PreOp Information During COVID19 for Spine Surgery Presented







- Slides: 56
Pre-Op Information During COVID-19 for Spine Surgery Presented by: April Asuncion Higgins, BSN, RN, CMSRN & Christine Griffin, RN
Time Sensitive Tasks to Complete Before Your Surgery Ø Nasal swab for MRSA/MSSA Ø Must be completed before surgery, on the same day as your COVID-19 test Ø COVID-19 Testing: at GBMC’s COVID Testing Site Ø 3 -7 days before surgery Ø Prevention of COVID-19 Exposure Ø Guidelines to follow Ø Preop CHG Wash Kit with directions Ø Begin 3 nights before surgery
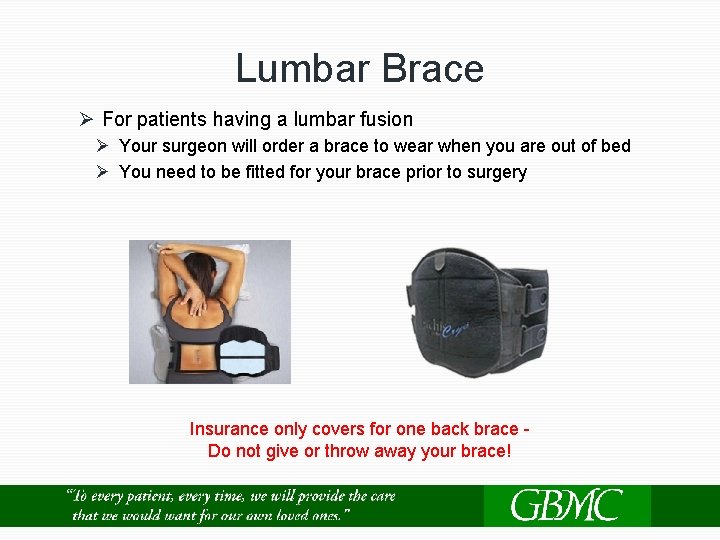
Getting Fitted For A Back Brace Ø Patient of Dr. Rami or Dr. Iguchi Ø If you received a prescription for a lumbar back brace for after a lumbar fusion surgery Ø Must get fitted for your brace prior to surgery Ø The Medical supply company will reach out to you to arrange a fitting date and time (Bring brace with you when you come in for surgery) Ø Patients of Ortho. MD - Dr. Buraimoh Ø Check with surgeon and/or the office to determine if a lumbar back brace is needed Ø They will fit you for a brace at the office if needed
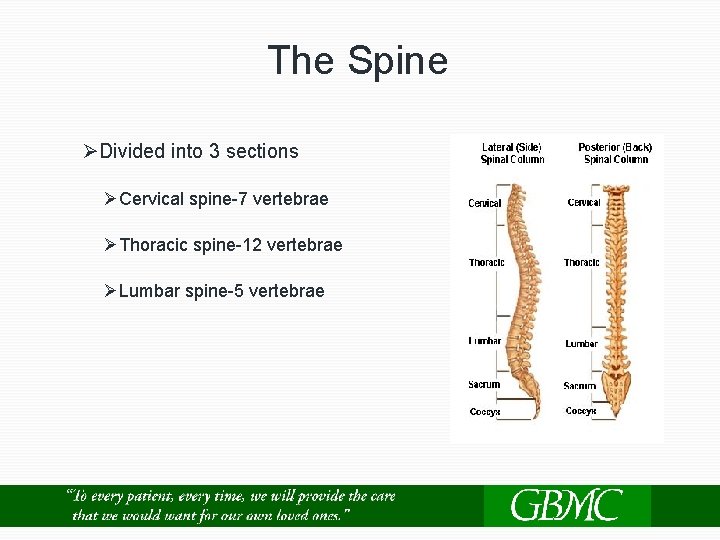
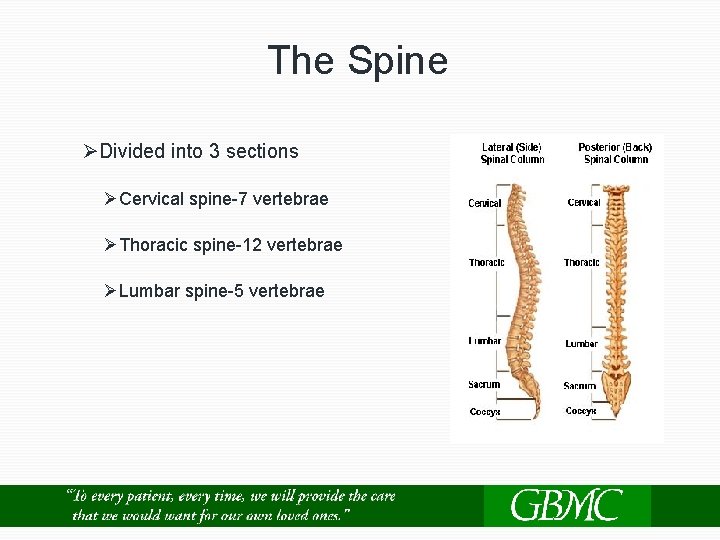
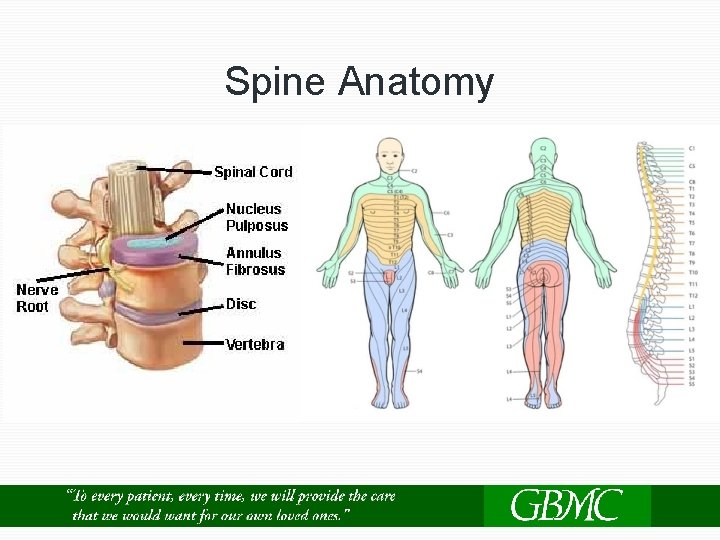
The Spine ØDivided into 3 sections ØCervical spine-7 vertebrae ØThoracic spine-12 vertebrae ØLumbar spine-5 vertebrae
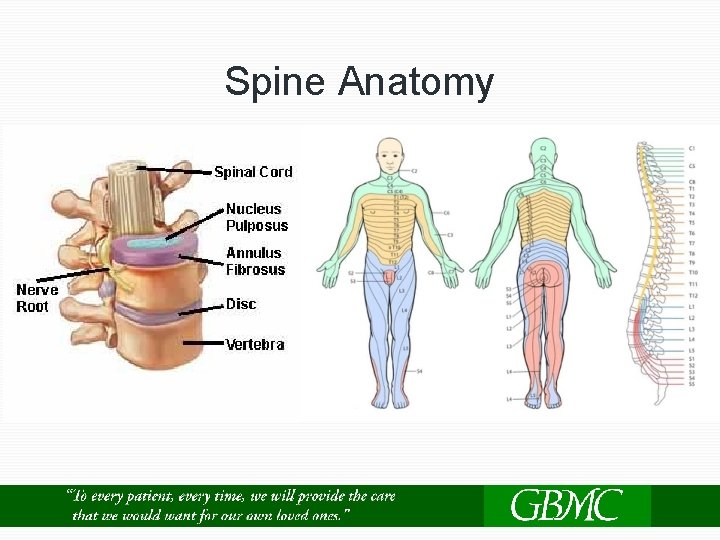
Spine Anatomy
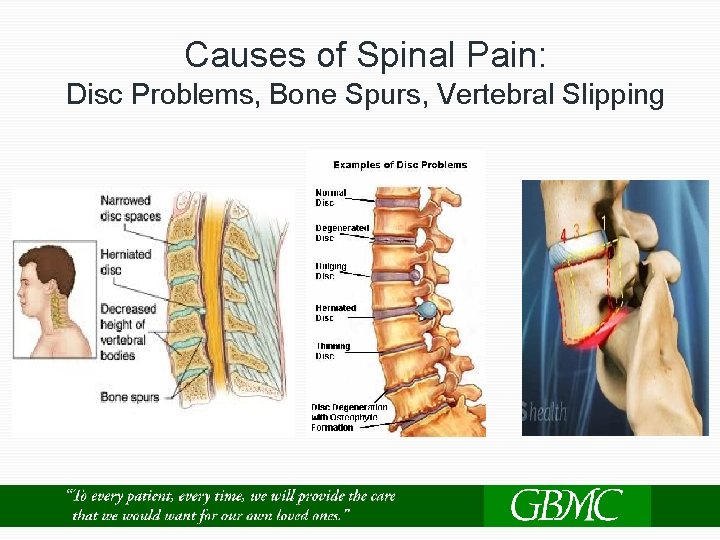
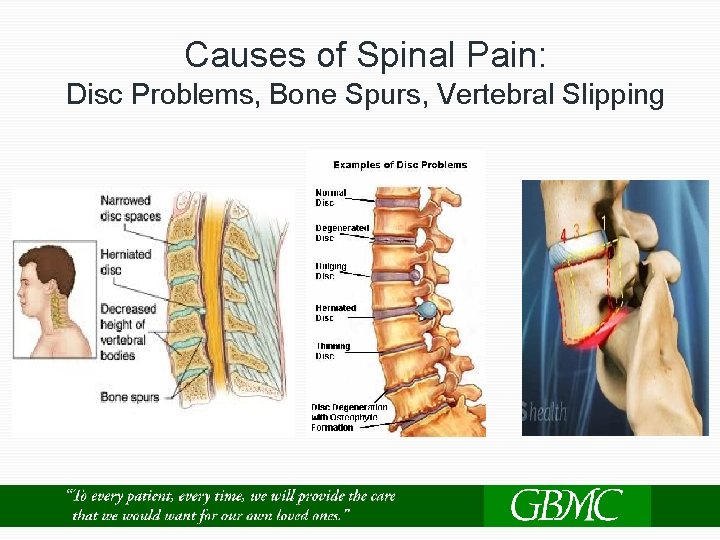
Causes of Spinal Pain: Disc Problems, Bone Spurs, Vertebral Slipping
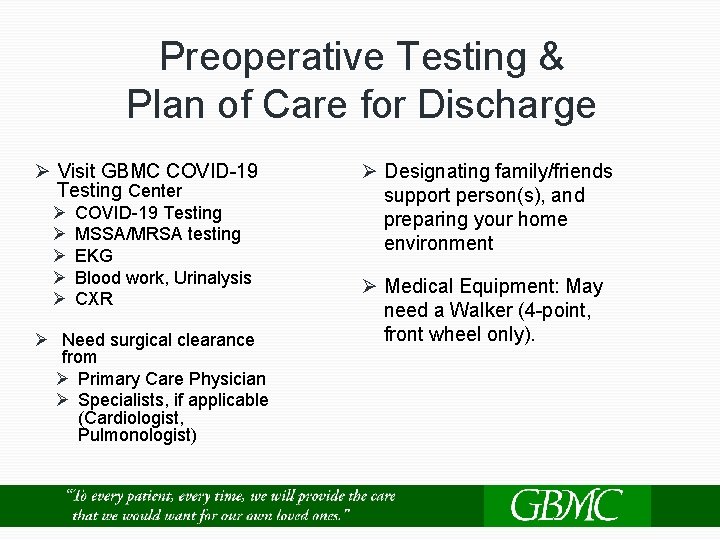
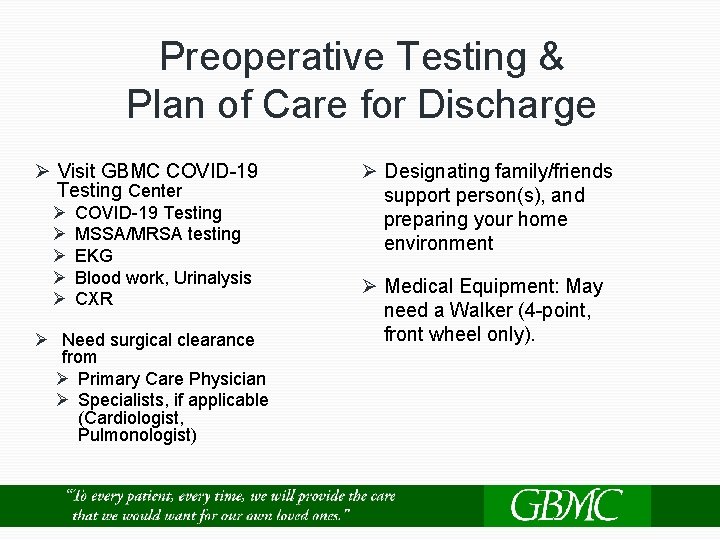
Preoperative Testing & Plan of Care for Discharge Ø Visit GBMC COVID-19 Testing Center Ø Ø Ø COVID-19 Testing MSSA/MRSA testing EKG Blood work, Urinalysis CXR Ø Need surgical clearance from Ø Primary Care Physician Ø Specialists, if applicable (Cardiologist, Pulmonologist) Ø Designating family/friends support person(s), and preparing your home environment Ø Medical Equipment: May need a Walker (4 -point, front wheel only).
COVID-19 Testing Policies Ø Mandatory COVID-19 test must be completed 3 -7 days before your surgery Ø The GBMC Health Partners’ Call Center will call to set up an appointment Ø A positive test result will cause a cancellation of your surgery. Ø It is important to answer any call you receive from GBMC in the days prior to your surgery
COVID-19 Pre-Procedure Requirement After the test Ø Wear a mask Ø Make only necessary trips Ø Medical care Ø Work Ø Maintain appropriate physical distance from others Ø Avoid gatherings of 10 people or more Ø Continue proper handwashing Ø Cover your mouth when you cough and sneeze Ø If possible, avoid sharing personal household items and use a separate bathroom in your home Ø Clean all "high-touch" surfaces every day Ø Call 911 if you have a medical emergency
COVID-19 Pre-Procedure Requirement Notify your surgeon if you have any of the following: Ø Fever ≥ 38. 0 C (100 F) in the last 24 hours Ø New respiratory symptoms Ø Cough Ø Shortness of breath Ø Sore throat Ø Chills Ø Muscle pain Ø New loss of taste or smell
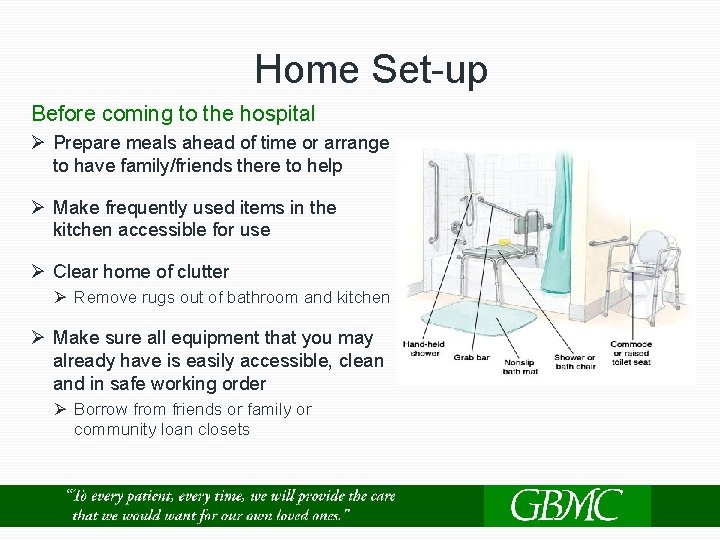
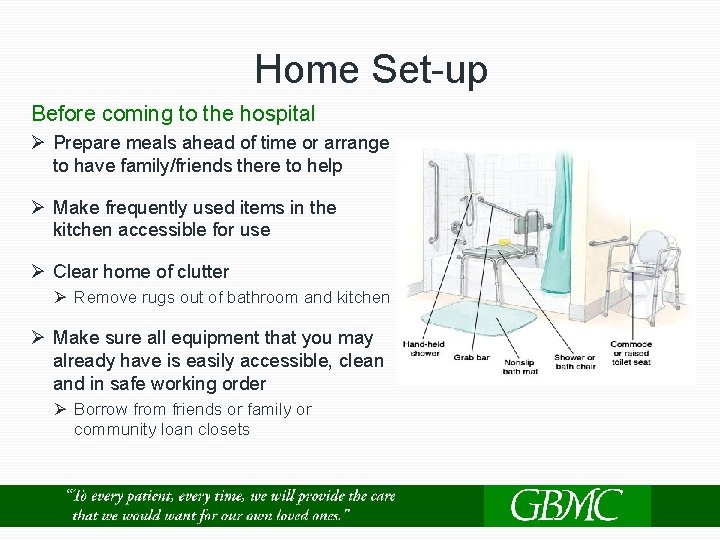
Home Set-up Before coming to the hospital Ø Prepare meals ahead of time or arrange to have family/friends there to help Ø Make frequently used items in the kitchen accessible for use Ø Clear home of clutter Ø Remove rugs out of bathroom and kitchen Ø Make sure all equipment that you may already have is easily accessible, clean and in safe working order Ø Borrow from friends or family or community loan closets
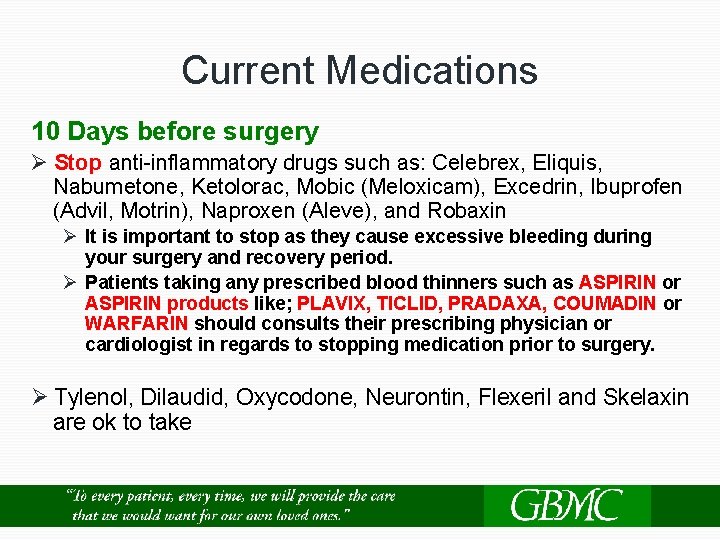
Current Medications 10 Days before surgery Ø Stop anti-inflammatory drugs such as: Celebrex, Eliquis, Nabumetone, Ketolorac, Mobic (Meloxicam), Excedrin, Ibuprofen (Advil, Motrin), Naproxen (Aleve), and Robaxin Ø It is important to stop as they cause excessive bleeding during your surgery and recovery period. Ø Patients taking any prescribed blood thinners such as ASPIRIN or ASPIRIN products like; PLAVIX, TICLID, PRADAXA, COUMADIN or WARFARIN should consults their prescribing physician or cardiologist in regards to stopping medication prior to surgery. Ø Tylenol, Dilaudid, Oxycodone, Neurontin, Flexeril and Skelaxin are ok to take
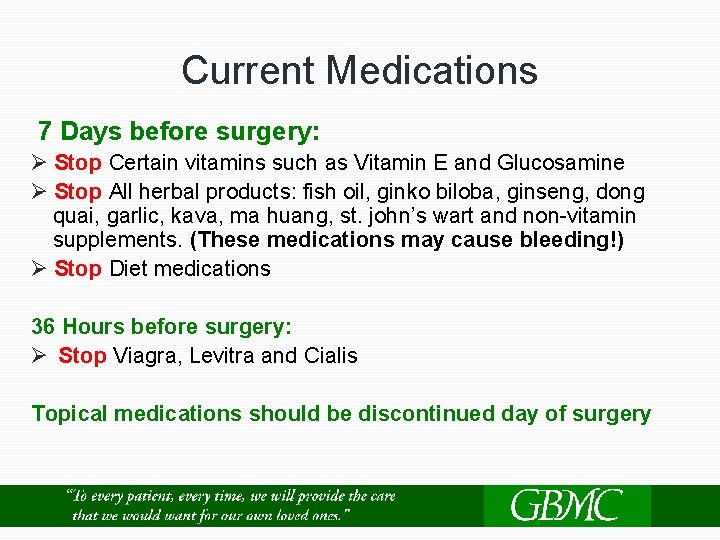
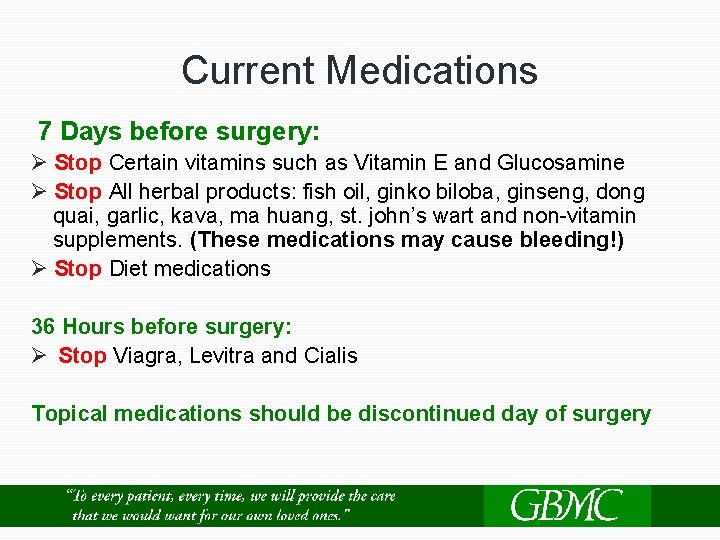
Current Medications 7 Days before surgery: Ø Stop Certain vitamins such as Vitamin E and Glucosamine Ø Stop All herbal products: fish oil, ginko biloba, ginseng, dong quai, garlic, kava, ma huang, st. john’s wart and non-vitamin supplements. (These medications may cause bleeding!) Ø Stop Diet medications 36 Hours before surgery: Ø Stop Viagra, Levitra and Cialis Topical medications should be discontinued day of surgery
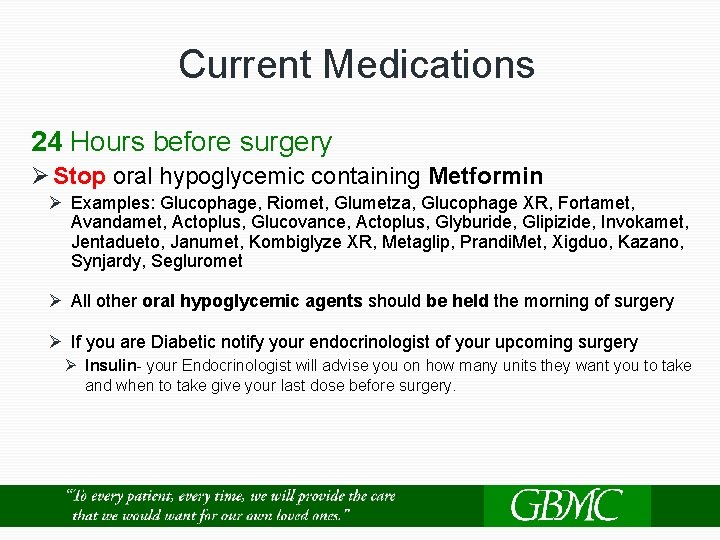
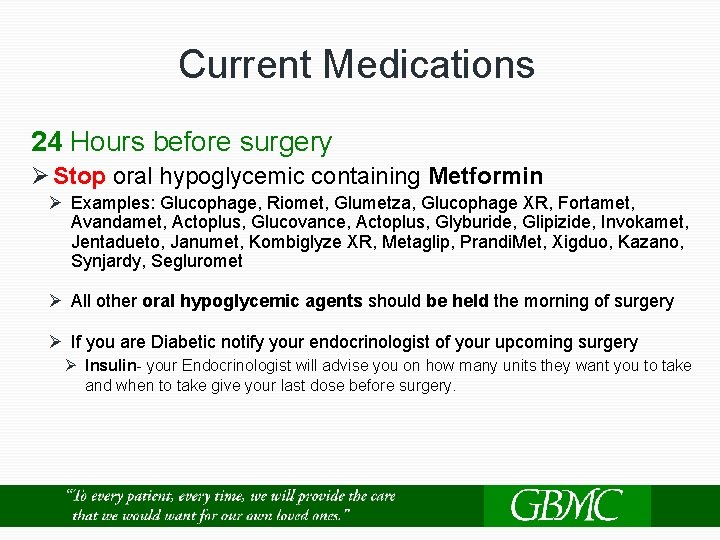
Current Medications 24 Hours before surgery Ø Stop oral hypoglycemic containing Metformin Ø Examples: Glucophage, Riomet, Glumetza, Glucophage XR, Fortamet, Avandamet, Actoplus, Glucovance, Actoplus, Glyburide, Glipizide, Invokamet, Jentadueto, Janumet, Kombiglyze XR, Metaglip, Prandi. Met, Xigduo, Kazano, Synjardy, Segluromet Ø All other oral hypoglycemic agents should be held the morning of surgery Ø If you are Diabetic notify your endocrinologist of your upcoming surgery Ø Insulin- your Endocrinologist will advise you on how many units they want you to take and when to take give your last dose before surgery.
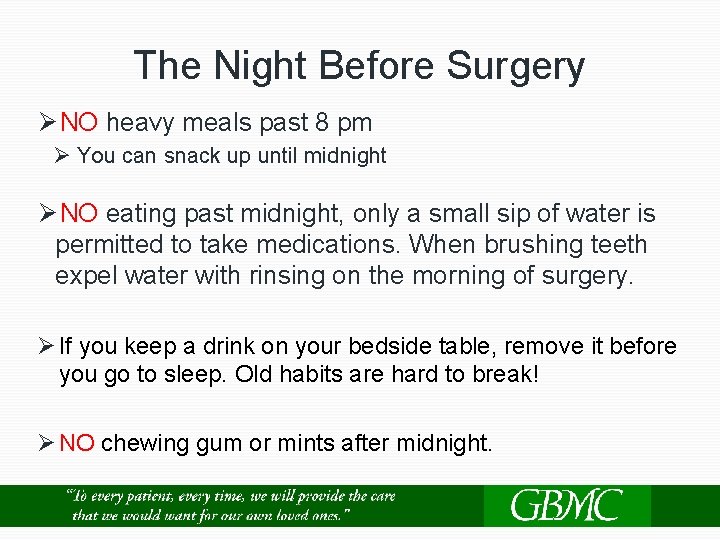
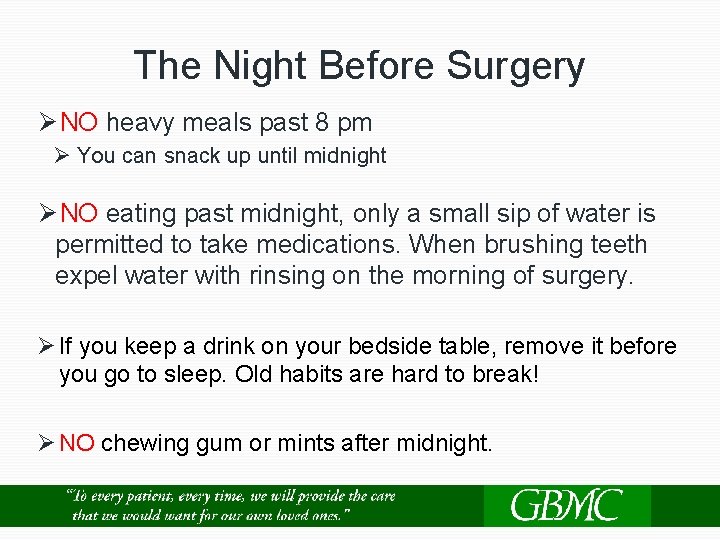
The Night Before Surgery Ø NO heavy meals past 8 pm Ø You can snack up until midnight Ø NO eating past midnight, only a small sip of water is permitted to take medications. When brushing teeth expel water with rinsing on the morning of surgery. Ø If you keep a drink on your bedside table, remove it before you go to sleep. Old habits are hard to break! Ø NO chewing gum or mints after midnight.
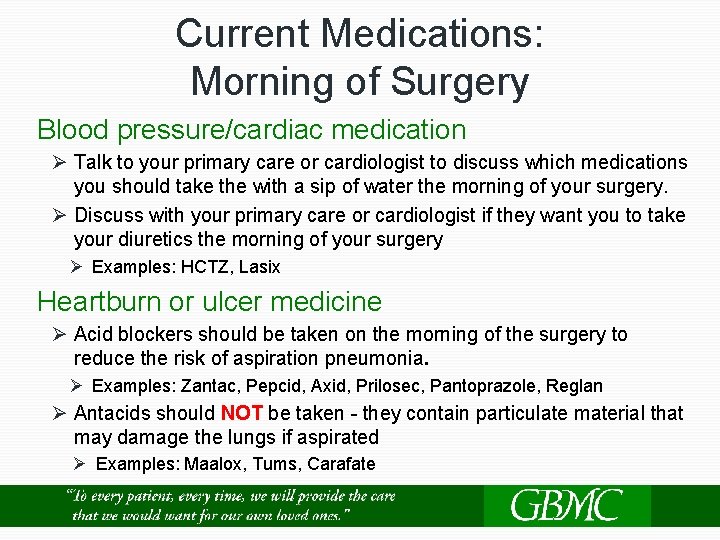
Current Medications: Morning of Surgery Blood pressure/cardiac medication Ø Talk to your primary care or cardiologist to discuss which medications you should take the with a sip of water the morning of your surgery. Ø Discuss with your primary care or cardiologist if they want you to take your diuretics the morning of your surgery Ø Examples: HCTZ, Lasix Heartburn or ulcer medicine Ø Acid blockers should be taken on the morning of the surgery to reduce the risk of aspiration pneumonia. Ø Examples: Zantac, Pepcid, Axid, Prilosec, Pantoprazole, Reglan Ø Antacids should NOT be taken - they contain particulate material that may damage the lungs if aspirated Ø Examples: Maalox, Tums, Carafate
How to Prevent Infection and Complications Ø Control your blood sugar before, during and after your surgery Ø Exercising and healthy weight loss Ø Stop smoking (including ecigarettes and vaping) 2 weeks before surgery Ø Good nutrition with adequate calories and protein Ø Change position frequently Ø Dental exam in the last six months Ø Keep pets are away from the incision site Ø Applying fresh linens to bed before surgery
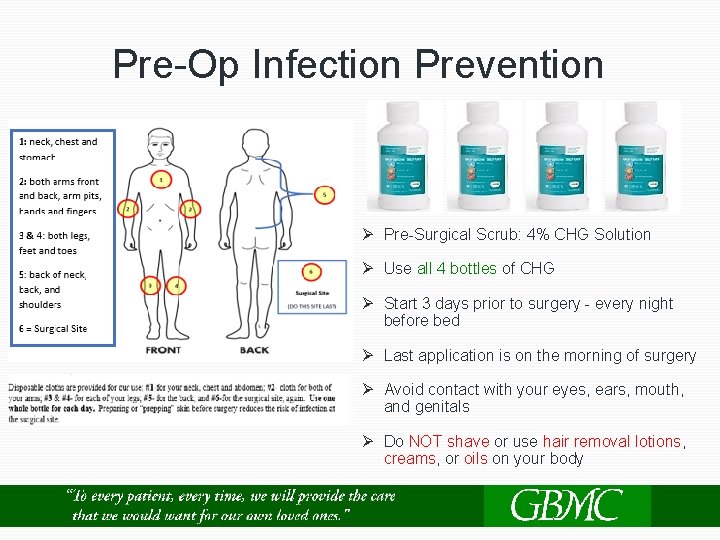
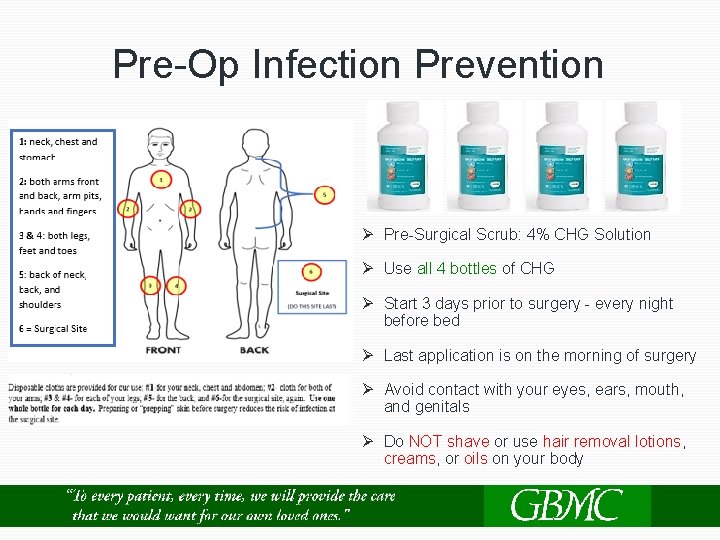
Pre-Op Infection Prevention Ø Pre-Surgical Scrub: 4% CHG Solution Ø Use all 4 bottles of CHG Ø Start 3 days prior to surgery - every night before bed Ø Last application is on the morning of surgery Ø Avoid contact with your eyes, ears, mouth, and genitals Ø Do NOT shave or use hair removal lotions, creams, or oils on your body
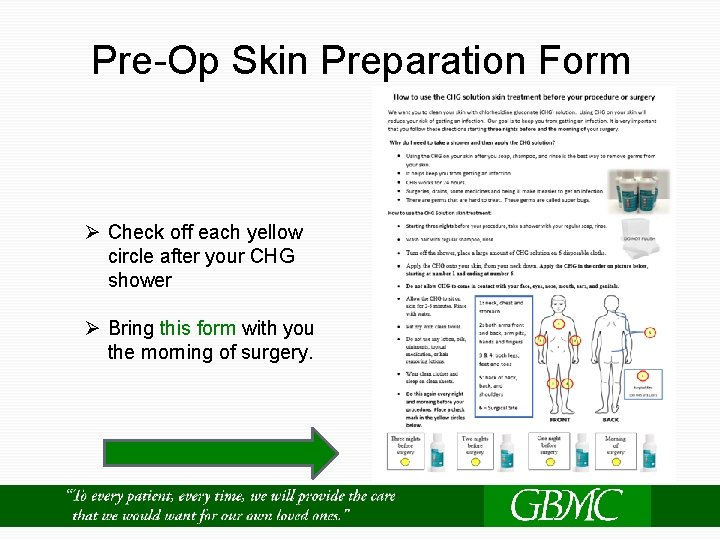
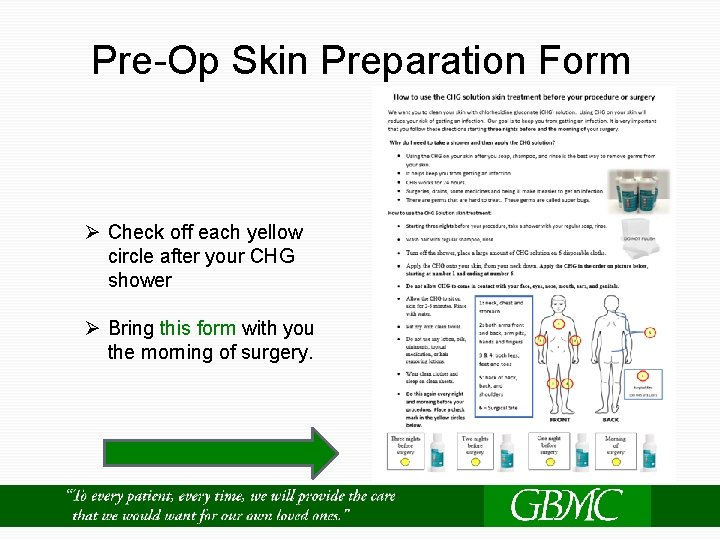
Pre-Op Skin Preparation Form Ø Check off each yellow circle after your CHG shower Ø Bring this form with you the morning of surgery.
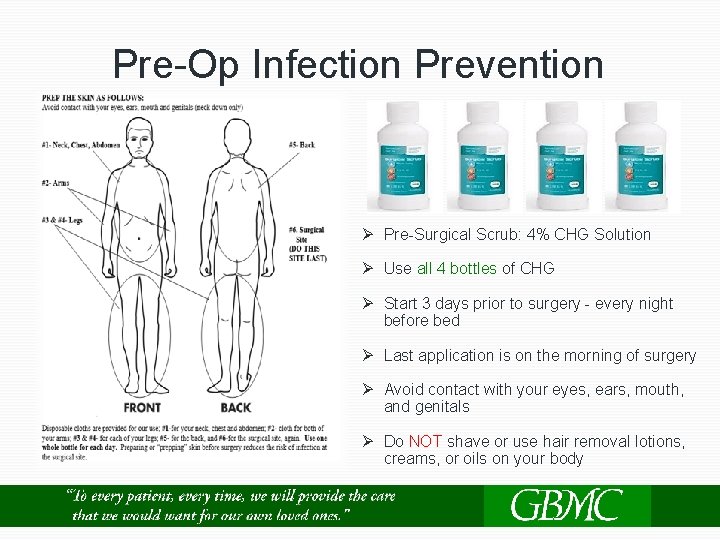
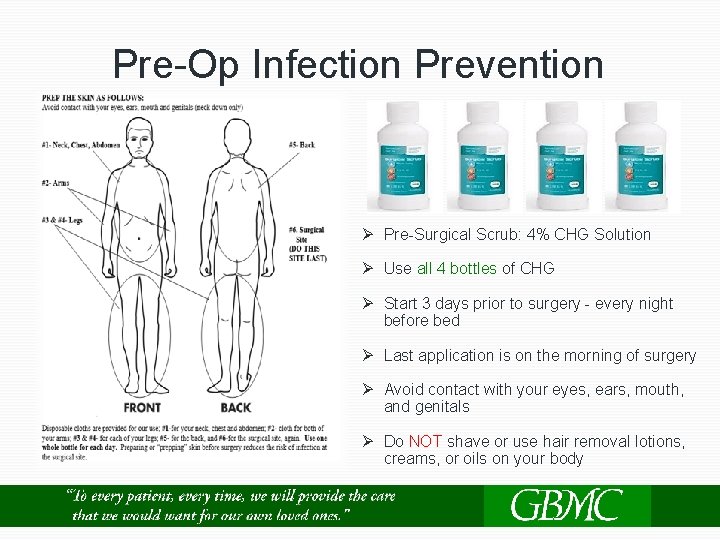
Pre-Op Infection Prevention Ø Pre-Surgical Scrub: 4% CHG Solution Ø Use all 4 bottles of CHG Ø Start 3 days prior to surgery - every night before bed Ø Last application is on the morning of surgery Ø Avoid contact with your eyes, ears, mouth, and genitals Ø Do NOT shave or use hair removal lotions, creams, or oils on your body
What to Bring to the Hospital Ø Your ID card Ø Insurance card Ø Advance directive Ø Preop CHG wash form Ø Bring in glasses, contact lenses, and hearing aids Ø Regular clothing Ø Loose fitting shorts or pants; elastic waist is easiest, under garments Ø Walking shoes with good ankle support (no open heel shoes). Do not buy new shoes - bring something comfortable Ø Any braces, shoe inserts or splints that you normally use Ø CPAP machine (if you have sleep apnea)

Arriving to the Hospital Ø Arrive at the hospital at least 2 hours before your surgery time Ø Park in Lily Garage. Enter Lobby E on the 3 rd floor of main hospital. Take Elevator E to 4 th floor, check in at admission desk
The Pre-operative Area In Pre-Op Ø You will be given a hospital gown to change into Ø Meet your surgical team – surgeon, nurse, anesthesiologist, tech Ø Admission database will be completed Ø Vital signs and IV will be started
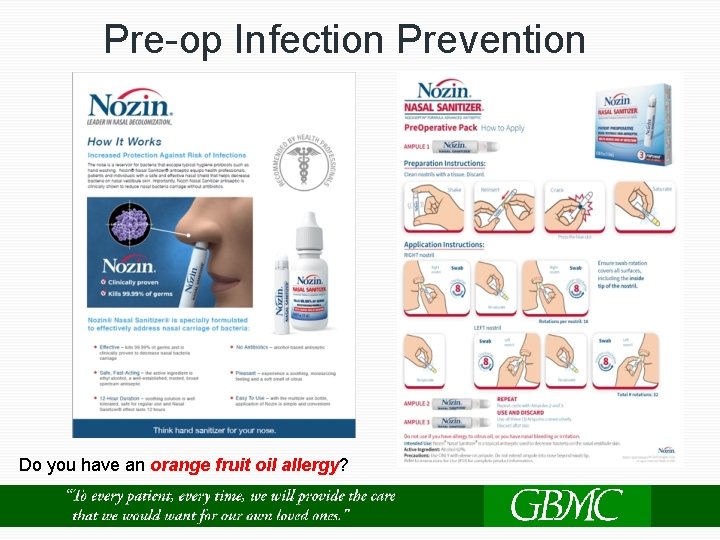
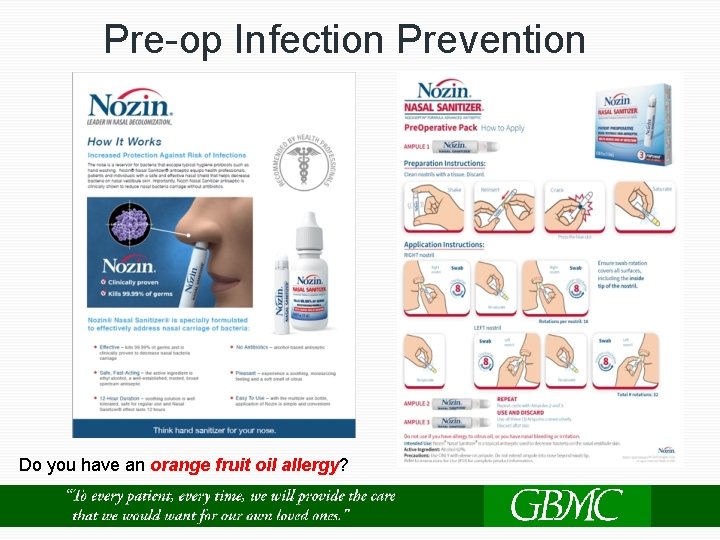
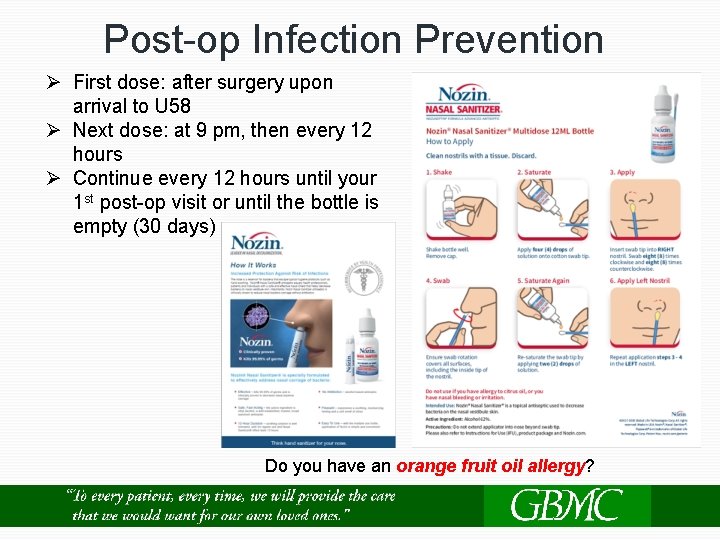
Pre-op Infection Prevention Do you have an orange fruit oil allergy?
After Surgery Recovery Room (PACU) Ø You will wake up and probably feel sleepy Ø Monitor vital signs Ø Manage pain Ø Continuous pulse ox placed on finger to monitor your oxygen level Admission to Unit 58 Ø Once your vital signs are stable, and pain is managed Ø Private room Ø Meet your RN (Registered Nurse) and NST (Nurse Support Tech) Ø Communication Board updated Ø A Welcome Folder
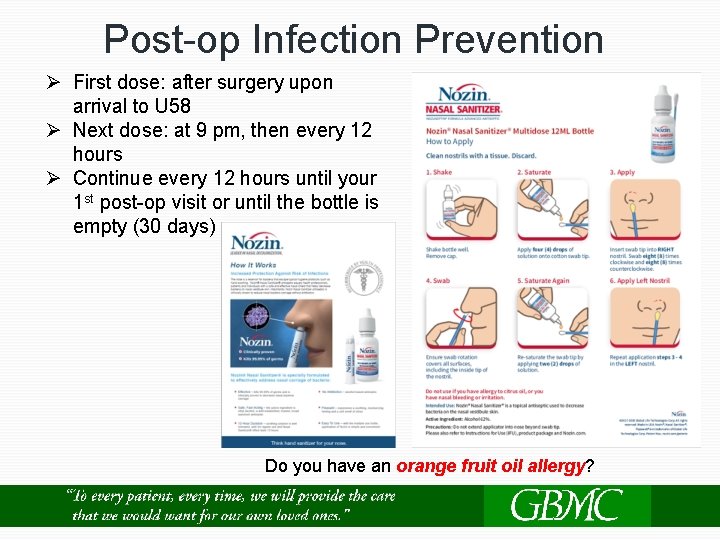
Post-op Infection Prevention Ø First dose: after surgery upon arrival to U 58 Ø Next dose: at 9 pm, then every 12 hours Ø Continue every 12 hours until your 1 st post-op visit or until the bottle is empty (30 days) Do you have an orange fruit oil allergy?
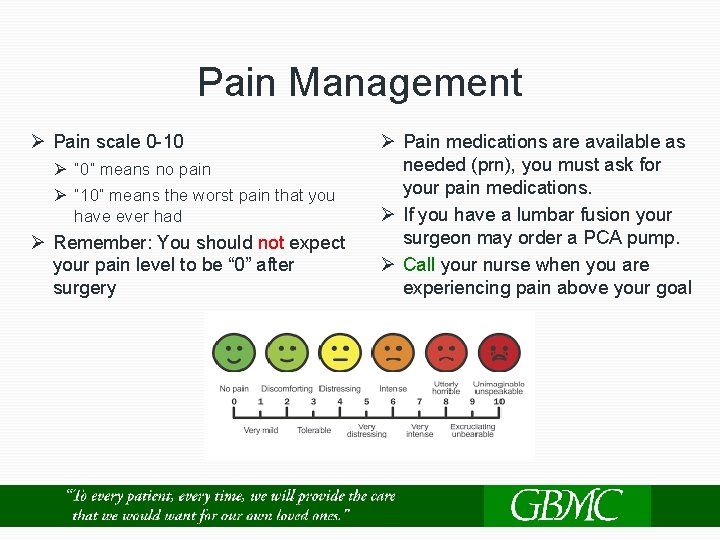
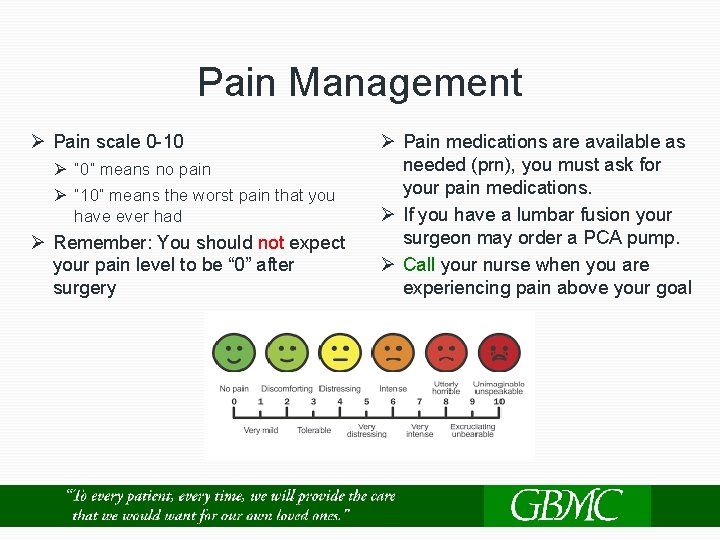
Pain Management Ø Pain scale 0 -10 Ø “ 0” means no pain Ø “ 10” means the worst pain that you have ever had Ø Remember: You should not expect your pain level to be “ 0” after surgery Ø Pain medications are available as needed (prn), you must ask for your pain medications. Ø If you have a lumbar fusion your surgeon may order a PCA pump. Ø Call your nurse when you are experiencing pain above your goal
Equipment Ø Urinary catheter Ø Sequential compression device (SCD) Ø Oxygen Ø Pulse oximetry Ø Incentive Spirometry (IS) Ø Drains: Jackson Pratt (JP) or Hemovac Ø Abdominal Binder Ø Brace or collar
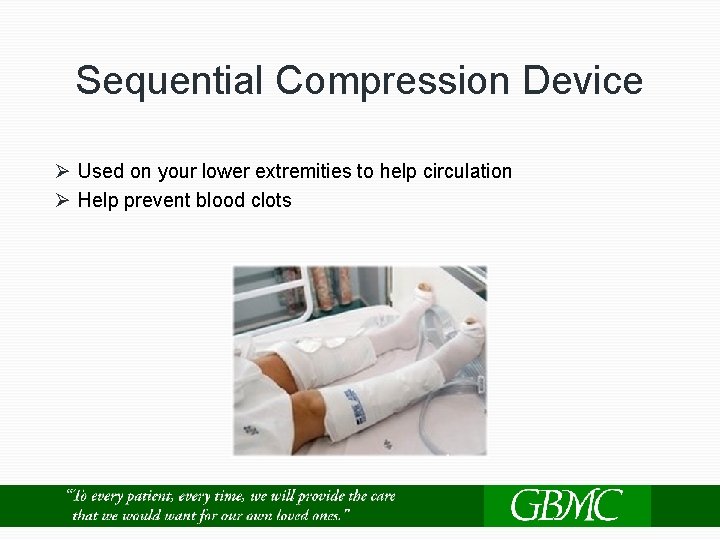
Sequential Compression Device Ø Used on your lower extremities to help circulation Ø Help prevent blood clots
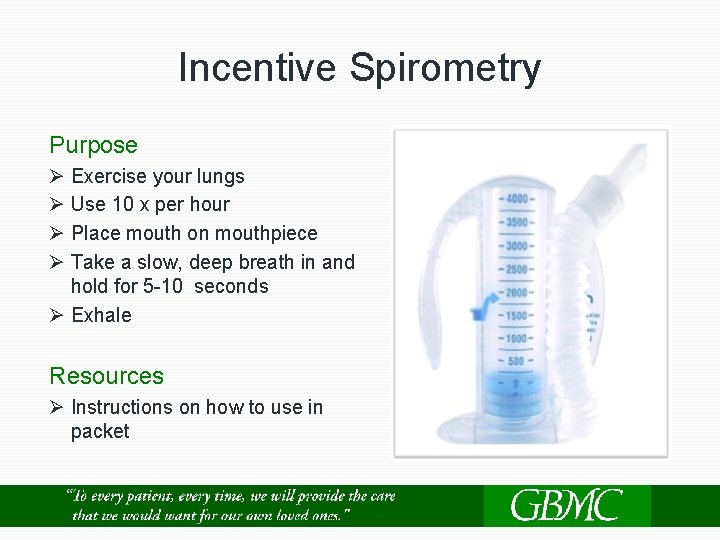
Incentive Spirometry Purpose Ø Exercise your lungs Ø Use 10 x per hour Ø Place mouth on mouthpiece Ø Take a slow, deep breath in and hold for 5 -10 seconds Ø Exhale Resources Ø Instructions on how to use in packet
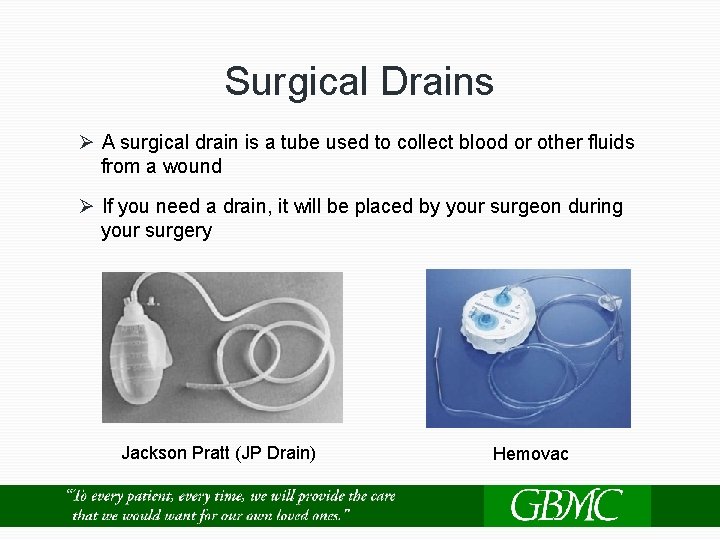
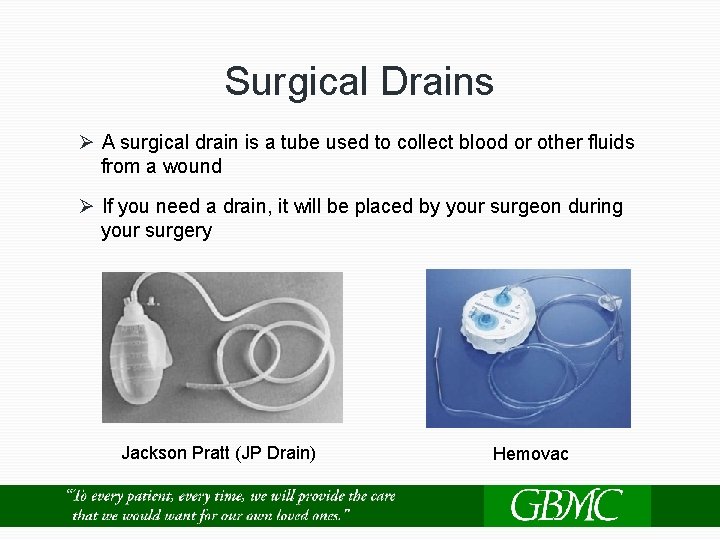
Surgical Drains Ø A surgical drain is a tube used to collect blood or other fluids from a wound Ø If you need a drain, it will be placed by your surgeon during your surgery Jackson Pratt (JP Drain) Hemovac
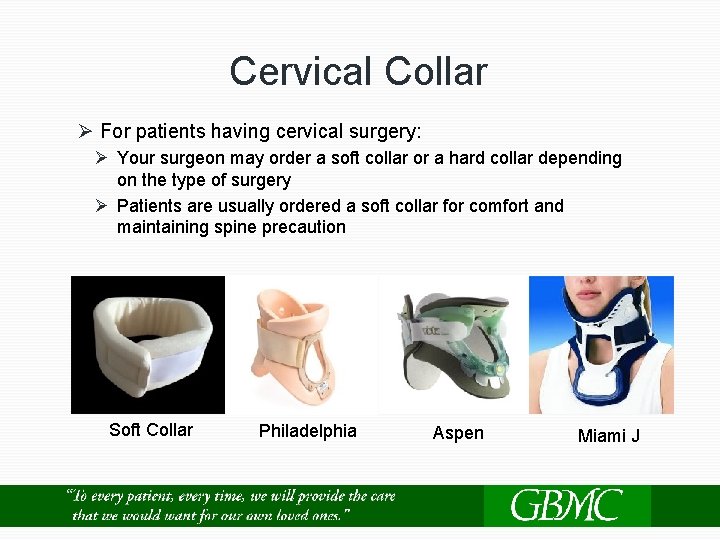
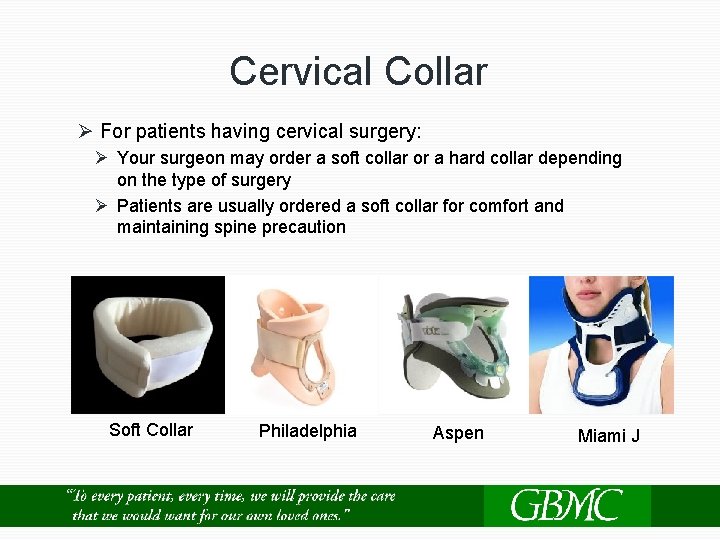
Cervical Collar Ø For patients having cervical surgery: Ø Your surgeon may order a soft collar or a hard collar depending on the type of surgery Ø Patients are usually ordered a soft collar for comfort and maintaining spine precaution Soft Collar Philadelphia Aspen Miami J
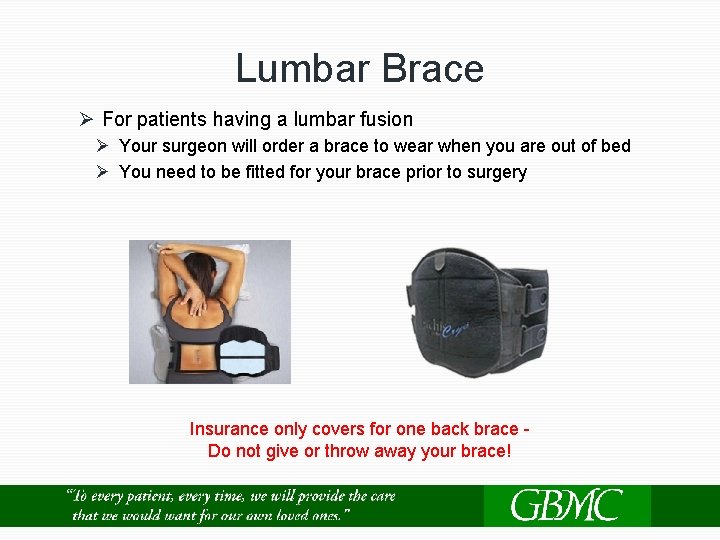
Lumbar Brace Ø For patients having a lumbar fusion Ø Your surgeon will order a brace to wear when you are out of bed Ø You need to be fitted for your brace prior to surgery Insurance only covers for one back brace - Do not give or throw away your brace!
Fall Risk Ø Red non-skid socks will be placed on you, signaling that you are at a high risk for experiencing a fall Ø Do NOT get up without the help of staff assisting you. Ø Use your call bell
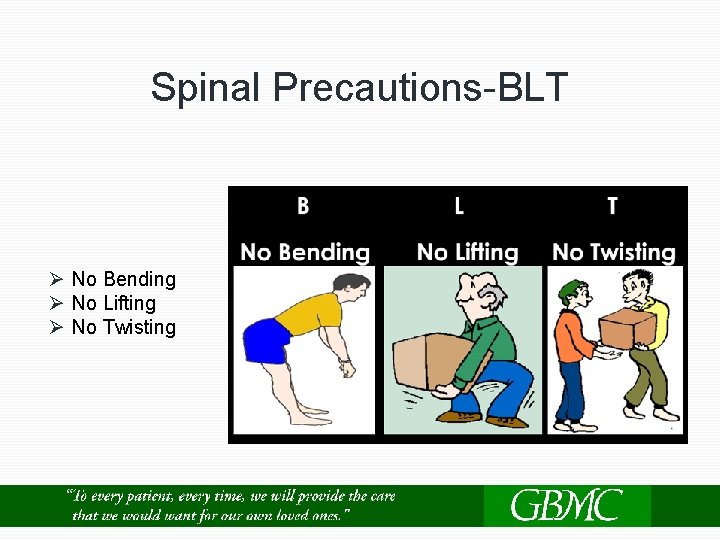
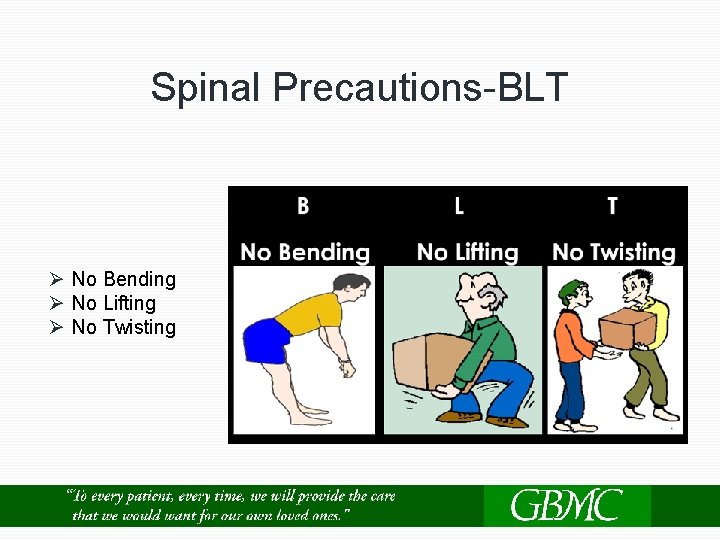
Spinal Precautions-BLT Ø No Bending Ø No Lifting Ø No Twisting
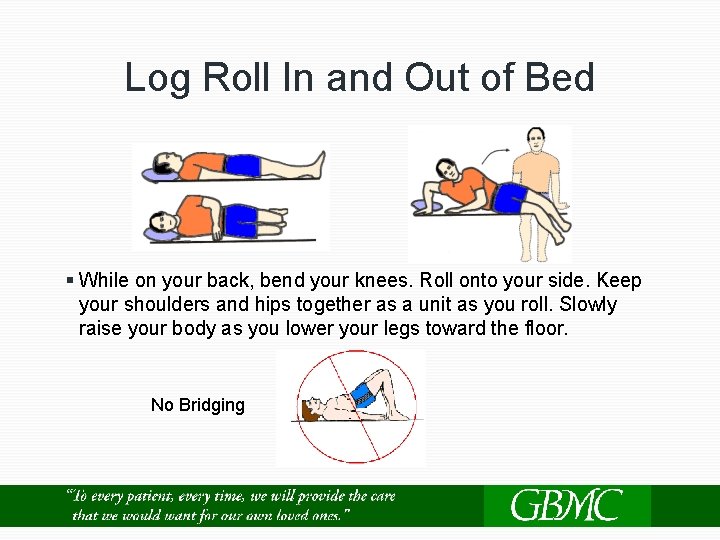
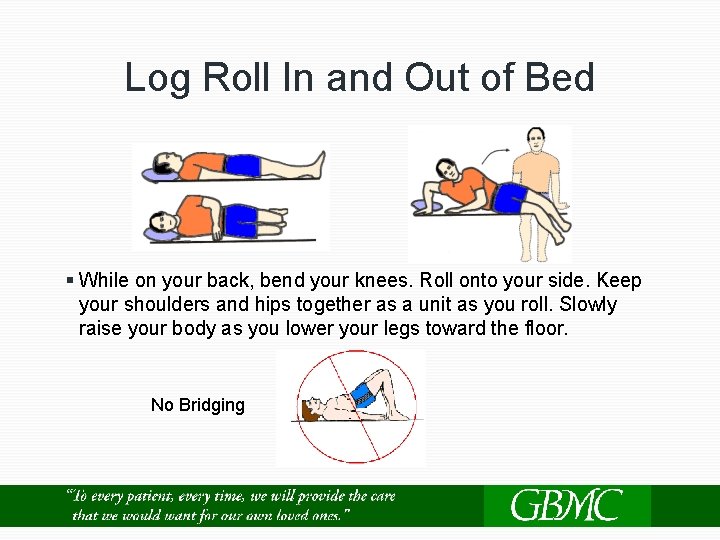
Log Roll In and Out of Bed § While on your back, bend your knees. Roll onto your side. Keep your shoulders and hips together as a unit as you roll. Slowly raise your body as you lower your legs toward the floor. No Bridging
What to Expect in the Hospital Post-op day 1 Ø If you have a urinary catheter, it will be discontinued Ø If you have a PCA, it will be discontinued and oral pain medication will be started Ø You will be evaluated by physical therapy (PT) and occupational therapy (OT) Ø You will have one individual therapy session every day starting the morning after your surgery Post-op days 2 & 3 Ø More therapy - walking in halls and going to the gym to practice getting in and out of the tub/shower, in and out of the car, and going up and down stairs Ø If you have a drain, it will be discontinued depending on the amount of drainage
Rehabilitation: PT versus OT Physical Therapy – helps you Occupational Therapy – helps with functional mobility you with functional activities of daily living (ADL) Ø Walking Ø Getting in/out of bed Ø Transfers into/out of a chair Ø Going up/down steps Ø Doing your exercise program Ø Getting dressed and bathed Ø Getting in/out of tub/shower Ø Using the toilet Ø Car transfers Ø How to use adaptive equipment if needed Ø Getting items out of refrigerator/cabinets

Medical Equipment Needs Raised toilet seats, bedside commodes, and toilet seat frames Ø Raise the height of your toilet Bedside commode Ø Can be used next to your bed Ø Can be used as a shower chair for your walk in shower Raised Toilet Seat Toilet Safety Frame Bedside Commode Tub/Shower Chair Tub Seat/Shower Chair Ø Decreases the risk of falls in the shower or tub Ø Allows you to safely sit while showering if you have pain or dizziness Ø Shower doors on bathtubs may need to be removed

Medical Equipment Needs ge n o n Lo he r ea c R ed l nd Sp a H g n c o S id a k Lo ng S or h e ho
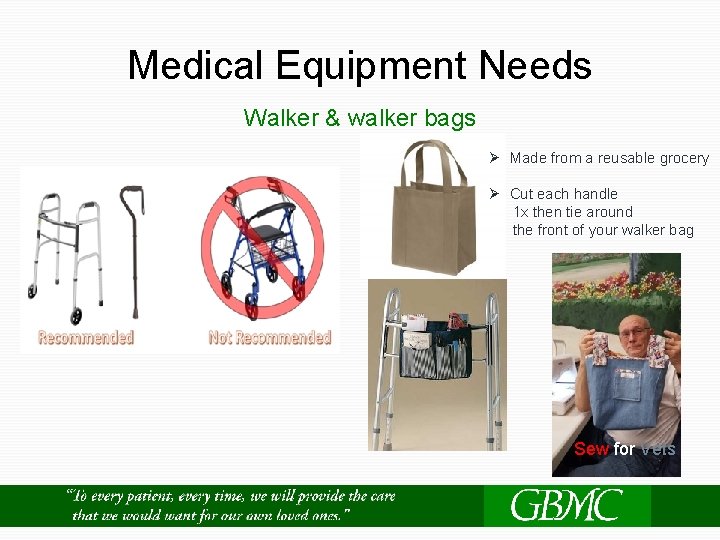
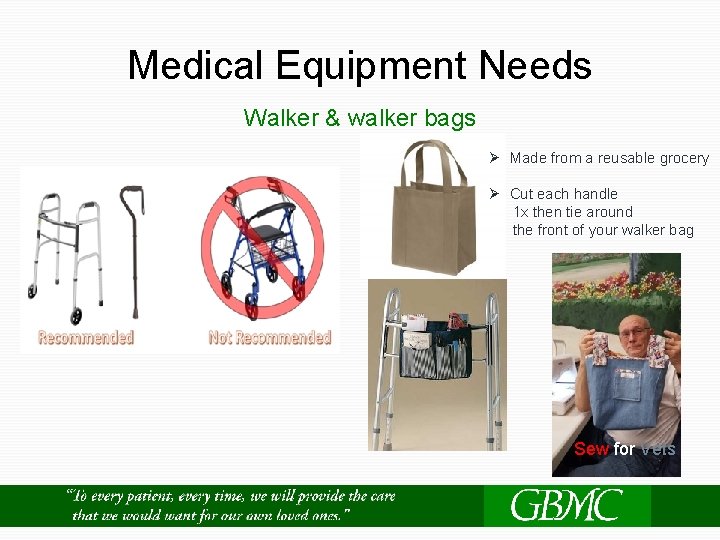
Medical Equipment Needs Walker & walker bags Ø Made from a reusable grocery Ø Cut each handle 1 x then tie around the front of your walker bag Sew for Vets
Case Management The Case Manager on Unit 58 will visit you the day after your surgery to continue working on your discharge planning needs Ø Home with Out-Patient Therapy Ø Home with Home Physical Therapy Ø Skilled Nursing Facility (SNF) Ø Equipment for home Ø Offering resources
Medical Orders for Life-Sustaining Treatment (MOLST) MOLST Ø Portable medical order form covering options for cardiopulmonary resuscitation and other life-sustaining treatments Ø Does not expire Ø Medical orders are based on a patient’s wishes about medical treatments Ø The advance practitioner or surgeon will have the paperwork. Ø Are not Advance Directives Ø All patients that are transferred to another facility will require a MOLST form prior to EMS transport
Discharge Day Ø Pt will need to clear you for discharge Ø You will need to know your spinal precautions. Ø OT will teach you how to get in and out of the car maintaining your spinal precautions.
Preventing COVID-19 After Surgery While in the hospital Ø Wear your mask whenever leaving your hospital room for therapy or any diagnostic tests Ø Wash your hands often When you get home Ø Wash hands often, Ø Cover your cough and sneeze Ø Wear a mask in public areas Ø Minimize going out into public areas Ø Avoid traveling Ø Avoid sick people
Average Length of Hospital Stay Ø Cervical Fusion: Anterior approach (from the front), 23 hour stay Ø Cervical Fusion: Posterior approach (from the back), 2 days Ø Lumbar Fusion: 2 -3 night stay YOU WILL NEED SOMEONE TO DRIVE YOU HOME WHEN YOU ARE RELEASED FOLLOWING SURGERY!
General Post-Op Care Ø Allow approximately 6 weeks for lumbar surgery and 4 weeks for cervical surgery for healing. Ø Walking is the only exercise encouraged. Ø No lifting anything over 8 -10 lbs. Ø Minimize the use of stair and cars. Ø No driving until you are seen for your 6 week post-op visit, unless otherwise instructed. Ø You will be sent home with prescriptions for pain medication. If you need a refill, call the office 3 days in advance. Prescriptions will not be addressed on weekends or after hours. Ø The Maryland Department of Health & Mental Hygiene, you will be prescribed an opioid antidote called Naloxone (Narcan) in the event of an overdose.
General Post-Op Care Ø Notify the office if weakness, numbness, or pain worsens Ø Notify the surgeon if you have trouble swallowing, swelling/mass, increase hoarseness to your voice Ø Notify the office for a temperature above 100. 5 Ø Schedule your post-op visit 7 -14 days after surgery for a wound check for suture/staple removal Ø
Wound Care Ø Keep wound clean and dry. Ø If you have steri-strips, they will fall off on their own. Ø You may take a shower, if your incision is not draining. Do not scrub the incision. Dry area completely after showering. NO tub bathing for at least 4 weeks after surgery. Ø Do not use lotions or moisturizes on your incision. Ø Do not manipulate (pick or probe) your incision in any way. Ø Notify the office immediately for any drainage, redness, tenderness, swelling.
Wound Care Ø A simple visual check should be all that is needed each day Ø Change dressing per your surgeon's instructions. Ø Keep incision out of direct sunlight. Ø Do not actively clean your incision unless you are specifically instructed to do so.

Preventing Surgical Site Infection Ø Use CHG with daily showers. Use 1 Ø Nozin: Continue every 12 hours until bottle each day for 5 days, for any your 1 st post-op visit or until the bottle is concerns check with your surgeon if you empty (30 days) need to use this past this point.
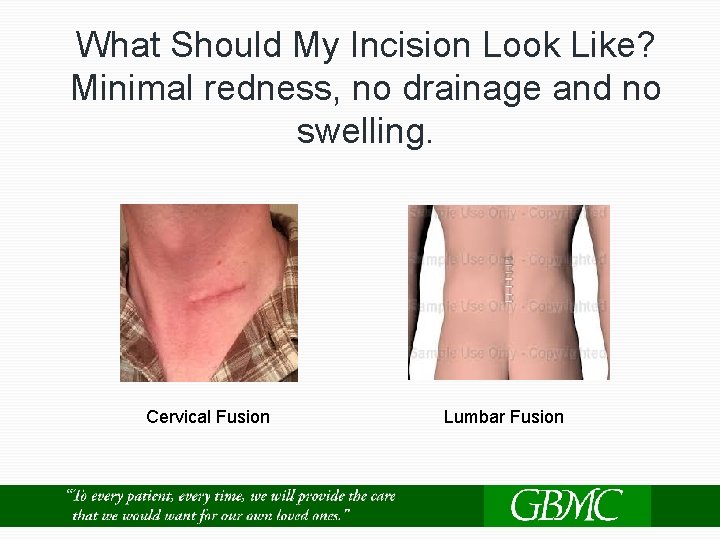
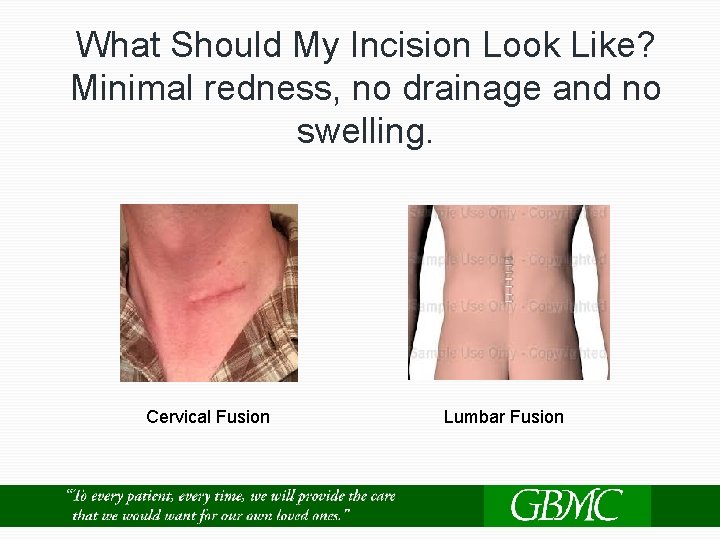
What Should My Incision Look Like? Minimal redness, no drainage and no swelling. Cervical Fusion Lumbar Fusion

What Should My Incision NOT Look Like? Swelling, spreading redness, warm, and tender.

What Should My Incision Not Look Like? Do not let your waist band rub across your incision!
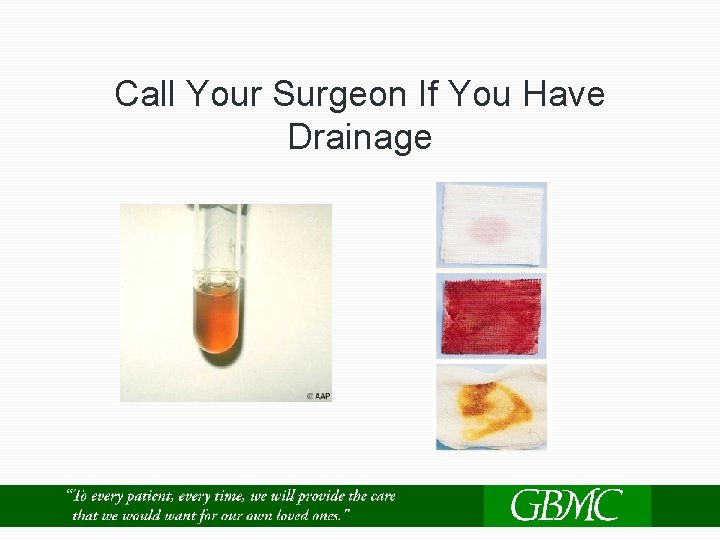
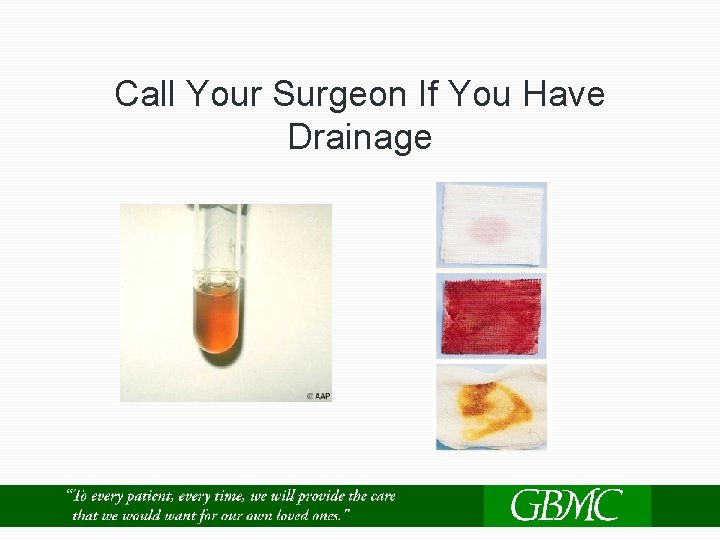
Call Your Surgeon If You Have Drainage

Thank you for choosing GBMC for your Spine Surgery! Joint and Spine Center 6701 N Charles St Towson, MD 21204 Phone: 443 -849 -6261 Email: jointspinecenter@gbmc. org Website: www. gbmc. org/Jointand. Spine "To every patient, every time, we will provide the care