Preop evaluation for pulmonary surgery Dr S Parthasarathy


- Slides: 36
Preop evaluation for pulmonary surgery Dr. S. Parthasarathy MD. , DA. , DNB, MD (Acu), Dip. Diab. Dip. Software statistics Ph. D ( physiology), IDRA , FICA
Why actually we need this topic ? • In US 30000 lung resection surgeries / year • Because newer gadgets have made diagnosis earlier and surgery better !! • Is it operable with acceptable risk ? • Not making fit alone • We can suggest to the surgical team !
Yes there are problems !! • Major respiratory complications— atelectasis, pneumonia, and respiratory failure — occur in 15% to 20% of • patients and account for the majority of the expected 3% to 4% mortality rate.
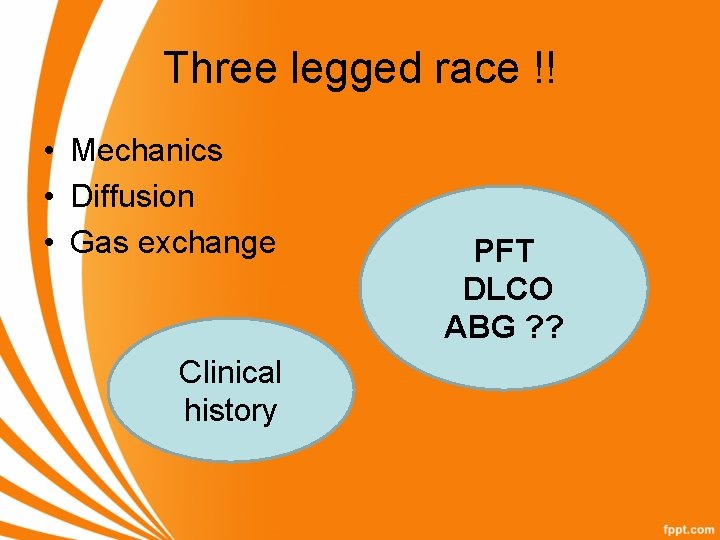
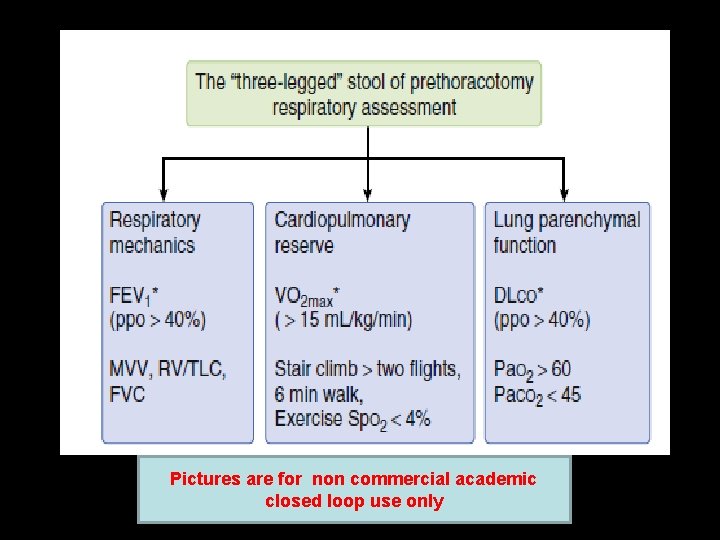
Three legged race !! • Mechanics • Diffusion • Gas exchange Clinical history PFT DLCO ABG ? ?
• • • Functional capacity Smoker H/O COPD, bronchiectasis Co existing diseases Pulmonary hypertension and cardiac Tuberculosis , steroids , ATT and liver disease • Metastasis •

Other history • The presence of wheezing, rales, rhonchi, or other abnormal breath sounds suggests the need for further medical intervention– • Clubbing dysphagia horner s syndrome hoarseness • ECG changes – pulmonary hypertension • Or Low QRS complexes – hyperinflation
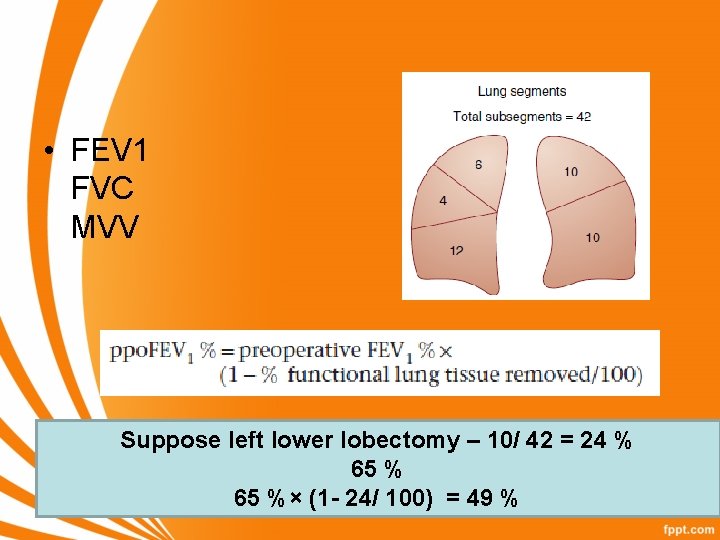
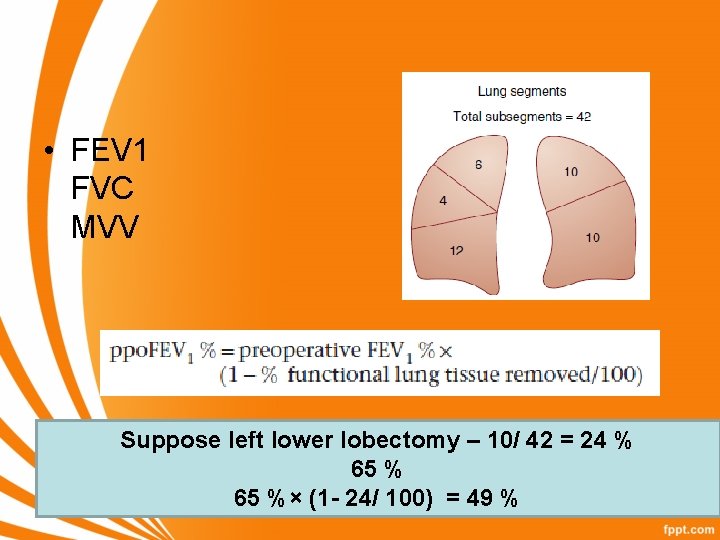
• FEV 1 FVC MVV Suppose left lower lobectomy – 10/ 42 = 24 % 65 %× (1 - 24/ 100) = 49 %
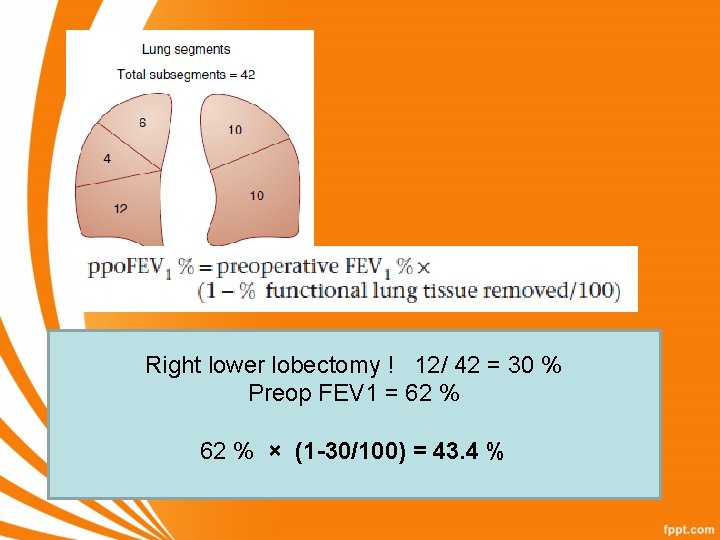
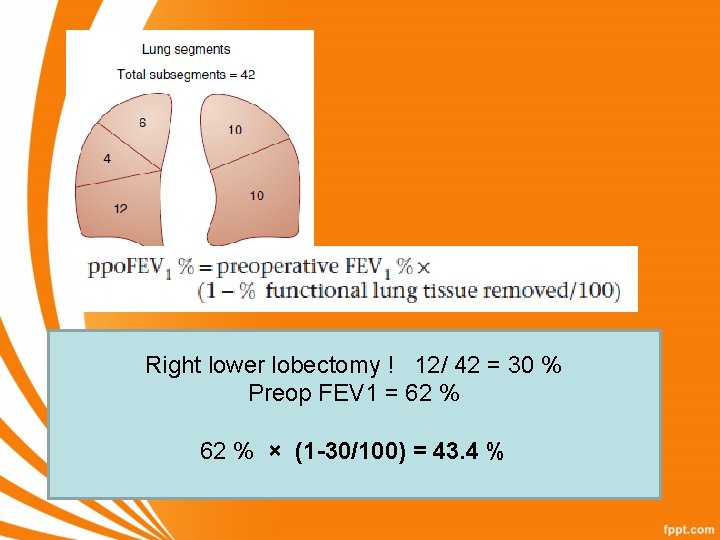
Right lower lobectomy ! 12/ 42 = 30 % Preop FEV 1 = 62 % × (1 -30/100) = 43. 4 %
PEFR - simple • PEF of less than 200 L/m indicates that effective coughing is difficult and pulmonary complications rate are high
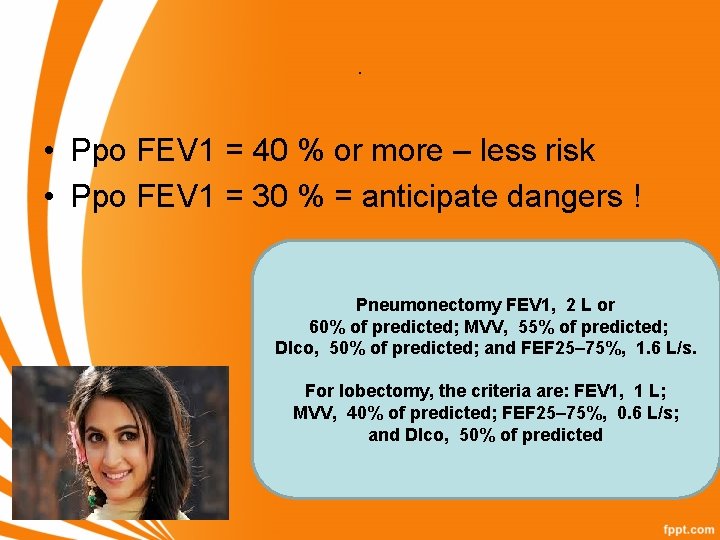
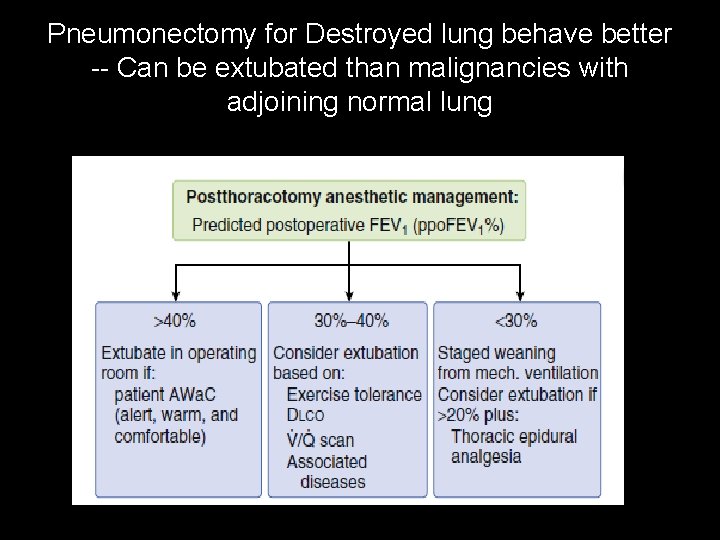
. • Ppo FEV 1 = 40 % or more – less risk • Ppo FEV 1 = 30 % = anticipate dangers ! Pneumonectomy FEV 1, 2 L or 60% of predicted; MVV, 55% of predicted; Dlco, 50% of predicted; and FEF 25– 75%, 1. 6 L/s. For lobectomy, the criteria are: FEV 1, 1 L; MVV, 40% of predicted; FEF 25– 75%, 0. 6 L/s; and Dlco, 50% of predicted
Problem in PFT in India !! • Reliability of the test !! • Patients to understand repeat ! • An easy 20 % rise we have seen if we do it again after ten minutes • Believe the test 100% only if we are sure
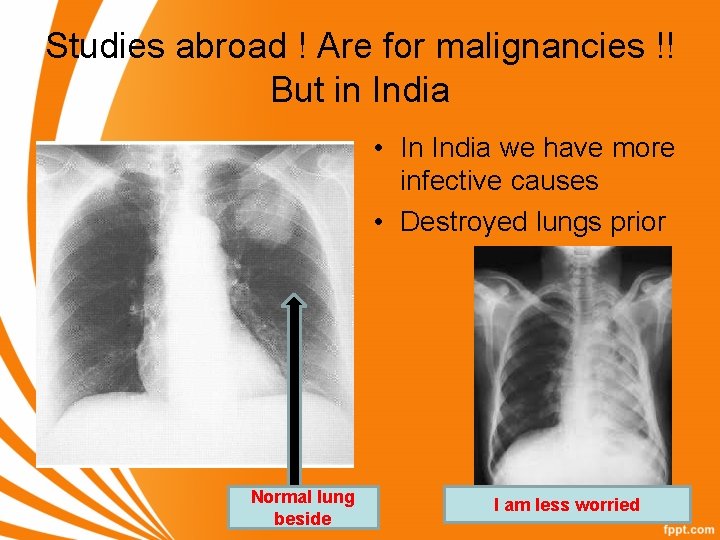
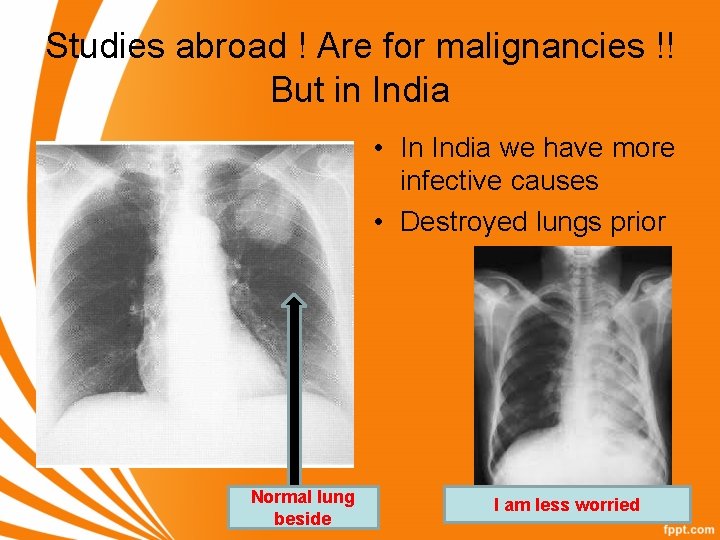
Studies abroad ! Are for malignancies !! But in India • In India we have more infective causes • Destroyed lungs prior Normal lung beside I am less worried
DLCO • DLCO, also known as the TLCO, is a measurement of the conductance or ease of transfer for CO molecules from alveolar gas to the hemoglobin of the red blood cells in the pulmonary circulation. • It often is helpful for evaluating the presence of possible parenchymal lung disease when spirometry and/or lung volume determinations suggest a reduced vital capacity, RV, and/or TLC. -- ml/min/Hg
Single breath wash out technique • A ppo DLco less than 40% predicted correlates with both increased respiratory and cardiac complications and is usually independent of the FEV 1. • Preop chemo given – DLCO better than FEV 1
ABG • Arterial blood gas data such as partial pressure of oxygen in the blood (Pa. O 2) less than 60 mm Hg or • partial pressure of carbon dioxide in the blood (Pa. CO 2) greater than 45 mm Hg have been used as cutoff values for pulmonary resection
Cardiopulmonary Interaction • maximal oxygen consumption (VO 2 max) is the most useful predictor of post thoracotomy outcome. • Less than 15 ml / kg/min – risks • Less than 10 ml/kg/min – danger
6 minute walk test • • Distance / 30 is the approx VO 2 max Example 600 meters in 6 minutes 600/30 = 20 ml/kg/minute – OK Flight of stairs more two – 12 ml/kg/minute
Prince et al • A new index, postoperative multiplying designated product the (PPP), percentage the predicted obtained of by predicted postoperative FEV 1 by the percentage of predicted postoperative DLCO • < 1650 – risk is more
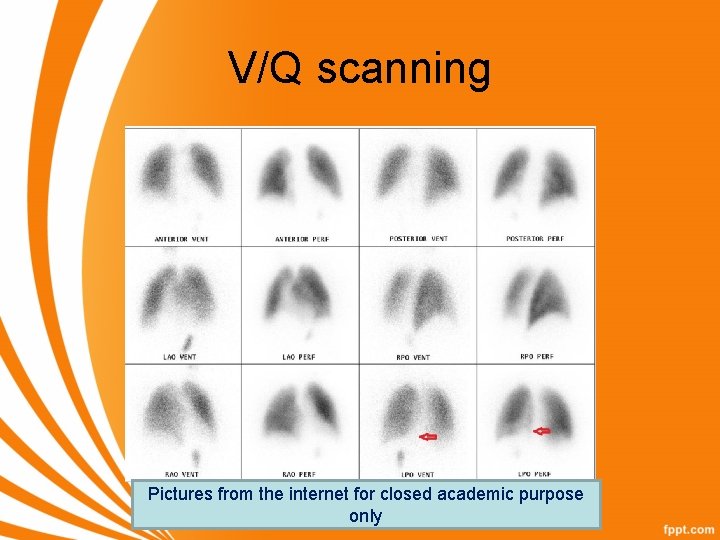
V/Q scanning • The difference between the ventilation and perfusion study in predicting postoperative loss of function was not significant although the predicted values from the ventilation study tended to be slightly closer to the postoperative spirometric measurements. • Yes we can do !
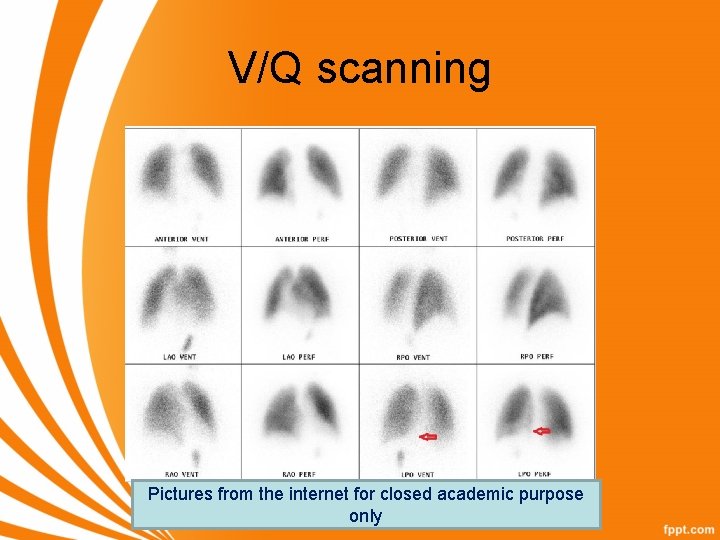
V/Q scanning Pictures from the internet for closed academic purpose only
• Those who reach a walk distance >400 m on the shuttle walk test or are able to climb >22 m on the stair climbing test are also considered at low risk
Everything is not OK • Differential lung tests • • tests assessing differential lung function include broncho spirometry, lateral position testing, total unilateral pulmonary artery occlusion. Costly and laborious equipment
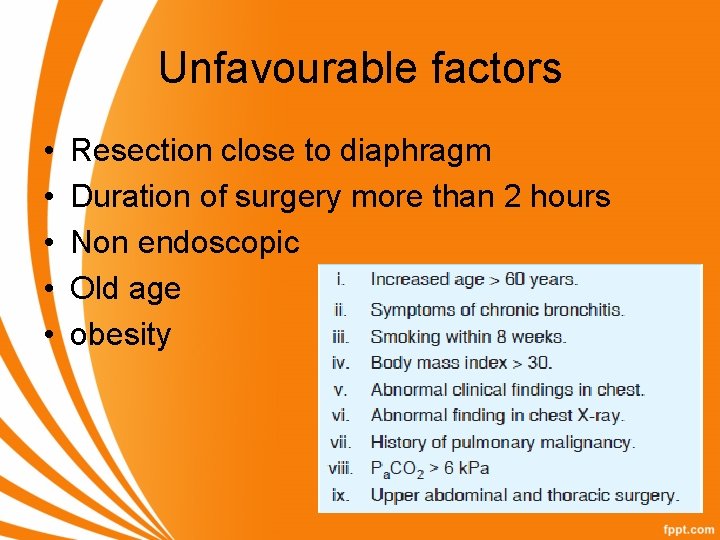
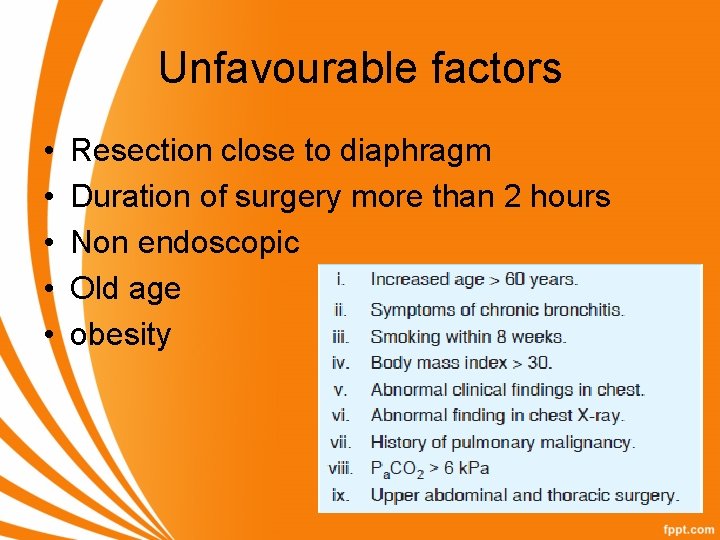
Unfavourable factors • • • Resection close to diaphragm Duration of surgery more than 2 hours Non endoscopic Old age obesity
Three legged race !!
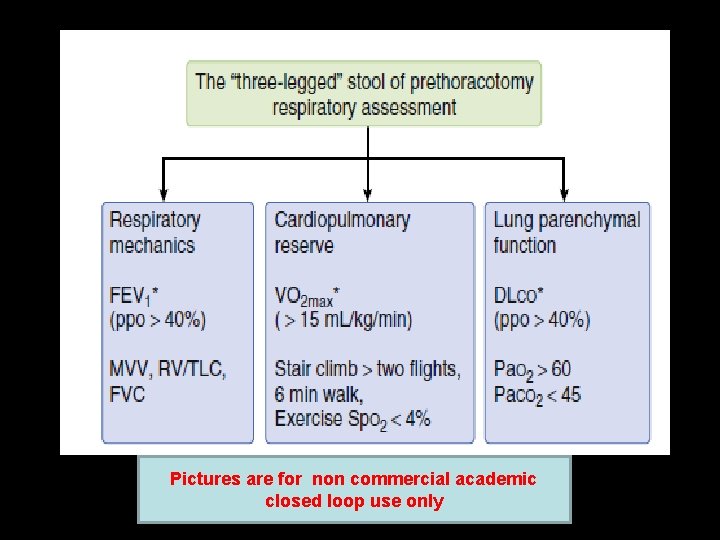
Pictures are for non commercial academic closed loop use only

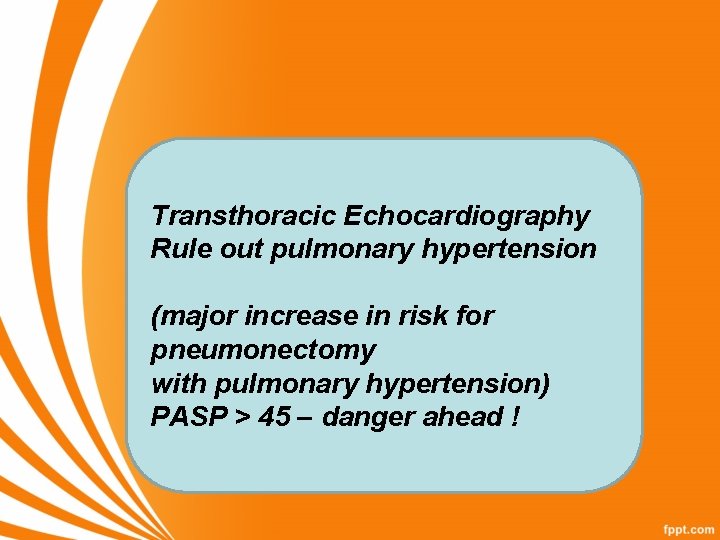
Transthoracic Echocardiography Rule out pulmonary hypertension (major increase in risk for pneumonectomy with pulmonary hypertension) PASP > 45 – danger ahead !
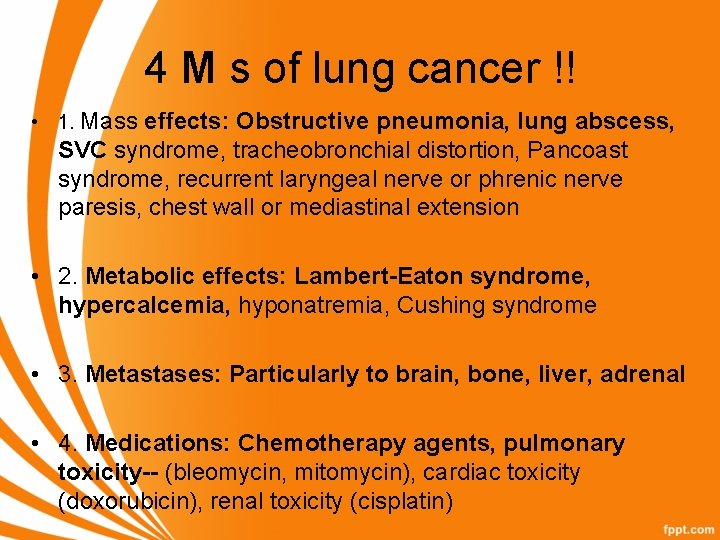
4 M s of lung cancer !! • 1. Mass effects: Obstructive pneumonia, lung abscess, SVC syndrome, tracheobronchial distortion, Pancoast syndrome, recurrent laryngeal nerve or phrenic nerve paresis, chest wall or mediastinal extension • 2. Metabolic effects: Lambert-Eaton syndrome, hypercalcemia, hyponatremia, Cushing syndrome • 3. Metastases: Particularly to brain, bone, liver, adrenal • 4. Medications: Chemotherapy agents, pulmonary toxicity-- (bleomycin, mitomycin), cardiac toxicity (doxorubicin), renal toxicity (cisplatin)
Dangers of bullae • Risk of rupture with positive pressure and ? pneumothorax • Increased dead space • Compression of healthy adjacent lung
Thoracoscopy – be slightly lineant • spirometry threshold for increased risk for VATS seems to be a ppo. FEV 1 of 30% versus 40% for open thoracotomy
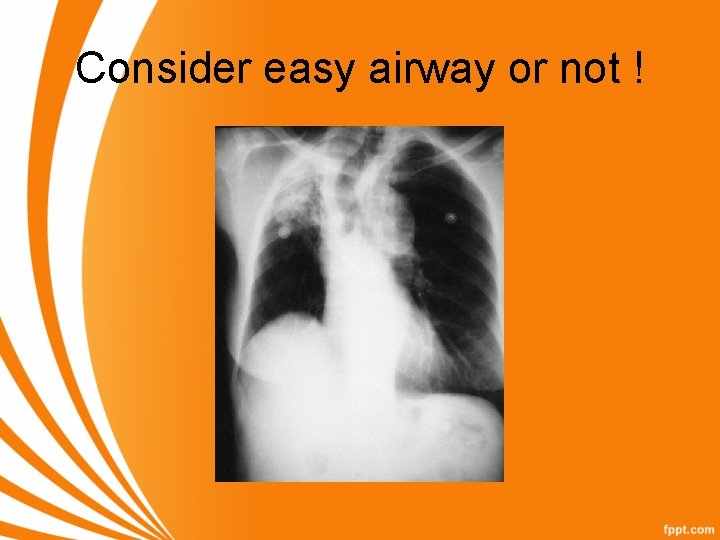
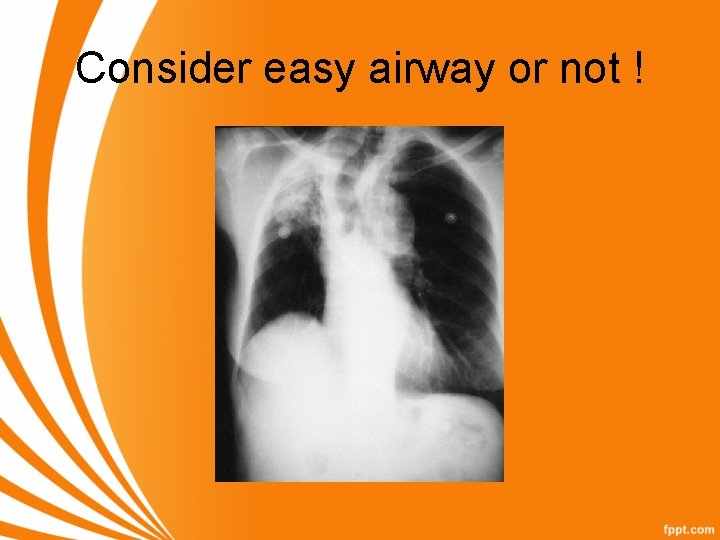
Consider easy airway or not !
Other routine tests XRay chest PA CT chest
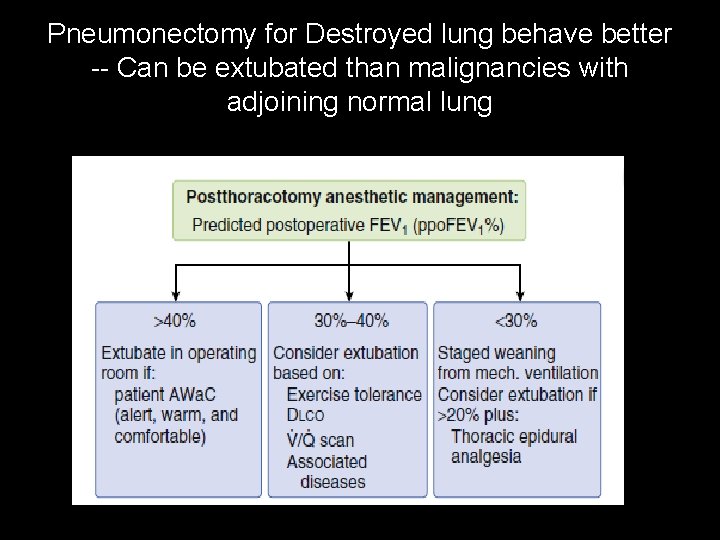
Pneumonectomy for Destroyed lung behave better -- Can be extubated than malignancies with adjoining normal lung
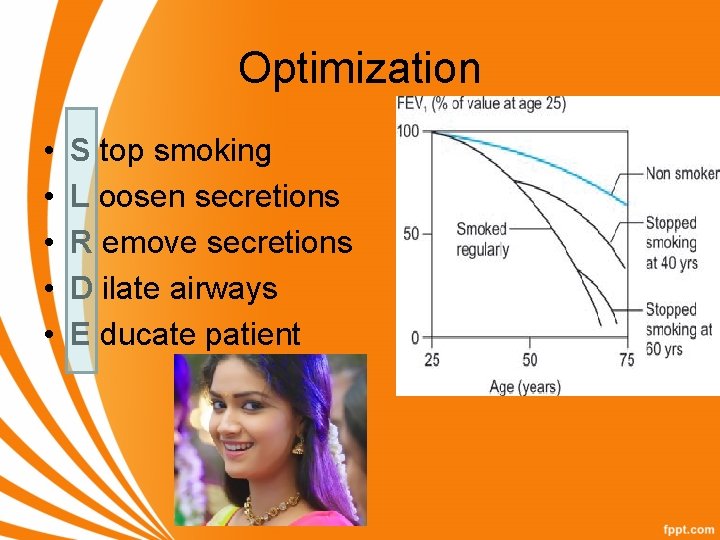
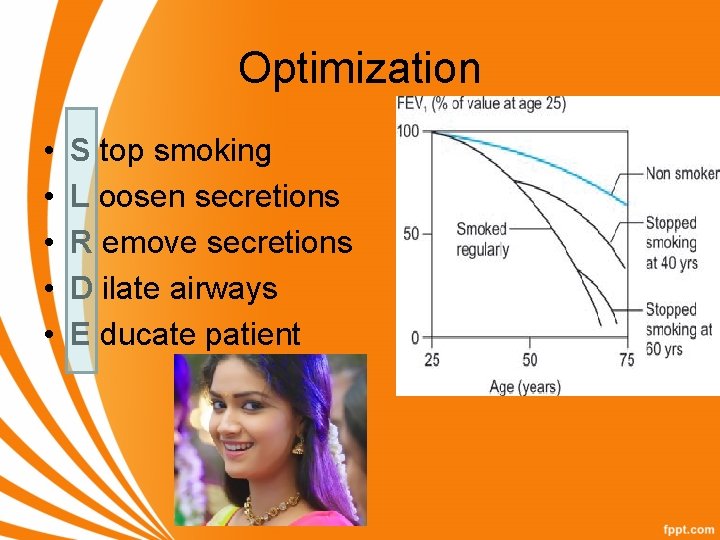
Optimization • • • S top smoking L oosen secretions R emove secretions D ilate airways E ducate patient
SLRDE • Pulmonary complications are decreased in thoracic surgical patients who cease smoking for more than 4 weeks before surgery… • Administer mucolytics, Hydrate well • Antibiotics • bronchodilators • Physiotherapy , incentive spirometry postop analgesia
Summary • • History Xray , CT, routine test PFT PPO FEV 1 Dlco , VQ scan CPET Risk factors SLRDE Thank you