Radiological Category Ultrasound Principal Modality 1 Ultrasound Principal




- Slides: 14
Radiological Category: Ultrasound Principal Modality (1): Ultrasound Principal Modality (2): None Case Report #0448 Submitted by: Gustav A. Blomquist, M. D. Faculty reviewer: Eduardo Matta, M. D. Date accepted: 11 January 2008
Case History 27 -year-old female presents to the ER with 1 week of SOB, constipation, nausea, vomiting and diarrhea. The patient complains of abdominal fullness and diffuse pain, which is greatest in the right lower quadrant. No history of collagen vascular disease, fever or chills. Part of the history is temporarily withheld. An ultrasound is ordered…
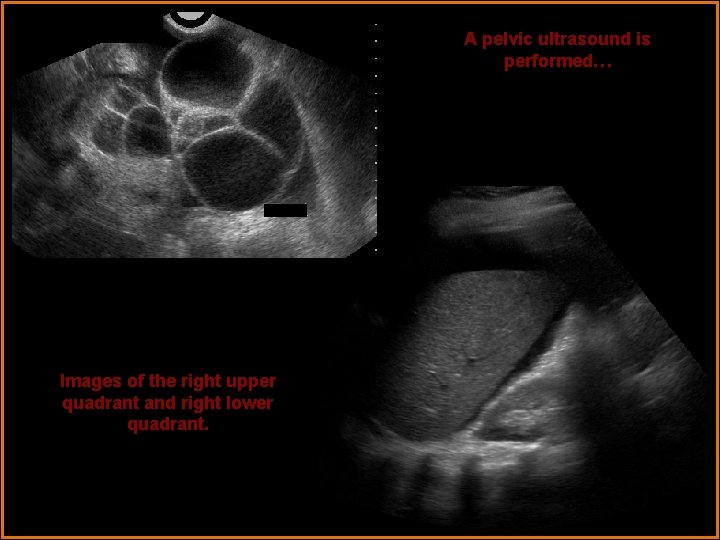
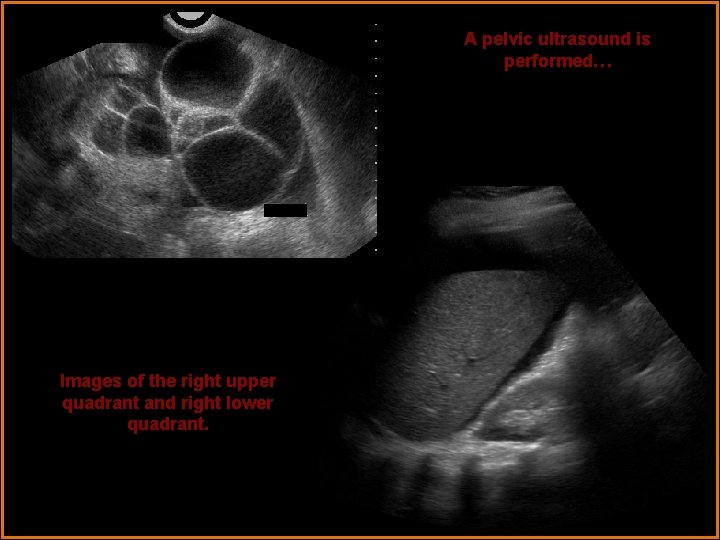
A pelvic ultrasound is performed… Images of the right upper quadrant and right lower quadrant.
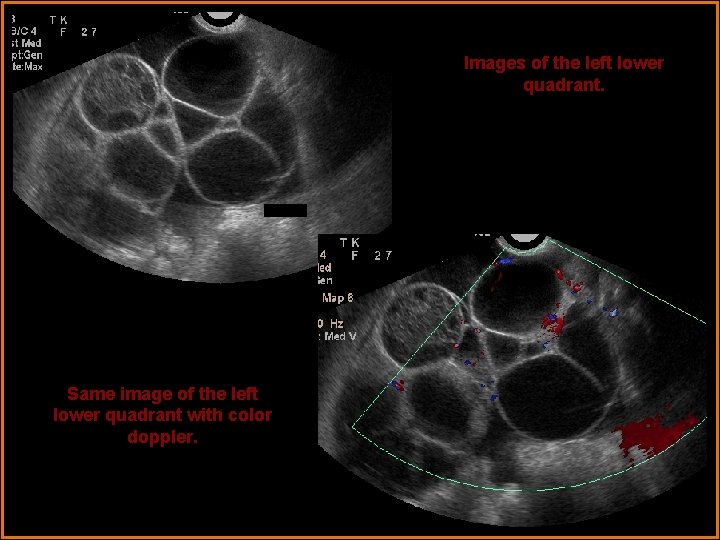
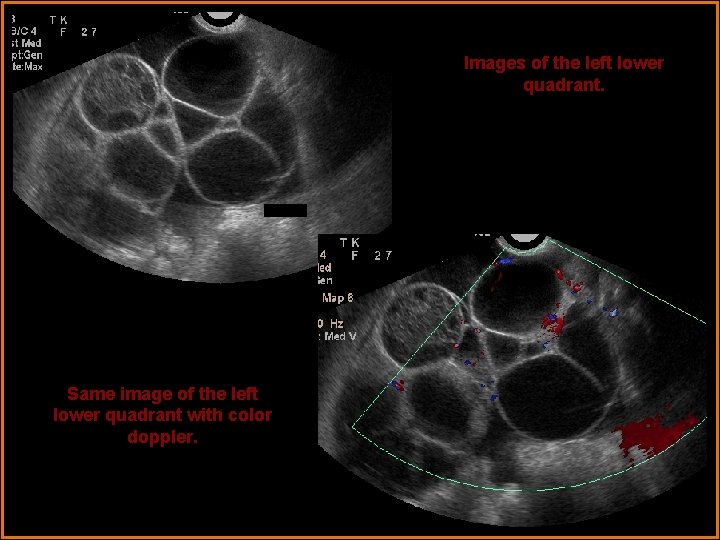
Images of the left lower quadrant. Same image of the left lower quadrant with color doppler.

Images of the uterus
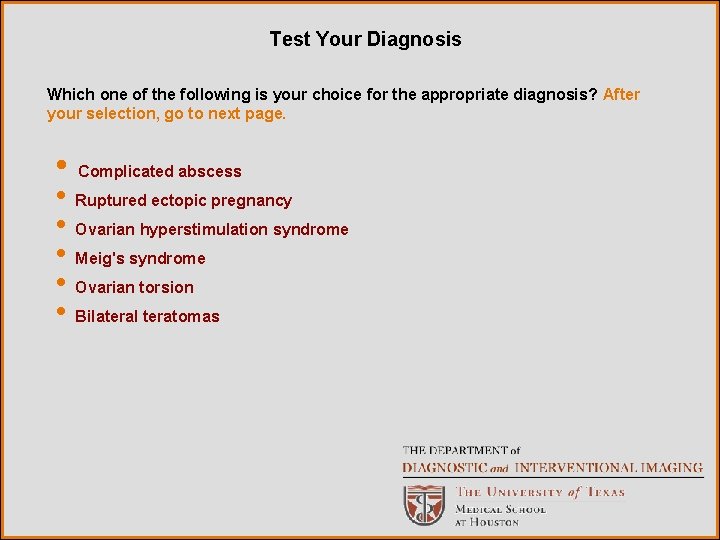
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Complicated abscess • Ruptured ectopic pregnancy • Ovarian hyperstimulation syndrome • Meig's syndrome • Ovarian torsion • Bilateral teratomas
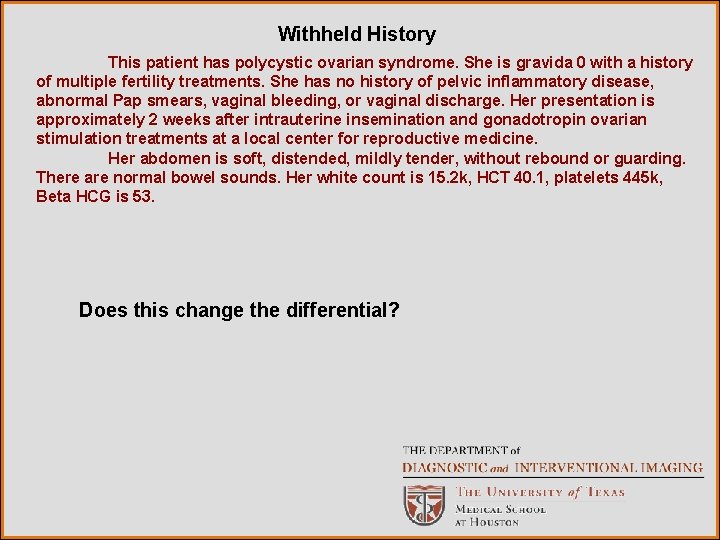
Withheld History This patient has polycystic ovarian syndrome. She is gravida 0 with a history of multiple fertility treatments. She has no history of pelvic inflammatory disease, abnormal Pap smears, vaginal bleeding, or vaginal discharge. Her presentation is approximately 2 weeks after intrauterine insemination and gonadotropin ovarian stimulation treatments at a local center for reproductive medicine. Her abdomen is soft, distended, mildly tender, without rebound or guarding. There are normal bowel sounds. Her white count is 15. 2 k, HCT 40. 1, platelets 445 k, Beta HCG is 53. Does this change the differential?

Here is one more look…

Findings and Differentials Ultrasound Findings: The ovaries are large with multiple enlarged follicles. The ovaries measure 10 to 15 cm each. Ovarian doppler flow was normal bilaterally. The uterus is normal is size with a normal appearing endometrium. Moderate ascites is present within the pelvis and abdomen. Differentials: • Ovarian hyperstimulation syndrome with pregnancy • Ruptured ectopic pregnancy • Complicated abscess with pregnancy
Discussion Ovarian Hyperstimulation Syndrome (OHS) is one of several serious complications of infertility therapy. As in this case, some fertility treatments use exogenous gonadotropins to mature multiple follicles, and h. CG (or a Gn. RH agonist) to trigger ovulation. Clinical symptoms of OHS usually arise 5 to 10 days after administration of the ovulatory trigger. OHS is characterized by ovarian enlargement due to multiple ovarian cysts and fluid shift from the intravascular space. The fluid shift, which can result in hypovolemic shock and electrolyte abnormality, is thought to result from an increase in capillary permeability during maturation and luteinization of multiple follicles. Three grades of OHS can be distinguished by clinical and sonographic criteria: In mild, Grade 1, OHS, the patient may have mild abdominal discomfort and little to no weight gain. The ovaries are enlarged, but less than 5 cm in diameter. In moderate, Grade 2, OHS, the ovaries measure between 5 and 10 cm with weight gain.
Discussion In severe, Grade 3, OHS, the ovaries are greater than 10 cm in diameter and at increased risk for ovarian rupture or torsion. Serum estradiol levels become markedly elevated (> 4000 pg/m. L), and a steep rise in estradiol may be seen. Severe OHS can be complicated by significant loss of fluids due to ascites and pleural effusions(third spacing), which can lead to hemoconcentration, hypotension, oliguria and electrolyte imbalances. The marked hemoconcentration may lead to thromboembolic phenomena and DIC. Other complications include liver and kidney dysfunction, acute respiratory distress syndrome, and death. MRI is useful when the ovaries become very large. Gadolinium enhances the ovarian parenchyma, which is not replaced by cysts. In the absence of pregnancy, the syndrome resolves in 3 – 7 days. In the pregnant patient, the syndrome resolves slowly over a period of 6 – 8 weeks. Treatment is predominantly supportive and is aimed at maintaining hemodynamic stability and minimizing electrolyte imbalances. Transabdominal or transvaginal ultrasoundguided paracentesis has been shown to be an effective treatment. Mild forms can be managed on an outpatient basis, while severe OHS requires hospitalization and even monitoring in the intensive care unit.
Discussion Risk factors include young thin women, a previous history of OHS, women with the "necklace sign" of multiple peripheral follicles in the ovary, or polycystic ovary disease. Luteinization is an integral contributor to the development of OHS, therefore the administration of human chorionic gonadotropin increases the risk. Spontaneous OHS can also occur when there is supraphysiologic production of h. CG, such as in molar pregnancies or multiple gestations. Ultrasound may play a role in identifying patients at risk for OHS prior to induction, and in evaluating patients when the condition is suspected. Ultrasound findings suggesting an increased risk include multiple peripheral ovarian follicles, a polycystic ovarian morphology, and the presence of more than four follicles measuring greater than 15 mm. Patients with OHS, sonographically, have numerous large thin-walled ovarian cysts are seen, peripherally placed and replacing most of the ovary. Free intraperitoneal fluid and pleural effusions are readily imaged. Ultrasound guided paracentesis or thoracentesis has been used for symptom relief.
Diagnosis • Ovarian hyperstimulation syndrome • Early pregnancy The patient was admitted to the gynecology service for ovarian hyperstimulation syndrome and early pregnancy. This patient’s course was complicated by initial enlargement of the ovaries. She did not develop a right sided pleural effusion. Her nausea, vomiting and constipation were treated symptomatically. TED hose and sequential compression devices were applied for DVT prophylaxis. Her initial beta HCG of 53 proceeded to double appropriately, and on the day of discharge the beta HCG was 546.

Bibliography 1. ACR Case in Point 2. Aunt Minnie. com 3. Beerendonk C, et al. Ovarian hyperstimulation syndrome: facts and fallacies. Obstetrical and Gynecological Survey. 1998; 53: 439449. 4. Callen PW. Ultrasonography in obstetrics and gynecology. Philadelphia: Saunders, 1994. 6. Man A, et al. Pleural effusion as a presenting symptom of ovarian hyperstimulation syndrome. European Respiration Journal. 1997; 10: 2425 -2426. 5. Kaiser U. The pathogenesis of the ovarian hyperstimulation syndrome. NEJM 2003; 349: 729 -732. 6. Johnson PT, Kurtz, AB. Case Review, Obstetric and gynecologic ultrasound. Mosby 2001: 157 -158. 7. Roden S, et al. An uncommon etiology of isolated pleural effusion: the ovarian hyperstimulation syndrome. Chest. 2000; 118: 256 -258. 8. www. uptodate. com
 Ferriman–gallwey score
Ferriman–gallwey score Erate category 2 eligible equipment
Erate category 2 eligible equipment National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health Stefan savi
Stefan savi Exteroceptors
Exteroceptors Modality in software engineering
Modality in software engineering Epistemic modality
Epistemic modality Modality in software engineering
Modality in software engineering Cardinality and modality
Cardinality and modality Lexical vs auxiliary verbs
Lexical vs auxiliary verbs Modality microsoft services
Modality microsoft services Low modality examples
Low modality examples