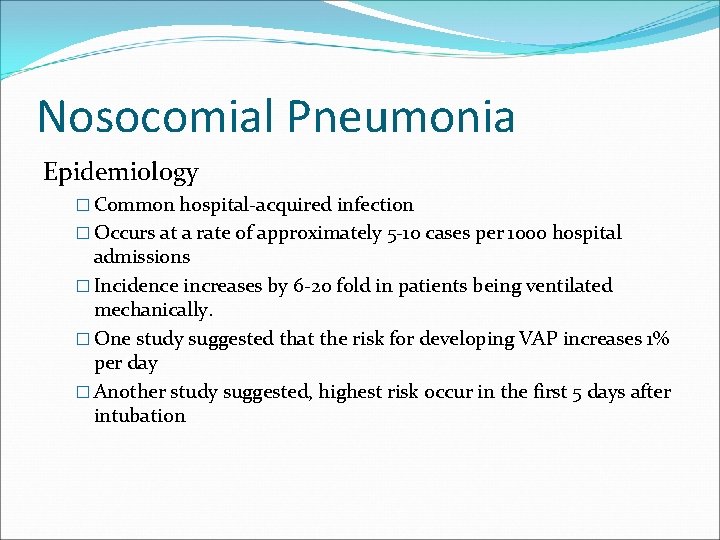
Nosocomial Pneumonia Nosocomial Pneumonia Epidemiology Common hospitalacquired infection
- Slides: 31
Nosocomial Pneumonia
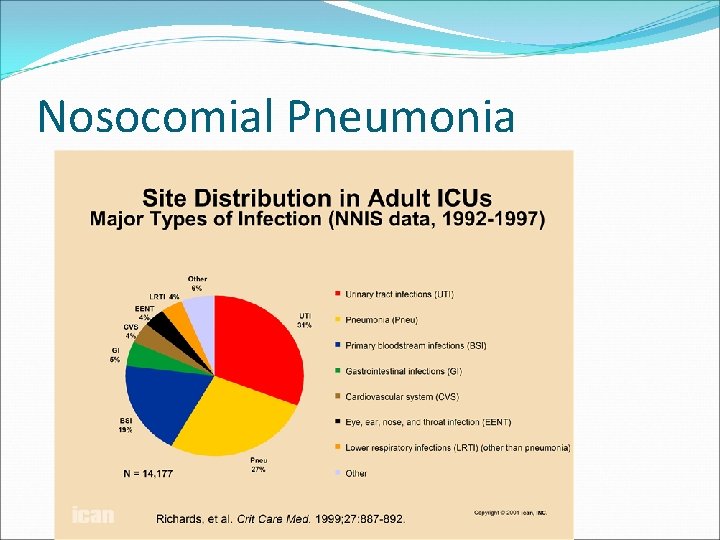
Nosocomial Pneumonia Epidemiology � Common hospital-acquired infection � Occurs at a rate of approximately 5 -10 cases per 1000 hospital admissions � Incidence increases by 6 -20 fold in patients being ventilated mechanically. � One study suggested that the risk for developing VAP increases 1% per day � Another study suggested, highest risk occur in the first 5 days after intubation
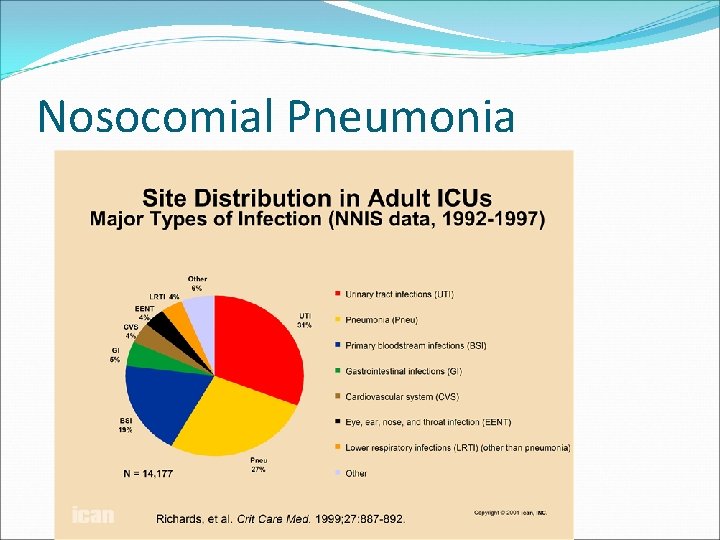
Nosocomial Pneumonia
Nosocomial Pneumonia Epidemiology �Nosocomial pneumonia is the leading cause of death due to hospital acquired infections �Associated with substantial morbidity �Has an associated crude mortality of 30 -50% �Hospital stay increases by 7 -9 days per patient �Estimated cost > 1 billion dollars/year
Nosocomial Pneumonia �Hence, the importance of focusing on: �Accurate diagnosis �Appropriate treatment �Preventive measures
Nosocomial Pneumonia �Pathogenesis �Risk factors �Etiologic agents �Differential diagnosis �Treatment �Prevention
Nosocomial Pneumonia Pathogenesis
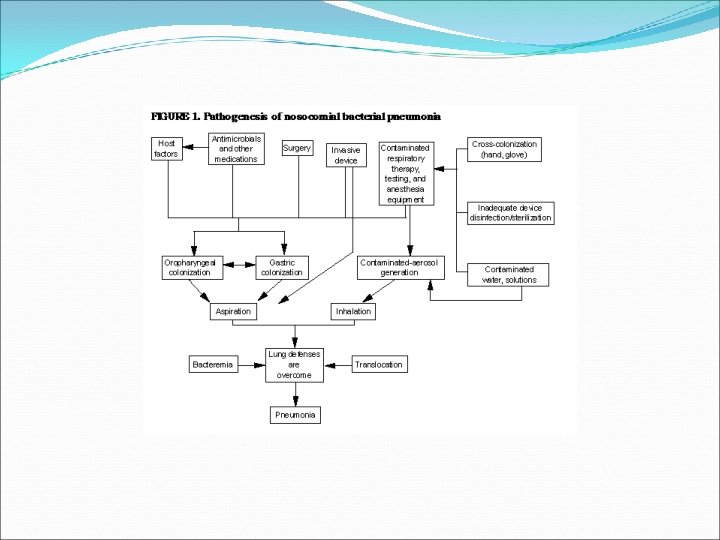
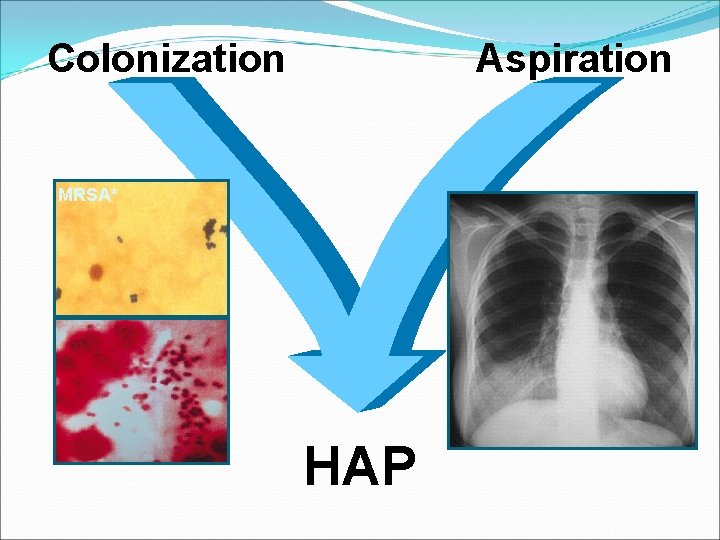
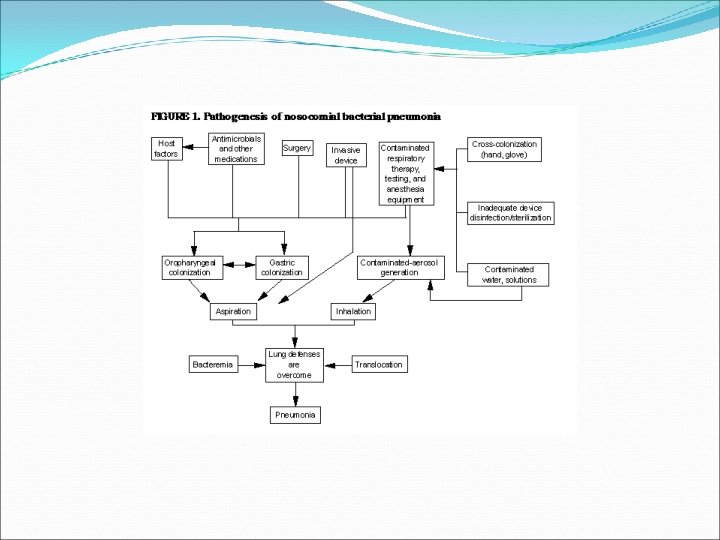
Nosocomial Pneumonia �Microaspiration may occur in up to 45% of healthy volunteers during sleep �Oropharynx of hospitalized patients is colonized with GNR in 35 -75% of patients depending on the severity and type of underlying illness �Multiple factors are associated with higher risk of colonization with pathogenic bacteria and higher risk of aspiration
Nosocomial Pneumonia �Pathogenesis �Invasion of the lower respiratory tract by: � Aspiration of oropharyngeal/GI organisms � Inhalation of aerosols containing bacteria � Hematogenous spread
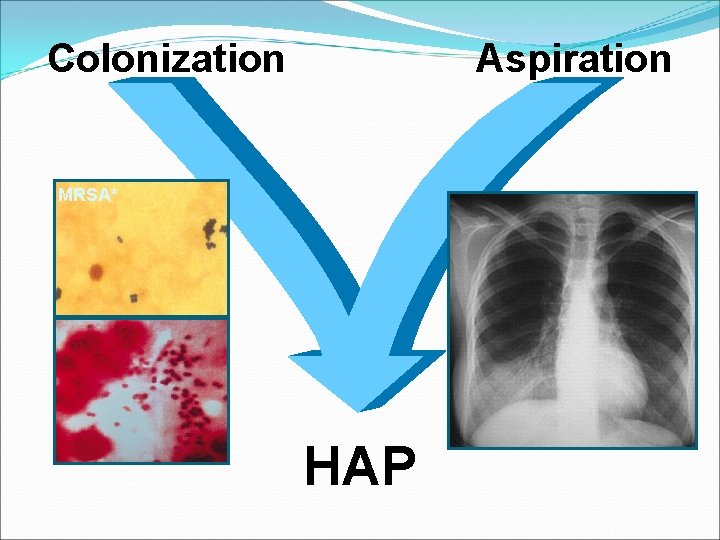
Colonization Aspiration MRSA* HAP
Nosocomial Pneumonia Risk Factors
Nosocomial Pneumonia �Risk Factors �Host Factors � Extremes of age, severe acute or chronic illnesses, immunosupression, coma, alcoholism, malnutrition, COPD, DM �Factors that enhance colonization of the oropharynx and stomach by pathogenic microorganisms � admission to an ICU, administration of antibiotics, chronic lung disease, endotracheal intubation, etc.
Nosocomial Pneumonia �Risk Factors �Conditions favoring aspiration or reflux � Supine position, depressed consciousness, endotracheal intubation, insertion of nasogastric tube �Mechanical ventilation � Impaired mucociliary function, injury of mucosa favoring bacterial binding, pooling of secretions in the subglottic area, potential exposure to contaminated respiratory equipment and contact with contaminated or colonized hands of HCWs �Factors that impede adequate pulmonary toilet � Surgical procedures that involve the head and neck, being immobilized as a result of trauma or illness, sedation etc.
Nosocomial Pneumonia Etiologic Agents
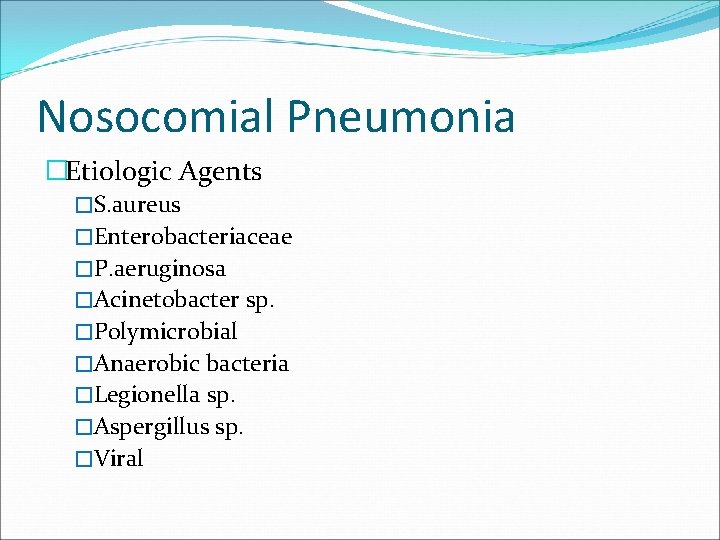
Nosocomial Pneumonia �Etiologic Agents �S. aureus �Enterobacteriaceae �P. aeruginosa �Acinetobacter sp. �Polymicrobial �Anaerobic bacteria �Legionella sp. �Aspergillus sp. �Viral
Nosocomial Pneumonia Diagnosis
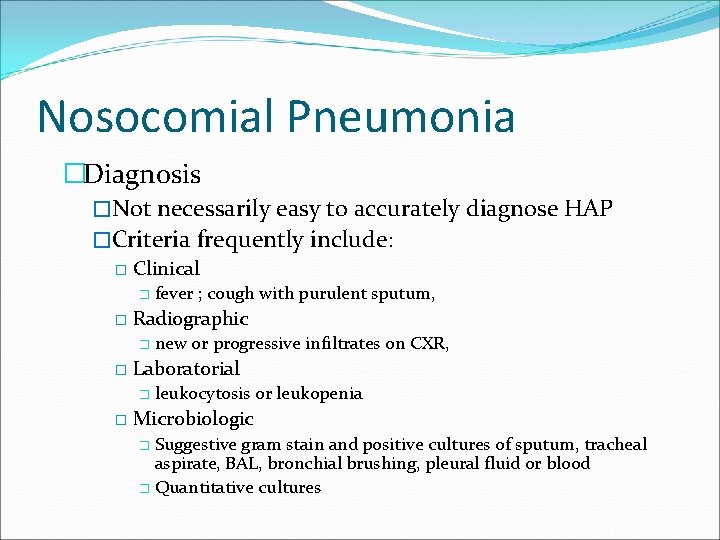
Nosocomial Pneumonia �Diagnosis �Not necessarily easy to accurately diagnose HAP �Criteria frequently include: � Clinical � � Radiographic � � new or progressive infiltrates on CXR, Laboratorial � � fever ; cough with purulent sputum, leukocytosis or leukopenia Microbiologic Suggestive gram stain and positive cultures of sputum, tracheal aspirate, BAL, bronchial brushing, pleural fluid or blood � Quantitative cultures �
Nosocomial Pneumonia �Problems �All above criteria fairly sensitive, but very non- specific, particularly in mechanically ventilated patients �Other criteria/problems include Positive cultures of blood and pleural fluid plus clinical findings (specific but poor sensitivity) � Rapid cavitation of pulmonary infiltrate absent Tb or cancer (rare) � Histopathologic examination of lung tissue (invasive) �
Nosocomial pneumonia �Bronchoscopically Directed Techniques for diagnosis of VAP and Quantitative cultures � Bronchoscopy with BAL/bronchial brushings (10, 000 to 100, 000 CFU/ml and less than 1% of squamous cells) � Protected specimen brush method (>10³ CFU/ml) � Protected BAL with a balloon tipped catheter (>5% of neutrophils or macrophages with intracellular organisms on a Wright-Giemsa stain)
Nosocomial pneumonia � Multiple studies looked into the accuracy of quantitative culture and microscopic examination of LRT secretions as compared to histopathologic examination and tissue cultures (either lung biopsy or immediate post mortem obtained samples) � Several trials conclude that use of FOB techniques and quantitative cultures are more accurate � At least 4 studies concluded that bronchoscopically directed techniques were not more accurate for diagnosis of VAP than clinical and X-ray criteria, combined with cultures of tracheal aspirate � Therefore no gold standard criteria exist
Nosocomial Pneumonia �Differential diagnosis �ARDS �Pulmonary edema �Pulmonary embolism �Atelectasis �Alveolar hemorrhage �Lung contusion
Nosocomial Pneumonia Treatment
Nosocomial Pneumonia �Antimicrobial Treatment �Broad spectrum penicillins � 3 rd and 4 th generation cephalosporins �Carbapenems �Quinolones �Aminoglycosides �Vancomycin �Linezolid
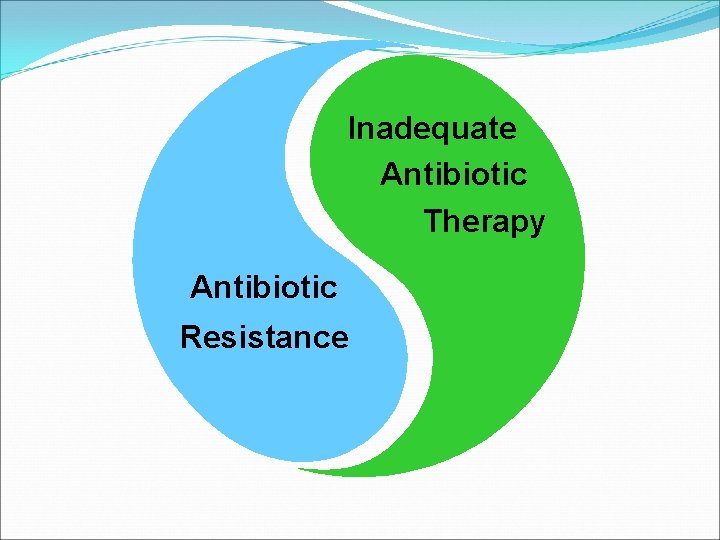
Inadequate Antibiotic Therapy Antibiotic Resistance
Nosocomial Pneumonia �Duration of antimicrobial treatment �Optimal duration of treatment has not been established �Most experts recommend 14 -21 days of treatment �Recent data support shorter treatment regimens (8 days)
Nosocomial Pneumonia Prevention
Nosocomial Pneumonia �Preventive Measures �Incentive spirometry �Promote early ambulation �Avoid CNS depressants �Decrease duration of immunosupression �Infection control measures �Educate and train personnel
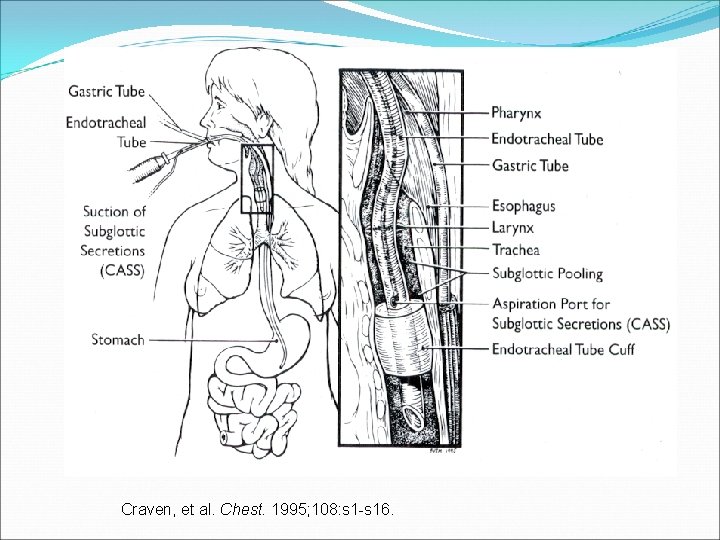
Nosocomial Pneumonia �Preventive Measures �Avoid prolonged nasal intubation �Suction secretions �Semi-recumbent position( 30 -45°head elevation) �Do not change ventilator circuits routinely more often than every 48 hours �Drain and discard tubing condensate �Use sterile water for respiratory humidifying devices �Subglottic secretions drainage
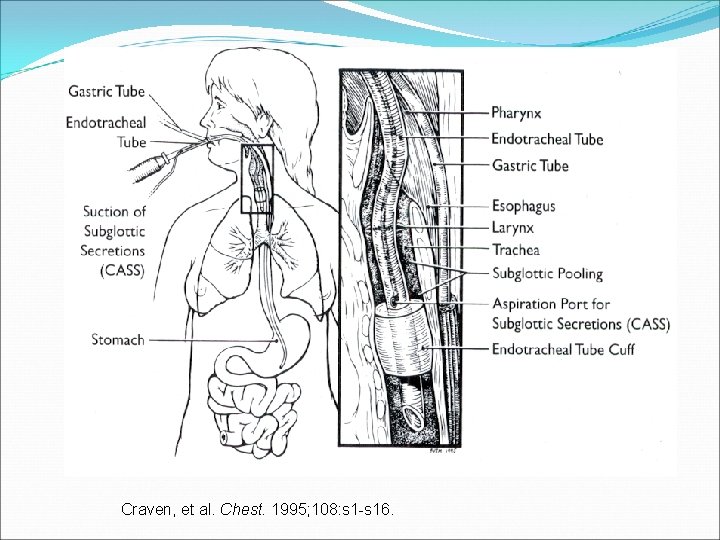
Craven, et al. Chest. 1995; 108: s 1 -s 16.
Nosocomial Pneumonia �Preventive Measures �Remove NGT when no longer needed �Avoid gastric overdistention �Stress ulcer prophylaxis: � sulcrafate; antacids; H 2 receptor antagonists �Acidification of enteral feedings �Prophylactic antibiotics � Inhaled antibiotics � Selective digestive decontamination �Chlorexidine oral rinses �Vaccines ( Influenza; Strep. pneumoniae)
 Beth has a nosocomial infection. how did she get it?
Beth has a nosocomial infection. how did she get it? Cbic recertification
Cbic recertification Innate immunity first line of defense
Innate immunity first line of defense Diabetic ketoacidosis epidemiology
Diabetic ketoacidosis epidemiology Attack rate epidemiology formula
Attack rate epidemiology formula Distribution in epidemiology
Distribution in epidemiology Scope of epidemiology
Scope of epidemiology Epidemiological triad
Epidemiological triad How dr. wafaa elsadr epidemiology professor
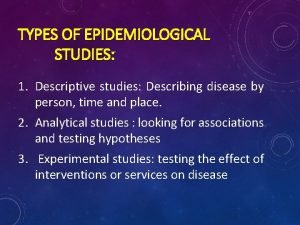
How dr. wafaa elsadr epidemiology professor Descriptive vs analytic epidemiology examples
Descriptive vs analytic epidemiology examples Bhisma murti
Bhisma murti Logistic regression epidemiology
Logistic regression epidemiology Wheel of causation example
Wheel of causation example How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Distribution in epidemiology
Distribution in epidemiology Difference between descriptive and analytic epidemiology
Difference between descriptive and analytic epidemiology Ramboman
Ramboman What is descriptive study in epidemiology
What is descriptive study in epidemiology John snow epidemiology
John snow epidemiology Pros and cons of cross sectional study
Pros and cons of cross sectional study Nutritional epidemiology
Nutritional epidemiology Prevalence calculation
Prevalence calculation Gordon nichols
Gordon nichols Defination of prevalence
Defination of prevalence Epidemiology definition
Epidemiology definition Effect modification epidemiology
Effect modification epidemiology Epidemiology person place time
Epidemiology person place time Epidemiology description
Epidemiology description Spurious association
Spurious association Risiko relatif dan odds ratio
Risiko relatif dan odds ratio Formula for attack rate
Formula for attack rate Epidemiology made easy
Epidemiology made easy