5 th lecture Hospitalacquired pneumonia Nosocomial pneumonia It
- Slides: 19
5 th lecture : Hospital-acquired pneumonia Nosocomial pneumonia • It is a new episode of pneumonia occurring at least 2 days after admission to hospital. • It is: the 2 nd most common hospital-acquired infection (HAI) & the leading cause of HAI-associated death It risky in: • The elderly • In intensive care units, • When mechanically ventilated
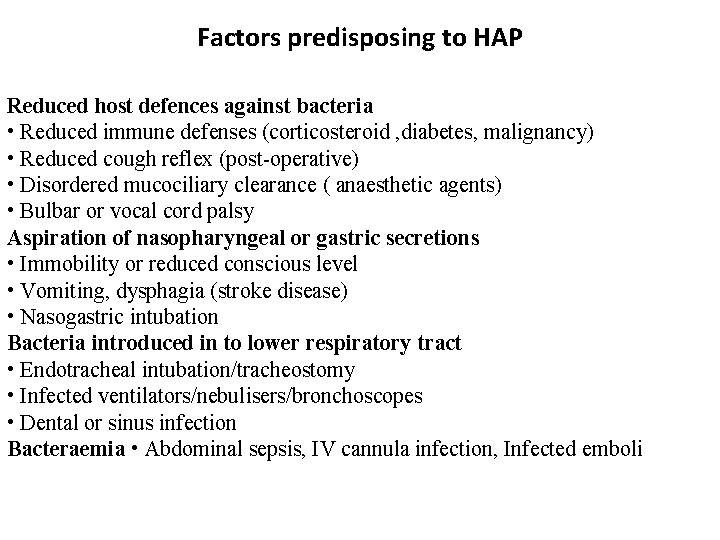
Factors predisposing to HAP Reduced host defences against bacteria • Reduced immune defenses (corticosteroid , diabetes, malignancy) • Reduced cough reflex (post-operative) • Disordered mucociliary clearance ( anaesthetic agents) • Bulbar or vocal cord palsy Aspiration of nasopharyngeal or gastric secretions • Immobility or reduced conscious level • Vomiting, dysphagia (stroke disease) • Nasogastric intubation Bacteria introduced in to lower respiratory tract • Endotracheal intubation/tracheostomy • Infected ventilators/nebulisers/bronchoscopes • Dental or sinus infection Bacteraemia • Abdominal sepsis, IV cannula infection, Infected emboli
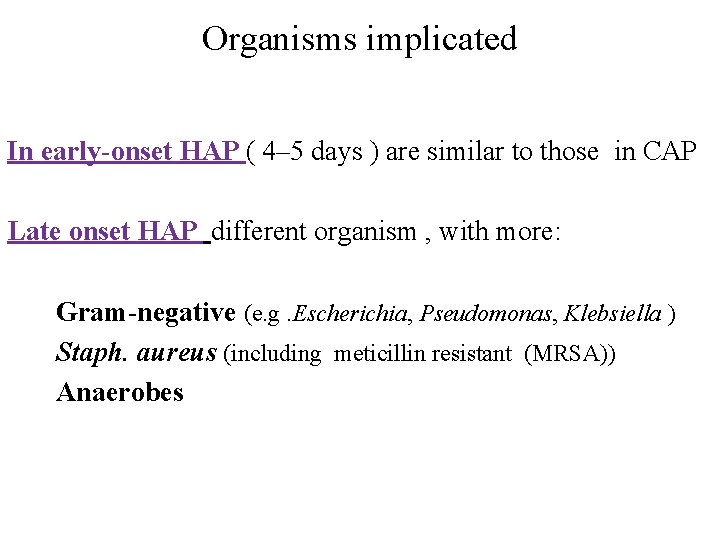
Organisms implicated In early-onset HAP ( 4– 5 days ) are similar to those in CAP Late onset HAP different organism , with more: Gram-negative (e. g. Escherichia, Pseudomonas, Klebsiella ) Staph. aureus (including meticillin resistant (MRSA)) Anaerobes
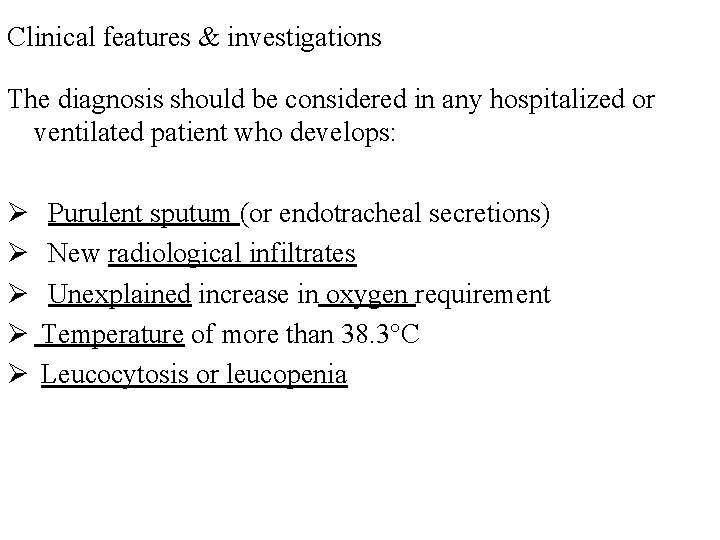
Clinical features & investigations The diagnosis should be considered in any hospitalized or ventilated patient who develops: Ø Ø Ø Purulent sputum (or endotracheal secretions) New radiological infiltrates Unexplained increase in oxygen requirement Temperature of more than 38. 3°C Leucocytosis or leucopenia
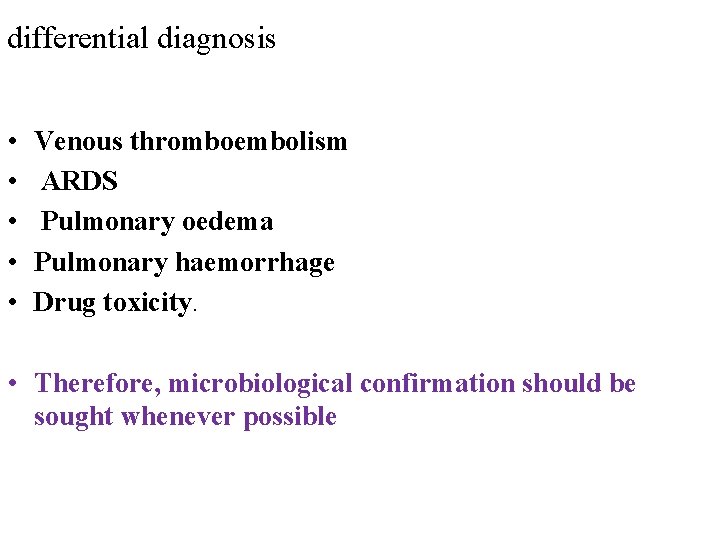
differential diagnosis • • • Venous thromboembolism ARDS Pulmonary oedema Pulmonary haemorrhage Drug toxicity. • Therefore, microbiological confirmation should be sought whenever possible
Management • The principles are similar to those for CAP, focusing on: adequate oxygenation, fluid balance & antibiotics • The choice of empirical antibiotic therapy is more challenging (diversity of pathogens & drug resistance) In early-onset HAP, pats. received no previous antibiotics, treated with: • co-amoxiclav or cefuroxime If the patient has received a course of recent antibiotics, • piperacillin/tazobactam • third generation cephalosporin.
In late-onset HAP the choice of antibiotics must cover Gram-negative Staph. aureus ( MRSA) & anaerobes Anti pseudomonal cover by: • carbapenem (meropenem) • a third-generation cephalosporin with aminoglycoside MRSA cover by glycopeptides (vancomycin)
The choice of agent Guided by: • knowledge of local patterns of microbiology & antibiotic resistance • It is usual to commence broad-based cover, discontinuing less appropriate antibiotics as culture results become available. duration of antibiotic therapy a matter for clinical judgments Physiotherapy aid expectoration in the immobile & elderly nutritional support is often required.
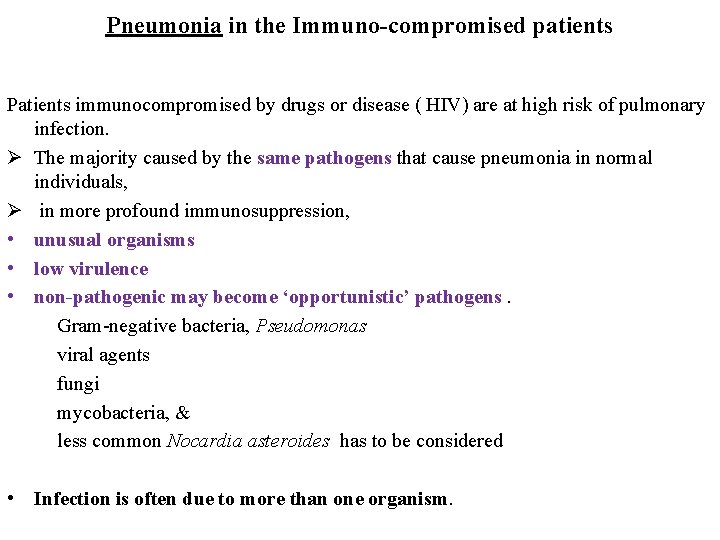
Pneumonia in the Immuno-compromised patients Patients immunocompromised by drugs or disease ( HIV) are at high risk of pulmonary infection. Ø The majority caused by the same pathogens that cause pneumonia in normal individuals, Ø in more profound immunosuppression, • unusual organisms • low virulence • non-pathogenic may become ‘opportunistic’ pathogens. Gram-negative bacteria, Pseudomonas viral agents fungi mycobacteria, & less common Nocardia asteroides has to be considered • Infection is often due to more than one organism.
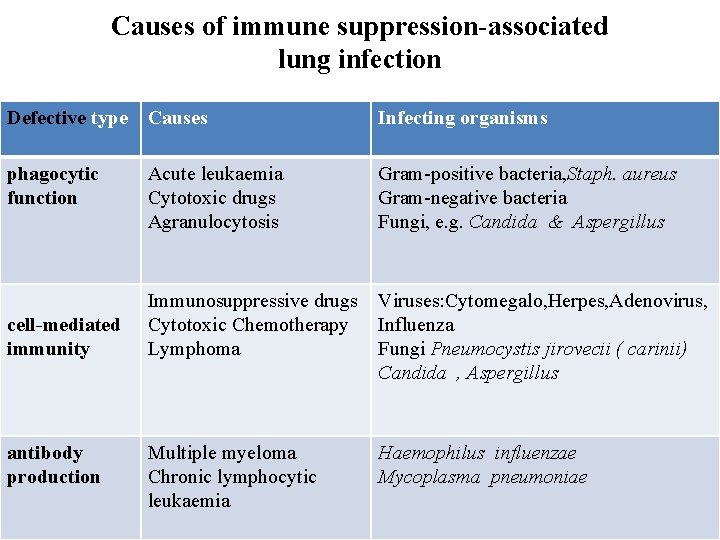
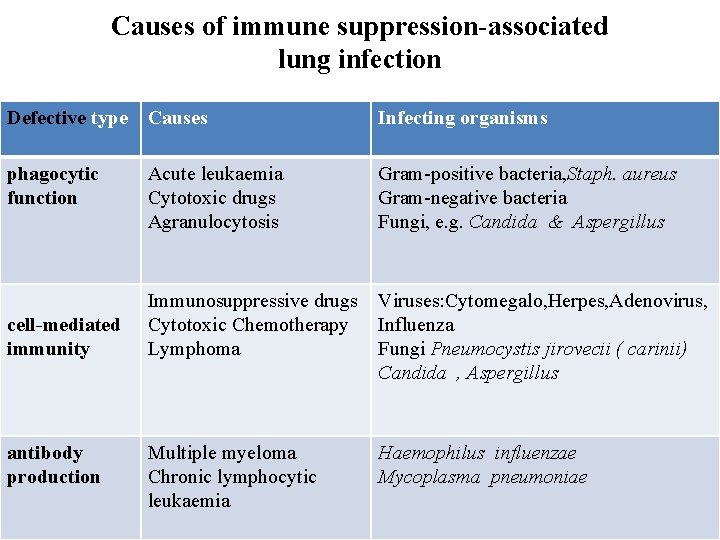
Causes of immune suppression-associated lung infection Defective type Causes Infecting organisms phagocytic function Acute leukaemia Cytotoxic drugs Agranulocytosis Gram-positive bacteria, Staph. aureus Gram-negative bacteria Fungi, e. g. Candida & Aspergillus Immunosuppressive drugs Cytotoxic Chemotherapy Lymphoma Viruses: Cytomegalo, Herpes, Adenovirus, Influenza Fungi Pneumocystis jirovecii ( carinii) Candida , Aspergillus Multiple myeloma Chronic lymphocytic leukaemia Haemophilus influenzae Mycoplasma pneumoniae cell-mediated immunity antibody production
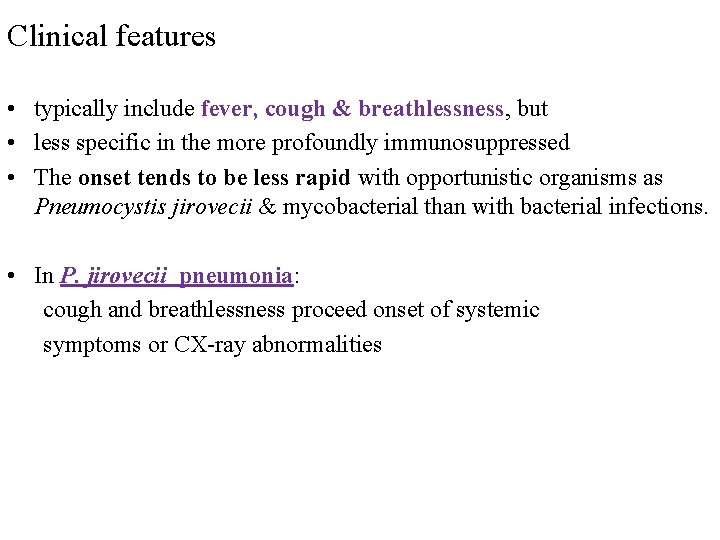
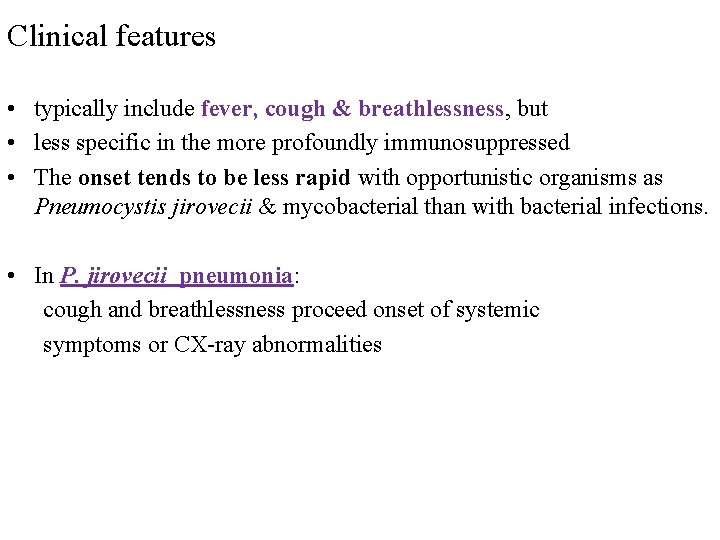
Clinical features • typically include fever, cough & breathlessness, but • less specific in the more profoundly immunosuppressed • The onset tends to be less rapid with opportunistic organisms as Pneumocystis jirovecii & mycobacterial than with bacterial infections. • In P. jirovecii pneumonia: cough and breathlessness proceed onset of systemic symptoms or CX-ray abnormalities
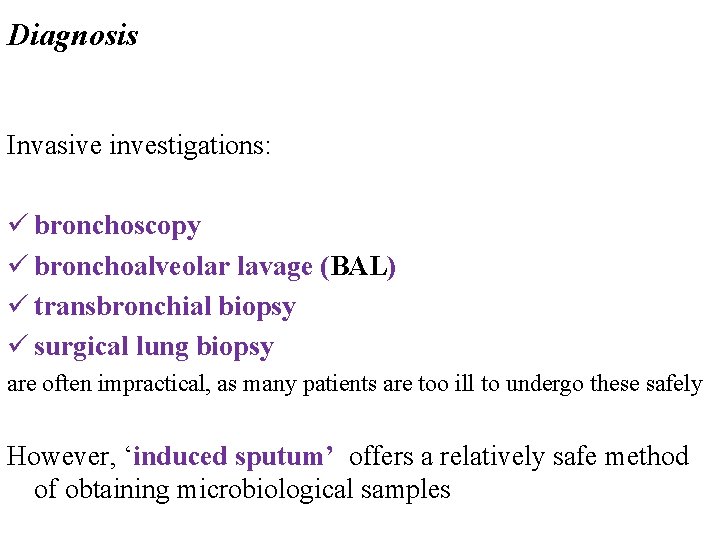
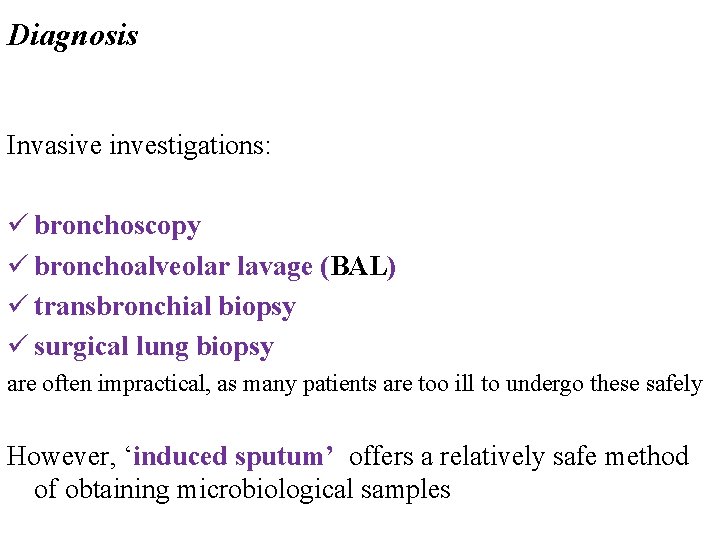
Diagnosis Invasive investigations: ü bronchoscopy ü bronchoalveolar lavage (BAL) ü transbronchial biopsy ü surgical lung biopsy are often impractical, as many patients are too ill to undergo these safely However, ‘induced sputum’ offers a relatively safe method of obtaining microbiological samples
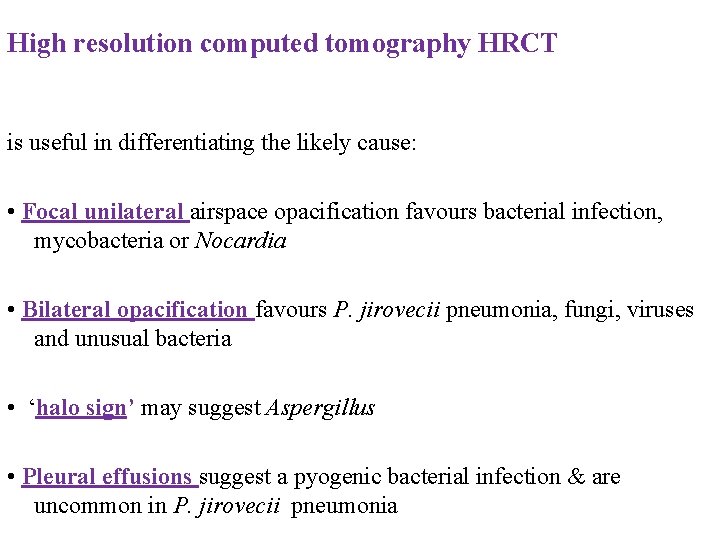
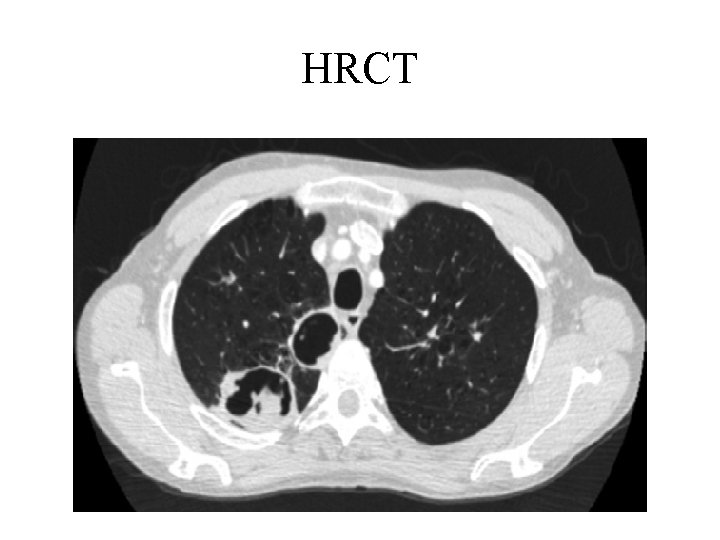
High resolution computed tomography HRCT is useful in differentiating the likely cause: • Focal unilateral airspace opacification favours bacterial infection, mycobacteria or Nocardia • Bilateral opacification favours P. jirovecii pneumonia, fungi, viruses and unusual bacteria • ‘halo sign’ may suggest Aspergillus • Pleural effusions suggest a pyogenic bacterial infection & are uncommon in P. jirovecii pneumonia
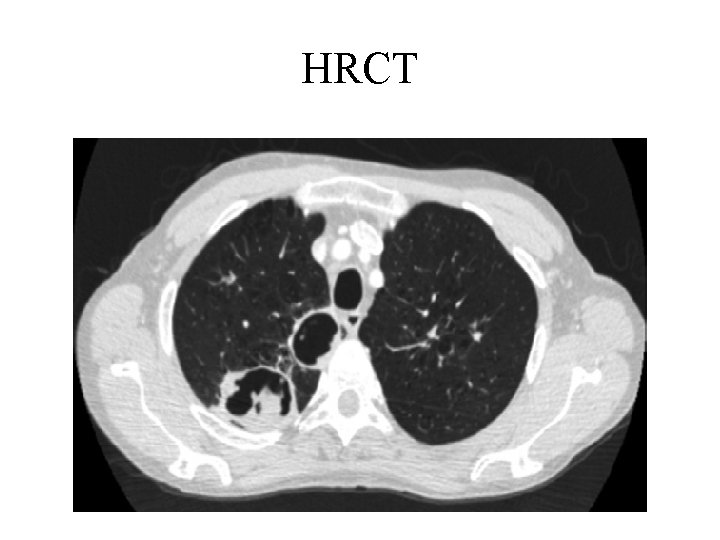
HRCT
Management • In theory, treatment should be based on the identified causative organism but, • In practice, this is frequently unknown and broad-spectrum antibiotic therapy is required, such as : • third-generation cephalosporin or a quinolone, plus an • antistaphylococcal , or • antipseudomonal penicillin plus aminoglycoside • treatment may be tailored according to the results of investigations and the clinical response. • These may dictate the addition of antifungal or antiviral therapies
Supportive pneumonia, Aspiration pneumonia & pulmonary Abscess • These conditions are considered together, as their aetiology and clinical features overlap. • Suppurative pneumonia is a destruction of the lung parenchyma by the inflammatory process & microabscess formation • Pulmonary abscess’ is refer to lesions in which there is a large localised collection of pus, or a cavity lined by chronic inflammatory tissue, from which pus has escaped by rupture into a bronchus.
Risk factor • Aspiration localize to dependent areas • Bronchial obstruction by a neoplasm, foreign body. • Infections due to a Mixture of anaerobes & aerobes Ø the most likely infecting organism is Staph. Aureus or Klebsiella pneumoniae. Ø Bacterial infection of a: pulmonary infarct or a collapsed lobe.
Clinical features of suppurative pneumonia Symptoms • Cough with large amounts of sputum, sometimes fetid and bloodstained • Pleural pain • Sudden expectoration of copious amounts of foul sputum if abscess ruptures into a bronchus Clinical signs • High remittent pyrexia • Profound systemic upset • Digital clubbing may develop quickly (10– 14 days) • Consolidation on chest examination; rarely signs of cavitation • Pleural rub common • Rapid deterioration in general health, with marked weight loss if not adequately treated
I investigations and management CXR: Ø homogeneous lobar or segmental opacity consistent with consolidation or collapse. Ø Abscesses (cavitation and fluid level) Ø Occasionally, a preexisting emphysematous bulla infected and appears as a cavity containing an air–fluid level. treated with • Intravenous co-amoxiclav 1. 2 g 3 times daily. • oral metronidazole 400 mg 3 times daily If an anaerobic. • Further modification of antibiotics may be required, depending on the clinical response and the microbiological results.
 Phagocytr
Phagocytr Beth has a nosocomial infection. how did she get it?
Beth has a nosocomial infection. how did she get it? 01:640:244 lecture notes - lecture 15: plat, idah, farad
01:640:244 lecture notes - lecture 15: plat, idah, farad Bronchiolitis
Bronchiolitis Blood concept map answer
Blood concept map answer Pneumonia
Pneumonia Pneumonia lung sound
Pneumonia lung sound Pneumonia lipoídica
Pneumonia lipoídica Lobær pneumoni
Lobær pneumoni Congenital pneumonia
Congenital pneumonia Iatrogeic
Iatrogeic Pneumonia
Pneumonia Pneumonia
Pneumonia Pneumonia
Pneumonia Atypical bacteria
Atypical bacteria Pathophysiology of pneumonia
Pathophysiology of pneumonia Klasifikasi asma
Klasifikasi asma Anatomical classification of pneumonia
Anatomical classification of pneumonia Why is tactile fremitus decreased in pleural effusion
Why is tactile fremitus decreased in pleural effusion Pneumonia lobar
Pneumonia lobar