Covid19 and pneumonia Pneumonia is an infection in








- Slides: 31

Covid_19 and pneumonia
Pneumonia is an infection in one or both lungs. Bacteria, viruses, and fungi cause it. The infection causes inflammation in the air sacs in your lungs, which are called alveoli. The alveoli fill with fluid or pus, making it difficult to breathe.
Both viral and bacterial pneumonia can spread to others through inhalation of airborne droplets from a sneeze or cough. You can also get these types of pneumonia by coming into contact with surfaces or objects that are contaminated with pneumonia-causing bacteria or viruses. You can contract fungal pneumonia from the environment. However, it doesn’t spread from person to person.
Symptoms of pneumonia
coughing that may produce phlegm (mucus) • fever • sweating or chills • shortness of breath that happens while doing normal • activities or even while resting chest pain that’s worse when you breathe or cough • feelings of tiredness or fatigue • loss of appetite • nausea or vomiting • headaches •
Types of pneumonia Pneumonia can also be classified according to where or how it was acquired. Hospital-acquired pneumonia (HAP) This type of bacterial pneumonia is acquired during a hospital stay. It can be more serious than other types, as the bacteria involved may be more resistant to antibiotics. Community-acquired pneumonia (CAP) refers to pneumonia that’s acquired outside of a medical or institutional setting. Ventilator-associated pneumonia (VAP) When people who are using a ventilator get pneumonia, it’s called VAP.
Pneumonia diagnosis
start by taking your medical history
physical exam: This will include listening to your lungs with a stethoscope for any abnormal sounds, such as crackling. Depending on the severity of your symptoms and your risk for complications may also order one or more of these tests:
Chest X-ray An X-ray : look for signs of inflammation in chest. If inflammation is present, the X-ray can also inform about its location and extent.
Blood culture This test uses a blood sample to confirm an infection. Culturing can also help identify what may be causing condition. Sputum culture During a sputum culture, a sample of mucus is collected after you’ve coughed deeply. It’s then sent to a lab to be analyzed to identify the cause of the infection. Pulse oximetry A pulse oximetry measures the amount of oxygen in your blood. A sensor placed on one of your fingers can indicate whether your lungs are moving enough oxygen through your bloodstream. CT scans provide a clearer and more detailed picture of your lungs. Fluid sample If your doctor suspects there’s fluid in the pleural space of your chest, they may take a fluid sample using a needle placed between your ribs. This test can help identify the cause of your infection. Bronchoscopy A bronchoscopy looks into the airways in your lungs. It does this using a camera on the end of a flexible tube that’s gently guided down your throat and into your lungs. Your doctor may do this test if your initial symptoms are severe, or if you’re hospitalized and not responding well to antibiotics.
viral infections that can cause pneumonia include: influenza (flu) • RSV infection • rhinoviruses (common cold) • human parainfluenza virus (HPIV) infection • human metapneumovirus (HMPV) infection Measles • chickenpox (varicella-zoster virus) • adenovirus infection • coronavirus infection •
Coronavirus COVID-19 (SARS-Co. V-2)
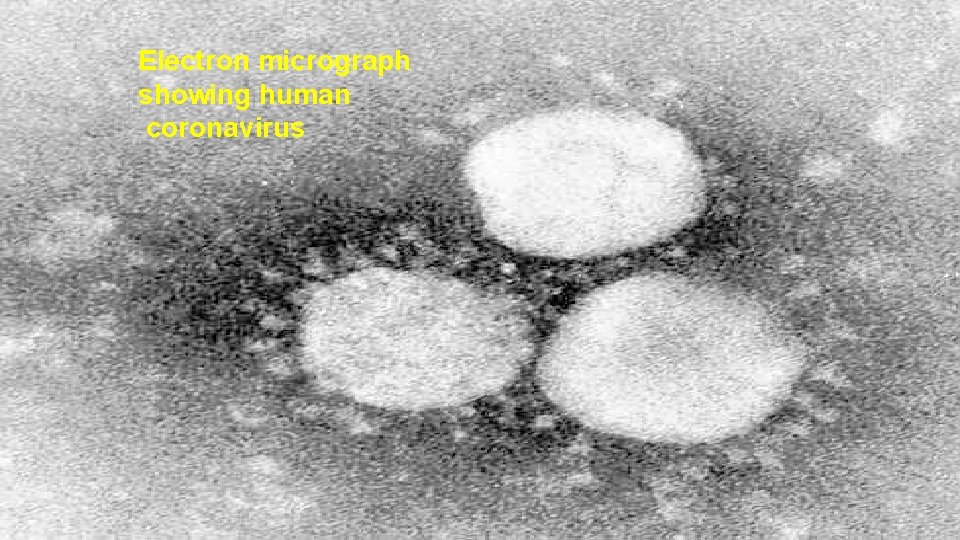
MICROBIOLOGY single-strand enveloped RNA virus belonging to the family Coronaviridae. Coronavirus name derived from the Latin corona, meaning crown. Viral envelope under electron microscopy appears crown-like due to small bulbar projections formed by the viral spike (S) peplomers. This topic covers the novel coronavirus 2019 (2019 -n. Co. V) now referred to as SARS-Co. V-2
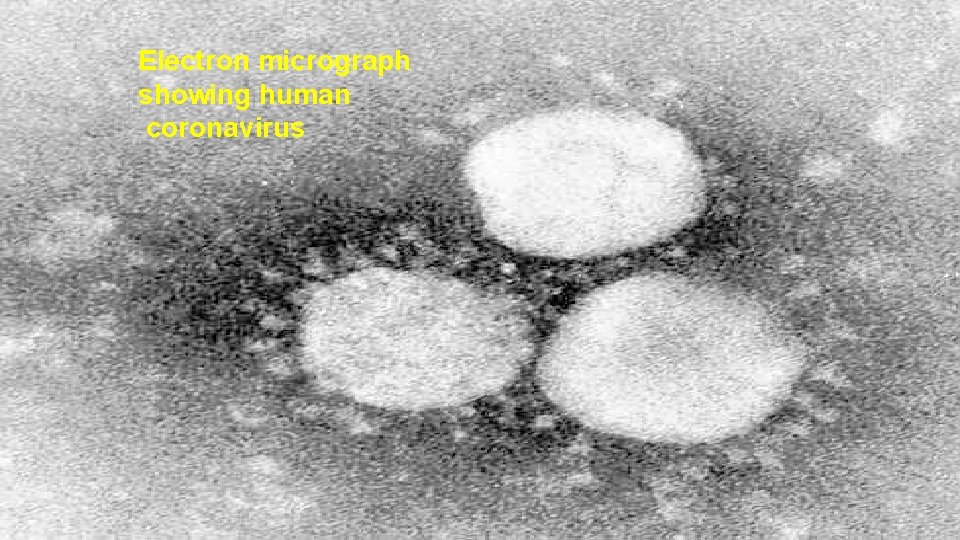
Electron micrograph showing human coronavirus
Transmission By respiratory droplets and by fomite. Virus found in respiratory secretions and saliva. Viral shedding by asymptomatic people may represent 25– 50% of total infections. Viral shedding may antedate symptoms by 1– 2 days. Viral titers are highest in the earliest phases of infection.
Aerosol spread could occur, thought to be mostly in hospital settings Airborne transmission frequency is debated. Some widely publicized evidence is based on experimental aerosolization rather than human studies. To date, there has not been a well document case of aerosol transmission (e. g. , through HVAC ventilatory systems or airplanes). Stool shedding also described later in disease, but uncertain what role, if any, that plays
Incubation period Mean of 6. 4 days, range 2– 12. For people quarantined, 14 d observation recommended to exclude infection, though 24 d asymptomatic time from exposure described. Viral shedding occurs following recovery, but unclear what role this plays in transmission
These symptoms may appear 2 -14 days after exposure to the virus: Fever • Cough • Shortness of breath or difficulty breathing • Chills • Repeated shaking with chills • Muscle pain • Headache • Sore throat • New loss of taste or smell •
Symptoms Fever (44%– 98%) Range may be lower at initial hospital presentation or in the outpatient setting Cough (46– 82%, usually dry) Shortness of breath at onset (31%) Myalgia or fatigue (11– 44%) Loss of taste or smell Potential sign in early infection, but not unique to COVID-19 as may be seen with other viral infections. Less common symptoms: Pharyngitis Headache Productive cough GI symptoms Have been described as a presenting symptom, and potentially heralding more severe illness. Hemoptysis
In COVID-19 pneumonia Leukopenia in ~70% of hospitalized patients. LDH may be modestly elevated. LFTs elevated more commonly than in typical Community-Acquired Pneumonia cases. Chest CT may show ground-glass opacities that may evolve into consolidation or ARDS. Findings appear to peak at 10 d of illness, resolution begins after day 14. CT may show lung findings (such as ground-glass opacities) before the development of symptoms. Among hospitalized patients, about one-third need to be in the ICU/intubated with an ARDS picture. Elevations in IL-6 (> 40– 100), CRP (> 10 x normal), ferritin (> 1000) suggested correlating with a cytokine release syndrome-like picture and impending ARDS.
Confirmatory tests, molecular (PCR)
PCR sensitivity not known accurately Likely < 90% depending on the assay used, sample procurement methods and stage of illness. Second and third NP swabs described as needed in some patients; lower respiratory specimens (e. g. , BAL) may offer superior yields.







 Http://apps.tujuhbukit.com/covid19/
Http://apps.tujuhbukit.com/covid19/ Do if you covid19
Do if you covid19 Covid19 athome rapid what know
Covid19 athome rapid what know What do if test positive covid19
What do if test positive covid19 Vaksin covid19
Vaksin covid19 Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 16 infection control and standard precautions
Chapter 16 infection control and standard precautions Chapter 16 infection control and standard precautions
Chapter 16 infection control and standard precautions Federal agencies milady
Federal agencies milady Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Certification board of infection control and epidemiology
Certification board of infection control and epidemiology What causes tactile fremitus
What causes tactile fremitus Bronchopneumonia vs lobar pneumonia
Bronchopneumonia vs lobar pneumonia Atypical pneumonia
Atypical pneumonia Wound infection continuum
Wound infection continuum Kidney infection
Kidney infection Torch infection
Torch infection Infection nosocomiale
Infection nosocomiale Infection nosocomiale
Infection nosocomiale Dental radiographic interpretation ppt
Dental radiographic interpretation ppt Neonatal sepsis
Neonatal sepsis Test idr
Test idr Infection nosocomiale
Infection nosocomiale Circuit du linge propre
Circuit du linge propre Infection controlcare home
Infection controlcare home Stages of infection
Stages of infection Infection nosocomiale
Infection nosocomiale Palmar fascial spaces
Palmar fascial spaces Chain of infection cycle
Chain of infection cycle Chapter 16 preventing infection
Chapter 16 preventing infection Chapter 15 infection control
Chapter 15 infection control