Treatment in Recurrent Cervical Cancer Surgery Pelvic exenteration


- Slides: 37
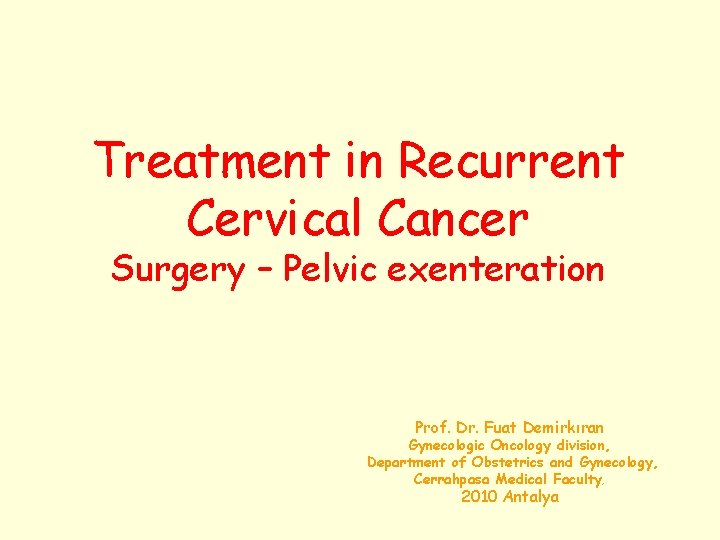
Treatment in Recurrent Cervical Cancer Surgery – Pelvic exenteration Prof. Dr. Fuat Demirkıran Gynecologic Oncology division, Department of Obstetrics and Gynecology, Cerrahpasa Medical Faculty, 2010 Antalya
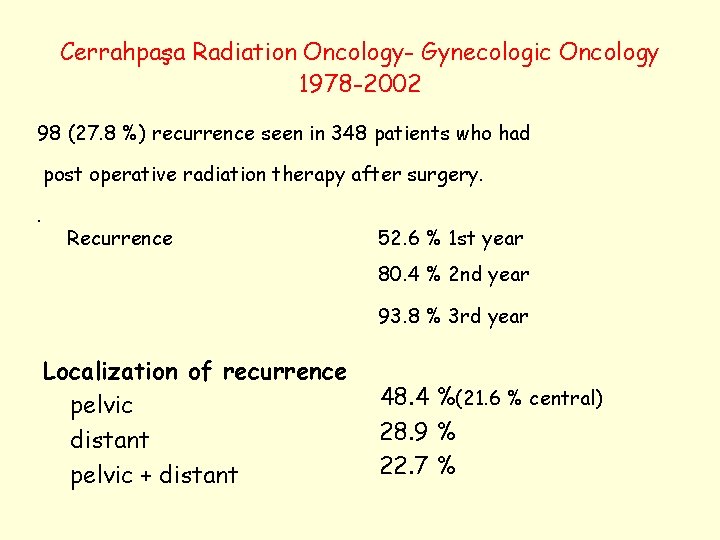
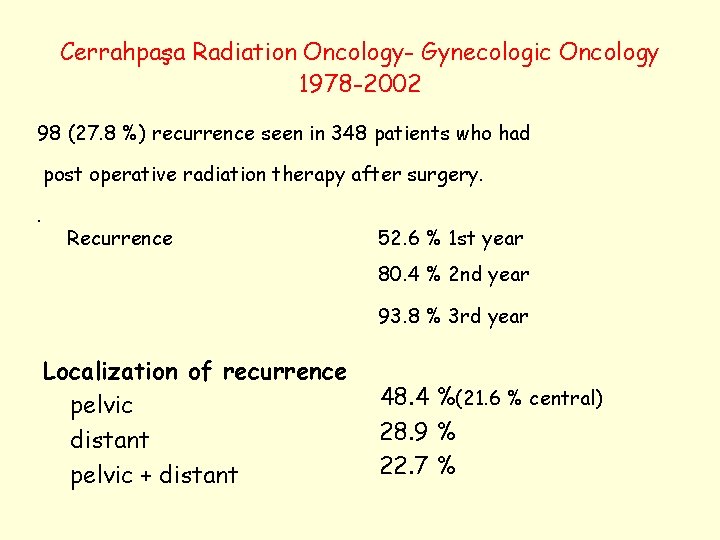
Cerrahpaşa Radiation Oncology- Gynecologic Oncology 1978 -2002 98 (27. 8 %) recurrence seen in 348 patients who had post operative radiation therapy after surgery. . Recurrence 52. 6 % 1 st year 80. 4 % 2 nd year 93. 8 % 3 rd year Localization of recurrence pelvic distant pelvic + distant 48. 4 %(21. 6 % central) 28. 9 % 22. 7 %
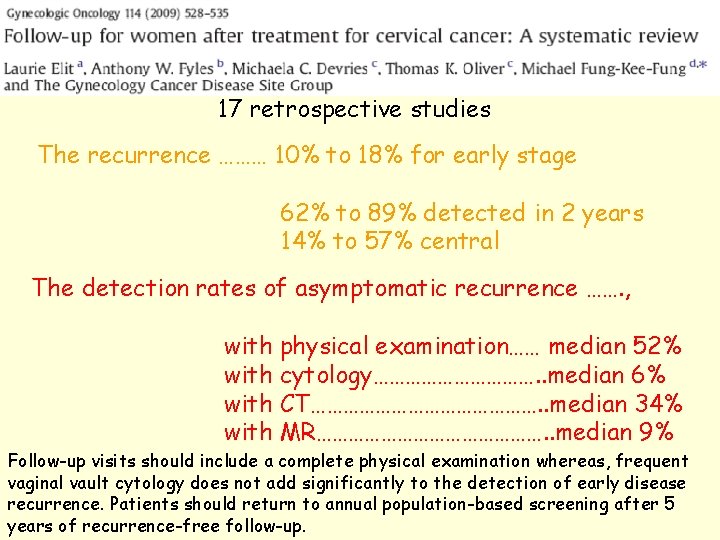
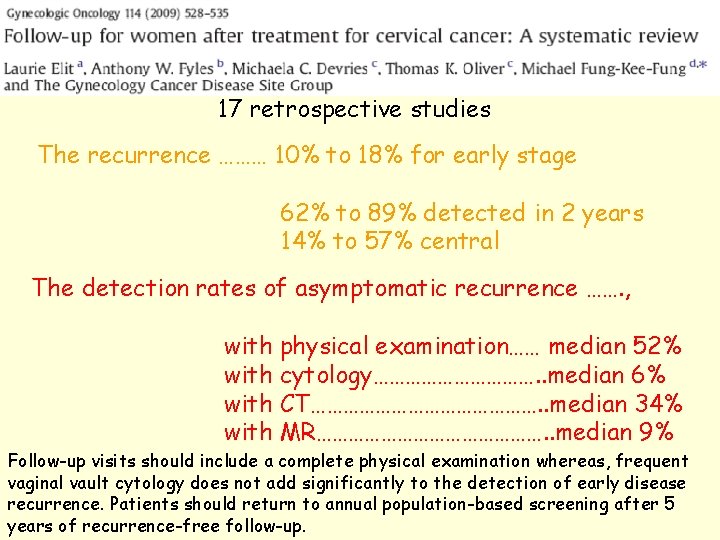
17 retrospective studies The recurrence ……… 10% to 18% for early stage 62% to 89% detected in 2 years 14% to 57% central The detection rates of asymptomatic recurrence ……. , with physical examination…… median 52% with cytology……………. . median 6% with CT…………………. . median 34% with MR…………………. . median 9% Follow-up visits should include a complete physical examination whereas, frequent vaginal vault cytology does not add significantly to the detection of early disease recurrence. Patients should return to annual population-based screening after 5 years of recurrence-free follow-up.
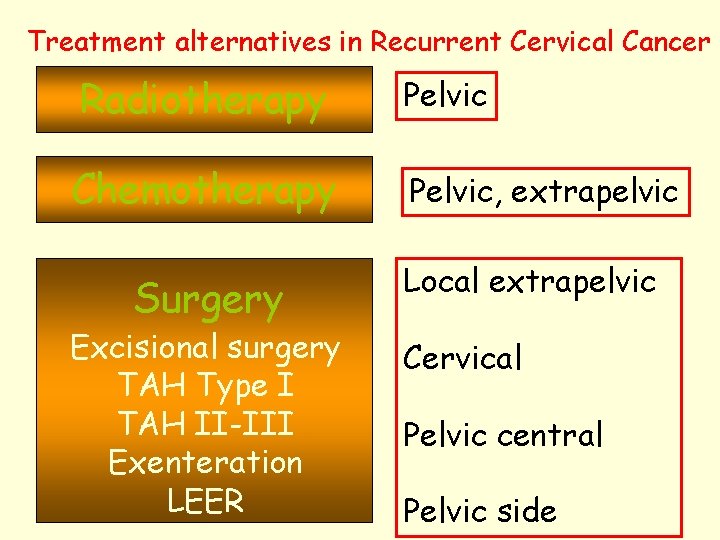
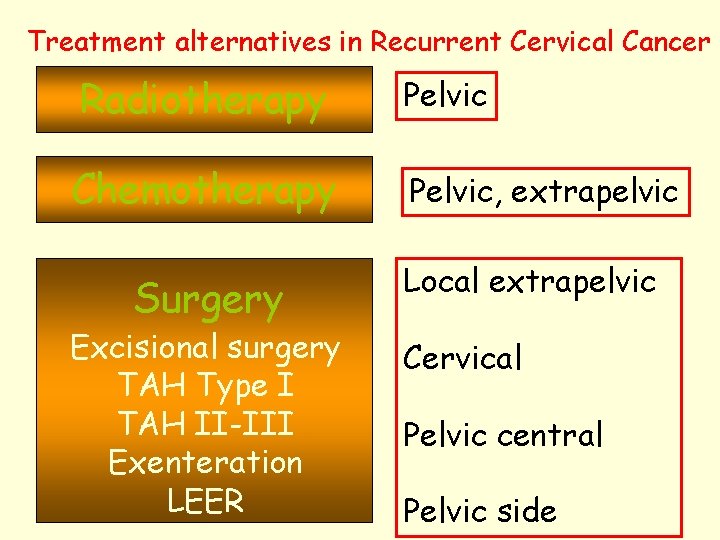
Treatment alternatives in Recurrent Cervical Cancer Radiotherapy Chemotherapy Surgery Excisional surgery TAH Type I TAH II-III Exenteration LEER Pelvic, extrapelvic Local extrapelvic Cervical Pelvic central Pelvic side
Excisional Surgery
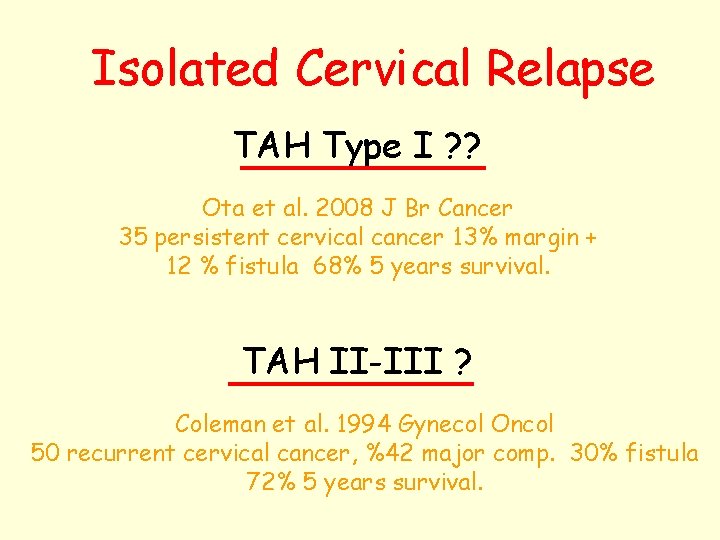
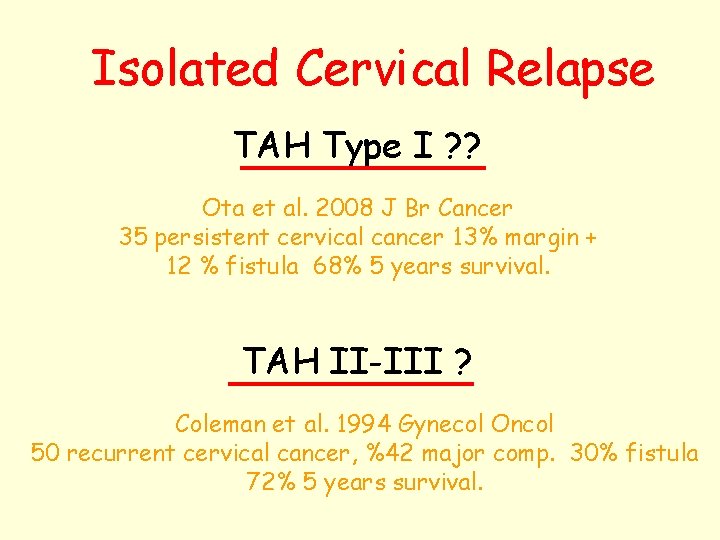
Isolated Cervical Relapse TAH Type I ? ? Ota et al. 2008 J Br Cancer 35 persistent cervical cancer 13% margin + 12 % fistula 68% 5 years survival. TAH II-III ? Coleman et al. 1994 Gynecol Oncol 50 recurrent cervical cancer, %42 major comp. 30% fistula 72% 5 years survival.
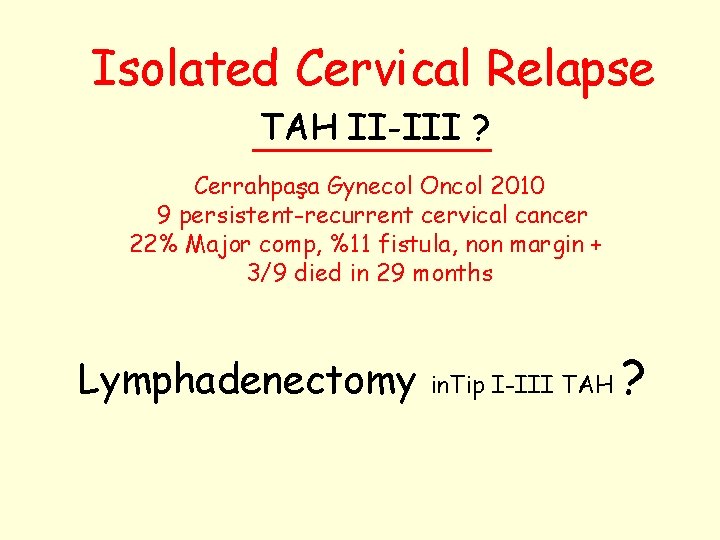
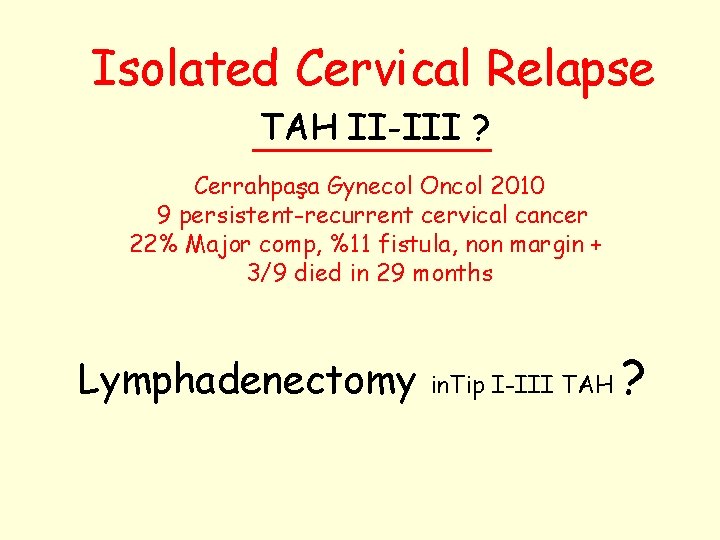
Isolated Cervical Relapse TAH II-III ? Cerrahpaşa Gynecol Oncol 2010 9 persistent-recurrent cervical cancer 22% Major comp, %11 fistula, non margin + 3/9 died in 29 months Lymphadenectomy in. Tip I-III TAH ?
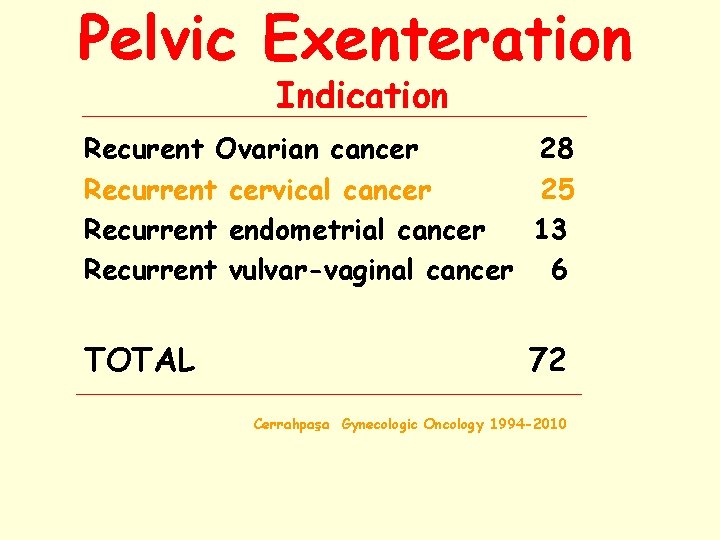
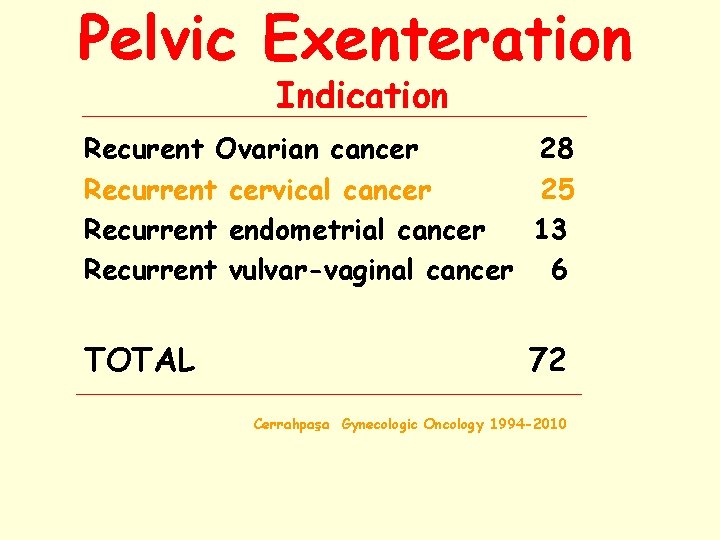
Pelvic Exenteration Indication Recurent Ovarian cancer 28 Recurrent cervical cancer 25 Recurrent endometrial cancer 13 Recurrent vulvar-vaginal cancer 6 TOTAL 72 Cerrahpaşa Gynecologic Oncology 1994 -2010
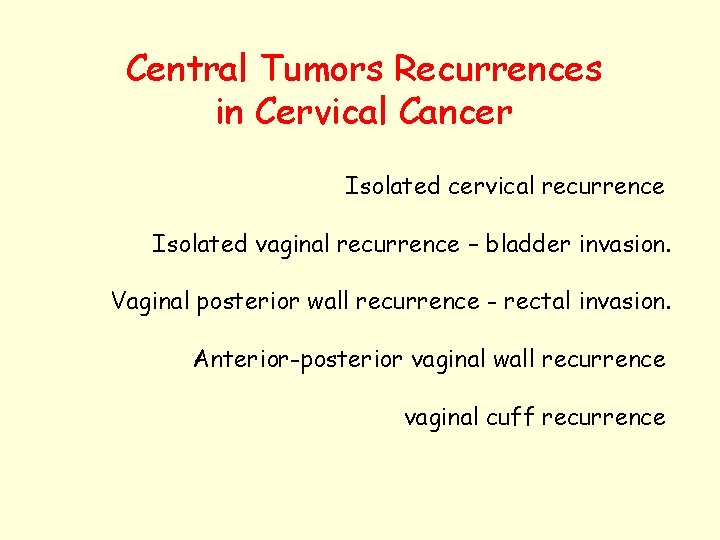
Central Tumors Recurrences in Cervical Cancer Isolated cervical recurrence Isolated vaginal recurrence – bladder invasion. Vaginal posterior wall recurrence - rectal invasion. Anterior-posterior vaginal wall recurrence vaginal cuff recurrence
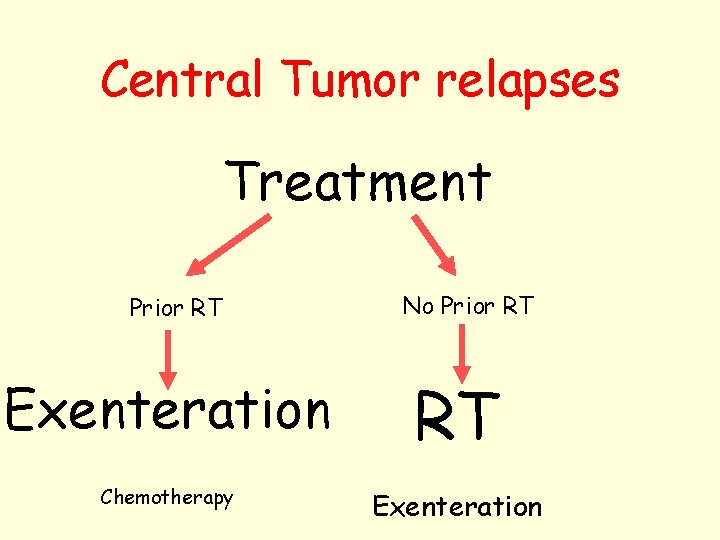
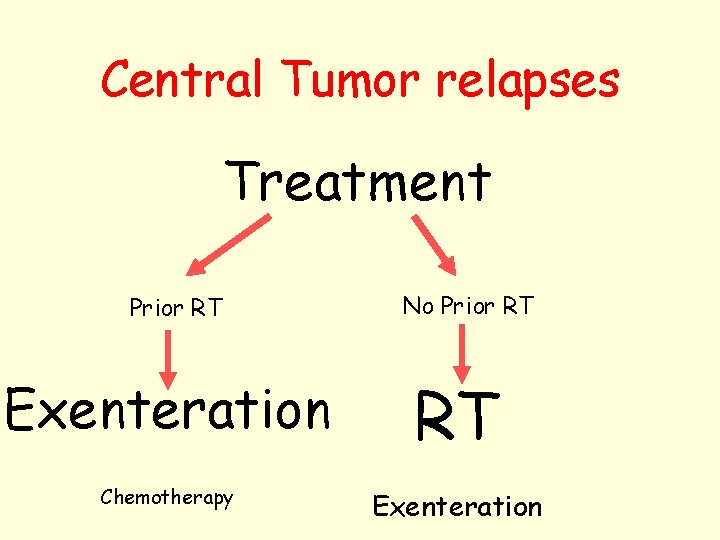
Central Tumor relapses Treatment Prior RT No Prior RT Exenteration RT Chemotherapy Exenteration
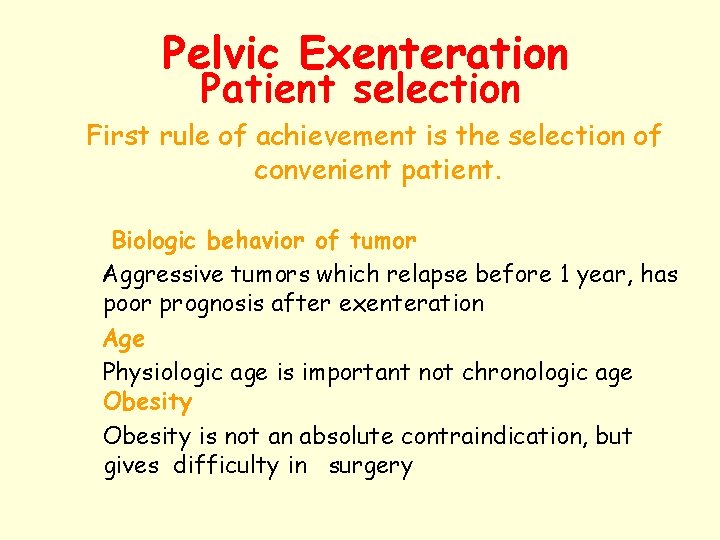
Pelvic Exenteration Patient selection First rule of achievement is the selection of convenient patient. Biologic behavior of tumor Aggressive tumors which relapse before 1 year, has poor prognosis after exenteration Age Physiologic age is important not chronologic age Obesity is not an absolute contraindication, but gives difficulty in surgery
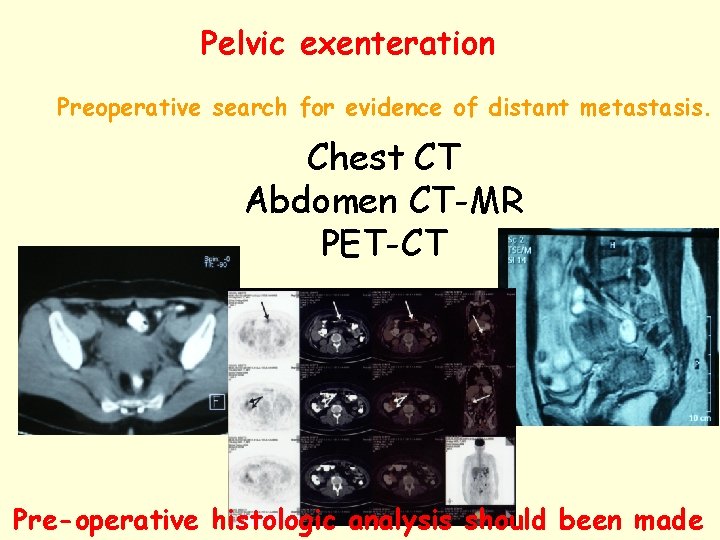
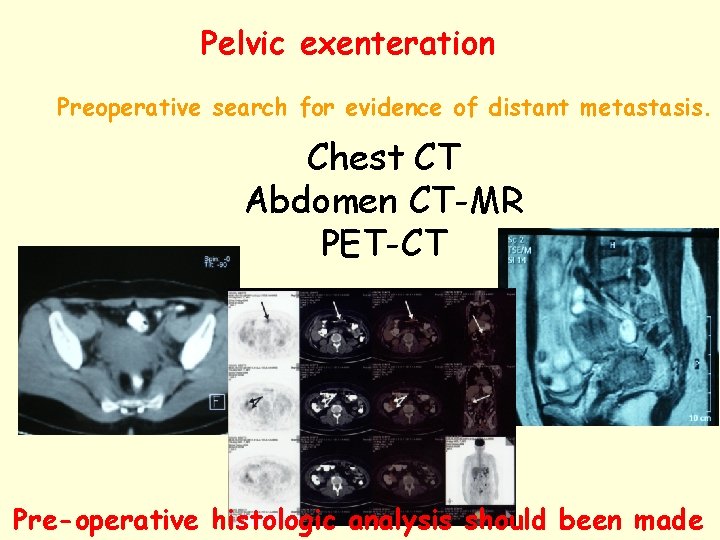
Pelvic exenteration Preoperative search for evidence of distant metastasis. Chest CT Abdomen CT-MR PET-CT Pre-operative histologic analysis should been made
Pelvic Exenteration Patient selection There will be a psychological devastation if patient found to be inoperable during operation because of introabdominal metastasis or non operable condition arise So, Fine needle aspiration biopsy should made in suspicious lesions. Pelvic, paraaortic lymph node and pelvic wall invasions should carefully evaluated. Despite all of these, surgery can’t be made in 25 -30 % of patients
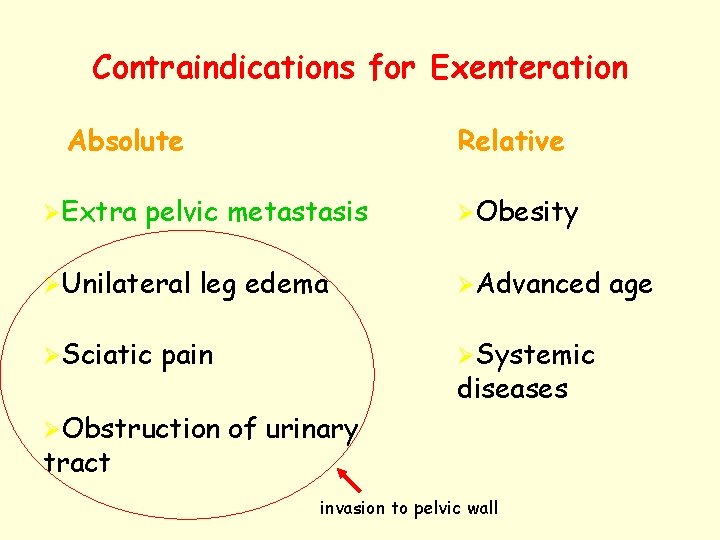
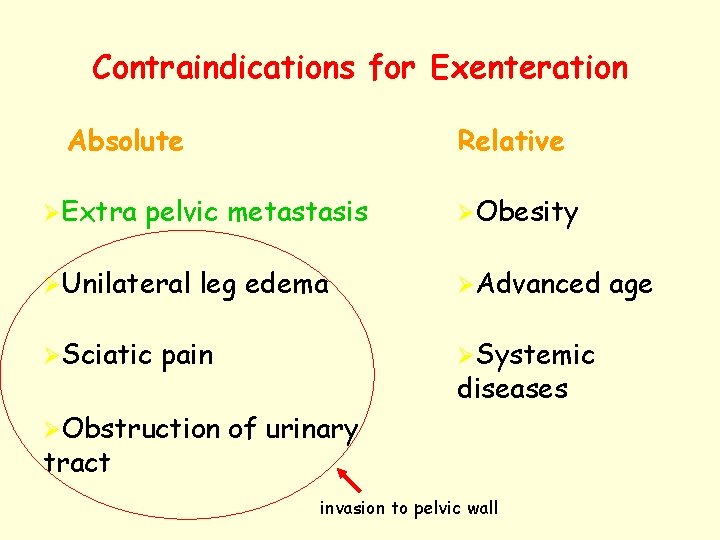
Contraindications for Exenteration Absolute ØExtra Relative pelvic metastasis ØUnilateral ØSciatic leg edema pain ØObstruction tract ØObesity ØAdvanced ØSystemic diseases of urinary invasion to pelvic wall age
Even if everything is OK Patient and her relatives should be informed about surgical morbidity, mortality type of exenteration changing decisions at the operation possibility of inoperability stoma treatment alternatives success rate
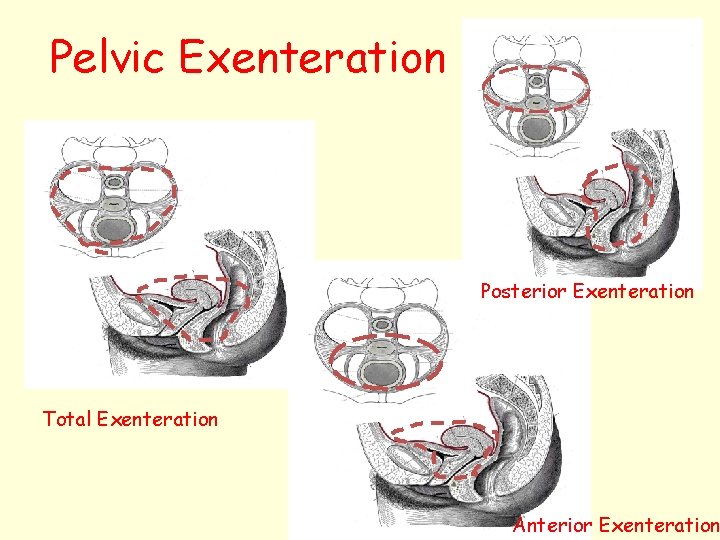
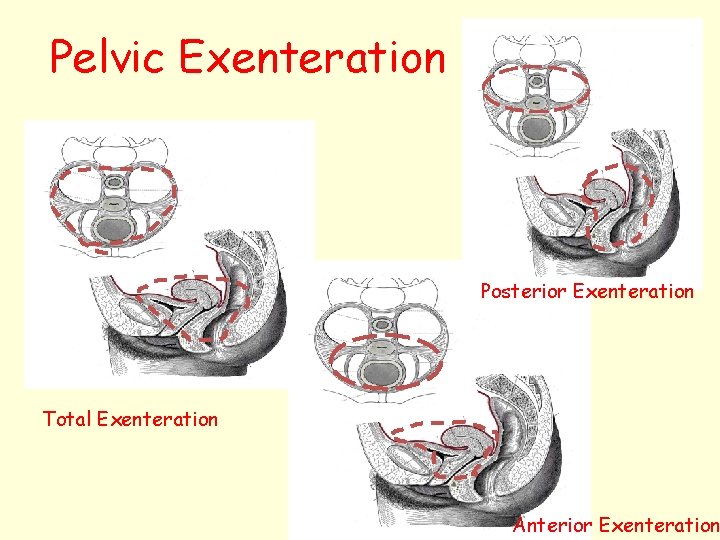
Pelvic Exenteration Posterior Exenteration Total Exenteration Anterior Exenteration
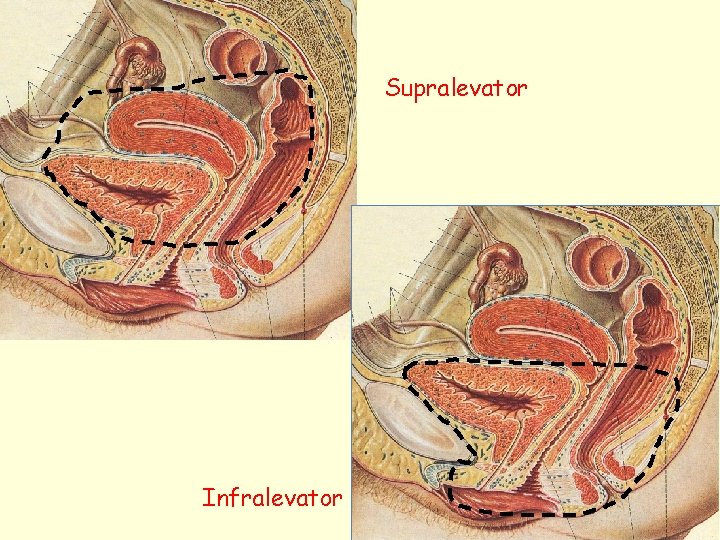
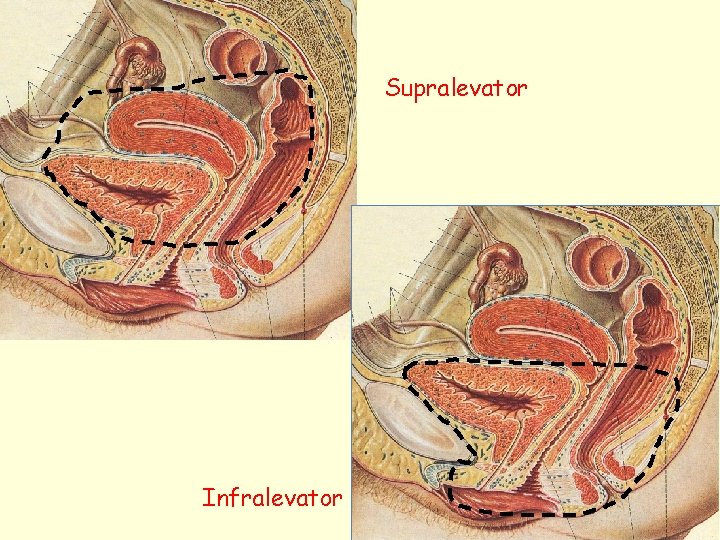
Supralevator Infralevator
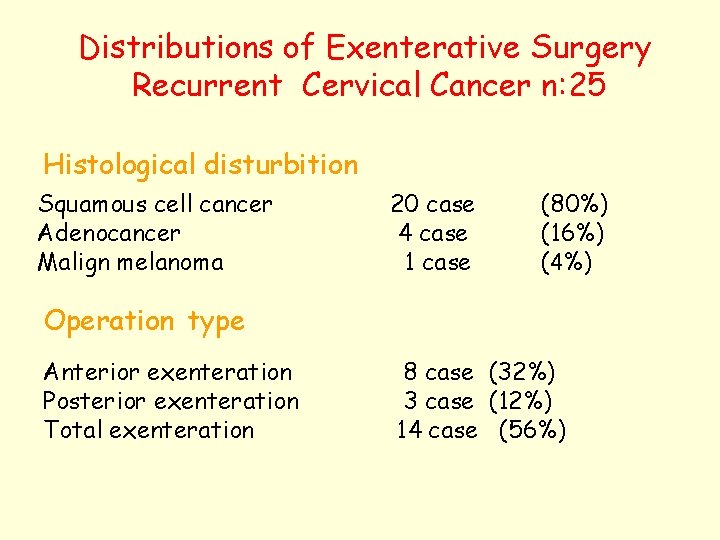
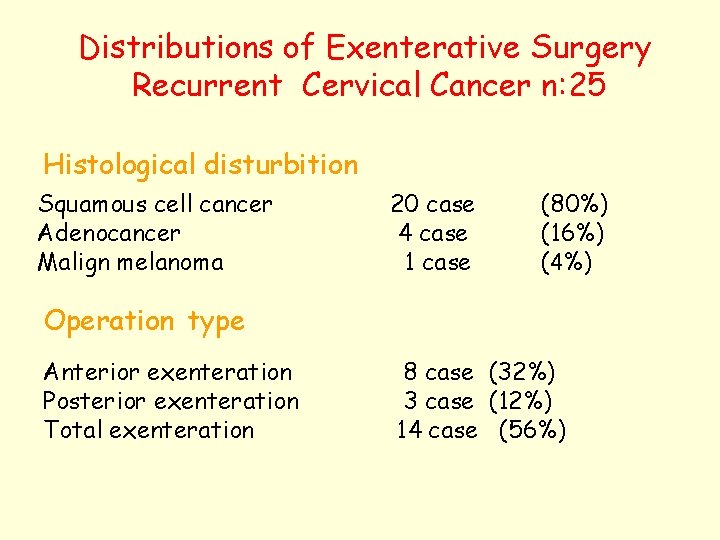
Distributions of Exenterative Surgery Recurrent Cervical Cancer n: 25 Histological disturbition Squamous cell cancer Adenocancer Malign melanoma 20 case 4 case 1 case (80%) (16%) (4%) Operation type Anterior exenteration Posterior exenteration Total exenteration 8 case (32%) 3 case (12%) 14 case (56%)
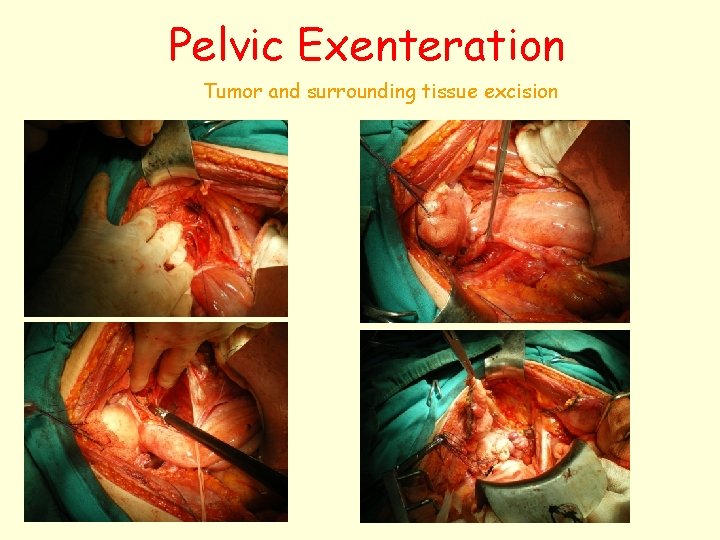
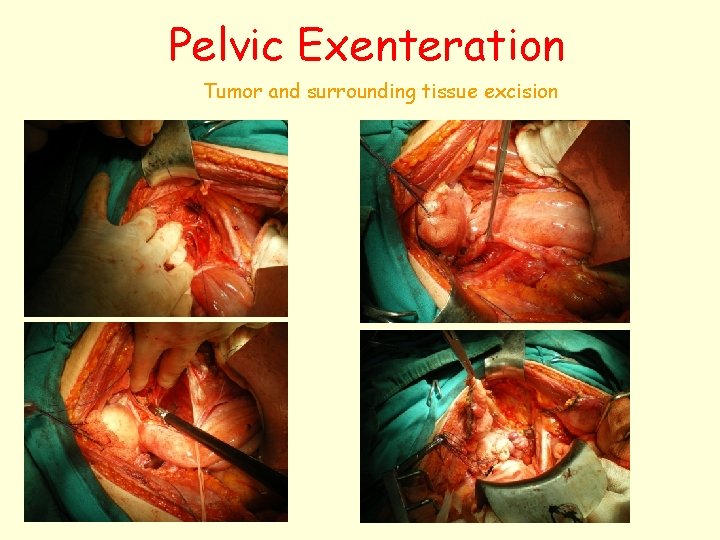
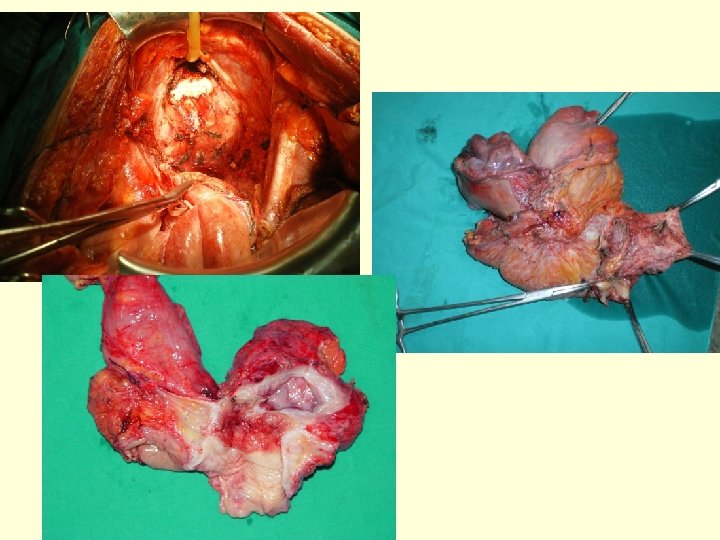
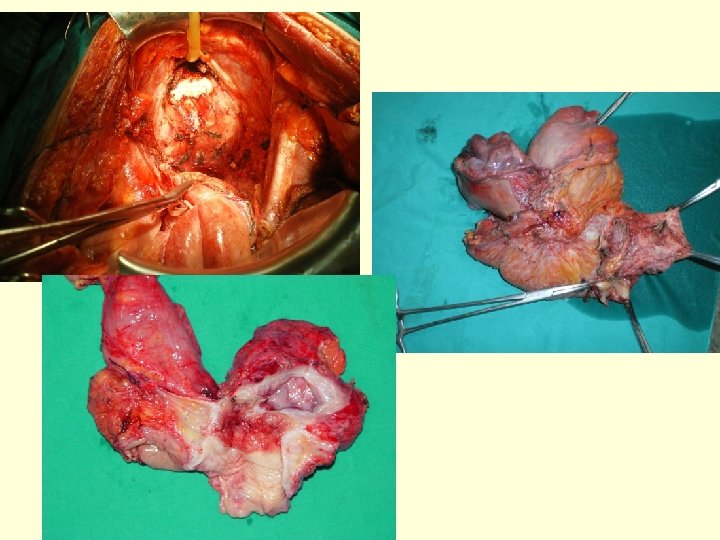
Pelvic Exenteration Tumor and surrounding tissue excision
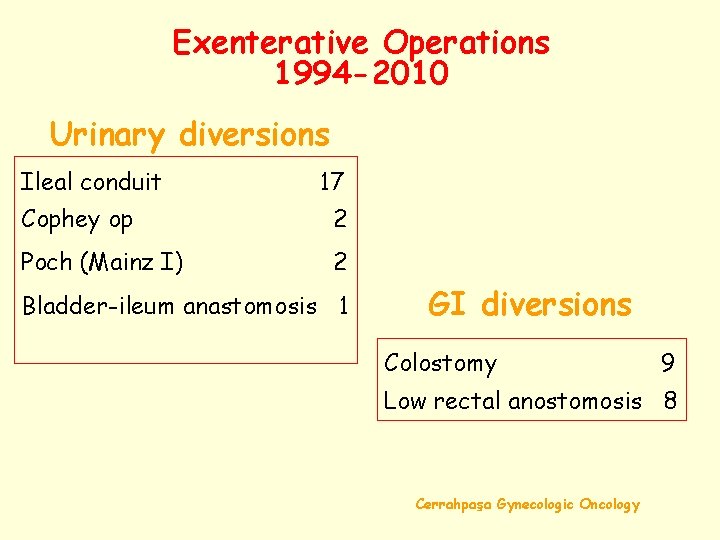
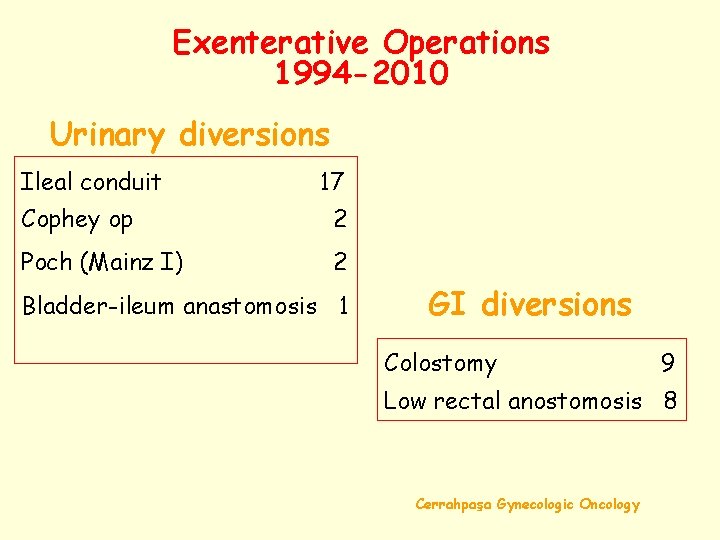
Exenterative Operations 1994 -2010 Urinary diversions Ileal conduit 17 Cophey op 2 Poch (Mainz I) 2 Bladder-ileum anastomosis 1 GI diversions Colostomy 9 Low rectal anostomosis 8 Cerrahpaşa Gynecologic Oncology
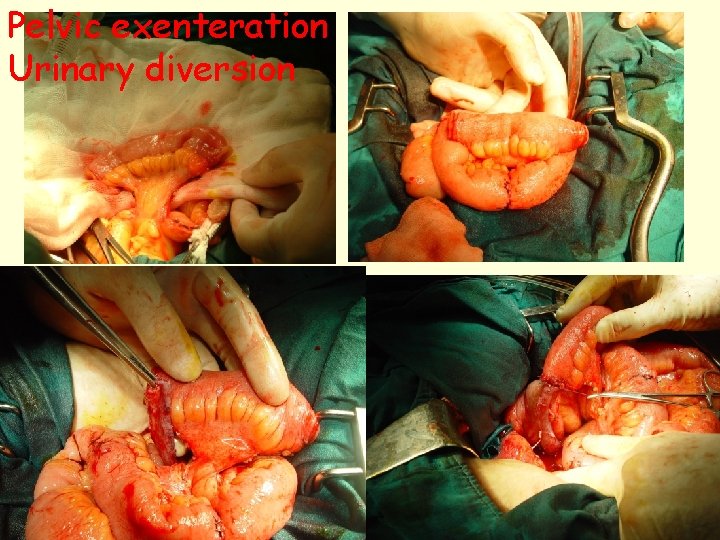
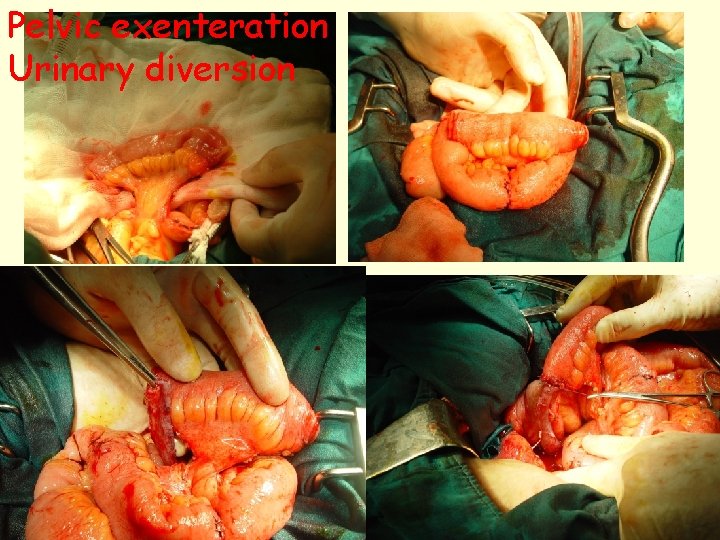
Pelvic exenteration Urinary diversion

Pelvic Exenteration GI diversion
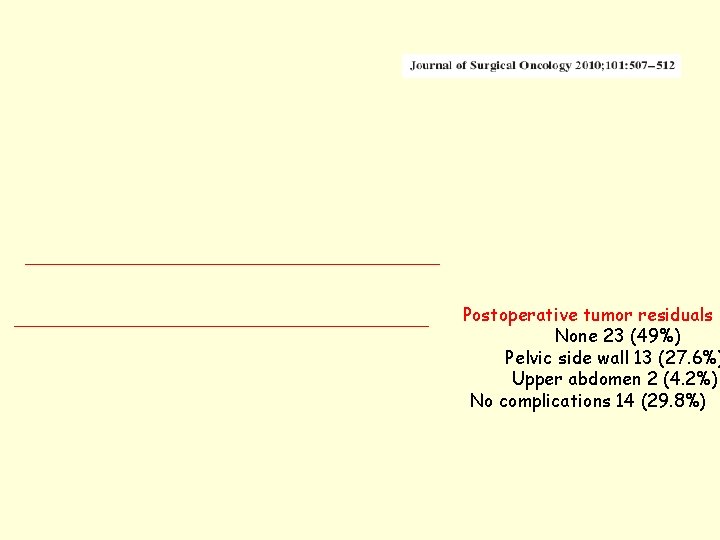
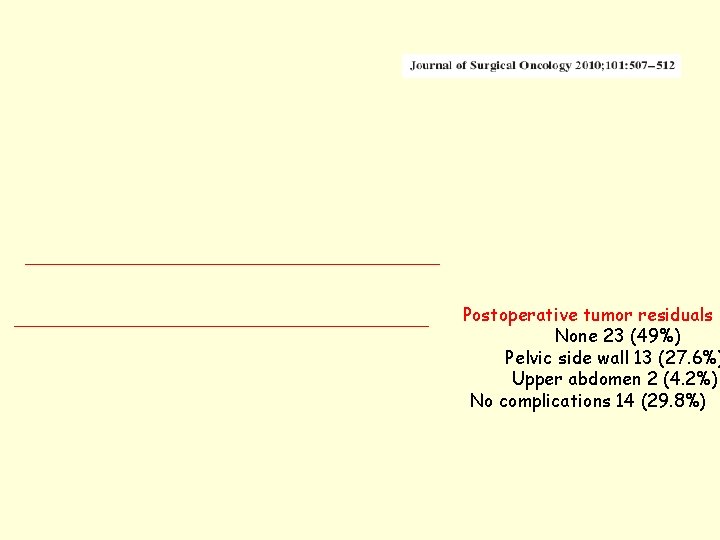
Postoperative tumor residuals None 23 (49%) Pelvic side wall 13 (27. 6%) Upper abdomen 2 (4. 2%) No complications 14 (29. 8%)

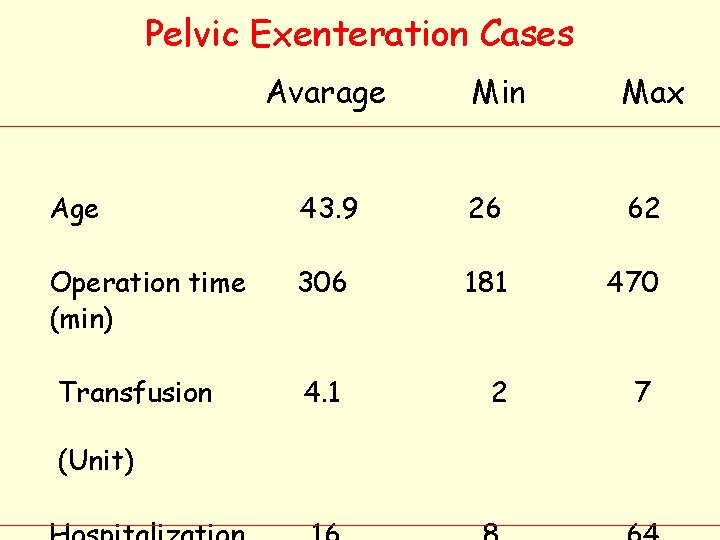
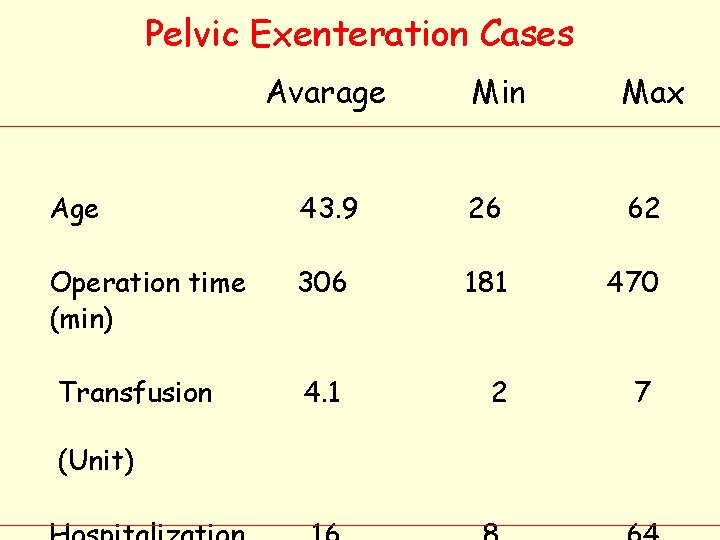
Pelvic Exenteration Cases Avarage Min Max Age 43. 9 26 62 Operation time (min) 306 181 470 4. 1 2 7 Transfusion (Unit)
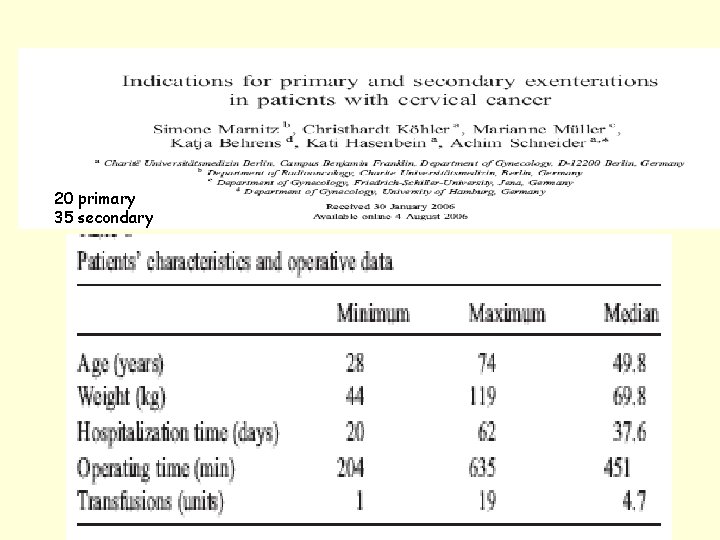
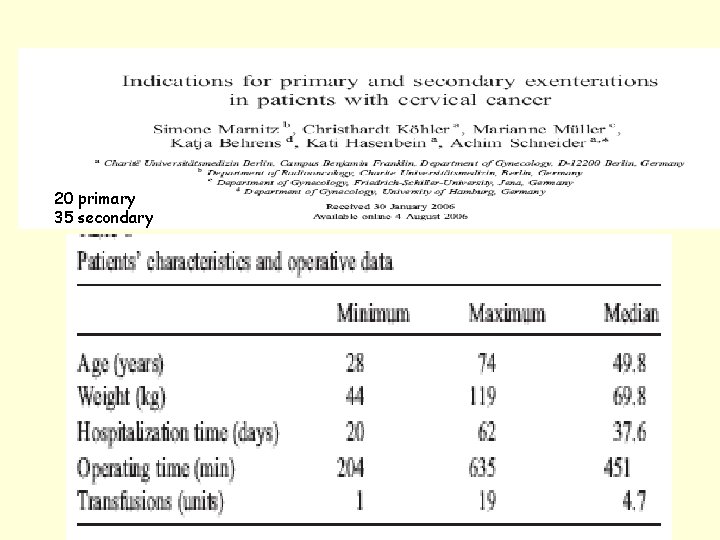
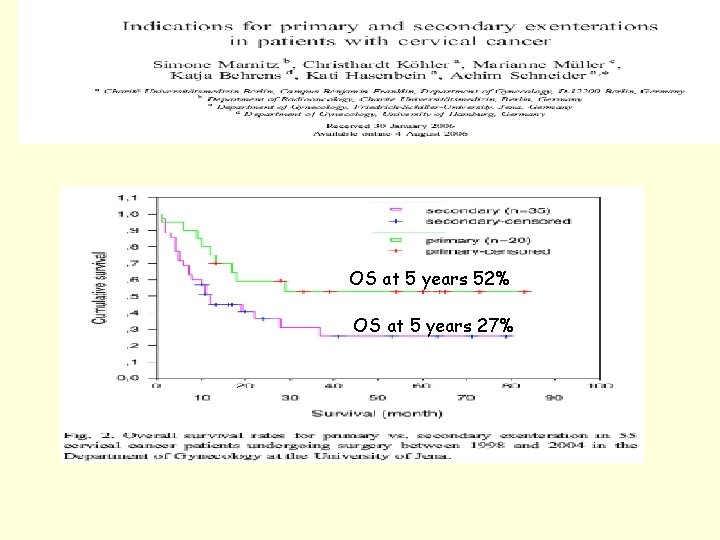
20 primary 35 secondary
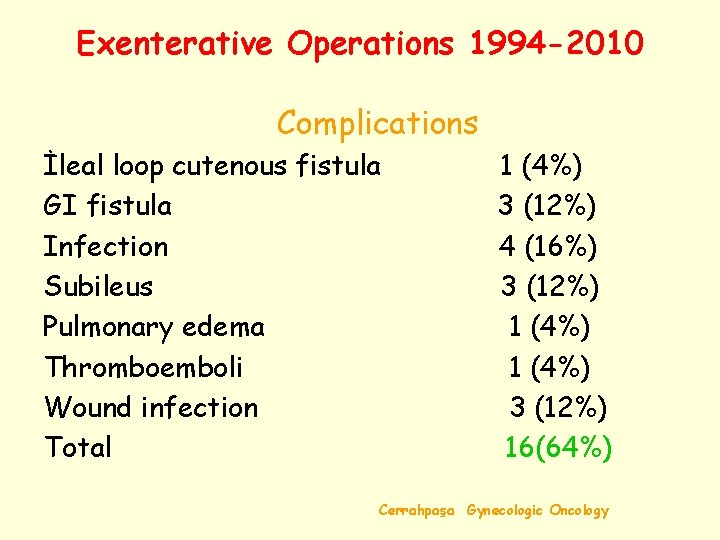
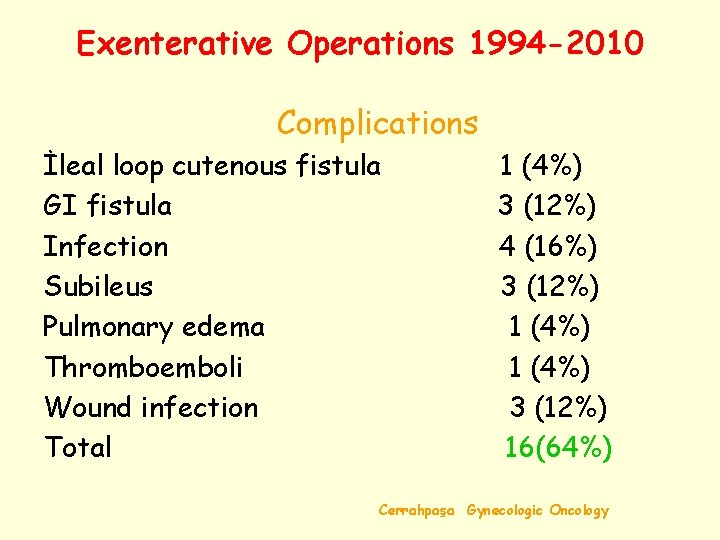
Exenterative Operations 1994 -2010 Complications İleal loop cutenous fistula GI fistula Infection Subileus Pulmonary edema Thromboemboli Wound infection Total 1 (4%) 3 (12%) 4 (16%) 3 (12%) 1 (4%) 3 (12%) 16(64%) Cerrahpaşa Gynecologic Oncology
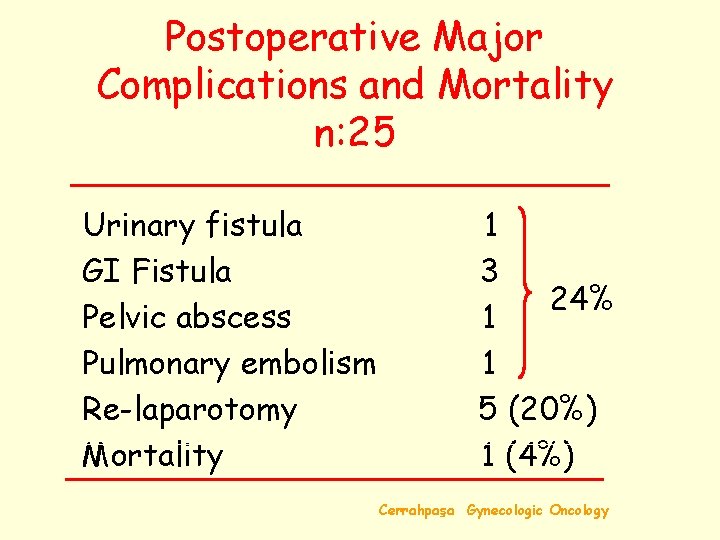
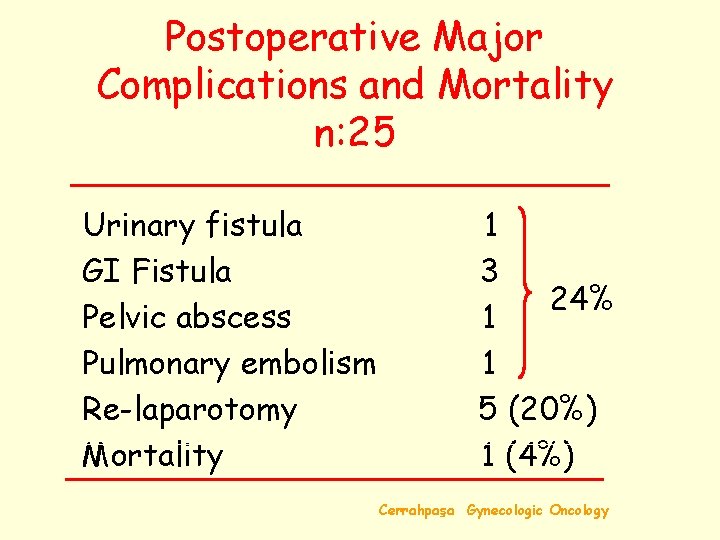
Postoperative Major Complications and Mortality n: 25 Urinary fistula GI Fistula Pelvic abscess Pulmonary embolism Re-laparotomy Mortality 1 3 24% 1 1 5 (20%) 1 (4%) Cerrahpaşa Gynecologic Oncology
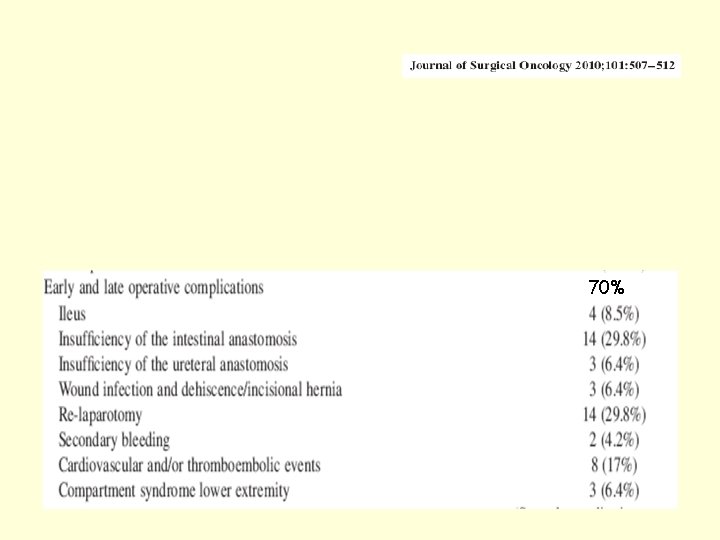
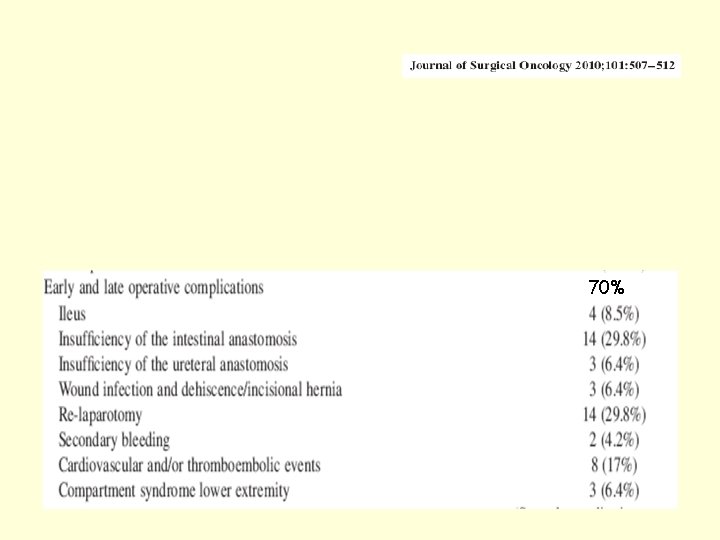
70%
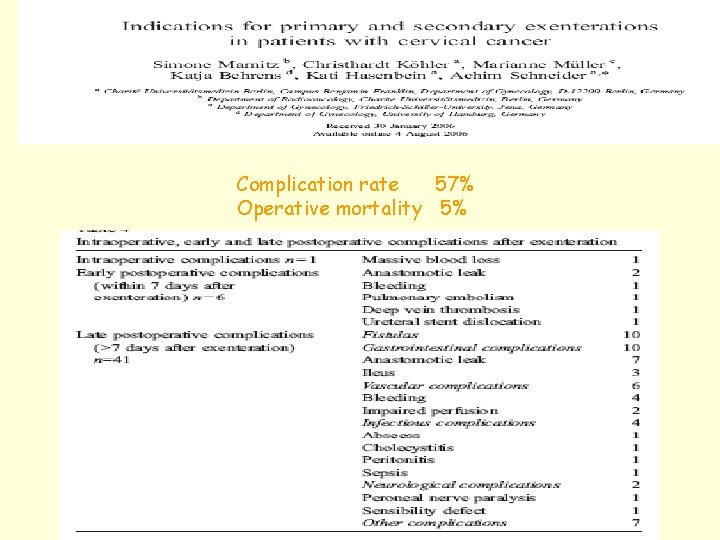
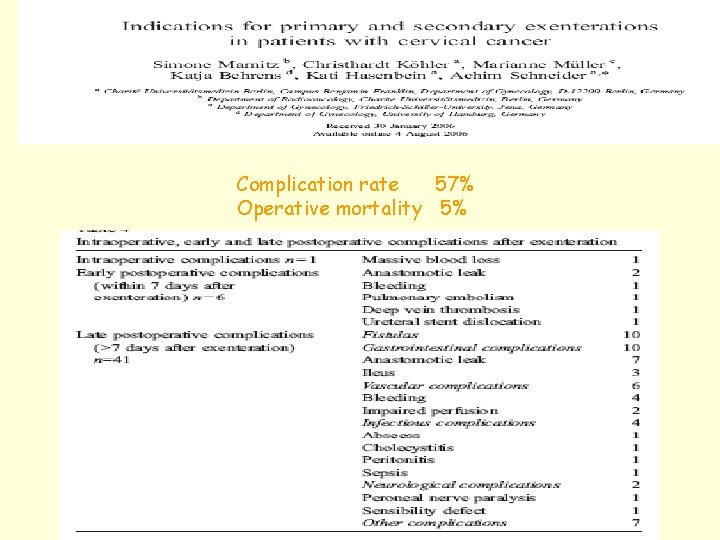
Complication rate 57% Operative mortality 5%
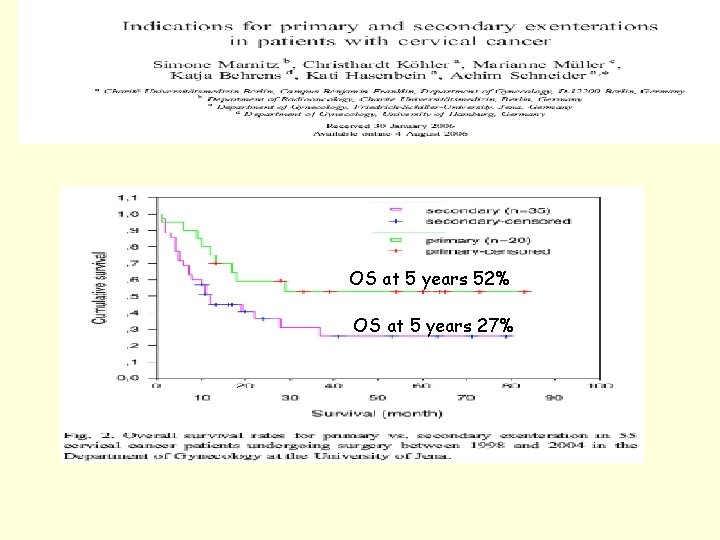
OS at 5 years 52% OS at 5 years 27%
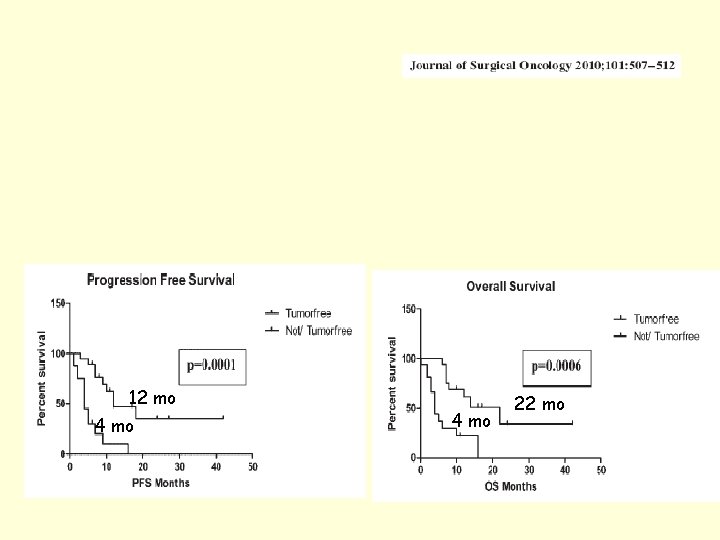
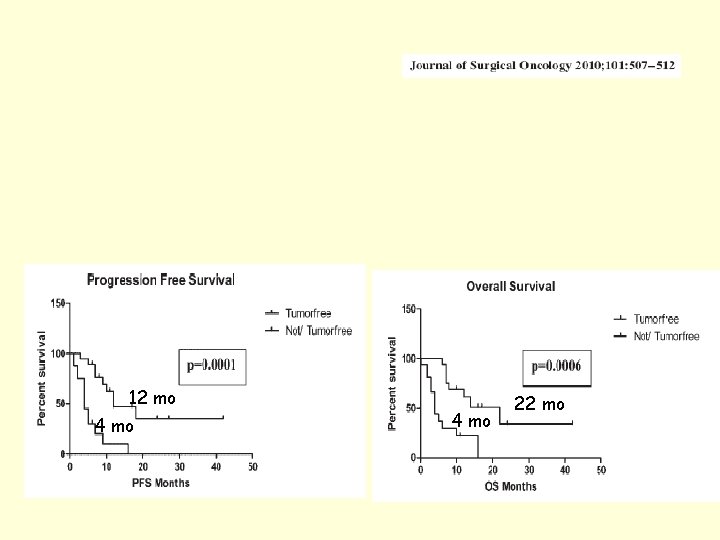
12 mo 4 mo 22 mo
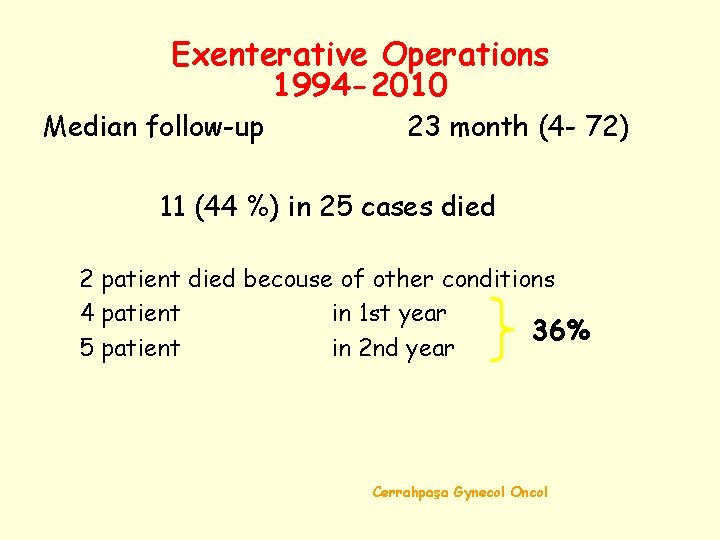
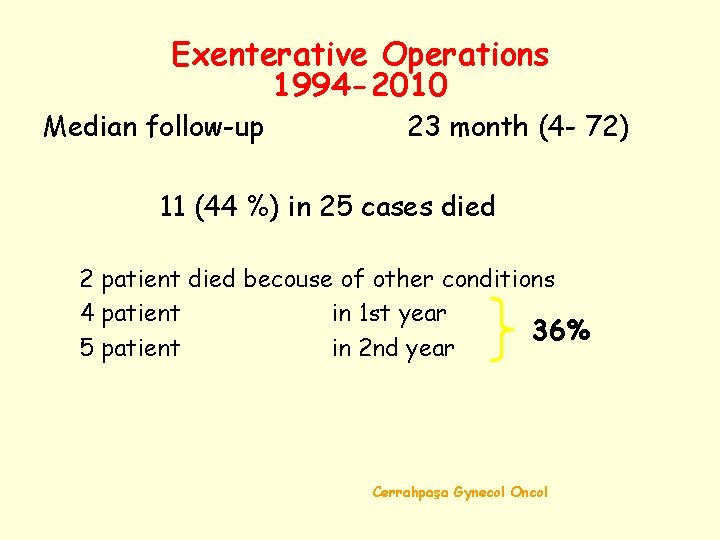
Exenterative Operations 1994 -2010 Median follow-up 23 month (4 - 72) 11 (44 %) in 25 cases died 2 patient died becouse of other conditions 4 patient in 1 st year 36% 5 patient in 2 nd year Cerrahpaşa Gynecol Oncol
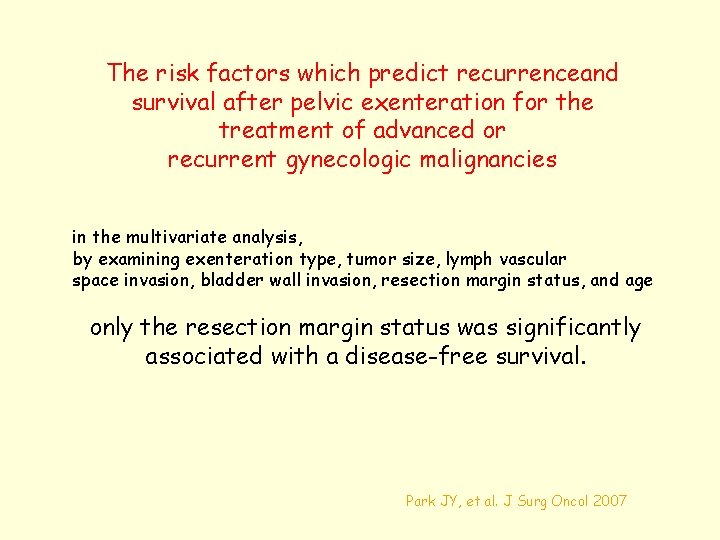
The risk factors which predict recurrenceand survival after pelvic exenteration for the treatment of advanced or recurrent gynecologic malignancies in the multivariate analysis, by examining exenteration type, tumor size, lymph vascular space invasion, bladder wall invasion, resection margin status, and age only the resection margin status was significantly associated with a disease-free survival. Park JY, et al. J Surg Oncol 2007
Conclusions Surgical therapy due to recurrent cervical cancer may be associated with a high morbidity. But complete tumor resection is associated with a significantly higher overall and PFS.