SIMPLIFYING PELVIC ORGAN PROLAPSE Frank A Potestio MSc

- Slides: 46
SIMPLIFYING PELVIC ORGAN PROLAPSE Frank A. Potestio, MSc, MD, FRCSC Associate Professor NOSM
DISCLOSURE �No conflict of interest
LEARNING OBJECTIVES At the end of this session participants will be able to 1. Classify and quantify the compartments of pelvic organ prolapse (POP) 2. Plan the evaluation and appropriate referral of women with problematic POP 3. Select an ongoing maintenance and monitoring plan for women with a pessary in place
CASE STUDY I A 68 y. o. female presents with pelvic pressure and a bulging vaginally. She also complains of urinary frequency and urgency, as well as nocturia. Examination reveals a stage 3 uterine prolapse with a stage 2 cystocoele. The vagina is also atrophic. Urine culture 2 days ago was negative. You recommend
CASE STUDY I �Surgery to correct pelvic organ prolapse �Use of a pessary �Vaginal estrogen for urogenital atrophy �Medical therapy for overactive bladder �Referral to urogynecologist
INTRODUCTION �Pelvic hernia �Affects up to 50 % of parous women � 10 -20 % symptomatic � 11 % undergo surgery by age 80 � 29 – 40 % reoperation within 3 years
SYMPTOMS OF POP �Bulging �Pelvic pressure �Back ache �Bladder, bowel and sexual dysfunction
RISK FACTORS �Parity �Intrinsic weakness or atrophy �Obesity �Hysterectomy �Constipation �Connective tissue disorders
CONFOUNDERS �Urinary incontinence (latent) �Genitourinary syndrome of menopause �Urinary tract infections
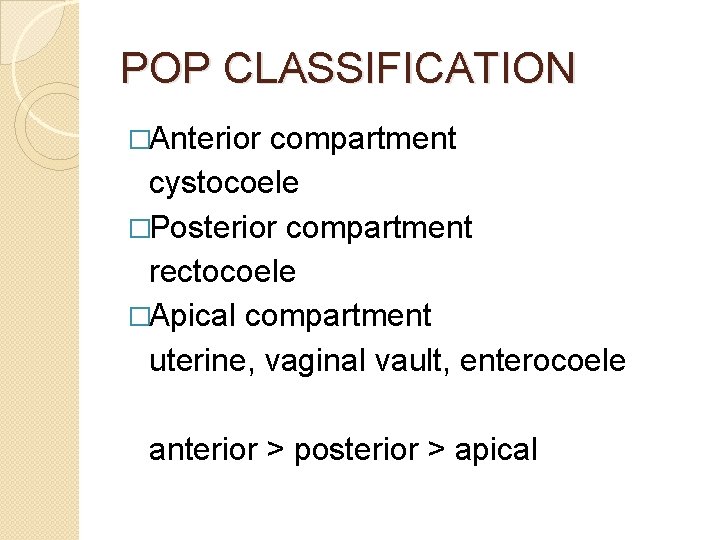
POP CLASSIFICATION �Anterior compartment cystocoele �Posterior compartment rectocoele �Apical compartment uterine, vaginal vault, enterocoele anterior > posterior > apical
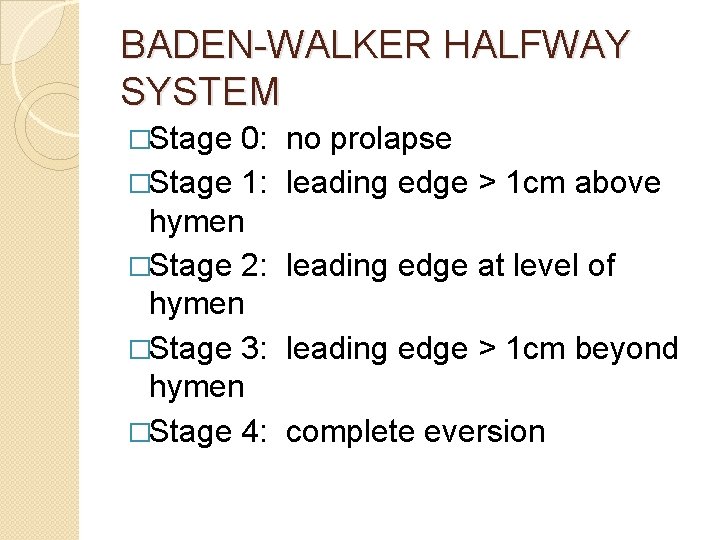
BADEN-WALKER HALFWAY SYSTEM �Stage 0: �Stage 1: hymen �Stage 2: hymen �Stage 3: hymen �Stage 4: no prolapse leading edge > 1 cm above leading edge at level of leading edge > 1 cm beyond complete eversion
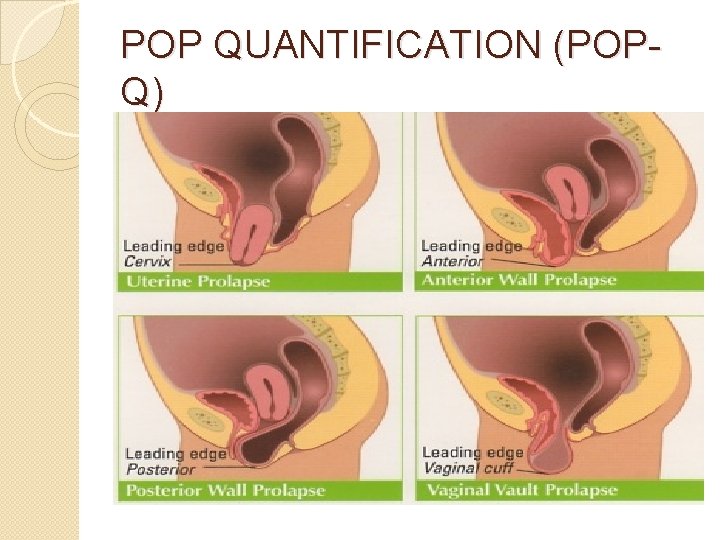
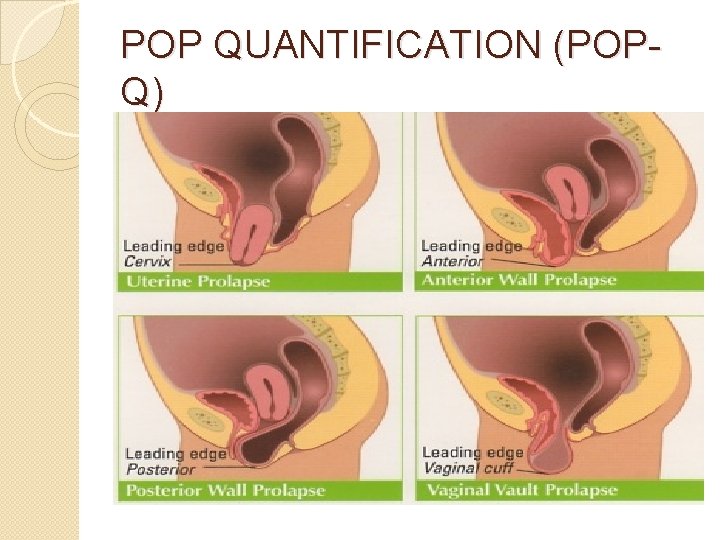
POP QUANTIFICATION (POPQ)
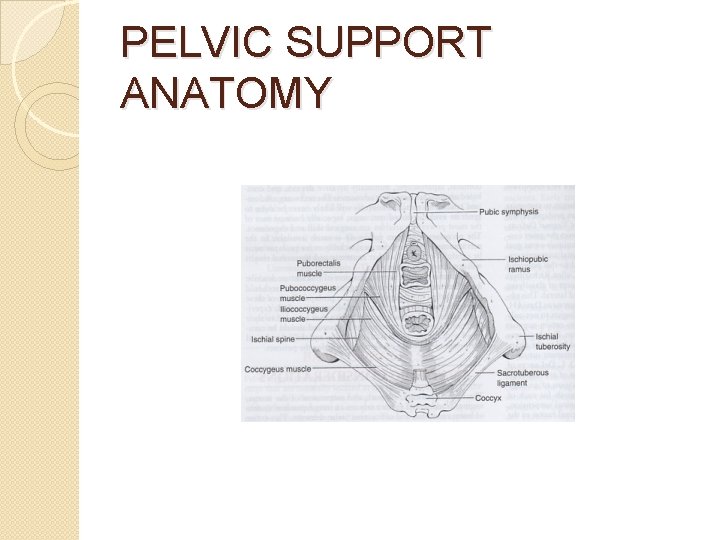
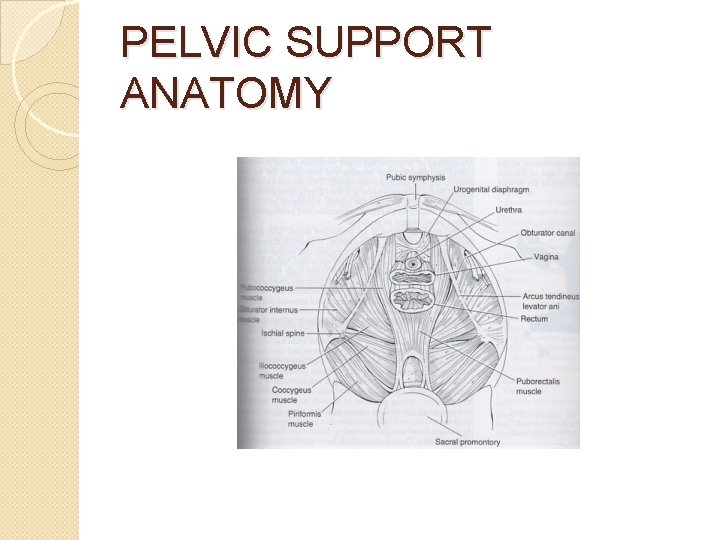
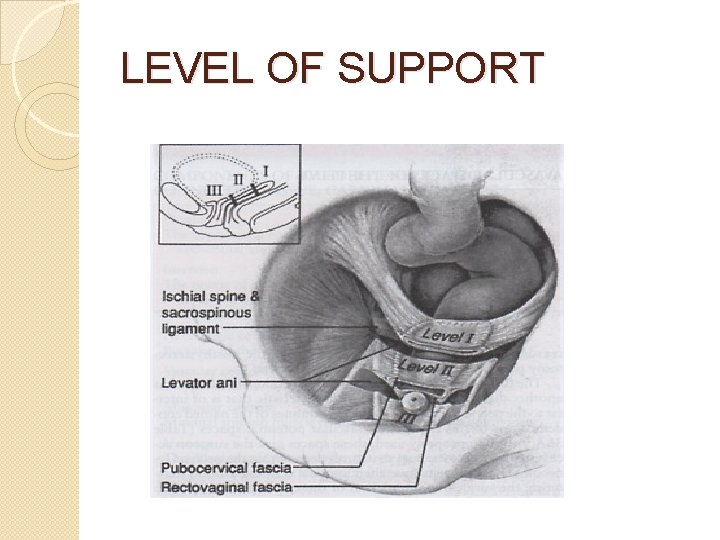
ANATOMY OF PELVIC SUPPORT Complex Interaction �Muscles (levator ani) �Fasciae (urogenital diaphragm, endopelvic) �Ligaments (uterosacral, cardinal)
PATHOPHYSIOLOGY OF POP �Attenuation or stretching of pelvic connective tissue �Site-specific breaks or tears �Anatomical defects in pelvic support
PRINCIPLES OF SURGERY �Restore normal anatomy & function �Distal plications �Site–specific repairs �Grafts, meshes bolster defect-specific repairs
PROSPECT TRIAL (2017) �Synthetic mesh: biological graft: native tissue �Augmentation surgery did not improve outcomes in terms of effectiveness or quality of life �> 1/10 women had a mesh complication
PESSARY FOR PROLAPSE �First-line treatment � 70 – 90 % can be properly fitted �Bulging reduced in 70 – 90 % �Pressure symptoms relieved in 30 – 50 % � 20 – 30 % continence rate
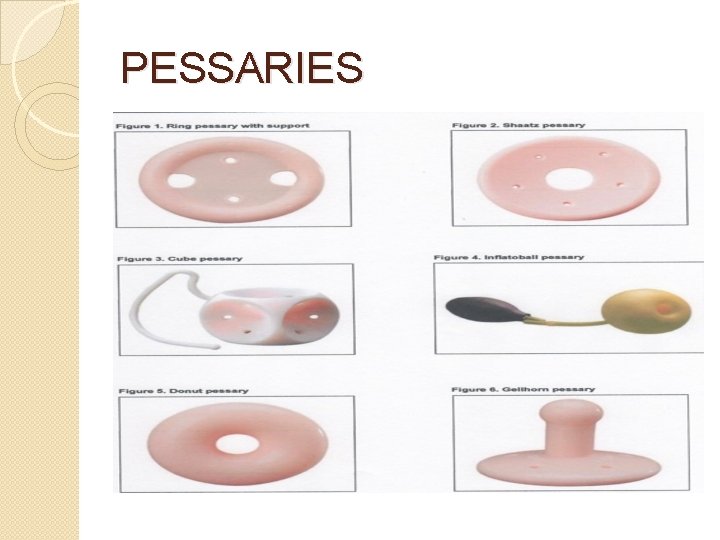
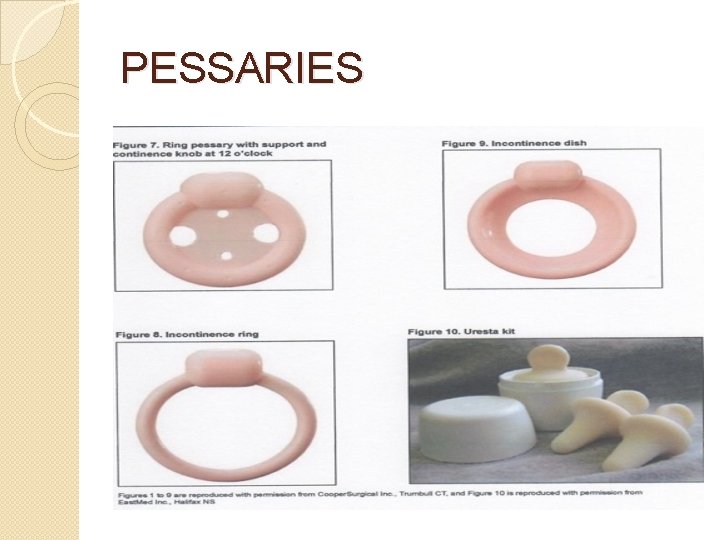
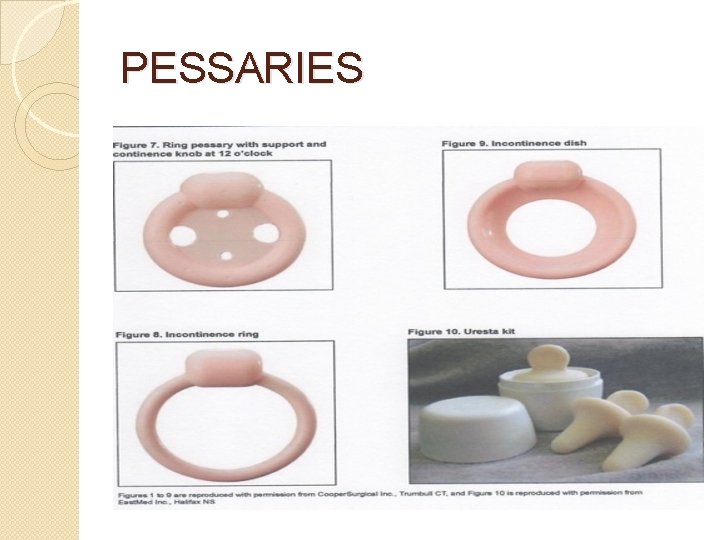
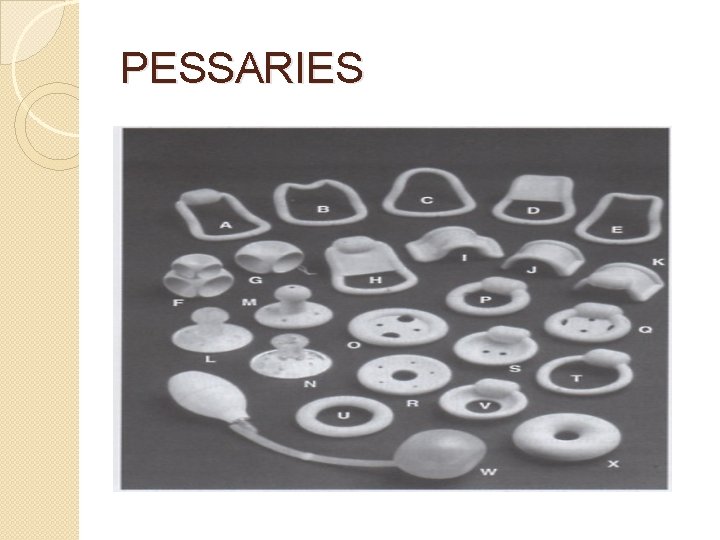
TYPES OF PESSARIES �Support ring, Shaatz, Smith, Hodge, Gehrung �Space-occupying cube, donut, inflatoball �Combination Gellhorn �Incontinence
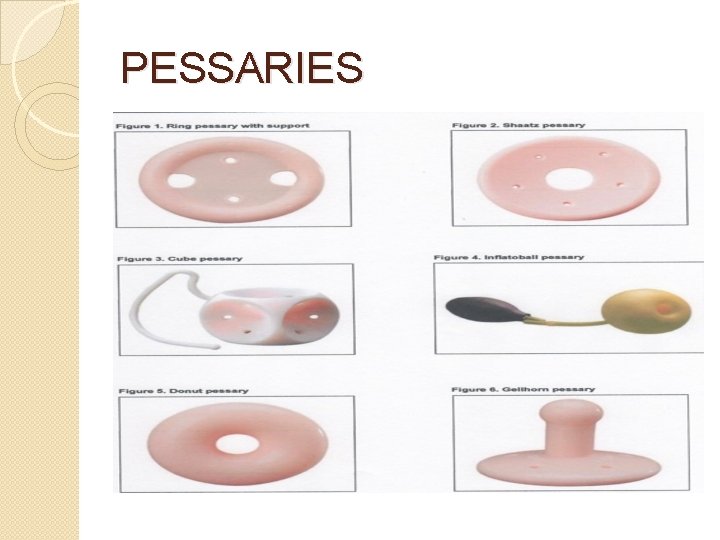
PESSARIES
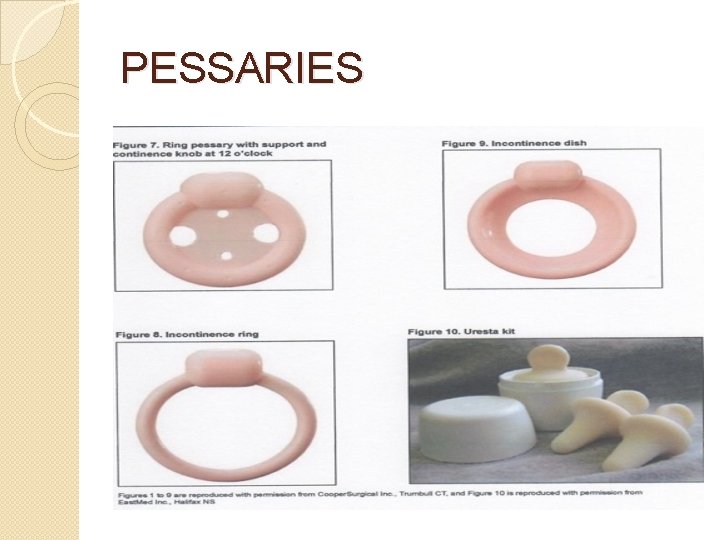
PESSARIES
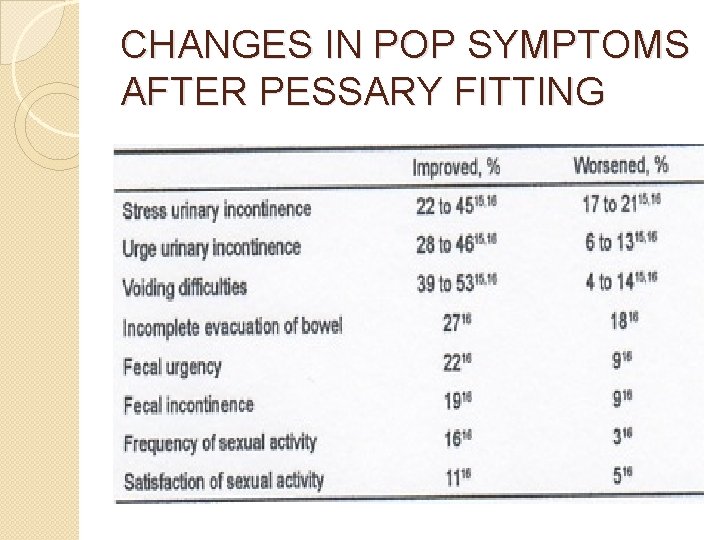
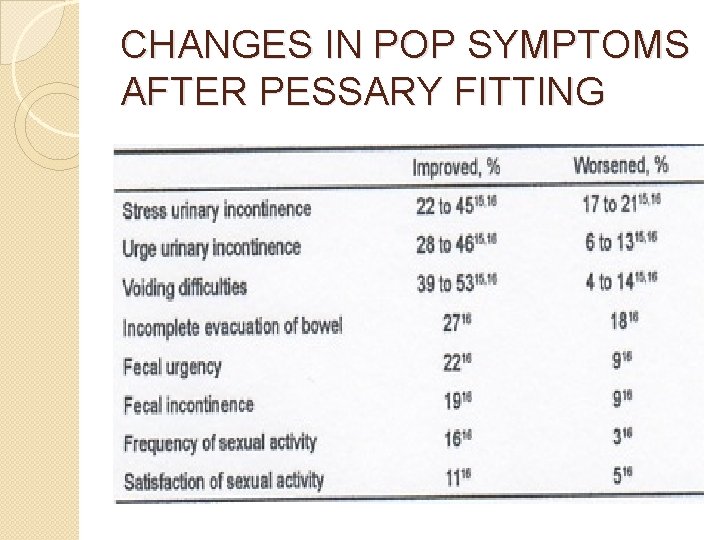
CHANGES IN POP SYMPTOMS AFTER PESSARY FITTING
PESSARY CARE �Proper fitting and adequate patient education �Initial follow-up within 2 -4 weeks � 3 month follow-up if unable to perform self care � 6 month or 1 year intervals if no complications arise
CASE STUDY 2 The 68 y. o. female who you successfully fitted with a ring pessary to manage her symptomatic cystocoele and uterine prolapse now presents at her 1 year follow-up with vaginal bleeding. She has been compliant with her routine 3 month pessary care visits with no concerns. You recommend
CASE STUDY 2 �Cleaning & reinsertion of pessary with reassurance �Removal of pessary & examination (including swabs) �Pap smear �Endometrial biopsy
PESSARY COMPLICATIONS �Erosions (2 -9 %) local pressure leads to devascularization �Infections (2 -3 %) physiologic response to friction �Rarely major vesicovaginal fistulae, bowel fistulae, incarceration
DISCONTINUATION OF PESSARY �Posterior wall prolapse �Urinary incontinence �Complications
SUMMARY �Examination documenting defects in pelvic support (compartment, stage) �Refer women who desire reconstructive surgery that restore normal support and function �Pessaries should be considered in all women presenting with symptomatic prolapse
REFERENCES Chan M et al. , What are the Clinical Factors that are Predictive of Persistent Pessary Use at 12 Months? JOGC 2019; 41(9): 1276 -1281. � Larouche M et al. , Transvaginal Mesh Procedures for Pelvic Organ Prolapse. JOGC 2017; 39(11): 1085 -1097. � Glazener C et al. Mesh, Graft or Standard Repair for Women having Primary Transvaginal Anterior or Posterior Compartment Prolapse Surgery: Two Parallel-Group Multicentre Randomised, Controlled Trials (PROSPECT). Lancet 2017; 389(1): 381 -392. � Magali R et al. , Technical Update on Pessary Use. JOGC 2013; 35(7): 1276 -1281. � Beckmann R et al. Pelvic Support Defects, Urinary Incontinence and Urinary Tract Infections. Obstetrics and Gynecology 7 th edition 2014; 30: 277 -286. � Rock J et al. , Surgical / Nonsurgical Correction of Defects in Pelvic Support. Telinde’s Operative Gynecology 10 th ed. , 2011. �

CASE STUDY II A 88 y. o. female presents with painful vaginal vault prolapse and has tried a number of pessaries without success. She had an abdominal hysterectomy 40 years ago. Medical review reveals CAD with persistent angina and moderate COPD from prior smoking. She desires surgical correction if possible and is not sexually active. The most reasonable procedure for her is
CASE STUDY II �Transabdominal sacrocolpopexy �Sacrospinous ligament suspension �Le. Fort partial colpocleisis �Total colpocleisis
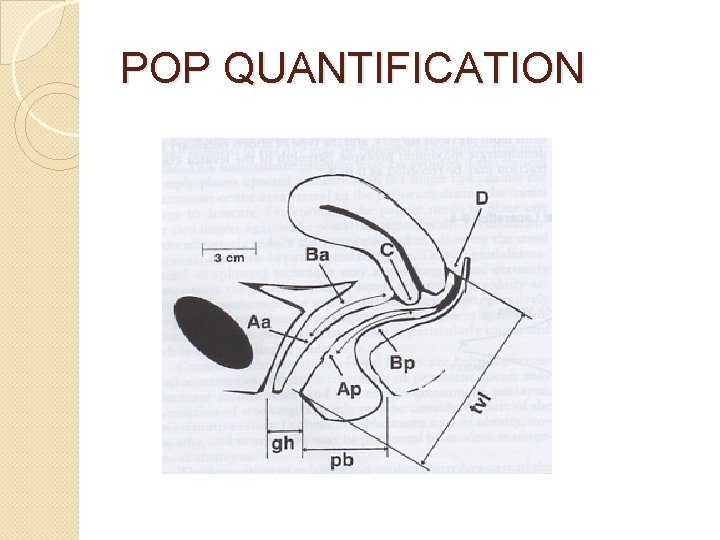
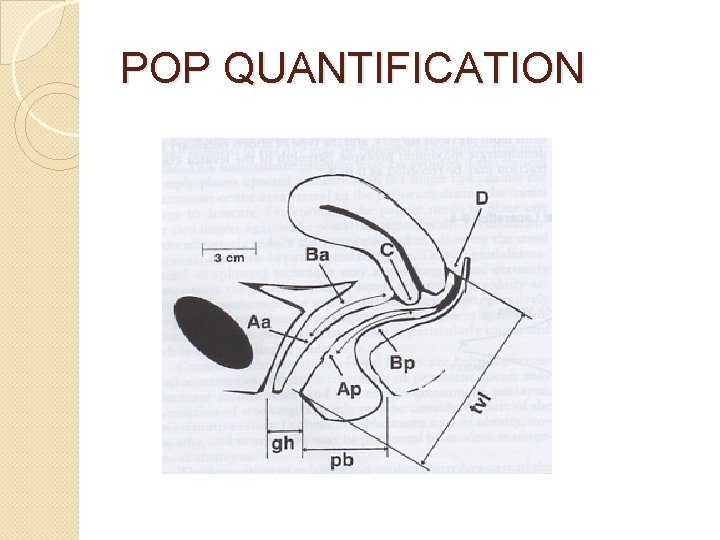
POP QUANTIFICATION
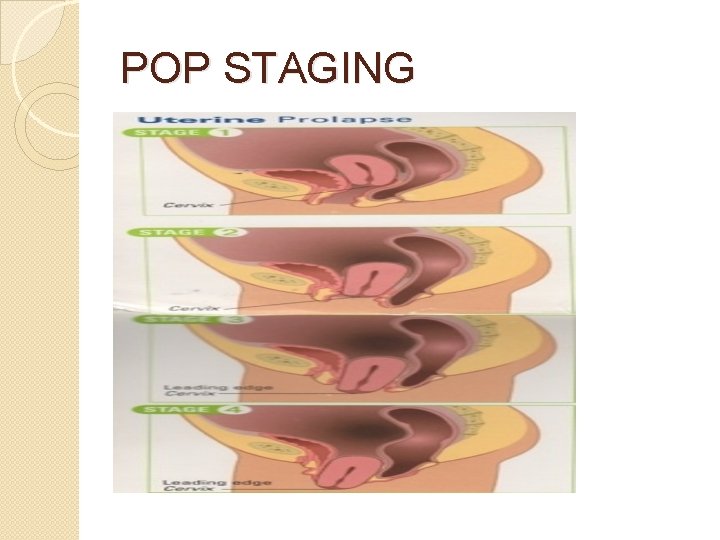
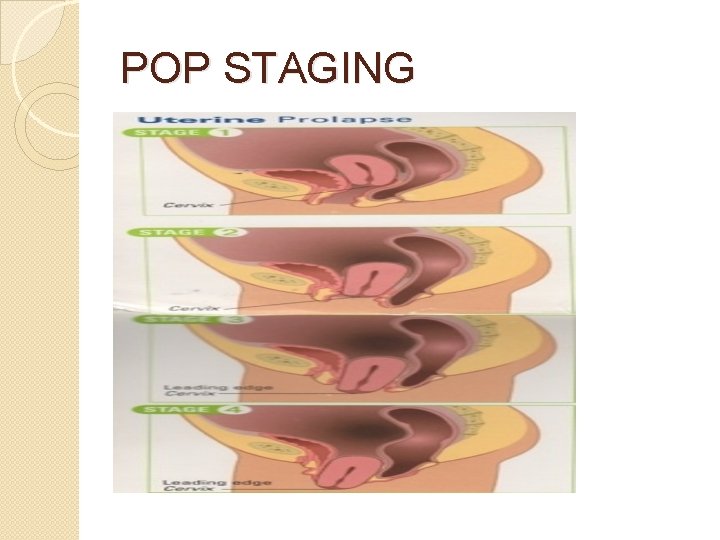
POP STAGING
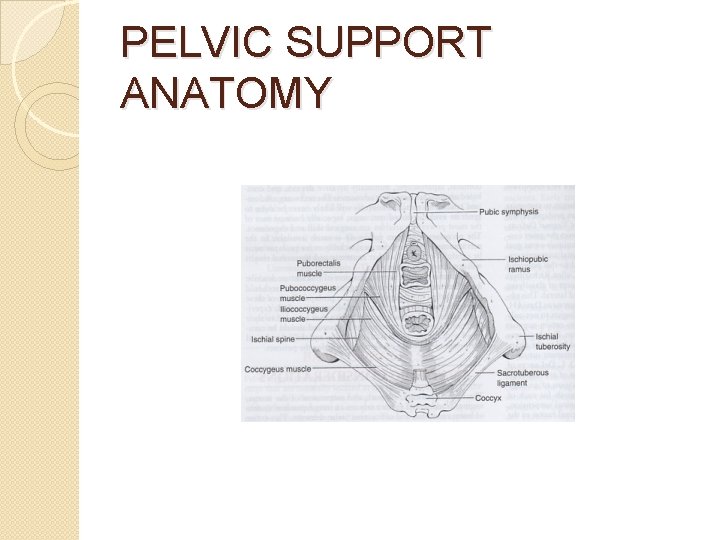
PELVIC SUPPORT ANATOMY
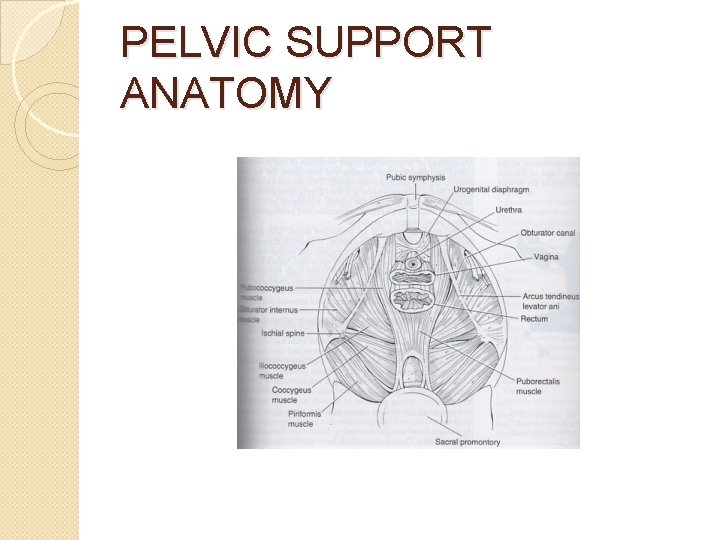
PELVIC SUPPORT ANATOMY
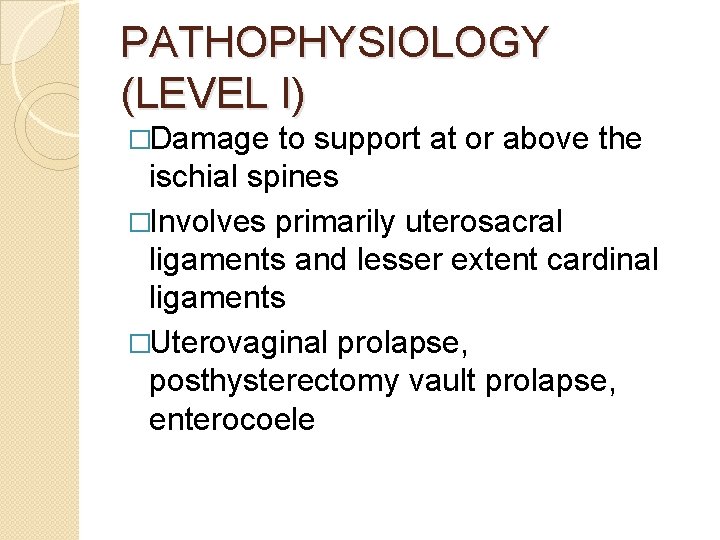
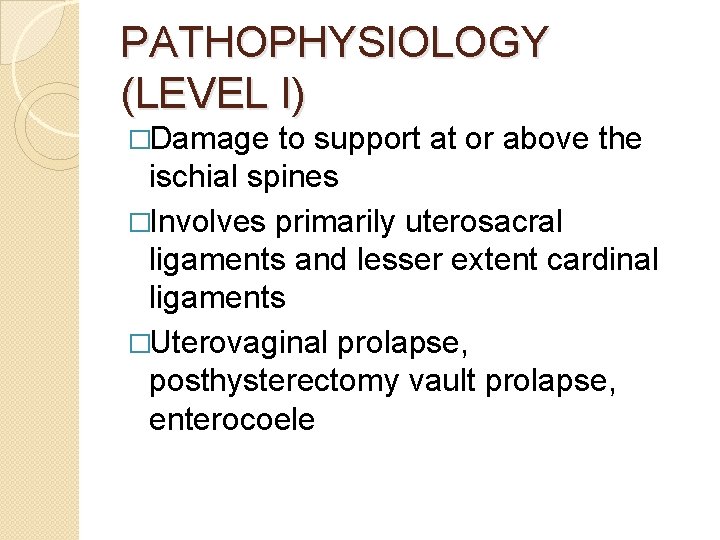
PATHOPHYSIOLOGY (LEVEL I) �Damage to support at or above the ischial spines �Involves primarily uterosacral ligaments and lesser extent cardinal ligaments �Uterovaginal prolapse, posthysterectomy vault prolapse, enterocoele
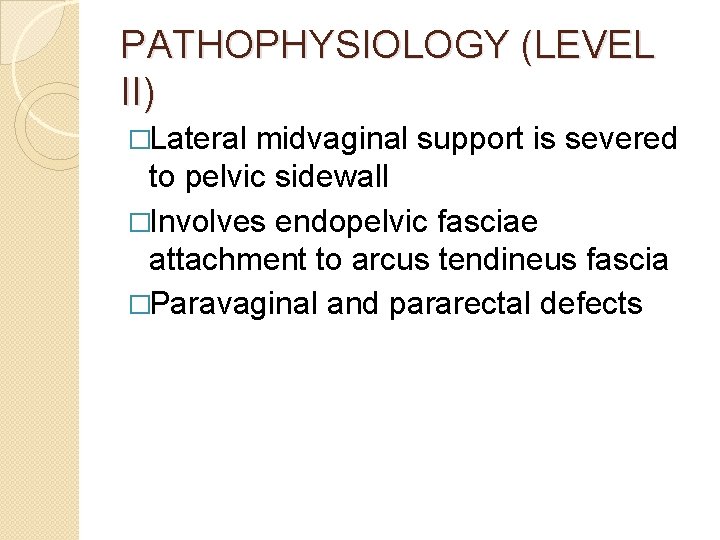
PATHOPHYSIOLOGY (LEVEL II) �Lateral midvaginal support is severed to pelvic sidewall �Involves endopelvic fasciae attachment to arcus tendineus fascia �Paravaginal and pararectal defects
PATHOPHYSIOLOGY (LEVEL III) �Damage to fusion of urogenital diaphragm anteriorly or proximal perineum posteriorly �Central defects of fabric of pubocervical and rectovaginal septa �Cystocoele, rectocoele
PELVIC SUPPORT DISORDERS �Historic: attenuation or stretching of pelvic connective tissue �Recent: site-specific breaks or tears in connective tissue �Identifiable anatomical defects in pelvic support (Levels I, III)
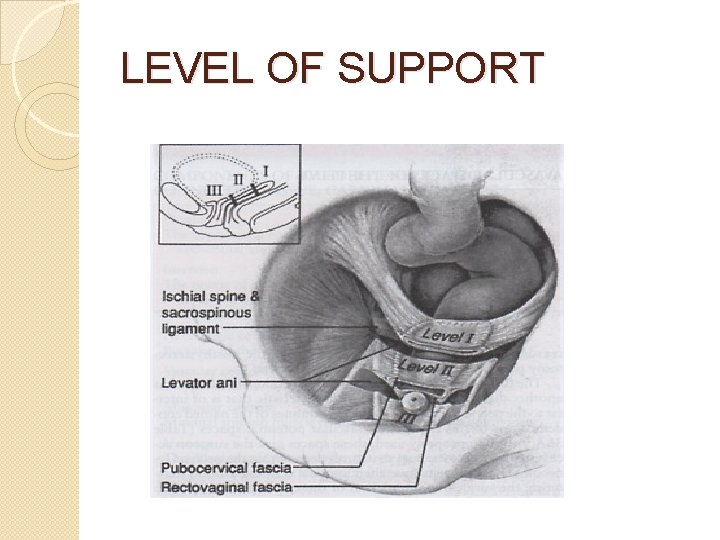
LEVEL OF SUPPORT
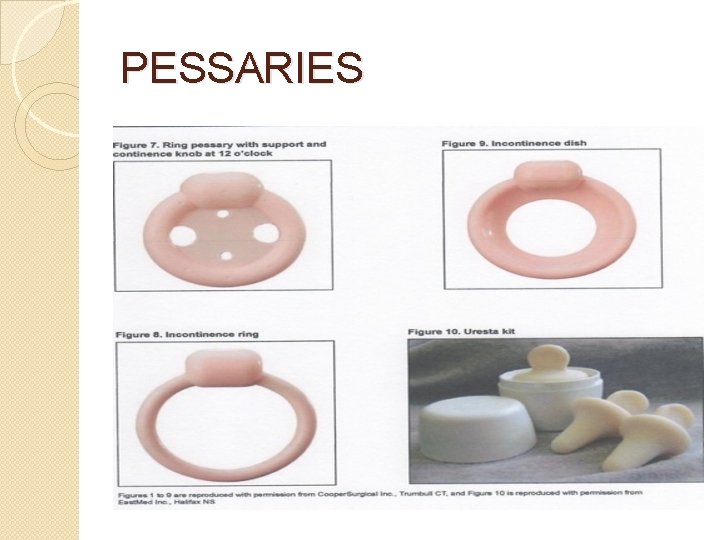
PESSARIES
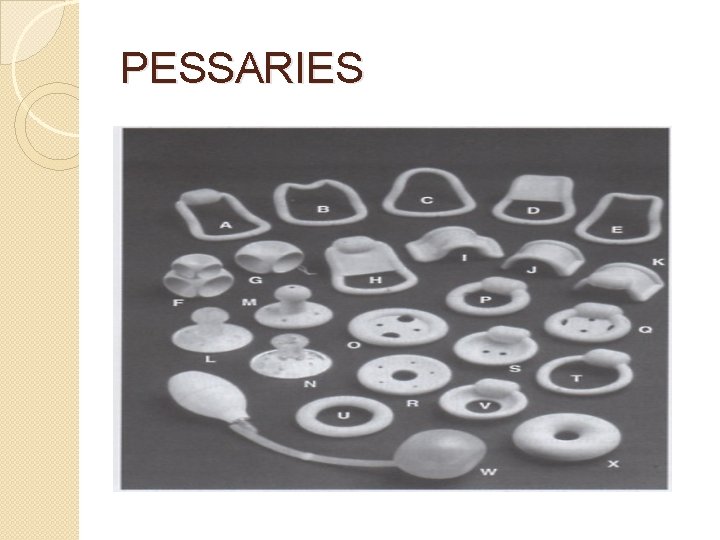
PESSARIES
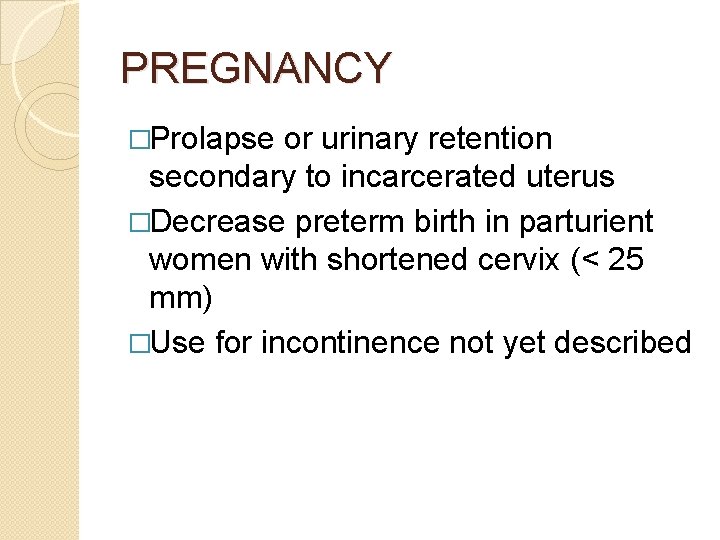
PREGNANCY �Prolapse or urinary retention secondary to incarcerated uterus �Decrease preterm birth in parturient women with shortened cervix (< 25 mm) �Use for incontinence not yet described
PROCEDURES FOR POP �Anterior and posterior colporrhaphy �Mc. Call culdoplasty �Sacrospinous and uterosacral ligament vault suspensions �Abdominal / laparoscopic sacral colpopexy �colpocleisis
GRAFT USE IN PELVIC FLOOR SURGERY �Synthetic polypropylene �Xenografts porcine dermis, porcine small intestine submucosa �Allografts cadaveric
TRANSVAGINAL MESH PROCEDURES �Address specific anatomical defects of the pelvic floor �Maintain durability of repair �Adverse sequelae include mesh erosion, dyspareunia, pelvic pain, mesh shrinkage, de novo stress incontinence