Chapter 19 Disease Transmission and Infection Control Copyright


- Slides: 67
Chapter 19 Disease Transmission and Infection Control Copyright 2003, Elsevier Science (USA). All rights reserved. No part of this product may be reproduced or transmitted in any form or by any means, electronic or mechanical, including input into or storage in any information system, without permission in writing from the publisher. Power. Point® presentation slides may be displayed and may be reproduced in print form for instructional purposes only, provided a proper copyright notice appears on the last page of each print-out. Produced in the United States of America ISBN 0 -7216 -9770 -4
Introduction As a member of the dental health care team, the dental assistant is at risk of exposure to disease agents through contact with blood or other potentially infectious materials. By carefully following infection control and safety guidelines, you can minimize your risk of disease transmission in the dental office. Copyright 2003, Elsevier Science (USA). All rights reserved.
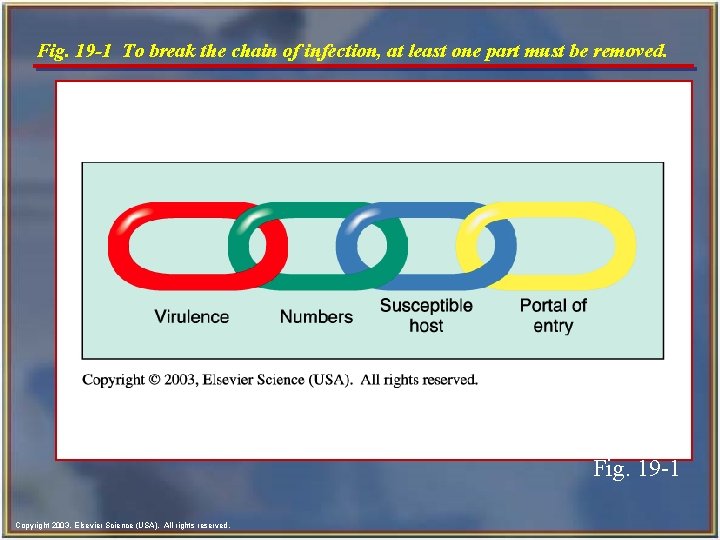
The Chain of Infection n The chain of infection consists of four parts: • Virulence • Numbers • Susceptible host • Portal of entry Copyright 2003, Elsevier Science (USA). All rights reserved.
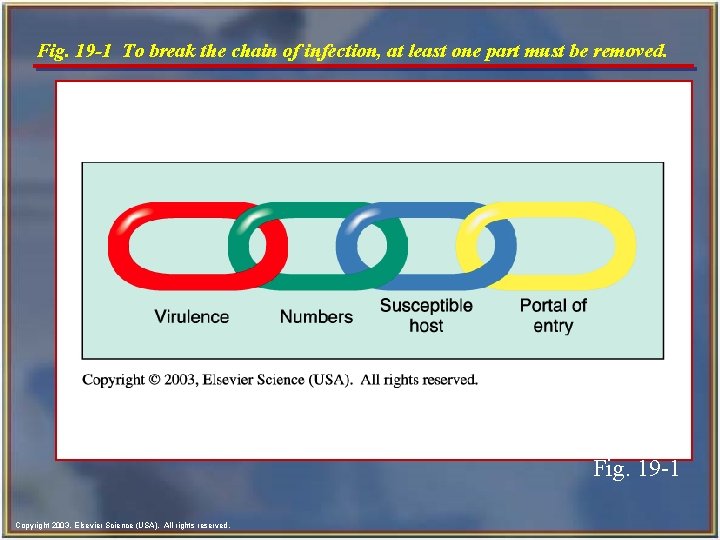
Fig. 19 -1 To break the chain of infection, at least one part must be removed. Fig. 19 -1 Copyright 2003, Elsevier Science (USA). All rights reserved.
Virulence n n n The virulence of an organism refers to the degree of pathogenicity or strength of that organism in its ability to produce disease. Because we cannot change the virulence of microorganisms, we must rely on our body defenses and specific immunizations. Avoid coming in contact with microorganisms by always following the infection control techniques. Copyright 2003, Elsevier Science (USA). All rights reserved.
Numbers n n n In addition to being virulent, pathogenic microorganisms must be present in large enough numbers to overwhelm the body’s defenses. The number of pathogens may directly be related to the amount of bioburden that is present. (Bioburden refers to organic materials such as blood and/or saliva. ) The use of the dental dam and high volume evacuation help minimize bioburden on surfaces and reduces the number of microorganisms in the aerosol. Copyright 2003, Elsevier Science (USA). All rights reserved.
Susceptible Host n n n A susceptible host is a person who is unable to resist infection by the pathogen. An individual who is in poor health, is chronically fatigued and under extreme stress, or has a weakened immune system is more likely to become infected. Therefore staying healthy, washing hands frequently, and keeping immunizations up-to-date will help members of the dental team resist infection and stay healthy. Copyright 2003, Elsevier Science (USA). All rights reserved.
Portal of Entry n n n To cause infection, the pathogens must have a portal of entry (or means of getting into the body). The portals of entry for airborne pathogens are through the mouth and nose. Bloodborne pathogens must have access to the blood supply as a means of entry into the body. This can occur through a break in the skin caused by a needle stick, a cut, or even a human bite. Copyright 2003, Elsevier Science (USA). All rights reserved.
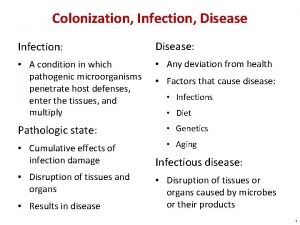
Types of Infections n n Acute infection: Symptoms are often quite severe and usually appear soon after the initial infection occurs. Chronic infections: Those in which the microorganism is present for a long period; some may persist for life. Latent infection: A persistent infection in which the symptoms come and go. Cold sores (oral herpes simplex) and genital herpes are latent viral infections. Opportunistic infections: Caused by normally nonpathogenic organisms and occur in individuals whose resistance is decreased or compromised. Copyright 2003, Elsevier Science (USA). All rights reserved.
Methods of Disease Transmission n Direct transmission: By coming into direct contact with the infectious lesion or infected body fluids (e. g. , blood, saliva, semen, vaginal secretions). Indirect: Transfer of organisms to a susceptible person can occur by, for example, handling contaminated instruments or touching contaminated surfaces and then touching the face, eyes, or mouth. Splash or spatter: Diseases can be transmitted during a dental procedure by splashing the mucosa (mouth or eyes) or nonintact skin with blood or bloodcontaminated saliva. Copyright 2003, Elsevier Science (USA). All rights reserved.
Methods of Disease Transmission- cont’d n n Airborne transmission, also known as droplet infection: Spread of disease through droplets of moisture containing bacteria or viruses. Aerosols: Containing saliva, blood, and microorganisms are created by the use of the highspeed handpiece, air-water syringe, and ultrasonic scaler during dental procedures. n Mists: Droplet particles larger than those generated by the aerosol spray. n Spatter: Large droplet particles contaminated with blood, saliva, and other debris. Copyright 2003, Elsevier Science (USA). All rights reserved.
Methods of Disease Transmission- cont’d n n Parenteral transmission can occur through needlestick injuries, human bites, cuts, abrasions, or any break in the skin. Bloodborne transmission occurs through direct or indirect contact with blood and other body fluids. Food and water transmission occurs by contaminated food that has not been cooked or refrigerated properly or water that has been contaminated with human or animal fecal material. Fecal/oral transmission: Many pathogens are present in fecal matter. If proper sanitation procedures, such as handwashing after use of the toilet, are not followed, these pathogens may be transmitted by touching another person or by contact with surfaces or food. Copyright 2003, Elsevier Science (USA). All rights reserved.
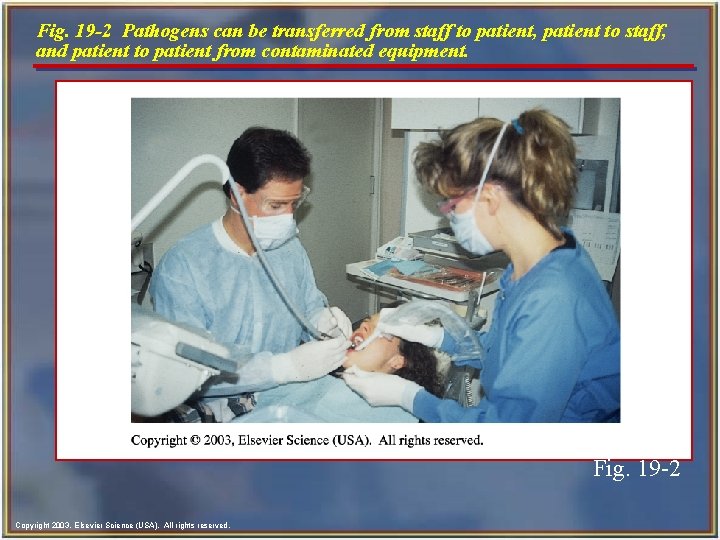
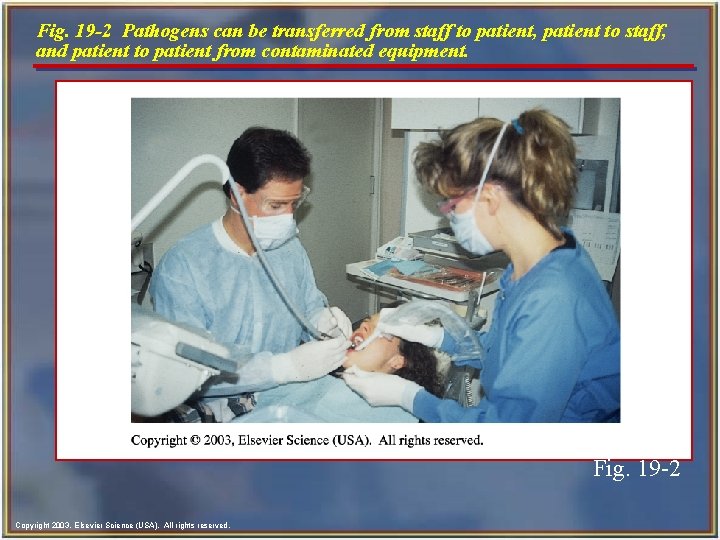
Fig. 19 -2 Pathogens can be transferred from staff to patient, patient to staff, and patient to patient from contaminated equipment. Fig. 19 -2 Copyright 2003, Elsevier Science (USA). All rights reserved.
Disease Transmission in the Dental Office n Every dental office should have an infection control program designed to prevent the transmission of disease from: • Patient to dental team • Dental team to patient • Patient to patient • Dental office to community (includes dental team’s family) • Community to patient Copyright 2003, Elsevier Science (USA). All rights reserved.
The Immune System n n The human body receives resistance to communicable diseases from the immune system. A communicable disease is one that can be transmitted from one person to another or by contact with the body fluids from another person. n When immunity is present at birth, it is called inherited immunity. n Immunity that is developed during a person’s lifetime is called acquired immunity. • Acquired immunity can occur either naturally or artificially. Copyright 2003, Elsevier Science (USA). All rights reserved.
Acquired Immunity n Acquired immunity can occur either naturally or artificially: 1. Natural acquired immunity: Occurs when a person has contracted and is recovering from a disease. 1. Active immunity 2. Passive immunity 2. Artificially acquired immunity: Antibodies can be introduced into the body artificially by immunization or vaccination. Copyright 2003, Elsevier Science (USA). All rights reserved.
OSHA Bloodborne Pathogens Standard n n n The bloodborne pathogen standard (BBP) is the most important infection control law in dentistry. It is designed to protect employees against occupational exposure to bloodborne pathogens, such as hepatitis B, hepatitis C, and human immunodeficiency virus (HIV). Employers are required to protect their employees from exposure to blood and other potentially infectious materials (OPIM) in the workplace and to provide proper care to the employee if an exposure should occur. Copyright 2003, Elsevier Science (USA). All rights reserved.
OSHA Bloodborne Pathogens Standardcont’d n n The BBP applies to any type of facility in which employees might be exposed to blood and/or other body fluids, including dental and medical offices, hospitals, funeral homes, emergency medical services, nursing homes, and the like. OSHA requires that a copy of the BBP be present in every dental office and clinic. Copyright 2003, Elsevier Science (USA). All rights reserved.
Requirements of the Standard n n n Exposure control plan clearly describes how that office complies with the standard. Universal precautions means that the same infection control procedures for any given dental procedure must be used for all patients receiving that same dental procedure; universal precautions are procedure specific, not patient specific. It is not possible to identify those individuals who are infectious, so infection precautions are used for all health care personnel and their patients. Copyright 2003, Elsevier Science (USA). All rights reserved.
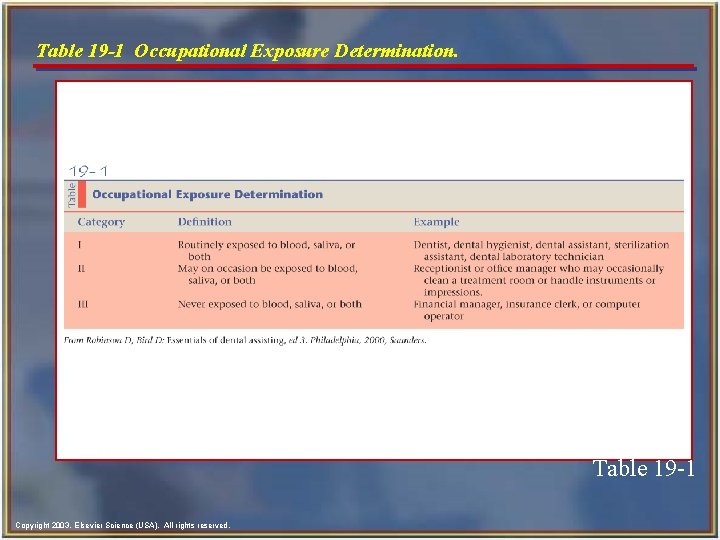
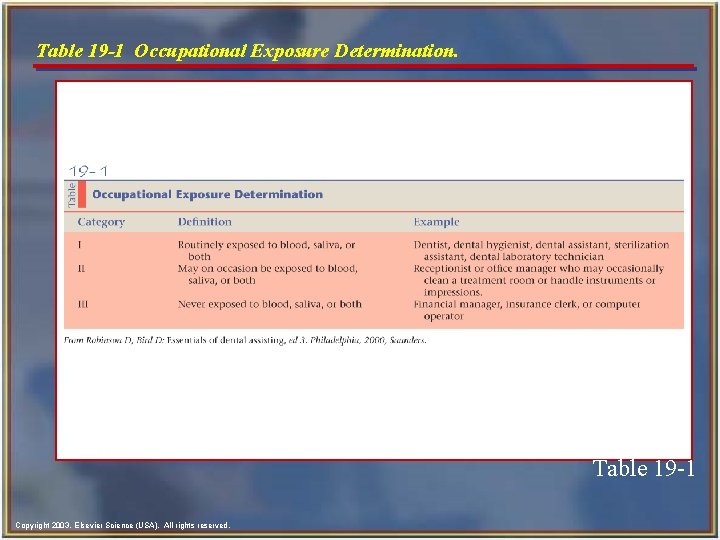
Table 19 -1 Occupational Exposure Determination. Table 19 -1 Copyright 2003, Elsevier Science (USA). All rights reserved.
Postexposure Incidents n n Before an accident occurs, the BBP requires the employer to have a plan in writing that explains exactly what steps the employee must follow after the exposure incident and the type of medical follow-up that will be provided to the employee at no charge. In addition, the employer must provide training to the employee regarding what to do if an exposure incident should occur. Copyright 2003, Elsevier Science (USA). All rights reserved.
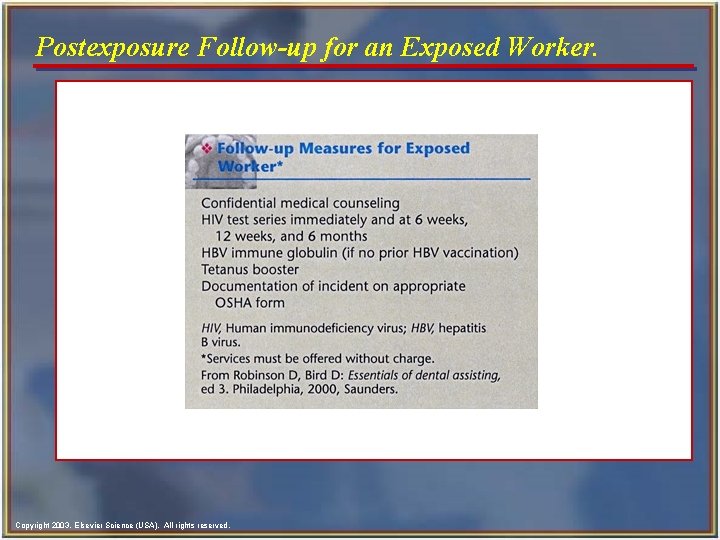
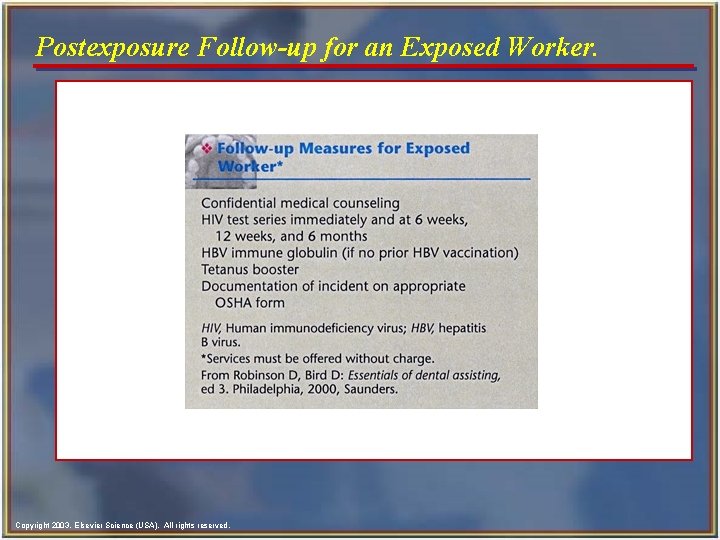
Postexposure Follow-up for an Exposed Worker. Copyright 2003, Elsevier Science (USA). All rights reserved.
Hepatitis B Immunization n OSHA requires the dentist to offer the hepatitis B virus (HBV) vaccination series to all employees whose jobs include category I and II tasks. n Vaccine must be offered within 10 days of employment. n The dentist/employer must obtain proof from the physician who administered the vaccination. n n The employee has the right to refuse the HBV vaccine; however, the employee must sign an informed refusal form that is kept on file in the dental office. The employee always has the right to change his or her mind and receive the vaccine at a later date at no charge. Copyright 2003, Elsevier Science (USA). All rights reserved.
Hepatitis B Vaccine n n n The vaccine is administered in a series of three injections. The most common vaccination schedule is 0, 1, and 6 months. The preferred injection site is in the deltoid muscle (on the arm) because the seroconversion rate (development of immunity) is higher than when the vaccine is administered in the buttocks. The Centers for Disease Control and Prevention (CDC) state that pregnancy should not be considered a contraindication to the HBV vaccine; however, the woman’s obstetrician should be consulted. Copyright 2003, Elsevier Science (USA). All rights reserved.
Postvaccine Testing n n n Between 6 weeks and 6 months after the final vaccination of the series has been completed, it is recommended that a blood test be performed to ensure that the individual has developed immunity. This testing is not required by current OSHA regulations. Individuals who have not developed immunity should be evaluated by their physician to determine the need for a additional dose of the HBV vaccine. Copyright 2003, Elsevier Science (USA). All rights reserved.
Need for a Booster n n n Routine booster doses of the HBV vaccine are not recommended by the CDC. The CDC does not recommend routine blood testing (after the initial testing to determine initial immunity) to monitor the HBV antibody level in individuals who have already had the vaccine. The exception to this recommendation is if an immunized individual had a documented exposure incident and the attending physician orders the administration of a booster dose. Copyright 2003, Elsevier Science (USA). All rights reserved.
Employee Medical Records n n n The dentist/employer must keep a confidential medical record for each employee. These records are confidential and must be stored in a locked file. The employer must keep these records for 30 years. Copyright 2003, Elsevier Science (USA). All rights reserved.
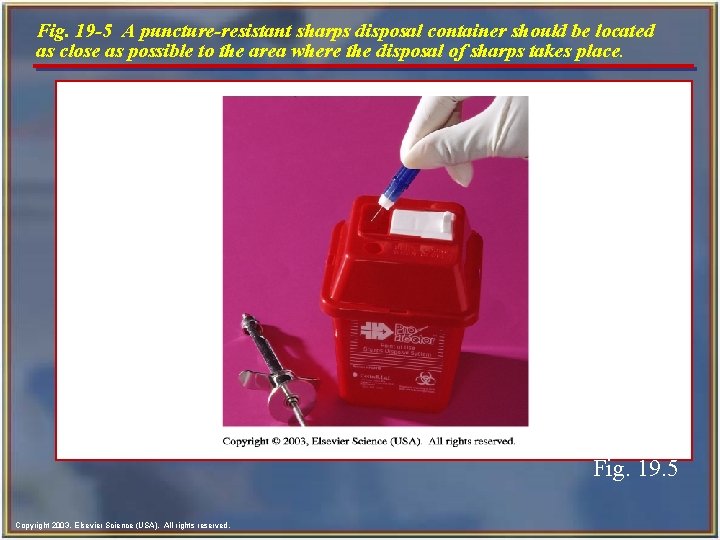
Managing Contaminated Sharps n n Contaminated needles and other disposable sharps, such as scalpel blades, orthodontic wires, and broken glass, must be placed into a sharps container. The sharps container must be puncture-resistant, closable, leakproof, and color-coded or labeled with the biohazard symbol. n Sharps containers must be located as close as possible to the place of immediate disposal. n Do not cut, bend, or break the needles before disposal. n Never attempt to remove a needle from a disposable syringe. Copyright 2003, Elsevier Science (USA). All rights reserved.
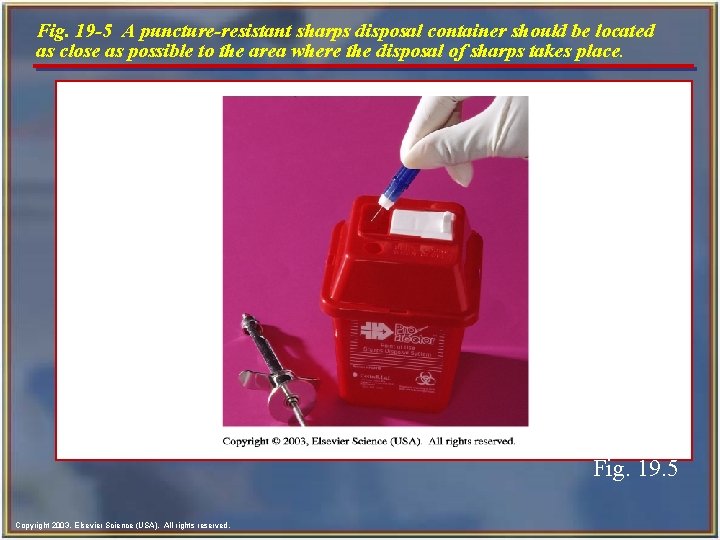
Fig. 19 -5 A puncture-resistant sharps disposal container should be located as close as possible to the area where the disposal of sharps takes place. Fig. 19. 5 Copyright 2003, Elsevier Science (USA). All rights reserved.
Handwashing n Wash your hands each time before you put on gloves and immediately after you remove gloves. n Wash your hands when you inadvertently touch contaminated objects or surfaces while barehanded. n n n Always use liquid soap during handwashing. Bar soap should never be used because it may transmit contamination. For most routine dental procedures, such as examinations and nonsurgical procedures, an antimicrobial soap can be used. For surgical procedures, you should use a germicidal surgical scrub product. Copyright 2003, Elsevier Science (USA). All rights reserved.
Hand Care n n Dry hands well before donning gloves. Keep nails short and well manicured, and rings, except for wedding rings, fingernail polish, and artificial nails are not to be worn at work. Microorganisms thrive around rough cuticles and can enter the body through any break in the skin. Dental personnel with open sores or weeping dermatitis must avoid activities involving direct patient contact and handling contaminated instruments or equipment until the condition on the hands is healed. Copyright 2003, Elsevier Science (USA). All rights reserved.
Personal Protective Equipment (PPE) n n OSHA requires the employer to provide employees with appropriate personal protective equipment (PPE) without charge to the employee. Examples of PPE include: • Protective clothing • Surgical masks • Face shields • Protective eyewear • Disposable patient treatment gloves • Heavy-duty utility gloves Copyright 2003, Elsevier Science (USA). All rights reserved.
Protective Clothing n n Types of protective clothing can include smocks, slacks, skirts, laboratory coats, surgical scrubs (hospital operating room clothing), scrub (surgical) hats, pants, and shoe covers. The type of protective clothing you should wear is based on the degree of anticipated exposure to infectious materials. n The BBP prohibits the employee from taking protective clothing home to be laundered. n Laundering contaminated protective clothing is the responsibility of the employer. Copyright 2003, Elsevier Science (USA). All rights reserved.
Protective Clothing Requirements n n Protective clothing should be made of fluid-resistant material. To minimize the amount of uncovered skin, clothing should have long sleeves and a high neckline. Note: The type and characteristics of protective clothing depend on the degree of exposure anticipated. The design of the sleeve should allow the cuff to be tucked inside the band of the glove. During high-risk procedures, protective clothing must cover dental personnel at least to the knees when seated. • Buttons, trim, zippers, and other ornamentation should be kept to a minimum. Copyright 2003, Elsevier Science (USA). All rights reserved.
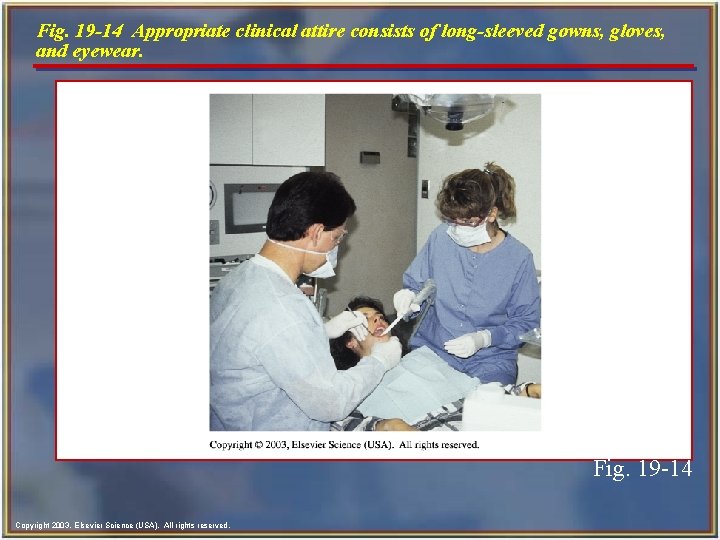
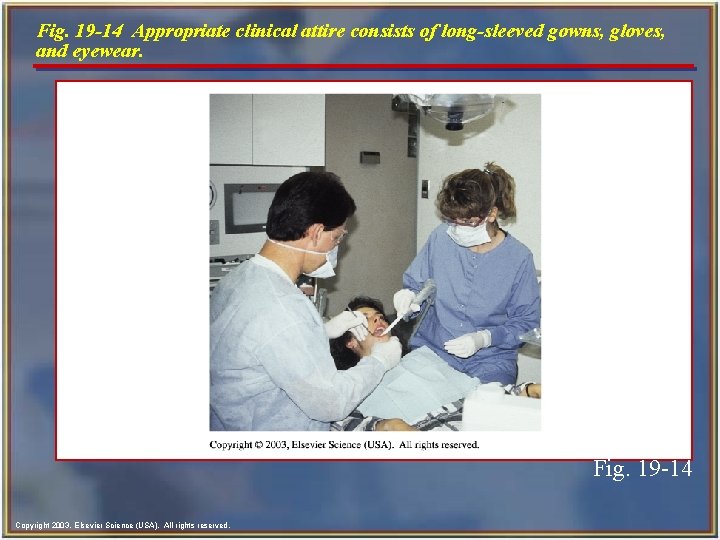
Fig. 19 -14 Appropriate clinical attire consists of long-sleeved gowns, gloves, and eyewear. Fig. 19 -14 Copyright 2003, Elsevier Science (USA). All rights reserved.
Protective Masks n n n A mask is worn over the nose and mouth to protect you from inhaling possible infectious organisms spread by the aerosol spray of the handpiece or air-water syringe and accidental splashes. A mask with at least 95% filtration efficiency for particles 3 to 5 mm in diameter should be worn whenever splash or spatter is likely. The two most commonly used types of masks are the dome-shaped and flat types. Copyright 2003, Elsevier Science (USA). All rights reserved.
Guidelines for the Use of Masks n n n Masks should be changed for every patient or more often. Masks should be handled by touching the side edges only to avoid contact with the more heavily contaminated body of the mask. The mask should conform well to the shape of the face. Masks should not contact the mouth when being worn because the moisture generated will decrease the mask filtration efficiency. A damp or wet mask is not an effective mask. Copyright 2003, Elsevier Science (USA). All rights reserved.
Protective Eyewear n Protective eyewear is worn to protect eyes against the danger of eye damage resulting from aerosolized pathogens. n Protective eyewear also prevents splattered solutions or caustic chemicals from injuring the eyes. n n n OSHA requires the use of eyewear with both front and side protection (solid side shields) for use during exposureprone procedures. If you wear contact lens, you must wear protective eyewear with side shields or a face shield. After each treatment or patient visit, clean and decontaminate your protective eyewear according to the manufacturer's instructions. Copyright 2003, Elsevier Science (USA). All rights reserved.
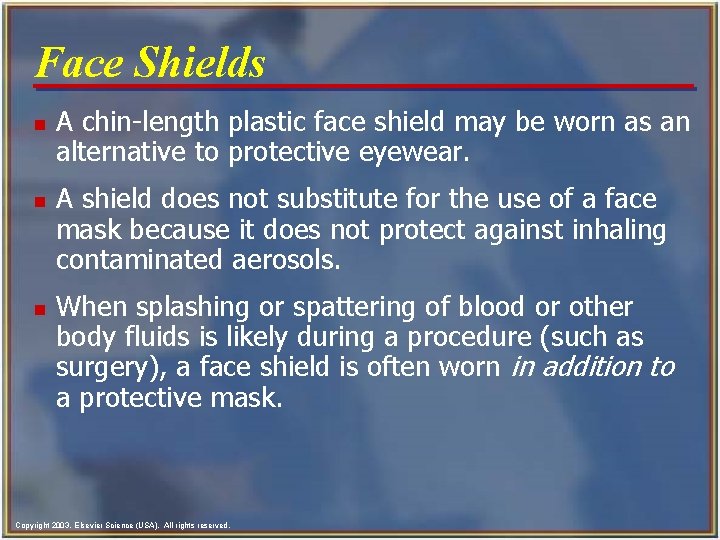
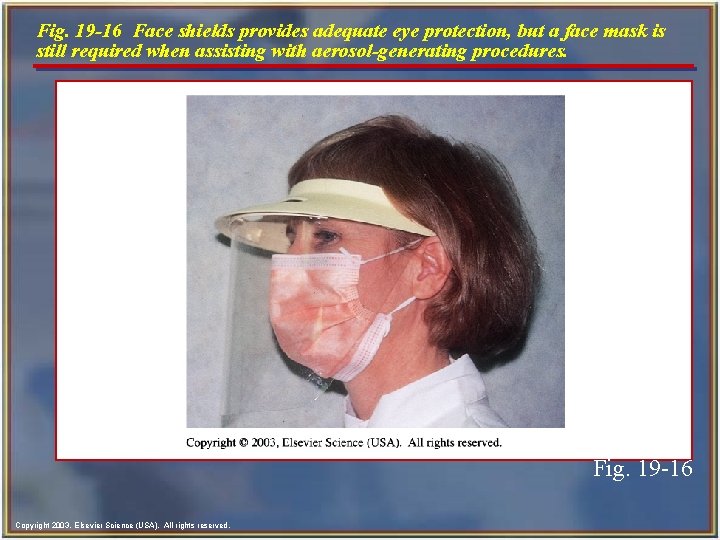
Face Shields n n n A chin-length plastic face shield may be worn as an alternative to protective eyewear. A shield does not substitute for the use of a face mask because it does not protect against inhaling contaminated aerosols. When splashing or spattering of blood or other body fluids is likely during a procedure (such as surgery), a face shield is often worn in addition to a protective mask. Copyright 2003, Elsevier Science (USA). All rights reserved.
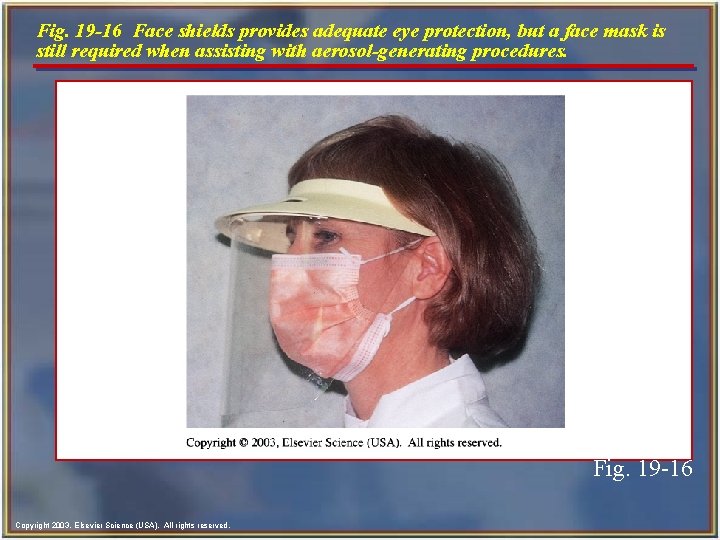
Fig. 19 -16 Face shields provides adequate eye protection, but a face mask is still required when assisting with aerosol-generating procedures. Fig. 19 -16 Copyright 2003, Elsevier Science (USA). All rights reserved.
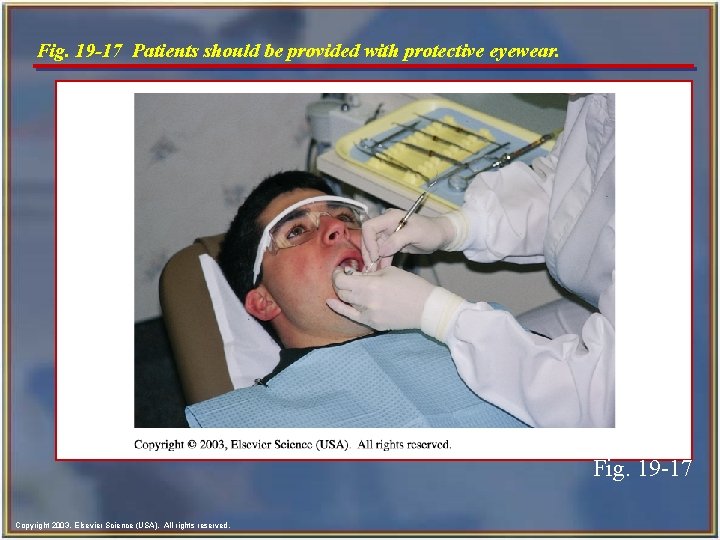
Protective Eyewear for Patients n n Patients should be provided with protective eyewear because they also may be subject to eye damage during the procedure. This may result from: • Handpiece spatter • Spilled or splashed dental materials, including caustic chemical agents • Airborne bits of acrylic or tooth fragments Copyright 2003, Elsevier Science (USA). All rights reserved.
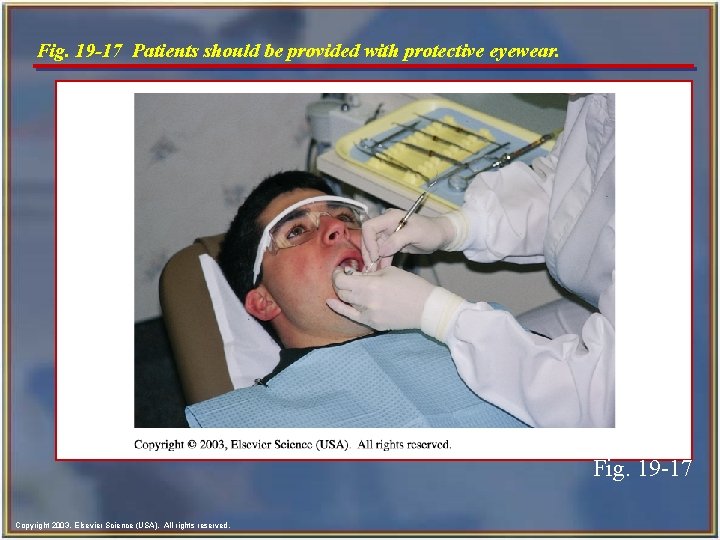
Fig. 19 -17 Patients should be provided with protective eyewear. Fig. 19 -17 Copyright 2003, Elsevier Science (USA). All rights reserved.
Gloves n n Gloves must be worn by the dentist, dental assistant, and dental hygienist during all patient treatment in which there is the possibility of contact with the patient's blood, saliva, or mucous membranes or with contaminated items or surfaces. The types of gloves used in a dental practice should be determined by the various procedures performed in the practice. Copyright 2003, Elsevier Science (USA). All rights reserved.
Guidelines for the Use of Gloves n n All gloves used in patient care must be discarded after a single use. These gloves may not be washed, disinfected, or sterilized; however, they may be rinsed with water to remove excess powder. Latex, vinyl, or other disposable medical-quality gloves may be used for patient examinations and dental procedures. Torn or damaged gloves must be replaced immediately. Copyright 2003, Elsevier Science (USA). All rights reserved.
Guidelines for the Use of Gloves- cont’d n Do not wear jewelry under gloves. (Rings harbor pathogens and may tear the glove. ) n Change gloves frequently. (If the procedure is long, change gloves about once each hour. ) n n Contaminated gloves should be removed before leaving the chairside during patient care and replaced with new gloves before returning to patient care. Hands must be washed after glove removal and before regloving. Copyright 2003, Elsevier Science (USA). All rights reserved.
Gloves Damaged During Treatment n n Gloves are effective only when they are intact (not damaged, torn, ripped, or punctured). If gloves are damaged during treatment, they must be changed immediately. The procedure for regloving is: 1. Excuse yourself and leave the chairside. 2. Remove and discard the damaged gloves. 3. Wash hands thoroughly. 4. Reglove before returning to the dental procedure. Copyright 2003, Elsevier Science (USA). All rights reserved.

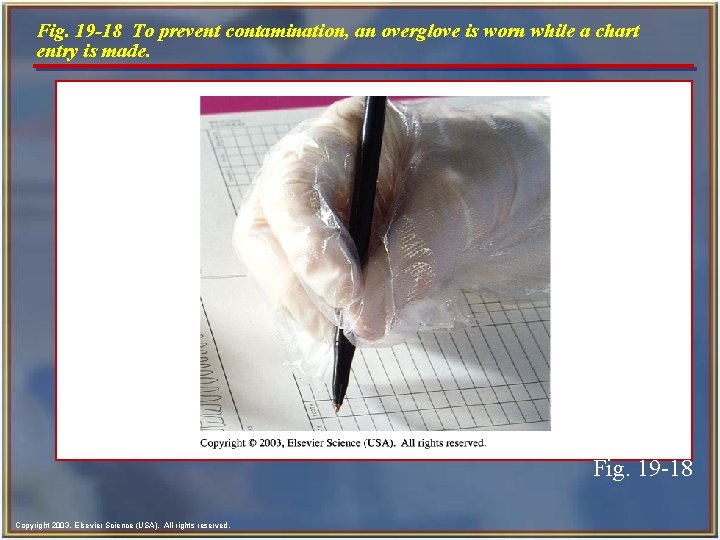
Overgloves n n Overgloves, which also are known as "food handler" gloves, are made of lightweight, inexpensive, clear plastic. These may be worn over contaminated treatment gloves (overgloving) to prevent the contamination of clean objects handled during treatment. Copyright 2003, Elsevier Science (USA). All rights reserved.
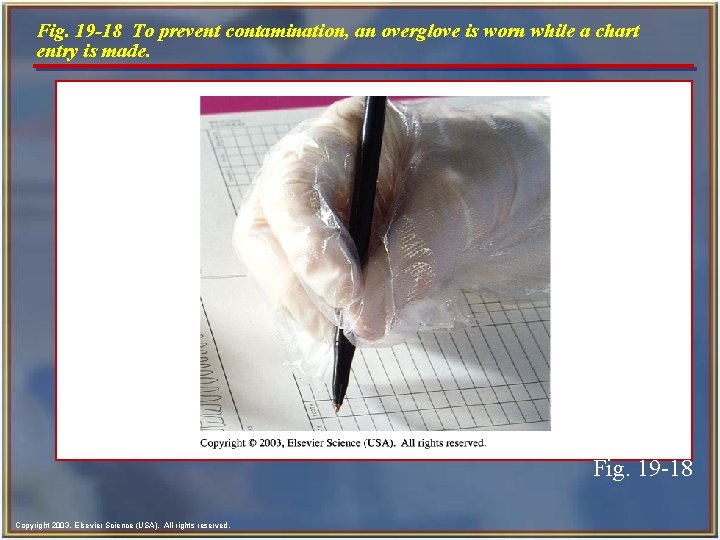
Fig. 19 -18 To prevent contamination, an overglove is worn while a chart entry is made. Fig. 19 -18 Copyright 2003, Elsevier Science (USA). All rights reserved.
Guidelines for the Use of Overgloves n n Overgloves are not acceptable alone as a hand barrier or for intraoral procedures. Overgloves must be worn carefully to avoid contamination during handling with contaminated procedure gloves. Overgloves are placed before the secondary procedure is performed and are removed before the patient treatment that was in progress is resumed. Overgloves are discarded after a single use. Copyright 2003, Elsevier Science (USA). All rights reserved.
Sterile Surgical Gloves n n n Sterile gloves should be worn for invasive procedures involving the cutting of bone or significant amounts of blood or saliva, such as oral surgery or periodontal treatment. Sterile gloves are supplied in prepackaged units to maintain sterility before use. They are provided in specific sizes and are fitted to the left or right hand. Copyright 2003, Elsevier Science (USA). All rights reserved.
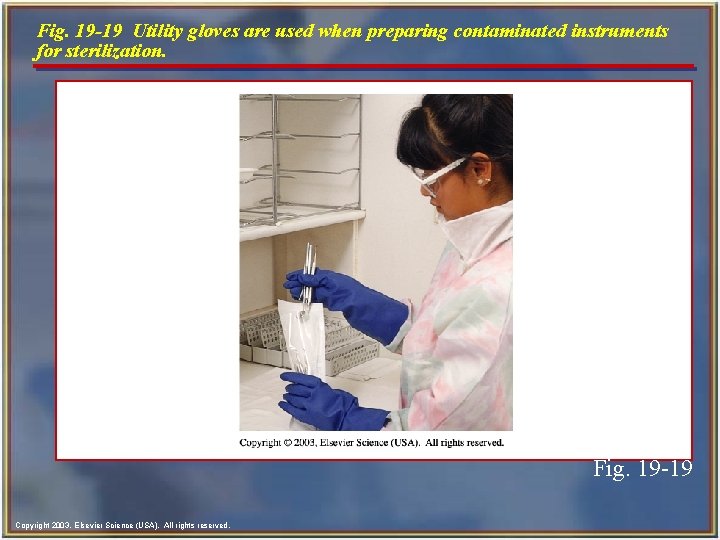
Utility Gloves n n Utility gloves are not used for direct patient care. Utility gloves must be worn when the treatment room is cleaned and disinfected between patients, while contaminated instruments are being cleaned or handled, and for surface cleaning and disinfecting. Utility gloves may be washed, disinfected, or sterilized and reused; however, they must be discarded when they become worn and no longer have the ability to provide barrier protection. Used utility gloves must be considered contaminated and handled appropriately until they have been properly disinfected or sterilized. Copyright 2003, Elsevier Science (USA). All rights reserved.
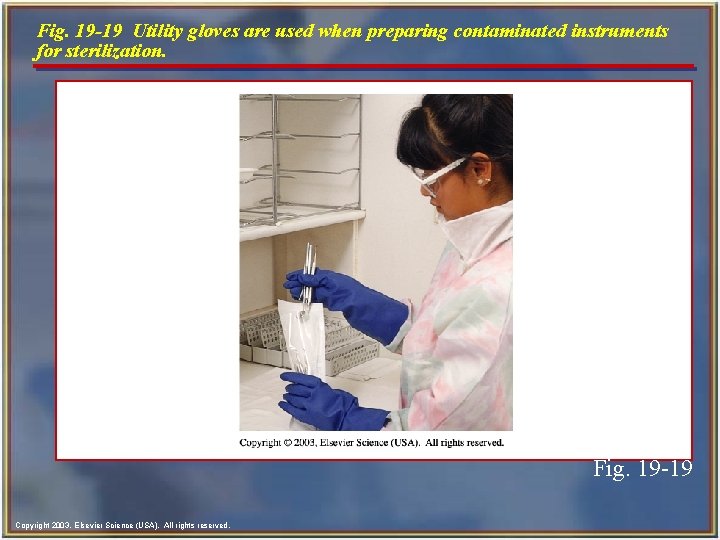
Fig. 19 -19 Utility gloves are used when preparing contaminated instruments for sterilization. Fig. 19 -19 Copyright 2003, Elsevier Science (USA). All rights reserved.
Nonlatex-Containing Gloves n n Health care providers or patients may experience serious allergic reactions to latex. For the person who is sensitive to latex, there are gloves made from vinyl, nitrile, and other nonlatexcontaining materials. Copyright 2003, Elsevier Science (USA). All rights reserved.
Maintaining Infection Control While Gloved n n n During a dental procedure, it may be necessary to touch surfaces or objects such as drawer handles or materials containers. If you touch these with a gloved hand, both the surface and glove become contaminated. To minimize the possibility of cross-contamination, you can use an overglove when it is necessary to touch a surface. Copyright 2003, Elsevier Science (USA). All rights reserved.
Glove Caution n n Chemicals such as glutaraldehyde and acrylates readily permeate (pass through) latex gloves and can irritate the skin, and that irritation is mistaken for an allergic reaction to the chemicals in the latex glove. This is why latex gloves should never be worn when handling chemicals. Copyright 2003, Elsevier Science (USA). All rights reserved.
Latex Allergies n There are three common types of latex allergic reactions. n Two types involve an immune reaction, and one type involves only surface irritation. • Irritant dermatitis, a nonimmunologic process, (does not involve the body's immune system) is caused by contact with a substance that produces a chemical irritation to the skin. The skin becomes reddened, dry, irritated, and, in severe cases, cracked. Irritant dermatitis can be reversed by identifying and correcting the cause of the problem. Copyright 2003, Elsevier Science (USA). All rights reserved.
Latex Allergies- cont’d n Type IV sensitivity • The most common type of latex allergy, type IV sensitivity, is a delayed contact reaction, and it involves the immune system. • It may take up to 48 or 72 hours for the red, itchy rash to appear. • The reactions are limited to the areas of contact and do not involve the entire body. • An immune response is produced by the chemicals that are used to process the latex used in manufacturing the gloves; it is not caused by the proteins in the latex. Copyright 2003, Elsevier Science (USA). All rights reserved.
Latex Allergies- cont’d n Type I allergic reaction • This is the most dangerous type of latex allergy, and it can result in death. • The reaction is in response to the latex protein in the glove (in contrast to the reaction to chemical additives in type IV). • There is a severe immunologic (immune system) response that usually occurs 2 to 3 minutes after the latex allergens contact the skin or mucous membranes. Copyright 2003, Elsevier Science (USA). All rights reserved.
Treatment of Latex Allergies n n There is no specific cure for latex allergy. The only options are prevention, avoidance of latexcontaining products, and treatment of the symptoms. Anyone who suspects he or she may have an allergy to latex should see a qualified health care provider to have a test to confirm the allergy. Once anyone is diagnosed as having a latex allergy, he or she should practice latex avoidance in all aspects of his or her personal and professional lives. Copyright 2003, Elsevier Science (USA). All rights reserved.
Remember… n When one employee in the dental office has been diagnosed as having a latex allergy, all staff members should use practices to minimize the use of latex-containing products. These practices include the wearing of powder-free gloves by all dental staff members to minimize the risk of airborne latex particles. Copyright 2003, Elsevier Science (USA). All rights reserved.
Latex-Sensitive Patients n n In the health care setting, patients with latex allergies should be treated using alternatives to latex. Vinyl gloves and a nonlatex rubber dam should be available in all dental offices. Copyright 2003, Elsevier Science (USA). All rights reserved.
Fig. 19 -21 Latex-free gloves. Fig. 19 -21 Copyright 2003, Elsevier Science (USA). All rights reserved.
Waste Management in the Dental Office n n n Dental practices are subject to a wide variety of federal, state, and local regulations concerning waste management issues. The Environmental Protection Agency (EPA) and the majority of state and local regulations do not categorize saliva or saliva-soaked items as infectious waste. Conversely, because of the high probability that blood may be carried in saliva during dental procedures, CDC guidelines and OSHA regulations consider saliva in dentistry to be a potentially infectious body fluid. Copyright 2003, Elsevier Science (USA). All rights reserved.

Classifications of Waste n n n General waste: All nonhazardous, nonregulated waste should be discarded in covered containers. Examples include disposable paper towels, paper mixing pads, and empty food containers. Contaminated waste is waste that has had contact with blood or other body fluids. Examples include used barriers and patient napkins. Hazardous waste poses a risk to humans and the environment. Toxic chemicals and materials are hazardous waste. Examples include scrap amalgam, spent fixer solution, and lead foil from x-ray film packets. Copyright 2003, Elsevier Science (USA). All rights reserved.
Classifications of Waste- cont’d n n Some items, such as extracted teeth with amalgam restorations, may be both hazardous waste (because of the amalgam) and infectious waste (because of the blood). Infectious or regulated waste (biohazard), is contaminated waste that is capable of transmitting an infectious disease. • Blood and blood-soaked materials • Pathological waste • Sharps Copyright 2003, Elsevier Science (USA). All rights reserved.
Handling Dental Office Waste n n Contaminated waste: Items that may contain the body fluids of patients, such as gloves and patient napkins, should be placed in a lined trash receptacle. Medical waste is any solid waste that is generated in the diagnosis, treatment, or immunization of human beings or animals in research. • Infectious waste is a subset of medical waste. Only a small percentage of medical waste is infectious and needs to be regulated. • Must be labeled with the universal biohazard symbol. Copyright 2003, Elsevier Science (USA). All rights reserved.
Other Infection Control Considerations n n n Never eat, drink, smoke, apply cosmetics or lip balm, or handle contact lenses in any area of the dental office where there is possible contamination, such as the dental treatment rooms, dental laboratory, sterilization area, or the x-ray processing area. Never store food or drink in refrigerators that contain any potentially contaminated items. You can minimize the amount of splash and spatter contamination produced during dental procedures with the skillful use of a dental dam and high-volume evacuation. Copyright 2003, Elsevier Science (USA). All rights reserved.
 Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Chapter 16 infection prevention and control
Chapter 16 infection prevention and control Chapter 16 infection control and standard precautions
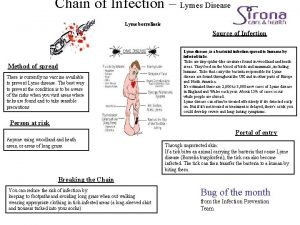
Chapter 16 infection control and standard precautions Chain of infection for lyme disease
Chain of infection for lyme disease An exogenous disease originates outside the body.
An exogenous disease originates outside the body. Chapter 15:5 sterilizing with an autoclave
Chapter 15:5 sterilizing with an autoclave One celled plantlike organisms that multiply rapidly
One celled plantlike organisms that multiply rapidly Chapter 10 infection control
Chapter 10 infection control Communicable disease and non communicable disease
Communicable disease and non communicable disease Phenolic disinfectants have milady
Phenolic disinfectants have milady Cbic recertification
Cbic recertification Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Factors that affect disease transmission
Factors that affect disease transmission Disease transmission
Disease transmission Factors that influence disease transmission
Factors that influence disease transmission Disease transmission
Disease transmission Labial mounting method
Labial mounting method Cic certification exam
Cic certification exam Infection control meaning
Infection control meaning Darkroom infection control guidelines
Darkroom infection control guidelines Learning objectives for infection control
Learning objectives for infection control Infection control conclusion
Infection control conclusion Neutropenic precautions
Neutropenic precautions Infection control is everyone's responsibility
Infection control is everyone's responsibility Infection control
Infection control Infection control
Infection control Infection control information
Infection control information Standard 3 infection control
Standard 3 infection control Infection control orientation
Infection control orientation Infection control
Infection control Infection control audits
Infection control audits Environmental controls infection control
Environmental controls infection control Examples of service excellence in healthcare
Examples of service excellence in healthcare Infection control committee
Infection control committee Conclusion of infection control
Conclusion of infection control 10 principles of infection control
10 principles of infection control Infection control champion
Infection control champion Unit 13 infection control
Unit 13 infection control Infection control surveyor worksheet
Infection control surveyor worksheet European centre for disease prevention and control
European centre for disease prevention and control Society for disease control and research
Society for disease control and research Pest and disease control
Pest and disease control Major disease of sugarcane
Major disease of sugarcane Transmission control protocol
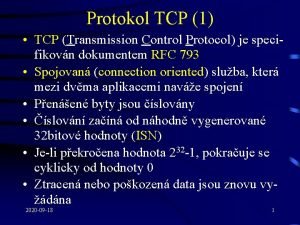
Transmission control protocol Transmission control block
Transmission control block Tcp (transmission control protocol) to protokół
Tcp (transmission control protocol) to protokół Transmission control protocol
Transmission control protocol Chapter 16 preventing infection
Chapter 16 preventing infection Chapter 15 preventing infection
Chapter 15 preventing infection Define infection prevention chapter 5
Define infection prevention chapter 5 Disease control phase
Disease control phase Disease control
Disease control Disease control
Disease control Center for disease control
Center for disease control Center for disease control
Center for disease control Chapter 35 immune system and disease
Chapter 35 immune system and disease Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease The human body in health and disease chapter 2 answer key
The human body in health and disease chapter 2 answer key The human body in health and disease chapter 2 answer key
The human body in health and disease chapter 2 answer key Chapter 2 the human body in health and disease
Chapter 2 the human body in health and disease Process and product control
Process and product control Negative control vs positive control examples
Negative control vs positive control examples Flow control and error control
Flow control and error control Wound infection continuum
Wound infection continuum