Respiratory Infections Caroline Kowal Preceptor Dr Rhonda Ness













- Slides: 79
Respiratory Infections Caroline Kowal Preceptor: Dr. Rhonda Ness Core Rounds Dec 11, 2003


Objectives n Alberta Clinical Practice Guidelines Community Acquired Pneumonia Adult/Child n Nursing home acquired Pneumonia n n n Immunocompromised Alcoholics
n n Guidelines not prospectively validated Prior studies of pneumonia guidelines have reported: decreased lengths of stay, admission rates, and costs n no change in clinical outcomes. n
Definitions n Community Acquired Pneumonia (CAP) – Pneumonia in pt not hospitalized last 14 d, OR hospitalized <4 d prior to onset sx Adult - >16 y age
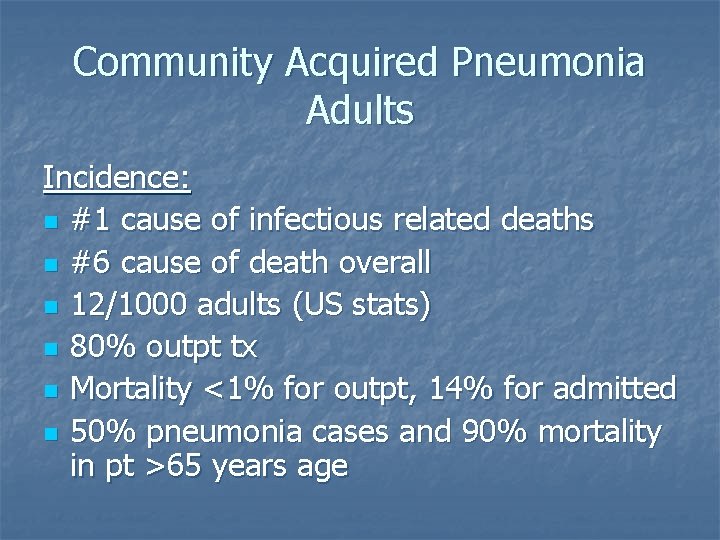
Community Acquired Pneumonia Adults Incidence: n #1 cause of infectious related deaths n #6 cause of death overall n 12/1000 adults (US stats) n 80% outpt tx n Mortality <1% for outpt, 14% for admitted n 50% pneumonia cases and 90% mortality in pt >65 years age

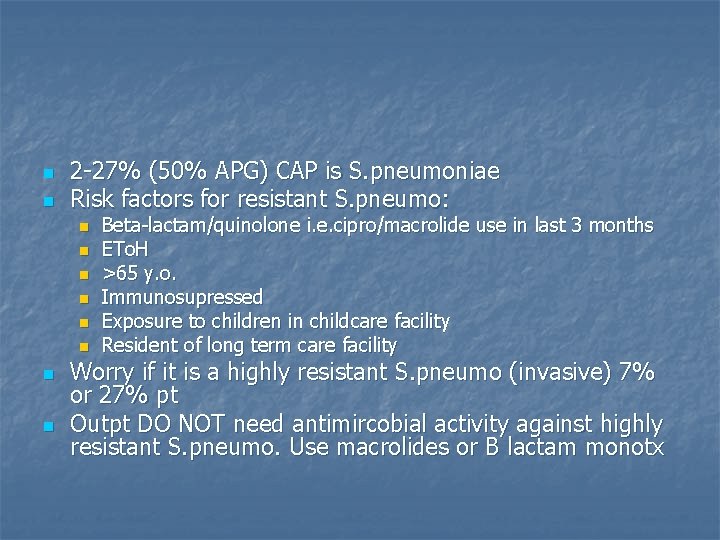
n n 2 -27% (50% APG) CAP is S. pneumoniae Risk factors for resistant S. pneumo: n n n n Beta-lactam/quinolone i. e. cipro/macrolide use in last 3 months ETo. H >65 y. o. Immunosupressed Exposure to children in childcare facility Resident of long term care facility Worry if it is a highly resistant S. pneumo (invasive) 7% or 27% pt Outpt DO NOT need antimircobial activity against highly resistant S. pneumo. Use macrolides or B lactam monotx
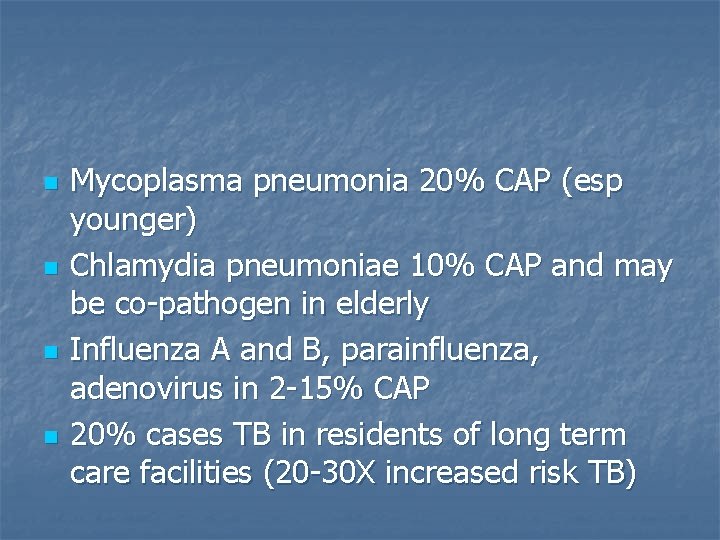
n n Mycoplasma pneumonia 20% CAP (esp younger) Chlamydia pneumoniae 10% CAP and may be co-pathogen in elderly Influenza A and B, parainfluenza, adenovirus in 2 -15% CAP 20% cases TB in residents of long term care facilities (20 -30 X increased risk TB)
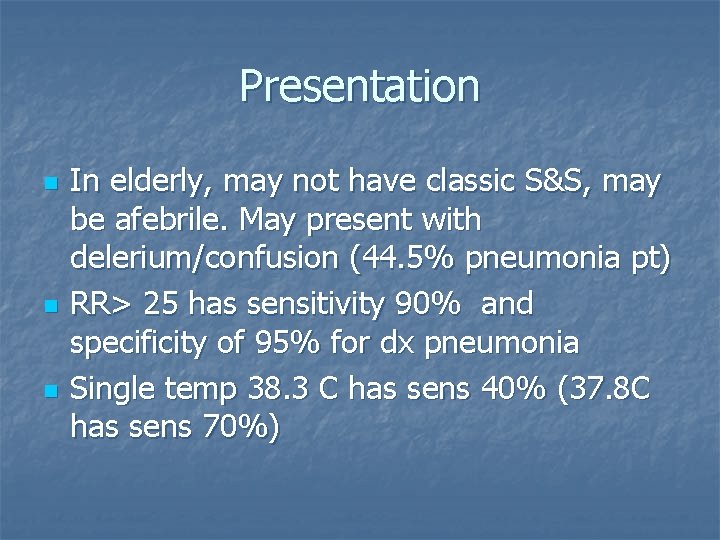
Presentation n In elderly, may not have classic S&S, may be afebrile. May present with delerium/confusion (44. 5% pneumonia pt) RR> 25 has sensitivity 90% and specificity of 95% for dx pneumonia Single temp 38. 3 C has sens 40% (37. 8 C has sens 70%)
Investigations n Blood culture only if pt has hx of chills/rigors n Blood culture within 24 h presentation associated with a decreased 30 d mortality in CAP (Meehan, TP, et al. Quality of care, process, and outcomes in elderly patients with pneumonia JAMA 1997; 278: 2080 -2084) n Do 3 sets: n n 1 aerobic/1 anaerobic 1 aerobic from 2 nd site at same time
Blood culture evidence? n n Mortality rate from bacteremic pneumococcal CAP has shown little improvement in the past three decades, remaining between 19% and 28%, (depending on the population and institution studied) Helpful in 15% pt
Blood gases n n n Sa. O 2 <90% or pt has COPD take ABG on room air or baseline 02 level if on chronic O 2 therapy Thoracentesis if effusion >10 mm on lateral XR Recurrent pneumonia – need w/u for immunosupression or structural ab. N
Gram stain n n Adequate if < 25 epithelial cells per lowpowered field >10 gram-positive, lancet-shape diplococci in a hpf is a sensitive and specific predictor of pneumococcal pneumonia Gram stain not helpful for other types pneumonia NPV 80%
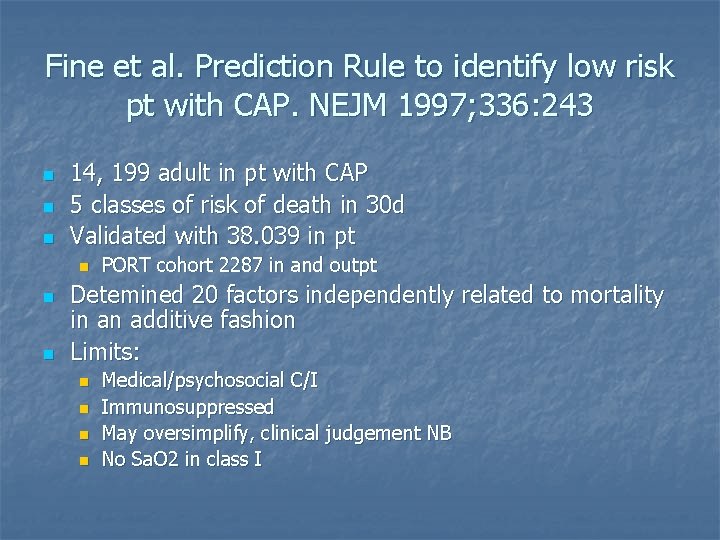
Fine et al. Prediction Rule to identify low risk pt with CAP. NEJM 1997; 336: 243 n n n 14, 199 adult in pt with CAP 5 classes of risk of death in 30 d Validated with 38. 039 in pt n n n PORT cohort 2287 in and outpt Detemined 20 factors independently related to mortality in an additive fashion Limits: n n Medical/psychosocial C/I Immunosuppressed May oversimplify, clinical judgement NB No Sa. O 2 in class I
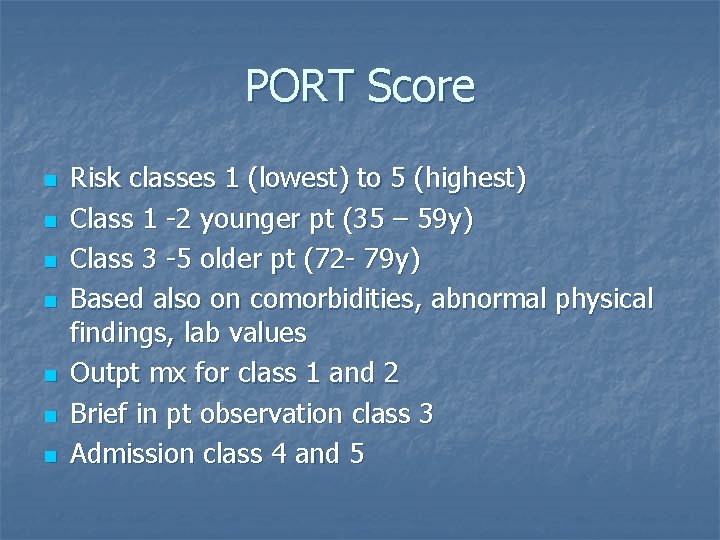
PORT Score n n n n Risk classes 1 (lowest) to 5 (highest) Class 1 -2 younger pt (35 – 59 y) Class 3 -5 older pt (72 - 79 y) Based also on comorbidities, abnormal physical findings, lab values Outpt mx for class 1 and 2 Brief in pt observation class 3 Admission class 4 and 5
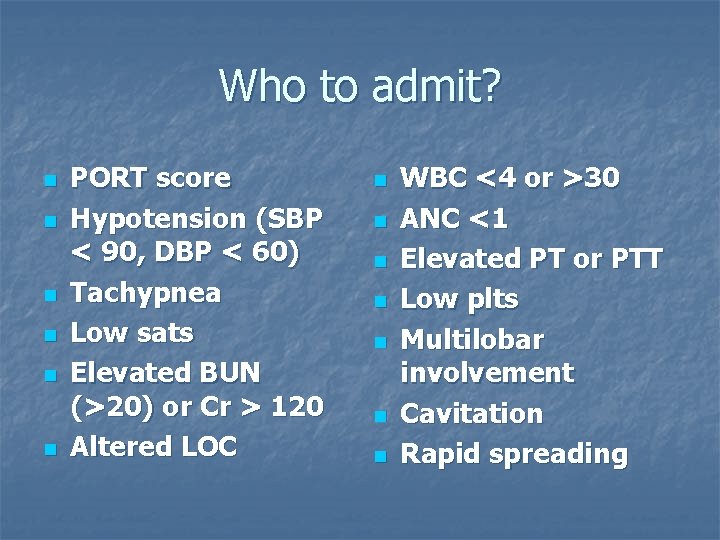
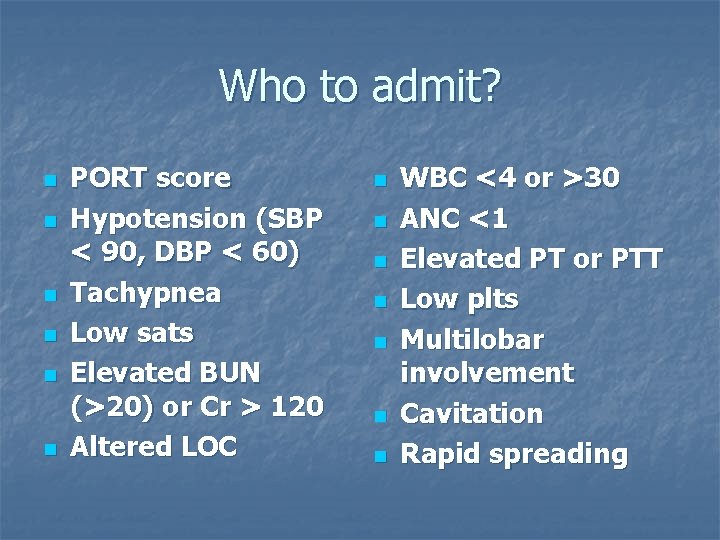
Who to admit? n n n PORT score Hypotension (SBP < 90, DBP < 60) Tachypnea Low sats Elevated BUN (>20) or Cr > 120 Altered LOC n n n n WBC <4 or >30 ANC <1 Elevated PT or PTT Low plts Multilobar involvement Cavitation Rapid spreading
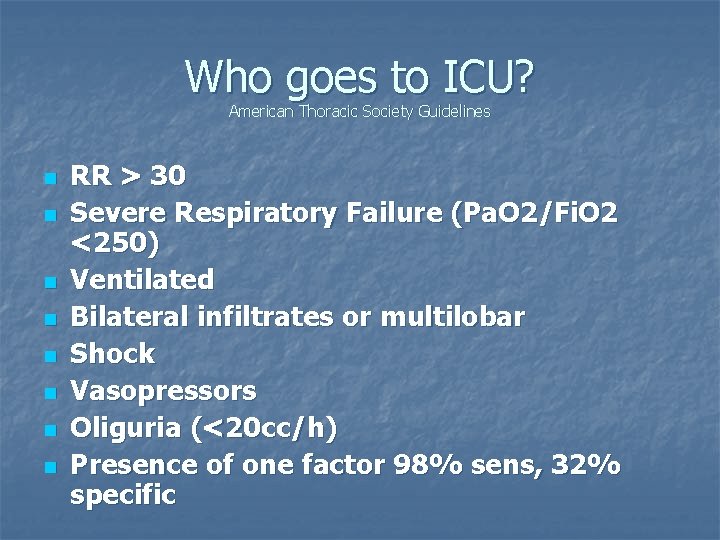
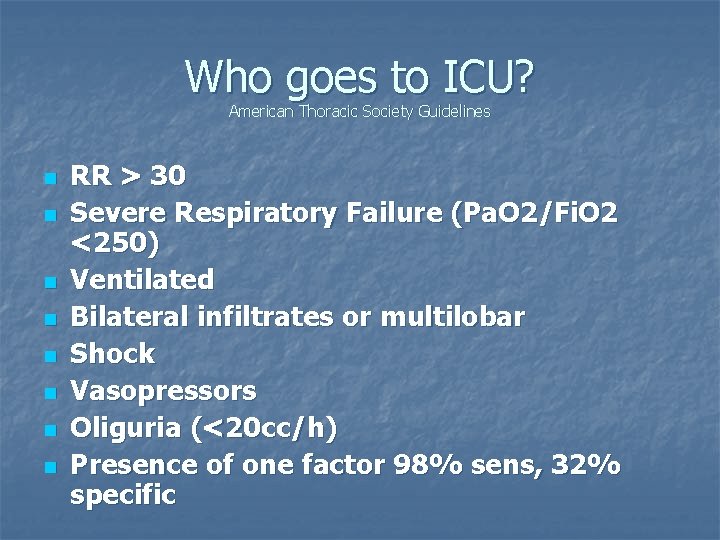
Who goes to ICU? American Thoracic Society Guidelines n n n n RR > 30 Severe Respiratory Failure (Pa. O 2/Fi. O 2 <250) Ventilated Bilateral infiltrates or multilobar Shock Vasopressors Oliguria (<20 cc/h) Presence of one factor 98% sens, 32% specific
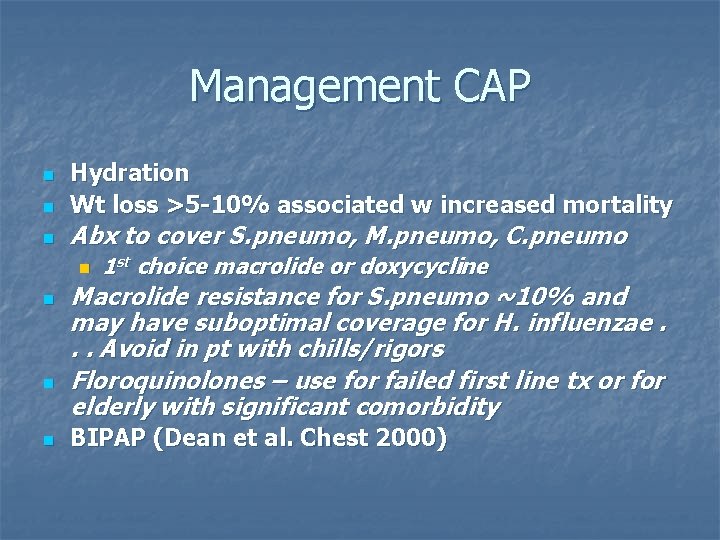
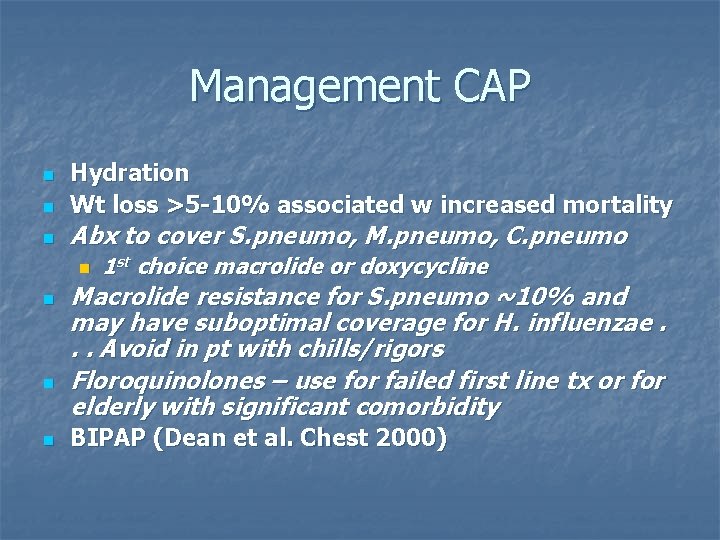
Management CAP n Hydration Wt loss >5 -10% associated w increased mortality n Abx to cover S. pneumo, M. pneumo, C. pneumo n n n 1 st choice macrolide or doxycycline Macrolide resistance for S. pneumo ~10% and may have suboptimal coverage for H. influenzae. . . Avoid in pt with chills/rigors Floroquinolones – use for failed first line tx or for elderly with significant comorbidity BIPAP (Dean et al. Chest 2000)
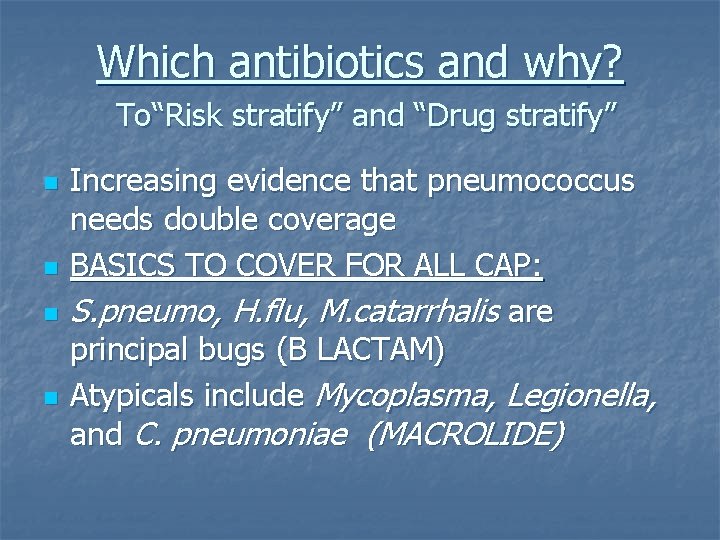
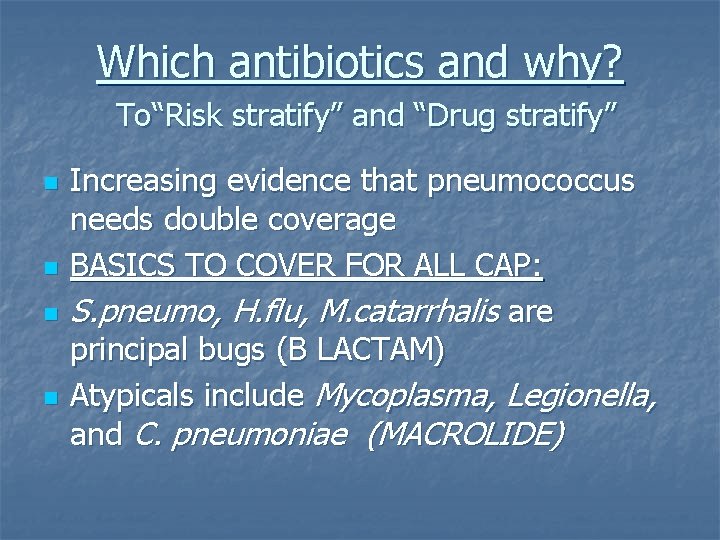
Which antibiotics and why? To“Risk stratify” and “Drug stratify” n n Increasing evidence that pneumococcus needs double coverage BASICS TO COVER FOR ALL CAP: S. pneumo, H. flu, M. catarrhalis are principal bugs (B LACTAM) Atypicals include Mycoplasma, Legionella, and C. pneumoniae (MACROLIDE)
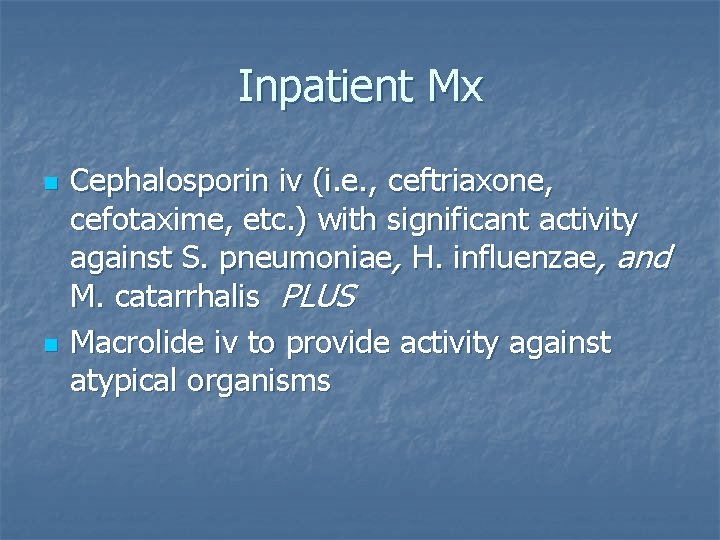
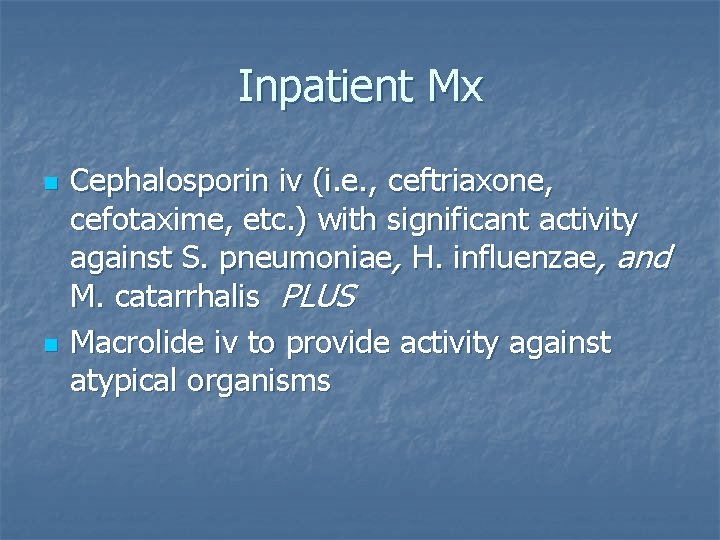
Inpatient Mx n n Cephalosporin iv (i. e. , ceftriaxone, cefotaxime, etc. ) with significant activity against S. pneumoniae, H. influenzae, and M. catarrhalis PLUS Macrolide iv to provide activity against atypical organisms
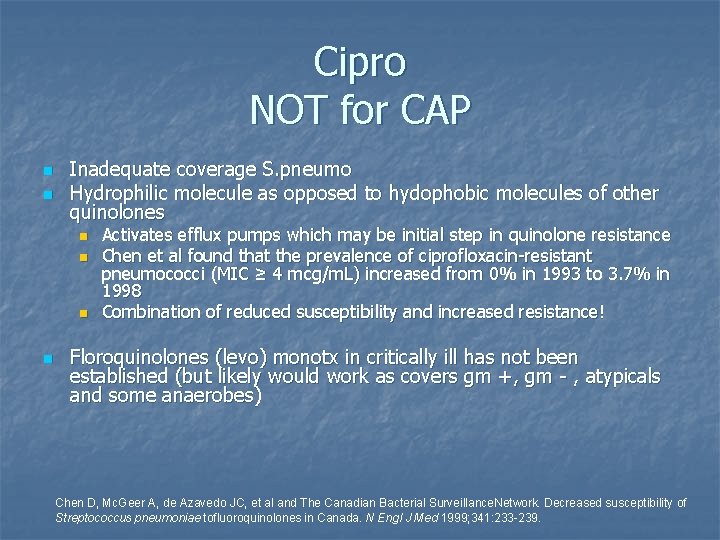
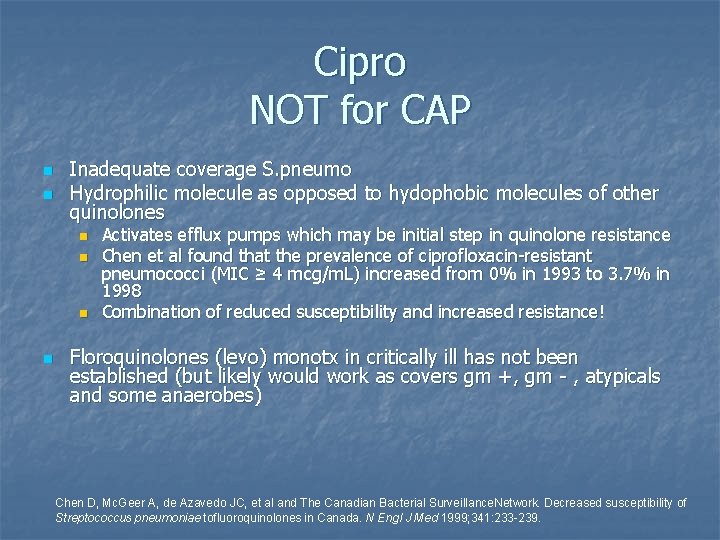
Cipro NOT for CAP n n Inadequate coverage S. pneumo Hydrophilic molecule as opposed to hydophobic molecules of other quinolones n n Activates efflux pumps which may be initial step in quinolone resistance Chen et al found that the prevalence of ciprofloxacin-resistant pneumococci (MIC ≥ 4 mcg/m. L) increased from 0% in 1993 to 3. 7% in 1998 Combination of reduced susceptibility and increased resistance! Floroquinolones (levo) monotx in critically ill has not been established (but likely would work as covers gm +, gm - , atypicals and some anaerobes) Chen D, Mc. Geer A, de Azavedo JC, et al and The Canadian Bacterial Surveillance. Network. Decreased susceptibility of Streptococcus pneumoniae tofluoroquinolones in Canada. N Engl J Med 1999; 341: 233 -239.
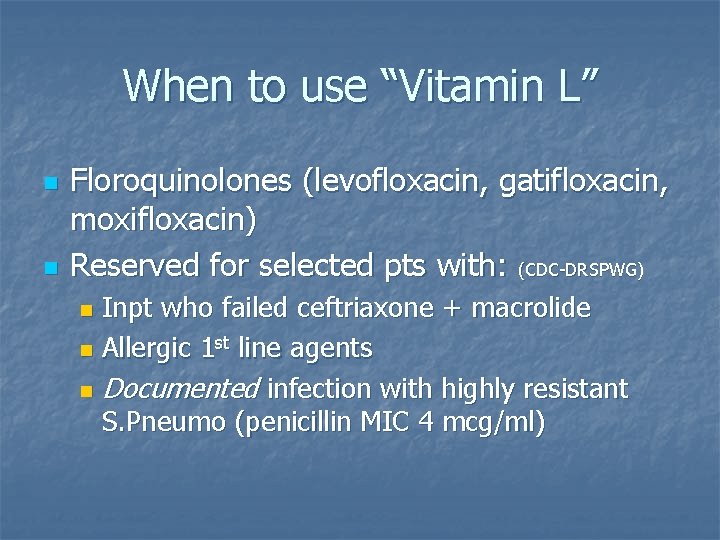
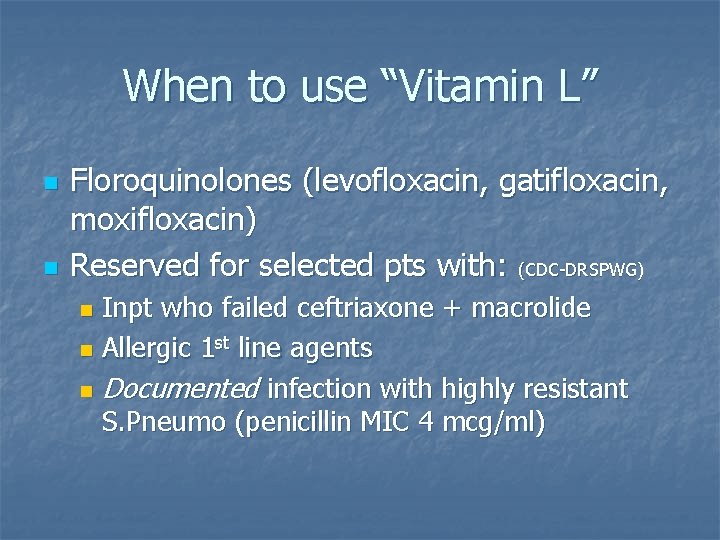
When to use “Vitamin L” n n Floroquinolones (levofloxacin, gatifloxacin, moxifloxacin) Reserved for selected pts with: (CDC-DRSPWG) Inpt who failed ceftriaxone + macrolide n Allergic 1 st line agents n Documented infection with highly resistant S. Pneumo (penicillin MIC 4 mcg/ml) n
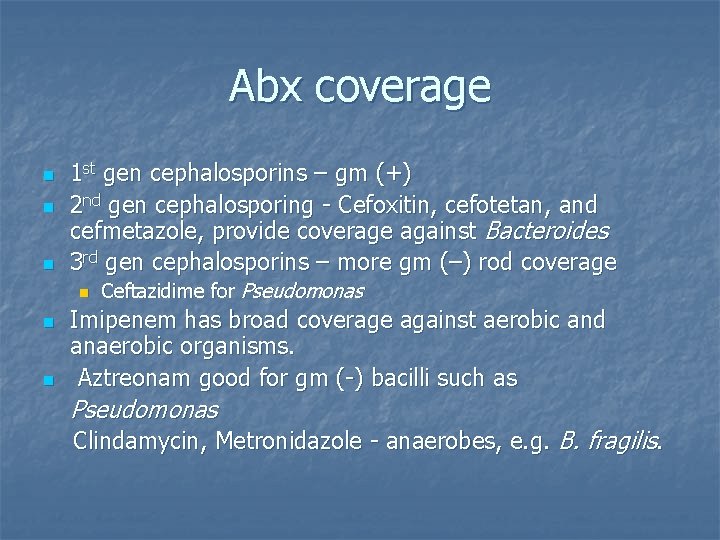
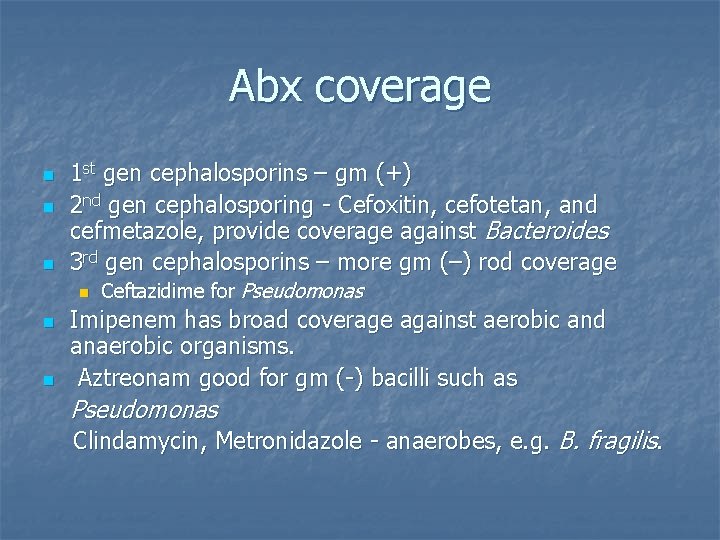
Abx coverage n n n 1 st gen cephalosporins – gm (+) 2 nd gen cephalosporing - Cefoxitin, cefotetan, and cefmetazole, provide coverage against Bacteroides 3 rd gen cephalosporins – more gm (–) rod coverage n n n Ceftazidime for Pseudomonas Imipenem has broad coverage against aerobic and anaerobic organisms. Aztreonam good for gm (-) bacilli such as Pseudomonas Clindamycin, Metronidazole - anaerobes, e. g. B. fragilis.
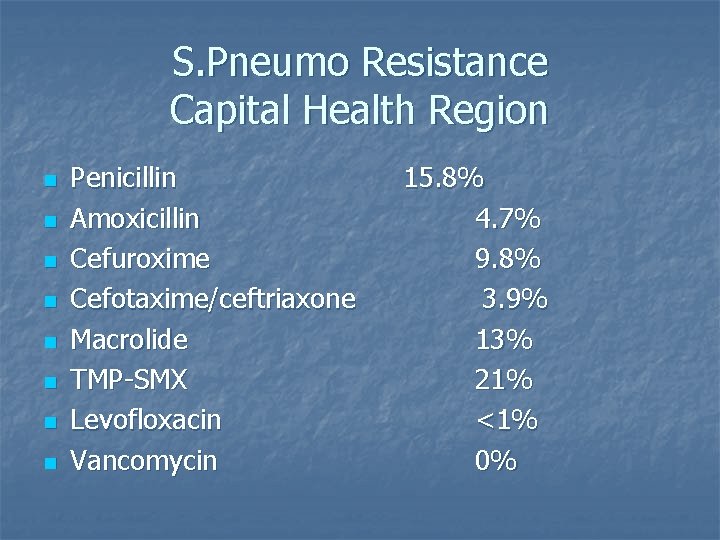
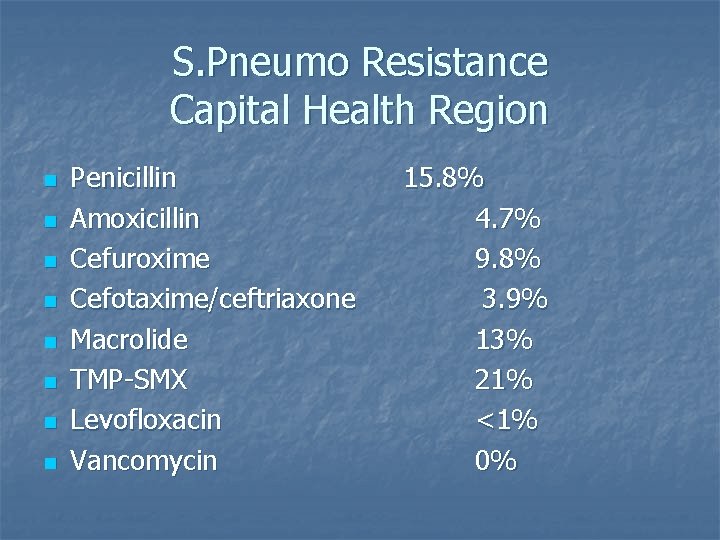
S. Pneumo Resistance Capital Health Region n n n n Penicillin Amoxicillin Cefuroxime Cefotaxime/ceftriaxone Macrolide TMP-SMX Levofloxacin Vancomycin 15. 8% 4. 7% 9. 8% 3. 9% 13% 21% <1% 0%
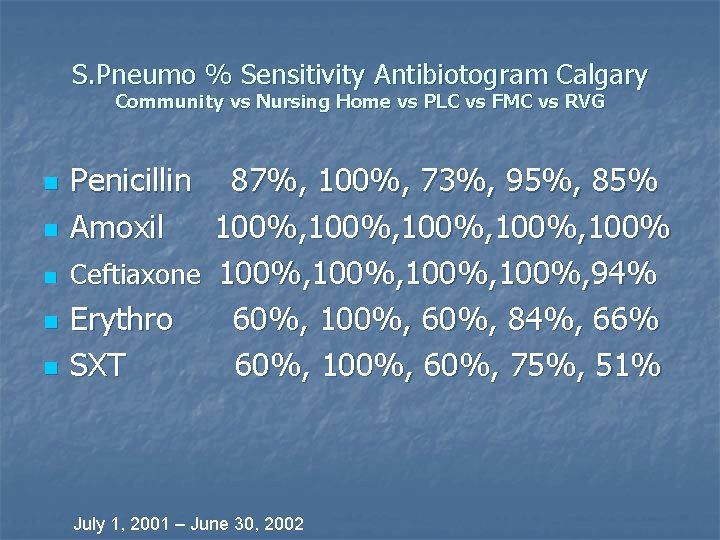
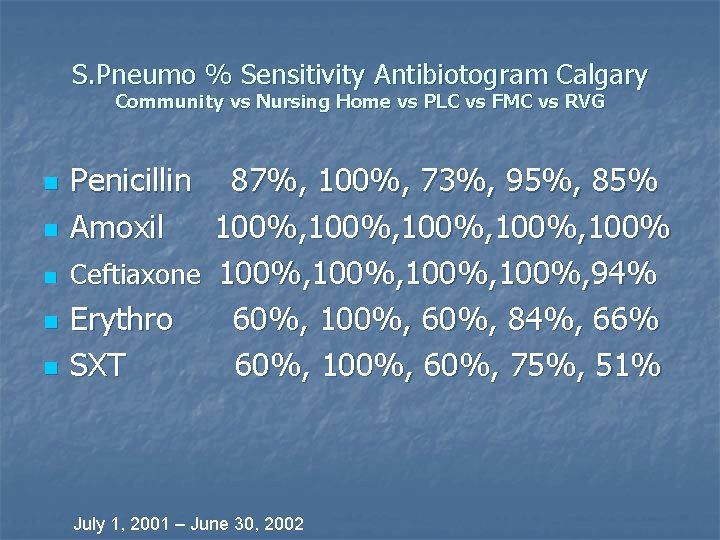
S. Pneumo % Sensitivity Antibiotogram Calgary Community vs Nursing Home vs PLC vs FMC vs RVG n n n Penicillin 87%, 100%, 73%, 95%, 85% Amoxil 100%, 100% Ceftiaxone 100%, 94% Erythro 60%, 100%, 60%, 84%, 66% SXT 60%, 100%, 60%, 75%, 51% July 1, 2001 – June 30, 2002
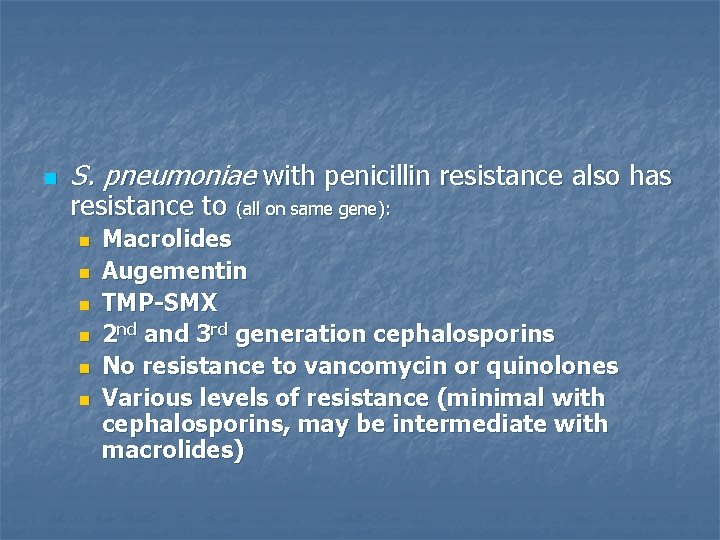
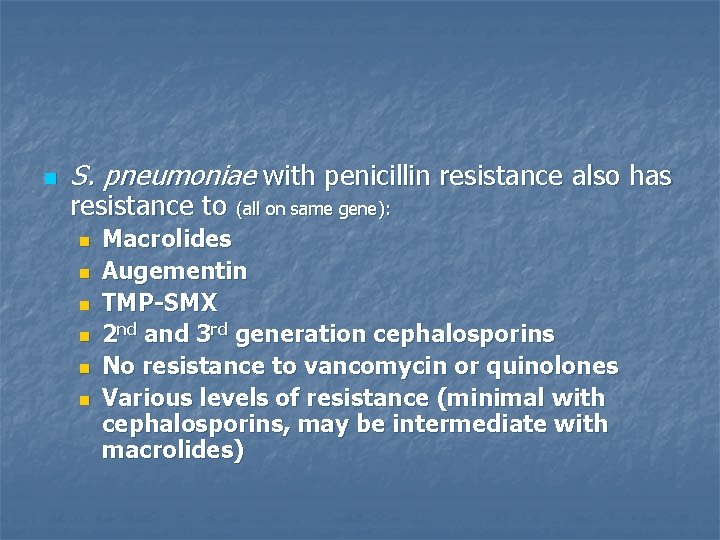
n S. pneumoniae with penicillin resistance also has resistance to (all on same gene): n n n Macrolides Augementin TMP-SMX 2 nd and 3 rd generation cephalosporins No resistance to vancomycin or quinolones Various levels of resistance (minimal with cephalosporins, may be intermediate with macrolides)
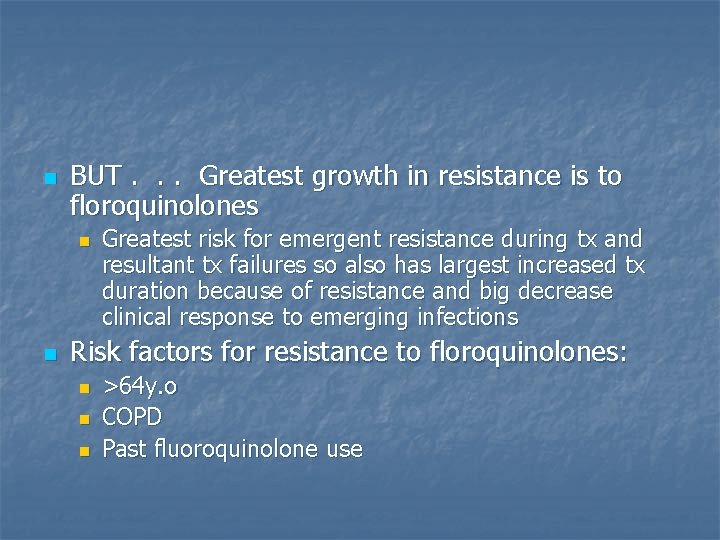
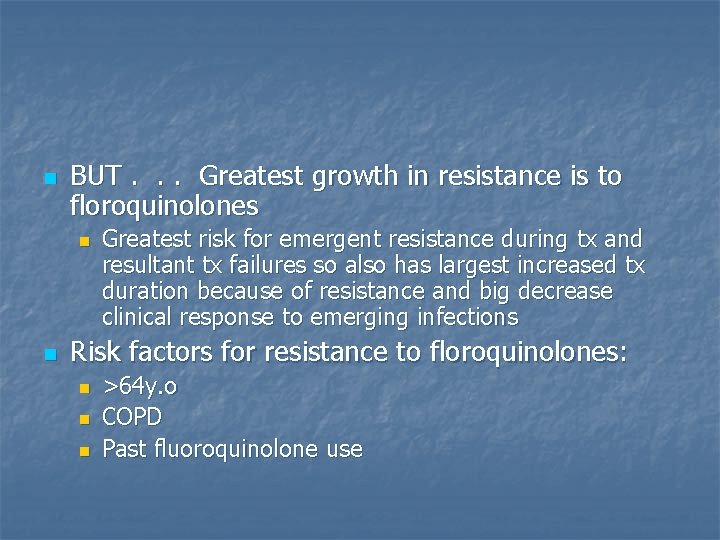
n BUT. . . Greatest growth in resistance is to floroquinolones n n Greatest risk for emergent resistance during tx and resultant tx failures so also has largest increased tx duration because of resistance and big decrease clinical response to emerging infections Risk factors for resistance to floroquinolones: n n n >64 y. o COPD Past fluoroquinolone use
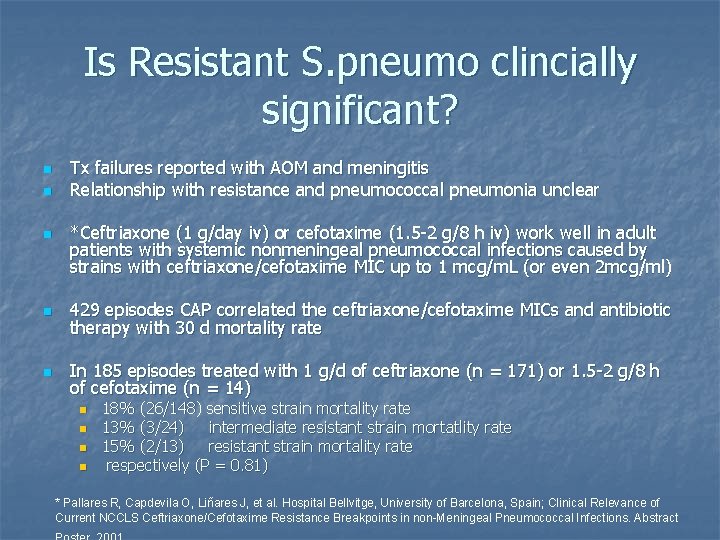
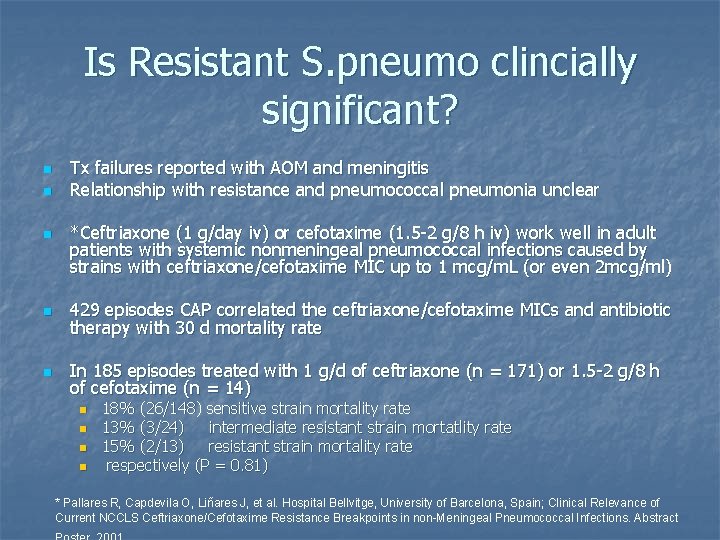
Is Resistant S. pneumo clincially significant? n n n Tx failures reported with AOM and meningitis Relationship with resistance and pneumococcal pneumonia unclear *Ceftriaxone (1 g/day iv) or cefotaxime (1. 5 -2 g/8 h iv) work well in adult patients with systemic nonmeningeal pneumococcal infections caused by strains with ceftriaxone/cefotaxime MIC up to 1 mcg/m. L (or even 2 mcg/ml) n 429 episodes CAP correlated the ceftriaxone/cefotaxime MICs and antibiotic therapy with 30 d mortality rate n In 185 episodes treated with 1 g/d of ceftriaxone (n = 171) or 1. 5 -2 g/8 h of cefotaxime (n = 14) n n 18% (26/148) sensitive strain mortality rate 13% (3/24) intermediate resistant strain mortatlity rate 15% (2/13) resistant strain mortality rate respectively (P = 0. 81) * Pallares R, Capdevila O, Liñares J, et al. Hospital Bellvitge, University of Barcelona, Spain; Clinical Relevance of Current NCCLS Ceftriaxone/Cefotaxime Resistance Breakpoints in non-Meningeal Pneumococcal Infections. Abstract
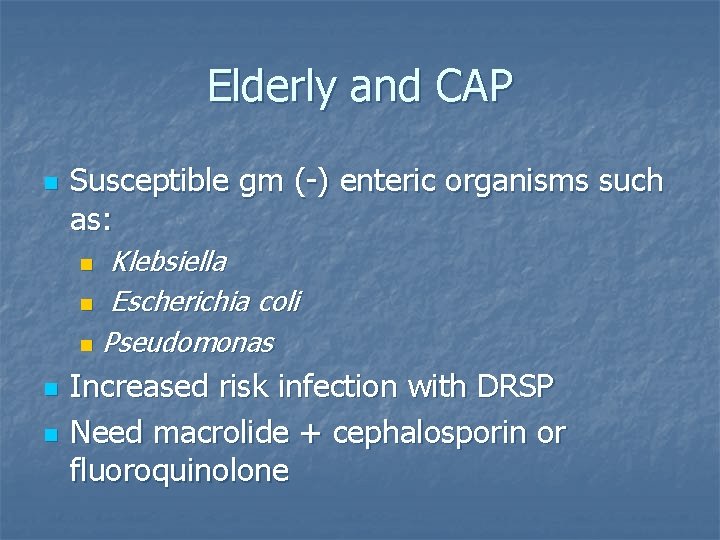
Elderly and CAP n Susceptible gm (-) enteric organisms such as: Klebsiella n Escherichia coli n Pseudomonas n n n Increased risk infection with DRSP Need macrolide + cephalosporin or fluoroquinolone
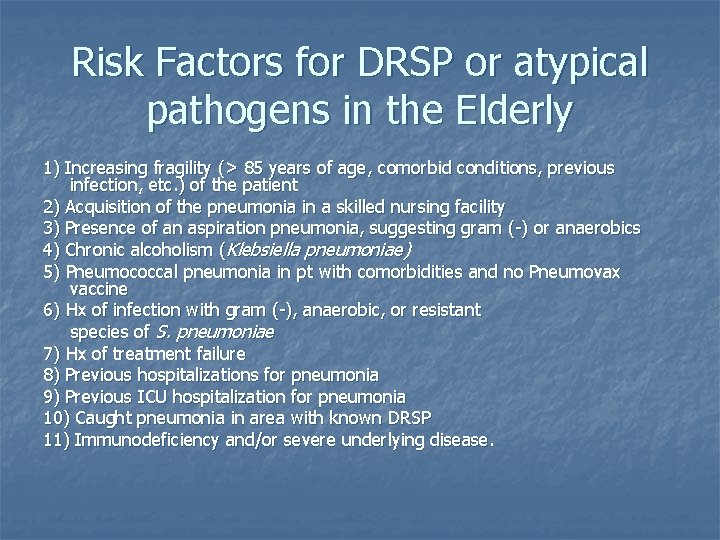
Risk Factors for DRSP or atypical pathogens in the Elderly 1) Increasing fragility (> 85 years of age, comorbid conditions, previous infection, etc. ) of the patient 2) Acquisition of the pneumonia in a skilled nursing facility 3) Presence of an aspiration pneumonia, suggesting gram (-) or anaerobics 4) Chronic alcoholism (Klebsiella pneumoniae) 5) Pneumococcal pneumonia in pt with comorbidities and no Pneumovax vaccine 6) Hx of infection with gram (-), anaerobic, or resistant species of S. pneumoniae 7) Hx of treatment failure 8) Previous hospitalizations for pneumonia 9) Previous ICU hospitalization for pneumonia 10) Caught pneumonia in area with known DRSP 11) Immunodeficiency and/or severe underlying disease.
Admission Criteria n n Pneumonia Severity of Illness score Give abx within 8 hours of arrival to hospital (decreases mortality)
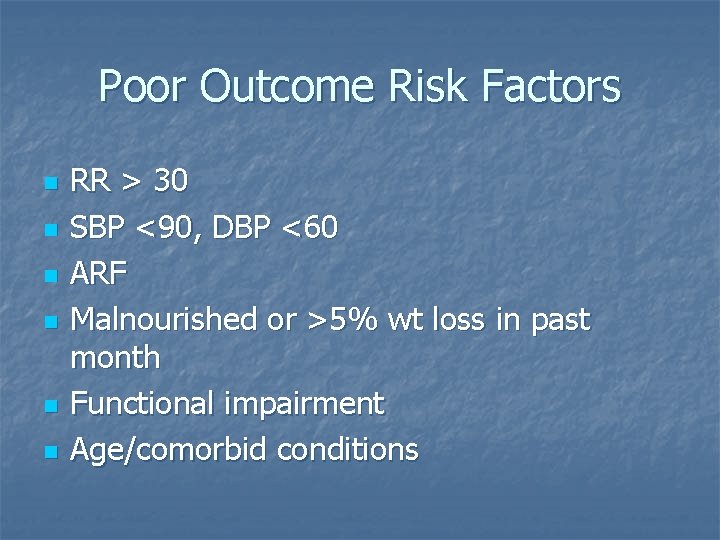
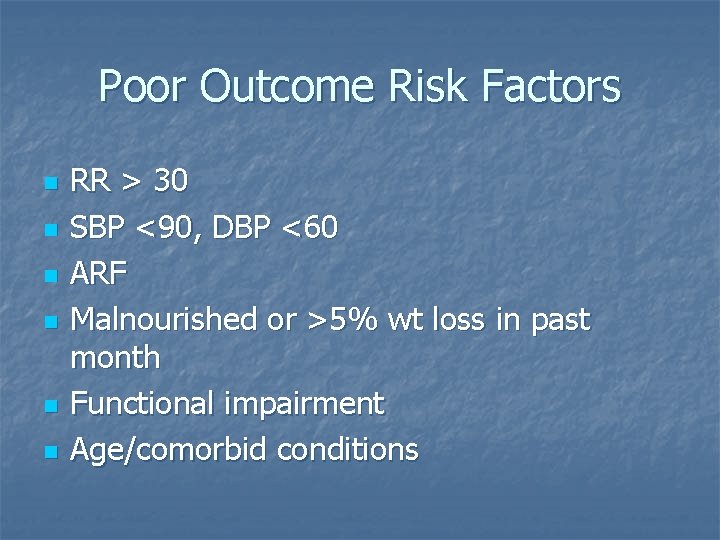
Poor Outcome Risk Factors n n n RR > 30 SBP <90, DBP <60 ARF Malnourished or >5% wt loss in past month Functional impairment Age/comorbid conditions
. n Numerous studies showing that pneumonia guidelines can reduce mortality and reduce unnecessary use of resources
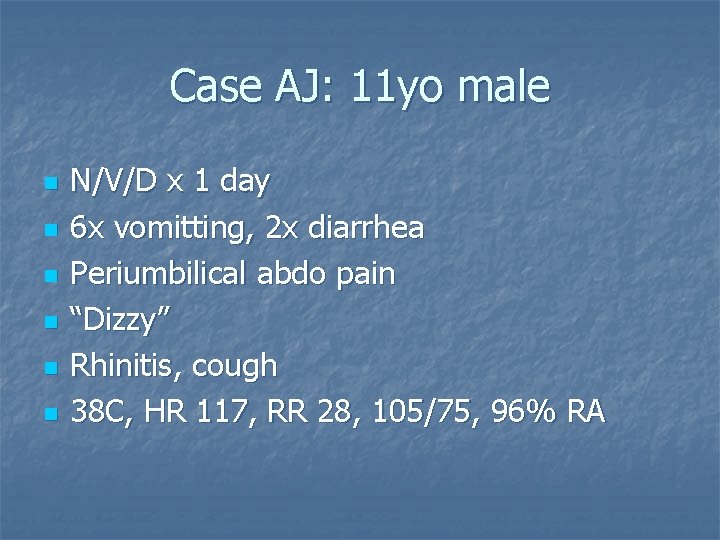
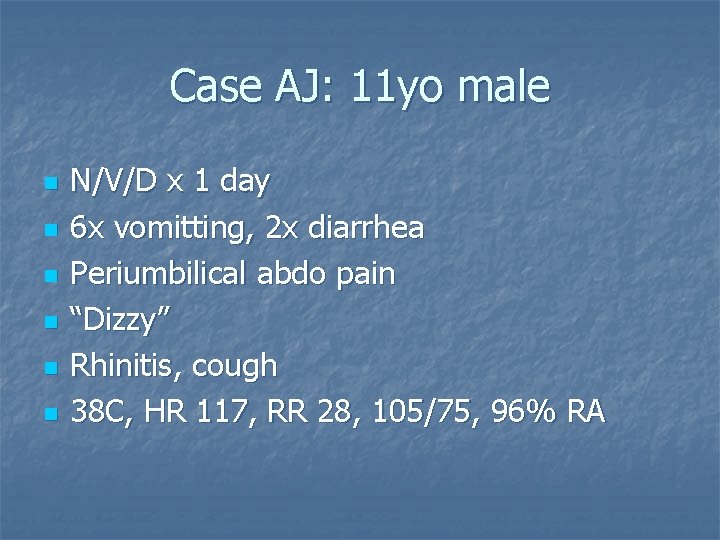
Case AJ: 11 yo male n n n N/V/D x 1 day 6 x vomitting, 2 x diarrhea Periumbilical abdo pain “Dizzy” Rhinitis, cough 38 C, HR 117, RR 28, 105/75, 96% RA
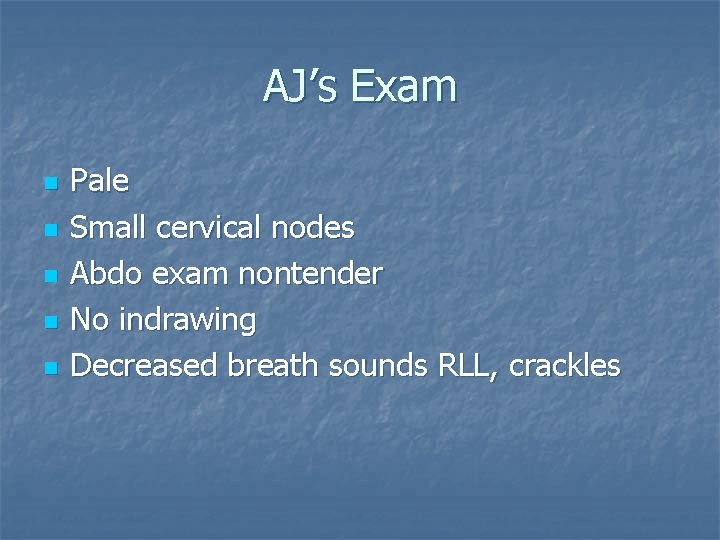
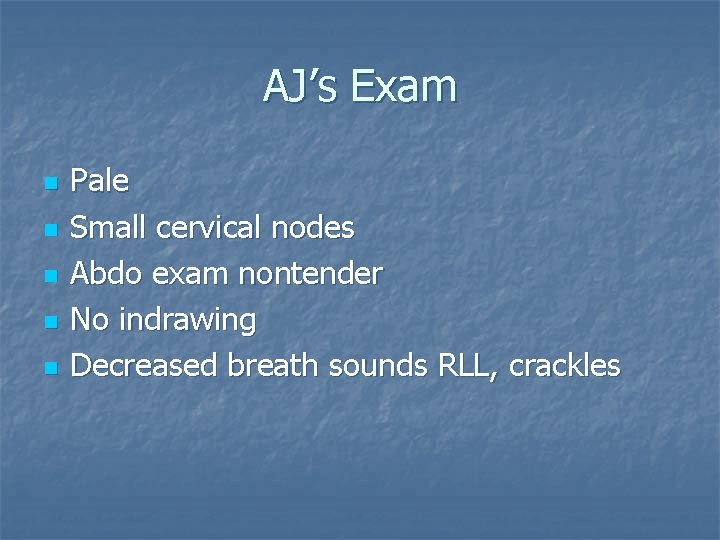
AJ’s Exam n n n Pale Small cervical nodes Abdo exam nontender No indrawing Decreased breath sounds RLL, crackles

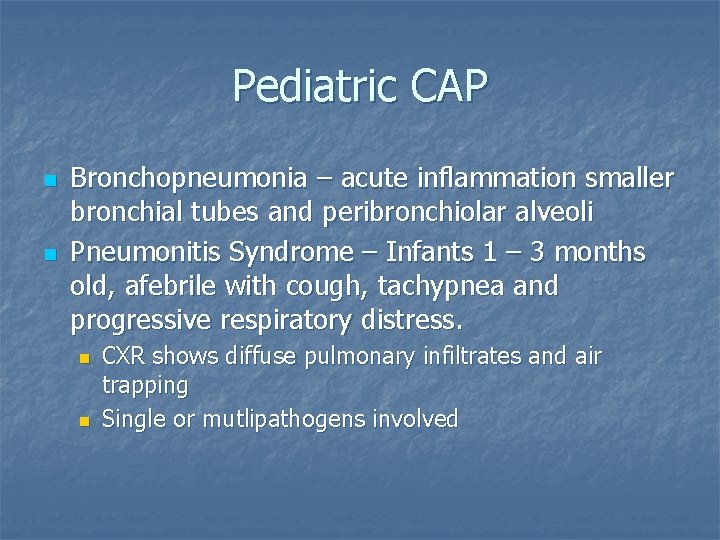
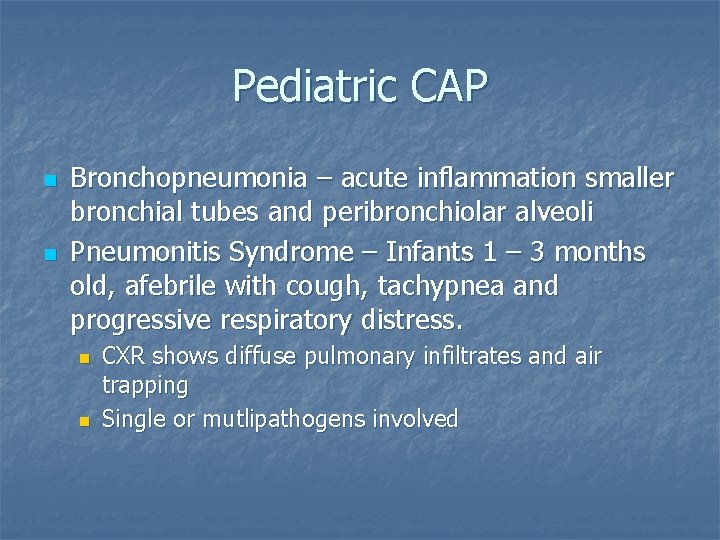
Pediatric CAP n n Bronchopneumonia – acute inflammation smaller bronchial tubes and peribronchiolar alveoli Pneumonitis Syndrome – Infants 1 – 3 months old, afebrile with cough, tachypnea and progressive respiratory distress. n n CXR shows diffuse pulmonary infiltrates and air trapping Single or mutlipathogens involved
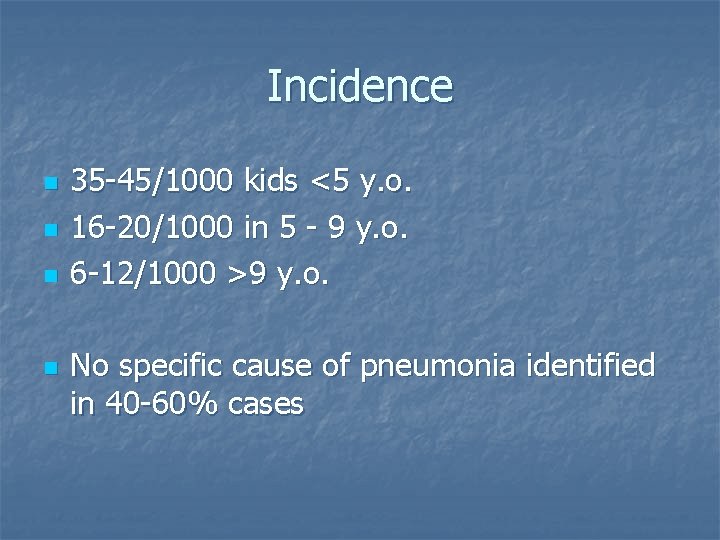
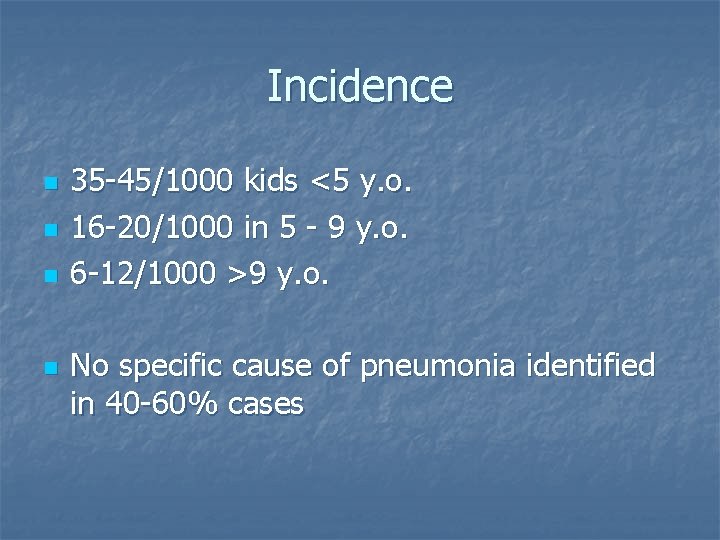
Incidence n n 35 -45/1000 kids <5 y. o. 16 -20/1000 in 5 - 9 y. o. 6 -12/1000 >9 y. o. No specific cause of pneumonia identified in 40 -60% cases
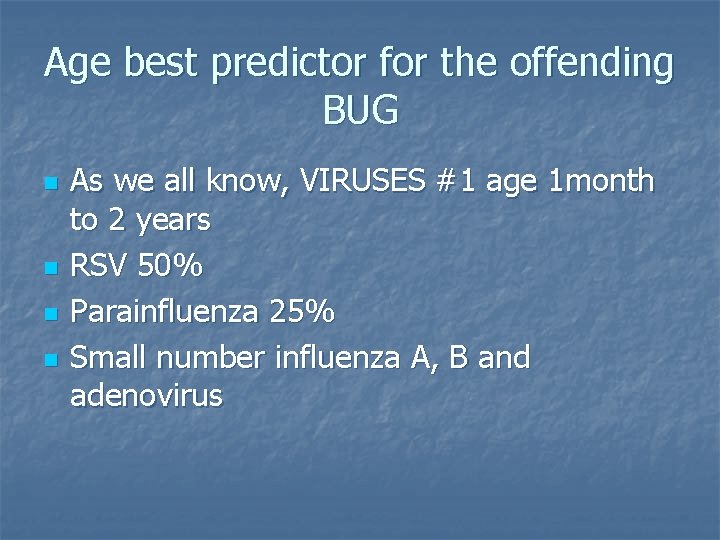
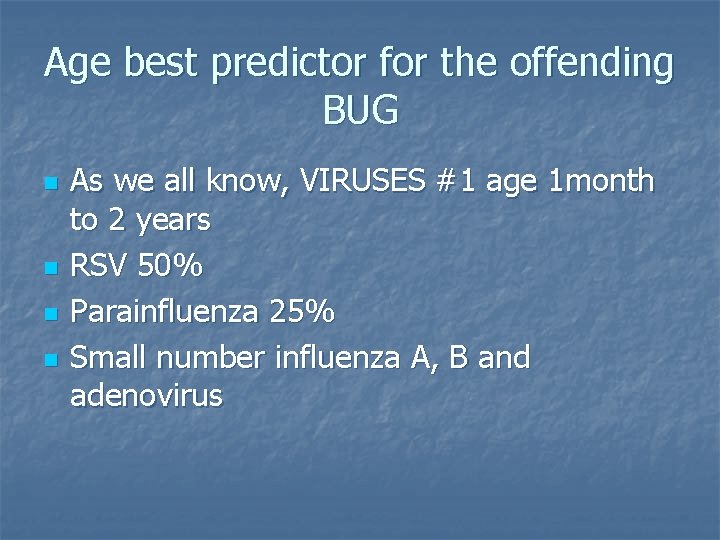
Age best predictor for the offending BUG n n As we all know, VIRUSES #1 age 1 month to 2 years RSV 50% Parainfluenza 25% Small number influenza A, B and adenovirus
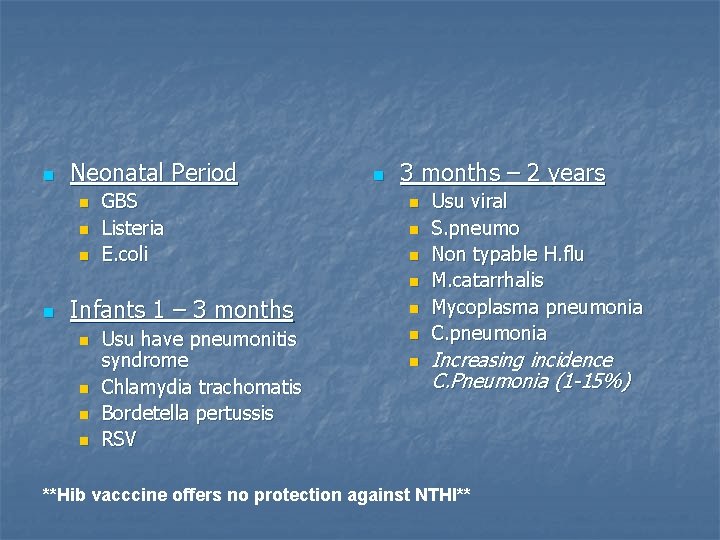
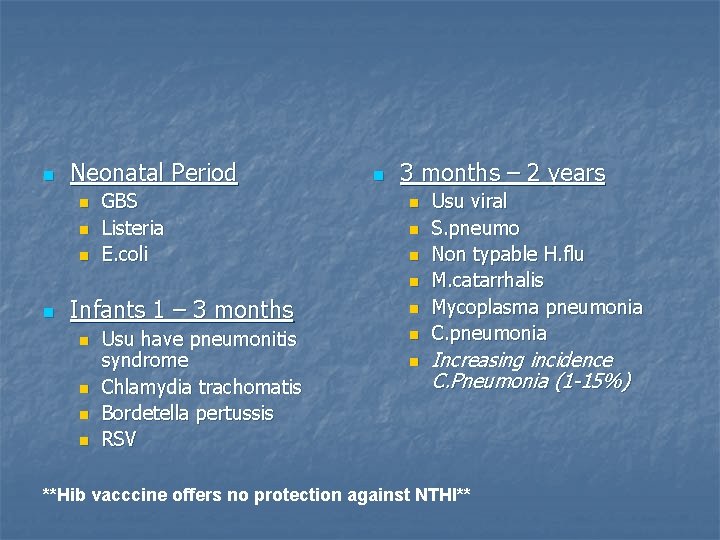
n Neonatal Period n n n GBS Listeria E. coli n 3 months – 2 years n n n Infants 1 – 3 months n n Usu have pneumonitis syndrome Chlamydia trachomatis Bordetella pertussis RSV n n n Usu viral S. pneumo Non typable H. flu M. catarrhalis Mycoplasma pneumonia C. pneumonia Increasing incidence C. Pneumonia (1 -15%) **Hib vacccine offers no protection against NTHI**
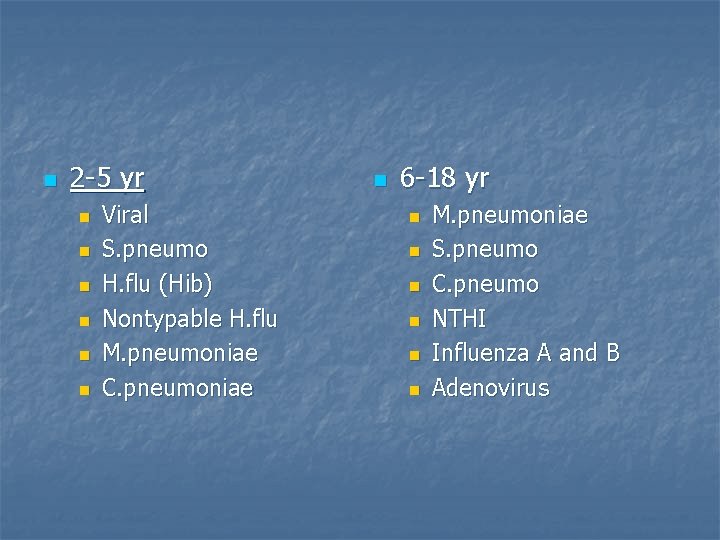
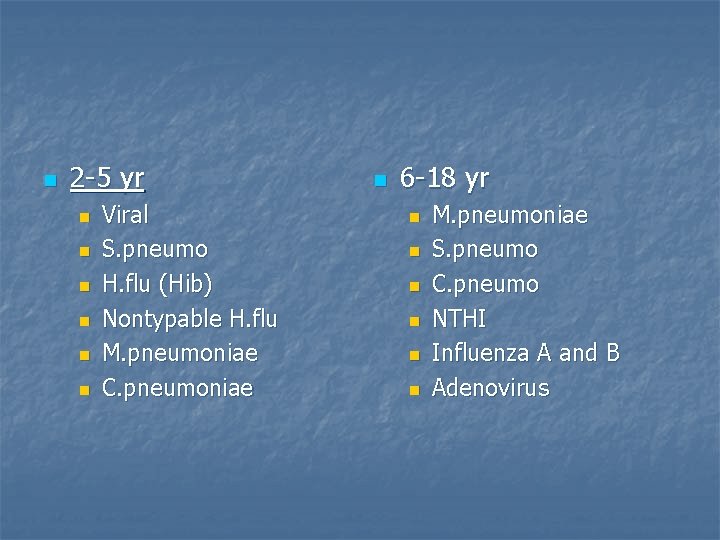
n 2 -5 yr n n n Viral S. pneumo H. flu (Hib) Nontypable H. flu M. pneumoniae C. pneumoniae n 6 -18 yr n n n M. pneumoniae S. pneumo C. pneumo NTHI Influenza A and B Adenovirus
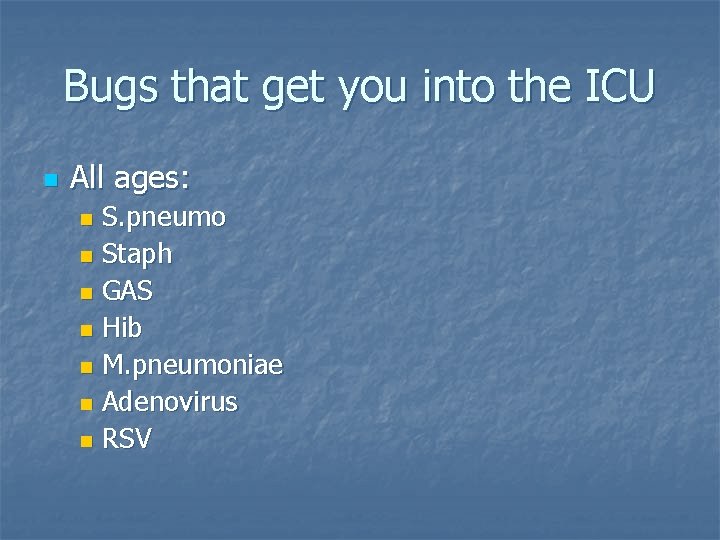
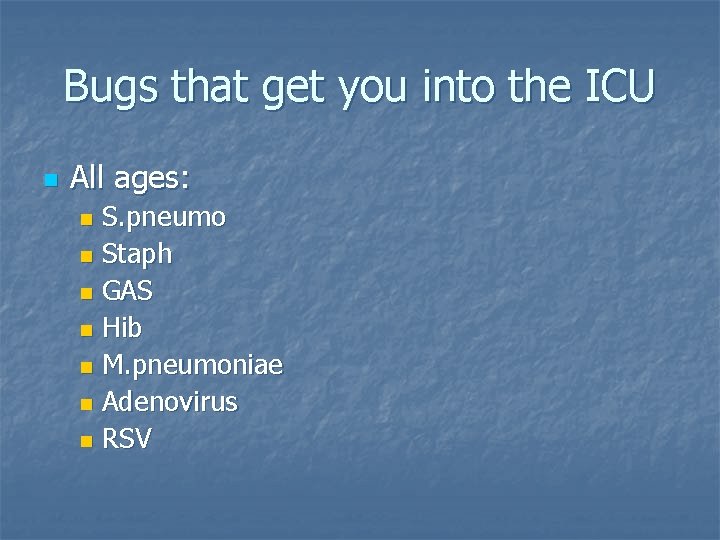
Bugs that get you into the ICU n All ages: S. pneumo n Staph n GAS n Hib n M. pneumoniae n Adenovirus n RSV n
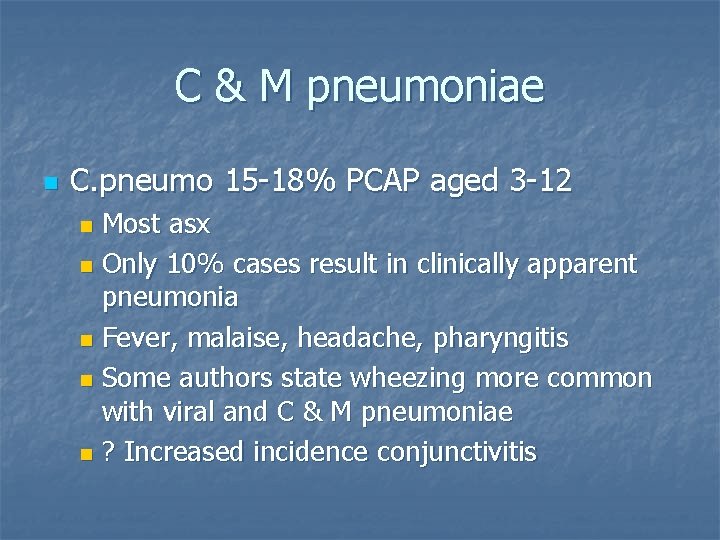
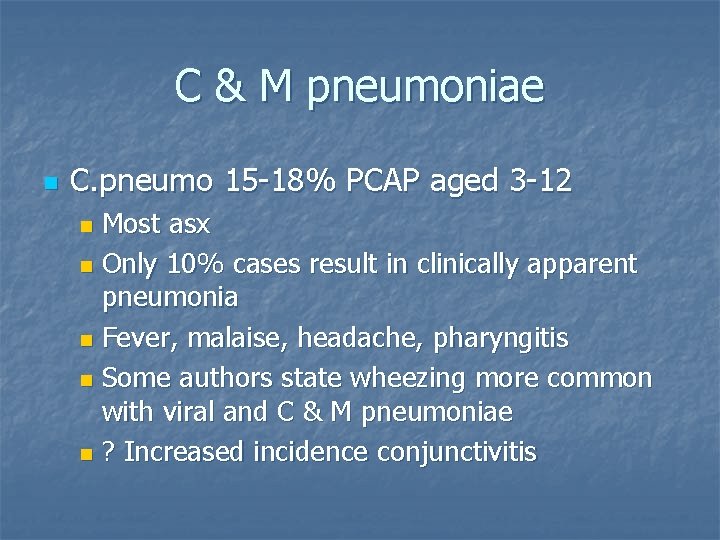
C & M pneumoniae n C. pneumo 15 -18% PCAP aged 3 -12 Most asx n Only 10% cases result in clinically apparent pneumonia n Fever, malaise, headache, pharyngitis n Some authors state wheezing more common with viral and C & M pneumoniae n ? Increased incidence conjunctivitis n
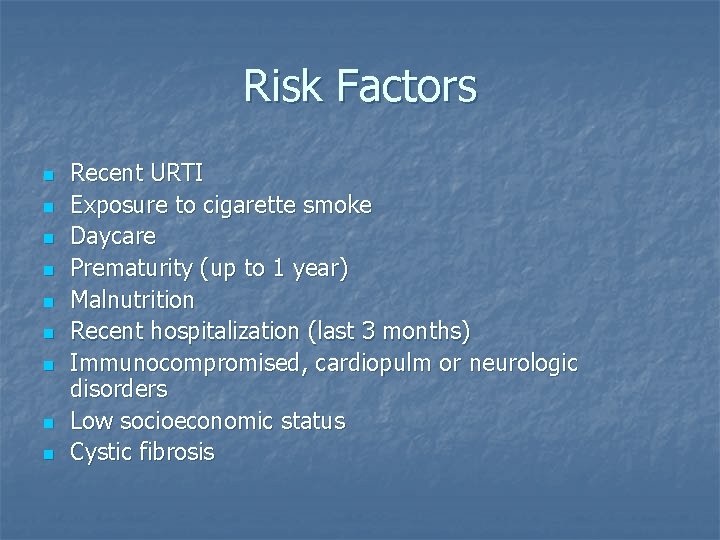
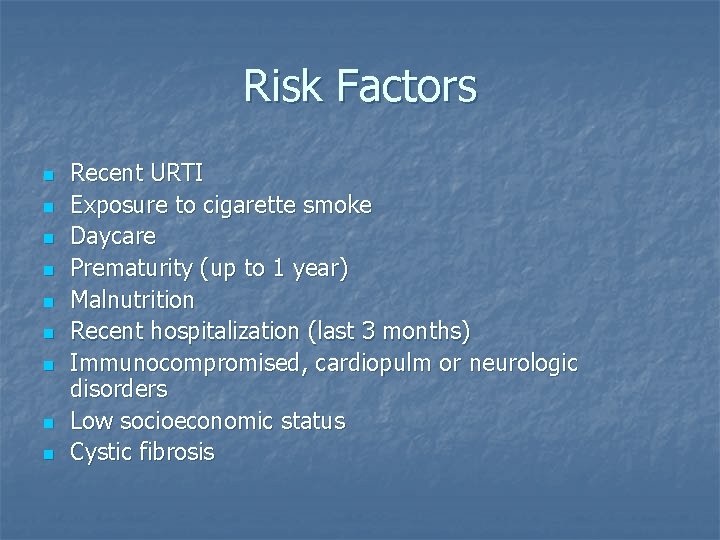
Risk Factors n n n n n Recent URTI Exposure to cigarette smoke Daycare Prematurity (up to 1 year) Malnutrition Recent hospitalization (last 3 months) Immunocompromised, cardiopulm or neurologic disorders Low socioeconomic status Cystic fibrosis
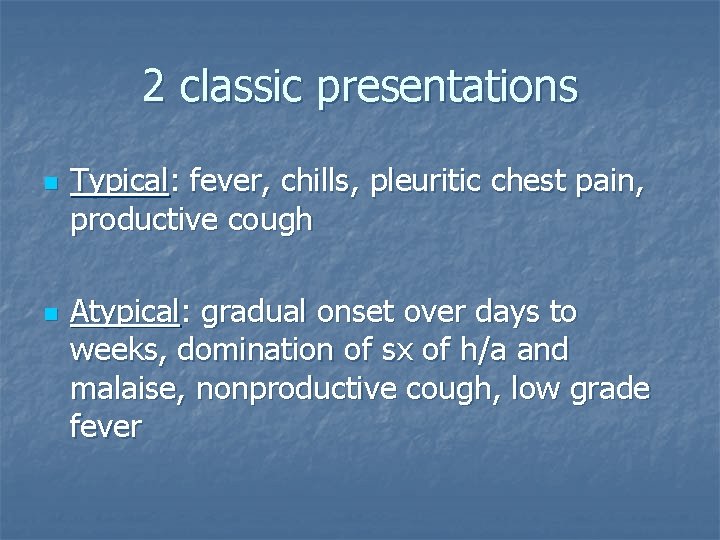
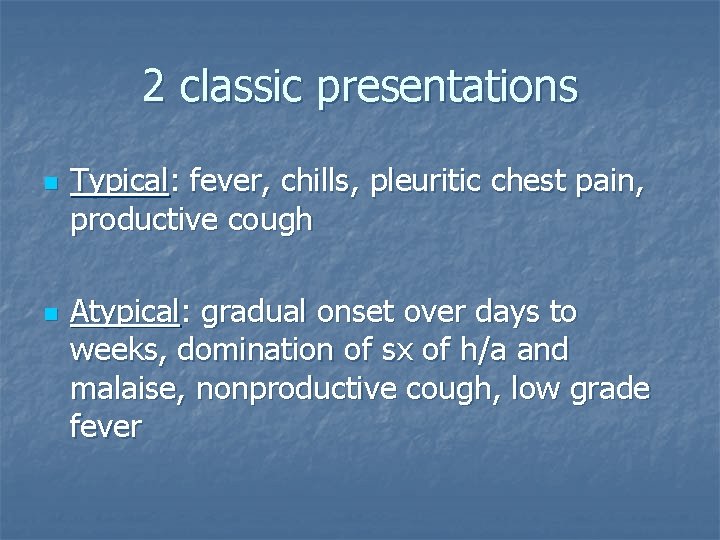
2 classic presentations n n Typical: fever, chills, pleuritic chest pain, productive cough Atypical: gradual onset over days to weeks, domination of sx of h/a and malaise, nonproductive cough, low grade fever

n n n Fever, rigors, pleuritic chest/abdominal pain suggest pneumococcal pneumonia Temp >38. 5 C RR >50/min in <11 months RR >40/min in >11 months RR >28 in 5 -16 years
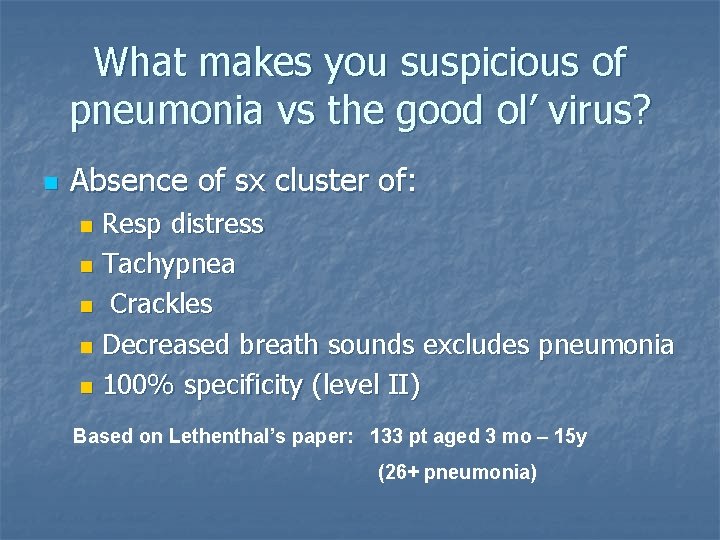
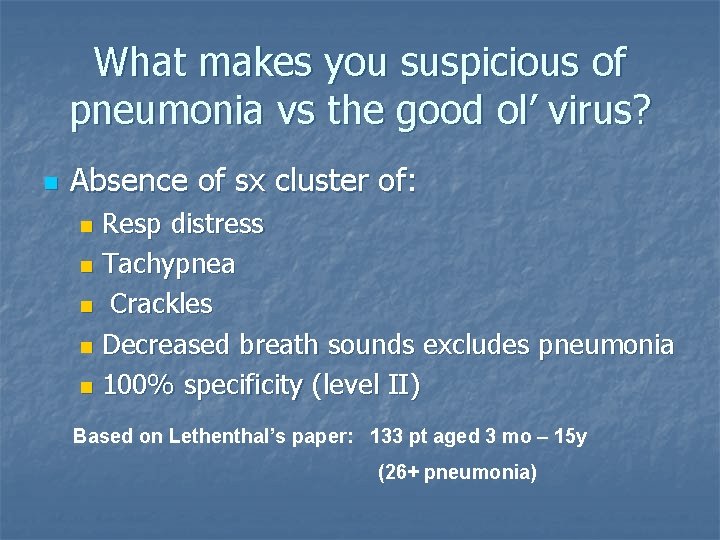
What makes you suspicious of pneumonia vs the good ol’ virus? n Absence of sx cluster of: Resp distress n Tachypnea n Crackles n Decreased breath sounds excludes pneumonia n 100% specificity (level II) n Based on Lethenthal’s paper: 133 pt aged 3 mo – 15 y (26+ pneumonia)
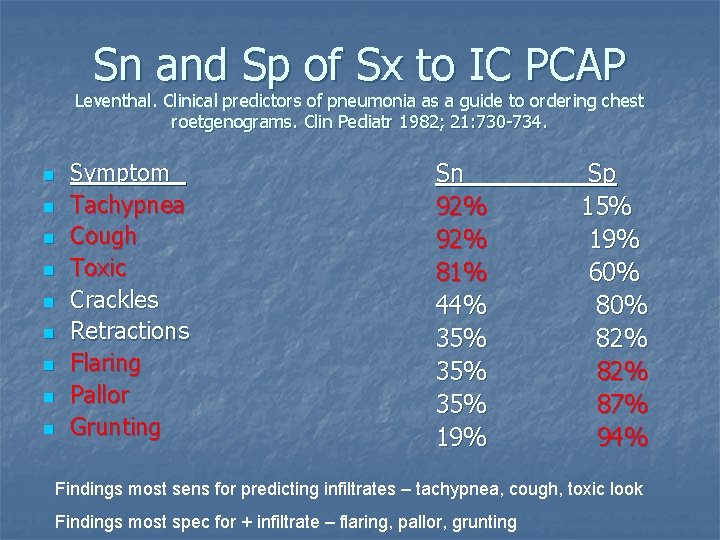
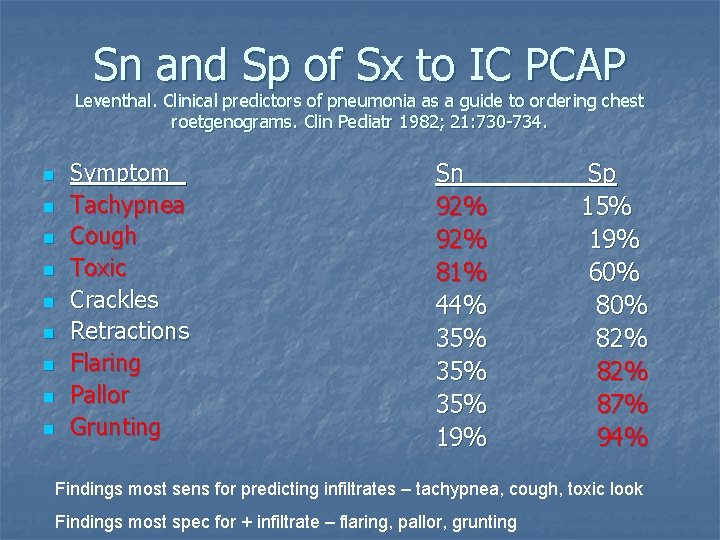
Sn and Sp of Sx to IC PCAP Leventhal. Clinical predictors of pneumonia as a guide to ordering chest roetgenograms. Clin Pediatr 1982; 21: 730 -734. n n n n n Symptom Tachypnea Cough Toxic Crackles Retractions Flaring Pallor Grunting Sn 92% 81% 44% 35% 35% 19% Sp 15% 19% 60% 82% 87% 94% Findings most sens for predicting infiltrates – tachypnea, cough, toxic look Findings most spec for + infiltrate – flaring, pallor, grunting
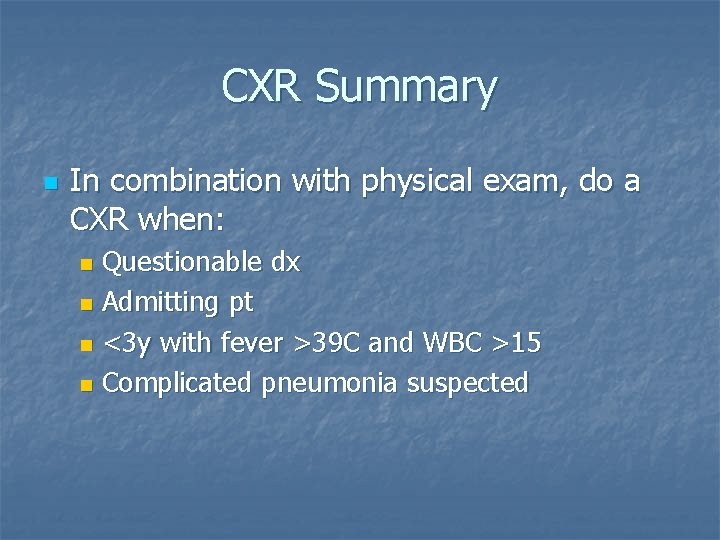
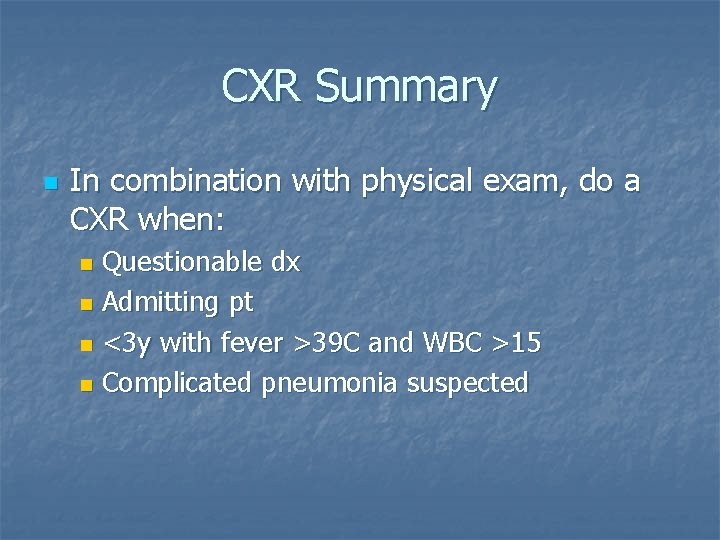
CXR Summary n In combination with physical exam, do a CXR when: Questionable dx n Admitting pt n <3 y with fever >39 C and WBC >15 n Complicated pneumonia suspected n
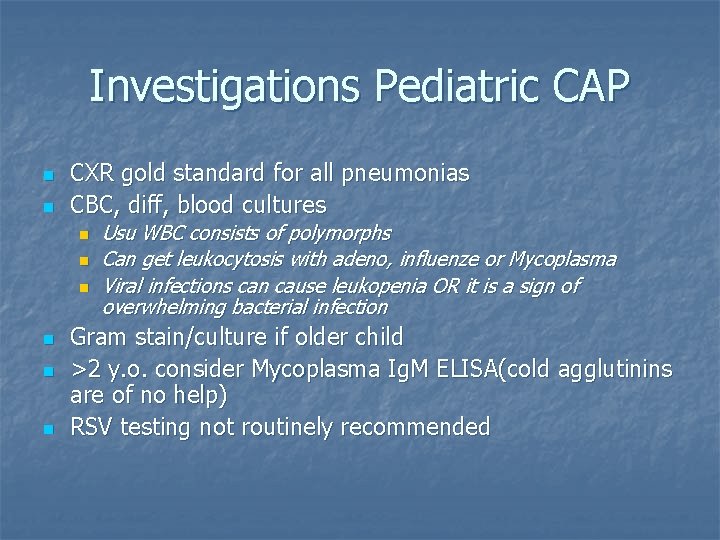
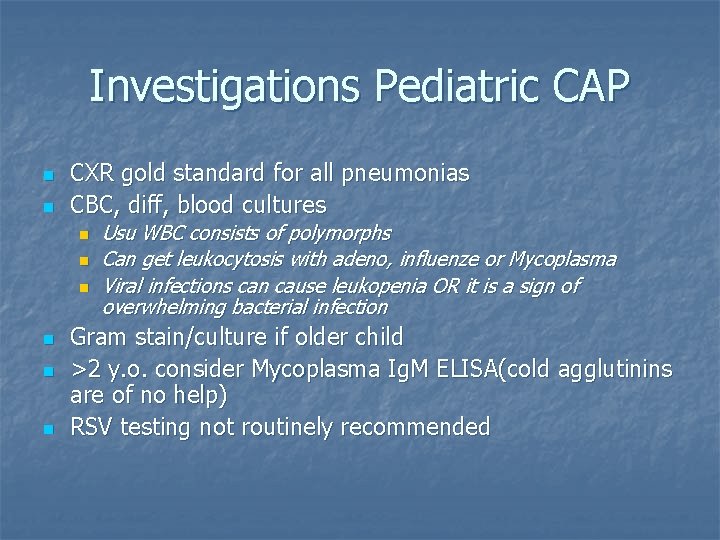
Investigations Pediatric CAP n n CXR gold standard for all pneumonias CBC, diff, blood cultures n n n Usu WBC consists of polymorphs Can get leukocytosis with adeno, influenze or Mycoplasma Viral infections can cause leukopenia OR it is a sign of overwhelming bacterial infection Gram stain/culture if older child >2 y. o. consider Mycoplasma Ig. M ELISA(cold agglutinins are of no help) RSV testing not routinely recommended
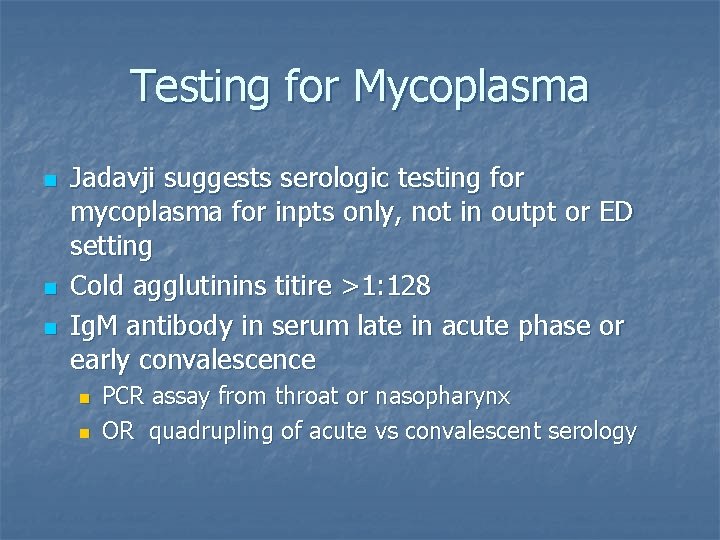
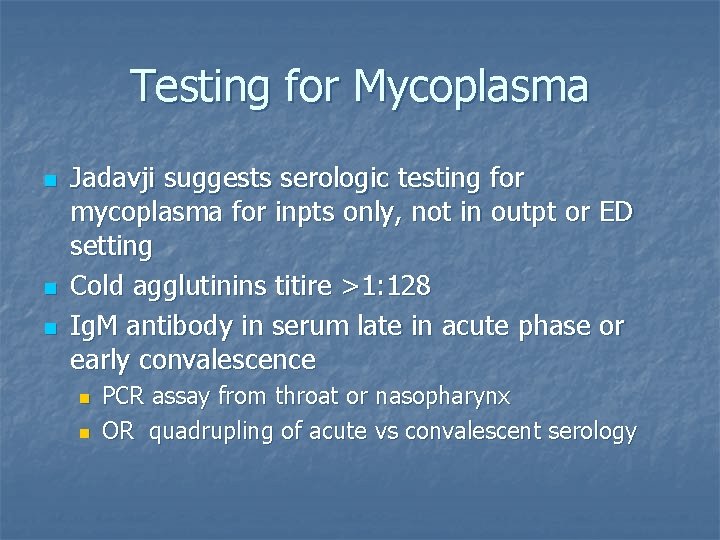
Testing for Mycoplasma n n n Jadavji suggests serologic testing for mycoplasma for inpts only, not in outpt or ED setting Cold agglutinins titire >1: 128 Ig. M antibody in serum late in acute phase or early convalescence n n PCR assay from throat or nasopharynx OR quadrupling of acute vs convalescent serology
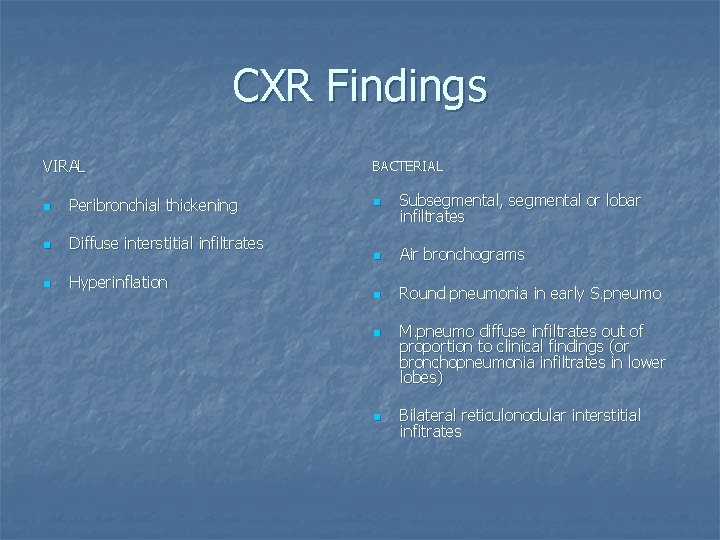
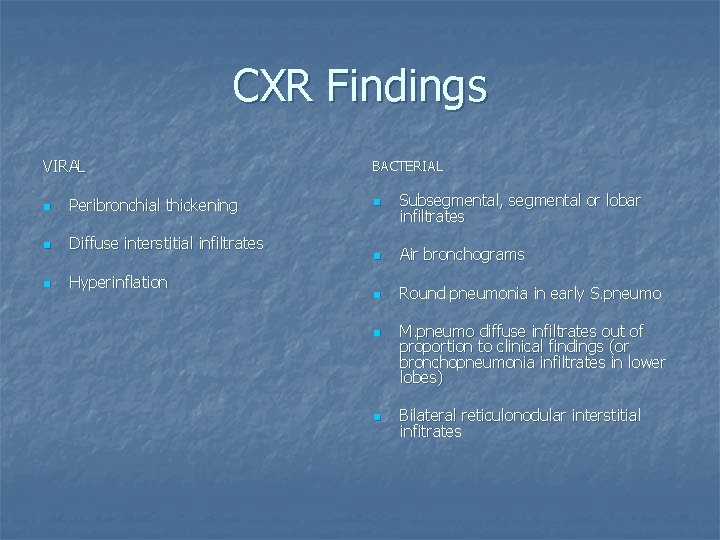
CXR Findings VIRAL n Peribronchial thickening n Diffuse interstitial infiltrates n Hyperinflation BACTERIAL n Subsegmental, segmental or lobar infiltrates n Air bronchograms n Round pneumonia in early S. pneumo n n M. pneumo diffuse infiltrates out of proportion to clinical findings (or bronchopneumonia infiltrates in lower lobes) Bilateral reticulonodular interstitial infitrates
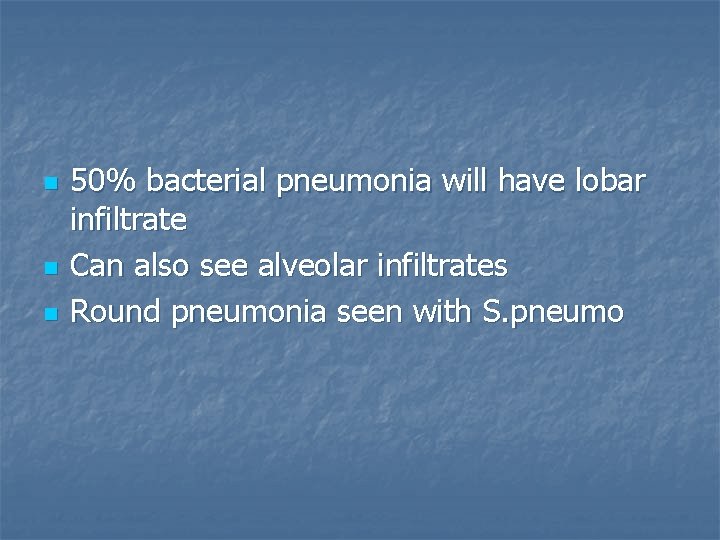
n n n 50% bacterial pneumonia will have lobar infiltrate Can also see alveolar infiltrates Round pneumonia seen with S. pneumo




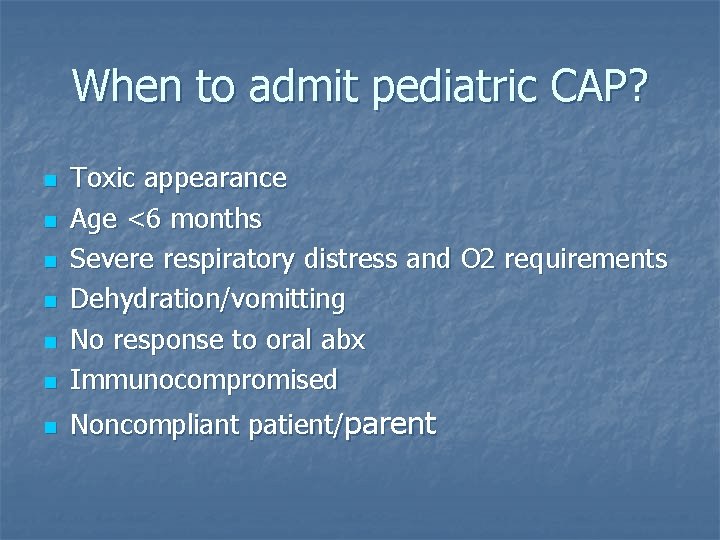
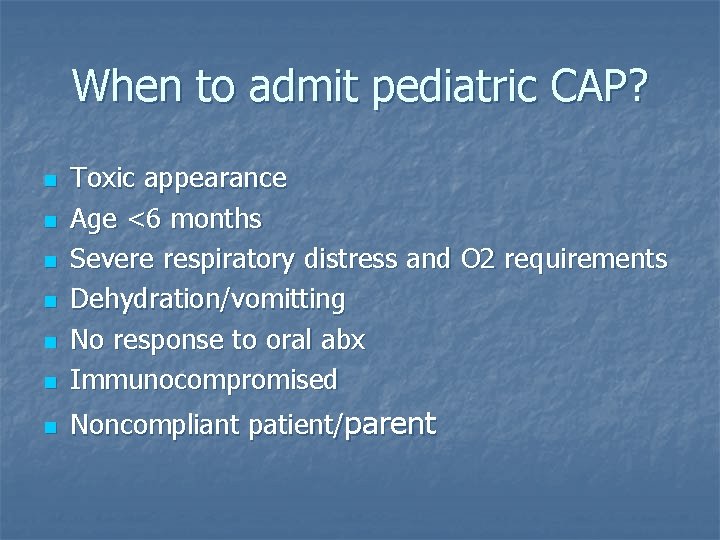
When to admit pediatric CAP? n Toxic appearance Age <6 months Severe respiratory distress and O 2 requirements Dehydration/vomitting No response to oral abx Immunocompromised n Noncompliant patient/parent n n n
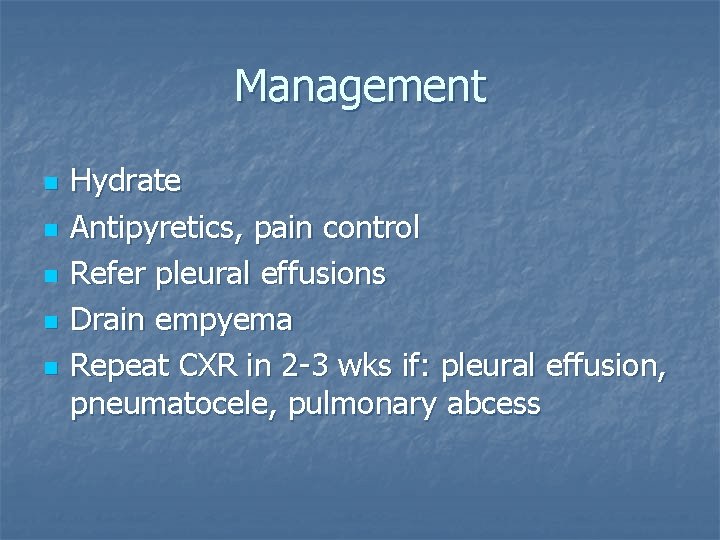
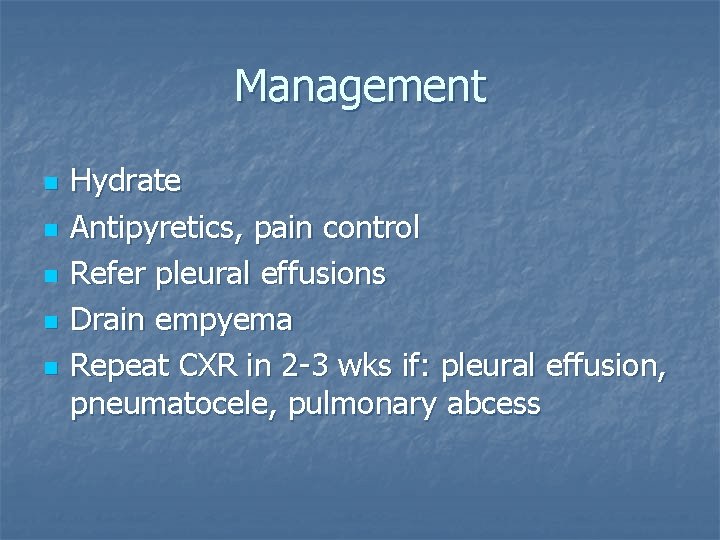
Management n n n Hydrate Antipyretics, pain control Refer pleural effusions Drain empyema Repeat CXR in 2 -3 wks if: pleural effusion, pneumatocele, pulmonary abcess
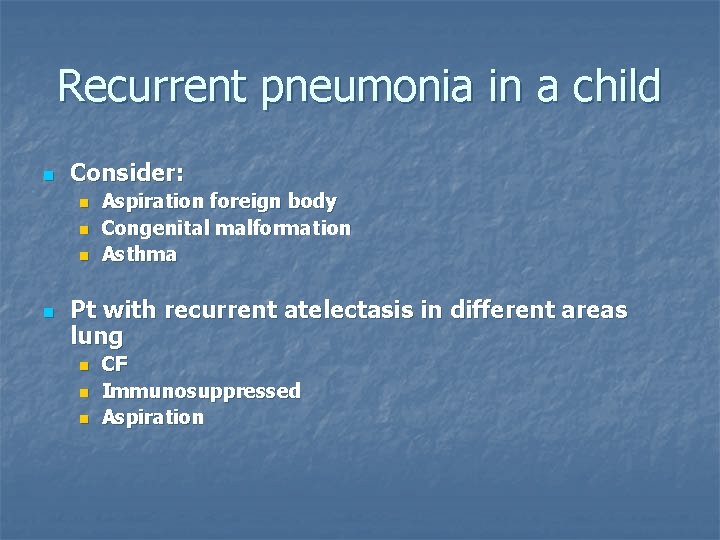
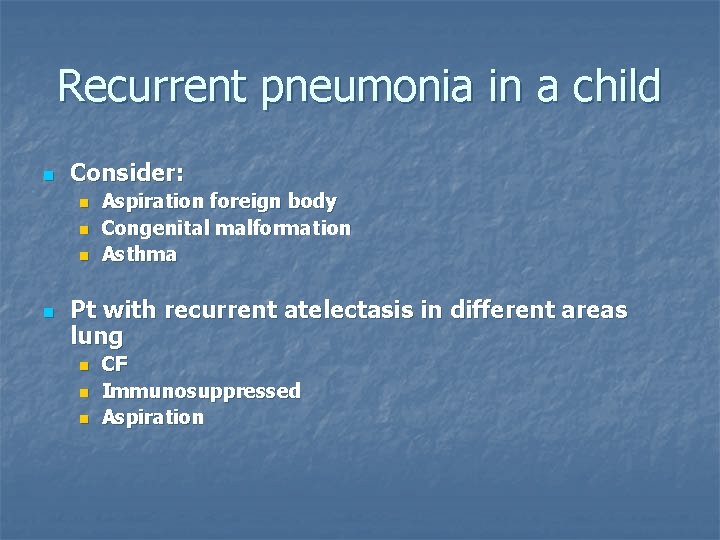
Recurrent pneumonia in a child n Consider: n n Aspiration foreign body Congenital malformation Asthma Pt with recurrent atelectasis in different areas lung n n n CF Immunosuppressed Aspiration
n n Oral treatment adequate IV abx reserved for neonates and pt with severe pneumonia
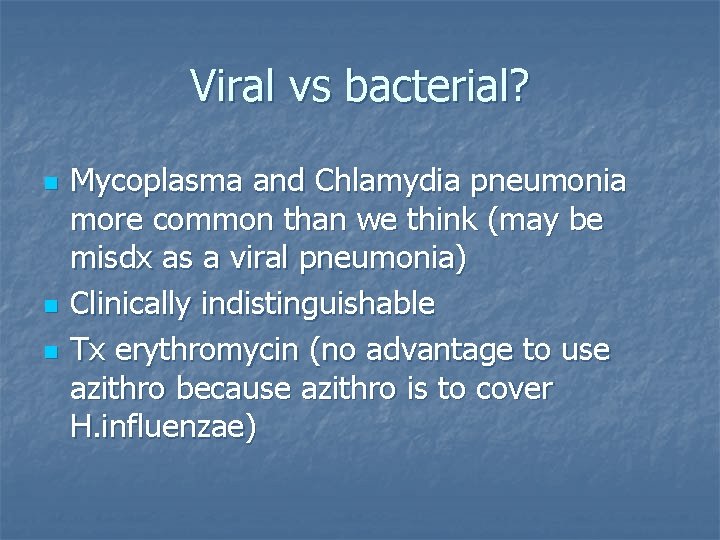
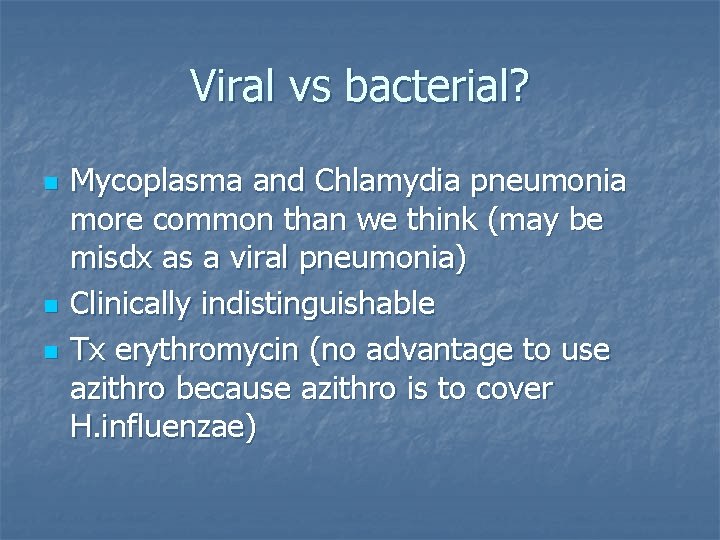
Viral vs bacterial? n n n Mycoplasma and Chlamydia pneumonia more common than we think (may be misdx as a viral pneumonia) Clinically indistinguishable Tx erythromycin (no advantage to use azithro because azithro is to cover H. influenzae)
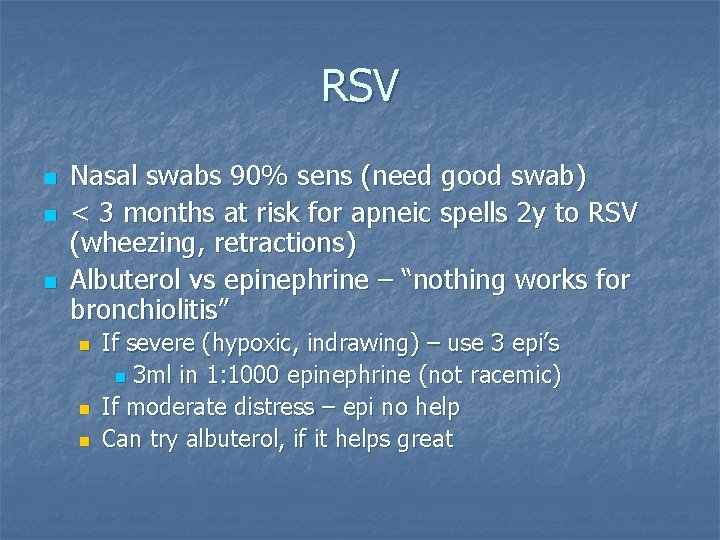
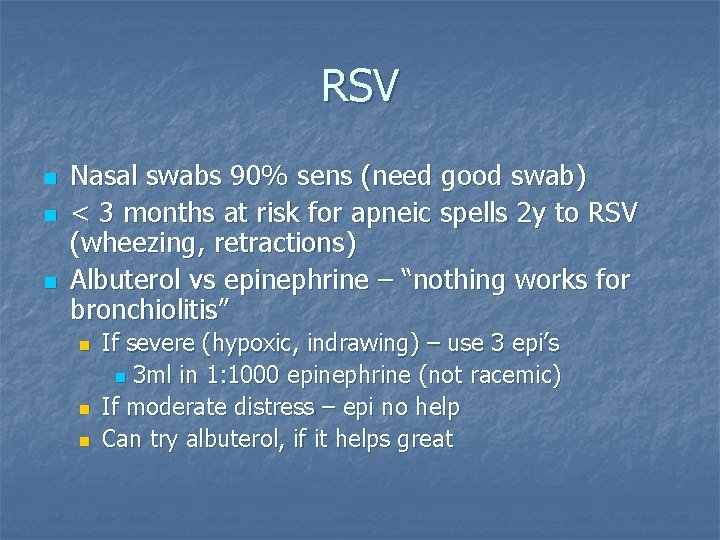
RSV n n n Nasal swabs 90% sens (need good swab) < 3 months at risk for apneic spells 2 y to RSV (wheezing, retractions) Albuterol vs epinephrine – “nothing works for bronchiolitis” n n n If severe (hypoxic, indrawing) – use 3 epi’s n 3 ml in 1: 1000 epinephrine (not racemic) If moderate distress – epi no help Can try albuterol, if it helps great
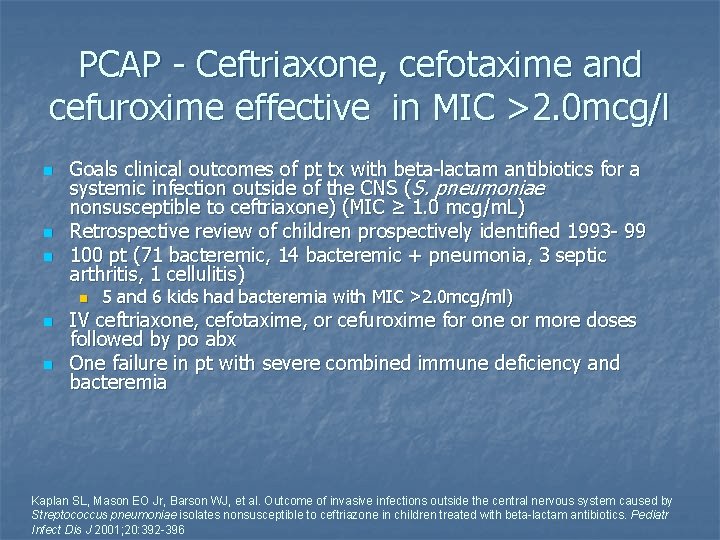
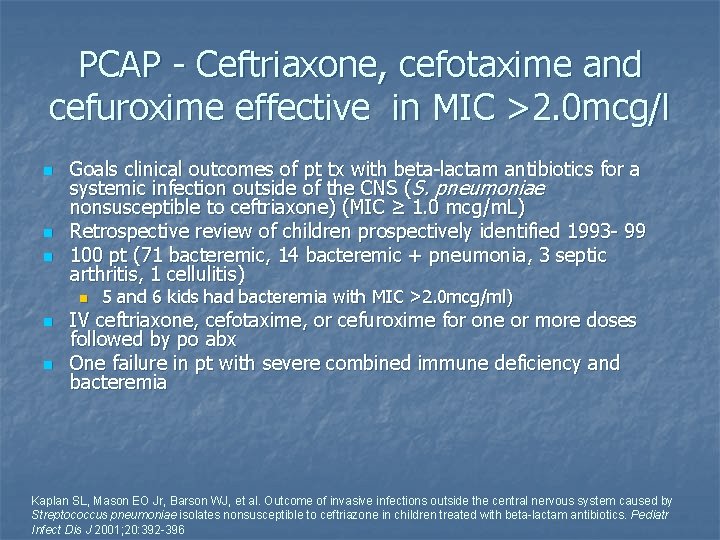
PCAP - Ceftriaxone, cefotaxime and cefuroxime effective in MIC >2. 0 mcg/l n n n Goals clinical outcomes of pt tx with beta-lactam antibiotics for a systemic infection outside of the CNS (S. pneumoniae nonsusceptible to ceftriaxone) (MIC ≥ 1. 0 mcg/m. L) Retrospective review of children prospectively identified 1993 - 99 100 pt (71 bacteremic, 14 bacteremic + pneumonia, 3 septic arthritis, 1 cellulitis) n n n 5 and 6 kids had bacteremia with MIC >2. 0 mcg/ml) IV ceftriaxone, cefotaxime, or cefuroxime for one or more doses followed by po abx One failure in pt with severe combined immune deficiency and bacteremia Kaplan SL, Mason EO Jr, Barson WJ, et al. Outcome of invasive infections outside the central nervous system caused by Streptococcus pneumoniae isolates nonsusceptible to ceftriazone in children treated with beta-lactam antibiotics. Pediatr Infect Dis J 2001; 20: 392 -396

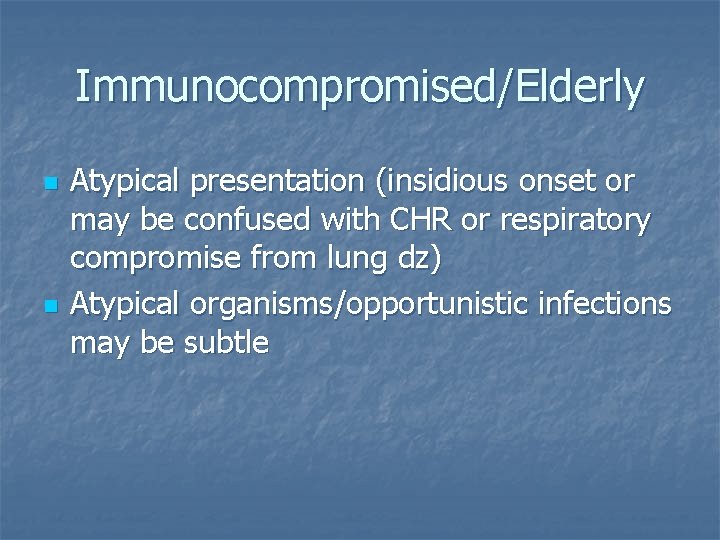
Immunocompromised/Elderly n n Atypical presentation (insidious onset or may be confused with CHR or respiratory compromise from lung dz) Atypical organisms/opportunistic infections may be subtle
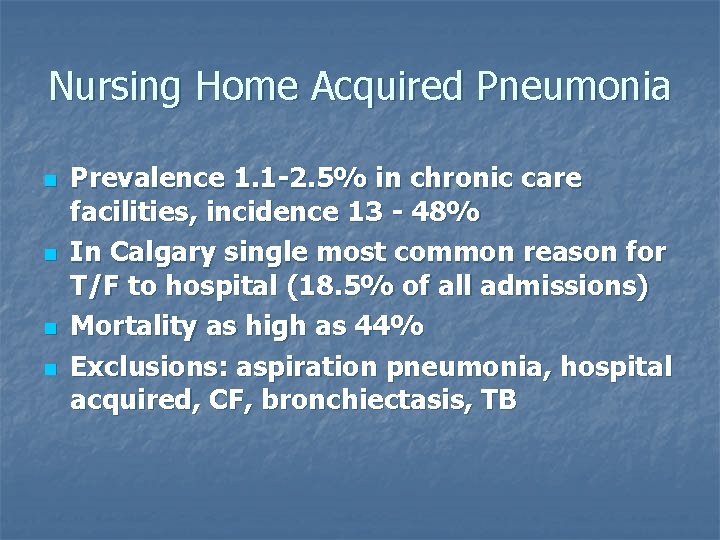
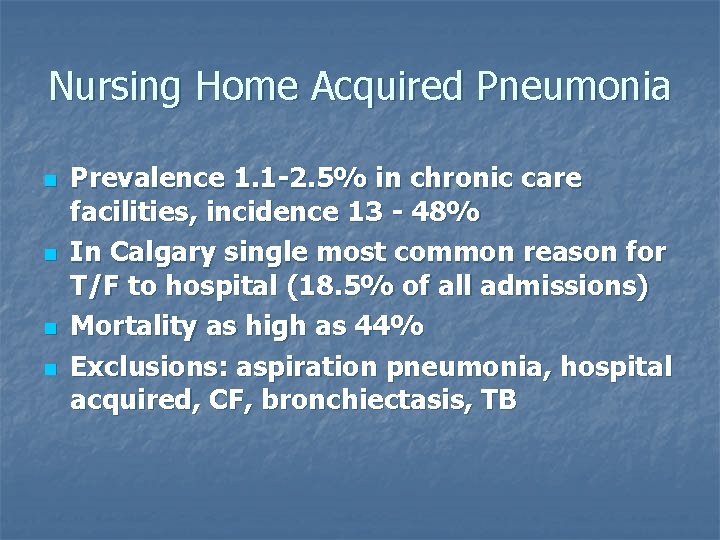
Nursing Home Acquired Pneumonia n n Prevalence 1. 1 -2. 5% in chronic care facilities, incidence 13 - 48% In Calgary single most common reason for T/F to hospital (18. 5% of all admissions) Mortality as high as 44% Exclusions: aspiration pneumonia, hospital acquired, CF, bronchiectasis, TB
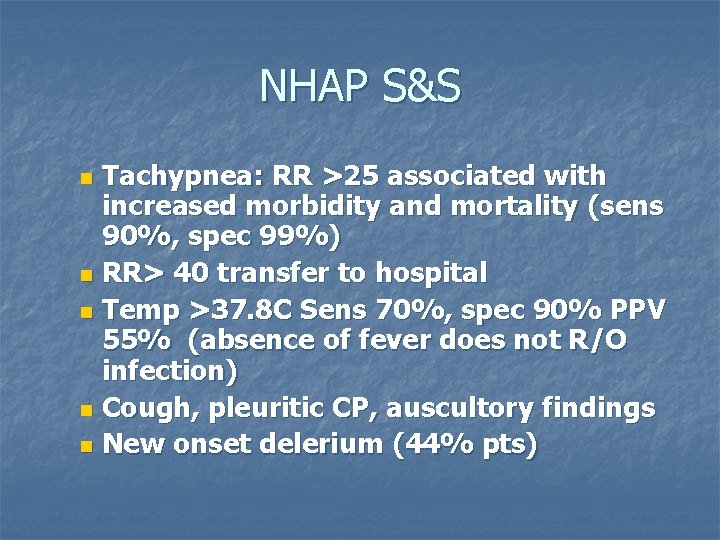
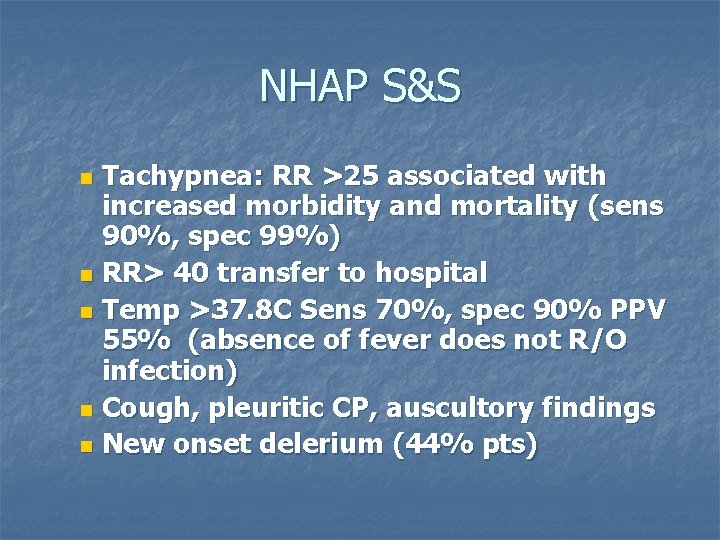
NHAP S&S Tachypnea: RR >25 associated with increased morbidity and mortality (sens 90%, spec 99%) n RR> 40 transfer to hospital n Temp >37. 8 C Sens 70%, spec 90% PPV 55% (absence of fever does not R/O infection) n Cough, pleuritic CP, auscultory findings n New onset delerium (44% pts) n
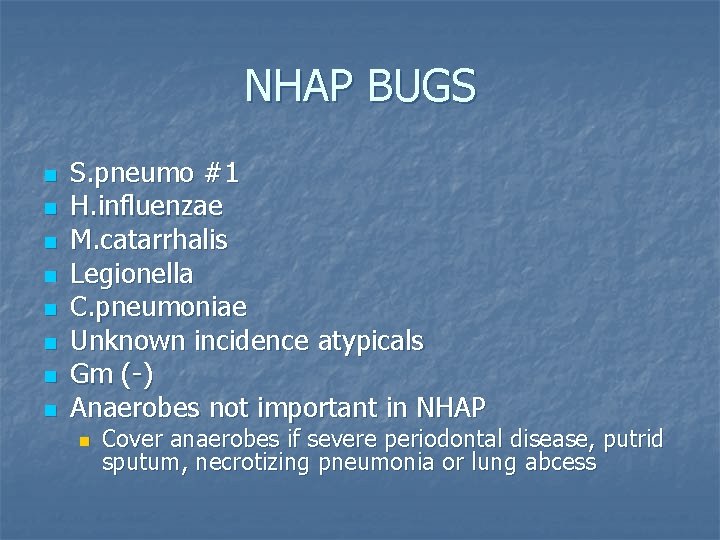
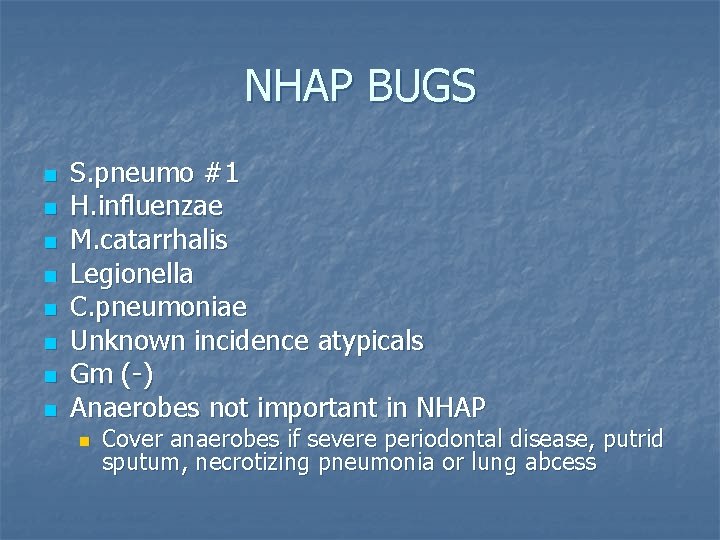
NHAP BUGS n n n n S. pneumo #1 H. influenzae M. catarrhalis Legionella C. pneumoniae Unknown incidence atypicals Gm (-) Anaerobes not important in NHAP n Cover anaerobes if severe periodontal disease, putrid sputum, necrotizing pneumonia or lung abcess
Wt loss in elderly n Wt loss >5 -10% associated w increased mortality n >5% in 30 days or 10% in 6 months

NHAP Tx n n Amoxil first line if still in home Add macrolide if severe pneumonia or underlying lung dz (keep in mind 10% S. pneumo resistance to macrolides, may not cover H. flu) n n n Cefuroxime if worried about Staph Doxy is an excellent choice, low R Fluoroquinolones if failed intial therapy or multiple comorbidities. Try to avoid to decrease resistance formation. (levo overused in NH in particular)
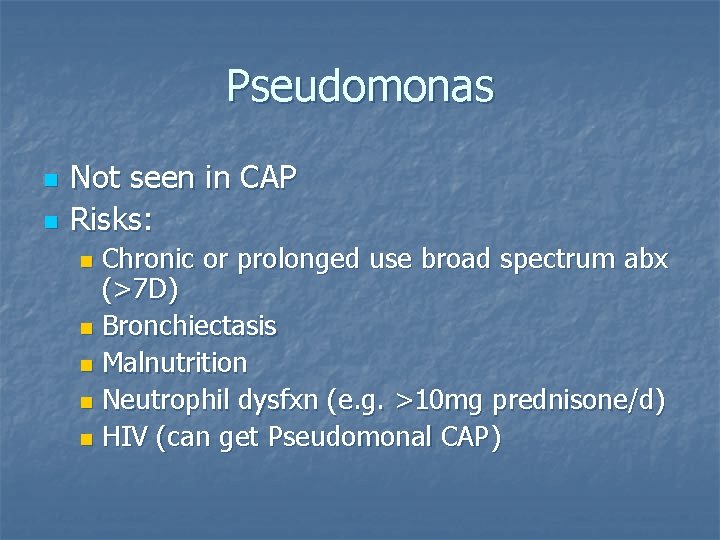
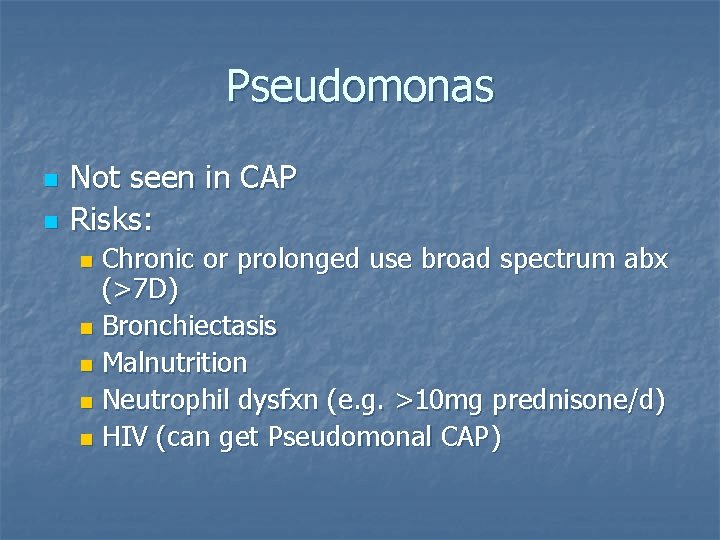
Pseudomonas n n Not seen in CAP Risks: Chronic or prolonged use broad spectrum abx (>7 D) n Bronchiectasis n Malnutrition n Neutrophil dysfxn (e. g. >10 mg prednisone/d) n HIV (can get Pseudomonal CAP) n
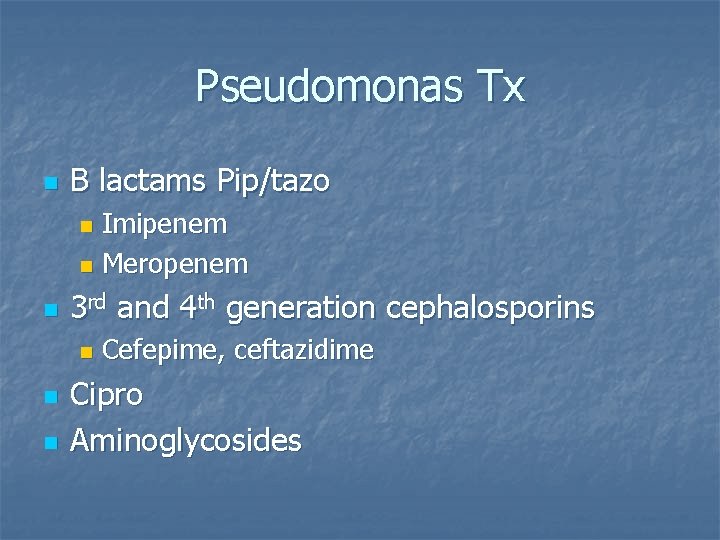
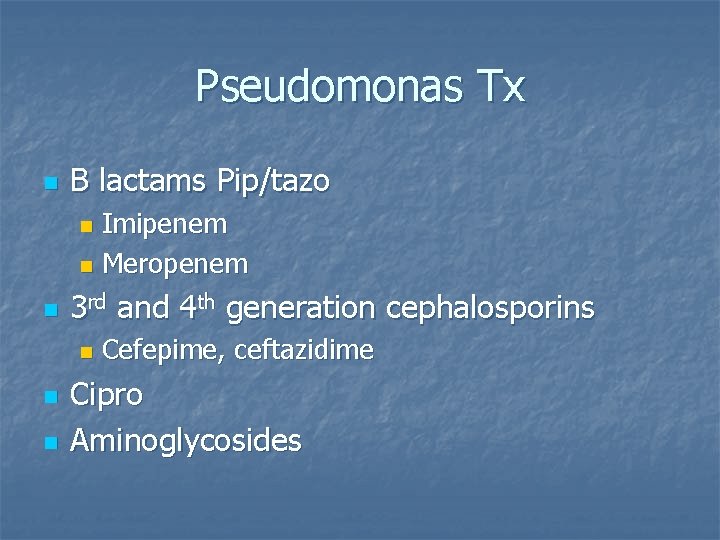
Pseudomonas Tx n B lactams Pip/tazo Imipenem n Meropenem n n 3 rd and 4 th generation cephalosporins n n n Cefepime, ceftazidime Cipro Aminoglycosides
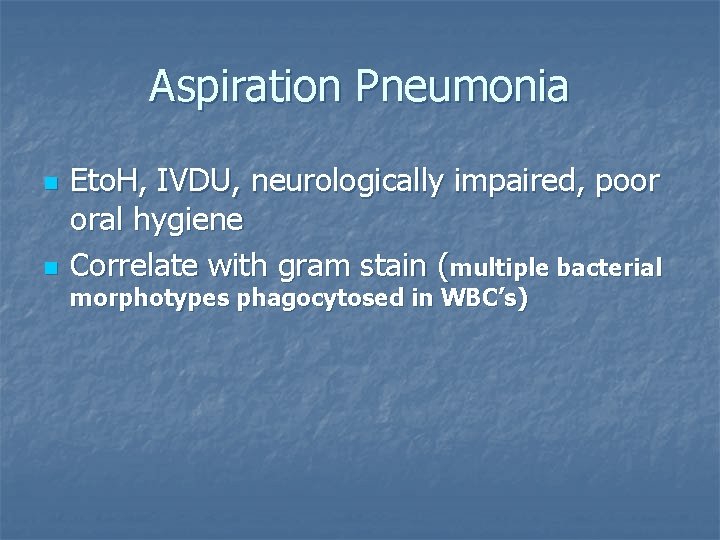
Aspiration Pneumonia n n Eto. H, IVDU, neurologically impaired, poor oral hygiene Correlate with gram stain (multiple bacterial morphotypes phagocytosed in WBC’s)
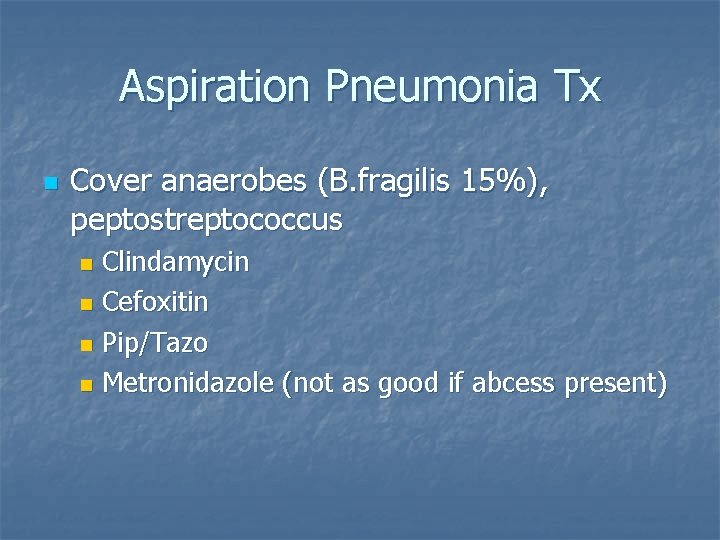
Aspiration Pneumonia Tx n Cover anaerobes (B. fragilis 15%), peptostreptococcus Clindamycin n Cefoxitin n Pip/Tazo n Metronidazole (not as good if abcess present) n


 Caroline kowal
Caroline kowal Respiratory zone and conducting zone
Respiratory zone and conducting zone Gatunki literackie młodej polski
Gatunki literackie młodej polski Symbol kl
Symbol kl Dr lionel kowal
Dr lionel kowal Drug rehab firth
Drug rehab firth Witold kowal ue wroc
Witold kowal ue wroc Renata kowal
Renata kowal Dr lionel kowal
Dr lionel kowal Jak wygląda kowal
Jak wygląda kowal Agata kowal
Agata kowal Lionel kowal
Lionel kowal Minute taking made easy
Minute taking made easy Magi household
Magi household The magic by rhonda byrne review
The magic by rhonda byrne review Evolut sizing chart
Evolut sizing chart Rhonda keen
Rhonda keen Kippi vaught
Kippi vaught Dr rhonda nelson
Dr rhonda nelson Greatest velocity change
Greatest velocity change Rhonda sexton
Rhonda sexton Lovk ness monster
Lovk ness monster What is proximity control
What is proximity control Less suffix words
Less suffix words Classification of acute gingival infections
Classification of acute gingival infections Infections opportunistes digestives
Infections opportunistes digestives Jacob kounin theory
Jacob kounin theory Christopher chase
Christopher chase Lene ness jensen
Lene ness jensen Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Rural broadband solutions in loch ness
Rural broadband solutions in loch ness Methotrexate yeast infection
Methotrexate yeast infection Loch ness odjuret
Loch ness odjuret Eye infections
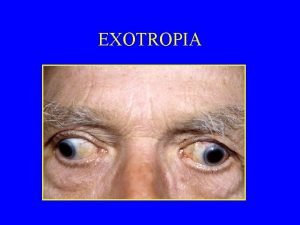
Eye infections Storch infections
Storch infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Monstruo lago ness
Monstruo lago ness Bone and joint infections
Bone and joint infections Elsa fayer seins
Elsa fayer seins 5 adverbs
5 adverbs Ness
Ness Genital infections
Genital infections Storch infections
Storch infections множественное число ship
множественное число ship Opportunistic infections
Opportunistic infections Salmonella life cycle
Salmonella life cycle Example of ripple effect in classroom
Example of ripple effect in classroom Johnson and johnson botnet infections
Johnson and johnson botnet infections Opportunistic infections
Opportunistic infections Amber blumling
Amber blumling Postpartum infections
Postpartum infections Preceptor ship
Preceptor ship Thank you note to preceptor after orientation
Thank you note to preceptor after orientation A nurse preceptor is orienting a newly licensed nurse
A nurse preceptor is orienting a newly licensed nurse Preceptor de nero
Preceptor de nero Preceptor
Preceptor One minute preceptor method
One minute preceptor method Sanford avner
Sanford avner Bad preceptor
Bad preceptor Thank you note to preceptor after orientation
Thank you note to preceptor after orientation Tipos de acompañamiento escolar
Tipos de acompañamiento escolar Harvard preceptor
Harvard preceptor Preceptor evaluation
Preceptor evaluation Olc heartfulness
Olc heartfulness Spain royal family tree
Spain royal family tree Jacobean and caroline age
Jacobean and caroline age Me llamo victoria
Me llamo victoria Caroline neckebroeck
Caroline neckebroeck Aportaciones de caroline herschel
Aportaciones de caroline herschel Caroline haslam
Caroline haslam Caroline nyczak
Caroline nyczak The widow at windsor summary sparknotes
The widow at windsor summary sparknotes Caroline liqui lung
Caroline liqui lung Caroline costongs
Caroline costongs Caroline ray casting
Caroline ray casting Caroline inglis
Caroline inglis Dr caroline matthes
Dr caroline matthes Caroline schönning
Caroline schönning Caroline herschel siblings
Caroline herschel siblings Caroline neckebroeck
Caroline neckebroeck