Infection Control Cannulation Venepuncture Infection Control Nurses NGT




- Slides: 25
Infection Control Cannulation & Venepuncture Infection Control Nurses NGT
Aims and Objectives • Discuss types of infection associated with venepuncture and cannulation. • List the measures taken to prevent infection. • Describe the safe handling of sharps. • List the first aid measures to be taken in a needlestick injury. • Describe the safe handling and transportation of specimens.
Types of infections associated with IV Devices • • • Local site infection. Phlebitis. Bacteraemia. Septicaemia. Metastatic infection.
Factors influencing the risk of infection • Duration of cannulation. • Type of cannula (e. g. peripheral, central, Hickman). • Insertion site. • Cannula material.

Staphylococcus epidermidis
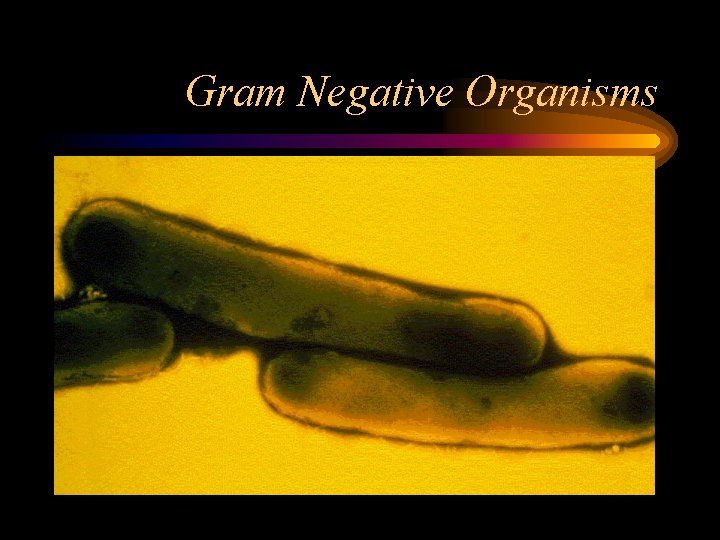
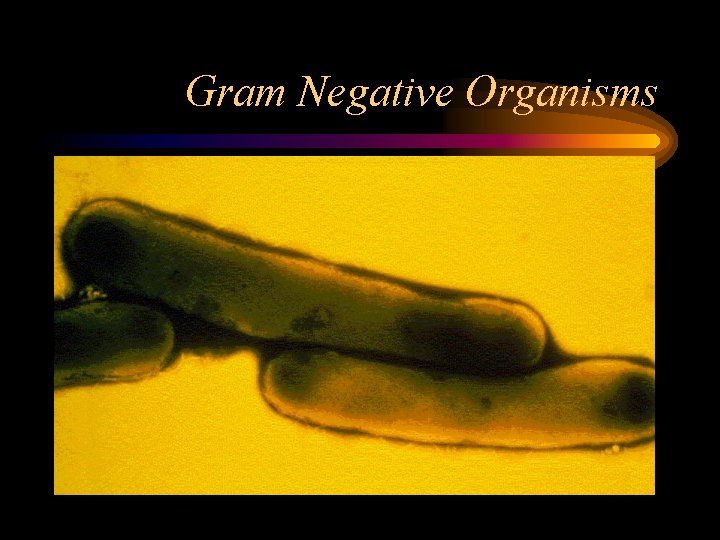
Gram Negative Organisms
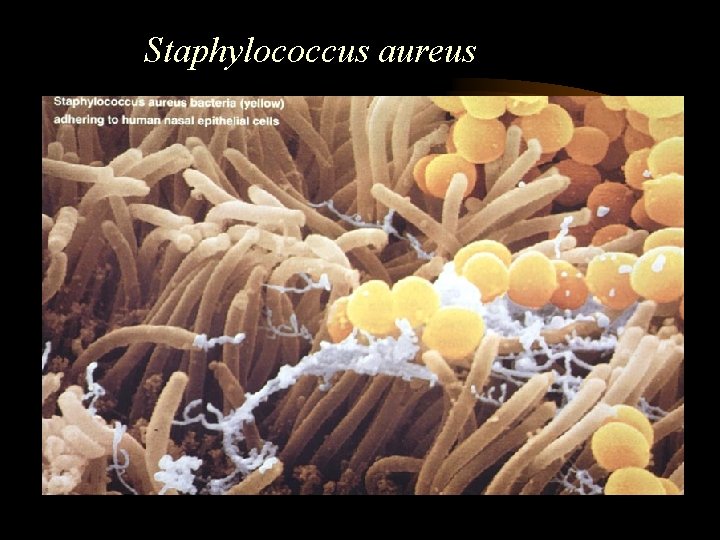
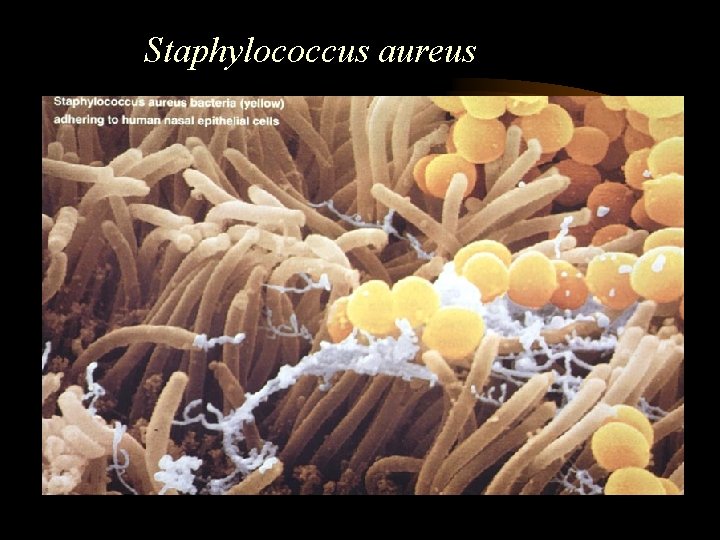
Staphylococcus aureus

Sources of Infection • • • All healthcare workers. The patient. The venflon or vacutainer. The disinfectant. The environment.
You are introducing a foreign object into a sterile area. Every IV device is an infection opportunity.

Other risks • Needlestick injury to the operator. • Cross infection of patients. • Needlestick injury to others.
How you can be exposed. • needlestick injury. • accidental splash contamination of broken skin and mucus membranes. Prevention strategies. • NO recapping of needles. • use of personal protective equipment e. g. gloves, aprons, goggles or face visors.
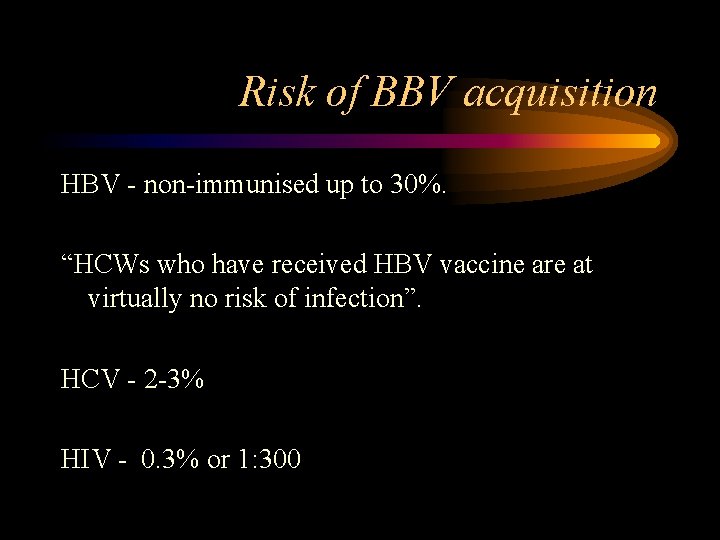
Risk of BBV acquisition HBV - non-immunised up to 30%. “HCWs who have received HBV vaccine are at virtually no risk of infection”. HCV - 2 -3% HIV - 0. 3% or 1: 300
Cross-infection disasters There have been reported outbreaks of HBV caused by nurses not changing their gloves. A healthcare worker ran out of butterflies, so she washed and reused them.
Preparation • • Have all your equipment in one place. Have some paper towels in case of spills. Have a sharps box. If necessary get some help.
What do you need? • • Training. Hand hygiene. Gloves. Sterile equipment within its expiry date and all packaging intact. • Skin cleansing. • Dressings.
Do you need help? • One of the leading causes of NSI is the patient moving unexpectedly. • More likely to get a NSI if inexperienced. • Don’t like the situation, don’t do it on your own.
NSI • • Bleed. Wash (don’t scrub). Cover. Report it, to the nurse in charge, then Occupational Health or A&E within 1 hour. • Treat. • Fill out an IR 1.
• This is the Needlestick Injury Flip chart for GGHB
After insertion • • • Dressing. Dispose of waste. Remove gloves. Hand hygiene. Document & care plan.

Labelling of specimens Biohazard labels should be applied to specimens known or suspected to contain blood borne viruses or tuberculosis.
Safe handling and transportation of specimens • Ensure container is leak-proof and can be sealed securely. • Remove all traces of blood from the outside of the container. • Place biohazard label on the container and form if appropriate. • Ensure the container is sealed in a specimen bag. • Ensure a fully completed form is placed in the separate pocket.
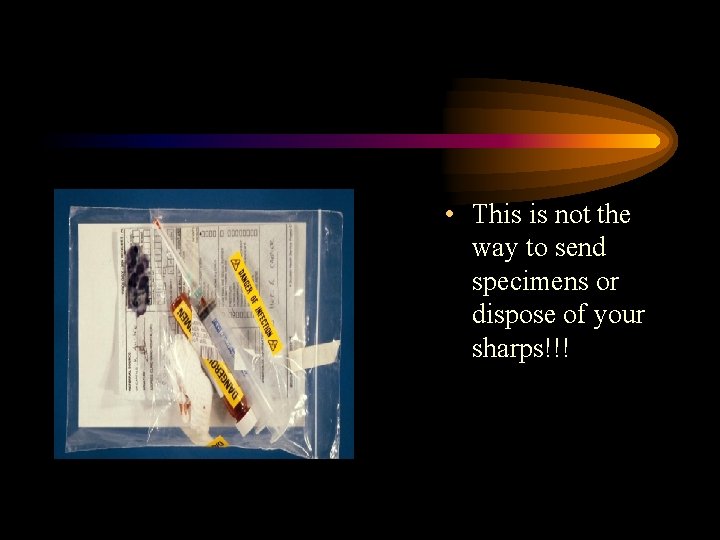
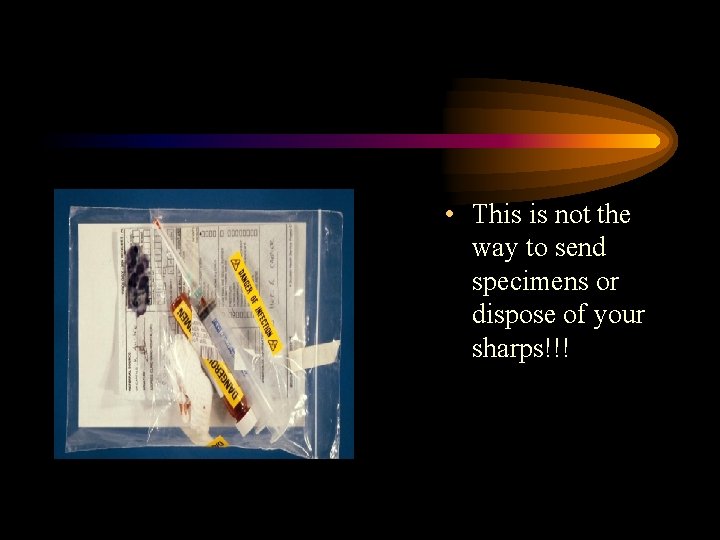
• This is not the way to send specimens or dispose of your sharps!!!
Remember! HAND HYGIENE. The most important measure in preventing infection.