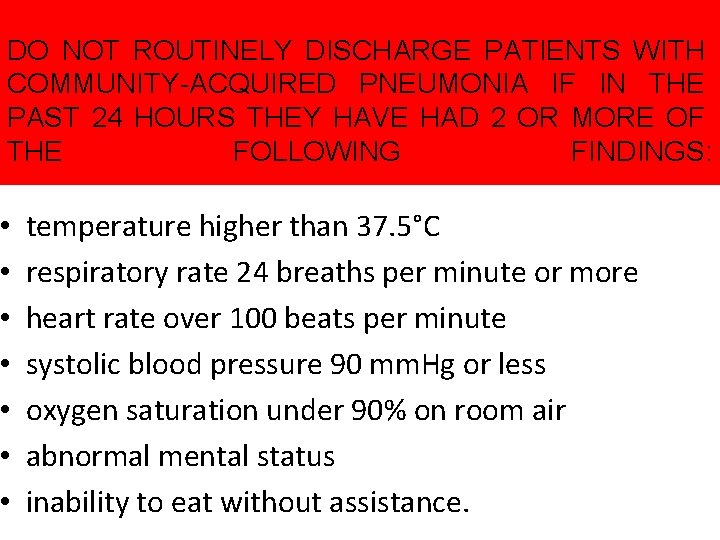
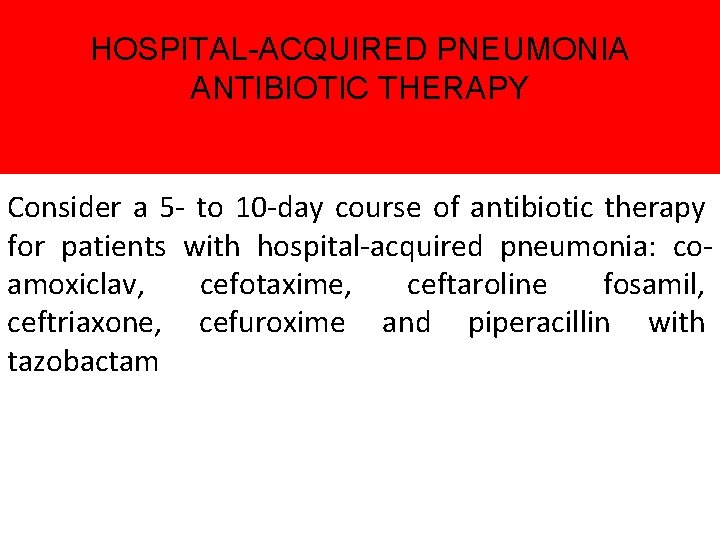
DO NOT ROUTINELY DISCHARGE PATIENTS WITH COMMUNITY-ACQUIRED PNEUMONIA IF IN THE PAST 24 HOURS THEY HAVE HAD 2 OR MORE OF THE FOLLOWING FINDINGS: • • temperature higher than 37. 5°C respiratory rate 24 breaths per minute or more heart rate over 100 beats per minute systolic blood pressure 90 mm. Hg or less oxygen saturation under 90% on room air abnormal mental status inability to eat without assistance.
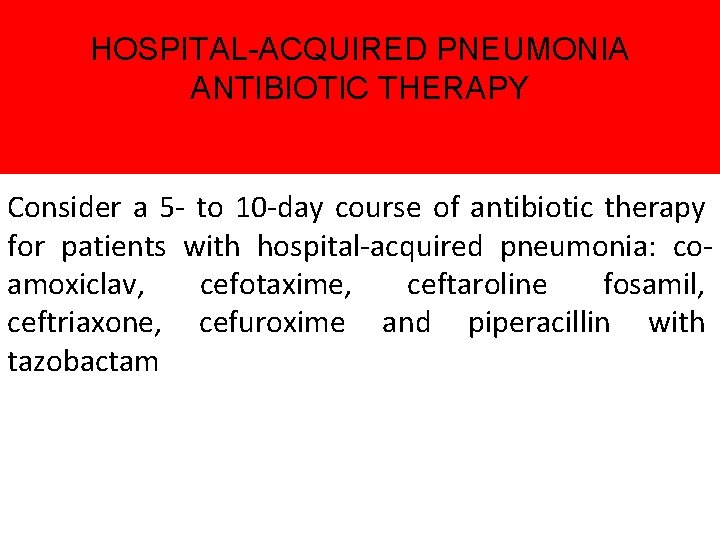
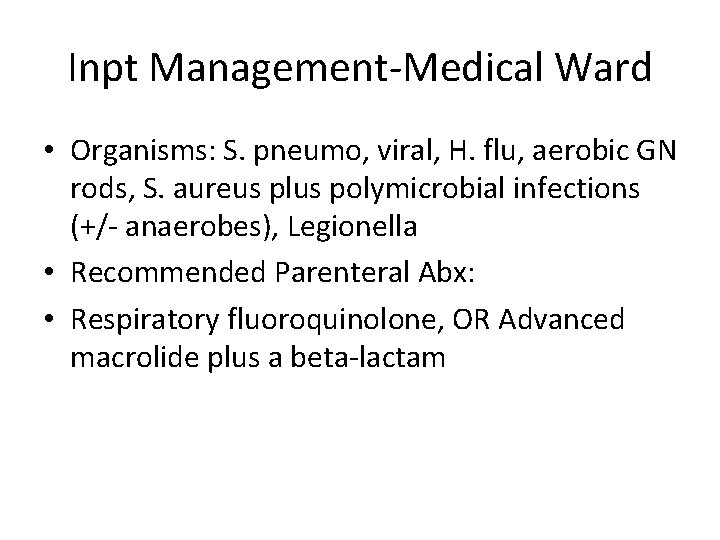
HOSPITAL-ACQUIRED PNEUMONIA ANTIBIOTIC THERAPY Consider a 5 - to 10 -day course of antibiotic therapy for patients with hospital-acquired pneumonia: coamoxiclav, cefotaxime, ceftaroline fosamil, ceftriaxone, cefuroxime and piperacillin with tazobactam
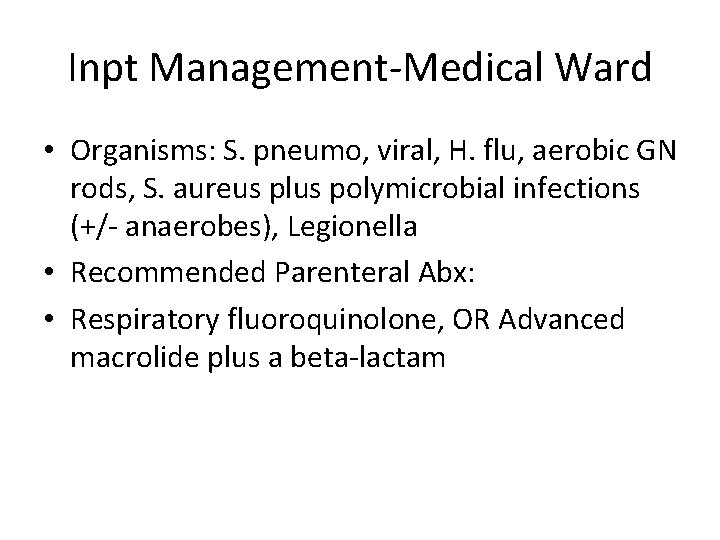
Inpt Management-Medical Ward • Organisms: S. pneumo, viral, H. flu, aerobic GN rods, S. aureus plus polymicrobial infections (+/- anaerobes), Legionella • Recommended Parenteral Abx: • Respiratory fluoroquinolone, OR Advanced macrolide plus a beta-lactam
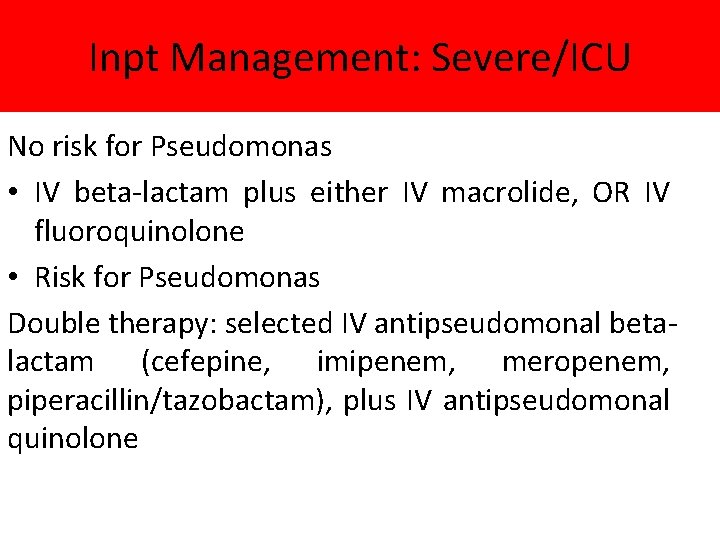
Inpt Management: Severe/ICU No risk for Pseudomonas • IV beta-lactam plus either IV macrolide, OR IV fluoroquinolone • Risk for Pseudomonas Double therapy: selected IV antipseudomonal betalactam (cefepine, imipenem, meropenem, piperacillin/tazobactam), plus IV antipseudomonal quinolone
SUPPORTIVE CARE Fluids, supplemental oxygen therapy, respiratory monitoring.
SEVERITY OF CAP WITH POOR PROGNOSIS RR > 30; Pa. O 2/Fi. O 2 < 250, or PO 2 < 60 on room air Need for mechanical ventilation Multi lobar involvement Hypotension Need for vasopressors Oliguria Altered mental status
COMPLICATIONS • • Acute respiratory distress syndrome (ARDS) Pleural effusion Lung abscesses Respiratory failure (which requires mechanical ventilator) Sepsis, which may lead to organ failure Atelectasis Electrolytes and water disbalance Ilium paralytic
 Lecturer's name or lecturer name
Lecturer's name or lecturer name Tanya solorzano
Tanya solorzano Sushi light envigado
Sushi light envigado Difference between internal check and internal control
Difference between internal check and internal control Internal control and internal check
Internal control and internal check Physician associate lecturer
Physician associate lecturer Spe distinguished lecturer
Spe distinguished lecturer Teacher good morning students
Teacher good morning students Photography lecturer
Photography lecturer Lecturer in charge
Lecturer in charge Designation lecturer
Designation lecturer Designation of lecturer
Designation of lecturer Gcwak
Gcwak Lecturer name
Lecturer name Pearson lecturer resources
Pearson lecturer resources 140000/120
140000/120 Lector vs lecturer
Lector vs lecturer Lecturer in charge
Lecturer in charge Cfa lecturer handbook
Cfa lecturer handbook Lecturer asad ali
Lecturer asad ali Unm internal medicine residency
Unm internal medicine residency Umass anesthesiology residency
Umass anesthesiology residency What is tir
What is tir The father of modern medicine
The father of modern medicine Legacy health internal medicine residency
Legacy health internal medicine residency Uihc internal medicine residency
Uihc internal medicine residency Psychiatry shelf percentiles
Psychiatry shelf percentiles Brittany shrefler md
Brittany shrefler md What is pain jeopardy
What is pain jeopardy Unm emergency medicine residents
Unm emergency medicine residents Uthscsa internal medicine residents
Uthscsa internal medicine residents Internal medicine society of australia and new zealand
Internal medicine society of australia and new zealand Edema documentation example
Edema documentation example Romero britto person
Romero britto person Great coffee de romero britto
Great coffee de romero britto Vanessa espericueta
Vanessa espericueta Cuanto mide el romero
Cuanto mide el romero Julio romero de torres pinto a la mujer morena
Julio romero de torres pinto a la mujer morena Pecos romero edad
Pecos romero edad