TB Infection Control Engineering Environmental Controls Kevin P
TB Infection Control: Engineering (Environmental) Controls Kevin P. Fennelly, MD, MPH Division of Pulmonary & Critical Care Medicine Center for Emerging Pathogens UMDNJ-New Jersey Medical School
Objectives • To review fundamental principles and practices of TB infection control related to engineering controls • To discuss advantages and limitations to different engineering control measures. • To discuss how engineering controls are used in the total TB Infection Control Plan. • To discuss issues and questions specific to your experiences in Chiapas.
Key Points • Engineering controls (EC) are the 2 nd priority in control measures AFTER administrative controls, • But they are complementary • Dilution ventilation is the most important EC – Protects HCWs, other patients, visitors – Has limits defined by technology, expense, comfort • Negative pressure or directional airfllow keeps contaminated air away from HCWs • UVGI and filtration devices are adjuncts or backups for high-risk areas – Require maintenance – Need to consider cost-effectiveness
Fundamentals of Infection Control • Administrative controls: reduce risk of exposure • Environmental controls: prevent spread and reduce concentration of droplet nuclei • Respiratory protection controls: further reduce risk of exposure to wearer only

Hierarchy of Infection Control Administrative Controls Environmental Controls Respiratory Protection
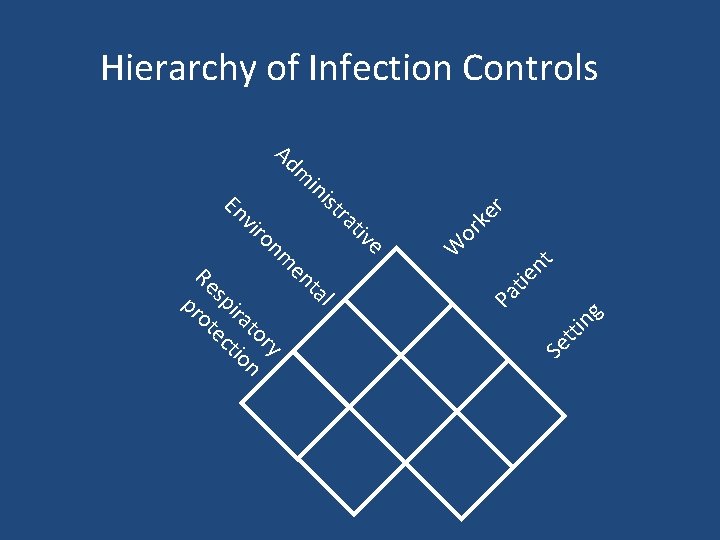
Se tti ng Pa tie nt e tiv ra l ist ta in m en m Ad ry on to n vir ira tio En sp ec Re rot p W or ke r Hierarchy of Infection Controls
TB-Infection Controls: Simplified • Administrative: WHO? – Who is a TB suspect? – Who is at risk from exposure? – Who has infectious TB? – Who has drug resistant TB? • Environmental: WHERE? – Where is optimal place to minimize risk? • Personal Respiratory Protection: Special high risk settings
Environmental Controls • Control source of infection • Dilute and remove contaminated air • Control airflow – Keep infectious air moving outside – Keep HCWs ‘upwind’ , infectious patients ‘downwind’
Airborne Infection Isolation Room Policies • Environmental factors and entry of visitors and HCWs should be controlled • Air changes per hour (ACH) (volume /time) – >6 ACH (existing) – >12 ACH (new) • Minimum of 2 ACH of outdoor air • HCWs should wear at least N 95 respirators
What is ventilation? • Movement of air • “Pushing” and/or “pulling” of particles and vapors • Preferably in a controlled manner 10
Ventilation control • Types of ventilation – Natural – Local – General 11
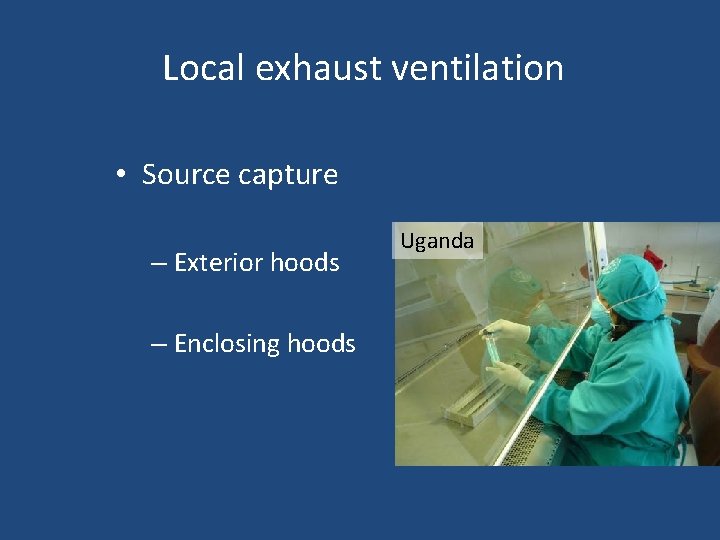
Local exhaust ventilation • Source capture – Exterior hoods – Enclosing hoods Uganda
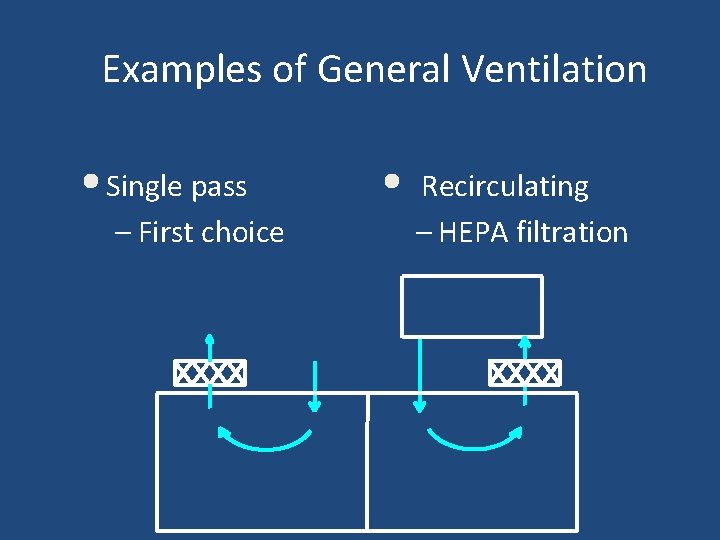
Examples of General Ventilation • Single pass – First choice • Recirculating – HEPA filtration
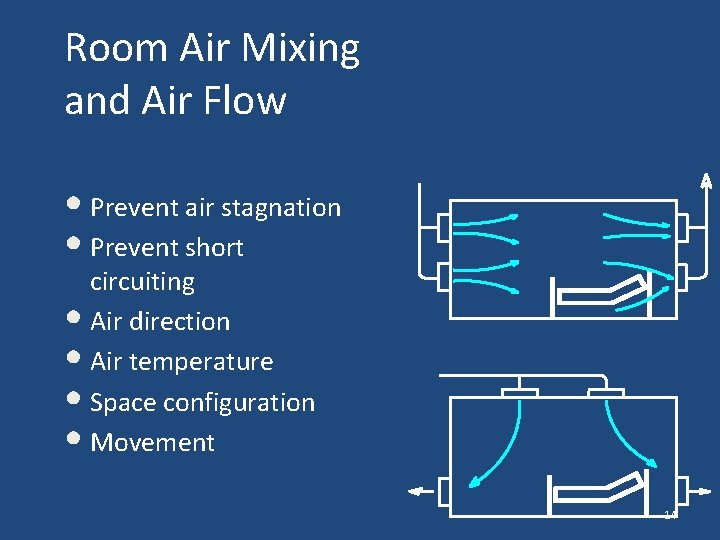
Room Air Mixing and Air Flow • Prevent air stagnation • Prevent short circuiting • Air direction • Air temperature • Space configuration • Movement 14
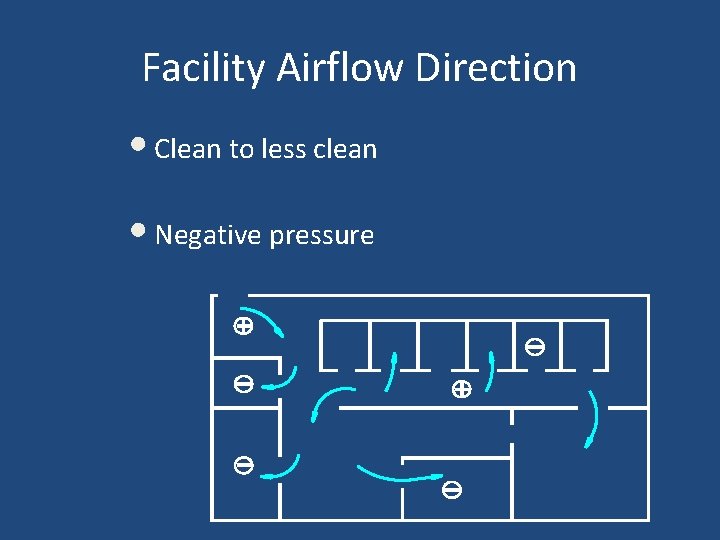
Facility Airflow Direction • Clean to less clean • Negative pressure
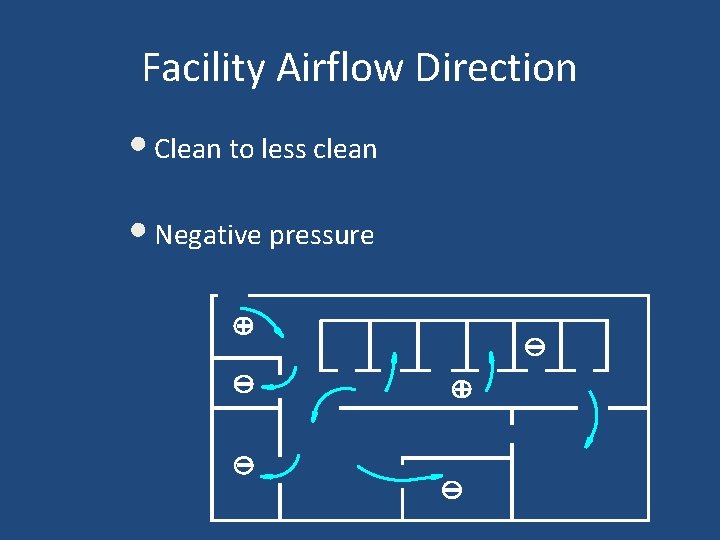
Facility Airflow Direction • Clean to less clean • Negative pressure
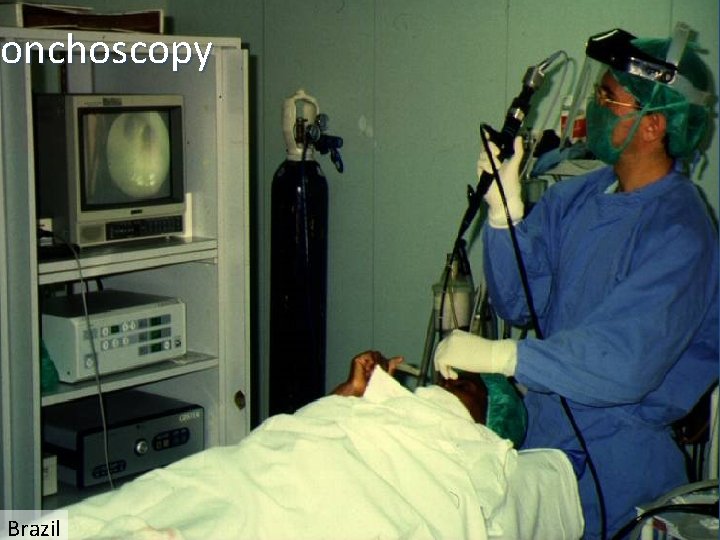
ronchoscopy Brazil 17

18
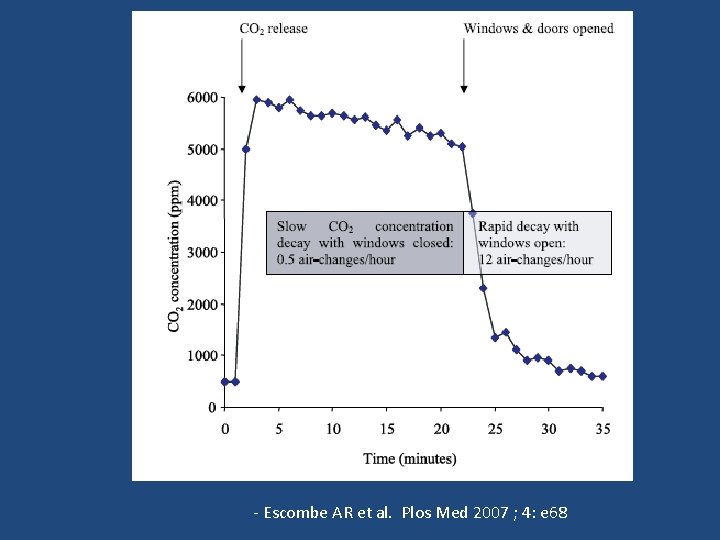
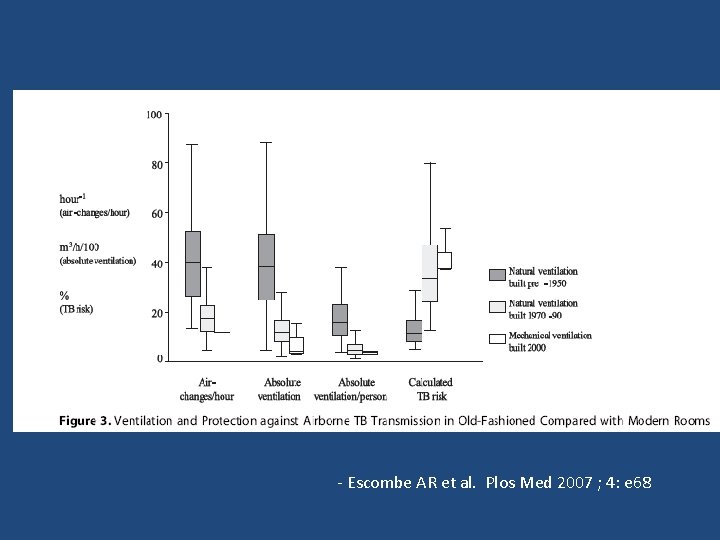
- Escombe AR et al. Plos Med 2007 ; 4: e 68
- Escombe AR et al. Plos Med 2007 ; 4: e 68

Natural vs Mechanical Ventilation • Good natural ventilation is better than bad mechanical ventilation. • Major limitation of natural ventilation is that it depends upon outdoor weather conditions. • Can control odor and improve comfort of occupants , but not if very cold or very hot. • Usually we do not have a choice and must work with where we are!
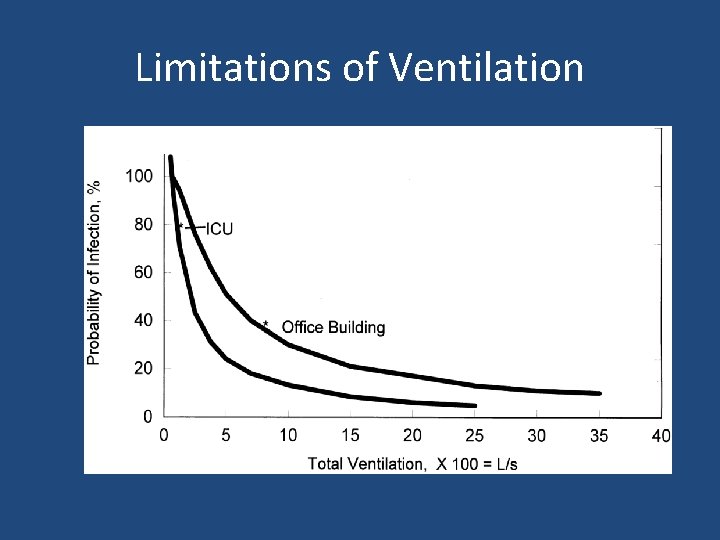
Limitations of Ventilation
HEPA filtration Must be used – When discharging air from local exhaust ventilation booths or enclosures directly into the surrounding room, and – When discharging air from an AII room into the general ventilation system 24
Room Air Cleaners 25

TB Outpatient unit – Helio Fraga Institute, Mo. H, Rio de Janeiro 26
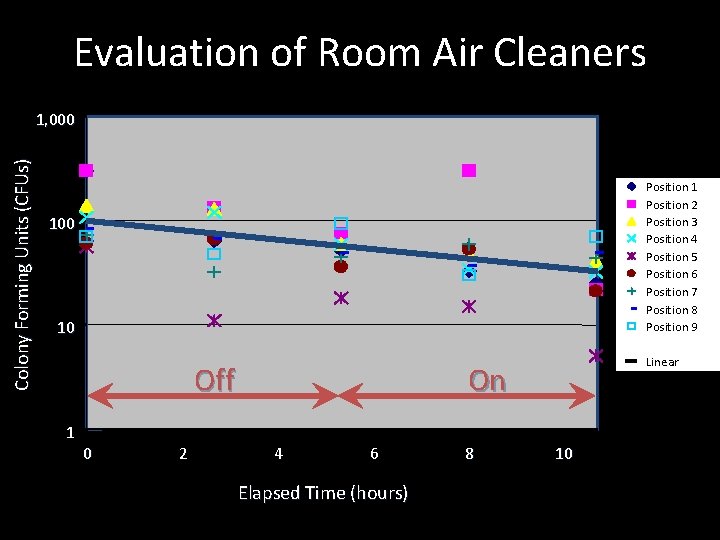
Evaluation of Room Air Cleaners Colony Forming Units (CFUs) 1, 000 Position 1 Position 2 Position 3 Position 4 Position 5 Position 6 Position 7 Position 8 Position 9 100 10 Off 1 0 2 Linear On 4 6 8 10 Elapsed Time (hours) 27
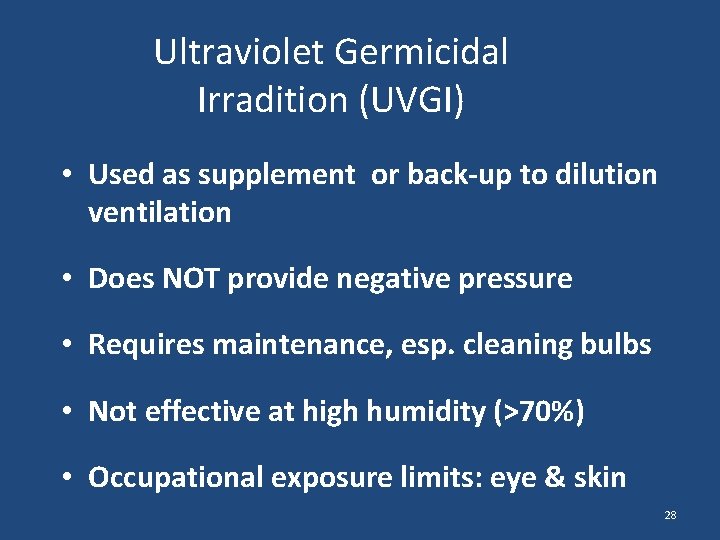
Ultraviolet Germicidal Irradition (UVGI) • Used as supplement or back-up to dilution ventilation • Does NOT provide negative pressure • Requires maintenance, esp. cleaning bulbs • Not effective at high humidity (>70%) • Occupational exposure limits: eye & skin 28
29
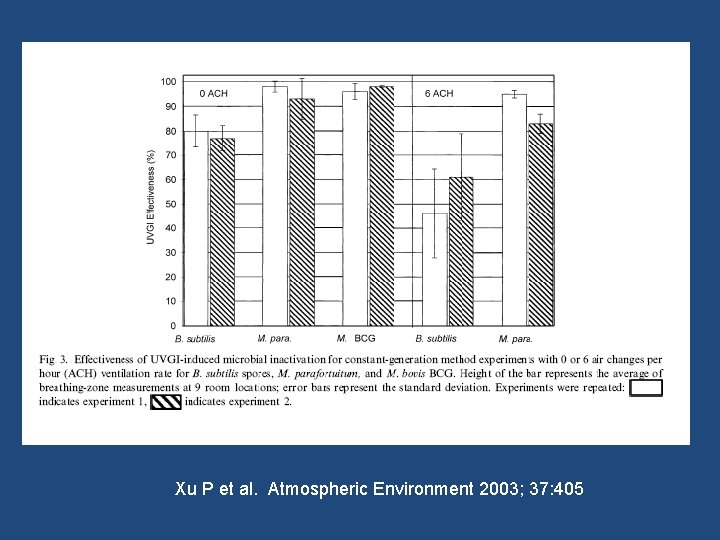
Xu P et al. Atmospheric Environment 2003; 37: 405

31
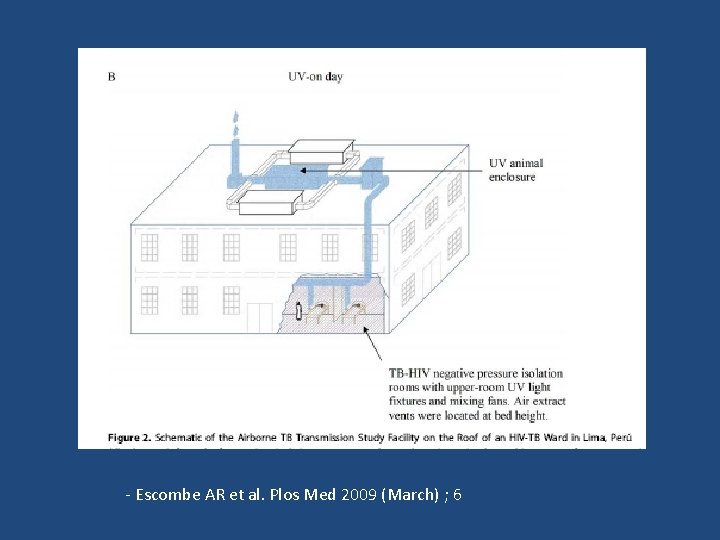
- Escombe AR et al. Plos Med 2009 (March) ; 6
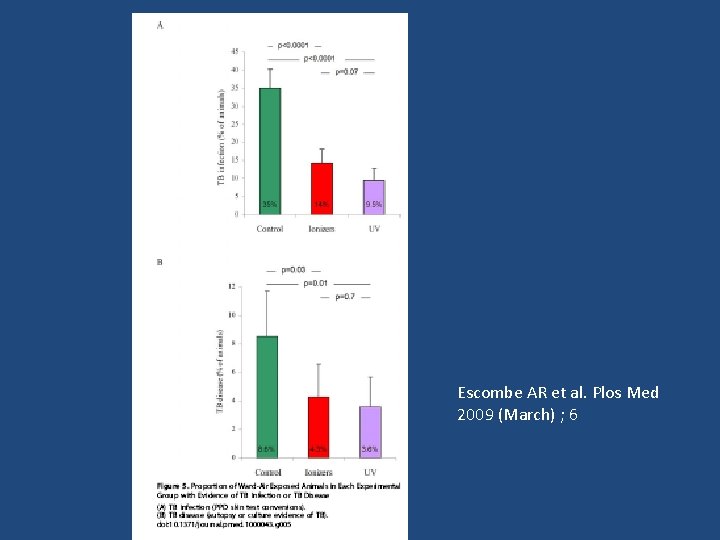
Escombe AR et al. Plos Med 2009 (March) ; 6
Environmental Controls: Which one and When? • Dilution ventilation, UVGI, and HEPA filter units are all effective under IDEAL laboratory conditions • Best data in field support dilution ventilation • Advantage of ventilation is usually ‘always on’, minimizing human errors. • Disadvantages of UVGI and HEPAs – Maintenance (increased human errors) – Large variability of effectiveness – May cause false sense of reassurance
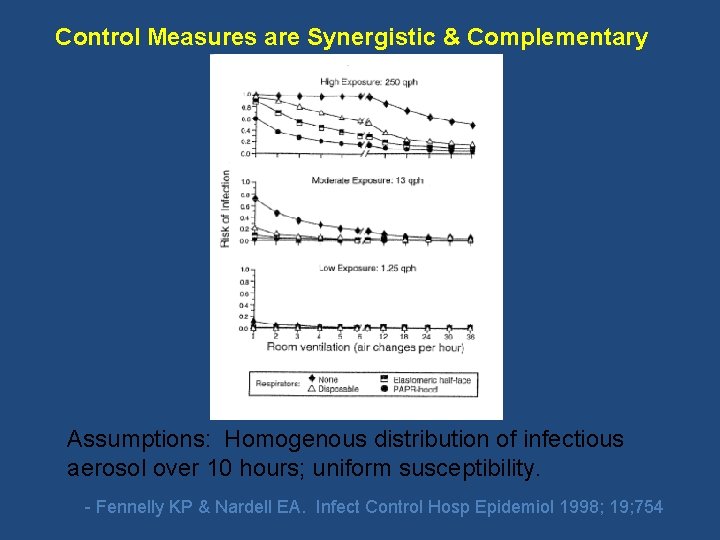
Control Measures are Synergistic & Complementary Assumptions: Homogenous distribution of infectious aerosol over 10 hours; uniform susceptibility. - Fennelly KP & Nardell EA. Infect Control Hosp Epidemiol 1998; 19; 754
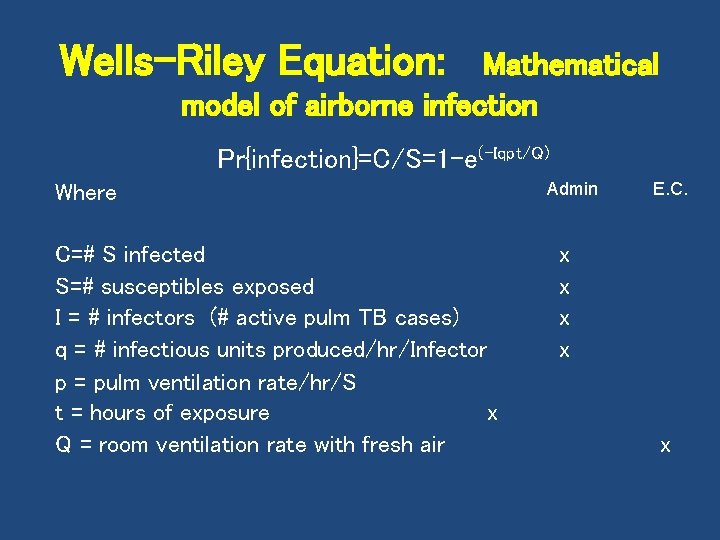
Wells-Riley Equation: Mathematical model of airborne infection Pr{infection}=C/S=1 -e(-Iqpt/Q) Where C=# S infected S=# susceptibles exposed I = # infectors (# active pulm TB cases) q = # infectious units produced/hr/Infector p = pulm ventilation rate/hr/S t = hours of exposure x Q = room ventilation rate with fresh air Admin E. C. x x x
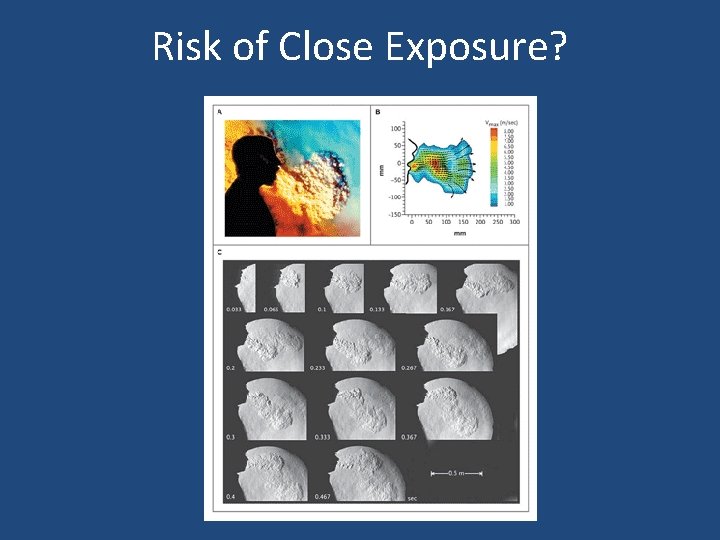
Risk of Close Exposure?
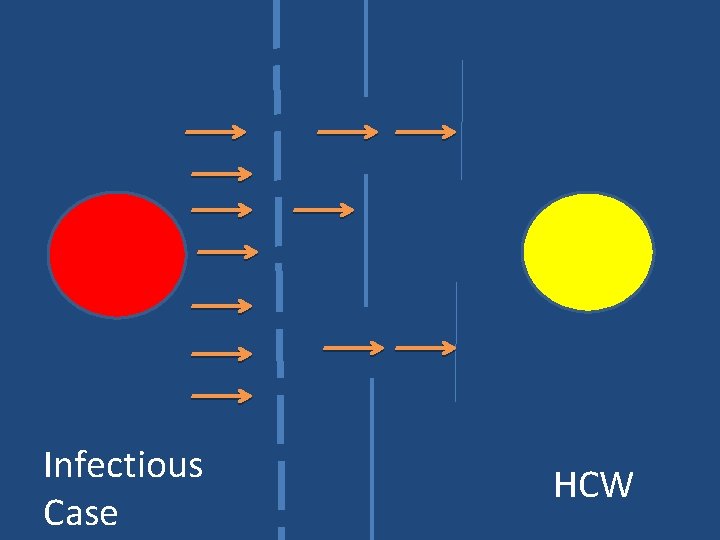
Infectious Case HCW
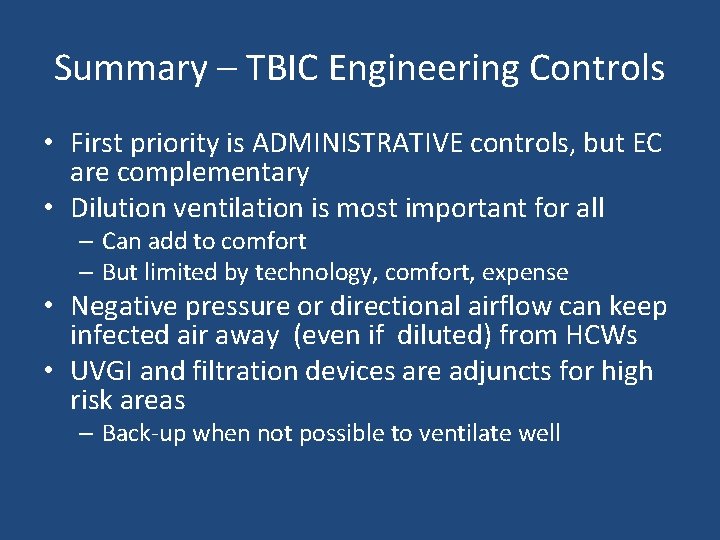
Summary – TBIC Engineering Controls • First priority is ADMINISTRATIVE controls, but EC are complementary • Dilution ventilation is most important for all – Can add to comfort – But limited by technology, comfort, expense • Negative pressure or directional airflow can keep infected air away (even if diluted) from HCWs • UVGI and filtration devices are adjuncts for high risk areas – Back-up when not possible to ventilate well
- Slides: 39