Colonization Infection Disease Infection Disease A condition in
- Slides: 53
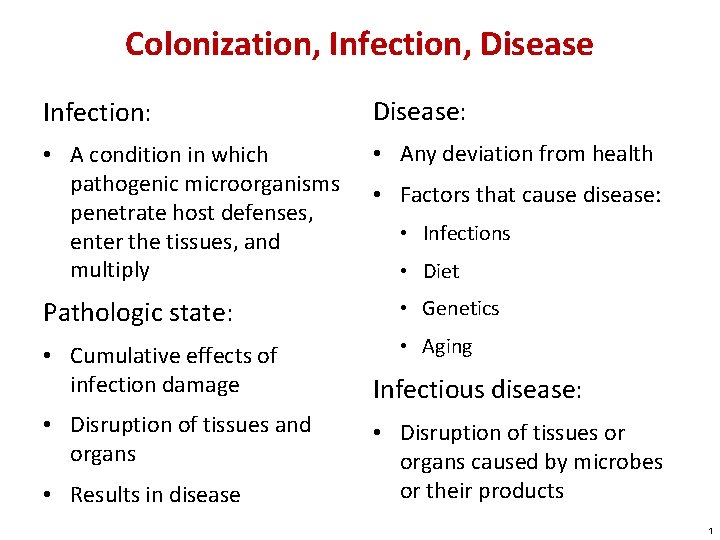
Colonization, Infection, Disease Infection: Disease: • A condition in which pathogenic microorganisms penetrate host defenses, enter the tissues, and multiply • Any deviation from health • Factors that cause disease: • Infections • Diet Pathologic state: • Genetics • Cumulative effects of infection damage • Aging • Disruption of tissues and organs • Results in disease Infectious disease: • Disruption of tissues or organs caused by microbes or their products 1
Resident Biota Normal biota: • Large and diverse collection of microbes living on and in the body • Also known as resident or indigenous biota or normal flora • Include an array of bacteria, fungi, protozoa, and viruses • These organisms have a profound effect on human biology 2
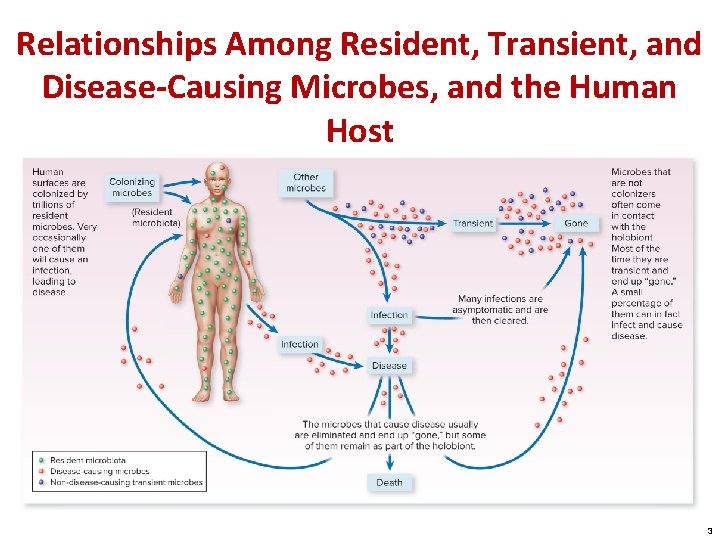
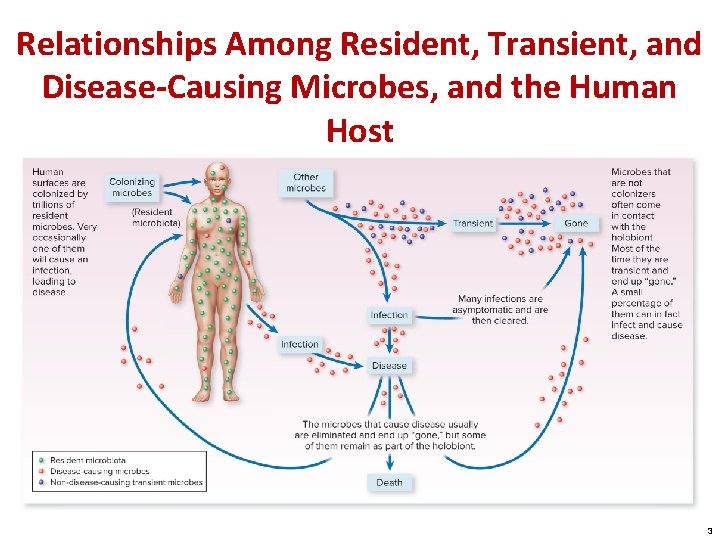
Relationships Among Resident, Transient, and Disease-Causing Microbes, and the Human Host 3
The Human Microbiome Project Preliminary results: • Human cells contain 22, 000 protein encoding genes; microbes that inhabit humans contain 8 million • We have a lot of microbes in places we used to think were sterile • All healthy people harbor potentially dangerous pathogens, but in low numbers 4
The Importance of Gut Biota The makeup of your intestinal biota can influence many facets of your overall health Differences in the gut microbiome have preliminarily been associated with differences in the risk for: • • Crohn’s disease Obesity Heart disease Asthma Autism Diabetes Moods 5
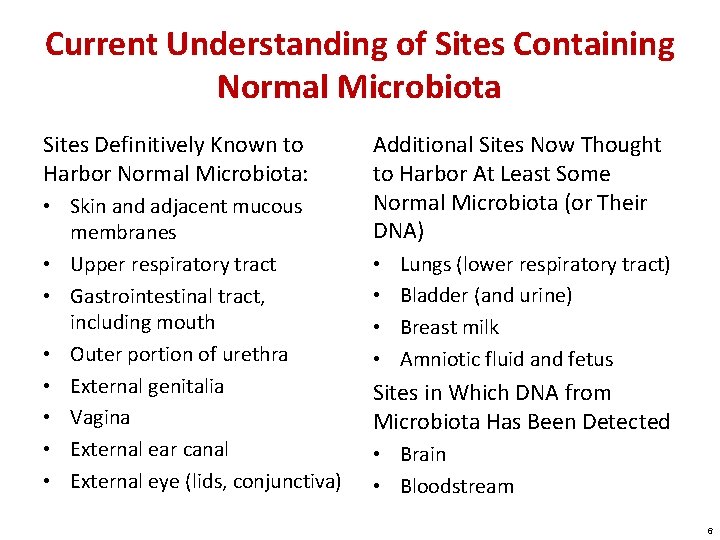
Current Understanding of Sites Containing Normal Microbiota Sites Definitively Known to Harbor Normal Microbiota: • Skin and adjacent mucous membranes • Upper respiratory tract • Gastrointestinal tract, including mouth • Outer portion of urethra • External genitalia • Vagina • External ear canal • External eye (lids, conjunctiva) Additional Sites Now Thought to Harbor At Least Some Normal Microbiota (or Their DNA) • • Lungs (lower respiratory tract) Bladder (and urine) Breast milk Amniotic fluid and fetus Sites in Which DNA from Microbiota Has Been Detected • Brain • Bloodstream 6
Acquiring Resident Biota Benefits of normal biota: • Influence the development of organs • Prevent the overgrowth of harmful microorganisms Microbial antagonism: • The general antagonistic effect “good” microbes have against intruder microorganisms • Microbes in a steady, established relationship are unlikely to be displaced by incoming microbes 7
Factors That Weaken Host Defenses and Increase Susceptibility to Infection • Age: the very young and the very old • Genetic defects in immunity and acquired defects in immunity (AIDS) • Pregnancy • Surgery and organ transplants • Underlying disease: cancer, liver malfunction, diabetes • Chemotherapy/immunosuppressive drugs • Physical and mental stress • Other infections 8
Endogenous Infections • Caused by biota already in the body • Can occur when normal biota is introduced to a site that was previously sterile • Example: Escherichia coli entering the bladder, resulting in a UTI 9
Initial Colonization of the Newborn A growing number of doctors and scientists believe fetuses are seeded with normal microbiota in utero • These microbes are important for healthy full-term pregnancies and healthy newborns We know exposure occurs during birth when the baby becomes colonized with the mother’s vaginal biota 10
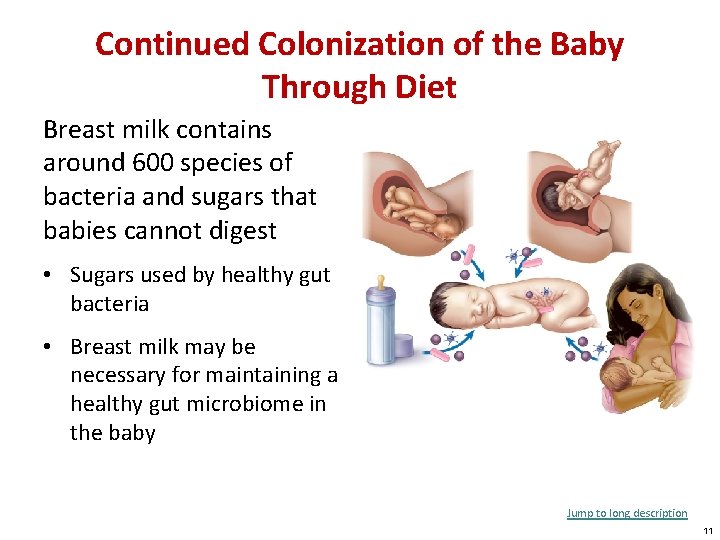
Continued Colonization of the Baby Through Diet Breast milk contains around 600 species of bacteria and sugars that babies cannot digest • Sugars used by healthy gut bacteria • Breast milk may be necessary for maintaining a healthy gut microbiome in the baby Jump to long description 11
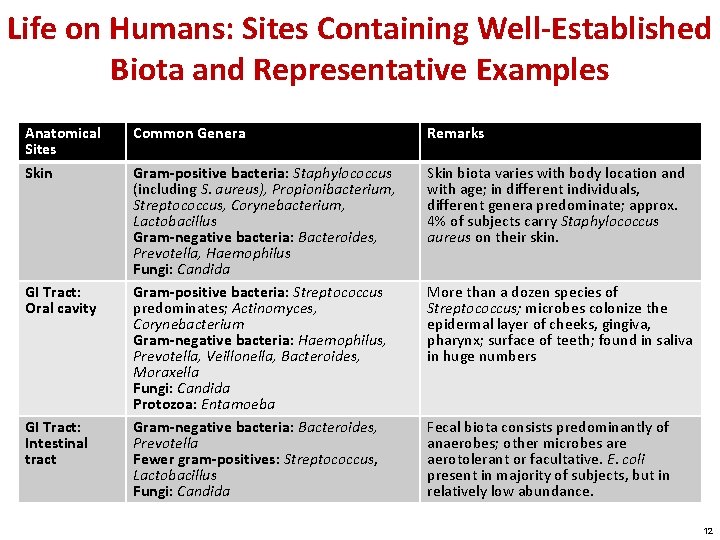
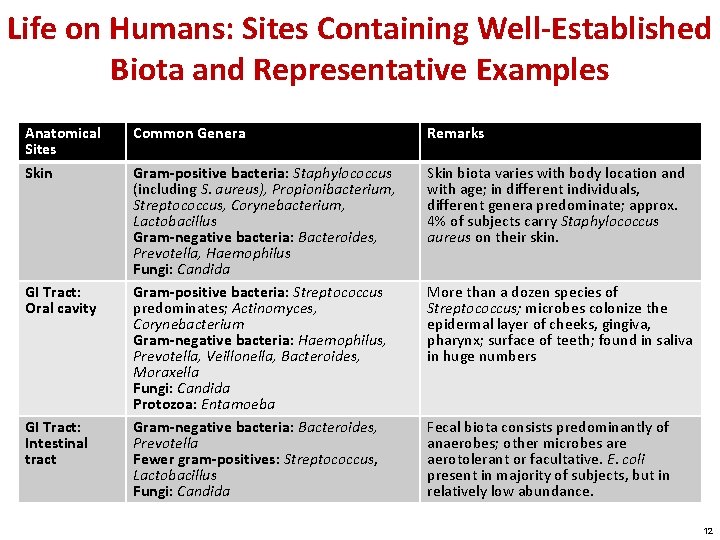
Life on Humans: Sites Containing Well-Established Biota and Representative Examples Anatomical Sites Skin GI Tract: Oral cavity GI Tract: Intestinal tract Common Genera Remarks Gram-positive bacteria: Staphylococcus (including S. aureus), Propionibacterium, Streptococcus, Corynebacterium, Lactobacillus Gram-negative bacteria: Bacteroides, Prevotella, Haemophilus Fungi: Candida Gram-positive bacteria: Streptococcus predominates; Actinomyces, Corynebacterium Gram-negative bacteria: Haemophilus, Prevotella, Veillonella, Bacteroides, Moraxella Fungi: Candida Protozoa: Entamoeba Gram-negative bacteria: Bacteroides, Prevotella Fewer gram-positives: Streptococcus, Lactobacillus Fungi: Candida Skin biota varies with body location and with age; in different individuals, different genera predominate; approx. 4% of subjects carry Staphylococcus aureus on their skin. More than a dozen species of Streptococcus; microbes colonize the epidermal layer of cheeks, gingiva, pharynx; surface of teeth; found in saliva in huge numbers Fecal biota consists predominantly of anaerobes; other microbes are aerotolerant or facultative. E. coli present in majority of subjects, but in relatively low abundance. 12
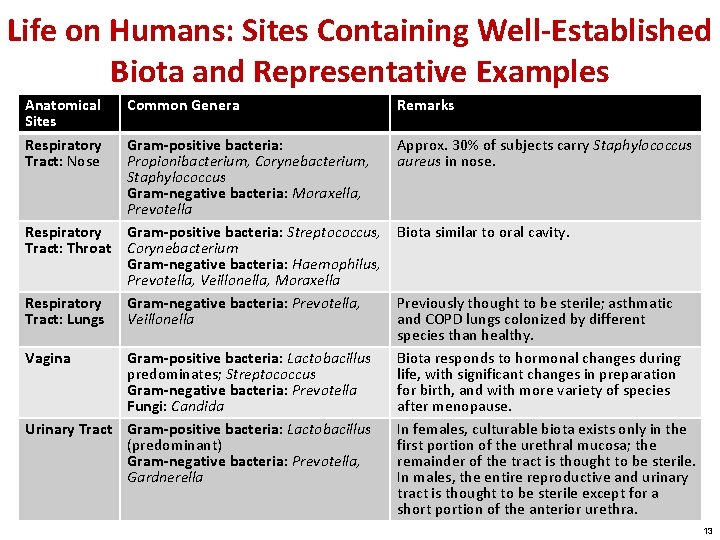
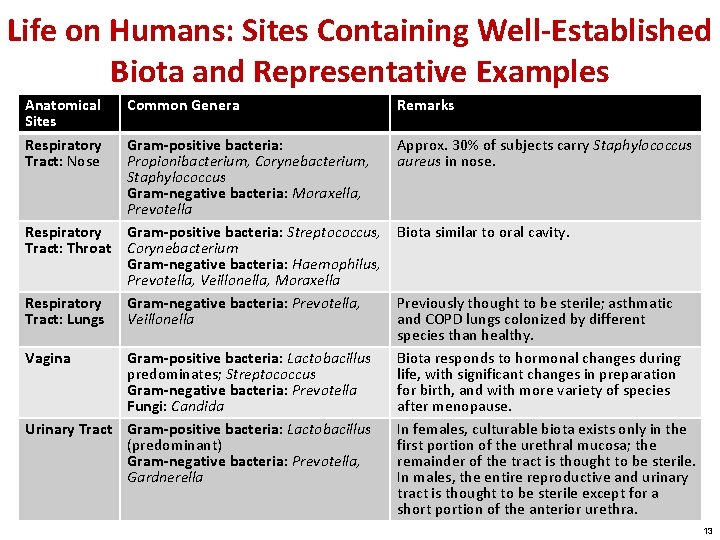
Life on Humans: Sites Containing Well-Established Biota and Representative Examples Anatomical Sites Respiratory Tract: Nose Respiratory Tract: Throat Respiratory Tract: Lungs Vagina Common Genera Remarks Gram-positive bacteria: Propionibacterium, Corynebacterium, Staphylococcus Gram-negative bacteria: Moraxella, Prevotella Gram-positive bacteria: Streptococcus, Corynebacterium Gram-negative bacteria: Haemophilus, Prevotella, Veillonella, Moraxella Gram-negative bacteria: Prevotella, Veillonella Approx. 30% of subjects carry Staphylococcus aureus in nose. Gram-positive bacteria: Lactobacillus predominates; Streptococcus Gram-negative bacteria: Prevotella Fungi: Candida Urinary Tract Gram-positive bacteria: Lactobacillus (predominant) Gram-negative bacteria: Prevotella, Gardnerella Biota similar to oral cavity. Previously thought to be sterile; asthmatic and COPD lungs colonized by different species than healthy. Biota responds to hormonal changes during life, with significant changes in preparation for birth, and with more variety of species after menopause. In females, culturable biota exists only in the first portion of the urethral mucosa; the remainder of the tract is thought to be sterile. In males, the entire reproductive and urinary tract is thought to be sterile except for a short portion of the anterior urethra. 13
The Progress of Infection Pathogen: • A microbe whose relationship with its host is parasitic • Results in infection and disease True pathogens: • Capable of causing disease in healthy persons with normal immune systems Opportunistic pathogens: • Cause disease when: • The host’s defenses are compromised • When they become established in a part of the body that is not natural to them 14
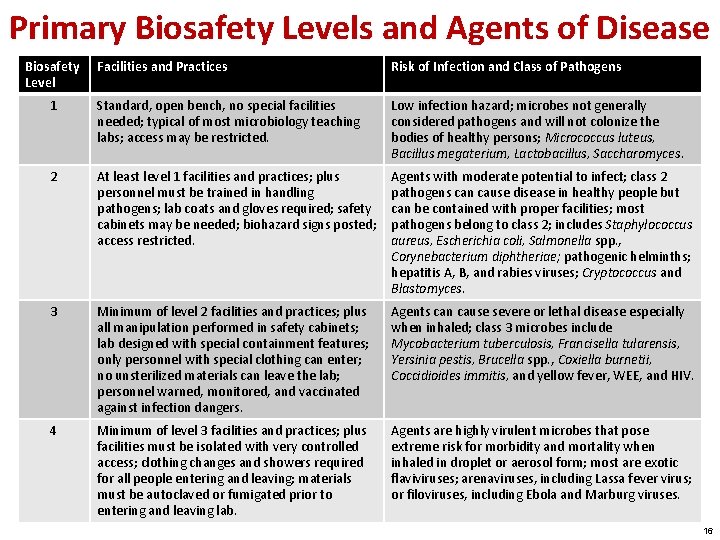
Biosafety Levels • A system of biosafety categories adopted by the Centers for Disease Control and Prevention (CDC) • Based on the general degree of pathogenicity and the relative danger in handling these pathogens 15
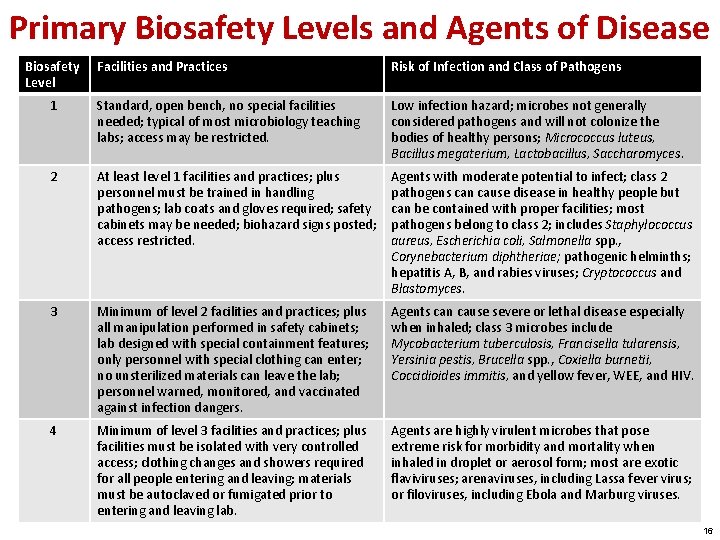
Primary Biosafety Levels and Agents of Disease Biosafety Level Facilities and Practices Risk of Infection and Class of Pathogens 1 Standard, open bench, no special facilities needed; typical of most microbiology teaching labs; access may be restricted. Low infection hazard; microbes not generally considered pathogens and will not colonize the bodies of healthy persons; Micrococcus luteus, Bacillus megaterium, Lactobacillus, Saccharomyces. 2 At least level 1 facilities and practices; plus personnel must be trained in handling pathogens; lab coats and gloves required; safety cabinets may be needed; biohazard signs posted; access restricted. Agents with moderate potential to infect; class 2 pathogens can cause disease in healthy people but can be contained with proper facilities; most pathogens belong to class 2; includes Staphylococcus aureus, Escherichia coli, Salmonella spp. , Corynebacterium diphtheriae; pathogenic helminths; hepatitis A, B, and rabies viruses; Cryptococcus and Blastomyces. 3 Minimum of level 2 facilities and practices; plus all manipulation performed in safety cabinets; lab designed with special containment features; only personnel with special clothing can enter; no unsterilized materials can leave the lab; personnel warned, monitored, and vaccinated against infection dangers. Agents can cause severe or lethal disease especially when inhaled; class 3 microbes include Mycobacterium tuberculosis, Francisella tularensis, Yersinia pestis, Brucella spp. , Coxiella burnetii, Coccidioides immitis, and yellow fever, WEE, and HIV. 4 Minimum of level 3 facilities and practices; plus facilities must be isolated with very controlled access; clothing changes and showers required for all people entering and leaving; materials must be autoclaved or fumigated prior to entering and leaving lab. Agents are highly virulent microbes that pose extreme risk for morbidity and mortality when inhaled in droplet or aerosol form; most are exotic flaviviruses; arenaviruses, including Lassa fever virus; or filoviruses, including Ebola and Marburg viruses. 16
Virulence: • Degree of pathogenicity • Indicated by a microbe’s ability to: • Establish itself in the host • Cause damage Virulence factor: • Any characteristic or structure of the microbe that contributes to toxin production or induction of an injurious host response 17
The Size of the Inoculum Infectious dose (ID): a minimum number of microbes required for an infection to proceed • Determined experimentally for many microbes • Microbes with a smaller infectious dose have greater virulence 18
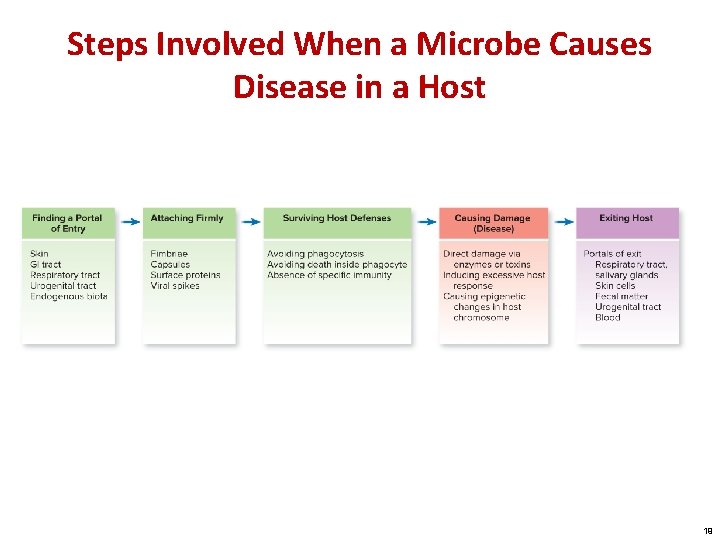
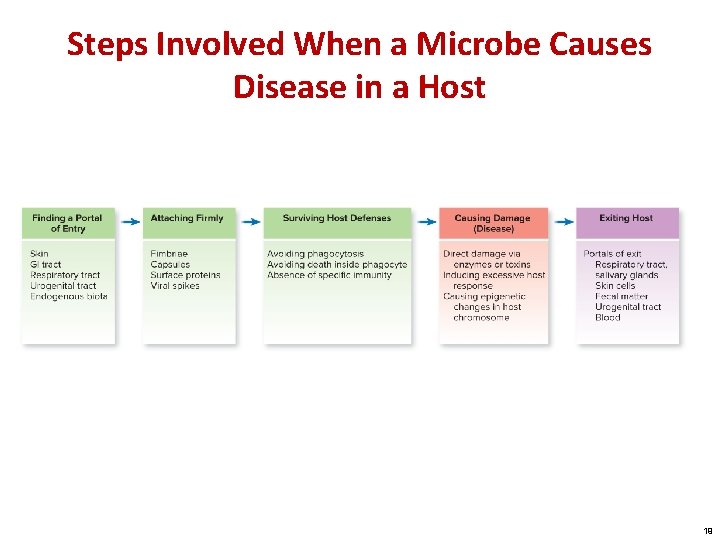
Steps Involved When a Microbe Causes Disease in a Host 19
Becoming Established: Step One—Portals of Entry Portal of entry: • A characteristic route taken by a microbe to initiate infection • Usually through skin or mucous membranes • Exogenous: originating from outside the body • The environment, another person, or animal • Endogenous: already existing on or in the body • Normal biota or a previously silent infection 20
Infectious Agents That Enter the Skin Sites of entry: • Nicks • Abrasions • Punctures, some tiny and inapparent Intact skin is a very tough barrier that few microbes can penetrate Some infectious agents create their own passageways into the skin using digestive enzymes 21
The Gastrointestinal Tract as Portal Entry through food, drink, or other ingested substances • Adapted to survive digestive enzymes and abrupt p. H changes 22
The Respiratory Portal of Entry Gateways to the respiratory tract: • Oral cavity • Nasal cavity Continuous mucous membrane covering the upper respiratory tract, sinuses, and auditory tubes • Microbes often transferred from one site to another Extent to which an agent is carried into the respiratory tree is based on its size • Small cells are inhaled more deeply than larger ones 23
Urogenital Portals of Entry Sexually transmitted infections (STIs): • Pathogens transmitted by sexual means • Account for 4% of infections worldwide • 13 million new cases in the United States each year Entry points through the skin or mucosa of: • • • Penis External genitalia Vagina Cervix Urethra 24
Pathogens That Infect During Pregnancy and Birth The placenta is an exchange organ: • Formed by maternal and fetal tissues • Separates the blood of the developing fetus from that of the mother • Permits diffusion of dissolved nutrients and gases to the fetus • A few microbes cross the placenta and are spread by the umbilical vein into the fetal tissues • Other infections are transmitted perinatally as the child passes through the birth canal 25
Becoming Established: Step Two—Attaching to the Host Adhesion: • A process by which microbes gain a more stable foothold on host tissues • Dependent on binding between specific molecules on both the host and pathogen • A particular pathogen is limited to only those cells and organisms to which it can bind • Once attached, a pathogen can invade body compartments Quorum sensing: • Chemical communication between nearby bacteria critical to establishment of infection 26
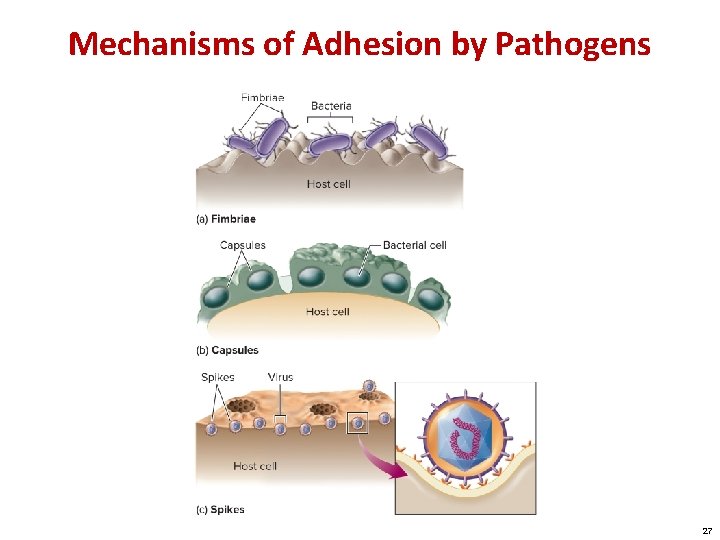
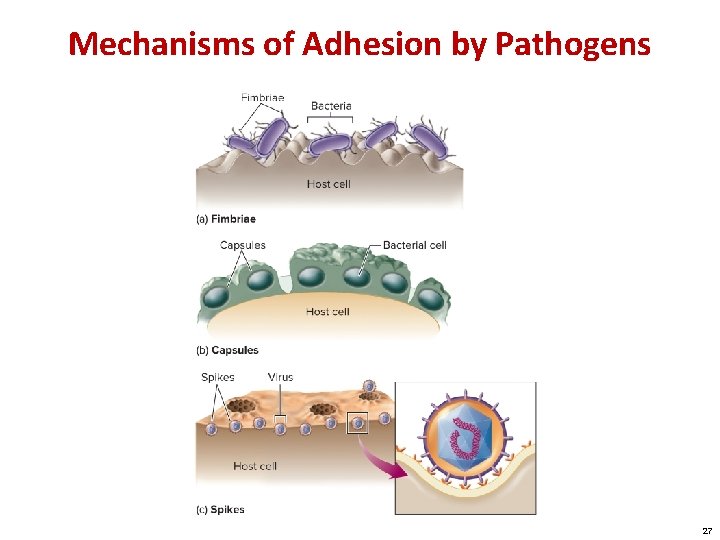
Mechanisms of Adhesion by Pathogens 27
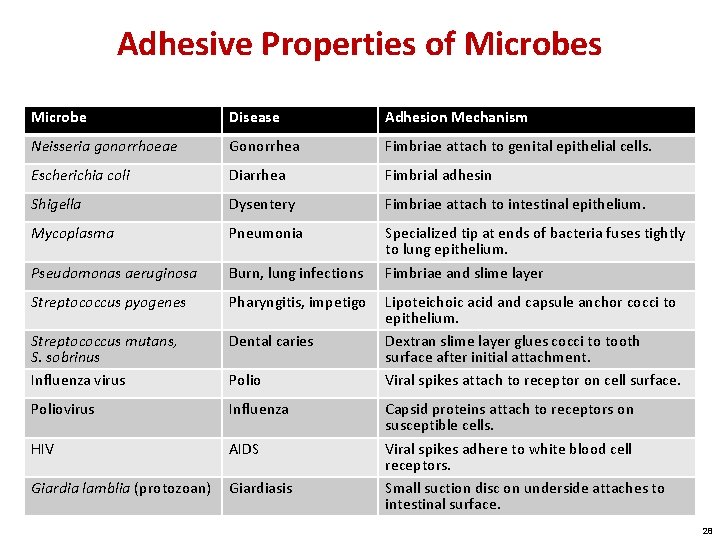
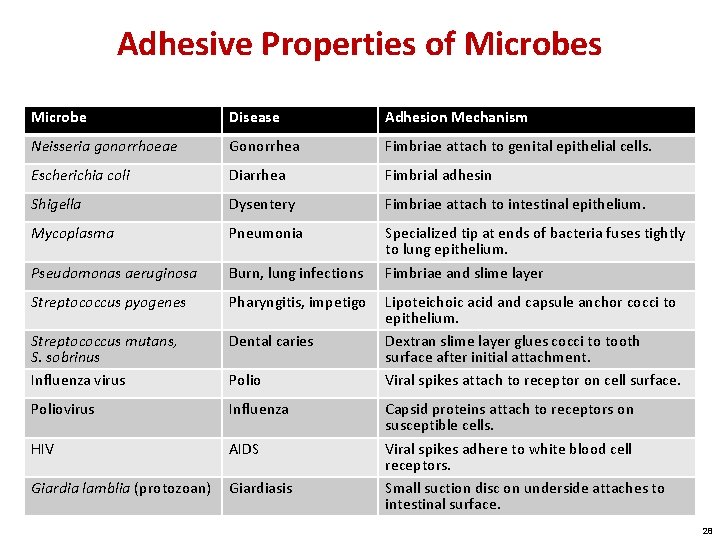
Adhesive Properties of Microbes Microbe Disease Adhesion Mechanism Neisseria gonorrhoeae Gonorrhea Fimbriae attach to genital epithelial cells. Escherichia coli Diarrhea Fimbrial adhesin Shigella Dysentery Fimbriae attach to intestinal epithelium. Mycoplasma Pneumonia Pseudomonas aeruginosa Burn, lung infections Specialized tip at ends of bacteria fuses tightly to lung epithelium. Fimbriae and slime layer Streptococcus pyogenes Pharyngitis, impetigo Streptococcus mutans, S. sobrinus Influenza virus Dental caries Poliovirus Influenza HIV AIDS Giardia lamblia (protozoan) Giardiasis Polio Lipoteichoic acid and capsule anchor cocci to epithelium. Dextran slime layer glues cocci to tooth surface after initial attachment. Viral spikes attach to receptor on cell surface. Capsid proteins attach to receptors on susceptible cells. Viral spikes adhere to white blood cell receptors. Small suction disc on underside attaches to intestinal surface. 28
Becoming Established: Step 3—Surviving Host Defenses Phagocytes: • White blood cells that engulf and destroy pathogens by means of enzymes and antimicrobial chemicals Antiphagocytic factors: • Virulence factor used by pathogens to avoid phagocytes • Circumvent some part of the phagocytic process 29
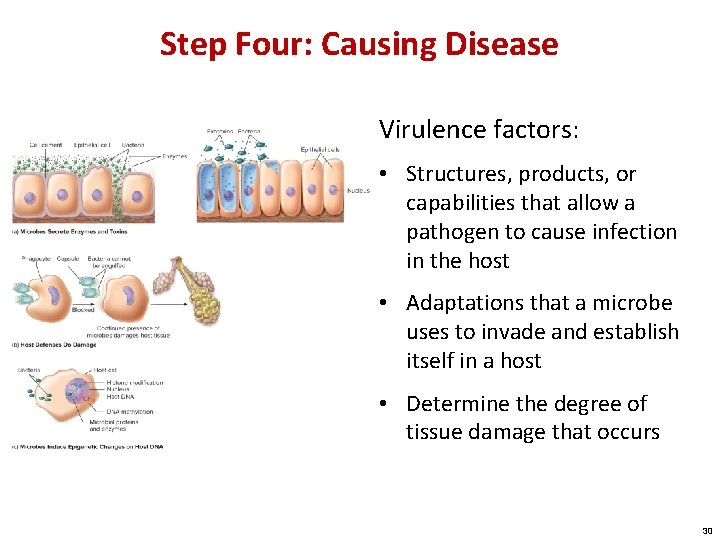
Step Four: Causing Disease Virulence factors: • Structures, products, or capabilities that allow a pathogen to cause infection in the host • Adaptations that a microbe uses to invade and establish itself in a host • Determine the degree of tissue damage that occurs 30
Direct Damage via Enzymes Exoenzymes: • Secreted by pathogenic bacteria, fungi, protozoa, and worms • Break down and inflict damage on tissues • Dissolve host’s defense barriers and promote the spread of microbes into deeper tissues Examples: • Mucinase • Keratinase • Hyaluronidase 31
Toxins: A Potent Source of Cellular Damage Toxin: • A specific chemical product of microbes, plants, and some animals that is poisonous to other organisms Exotoxin: • Secreted by a living bacterial cell to the infected tissues • Many types Endotoxin: • Not actively secreted • Shed from the outer membrane • Only found in gram-negative bacteria 32
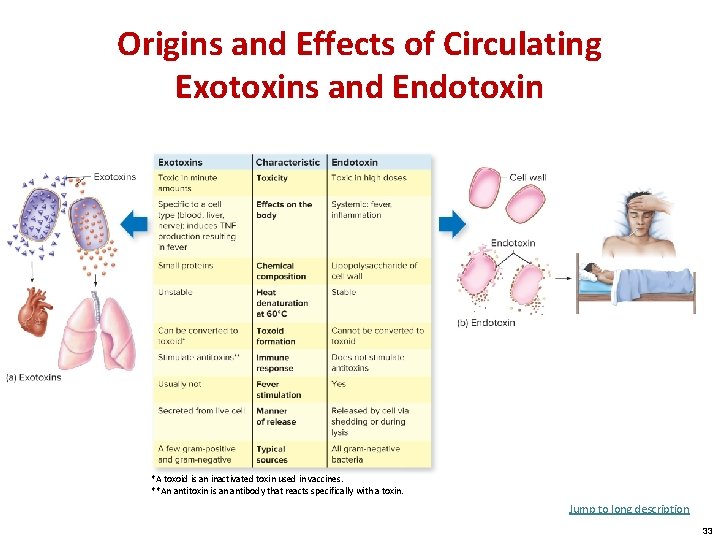
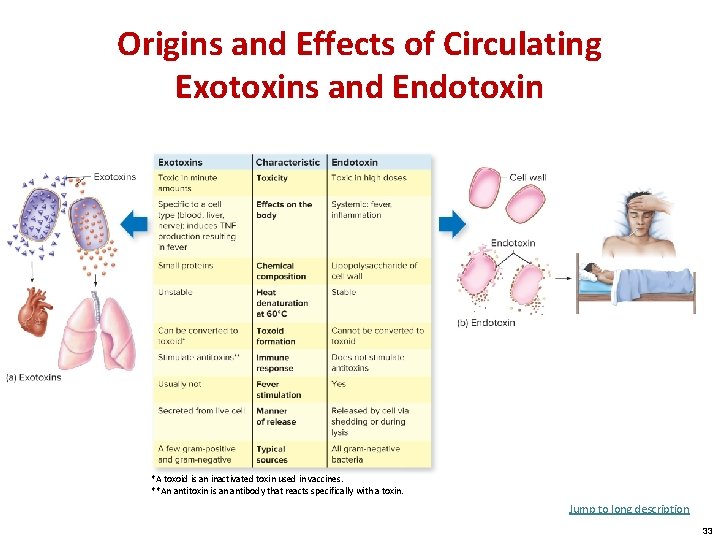
Origins and Effects of Circulating Exotoxins and Endotoxin *A toxoid is an inactivated toxin used in vaccines. **An antitoxin is an antibody that reacts specifically with a toxin. Jump to long description 33
Inducing an Injurious Host Response Many cases of microbial diseases are the result of indirect damage or the host’s excessive or inappropriate response to a microorganism • Pathogenicity is a trait not solely determined by microorganisms • Pathogenicity is a consequence of an interplay between microbe and host 34
Localized Infection Microbe enters the body and remains confined to a specific tissue: • Boils • Fungal skin infections • Warts 35
Systemic Infection When an infection spreads to several sites and tissue fluids, usually in the bloodstream • Viral: measles, rubella, chicken pox, AIDS • Bacterial: brucellosis, anthrax, typhoid fever, syphilis • Fungal: histoplasmosis, cryptococcosis Infectious agents can travel by means of nerves or cerebrospinal fluid 36
Focal Infection Exists when the infectious agent breaks loose from a local infection and is carried to other tissues Examples: • Tuberculosis • Streptococcal pharyngitis: scarlet fever • Toxemia: infection remains localized, toxins are carried through the blood to the target tissue 37
Mixed Infection • Several agents establish themselves simultaneously at the infection site • Polymicrobial diseases: gas gangrene, wound infections, dental caries, human bite infections 38
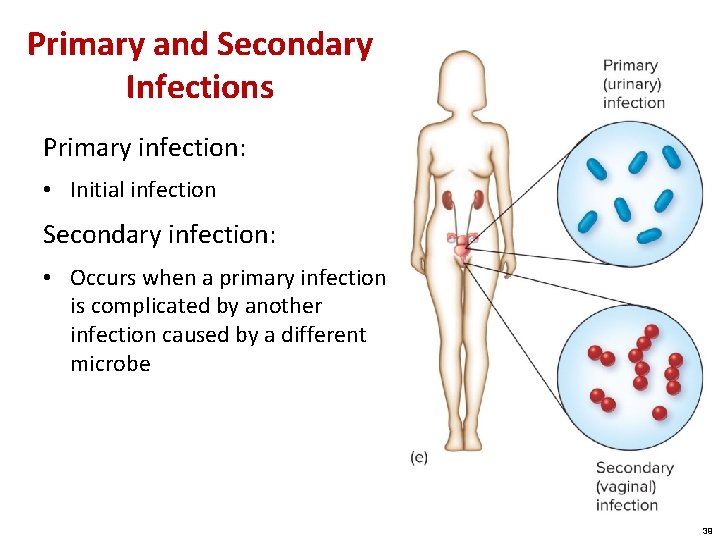
Primary and Secondary Infections Primary infection: • Initial infection Secondary infection: • Occurs when a primary infection is complicated by another infection caused by a different microbe 39
Acute versus Chronic Infections Acute infections: • Come on rapidly • Have short-lived effects Chronic infections: • Progress and persist over a long period of time 40
Signs and Symptoms: Warning Signals of Disease Sign: • Any objective evidence of disease as noted by an observer • More precise than symptoms Symptom: • Subjective evidence of disease as sensed by the patient Syndrome: • A disease identified or defined by a certain complex of signs and symptoms 41
Signs of Infection in the Blood Leukocytosis: Bacteremia: • Increase in the level of white blood cells • Small numbers of bacteria are present in the blood but not multiplying Leukopenia: • Decrease in the level of white blood cells Septicemia: Viremia: • Presence of viruses in the blood, whether or not they are actively multiplying • General state in which microbes are multiplying in the blood and are present in large numbers 42
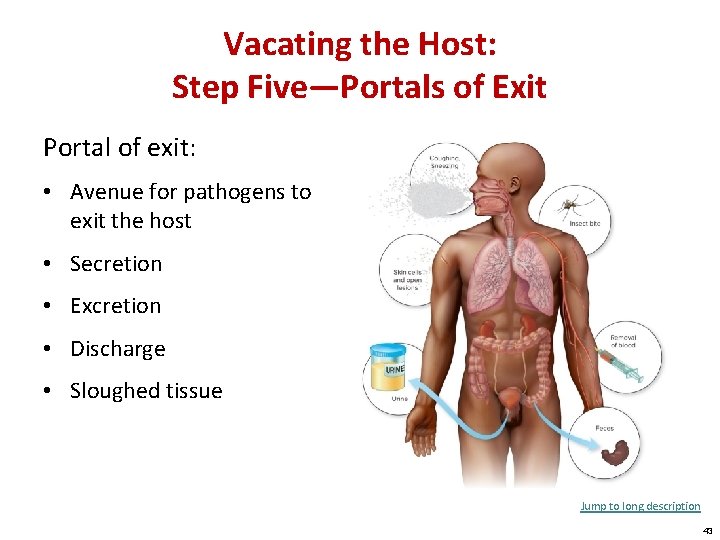
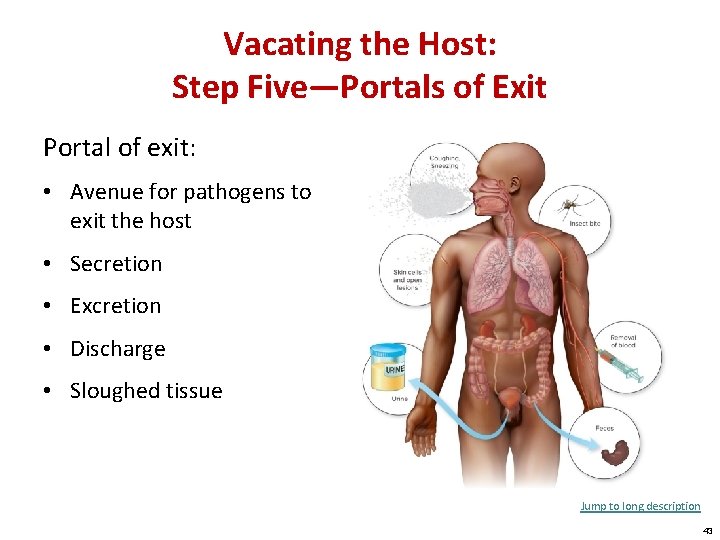
Vacating the Host: Step Five—Portals of Exit Portal of exit: • Avenue for pathogens to exit the host • Secretion • Excretion • Discharge • Sloughed tissue Jump to long description 43
Respiratory and Salivary Portals Escape media for pathogens that infect the upper and lower respiratory tract: • Mucus • Sputum • Nasal drainage • Other moist secretions 44
Skin Scales The outer layer of skin and scalp is constantly being shed into the environment • Household dust is composed of skin cells • A single person can shed several billion skin cells a day 45
Fecal Exit Some intestinal pathogens cause irritation in the intestinal mucosa that increases the motility of the bowel • Resulting diarrhea provides a rapid exit for the pathogen • Helminth worms release eggs and cysts through the feces • Feces containing pathogens are a public health problem when allowed to contaminate drinking water or when used to fertilize crops 46
Urogenital Tract Agents involved in STIs leave the host in vaginal discharge or semen Source of neonatal infections that infect the infant as it passes through the birth canal: • Herpes simplex • Chlamydia • Candida albicans Pathogens that affect the kidney are discharged in the urine 47
Removal of Blood or Bleeding Blood has a portal of exit when it is removed or released through vascular puncture Blood-feeding animals are common transmitters of pathogens: • Ticks • Fleas • Mosquitoes 48
The Persistence of Microbes and Pathologic Conditions Latency: • A dormant state of an infectious agent • During this state, a microbe can periodically become active and produce a recurrent disease Sequelae: • Long-term or permanent damage to organs and tissues 49
Four Phases of Infection and Disease Incubation period: • The time from initial contact with the infectious agent to the appearance of first symptoms Prodromal period: • When the earliest notable symptoms of infection appear Period of invasion: • Infectious agent multiplies at high levels, exhibits greatest virulence, and becomes well established in its target tissue Convalescent stage: • Patient responds to infection and symptoms decline 50
Acquisition and Transmission of Infectious Agents Communicable disease: • Occurs when an infected host can transmit the infectious agent to another host and establish infection in that host Contagious: • The agent is highly communicable, especially through direct contact Noncommunicable: • Does not arise through transmission of the infectious agent from host to host 51
Epidemiology: Study of Disease in Populations Epidemiology: • Effects of diseases on the community • Involves the study of the frequency and distribution of disease and other health-related factors in defined populations Reportable diseases: • Notifiable diseases • By law, some diseases must be reported to authorities • Other diseases are reported on a voluntary basis 52
Epidemiological Statistics Prevalence of disease: • Total number of existing cases with respect to the entire population Incidence of disease: • Measures the number of new cases over a certain time period • Also known as case or morbidity rate Mortality rate: • Measures the number of deaths in a population due to a certain disease 53
 Geometric symbol
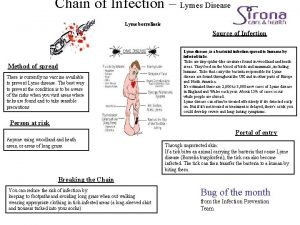
Geometric symbol Chain of infection for lyme disease
Chain of infection for lyme disease Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Puncture resistant container
Puncture resistant container Infection or disease that originates within the body
Infection or disease that originates within the body Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Canada colonization
Canada colonization Early voyages of exploration
Early voyages of exploration 3 g's spanish colonization
3 g's spanish colonization Space colonization
Space colonization Glory in spanish colonization
Glory in spanish colonization Between 1859 and 1893 vietnam
Between 1859 and 1893 vietnam French colonization apush
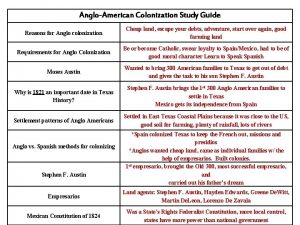
French colonization apush Reason for colonization
Reason for colonization Colonization acrostic poem
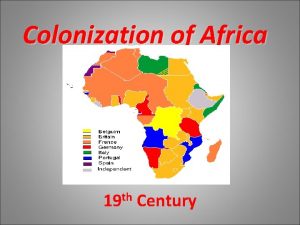
Colonization acrostic poem Colonization of africa
Colonization of africa Jamestown reason for colonization
Jamestown reason for colonization Wilson whap
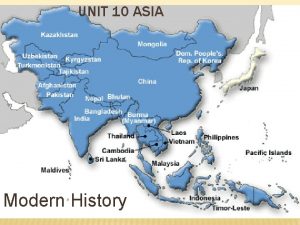
Wilson whap Asia colonization map
Asia colonization map Colonization of south america
Colonization of south america Unit 1 exploration and colonization
Unit 1 exploration and colonization Dana alotaibi death
Dana alotaibi death Colonization
Colonization Reasons for colonization in america
Reasons for colonization in america What role did erasmo seguin and jose antonio navarro
What role did erasmo seguin and jose antonio navarro Aliping namamahay
Aliping namamahay Colonial class system
Colonial class system Imperial colonization law
Imperial colonization law Bacteria defenition
Bacteria defenition Early european exploration and colonization resulted in -
Early european exploration and colonization resulted in - Spanish colonization of the americas
Spanish colonization of the americas Colonization
Colonization Unit 2 exploration and georgia colonization
Unit 2 exploration and georgia colonization Communicable disease and non communicable disease
Communicable disease and non communicable disease Chapter 10 infection control
Chapter 10 infection control Subclinical infection
Subclinical infection Inamnimate
Inamnimate Unit 13 infection control
Unit 13 infection control Postpartum infection
Postpartum infection Infection control audits
Infection control audits Renal lobe and lobule
Renal lobe and lobule Root locus drawer
Root locus drawer Bacterial infection
Bacterial infection Chapter 15:8 using sterile techniques
Chapter 15:8 using sterile techniques Chapter 15 preventing infection
Chapter 15 preventing infection Infection nosocomiale
Infection nosocomiale Non odontogenic infection
Non odontogenic infection Types of infection
Types of infection Learning objectives for infection control
Learning objectives for infection control Infection control committee
Infection control committee Torch infection
Torch infection Différence entre ias et infection nosocomiale
Différence entre ias et infection nosocomiale Kidney infection when to go to hospital
Kidney infection when to go to hospital Surgical site infection bundle checklist
Surgical site infection bundle checklist