NOSOCOMIAL INFECTION Dr Sathya Anandam Hospital infection is
- Slides: 22
NOSOCOMIAL INFECTION Dr Sathya Anandam
Hospital infection is generally defined as any infection acquired while in the hospital, occurring 48 hrs. or more after admission and up to 48 hrs. after discharge.
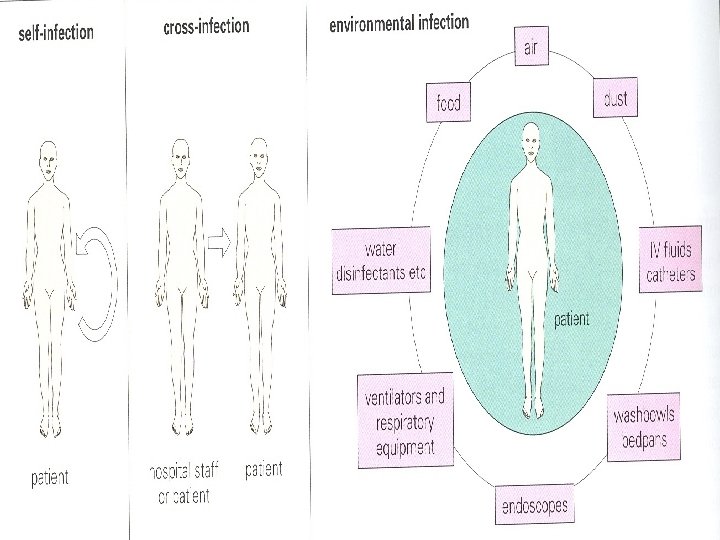
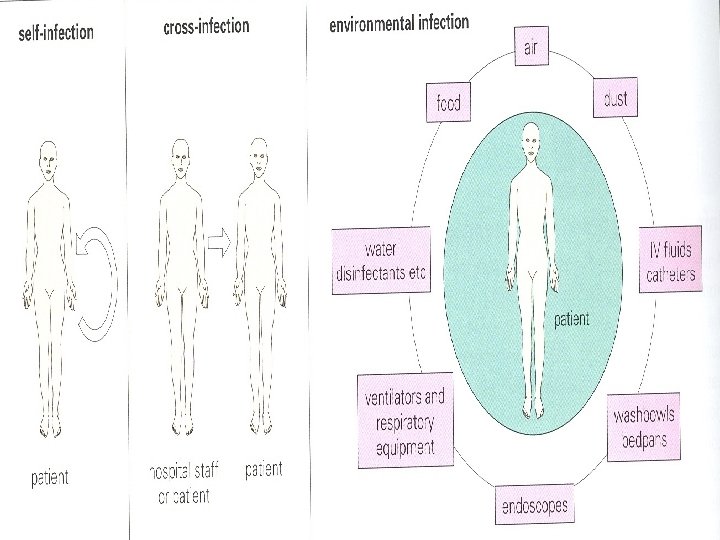
Sources of Hospital Infection: o Exogenous Source - from another patient-cross infection or from the hospital environment. o Endogenous Source - another site within the patient (self or autoinfection. )
Common Hospital Infections: o Urinary Tract Infection -28% o Surgical Wound Infection -17% o Respiratory Tract Infection -17% o Bacteremia –due to IV devices 16%, others 20%
Important causes of hospital infections: • In pre-antibiotic era the majority of infections were caused by Gram positive organisms particularly S. pyogenes and S. aureus. • But after the advent of penicillin, Gram negative organisms such as E. coli and P. aeruginosa emerged as an important pathogen.
• More recently broad spectrum antibiotics and invasive techniques resulted in VRE, MRSA, multidrug resistant Gram negative organisms including ESBL producers are the common causes of hospital infection.
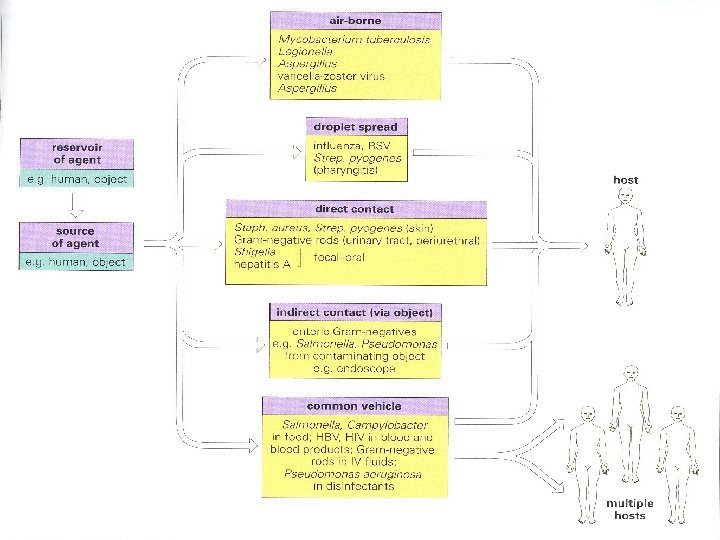
Source and Route of Spread of Hospital Infection: o Health care personnel o Patients o Inanimate Environment
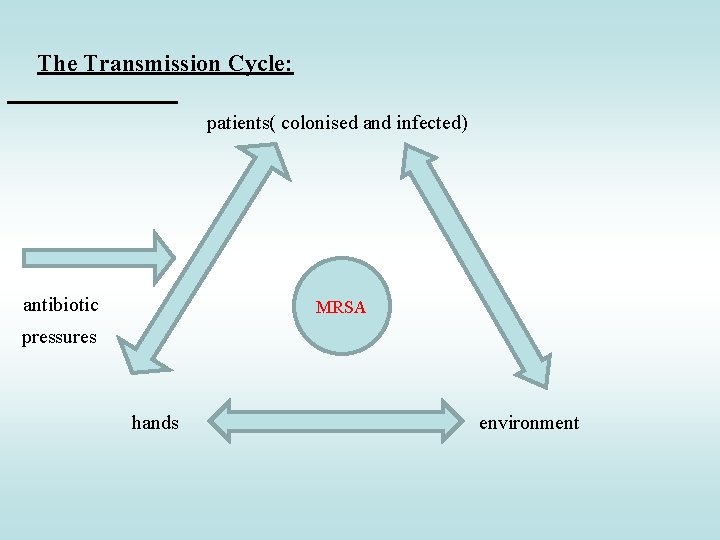
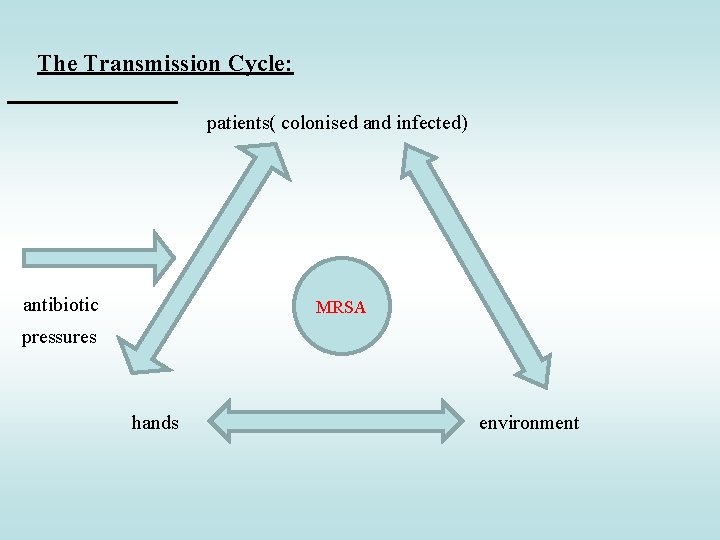
The Transmission Cycle: patients( colonised and infected) antibiotic MRSA pressures hands environment
Staphylococcal carriers: • S. aureus colonizes many sites in the human body of which the anterior nares are the most common carriage site. • About 30% of the population carry S. aureus, out of which 20% are colonized and 10% are transient carriers. • Some people have an inherent tendency to always carry S. aureus and they recolonise very quickly after eradication attempts.
The predisposing factors: • Age - patients at extreme ages. • Underlying diseases – liver disorder, diabetes, renal failure etc. • Specific medicaments – cytotoxic drugs, steroids, post transplant immunosuppression. • Invasive procedures – surgery, intravenous and urinary catheters, peritoneal dialysis.
Consequences of hospital infections: • • • Serious illness or death Prolonged hospital stay Drug resistance Economic burden Infected patient becoming source for others in the hospital and community.
Prevention of Hospital Infection: Three main strategies: o Excluding the sources of infection from the hospital environment. o Breaking the chain of infection by interrupting the transmission of infection from source to the susceptible host. o Enhancing the host’s ability to resist infection.
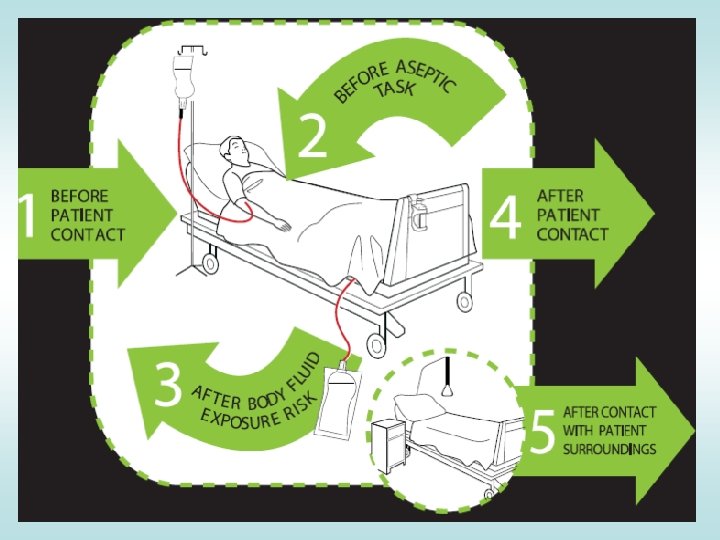
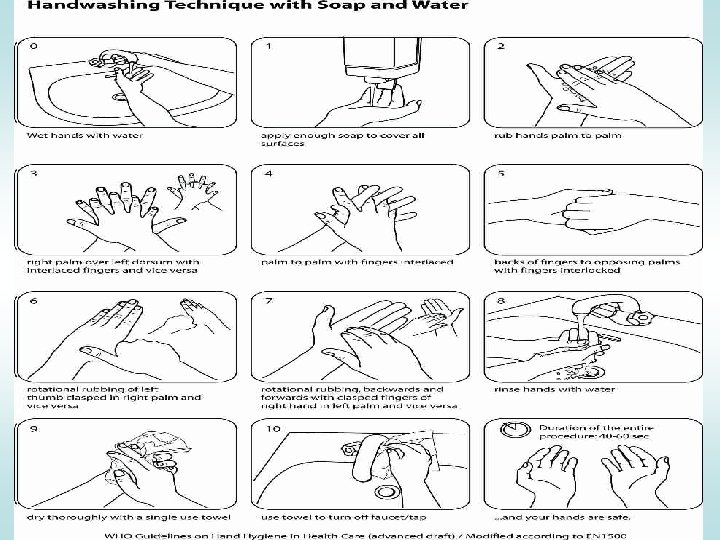
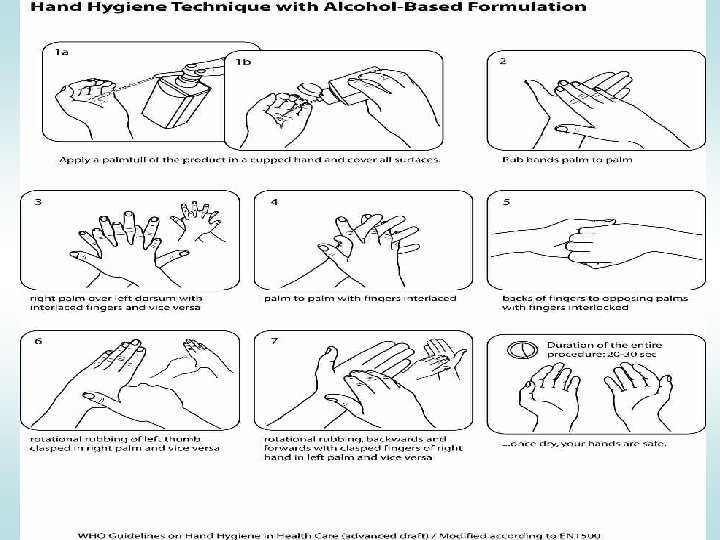
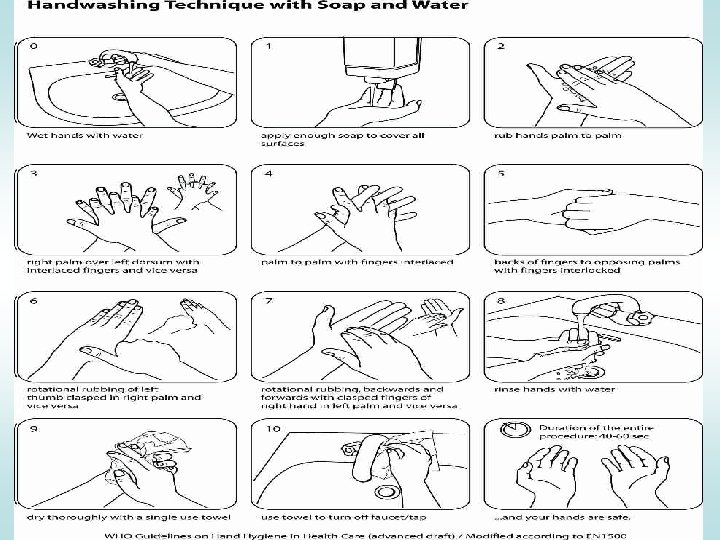
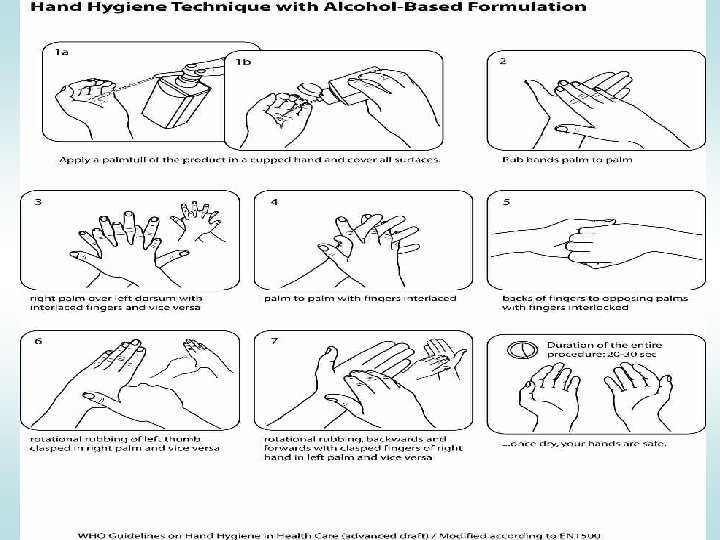
Standard Precautions : • • • Hand Washing Gloves Mask, Eye Protection, Face Shield Gown Environmental Control Appropriate sharp disposal Transmission based precautions: • • • Air borne precautions Droplet precautions Contact precautions
• Cleaning has two main functions. ü non-microbiological : to improve the appearance. ü microbiological : to reduce the number of microbes, : to reduce the risk of infection for people in contact with that object. • usually a great emphasis is given to the cleaning of floors and toilets. • the role of near-patient hand-touch sites ( bed rails, bedside lockers, infusion pumps door handles, nurse call button etc. ) in transmission of infection has not been given importance which should be considered.
Hospital Infection Control Program: • Detect and monitor hospital acquired infection and to prevent & control their spread. • Establishment and monitoring of policies and procedures designed to prevent infection (eg. catheter care policy, antibiotic policy etc. ) • The investigation of outbreaks.
Infection Control Committee: • Infection control officer-Microbiologist or physician • The infection control practitioner (often a nurse with special training) • The hospital epidemiologist (usually an infectious disease physician) • The members of the committee would also include representatives of all the major specialities, house keeping, CSSD, and hospital administration.
The role of infection committee: • • • Surveillance Policy development Outbreak investigation Education and training of the health care personnel Hospital employee health.
Vijay Pratap Raghuvanshi M. Phil & MHA
Vijay Pratap Raghuvanshi M. Phil & MHA
 Beth has a nosocomial infection. how did she get it?
Beth has a nosocomial infection. how did she get it? Innate immunity first line of defense
Innate immunity first line of defense Dr anuradha sathya
Dr anuradha sathya Sathya sai international organisation uk
Sathya sai international organisation uk Brahmarpanam prayer
Brahmarpanam prayer Mantra pushpam meaning
Mantra pushpam meaning Ashta daridra
Ashta daridra Om sri sathya sai baba
Om sri sathya sai baba Sathya robot
Sathya robot Sri sathya sai organisation uk
Sri sathya sai organisation uk Finding the principal amount
Finding the principal amount Kidney infection when to go to hospital
Kidney infection when to go to hospital 100 bedded hospital staff requirements
100 bedded hospital staff requirements Infection nosocomiale
Infection nosocomiale Mycotic infection rabbit
Mycotic infection rabbit Defination of infection
Defination of infection Wound infection continuum
Wound infection continuum Why are viruses considered nonliving
Why are viruses considered nonliving Infection nosocomiale
Infection nosocomiale Koilocyt
Koilocyt Primo infection
Primo infection Chain of infection
Chain of infection Spirochete gram positive or negative
Spirochete gram positive or negative