PREVENTION OF NOSOCOMIAL PNEUMONIA Nosocomial Pneumonia Second most




- Slides: 37

PREVENTION OF NOSOCOMIAL PNEUMONIA
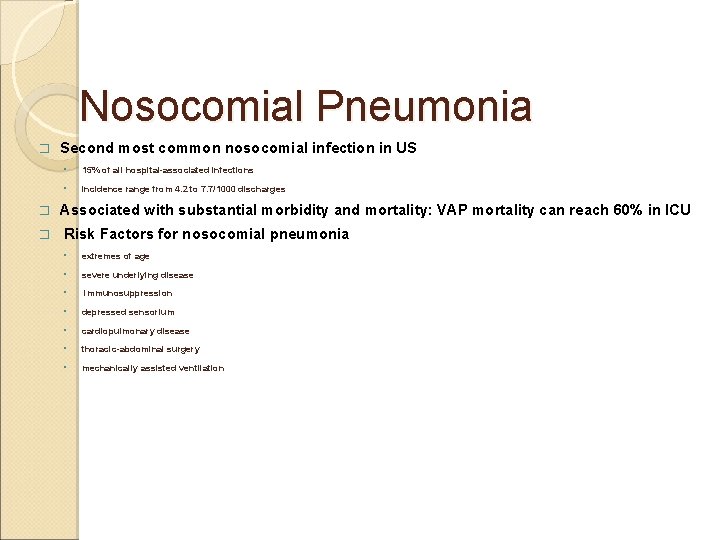
Nosocomial Pneumonia � � � Second most common nosocomial infection in US ◦ 15% of all hospital-associated infections ◦ incidence range from 4. 2 to 7. 7/1000 discharges Associated with substantial morbidity and mortality: VAP mortality can reach 60% in ICU Risk Factors for nosocomial pneumonia ◦ extremes of age ◦ severe underlying disease ◦ immunosuppression ◦ depressed sensorium ◦ cardiopulmonary disease ◦ thoracic-abdominal surgery ◦ mechanically assisted ventilation
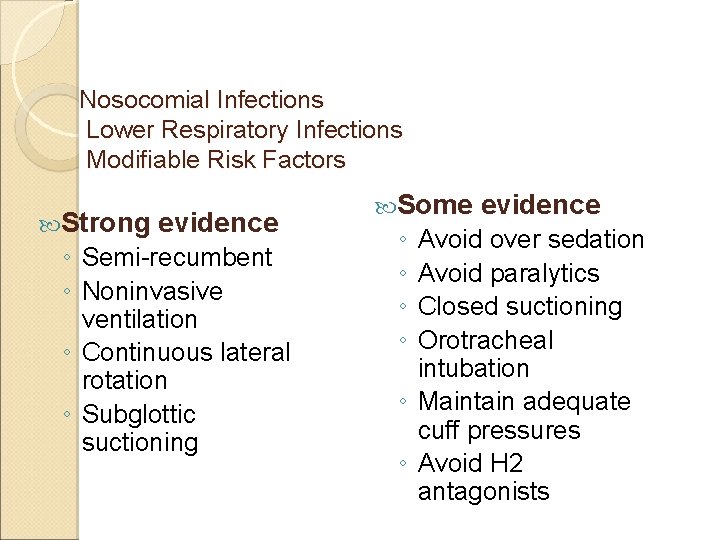
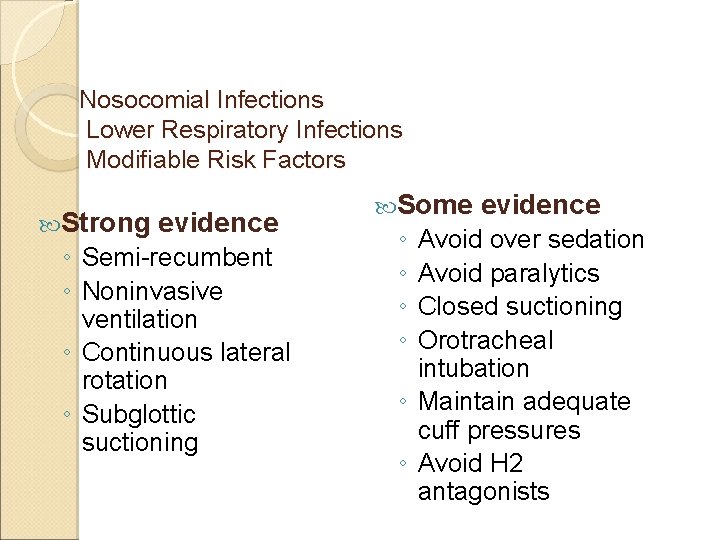
Nosocomial Infections Lower Respiratory Infections Modifiable Risk Factors Strong evidence ◦ Semi-recumbent ◦ Noninvasive ventilation ◦ Continuous lateral rotation ◦ Subglottic suctioning Some ◦ ◦ evidence Avoid over sedation Avoid paralytics Closed suctioning Orotracheal intubation ◦ Maintain adequate cuff pressures ◦ Avoid H 2 antagonists
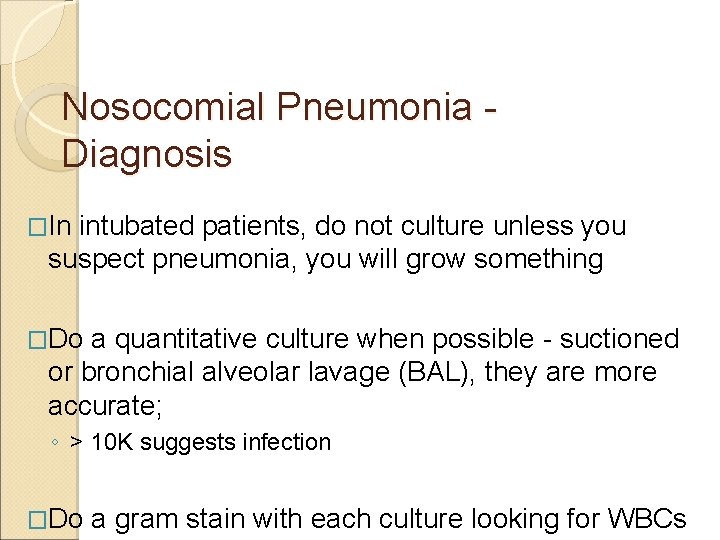
Nosocomial Pneumonia Diagnosis �In intubated patients, do not culture unless you suspect pneumonia, you will grow something �Do a quantitative culture when possible - suctioned or bronchial alveolar lavage (BAL), they are more accurate; ◦ > 10 K suggests infection �Do a gram stain with each culture looking for WBCs
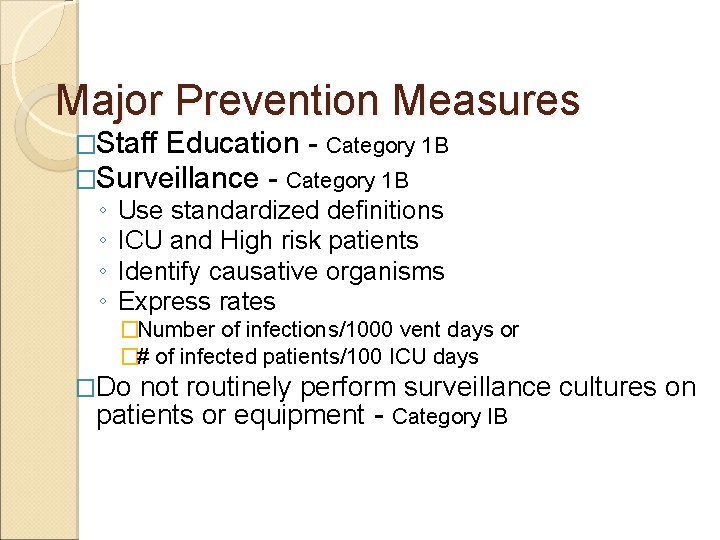
Major Prevention Measures �Staff Education - Category 1 B �Surveillance - Category 1 B ◦ ◦ Use standardized definitions ICU and High risk patients Identify causative organisms Express rates �Number of infections/1000 vent days or �# of infected patients/100 ICU days �Do not routinely perform surveillance cultures on patients or equipment - Category IB
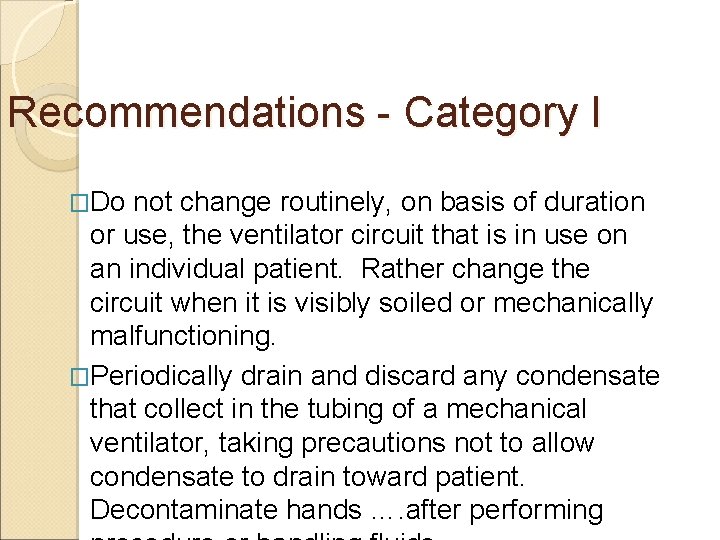
Recommendations - Category I �Do not change routinely, on basis of duration or use, the ventilator circuit that is in use on an individual patient. Rather change the circuit when it is visibly soiled or mechanically malfunctioning. �Periodically drain and discard any condensate that collect in the tubing of a mechanical ventilator, taking precautions not to allow condensate to drain toward patient. Decontaminate hands …. after performing
Category I �Use only sterile, filtered or pasteurized fluid for nebulization and dispense into the nebulizer aseptically. �Decontaminate hands with soap and water or waterless antiseptic agent after contact……. �Change gloves and decontaminate hands…. . .
Major Prevention Measures �Interruption of Transmission of Microorganisms ◦ Sterilization and disinfection of equipment �General Measures �Mechanical Ventilators, Breathing Circuits, Humidifiers, Heat and Moisture Exchange, Nebulizers �Wall Humidifiers �Small volume medication nebulizers �Mist Tents �Other devices �Anesthesia Machines and system �Pulmonary Function testing Equipment �Room air humidifiers and faucet aerators
Supine Body Position & VAP �RCT: 39 semirecumbent vs 47 supine pts �Risk Factors ◦ Supine Position OR = 6. 8 (1. 7 -26. 7) ◦ Enteral Nutrition OR = 5. 7 (1. 5 -22. 8) ◦ MV>7 days OR = 10. 9 (3. 0 -40. 4) �VAP= 50% in supine patients with enteral feeding
Major Prevention Measures �Interruption of Person to Person Transmission of Bacteria ◦ SP ◦ Care of patients with trachs ◦ Suctioning �Modifying Host Risks ◦ Vaccines -pneumococcal vaccine- Category IA ◦ Prevention of Aspiration Precautions ◦ Other prohylactic procedures for Pneumonia
Major Prevention Measures �Prevention of Healthcare associated Disease ◦ Legionairre’s Disease ◦ Pulmonary Aspergillosis ◦ RSV, Parainfluenza, and Adenovirus ◦ Influenza
Smoking cessation Decrease risk of VAP if stop smoking prior to surgery
Oral Hygiene

Performance Measures �How do you measure compliance in your facility?
Performance Measures for Pneumonia Prevention � Measure VAP rates using established benchmarks and standardized definitions ◦ (e. g. CDC NNIS definitions and rates) � Provide feedback to staff and leadership about facility/unit-specific VAP rates � Aggressive education on evidence-based prevention measures to reduce pneumonia � Involve process owners: ICU nurses, MDs, Respiratory Therapy staff!
Influenza Performance Monitors 2. Establish a influenza vaccination program, , monitoring the % of eligible patients in acute-care settings or patients or residents in long-term–care settings who receive the vaccine. 3. Before and during the influenza season, monitor and record # of eligible health-care personnel who receive influenza vaccine and determine the desired unit/facility-specific vaccination rates (recommended by ACIP. )
Performance Monitors for RSV 4. Monitor the (#) number of cases of healthcare–associated RSV infections by geographic location within the facility. Give prompt feedback to appropriate staff members to improve adherence to recommended infection control precautions.

Performance Monitors for Construction-Related Aspergillosis 6. During construction or renovation activities in the facility, monitor personnel adherence to infection-control measures (e. g. , use of barriers, maintenance of negative room pressure) that are aimed at minimizing dust dispersion patients in patientcare areas. Review all cases of healthcare–associated aspergillosis to determine the presence of remediable
Performance Monitors for Pertussis 7. Periodically monitor the frequency of diagnostic testing for pertussis and the time interval between suspicion of the infection and initiation of isolation precautions for patients in whom pertussis is suspected.
Preventing Other Device-Related Infections
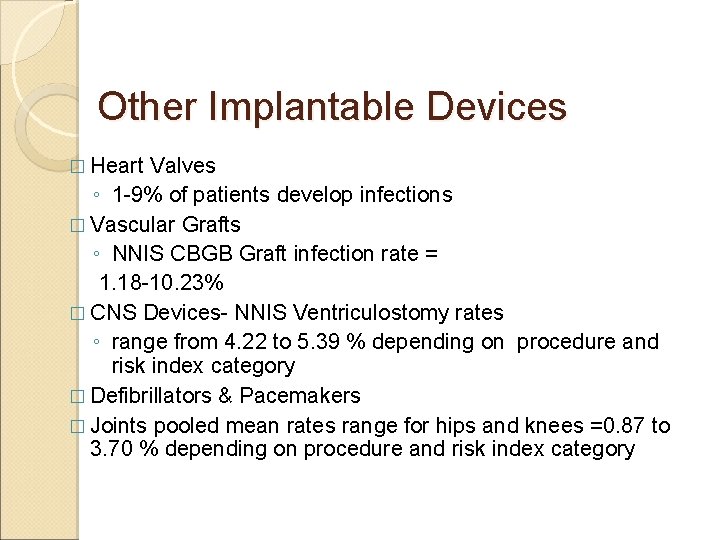
Other Implantable Devices � Heart Valves ◦ 1 -9% of patients develop infections � Vascular Grafts ◦ NNIS CBGB Graft infection rate = 1. 18 -10. 23% � CNS Devices- NNIS Ventriculostomy rates ◦ range from 4. 22 to 5. 39 % depending on procedure and risk index category � Defibrillators & Pacemakers � Joints pooled mean rates range for hips and knees =0. 87 to 3. 70 % depending on procedure and risk index category
Basic Principles & Facts �Same Strategies as preventing SSIs �Settings ◦ OR ◦ Other areas �Monitor Process and Outcomes �Education
Performance Improvement by Infection Risk Reduction Strategies for Invasive Procedures and Insertion of Devices in Special Settings Cardiac Cath Lab & Radiology Source: Loretta Fauerbach, Shands Hosp. U of FL
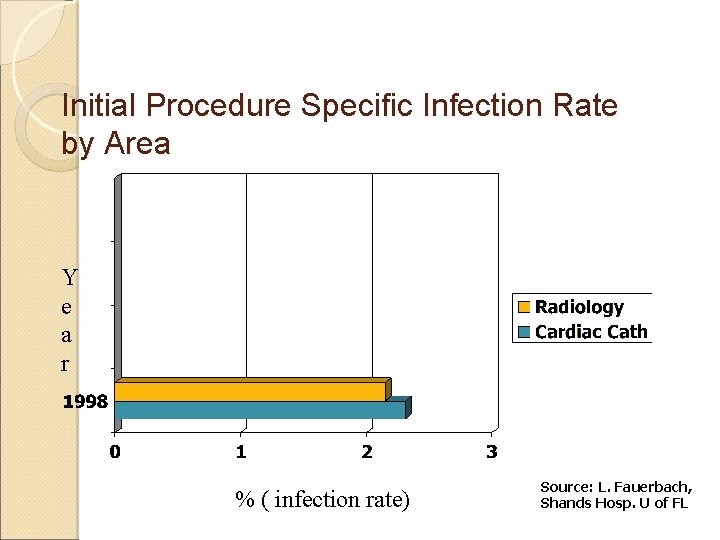
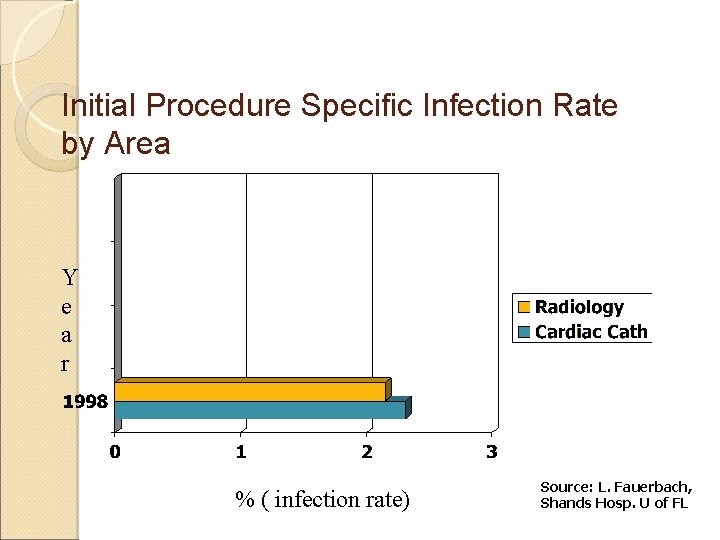
Initial Procedure Specific Infection Rate by Area Y e a r % ( infection rate) Source: L. Fauerbach, Shands Hosp. U of FL
Performance Improvement Team �Infection Control Practitioners �Hospital Epidemiologist �OR Educator �Cardiac Cath Lab Staff �Special Procedures Radiology Staff �Medical Directors for both areas �CSS manager �Surgeon
Action Plan �Observational Studies in Radiology and Cardiac Cath Lab �Continue infection surveillance activities �Formulate recommendations specific for each unit ◦ Literature review �Educate physicians and staff �Measure impact through surveillance and provide feedback
Surveillance �Performed by the ICPs ◦ Review of Lab reports ◦ Reports from unit/medical staff ◦ Chart review �Procedure specific (SSI) rates �Bacteremias ◦ (calculated per 100 patients since device days were not available)
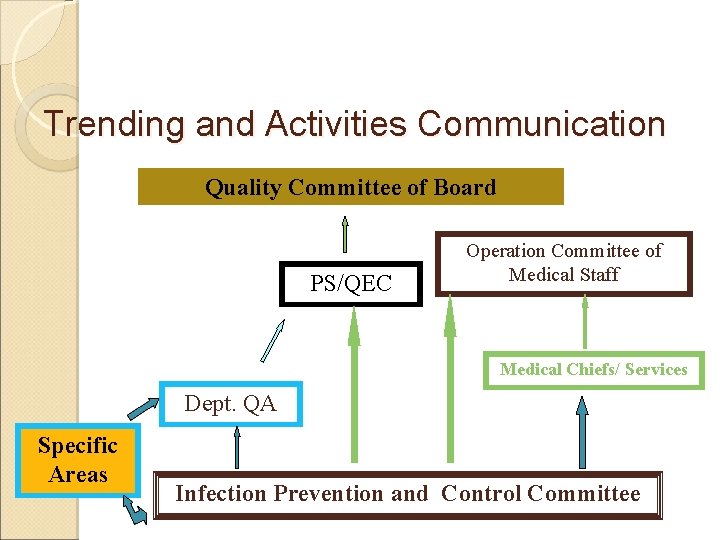
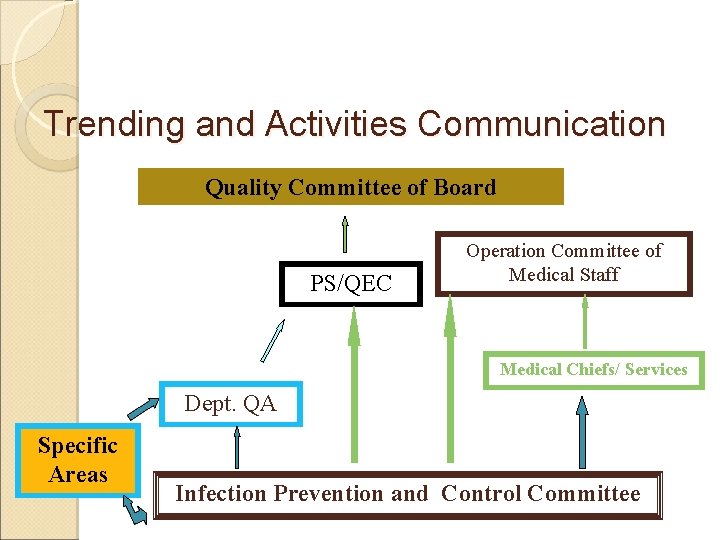
Trending and Activities Communication Quality Committee of Board PS/QEC Operation Committee of Medical Staff Medical Chiefs/ Services Dept. QA Specific Areas Infection Prevention and Control Committee
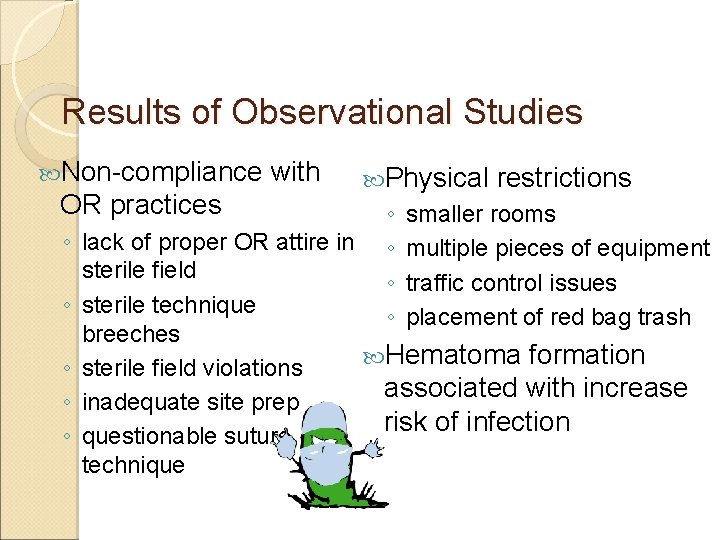
Results of Observational Studies Non-compliance OR practices with Physical ◦ ◦ restrictions smaller rooms multiple pieces of equipment traffic control issues placement of red bag trash ◦ lack of proper OR attire in sterile field ◦ sterile technique breeches Hematoma formation ◦ sterile field violations associated with increase ◦ inadequate site prep risk of infection ◦ questionable suture technique
References for Recommendations �HICPAC’s “Guidelines for Prevention of Surgical Site Infections, 1998” �AORN Standards, 1997 �APIC Text Infection Control and Applied Epidemiology: Principles and Practice, 1996 �Alexander’s Care of the Patient in Surgery
Special Procedures Area Radiology
Cardiac Cath Lab
Interventions �Established training by surgeon for medical staff in Cardiac Cath Lab and Special Procedure Area for Radiology ◦ Suture Technique ◦ Tissue handling techniques to reduce risk of hematoma formation ◦ Other OR recommended practices
Interventions �Adopted/revised protocols for site prep ◦ Larger area ◦ Appropriate use of skin antiseptics �Recommended the use of chlorhexidine gluconate (CHG) �Instituted Pre-operative showering with CHG �Provided feedback to staff on outcome after implementation of recommendations
Interventions �OR personnel inserviced unit staff ◦ Appropriate OR attire ◦ Sterile technique ◦ Instrument handling ◦ Traffic Control ◦ Room set up �Handling of red bag trash �Covering cables �Table set up
Key to Preventing Device Related Infections and Meeting Evolving Challenges Keep learning Keep monitoring Keep implementing new patient safety infection control initiatives Keep educating

BSI UTI VAP ALL HAI!
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Ciliary escalator
Ciliary escalator Beth has a nosocomial infection. how did she get it?
Beth has a nosocomial infection. how did she get it? 27 miles per gallon into kilometers per liter
27 miles per gallon into kilometers per liter In the name of allah the most gracious
In the name of allah the most gracious In the name of allah the most gracious the most merciful
In the name of allah the most gracious the most merciful In the name of allah the beneficent the merciful
In the name of allah the beneficent the merciful Name of organisms
Name of organisms The most gracious
The most gracious In the name of allah the beneficent the merciful
In the name of allah the beneficent the merciful In the name of allah the most beneficent the most merciful
In the name of allah the most beneficent the most merciful The arrangement chapter 9
The arrangement chapter 9 Most general to most specific classification
Most general to most specific classification Aqeedah meaning
Aqeedah meaning In the name of allah the most beneficent the most merciful
In the name of allah the most beneficent the most merciful In the name of god most gracious prayer
In the name of god most gracious prayer Most general to most specific classification
Most general to most specific classification In the name of god most gracious prayer
In the name of god most gracious prayer Guddi baji
Guddi baji Pneumonia
Pneumonia Legionella pneumonia
Legionella pneumonia Aspiration pneumonia
Aspiration pneumonia Pt normal range
Pt normal range Signs of dying from aspiration pneumonia
Signs of dying from aspiration pneumonia Diagnosis banding pneumonia
Diagnosis banding pneumonia Pneumonia hospitalar
Pneumonia hospitalar Jiroveci pneumonia
Jiroveci pneumonia L
L Pneumonia severity index
Pneumonia severity index Pneumonia intersticial
Pneumonia intersticial Pneumonia and tactile fremitus
Pneumonia and tactile fremitus Pneumonia
Pneumonia Septae
Septae Anatomical classification of pneumonia
Anatomical classification of pneumonia Post primary tb
Post primary tb Anatomical classification of pneumonia
Anatomical classification of pneumonia Pneumonia tipica e atipica
Pneumonia tipica e atipica Verminous pneumonia definition
Verminous pneumonia definition